Similarities between ocd and ocpd
OCPD vs OCD: What’s the Difference? Traits and Characteristics
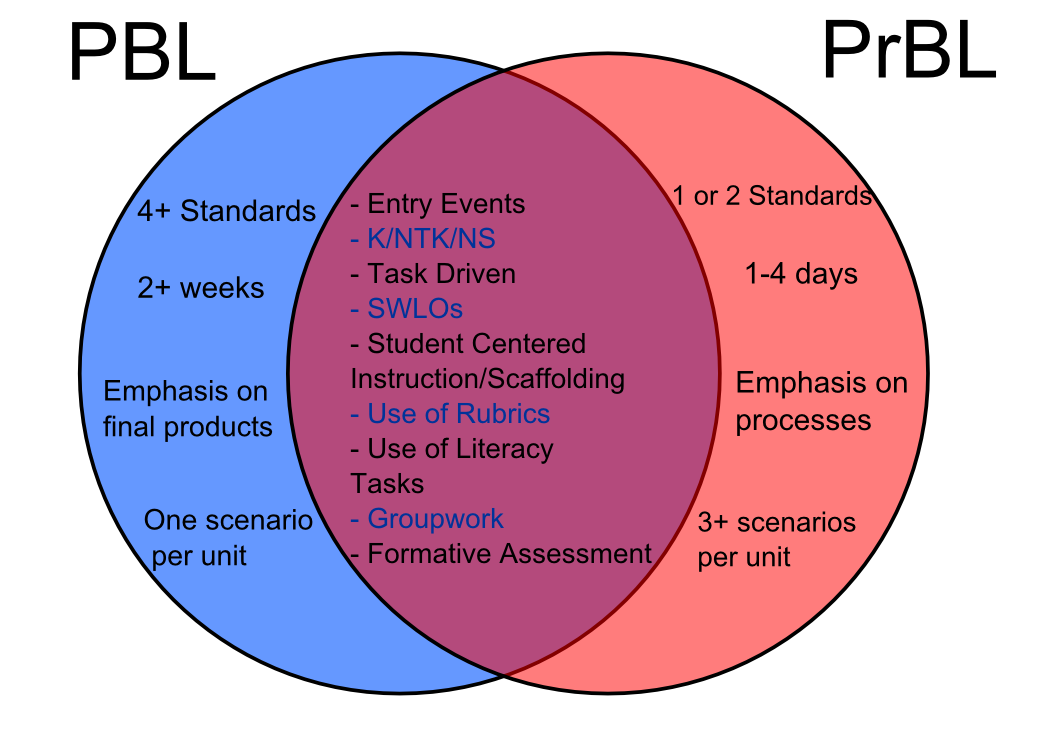
While obsessive-compulsive disorder (OCD) and obsessive-compulsive personality disorder (OCPD) share a similar name, these two mental health conditions have separate symptoms and treatment styles.
Article at a Glance:
Learning the difference between the two disorders is challenging. Remember these key OCPD vs. OCD points:
- OCPD is a personality disorder marked by perfectionism and a need for control
- OCD is characterized by obsessions and compulsions that take up a lot of time
- People with OCD are usually self-aware, but people with OCPD typically are not
- The prognosis is generally better for OCD than OCPD, but both conditions improve with treatment
- Treatment for both OCPD and OCD can involve psychotherapy:
- Exposure and Response Prevention helps OCD
- Talk therapy aimed at decreasing perfectionism and aiding relationships helps OCPD
What Is The Difference Between OCD and OCPD?
Though obsessive-compulsive personality disorder (OCPD) may sound like obsessive-compulsive disorder (OCD), it is not the same. Both conditions do, however, have a unique ability to create distress as these disorders interfere with a person’s thoughts, feelings actions.
For someone who has one of these disorders, learning the characteristics of and differences between OCPD vs. OCD can help them better understand their condition. With this knowledge, a person can find the best treatments available.
Characteristics of OCPD
As the name implies, OCPD is a personality disorder, which means the condition is more likely to be ingrained into a person’s life.
Typically, personality disorders:
- Last a long time with consistent symptoms
- Are challenging to treat
- Cause significant harm to the person and their relationships
- Start during the late teens or early twenties
Perhaps the most noteworthy characteristic of obsessive-compulsive personality disorder is perfectionism. Having OCPD means that a person has an intense need for perfection in themselves, their actions and the people around them.
Additional signs and symptoms of OCPD include:
- A strict focus on being organized, attention to detail and sticking to schedules
- A lack of leisure time due to being consumed with work
- Being inflexible about moral and ethics, or seeing situations in absolute terms
- Difficulty throwing away old and worthless items
- Being unable to let others help
- Hoarding money
- Being stubborn and set in their ways
- Perfectionism that stands in the way of happiness and healthy relationships
OCPD is generally more common than OCD, affecting 7.8% of both men and women.
OCD Traits and Characteristics
In contrast to OCPD, OCD is different in that it involves obsessions and compulsions that affect every part of a person’s life. Obsessions and compulsions are the hallmarks of OCD.
Obsessions are characterized by:
- Intense and unwanted thoughts that trigger stress and anxiety
- Thoughts a person tries to block with another idea or a behavior
Compulsions are characterized by:
- Behaviors a person feels driven to complete repetitively
- Behaviors completed that limit the presence of obsessions
The final significant symptom of OCD is spending large amounts of time during the day performing OCD rituals.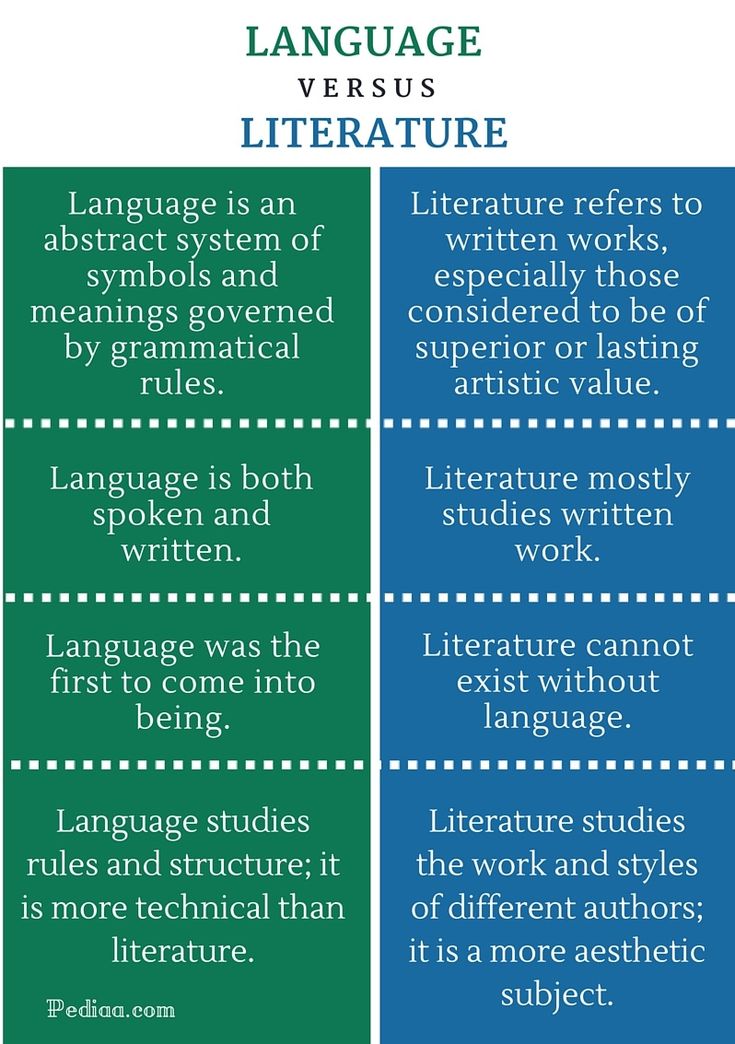 For example, needing five extra minutes to check the stove does not mean a person has OCD, but spending five hours in the shower might.
For example, needing five extra minutes to check the stove does not mean a person has OCD, but spending five hours in the shower might.
Beyond the presence of obsessions and compulsions, OCD can result in:
- High anxiety in all aspects of life
- Poor relationships
- Inability to maintain work or school commitments
- Increased depression
- Extreme discomfort when leaving home
Depending on a person’s condition, their OCD could cause additional repercussions. For example, if the person compulsively washes their hands, they could have dry, cracked skin.
Differentiating OCPD vs OCD Diagnosis
When determining if a person struggles with obsessive-compulsive personality disorder vs. obsessive-compulsive disorder, experts complete a thorough mental health evaluation using the guidelines for diagnosis in The Diagnostic and Statistical Manual of Mental Disorders, fifth (DSM-5). Professionals may also gather information from friends and family members to get a complete perspective.
Critical elements in differentiating OCPD vs. OCD are the obsessions and compulsions. A person with OCPD will have some rigid behaviors, but they will not engage in the overwhelming need for repetition linked to OCD compulsions.
Another basis for determining OCD vs. OCPD is the level of insight and self-awareness. Most often, a person is fully aware of OCD and the problems it causes, but OCPD is different. A person with OCPD usually believes their thoughts and behaviors are normal, and other people are the ones who need to change.
A mental health professional will also investigate the impact of the condition. Usually, OCD affects all aspects of life, making work, school or healthy relationships impossible. In contrast, OCPD could relate to improved performance at work or school, but relationships with other people are likely to suffer.
A person who is in a relationship with someone who has OCPD may feel:
- Like a disappointment
- Overly controlled or manipulated
- Frustrated and angry
Treatment Methods
People with OCD often see the need for treatment while people with OCPD don’t think it will be helpful. A person who has OCPD may encourage their loved ones to seek treatment instead of themselves.
A person who has OCPD may encourage their loved ones to seek treatment instead of themselves.
Due to a person’s lack of insight and self-awareness, obsessive compulsive personality disorder treatment may be more challenging than treatment for other conditions. The preferred treatment for OCPD is talk therapy.
Psychotherapy may focus on achieving short-term goals like:
- Reducing stress and learning relaxation techniques
- Improving healthy coping skills
- Building new relationships and strengthening existing ones
- Learning ways to communicate clearly and kindly
If someone responds well to these treatments, the therapy sessions can shift to a long-term treatment plan with a focus on reducing the feelings of perfectionism and their need for control. This form of treatment can be challenging and time-intensive, though.
Typically, OCD treatment follows another course. A form of cognitive-behavioral therapy called Exposure and Response Prevention aims to expose a person to obsessions while preventing their compulsions. If someone compulsively washes their hands, the therapist may encourage the person to touch something dirty without immediately washing. Their anxiety will rise initially but then fall with time, making the compulsion unnecessary.
If someone compulsively washes their hands, the therapist may encourage the person to touch something dirty without immediately washing. Their anxiety will rise initially but then fall with time, making the compulsion unnecessary.
When the compulsions end, the obsessions gradually diminish, making Exposure and Response Prevention an effective treatment.
A psychiatrist may offer medication to help reduce the symptoms of OCD as well. Medications paired with therapy seem to be the most successful treatment methods for OCD.
Conversely, medications are used less frequently with OCPD. If a doctor does prescribe them, it may only be in the short-term to address possible mood or anxiety issues.
Related Topic: Obsessive rumination disorder treatment
Prognosis
By seeking out effective, evidence-based treatments as soon as symptoms arise, a person can significantly improve the prognosis for either OCPD or OCD. One study of Exposure and Response Prevention shows that treatment can reduce OCD symptoms by between 65 and 50 percent after only 14 therapy sessions.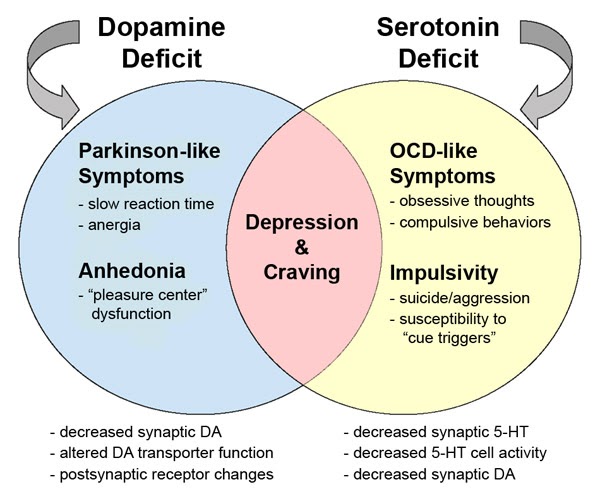 The benefits of talk therapy and counseling usually continue for months after treatment ends.
The benefits of talk therapy and counseling usually continue for months after treatment ends.
Like with other personality disorders, the outcome of OCPD treatments are less predictable. Although therapy can help a person reduce their need for perfectionism and control, the change takes time. In many cases, it takes an ultimatum from a boss or spouse for a person to accept the need for treatment and engage in the process.
With either OCPD or OCD, the presence of co-occurring conditions like depression, anxiety and substance use disorders can complicate treatment, resulting in a poorer prognosis. To find treatment for substance use and co-occurring mental health issues, contact The Recovery Village today.
Editor – Camille Renzoni
Cami Renzoni is a creative writer and editor for The Recovery Village. As an advocate for behavioral health, Cami is certified in mental health first aid and encourages people who face substance use disorders to ask for the help they deserve. Read more
Read more
Medically Reviewed By – Eric Patterson, LPC
Eric Patterson is a licensed professional counselor in the Pittsburgh area who is dedicated to helping children, adults, and families meet their treatment goals. Read more
American Psychiatric Association. “Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition.” Published in 2013. Accessed March 2019.
International OCD Foundation. “Exposure and Response Prevention (ERP).” (n.d.) Accessed March 2, 2019.
Jones, Mairwen K. et. al. “The Efficacy of Exposure and Response Pr[…]l Case Illustration.” US National Library of Medicine, National Institutes of Health, published in 2012. Accessed March 2, 2019.
National Institute of Mental Health. “Obsessive-Compulsive Disorder.” Published in January 2016. Accessed on March 2, 2019.
U.S. National Library of Medicine: MedLine Plus. “Obsessive-Compulsive Personality Disorder.” November 18, 2016. Accessed on March 2, 2019.
Van Noppen, Barbara. “Obsessive-Compulsive Personality Disorder (OCPD).” International OCD Foundation, 2010. Accessed on March 2, 2019.
“Obsessive-Compulsive Personality Disorder (OCPD).” International OCD Foundation, 2010. Accessed on March 2, 2019.
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
OCD vs. OCPD: What's the Difference?
Written by Amber Felton
Medically Reviewed by Poonam Sachdev on August 17, 2022
In this Article
- OCD vs. OCPD
- OCD Symptoms vs. OCPD Symptoms
- Diagnosing OCD vs. OCPD
- Differences Between OCPD and OCD
- OCD Treatment vs.
 OCPD Treatment
OCPD Treatment
You’ve probably heard of OCD or obsessive compulsive disorder. But have you heard of OCPD? OCPD, or obsessive compulsive personality disorder, shares some similarities to OCD, but there are also many differences between the two. Let’s compare OCD vs. OCPD.
OCD vs. OCPD
OCD is a mental health disorder characterized by excessive thoughts and repetitive behaviors. OCPD, on the other hand, is a personality disorder. Unlike a mental health disorder that may be short-term and treatable, a personality disorder is a lifelong disorder that disrupts thoughts, behavior, and mood. These issues can cause great distress to an individual.
OCD Symptoms vs. OCPD Symptoms
The characteristics of a person who has OCD come down to excessive and sometimes intrusive thoughts, images, and impulses. Some of the most common obsessions in OCD patients include:
- Contamination: Fear of contamination from body fluids, germs, household chemicals, and environmental pollutants
- Sexual: Unwanted sexual thoughts and mental images
- Violent: Excessive fear of harming oneself or someone else, or excessive mental images of violence or horror
- Religious: Obsessive concern regarding offending God or being damned
- Identity: Obsessive thoughts regarding sexual orientation or gender identity
- Responsibility: Fear of something terrible happening and being responsible or fear of causing harm to someone by not being careful enough
- Perfectionism: Fear of making mistakes and obsessive concern with being perfect
- Relationships: Excessive fear regarding one’s partner and the flaws and qualities of the partner
Compulsions in OCD include:
- Excessive washing and cleaning
- Repeating words or tasks
- Overchecking situations to make sure that you did not harm others
- Rearranging things until they feel right
- Counting while doing a task
- Praying to prevent harm
Symptoms specific to those with OCPD include:
- Obsessive devotion to work that affects other activities
- Obsessive fixation on rules, lists, and details that are minor
- The inability to finish tasks due to excessive perfectionism
- Obsession with moral and ethical codes
- Hoarding tendencies
Diagnosing OCD vs.
 OCPD
OCPDOCD has no tests available for diagnosing it in individuals. Instead, your health care professional will ask you a series of questions to make the diagnosis. These questions often relate to specific factors like obsessions and compulsions.
On the other hand, to receive an OCPD diagnosis, you must exhibit four or more symptoms out of the following eight signs:
- Perfectionism that limits finishing tasks
- Neglecting relationships due to a devotion to work
- Hoarding money for worst-case scenarios
- Obsessing over ethics, value, and morality
- Not wanting to assign tasks without a guarantee that those assigned will perform them exactly as asked
- Not wanting to part with worthless items
- A disposition that is stubborn or rigid
- Obsession with maintaining order by using lists, schedules, and rules
In addition to meeting at least four of the above symptoms, they must have been present in a long-term pattern that formed prior to early adulthood. The diagnosis of OCPD will involve a screening questionnaire, much like an OCD diagnosis. In this questionnaire, you will be required to report on your own behaviors throughout the year. Once the screening is complete, your health care professional will conduct an interview with you. They may also gather information from your family, friends, and peers.
The diagnosis of OCPD will involve a screening questionnaire, much like an OCD diagnosis. In this questionnaire, you will be required to report on your own behaviors throughout the year. Once the screening is complete, your health care professional will conduct an interview with you. They may also gather information from your family, friends, and peers.
A mental health professional will also need to rule out other similar disorders. They will want to make sure that you don't have OCD instead. Unfortunately, it can be difficult to tell OCD and OCPD apart. This may make you feel hesitant to seek help or a diagnosis if you suspect that you have OCPD. But it’s important to realize that receiving a formal diagnosis can help give you insight and a better understanding of yourself. It will also help you in moving forward.
Differences Between OCPD and OCD
The main difference between these two disorders is that OCD can develop later on in life from certain factors or events, whereas OCPD is a personality disorder that a person is born with.
Those with OCPD have a lot of the same symptoms. But what makes these two disorders different is the fact that individuals with OCPD often lack self-awareness. This means that they're more susceptible to acting on their impulses without realizing them and causing harm to themselves or those around them.
Another difference between OCD and OCPD patients is that people with OCD attempt to control specific factors to disengage their obsessions. On the other hand, people with OCPD usually like to control the whole situation at large.
There are also emotional differences between patients with OCD and OCPD. For example, those with OCD are more prone to feeling anxious, especially when things aren’t how they want them to be. People with OCPD are more susceptible to feelings of anger and rage instead.
Another stark difference between these two disorders is that people with OCD are often insecure about their obsessions and compulsions, whereas OCPD patients do their best to hide their insecurities not just from others but also from themselves.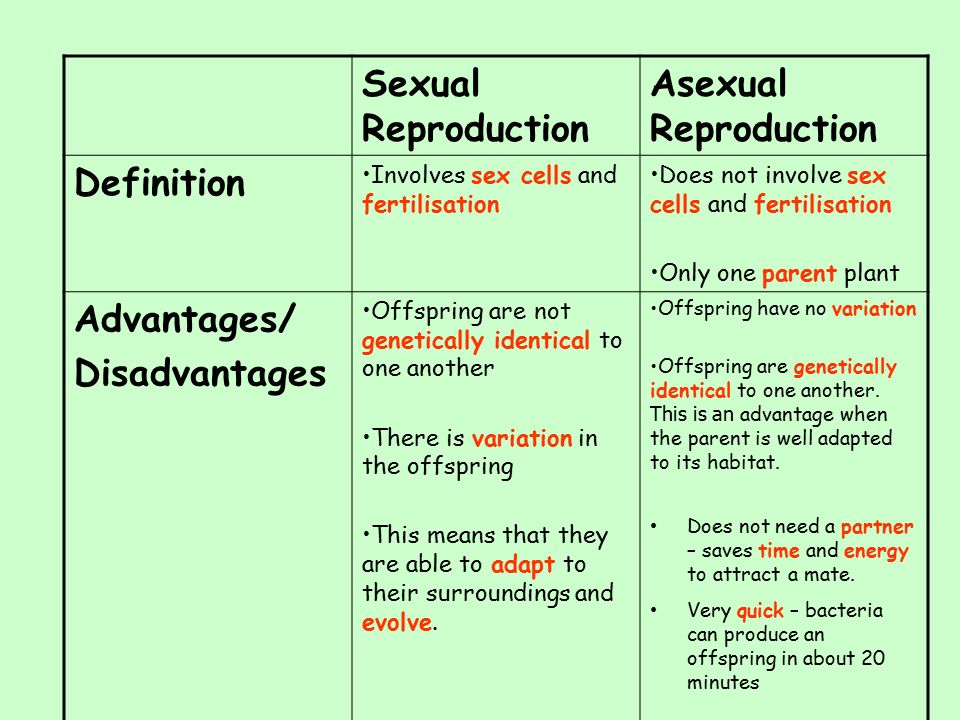
Lastly, OCD patients like to engage in compulsive behaviors and rituals, while OCPD patients prefer to plan and work.
OCD Treatment vs. OCPD Treatment
While these two disorders are distinct, there’s no denying that there’s also a significant link between the two, with similar symptoms. Treatment can be difficult, especially for those who have both disorders. With the co-occurrence of these disorders, the effects and symptoms of OCD are often amplified, leading to a higher rate of depression and alcohol consumption.
Additionally, those who have both OCD and OCPD seem not to respond well to cognitive behavioral therapy. They also don't respond well to exposure and ritual prevention. This could be due to OCPD patients' issues with commitment and trust. It can take time and patience to see results in the treatment of these two disorders.
Obsessive-compulsive disorder
A prominent role among mental illnesses is played by syndromes (complexes of symptoms), united in the group of obsessive-compulsive disorder (OCD), which received its name from the Latin terms obsessio and compulsio.
Obsession (lat. obsessio - taxation, siege, blockade).
Compulsions (lat. compello - I force). 1. Obsessive drives, a kind of obsessive phenomena (obsessions). Characterized by irresistible attraction that arises contrary to the mind, will, feelings. Often they are unacceptable to the patient, contrary to his moral and ethical properties. Unlike impulsive drives, compulsions are not realized. These drives are recognized by the patient as wrong and painfully experienced by them, especially since their very appearance, due to its incomprehensibility, often gives rise to a feeling of fear in the patient 2. The term compulsions is also used in a broader sense to refer to any obsessions in the motor sphere, including obsessive rituals.
In domestic psychiatry, obsessive states were understood as psychopathological phenomena, characterized by the fact that phenomena of a certain content repeatedly appear in the mind of the patient, accompanied by a painful feeling of coercion [Zinoviev PM, 193I]. For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account.
For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account. Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A.
Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A. M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
Currently, almost all obsessive-compulsive disorders are united in the International Classification of Diseases under the concept of "obsessive-compulsive disorder".
OKR concepts have undergone a fundamental reassessment over the past 15 years. During this time, the clinical and epidemiological significance of OCD has been completely revised. If it was previously thought that this is a rare condition observed in a small number of people, now it is known that OCD is common and causes a high percentage of morbidity, which requires the urgent attention of psychiatrists around the world. Parallel to this, our understanding of the etiology of OCD has broadened: the vaguely formulated psychoanalytic definition of the past two decades has been replaced by a neurochemical paradigm that explores the neurotransmitter disorders that underlie OCD.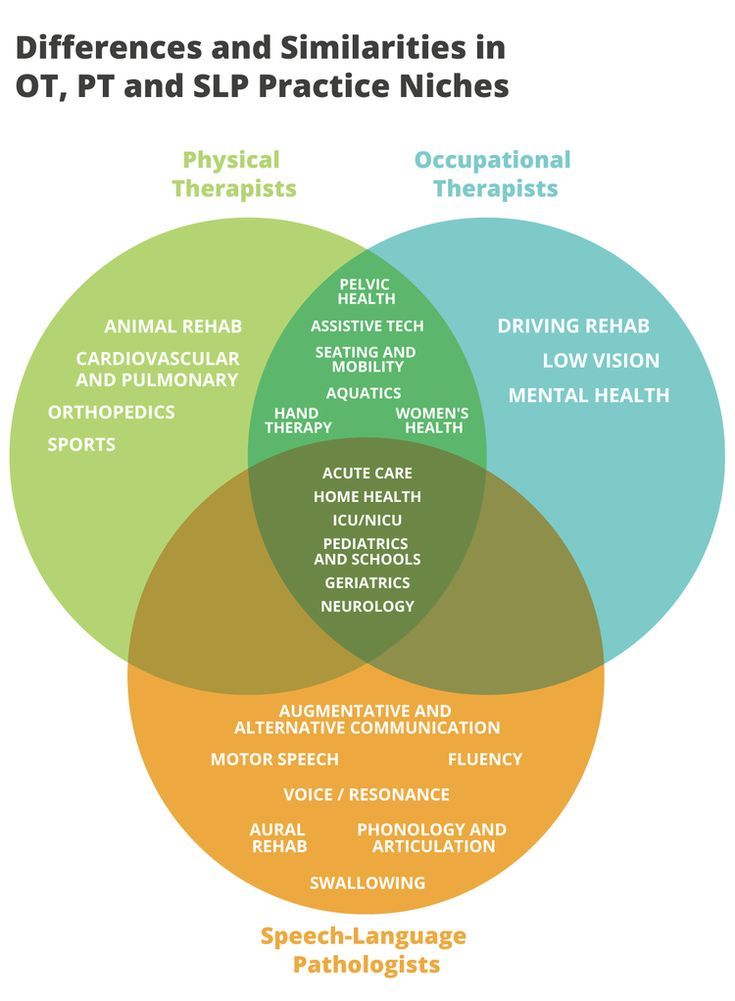 And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
The discovery that intense serotonin reuptake inhibition (SSRI) was the key to effective treatment for OCD was the first step in a revolution and spurred clinical research that showed the efficacy of such selective inhibitors.
As described in ICD-10, the main features of OCD are repetitive intrusive (obsessive) thoughts and compulsive actions (rituals).
In a broad sense, the core of OCD is the syndrome of obsession, which is a condition with a predominance in the clinical picture of feelings, thoughts, fears, memories that arise in addition to the desire of patients, but with awareness of their pain and a critical attitude towards them. Despite the understanding of the unnaturalness, illogicality of obsessions and states, patients are powerless in their attempts to overcome them. Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessions in the ICD-10 are included in the group of neurotic disorders.
The prevalence of OCD in the population is quite high. According to some data, it is determined by an indicator of 1.5% (meaning "fresh" cases of diseases) or 2-3%, if episodes of exacerbations observed throughout life are taken into account. Those suffering from obsessive-compulsive disorder make up 1% of all patients receiving treatment in psychiatric institutions. It is believed that men and women are affected approximately equally.
CLINICAL PICTURE
The problem of obsessive-compulsive disorders attracted the attention of clinicians already at the beginning of the 17th century. They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.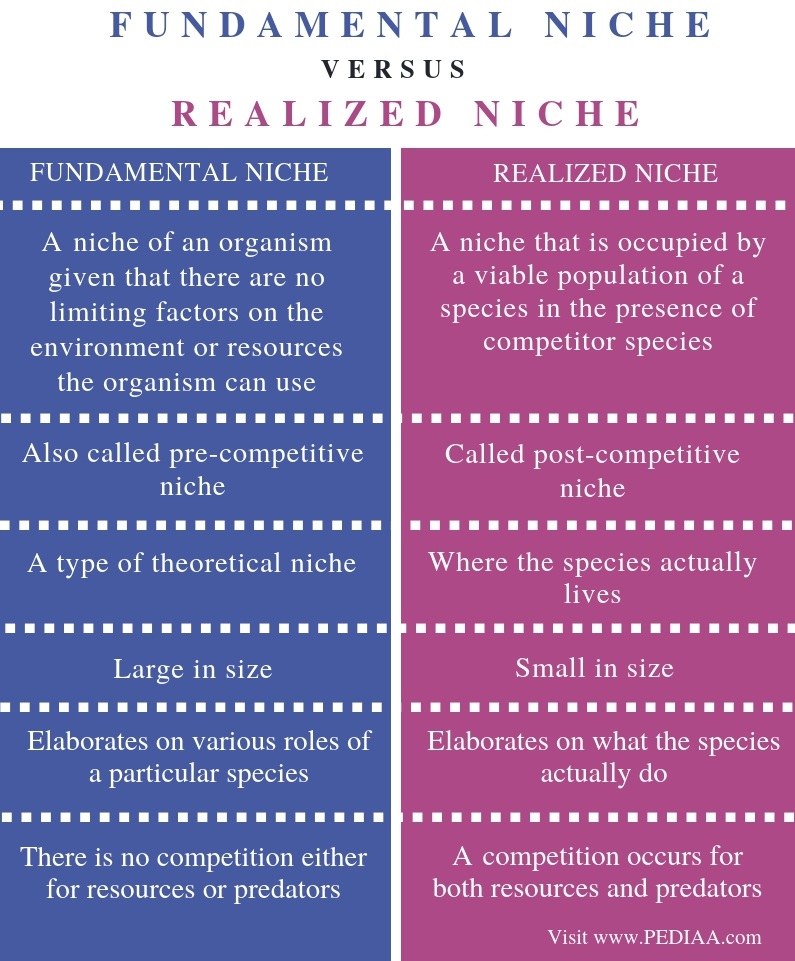
Main clinical manifestations of OCD:
Obsessional thoughts - painful, arising against the will, but recognized by the patient as their own, ideas, beliefs, images, which in a stereotyped form forcibly invade the patient's consciousness and which he tries to resist in some way. It is this combination of an inner sense of compulsive urge and efforts to resist it that characterizes obsessional symptoms, but of the two, the degree of effort exerted is the more variable. Obsessive thoughts may take the form of single words, phrases, or lines of poetry; they are usually unpleasant to the patient and may be obscene, blasphemous, or even shocking.
Obsessional imagery is vivid scenes, often violent or disgusting, including, for example, sexual perversion.
Obsessional impulses are urges to do things that are usually destructive, dangerous or shameful; for example, jumping into the road in front of a moving car, injuring a child, or shouting obscene words while in society.
Obsessional rituals include both mental activities (eg, counting repeatedly in a particular way, or repeating certain words) and repetitive but meaningless acts (eg, washing hands twenty or more times a day). Some of them have an understandable connection with the obsessive thoughts that preceded them, for example, repeated washing of hands - with thoughts of infection. Other rituals (for example, regularly laying out clothes in some complex system before putting them on) do not have such a connection. Some patients feel an irresistible urge to repeat such actions a certain number of times; if that fails, they are forced to start all over again. Patients are invariably aware that their rituals are illogical and usually try to hide them. Some fear that such symptoms are a sign of the onset of insanity. Both obsessive thoughts and rituals inevitably lead to problems in daily activities.
Obsessive rumination (“mental chewing gum”) is an internal debate in which the arguments for and against even the simplest everyday actions are endlessly revised. Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Compulsive actions - repetitive stereotypical actions, sometimes acquiring the character of protective rituals. The latter are aimed at preventing any objectively unlikely events that are dangerous for the patient or his relatives.
In addition to the above, in a number of obsessive-compulsive disorders, a number of well-defined symptom complexes stand out, and among them are obsessive doubts, contrasting obsessions, obsessive fears - phobias (from the Greek. phobos).
Obsessive thoughts and compulsive rituals may intensify in certain situations; for example, obsessive thoughts about harming other people often become more persistent in the kitchen or some other place where knives are kept. Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Obsessions (obsessions) are divided into figurative or sensual, accompanied by the development of affect (often painful) and obsessions of affectively neutral content.
Sensual obsessions include obsessive doubts, memories, ideas, drives, actions, fears, an obsessive feeling of antipathy, an obsessive fear of habitual actions.
Obsessive doubts - intrusively arising contrary to logic and reason, uncertainty about the correctness of committed and committed actions. The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
Obsessive memories include persistent, irresistible painful memories of any sad, unpleasant or shameful events for the patient, accompanied by a sense of shame, repentance. They dominate the mind of the patient, despite the efforts and efforts not to think about them.
Obsessive impulses - urges to commit one or another tough or extremely dangerous action, accompanied by a feeling of horror, fear, confusion with the inability to get rid of it. The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
Manifestations of obsessive ideas can be different. In some cases, this is a vivid "vision" of the results of obsessive drives, when patients imagine the result of a cruel act committed. In other cases, obsessive ideas, often referred to as mastering, appear in the form of implausible, sometimes absurd situations that patients take for real. An example of obsessive ideas is the patient's conviction that the buried relative was alive, and the patient painfully imagines and experiences the suffering of the deceased in the grave. At the height of obsessive ideas, the consciousness of their absurdity, implausibility disappears and, on the contrary, confidence in their reality appears. As a result, obsessions acquire the character of overvalued formations (dominant ideas that do not correspond to their true meaning), and sometimes delusions.
An obsessive feeling of antipathy (as well as obsessive blasphemous and blasphemous thoughts) - unjustified, driven away by the patient from himself antipathy towards a certain, often close person, cynical, unworthy thoughts and ideas in relation to respected people, in religious persons - in relation to saints or ministers churches.
Obsessive acts are acts done against the wishes of the sick, despite efforts made to restrain them. Some of the obsessive actions burden the patients until they are realized, others are not noticed by the patients themselves. Obsessive actions are painful for patients, especially in those cases when they become the object of attention of others.
Obsessive fears, or phobias, include an obsessive and senseless fear of heights, large streets, open or confined spaces, large crowds of people, the fear of sudden death, the fear of falling ill with one or another incurable disease. Some patients may develop a wide variety of phobias, sometimes acquiring the character of fear of everything (panphobia). And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
Hypochondriacal phobias (nosophobia) - an obsessive fear of some serious illness. Most often, cardio-, stroke-, syphilo- and AIDS phobias are observed, as well as the fear of the development of malignant tumors. At the peak of anxiety, patients sometimes lose their critical attitude to their condition - they turn to doctors of the appropriate profile, require examination and treatment. The implementation of hypochondriacal phobias occurs both in connection with psycho- and somatogenic (general non-mental illnesses) provocations, and spontaneously. As a rule, hypochondriacal neurosis develops as a result, accompanied by frequent visits to doctors and unreasonable medication.
Specific (isolated) phobias - obsessive fears limited to a strictly defined situation - fear of heights, nausea, thunderstorms, pets, treatment at the dentist, etc. Since contact with situations that cause fear is accompanied by intense anxiety, the patients tend to avoid them.
Obsessive fears are often accompanied by the development of rituals - actions that have the meaning of "magic" spells that are performed, despite the critical attitude of the patient to obsession, in order to protect against one or another imaginary misfortune: before starting any important business, the patient must perform some that specific action to eliminate the possibility of failure. Rituals can, for example, be expressed in snapping fingers, playing a melody to the patient or repeating certain phrases, etc. In these cases, even relatives are not aware of the existence of such disorders. Rituals, combined with obsessions, are a fairly stable system that usually exists for many years and even decades.
Obsessions of affectively neutral content - obsessive sophistication, obsessive counting, recalling neutral events, terms, formulations, etc. Despite their neutral content, they burden the patient, interfere with his intellectual activity.
Contrasting obsessions ("aggressive obsessions") - blasphemous, blasphemous thoughts, fear of harming oneself and others. Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc.
Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc. ). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
Obsessions of pollution (mysophobia). This group of obsessions includes both the fear of pollution (earth, dust, urine, feces and other impurities), as well as the fear of penetration into the body of harmful and toxic substances (cement, fertilizers, toxic waste), small objects (glass fragments, needles, specific types of dust), microorganisms. In some cases, the fear of contamination can be limited, remain at the preclinical level for many years, manifesting itself only in some features of personal hygiene (frequent change of linen, repeated washing of hands) or in housekeeping (thorough handling of food, daily washing of floors). , "taboo" on pets). This kind of monophobia does not significantly affect the quality of life and is evaluated by others as habits (exaggerated cleanliness, excessive disgust). Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.
Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease. In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
A special place in the series of obsessions is occupied by obsessive actions in the form of isolated, monosymptomatic movement disorders. Among them, especially in childhood, tics predominate, which, unlike organically conditioned involuntary movements, are much more complex motor acts that have lost their original meaning. Tics sometimes give the impression of exaggerated physiological movements. This is a kind of caricature of certain motor acts, natural gestures. Patients suffering from tics can shake their heads (as if checking whether the hat fits well), make hand movements (as if discarding interfering hair), blink their eyes (as if getting rid of a mote). Along with obsessive tics, pathological habitual actions (lip biting, gnashing of teeth, spitting, etc.) are often observed, which differ from obsessive actions proper in the absence of a subjectively painful sense of persistence and experience them as alien, painful. Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
The course of obsessive-compulsive disorder.
Unfortunately, chronization must be indicated as the most characteristic trend in the OCD dynamics. Cases of episodic manifestations of the disease and complete recovery are relatively rare. However, in many patients, especially with the development and preservation of one type of manifestation (agoraphobia, obsessive counting, ritual handwashing, etc.), a long-term stabilization of the condition is possible. In these cases, there is a gradual (usually in the second half of life) mitigation of psychopathological symptoms and social readaptation. For example, patients who experienced fear of traveling on certain types of transport, or public speaking, cease to feel flawed and work along with healthy people. In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
More severe and complex OCDs such as phobias of infection, pollution, sharp objects, contrasting performances, multiple rituals, on the other hand, may become persistent, resistant to treatment, or show a tendency to recur with disorders that persist despite active therapy. Further negative dynamics of these conditions indicates a gradual complication of the clinical picture of the disease as a whole.
DIFFERENTIAL DIAGNOSIS
It is important to distinguish OCD from other disorders that involve compulsions and rituals. In some cases, obsessive-compulsive disorder must be differentiated from schizophrenia, especially when the obsessive thoughts are unusual in content (eg, mixed sexual and blasphemous themes) or the rituals are exceptionally eccentric. The development of a sluggish schizophrenic process cannot be ruled out with the growth of ritual formations, their persistence, the emergence of antagonistic tendencies in mental activity (inconsistency of thinking and actions), and the uniformity of emotional manifestations. Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.
Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation. In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
Genetic factors
Speaking about hereditary predisposition to OCD, it should be noted that obsessive-compulsive disorders are found in approximately 5-7% of parents of patients with such disorders. Although this figure is low, it is higher than in the general population. While the evidence for a hereditary predisposition to OCD is still uncertain, psychasthenic personality traits can be largely explained by genetic factors.
FORECAST
Approximately two-thirds of OCD patients improve within a year, more often by the end of this period. If the disease lasts more than a year, fluctuations are observed during its course - periods of exacerbations are interspersed with periods of improvement in health, lasting from several months to several years. The prognosis is worse if we are talking about a psychasthenic personality with severe symptoms of the disease, or if there are continuous stressful events in the patient's life. Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
TREATMENT: BASIC METHODS AND APPROACHES
Despite the fact that OCD is a complex group of symptom complexes, the principles of treatment for them are the same. The most reliable and effective method of treating OCD is considered to be drug therapy, during which a strictly individual approach to each patient should be manifested, taking into account the characteristics of the manifestation of OCD, age, gender, and the presence of other diseases. In this regard, we must warn patients and their relatives against self-treatment. If any disorders similar to mental ones appear, it is necessary, first of all, to contact the specialists of the psycho-neurological dispensary at the place of residence or other psychiatric medical institutions to establish the correct diagnosis and prescribe competent adequate treatment. At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
When treating, it must be borne in mind that obsessive-compulsive disorders often have a fluctuating course with long periods of remission (improvement). The apparent suffering of the patient often seems to call for vigorous effective treatment, but the natural course of the condition must be kept in mind in order to avoid the typical error of over-intensive therapy. It is also important to consider that OCD is often accompanied by depression, the effective treatment of which often leads to an alleviation of obsessional symptoms.
The treatment of OCD begins with an explanation of the symptoms to the patient and, if necessary, with reassurance that they are the initial manifestation of insanity (a common concern for patients with obsessions). Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Drug therapy
The following therapeutic approaches exist for the currently identified types of OCD. Of the pharmacological drugs for OCD, serotonergic antidepressants, anxiolytics (mainly benzodiazepine), beta-blockers (to stop autonomic manifestations), MAO inhibitors (reversible) and triazole benzodiazepines (alprazolam) are most often used. Anxiolytic drugs provide some short-term relief of symptoms, but should not be given for more than a few weeks at a time. If anxiolytic treatment is required for more than one to two months, small doses of tricyclic antidepressants or small antipsychotics sometimes help. The main link in the treatment regimen for OCD, overlapping with negative symptoms or ritualized obsessions, are atypical antipsychotics - risperidone, olanzapine, quetiapine, in combination with either SSRI antidepressants or other antidepressants - moclobemide, tianeptine, or with high-potency benzodiazepine derivatives ( alprazolam, clonazepam, bromazepam).
Any comorbid depressive disorder is treated with antidepressants at an adequate dose. There is evidence that one of the tricyclic antidepressants, clomipramine, has a specific effect on obsessive symptoms, but the results of a controlled clinical trial showed that the effect of this drug is insignificant and occurs only in patients with distinct depressive symptoms.
In cases where obsessive-phobic symptoms are observed within the framework of schizophrenia, intensive psychopharmacotherapy with proportional use of high doses of serotonergic antidepressants (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram) has the greatest effect. In some cases, it is advisable to connect traditional antipsychotics (small doses of haloperidol, trifluoperazine, fluanxol) and parenteral administration of benzodiazepine derivatives.
Psychotherapy
Behavioral psychotherapy
One of the main tasks of the specialist in the treatment of OCD is to establish fruitful cooperation with the patient. It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.
It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy. In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
Social rehabilitation
We have already noted that obsessive-compulsive disorder has a fluctuating (fluctuating) course and over time the patient's condition may improve regardless of which particular methods of treatment were used. Until recovery, patients can benefit from supportive conversations that provide continued hope for recovery. Psychotherapy in the complex of treatment and rehabilitation measures for patients with OCD is aimed at both correcting avoidant behavior and reducing sensitivity to phobic situations (behavioral therapy), as well as family psychotherapy to correct behavioral disorders and improve family relationships.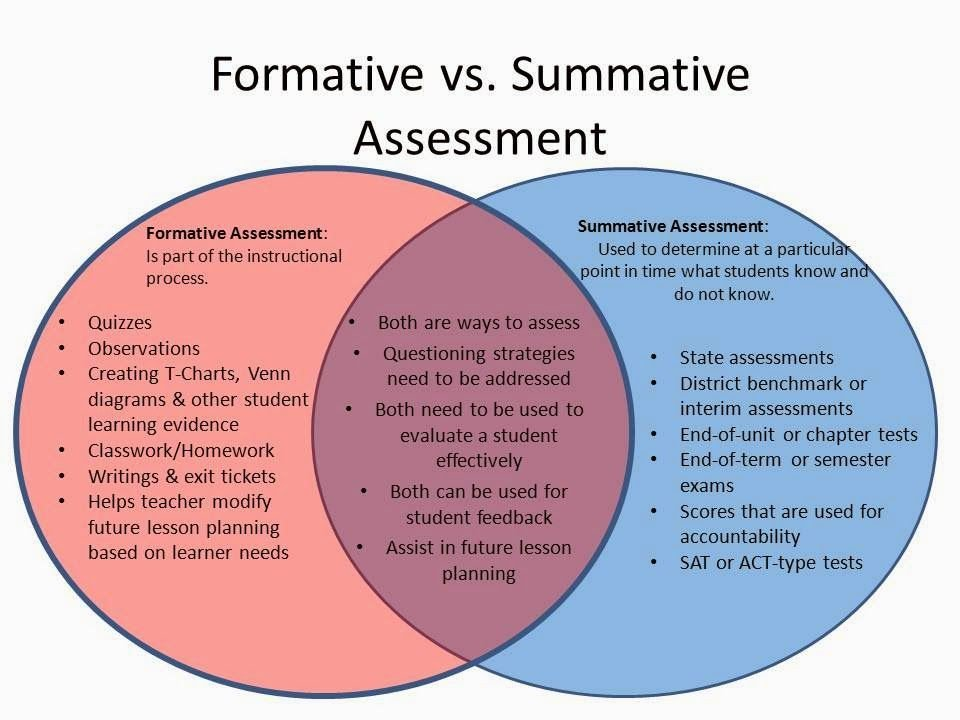 If marital problems exacerbate symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.
If marital problems exacerbate symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.
All of these methods, when used judiciously, can increase the effectiveness of drug therapy, but are not capable of completely replacing drugs. It should be noted that explanatory psychotherapy does not always help, and some patients with OCD even worsen because such procedures encourage them to think painfully and unproductively about the subjects discussed in the course of treatment. Unfortunately, science still does not know how to cure mental illness once and for all. OCD often has a tendency to recur, which requires long-term prophylactic medication.
FGBNU NTsPZ. Dissertations. Masikhina Svetlana Nikolaevna. Schizophrenia with obsessive-compulsive disorders in childhood (clinical typology, dynamics, principles of therapy).
Masikhina Svetlana Nikolaevna
Schizophrenia with obsessive-compulsive disorders in childhood
(clinical typology, dynamics, principles of therapy)
Abstract of the dissertation for the degree of candidate of medical sciences
GENERAL CHARACTERISTICS OF THE WORK
Relevance of the study.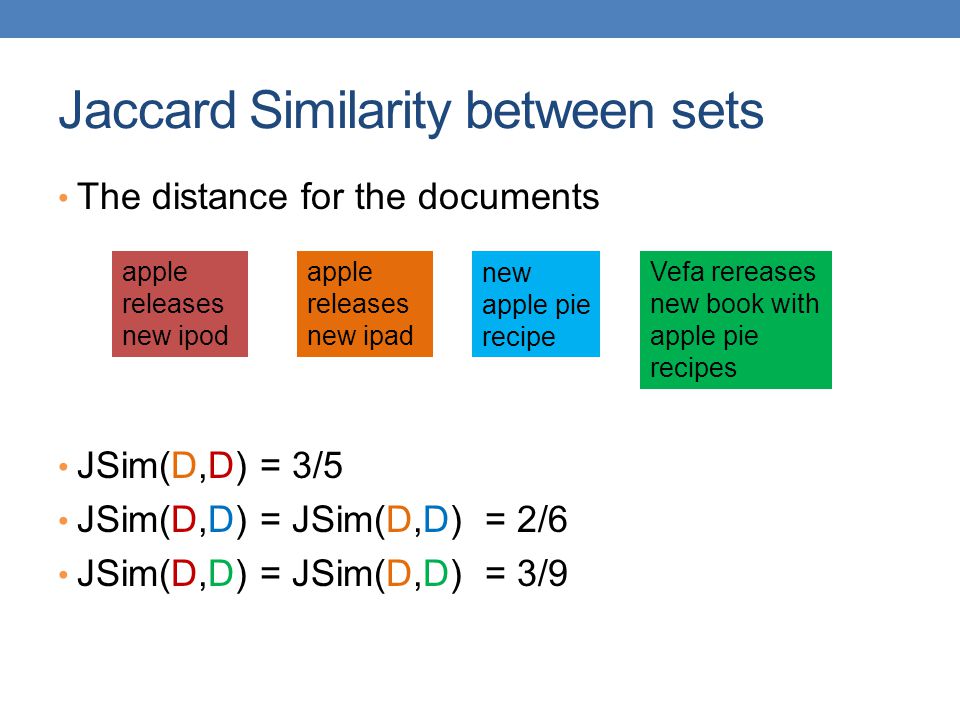
Despite many years of experience in clinical research, the problem of therapy, rehabilitation and assessment of the adaptive capabilities of children suffering from obsessive-compulsive disorders (OCD) still exists. The chronic course and low curability of OCD in childhood are often due to the fact that OCD acts as one of the manifestations of the schizophrenic process (Bleuler E. 1920, Kameneva E.N. 1954, Simson T.P., Deglin V.R., Kudryavtseva V.P. 1954, Sukhareva G.E. 1955, Rosen I. 1957, Bender L. 1966, Zohar A. 1998). In this regard, both early diagnosis of the endogenous procedural nature of OCD and a holistic clinical assessment of the psychopathological syndrome, the structure of which determines the choice of adequate therapeutic tactics, are relevant.
The psychopathological and ontogenetic features of OCD, which form in the structure of the schizophrenic process, have been considered in sufficient detail within the framework of various clinical approaches. The problem was covered in works on low-progressive neurosis-like schizophrenia (Vrono M.Sh. 1971, Kashnikova A.A. 1973, Kalinina M.A. 1973) and in studies of the initial stage of paranoid schizophrenia (Simson T.P. 1948, Tsivilko M.A. 1967), in foreign child psychiatry a form of childhood schizophrenia is described with a picture of panneurosis F (Bender L. 1966). In recent years, studies have become widespread (including on children's cohorts) within the concept of the obsessive-compulsive spectrum (Rapoport J. 1998), as well as studies of the comorbidity of OCD and symptoms of schizophrenia (Geller D. 1996).
The problem was covered in works on low-progressive neurosis-like schizophrenia (Vrono M.Sh. 1971, Kashnikova A.A. 1973, Kalinina M.A. 1973) and in studies of the initial stage of paranoid schizophrenia (Simson T.P. 1948, Tsivilko M.A. 1967), in foreign child psychiatry a form of childhood schizophrenia is described with a picture of panneurosis F (Bender L. 1966). In recent years, studies have become widespread (including on children's cohorts) within the concept of the obsessive-compulsive spectrum (Rapoport J. 1998), as well as studies of the comorbidity of OCD and symptoms of schizophrenia (Geller D. 1996).
Clinical systematization of conditions with a predominance of OCD in the picture of childhood schizophrenia show that both productive (Lebovici S. 1985, Kalinina M.A. 1993, Geller D. 1996, etc.) and negative psychopathological ones can be present in the structure of a complex OCD symptom complex. disorders - mainly at the remote stages of the dynamics of the schizophrenic process (Danilova M. B. 1966, Shurkute A.A. 1987, Fenton & McGlashan 1986, Berman I. 1995, Zohar A. 1997, Smulevich A.B. et al. 1999). There are data on the relationship of endogenous procedural OCD with non-psychotic disorders - affective disorders and anxiety-phobic disorders (Lebovici S. 1985, Kalinina M.A. 1993, Geller D. 1996, etc.), as well as the possible transformation of OCD into side of disorders of the paranoid register (Skanavi E.E. 1954, Golovan L.I. 1965, Zavidovskaya G.I. 1971, Vrono M.Sh. 1971, Lebovici S. 1985, Insel T. 1986 etc.).
B. 1966, Shurkute A.A. 1987, Fenton & McGlashan 1986, Berman I. 1995, Zohar A. 1997, Smulevich A.B. et al. 1999). There are data on the relationship of endogenous procedural OCD with non-psychotic disorders - affective disorders and anxiety-phobic disorders (Lebovici S. 1985, Kalinina M.A. 1993, Geller D. 1996, etc.), as well as the possible transformation of OCD into side of disorders of the paranoid register (Skanavi E.E. 1954, Golovan L.I. 1965, Zavidovskaya G.I. 1971, Vrono M.Sh. 1971, Lebovici S. 1985, Insel T. 1986 etc.).
Follow-up studies of the outcomes of childhood schizophrenia with OCD have shown that it is possible to form a defect, the manifestations of which can vary from gradually increasing shallow personality changes to severe deficient disorders close to final states (Sukhareva G.E. 1935, Vrono M.Sh. 1971, yoryeva O.P. 1970 and others). Along with the description of a relatively favorable course of the schizophrenic process that began in childhood with a predominance of OCD, the dynamics of which does not lead to the formation of deep negative changes (Kameneva E. N. 1954, Bender L. 1966, yoryeva O.P. 1970), there are ideas about the Disabling F the nature of childhood schizophrenia with OCD (Fenton & McGlashan 1986, Berman I. 1995, Zohar A. 1997) without a well-defined distinction between clinical factors influencing the outcome of the disease.
N. 1954, Bender L. 1966, yoryeva O.P. 1970), there are ideas about the Disabling F the nature of childhood schizophrenia with OCD (Fenton & McGlashan 1986, Berman I. 1995, Zohar A. 1997) without a well-defined distinction between clinical factors influencing the outcome of the disease.
Thus, it is clear that a heterogeneous group of conditions with a predominance of OCD, developing in the clinical picture of the schizophrenic process in childhood, is of research interest. To date, the influence of the characteristics of an early-onset schizophrenic process on the structure of OCD and the prognosis of the disease has not been sufficiently studied, the relationship between OCD and various types of deficient disorders remains poorly understood, and the issues of therapy and rehabilitation of patients are topical. Evidence of successful psychopharmacological use of highly selective 5-HT2 receptor-selective serotonin reuptake inhibitor (SSRI) antidepressants, atypical antipsychotics, in the treatment of schizophrenia with OCD (Patel B.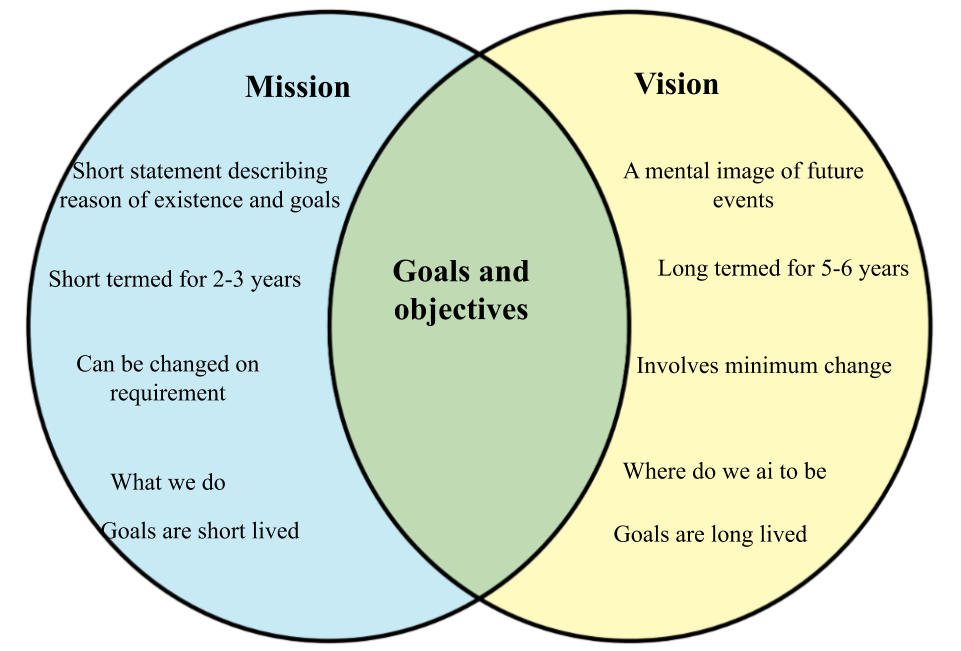 1993, Rasmussen S. 1997, McDougle 1995) provide grounds for an additional biochemical study of the homeostasis of the serotonin system in the studied group of conditions.
1993, Rasmussen S. 1997, McDougle 1995) provide grounds for an additional biochemical study of the homeostasis of the serotonin system in the studied group of conditions.
Purpose and objectives of the study.
The purpose of this study was to analyze the clinical and dynamic structure of OCD, taking into account the characteristics of the schizophrenic process that manifests itself in childhood. According to the set goal, the following tasks were solved in the work:
1. - clarification of the general patterns of the clinical dynamics of the schizophrenic process with a predominance of OCD in childhood;
2. - typological differentiation of OCD in the structure of schizophrenia in childhood on the basis of established features of the pre-manifest period, progression and course of the schizophrenic process, predominant syndromic relationships and various types of deficient changes;
3. - comparison of biochemical parameters of the serotoninergic system with clinical manifestations of OCD in the structure of schizophrenia manifesting in childhood, using a model for studying the level of immunoreactive serotonin transporter protein (IR-SERT) on platelet membranes;
4. - optimization of therapeutic measures in accordance with the data obtained in the study.
- optimization of therapeutic measures in accordance with the data obtained in the study.
Material and research methods.
The study was conducted from 1998 to 2001. on the basis of the Department for the Study of Problems of Child Psychiatry with a group for the study of child autism at the NTSPZ RAMS (Head of the Clinical Department, Doctor of Medical Sciences I.A. Kozlova).
The material included in the study was selected from the contingent of children who consulted in the outpatient department of the National Center for Health Care of the Russian Academy of Medical Sciences and, depending on the severity of the condition, were hospitalized in the children's department of the National Center for Health Care of the Russian Academy of Medical Sciences. When selecting patients, the ICD-10 diagnostic criteria for obsessive-compulsive disorder (F 42), schizophrenia (children's type) (F 20.83) and neurosis-like schizophrenia (F 21.3) were used. Patients were followed up for 3 years, which made it possible to establish the signs and rate of progression, to assess the type of course of the schizophrenic process.
The study did not include patients with malignant early-onset schizophrenia, current organic CNS disease, and severe somatic pathology.
The study sample consisted of 60 patients (47 boys, 13 girls) with the diagnoses of schizophrenia (children's type) F (SDT) (39 cases) and uneurosis-like schizophrenia F (NS) (21 cases) verified during follow-up. In the clinical picture of the disease of selected patients, persistent manifestations of OCD were detected. The duration of the disease since the onset of the first clinical signs of OCD ranged from 1 to 5 years (average 2.7 + _ 2.6 years). The age of patients included in the study was limited to the interval from 7 to 15 years (mean age 13.8 +_2.1 years).
The structure of psychopathological syndromes and their dynamics in the observations classified as NS diagnostic category reflected the patterns of the course of the schizophrenic process with a gradual onset and a slight rate of progression. The diagnosis of NS was established according to the clinical signs necessary for the diagnosis of a sluggish schizophrenic process (Smulevich A. B., 1987), taking into account the peculiarities of the manifestation of the disease in childhood (Sukhareva G.E., 1959, Yeryeva O.P. 1970): -retrospective detection of schizotypal dysontogenesis in the pre-manifest period; - clinically outlined manifestation of OCD during periods of age-related crises; - the presence of OCD during the course of the disease as a leading symptom; - identification in the mental status of patients of rudimentary disorders that are preferable for the schizophrenic process; - identification of deficient symptoms and its dynamics in the form of an increase in the features of disharmonic personal development without signs of mental retardation.
B., 1987), taking into account the peculiarities of the manifestation of the disease in childhood (Sukhareva G.E., 1959, Yeryeva O.P. 1970): -retrospective detection of schizotypal dysontogenesis in the pre-manifest period; - clinically outlined manifestation of OCD during periods of age-related crises; - the presence of OCD during the course of the disease as a leading symptom; - identification in the mental status of patients of rudimentary disorders that are preferable for the schizophrenic process; - identification of deficient symptoms and its dynamics in the form of an increase in the features of disharmonic personal development without signs of mental retardation.
The diagnostic category of CWD included patients whose mental status included, along with OCD, psychopathological phenomena of the psychotic register, or signs of dissociated mental retardation were determined (Kozlova I.A. 1999).
The study was conducted by clinical and follow-up methods, with a summary of both retrospective and prospective clinical characteristics of the patients' condition.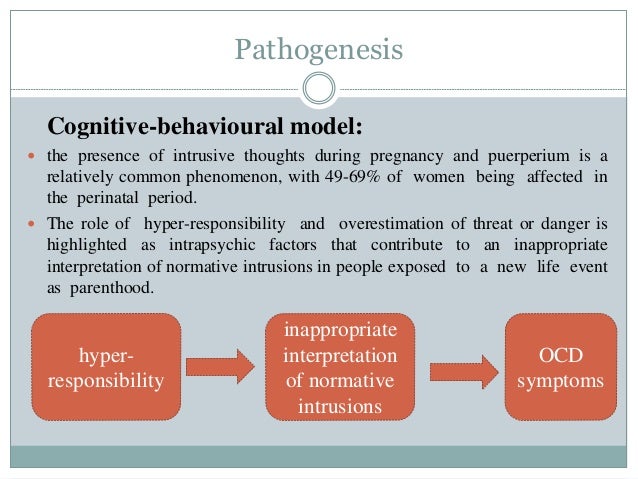 The data for each patient were recorded in the protocol, in the content of which the clinical parameters standardized within the framework of the study were presented. In order to unify the description of OCD symptoms, the Standard Clinical Scale for Obsessive-Compulsive Disorders (Children's Version) (CY-BOCS; Goodman W., 19) was used.86; Hardin M., 1991). According to the results of linear regression analysis, statistically significant correlations of standardized clinical parameters were revealed. The data of statistical analysis confirmed and supplemented the results obtained in the course of clinical and dynamic observation of patients and were the basis for the proposed typological differentiation.
The data for each patient were recorded in the protocol, in the content of which the clinical parameters standardized within the framework of the study were presented. In order to unify the description of OCD symptoms, the Standard Clinical Scale for Obsessive-Compulsive Disorders (Children's Version) (CY-BOCS; Goodman W., 19) was used.86; Hardin M., 1991). According to the results of linear regression analysis, statistically significant correlations of standardized clinical parameters were revealed. The data of statistical analysis confirmed and supplemented the results obtained in the course of clinical and dynamic observation of patients and were the basis for the proposed typological differentiation.
Additionally, the functional state of the serotonergic system of patients was assessed. The biochemical study was carried out by the staff of the Laboratory of Clinical Biochemistry of the Scientific Center for Health Care of the Russian Academy of Medical Sciences (head of the laboratory - Candidate of Medical Sciences Brusov O. S.).
S.).
Platelet membranes were used as a model of the presynaptic terminal and serotonergic synapse of the brain. An associative study of the level of IR-SERT was carried out using site-specific antibodies (according to the method of Qian Y. et al. 1995).
The biochemical study included 11 patients of the surveyed sample (4 observations - SDT, 7 observations - NSH, mean age 12.3 +_2.5), of which 7 - at the time of the study of the IR-SERT level, were in a state of clinical exacerbation of symptoms of the schizophrenic process with OCD, 3 - in a state of therapeutic remission, 1 - in a state of clinical remission. The control group was represented by 32 mentally healthy donors.
Patients were assessed using the CY-BOCS and the Positive and Negative Disorder Scale for Schizophrenia (PANSS) (Kay S.R. 1987). The scaling data were recorded in the study protocols.
Statistical processing of the obtained results was carried out using computer programs Excel, Version 7.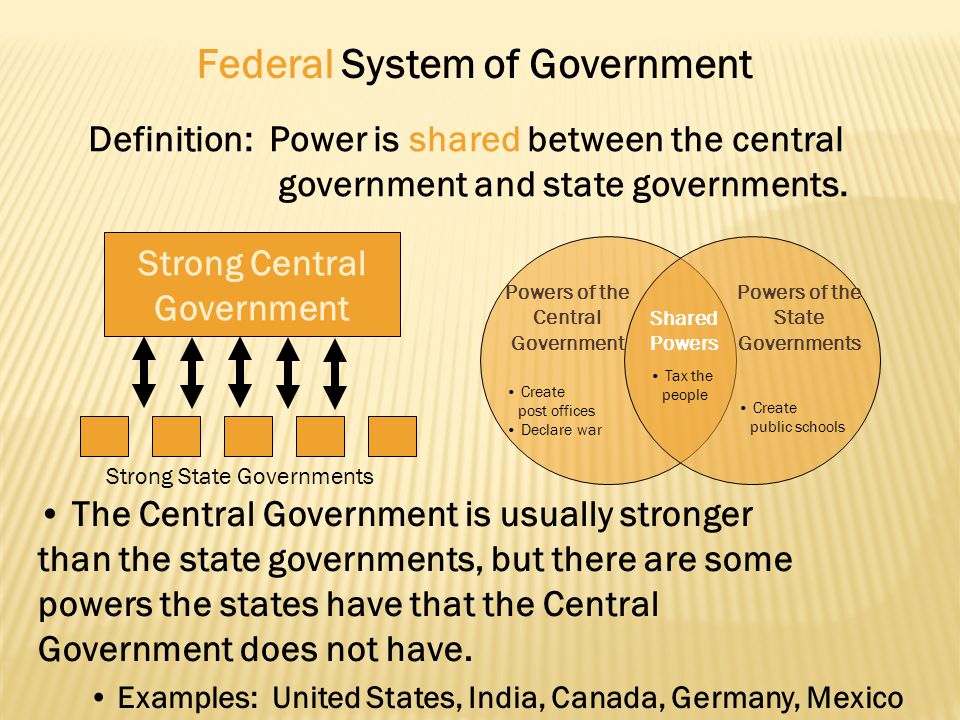 00., Statistic Demo.
00., Statistic Demo.
Scientific novelty.
The study, conducted on a representative clinical material, provides a number of new data on the features of the clinical structure of OCD in the picture of schizophrenia that manifests itself in childhood. Taking into account the data confirmed by the results of statistical analysis, for the first time, clinical types of conditions with a predominance of OCD in the picture of the schizophrenic process in childhood were identified: type 1 - OCD associated with disorders of the affective and neurosis-like registers, type 2 - OCD associated with disorders of the paranoid register, type 3 type - OCD associated with inert affective and negative disorders.
The presented typology allows predicting the further nature of the course of the disease, the level of emerging negative changes, differentiating therapeutic tactics and adequately assessing the adaptive capabilities of patients.
For the first time, data were obtained on the % content of IR-SERT (relative to control) in children with schizophrenia with OCD. The revealed correlations between clinical parameters and the level of IR-SERT may confirm the assumptions about the involvement of the serotonin system in the pathogenesis of schizophrenia with OCD in children. This allows us to supplement the rationale for the widespread use of psychotropic drugs that are highly selective for the serotonin system (SSRIs, atypical antipsychotics).
The revealed correlations between clinical parameters and the level of IR-SERT may confirm the assumptions about the involvement of the serotonin system in the pathogenesis of schizophrenia with OCD in children. This allows us to supplement the rationale for the widespread use of psychotropic drugs that are highly selective for the serotonin system (SSRIs, atypical antipsychotics).
Practical significance of the study.
The data presented in the dissertation work allow to obtain a number of information about the nature and intensity of the schizophrenic process based on structural typology, to determine the clinical and social prognosis in the provision of specialized psychiatric care to children suffering from schizophrenia with OCD.
The results of the study make it possible to optimize therapeutic measures aimed at reducing painful manifestations.
Quantitative assessment of the level of IR-SERT on platelet membranes of patients with OCD in the framework of the schizophrenic process that manifests itself in childhood can be used as a putative marker of the severity of the condition at admission and during treatment.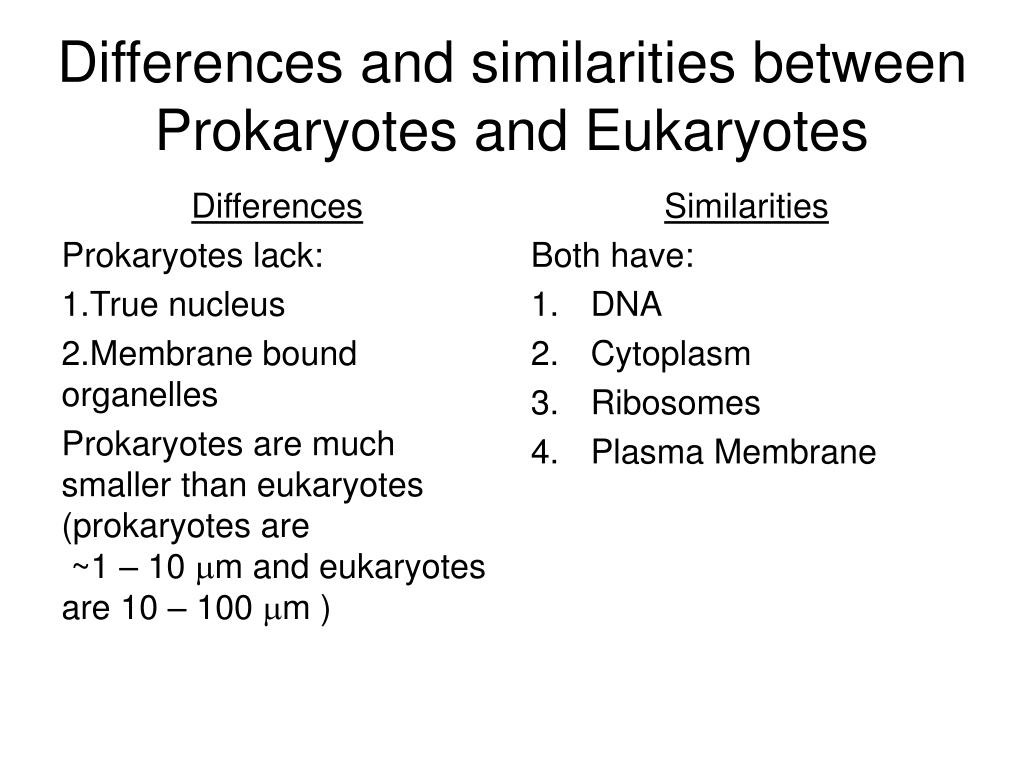
Approbation of work.
The results of the dissertation work were presented in the form of reports at the Conference of young scientists in memory of A.V. Snezhnevsky F, held at the NTsPZ RAMS (June 2000), at the VII National Congress of Humans and Drugs (Moscow, April 2000). The dissertation was approved at the interdepartmental scientific conference of the National Center for Health Sciences of the Russian Academy of Medical Sciences on May 31, 2001.
Publications on the topic of the dissertation.
Based on the dissertation materials, 8 papers were published, including in the Uzhurnal Neurologii i Psychiatry im. KorsakovaF. The list of publications is given at the end of the abstract.
Scope and structure of work.
The dissertation is presented on .E pages of typewritten text and contains an introduction, 6 chapters: -review of the literature on the research topic, -characterization of the research material and methods, -general patterns of clinical dynamics of OCD in the structure of the schizophrenic process in childhood, -clinical typology of conditions with the predominance of OCD in the structure of schizophrenia manifesting in childhood, -biochemical analysis of the state of the serotonin system in patients with schizophrenia with OCD manifesting in childhood, -principles of therapy; conclusion, conclusions, bibliographic index - 170 sources (of which 67 are domestic, 103 are foreign).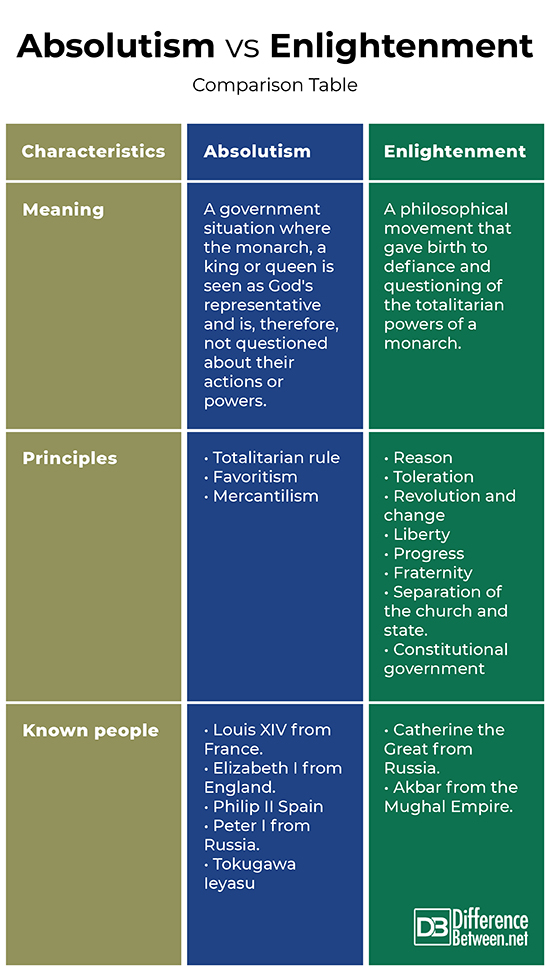 The application contains 4 tables, 7 figures.
The application contains 4 tables, 7 figures.
RESULTS OF THE STUDY
As a result of clinical, dynamic and statistical analysis of the data obtained for the studied group of patients, it was found that the structure of OCD syndromic relationships is determined by the characteristics of the schizophrenic process: the level of negative disorders formed in the pre-manifest period, the rate of progression and the type course of the schizophrenic process.
Clinical picture of the pre-manifest period, which combines premorbids that are difficult to distinguish in childhood and the initial stage of the disease (Eryeva O.P. 1970), the studied patients were heterogeneous. The main stereotypes of the development of the disease at the pre-manifest stage were characterized by: - schizotypal dysontogenesis with conditionally reactive neurosis-like episodes; - schizotypic dysontogenesis with autochthonous psychopathological disorders; -progredient schizotypal dysontogenesis.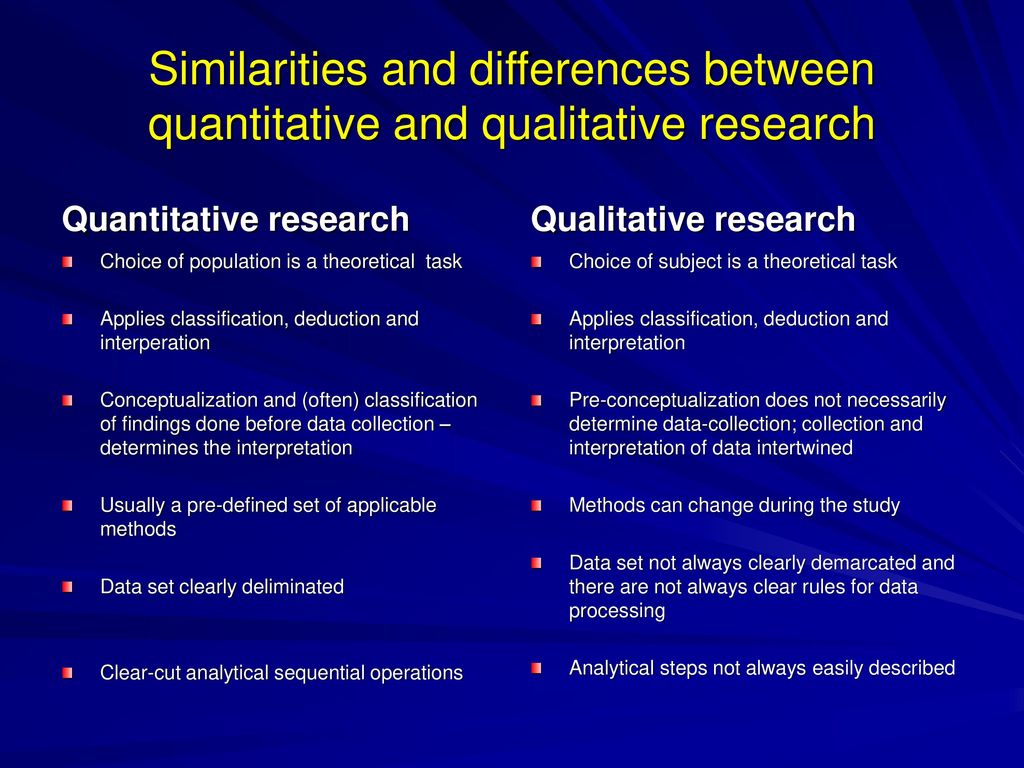
Conditionally reactive states that developed after psycho- or somatogeny were short-lived, their structure included erased depressive disorders, transient neurosis-like disorders, transient symptoms of logoneurosis, psychosomatic disorders in the form of vegetative-vascular disorders, neurosis-like enuresis. Yoti states were formed against the background of a distorted schizotypal type of personal development with features of sensitivity, disharmonic infantilism.
Autochthonous psychopathological disorders (affective, hyperdynamic disorders, pathological fantasizing, episodes of night terrors) were detected from an early period of development, were of an erased nature and did not lead to decompensation. Presumably, in a number of cases, such conditions developed after early episodes with an undeveloped psychopathological picture, described in the literature as Umicroepisodes F (Kameneva E.N., 1959, Kozlova I.A. 1967), Worn fur coats F (Vrono M.Sh. 1971), Uforpost syndromes (Asperger H.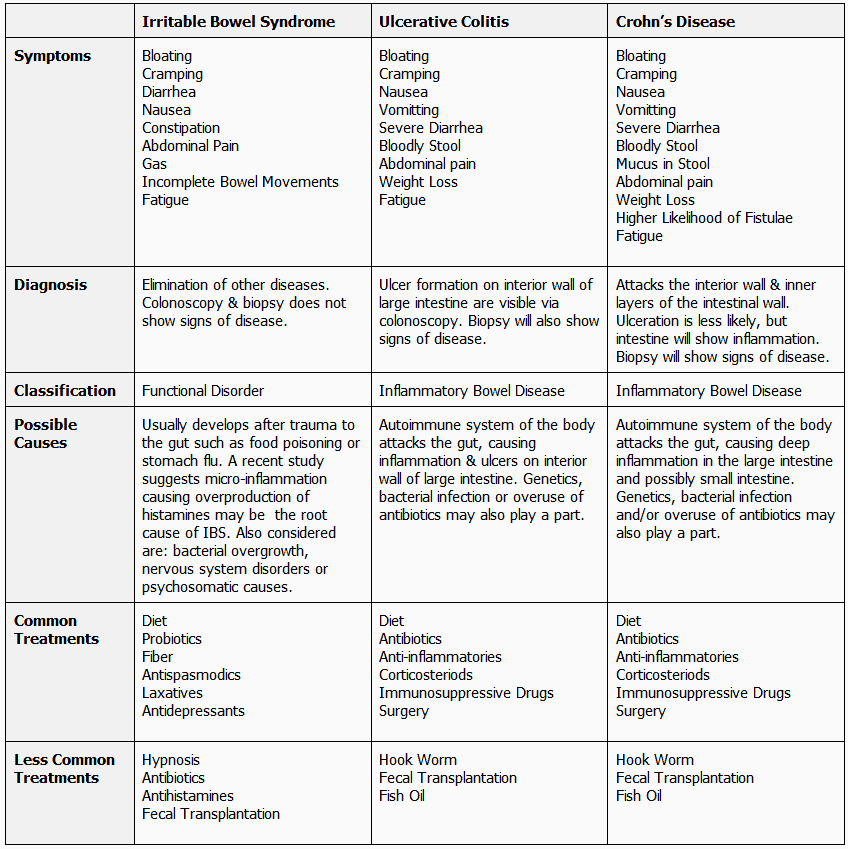 , 1961). Within the framework of these pre-manifest states, a development distorted by the schizotypal type was formed without signs of delay, which indicated the stabilization of the pathological process at a certain stage and a relatively favorable course of the disease.
, 1961). Within the framework of these pre-manifest states, a development distorted by the schizotypal type was formed without signs of delay, which indicated the stabilization of the pathological process at a certain stage and a relatively favorable course of the disease.
In the picture of progressive schizotypal dysontogenesis, along with dissociation, signs of mental retardation were revealed. The formation of such states can be associated with the stage of negative schizophrenia, preceding the appearance of outlined seizures in which productive symptoms appear, which is often characteristic of the dynamics of the schizophrenic process that manifests itself in childhood (Sukhareva G.E. 1935, Vrono M.Sh. 1971).
During the period of clinical manifestation, the symptoms of OCD acted in the structure of complex symptom complexes and persisted in the further dynamics of the disease as a leading symptom, aggravated in repeated attacks, or persisting within the framework of a continuous course of sluggish and approaching paranoid (Kozlova I.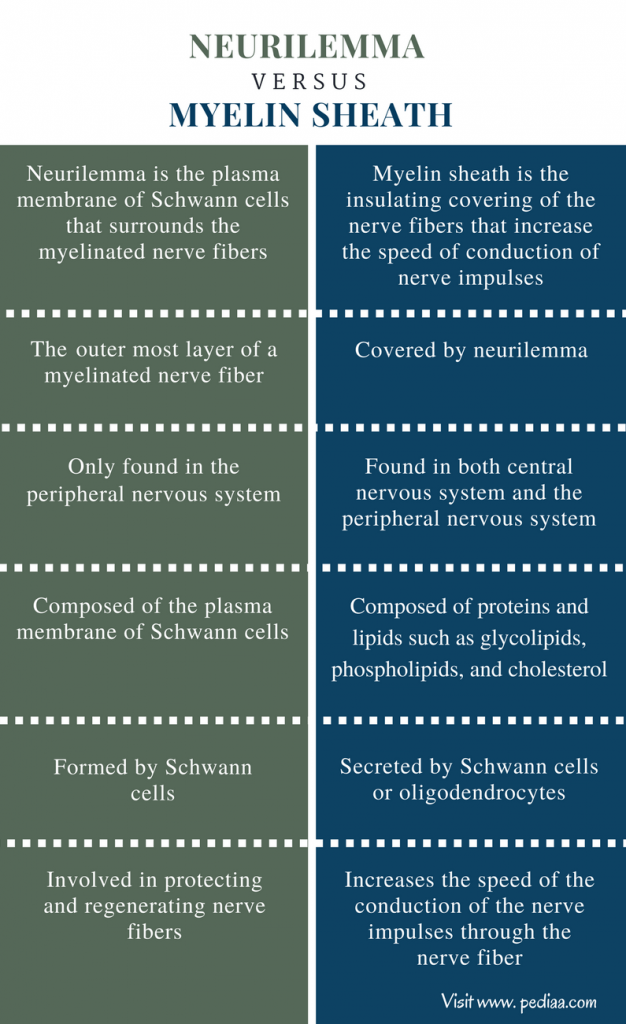 A. 1999) schizophrenia .
A. 1999) schizophrenia .
When typologically differentiating obsessive-compulsive states, the characteristics of the current schizophrenic process were taken into account, which determine the structural features of the leading obsessive-compulsive syndrome. Accordingly, the studied conditions were divided into several clinical types: type 1 - OCD associated with disorders of the affective and neurosis-like registers; Type 2 - OCD associated with disorders of the paranoid register, type 3 - OCD associated with inert affective and negative disorders.
1 type - OCD associated with affective and neurosis-like register disorders. The typological variant included 21 (48%) cases (16 boys, 5 girls), all cases diagnostically met the criteria for neurosis-like schizophrenia. The average age of patients at the time of determination in the clinical picture of OCD was 7.3 +_1.3 years. In most cases, the studied symptoms developed during the second age crisis (7-8 years).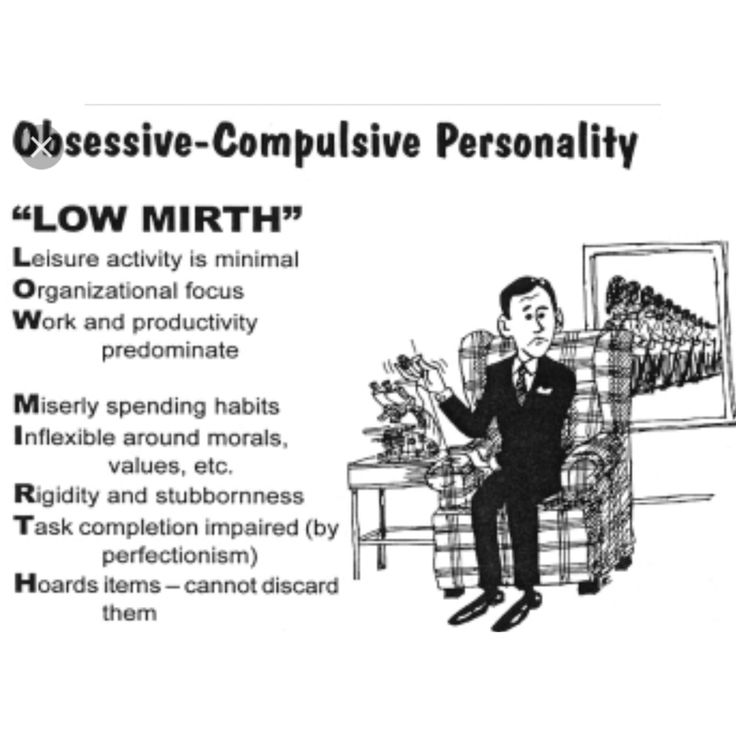
The manifestation of OCD was preceded by a period of schizotypal dysontogenesis with episodes of conditionally reactive states and autochthonous psychopathological disorders. OCD, characteristic of this type, was represented by obsessive phenomena that appear mainly in the emotional sphere (Scanavi E.E. 1954) - obsessive fears and ideas of contrasting content, accompanied by ritual behavior close to Purposeful protection measures (Shyurkute A.A. 1987) . The plot of the OCD had a mundane content, disorders were not characterized by a complex system of rituals.
Compulsive symptoms prevailed in children aged 7-11 years and were represented by elementary motor acts, motor rituals with a mild ego-dystonic component of the disorder. Patients aged 13-15 had both compulsive and obsessional disorders, accompanied by a distinct ego-dystonic awareness.
In the psychopathological structure of the leading syndrome, along with OCD, there were depressive disorders, anxiety-phobic phenomena (generalized anxiety, isolated phobias, social anxiety disorder), hypochondriacal and depersonalization disorders.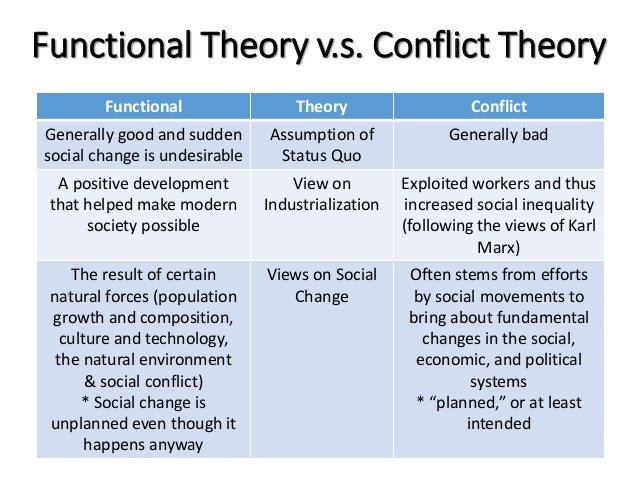
With the predominance of anxiety-phobic disorders, OCD were represented by elementary movements and, as ontogenetic maturation, by rituals of control associated with precautionary measures against an accident, Terrifying representations (Kashnikova A.A. 1973).
Observations of OCD, associated mainly with depersonalization disorders, were represented by doubts about the completeness of the action, in some cases - judgments, feelings, ideas (Janet P. 1903), which were accompanied by a repetition of ordinary actions - simple and complex movements, ritual questions.
With the predominance of hypochondriacal coloring, compulsive symptoms intensified in a situation of possible contact with an infection, accompanied by rituals of control and, over time, complicated by doubts and mastering ideas, which were joined by disorders indicating endogenous procedural transformation (somatopsychic depersonalization with phenomena of essential senestopathies) . The generalization of rituals was associated with the attachment of sensitive ideas of attitude.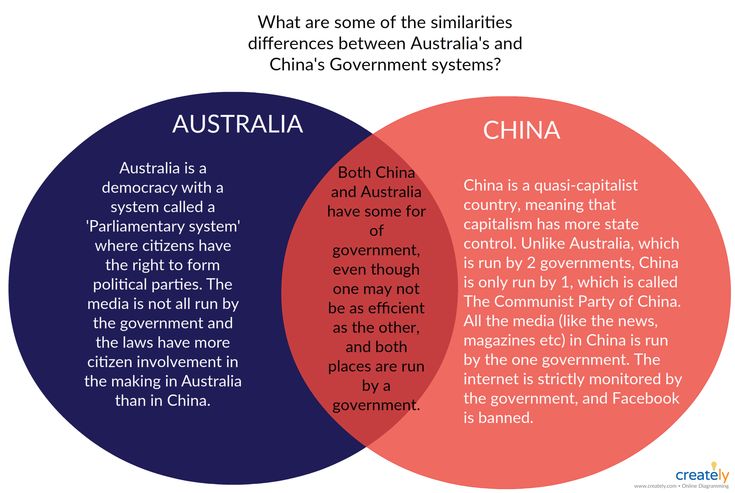 With the full availability of behavioral motives, an increase in the number of avoided objects was observed. In the structure of such states, OKRs approached overvalued ideas in terms of affective charge, uncorrectable behavior. Acute disorders of thinking were revealed (perseverativeness, thoroughness with distractibility to side associations).
With the full availability of behavioral motives, an increase in the number of avoided objects was observed. In the structure of such states, OKRs approached overvalued ideas in terms of affective charge, uncorrectable behavior. Acute disorders of thinking were revealed (perseverativeness, thoroughness with distractibility to side associations).
OCD within the selected type was not persistent, the course of the disease was paroxysmal, there were long-term remissions with the restoration of the adaptive capabilities of patients. After the attack, deficient changes were revealed in the form of a distorted development with acquired anancaste and mosaic psychopath-like features, which later did not show a tendency to progressive deepening.
Co 2 type - OCD associated with paranoid disorders - conditions are assigned, in the psychopathological structure of which, along with OCD, paranoid phenomena were detected. . The typological group included 14 (23%) observations (8 boys, 6 girls aged 9 to 14 years, average age 13 + _ 1.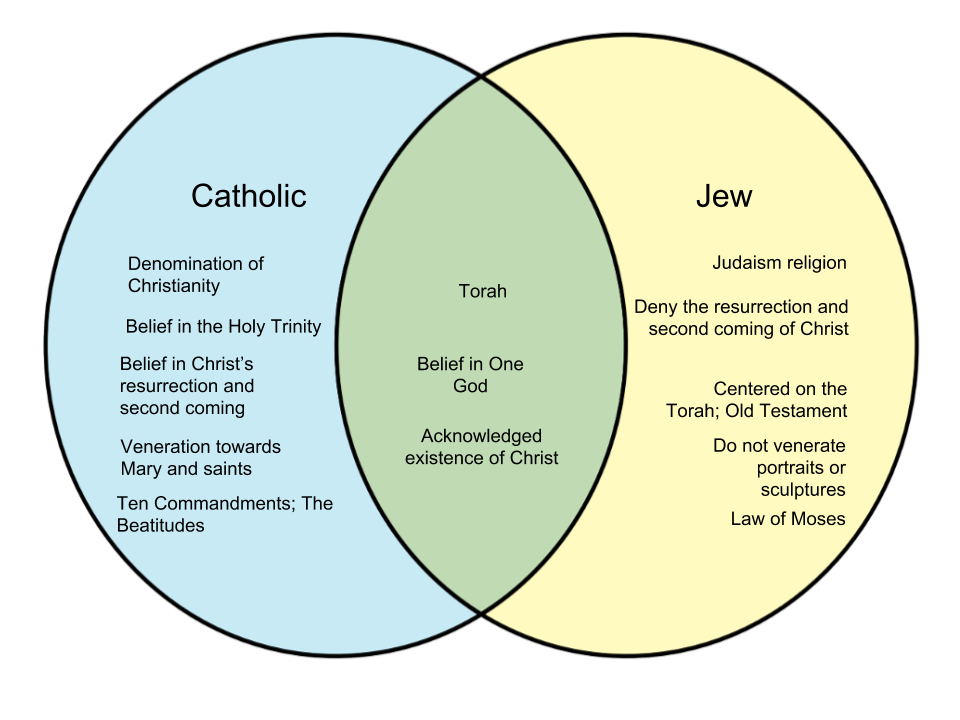 8 years. The conditions developed during prolonged attacks in the framework of schizophrenia approaching paranoid (according to with ICD - schizophrenia (children's type).The manifest state was preceded by a period of schizotypal dysontogenesis without signs of mental deficiency with conditionally reactive states.0003
8 years. The conditions developed during prolonged attacks in the framework of schizophrenia approaching paranoid (according to with ICD - schizophrenia (children's type).The manifest state was preceded by a period of schizotypal dysontogenesis without signs of mental deficiency with conditionally reactive states.0003
OCD was represented by aggressive obsessions, contagion obsessions, and somatic obsessions (CY-BOCS, Goodman et al. 1997), accompanied by repetition of actions, rituals of washing, avoidance, comparison, respectively. The obsessional component gradually took on a monomorphic character and was accompanied by a generalization of rituals. OCD within the selected type was characterized by both a partial overlap of obsessive symptoms with disorders of the paranoid register, and a complete transformation of obsessive disorders into paranoid ones.
In the first case, the generalization and systematization of OCD was realized along the path of strengthening associations caused by surrounding objects (Zavidovskaya GI 1971).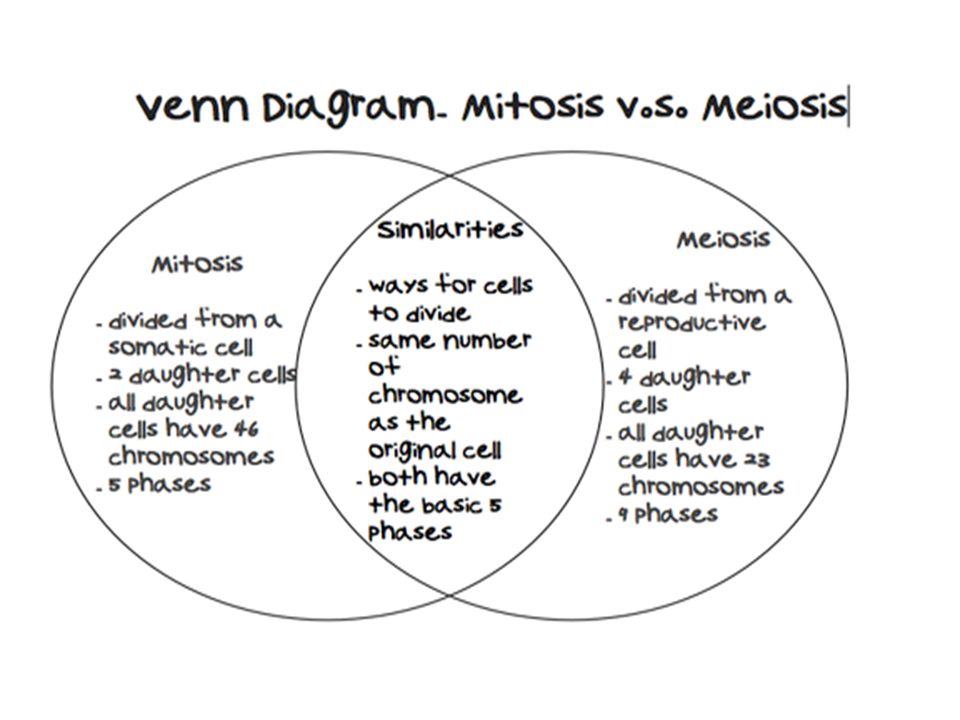 The range of associations was actively supplemented by the participation of imagination mechanisms: frightening ideas or fears of infection, changes in appearance, etc. caused previously indifferent objects, to which fantastic properties were attributed by patients. The states were accompanied by fragmentary hallucinations of the imagination. Patients lost the ego-dystonic component of OCD symptoms, the motives of their behavior became inaccessible, the rituals of the former plot took on the character of delusional behavior.
The range of associations was actively supplemented by the participation of imagination mechanisms: frightening ideas or fears of infection, changes in appearance, etc. caused previously indifferent objects, to which fantastic properties were attributed by patients. The states were accompanied by fragmentary hallucinations of the imagination. Patients lost the ego-dystonic component of OCD symptoms, the motives of their behavior became inaccessible, the rituals of the former plot took on the character of delusional behavior.
In the second, obsessional symptoms were completely replaced by paranoid ones with a change in the plot of disorders: fragmentary interpretive elements of the Alien Parents' delirium, poisoning, and bodily metamorphosis were revealed.
The course of the disease was paroxysmal-progressive in nature within the framework of schizophrenia approaching paranoid. During the period of weakening of paranoid symptoms, obsessive-compulsive disorders again came to the fore in the clinical picture, with a partial loss of the ego-dystonic component of the disorder, which was associated with the formation of fairly pronounced post-attack negative changes.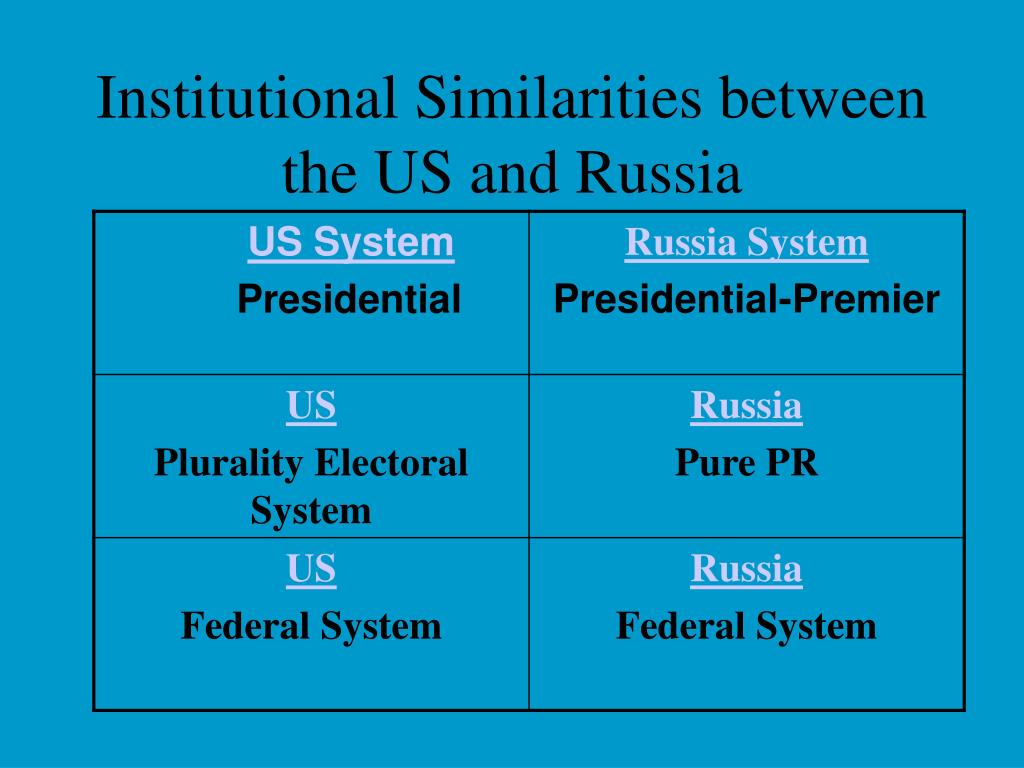
3 type - OCD associated with inert affective and negative disorders appeared against the background of fairly distinct negative changes, dissociated development with mosaic psychopathic features and a deficit of mental activity, close to a Waligophrenia-like F defect. Conditions were formed within the framework of a continuous course of sluggish and approaching paranoid schizophrenia.
The typological group included 25 (19%) observations (3 girls, 22 boys). The formation of the outlined states with obsessive-compulsive symptoms was preceded by a period of progressive schizotypal dysontogenesis (17 patients). OCD similar in clinical structure was detected in post-attack states of schizophrenia approaching paranoid (8 patients). The average age of patients at the time of detection in the clinical picture of disorders of the selected type was 13.8 +_1.2 years.
OCD was characterized by a partial, formally recognized ego-dystonic component of the disorder, without attempts to resist symptoms; in a number of observations, critical motives did not reach ontogenetic formation due to the early appearance of negative disorders.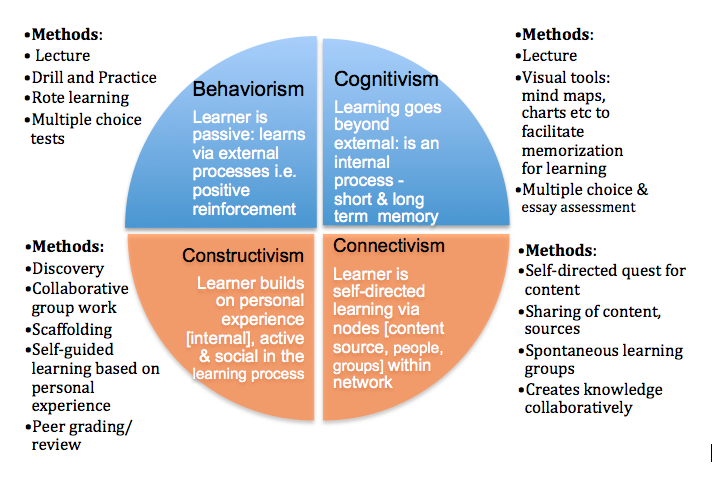 OCD was accompanied by pronounced negative changes: cognitive impairment, a decrease in the social orientation of behavior, and gross egocentrism. In the majority of observations, OCD was represented by a subcategory of disorders, C, with a predominance of compulsions. The compulsive symptoms had a pronounced process-transformed character and acquired a phenomenological similarity with catatonic stereotypes (Jahrreiss W. 1926. Shurkute A.A. 1987) by the nature of impulsiveness, affective emptiness. Compulsive disorders were represented by elementary motor acts, stereotyped ritual questions, inert rituals of washing, mental rituals - representations of a protective nature of ridiculous content. Doubts that appeared in the structure of previous attacks took on the character of rumination. In general, the rituals were characterized by ambivalence and pretentiousness, an auto-aggressive orientation, which took on a chronic impulsive character. The symptomatology was persistent, accompanied by inert bipolar affective disorders and partially persisted during the period of incomplete therapeutic remissions.
OCD was accompanied by pronounced negative changes: cognitive impairment, a decrease in the social orientation of behavior, and gross egocentrism. In the majority of observations, OCD was represented by a subcategory of disorders, C, with a predominance of compulsions. The compulsive symptoms had a pronounced process-transformed character and acquired a phenomenological similarity with catatonic stereotypes (Jahrreiss W. 1926. Shurkute A.A. 1987) by the nature of impulsiveness, affective emptiness. Compulsive disorders were represented by elementary motor acts, stereotyped ritual questions, inert rituals of washing, mental rituals - representations of a protective nature of ridiculous content. Doubts that appeared in the structure of previous attacks took on the character of rumination. In general, the rituals were characterized by ambivalence and pretentiousness, an auto-aggressive orientation, which took on a chronic impulsive character. The symptomatology was persistent, accompanied by inert bipolar affective disorders and partially persisted during the period of incomplete therapeutic remissions.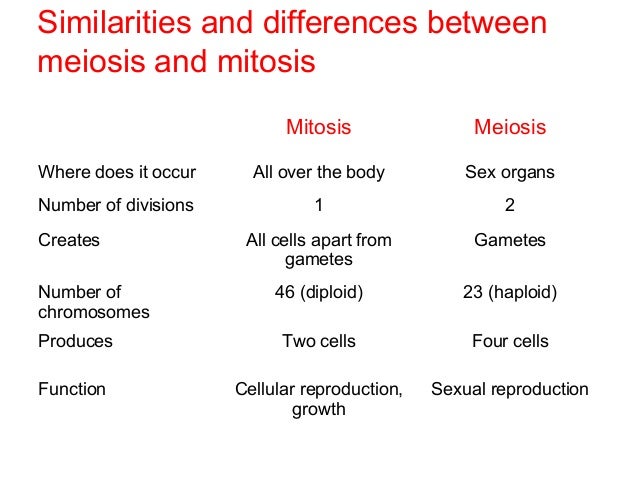
Thus, the typology of conditions presented in the study with a predominance of OCD, which form in the clinical picture of schizophrenia manifesting in childhood, allows us to assume the rate of progression and the nature of the course of the disease, to predict the depth of emerging negative changes and the type of supposed remission.
As part of the ongoing study, a comparison was made of biochemical parameters of the serotonergic system with clinical manifestations of OCD in the structure of schizophrenia manifesting in childhood. The study obtained data on the % content of IR-SERT platelets in patients with OCD, conducted a correlation analysis between the level of IR-SERT and the severity of the clinical condition of patients, assessed by clinical scales CY-BOCS and PANSS.
The study group of patients in a state of clinical exacerbation of symptoms did not show significant differences in the state of platelet IR-SERT compared with control values.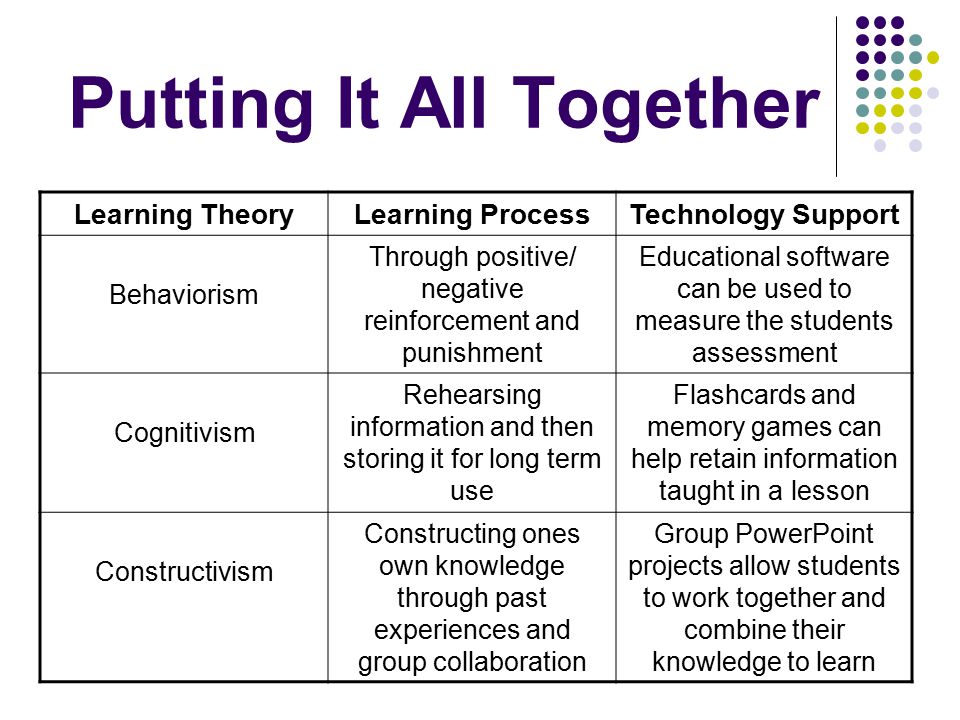 Patients in remission were characterized by a marked decrease in the level of IR-SERT platelets, both in comparison with control values and in comparison with the group in a state of clinical exacerbation (p<0.011).
Patients in remission were characterized by a marked decrease in the level of IR-SERT platelets, both in comparison with control values and in comparison with the group in a state of clinical exacerbation (p<0.011).
These data may indicate a decrease in the functional activity of the carrier protein and, as a result, an increase in the concentration of serotonin in the synaptic clefts of CNS neurons, i.e., activation of the serotonin system in patients during treatment. Thus, the hypofunction of the serotonin system correlates, and possibly is the cause, of the exacerbation of the clinical condition. Chronic blockade of the carrier protein leads to a decrease in the content of IR-SERT and, as a result, to the normalization of the activity of the serotonin system. At the same time, there is a significant reduction in the severity of the condition of patients. Thus, it becomes possible to quantify the condition of patients not only at admission, but also during treatment.
The revealed correlations between clinical parameters and IR-SERT also indicate the involvement of the serotonin system in the pathogenesis of OCD.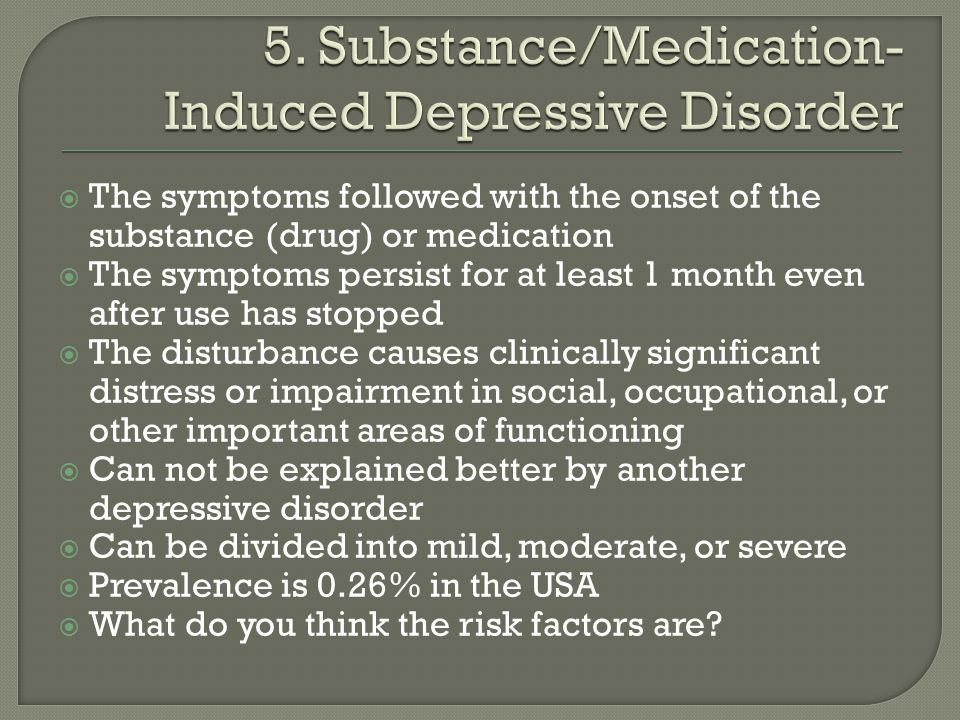 This makes it possible to substantiate the widespread use of psychotropic drugs that are highly selective for the serotonin system (SSRIs, atypical antipsychotics) as a putative pathogenetic treatment of such conditions in children.
This makes it possible to substantiate the widespread use of psychotropic drugs that are highly selective for the serotonin system (SSRIs, atypical antipsychotics) as a putative pathogenetic treatment of such conditions in children.
In the framework of this study, at the stage of active therapeutic rehabilitation of patients with OCD in the picture of the schizophrenic process manifesting in childhood, combined therapy methods were used with the use of drugs that have the ability to selectively affect the functional activity of the serotonin system.
The principles of psychopharmacotherapy were built taking into account the identified features of the clinical structure of conditions.
Antidepressants of the SSRI group (fluoxetine up to 40 mg/day, sertraline up to 100 mg/day) in combination with atypical antipsychotics (rispolept at a therapeutic dose suggesting a predominant effect on 5 HT 2 receptors - up to 3-4 mg / day), as well as benzodiazepine derivatives (clonazepam up to 2-4 mg / day).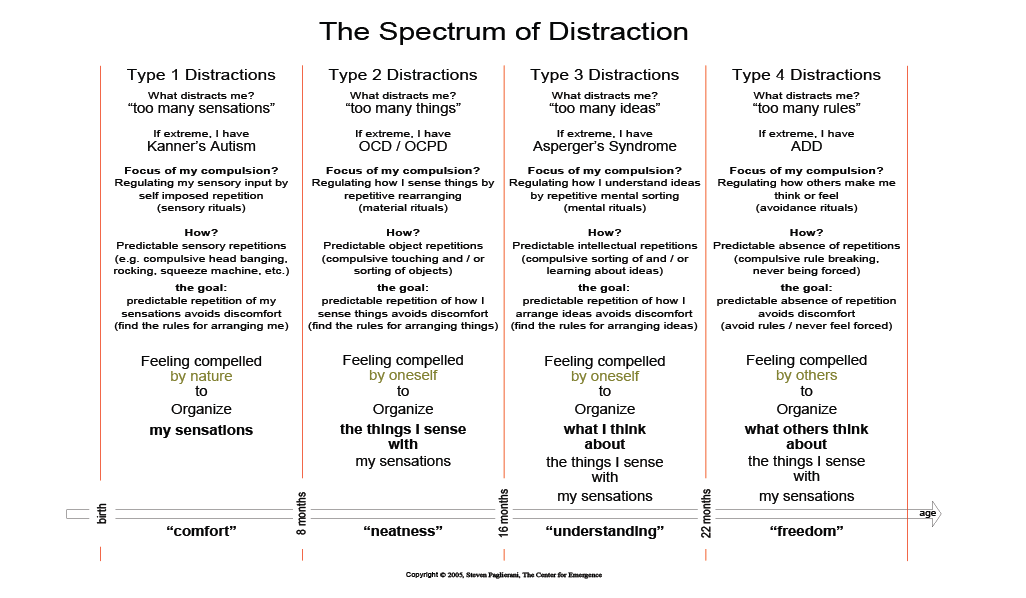 Perhaps a combination of antidepressants of the SSRI group with the traditional antipsychotic - trifluoperazine (stelazin up to 10 mg / day.).
Perhaps a combination of antidepressants of the SSRI group with the traditional antipsychotic - trifluoperazine (stelazin up to 10 mg / day.).
Therapy of conditions with a predominance of OCD, classified in the 2nd typological group, within the framework of approaching paranoid schizophrenia, was carried out using antipsychotic doses of traditional and atypical neuroleptics - trifluperazine (stelazin) up to 30 mg / day, clozapine (azaleptin) up to 100 mg / day. day, rispolept up to 8 mg / day. in combination with SSRI antidepressants and tricyclic antidepressants.
Therapeutic effect on type 3 OCD was effective with the combined use of atypical neuroleptics (rispolept up to 8 mg/day) with mood stabilizers (lithium carbonate up to 1200 mg/day under the control of the concentration of the drug in blood plasma).
Thus, the data obtained in the course of this study on the effectiveness of various psychopharmacological drugs in the treatment of OCD in the picture of schizophrenia manifesting in childhood can serve as a basis for optimizing therapeutic measures at the stage of medical and medical rehabilitation of patients.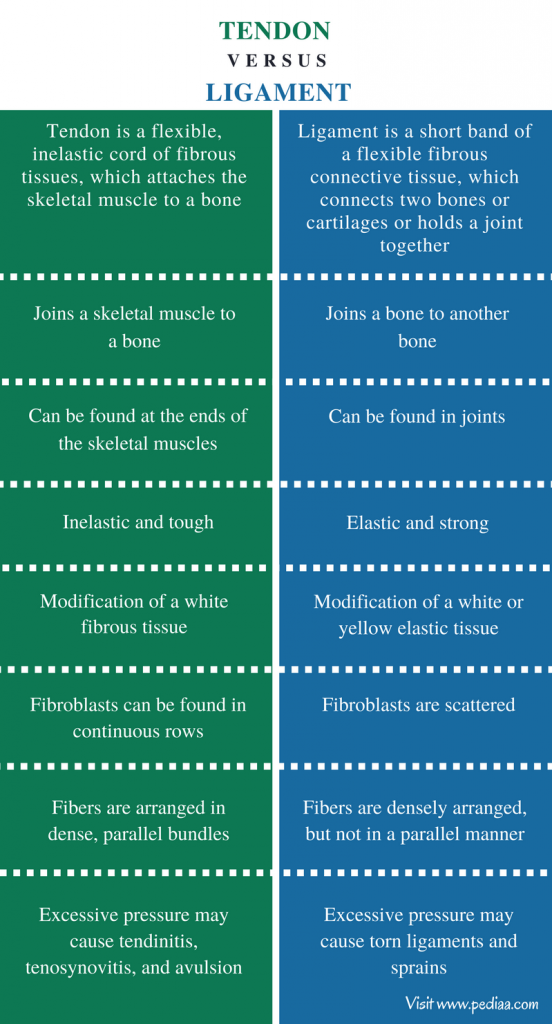
Conclusions.
1. The psychopathological structure of the obsessive-compulsive syndrome, which is formed within the framework of schizophrenia, manifesting in childhood, reveals significant heterogeneity and depends on the clinical characteristics of the schizophrenic process, which determine the predominance of productive or negative disorders in the structure of the syndrome:
-
clinical features and duration of the pre-manifest period, which determine the level of negative disorders at the time of OCD manifestation;
-
progression and type of course of the schizophrenic process.
-
Differentiation of the features of the psychopathological structure of OCD in schizophrenia manifesting in childhood makes it possible to distinguish:
2.1 type 1 - OCD associated with disorders of the affective and neurosis-like registers, characterized by:
- a period of schizotypal dysontogenesis with episodes of conditionally reactive states and autochthonous psychopathological disorders preceding the manifestation of the outlined OCD;
-
polymorphism of clinical manifestations of OCD, along with the routine of their content, a slight tendency to generalization of disorders;
-
a predominant combination of OCD with disorders of the non-psychotic register - anxiety-phobic, depressive, depersonalization and hypochondriacal disorders;
-
procedural transformation of a productive symptom complex in the form of joining senestopathies and ideas of relation;
-
deficient changes (dissociated development with acquired anancaste and mosaic psychopathic features), which are formed in the subsequent dynamics of the disease, without a tendency to progressive deepening.
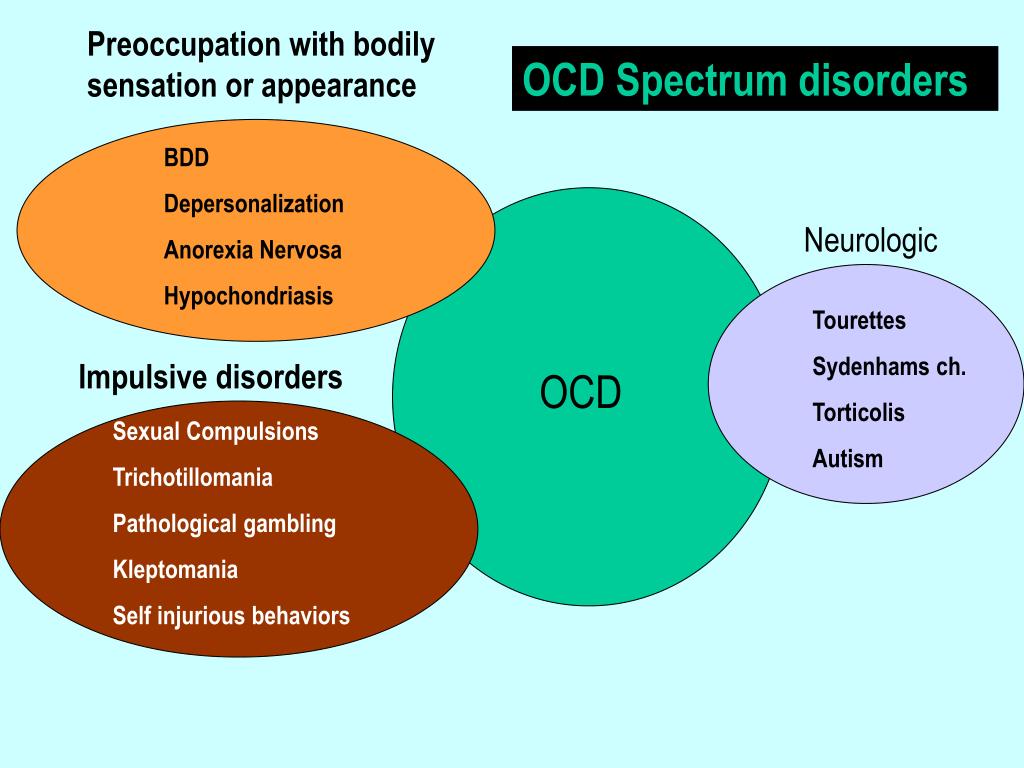
2.2. type 2 - OCD associated with disorders of the paranoid register, characterized by:
-
a period of schizotypal dysontogenesis with conditionally reactive states preceding the manifest state;
-
monomorphic clinical manifestations of OCD with a pronounced tendency to generalization and systematization;
-
both partial overlap of obsessional symptoms with paranoid register disorders (rudiments of delusional imagination and hallucinations of the imagination) and complete replacement of OCD with paranoid symptoms;
-
formation in the subsequent dynamics of the disease of negative disorders, reflecting the pronounced progression of the schizophrenic process.
2..3 3 type - OCD associated with inert affective and negative disorders , characterized by:
- the formation of an established type of disorders against the background of dissociated development with mosaic psychopathic features and a deficit of mental activity that developed during the period of progredient schizotypal dysontogenesis, or at the post-attack stage of schizophrenia approaching paranoid ;
-
pronounced signs of OCD process transformation - rigid monomorphism of compulsive symptoms, phenomenological similarity of OCD with catatonic stereotypes;
-
a combination of OCD predominantly with inert bipolar affective disorders of a continual nature and negative disorders (cognitive impairment, decreased social orientation of behavior, gross egocentrism).
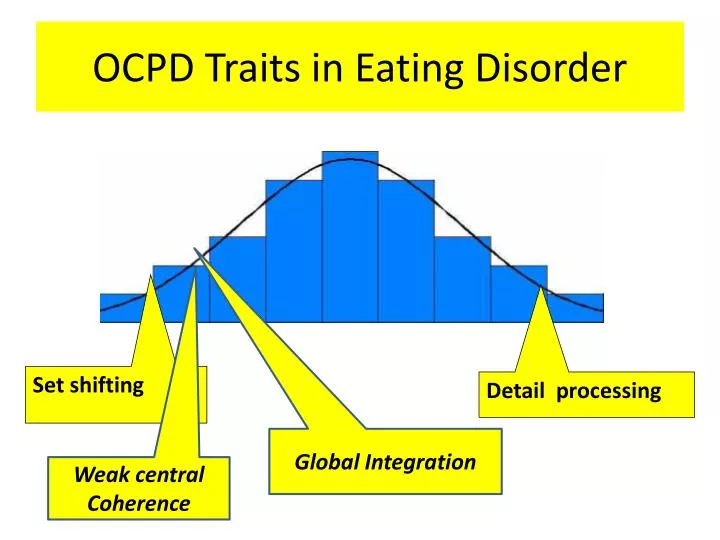
3. The group of patients with OCD, developing in the picture of schizophrenia, manifesting in childhood, is characterized by disturbances in the biochemical homeostasis of the serotonin system, registered during the study of the state of the immunoreactive serotonin transporter protein (IR-SERT).
3.1 Quantitative assessment of the IR-SERT content of platelets in patients with OCD as part of a schizophrenic process that manifests itself in childhood can serve as a marker of the severity of the condition on admission and during treatment: significant differences in the level of IR-SERT platelets compared with control values;
- in remission, a marked decrease in the level of IR-SERT of platelets is detected, both in comparison with control values and in comparison with indicators in the state of clinical exacerbation (p<0.011).
4. The choice of tactics in the treatment of OCD, which is formed in the picture of the schizophrenic process in childhood, should take into account the peculiarities of the psychopathological structure of OCD, the expediency of using highly selective drugs for serotonin receptors, and the need for an intensive nature of the therapy.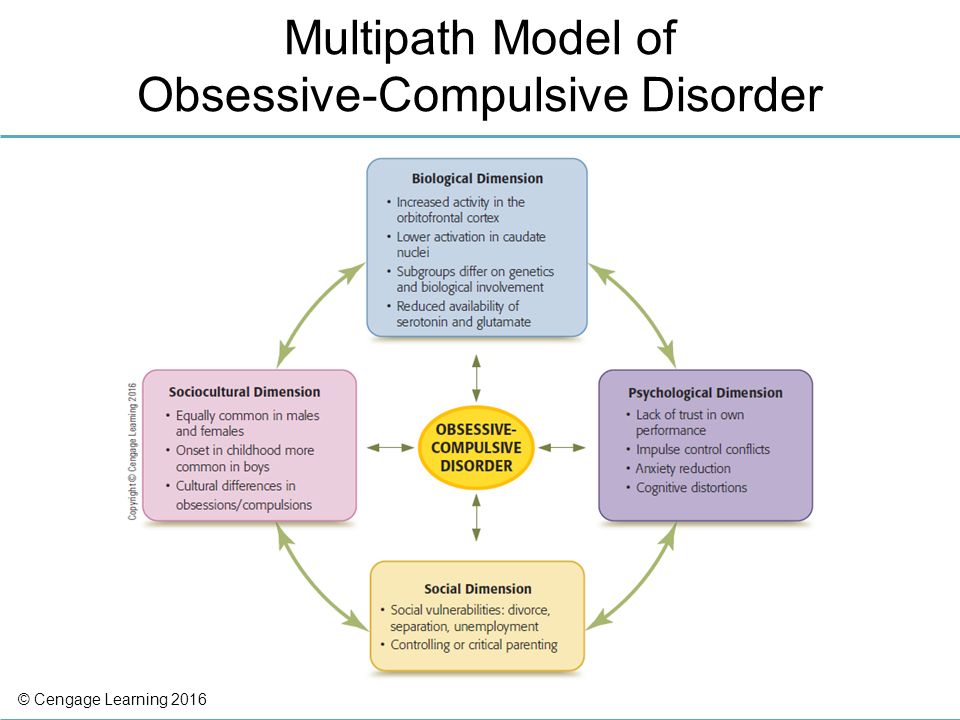
4.1 In the treatment of OCD associated with disorders of affective and neurosis-like registers , it is necessary to use antidepressants of the SSRI group (fluoxetine, sertraline) in combination with atypical antipsychotics (rispolept) in doses that presuppose a predominant effect on 5HT2 receptors, as well as benzodiazepine derivatives ( clonazepam).
4.2 In the treatment of OCD associated with disorders of the paranoid register, it is necessary to use traditional trifluperazine (stelazine), and atypical neuroleptics - clozapine (azaleptin), rispolept in antipsychotic doses in combination with antidepressants of the SSRI group and tricyclic antidepressants.
4.3 In the treatment of OCD associated with inert affective and negative disorders , a combination of atypical antipsychotics with mood stabilizers (lithium carbonate) should be used.
List of papers published on the topic of the dissertation.
-
Obsessive-compulsive disorders in childhood // Collection of Anxiety and Obsessions, ed.
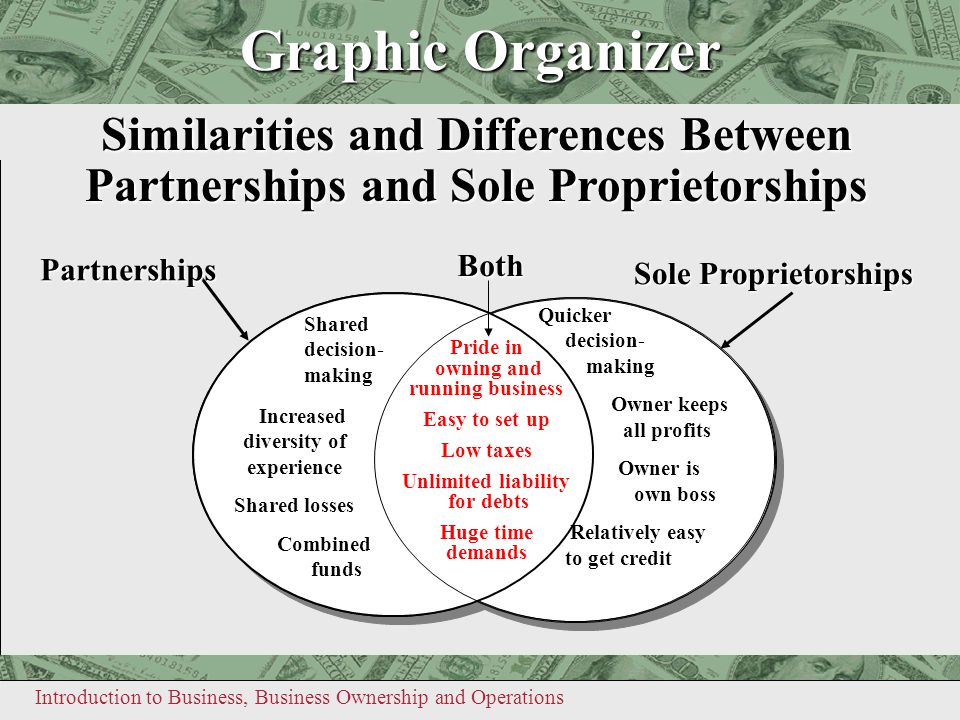 corresponding member RAMS prof. Smulevich A.B. - Moscow 1998. -p. 144-157. (co-authored with Kozlova I.A., Savostyanova O.L.).
corresponding member RAMS prof. Smulevich A.B. - Moscow 1998. -p. 144-157. (co-authored with Kozlova I.A., Savostyanova O.L.). -
Comorbidity of obsessive-compulsive disorders with schizotypal personality disorders in childhood // Abstracts of the Х1V Congress of the International Association of Child and Adolescent Psychiatry - Stockholm, Sweden, August 2-6, 1998g. - p.106 (co-authored with Kozlova I.A., Savostyanova O.L.)
-
On the problem of the correlation between depressive and obsessive symptoms in children // Abstracts of the republican conference "New approaches to the diagnosis and treatment of affective disorders" - Moscow 1998. - p.84.
-
Age features of obsessive-compulsive disorders in children and adolescents // Proceedings of the Congress on the protection of a psychologist. health of children and adolescents. - Moscow 1998. - p.78.
-
Clinical and dynamic study of schizophrenia with OCD in childhood.