Can you take cymbalta at night
How To Sleep While Taking Cymbalta: What To Know
Cymbalta is a prescription medication that can help alleviate symptoms of depression, anxiety, and chronic pain.
But it can also have side effects, most commonly nausea, fatigue, and dry mouth.
Many people starting Cymbalta also have insomnia, or difficulty sleeping.
Poor sleep can have adverse effects on your physical health, and it can also make it difficult to find joy in daily life activities, a common goal for many people seeking treatment for mental health conditions.
In this article, I’ll describe how Cymbalta works, how it may affect your sleep, and some strategies that may help to improve your sleep while taking Cymbalta.
I’ll also tell you some signs that you should talk to your doctor.
What is Cymbalta?
Cymbalta is a type of medication called a serotonin and norepinephrine reuptake inhibitor, or SNRI.
SNRIs work by affecting chemicals in the brain known as neurotransmitters.
These neurotransmitters (serotonin and norepinephrine) can help regulate mood, stress, and even pain perception.
Because Cymbalta works by affecting two specific neurotransmitters, it can also be referred to as a dual reuptake inhibitor or dual-acting antidepressant.
Feeling Down?
Take our free assessment and learn about your options.
Get Started
What does it treat?
Cymbalta is often prescribed to treat major depressive disorder, or MDD.
It can also be prescribed to treat:
- Generalized anxiety disorder (GAD)
- Chronic pain, including fibromyalgia, arthritis, and diabetic neuropathy
It can take between 2-8 weeks for Cymbalta to start taking effect.
Some mild side effects can occur during that period, including nausea, dizziness, fatigue, dry mouth, and insomnia.
Many of these side effects will resolve on their own, but not always.
To ensure you’re reducing the risk for side effects as much as possible, take Cymbalta exactly as directed by your provider.
Don’t take Cymbalta more or less frequently than recommended by your provider, and don’t double up on doses.
If you feel that you need to adjust your Cymbalta dose, don’t do so on your own.
Talk to your prescriber before making any changes.
Cymbalta and Insomnia
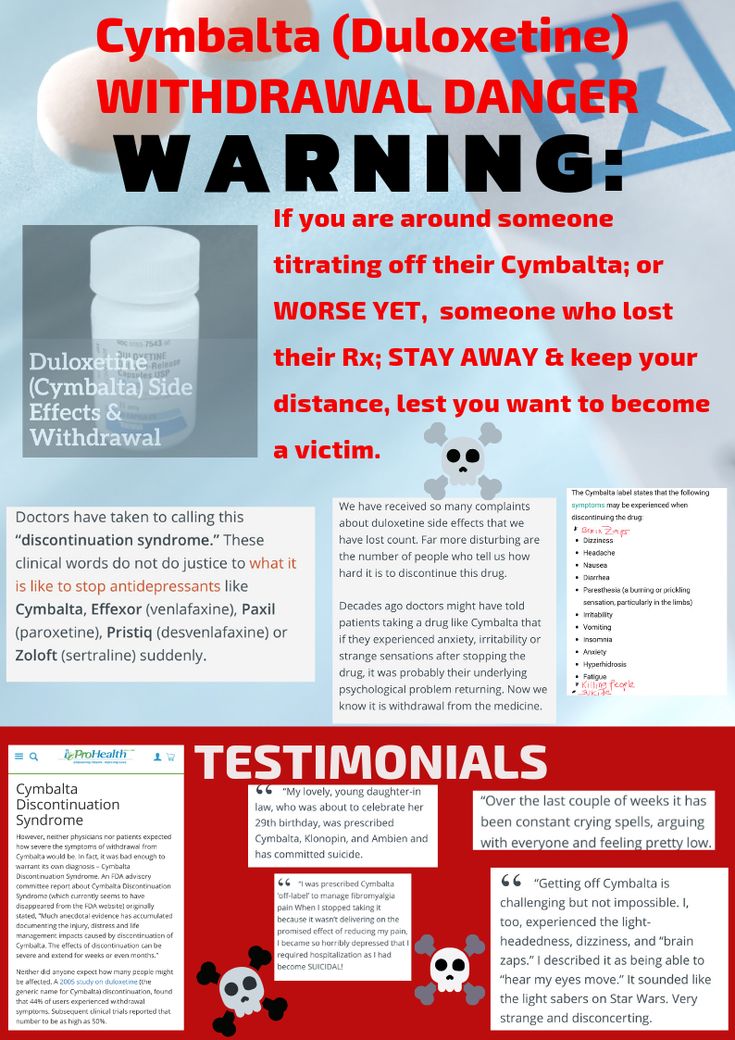
Unfortunately, insomnia is a common side effect experienced by some people who take Cymbalta.
Roughly 10% or more of patients taking Cymbalta report insomnia.
Insomnia can mean difficulty falling asleep, difficulty staying asleep, waking up earlier than desired, or waking up and still feeling tired.
There are many possible causes of insomnia, but if you’re experiencing signs for the first time after starting medication, it’s possible that you have Cymbalta-induced insomnia.
Insomnia can also be a side effect of Cymbalta withdrawal and discontinuation.
If you’re experiencing signs of insomnia or any other bothersome side effects while taking Cymbalta, reach out to your provider for guidance and help.
How to Sleep While Taking Cymbalta
During the first few weeks on a new antidepressant like Cymbalta, it’s helpful to let your provider know if new symptoms or side effects emerge, including insomnia.
In some cases, your provider may recommend waiting to see if your insomnia resolves on its own as you continue the medication.
If not, they may recommend one of the following alternatives.
Slowly increase dosage
When starting a new antidepressant, it’s common for your provider to start you at a lower dose and gradually increase the dosage until you reach the recommended therapeutic amount (usually 60 mg per day).
However, if you start to experience new side effects like insomnia as the dosage increases, your provider may recommend slowing the dose increase to minimize side effects and give your body time to adjust to the medication.
Reduce dosage if needed
Your provider may recommend reducing your dosage or discontinuing the medication altogether.
Higher doses of Cymbalta can exacerbate insomnia and other sleep disturbances, which is why your provider may recommend lowering the dosage if you’re still able to reap the therapeutic benefits of the medication.
Otherwise, stopping the medication may be the best option for you.
In that case, do not stop taking Cymbalta abruptly or suddenly.
It’s crucial that you work with your provider to gradually taper off of Cymbalta to avoid experiencing withdrawal symptoms.
Establish a routine
One way to support getting adequate, quality sleep is to establish a regular sleeping routine.
Going to bed at the same time every night (within one hour of variation) and waking up at the same time each day (also within one hour of variation) can help get your circadian rhythms into a reliable pattern.
Avoiding screens for at least an hour before bed can also help, as can sleeping in a cool room.
Relaxation techniques including deep breathing exercises, imagery, and others, can also help your mind and body relax before bed.
Use sleep aids
Over-the-counter (OTC) sleep aids have become a popular resource in recent years for people hoping to get good, consistent sleep.
Melatonin, when taken at typical doses of 1-5 mg nightly, is safe to use while taking Cymbalta.
Evidence suggests that melatonin supplements can help some people to improve total sleep time, sleep quality, and sleep latency (how long it takes to fall asleep).
Melatonin may also be particularly helpful in treating chronic insomnia in people aged 55 and older.
However, some supplements can cause adverse reactions when taken with Cymbalta and should be avoided, including St. John’s wort.
Check with your provider or pharmacist before adding any OTC sleep aid or supplement to your routine to be sure it will not have an adverse interaction with Cymbalta.
Avoid caffeine or exercise before bed
Regular exercise can support a healthy sleeping schedule, but exercising right before bedtime may impair the quality of your sleep.
Though there’s little evidence to suggest that you need to avoid exercising in the afternoon or evening (in fact, some research suggests that afternoon workouts can yield the best performance in some athletes), make sure that the end of your workout occurs at least 60-90 minutes before bedtime.
Drinking or consuming caffeine close to bedtime can interfere with circadian melatonin rhythms and block sleep-promoting chemical receptors, making it difficult to sleep.
Though the rate at which you metabolize caffeine can vary depending on the individual, one study found that consuming caffeine even six hours before bedtime can reduce sleep time by one hour.
Feeling Down?
Take our free assessment and learn about your options.
Get Started
When to See a Doctor
For most people, Cymbalta can be a safe and effective treatment option for depression, anxiety, or chronic pain.
But if you’re experiencing insomnia or any other bothersome side effects while taking the medication, reach out to your provider to discuss whether adjusting the dose or switching to another antidepressant may help.
Reach out to your provider if you experience any of these rare, but serious, symptoms:
- Severe dizziness
- Hives, or a red or purple rash with blistering or peeling
- Itching or swelling, particularly of the mouth, face, or throat
- Trouble breathing
- Seizure
Additional signs that the medication may not be working appropriately can include these serious side effects:
- Panic attacks
- Worsening mood
- Feeling agitated, impulsive, aggressive, restless, or hyperactive
- Confusion
- Thoughts of suicide
If you experience any of the above symptoms, talk to your provider as soon as possible.
If you’re having a mental health emergency, call 911 or go to the nearest emergency room. You can also get free 24/7 support from a suicide and crisis expert by calling or texting 988. If you’d prefer to chat online, you can chat with a suicide and crisis expert by visiting the Lifeline Chat.
How K Health Can Help
Think you might need a prescription for Cymbalta (Duloxetine)?
K Health has clinicians standing by 24/7 to evaluate your symptoms and determine if Cymbalta is right for you.
Get started with our free assessment, which will tell you in minutes if treatment could be a good fit. If yes, we’ll connect you right to a clinician who can prescribe medication and have it shipped right to your door.
Frequently Asked Questions
Can Cymbalta make it hard to sleep?
Yes. Insomnia, or difficulty sleeping, is a common side effect when taking Cymbalta. For some people, insomnia will resolve on its own as your body adjusts to taking the medication.
Can I take a sleep aid with Cymbalta?
Melatonin can be used to help you sleep while taking Cymbalta, but some drugs should be avoided when taking the antidepressant medication, including St. John’s wort. Check with your provider or pharmacist before adding any OTC sleep aid or supplement to your routine to be sure it will not have an adverse interaction with Cymbalta.
John’s wort. Check with your provider or pharmacist before adding any OTC sleep aid or supplement to your routine to be sure it will not have an adverse interaction with Cymbalta.
Can you take Cymbalta at night before bed?
Though many people prefer to take Cymbalta in the morning, it can cause drowsiness in some people. If you experience drowsiness as a side effect of taking Cymbalta, talk to your provider about taking the medication in the evening.
How common is insomnia with Cymbalta?
Insomnia is very common when taking Cymbalta. Over 10% of patients taking the drug reported insomnia as a side effect.
K Health articles are all written and reviewed by MDs, PhDs, NPs, or PharmDs and are for informational purposes only. This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
K Health has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
-
Caffeine Effects on Sleep Taken 0, 3, or 6 Hours before Going to Bed. (2013).
https://jcsm.aasm.org/doi/10.5664/jcsm.3170 -
Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline.
 (2017).
(2017).
https://jcsm.aasm.org/doi/10.5664/jcsm.6470 -
Comparing Performance During Morning vs. Afternoon Training Sessions in Intercollegiate Basketball Players. (2017).
https://pubmed.ncbi.nlm.nih.gov/28538305/ -
Cymbalta (duloxetine hydrochloride) capsules.
 (2008).
(2008).
https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022516lbl.pdf -
Duloxetine (Cymbalta). (2020).
https://www.nami.org/About-Mental-Illness/Treatments/Mental-Health-Medications/Types-of-Medication/Duloxetine-(Cymbalta) -
Duloxetine in the treatment of major depressive disorder.
 (2007).
(2007).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2654630/ -
Effects of caffeine on the human circadian clock in vivo and in vitro. (2015).
https://www.science.org/doi/10.1126/scitranslmed.aac5125 -
Effects of Evening Exercise on Sleep in Healthy Participants: A Systematic Review and Meta-Analysis.
 (2019).
(2019).
https://pubmed.ncbi.nlm.nih.gov/30374942/ -
Meta-Analysis: Melatonin for the Treatment of Primary Sleep Disorders. (2013).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3656905/ -
Normalizing sleep quality disturbed by psychiatric polypharmacy: a single patient open trial (SPOT).
 (2016).
(2016).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5527988/ -
The energy hypothesis of sleep revisited. (2008).
https://www.sciencedirect.com/science/article/pii/S0301008208000865
How to Sleep While Taking Cymbalta
Pay Attention to Symptoms and Side Effects
It’s important to pay close attention to the side effects you experience when first taking Cymbalta. You should also know the warning signs of an allergic reaction and other serious conditions. This is especially important when taking an antidepressant or other SNRI that can drastically affect your mood. Keep track of any side effects including their intensity and frequency in a journal or diary and report them to your healthcare provider.
You should also know the warning signs of an allergic reaction and other serious conditions. This is especially important when taking an antidepressant or other SNRI that can drastically affect your mood. Keep track of any side effects including their intensity and frequency in a journal or diary and report them to your healthcare provider.
Pay close attention to your sleep patterns and habits within the first few weeks of taking Cymbalta. In most cases, your doctor may suggest you give your body time to adjust to the medication before stopping its use. If insomnia symptoms don’t improve, they may recommend a different antidepressant.
Limit Caffeine and Other Stimulants
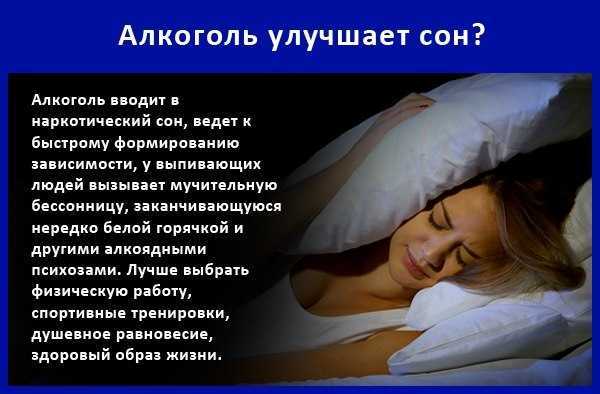
When you’re feeling overly fatigued, it can be tempting to reach for coffee, an energy drink, or another form of caffeine for a much-needed energy boost. Unfortunately, doing so while taking Cymbalta can worsen insomnia symptoms.
Technically, caffeine is a drug. And anytime you combine one or more drugs in your body, you’re at an increased risk of experiencing unwanted side effects. When you consume caffeine and other stimulants like nicotine too late in the day or too close to bedtime, it can make it increasingly difficult to fall asleep. Caffeine also affects your body’s cortisol levels, blood pressure, and heart rate which are all contributing factors to insomnia. Swap this type of energy boost for a more natural one, like exercise. Be sure to exercise early in the morning and not too close to bedtime, as physical activity can also make you too aroused or alert to fall asleep.
When you consume caffeine and other stimulants like nicotine too late in the day or too close to bedtime, it can make it increasingly difficult to fall asleep. Caffeine also affects your body’s cortisol levels, blood pressure, and heart rate which are all contributing factors to insomnia. Swap this type of energy boost for a more natural one, like exercise. Be sure to exercise early in the morning and not too close to bedtime, as physical activity can also make you too aroused or alert to fall asleep.
Try an OTC Sleep Aid
When nothing else seems to work, you can combat insomnia symptoms using an over-the-counter sleep aid or natural supplement like melatonin. Melatonin is a natural sleep hormone that can help you establish healthy sleep patterns. Keep in mind, though, that taking a melatonin supplement while on Cymbalta may increase certain side effects including drowsiness, dizziness, difficulty concentrating, and confusion. Certain sleep aids like St. John’s wort don’t interact well with Cymbalta and should be avoided. For this reason, always confer with your doctor before taking an OTC sleep aid to treat Cymbalta-induced insomnia.
For this reason, always confer with your doctor before taking an OTC sleep aid to treat Cymbalta-induced insomnia.
Alter Your Cymbalta Schedule and Dosage
Take into account how you feel after taking your daily dose of Cymbalta. If you feel tired or drowsy, taking it at night may actually help you sleep. If, instead, you feel energized or alert after taking the drug, try incorporating it into your morning routine. That way, the stimulating side effects have time to wear off before bed. While Cymbalta should be taken at the same time each day, it doesn’t matter if it’s taken at night or in the morning, so you can alter your schedule as needed. Once you choose a time, though, it’s important to remain consistent.
You may also need to increase or lower the dosage you’re taking, based on how your body reacts. Most doctors start patients on a low dose of an antidepressant to see how they react. The recommended amount of Cymbalta is 60 mg, but don’t be surprised if your doctor prescribes half this dose to start. Stick with the recommended dose for 14 days to give your body time to adjust, even if you’re experiencing insomnia symptoms. If these symptoms persist for more than 14 days, your doctor may recommend adjusting the dosage or trying a different medication. Never stop taking Cymbalta abruptly. Doing so can cause unwanted side effects and withdrawal symptoms. Your doctor will help you slowly wean off the medication safely.
Stick with the recommended dose for 14 days to give your body time to adjust, even if you’re experiencing insomnia symptoms. If these symptoms persist for more than 14 days, your doctor may recommend adjusting the dosage or trying a different medication. Never stop taking Cymbalta abruptly. Doing so can cause unwanted side effects and withdrawal symptoms. Your doctor will help you slowly wean off the medication safely.
Adopt Healthy Habits at Night (and Eliminate Others)
All of the activities and rituals you perform leading up to bedtime can drastically impact your sleep. If you’re currently taking Cymbalta and suffering from insomnia, you may need to adjust your nighttime routine and adopt healthier, more beneficial habits. For example, limit screen time before bed. The blue light from your smartphone, laptop, and television screen can interfere with your brain’s natural ability to release melatonin, tricking your body into thinking you should be awake and alert instead of asleep. Avoid heavy or fattening meals before bed that are hard to digest and may cause gastrointestinal discomfort or frequent bathroom trips.
Avoid heavy or fattening meals before bed that are hard to digest and may cause gastrointestinal discomfort or frequent bathroom trips.
Practice relaxing techniques and activities like meditation, reading, listening to music, journaling, or taking a warm bath. Try to perform these activities at the same time and in the same order each night. Over time, these routine behaviors will trigger your brain and body that it’s time to prepare for sleep, making it easier for you to drift off and stay asleep.
Duloxetine for the treatment of painful neuropathy, chronic pain or fibromyalgia
Review question
Does duloxetine work to treat pain generated by nerves when damaged by disease or pain caused by fibromyalgia?
Relevance
Duloxetine is a medicine used to treat depression and urinary incontinence (urinary leakage), and may also be useful for certain types of pain. Pain can occur spontaneously when there is damage to the nerves that carry pain information to the brain (neuropathic pain). When nerve damage occurs outside of the spinal cord, it is called peripheral neuropathy. Another type of pain, nociceptive pain, occurs when nerves sense damage to another tissue (such as a prick in the skin). Some types of pain of unknown origin occur without visible nerve or tissue damage. This type of pain occurs, for example, with fibromyalgia. The purpose of this review was to evaluate the benefits and harms of duloxetine for the treatment of neuropathic pain and chronic pain of all types. nine0005
When nerve damage occurs outside of the spinal cord, it is called peripheral neuropathy. Another type of pain, nociceptive pain, occurs when nerves sense damage to another tissue (such as a prick in the skin). Some types of pain of unknown origin occur without visible nerve or tissue damage. This type of pain occurs, for example, with fibromyalgia. The purpose of this review was to evaluate the benefits and harms of duloxetine for the treatment of neuropathic pain and chronic pain of all types. nine0005
Study profile
We reviewed all published scientific literature and found 18 trials with a total of 6407 participants that were of sufficient quality to include in this review. Eight clinical trials examined the effect of duloxetine in painful diabetic neuropathy and six in pain associated with fibromyalgia. Three trials looked at painful physical symptoms associated with depression, and one small study looked at duloxetine for stroke pain or spinal cord disease (central pain). nine0005
nine0005
Main findings and quality of evidence
The usual dose of duloxetine is 60 mg. There was moderate-quality evidence that duloxetine at this dose reduced pain in painful diabetic peripheral neuropathy and fibromyalgia. In diabetic peripheral neuropathic pain, 50% or slightly more had an improvement on duloxetine 60 mg per day more than one and a half times more often than in the placebo group. In other words, five people with diabetic peripheral neuropathy must receive duloxetine in order for one of them to achieve an effect of 50% or more. The effect on fibromyalgia was similar, but the number of patients needed to be treated for improvement of 50% or more was eight. Based on only one study, it is not possible to determine whether the 20 mg dose is effective, and the 120 mg dose was no more effective than 60 mg. nine0005
We calculated that there were sufficient trials for diabetic neuropathy to draw these conclusions and no further trials are required. For fibromyalgia and the painful symptoms associated with depression, more trials are needed to make strong claims about the effectiveness of duloxetine.
For fibromyalgia and the painful symptoms associated with depression, more trials are needed to make strong claims about the effectiveness of duloxetine.
Most people who take duloxetine will have at least one side effect. They are mostly minor and the most common are feeling unwell, insomnia or drowsiness, headache, dry mouth, constipation or dizziness. About one in six people will stop taking duloxetine due to side effects. Serious problems associated with duloxetine are very rare. nine0005
Although duloxetine is useful in the treatment of neuropathic pain and fibromyalgia, there is little evidence from clinical trials comparing duloxetine with other antidepressants as to which is better.
We conclude that duloxetine can be used to treat pain associated with diabetic neuropathy and possibly fibromyalgia.
The information contained in this review is current up to November 2013, when the most recent literature search was made.
Translation notes:
Translation notes: Translation: Alexandrova Elvira Grigorievna. Editing: Gamirova Rimma Gabdulbarovna, Ziganshina Lilia Evgenievna. Russian translation project coordination: Kazan Federal University. For questions related to this transfer, please contact us at: [email protected]
Editing: Gamirova Rimma Gabdulbarovna, Ziganshina Lilia Evgenievna. Russian translation project coordination: Kazan Federal University. For questions related to this transfer, please contact us at: [email protected]
do they help, treat or relieve symptoms, do they cause addiction, do they make you gain weight
Daniil Davydov
medical journalist
Author profile
In 2017, 3.4% of the world's population — that is, 264 million people — suffered from depression.
At the same time, the cures for this disease are surrounded by many myths. Antidepressants are accused of ineffectiveness and severe side effects, but often the problem is not with the drugs themselves, but with their misuse.
We collected 8 myths about antidepressants and found out how close they are to the truth.
Go to the doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
Myth 1
Antidepressants almost never helpMost likely, this myth arose due to the fact that antidepressants do not work in all patients - so even some doctors and scientists doubt their effectiveness. However, antidepressants cannot be called ineffective, there are just important nuances in the use of these drugs. nine0005
Antidepressants are a class of drugs that normalize the level of neurotransmitters, that is, chemicals that help nerve cells in the brain exchange information.
What are Antidepressants - International Drug Database RxLis
What Medications Help Clinical Depression in Adults - International Primer for Physicians UpToDate
How Antidepressants Help Pain - Mayo Clinic Bulletin
All antidepressants used to treat depression adults working — The Lancet
Who antidepressants work for and who they don't - clinical guidelines for British doctorsPDF, 141 KB
These medicines help people whose problems are related to a deficiency or excess of neurotransmitters. Antidepressants reduce symptoms of depression, obsessive-compulsive disorder, generalized anxiety disorder, post-traumatic stress disorder, and bipolar affective disorder.
Antidepressants reduce symptoms of depression, obsessive-compulsive disorder, generalized anxiety disorder, post-traumatic stress disorder, and bipolar affective disorder.
There is evidence that antidepressants are effective for chronic pain. Antidepressants increase the amount of neurotransmitters in the spinal cord, which reduces pain signals. nine0005
Most specialists have no doubts that antidepressants work. For example, according to the British Royal College of Psychiatry, 50-65% of people with depression who take antidepressants feel better - compared with 25-30% of those who take a placebo.
However, there are situations where the benefit of antidepressants is questionable. For example, antidepressants are good for treating moderate to severe depression, but do not work well for people with mild depression - psychotherapy is more suitable for them. nine0005
And there are situations when these medicines were prescribed by mistake. Then antidepressants really won't help.
When antidepressants don't help
Sergey Divisenko
psychotherapist
There are three cases when antidepressants most often cause problems.
The antidepressant didn't work because the doctor prescribed the wrong dose. The minimum doses of these drugs do not help in half of the cases. Then competent doctors increase the doses to those recommended in clinical guidelines, while illiterate ones refuse them. nine0005
Sometimes, in order for antidepressants to work, they need to be augmented—i.e., enhanced—with other classes of drugs. For example, second-generation antipsychotics, or normothymics, that is, drugs that stabilize mood. If this is not done, the person taking antidepressants will not feel relief.
The antidepressant didn't work because the doctor misdiagnosed and was trying to treat a condition that these drugs don't work for. To help a person, one had to either use other drugs or use non-drug methods of treatment: for example, psychotherapy, transcranial stimulation, or electroconvulsive therapy. nine0005
nine0005
For example, in bipolar disorder, symptoms can be very similar to depression or anxiety. But with bipolar disorder, antidepressants help only if they are used together with other drugs - mood stabilizers. By themselves, they will either work for a short time, or they will not work, or they can cause a phase inversion - that is, a person will switch from a depressive phase to a manic one.
The patient was not helped by a particular antidepressant, but another might. nine0096 Antidepressants differ in the principle of action - on this basis they are divided into classes. It happens that one antidepressant does not work, but another from the same or another class helps. If the treatment does not work, you should not stop drug therapy, but continue to look for a drug that will help this particular patient.
Myth 2
Antidepressants only relieve symptoms, but do not eliminate the cause of the disorder In most cases, this is not a myth. However, in some situations, antidepressants act on the cause of the disorder. nine0005
However, in some situations, antidepressants act on the cause of the disorder. nine0005
Depression is a heterogeneous disease. Experts identify a different number of subtypes of depression - from 4 to 12. But for our purposes, depression can be divided into two large subtypes.
American Criteria for Depressive Disorders - A Handbook for Psychiatrists DSM-5PDF, 32 MB
Understanding Depression - An International Primer for Physicians UpToDate
associated with depression. Disorders that can be attributed to this group are more common. nine0005
If these causes affect a person long enough and he does not understand how to deal with them, depression may develop. In this situation, antidepressants act as drugs that alleviate the symptoms of the disease. To influence the cause of the problem, psychotherapy is needed.
Depression provoked by internal causes. Approximately 7% of people with depression have the correct way of thinking, there are no internal conflicts and injuries, and there are no serious illnesses. In this situation, the cause of depression is the lack of neurotransmitters: serotonin, norepinephrine and dopamine in the synapses of brain nerve cells. In such people, the antidepressant acts precisely on the cause of the disease, that is, it corrects the production of serotonin in neuronal synapses. nine0005
In this situation, the cause of depression is the lack of neurotransmitters: serotonin, norepinephrine and dopamine in the synapses of brain nerve cells. In such people, the antidepressant acts precisely on the cause of the disease, that is, it corrects the production of serotonin in neuronal synapses. nine0005
Myth 3
As soon as it gets better, you can stop taking the antidepressantThis is also not entirely a myth - it would be more correct to call it a belief that is true only for some, but not for all patients with depression.
It is generally advised to continue taking antidepressants for at least six months after remission. If the duration of the disease is short, that is, the person was ill for about two weeks, then for the onset of remission, one or two months of medication is usually needed. If the duration of the disease is long, from several months or years, then more time is required for the onset of remission. It’s impossible to say exactly how much: different people with depression have different recovery times. nine0005
nine0005
Some people have recurrent depression. In this case, the period during which you need to take the medicine depends on how many bouts of depression have already been during your life. If more than three, it is recommended to take antidepressants for several years or for life.
Myth 4
Antidepressants cause addictionPerhaps the roots of this myth are that some people need to take depression medication for life. And at the beginning of treatment, some patients have to increase the dose. But in fact, antidepressants do not cause either true physical or drug dependence. nine0005
True physical dependence on a drug is a situation where a person becomes so addicted to a drug that when it is withdrawn, the symptoms of the disease sharply increase. People who are dependent on the drug have to increase the dosage, otherwise the drug stops helping.
What is True Drug Addiction—Bulletin of the National Institute for the Study of Drug AbusePDF, 7 MB
What is Drug Addiction—Bulletin of the American Psychiatric Association
Drug dependence may include physical dependence on a drug. But this addiction has a unique feature. Dependence can also develop in a healthy person who used the drug not to recover, but to enjoy it. But when he tries to quit the drug, he still experiences physical suffering, which is called the withdrawal syndrome. As a result, a person is forced to look for a new dose of a drug.
But this addiction has a unique feature. Dependence can also develop in a healthy person who used the drug not to recover, but to enjoy it. But when he tries to quit the drug, he still experiences physical suffering, which is called the withdrawal syndrome. As a result, a person is forced to look for a new dose of a drug.
Although a person who takes antidepressants to treat depression gets better, the drugs themselves are neither pleasurable nor addictive. Taking them as drugs is useless.
Of all the drugs that are used in psychiatry, true physical dependence can only be caused by psychostimulants that activate mental activity and anti-anxiety, that is, benzodiazepine tranquilizers. Antidepressants are not included in this list, because there is no need to increase the dosage of correctly selected drugs from this group. nine0005
However, some people who stop taking antidepressants early sometimes experience withdrawal symptoms such as nausea, hand tremors, and some feel “shocks” in the head, similar to the sensations of an electric shock. Depressive symptoms return to patients who need to take the medicine for a very long time.
Depressive symptoms return to patients who need to take the medicine for a very long time.
Antidepressants are sometimes abused, but they cannot cause addiction - Journal of Modern Psychiatry
To avoid unpleasant consequences, stop taking antidepressants only if the attending physician says that they are no longer needed. But even in this situation, it is necessary to cancel antidepressants slowly, that is, gradually reducing the dose. This will help avoid unpleasant side effects. nine0005
Myth 5
A person on antidepressants becomes lethargic and loses interest in lifeThis popular myth is based on real but outdated data.
These mental changes are seen in patients taking first-generation tricyclic antidepressants such as amitriptyline. It has a sedative, that is, a sedative effect. A person who takes high doses of amitriptyline can indeed become sleepy and indifferent to the outside world. nine0005
Amitriptyline - Sedative - Drugs.com International Drug Database
SSRIs do not sedate - Drugs. com International Drug Database
com International Drug Database
Current second-generation antidepressants that are recommended to start treatment with, such as selective serotonin reuptake inhibitors, or SSRIs almost never cause drowsiness and apathy.
On the contrary, in most people with depression they return interest in life. nine0005
Sometimes SSRIs do cause drowsiness, but this has not yet been proven
Sergey Divisenko
psychotherapist
It is believed that in rare cases, modern antidepressants can provoke SSRI-induced apathy. But this condition is extremely rare.
And even then psychiatrists still doubt that the cause is precisely in the drugs, and not in the patient's condition. After all, some people during the time of taking antidepressants may develop other adverse mental states in which apathy occurs: for example, schizotypal disorder, which was not noticed before. nine0005
Myth 6
Antidepressants have many side effects This is partly true: both SSRIs and antidepressants from other groups have side effects. But it is quite possible to deal with them.
But it is quite possible to deal with them.
At the start of treatment, when people first start taking antidepressants, many complain of increased anxiety, dry mouth, nausea, and trouble sleeping. But after a few days or weeks after the start of the course of treatment, these symptoms usually disappear. If the side effects do not stop, it makes sense to consult a doctor - he will replace the antidepressant. nine0005
Dealing with antidepressant side effects - advice from the Mayo Clinic staff
Here's what to do before the side effects go away:
- Take your antidepressant with meals, unless the instructions say otherwise, so the antidepressant will be less annoying stomach;
- put a bottle of clean water on the desktop - if your mouth is dry, you can take a sip. Unsweetened lollipops and chewing gum also help with dry mouth; nine0206
- take a walk for at least half an hour before going to bed - this will make it easier to fall asleep.
 If you can’t sleep at all, you can ask your doctor to pick up sleeping pills.
If you can’t sleep at all, you can ask your doctor to pick up sleeping pills.
The second most common side effect is increased anxiety at the beginning of antidepressant use. To avoid this problem, psychiatrists resort to two effective methods:
- titrate the dose - that is, start with the minimum dose of the antidepressant and then gradually increase it;
- at the beginning of the reception, sedatives - tranquilizers are prescribed together with an antidepressant. nine0206
The third common side effect of SSRIs, especially sertraline, known as Zoloft, and escitalopram, better known as Cipralex, is decreased libido. Approximately 20-30% of people taking antidepressants from this group experience a decrease in sexual desire to one degree or another. At the same time, it is difficult to say how much the drugs are to blame, because approximately 35-50% of people with depression have already experienced sexual dysfunction.
Many people with depression experience sexual dysfunction before starting antidepressants - Harvard Medical School Bulletin
Switching to another antidepressant usually helps, but many people prefer to wait until the medication can be stopped. In some cases, psychiatrists prescribe antidepressants from other groups in addition to the libido-lowering antidepressant. Sometimes it helps to regain interest in sex.
In some cases, psychiatrists prescribe antidepressants from other groups in addition to the libido-lowering antidepressant. Sometimes it helps to regain interest in sex.
Myth 7
Weight gain due to antidepressantsThis is not a myth, but a half-truth. There are both antidepressants that contribute to weight gain, and those that do not have a similar effect. nine0005
The most common complaint about weight gain during treatment is people taking the tetracyclic antidepressant mirtazapine, which actually increases appetite. Another weight gaining antidepressant is paroxetine, better known by the trade name Paxil. But "Zoloft" and "Cipralex" do not contribute to weight gain.
If a patient feels that an antidepressant is causing them to overeat, it is wise to consult a doctor and discuss a change of medication. nine0005
Myth 8
Antidepressants are expensive True, but not for all patients. Most people can cure depression and not go broke.
Antidepressants from different groups vary greatly in price. There are both very expensive drugs and relatively low-cost drugs among them. At the same time, both of them work equally well. However, there are situations when a cheap antidepressant cannot be dispensed with.
On the left - inexpensive "Zoloft" for 327 R, a drug based on sertraline, on the right - the most expensive antidepressant "Ixel" based on milnacipran for 2453 R For example, there is a good antidepressant venlafaxine. The maximum dose of venlafaxine can reach up to 375 mg per day. If these are inexpensive tablets of a domestic manufacturer, then a course of treatment for a month costs about 2000 R. But sometimes inexpensive tablets are not very well tolerated: they cause headache, nausea, sweating, tachycardia, that is, rapid heartbeat. In such cases, you need to switch to a prolonged form of venlafaxine - "Venlafaxine Retard", or "Velaxin XR". But this drug is more expensive: a course of treatment will cost about 5000 R per month.