Statistics for dissociative identity disorder
Dissociative Identity Disorder - StatPearls
Continuing Education Activity
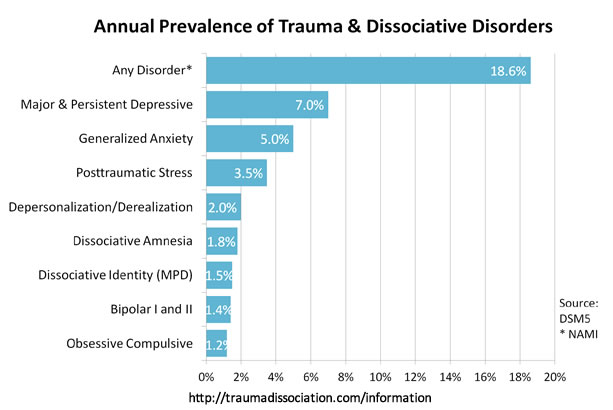
Dissociative identity disorder (DID) is a rare psychiatric disorder diagnosed in about 1.5% of the global population. This disorder is often misdiagnosed and often requires multiple assessments for an accurate diagnosis. Patients often present with self-injurious behavior and suicide attempts. This activity reviews the evaluation and treatment of dissociative identity disorder and explains the role of an interprofessional team in caring for patients diagnosed with dissociative identity disorder (DID). This activity also reviews the association between DID and suicidal behavior.
Objectives:
Describe the constellation of behavioral symptoms that lead to a diagnosis of dissociative identity disorder.
Review risk factors for the development of a diagnosis of dissociative identity disorder.
Explain the different modalities of evidence-based treatment for dissociative identity disorder.
Outline some interprofessional strategies that can improve patient outcomes in patients with dissociative identity disorder.
Access free multiple choice questions on this topic.
Introduction
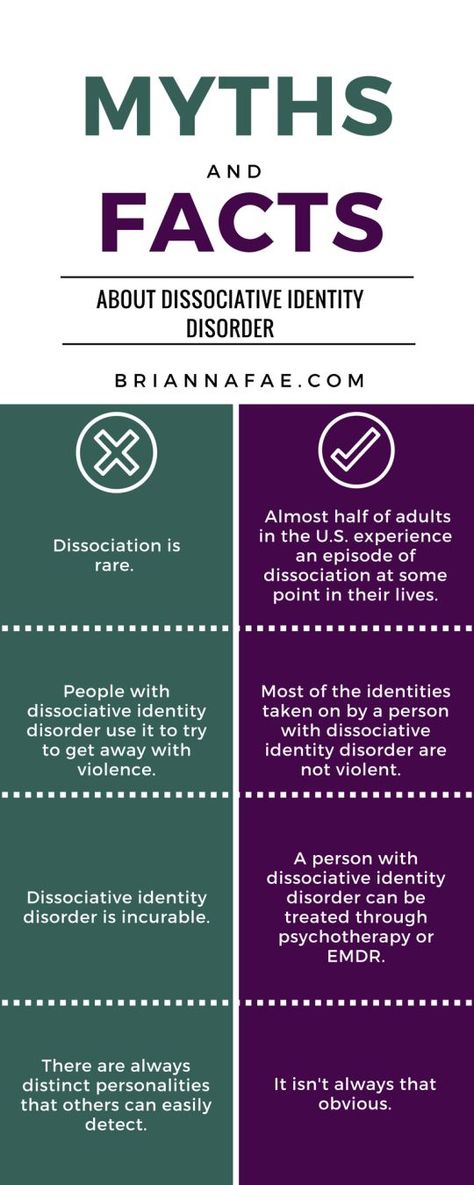
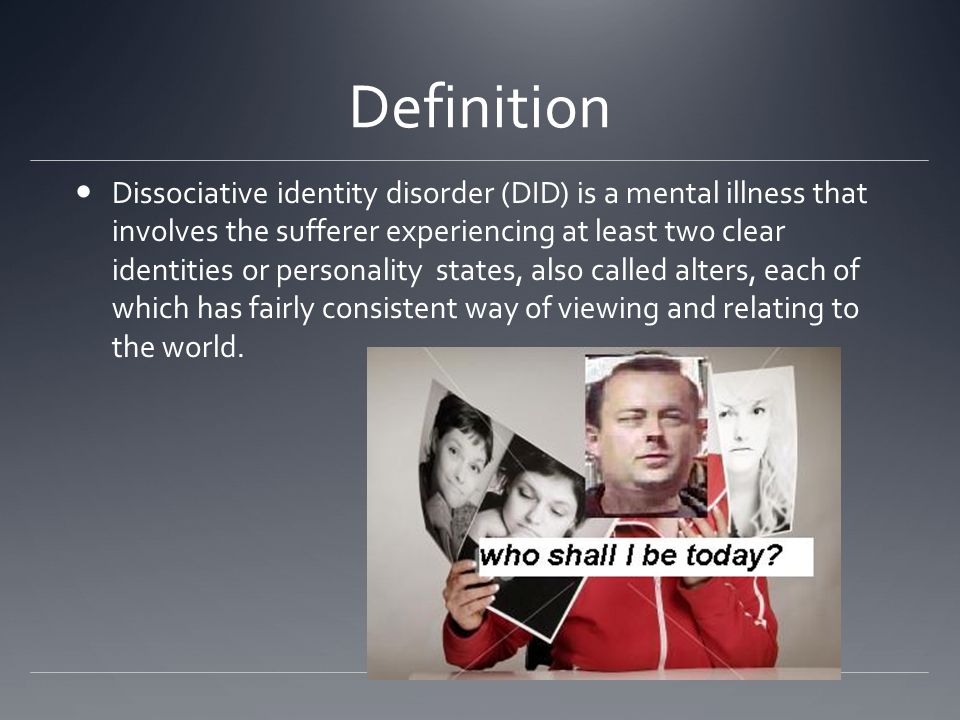
Dissociative identity disorder (DID) is a rare disorder associated with severe behavioral health symptoms. DID was previously known as Multiple Personality Disorder until 1994. Approximately 1.5% of the population internationally has been diagnosed with a dissociative identity disorder.[1] Often patients with this diagnosis have several emergency presentations, often with self-injurious behavior and even substance use.[2]
Of note, DID has been observed and described in several countries and has been associated with terms such as "outer world possession" and "possession by demons."[3] Several case reports have been described with those terms; however, trauma and its association came with DID much later.
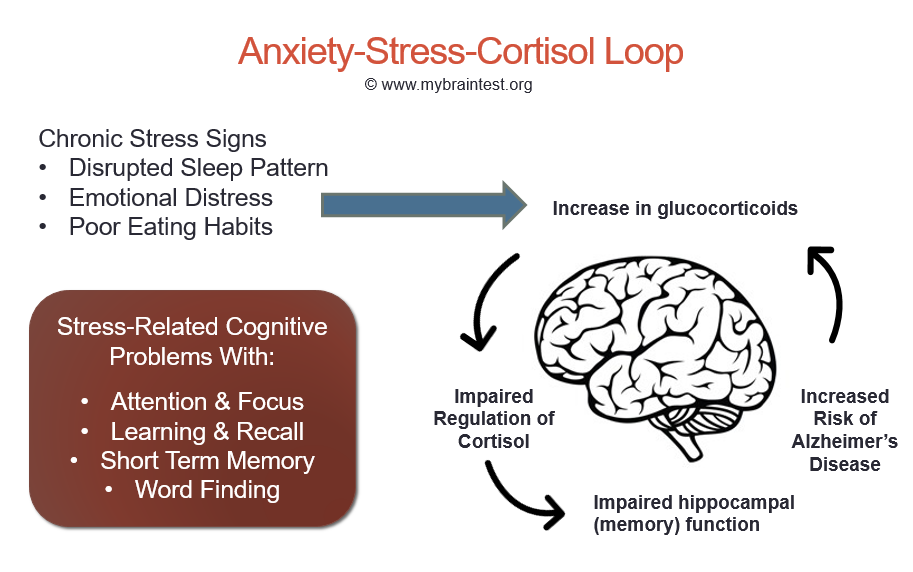
Etiology
Dissociative identity disorder is typically associated with severe childhood trauma and abuse.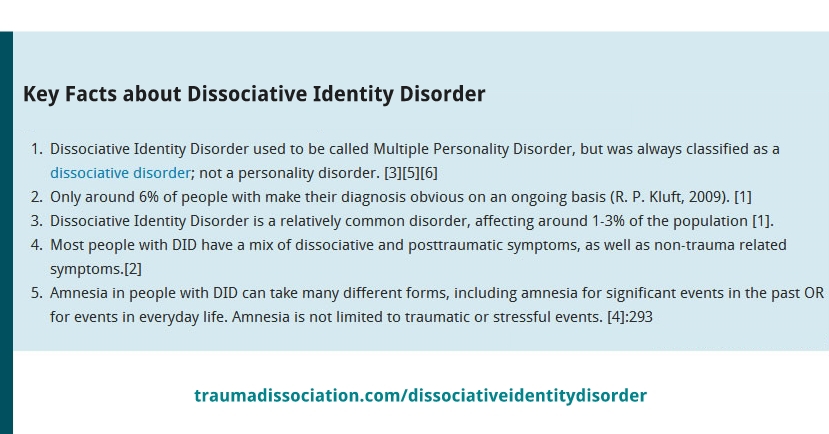 [4] Dalenberg and his team have detailed the role of trauma in the development of dissociative disorder and dismissed the previous model, which was based on fantasy and often associated with suggestibility, cognitive distortions, and fantasy. However, newer research tends to describe a combination of both severe traumas (which may be in any form-physical/emotional/sexual)as well as some effects of cognitive suggestion. Stress experienced by an individual secondary to trauma has been seen to be contributory toward the formation of an accurate understanding of the trauma being unreal, even posttraumatic dissociation such as leaving one's body, etc., and poor sleep. However, in the fantasy theory-it has been seen that people with high levels of vulnerability, predisposition of psychological symptoms, media influences, and likely social isolation and vulnerability.[5]
[4] Dalenberg and his team have detailed the role of trauma in the development of dissociative disorder and dismissed the previous model, which was based on fantasy and often associated with suggestibility, cognitive distortions, and fantasy. However, newer research tends to describe a combination of both severe traumas (which may be in any form-physical/emotional/sexual)as well as some effects of cognitive suggestion. Stress experienced by an individual secondary to trauma has been seen to be contributory toward the formation of an accurate understanding of the trauma being unreal, even posttraumatic dissociation such as leaving one's body, etc., and poor sleep. However, in the fantasy theory-it has been seen that people with high levels of vulnerability, predisposition of psychological symptoms, media influences, and likely social isolation and vulnerability.[5]
Several prominent psychologists such as Kluft have broken down the theory behind DID-in-sum. The theory describes predisposing factors for dissociation, which include an ability to dissociate, overwhelming traumatic experiences that distort reality, creation of alters with specific names and identities, and lack of external stability, which leads to the child's self-soothing to tolerate these stressors.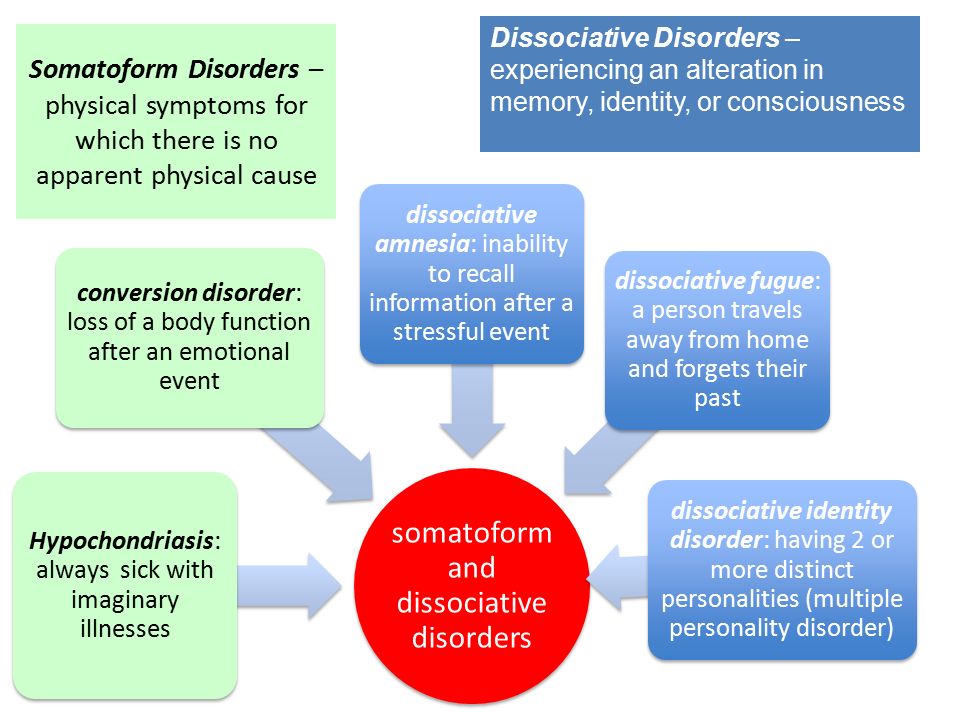 These four factors must be present for DID to develop.[6]
These four factors must be present for DID to develop.[6]
Epidemiology
Dissociative disorders show a prevalence of 1% to 5% in the international population. Severe dissociative identity disorder is present in 1% to 1.5% of this population. Patients may spend up to 5 to 12.5 years in treatment before being diagnosed with a dissociative identity disorder.[7] Patients with DID come with increased rates of non-suicidal self-injurious behavior and suicide attempts.[8]
Pathophysiology
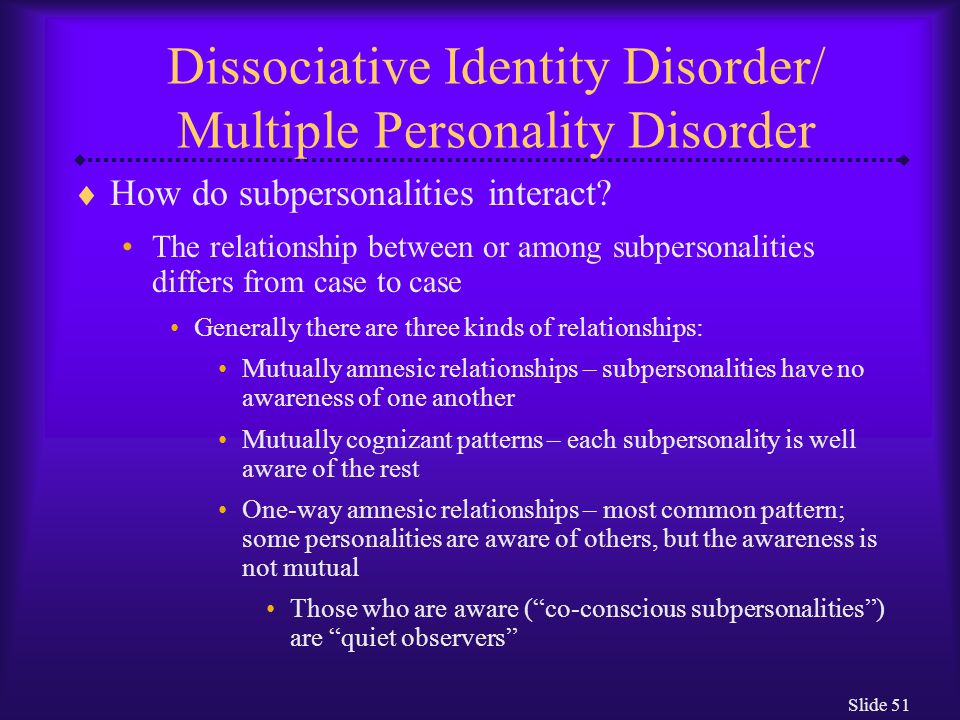
The DID person, per the International Society for the Study of Trauma and Dissociation, is described as a person who experiences separate identities that function independently of each other and are autonomous of each other. The International Society describes alternate identities or alters as independent identities which have their own distinct behaviors, have memories that are distinct from others, and even may differ in language and expressions used. Signs of a switch to an altered state include trance-like behavior, eye blinking, eye-rolling, and changes in posture.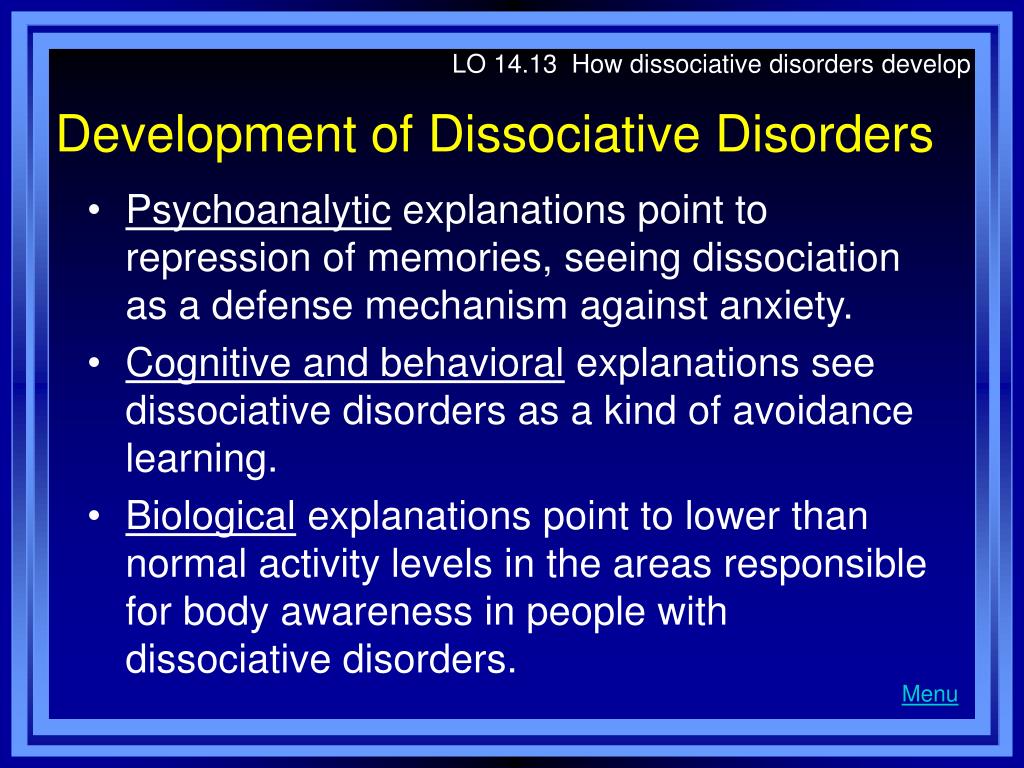
The major hypothesis by Putnam et al. is that “alternate identities result from the inability of many traumatized children to develop a unified sense of self that is maintained across various behavioral states, particularly if the traumatic exposure first occurs before the age of 5 “.[9] The theories have been studied by groups in the inpatient unit services in the 1990s.
History and Physical
The way to diagnose dissociative identity disorder is via detailed history taken by both psychiatric practitioners and experienced psychologists. Often persons with DID are misdiagnosed with other personality disorders, most commonly borderline personality disorder, as elements of dissociation are prominently seen and even amnesia. Often longitudinal assessments over long periods and careful history taking are required to complete diagnostic evaluations. History is often gathered from multiple sources as well. Often neurological examinations are required as well to rule out autoimmune encephalitis, often requiring electroencephalograms, lumbar punctures, and brain imaging.
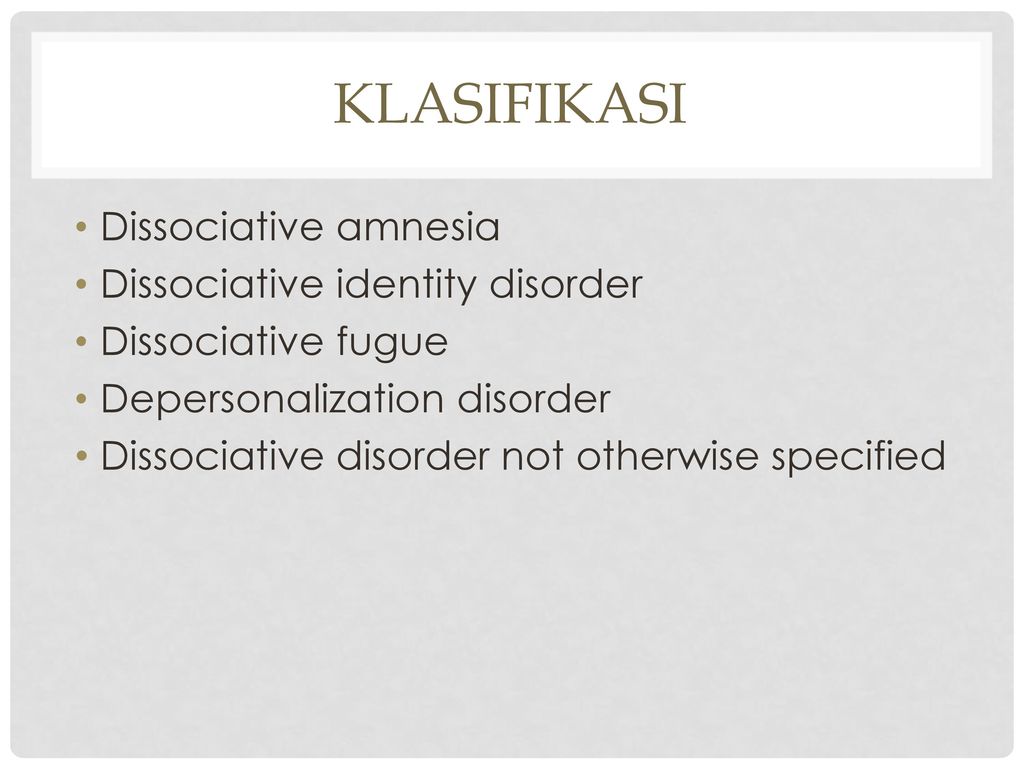
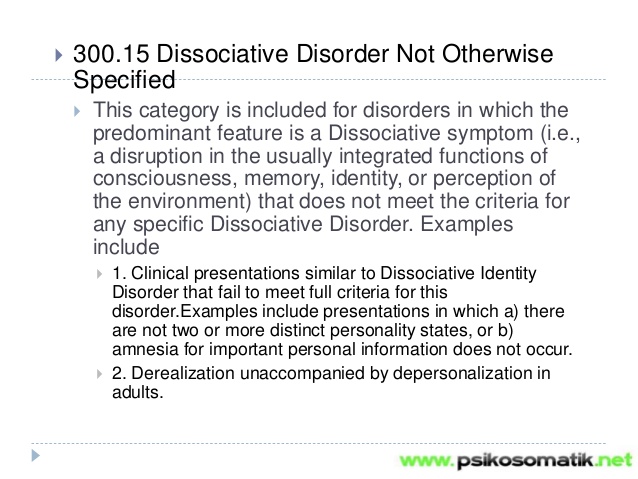
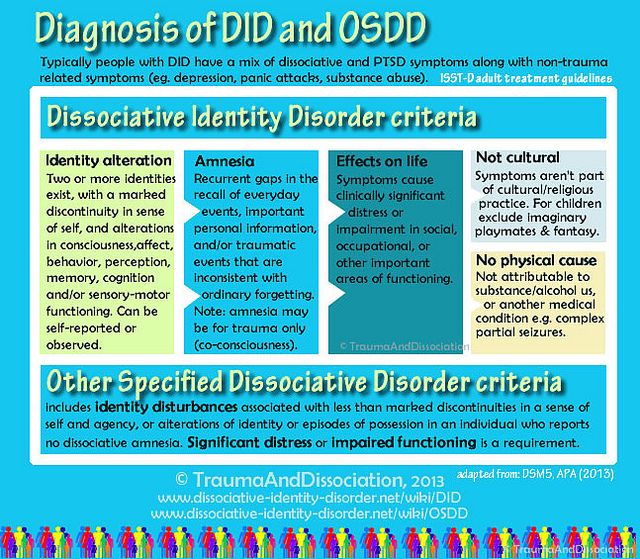
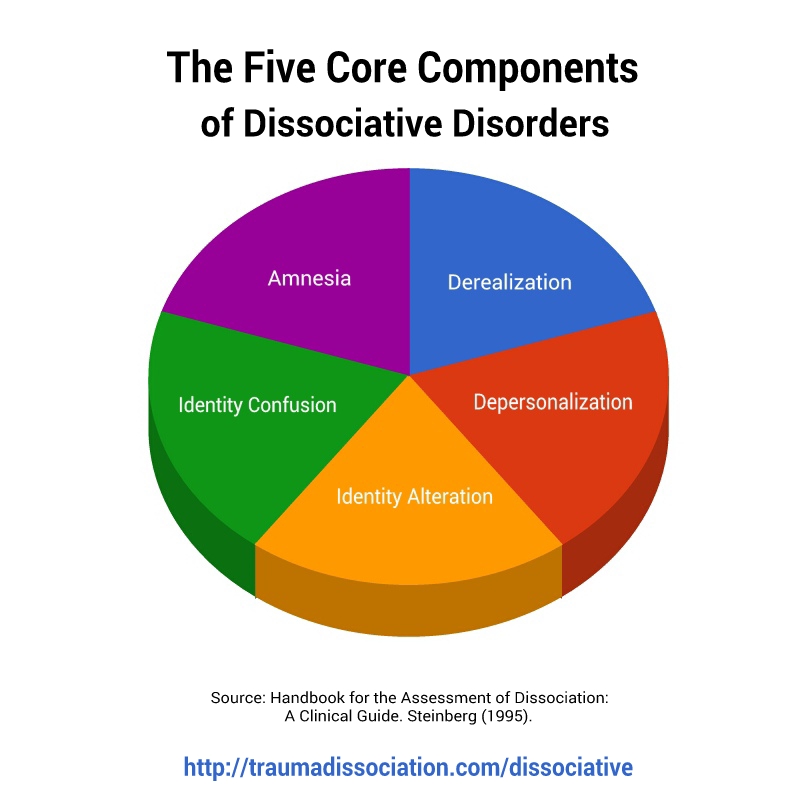
Dissociative Disorders are classically characterized as a disruption of normal consciousness/memory/identity and behavior. The disorders are classically broken down into "positive " and "negative " symptoms -positive symptoms are often associated with "new personalities, derealization," and negative symptoms are symptoms such as autism and paralysis.[10] Dissociative Identity Disorder is part of the larger dissociative disorders spectrum however has more specific criteria that are outlined by the Diagnostic And Statistical Manual Edition-5.
The Diagnostic and Statistical Manual (DSM-5)criteria for DID include at least two or more distinct personalities. Each personality varies in behavior, sense of consciousness, memory, and perception of the outside world. Persons with DID experience amnesia, which essentially are distinct gaps in memory and recollections of daily and traumatic events. They cannot be directly related to substance use or part of cultural norms or practices. Importantly, these symptoms must cause a notable lack of functioning in day-to-day life.[11][10]
Importantly, these symptoms must cause a notable lack of functioning in day-to-day life.[11][10]
Evaluation
As explained above, a detailed history from multiple sources and multiple longitudinal assessments over time is of the essence. However, some evaluation tools have been developed to diagnose DID. Some of these are below:
Dissociative Experiences Scale -28-item self-report instrument whose items tap the absorption of outside information, use of imagination depersonalization, derealization, and amnesia primarily.[12]
Dissociation Questionnaire -63 questions that measure-measures identity confusion and fragmentation, loss of control, amnesia, and absorption.
Difficulties in Emotion Regulation Scale (DERS)- 36-question subjective questions around challenges in goal-directed work, impulsivity, emotional responses to situations, ability to self regulate emotions, etc.[13]
Treatment / Management
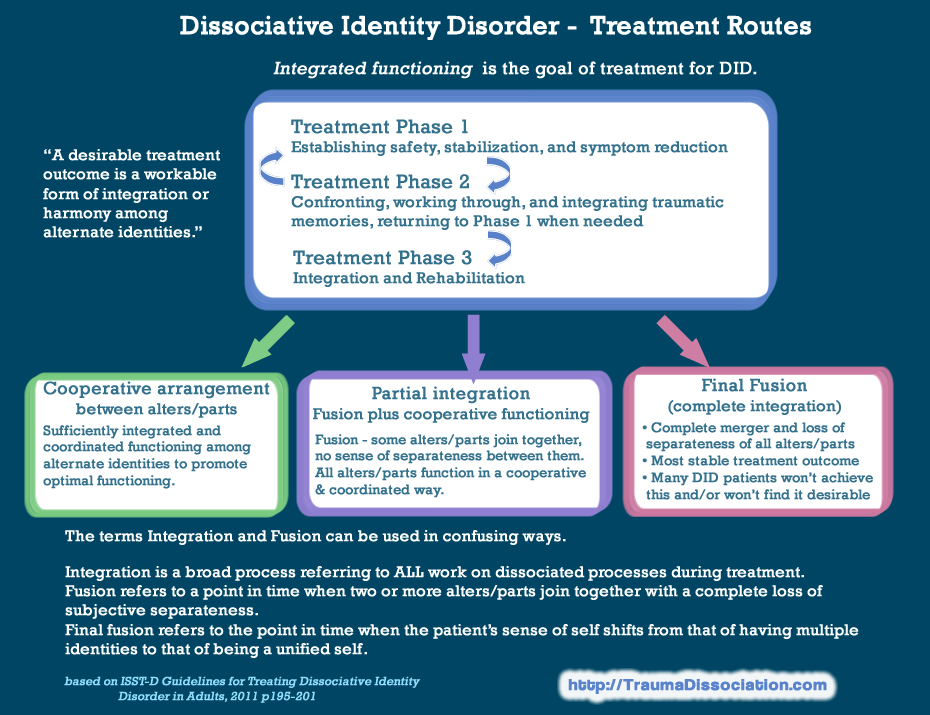
Some treatment approaches for dissociative identity disorder include basic structures from work with personality disorders in a three-pronged approach:
Establishing safety, stabilization, and symptom reduction;
Confronting, working through, and integrating traumatic memories
Identity integration and rehabilitation.
 [14]
[14]
The first step focuses on the safety of patients with DID as many patients present with suicidal ideation and self-injurious behavior.[8] It is important to mitigate that risk. The second phase focuses on working with traumatic memories includes tolerating, processing, and integrating past trauma. This may focus on continuing to re-access traumatic memories with different alternate identities and may help with sharing of memories. The third and final phase of treatment focuses essentially on the patient’s relationship to self as a whole and to the rest of the world. Through all the phases of treatment, a strong therapeutic alliance and trust are encouraged
The most common approach is via psychodynamic psychotherapy steps which are broken down above. Recent approaches include the use of trauma-focused cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT).[15] There are no controlled clinical trials for CBT. The reason DBT skills are used is essentially secondary to some of the overlapping symptoms between borderline personality disorder and DID.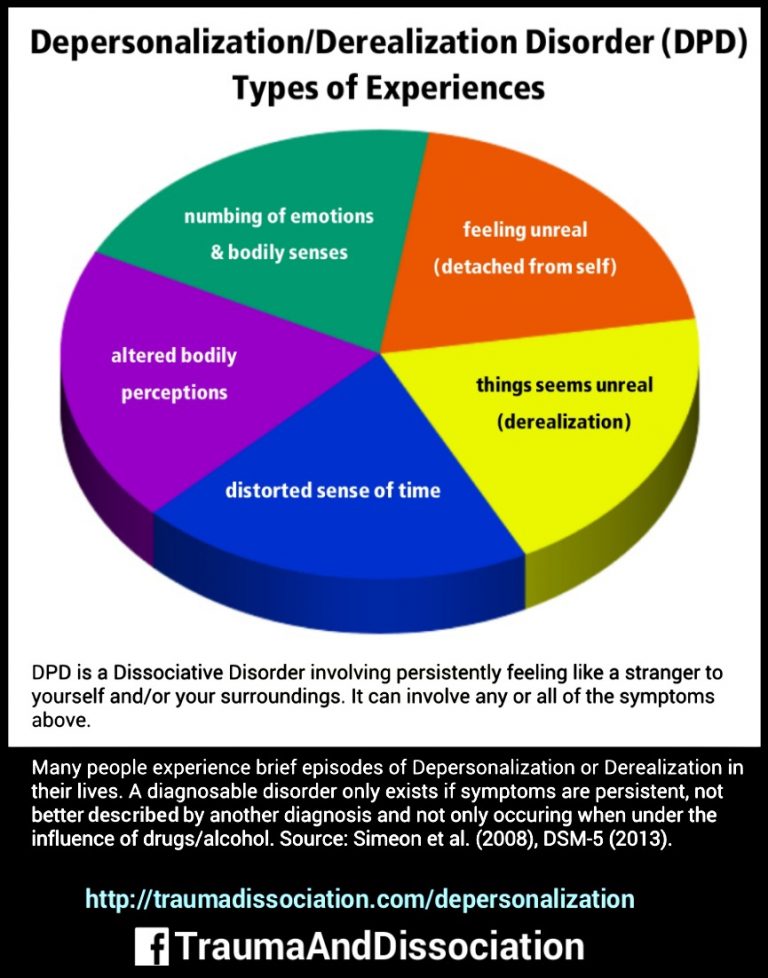 Even with varying therapy approaches- some core features of treatment include more education, emotional regulation, managing stressors, and daily functioning.
Even with varying therapy approaches- some core features of treatment include more education, emotional regulation, managing stressors, and daily functioning.
Another mode of treatment is the use of hypnosis as therapy. DID patients are more hypnotizable than other clinical populations according to literature.[16] There have been some studies as recent as 2009 that have shown efficacy in the use of hypnosis to treat DID.[17] Many DID patients are considered autohypnotic. Some techniques include accessing alternate identities not present in the session, an intervention that can facilitate the emergence of identities critical to the therapeutic process.[6]
Another mode of treatment has been the use of Eye Movement Desensitization and Reprocessing (EMDR). The guidelines however advocate for EMDR to be used as part of integrative treatment. EMDR processing is recommended only when the patient is generally stable and has adequate coping skills.EMDR interventions for symptom reduction and containment, ego strengthening, work with alternate identities, and, when appropriate, the negotiation of consent and preparation of alternate identities.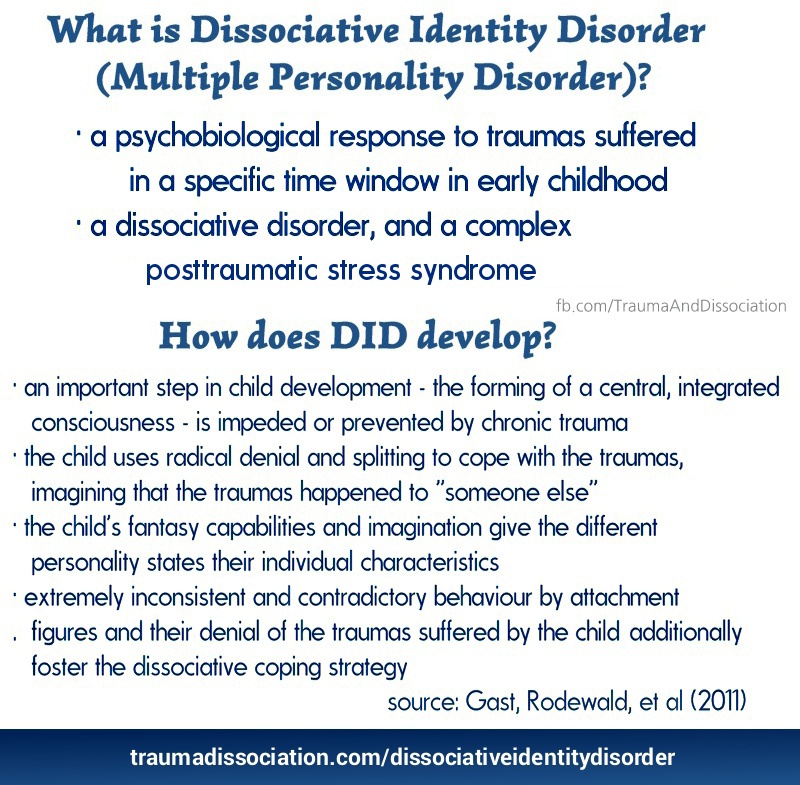 [18]
[18]
Psychopharmacology is not the primary treatment for DID. Medications may be used to target certain symptoms reported. Most commonly used medications include medications for mood disorders and PTSD (post-traumatic stress disorder).[19] The challenges of using psychopharmacological medications remain as different alters may report different symptoms and some alter may report compliance and some may not. The literature review has shown that many medications have been used for DID including antipsychotic medications, mood stabilizers, and even stimulants however no medication has been effective in the treatment of DID.[20]
Differential Diagnosis
As mentioned above, the most common differential diagnosis includes borderline personality disorder, histrionic personality disorder, and even primary psychotic disorders such as schizophrenia and schizoaffective disorders. As mentioned, patients with DID often present with symptoms of dissociation and amnesia, which are also seen in patients with borderline personality disorder. Often patients' symptoms are considered symptoms of psychosis as alters as mistaken as hallucinations and which often precipitate the use of antipsychotic medications. Given that trauma is a focus, Post Traumatic Stress Disorder is also a differential diagnosis.
Often patients' symptoms are considered symptoms of psychosis as alters as mistaken as hallucinations and which often precipitate the use of antipsychotic medications. Given that trauma is a focus, Post Traumatic Stress Disorder is also a differential diagnosis.
The most common differential diagnosis is borderline personality disorder.[21] Borderline personality disorder is also associated with extensive trauma, which often presents with micropsychotic and dissociative symptoms.
Pertinent Studies and Ongoing Trials
There have been case studies and case reports formerly reported in the '90s and early 2000s. Some more treatment interventions have been described in naturalistic and longitudinal studies that continue to inform outcomes.[7]
Prognosis
Dissociative identity disorder is, unfortunately, a medical condition that is often diagnosed later in life. Often patients are misdiagnosed with other diagnoses as described above and treated with medications and even therapies that may not directly address DID. Once in treatment, this tends to be lifelong as DID patients continue to require reality-based and grounding interventions. Safety planning with DID patients is lifelong. The prognosis without treatment and correct diagnosis are poor.
Once in treatment, this tends to be lifelong as DID patients continue to require reality-based and grounding interventions. Safety planning with DID patients is lifelong. The prognosis without treatment and correct diagnosis are poor.
Complications
The patients remain at increased risk of self-injurious behavior given the presence of alters as well as latent trauma.[22] There have been newer research studies that have described suicidal ideation, especially during dissociation, which describes decreased pain tolerance and more emotional dysregulation. Most treatment interventions advocate for safety planning and reality testing before the use of more advanced psychotherapy techniques
Inpatient hospitalizations and day treatment programs may also be recommended for patients who struggle with thoughts of self-injurious behavior, poor impulse control, or acute mood dysregulation. Medications may be added for mood stabilization.
Deterrence and Patient Education
Patient education must focus on informing patients on the correct diagnosis when it is determined. Family members are encouraged to be educated about the nature of this illness, including the presence of alters as well as safety and grounding techniques. Another vital aspect continues to maintain a strong therapeutic alliance with the treatment team and engage in maintaining safety techniques.
Family members are encouraged to be educated about the nature of this illness, including the presence of alters as well as safety and grounding techniques. Another vital aspect continues to maintain a strong therapeutic alliance with the treatment team and engage in maintaining safety techniques.
Education may be done with multiple alters that do not communicate with each other, and this must be recognized. On the other hand, DID patients often do not want their diagnosis shared publicly, and their privacy must be respected.
Enhancing Healthcare Team Outcomes
Dissociative identity disorder requires treatment by an interprofessional healthcare team - this will often consist of medical specialists such as a psychiatrist, mid-level practitioners, nursing staff, specialized therapists, trauma counselors, peer counselors, and therapists who all communicate and collaborate with each other. A psychiatrist and primary care physician complete the team. Maintaining a strong therapeutic alliance with both patient and involved family members continues to be of utmost importance. DID patients require frequent check-ins and follow-up appointments and an almost daily focus on safety planning and reality-based interventions.
DID patients require frequent check-ins and follow-up appointments and an almost daily focus on safety planning and reality-based interventions.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Brand BL, Schielke HJ, Putnam KT, Putnam FW, Loewenstein RJ, Myrick A, Jepsen EKK, Langeland W, Steele K, Classen CC, Lanius RA. An Online Educational Program for Individuals With Dissociative Disorders and Their Clinicians: 1-Year and 2-Year Follow-Up. J Trauma Stress. 2019 Feb;32(1):156-166. [PMC free article: PMC6590319] [PubMed: 30698858]
- 2.
Spiegel D, Lewis-Fernández R, Lanius R, Vermetten E, Simeon D, Friedman M. Dissociative disorders in DSM-5. Annu Rev Clin Psychol. 2013;9:299-326. [PubMed: 23394228]
- 3.
van Duijl M, Nijenhuis E, Komproe IH, Gernaat HB, de Jong JT. Dissociative symptoms and reported trauma among patients with spirit possession and matched healthy controls in Uganda.
 Cult Med Psychiatry. 2010 Jun;34(2):380-400. [PMC free article: PMC2878595] [PubMed: 20401630]
Cult Med Psychiatry. 2010 Jun;34(2):380-400. [PMC free article: PMC2878595] [PubMed: 20401630]- 4.
Lynn SJ, Lilienfeld SO, Merckelbach H, Giesbrecht T, McNally RJ, Loftus EF, Bruck M, Garry M, Malaktaris A. The trauma model of dissociation: inconvenient truths and stubborn fictions. Comment on Dalenberg et al. (2012). Psychol Bull. 2014 May;140(3):896-910. [PubMed: 24773505]
- 5.
Candel I, Merckelbach H. Peritraumatic dissociation as a predictor of post-traumatic stress disorder: a critical review. Compr Psychiatry. 2004 Jan-Feb;45(1):44-50. [PubMed: 14671736]
- 6.
Kluft RP. An overview of the psychotherapy of dissociative identity disorder. Am J Psychother. 1999 Summer;53(3):289-319. [PubMed: 10586296]
- 7.
Brand BL, Loewenstein RJ, Spiegel D. Dispelling myths about dissociative identity disorder treatment: an empirically based approach. Psychiatry. 2014 Summer;77(2):169-89. [PubMed: 24865199]
- 8.
Foote B, Smolin Y, Neft DI, Lipschitz D. Dissociative disorders and suicidality in psychiatric outpatients. J Nerv Ment Dis. 2008 Jan;196(1):29-36. [PubMed: 18195639]
- 9.
Ross CA, Anderson G, Fleisher WP, Norton GR. The frequency of multiple personality disorder among psychiatric inpatients. Am J Psychiatry. 1991 Dec;148(12):1717-20. [PubMed: 1957936]
- 10.
Spiegel D, Loewenstein RJ, Lewis-Fernández R, Sar V, Simeon D, Vermetten E, Cardeña E, Dell PF. Dissociative disorders in DSM-5. Depress Anxiety. 2011 Sep;28(9):824-52. [PubMed: 21910187]
- 11.
Brand BL, Sar V, Stavropoulos P, Krüger C, Korzekwa M, Martínez-Taboas A, Middleton W. Separating Fact from Fiction: An Empirical Examination of Six Myths About Dissociative Identity Disorder. Harv Rev Psychiatry. 2016 Jul-Aug;24(4):257-70. [PMC free article: PMC4959824] [PubMed: 27384396]
- 12.
Dubester KA, Braun BG. Psychometric properties of the Dissociative Experiences Scale.
 J Nerv Ment Dis. 1995 Apr;183(4):231-5. [PubMed: 7714511]
J Nerv Ment Dis. 1995 Apr;183(4):231-5. [PubMed: 7714511]- 13.
Hallion LS, Steinman SA, Tolin DF, Diefenbach GJ. Psychometric Properties of the Difficulties in Emotion Regulation Scale (DERS) and Its Short Forms in Adults With Emotional Disorders. Front Psychol. 2018;9:539. [PMC free article: PMC5917244] [PubMed: 29725312]
- 14.
Frankel FH. Adult reconstruction of childhood events in the multiple personality literature. Am J Psychiatry. 1993 Jun;150(6):954-8. [PubMed: 8494076]
- 15.
Putnam FW, Loewenstein RJ. Treatment of multiple personality disorder: a survey of current practices. Am J Psychiatry. 1993 Jul;150(7):1048-52. [PubMed: 8100401]
- 16.
Frischholz EJ, Lipman LS, Braun BG, Sachs RG. Psychopathology, hypnotizability, and dissociation. Am J Psychiatry. 1992 Nov;149(11):1521-5. [PubMed: 1415819]
- 17.
Ross CA. Re: The effects of hypnosis on dissociative identity disorder. Can J Psychiatry.
 2000 Apr;45(3):298-9. [PubMed: 10779893]
2000 Apr;45(3):298-9. [PubMed: 10779893]- 18.
Fine CG, Berkowitz AS. The wreathing protocol: the imbrication of hypnosis and EMDR in the treatment of dissociative identity disorder and other dissociative responses. Eye Movement Desensitization Reprocessing. Am J Clin Hypn. 2001 Jan-Apr;43(3-4):275-90. [PubMed: 11269630]
- 19.
Loewenstein RJ. Rational psychopharmacology in the treatment of multiple personality disorder. Psychiatr Clin North Am. 1991 Sep;14(3):721-40. [PubMed: 1946032]
- 20.
Dorahy MJ, Brand BL, Sar V, Krüger C, Stavropoulos P, Martínez-Taboas A, Lewis-Fernández R, Middleton W. Dissociative identity disorder: An empirical overview. Aust N Z J Psychiatry. 2014 May;48(5):402-17. [PubMed: 24788904]
- 21.
Brand BL, Lanius RA. Chronic complex dissociative disorders and borderline personality disorder: disorders of emotion dysregulation? Borderline Personal Disord Emot Dysregul. 2014;1:13. [PMC free article: PMC4579511] [PubMed: 26401297]
- 22.
Rabasco A, Andover MS. The interaction of dissociation, pain tolerance, and suicidal ideation in predicting suicide attempts. Psychiatry Res. 2020 Feb;284:112661. [PubMed: 31708251]
Dissociative Identity Disorder - StatPearls
Continuing Education Activity
Dissociative identity disorder (DID) is a rare psychiatric disorder diagnosed in about 1.5% of the global population. This disorder is often misdiagnosed and often requires multiple assessments for an accurate diagnosis. Patients often present with self-injurious behavior and suicide attempts. This activity reviews the evaluation and treatment of dissociative identity disorder and explains the role of an interprofessional team in caring for patients diagnosed with dissociative identity disorder (DID). This activity also reviews the association between DID and suicidal behavior.
Objectives:
Describe the constellation of behavioral symptoms that lead to a diagnosis of dissociative identity disorder.
Review risk factors for the development of a diagnosis of dissociative identity disorder.
Explain the different modalities of evidence-based treatment for dissociative identity disorder.
Outline some interprofessional strategies that can improve patient outcomes in patients with dissociative identity disorder.
Access free multiple choice questions on this topic.
Introduction
Dissociative identity disorder (DID) is a rare disorder associated with severe behavioral health symptoms. DID was previously known as Multiple Personality Disorder until 1994. Approximately 1.5% of the population internationally has been diagnosed with a dissociative identity disorder.[1] Often patients with this diagnosis have several emergency presentations, often with self-injurious behavior and even substance use.[2]
Of note, DID has been observed and described in several countries and has been associated with terms such as "outer world possession" and "possession by demons. "[3] Several case reports have been described with those terms; however, trauma and its association came with DID much later.
"[3] Several case reports have been described with those terms; however, trauma and its association came with DID much later.
Etiology
Dissociative identity disorder is typically associated with severe childhood trauma and abuse.[4] Dalenberg and his team have detailed the role of trauma in the development of dissociative disorder and dismissed the previous model, which was based on fantasy and often associated with suggestibility, cognitive distortions, and fantasy. However, newer research tends to describe a combination of both severe traumas (which may be in any form-physical/emotional/sexual)as well as some effects of cognitive suggestion. Stress experienced by an individual secondary to trauma has been seen to be contributory toward the formation of an accurate understanding of the trauma being unreal, even posttraumatic dissociation such as leaving one's body, etc., and poor sleep. However, in the fantasy theory-it has been seen that people with high levels of vulnerability, predisposition of psychological symptoms, media influences, and likely social isolation and vulnerability.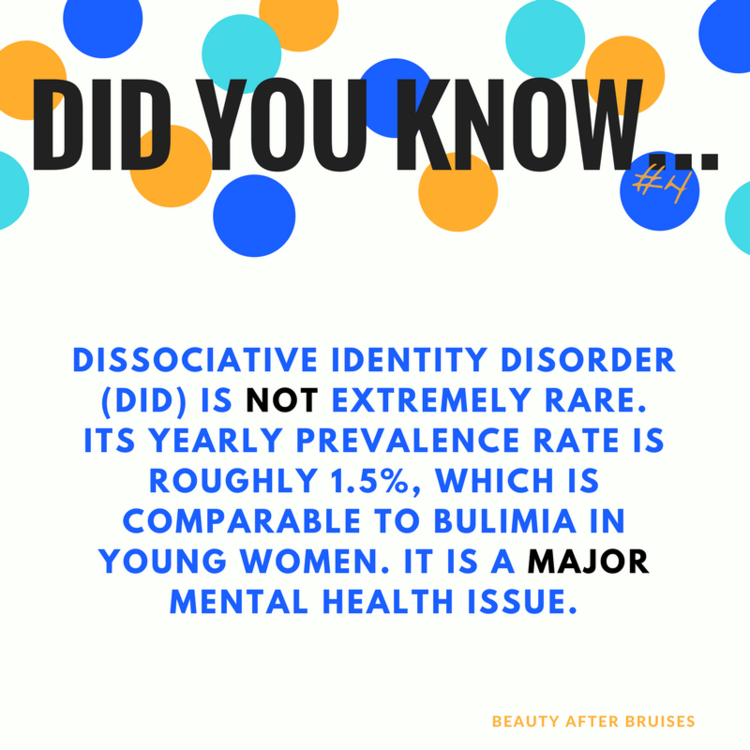 [5]
[5]
Several prominent psychologists such as Kluft have broken down the theory behind DID-in-sum. The theory describes predisposing factors for dissociation, which include an ability to dissociate, overwhelming traumatic experiences that distort reality, creation of alters with specific names and identities, and lack of external stability, which leads to the child's self-soothing to tolerate these stressors. These four factors must be present for DID to develop.[6]
Epidemiology
Dissociative disorders show a prevalence of 1% to 5% in the international population. Severe dissociative identity disorder is present in 1% to 1.5% of this population. Patients may spend up to 5 to 12.5 years in treatment before being diagnosed with a dissociative identity disorder.[7] Patients with DID come with increased rates of non-suicidal self-injurious behavior and suicide attempts.[8]
Pathophysiology
The DID person, per the International Society for the Study of Trauma and Dissociation, is described as a person who experiences separate identities that function independently of each other and are autonomous of each other.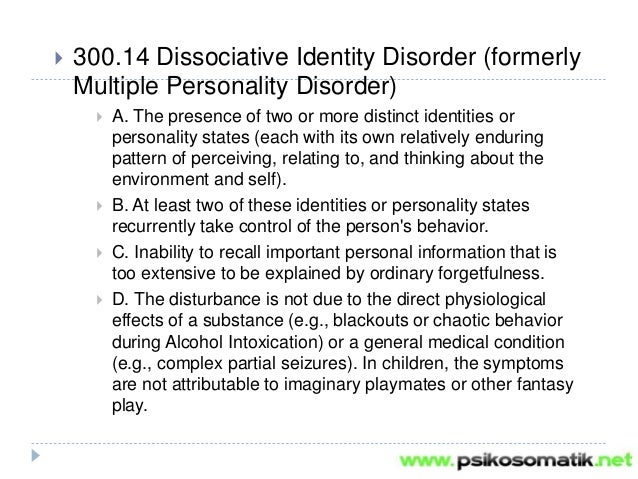 The International Society describes alternate identities or alters as independent identities which have their own distinct behaviors, have memories that are distinct from others, and even may differ in language and expressions used. Signs of a switch to an altered state include trance-like behavior, eye blinking, eye-rolling, and changes in posture.
The International Society describes alternate identities or alters as independent identities which have their own distinct behaviors, have memories that are distinct from others, and even may differ in language and expressions used. Signs of a switch to an altered state include trance-like behavior, eye blinking, eye-rolling, and changes in posture.
The major hypothesis by Putnam et al. is that “alternate identities result from the inability of many traumatized children to develop a unified sense of self that is maintained across various behavioral states, particularly if the traumatic exposure first occurs before the age of 5 “.[9] The theories have been studied by groups in the inpatient unit services in the 1990s.
History and Physical
The way to diagnose dissociative identity disorder is via detailed history taken by both psychiatric practitioners and experienced psychologists. Often persons with DID are misdiagnosed with other personality disorders, most commonly borderline personality disorder, as elements of dissociation are prominently seen and even amnesia. Often longitudinal assessments over long periods and careful history taking are required to complete diagnostic evaluations. History is often gathered from multiple sources as well. Often neurological examinations are required as well to rule out autoimmune encephalitis, often requiring electroencephalograms, lumbar punctures, and brain imaging.
Often longitudinal assessments over long periods and careful history taking are required to complete diagnostic evaluations. History is often gathered from multiple sources as well. Often neurological examinations are required as well to rule out autoimmune encephalitis, often requiring electroencephalograms, lumbar punctures, and brain imaging.
Dissociative Disorders are classically characterized as a disruption of normal consciousness/memory/identity and behavior. The disorders are classically broken down into "positive " and "negative " symptoms -positive symptoms are often associated with "new personalities, derealization," and negative symptoms are symptoms such as autism and paralysis.[10] Dissociative Identity Disorder is part of the larger dissociative disorders spectrum however has more specific criteria that are outlined by the Diagnostic And Statistical Manual Edition-5.
The Diagnostic and Statistical Manual (DSM-5)criteria for DID include at least two or more distinct personalities. Each personality varies in behavior, sense of consciousness, memory, and perception of the outside world. Persons with DID experience amnesia, which essentially are distinct gaps in memory and recollections of daily and traumatic events. They cannot be directly related to substance use or part of cultural norms or practices. Importantly, these symptoms must cause a notable lack of functioning in day-to-day life.[11][10]
Each personality varies in behavior, sense of consciousness, memory, and perception of the outside world. Persons with DID experience amnesia, which essentially are distinct gaps in memory and recollections of daily and traumatic events. They cannot be directly related to substance use or part of cultural norms or practices. Importantly, these symptoms must cause a notable lack of functioning in day-to-day life.[11][10]
Evaluation
As explained above, a detailed history from multiple sources and multiple longitudinal assessments over time is of the essence. However, some evaluation tools have been developed to diagnose DID. Some of these are below:
Dissociative Experiences Scale -28-item self-report instrument whose items tap the absorption of outside information, use of imagination depersonalization, derealization, and amnesia primarily.[12]
Dissociation Questionnaire -63 questions that measure-measures identity confusion and fragmentation, loss of control, amnesia, and absorption.

Difficulties in Emotion Regulation Scale (DERS)- 36-question subjective questions around challenges in goal-directed work, impulsivity, emotional responses to situations, ability to self regulate emotions, etc.[13]
Treatment / Management
Some treatment approaches for dissociative identity disorder include basic structures from work with personality disorders in a three-pronged approach:
Establishing safety, stabilization, and symptom reduction;
Confronting, working through, and integrating traumatic memories
Identity integration and rehabilitation.[14]
The first step focuses on the safety of patients with DID as many patients present with suicidal ideation and self-injurious behavior.[8] It is important to mitigate that risk. The second phase focuses on working with traumatic memories includes tolerating, processing, and integrating past trauma. This may focus on continuing to re-access traumatic memories with different alternate identities and may help with sharing of memories. The third and final phase of treatment focuses essentially on the patient’s relationship to self as a whole and to the rest of the world. Through all the phases of treatment, a strong therapeutic alliance and trust are encouraged
The third and final phase of treatment focuses essentially on the patient’s relationship to self as a whole and to the rest of the world. Through all the phases of treatment, a strong therapeutic alliance and trust are encouraged
The most common approach is via psychodynamic psychotherapy steps which are broken down above. Recent approaches include the use of trauma-focused cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT).[15] There are no controlled clinical trials for CBT. The reason DBT skills are used is essentially secondary to some of the overlapping symptoms between borderline personality disorder and DID. Even with varying therapy approaches- some core features of treatment include more education, emotional regulation, managing stressors, and daily functioning.
Another mode of treatment is the use of hypnosis as therapy. DID patients are more hypnotizable than other clinical populations according to literature.[16] There have been some studies as recent as 2009 that have shown efficacy in the use of hypnosis to treat DID. [17] Many DID patients are considered autohypnotic. Some techniques include accessing alternate identities not present in the session, an intervention that can facilitate the emergence of identities critical to the therapeutic process.[6]
[17] Many DID patients are considered autohypnotic. Some techniques include accessing alternate identities not present in the session, an intervention that can facilitate the emergence of identities critical to the therapeutic process.[6]
Another mode of treatment has been the use of Eye Movement Desensitization and Reprocessing (EMDR). The guidelines however advocate for EMDR to be used as part of integrative treatment. EMDR processing is recommended only when the patient is generally stable and has adequate coping skills.EMDR interventions for symptom reduction and containment, ego strengthening, work with alternate identities, and, when appropriate, the negotiation of consent and preparation of alternate identities.[18]
Psychopharmacology is not the primary treatment for DID. Medications may be used to target certain symptoms reported. Most commonly used medications include medications for mood disorders and PTSD (post-traumatic stress disorder).[19] The challenges of using psychopharmacological medications remain as different alters may report different symptoms and some alter may report compliance and some may not.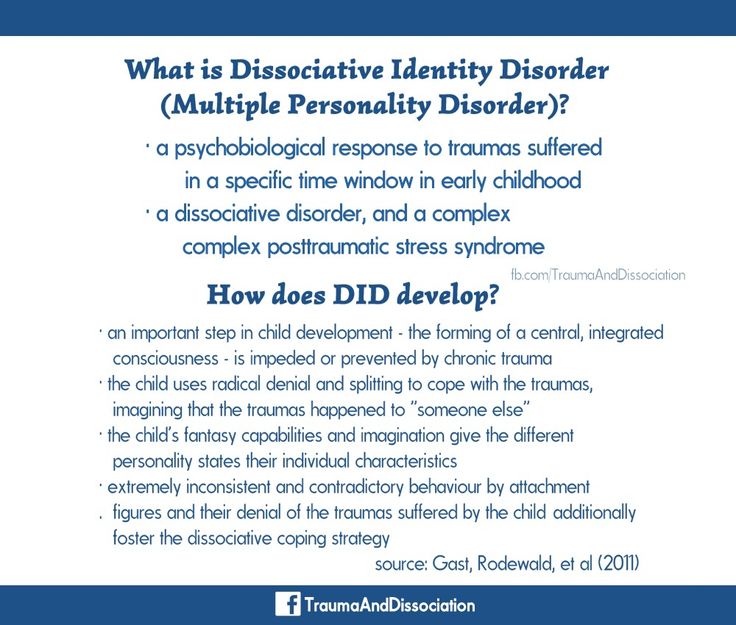 The literature review has shown that many medications have been used for DID including antipsychotic medications, mood stabilizers, and even stimulants however no medication has been effective in the treatment of DID.[20]
The literature review has shown that many medications have been used for DID including antipsychotic medications, mood stabilizers, and even stimulants however no medication has been effective in the treatment of DID.[20]
Differential Diagnosis
As mentioned above, the most common differential diagnosis includes borderline personality disorder, histrionic personality disorder, and even primary psychotic disorders such as schizophrenia and schizoaffective disorders. As mentioned, patients with DID often present with symptoms of dissociation and amnesia, which are also seen in patients with borderline personality disorder. Often patients' symptoms are considered symptoms of psychosis as alters as mistaken as hallucinations and which often precipitate the use of antipsychotic medications. Given that trauma is a focus, Post Traumatic Stress Disorder is also a differential diagnosis.
The most common differential diagnosis is borderline personality disorder.[21] Borderline personality disorder is also associated with extensive trauma, which often presents with micropsychotic and dissociative symptoms.
Pertinent Studies and Ongoing Trials
There have been case studies and case reports formerly reported in the '90s and early 2000s. Some more treatment interventions have been described in naturalistic and longitudinal studies that continue to inform outcomes.[7]
Prognosis
Dissociative identity disorder is, unfortunately, a medical condition that is often diagnosed later in life. Often patients are misdiagnosed with other diagnoses as described above and treated with medications and even therapies that may not directly address DID. Once in treatment, this tends to be lifelong as DID patients continue to require reality-based and grounding interventions. Safety planning with DID patients is lifelong. The prognosis without treatment and correct diagnosis are poor.
Complications
The patients remain at increased risk of self-injurious behavior given the presence of alters as well as latent trauma.[22] There have been newer research studies that have described suicidal ideation, especially during dissociation, which describes decreased pain tolerance and more emotional dysregulation.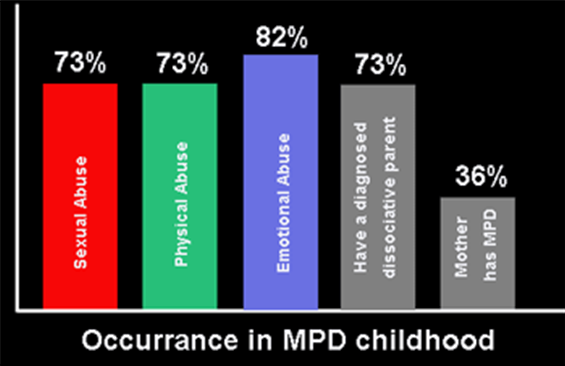 Most treatment interventions advocate for safety planning and reality testing before the use of more advanced psychotherapy techniques
Most treatment interventions advocate for safety planning and reality testing before the use of more advanced psychotherapy techniques
Inpatient hospitalizations and day treatment programs may also be recommended for patients who struggle with thoughts of self-injurious behavior, poor impulse control, or acute mood dysregulation. Medications may be added for mood stabilization.
Deterrence and Patient Education
Patient education must focus on informing patients on the correct diagnosis when it is determined. Family members are encouraged to be educated about the nature of this illness, including the presence of alters as well as safety and grounding techniques. Another vital aspect continues to maintain a strong therapeutic alliance with the treatment team and engage in maintaining safety techniques.
Education may be done with multiple alters that do not communicate with each other, and this must be recognized. On the other hand, DID patients often do not want their diagnosis shared publicly, and their privacy must be respected.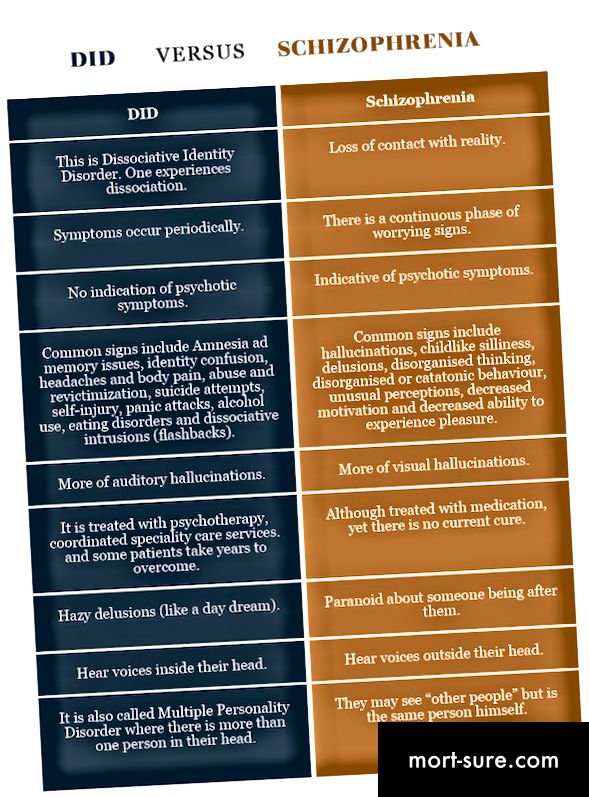
Enhancing Healthcare Team Outcomes
Dissociative identity disorder requires treatment by an interprofessional healthcare team - this will often consist of medical specialists such as a psychiatrist, mid-level practitioners, nursing staff, specialized therapists, trauma counselors, peer counselors, and therapists who all communicate and collaborate with each other. A psychiatrist and primary care physician complete the team. Maintaining a strong therapeutic alliance with both patient and involved family members continues to be of utmost importance. DID patients require frequent check-ins and follow-up appointments and an almost daily focus on safety planning and reality-based interventions.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Brand BL, Schielke HJ, Putnam KT, Putnam FW, Loewenstein RJ, Myrick A, Jepsen EKK, Langeland W, Steele K, Classen CC, Lanius RA.
 An Online Educational Program for Individuals With Dissociative Disorders and Their Clinicians: 1-Year and 2-Year Follow-Up. J Trauma Stress. 2019 Feb;32(1):156-166. [PMC free article: PMC6590319] [PubMed: 30698858]
An Online Educational Program for Individuals With Dissociative Disorders and Their Clinicians: 1-Year and 2-Year Follow-Up. J Trauma Stress. 2019 Feb;32(1):156-166. [PMC free article: PMC6590319] [PubMed: 30698858]- 2.
Spiegel D, Lewis-Fernández R, Lanius R, Vermetten E, Simeon D, Friedman M. Dissociative disorders in DSM-5. Annu Rev Clin Psychol. 2013;9:299-326. [PubMed: 23394228]
- 3.
van Duijl M, Nijenhuis E, Komproe IH, Gernaat HB, de Jong JT. Dissociative symptoms and reported trauma among patients with spirit possession and matched healthy controls in Uganda. Cult Med Psychiatry. 2010 Jun;34(2):380-400. [PMC free article: PMC2878595] [PubMed: 20401630]
- 4.
Lynn SJ, Lilienfeld SO, Merckelbach H, Giesbrecht T, McNally RJ, Loftus EF, Bruck M, Garry M, Malaktaris A. The trauma model of dissociation: inconvenient truths and stubborn fictions. Comment on Dalenberg et al. (2012). Psychol Bull. 2014 May;140(3):896-910. [PubMed: 24773505]
- 5.
Candel I, Merckelbach H. Peritraumatic dissociation as a predictor of post-traumatic stress disorder: a critical review. Compr Psychiatry. 2004 Jan-Feb;45(1):44-50. [PubMed: 14671736]
- 6.
Kluft RP. An overview of the psychotherapy of dissociative identity disorder. Am J Psychother. 1999 Summer;53(3):289-319. [PubMed: 10586296]
- 7.
Brand BL, Loewenstein RJ, Spiegel D. Dispelling myths about dissociative identity disorder treatment: an empirically based approach. Psychiatry. 2014 Summer;77(2):169-89. [PubMed: 24865199]
- 8.
Foote B, Smolin Y, Neft DI, Lipschitz D. Dissociative disorders and suicidality in psychiatric outpatients. J Nerv Ment Dis. 2008 Jan;196(1):29-36. [PubMed: 18195639]
- 9.
Ross CA, Anderson G, Fleisher WP, Norton GR. The frequency of multiple personality disorder among psychiatric inpatients. Am J Psychiatry. 1991 Dec;148(12):1717-20. [PubMed: 1957936]
- 10.
Spiegel D, Loewenstein RJ, Lewis-Fernández R, Sar V, Simeon D, Vermetten E, Cardeña E, Dell PF.
 Dissociative disorders in DSM-5. Depress Anxiety. 2011 Sep;28(9):824-52. [PubMed: 21910187]
Dissociative disorders in DSM-5. Depress Anxiety. 2011 Sep;28(9):824-52. [PubMed: 21910187]- 11.
Brand BL, Sar V, Stavropoulos P, Krüger C, Korzekwa M, Martínez-Taboas A, Middleton W. Separating Fact from Fiction: An Empirical Examination of Six Myths About Dissociative Identity Disorder. Harv Rev Psychiatry. 2016 Jul-Aug;24(4):257-70. [PMC free article: PMC4959824] [PubMed: 27384396]
- 12.
Dubester KA, Braun BG. Psychometric properties of the Dissociative Experiences Scale. J Nerv Ment Dis. 1995 Apr;183(4):231-5. [PubMed: 7714511]
- 13.
Hallion LS, Steinman SA, Tolin DF, Diefenbach GJ. Psychometric Properties of the Difficulties in Emotion Regulation Scale (DERS) and Its Short Forms in Adults With Emotional Disorders. Front Psychol. 2018;9:539. [PMC free article: PMC5917244] [PubMed: 29725312]
- 14.
Frankel FH. Adult reconstruction of childhood events in the multiple personality literature. Am J Psychiatry.
 1993 Jun;150(6):954-8. [PubMed: 8494076]
1993 Jun;150(6):954-8. [PubMed: 8494076]- 15.
Putnam FW, Loewenstein RJ. Treatment of multiple personality disorder: a survey of current practices. Am J Psychiatry. 1993 Jul;150(7):1048-52. [PubMed: 8100401]
- 16.
Frischholz EJ, Lipman LS, Braun BG, Sachs RG. Psychopathology, hypnotizability, and dissociation. Am J Psychiatry. 1992 Nov;149(11):1521-5. [PubMed: 1415819]
- 17.
Ross CA. Re: The effects of hypnosis on dissociative identity disorder. Can J Psychiatry. 2000 Apr;45(3):298-9. [PubMed: 10779893]
- 18.
Fine CG, Berkowitz AS. The wreathing protocol: the imbrication of hypnosis and EMDR in the treatment of dissociative identity disorder and other dissociative responses. Eye Movement Desensitization Reprocessing. Am J Clin Hypn. 2001 Jan-Apr;43(3-4):275-90. [PubMed: 11269630]
- 19.
Loewenstein RJ. Rational psychopharmacology in the treatment of multiple personality disorder. Psychiatr Clin North Am.
 1991 Sep;14(3):721-40. [PubMed: 1946032]
1991 Sep;14(3):721-40. [PubMed: 1946032]- 20.
Dorahy MJ, Brand BL, Sar V, Krüger C, Stavropoulos P, Martínez-Taboas A, Lewis-Fernández R, Middleton W. Dissociative identity disorder: An empirical overview. Aust N Z J Psychiatry. 2014 May;48(5):402-17. [PubMed: 24788904]
- 21.
Brand BL, Lanius RA. Chronic complex dissociative disorders and borderline personality disorder: disorders of emotion dysregulation? Borderline Personal Disord Emot Dysregul. 2014;1:13. [PMC free article: PMC4579511] [PubMed: 26401297]
- 22.
Rabasco A, Andover MS. The interaction of dissociation, pain tolerance, and suicidal ideation in predicting suicide attempts. Psychiatry Res. 2020 Feb;284:112661. [PubMed: 31708251]
Dissociative Identity Disorder: how a girl survived her father's abuse, splitting herself into 2500 identities
- France Mao
- BBC Sydney
you to understand the events.
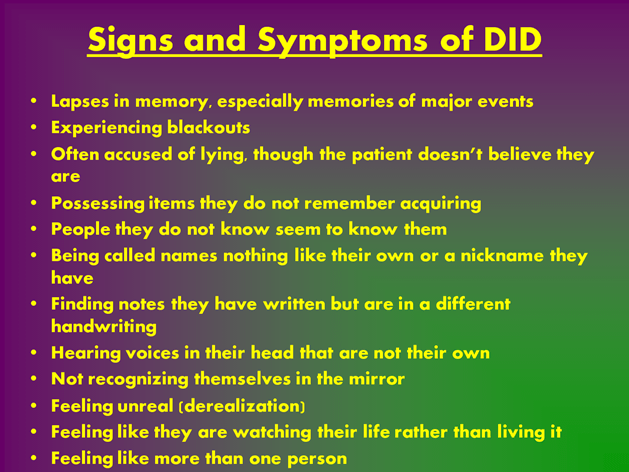
Photo copyright JENI HAYNES/ NINE NETWORK
Photo captionJenny Haynes' six personal identities were allowed to testify in court against her father
One female witness was heard in court that day. But six people spoke through her lips, ready to talk about the bullying she experienced.
"I went into the courtroom, took my seat, took the oath, and then a few hours later I returned to my body and left there," Janie Haynes recalled this day in an interview with the BBC.
When Janie was a child, she was constantly raped by her father, Richard Haynes. Australian police call what happened to her one of the worst cases of child abuse in the history of the country.
To cope with the psychological trauma, her mind resorted to an amazing tactic - it invented new personal identities for her to distance herself from the pain she was experiencing. The bullying was so brutal and continuous that Janie says she had to invent 2,500 different personalities to survive.
- Crowded Inside: A film about living with dissociative identity disorder
- Christina Blasey Ford remembers sexual abuse 36 years later. It's okay
- "Father with a swastika". A well-known athlete in Belarus accuses her father of sexual abuse
Court hearings took place in March, in which Jeni testified against her father on behalf of several of these individuals. Among them was a four-year-old girl named Symphony.
This was the first time in Australia, and probably the world, that a victim diagnosed with dissociative identity disorder testified on behalf of their multiple identities and managed to secure a conviction.
"We weren't afraid. We waited so long to tell everyone exactly what he did to us, and now he couldn't silence us," she said.
On September 6, a court in Sydney sentenced 74-year-old Richard Haynes to 45 years in prison.
Attention: the text contains a description of child abuse and abuse
"Even in my head I did not feel safe"
The Haynes family moved to Australia from London at 1974 year. Janie was four years old, but her father had already begun to mock her. In Sydney, his actions became completely sadistic and were repeated almost daily.
Photo copyright, JENI HAYNES
Photo caption,Jeni's multiple selves became her way of hiding from violence
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of Story Podcast
"My father's bullying was calculated and planned. It was deliberate and he enjoyed it every minute," Janie told the court. As a minor victim, she had the right to remain anonymous, but chose to waive it in order to be able to reveal her father's name.
As a minor victim, she had the right to remain anonymous, but chose to waive it in order to be able to reveal her father's name.
"He heard me begging him to stop, he heard me crying, he saw the pain and horror he caused in me, he saw the blood and the physical damage he inflicted. And the next day he consciously did it again" , - she said.
Haynes taught his daughter that he could read her mind, she said. He threatened to kill her mother, brother, and sister even if she even considered torturing her, let alone tell them about it.
"My inner world was taken over by my father. I didn't feel safe even in my head. I lost the ability to comprehend what was happening to me and draw my own conclusions," Janie said.
To hide her feelings, she expressed her thoughts through song lyrics:
"He ain't heavy/he's my brother" (He's not a burden, he's my brother) - when she was worried about her brother and sister.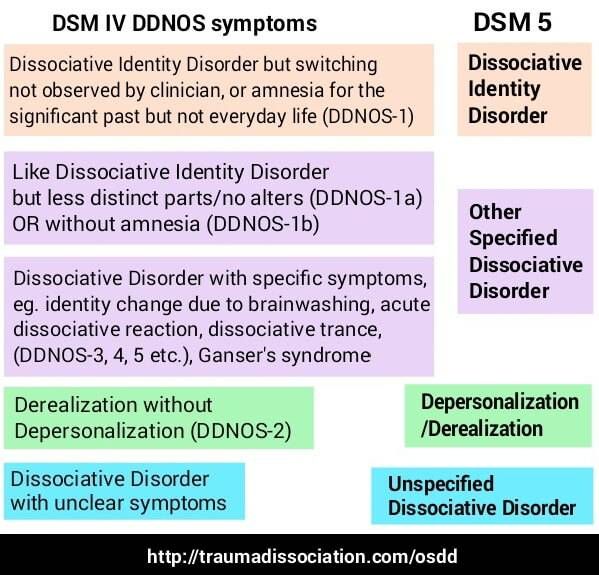
"Do you really want to hurt me/ Do you really want to make me cry" when thinking about her experience.
Her father limited her contact at school to minimize her contact with adults. Janie learned to be quiet and inconspicuous because if she was "noticed", such as when the swimming coach told her father that the girl needed to develop her talent, her father punished her.
Photo copyright, Jeni Haynes
Photo caption,Richard Haynes and his three children, Jeni is on the right
Jeni did not receive medical treatment for injuries from beatings and rape. As a result, she developed serious chronic diseases.
Janie is now 49 years old. Her eyesight is irreparably damaged, her jaw, intestines, anus and coccyx are damaged. She had to undergo several major surgeries, including a colostomy in 2011.
The violence in Janie's life continued until the age of 11, when her family returned to Britain.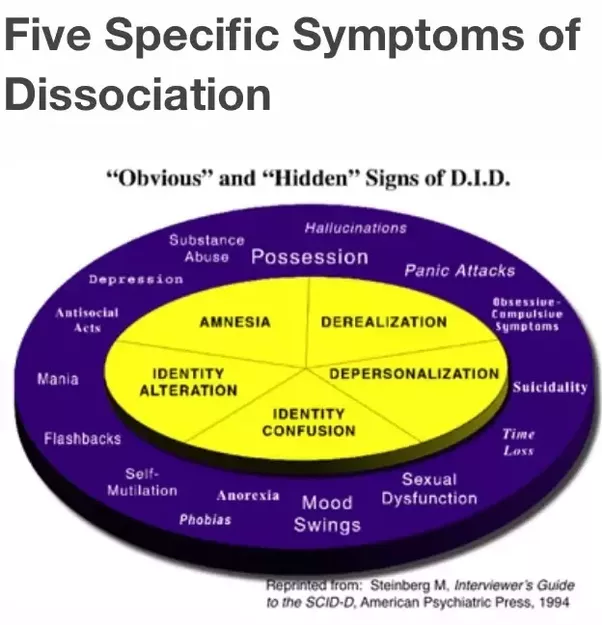 Shortly thereafter, at 1984, her parents divorced. She thinks that no one, not even her mother, knew what she had been through.
Shortly thereafter, at 1984, her parents divorced. She thinks that no one, not even her mother, knew what she had been through.
"Actually he bullied Symphony"
Modern Australian experts call Janie's condition Dissociative Identity Disorder (DID). They say it has a lot to do with the horrendous abuse she experienced as a child—experienced at home, in a place that was supposed to be safe.
"DID is really a survival strategy," child psychologist Pam Stavropoulos, an expert on childhood trauma, told the BBC.
Image copyright JENI HAYNES
Image captionFor most of her childhood Jeni told herself she was Symphony
experiences of abuse and psychological trauma," she said.
The younger the traumatized child and the worse the treatment, the more likely it is that he will resort to dissociation to cope, resulting in a split personality.
Janie said that the first personal identity that appeared in her was Symphony, a four-year-old girl who exists in her own temporary reality.
"She suffered every minute when my dad abused me. When he abused me - his daughter Janie - he was actually bullying Symphony," Janie said.
As the years passed, Symphony herself began to invent new identities to cope with the violence she experienced. Each of the hundreds and hundreds of personalities had a role to play in coping with the elements of violence, whether it was a particularly terrifying episode or images or smells that evoked traumatic memories.
"The alter personality came out from behind the Symphony and became a distraction. My alter personalities served as protection for me from my father," Janie said.
While we were talking about this, about half an hour after the interview began, Symphony appeared. Janie warned that this could happen. The fact that she is about to switch can be guessed by the fact that it becomes more difficult for her to formulate an answer.
"Hi, my name is Symphony. Janie is having a problem. Let me tell you everything if you don't mind," she says quickly.
Janie is having a problem. Let me tell you everything if you don't mind," she says quickly.
Symphony has a higher voice, more lively intonation. She speaks like a little girl, barely catching her breath between words. We talked for 15 minutes. She remembers in great detail the events associated with the "evil dad" that took place decades ago. It's impressive.
"That's what I did. I took everything that I consider valuable in myself, everything that is important and pleasant for me, and hid it from my dad. Therefore, when he mocked me, he mocked not a thinking human being", Symphony said.
Janie's personalities that helped her survive
Photo caption,Janie and some of her essences
- Muscles is a Billy Idol-style teenager. He is tall and wears clothes that flaunt his strong arms. He is calm and caring.
- Volcano - very tall and strong, dressed in black leather from head to toe.
 Hair is dyed straw.
Hair is dyed straw. - Ricky is only eight years old, but he wears an old gray suit. He has short hair and bright red hair.
- Judas is short with red hair. He wears gray trousers from his school uniform and a bright green sweater. Always looks like he's about to say something.
- Linda/Maggot is tall and slender, wearing a 1950s skirt with pink poodle appliqués. Her hair is collected in an elegant bun, and her eyebrows are in a house.
- Rick wears huge glasses - the same as Richard Haynes wore. They cover his face.
In March, Janie was allowed to testify in court on behalf of Symphony and five other personalities, each of whom could talk about different aspects of the abuse experienced. Only the judge was present at the hearing, because the lawyers felt that the testimony would be too traumatic for the jury.
Haynes was initially charged with 367 charges, including multiple counts of rape, sodomy, lewd acts and carnal depravity of a child under 10 years of age.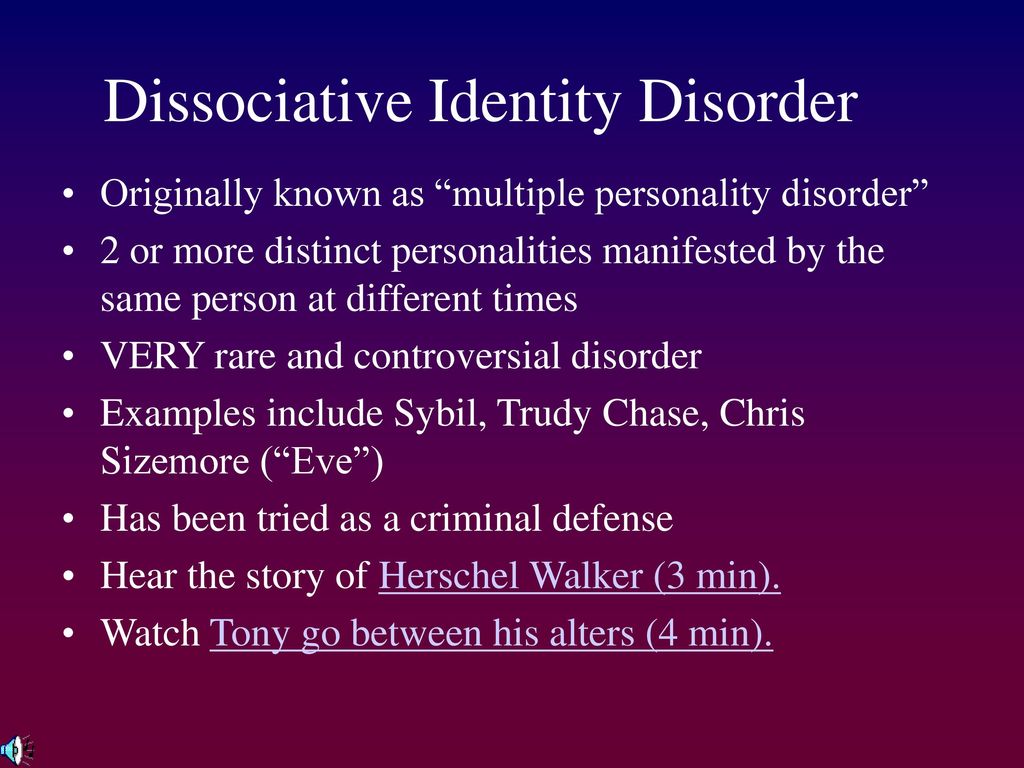 Janie, in her various personalities, was able to testify at length in court on each episode. Her multiple selves helped her retain memories that would otherwise have been lost due to trauma.
Janie, in her various personalities, was able to testify at length in court on each episode. Her multiple selves helped her retain memories that would otherwise have been lost due to trauma.
Prosecutors also called in DID psychologists to explain Janie's condition and assess the credibility of her testimony.
"My memories as someone with MRI are as intact today as they were the day they were formed," Janie told the BBC. After that, she briefly spoke about herself in the plural: "Our memories are just frozen in time. If I need them, I'll just go and get them."
Symphony's intention was to reconstruct "in great detail" the details of the crimes committed during her seven years in Australia. Muscled, burly 18-year-old boy, could testify to the physical abuse, and the elegant young woman Linda had to tell how the abuse affected Janie's performance in school and her ability to connect with people.
Image copyright JENI HAYNES
Image captionThe Haynes family home in Greenacre, Sydney west
Symphony hoped to "use her testimonies to grow up," Janie explains.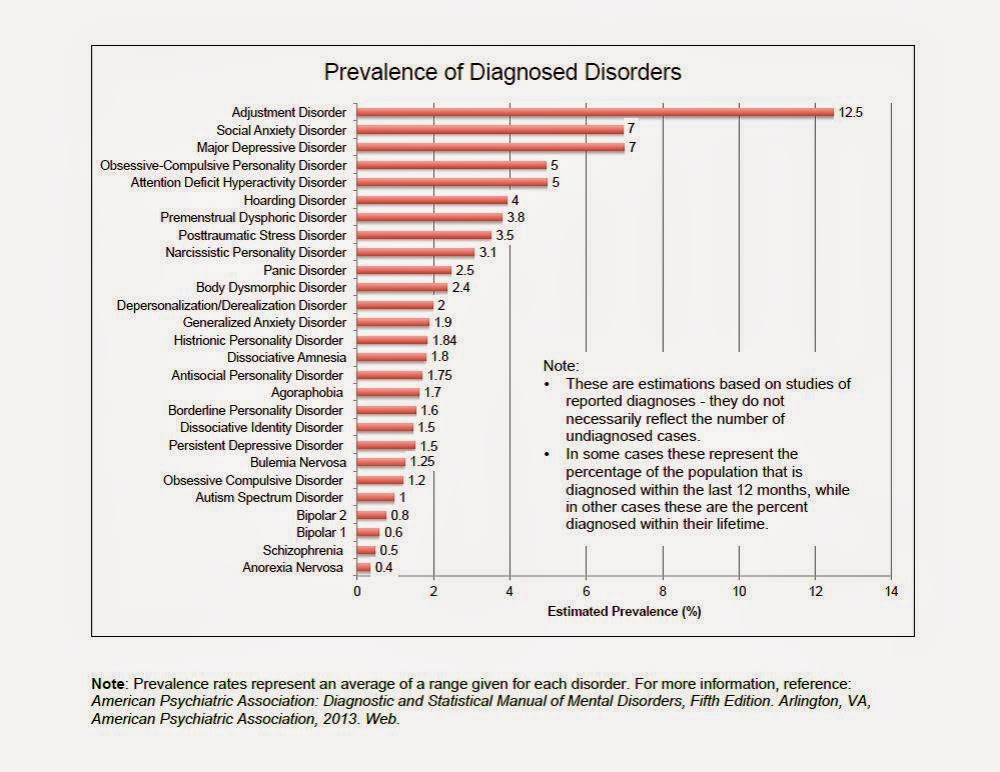 got scared and gave up, couldn't handle it."
got scared and gave up, couldn't handle it."
After more than two hours of Symphony's testimony on the second day of the hearing, Janie's father changed his testimony and pleaded guilty on 25 counts - the worst, according to Janie.
Dozens more were counted towards his sentencing.
"DID saved my life"
"This case is a milestone, to the best of our knowledge, this is the first time that multiple identities of a person with DID have been accepted by the court system and ultimately led to the conviction of the perpetrator," explains Dr. Kathy Keselman is president of the Blue Knot Foundation, an Australian organization that helps survivors of childhood trauma.
Image copyright JENI HAYNES
Image caption,Richard Haynes pleaded guilty to more than two dozen acts of child sexual abuse
Janie first reported the abuse in 2009. The police investigation leading to the sentencing and imprisonment of Richard Haynes lasted 10 years.
In 2017, he was extradited to Australia from Darlington in the North East of England, where he was serving a seven-year sentence for another crime. Before that, he lived with various relatives of Janie, whom he told that his daughter was lying and manipulating people.
Upon learning of Janie's abuse, her mother, who divorced Haynes in 1984, became active in helping her get justice.
But for decades, Janie's attempts to get help with her injuries have met with reluctance from specialists. She says counselors and therapists turned her down because her story made them distrustful or felt so traumatic that they couldn't deal with it themselves.
Dissociative Identity Disorder
- Refusal to communicate - detachment from oneself or the world - is considered a normal reaction to trauma.
- DID can be triggered by experience if a person (especially in childhood) has experienced trauma for a long time.
- Lack of adult support, or the presence of an adult who says the injury was not real, may contribute to the development of DID.
- A person with DID may feel that there are multiple selves within them that think, act, or speak differently and may even have conflicting memories and experiences.
- There is no specific medical treatment for DID - specialists mostly use talking therapy to help patients.
Despite the fact that today this diagnosis is recognized and its existence is evidence-based, DID usually raises doubts among the layman and even some doctors.
"The nature of this condition is such that it causes distrust and discomfort due to its causes. Partly because people find it difficult to believe that children can be subjected to such abuse," says Dr. Stavropoulos. "That's why Janie's case is so important - because this case provides a wider awareness of this very complex, but not uncommon condition, which has not yet been fully accepted.
Janie says her DID saved her life and soul. At the same time, her condition and her trauma led to serious life difficulties.
Photo copyright, JENI HAYNES
Photo caption,Some of Jeni's personalities are very intelligent and experienced adults
Jeni has devoted her entire life to studying, earning her Master's and Doctorate degrees in Law and Philosophy. But she couldn't work full time. She now lives with her mother, and both of them depend on their social pensions.
In her statement of harm, Janie notes that she and her personalities "live in fear, constantly on guard. We must hide our multiplicity and strive for consistency in behavior, relationships, conversations and beliefs, which is often impossible. Very difficult to manage opinions and views, having 2,500 voices inside."
"I shouldn't have lived like this," she says. "Make no mistake, it was my father who caused me to have DID."
On September 6, when my father was sentenced to 45 years in prison, Janie was sitting a few meters away from him.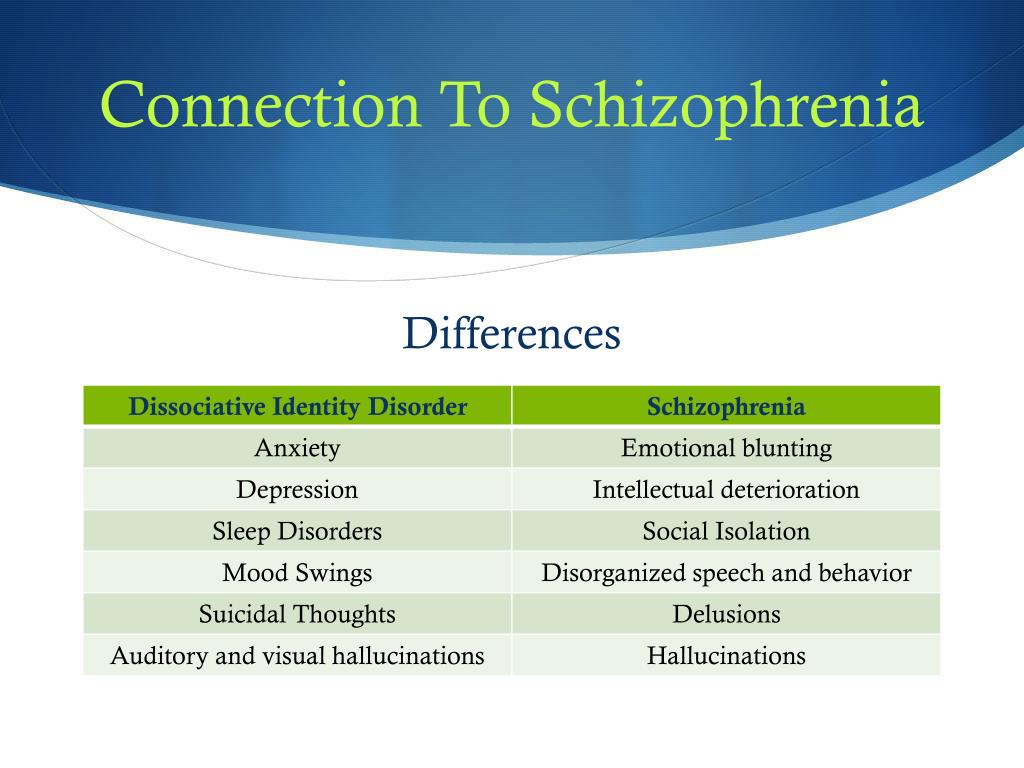 Haynes, a seriously ill man, will not be able to apply for parole until 33 years later.
Haynes, a seriously ill man, will not be able to apply for parole until 33 years later.
At sentencing, Judge Sarah Haggett said it was likely that Haynes would die in prison. His crimes, she said, were "terrifyingly heinous and perverted."
According to the judge, the verdict cannot reflect the seriousness of the harm caused to the defendant.
"I'm passionate about my story," Janie told the BBC before her sentencing. Behind me".
"If you have DID as a result of violence, you can now get justice. You can go to the police and they will believe you. Your diagnosis is no longer an obstacle to justice," Janie says.
I am not alone, I am many
4108
Bookmark
Dissociative identity disorder is one of the types of mental disorders when a person's identity consists of many parts that do not make up a single whole. It is as if several personalities live in a person, who change and do not always know about each other. These states are also called ego states or alters. They may well be of different ages, genders, characters, nationalities, views and values. When switching, memories are not necessarily transferred from one person to another, i.e. a person may partially or not remember events that happened in another ego state.
It is as if several personalities live in a person, who change and do not always know about each other. These states are also called ego states or alters. They may well be of different ages, genders, characters, nationalities, views and values. When switching, memories are not necessarily transferred from one person to another, i.e. a person may partially or not remember events that happened in another ego state.
The disease occurs in 1-3% of the world's population. Until the 2000s, the existence of this disorder was in doubt. But studies have shown that the activity that occurs in the patient's brain, switching between personalities, cannot be repeated. Various factors influence the development of this disorder: childhood trauma, physical, sexual and emotional abuse, and other mental disorders.
Personalities living in the patient may be in a position of "passive influence". They do not act as performers of actions, but can manifest themselves in the form of voices in the head. Then the person perceives this not as his thoughts and can voice what he did not intend or did not even remember. Each person can have their own voices, mannerisms and even names. But the central person may not know about all of them.
Then the person perceives this not as his thoughts and can voice what he did not intend or did not even remember. Each person can have their own voices, mannerisms and even names. But the central person may not know about all of them.
Among the symptoms of dissociative identity disorder, the presence of two or more personality states is distinguished, which manifest themselves in changes in behavior, memory and thinking, as well as gaps in memory, when a person does not remember events that happened to him in certain periods of life. Symptoms can be detected at different ages, including in children and adolescents.
Common signs of a split personality:
- the person does not remember conflicts;
- difficulty walking;
- weakness in arms due to conflicts;
- people swing to relieve the alarm;
- a person feels separation from the body;
- no control over one's desires;
- there is no exact awareness of one's gender identity;
- emotional instability;
- pathological fantasizing;
- boredom and frustration.

Only a doctor makes a diagnosis of a split personality.
Dissociation is a method of psychological defense when a person moves away from what is happening, thinking that it is not connected with him. At this moment, thoughts, feelings, memories are disconnected and lose touch with the awareness of reality. The mechanism helps to avoid unbearable emotional shocks, for example, after a catastrophe, an accident. But with excessive manifestation, it develops dissociative disorders.
There is a version that the first cases of multiple personality appeared in the Paleolithic times, as evidenced by cave paintings. They depict shamans who could turn into animals or let spirits in. Later, such cases were perceived as demon possession. The Swiss Renaissance physician Paracelsus described a woman who had two personalities and stole money from herself.
In 1784, the Marquis Armand Marie-Jacques de Puysegur put his worker Victor into a somnambulistic state with the help of magnetic techniques. Victor was awake in his sleep, but the next morning he did not remember anything. Puysegur called this phenomenon "magnetic somnambulism" and opened a period of study of dissociative identity disorder from the point of view of the theory of magnetic sleep. Cases have been described where the second person of a German girl spoke French and claimed her French aristocratic origin.
Victor was awake in his sleep, but the next morning he did not remember anything. Puysegur called this phenomenon "magnetic somnambulism" and opened a period of study of dissociative identity disorder from the point of view of the theory of magnetic sleep. Cases have been described where the second person of a German girl spoke French and claimed her French aristocratic origin.
The period of dissociation theory began in 1880. Cases of disorder were considered as the presence of several centers of the psyche, which appear in the struggle with traumatic experiences. There is a description of the case of Louis Vivet, who had six personalities with separate memories and patterns of behavior. At this time, books and publications appeared with the stories of patients with dissociative disorder.
In 1973, the book "Sibyl" appeared, which tells the real story of Shirley Ardell Mason, who had 16 personalities. For 10 years, she managed to cure the disorder. Another well-known book about dissociative disorder was written by D.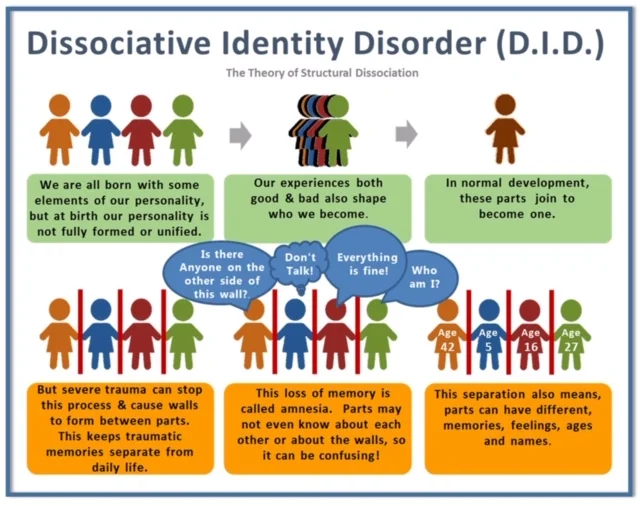 Keyes, The Multiple Minds of Billy Milligan. It is based on an interview with Billy Milligan himself, who had 24 personalities, and his doctor.
Keyes, The Multiple Minds of Billy Milligan. It is based on an interview with Billy Milligan himself, who had 24 personalities, and his doctor.
London-based artist Kim Noble is a contemporary example. At 61, she has 20 personalities, including women, men and children. Most often, her mind is led by Patricia, who is the only one who knows about the bank card where the money comes from. 14 of her personalities paint pictures, and each has its own style, color, approach. Kim has a daughter, but not all individuals know about her, so sometimes a woman thinks that her friends left their child for a while. Social workers check Kim's condition daily and make sure the house has everything she needs. There were many times in Kim Noble's life when a sudden change of personality could end in death. Because of this, as a teenager, she suffered from anorexia, bulimia, and resorted to suicide. One day, Kim was driving a truck and there was a switch to a personality that didn't take her away.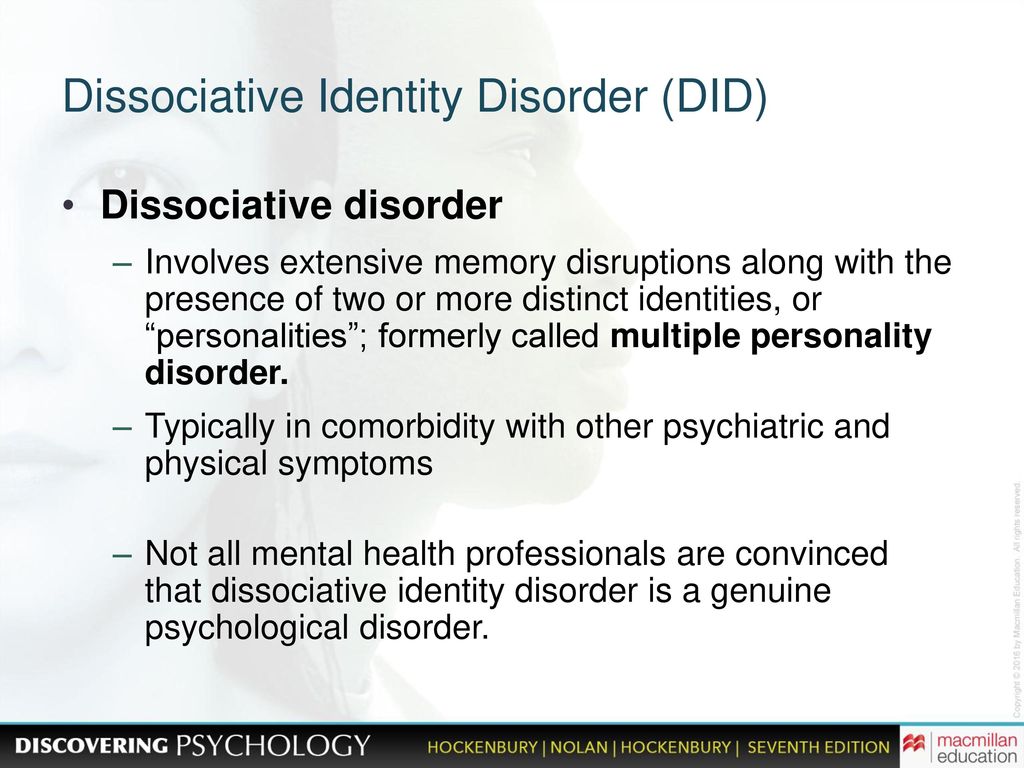 Kim crashed into a row of cars and was arrested. Then she was diagnosed with schizophrenia. Switching between personalities happens 3-4 times a day, the woman herself talks about this. She wrote an autobiographical book, All Me, about her disorder.
Kim crashed into a row of cars and was arrested. Then she was diagnosed with schizophrenia. Switching between personalities happens 3-4 times a day, the woman herself talks about this. She wrote an autobiographical book, All Me, about her disorder.
People with dissociative identity disorder need support and care. Even if they resist, it is important to be patient and help them understand the need for treatment so that the decision can be made on their own. If you follow the recommendations of specialists, you can cope with the disease and improve your life.
Main page photo: kartinkin.net
Page photo: yt3.ggpht.com
Author Olga Skibina
dissociative disorder personality psyche
Source: probolezny.ru, arbat25.ru, ru.wikipedia.org
Information provided by the Information Agency "Scientific Russia". Mass media registration certificate: IA No. ФС77-62580, issued Federal Service for Supervision of Communications, Information Technology and Mass Communications on July 31, 2015.
SCIENCE FOR CHILDREN
SFU scientists have proposed a new method for treating bone defects
17:30 / Medicine
Scientists have created a transparent and ultra-strong material for Russian cosmonautics
16:30 / Chemistry
FIAN has created a chemical magnet for future nanomotors
15:30 / Physics, Chemistry improved Siberian sources
electrons for new generation gadgets14:40 / Mathematics, New technologies, Physics
MTUCI will host the International Conference MoNeTec-2022
14:30 / Information technology
Different types of social spiders use different strategies for group hunting
14:00 / Biology
Scientists have discovered the mechanisms of infection by dangerous parasitic worms of frogs and toads
13:30 / Biology
in the service of Peter I. On the project of deciphering the Emperor's manuscripts - Corresponding Member of the Russian Academy of Sciences Alexei Sirenov13:00 / Information Technology, History, Science and Society, New Technologies, Education, Philology
Academicians of the Russian Academy of Sciences were awarded the President's honorary diplomas for their contribution to the development of science
12:45 / Science and Society, Education
Academicians and Corresponding Members of the Russian Academy of Sciences were awarded state awards of the Russian Federation .