Suicidal ideation care plan
3 Suicide Behaviors Nursing Care Plans
Home » Nursing Care Plans » 3 Suicide Behaviors Nursing Care Plans
Updated on
By Paul Martin, BSN, R.N.
ADVERTISEMENTS
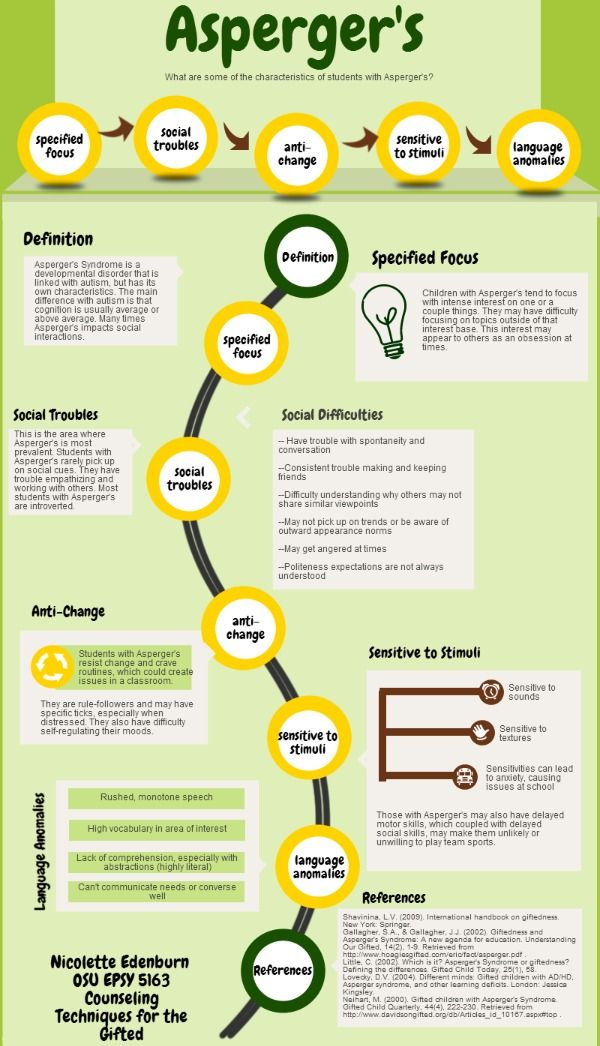
Suicide is the intentional act of killing oneself. Suicidal thoughts are common in people with depression, schizophrenia, alcohol/substance abuse and personality disorders (antisocial, borderline, and paranoid). Physical illness (chronic illness such as HIV, AIDS, recent surgery, pain) and environmental factors (unemployment, family history of depression, isolation, recent loss) can play a role in the suicide behavior.
Nursing Care PlansThe nursing care plan for suicidal patients involves providing a safe environment, initiating a no-suicide contract, creating a support system and ensuring close supervision.
Here are three (3) nursing care plans (NCP) and nursing diagnosis for suicide behaviors:
- Risk For Suicide
- Ineffective Coping
- Hopelessness
ADVERTISEMENTS
Risk For SuicideNursing Diagnosis
- Risk For Suicide
Risk Factors
- Alcohol and substance abuse/use.
- Abuse in childhood.
- Family history of suicide.
- Fits demographic (children, adolescent, young adult male, elderly male, Native American, Caucasian).
- Grief, bereavement/loss of an important relationship.
- History of prior suicide attempt.
- Hopelessness/helplessness.
- Legal or disciplinary problems.
- Physical illness, chronic pain, terminal illness.
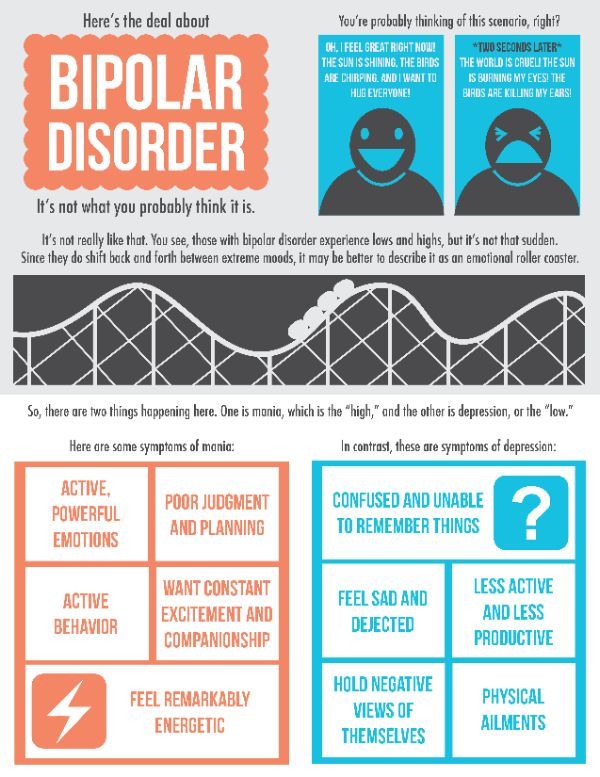
- Psychiatric illness (e.g., bipolar disorder, depression, schizophrenia).
- Poor support system, loneliness.
Possibly evidenced by
- Statements of despair, helplessness, hopelessness and nothing left to live for.
- Suicide plan (clear and specific, lethal method and available means).
- Suicide behavior (attempt, ideation, talk, plan, available means).
- Suicide cues
- Covert: Making out a will, giving valuables away, writing forlorn love notes, taking out large life insurance policy.
- Overt: “No one will miss me”; “No reason to live for”; “I’d be better off dead”.

Desired Outcomes
- Patient will refrain from attempting suicide.
- Patient will make a no-suicide contract with the nurse covering the next 24 hours, then renegotiate the terms at that time (If in hospital and accepted at your institution).
- Patient will remain safe while in the hospital, with the aid of nursing intervention and support (if in the hospital).
- Patient will stay with a friend or family if the person still has the potential for suicide (if in the community).
- Patient will join family in crisis family counseling.
- Patient will have links to self-help groups in the community.
- Patient will keep an appointment for the next day with a crisis counselor (if in the community).
- Patient will identify at least one goal for the future.
- Patient will uphold a suicide contract.
- Patient will state that he or she wants to live.
- Patient will name at least one acceptable alternative to his or her situation.
- Patient will name two people he/she can call if thoughts of suicide recur before discharge.
| Nursing Interventions | Rationale |
|---|---|
| In the Community: | |
| Arrange for the client to stay with family or friends. A hospitalization is considered if there is no one is available especially if the person is highly suicidal. | Relieve isolation and provide safety and comfort. |
| Encourage the client to avoid decisions during the time of crisis until alternatives can be considered. | During crisis situations, people are unable to think clearly or evaluate their options readily. |
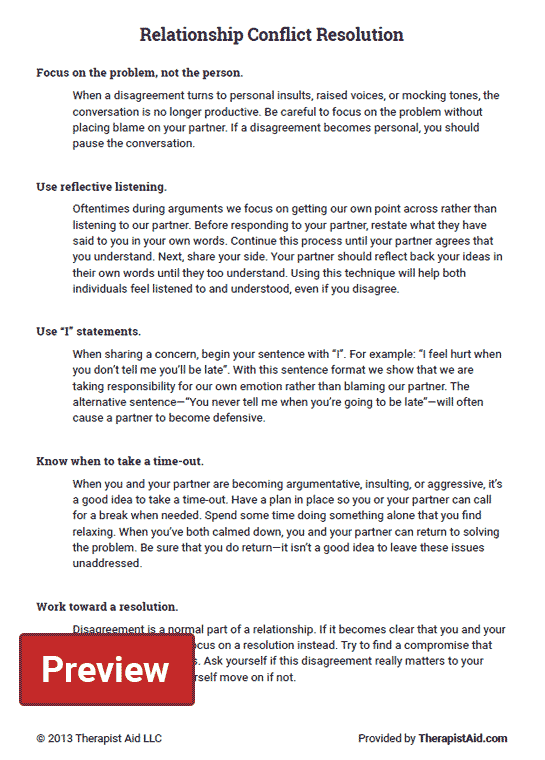
| Encourage the client to talk freely about feelings and help plan alternative ways of handling disappointment, anger, and frustration. | Gives client other ways of dealing with strong emotions and gaining a sense of control over their lives. |
Weapons and pills are removed by friends, relatives, or the nurse. | To provide a safe environment, free from things that may harm the client. |
| If anxiety is extremely high, or client has not slept in days, a tranquilizer might be prescribed. Only a 1 to 3 day supply of medication should be given. Family member or significant other should monitor pills for safety. | Relief of anxiety and restoration of sleep loss can help the client think more clearly and might help restore some sense of well-being. |
| Contact family members, arrange for individual and/ or family crisis counseling. Activate links to self-help groups. | Reestablishes social ties. Diminishes sense of isolation, and provides contact from individuals who care about the suicidal person. |
| In the Hospital: | |
During the crisis period, health care workers will continue to emphasize the following four points:
| Because of “tunnel vision“, clients do not have perspective on their lives. These statements give perspective to the client and help offer hope for the future. |
| Forensic Issues: | |
| Follow unit protocol for suicide regarding creating a safe environment (taking away potential weapons– belts, sharp objects, items, and so on). | Provide safe environment during time client is actively suicidal and impulsive; self-destructive acts are perceived as ties, the only way out of an intolerable situation. |
| Keep accurate and thorough records of client’s behaviors (verbal and physical) and all nursing/physician actions. | These might become court documents. If client checks and attention to client’s needs or request are not documented, they do not exist in a court of law. |
Put on either suicide precaution (one-on-one monitoring at one arm’s length away) or suicide observation (15-minute visual check of mood, behavior, and verbatim statements), depending on level of suicide potential. | Protection and preservation of the client’s life at all costs during crisis is part of medical and nursing staff responsibility. Follow unit protocol. |
| Keep accurate and timely records, document client’s activity, usually every 15 minutes (what client is doing, with whom, and so on). Follow unit protocol. | Accurate documentation is vital. The chart is a legal document as to client’s “ongoing status,” intervention taken, and by whom. |
| Encourage the client to talk about their feelings and problem solve alternatives. | Talking about feelings and looking at alternatives can minimize suicidal acting out. |
| Construct a no-suicide contract between the suicidal client and nurse. Use clear, simple language. When the contract is up, it is renegotiated (If this is accepted procedure at your institution). | The no-suicide contract helps client know what to do when they begin to feel overwhelmed by pain (e.g., “I will speak to my nurse/counselor/support group/family member when I first begin to feel the need to end my life”). |
ADVERTISEMENTS
ADVERTISEMENTS
Recommended ResourcesRecommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
- Nursing Care Plans: Nursing Diagnosis and Intervention (10th Edition)
An awesome book to help you create and customize effective nursing care plans. We highly recommend this book for its completeness and ease of use. - Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions and Rationales
A quick-reference tool to easily select the appropriate nursing diagnosis to plan your patient’s care effectively. - NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023 (12th Edition)
The official and definitive guide to nursing diagnoses as reviewed and approved by the NANDA-I. This book focuses on the nursing diagnostic labels, their defining characteristics, and risk factors – this does not include nursing interventions and rationales.
This book focuses on the nursing diagnostic labels, their defining characteristics, and risk factors – this does not include nursing interventions and rationales. - Nursing Diagnosis Handbook, 12th Edition Revised Reprint with 2021-2023 NANDA-I® Updates
Another great nursing care plan resource that is updated to include the recent NANDA-I updates. - Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5(TM))
Useful for creating nursing care plans related to mental health and psychiatric nursing. - Ulrich & Canale’s Nursing Care Planning Guides, 8th Edition
Claims to have the most in-depth care plans of any nursing care planning book. Includes 31 detailed nursing diagnosis care plans and 63 disease/disorder care plans. - Maternal Newborn Nursing Care Plans (3rd Edition)
If you’re looking for specific care plans related to maternal and newborn nursing care, this book is for you.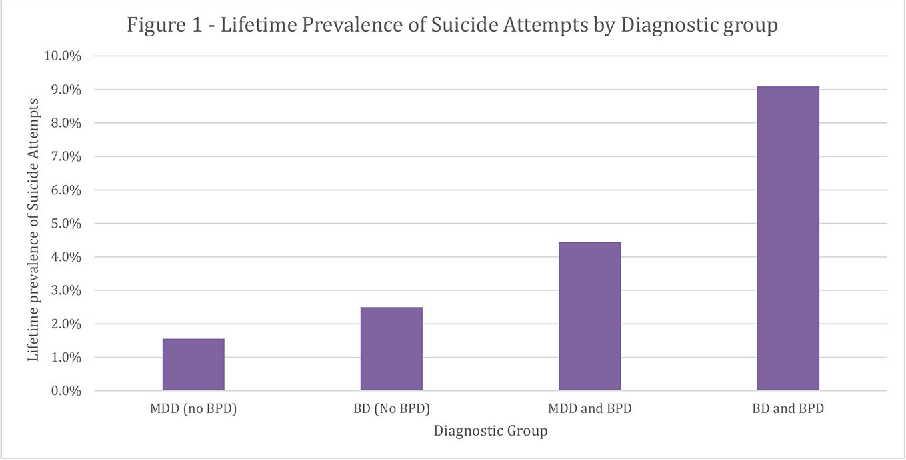
- Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care (7th Edition)
An easy-to-use nursing care plan book that is updated with the latest diagnosis from NANDA-I 2021-2023. - All-in-One Nursing Care Planning Resource: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health (5th Edition)
Definitely an all-in-one resources for nursing care planning. It has over 100 care plans for different nursing topics.
Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ!
Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch. - Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing
Our comprehensive guide on how to create and write diagnostic labels.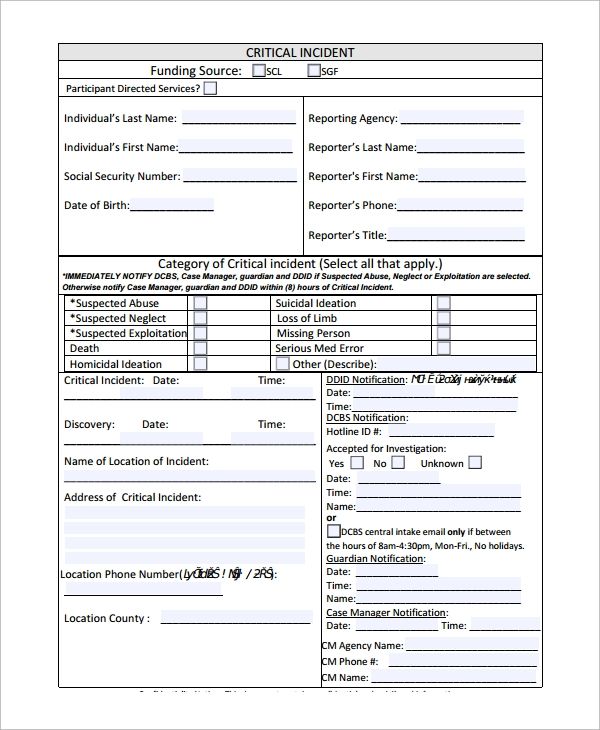 Includes detailed nursing care plan guides for common nursing diagnostic labels.
Includes detailed nursing care plan guides for common nursing diagnostic labels.
Other care plans for mental health and psychiatric nursing:
- Alcohol Withdrawal | 5 Care Plans
- Anxiety and Panic Disorders | 7 Care Plans
- Bipolar Disorders | 6 Care Plans
- Major Depression | 9 Care Plans
- Personality Disorders | 4 Care Plans
- Schizophrenia | 6 Care Plans
- Sexual Assault | 1 Care Plan
- Substance Dependence and Abuse | 8 Care Plans
- Suicide Behaviors | 3 Care Plans
ADVERTISEMENTS
Categories Mental Health and Psychiatric Care Plans, Nursing Care Plans Tags depression, hopelessness, ineffective coping, major depression, Personality Disorders, Risk for Suicide, Suicide
Paul Martin, BSN, R.N.
Paul Martin is a registered nurse with a bachelor of science in nursing since 2007. Having worked as a medical-surgical nurse for five years, he handled different kinds of patients and learned how to provide individualized care to them. Now, his experiences working in the hospital is carried over to his writings to help aspiring students achieve their goals. He is currently working as a nursing instructor and have a particular interest in nursing management, emergency care, critical care, infection control, and public health. As a writer at Nurseslabs, his goal is to impart his clinical knowledge and skills to students and nurses helping them become the best version of themselves and ultimately make an impact in uplifting the nursing profession.
Having worked as a medical-surgical nurse for five years, he handled different kinds of patients and learned how to provide individualized care to them. Now, his experiences working in the hospital is carried over to his writings to help aspiring students achieve their goals. He is currently working as a nursing instructor and have a particular interest in nursing management, emergency care, critical care, infection control, and public health. As a writer at Nurseslabs, his goal is to impart his clinical knowledge and skills to students and nurses helping them become the best version of themselves and ultimately make an impact in uplifting the nursing profession.
© 2022 Nurseslabs | Ut in Omnibus Glorificetur Deus!
Risk for Suicide Nursing Care Plan - Nursing Diagnosis and Care Planning
Home » Nursing Care Plans » Nursing Diagnosis » Risk for Suicide Nursing Care Plan
Updated on
By Gil Wayne, BSN, R. N.
N.
ADVERTISEMENTS
Use this nursing diagnosis guide to help you create a Risk for Suicide Level nursing care plan.
Suicide is a serious public health problem that is increasing exponentially in every part of the world. The majority of patients who engage in suicidal attempts have a psychiatric disorder. Mood disorders such as depression and bipolar manic-depression are by far the most prevalent psychiatric conditions linked to suicide. Whereas patients with schizophrenia or an organic brain disorder are strongly linked to a higher-than-normal chance of suicide and suicide attempts with voices that tell them to hurt himself or herself. Other factors that may affect the risk for suicide include mental disorders, substance misuse, psychological states, cultural, family, and social situations, and genetics.
Common suicide methods in men include asphyxiation, hanging, firearms, jumping, moving objects, sharp objects, and vehicle exhaust gas, while women tend to use a vaster variety of suicide methods than men. Common suicide methods in women include self-poisoning, exsanguination, drowning, hanging, and firearms.
Common suicide methods in women include self-poisoning, exsanguination, drowning, hanging, and firearms.
The role of the nurses particular to suicide prevention or patients at risk for suicide includes both systems and patient-level interventions. At the systems level, the nurse evaluates and controls environmental safety, improves protocols, policies, and practices consistent with zero suicide, and associates in training for all milieu staff. At the patient level, the nurse assesses outcomes of all interventions, evaluates risk for suicide, monitors and manages at-risk patients, and provides suicide-specific psychotherapeutic interventions. Nurses’ hands-on patient care is vital by taking all threats or suicide attempts seriously and emphasizing a relationship alliance by developing rapport for the patient.
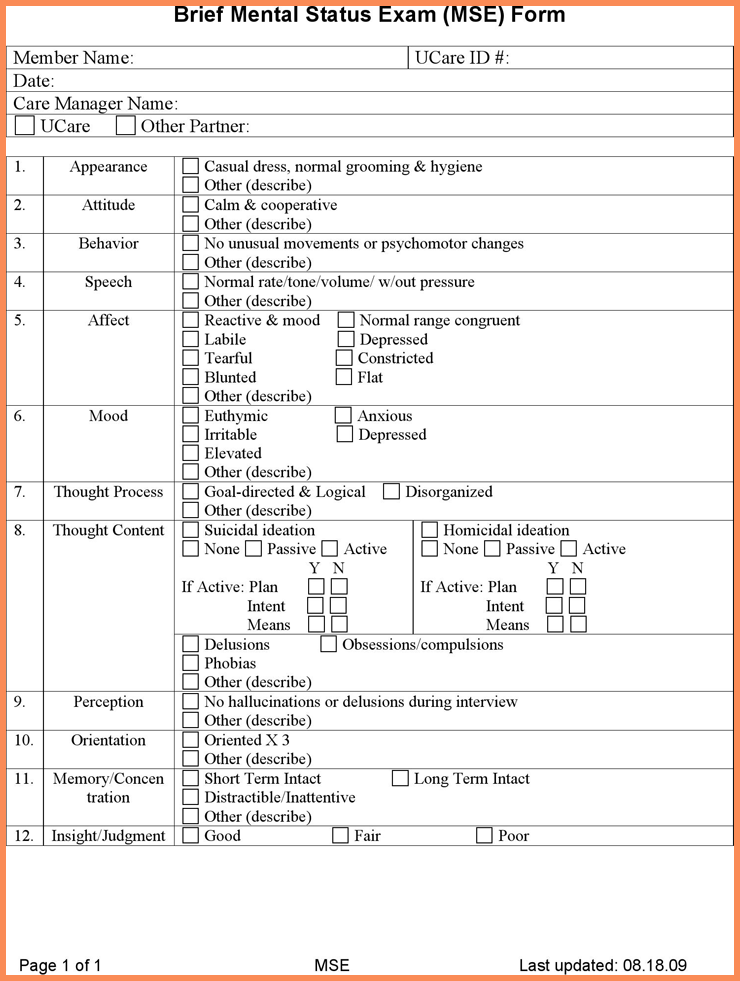
Risk for Suicide Nursing AssessmentAssessment is necessary in order to identify potential problems that may have lead to suicide and also name any event that may happen during nursing care.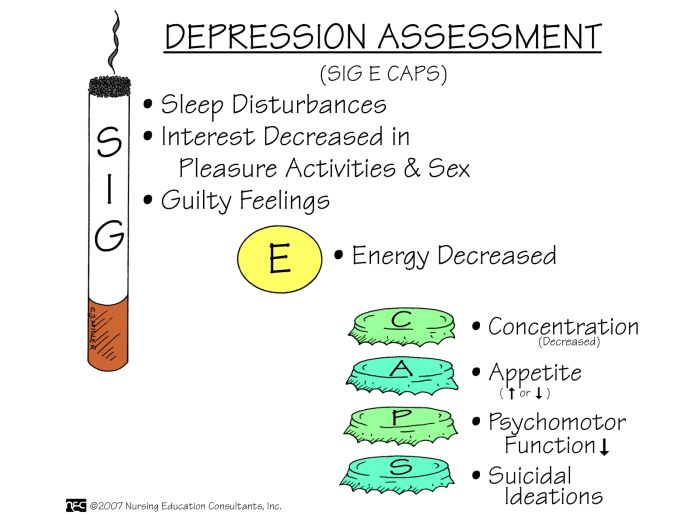
ADVERTISEMENTS
| Assessment | Rationale |
|---|---|
| Talk to the patient to evaluate the potential for self-injury. | Patients considering suicide may display verbal and behavioral cues about their intent to end their life. |
| Ask the following questions: | |
| Suicide ideation is the manner of thinking about killing oneself. The patient’s risk for suicide progresses as these thoughts become more frequent. |
| The patient’s status of suicide risk is distinguished if there is a history of earlier suicide attempts. |
| This allows for the person to discuss feelings and issues openly. |
| Citing a plan and the ability to carry it out greatly increase the risk for suicide. The more harmful the plan, the more serious the risk for suicide. The more harmful the plan, the more serious the risk for suicide. |
| Patients with suicidal thoughts may sense their authority of suicidal thoughts slipping away, or they may feel themselves surrender to a desire to end their life. |
| Observe for risk factors that may increase the chance of suicide attempt. | It is a myth that suicide occurs without forewarning. It is also a myth that there is a typical type of a suicidal person. Anyone can be a victim of suicide. |
| This increases the risk for suicide. |
| Most of the patients with suicide attempts give verbal cues of their plans to do so. The person may talk idealistically about release from his or her life and the resolution of problems.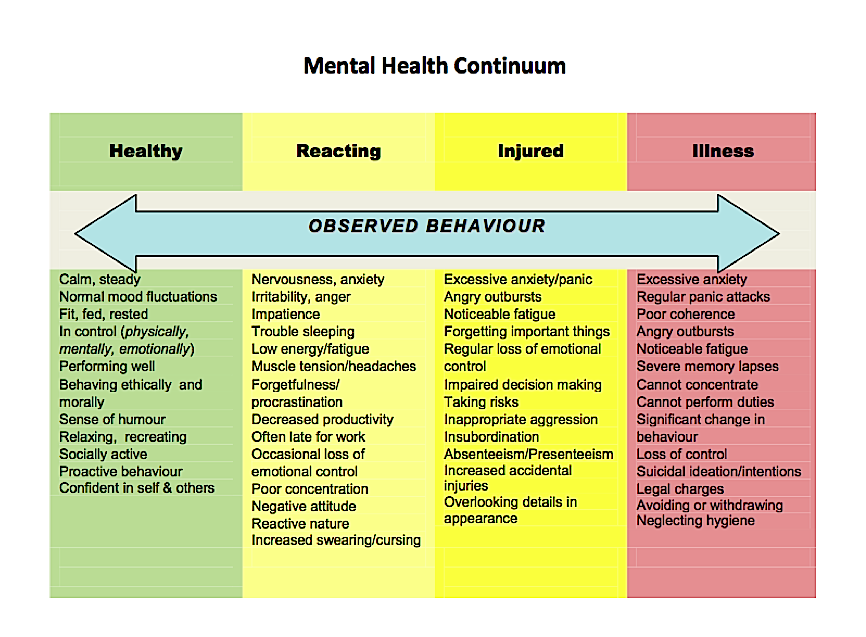 |
| Alcohol and drug abuse increase the risk of suicide. The highest risk is among patients who have substance abuse problems. |
| History of severe insomnia is one factor associated with suicide risk. |
| Mood disorders such as depression and bipolar manic-depression are by far the most prevalent psychiatric conditions linked to suicide. |
| This sudden behavioral modification may represent the person’s decision to carry out a suicide plan. |
| Men die by suicide around four times more frequently than women, whereas women attempt suicide two to three times more frequently than men. |
| This action signifies the person’s detachment and withdrawal from life.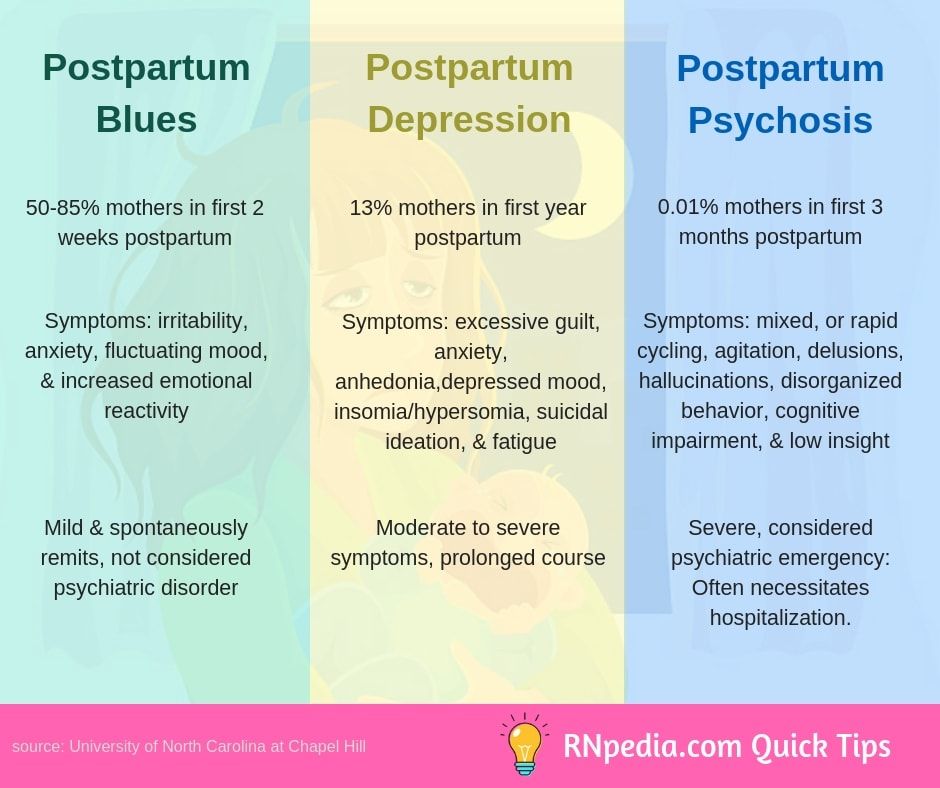 |
| Determine particular stressors. | Determining causative factors aids in developing appropriate coping strategies. Suicide seemed to be an acceptable solution when a person can not find any more solution to his or her problem. |
| Appraise all possible and beneficial coping methods. | Patients with history of ineffective coping may need new resources. |
| Assess the need for hospitalization and safety precautions. | Patient safety is always a priority. Patients with suicidal attempts should be in a setting with direct supervision. |
| Assess all support resources available to the patient. | Depression leads to a sense of hopelessness and the person involved may isolate himself or herself and may be unable to consider available supports. |
| Assess decision-making and problem-solving energy. | Impulsivity may be an element of mood and bipolar disorder. Patients may need supervision in decision-making until the mood has been stabilized.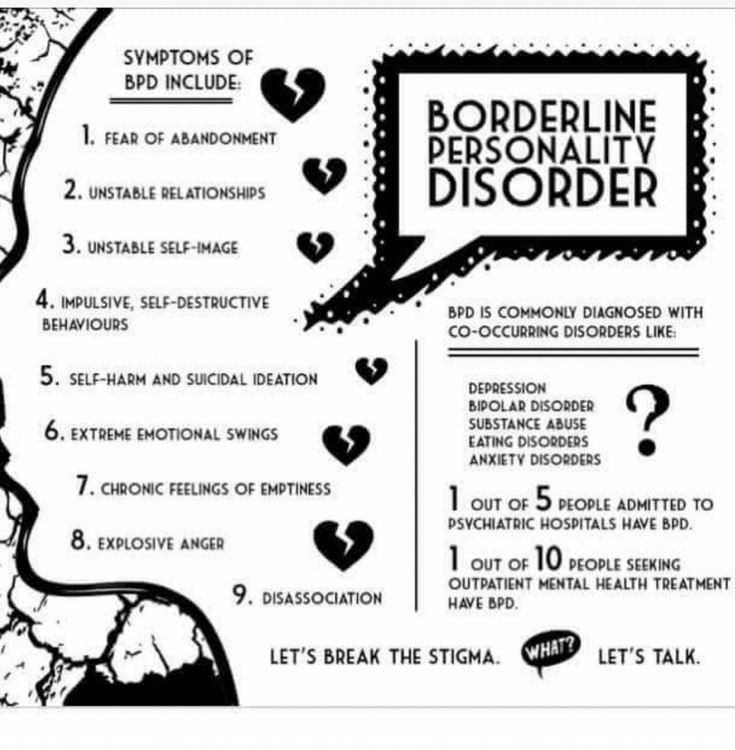 |
The following are the therapeutic nursing interventions for Risk for Suicide nursing diagnosis:
| Nursing Interventions | Rationale |
|---|---|
| Render close patient supervision by sustaining observation or awareness of the patient at all times. | Suicide may be an impulsive act with little or no warning. Close supervision is a must. |
| Provide a safe environment. Weapons and pills should be removed by friends, relatives, or the nurse. | Removing potentially harmful objects prevents the patient from acting or sudden self-destructive impulses. |
| Present opportunities for the patient to express thoughts, and feelings in a nonjudgmental environment. | It is helpful for the patient to talk about suicidal thoughts and intentions to harm themselves. Expressing their thoughts and feelings may lessen their intensity. Also, they need to see that staff are open to discussion. Also, they need to see that staff are open to discussion. |
| Create a verbal or written contract stating that the patient will not act on impulse to do self-harm. | This method establishes permission to talk about the subject. |
| Stay with the patient more often. | This approach provides the patient with a sense of security and strengthens self-worth. |
| Disincline the patient in making decisions during severe stress. | Patients can learn to recognize mood changes that indicate problems with impulsivity or indicate a deepening depressive state. |
| Help the patient with problem-solving in a constructive manner. | Patients can get to identify situational, interpersonal, or emotional triggers and learn to assess a problem and implement problem-solving measures before reacting. |
Arrange for the client to stay with family or friends. A hospitalization is considered if there is no one is available especially if the person is highly suicidal.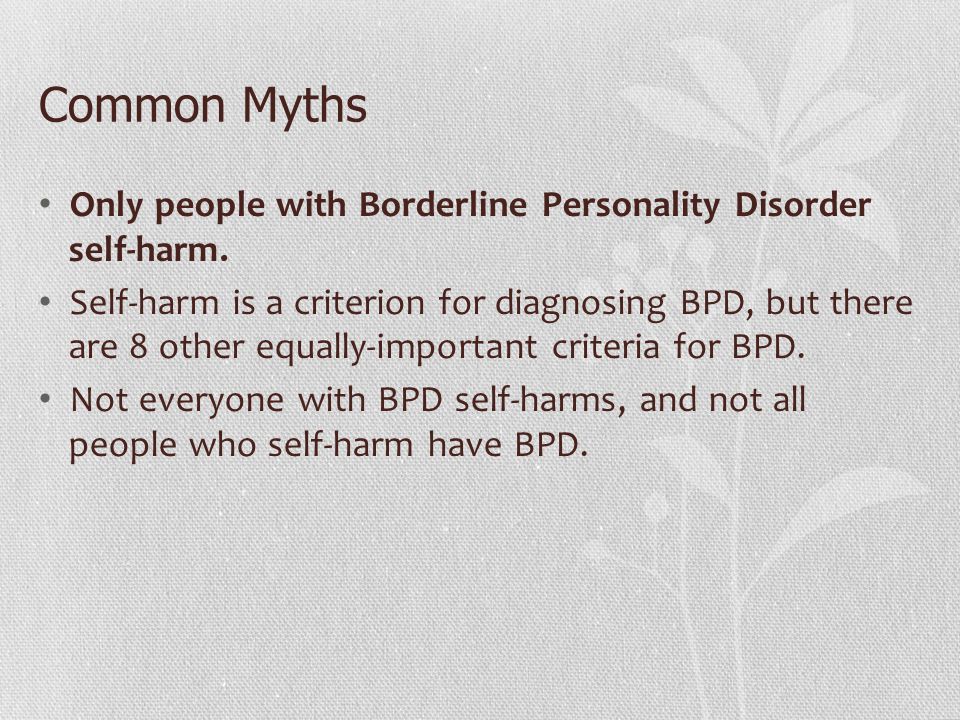 | Relieve isolation and provide safety and comfort. |
| Educate the patient in the appropriate use of medications to facilitate his or her ability to cope. | Drug therapy may benefit the patient endure underlying health problems such as depression. |
| Contact family members, arrange for individual and/ or family crisis counseling. Activate links to self-help groups. | Reestablishes social ties. Diminishes sense of isolation, and provides contact from individuals who care about the suicidal person. |
| Educate the patient cognitive-behavioral self-management responses to suicidal thoughts. | Patient learns to identify negative thoughts and develops positive approaches and positive thinking. |
| Introduce the use of self-expression methods to manage suicidal feelings. | Patients are better to acknowledge and safely handle suicidal feelings by programs such as keeping journals and calling hotlines. |
Recommended nursing diagnosis and nursing care plan books and resources.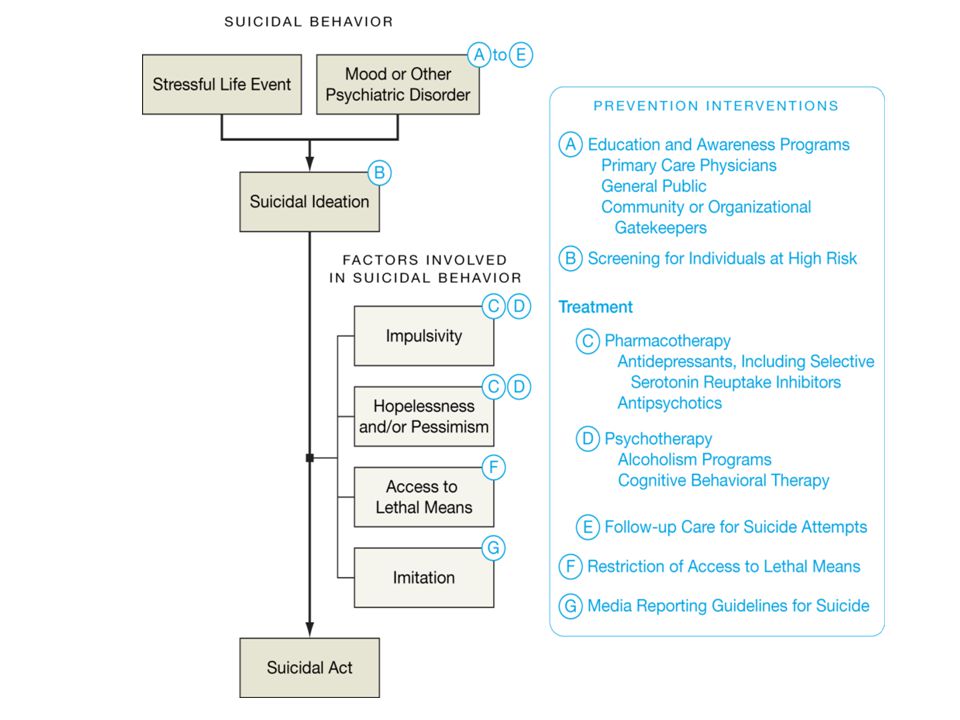
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
- Nursing Care Plans: Nursing Diagnosis and Intervention (10th Edition)
An awesome book to help you create and customize effective nursing care plans. We highly recommend this book for its completeness and ease of use. - Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions and Rationales
A quick-reference tool to easily select the appropriate nursing diagnosis to plan your patient’s care effectively. - NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023 (12th Edition)
The official and definitive guide to nursing diagnoses as reviewed and approved by the NANDA-I. This book focuses on the nursing diagnostic labels, their defining characteristics, and risk factors – this does not include nursing interventions and rationales.
- Nursing Diagnosis Handbook, 12th Edition Revised Reprint with 2021-2023 NANDA-I® Updates
Another great nursing care plan resource that is updated to include the recent NANDA-I updates. - Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5(TM))
Useful for creating nursing care plans related to mental health and psychiatric nursing. - Ulrich & Canale’s Nursing Care Planning Guides, 8th Edition
Claims to have the most in-depth care plans of any nursing care planning book. Includes 31 detailed nursing diagnosis care plans and 63 disease/disorder care plans. - Maternal Newborn Nursing Care Plans (3rd Edition)
If you’re looking for specific care plans related to maternal and newborn nursing care, this book is for you. - Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care (7th Edition)
An easy-to-use nursing care plan book that is updated with the latest diagnosis from NANDA-I 2021-2023.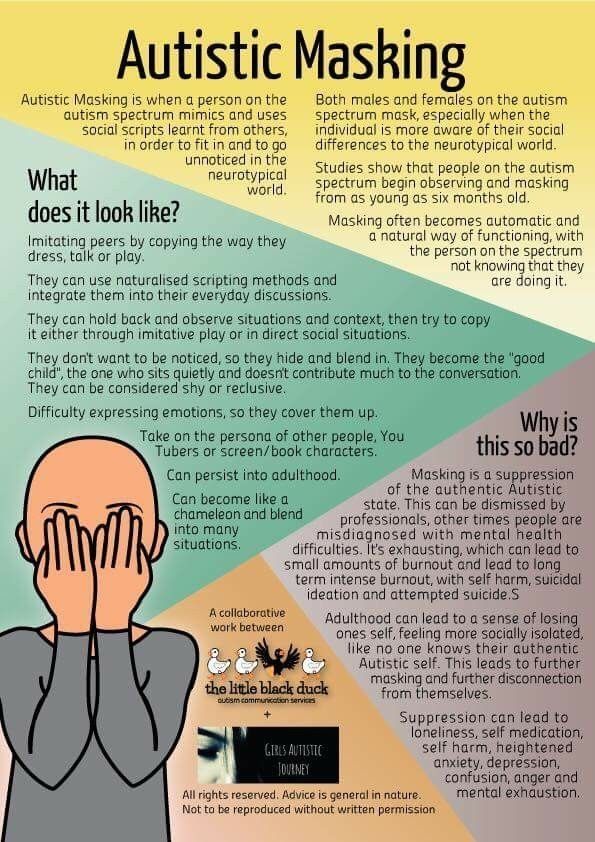
- All-in-One Nursing Care Planning Resource: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health (5th Edition)
Definitely an all-in-one resources for nursing care planning. It has over 100 care plans for different nursing topics.
Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ!
Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch. - Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing
Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
ADVERTISEMENTS
Categories Nursing Diagnosis Tags Nursing Care Plan, Nursing Care Plans, Nursing Diagnoses, Nursing Diagnosis, psychiatric nursing, Risk for Suicide, Suicide
Gil Wayne, BSN, R.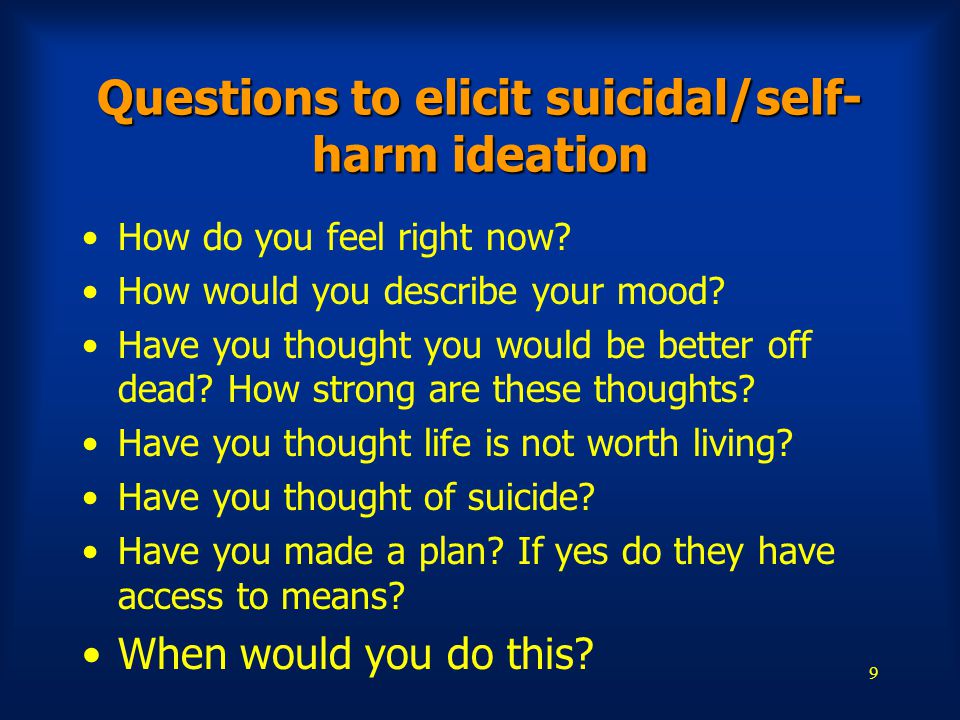 N.
N.
Gil Wayne graduated in 2008 with a bachelor of science in nursing. He earned his license to practice as a registered nurse during the same year. His drive for educating people stemmed from working as a community health nurse. He conducted first aid training and health seminars and workshops for teachers, community members, and local groups. Wanting to reach a bigger audience in teaching, he is now a writer and contributor for Nurseslabs since 2012 while working part-time as a nurse instructor. His goal is to expand his horizon in nursing-related topics. He wants to guide the next generation of nurses to achieve their goals and empower the nursing profession.
© 2022 Nurseslabs | Ut in Omnibus Glorificetur Deus!
Get help & support for suicide
If you’re in emotional distress or suicidal crisis, find help in your area with Find a helpline.
If you believe that someone else is in danger of suicide and you have their contact information, contact your local law enforcement for immediate help.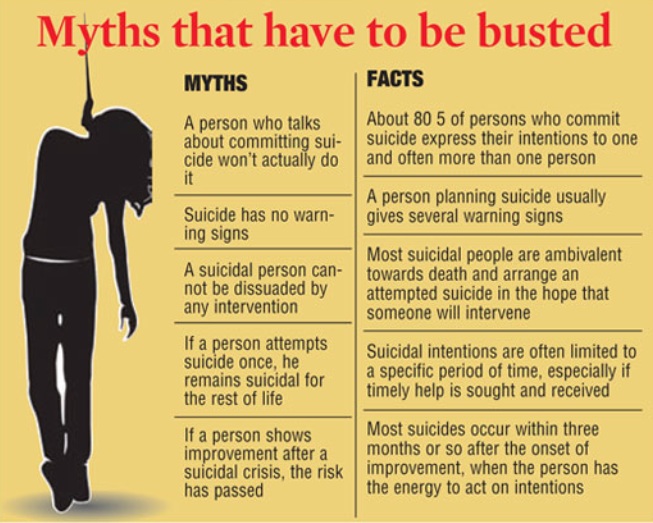 You can also encourage the person to contact a suicide prevention hotline using the information above.
You can also encourage the person to contact a suicide prevention hotline using the information above.
Learn more about personal crisis information with Google Search.
Google’s crisis information comes from high-quality websites, partnerships, medical professionals, and search results.
Important: Partnerships vary by country and region.
| Country | Hotline organization | Website | Phone number |
|---|---|---|---|
| Argentina | Centro de Asistencia al Suicida | www.asistenciaalsuicida.org | (011) 5275-1135 |
| Australia | Lifeline Australia | www.lifeline.org | 13 11 14 |
| Austria | Telefon Seelsorge Osterreich | www.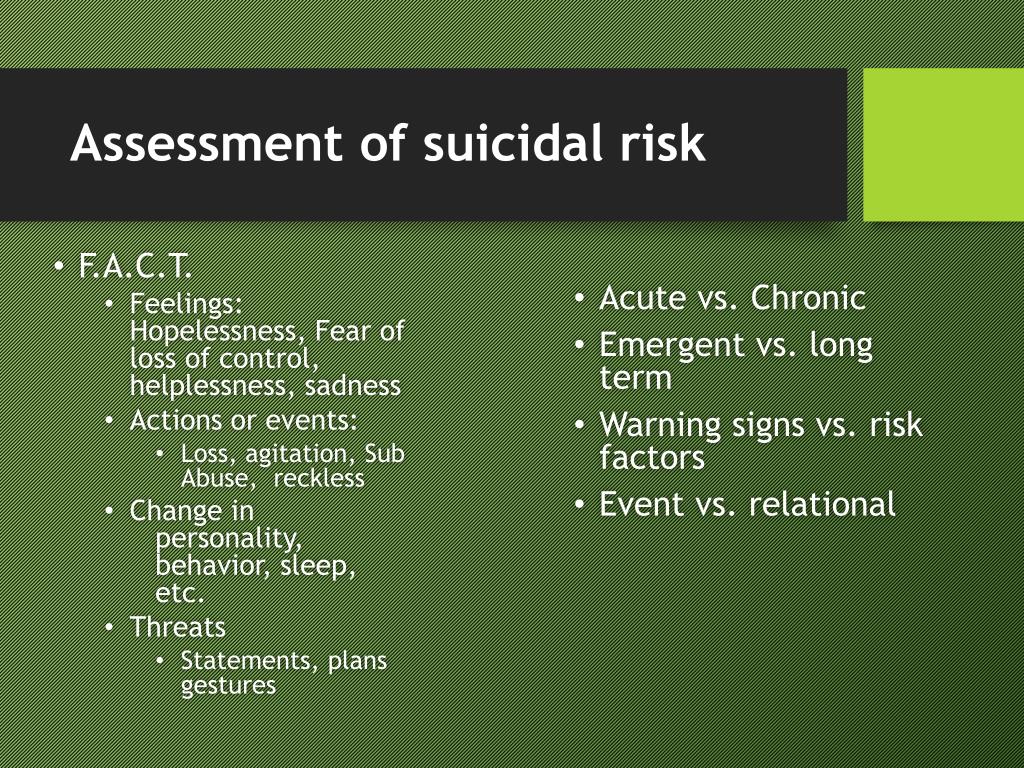 telefonseelsorge.at telefonseelsorge.at | 142 |
| Belgium | Center de Prevention du Suicide | www.preventionsuicide.be | 0800 32 123 |
| Belgium | CHS Helpline | www.chsbelgium.org | 02 648 40 14 |
| Belgium | Zelfmoord 1813 | www.zelfmoord1813.be | 1813 |
| Brazil | Centro de Valorização da Vida | www.cvv.org | 188 |
| Canada | Crisis Services Canada | crisisservicescanada.ca | 833-456-4566 |
| Chile | Ministry of Health of Chile | www.hospitaldigital.gob | 6003607777 |
| China | Beijing Suicide Research and Prevention Center | www.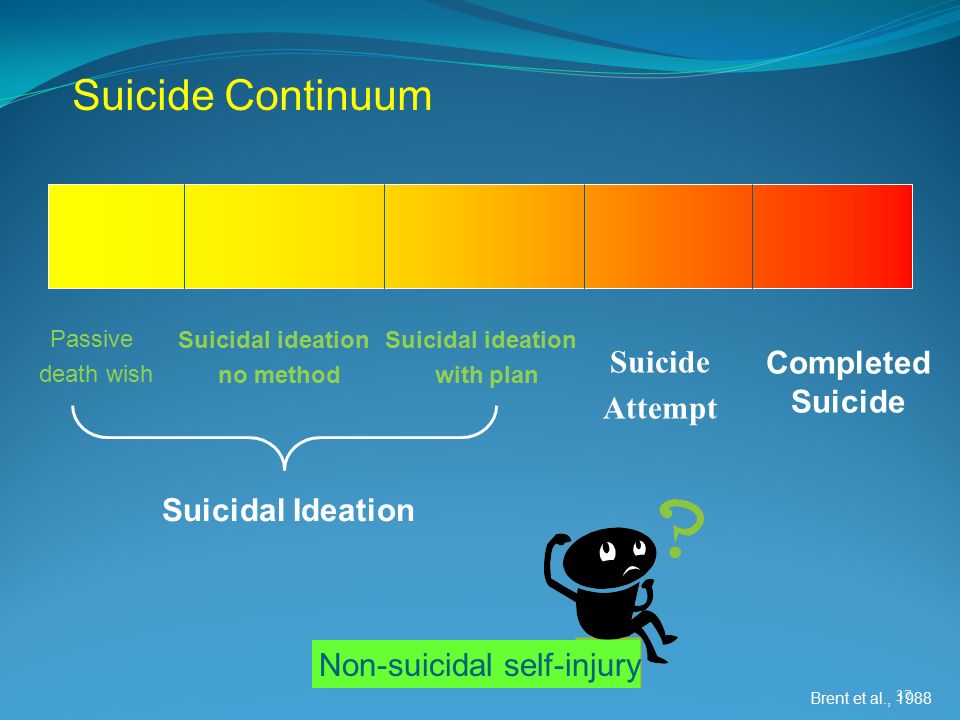 crisis.org crisis.org | 800-810-1117 |
| Costa Rica | Colegio de Profesionales en Psicologia de Costa Rica | psicologiacr.com/aqui-estoy | 2272-3774 |
| France | SOS Amitié | www.sos-amitie.org | 09 72 39 40 50 |
| Germany | Telefon Seelsorge Deutschland | www.telefonseelsorge.de | 0800 1110111 |
| Hong Kong | Suicide Prevention Services | www.sps.org | 2382 0000 |
| India | iCall Helpline | icallhelpline.org | 9152987821 |
| Ireland | Samaritans Ireland | www.samaritans.org/how-we-can-help | 116 123 |
| Israel | [Eran] ער"ן | www. eran.org eran.org | 1201 |
| Italy | Samaritans Onlus | www.samaritansonlus.org | 06 77208977 |
| Japan | Ministry of Education, Culture, Sports, Science and Technology | www.mext.go.jp | 81-0120-0-78310 |
| Japan | Ministry of Health, Labor and Welfare of Japan | www.mhlw.go | 0570-064-556 |
| Malaysia | Befrienders KL | www.befrienders.org | 03-76272929 |
| Netherlands | 113Online | www.113.nl | 0800-0113 |
| New Zealand | Lifeline Aotearoa Incorporated | www.lifeline.org | 0800 543 354 |
| Norway | Mental Helse | mentalhelse.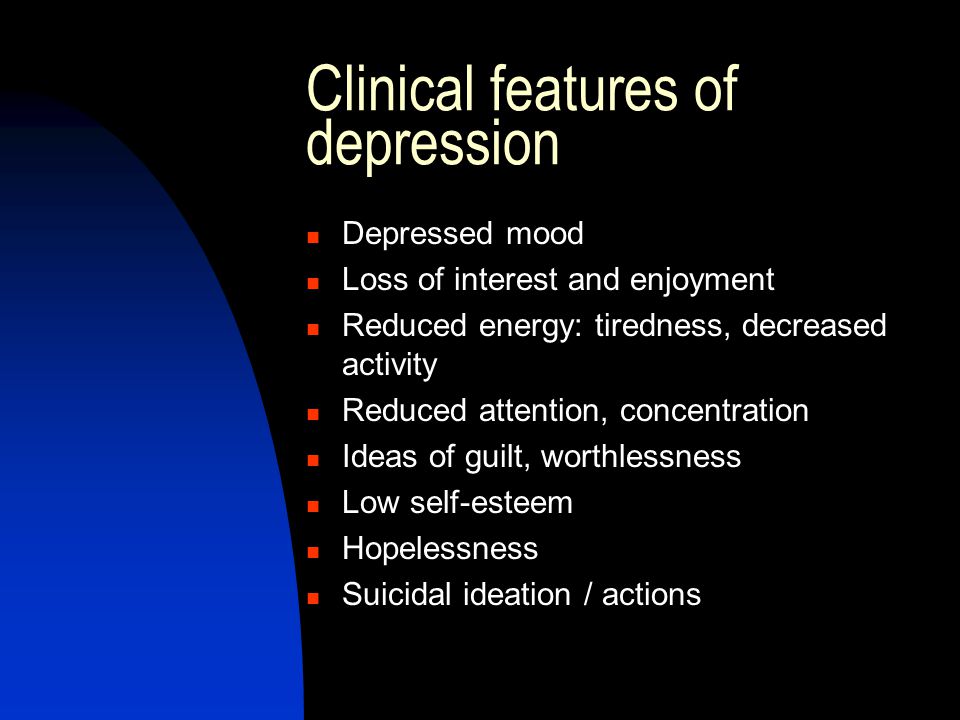 no no | 116 123 |
| Pakistan | Umang Pakistan | www.umang.com.pk/ | 0311-7786264 |
| Peru | Linea 113 Salud | www.gob.pe/555-recibir-informacion-y-orientacion-en-salud | 113 |
| Philippines | Department of Health - Republic of the Philippines | doh.gov.ph/NCMH-Crisis-Hotline | 0966-351-4518 |
| Portugal | SOS Voz Amiga | www.sosvozamiga.org | 213 544 545 963 524 660 912 802 669 |
| Russia | Fund to Support Children in Difficult Life Situations | www.ya-parent.ru | 8-800-2000-122 |
| Singapore | Samaritans of Singapore | www. sos.org sos.org | 1-767 |
| South Africa | South African Depression and Anxiety Group | www.sadag.org | 0800 567 567 |
| South Korea | Korea Suicide Prevention Center중앙자살예방센터 | www.spckorea.or | 1393 |
| Spain | Telefono de la Esperanza | www.telefonodelaesperanza.org | 717 003 717 |
| Switzerland | Die Dargebotene Hand | www.143.ch | 143 |
| Taiwan | 国际生命线台湾总会 [International Lifeline Taiwan Association] | www.life1995.org | 1995 |
| Ukraine | Lifeline Ukraine | lifelineukraine.com | 7333 |
| United Kingdom | Samaritans | www. samaritans.org/how-we-can-help samaritans.org/how-we-can-help | 116 123 |
| United States | 988 Suicide & Crisis Lifeline | 988lifeline.org | 988 |
How can we improve it?
Ask the Help Community
Get answers from community expertsTransfers
home
Parents
Helpline
Information about the unified all-Russian children’s helpline
0446 8-800-2000-122 .
When calling this number in any locality of the Russian Federation from fixed or mobile phones, children in difficult life situations, adolescents and their parents, other citizens can receive emergency psychological assistance, which is provided by specialists of services already operating in the constituent entities of the Russian Federation that provide services for telephone counseling and connected to a single all-Russian number of children's helpline.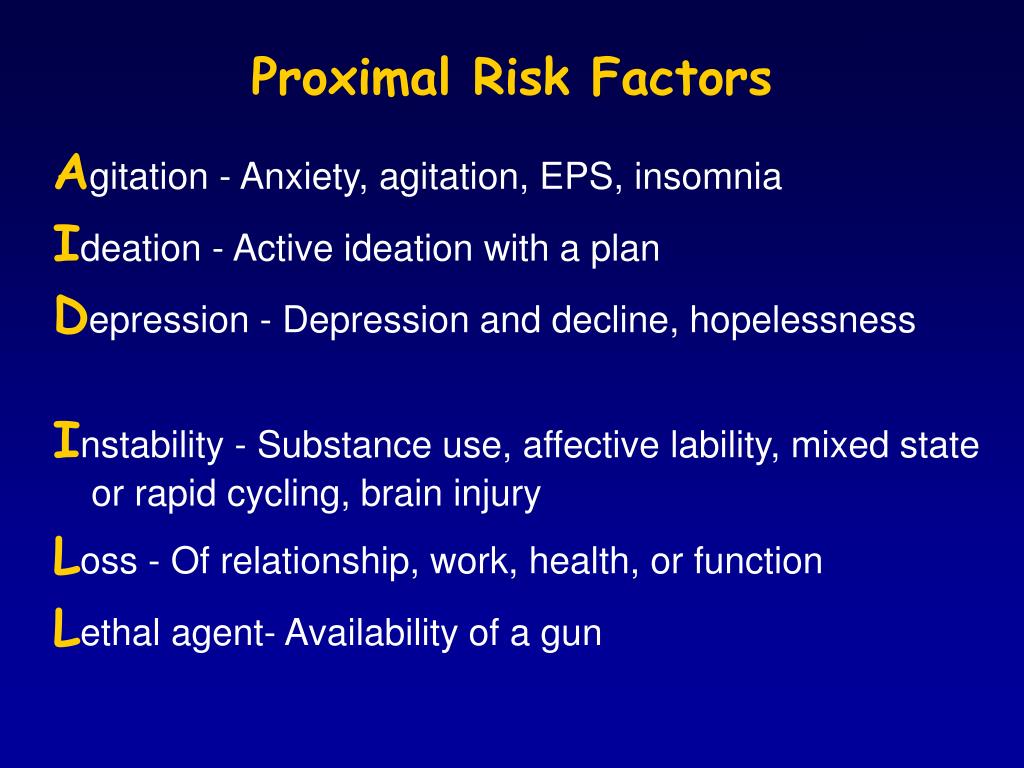
Confidentiality and free of charge are the two main principles of the children's helpline. This means that every child and parent can anonymously and free of charge receive psychological assistance and the secrecy of his call to the helpline is guaranteed.
Working hours of the children's helpline in the constituent entities of the Russian Federation
(as of October 1, 2013)
| Name of the subject of the Russian Federation 9Arkhangelsk region 09.00-22.00 | |||
| 22 | with Nenets Autonomous Okrug | daily 09.00-17.30 | |
| 23 | Vologda region | around the clock | |
| 24 | Kaliningrad region | daily0039 | around the clock |
| 35 | Chechen Republic 08.30-20.00 | ||
| South Federal District | |||
| 37 | Republic of Adygea | ||
| Kalmykia | Pon-Pip.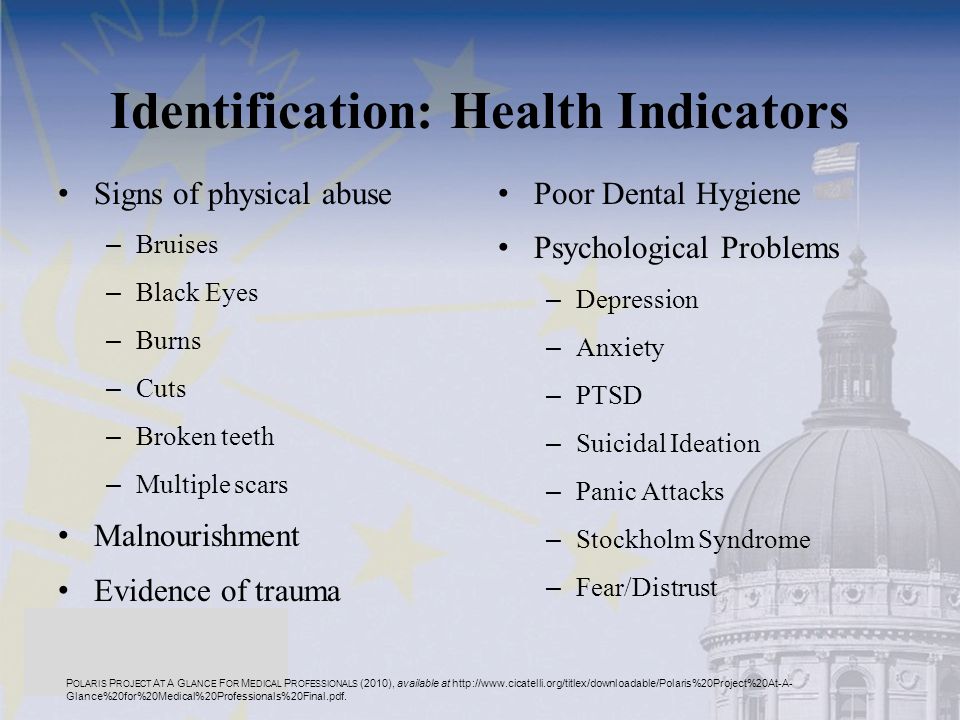 8.00-17.00 8.00-17.00 | ||
| 3 | |||
| 80 | Magadan region | Pon.-Pon. 10.00.22.00 | |
| 81 | Sakhalin Region | ||
| 900 | |||
| 83 | Chukotka AO | Mon-Fri 09.00-22.00, closed 16.00-22.00 | |
Infographics. The principle of operation of a single federal helpline number for children, adolescents and their parents
Information from the regions about the work of the children's helpline
12/28/2016
What to do when there is a problem, but there is no one to tell about it?
12/28/2016
Online psychologists are ready to save children from bullying
12/28/2016
What problems do residents of the Irkutsk region call the helpline
09.1 for children1.2016
3
3
09.