Ssri induced mania
Is Antidepressant-Induced Mania Possible?
Feeling invincible, impulsive, and endlessly energetic aren’t signs typically linked to depression — unless you may be experiencing antidepressant-induced mania linked to undiagnosed bipolar disorder.
Taking antidepressants may increase your chances of a manic episode in bipolar disorder but also in conditions that don’t typically feature the symptom — for example, major depressive disorder, if you have bipolar disorder that’s gone undiagnosed.
Not everyone taking antidepressants will experience mania.
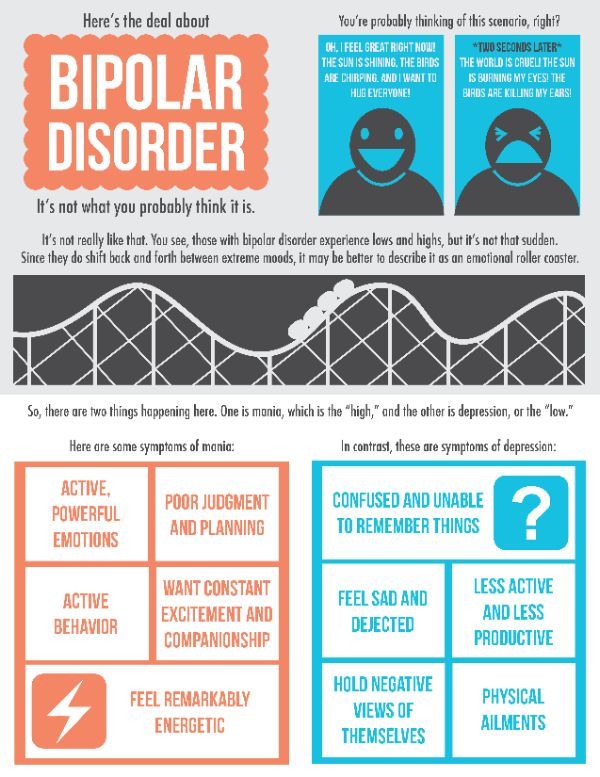
Mania is a mood episode that presents with symptoms like agitation, elevated mood, and impulsivity. It’s primarily a formal symptom of bipolar disorder.
What are mania and hypomania?
Mania is a state of heightened mood, agitation, and intense physical and mental energy that can lead to major impairment in social or occupational areas of function. It can present in a number of ways, but often involves:
- rapid speech
- decreased need for sleep
- feelings of grandiosity
- racing thoughts
- irritability
- impulsivity
- distractibility
Hypomania is a milder version of mania that involves some of the same symptoms but not to the point of causing significant impairment or keeping you from your everyday routine.
Antidepressants may increase the chances of an episode of mania or hypomania in certain people being treated for either unipolar or bipolar depression. That’s why some people say that antidepressants can make bipolar disorder worse. But it isn’t that simple.
While antidepressants are primarily prescribed for the treatment of major depressive disorder (unipolar or clinical depression), they may also be used to treat conditions featuring depressive episodes, like bipolar disorder.
In some cases, antidepressants are also used in the management of chronic pain, anxiety, and chronic insomnia.
Mania or affective switching?
During antidepressant treatment, shifting from an episode of depression to one that involves agitation is known as affective switching.
Some conditions, like bipolar disorder, are naturally characterized by cyclic affective switching. This means that people go through mood episodes in a given period of time. Antidepressant-induced mania isn’t part of the bipolar disorder cycle.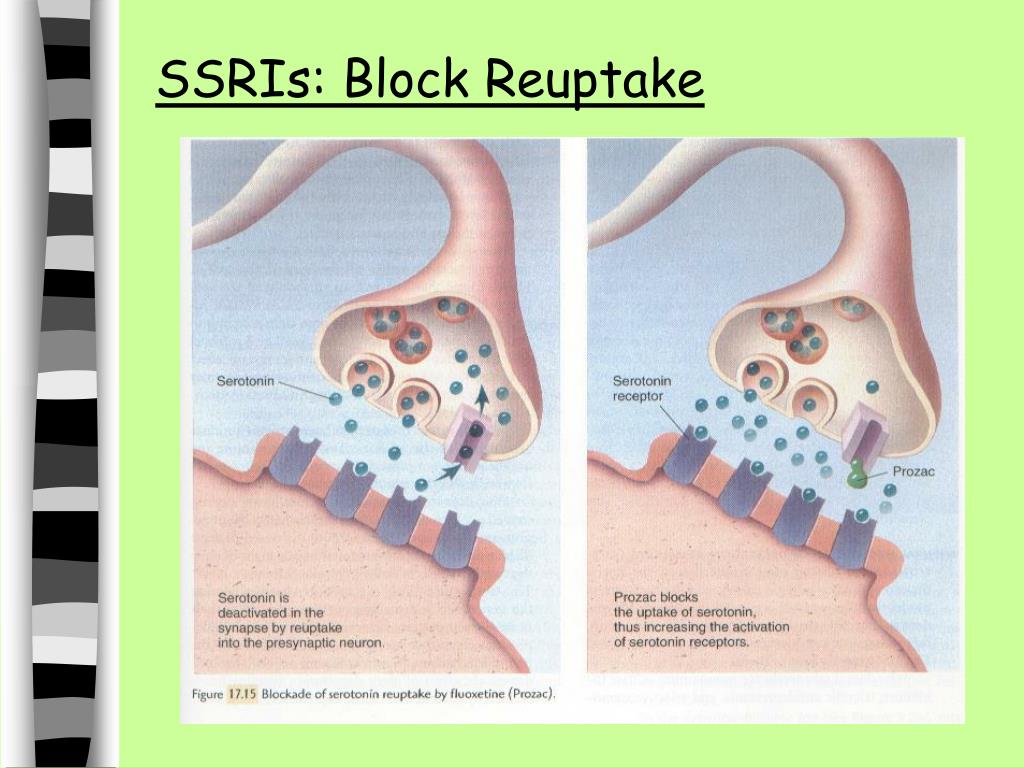
When you live with depression, you don’t go through mood episodes, like in bipolar disorder. Your mood typically stays the same, particularly in untreated depression. This is why mania during depression treatment can be the result of undiagnosed bipolar disorder.
But if you experience antidepressant-induced mania during your depression treatment, do you still have major depression or is it now bipolar disorder? Maybe neither.
Some experts argue that experiencing antidepressant-induced mania can’t be properly classified under current diagnostic criteria for depression or bipolar disorder and should have its own subtype category in the list of diagnoses.
Mania in bipolar disorder
Mania and hypomania are formal symptoms of bipolar disorder.
Mania is not a formal symptom of depression, a condition defined as persistent low mood and inability to experience joy.
You may go through depressive episodes when living with bipolar disorder, but it’s the presence of mania or hypomania that defines this condition.
You can experience bipolar disorder without depression, but you can’t experience bipolar disorder without mania or hypomania.
Who is more likely to experience antidepressant-induced mania?
People already living with bipolar disorder are more likely to experience a sudden episode of mania after taking certain antidepressants. But not everyone with the condition.
A 2018 review of bipolar depression notes that antidepressant-induced affective switching appears more common among people who:
- experience depression with mixed features
- are on older generation antidepressants
- have a history of substance use disorder
You may be more likely to experience antidepressant-induced mania if you:
- live with bipolar I disorder
- are receiving antidepressant monotherapy
- already experience rapid mood cycling
Women, younger people, and those with a family history of bipolar disorder, may have an increased chance of antidepressant-induced hypomania, according to a 2020 unipolar depression review.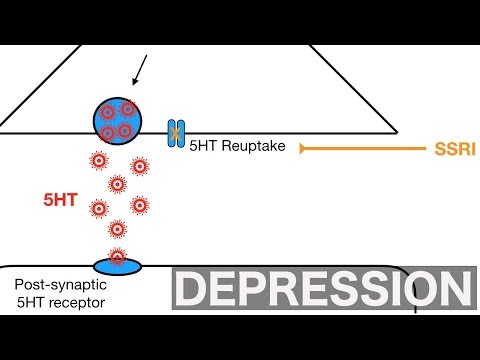
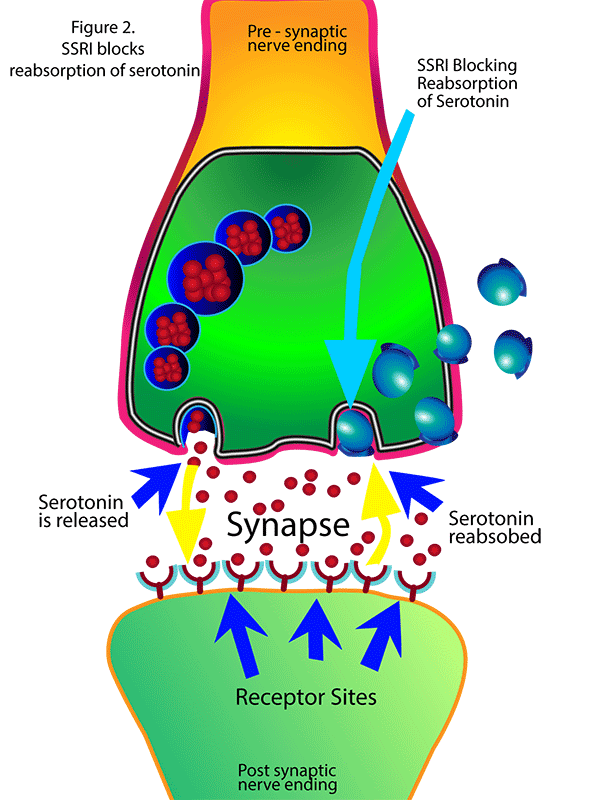
Research suggests the use of older generation antidepressants, known as tricyclics, may cause a greater chance of mania compared to modern antidepressant options.
Tricyclic antidepressants include:
- doxepin
- imipramine
- amitriptyline
- clomipramine
- desipramine
- nortriptyline
- amoxampine
- protriptyline
- trimipramine
Antidepressant-induced mania is not considered a common side effect of antidepressants.
According to cross-sectional patient data collected over a 2-year period, the challenges people may experience when taking these medications include:
- indigestion
- nausea
- abdominal pain
- diarrhea
- constipation
- sudden heat stroke
- intense sweating
- dry mouth
- changes in sleeping patterns
- diminished sex drive
- changes in weight
Different antidepressants may come with side effects more common to their class.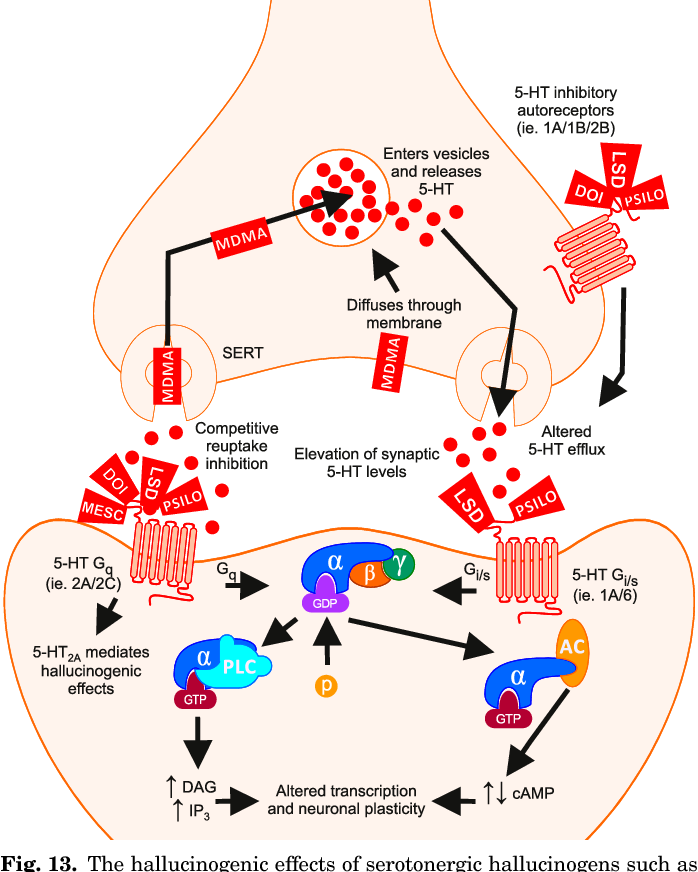
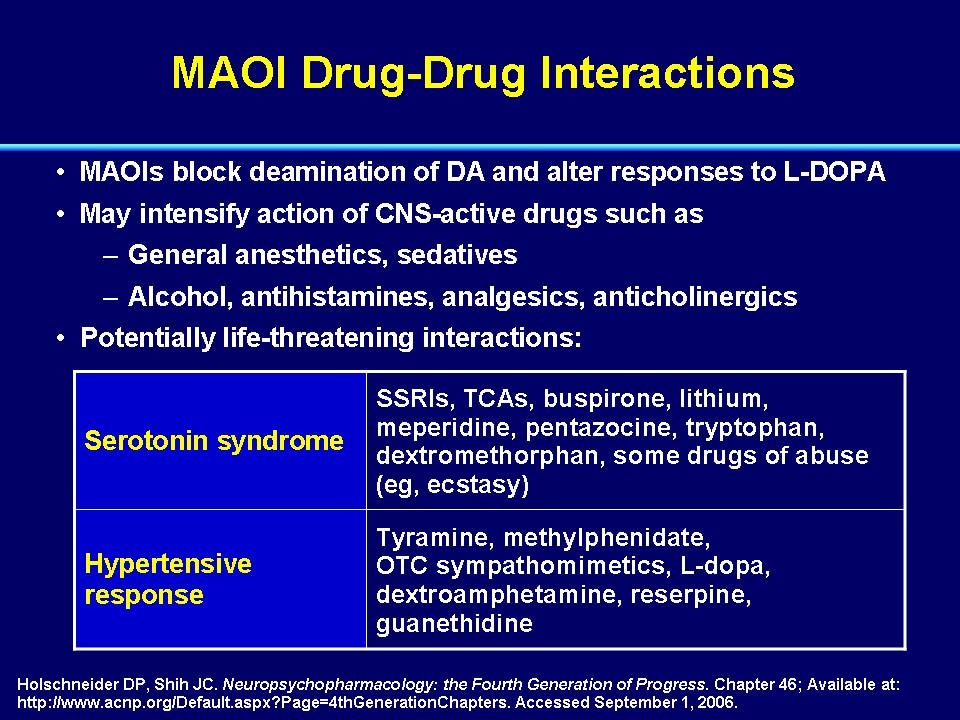
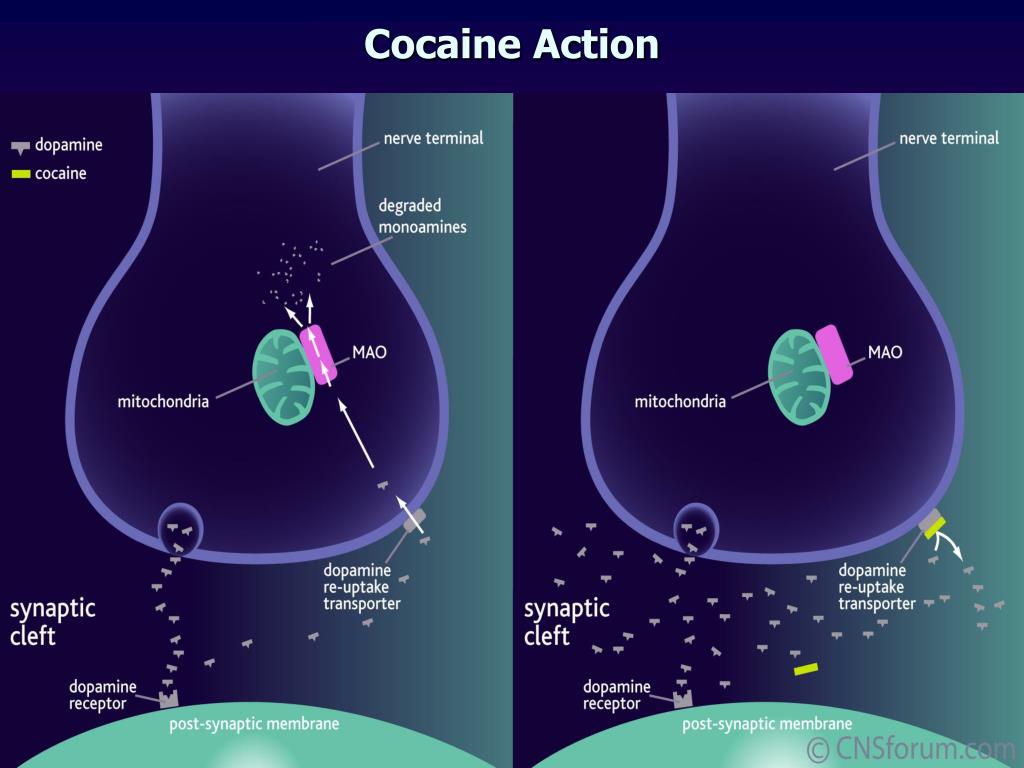
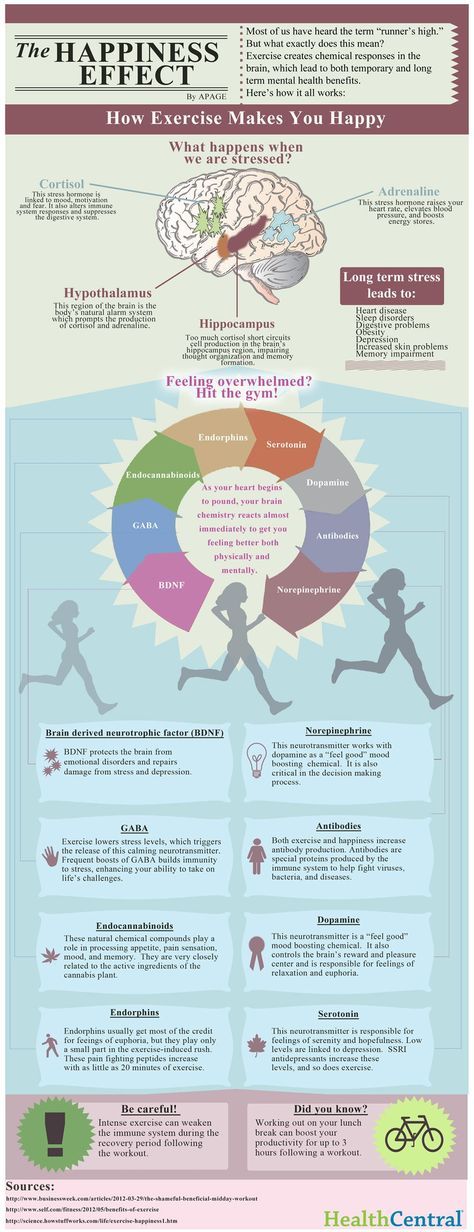
Selective serotonin reuptake inhibitors (SSRIs), for example, are known to have common side effects of dizziness, anxiety, headaches, and restlessness.
There’s no scientific evidence suggesting antidepressants cause or trigger bipolar disorder.
Antidepressants may increase the chance you’ll experience an episode of mania if you have major depressive disorder when you also have bipolar disorder but haven’t yet received a diagnosis.
Experts have not reached a consensus on determining if this experience should lead to a new bipolar disorder diagnosis.
Currently, researchers are considering including a bipolar or depressive disorder subtype that may be specific to antidepressant sensitivity causing a manic episode.
If you’ve been diagnosed with major depressive disorder, experiencing mania is not typical. Any moods related to elation, agitation, or grandiosity may be medication-induced or could mean you also have bipolar disorder.
If you live with bipolar disorder, you can also experience antidepressant-induced mania outside of your cyclic mood cycles.
While antidepressant-induced mania remains diagnostically controversial, mood stabilizers may help prevent this type of affective switching, regardless of the underlying condition.
Article resources
- Barbuti M, et al. (2017). Antidepressant-induced hypomania/mania in patients with major depression: Evidence from the BRIDGE-II-MIX study. https://www.sciencedirect.com/science/article/abs/pii/S0165032717300290
- Beaupre M, et al. (2020). Antidepressant-associated mania in bipolar disorder: A review and meta-analysis of potential clinical and genetic risk factors. https://journals.lww.com/psychopharmacology/Abstract/2020/03000/Antidepressant_Associated_Mania_in_Bipolar.11.aspx
- Bipolar disorder. (2020). https://www.nimh.nih.gov/health/topics/bipolar-disorder
- Dailey MW, et al. (2022). Mania. https://www.ncbi.nlm.nih.gov/books/NBK493168/
- Gill N, et al. (2020). A review of antidepressant-associated hypomania in those diagnosed with unipolar depression—risk factors, conceptual models, and management.
 https://www.researchgate.net/publication/340175853_A_Review_of_Antidepressant-Associated_Hypomania_in_Those_Diagnosed_with_Unipolar_Depression-Risk_Factors_Conceptual_Models_and_Management
https://www.researchgate.net/publication/340175853_A_Review_of_Antidepressant-Associated_Hypomania_in_Those_Diagnosed_with_Unipolar_Depression-Risk_Factors_Conceptual_Models_and_Management - Gitlin MJ. (2018). Antidepressants in bipolar depression: An enduring controversy. https://journalbipolardisorders.springeropen.com/articles/10.1186/s40345-018-0133-9
- Patel R, et al. (2015). Do antidepressants increase the risk of mania and bipolar disorder in people with depression? A retrospective electronic case register cohort study. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4679886/
- Ramic E, et al. (2020). Assessment of the antidepressant side effects occurrence in patients treated in primary care. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7428926/
- Table 2 list of antidepressants and their categorizations. (n.d.). https://www.ncbi.nlm.nih.gov/books/NBK36406/table/ch2.t2/
Antidepressant-induced mania: an overview of current controversies
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Wiley
Full text links
Review
. 2003 Dec;5(6):407-20.
2003 Dec;5(6):407-20.
doi: 10.1046/j.1399-5618.2003.00067.x.
Joseph F Goldberg 1 , Christine J Truman
Affiliations
Affiliation
- 1 Department of Psychiatry Research, The Zucker Hillside Hospital, Glen Oaks, NY 11004, USA. [email protected]
- PMID: 14636364
- DOI: 10.1046/j.1399-5618.2003.00067.x
Review
Joseph F Goldberg et al. Bipolar Disord. 2003 Dec.
. 2003 Dec;5(6):407-20.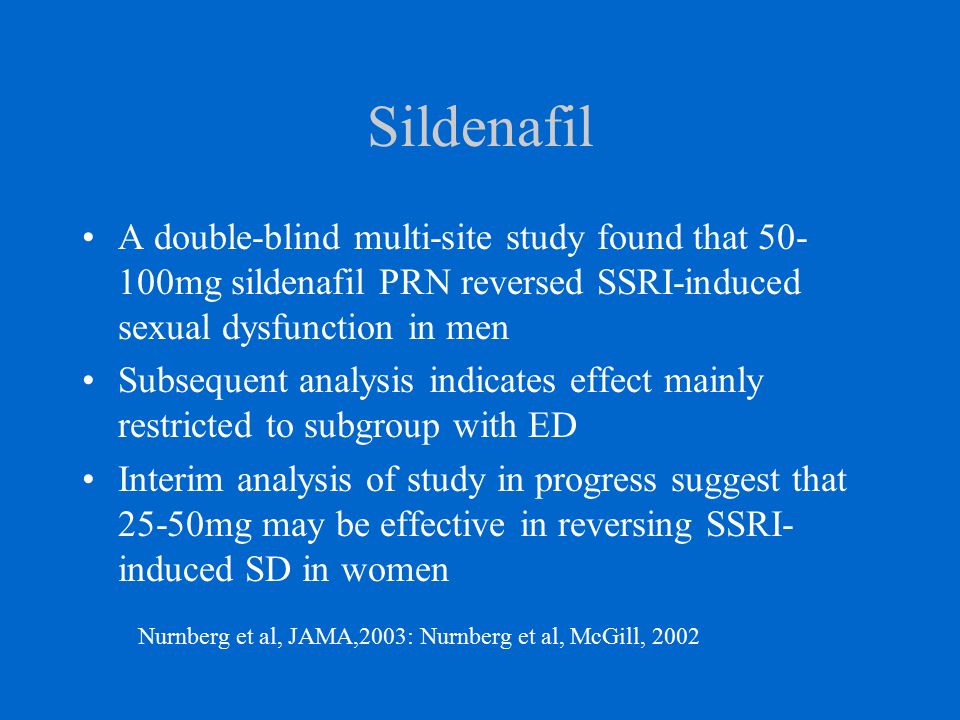
doi: 10.1046/j.1399-5618.2003.00067.x.
Authors
Joseph F Goldberg 1 , Christine J Truman
Affiliation
- 1 Department of Psychiatry Research, The Zucker Hillside Hospital, Glen Oaks, NY 11004, USA. [email protected]
- PMID: 14636364
- DOI: 10.1046/j.1399-5618.2003.00067.x
Abstract
Objective: The prevalence, characteristics, and possible risk factors associated with antidepressant-induced mania remain poorly described.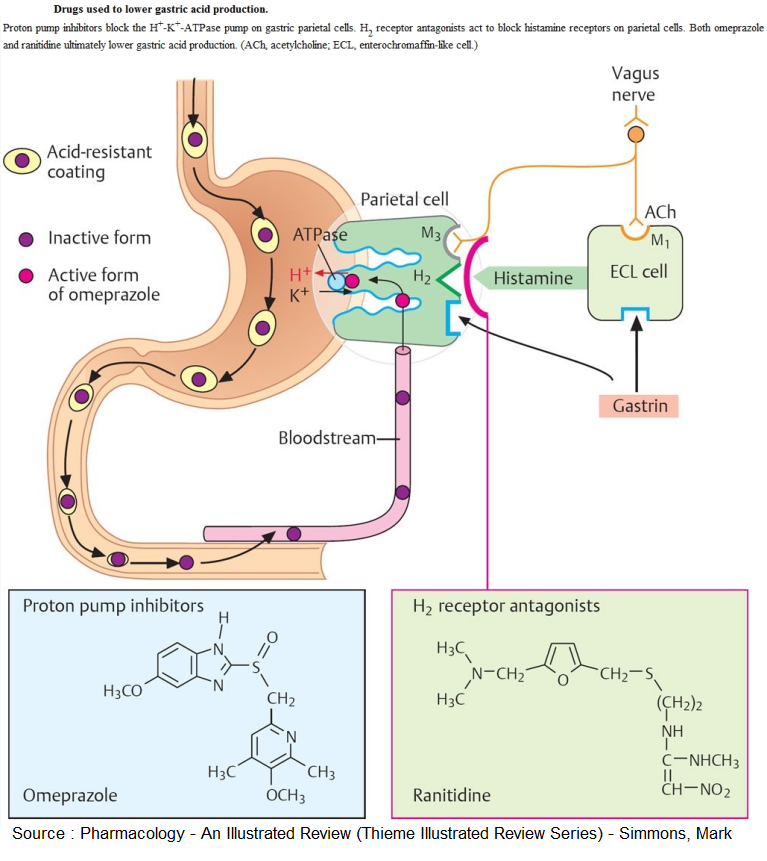 The present review sought to identify published rates of antidepressant-induced mania and describe risk factors for its emergence.
The present review sought to identify published rates of antidepressant-induced mania and describe risk factors for its emergence.
Methods: A MedLine search was conducted of journals that focused on mania or hypomania associated with recent antidepressant use. Data from published reports were augmented with relevant findings from recent clinical trials presented at scientific conferences.
Results: Antidepressant-induced manias have been reported with all major antidepressant classes in a subgroup of about 20-40% of bipolar patients. Lithium may confer better protection against this outcome when compared with other standard mood stabilizers, although switch rates have been reported with comparable frequencies on or off mood stabilizers. Evidence across studies most consistently supports an elevated risk in patients with (i) previous antidepressant-induced manias, (ii) a bipolar family history, and (iii) exposure to multiple antidepressant trials.
Conclusion: About one-quarter to one-third of bipolar patients may be inherently susceptible to antidepressant-induced manias. Bipolar patients with a strong genetic loading for bipolar illness whose initial illness begins in adolescence or young adulthood may be especially at risk. Further efforts are needed to better identify high-vulnerability subgroups and differentiate illness-specific from medication-specific factors in mood destabilization.
Similar articles
-
Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers.
Leverich GS, Altshuler LL, Frye MA, Suppes T, McElroy SL, Keck PE Jr, Kupka RW, Denicoff KD, Nolen WA, Grunze H, Martinez MI, Post RM.
 Leverich GS, et al. Am J Psychiatry. 2006 Feb;163(2):232-9. doi: 10.1176/appi.ajp.163.2.232. Am J Psychiatry. 2006. PMID: 16449476 Clinical Trial.
Leverich GS, et al. Am J Psychiatry. 2006 Feb;163(2):232-9. doi: 10.1176/appi.ajp.163.2.232. Am J Psychiatry. 2006. PMID: 16449476 Clinical Trial. -
The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study.
Goldberg JF, Whiteside JE. Goldberg JF, et al. J Clin Psychiatry. 2002 Sep;63(9):791-5. doi: 10.4088/jcp.v63n0907. J Clin Psychiatry. 2002. PMID: 12363119
-
Bipolar disorder, antidepressants and induction of hypomania or mania. A systematic review.
Visser HM, Van Der Mast RC. Visser HM, et al. World J Biol Psychiatry. 2005;6(4):231-41. doi: 10.1080/15622970510029885. World J Biol Psychiatry. 2005. PMID: 16272078
-
Antidepressants in bipolar disorder: the case for caution.
Ghaemi SN, Hsu DJ, Soldani F, Goodwin FK. Ghaemi SN, et al. Bipolar Disord. 2003 Dec;5(6):421-33. doi: 10.1046/j.1399-5618.2003.00074.x. Bipolar Disord. 2003. PMID: 14636365 Review.
-
Antidepressant-associated mood elevations in bipolar II disorder compared with bipolar I disorder and major depressive disorder: a systematic review and meta-analysis.
Bond DJ, Noronha MM, Kauer-Sant'Anna M, Lam RW, Yatham LN. Bond DJ, et al. J Clin Psychiatry. 2008 Oct;69(10):1589-601. doi: 10.4088/jcp.v69n1009. J Clin Psychiatry. 2008. PMID: 19192442 Review.
See all similar articles
Cited by
-
Clinical research diagnostic criteria for bipolar illness (CRDC-BP): rationale and validity.
Ghaemi SN, Angst J, Vohringer PA, Youngstrom EA, Phelps J, Mitchell PB, McIntyre RS, Bauer M, Vieta E, Gershon S. Ghaemi SN, et al. Int J Bipolar Disord. 2022 Oct 13;10(1):23. doi: 10.1186/s40345-022-00267-3. Int J Bipolar Disord. 2022. PMID: 36227452 Free PMC article. Review.
-
Antidepressant Treatment and Manic Switch in Bipolar I Disorder: A Clinical and Molecular Genetic Study.
Chen CK, Wu LS, Huang MC, Kuo CJ, Cheng AT. Chen CK, et al. J Pers Med. 2022 Apr 11;12(4):615. doi: 10.3390/jpm12040615. J Pers Med. 2022. PMID: 35455731 Free PMC article.
-
Transcranial magnetic stimulation-associated mania with psychosis: A case report.
Knox ED, Bota RG. Knox ED, et al. Ment Health Clin.
 2021 Nov 8;11(6):373-375. doi: 10.9740/mhc.2021.11.373. eCollection 2021 Nov. Ment Health Clin. 2021. PMID: 34824963 Free PMC article.
2021 Nov 8;11(6):373-375. doi: 10.9740/mhc.2021.11.373. eCollection 2021 Nov. Ment Health Clin. 2021. PMID: 34824963 Free PMC article. -
Gut Hormones as Potential Therapeutic Targets or Biomarkers of Response in Depression: The Case of Motilin.
Rajkumar RP. Rajkumar RP. Life (Basel). 2021 Aug 29;11(9):892. doi: 10.3390/life11090892. Life (Basel). 2021. PMID: 34575041 Free PMC article. Review.
-
Mapping mania symptoms based on focal brain damage.
Cotovio G, Talmasov D, Barahona-Corrêa JB, Hsu J, Senova S, Ribeiro R, Soussand L, Velosa A, Silva VCE, Rost N, Wu O, Cohen AL, Oliveira-Maia AJ, Fox MD. Cotovio G, et al. J Clin Invest. 2020 Oct 1;130(10):5209-5222. doi: 10.1172/JCI136096. J Clin Invest.
 2020. PMID: 32831292 Free PMC article.
2020. PMID: 32831292 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Grant support
- K-23 MH-01936/MH/NIMH NIH HHS/United States
Full text links
Wiley
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
Typology, pathomorphosis and therapy of non-psychotic affective disorders in patients with epilepsy
1. Avakyan G.G. Depression and epilepsy: two sides of the same coin / G.G. Avakyan, O.L. Badalyan, S.G. Burd and others // Rus. honey. magazine - 2008. - T. 16, No. 12. - S. 16531658.
Avakyan G.G. Depression and epilepsy: two sides of the same coin / G.G. Avakyan, O.L. Badalyan, S.G. Burd and others // Rus. honey. magazine - 2008. - T. 16, No. 12. - S. 16531658.
2. Avrutsky G.Ya. Treatment of the mentally ill / G.Ya. Avrutsky, A.A. Neduva. -M.: Medicine, 1988. 528 p.
3. Aleksandrovsky Yu.A. Borderline mental disorders: Handbook. for doctors / Yu.A. Alexandrovsky. -2nd ed. - M .: Phoenix, 1997. 571 p.
4. Bilikevich T. Psychopathology of temporal lobe epilepsy / T. Bilikevich // Zhurn. neuropathology and psychiatry. S.S. Korsakov. 1970. - T. 70. - No. 9. - S. 1353-1356.
5. Boldyrev A.I. Viscero-vegetative paroxysms in the initial stage of epilepsy / A.I. Boldyrev // Tr. Moscow Research Institute of Psychiatry of the Ministry of Health of the RSFSR. 1966. - T. 45.-S. 198-202.
6. Boldyrev A.I. Mental characteristics of patients with epilepsy (43 years of experience in the study and treatment of patients with epilepsy) / A.I. Boldyrev. M.: Medicine, 2000. - 384 p.
M.: Medicine, 2000. - 384 p.
7. Boldyrev A.I. Epilepsy in adults / A.I. Boldyrev. M.: Medicine, 1971. -368 p.
8. Boldyrev A.I. Epileptic syndromes / A.I. Boldyrev. M.: Medicine, 1976.-264 p.
9. Boreyko V.B. Mental disorders in indications and long-term results of surgical treatment of patients with temporal lobe epilepsy: Ph.D. dis. . cand. honey. Sciences: 14.00.18. Sverdlovsk, 1973. - 24 p.
10. Borovikov V.P. STATISTICA: The art of computer data analysis. For professionals / V.P. Borovikov. St. Petersburg: Piter print, 2003. - 688 p.
11. Bragina N.N. Functional human asymmetries / N.N. Bragina, T.A. Dobrokhotov. M.: Medicine, 1988. - 240 p.
12. Brown T. Epilepsy: Clinical Guide / T. Brown, G. Holmes: trans. from English. M.: BINOM, 2006. - 288 p.
13. Wasserman L.I. Medical psychodiagnostics. Theory, practice and education / L.I. Wasserman, O.Yu. Shchelkova. St. Petersburg: Publishing House of St. Petersburg State University; M.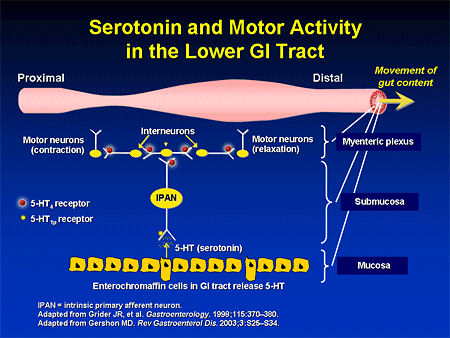 : Publishing Center "Academy.", 2003. - 736 p.
: Publishing Center "Academy.", 2003. - 736 p.
14. Vovin R.Ya. Preventive treatment of affective psychoses with finlepsin / R.Ya.Vovin, A.G. Digilov, A.I. Skorik // Zhurn. neuropathology and psychiatry. S.S. Korsakov. 1984. - T. 84, No. 8. - S. 1226-1230.
15. Vorobieva O.V. The effectiveness of the newest anticonvulsant pregabalin in the treatment of epileptic focal seizures / O.V. Vorobieva // Consilium medicum. 2007. - V. 9, No. 8. - S. 39-43.
16. Goldberg D. Common mental disorders: Biosocial model / D. Goldberg, P. Huxley: per. from English. Kyiv: Sfera, 1999. - 255 p.
17. Gromov S.A. controlled epilepsy. Clinic, diagnosis, treatment / S.A. Gromov. St. Petersburg: IIC "Baltika", 2004. - 302 p.
18. Gurevich M.O. On the diagnostic value of psychosensory disorders / M.O. Gurevich // 50 years of the Psychiatric Clinic. S.S. Korsakov. M., 1949. -S. 35-39.
19. Gurevich M.O. On the psychosensory form of epilepsy and on special conditions / M.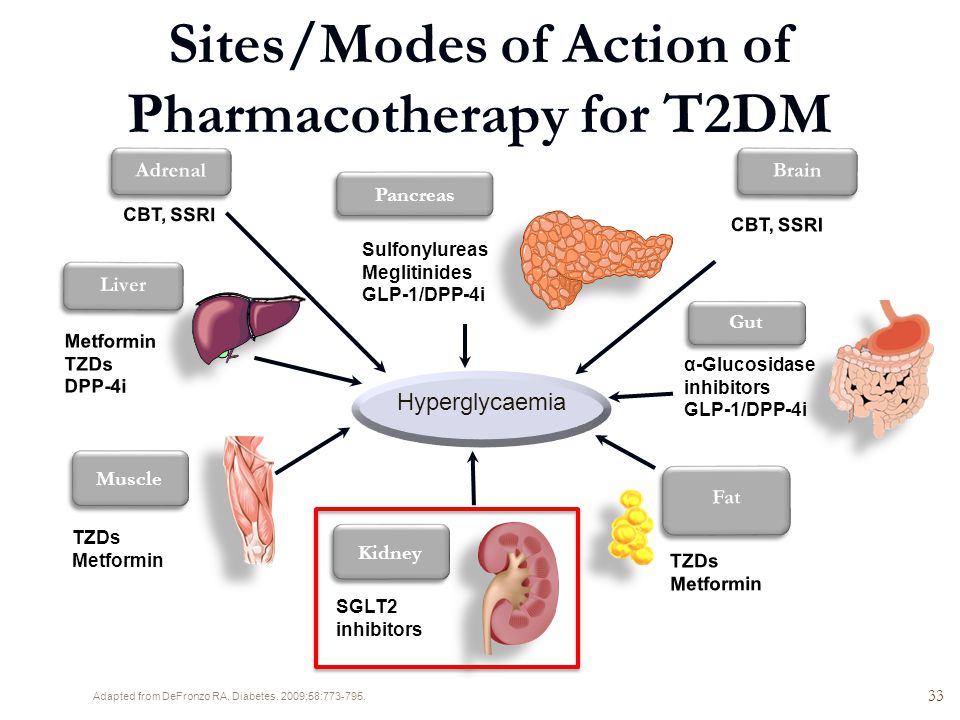 O. Gurevich //Tr. Moscow region conf. on epilepsy. - M., 1936. T. 4. - S. 5-10.
O. Gurevich //Tr. Moscow region conf. on epilepsy. - M., 1936. T. 4. - S. 5-10.
20. Gurevich M.O. On space perception disorders / M.O. Gurevich // Neuropathology, psychiatry and psychohygiene. 1936. - T. 4. - No. 5. - S. 527-535.
21. Gurovich I.Ya. The place of Paxil (paroxetine) among other antidepressants and clinical and social aspects of its use / I.Ya. Gurovich, A.B. Shmukler // Rus. honey. magazine 2007. - V. 15, No. 5. - S. 412-417.
22. Dysphoric conditions in children and adolescents with epilepsy (clinic, diagnosis, treatment): a guide for doctors / SPbNIPNI them. V.M. Bekhterev; comp.: I.V. Makarov, R.A. Kharitonov, Yu.A. Yakovleva and others - St. Petersburg, 2008.-17 p.
23. Dobrokhotova T.A. To the clinic of emotional-affective pathology with local (tumor) brain damage: abstract of the thesis. dis. . cand. honey. Sciences. -M.: 1968.-26 p.
24. Dobrokhotova T.A. Functional asymmetry and psychopathology of focal lesions of the brain / T.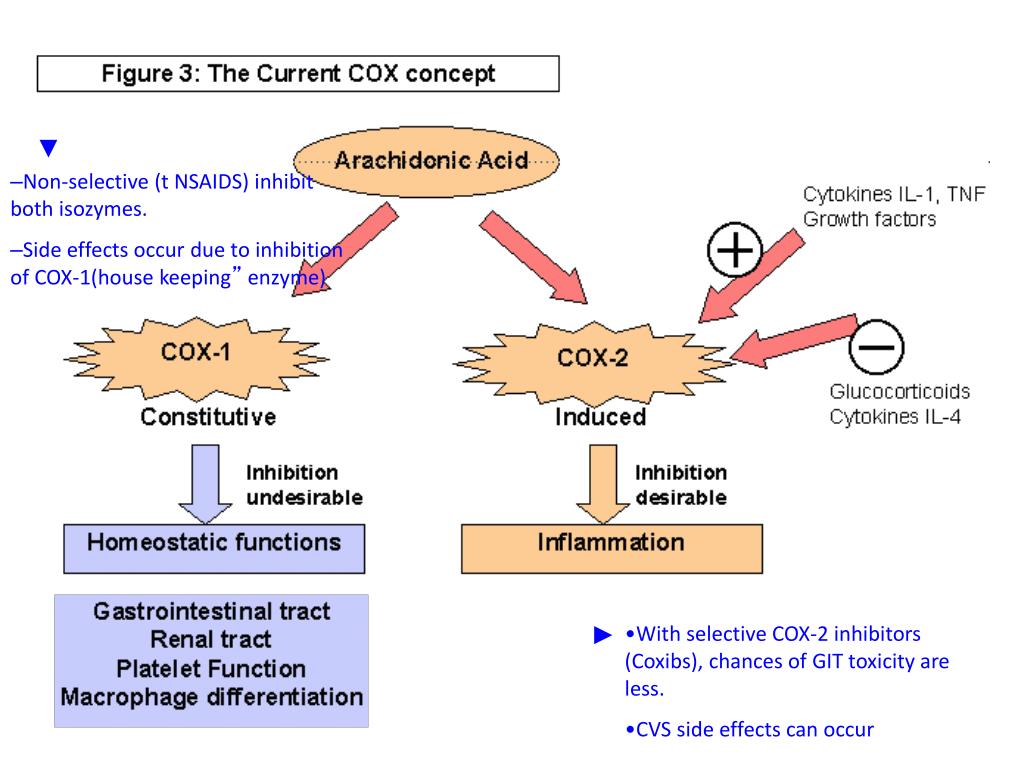 A. Dobrokhotova, N.N. Bragina - M .: Medicine, 1977. - 360 p.
A. Dobrokhotova, N.N. Bragina - M .: Medicine, 1977. - 360 p.
25. Drobizhev M.Yu. Treatment of depression in the general somatic network / M.Yu. Drobizhev // Psychiatry and psychopharmacology. 2004. - V.5, No. 5. - S. 190-193.
26. Eliseev O.P. Workshop on personality psychology / O.P. Eliseev. 2nd ed., rev. and reworked. - St. Petersburg: Peter, 2008. - 512 p.
27. Zharikov N.M. Psychiatry: Textbook / N.M. Zharikov, Yu.G. Tyulpin M.: Medicine, 2000. - 544 p.
28. Zenkov L.R. Keppra in the treatment of epilepsy / L.R. Zenkov. M.: OOO "Press Service", 2007. - 48 p.
29. Zenkov L.R. Clinical electroencephalography (with elements of epileptology). Guide for doctors. 3rd ed. / L.R. Zenkov. - M.: MEDpress-inform, 2004. - 368 p.
30. Kazakovtsev B.A. Mental disorders in epilepsy / B.A. Kazakovtsev. -M.: Amipress, 1999.-416 p.
31. Kalinin V.V. Anticonvulsant and psychotropic properties of antiepileptic drugs in the treatment of patients with epilepsy /, V.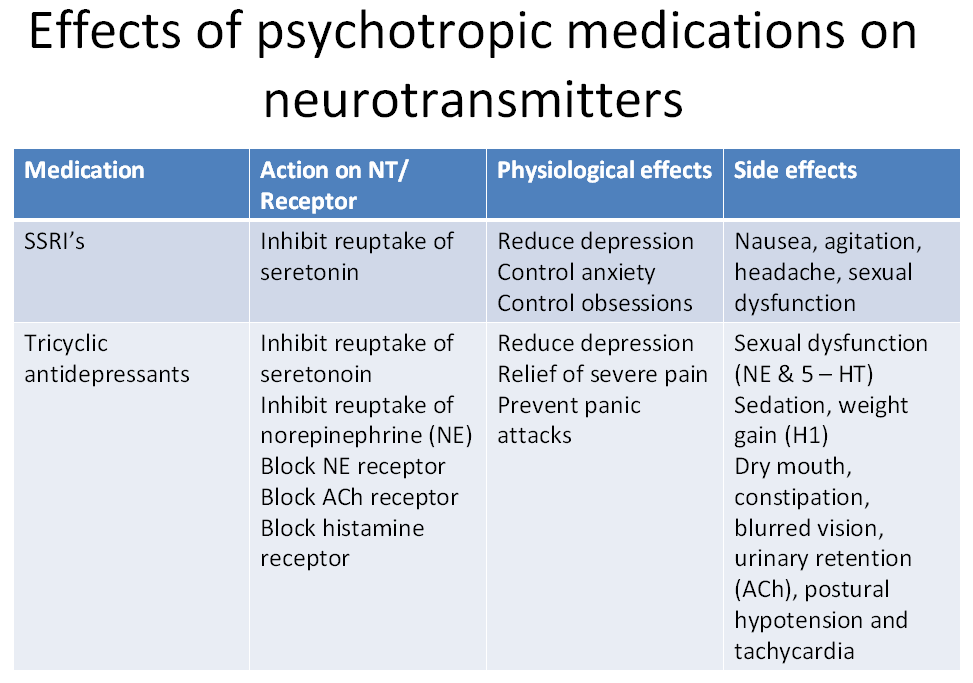 V. Kalinin, E.V. Zheleznova. M.: ArtInfo Publishing, 2008. - 29With.
V. Kalinin, E.V. Zheleznova. M.: ArtInfo Publishing, 2008. - 29With.
32. Kalinin V.V. Psychotropic and cognitive effects of topiramate in the treatment of patients with epilepsy / V.V. Kalinin, E.V. Zheleznova, L.V. Sokolova et al. // Zhurn. neurology and psychiatry. S.S. Korsakov. 2008. - T. 108, No. 2. - S. 63-69.
33. Karlov V.A. Epilepsy / V.A. Karlov. M.: Medicine, 1990. - 336 p.
34. Kissin M.Ya. Clinic and therapy of partial vegetative-visceral and "mental" seizures in patients with epilepsy: Textbook method. allowance / M.Ya.Kissin; ed. L.P. Rubina, I.V. Makarov. SPb., 2003. - 53 p.
35. Kissin M.Ya. Clinical epileptology / M.Ya. Kissin. -M.: GEOTAR-Media, 2009. 256 p.
36. Kissin M.Ya. States of consciousness in patients with simple partial seizures / M.Ya. Kissin // Paroxysmal brain. Multidisciplinary approach to the problem: Sat. abstract scientific conf. with international participation. SPb., 2004.-S. 53-54.
37. Kissin M.Ya. Structure and dynamics of non-psychotic mental disorders in patients with epilepsy in St. Petersburg: Abstract of the thesis. dis. . Dr. med. Sciences: 14.00.18. St. Petersburg, 2007. - 42 p.
Structure and dynamics of non-psychotic mental disorders in patients with epilepsy in St. Petersburg: Abstract of the thesis. dis. . Dr. med. Sciences: 14.00.18. St. Petersburg, 2007. - 42 p.
38. Kissin M.Ya. Structure and dynamics of mental disorders in patients with epilepsy // Psychiatry. 2006. - T. 7. - S. 361-371.
39. Kissin M.Ya. Epilepsy // Child Psychiatry: Proc. for universities / ed. E.G. Eidemiller. SPb., 2005. - S. 427-472.
40. Krasnov V.N. Psychiatric disorders in general medical practice / V.N. Krasnov // Rus. honey. magazine 2001. - V. 9, No. 25. - S. 1187-1191.
41. Kraepelin E. Introduction to the psychiatric clinic / E. Kraepelin. M.: BINOM, 2007.-493 s.
42. Lebedeva A.V. Features of depression in patients with epilepsy / A.V. Lebedeva // Rus. honey. magazine 2007. - V. 15, No. 10. - P. 892.
43. Maksutova A. Psychopharmacotherapy of epilepsy / A. Maksutova, V. Fresher. - Berlin-Vienna: Blackwell Wissenschafts-Verlag, 1998. 180 p.
180 p.
44. Maksutova A.L. Non-psychotic mental disorders in epilepsy / / A.L. Maksutova, E.V. Zheleznova // Rus. honey. magazine 2001. - V. 9, No. 25. - S. 1214.
45. Milevsky M.M. Classification of diseases in psychiatry and narcology: A guide for doctors / M.M. Milevsky. - M .: Triada X, 2003. - 184 p.
46. Morishita S. Prevalence of induced manic syndrome in patients treated with milnacipran: comparison with paroxetine (extended abstract) / S. Morishita, S. Aritab // Psychiatry and psychopharmacotherapy. 2007. - V. 9, No. 1. - S. 11-12.
47. Mosolov S.N. Clinical efficacy and tolerability of escitalopram in the treatment of moderate and severe depression / S.N. Mosolov, E.G. Kostyukova, A.V. Gorodnichevi et al. // Modern therapy of mental disorders. 2007. - No. 2. - S. 42-47.
48. Mosolov S.N. Clinical use of modern antidepressants / S.N. Mosolov. SPb.: Med. inform. agency, 1995. - 568 p.
49. Muratov V.A. Clinical lectures on nervous and mental diseases / V. A. Muratov. M.: Ed. A. Kartseva, 1900. - 268 p.
A. Muratov. M.: Ed. A. Kartseva, 1900. - 268 p.
50. Neznanov N.G. Epilepsy, quality of life, treatment / N.G. Neznanov, S.A. Gromov, V.A.Mikhailov. St. Petersburg: VMA Publishing House, 2005. - 294 p.
51. Fundamentals of clinical psychology and medical psychodiagnostics / Ovchinnikov B.V., Dyakonov I.F., Kolchev A.I. and others. St. Petersburg: ELBI-SPb, 2005. -320 p.
52. Mental disorders in epilepsy / V.V. Kalinin, E.V. Zheleznova, L.V. Sokolova et al. M., 2006. - 27 p.
53. Rebrova O.Yu. Statistical analysis of medical data. Application of the application package STATISTICA. 3rd ed. / O.Yu. Rebrova. - M.: MediaSphere, 2006. - 312 p.
54. Guide to psychiatry / ed. A.S. Tiganova. -M.: Medicine, 1999. -T. 1.-712 p.
55. Manual of psychiatry / ed. A.S. Tiganova. - M .: Medicine, 1999. -T. 2.-784 p.
56. Smulevich A.B. Depression in somatic and mental diseases / A.B. Smulevich. M.: Med. inform. agency. - 2003. - 432 p.
57. Sobchik L.N. Manual on the use of psychological diagnostics MMPI / L.N. Sobchik. M.: MZ RSFSR 1971. - 63 p.
Sobchik L.N. Manual on the use of psychological diagnostics MMPI / L.N. Sobchik. M.: MZ RSFSR 1971. - 63 p.
58. Tiganov A.S. Affective disorders and syndrome formation / A.S. Tiganov // Zhurn. neuropathology and psychiatry. Korsakova 1999. - T. 99, No. 1.-S.4-7.
59. Tiganov A.S. Endogenous depressions: issues of classification and systematics / A.S. Tiganov // Depressions and comorbid disorders / ed. A.B. Smulevich. M., 1997. - S. 8-12.
60. Frumkin Ya.P. To the diagnosis of epilepsy / Ya.P. Frumkin // Sat. scientific tr. cafe psychiatry of the Kyiv honey. in-ta. Kyiv, 1969. - No. 1.
61. Epilepsy. Personality changes. Treatment / S.A. Gromov, M.Ya. Kissin, O.N. Yakunina and others. St. Petersburg: IIC "Baltika", 2006. - 320 p.
62. Yakhin K.K. Clinical questionnaire for the detection and evaluation of neurotic conditions: guidelines for interns and doctors / K.K. Yakhin., D.M. Mendelevich. Kazan, 1978.-23 p.
63. Abraham G. Topiramate-induced suicidality / G. Abraham // Can. J. Psychiatry. -2003. Vol. 48, No. 2. - P.127-128.
Abraham // Can. J. Psychiatry. -2003. Vol. 48, No. 2. - P.127-128.
64. Aldenkampf A.P. Antiepileptic drug treatment and epileptic seizure effect on cognitive function / A.P. Aldenkampf // The Neuropsychiatry of Epilepsy / M. Trimble, B. Schmitz (eds). Cambrige, 2002. - P.256-267.
65. Altshuler L. Depression and epilepsy / L. Altshuler // Epilepsy and behavior / O. Devinsky, W.H. Theodore (eds). New York, 1991. - P.47-65.
66. Angst J. Epidemiologie der Depression / J. Angst // Resultate aus der Zurich-Studie-Depressionen. Therapiekonzepte in Vergleich. Berlin, Heidelberg, 1993.-S.3-12.
67. Asberg M. "Serotonin depression": a biochemical subgroup within the affective disorder? / Asberg M., Thoren P., Traskman L. et al. // Science. 1976. - Vol. 191, No. 4226. - P.478-480.
68. Bakchine S. Manic-like state after bilateral orbitofrontal and right temporoparietal injury: efficacy of clonidine / Bakchine S., Lacomblez L., Benoit N. et al. // Neurology. 1989. - Vol. 39, No. 6. - P.777-781.
1989. - Vol. 39, No. 6. - P.777-781.
69. Ballenger J.C. The use of anticonvulsants in manic-depressive illness / J.C. Ballenger // J. Clin. Psychiatry. 1988.-Vol. 49, Suppl. - P.21-25.
70. Barczak P. Hypomania following complex partial seizures. A report of three cases / Barczak P., Edmunds E., Betts T. // Br. J. Psychiatry. 1988. - Vol. 152.-P.137-139.
71. Barry J.J. Psychiatric uses for anticonvulsants / J.J. Barry // Merrit-Putnam Lectures. From ME monograph. West Hartford, 1999. - P.89-105.
72. Barry J.J. The recognition and management of mood disorders as a comorbidity of epilepsy / J.J. Barry // Epilepsia. 2003. - Vol. 44, Suppl. 4.-P.30-40.
73. Baxendale S.A. Epilepsy and depression: the effects of comorbidity on hippocampal volume-a pilot study / Baxendale S.A., Thompson P.J., Duncan J.S. //Seizure. 2005. - Vol. 14, No. 6. - P.435-438.
74. Bear D.M. Quantitative analysis of interictal behavior in temporal lobe epilepsy / Bear D.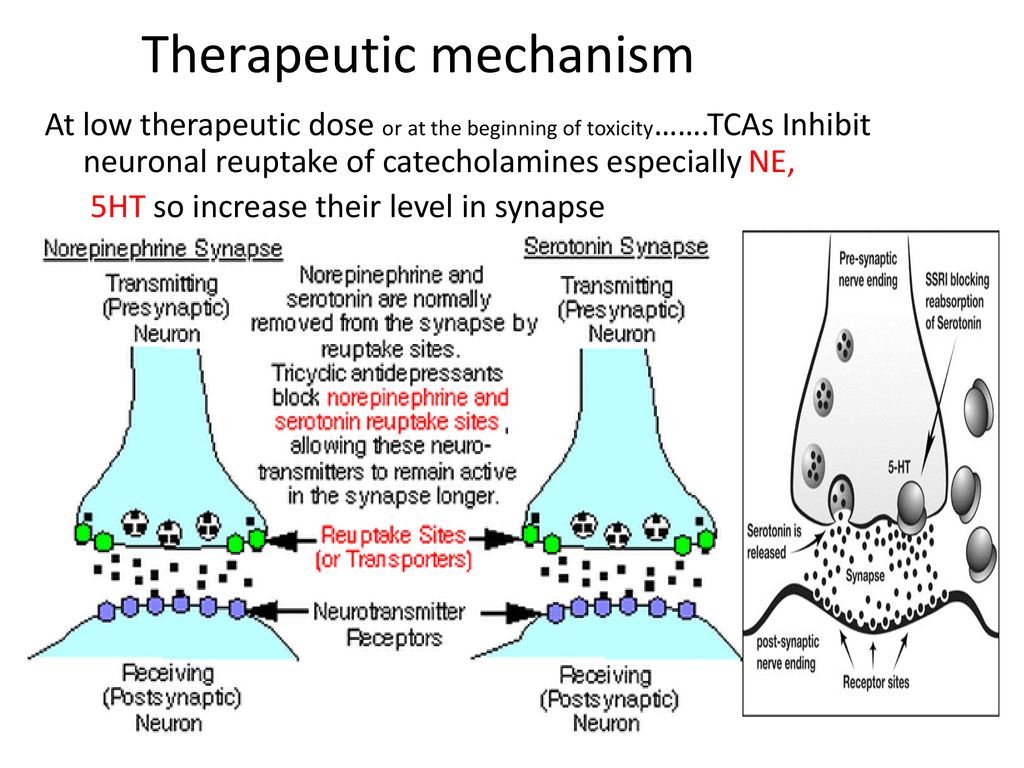 M., Fedio P. // Arch. Neurol. 1977. - Vol. 34, No. 8. - P.454-467.
M., Fedio P. // Arch. Neurol. 1977. - Vol. 34, No. 8. - P.454-467.
75. Ben-Menachem E. Evidence for sustained efficacy of levetiracetam as add-on epilepsy therapy / Ben-Menachem E., Edrich P., Van Vleymen B. et al. // Epilepsy Res. 2003. - Vol. 53, no. 1-2. - P.57-64.
76. Bercovici E. Serotonine depletion attenuates AY-9944-mediated atypical absence seizures / Bercovici E., Cortez M.A., Wang X. et al. // Epilepsy. 2006. - Vol. 47, No. 2. - P.240-246.
77. Berman R. Models of antidepressants action / Berman R., Charney D.C. // J. Clin. Psychiatry. 1999. - Vol. 60, Suppl. 14. - P. 16-20.
78. Bialer M. New antiepileptic drugs currently in clinical trials: is there a strategy in their development? / M. Bialer // Ther. drug monitor. 2002. - Vol. 24, No. 1. - P.85-90.
79. Blanchet P. Mood change preceding epileptic seizures / Blanchet P., Frommer G.P. // J. Nerv. Ment. Dis. 1986. - Vol. 174, No. 8. - P.471-476.
80. Blum D. Prevalence of major affective disorders and manic/hypomanic symptoms in persons with epilepsy: a community survey / Blum D. , Reed M., Metz A. // Neurology. 2002. - Vol. 58, Suppl 3. - P.A175.
, Reed M., Metz A. // Neurology. 2002. - Vol. 58, Suppl 3. - P.A175.
81. Blumer D. Antidepressant and double antidepressant treatment for the affective disorder of epilepsy / D. Blumer // J. Clin. Psychiatry. 1997. - Vol. 58, No. 1. - P.3-11.
82. Blumer D. Affective disorders / Blumer D., Altshuler L.L. // Epilepsy. /Ed. J. Engel et al. Philadelphia etc., 1998. - P. 2083-2099.
83. Blumer D. Dysphoric disorders and paroxysmal affects: recognition and treatment of epilepsy-related psychiatric disorders / Blumer D. // Harv. Rev. Psychiatry. 2000.-Vol. 8, No. 1. - P.8-17.
84. Blumer D. Epilepsy and suicide: a neuropsychiatric analysis / Blumer D. // The neuropsychiatry of epilepsy / Trimble M., Schmitz B. (eds). Cambridge, 2002.-P.107-116.
85. Borowicz K.K. Fluoxetine enhances the anticonvulsant effects of conventional antiepileptic drugs in maximal electroshock seizures in mice / Borowicz K.K., Stepien K „ Czuczwar S J. // Pharmacol. Rep. 2006. - Vol. 58, No. 1. - P. 83-90.
58, No. 1. - P. 83-90.
86. Brent D. Phenobarbital treatment and major depressive disorder in children with epilepsy: a naturalistic follow-up / Brent D., Crumrine P., Varma R. et al. // Pediatrics. 1987. - Vol. 80, No. 6. - P.909-917.
87. Brodie M.J. Pregabalin as adjunctive therapy for partial seizures / M.J. Brodie // Epilepsia. 2004. - Vol. 45, Suppl 6. - P. 19-27.
88. Bromfield E.B. Cerebral metabolism and depression in patients with complex partial seizures / Bromfield E.B., Altshuler L., Leideran D.B. et al. // Arch. Neurol. -1992. Vol. 49, No. 6. - P.617-623.
89. Brundtland G.H. Editorials: Mental health in the 21st century / Brundtland G.H. // Bull. World Health Organ. 2000. - Vol. 78, No. 4. - P.411.
90. Byrne A. Hypomania following increased epileptic activity / Byrne A. // Br. J. Psychiatry. 1988.-Vol. 153.-p. 573-574.
91. Calabrese J.R. A pilot study of topiramate as monotherapy in the treatment of acute mania / Calabrese J.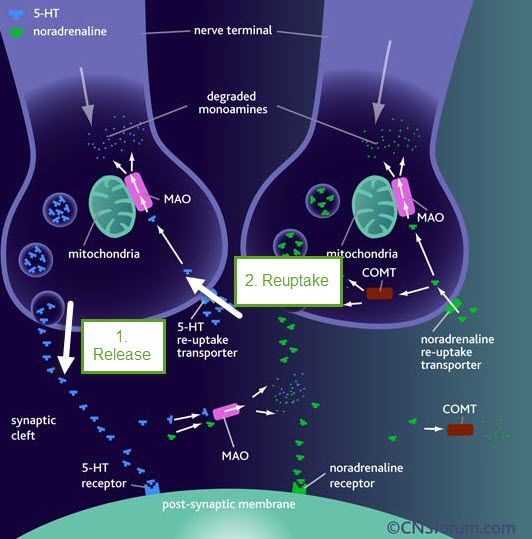 R., Keck P.E. Jr., McElroy S.L. et al. // J. Clin. Psychopharmacol. 2001. - Vol. 21, No. 3. - P.340-342.
R., Keck P.E. Jr., McElroy S.L. et al. // J. Clin. Psychopharmacol. 2001. - Vol. 21, No. 3. - P.340-342.
92. Charles C.L. Zonisamide-induced mania / Charles C.L., Stoesz L., Tollefson G. // Psychosomatics. 1990. - Vol. 31, No. 2. - P. 214-217.
93. Chugani H.T. Imaging of serotonin mechanisms in epilepsy / Chugani H.T., Chugani D.C. // Epilepsy Cur. 2005. - Vol. 5, No. 6. - P.201-206.
94. Cramer J.A. The influence of comorbid depression on seizure severity / Cramer J.A., Blum D., Reed M. // Epilepsia. 2003. - Vol.44, No. 12. - P.1578-1584.
95. Cramer J.A. Improved mood states with lamotrigine in patients with epilepsy / Cramer J.A., Hammer A.E., Kustra R.P. // Epilepsy Behav. 2004. - Vol.5, No. 5. -P.702-707.
96. Davis L.L. Valproate as an antidepressant in major depressive disorder / Davis L.L., Kabel D., Patel D. et al. // Psychopharmacol. Bull. 1996. - Vol. 32, No. 4. -P.647-652.
97. Devinsky O. Cognitive and behavioral effects of antiepileptic drugs / O. Devinsky // Epilepsia. 1995. - Vol. 36, Suppl. 2. - P.S46-S65.
Devinsky // Epilepsia. 1995. - Vol. 36, Suppl. 2. - P.S46-S65.
98. Devinsky O. Neurology of cognitive and behavioral disorders / Devinsky O., D'Esposito M. New York, 2004. - P.451.
99. Dietrich D.E., Kropp S., Emrich H.M. Oxcarbazepine in affective and schizoaffective disorders / Dietrich D.E., Kropp S., Emrich H.M. // Pharmacopsychiatry. 2001. - Vol. 34, No. 6. - P.242-250.
100. Dodrill C.B. Psychotropic effects of carbamazepine in epilepsy: a double-blind comparison with phenytoin / Dodrill C.B., Troupin A.S. // Neurology. 1977. - Vol. 27, No. 11. - P. 1023-1028.
101. Dudra-Jastrzebska M. Mood disorders in patients with epilepsy / Dudra-Jastrzebska M., Andres-Mach M.M., Luszczki J J. et al. // Pharmacol. Rep. 2007.-Vol. 59, No. 4. - P.369-378.
102. Dysthimic Disorder / Burton S.W., Akiskal H.S. (eds). London; Gaskell, 1990.-130 p.
103. Ettinger A. Depression and comorbidity in community-based patients with epilepsy or asthma / Ettinger A. , Reed M., Cramer J. // Neurology. 2004. - Vol. 63, No. 6. - P.1008-1014.
, Reed M., Cramer J. // Neurology. 2004. - Vol. 63, No. 6. - P.1008-1014.
104. Ettinger A.B. Psychotropic effects of antiepileptic drugs / Ettinger A.B. // Neurology. 2006. - Vol. 67, No. 11. - P. 1916-1925.
105. Ettinger A.B. Effect of lamotrigine on depressive symptoms in adult patients with epilepsy / Ettinger A.B., Kustra R.P., Hammer A.E. // Epilepsy Behav. 2007. Vol. 10, No. 1. - P.148-154.
106. Fakhoury T.A. Lamotrigine in patients with epilepsy and comorbid depressive symptoms / Fakhoury T.A., Barry J.J., Miller M. et al. // Epilepsy Behav. 2007.-Vol. 10, No. 1. - P.155-162.
107. Favale E. Anticonvulsant effect of fluoxetine in humans / Favale E., Rubino V., MainardiP. et al. //Neurology. 1995. - Vol. 45, No. 10. - P.1926-1927.
108. Fisher R.S. Update on the mechanism of action of new antiepileptic drugs / R.S. Fisher // Merritt-Putnam Lectures: Update on Epilepsy Management / American Epilepsy Society and Parke-Davis. S.I., 1998.-Vol. - P. 19-36.
- P. 19-36.
109. Forsgren L. An incident case referent study of epileptic seizures in adults / Forsgren L., Nystrom L.//Epilepsy Res. 1990.-Vol. 6, No. 1.-P.66-81.
110. Gilliam F. Optimizing health outcomes in active epilepsy / F. Gilliam // Neurology. 2002. - Vol. 58, Suppl 5. - P.S9-S20.
111. Gilliam F.G. Depression and epilepsy: Ignoring clinical expression of neuronal network dysfunction? / Gilliam F.G., Santos J., Vahle V. et al. // Epilepsy. 2004.-Vol. 45, Suppl. 2.-P. 28-33.
112. Gilliam F.G. Diagnosis and treatment of mood disorders in persons with epilepsy / Gilliam F.G. // Curr. Opin. Neurol. 2005. - Vol. 18, No. 2. - P.129-133.
113. Gil-Nagel A. Effect of lamotrigine on sexual function in patients with epilepsy / Gil-Nagel A., Lopez-Munoz F., Serratosa J.M. et al. //Seizure. 2006. - Vol. 15, No. 3. - P.142-149.
114. Gorman J.M. Efficacy comparison of escitalopram and citalopram in the treatment of major depressive disorder: pooled analysis of placebo-controlled trials Gorman J. M., Korotzer A., Su G. // CNS Spectr. 2002. - Vol.7, No. 4. Suppl. 1.-P.40-44.
M., Korotzer A., Su G. // CNS Spectr. 2002. - Vol.7, No. 4. Suppl. 1.-P.40-44.
115. Grunze H. Clinical relevance and treatment possibilities of bipolar rapid cycling /Grunze H., Amann B., Dittmann S. et al. // Neuropsychobiology. 2002. - Vol. 45, Suppl. 1.-P.20-26.
116. Grunze H. How might anticonvulsant drugs work in bipolar affective disorders / Grunze H., Amann B., Walden J. // Seizures, affective disorders and anticonvulsant drugs / M. Trimble et al. (eds). Guildford, 2002. - P. 117-130.
117. Gruhle H.W. Psychiatry for Arzte / H. W. Gruhle. 2 verm, und verb. Aufl. -Berlin: Springer 1922. - vi, 304 s.
118. Guelfi G.D. L'evolution clinique standartisee en psychiatrie, psychopathologie generale. Depression, anxiete et anxiodepression.- S.I.: Editions Medicales Pierre Fabre, 1993.
119. Hamilton M. The assessment of anxiety states by rating / M. Hamilton // Brit. J. Med. Psychol. 1959. - Vol. 32, No. 1. - P. 50-55.
120. Hamilton M. Development of a rating scale for primary depressive illness / M. Hamilton // Br. J. Soc. Clin. Psychol. 1967. - Vol. 6, No. 4. - P. 278-296.
Hamilton // Br. J. Soc. Clin. Psychol. 1967. - Vol. 6, No. 4. - P. 278-296.
121. Hesdorffer D.C. Major depression is a risk factor for seizures in older adults / Hesdorffer D.C., Hauser W.A., Annegers J.F. et al. // Ann. Neurology. 2000. - Vol. 47, No. 2. - P.246-249.
122. Hirsch E. Epilepsy, antiepileptic drug (AEDs) and cognition / Hirsch E., Schmitz B., Carreno M. // Acta Neurol. Scand. 2003. - Vol. 108, Suppl. 180.-P.23-32.
123. Hollander E. A preliminary double-blind, placebo-controlled trial of divalproex sodium in borderline personality / Hollander E., Allen A., Lopez R.P. et al. // J. Clin. Psychiatry. 2001. - Vol. 62, No. 3. - P.l99-203.
124. Hovorka J. Treatment of interictal depression with citalopram in patients with epilepsy / Hovorka J., Herman E., Nemcova I. // Epilepsy Behav. 2000. - Vol. 1, No. 6. - P.444-447.
125. Indaco A. Interictal depression in epilepsy / Indaco A., Carrieri P.B., Nappi C. et al. // Epilepsy Res. 1992. - Vol.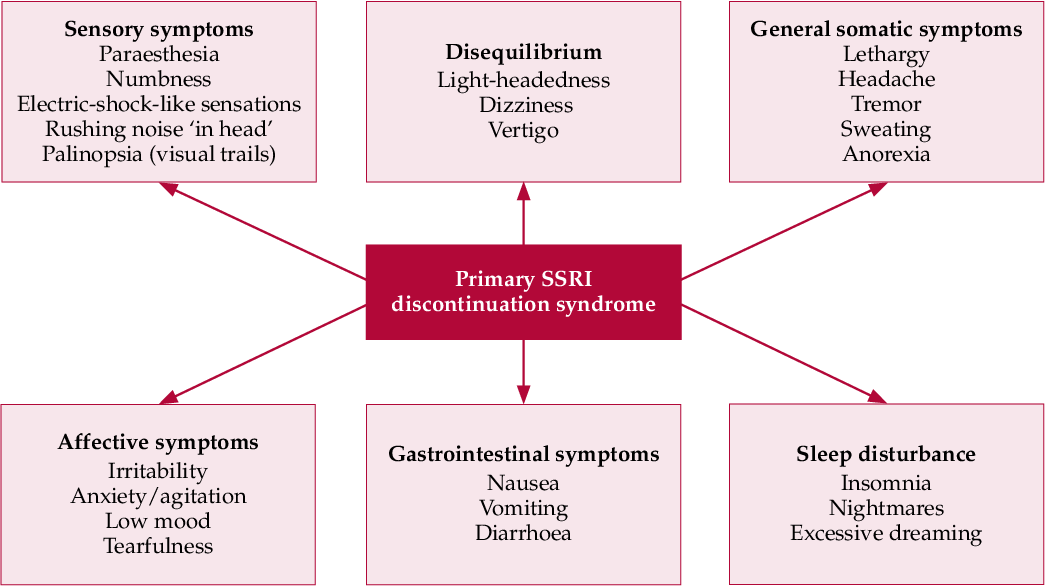 12, No. 1. - P. 45-50.
12, No. 1. - P. 45-50.
126. Jackson J. II. Selected writings: in 2 vol. /Ed. J. Tayl.-London: Hodder & Stoughton, 1931. Vol. 1. On epilepsy and epileptiform convulsions.
127. Jacoby A. The clinical course of epilepsy and its psychosocial correlates: findings from a U.K. Community study / Jacoby A., Baker G.A., Steen N. et al. // Epilepsy. 1996. - Vol. 37, No. 2. - P. 148-161.
128. Jobe P.C. A noradrenergic and serotonergic hypothesis of the linkage between epilepsy and affective disorders / Jobe P.C., Dailey J.W., Wernicke J.F. // Crit. Rev. neurobiol. 1999. - Vol. 13, No. 4. - P.317-356.
129. Jobe P.C. Genetically epilepsy-prone rats (GEPRs) in drug research / Jobe P.C., Dailey J.W. // CNS Drug Rev. 2000. - Vol. 6, No. 3. - P.241-260.
130. Jobe P.C. Common pathogenic mechanisms between depression and epilepsy: an experimental perspective / Jobe P.C. // Epilepsy Behav. 2003. - Vol. 4, Suppl 3. - P.S14-S24.
131. Jobe P.C. Affective disorder and epilepsy comorbidity: implications for development of treatments, preventions and diagnostic approaches / Jobe P. C. // clinic. EEG Neurosci. 2004. - Vol. 35, No. 1. - P.53-68.
C. // clinic. EEG Neurosci. 2004. - Vol. 35, No. 1. - P.53-68.
132. Jobe P.C. Current and future therapeutic opportunities in the comorbidity between the epilepsies and affective disorders / Jobe P.C. // clinic. EEG Neurosci. -2004.-Vol. 35, No. 1.-P.1-3.
133. Jobe P.C. Shared mechanisms of antidepressant and antiepileptic treatments: drugs and devices / Jobe P.C. // clinic. EEG Neurosci. 2004. - Vol. 35, No. 1. - P.25-37.
134. Jobe P.C., Browning R.A. The serotonergic and noradrenergic effecrs of antidepressant drugs are anticonvulsant, not preconvulsant / Jobe P.C. // Epilepsy Behav. 2005. - Vol. 7, No. 4. - P.602-619.
135. Kalinin V. Gender differences in risk factors of suicidal behavior in epilepsy Kalinin V., Polyansky D. // Epilepsy Behav. 2005. - Vol. 6, No. 3. - P.424-429.
136. Kalinin V.V. Suicidality and antiepileptic drugs. Is there a Link? / Kalinin V.V. // DrugSaf. 2007. - Vol. 30, No. 2. - P. 123-142.
137. Kanner A.M. Depressive disorders in epilepsy / Kanner A.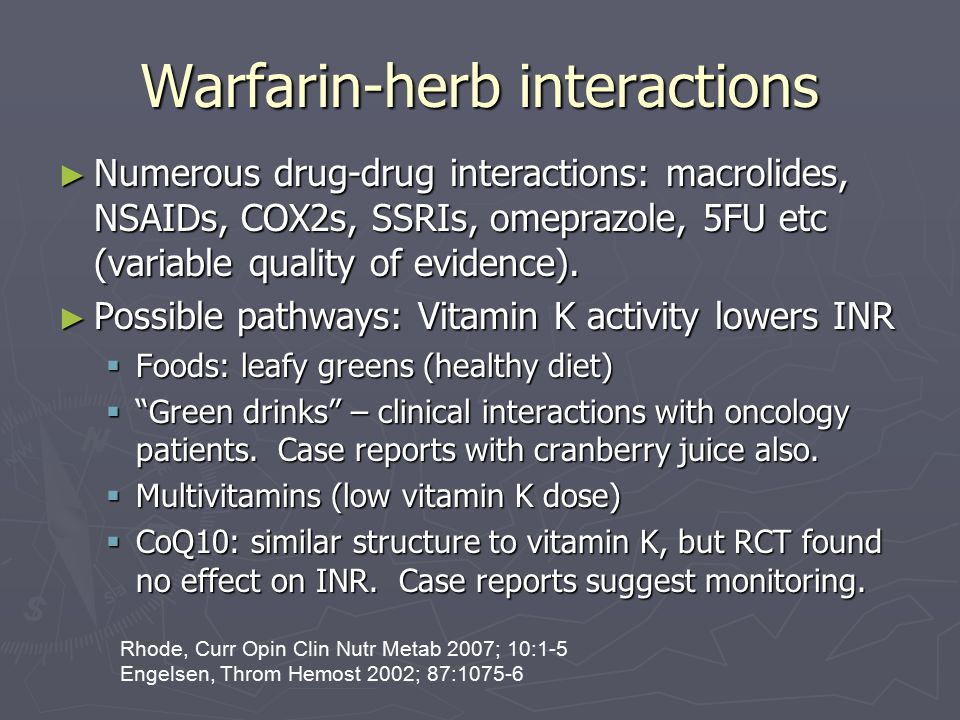 M., Nieto J.C. // Neurology. 1999. - Vol. 53, No. 5, Suppl 2. - P.S26-S32.
M., Nieto J.C. // Neurology. 1999. - Vol. 53, No. 5, Suppl 2. - P.S26-S32.
138. Kanner A.M. The use of sertralin in patients with epilepsy: is it safe? / Kanner A.M., Kozak A.M., Frey M.// Epilepsy Behav. 2000. - Vol. 1, No. 2. - P.100-105.
139. Kanner A.M. Is the psychopathology of epilepsy different from that of nonepileptic patients? / Kanner A.M., Barry J.J. // Epilepsy Behav. 2001. - Vol. 2, No. 3. - P.170-186.
140. Kanner A.M. Depression and epilepsy: how closely related are they? / Kanner A.M., Balabanov A. // Neurology. 2002. - Vol. 58, No. 8, Suppl 5. - P.S27-S39.
141. Kanner A.M. A past psychiatric history may be a risk factor for topiramat-related psychiatric and cognitive adverse events / Kanner A.M., Wuu J., Faught E. et al. // Epilepsy Behav. 2003. - Vol. 4, No. 5. - P.548-552.
142. Kanner A. Is major depression a neurological disorder with psychiatric symptoms? / Kanner A. // Epilepsy Behav. 2004. - Vol. 5, No. 5. - P.636-644.
143. Kanner A.M. Depression in epilepsy, a neurobiological perspective / Kanner A.M. // Epilepsy. 2005. - Vol. 5, No. 1. - P.21-27.
Kanner A.M. Depression in epilepsy, a neurobiological perspective / Kanner A.M. // Epilepsy. 2005. - Vol. 5, No. 1. - P.21-27.
144. Kanner A.M. Depression and epilepsy: A New perspective on two closely related disorders / Kanner A.M. // Epilepsy Curr. 2006. - Vol. 6, No. 5. - P.141-146.
145. Kanner A.M. Epilepsy, suicidal behavior, and depression: do they share common pathogenic mechanisms? / Kanner A.M. // Lancet Neurol. 2006. - Vol. 5, No. 2.—P.107-108.
146. Kanner A.M. Psychopathology and epilepsy: is it the chicken or the egg? / Kanner A.M. // Epilepsy Curr. 2006. - Vol. 6, No. 5. - P. 147-149.
147. Katon W. Depression and chronic mental illness / Katon W., Sullivan M.D. // J. Clin. Psychiatry. 1990. - Vol. 51, Suppl. -P.3-11.
148. Kessler R.C. Lifetime and 12-month prevalence of DSM-HI-R psychiatric disorders in the United States / Kessler R.C., McConagle K.A., Zhao S. et al. // Arch. Gen. Psychiatry. 1994. - Vol. 51, No. 1. - P.8-19.
149. Ketter T.A. Felbamate monotherapy has stimulant-like effects in patients with epilepsy / Ketter T.A., Malow B.A., Flamini R. et al. // Epilepsy Res. 1996. - Vol. 23, No. 2. - P.129-137.
Ketter T.A. Felbamate monotherapy has stimulant-like effects in patients with epilepsy / Ketter T.A., Malow B.A., Flamini R. et al. // Epilepsy Res. 1996. - Vol. 23, No. 2. - P.129-137.
150. Ketter T.A. Positive and negative psychiatric effects of antiepileptic drugs in patients with seizure disorders / Ketter T.A., Post R.M., Theodore W.H. // Neurology. 1999. - Vol. 53, Suppl. 2.-P. S53-S67.
151. Kimiskidis V.K. Depression and anxiety in epilepsy: the association with demographic and seizure-related variables / Kimiskidis V.K., Triantafyllou N.I., Kararizou E. et al. // Ann. Gen. Psychiatry. 2007. - Vol. 6.-P.28.
152. Kishimoto A. Long-term prophylactic effects of carbamazepine in affective disorder / Kishimoto A., Oqura C., Hazama H. et al. // Br. J. Psychiatry. 1983. Vol. 143.-P.327-331.
153. Koh S. Depressive behavior and selective down-regulation of serotonin receptor expression after early-life seizures: reversal by environmental enrichment / Koh S. , Magid R., Chung FI. et al. // Epilepsy Behav. 2007. - Vol. 10, No. 1. - P.26-31.
, Magid R., Chung FI. et al. // Epilepsy Behav. 2007. - Vol. 10, No. 1. - P.26-31.
154. Kraepelin E. Uber Erinnerungsfalschungen / Kraepelin E // Arch. Psychiatre. -1896.-Bd. 17. S.830-843.
155. Krishnamoorthy E.S. Forced normalization: clinical and therapeutic relevance / Krishnamoorthy E.S., Trimble M.R. // Epilepsy. 1999. - Vol. 40, Suppl. 10.-P.S57-S64.
156. Lambert M.V. Depression in' epilepsy: etiology, phenomenology and treatment / Lambert M.V., Robertson M.M. // Epilepsy. 1999. - Vol. 40, Suppl. 10.-P.S21-S47.
157. Lambert M.V. Neuropsychiatric aspects of epilepsy / Lambert M.V., Thompson P.J., Trimble M.// Principles and practice of behavioral neurology and neuropsychology / M.Rizzo, P.J. Eslinger (eds). Philadelphia (PA), 2004. - P.763-779.
158. Legrand du Saulle H. La folie du doute (avec delire de toucher). Paris, 1875. -p. 97.
159. Leppik I.E. Epilepsy in the elderly / I.E. Leppik // Epilepsia. 2006. - Vol. 47, Suppl l.-P. 65-70.
65-70.
160. Lopez-Gomez M. Primidone is associated with interictal depression in patients with epilepsy / Lopez-Gomez M., Ramirez-Bermudez J., Campillo C. et al. // Epilepsy Behav. 2005. - Vol. 6, No. 3 - P.413-416.
161. Loring D.W. Cognitive and behavioral effects of epilepsy treatment / Loring D.W., Meador K.J. // Epilepsy. 2001. - Vol. 42, Suppl. 8.-P.24-32.
162. Loscher W. Valproic acid. Mechanisms of action / Loscher W. // Antiepileptic drugs / R.H. Levy et al. (eds). 5th ed. - Philadelphia (PA), 2002. - P.767-779.
163. Marcotte D. Use of topiramate, a new anti-epileptic as a mood stabilizer / Marcotte D. // J. Affect. Discord. 1998. - Vol. 50, no. 2-3. - P.245-251.
164. Martinez-Perez B. Depression and epilepsy / Martinez-Perez B., Gonzalez-Goizueta E., Mauri-Llerda J.A. // Rev. Neurol. 2002. - Vol. 35, No. 6. - 580-586.
165. Mayer-Gross W. Clinical psychiatry. 2nd ed. / Mayer-Gross W., Slater E., Roth M. - London: Bailliere, Tindall & Cassel, 1960.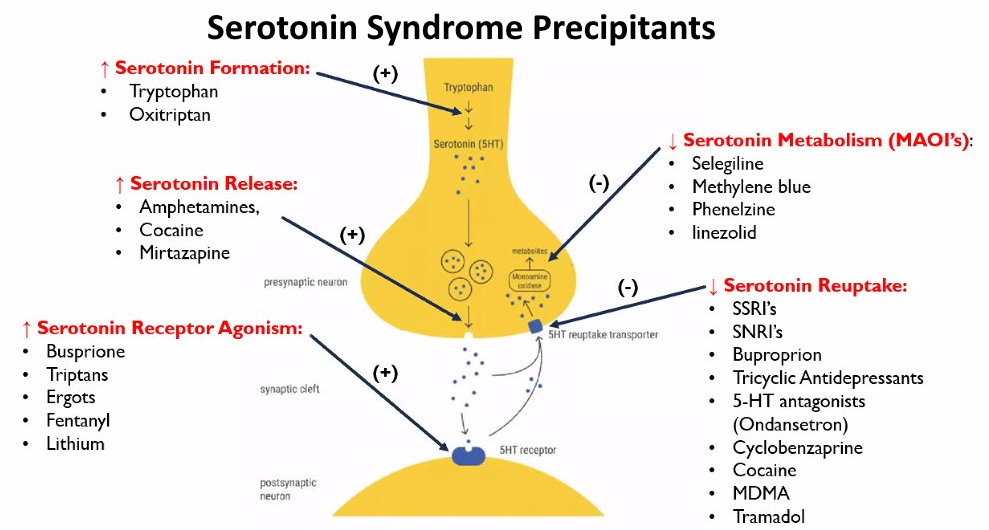 - 704 p.
- 704 p.
166. McKinley J. The Minnesota multiphasic personality inventory: the K scale / McKinley J., Hathaway S.R., Meehl P.E. // J. Consult. Psychol. 1948. - Vol. 12, No. 1. - P.20-31.
167. Mclean M.J. Oxcarbazepine. Mechanisms of action / Mclean MJ. // Antiepileptic drugs / R.H. Levy et al. (eds). 5th ed. - Philadelphia (PA), 2002. -P.452-458.
168. Mendez M.F. Disorders of mood and affect in epilepsy / Mendez M.F. // Psychological Disturbances in Epilepsy / J.C. Sakkellares, S. Berent (eds). Boston, Oxford, 1996.-P.l 25-141.
169. Mendez M.F. depression in epilepsy. Significance and phenomenology / Mendez M.F., Cummings J.L., Benson D.F. // Arch. Neurol. 1986. - Vol. 43, No. 8. -P.766-770.
170. Mendlevvicz J. Antidepressant selection: proceedings from a TCA/SSRI Concensus Conference / Mendlewicz J., Lecrubier Y. //Acta Psychiatr. Scand. Suppl.2000.-Vol. 403.-P.5-8.
171. Mental Illness in General Health Care: An International Study / T. B. Ustun, N. Sartorius (eds). Chichester, New York: Willey, 1995. xii, 398 p. .
B. Ustun, N. Sartorius (eds). Chichester, New York: Willey, 1995. xii, 398 p. .
172. Mischoulon D. Management of major depression in the primary care setting / Mischoulon D., McColl-Vuolo R., Howarth S. et al. // Psychother. Psychosom.2001. Vol. 70, No. 2. - P. 103-107.
173. Modrego P.J. Study of psychopathology in patients with chronic non-lesional epilepsy: a Minnesota multiphasic personality inventory profile controlled study /
174. Modrego PJ., Pina M.A., Galindo M. et al. // EUR. Neurol. 2002. - Vol. 48, No. 2. -P.80-86.
175. Montgomery S.A. A new depression scale designed to be sensitive to change / Montgomery S.A., Asberg M. // Br. J. Psychiatry. 1979. - Vol. 134.-P.382-389.
176. Mula M. Pharmacokinetic interactions between antiepileptic and antidepressant drugs / Mula M., Trimble M.R. // World J. Biol. Psychiatry. 2003. - Vol. 4, No. 1.-P.21-24.
177. Murray Ch. J.L., Lopes A.D. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020.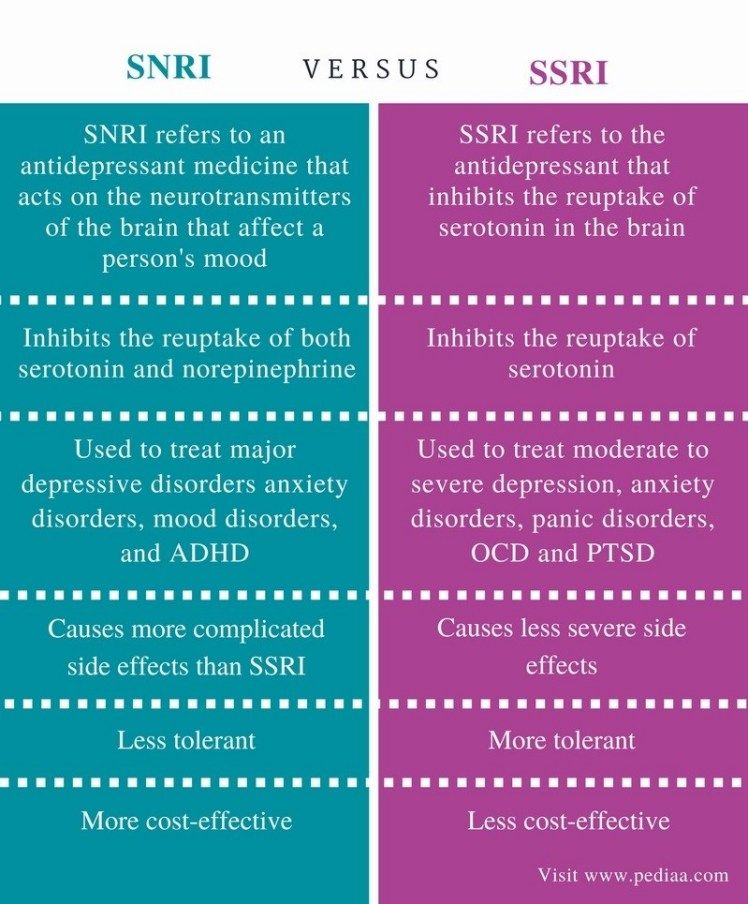 Cambridge, MA: Harvard University Press, 1996. - 990 P
Cambridge, MA: Harvard University Press, 1996. - 990 P
178. Musselman D.L. Biology of mood disorders / Musselman D.L., DeBattista C., Nathan K.L. et al. // Textbook of psychopharmacology / A.F. Schatzberg, C. B. Nemeroff (eds). 2nd ed. Washington, 1998. - P.549-588.
179. Okuma T. A history of the investigation on the mood-stabilizing effect of carbamazepine in Japan / Okuma T. // Seishin Shinkeiqaku Zasshi. 2002. - Vol. 104, No. 8. - P.647-655.
180. Okuma T. Anti-manic and prophylactic effects of carbamazepine (Tegretol) on manic depressive psychosis. A preliminary report / Okuma T., Kishimoto A., Inoue K. et al. // Folia Psychiatr. Neurol. Jpn. 1973. - Vol. 27, No. 4. - P.283-297.
181. Ormel J. Depression, anxiety, and social disability show synchrony of change in primary care patients / Ormel J., Von Korff M., Van den Brink W. et al. // Am. J. Public Health. 1993. - Vol. 83, No. 3. - P.385-390.
182. Penfield W. Speech and brain mechanisms / Penfield W.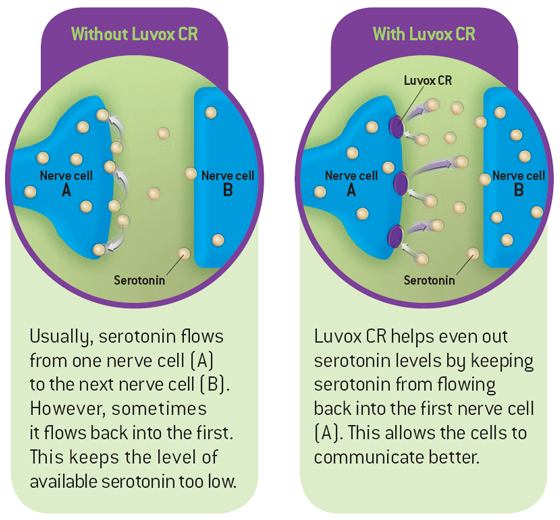 , Roberts L. -Princeton: Univ. Press, 1959.-286 p.
, Roberts L. -Princeton: Univ. Press, 1959.-286 p.
183. Post R.M. Kindling and carbamazepine in affective illness / Post R.M., Uhde T.W., Putnam F.W. et al. // J. Nerv. Ment. Dis. 1982. - Vol. 170, No. 12. - P.717-731.
184. Post R.M. Antidepressant effects of carbamazepine / Post R.M., Uhde T.W., Roy-Byrne P.P. et al. // Am. J. Psychiatry. 1986. - Vol. 143, No. 1. - P.29-34.
185. Prasher V.P. Seizures associated with fluoxetine therapy / Prasher V.P. //Seizure. 1993. - Vol. 2, No. 4. - P.315-317.
186. Puzynski S. Leki przeciwpadaczkowe (karbamazepina, walproiniany i lamotrygina) w terapii zaburzen afektywnych dwubiegunowych / Puzynski S. // Psychiatr. Paul 2002. - T. 36, No. 6, Apl. - L.53-61.
187. Quiske A. Depression in patients with temporal lobe epilepsy is related to mesial temporal sclerosis / Quiske A., Helmstaedter C., Lux S. et al. // Epilepsy Res. -2000. Vol. 39, No. 2. - P.121-125.
188. Reference physician's desk. 53rd ed.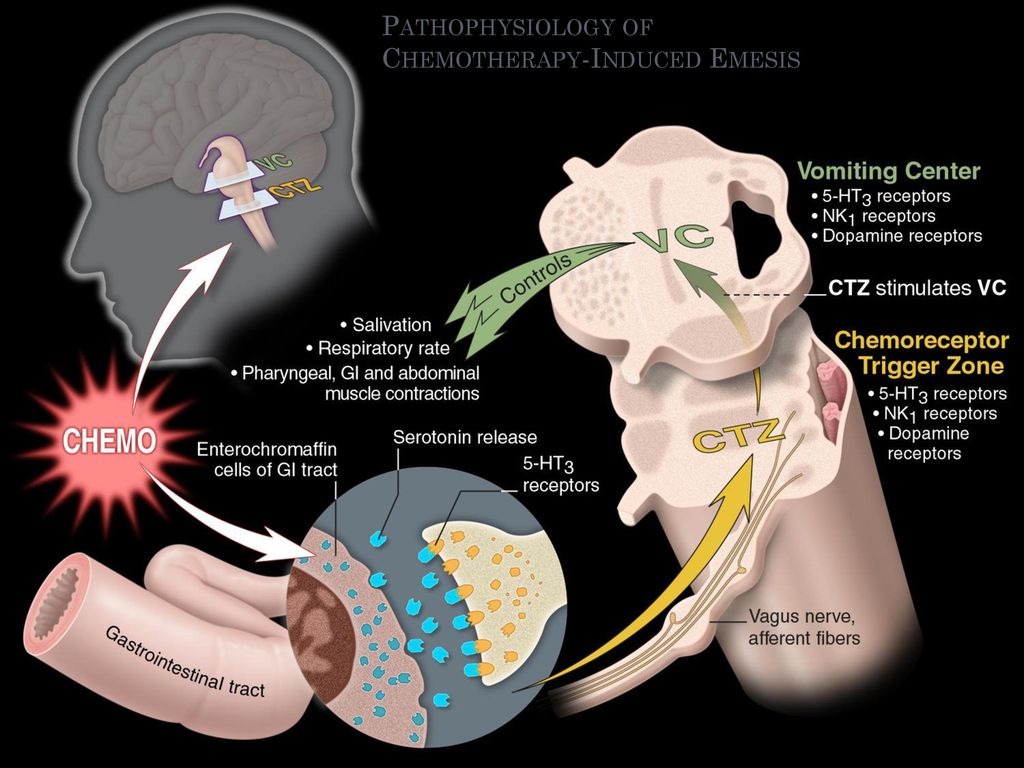 - Montvale: Medical Economics Co, 1999.
- Montvale: Medical Economics Co, 1999.
189. Reijs R. Mood effects of antiepileptic drugs / Reijs R., Aldenkampf A.P., De Krom M. // Epilepsy Behav. 2004. - Vol. 5, Suppl. 1.-P.66-76.
190. Reynolds E.H. Open, double-blind and long-term study of vigabatrin in chronic epilepsy / Reynolds E.H., Ring H.A., Farr I.N. et al. // Epilepsy. 1991. - Vol. 32, No. 4 - P.530-538.
191. Ring H.A. Depression in epilepsy / Ring H.A., Trimble M.R. // Depression in neurological disease / S.E. Starkstein, R.G. Robertson (eds). Baltimore 1993.-P.63-83.
192. Robertson M.M. Phenomenology of depression in epilepsy / Robertson M.M., Trimble M.R., Townsend H.R.// Epilepsia. 1987. - Vol. 28, No. 4. - P.364-372.
193. Robertson M.M. Affect and mood in epilepsy: an overview with a focus on depression / Robertson M.M. // Acta Neurol. Scand. Suppl. 1992. - Vol. 140.-P.127-132.
194. Schmitz B. Depression and Mania in Patients with Epilepsy / Schmitz B. // Epilepsia. 2005. - Vol. 46, Suppl. 4.-P.S45-S49.
2005. - Vol. 46, Suppl. 4.-P.S45-S49.
195. Seethalakshmi R. Depression in epilepsy: phenomenology, diagnosis and management / Seethalakshmi R., Krishnamoorthy E.S. // Epileptic Discord. 2007.-Vol. 9, No. l.-P. 1-10.
196. Shorvon S.D. Safety of topiramate: adverse events and relationship to dosing / Shorvon S.D. // Epilepsy. 1996 - Vol. 37, Suppl. 2. - P.S18-S22.
197. Skolnick P. Adaptation of N-methyl-D-aspartate (NMDA) receptors following antidepressant treatment: implications for the pharmacotherapy of depression / Skolnick P., Layer R.T., Popik P. et al. // Pharmacopsychiatry. 1996. - Vol. 29, No. 1.- P.23-26.
198. Smith D.B. Cognitive effects of antiepileptic drugs / Smith D.B. // Advances in neurology / D.M. Treiman, M. R. Trimble (eds). New York, 1991. - P.197-212.
199. Specchio L.M., Iudice A., Specchio N. et al. Citalopram as treatment of depression in patients with epilepsy // Clin. Neuropharmacol. 2004. - Vol. 27, No. 3. -P.133-136.
200. Stein G. Drug treatment of the personality disorders / Stein G. // Br. J Psychiatry. 1992. - Vol. 161. - P. 167-84.
201. Swann A.C. Valproic acid: clinical efficacy and use in psychiatric disorders / Swann A.C. // Antiepileptic drugs / Levy R.FI.et al. (eds). 5th ed. - Philadelphia, 2002.-P. 828-836.
202. Taylor D.C. Temporal lobe epilepsy: origin and significance of simple and complex auras / Taylor D.C., Lochery M. // J. Neurol. neurosurgery. Psychiatry. 1987 Vol. 50, No. 6. P.673-681.
203. Thome-Souza M.S. Sertraline and fluoxetine: safe treatments for children and adolescents with epilepsy and depression / Thome-Souza M.S., Kuczynski E., Valente K.D. // Epilepsy Behav. 2007. - Vol. 10, No. 3. - P.417-425.
204. Trimble M.R. Folic acid and mental symptoms in children with epilepsy / Trimble M.R., Corbett J.A., Donaldson D. // J. Neurosurg. Psychiatry. 1980. - Vol. 43, No. 11.-P. 1030-1034.
205. Trimble M.R., Perez M.R. Quantification of psychopathology in adult patients with epilepsy / Trimble M.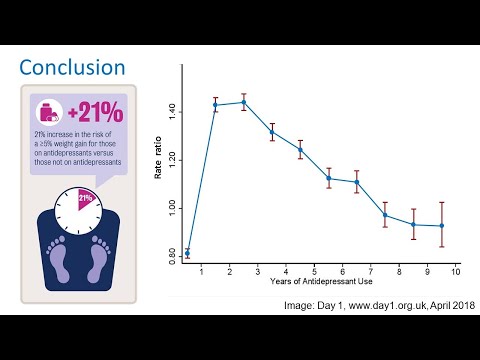 R., Perez M.R. // Epilepsy and behavior / Kulig B.M. et al. (eds). Lisse, 1980. - P. l 18-126.
R., Perez M.R. // Epilepsy and behavior / Kulig B.M. et al. (eds). Lisse, 1980. - P. l 18-126.
206. Trimble M.R. Anticonvulsant-induced psychiatric disorders / Trimble M.R. // DrugSaf. 1996. - Vol. 15, No. 3. - P.l59-166.f/
207. Trimble M.R. Neuropsyehiatric aspects of epilepsy / Trimble M.R., Ring H. A., Schmitz B. // Neuropsychiatry / Fogel B.S. et al. (eds). Baltimore, 1996. - Ch.33. -P.771-803.
208. Trimble M.R. New antiepileptic drugs and psychopathology / Trimble M.R. // Neuropsychobiology 1998. Vol. 38, No. 3. - P.149-151.
209. Wade A. Escitalopram 10 mg/day is effective and well tolerated in a placebo-controlled study in depression in primary care / Wade A., Michael Lemming O., Bang Hedegaard K. // Int. Clin. Psychopharmacol. 2002. - Vol. 17, No. 3. - P.95-102.
210. Wiegartz P. Co-morbid psychiatric disorder in chronic epilepsy: recognition and etiology of depression / Wiegartz P., Seidenberg M., Woodard A. et al. // Neurology. -1999.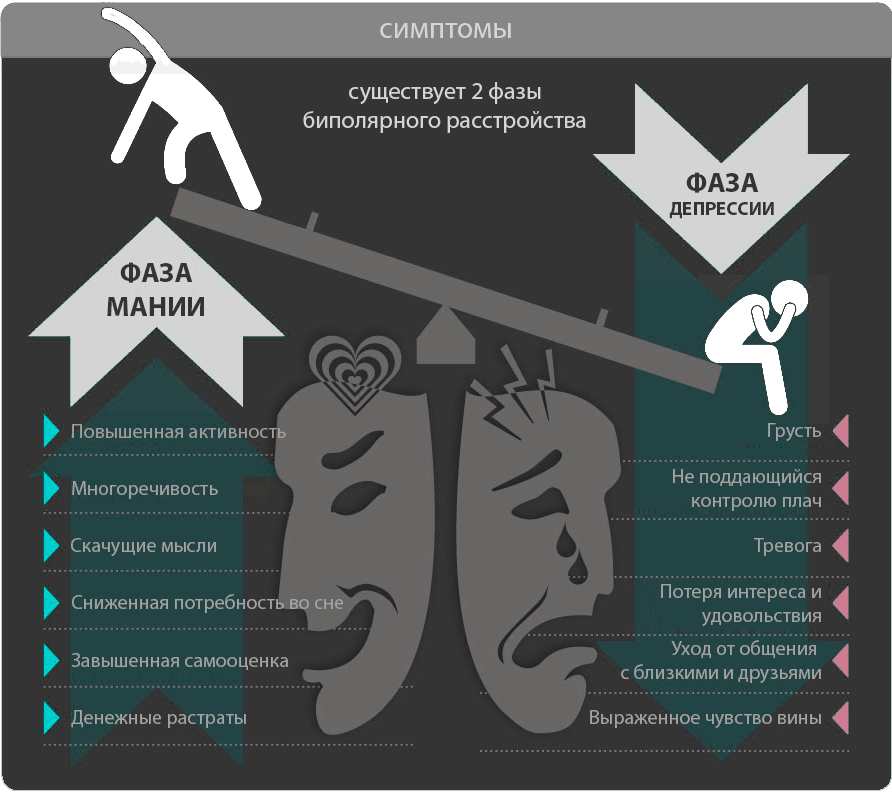 Vol. 53, No. 5, Suppl. 2. - P.S3-S8.
Vol. 53, No. 5, Suppl. 2. - P.S3-S8.
211. Williams D. The structure of emotion reflected in epileptic experiences / Williams D. // Brain. 1956. - Vol. 79, No. 1. - P.29-67.
212. Williams D. Modern views on the classification of epilepsy / Williams D. // Brit. Med. J. 1958. - Vol. 1, No. 5072.-P.661-663.
213. Wolf P. Manic episodes in epilepsy / Wolf P. // Advances in epileptology: thirteenth epilepsy international symposium / H. Akimoto et al. (eds). - New York, 1982. P.237-240.
214. Wolf P. Acute behavioral symptomatology at disappearance of epileptiform EEG abnormality: paradoxical or “forced normalization” / Wolf P. // Advances in neurology / D.B. Smith, et al. (eds). New York, 1991. - P. 127-142.
215. World mental health. Problems and priorities in low-income countries / R. Desjarlais et al. (eds). NY: Oxford University Press, 1995.-400p.
216. Young R.C. A rating scale for mania: reliability, validity and sensitivity / Young R.C. , Biggs J.T., Ziegler V.E. et al. // Br. J. Psychiatry. 1978. - Vol. 133.-P.429-35.
, Biggs J.T., Ziegler V.E. et al. // Br. J. Psychiatry. 1978. - Vol. 133.-P.429-35.
National Medical Research Center of Oncology. N.N. Blokhin
FIRST STAGE OF PROJECT COMPLETED SUCCESSFULLY
In September 2021, our Center won the competition of the Ministry of Science and Higher Education of the Russian Federation for the creation and development of a bioresource collection of cell lines and primary human tumors. For many years, the Center collected samples of tumors of different localizations, which were carefully and comprehensively studied in order to choose the best way to treat the patients of the Center. The collected tumor samples helped the Center's scientists develop new treatment tactics and test new drugs. In some cases, it was possible to preserve the viability of cells from tumor samples and create experimental models during long-term cultivation of tumor cells in nutrient media or transplantation into laboratory mice.
As a result, thousands of samples were dispersed among various institutes and laboratories of the Center, there was no unified register of samples, and information about them was distributed according to the principle of word of mouth. This situation did not contribute to the development of scientific research, it was necessary to create a single register of all biological samples of the center, a single information resource and a center for collective use. The Ministry of Higher Education and Science of the Russian Federation supported the scientists of the Center in this endeavor, and on September 28, 2021, Agreement No. 075-15-2021-1060 was signed between the Ministry and the Center on the implementation of the project "Creation and development of a bioresource collection of cell lines and primary human tumors" under the leadership of the Director of the Research Institute of Experimental Diagnostics and Therapy of Tumors Vyacheslav Stanislavovich Kosorukov.
In the 3 months that have passed since the beginning of the project, a new laboratory "Bioresource Collection of Cell Lines and Primary Tumors" was created at the Center, for which premises were allocated on the basis of the Research Institute of EDiTO and equipment was purchased: laminar cabinets for working with samples in sterile conditions, SO 2 - incubators for cultivating cell lines, cryostorage, as well as other devices and consumables. To form the scientific team of the new laboratory, an open competition was announced for filling the positions of researchers and director.
To form the scientific team of the new laboratory, an open competition was announced for filling the positions of researchers and director.
The creation of a laboratory is just one of the stages in solving the main task of this project: to make samples of the collection, as well as information about them, available to domestic and foreign scientists, to establish mechanisms for the functioning of the collection and its replenishment. First of all, it was necessary to carry out an inventory of all the samples available in various departments of the Center, which was successfully completed. In total, 10,664 samples of cell lines and hybridoma clones, 1,787 samples of transplanted tumor strains, and 2,466 samples of primary tumors and tissues were included in the registry. During the implementation of the first stage of the project, 1653 more samples (storage units) of cell lines and hybridoma clones and more than a hundred units of samples of transplanted strains and tumors were added to this number. For each sample of the Collection there is information about its characteristics, which is constantly supplemented, and this forms a large array of changing data. To use these data, a special information resource is required, and the development of such a resource was started from the first days of the project.
For each sample of the Collection there is information about its characteristics, which is constantly supplemented, and this forms a large array of changing data. To use these data, a special information resource is required, and the development of such a resource was started from the first days of the project.
An important component of the functioning of the collection is the analysis of the quality of samples, as well as the study of their genetic and phenotypic characteristics. At the first stage of the project, standards for the characterization of adhesive and suspension cell lines, hybridoma clones and monoclonal antibodies were developed, and corresponding methodologies were prepared.
The first assessments of the quality of the samples showed that most of them are well preserved, despite the long periods of preservation: most of the cell lines and transplanted tumor strains have shown their viability and the absence of microbiological contamination. In total, more than a hundred samples were examined and 134 tests were carried out for contamination with mycoplasma 29cell lines from commercial sources, 16 cell cultures obtained at the N.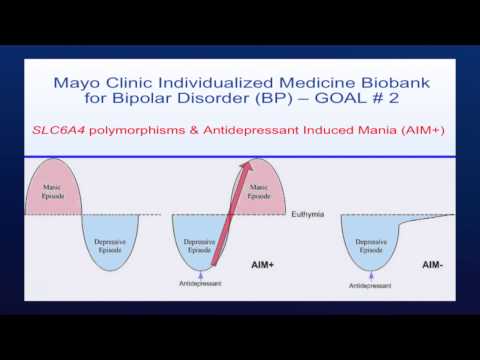 N. N.N. Blokhin” of the Ministry of Health of Russia, 17 transplantable tumor strains and 37 hybridoma clones. For hybridoma clones, their productivity and stability were additionally evaluated.
N. N.N. Blokhin” of the Ministry of Health of Russia, 17 transplantable tumor strains and 37 hybridoma clones. For hybridoma clones, their productivity and stability were additionally evaluated.
33 cell lines with the best quality indicators were selected to form the first lots of the collection - 50 samples (cryotubes) of each line of one passage. At the second stage of the project, the biological material of these lots will be characterized by genetic and immunochemical methods in accordance with the developed methodologies. To do this, it will be enough to unfreeze one or two cryovials from each lot, and as a result, get a complete and accurate picture of the properties of the remaining samples of the lot, which will be provided for research within the framework of the shared use center being created. Lots of characterized samples will be formed according to the same principle in the future.
Transplanted tumor strains and clinical samples of tumors are a valuable resource for many scientific studies, but their production and standardization are associated with a number of objective difficulties. Unlike cell lines, which can be generated and frozen in a few tens or hundreds of tubes, and then analyzed according to specific tasks, clinical samples require some preparation immediately after the collection of the material, and this preparation depends on the design of the experiment in which it will be used. sample. In an attempt to predict the future use of clinical samples, we applied several preparation options for each tumor sample. Samples for genetic analysis were isolated from the tumor tissue of each patient, cell and tissue lysates, cell suspensions were obtained, and paraffin blocks were made to perform immunochemical methods. Thus, samples from 15 primary tumors of various localizations were prepared and deposited: skin melanoma, uveal melanoma, ovarian cancer, liver cancer, rectal cancer, chorionepithelioma, gastrointestinal stromal tumor, as well as tumor samples of 10 transplantable strains obtained from malignant neoplasms of the cervix, body of the uterus, prostate, bladder, liver, colon and chorionepithelioma.
Unlike cell lines, which can be generated and frozen in a few tens or hundreds of tubes, and then analyzed according to specific tasks, clinical samples require some preparation immediately after the collection of the material, and this preparation depends on the design of the experiment in which it will be used. sample. In an attempt to predict the future use of clinical samples, we applied several preparation options for each tumor sample. Samples for genetic analysis were isolated from the tumor tissue of each patient, cell and tissue lysates, cell suspensions were obtained, and paraffin blocks were made to perform immunochemical methods. Thus, samples from 15 primary tumors of various localizations were prepared and deposited: skin melanoma, uveal melanoma, ovarian cancer, liver cancer, rectal cancer, chorionepithelioma, gastrointestinal stromal tumor, as well as tumor samples of 10 transplantable strains obtained from malignant neoplasms of the cervix, body of the uterus, prostate, bladder, liver, colon and chorionepithelioma. For transplanted strains of human tumors, the tumorigenicity of tumor cells was confirmed in experiments on athymic mice. Samples of these tumors were prepared for further study by genetic and immunochemical methods at the second stage of the project.
For transplanted strains of human tumors, the tumorigenicity of tumor cells was confirmed in experiments on athymic mice. Samples of these tumors were prepared for further study by genetic and immunochemical methods at the second stage of the project.
Cell lines and tumor samples as a research tool have their advantages and limitations. Cell lines are adapted to growth outside the body, so the processes occurring in them can be observed in vitro, but the two-dimensional nature of their growth does not fully reproduce all the features of the functioning of cells in the body. Transplanted tumor strains and tumor samples have a three-dimensional structure, therefore, they reproduce body tissues better, but the study of the processes occurring in them is limited by the impossibility of culturing them. The co-executor of this project is the Research Institute of Human Morphology named after academician Avtsyn, where methods have been developed for obtaining three-dimensional cell lines (tumoroids or spheroids), a kind of compromise version of a model system for studying tumor processes and the action of various kinds of substances.