Ssris safe for breastfeeding
Breastfeeding & Psychiatric Medications - MGH Center for Women's Mental Health
Given the prevalence of psychiatric illness during the postpartum period, a significant number of women may require pharmacological treatment while nursing. Appropriate concern is raised, however, regarding the safety of psychotropic drug use in women who choose to breastfeed while taking these medications. While many women with postpartum illness delay treatment because they are worried that the medications they take may harm the nursing infant, the accumulated data indicates that the risk of adverse events in the nursing infant is low.
General Principles
Given the many benefits of breastfeeding, some women taking psychiatric medications may wish to nurse their infants. When making this decision, several variables must be considered. These include the known and unknown risks of medication exposure for the baby via breast milk, the effects of untreated illness in the mother, and the benefits of and maternal preferences for breastfeeding.
There are established health benefits of breastfeeding for babies and mothers.
Efforts have been made to quantify the amount of psychotropic medications and their metabolites in the breast milk of nursing mothers. In order to more accurately measure the infant’s exposure to medication, serum drug levels in the infant have also been assessed. From the available data, it appears that all medications, including antidepressants, antipsychotic agents, mood stabilizers, and benzodiazepines, are secreted into the breast milk. However, concentrations of these agents in breast milk vary considerably. The amount of medication to which an infant is exposed depends on several factors: factors pertaining to the specific medication, the maternal dosage of medication, the frequency of dosing and infant feedings, and the rate of maternal drug metabolism.
The decision to breastfeed while taking medications is more complicated when a baby is premature or has medical complications. The nursing infant’s chances of experiencing toxicity are dependent not only on the amount of medication ingested but also on how well any ingested medication is metabolized.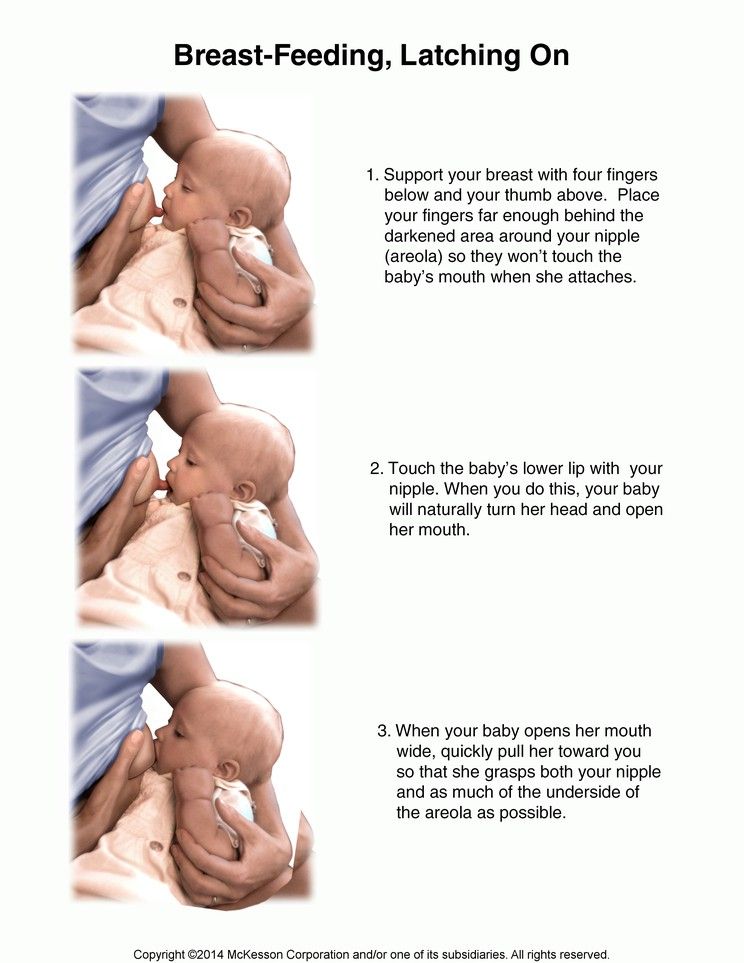 Most psychotropic medications are metabolized by the liver. During the first few weeks of a full-term infant’s life, there is a lower capacity for hepatic drug metabolism, which is about one-third to one-fifth of the adult capacity. Over the next few months, the capacity for hepatic metabolism increases significantly and, by about 2 to 3 months of age, it surpasses that of adults. In premature infants or in infants with signs of compromised hepatic metabolism (e.g., hyperbilirubinemia), breastfeeding typically is deferred because these infants are less able to metabolize drugs and may be more likely to experience adverse events.
Most psychotropic medications are metabolized by the liver. During the first few weeks of a full-term infant’s life, there is a lower capacity for hepatic drug metabolism, which is about one-third to one-fifth of the adult capacity. Over the next few months, the capacity for hepatic metabolism increases significantly and, by about 2 to 3 months of age, it surpasses that of adults. In premature infants or in infants with signs of compromised hepatic metabolism (e.g., hyperbilirubinemia), breastfeeding typically is deferred because these infants are less able to metabolize drugs and may be more likely to experience adverse events.
Antidepressants in general are considered to be relatively safe for use during breastfeeding when clinically warranted, and SSRIs in particular are one of the best studied classes of medications during breastfeeding. Excellent and thorough reviews on the topic of antidepressants and breastfeeding have been published (Burt 2001; Weissman 2004).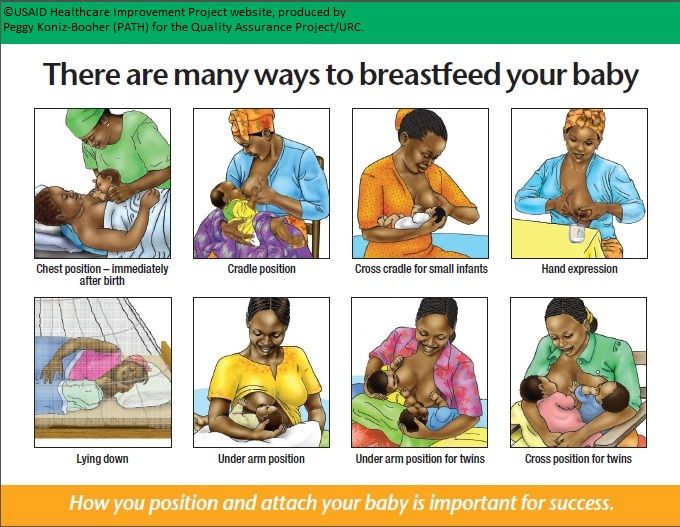 In the most rigorous studies, nursing women have repeatedly provided breast milk samples and infant blood samples in order for investigators to quantify medication exposure to the infant.
In the most rigorous studies, nursing women have repeatedly provided breast milk samples and infant blood samples in order for investigators to quantify medication exposure to the infant.
Data have accumulated regarding the use of various antidepressant medications during breastfeeding. Available data on the use of tricyclic antidepressants (TCAs), fluoxetine, paroxetine, and sertraline during breastfeeding have been encouraging and suggest that the amounts of drug to which the nursing infant is exposed is low and that significant complications related to neonatal exposure to antidepressants in breast milk appear to be rare. Typically very low or non-detectable levels of drug have been detected in the infant serum, and one recent report indicates that exposure to medication in breast milk does not result in clinically significant blockade of serotonin (5-HT) reuptake in infants.
Although less information is available on other antidepressants, serious adverse events related to exposure to these medications have not been reported. There have been a small number of case reports of adverse events in infants exposed to antidepressants in breast milk, including jitteriness, irritability, excessive crying, sleep disturbance, and feeding problems. In many cases it has not been possible to establish a causal link between these events and exposure to drug.
There have been a small number of case reports of adverse events in infants exposed to antidepressants in breast milk, including jitteriness, irritability, excessive crying, sleep disturbance, and feeding problems. In many cases it has not been possible to establish a causal link between these events and exposure to drug.
Many clinicians and their patients ask which antidepressant is the “safest” for breastfeeding. It is somewhat misleading to say that certain medications are “safer” than others. All medications taken by the mother are secreted into the breast milk, and there is no evidence to suggest that certain antidepressants pose significant risks to the nursing infant.
In terms of selecting an appropriate antidepressant, one should try to choose an antidepressant for which there are data to support its safety during breastfeeding (i.e., sertraline, paroxetine, fluoxetine, tricyclic antidepressants). However, some situations may warrant the use of antidepressants with less available safety data. For example, if a woman has responded to a particular antidepressant in the past, it would be reasonable to consider using that antidepressant again. If she has been taking an antidepressant during the course of her pregnancy and has been doing well, it would be prudent to continue with that same antidepressant after delivery, as switching to another antidepressant may put her at increased risk for relapse.
For example, if a woman has responded to a particular antidepressant in the past, it would be reasonable to consider using that antidepressant again. If she has been taking an antidepressant during the course of her pregnancy and has been doing well, it would be prudent to continue with that same antidepressant after delivery, as switching to another antidepressant may put her at increased risk for relapse.
We do not regularly measure drug levels in the breastfeeding mother or baby; however, there may be certain situations where information on exposure to drug in the child may help make decisions regarding treatment. If there is a significant change in the child’s behavior (e.g., irritability, sedation, feeding problems, or sleep disturbance), an infant serum drug level may be obtained. If levels are high, breastfeeding may be suspended. Similarly if the mother is taking a particularly high dosage of medication, it may be helpful to measure drug levels in the infant to determine the degree of exposure.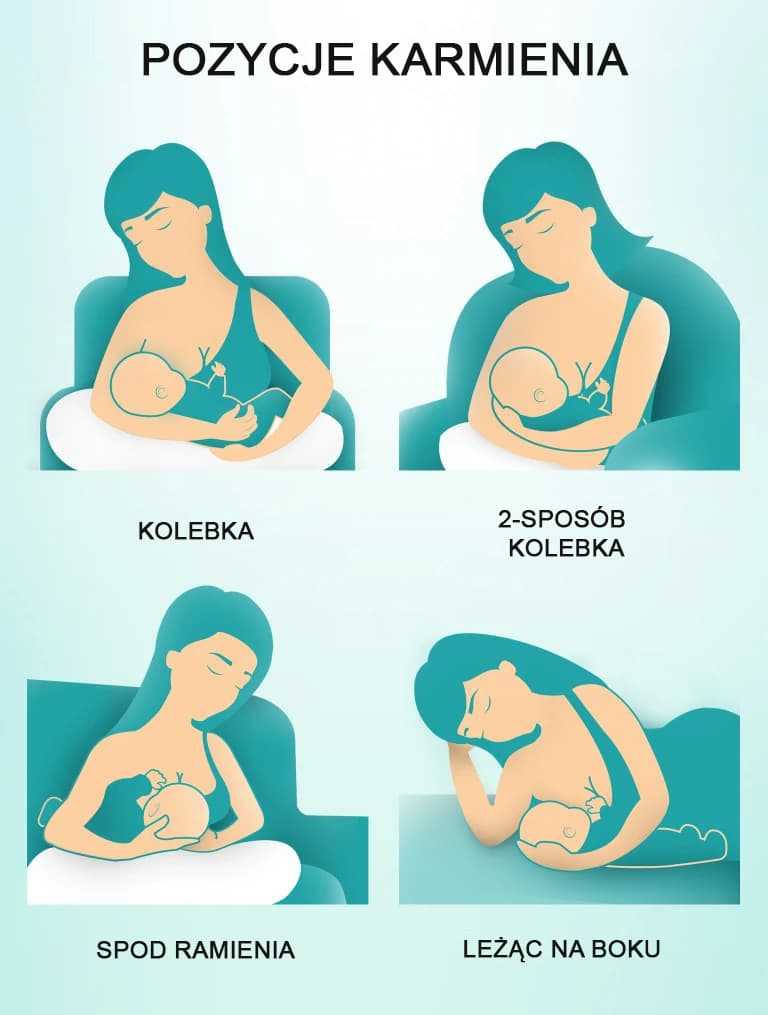
Anti-Anxiety Agents
Given the prevalence of anxiety symptoms during the postpartum period, anxiolytic agents are often used in this setting. Data regarding the use of benzodiazepines have been limited; however, the available data suggest that amounts of medication to which the nursing infant is exposed are low. Case reports of sedation, poor feeding, and respiratory distress in nursing infants have been published; however, the data, when pooled, suggest a relatively low incidence of adverse events in infants exposed to benzodiazepines in the breast milk.
Mood Stabilizers
For women with bipolar disorder, breastfeeding may pose more significant challenges. First, on-demand breastfeeding may significantly disrupt the mother’s sleep and thus may increase her vulnerability to relapse during the acute postpartum period. Second, there have been reports of toxicity in nursing infants related to exposure to various mood stabilizers, including lithium and carbamazepine, in breast milk.
Lithium is excreted at relatively high levels in the mother’s milk, and infant serum levels are about one-third to one-half of the mother’s serum levels. Reported signs of toxicity in nursing infants have included cyanosis, hypotonia, and hypothermia. Although breastfeeding typically is avoided in women taking lithium, some women may choose to use lithium while nursing. In this setting, the lowest possible effective dosage should be used and both maternal and infant serum lithium levels should be followed. In collaboration with the pediatrician, the child should be monitored closely for signs of lithium toxicity, and lithium levels, thyroid stimulating hormone (TSH), blood urea nitrogen (BUN), and creatinine should be monitored every 6-8 weeks while the child is nursing.
Several recent studies have suggested that lamotrigine reaches infants through breast milk in variable doses, with infant serum levels ranging from 20%-50% of the mother’s serum concentrations. In addition, maternal serum levels of lamotrigine increase significantly after delivery, which may contribute to the high levels found in nursing infants. None of these studies have reported any adverse events in breastfeeding newborns. To read more on the safety of lamotrigine versus lithium, please reference this past blog.
None of these studies have reported any adverse events in breastfeeding newborns. To read more on the safety of lamotrigine versus lithium, please reference this past blog.
One worry shared by clinicians and new mothers is the risk for Stevens-Johnson syndrome (SJS). This is a severe, potentially life-threatening rash, most commonly resulting from a hypersensitivity reaction to a medication, which occurs in about 0.1% of bipolar patients treated with lamotrigine. Thus far, there have been no reports of SJS in infants associated with exposure to lamotrigine. In fact, it appears that cases of drug-induced SJS are extremely rare in newborns. Despite the variable levels of medication found in infants in studies to date, none of these studies have reported any adverse events in the breastfeeding newborns. More research is required to assess the safety of lamotrigine in nursing infants, and decisions regarding the use of this drug in breastfeeding women involves a careful consideration of the risks and benefits of using this medication.
Although the American Academy of Pediatrics has deemed both carbamazepine (Tegretol) and valproic acid (Depakote) to be appropriate for use in breastfeeding mothers, few studies have assessed the impact of these agents on infant well-being. Both of these mood stabilizers have been associated in adults with abnormalities in liver function and fatal hepatotoxicity. Hepatic dysfunction secondary to carbamazepine exposure in breast milk has been reported several times. Most concerning is that the risk for hepatotoxicity appears to be greatest in children younger than 2 years of age; thus, nursing infants exposed to these agents may be particularly vulnerable to serious adverse events. In those women who choose to use valproic acid or carbamazepine while nursing, routine monitoring of drug levels and liver function tests in the infant is recommended. In this setting, ongoing collaboration with the child’s pediatrician is crucial.
Antipsychotic Agents
Information regarding the use of antipsychotic drugs is limited and is particularly lacking for the newer atypical agents. While the use of chlorpromazine has been associated with adverse events including sedation and developmental delay, adverse events appear to be rare when medium- or high-potency agents are used.
While the use of chlorpromazine has been associated with adverse events including sedation and developmental delay, adverse events appear to be rare when medium- or high-potency agents are used.
Less data, however, is available on the atypical antipsychotic agents. Data on clozapine suggest that it may be concentrated in the breast milk; however, there are no data on infant serum levels, making it difficult to interpret the relevance of this finding. Given the severity of adverse events associated with clozapine exposure in adults (i.e., decreased white blood cell count), the use of this medication should be reserved for those with treatment-refractory illness, and monitoring of white blood cell counts in the nursing infant is mandatory.
There is very limited data on the use of other atypical antipsychotic agents during lactation; however, limited data available on olanzapine, risperidone, and quetiapine suggest that the excretion of these medications in breast milk is low and that adverse effects appear to be rare. Monitoring of the infant is encouraged, as there has been one report of an infant who had sedation on a higher dose of olanzapine, which resolved after the mother’s dose was halved to 5mg/day. To date, there have been no reports on the use of the antipsychotic medications, ziprasidone (Geodon) and aripiprazole (Abilify) while breastfeeding.
Monitoring of the infant is encouraged, as there has been one report of an infant who had sedation on a higher dose of olanzapine, which resolved after the mother’s dose was halved to 5mg/day. To date, there have been no reports on the use of the antipsychotic medications, ziprasidone (Geodon) and aripiprazole (Abilify) while breastfeeding.
Treatment Guidelines
Consultations regarding the safety of psychiatric medications in breastfeeding women should include a discussion of the known benefits of breastfeeding to mother and infant and the possibility that exposure to medications in the breast milk may occur. Although routine assay of infant serum drug levels was recommended in earlier treatment guidelines, this procedure is probably not warranted; in most instances low or non-detectable infant serum drug levels will be evident and serious adverse side effects are rarely reported. This testing is indicated, however, if neonatal toxicity related to drug exposure is suspected. Infant serum monitoring is also indicated when the mother is nursing while taking lithium, valproic acid, carbamazepine, or clozapine.
Infant serum monitoring is also indicated when the mother is nursing while taking lithium, valproic acid, carbamazepine, or clozapine.
We have varying amounts of study pertaining to individual medications, with SSRIs being among the best studied medications in breastfeeding. Also, data that is available informs most specifically on the short-term safety of these medications, and long term systematic data are unavailable. Therefore, in each individual case, the known and unknown risks of exposure must be balanced with the risks of untreated maternal illness in the mother and her desire to breastfeed.
For the latest information on breastfeeding and psychiatric medication, please visit our blog.
How do I get an appointment?
Despite the high rate of postpartum depression seen in women after childbirth, the illness is frequently not treated because of women’s wish to breastfeed. Clinical consultation is offered to women who may benefit from use of medication while breastfeeding, taking into account all available information regarding the safety of this practice during lactation. Consultations regarding treatment options can be scheduled by calling our intake coordinator at 617-724-7792.
Consultations regarding treatment options can be scheduled by calling our intake coordinator at 617-724-7792.
At this time the Center does not have any active studies investigating breastfeeding and psychiatric medications. New studies may become active in the near future. In order to remain informed about any studies for which you may be eligible, click here
Antidepressant Use While Breastfeeding: What should I know?
The postpartum period can be a magical time when a mom finally gets to meet and spend time with their new baby. However, this time can also be challenging for many mothers. It is estimated that at least 1 in 7 mothers suffers from postpartum depression.1 Psychotherapy (counseling) is certainly useful during this time, but medication may also be necessary to adequately treat psychiatric illnesses. Needing and taking new medications while breastfeeding can bring about many questions. The InfantRisk Center is here to help you find answers.
Risks of NOT treating depression vs risks of taking antidepressants
Like any other medication, antidepressants have the potential to cause side effects (specific risks associated with medications are discussed in detail below). The side effects of these drugs have been the focus of many articles. Your provider’s first choice of antidepressants used are generally the ones with the lowest risk for harm.1
The side effects of these drugs have been the focus of many articles. Your provider’s first choice of antidepressants used are generally the ones with the lowest risk for harm.1
Importantly, the risks of not taking antidepressants when they are indicated can also cause serious risks to both mother and infant. Women who discontinue their antidepressants during or after pregnancy are three times more likely to develop another episode of depression when compared with women who continued to use antidepressants throughout the perinatal period.2 Similarly, one study found that adolescent mothers with untreated depression have a 20% increased frequency of suicide attempts.3
Untreated maternal depression can also affect the infant. One study found that infants of mothers with untreated depression had a lower social engagement score at 9 months when compared to infants of nondepressed mothers.4 Furthermore, results from 10 studies showed that maternal depression was associated with certain behavioral traits in infants including increased behavioral problems at age two, more difficult temperament, and less mature regulatory behavior. 4 Other studies have demonstrated that untreated depression hindered the development of the maternal-infant relationship and caused difficulty bonding when compared to the relationship between infants and mothers who were not depressed.4 Therefore, while antidepressant use can carry some side effects, this is generally preferred to untreated depression.
4 Other studies have demonstrated that untreated depression hindered the development of the maternal-infant relationship and caused difficulty bonding when compared to the relationship between infants and mothers who were not depressed.4 Therefore, while antidepressant use can carry some side effects, this is generally preferred to untreated depression.
How is the most appropriate antidepressant chosen during breastfeeding?
When a medication is necessary to treat depression, several factors are considered in prescribing an antidepressant. First, if a mom was successfully treated with a certain drug during pregnancy, she should continue that same drug. Similarly, if a mother has a history of successful treatment with a particular antidepressant outside of pregnancy, there is a good chance that it will work well postpartum.1 Second, specific side effects of different antidepressants should be considered as well as their relative infant dose (RID). The RID is the comparative amount of a medication that the infant receives through breastmilk relative to the dose of a medication that the mother receives.5 The current accepted RID threshold for safety is less than 10%.1
The RID is the comparative amount of a medication that the infant receives through breastmilk relative to the dose of a medication that the mother receives.5 The current accepted RID threshold for safety is less than 10%.1
What are the side effects and RIDs of specific antidepressants?
The InfantRisk Center believes that all parents should be empowered to make evidence-informed decisions together with their healthcare providers. While we will report adverse effects of antidepressants below, please remember than many mothers successfully breastfeed healthy infants while on antidepressants. We simply want you to be aware of the risks and benefits, and will report the rare instances we have of infant harm to provide a balanced picture.
Selective Serotonin Reuptake Inhibitors (SSRIs)
In general, SSRIs are considered first-line for treating depression while breastfeeding, but SSRIs differ from each other in important ways. For example, sertraline (RID of 0.5%) and paroxetine (RID of 1-1.5%) typically have undetectable blood levels in infants when breastfeeding moms use them.1 Paroxetine is considered to be safe while breastfeeding, but should be avoided during pregnancy due to possible harmful effects that it can have on a growing fetus.1 Other antidepressants like citalopram (RID of 4-8%) and escitalopram (RID of 3.5-4%) are also considered safe while breastfeeding, but may cause mild side effects like drowsiness and irritability in breastfed infants. Fluoxetine has an RID of 6%, which is under the general cutoff of 10%, but is not an ideal choice for breastfeeding. It has a very long half-life (meaning it takes a long time for it to break down in the body), and can accumulate in infants. Infant blood levels of fluoxetine may reach more than half of maternal blood levels. It may take an infant a long time to metabolize (break down) these high levels of drug after discontinuing the drug or breastfeeding.
For example, sertraline (RID of 0.5%) and paroxetine (RID of 1-1.5%) typically have undetectable blood levels in infants when breastfeeding moms use them.1 Paroxetine is considered to be safe while breastfeeding, but should be avoided during pregnancy due to possible harmful effects that it can have on a growing fetus.1 Other antidepressants like citalopram (RID of 4-8%) and escitalopram (RID of 3.5-4%) are also considered safe while breastfeeding, but may cause mild side effects like drowsiness and irritability in breastfed infants. Fluoxetine has an RID of 6%, which is under the general cutoff of 10%, but is not an ideal choice for breastfeeding. It has a very long half-life (meaning it takes a long time for it to break down in the body), and can accumulate in infants. Infant blood levels of fluoxetine may reach more than half of maternal blood levels. It may take an infant a long time to metabolize (break down) these high levels of drug after discontinuing the drug or breastfeeding. Therefore, fluoxetine may lead to longer-lasting infant side effects.1
Therefore, fluoxetine may lead to longer-lasting infant side effects.1
Tricyclic Antidepressants (TCAs)
TCAs have low RIDs of 1-2% and infant levels are usually either low or undetectable, however, these drugs are typically not first-line due to their numerous side effects in mothers and infants. For example, one case report of a breastfeeding mom who used amitriptyline showed that an infant developed extreme drowsiness, while many other infants tolerate it well.1 A different report where a breastfeeding mom used doxepin reported that her 8-week-old breastfed infant was found pale, limp, somnolent, and almost not breathing 4 days after doxepin dosage was increased from 10 mg daily to 25 mg three times a day (a 7-fold increase in dose). As a result, doxepin is typically avoided during breastfeeding. A TCA that is a good alternative to SSRIs is nortriptyline. It has few maternal adverse reactions, no active metabolites, and no reports of infant adverse events via breastfeeding thus far. 1 Currently, TCA’s are commonly used in addition to other antidepressants. In these cases, the dose of the TCA is often much lower, which substantially reduces the risk of adverse effects to both mom and infant. Many mothers breastfeed successfully while taking TCAs without infant side effects.
1 Currently, TCA’s are commonly used in addition to other antidepressants. In these cases, the dose of the TCA is often much lower, which substantially reduces the risk of adverse effects to both mom and infant. Many mothers breastfeed successfully while taking TCAs without infant side effects.
Serotonin Norepinephrine Reuptake Inhibitors (SNRIs)
Desvenlafaxine and venlafaxine have an RID of 6.5%. Infants whose mothers take desvenlafaxine have serum levels that range from undetectable to 37% of maternal levels. These SNRIs have caused drowsiness and/or agitation in some cases. Overall, they have few adverse reactions and there is no evidence that suggests they hinder development.1
Bupropion
Bupropion has a low transfer rate through breastmilk with an RID of 1.4-10.6%. Although research on its effects during breastfeeding is scarce, two babies who were breastfed by mothers using bupropion developed seizures.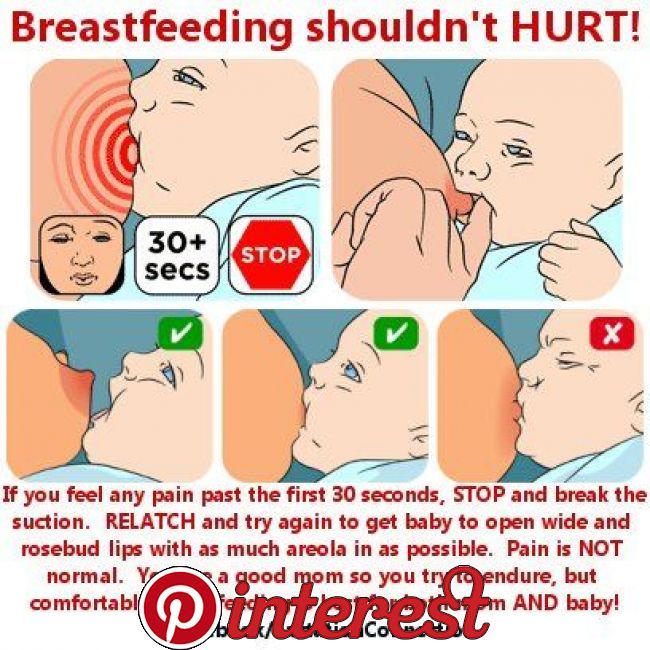 1 It is unknown if the seizures were directly related to bupropion in milk. An increased risk for seizures is a known adverse effect of bupropion in adults and infants. Adults and children with seizure disorders should avoid bupropion. Bupropion should be avoided in breastfeeding mothers if they believe their infant is at a high risk for seizures. For example, infants with a previous or family history of seizures, some infant heart malformations, strokes, head injuries, or some brain tumors or infections may be at higher risk of future seizures and should not be exposed to bupropion. However, if other drugs are ruled out, it may still be possible to safely breastfeed infants with low seizure risks while on bupropion.6
1 It is unknown if the seizures were directly related to bupropion in milk. An increased risk for seizures is a known adverse effect of bupropion in adults and infants. Adults and children with seizure disorders should avoid bupropion. Bupropion should be avoided in breastfeeding mothers if they believe their infant is at a high risk for seizures. For example, infants with a previous or family history of seizures, some infant heart malformations, strokes, head injuries, or some brain tumors or infections may be at higher risk of future seizures and should not be exposed to bupropion. However, if other drugs are ruled out, it may still be possible to safely breastfeed infants with low seizure risks while on bupropion.6
Other Antidepressants
There are many other options for depression treatment. Most have not yet been studied in lactating women and their infants. For more information, please call the InfantRisk Center to speak to a nurse or download our app MommyMeds.
How can antidepressant use during pregnancy affect breastfeeding?
Mothers who took antidepressants during pregnancy may need more help with breastfeeding. Selective Serotonin Reuptake Inhibitors (SSRIs) can delay the onset of milk secretion if taken during the last trimester of pregnancy.1 In regards to the newborn, taking antidepressants during the third trimester can cause a transient discontinuation syndrome which can make breastfeeding more challenging as it may result in decreased sucking and feeding, irritability, sleep disorders, hyperreflexia, and tremors among other side effects.1 Symptoms of discontinuation syndrome typically present around 48 hours after birth and typically resolve after 24-48 hours.7 Additionally, simply having depression during or before pregnancy is often enough to warrant more assistance with breastfeeding.1 These mothers can prepare for a successful breastfeeding journey by alerting their lactation consultants and supportive networks that they may need additional help.
Take away message
The right antidepressant for a breastfeeding mother can vary greatly depending on how that particular person (and their infant) metabolize the medication. It is important to consider if they have ever been treated successfully with a certain antidepressant in the past because this has a higher chance of being successful, even while breastfeeding.1 For previously untreated moms, the safest options during breastfeeding include sertraline and paroxetine since they have been comprehensively studied, have few adverse effects in the baby, and appear in low concentrations in milk. Bupropion can be used with caution due to its potential to increase risk of seizures in the infant.1 In regards to doxepin and fluoxetine, alternatives should be explored first since the potential side effects of these antidepressants are severe as mentioned above.1 Overall, it is important to note that although antidepressants do carry side effects, the alternative of having untreated depression could hinder parenting, lead to substantial developmental risks in the infant and also negatively impact breastfeeding itself. If you have concerns about your mental health, please speak with your healthcare provider for help.
If you have concerns about your mental health, please speak with your healthcare provider for help.
Diego Regalado, MS3
Christine D Garner, PhD, RD
Kaytlin Krutsch, PharmD
References
1. Anderson PO. Antidepressants and Breastfeeding. Breastfeed Med. 2021;16(1):5-7.
2. Womersley K, Ripullone K, Agius M. What are the risks associated with different Selective Serotonin Re-uptake Inhibitors (SSRIs) to treat depression and anxiety in pregnancy? An evaluation of current evidence. Psychiatr Danub. 2017;29(Suppl 3):629-644.
3. Bałkowiec-Iskra E, Mirowska-Guzel DM, Wielgoś M. Effect of antidepressants use in pregnancy on foetus development and adverse effects in newborns. Ginekol Pol. 2017;88(1):36-42.
4. Slomian J, Honvo G, Emonts P, Reginster JY, Bruyère O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Womens Health (Lond). 2019;15:1745506519844044.
2019;15:1745506519844044.
5. Hotham N, Hotham E. Drugs in breastfeeding. Aust Prescr. 2015;38(5):156-159.
6. Uguz F. A New Safety Scoring System for the Use of Psychotropic Drugs During Lactation. American Journal of Therapeutics. 2021;28(1):e118-e126.
7. Hale TW, Kendall-Tackett K, Cong Z, Votta R, McCurdy F. Discontinuation syndrome in newborns whose mothers took antidepressants while pregnant or breastfeeding. Breastfeed Med. 2010;5(6):283-288.
Can I take antidepressants while breastfeeding? - Empathy
At the beginning of August, WHO initiated the Breastfeeding Support Week around the world, the purpose of which is to remind women about the benefits of natural breastfeeding. We will touch upon such an urgent issue as the treatment of depression in nursing mothers.
Is it safe to take antidepressants while breastfeeding? Should breastfeeding mothers stop taking drugs? nine0006 The Deputy Chief Physician of the Empathy Center, Candidate of Medical Sciences, psychiatrist Irina Valerievna Gorshkova answers:
“The desire to continue breastfeeding is often the main reason women refuse to see a psychiatrist. This is not at all surprising, because the instructions for prescribed drugs may indicate that there is no data on their safety for nursing mothers, or it is written that the drug passes into breast milk. In this regard, there is often an opinion that taking antidepressants by a young mother is not safe for a child. However, this statement can be disputed. nine0003
This is not at all surprising, because the instructions for prescribed drugs may indicate that there is no data on their safety for nursing mothers, or it is written that the drug passes into breast milk. In this regard, there is often an opinion that taking antidepressants by a young mother is not safe for a child. However, this statement can be disputed. nine0003
For more than 10 years, studies have been conducted and published that prove the safety of using antidepressants during breastfeeding (mainly SSRIs). There are also many studies confirming the need to treat depression in a woman in the postpartum period, which directly affects the health of not only the mother, but also the baby. In simple terms, sometimes prescribing antidepressants while breastfeeding is a much smarter and safer decision than leaving a woman in a depressed state. nine0003
Breastfeeding is very important for the full development of the child, moreover, its beneficial effect on the health of both the baby and the mother has long been known. Therefore, unjustified cancellation of breastfeeding due to fear of antidepressants can negatively affect both the condition of the child and the psycho-emotional state of the woman, cause her to feel guilty and inferior.
Therefore, unjustified cancellation of breastfeeding due to fear of antidepressants can negatively affect both the condition of the child and the psycho-emotional state of the woman, cause her to feel guilty and inferior.
Prescribing antidepressants during breastfeeding is not only possible but necessary , provided that the doctor correlates the expected benefits and possible risks of taking the drug. And let's not forget that the treatment of depression involves not only medication, but also psychotherapy. With a mild degree of severity of a depressive episode, preference is given precisely to psychotherapeutic methods. Medication support is most often prescribed in combination with psychotherapy.”
How can we help?
nine0002 If you have found some of the described symptoms in yourself or your loved ones, this may indicate the development of a mental disorder. In this case, it is worth contacting a psychiatrist for diagnosis and initiation of timely treatment. In addition to face-to-face communication , we offer remote consultation service (online reception) , which is not inferior to a face-to-face meeting in terms of quality. Thus, you can get qualified help from a high-level specialist , no matter where you are located. nine0036 In addition to face-to-face communication , we offer remote consultation service (online reception) , which is not inferior to a face-to-face meeting in terms of quality. Thus, you can get qualified help from a high-level specialist , no matter where you are located. nine0036 |
In our center for mental health and psychological assistance, within walking distance from the Elektrozavodskaya metro station (Moscow) and the Novokosino metro station (Reutov), specialists who have extensive experience in treating mental disorders work. We use the most modern and advanced techniques, guided by the principles of evidence-based medicine. Effective assistance and confidentiality of information constituting a medical secret are guaranteed. nine0003
ANTIDEPRESSANTS. Breastfeeding
ANTIDEPRESSANTS
My doctor puts me on antidepressants and tells me to stop breastfeeding my baby, but I don't want to stop breastfeeding. Can I take antidepressants and continue to breastfeed my baby?
Can I take antidepressants and continue to breastfeed my baby?
Yes, but be careful. Most commonly used antidepressants belong to a group of medications collectively known as SSRIs (selective serotonin inhibitory maintenance drugs), such as Prozac (fluoxetine), Paxil (paroxetine), and Zoloft (sertraline). All of these medications work in a similar way, increasing levels of naturally occurring, mood-enhancing neurochemical serotonins in the brain. They differ mainly in the strength of their action and possible side effects. Their effect on different people is slightly different. Sertraline appears to be the safest drug to take while breastfeeding. In studies of infants whose mothers took sertraline, the drug was not found in the blood of infants or was present in small amounts. Next on our list is paroxetine, and the last thing we would recommend is fluoxetine, even though it is compatible with breastfeeding. There was a case of colic in an infant whose mother was taking fluoxetine. nine0003
nine0003
Consider alternatives before taking antidepressants. It may be a little reassuring to know that those mothers who required antidepressants before having a baby found that the relaxing effects of breastfeeding allowed them to significantly reduce their dosage or even stop taking these drugs altogether. In practice, the real cures are the ways to reduce stress in chapter 3. Mild depression can often be cured with simple changes in your lifestyle. Try using the O.S.O.P. (see Chapter 4), which emphasizes lifestyle, exercise, attitude change and nutrition. All four factors working together alleviate symptoms of depression. nine0003
Doctors sometimes recommend stopping breastfeeding for mothers who are taking antidepressants or other psychiatric medications because they feel it is the easiest and safest alternative. You may need to seek more information or get your doctor to learn more about breastfeeding medication. Reassure your healthcare provider that you would like to continue breastfeeding and that it is an important part of your care and upbringing of your baby. Abruptly stopping breastfeeding can cause depression in itself, so the impact of weaning on your feelings shouldn't be lightly dismissed. Make it clear to your doctor that you want to find a safe alternative. If depression makes you unable to effectively protect yourself and your child's interests, enlist the support of your spouse or a friend who is good at expressing your thoughts in conversations with the doctor. nine0003
Abruptly stopping breastfeeding can cause depression in itself, so the impact of weaning on your feelings shouldn't be lightly dismissed. Make it clear to your doctor that you want to find a safe alternative. If depression makes you unable to effectively protect yourself and your child's interests, enlist the support of your spouse or a friend who is good at expressing your thoughts in conversations with the doctor. nine0003
If both you and your doctor feel that you still need to take SSRI drugs, start with sertraline at the lowest dose that will achieve the desired effect.
If this does not work, consult your doctor and try paroxetine. If your doctor wants you to take fluoxetine, start at a low dose and then increase it gradually. If you require higher doses of these medicines and are concerned that they will affect your baby, ask your doctor to measure your baby's SSRI drug levels twice, preferably two to six hours after you take the medicine. Remember that these studies must be performed in a specialized laboratory and can be expensive. We would recommend resorting to such extreme circumstances only if you are taking relatively high doses of fluoxetine. A low blood level of the drug in an infant will reassure you that you can safely take fluoxetine while breastfeeding. nine0003
We would recommend resorting to such extreme circumstances only if you are taking relatively high doses of fluoxetine. A low blood level of the drug in an infant will reassure you that you can safely take fluoxetine while breastfeeding. nine0003
Make sure you are not taking an SSRI or any other antidepressant in combination with any other medicine without first checking with your doctor and/or pharmacist. SSRI drugs are incompatible with the following drugs: lithium, cimetidine (a decongestant), theophylline-containing drugs, anticonvulsants and other antidepressants.
Lithium, used to treat manic depression, is a drug that should be used with caution in mothers who are breastfeeding. If all alternatives have been explored and you and your doctor believe that this medicine is right for you and temporary weaning is not desirable, lithium can be taken while breastfeeding if the baby's lithium levels are closely monitored, approximately every two to four weeks. As with all drugs, more frequent feedings and younger infants increase the risk. nine0003
nine0003
Most antidepressants in the tricyclic category can be considered safe during breastfeeding, with the exception of doxepin. Elavil (amitriptyline) is safe to take while breastfeeding. Although a single dose of Valium (diazepam) is considered safe during breastfeeding, long-term use is not recommended.
Although St. John's Wort (Hypericum perforatum) is an effective antidepressant that has been scientifically proven, it has not been shown to be safe for breastfeeding mothers. There is an authoritative opinion that it can reduce maternal milk production. If you are advised to use St. John's wort as an antidepressant, it would be wise to consult your family doctor about the results of the latest studies on the safety of this drug in breastfeeding. Like many herbs, St. John's wort requires individual dosage and careful monitoring of the effect produced. Some mothers can safely take this herb without any change in milk flow or effect on the baby, others may not. nine0003
nine0003
The good news is that many antidepressants are safe to use while breastfeeding if prescribed precautions are followed. In fact, some mothers even enjoy the increase in milk supply after taking psychotherapeutic drugs, but this is certainly no reason to take them. Interestingly, some mothers who required antidepressants before pregnancy do not need these drugs during breastfeeding or may take reduced dosages. nine0003
17. Antidepressants
17. Antidepressants Contraindications: myasthenia gravis, hypersensitivity to the components of the drug. These are medicinal substances that eliminate the symptoms of depression in neuropsychiatric and somatic patients. In most cases, drug interactions
nine0024 Antidepressants Antidepressants The first medicinal substances that were used in the treatment of depression appeared at the end of the 50s of the last century. In 1957, when studying the action of some anti-tuberculosis drugs, attention was paid to their euphoric effect. Preparation,
In 1957, when studying the action of some anti-tuberculosis drugs, attention was paid to their euphoric effect. Preparation,
Antidepressants
Antidepressants These drugs have a selective effect on depression, they can be used in combination with neuroleptics to relieve affective-delusional syndromes. Moclobemide (Aurorix) is a selective MAO inhibitor type A. It is characterized by
Antidepressants
Antidepressants Antidepressants are psychotropic drugs, the action of which is primarily aimed at eliminating a depressive state. In a person prone to depression, they remove (or reduce) melancholy, lethargy, depressed mood, and
ANTIDEPRESSANTS
ANTIDEPRESSANTS My doctor puts me on antidepressants and suggests that I stop breastfeeding my baby, but I don't want to stop breastfeeding.