Sensitivity to smells and sounds
Hyperesthesia: Causes, Symptoms, and Treatment
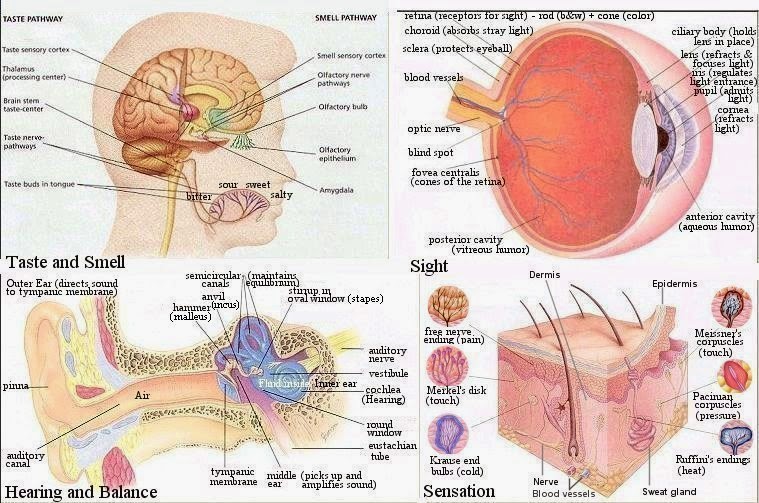
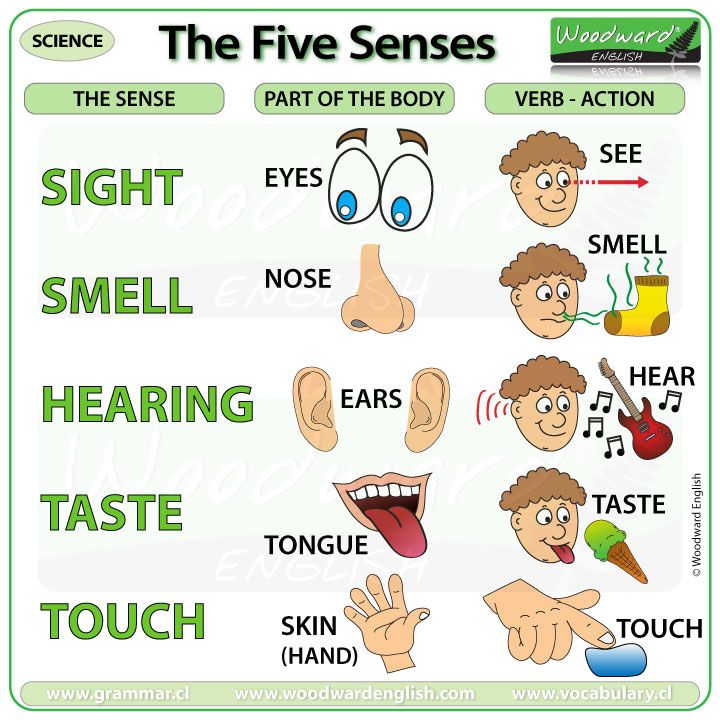
Hyperesthesia refers to increased sensitivity of any of your senses, such as sight, sound, touch, and smell. It can affect just one or all of the senses.
Often, the heightening of an individual sense is referred to by a separate name. For example, increased sensitivity to touch is called tactile sensitivity, and increased sensitivity to sound is called auditory sensitivity.
The term also refers to increased pain sensations. According to the International Association for the Study of Pain, hyperesthesia includes two different subcategories of enhanced pain sensation:
- Hyperalgesia. A stimulus triggers increased or extreme sensitivity to pain.
- Allodynia. A stimulus that is not usually painful suddenly triggers pain.
We explain how hyperesthesia shows itself, why it happens, and how to manage it.
The symptoms of hyperesthesia vary between people. They depend on which senses are affected and how severely:
- Some people with touch sensitivity can experience severe pain when a stimulus triggers their nerves.
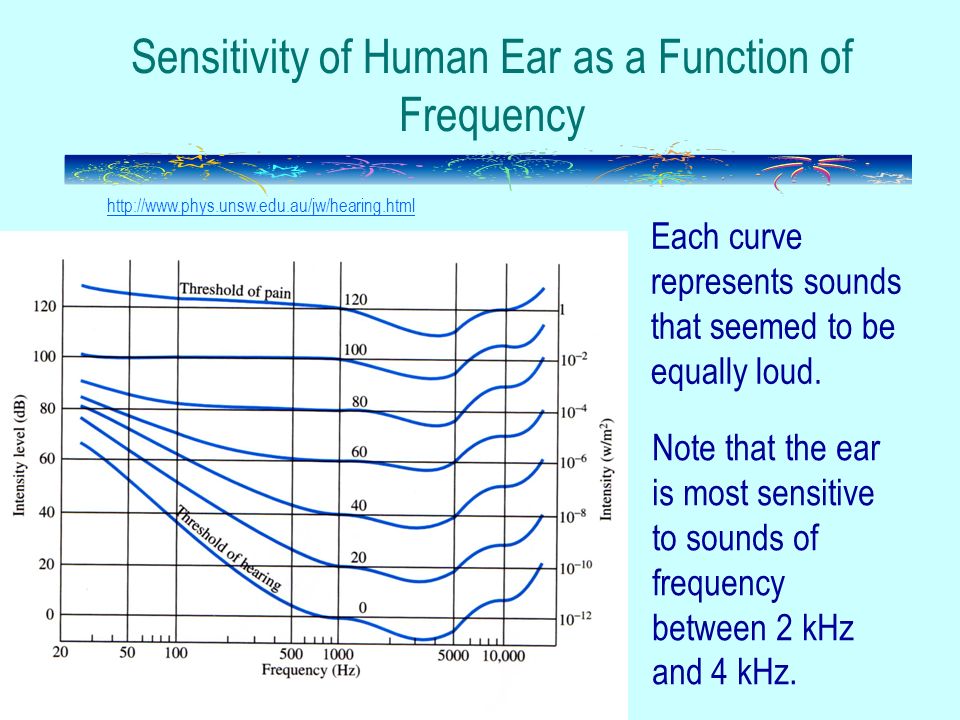
- People with auditory sensitivity can hear painfully loud noises when none have occurred in the environment.
- Those with smell sensitivity often report a wide range of smells without the presence of a stimulus.
Some people will experience a combination of these symptoms. Severe hyperesthesia can also affect the nervous system, which might lead to nerve inflammation and seizures.
Neuropathic pain is a common underlying cause of hyperesthesia, but many diseases or lesions of the nervous system can lead to this type of pain.
Associated health conditions and stimuli include (but are not limited to):
- systemic diseases like diabetes, nutritional deficiencies, and hypothyroidism
- infectious diseases, such as HIV, herpes, hepatitis C, and varicella
- toxic causes, including alcohol, certain chemotherapy drugs, and immunosuppressants
- mechanical causes, such as physical trauma, complex regional pain syndrome, nerve root compression, and phantom limb pain after an amputation
- hereditary causes like Charcot-Marie-Tooth disease
Risk factors
Children with autism, obsessive-compulsive disorder (OCD), and attention deficit hyperactivity disorder (ADHD) are more likely to develop hyperesthesia.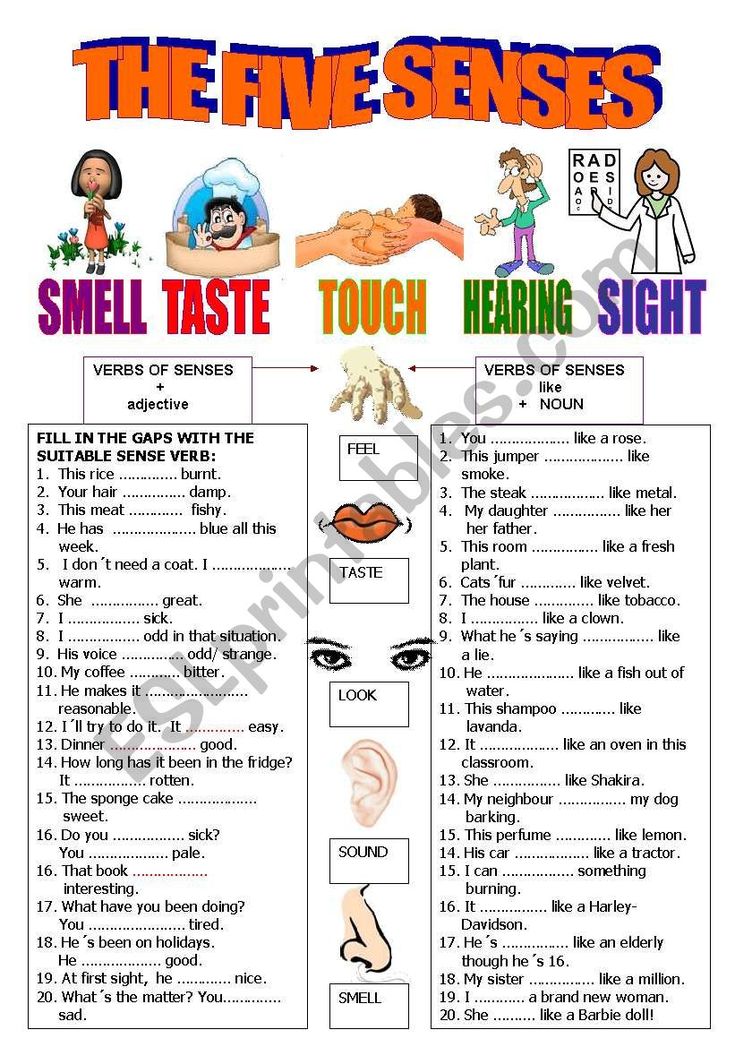
Many people in menopause also report a particular type of hyperesthesia called formication, in which they experience sensations on the skin such as tingling, crawling, or itching.
The treatment for hyperesthesia centers around addressing the underlying cause. If you experience hyperesthesia due to diabetic neuropathy, keeping your blood glucose under control can help keep the problem from getting worse.
If a vitamin B12 deficiency is causing the hyperesthesia, a physician might prescribe B12 supplements. After treating the underlying condition or removing the triggering stimulus, most people will find that the symptoms of hyperesthesia resolve.
If there’s an underlying problem in the brain or spinal cord, your doctor will assess and treat this accordingly.
Managing the effects of episodes
Some conditions linked to neuropathy, like diabetes, are chronic. It’s important to find methods of reducing the physical and emotional sensations around hypersensitivity.
What you can do
It’s important to remember that the condition is usually manageable. Making certain lifestyle changes can ease your symptoms considerably. You may want to try to:
- Reduce your caffeine and alcohol intake, or eliminate them completely.
- Eat a well-balanced, nutritious diet.
- Train yourself to stay calm during flares of hypersensitivity by regularly practicing yoga or meditation.
What your doctor can do
Some medical interventions might also help, including:
- Physical therapy. This can help people who experience increased pain as a result of their hyperesthesia regain mobility and improve their quality of life.
- Cognitive behavioral therapy (CBT). CBT can be effective in reducing the unpleasant responses caused by any stimulus.
- Antiepileptic drugs, including gabapentinoids. People experiencing seizures can take anticonvulsant medications to reduce the frequency and severity of their seizures.
 These medications can also help reduce hyperesthesia pain in people who don’t experience seizures.
These medications can also help reduce hyperesthesia pain in people who don’t experience seizures. - Anxiolytic medications. People can take anxiety-reducing medication if they are experiencing fear and anxiety around their condition. Hyperesthesia can be debilitating and affect your ability to be around the many stimuli of daily life. This can have a negative effect on your mental health.
- Antidepressant medications. Antidepressants can help reduce neuropathic pain as well as depression.
A 2020 review suggests a diet with plenty of flavonoids might help people reduce the effects of neuropathy. Flavonoids are compounds in plants that provide antioxidants, which help counter the harmful effects of damaging free radical molecules around your body.
However, the review largely used studies that tested the effects of flavonoids in a lab and on animals, rather than in humans. The review also focused only on peripheral neuropathy, but other types like central neuropathy might work differently.
So, it’s difficult to say that the findings can carry over to humans or all types of neuropathy, but they are promising.
What to do during an episode of hyperesthesia
In the moment, hyperesthesia can feel overwhelming and never-ending.
If you’re experiencing an episode of hyperesthesia, lie down in a dark room that’s as free from stimuli as possible. This can help the symptoms pass more quickly.
Try to remain calm and practice some deep breathing exercises.
Your outlook for hyperesthesia will depend on the underlying cause. Supplementing a B12 deficiency can clear up hyperesthesia symptoms entirely. For neurodiverse people, managing overstimulation will likely be a lifelong health goal.
Hyperesthesia can be unsettling and may cause pain, fear, and anxiety in those who live with it.
Hyperesthesia can exist on its own or as a symptom of another related health condition. Whichever applies to you, your doctors will try to diagnose the root cause so it can be treated effectively.
Odor and Noise Intolerance in Persons with Self-Reported Electromagnetic Hypersensitivity
1. IPCS/WHO Conclusions and recommendations of a workshop on multiple chemical sensitivities (MCS) Regulat. Toxicol. Pharmacol. 1996;24:188–189. doi: 10.1006/rtph.1996.0095. [CrossRef] [Google Scholar]
2. Hansson Mild K., Repacholi M., van Deventer E., Ravazzani P., editors. WHO International Workshop on Electromagnetic Field Hypersensitivity. World Health Organization; Prague, Czech Republic: 2004. [Google Scholar]
3. Hillert L., Berglind N., Arnetz B.B., Bellander T. Prevalence of self-reported hypersensitivity to electric or magnetic fields in a population-based questionnaire survey. Scand. J. Work. Environ. Health. 2002;28:33–41. doi: 10.5271/sjweh.644. [PubMed] [CrossRef] [Google Scholar]
4. Levallois P., Neutra R., Lee G., Hristova L. Study of self-reported hypersensitivity to electromagnetic fields in California. Environ. Health. Perspect. 2002;110(Suppl. 4):619–623. doi: 10.1289/ehp.02110s4619. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
doi: 10.1289/ehp.02110s4619. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Schreier N., Huss A., Roosli M. The prevalence of symptoms attributed to electromagnetic field exposure: A cross-sectional representative survey in Switzerland. Soz. Praventivmed. 2006;51:202–209. doi: 10.1007/s00038-006-5061-2. [PubMed] [CrossRef] [Google Scholar]
6. Eltiti S., Wallace D., Zougkou K., Russo R., Joseph S., Rasor P., Fox E. Development and evaluation of the electromagnetic hypersensitivity questionnaire. Bioelectromagnetics. 2007;28:137–151. doi: 10.1002/bem.20279. [PubMed] [CrossRef] [Google Scholar]
7. Schröttner J., Leitgeb N. Sensitivity to electricity: Temporal changes in Austria. BMC Public Health. 2008;8:310. doi: 10.1186/1471-2458-8-310. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
8. Seitz H., Stinner D., Eikmann T., Herr C., Roosli M. Electromagnetic hypersensitivity (EHS) and subjective health complaints associated with electromagnetic fields of mobile phone communication: A literature review published between 2000 and 2004. Sci. Total. Environ. 2005;349:45–55. doi: 10.1016/j.scitotenv.2005.05.009. [PubMed] [CrossRef] [Google Scholar]
Sci. Total. Environ. 2005;349:45–55. doi: 10.1016/j.scitotenv.2005.05.009. [PubMed] [CrossRef] [Google Scholar]
9. Johansson A., Nordin S., Heiden M., Sandström M. Symptoms, personality traits, and stress in people with mobile phone-related symptoms and electromagnetic hypersensitivity. J. Psychosom. Res. 2005;68:37–45. [PubMed] [Google Scholar]
10. Rubin G.J., Nieto-Hernandez R., Wessely S. Idiopathic environmental intolerance attributed to electromagnetic fields (formerly ‘electromagnetic hypersensitivity’): An updated systematic review of provocation studies. Bioelectromagnetics. 2010;31:1–11. [PubMed] [Google Scholar]
11. Bergdahl J. Psychologic aspects of patients with symptoms presumed to be caused by electricity or visual display units. Acta. Odontol. Scand. 1995;53:304–310. doi: 10.3109/00016359509005992. [PubMed] [CrossRef] [Google Scholar]
12. Bergdahl J., Marell L., Bergdahl M., Perris H. Psychobiological personality dimensions in two environmental-illness patient groups. Clin. Oral. Invest. 2005;9:251–256. doi: 10.1007/s00784-005-0015-2. [PubMed] [CrossRef] [Google Scholar]
Clin. Oral. Invest. 2005;9:251–256. doi: 10.1007/s00784-005-0015-2. [PubMed] [CrossRef] [Google Scholar]
13. Palmquist P., Claeson A.-S., Neely G., Stenberg B., Nordin S. Overlap in prevalence between various types of environmental intolerance. Int. J. Hyg. Environ. Health. 2014;217:427–434. doi: 10.1016/j.ijheh.2013.08.005. [PubMed] [CrossRef] [Google Scholar]
14. Carlsson Eek F. Ph.D. Thesis. Department of Occupational and Environmental Medicine, Lund University; Lund, Sweden: 2005. Subjective Annoyance Attributed to Electricity and Smells: Epidemiology and Stress Physiology. [Google Scholar]
15. Baliatsas C., Van Kamp I., Hooiveld M., Yzermans J., Lebret E. Comparing non-specific physical symptoms in environmentally sensitive patients: Prevalence, duration, functional status and illness behavior. J Psychosom Res. 2014;76:405–413. doi: 10.1016/j.jpsychores.2014.02.008. [PubMed] [CrossRef] [Google Scholar]
16. Sparks P.J., Daniell W., Black D.W., Kipen H.M., Altman L.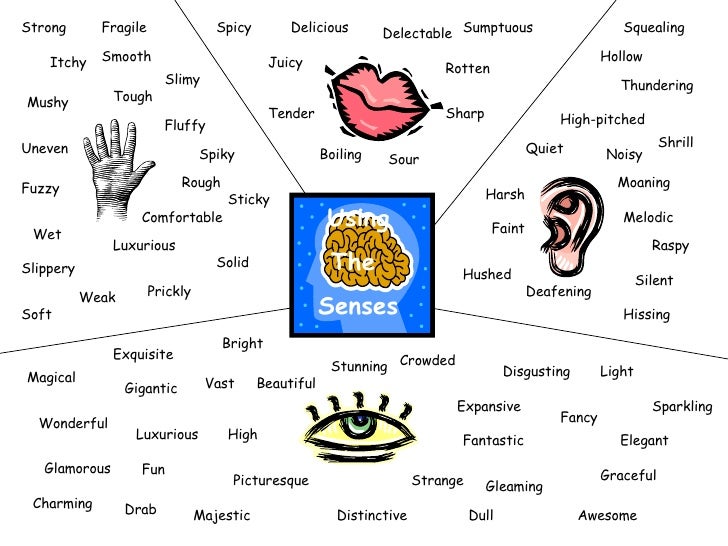 C., Simon G.E., Terr A.I. Multiple chemical sensitivity syndrome: A clinical perspective. I. Case definition, theories of pathogenesis, and research needs. J. Occup. Med. 1994;36:718–730. [PubMed] [Google Scholar]
C., Simon G.E., Terr A.I. Multiple chemical sensitivity syndrome: A clinical perspective. I. Case definition, theories of pathogenesis, and research needs. J. Occup. Med. 1994;36:718–730. [PubMed] [Google Scholar]
17. Black D.W. The relationship of mental disorders and idiopathic environmental intolerance. Occup. Med. 2000;15:557–570. [PubMed] [Google Scholar]
18. Bailer J., Witthoft M., Rist F. Modern health worries and idiopathic environmental intolerance. J. Psychosom. Res. 2008;65:425–433. doi: 10.1016/j.jpsychores.2008.05.006. [PubMed] [CrossRef] [Google Scholar]
19. Bailer J., Witthoft M., Rist F. Psychological predictors of short- and medium term outcome in individuals with idiopathic environmental intolerance (IEI) and individuals with somatoform disorders. J. Toxicol. Environ. Health A. 2008;71:766–775. doi: 10.1080/15287390801985562. [PubMed] [CrossRef] [Google Scholar]
20. Andersson L., Bende M., Millqvist E., Nordin S. Attention bias and sensitization in chemical sensitivity. J. Psychosom. Res. 2009;66:407–416. doi: 10.1016/j.jpsychores.2008.11.005. [PubMed] [CrossRef] [Google Scholar]
J. Psychosom. Res. 2009;66:407–416. doi: 10.1016/j.jpsychores.2008.11.005. [PubMed] [CrossRef] [Google Scholar]
21. Skovbjerg S., Zachariae R., Rasmussen A., Johansen J.D., Elberling J. Attention to bodily sensations and symptom perception in individuals with idiopathic environmental intolerance. Environ. Health Prev. Med. 2009;15:141–150. [PMC free article] [PubMed] [Google Scholar]
22. Bergdahl J., Anneroth G., Stenman E. Description of persons with symptoms presumed to be caused by electricity or visual display units: Oral aspects. Scand. J. Dental. Res. 1994;102:41–45. [PubMed] [Google Scholar]
23. sterberg K., Persson R., Karlson B., Carlsson Eek F., Orbaek P. Personality, mental distress, and subjective health complaints among persons with environmental annoyance. Human Exp. Toxicol. 2007;26:231–241. doi: 10.1177/0960327107070575. [PubMed] [CrossRef] [Google Scholar]
24. Persson R., Carlsson Eek F., Osterberg K., Orbaek P., Karlson B. A two-week monitoring of self-reported arousal, worry and attribution among persons with annoyance attributed to electrical equipment and smells.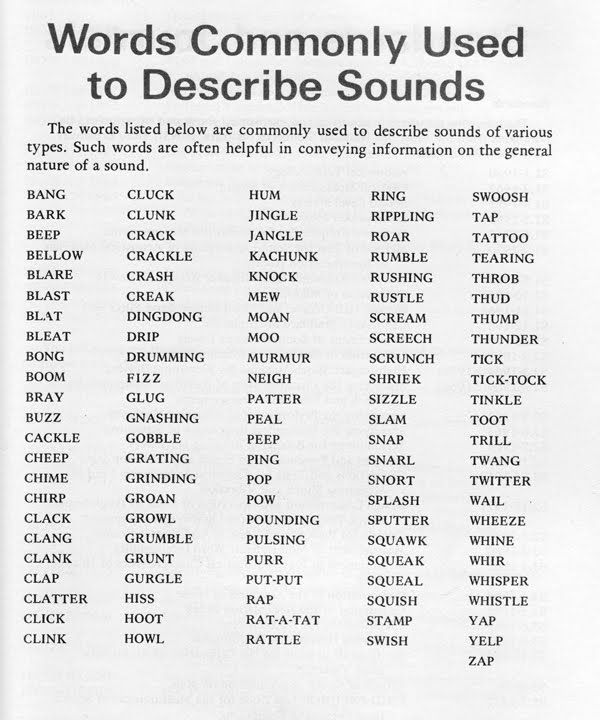 Scand. J. Psychol. 2008;49:345–356. doi: 10.1111/j.1467-9450.2008.00660.x. [PubMed] [CrossRef] [Google Scholar]
Scand. J. Psychol. 2008;49:345–356. doi: 10.1111/j.1467-9450.2008.00660.x. [PubMed] [CrossRef] [Google Scholar]
25. Vernon J.A. Pathophysiology of tinnitus: A special case: Hyperacusis and a proposed treatment. Am. J. Otol. 1987;8:201–202. [PubMed] [Google Scholar]
26. Weinstein N.D. Individual differences in reactions to noise: A longitudinal study in a college dormitory. J. Appl. Psychol. 1978;63:458–466. doi: 10.1037/0021-9010.63.4.458. [PubMed] [CrossRef] [Google Scholar]
27. Stansfeld S.A., Clark C.R., Jenkins L.M., Tarnopolsky A. Sensitivity to noise in a community sample: I. Measurement of psychiatric disorder and personality. Psychol. Med. 1985;15:243–254. doi: 10.1017/S0033291700023527. [PubMed] [CrossRef] [Google Scholar]
28. Marriage J., Barnes N.M. Is central hyperacusis a symptom of 5-hydroxytryptamine (5-HT) dysfunction? J. Laryngol. Otol. 1995;109:915–921. [PubMed] [Google Scholar]
29. Andersson G., Lindvall N., Hursti T., Carlbring P. Hypersensitivity to sound (hyperacusis): A prevalence study conducted via the Internet and post. Int. J. Audiol. 2002;41:545–554. doi: 10.3109/14992020209056075. [PubMed] [CrossRef] [Google Scholar]
Int. J. Audiol. 2002;41:545–554. doi: 10.3109/14992020209056075. [PubMed] [CrossRef] [Google Scholar]
30. Bell I.R., Hardin E.E., Baldwin C.M., Schwartz G.E. Increased limbic system symptomatology and sensitizability of young adults with chemical and noise sensitivities. Environ. Res. 1995;70:84–97. doi: 10.1006/enrs.1995.1052. [PubMed] [CrossRef] [Google Scholar]
31. Szarek M.J., Bell I.R., Schwartz G.E. Validation of a brief screening measure of environmental chemical sensitivity: The chemical odor intolerance index. J. Environ. Psychol. 1997;17:345–351. doi: 10.1006/jevp.1997.0071. [CrossRef] [Google Scholar]
32. Nordin S., Millqvist E., Löwhagen O., Bende M. The Chemical Sensitivity Scale: Psychometric properties and comparison with the noise sensitivity scale. J. Environ. Psychol. 2003;23:357–365. [Google Scholar]
33. Nordin S., Körning Ljungberg J., Claeson A.-S., Neely G. Stress and odor sensitivity in persons with noise sensitivity. Noise Health. 2013;15:173–177. doi: 10.4103/1463-1741.112366. [PubMed] [CrossRef] [Google Scholar]
doi: 10.4103/1463-1741.112366. [PubMed] [CrossRef] [Google Scholar]
34. Topf M. Personal and environmental predictors of patient disturbance due to hospital noise. J. Appl. Psychol. 1985;70:22–28. doi: 10.1037/0021-9010.70.1.22. [PubMed] [CrossRef] [Google Scholar]
35. Ekehammar B., Dornic S. Weinstein’s Noise Sensitivity Scale: Reliability and construct validity. Percept. Mot. Skills. 1990;70:129–130. doi: 10.2466/pms.1990.70.1.129. [PubMed] [CrossRef] [Google Scholar]
36. Sandström M., Lyskov E., Berglund A., Medvedev S., Hansson Mild K. Neurophysiological effects of flickering light in patients with perceived electrical hypersensitivity. J. Occup. Environ. Med. 1997;39:15–22. doi: 10.1097/00043764-199701000-00006. [PubMed] [CrossRef] [Google Scholar]
37. Lyskov E., Sandström M., Hansson Mild K. Neurophysiological study of patients with perceived ‘electrical hypersensitivity’ Int. J. Psychophysiol. 2001;42:233–241. doi: 10.1016/S0167-8760(01)00141-6. [PubMed] [CrossRef] [Google Scholar]
38. Lyskov E., Sandström M., Hansson Mild K. Provocation study of persons with perceived electrical hypersensitivity and controls using magnetic field exposure and recording of electrophysiological characteristics. Bioelectromagnetics. 2001;22:457–462. doi: 10.1002/bem.73. [PubMed] [CrossRef] [Google Scholar]
Lyskov E., Sandström M., Hansson Mild K. Provocation study of persons with perceived electrical hypersensitivity and controls using magnetic field exposure and recording of electrophysiological characteristics. Bioelectromagnetics. 2001;22:457–462. doi: 10.1002/bem.73. [PubMed] [CrossRef] [Google Scholar]
39. Wilén J., Johansson A., Kalezic N., Lyskov E., Sandström M. Psychophysiological tests and provocation of subjects with mobile phone related symptoms. Bioelectromagnetics. 2006;27:204–214. doi: 10.1002/bem.20195. [PubMed] [CrossRef] [Google Scholar]
40. Nelson J.J., Chen K. The relationship of tinnitus, hyperacusis, and hearing loss. Ear Nose Throat J. 2004;83:472–476. [PubMed] [Google Scholar]
41. Landgrebe M., Frick U., Hauser S., Hajak G., Langguth B. Association of tinnitus and electromagnetic hypersensitivity: Hints for a shared pathophysiology? PLoS One. 2009;4:5026. doi: 10.1371/journal.pone.0005026. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Nordin S., Bende M., Millqvist E. Normative data of the Chemical Sensitivity Scale. J. Environ. Psychol. 2004;24:399–403. doi: 10.1016/S0272-4944(03)00074-4. [CrossRef] [Google Scholar]
Nordin S., Bende M., Millqvist E. Normative data of the Chemical Sensitivity Scale. J. Environ. Psychol. 2004;24:399–403. doi: 10.1016/S0272-4944(03)00074-4. [CrossRef] [Google Scholar]
43. Eriksson N.M., Stenberg B.G. Baseline prevalence of symptoms related to indoor environment. Scand. J. Public Health. 2006;34:387–396. doi: 10.1080/14034940500228281. [PubMed] [CrossRef] [Google Scholar]
44. Barsky A.J., Borus J.F. Functional somatic syndromes. Ann. Intern. Med. 1999;130:910–921. doi: 10.7326/0003-4819-130-11-199906010-00016. [PubMed] [CrossRef] [Google Scholar]
45. Wessely S., Nimuan C., Sharpe M. Functional somatic syndromes: One or many? Lancet. 1999;354:936–939. doi: 10.1016/S0140-6736(98)08320-2. [PubMed] [CrossRef] [Google Scholar]
46. Jason L.A., Taylor R.R., Kennedy C.L. Chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities in a community-based sample of persons with chronic fatigue syndrome-like symptoms. Psychosom. Med. 2000;62:655–663.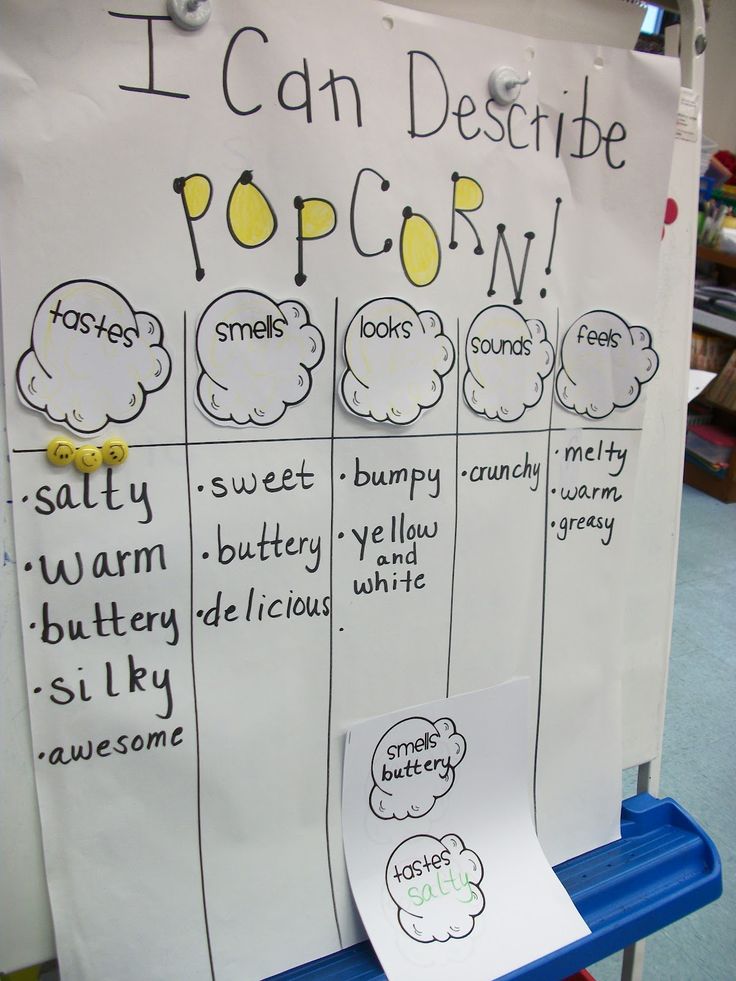 doi: 10.1097/00006842-200009000-00009. [PubMed] [CrossRef] [Google Scholar]
doi: 10.1097/00006842-200009000-00009. [PubMed] [CrossRef] [Google Scholar]
47. Eriksen H.R., Ursin H. Subjective health complaints, sensitization, and sustained cognitive activation (stress) J. Psychosom. Res. 2004;56:445–448. doi: 10.1016/S0022-3999(03)00629-9. [PubMed] [CrossRef] [Google Scholar]
48. Brosschot J.F. Cognitive-emotional sensitization and somatic health complaints. Scand. J. Psychol. 2002;43:113–121. doi: 10.1111/1467-9450.00276. [PubMed] [CrossRef] [Google Scholar]
49. Verkuil B., Brosschot J.F., Thayer J.F. A sensitive body or a sensitive mind? Associations among somatic sensitization, cognitive sensitization, health worry, and subjective health complaints. J. Psychosom. Res. 2007;63:673–681. doi: 10.1016/j.jpsychores.2007.08.010. [PubMed] [CrossRef] [Google Scholar]
50. Deary V., Chalder T., Sharpe M. The cognitive behavioural model of medically unexplained symptoms: A theoretical and empirical review. Clin. Psychol. Rev. 2007;27:781–797. doi: 10.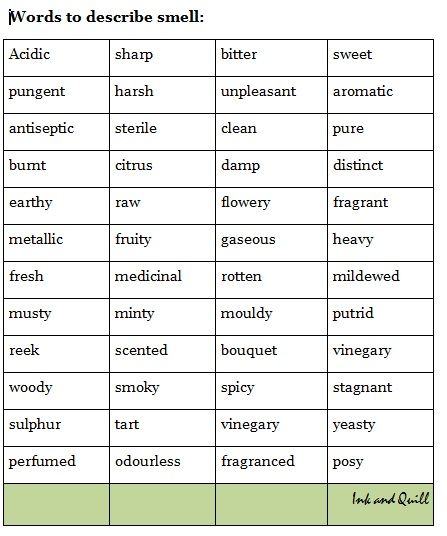 1016/j.cpr.2007.07.002. [PubMed] [CrossRef] [Google Scholar]
1016/j.cpr.2007.07.002. [PubMed] [CrossRef] [Google Scholar]
51. Eltiti S., Wallace D., Ridgewell A., Zougkou K., Russo R., Sepulveda F., Mirshekar-Syahkal D., Rasor P., Deeble R., Fox E. Does short-term exposure to mobile phone base station signals increase symptoms in individuals who report sensitivity to electromagnetic fields? A double-blind randomized provocation study. Environ. Health Perspect. 2007;115:1603–1608. doi: 10.1289/ehp.10286. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
52. Levitt B.B., Lai H. Biological effects from exposure to electromagnetic radiation emitted by cell tower base stations and other antenna arrays. Environ Rev. 2010;18:369–395. doi: 10.1139/A10-018. [CrossRef] [Google Scholar]
Hyperosmia - symptoms and causes
- Advantages
- Doctors
- Contacts
- Licenses
Benefits
-
The latest, constantly updated equipment
-
Interest-free installment plan for all services
-
Online ENT consultations
-
Departure of an ENT doctor at home
- nine0012 Friendly and qualified staff
-
24/7 ENT help
Hyperosmia is an increased sensitivity to odors.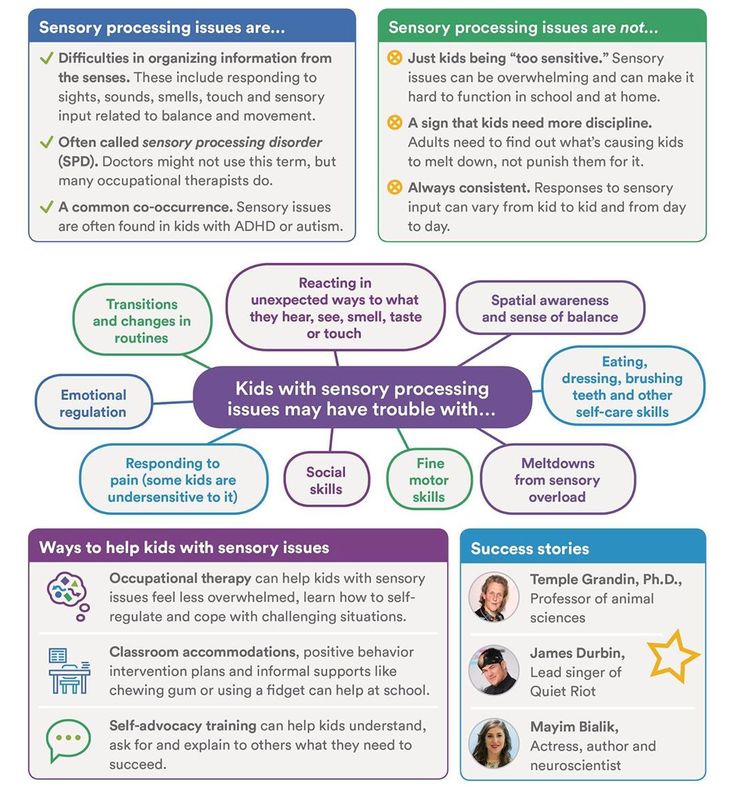 This condition can lead to discomfort and cause disruption of the usual rhythm of life. First of all, susceptibility to perfumes, household chemicals, and scented candles increases.
This condition can lead to discomfort and cause disruption of the usual rhythm of life. First of all, susceptibility to perfumes, household chemicals, and scented candles increases.
The causes and accompanying symptoms of hyperosmia can be varied. An otolaryngologist will help you understand the situation and suggest the most rational options for coping with the existing problem. The main thing is to see a doctor in time.
Causes of hyperosmia
There are several factors that determine the increased sensitivity to odors. These may be:
- Genetic predisposition - some people do have a more acute sense of smell than others. This pattern is often seen in perfumers. nine0004
- Pregnancy. The hormonal changes that occur during gestation, especially in the first trimester, can lead to the fact that a woman's sense of smell is aggravated. Pronounced aromas can even cause nausea and vomiting due to overexcitation of the corresponding centers of the medulla oblongata.
- Autoimmune pathologies. Quite often, adrenal insufficiency and systemic lupus erythematosus lead to an aggravation of the sense of smell.
- Borreliosis. Approximately every second person who has been bitten by a Borrelia-infected tick has increased susceptibility to odors. nine0004
- Type 1 diabetes mellitus. In the absence of adequate compensation for carbohydrate disorders, the activity of nerve receptors changes.
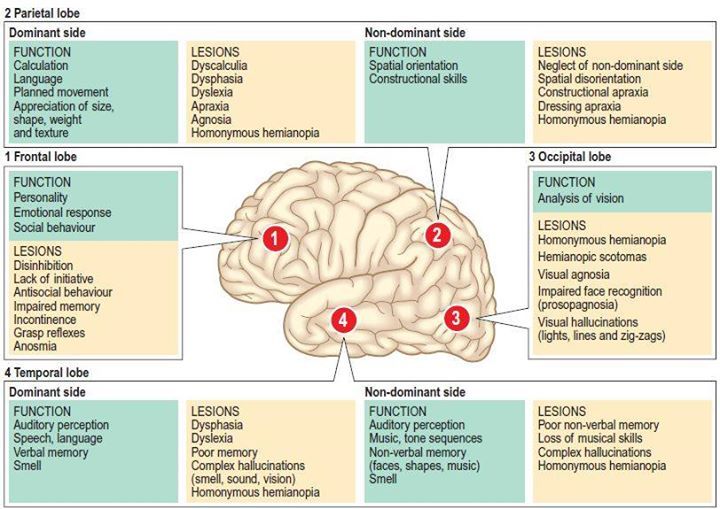
- Brain lesions. A similar situation can be observed in Alzheimer's disease, Parkinson's pathology, epilepsy, multiple sclerosis.
- Pathological processes of the nasal mucosa and paranasal sinuses. This is hyperosmia in the focus of inflammation, in the area of polypoid growths, etc.
- Long-term use of vasoconstrictor drugs. These drugs can excite or depress the olfactory receptors. nine0004
- Hypovitaminosis. Especially often hyperosmia develops against the background of cyanocobalamin deficiency.
- Migraine. This disease is accompanied by headache, which is often combined with nausea and vomiting.
Recently, doctors have to deal with hyperosmia in coronavirus. Of course, this infection is more characterized by a decrease in smell, but some patients also have an increased susceptibility to smells.
Symptoms of hyperosmia
Symptoms associated with hyperosmia are determined by the nature of the pathological process. Taking into account the underlying disease, the following manifestations may occur:
- skin rashes;
- runny nose, cough, fever, soreness of the nasal mucosa;
- hand tremors, headaches, dizziness, decreased memory and concentration;
- increased sensitivity of taste buds and a burning sensation of the tongue.
Treatment of hyperosmia
Hyperosmia in men and women is treated according to the main etiological factor. So, in case of inflammatory lesions of the nasal mucosa and paranasal sinuses, corticosteroids, immunomodulators and antibiotics are prescribed when the conditionally pathogenic flora is activated. The preferred route of administration is local (in the form of sprays, drops).
The preferred route of administration is local (in the form of sprays, drops).
If nasal polyps are found, they must be removed. The operation is performed by a minimally invasive endoscopic method, which is characterized by low trauma and a short rehabilitation period. nine0013
In the recovery phase, if hyperosmia persists and odors cannot be avoided, distraction therapy is recommended. It can be chewing gum or candy with a pronounced peppermint flavor.
If you are faced with the problem of hyperosmia, then do not tolerate this unpleasant condition. Sign up for a consultation with qualified otolaryngologists at the Ear, Nose and Throat Clinic. Our experts will help you to understand the reasons that led to the violation of smell, and will draw up a program of personalized treatment. Otolaryngologists of the Ear, Nose and Throat Clinic carry out treatment in accordance with international protocols for the provision of medical care for hyperosmia. nine0013
Seeing a doctor early can help keep you healthy.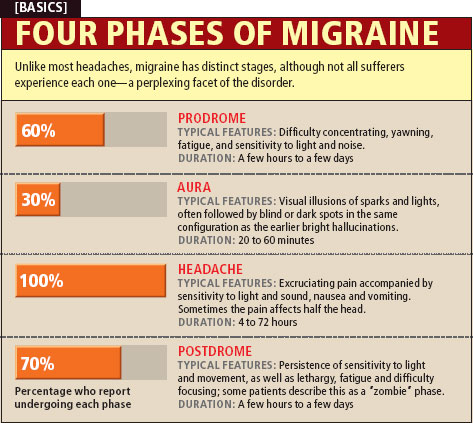
Do not delay treatment, call right now. We work around the clock in Moscow.
tel.: 8 (499) 501-15-53 (24 hours)
Exacerbation of the sense of smell - causes, diagnosis and treatment
Exacerbation of the sense of smell (hyperosmia) is an increased sensitivity to smells. Common physiological prerequisites for olfactory disorders are hormonal changes in women during pregnancy and in the premenstrual period. The symptom is characteristic of neurological and psychiatric diseases. To determine the cause of olfactory disorders, olfactometry, ENT examination, and instrumental methods of brain imaging are performed. Medications are aimed at treating the underlying pathology, so they are prescribed only after a diagnosis has been made. nine0013
Causes of increased sense of smell
Pregnancy
During gestation, a woman's body undergoes hormonal changes that cause hypersensitivity to aromas.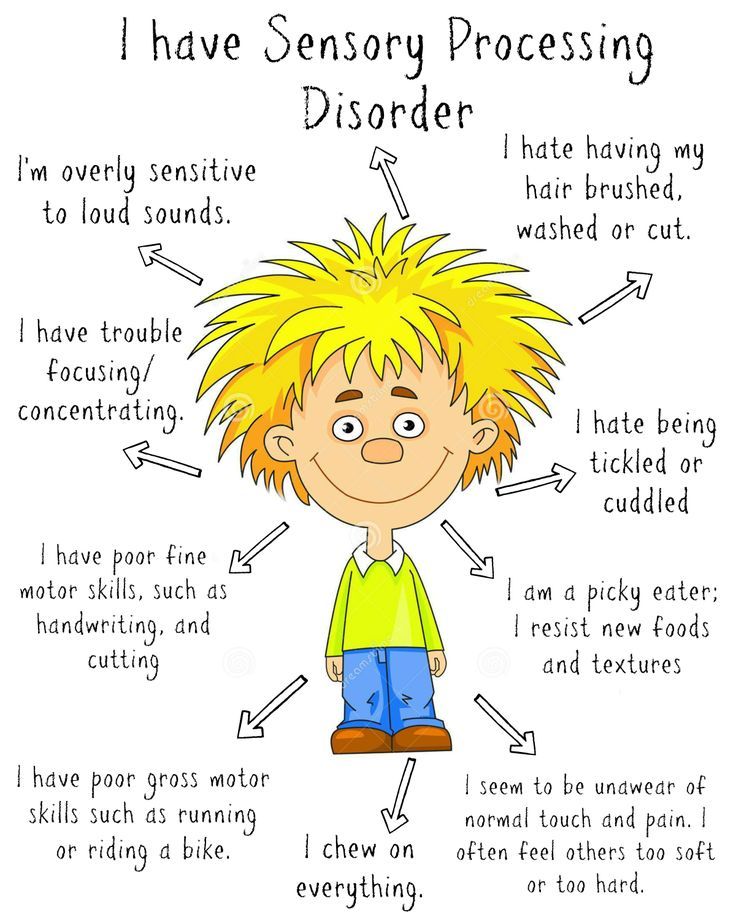 An increased sense of smell can be one of the first symptoms of pregnancy. Women often notice unpleasant pungent odors - fuel, fuel oil, rancid fat, combustion products that haunt them even indoors. Pleasant aromas, such as favorite perfumes or the smell of flowers, also seem very strong and intrusive, causing nausea and headaches. Some patients refuse to use cosmetics because of their smell. nine0013
An increased sense of smell can be one of the first symptoms of pregnancy. Women often notice unpleasant pungent odors - fuel, fuel oil, rancid fat, combustion products that haunt them even indoors. Pleasant aromas, such as favorite perfumes or the smell of flowers, also seem very strong and intrusive, causing nausea and headaches. Some patients refuse to use cosmetics because of their smell. nine0013
Hyperosmia is sometimes accompanied by a change in taste preferences - too strong aromas of familiar food provoke aversion in a pregnant woman, a gag reflex. Such symptoms are considered physiological, usually exacerbation of sensitivity to smells disappears after childbirth. The appearance of a future mother against the background of a change in the sense of smell of severe headaches, dizziness may indicate serious disorders, so such women need to consult a specialist. You also need to see a doctor if hyperosmia persists in the postpartum period. nine0013
Premenstrual period
A heightened sense of smell develops in women a few days before the onset of menstruation.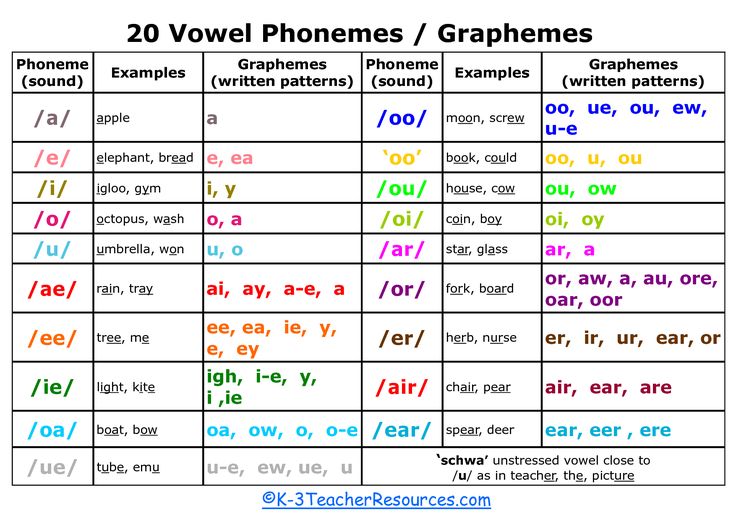 The symptom usually disappears with the onset of menstrual bleeding. Hyperosmia is characteristic of emotionally labile patients who are prone to tearfulness, rapid mood swings. At the same time, both the usual aromas of food, flowers, and the irritating smells of gasoline, acetone, etc. are intensified. Some women cannot travel by public transport during this period, since the increased susceptibility to smells of fuel, sweat causes nausea and headaches. nine0013
The symptom usually disappears with the onset of menstrual bleeding. Hyperosmia is characteristic of emotionally labile patients who are prone to tearfulness, rapid mood swings. At the same time, both the usual aromas of food, flowers, and the irritating smells of gasoline, acetone, etc. are intensified. Some women cannot travel by public transport during this period, since the increased susceptibility to smells of fuel, sweat causes nausea and headaches. nine0013
In most cases, the aggravation of the sense of smell is moderate, does not cause severe discomfort and does not interfere with the performance of daily work. Sometimes hyperosmia is combined with increased sensitivity to sounds of normal volume. In some women, the unpleasant symptoms of PMS persist during menstrual bleeding and even after the end of menstruation. This condition indicates hormonal disorders in the body, in which a consultation with a gynecologist or endocrinologist is indicated. nine0013
Diffuse toxic goiter
Exacerbation of the perception of various odors occurs due to changes in the functioning of olfactory receptors in the nasal mucosa, which is provoked by a sharp increase in the level of thyroid hormones. With thyrotoxicosis, patients react sharply to unpleasant odorous substances: they notice even faint odors of drugs, fuel combustion products. Patients complain of the constant presence of stench that bothers them both at home and on the street. Due to the increased sense of smell, taste is disturbed, some people develop an aversion to their favorite dishes. nine0013
With thyrotoxicosis, patients react sharply to unpleasant odorous substances: they notice even faint odors of drugs, fuel combustion products. Patients complain of the constant presence of stench that bothers them both at home and on the street. Due to the increased sense of smell, taste is disturbed, some people develop an aversion to their favorite dishes. nine0013
Migraine
In this disorder, the acute sense of smell occurs even before the onset of headaches. This condition is called migraine with aura, and its frequency is about 3.5%. Hyperosmia persists even after the onset of an attack - patients notice that even the presence of faint aromas worsens the condition, increases the intensity of headaches. In severe form, hypersensitivity to odors is combined with vomiting that does not bring relief. Exacerbation of the olfactory function and increased perception of smells can serve as a provoking factor for migraine, which is observed in 60% of cases. nine0013
Diseases of the brain
Various pathologies of a neurological nature cause damage to specialized centers in the cerebral cortex that are responsible for the recognition of aromas. At the same time, the sense of smell often increases gradually, complaints of intolerance to sharp medicinal or chemical odorous substances are typical. Patients also note an increased sensitivity to floral and herbal aromas, exhaust gases. The symptom is accompanied by headaches, periodic dizziness and fainting, sometimes disturbed by visual impairment. With the development of hyperosmia proceed:
At the same time, the sense of smell often increases gradually, complaints of intolerance to sharp medicinal or chemical odorous substances are typical. Patients also note an increased sensitivity to floral and herbal aromas, exhaust gases. The symptom is accompanied by headaches, periodic dizziness and fainting, sometimes disturbed by visual impairment. With the development of hyperosmia proceed:
- Brain tumors : astrocytoma, glioma, meningioma, etc.
- Degenerative diseases : multiple sclerosis, dyscirculatory encephalopathy.
Mental illnesses
Exacerbation of the sense of smell is manifested by both severe illnesses - schizophrenia, epilepsy, depression, and disorders of the neurotic register - neurasthenia, psychasthenia. Schizophrenia is characterized by olfactory hallucinations, when the patient constantly feels a certain aroma (the smell of feces, decay). The sense of smell may increase shortly before the onset of an epileptic seizure as a component of the sensory aura. When depressed, patients complain of a sensation of stench from an unknown source, some patients believe that this smell appears due to the decay of their own body. nine0013
When depressed, patients complain of a sensation of stench from an unknown source, some patients believe that this smell appears due to the decay of their own body. nine0013
Rare causes
- Complications after past infections : tick-borne encephalitis, typhus, Lyme disease.
- Endocrine pathology : type 1 diabetes mellitus, disorders of the hypothalamic-pituitary system.
- Autoimmune diseases : systemic lupus erythematosus, scleroderma.
Examination
Since the aggravation of sense of smell is more often caused by dysfunction of specific nerve centers in the brain, a consultation with a neurologist is indicated. During the diagnosis, the doctor assesses the degree of impairment of the olfactory function, examines in detail the state of the central nervous system in order to find the root cause of the symptom. For this, a comprehensive examination of both the nervous system and the peripheral part of the olfactory analyzer is carried out.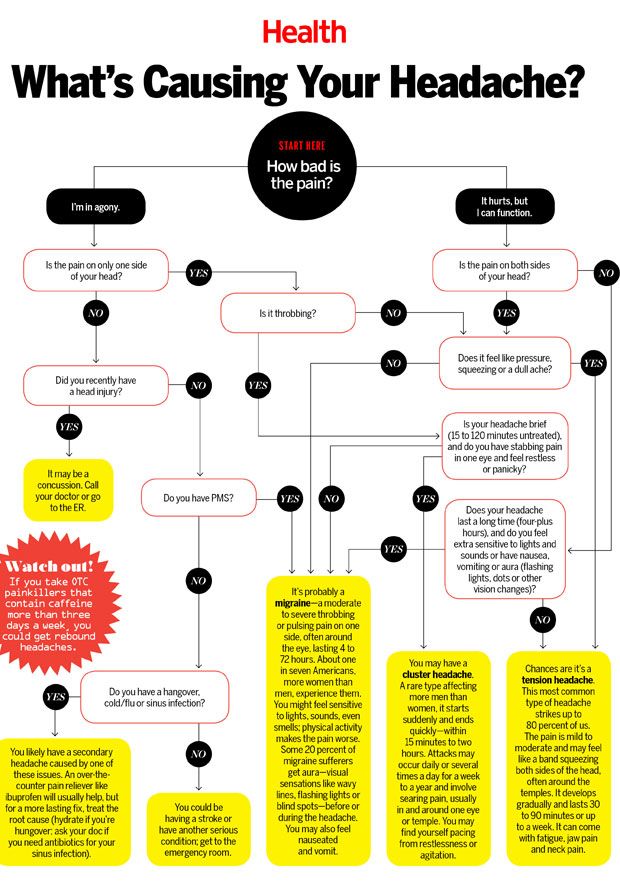 The most informative are:
The most informative are:
- Olfactometry . Recognition of certain odorous substances from test tubes allows an objective assessment of the quality and degree of increased perception of odors. The method of quantitative olfactometry is designed to measure the threshold of smell and the rate of adaptation of the olfactory analyzer.
- X-ray examination . To exclude organic brain damage, which could provoke an exacerbation of sensations during the perception of aromas, computed tomography is prescribed. With insufficient information content, the method is supplemented with MRI for accurate visualization of brain structures. nine0004
- EEG . The study of the electrical activity of the brain is necessary for the diagnosis of pathologies such as epilepsy, migraine, degenerative neurological diseases. With the help of electroencephalography, the frequency and amplitude of the waves, the presence of foci of increased excitability in the brain tissue are determined.

- ENT examination . All patients with an exacerbation of the sense of smell are recommended to perform rhinoscopy to visualize the mucous membrane of the superior nasal concha, which contains olfactory receptors. If a suspicious altered tissue is detected, a biopsy and cytomorphological examination are performed. nine0004
- Laboratory tests . Women of reproductive age measure the concentration of sex hormones on different days of the cycle. Also evaluate the levels of thyroxine and triiodothyronine, insulin. To exclude pregnancy, a blood test for human chorionic gonadotropin is prescribed.
In the absence of neurological reasons for the heightened sense of smell, women are prescribed an examination by a gynecologist. If hyperthyroidism or other endocrine disorders are suspected, patients are referred to a specialist for further diagnosis and treatment. If there are suspicious symptoms, a psychiatric evaluation may be required.