Signs and symptoms of tardive dyskinesia
Tardive Dyskinesia: Definition, Symptoms, Causes, Treatment
Written by WebMD Editorial Contributors
Your Guide To
Tardive Dyskinesia
- Symptoms
- Causes and Risk Factors
- Diagnosis
- Treatment and Prevention
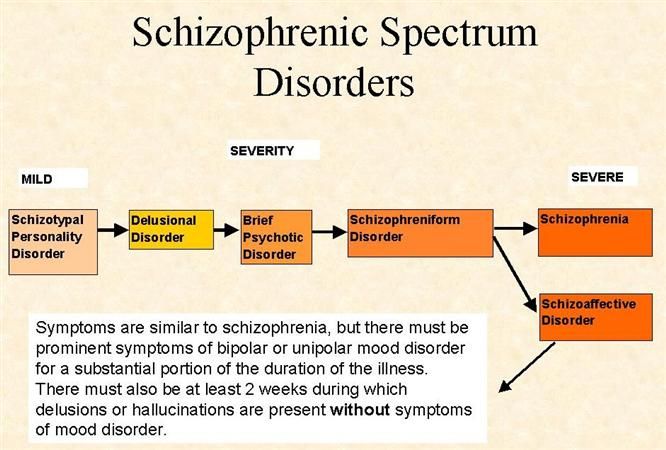
Tardive dyskinesia is a side effect of antipsychotic medications. These drugs are used to treat schizophrenia and other mental health disorders.
TD causes stiff, jerky movements of your face and body that you can't control. You might blink your eyes, stick out your tongue, or wave your arms without meaning to do so.
Not everyone who takes an antipsychotic drug will get it. But if it happens, it’s sometimes permanent. So if you have movements you can't control, let your doctor know right away. To ease your symptoms, your doctor may:
- Lower the dose
- Add another medication to what you’re taking to act as an antidote
- Switch you to a different drug
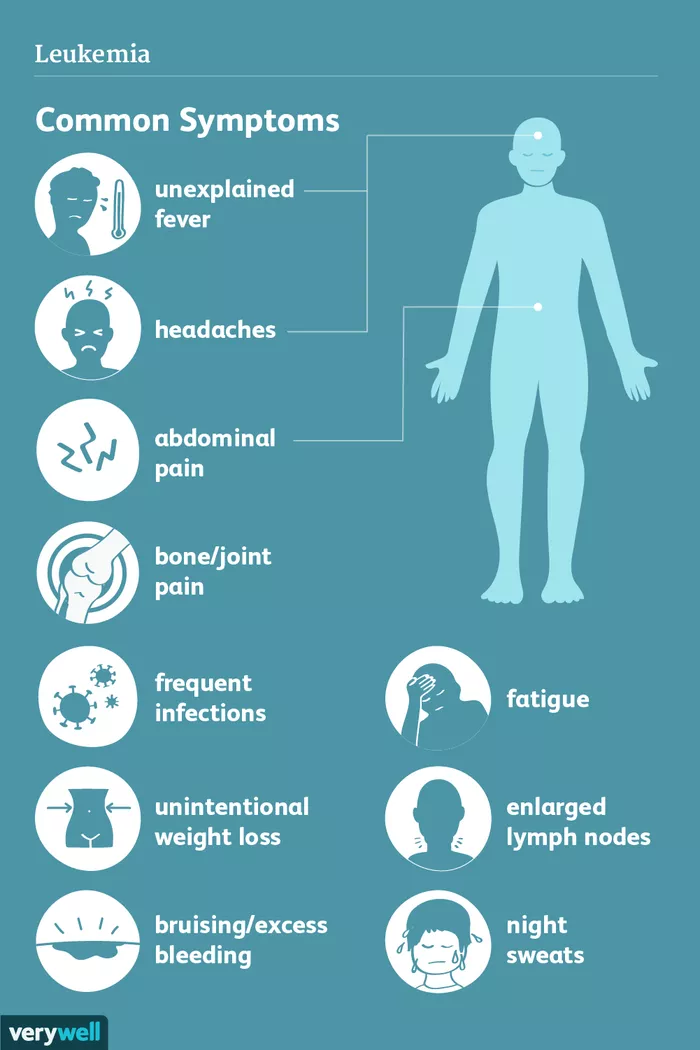
Symptoms
Tardive dyskinesia causes stiff, jerky movements that you can't control. They include:
Orofacial dyskinesia or oro-bucco-lingual dyskinesia: Uncontrolled movements in your face -- namely your lips, jaw, or tongue. You might:
- Stick out your tongue without trying
- Blink your eyes fast
- Chew
- Smack or pucker your lips
- Puff out your cheeks
- Frown
- Grunt
Dyskinesia of the limbs: It can also affect your arms, legs, fingers, and toes. That can cause you to:
- Wiggle your fingers
- Tap your feet
- Flap your arms
- Thrust out your pelvis
- Sway from side to side
These movements can be fast or slow. You may find it hard to work and stay active.
Causes and Risk Factors
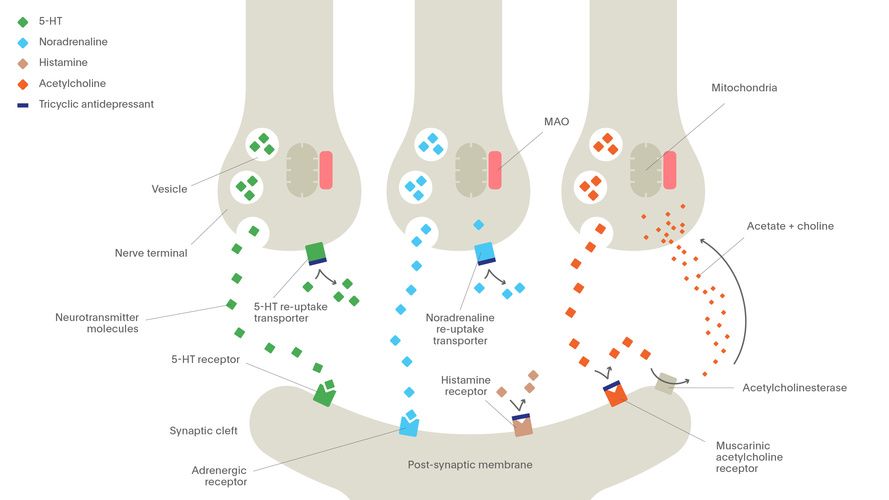
Antipsychotic meds treat schizophrenia, bipolar disorder, and other brain conditions. Doctors also call them neuroleptic drugs.
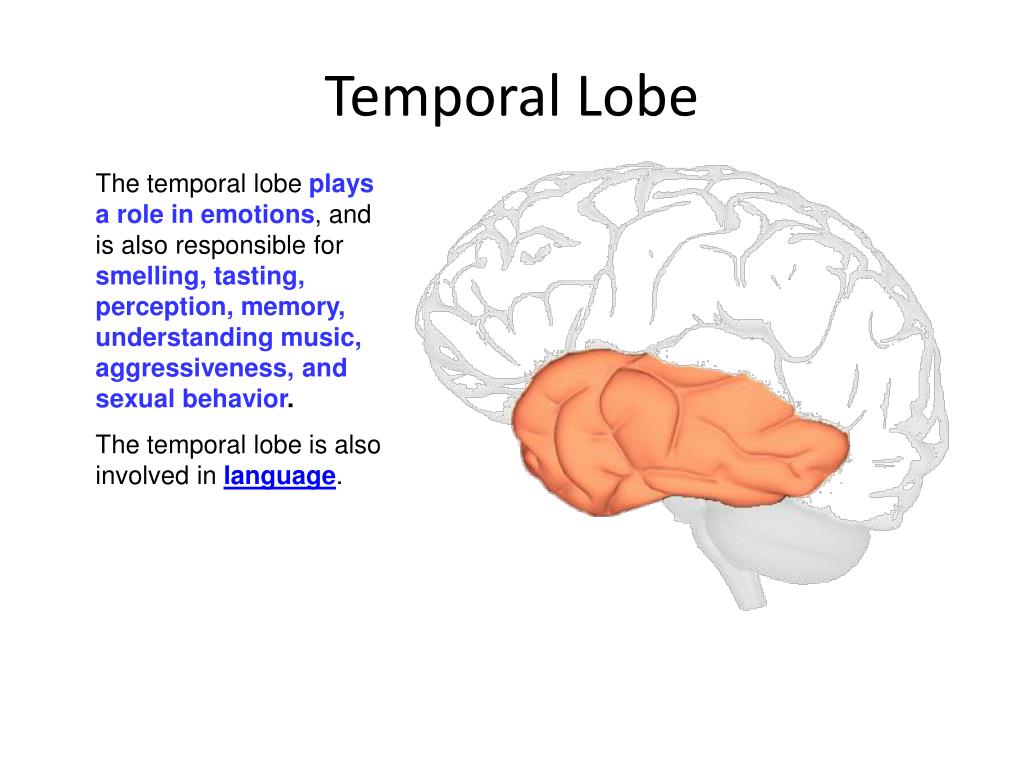
They block a brain chemical called dopamine. It helps cells talk to each other and makes the muscles move smoothly. When you have too little of it, your movements can become jerky and out of control.
When you have too little of it, your movements can become jerky and out of control.
You can get TD if you take an antipsychotic drug. Usually you have to be on it for 3 months or more. But there have been rare cases of it after a single dose of an antipsychotic medicine. Older versions of these drugs are more likely to cause this problem than newer ones. Some studies find a similar risk from both types, though.
Antipsychotic medications that can cause tardive dyskinesia include antipsychotics like:
- Haloperidol (Haldol)
- Fluphenazine
- Risperidone (Risperdal)
- Olanzapine (Zyprexa)
Your chances of getting TD go up the longer you take an antipsychotic medicine.
Some drugs that treat nausea, reflux, and other stomach problems can also cause TD if you take them for more than 3 months. These include:
- Metoclopramide (Reglan)
- Prochlorperazine (Compazine)
You're more likely to get it if you:
- Are a woman who has gone through menopause
- Are over age 55
- Abuse alcohol or drugs
- Are African American or Asian American
Diagnosis
TD can be hard to diagnose. Symptoms might not appear until months or years after you start taking antipsychotic medicine. Or you might first notice the movements after you've already stopped taking the drug. The timing can make it hard to know whether the medicine caused your symptoms.
Symptoms might not appear until months or years after you start taking antipsychotic medicine. Or you might first notice the movements after you've already stopped taking the drug. The timing can make it hard to know whether the medicine caused your symptoms.
Abnormal Involuntary Movement Scale (AIMS): If you take medicine for mental health conditions, your doctor should check you at least once a year to make sure you don't have TD. They can give you a physical exam called the Abnormal Involuntary Movement Scale, which will help them rate any abnormal movements.
They can also do tests to find out whether you have another disorder that causes abnormal movements, like:
- Cerebral palsy
- Huntington's disease
- Parkinson's disease
- Stroke
- Tourette's syndrome
To rule out these conditions, you may get:
- Blood tests
- Imaging scans of the brain, such as a CT or MRI scan
Treatment and Prevention
The goal is to prevent TD. When your doctor prescribes a new drug to treat a mental health disorder, ask about its side effects. The benefits of the drug should outweigh the risks.
When your doctor prescribes a new drug to treat a mental health disorder, ask about its side effects. The benefits of the drug should outweigh the risks.
If you have movement problems, tell your doctor but don't stop taking the drug on your own. Your doctor can take you off the medicine that caused the movements, or lower the dose.
You might need to switch to a newer antipsychotic drug that may be less likely to cause TD.
There are two FDA-approved medicines to treat tardive dyskinesia:
- Deutetrabenazine (Austedo)
- Valbenazine (Ingrezza)
Both of these medicines work in similar ways to regulate the amount of dopamine flow in brain areas that control certain kinds of movements. Both can sometimes cause drowsiness. Austedo also has been shown to sometimes cause depression when used in patients with Huntington's disease.
There's no proof that natural remedies can treat it, but some might help with movements:
- Ginkgo biloba
- Melatonin
- Vitamin B6
- Vitamin E
Talk to your doctor before you take any supplements for your symptoms.
Austedo Oral: Uses, Side Effects, Interactions, Pictures, Warnings & Dosing
Warnings:
If you have Huntington's disease, deutetrabenazine can sometimes increase the risk of depression and suicidal thoughts/attempts. People with Huntington's disease are already more likely to have depression and suicidal thoughts/attempts. Talk with your doctor about the risks and benefits of this medication. People with Huntington's disease and depression must not use deutetrabenazine if they are not being treated for depression or if they still have symptoms of depression with medication/treatment. Tell your doctor right away if you or your family/caregivers notice that you have new/worsening symptoms of depression, sadness, loss of interest in activities you used to enjoy, suicidal thoughts/attempts, or other mental/mood/behavior changes (such as new/worsening anxiety, panic attacks, trouble sleeping, irritability, hostile/angry feelings).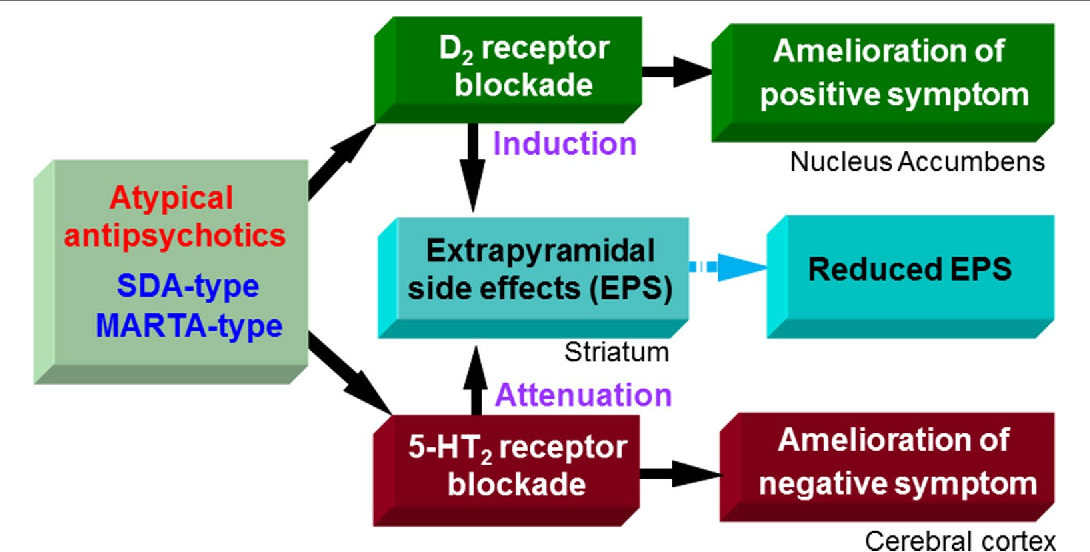
Warnings:
If you have Huntington's disease, deutetrabenazine can sometimes increase the risk of depression and suicidal thoughts/attempts. People with Huntington's disease are already more likely to have depression and suicidal thoughts/attempts. Talk with your doctor about the risks and benefits of this medication. People with Huntington's disease and depression must not use deutetrabenazine if they are not being treated for depression or if they still have symptoms of depression with medication/treatment. Tell your doctor right away if you or your family/caregivers notice that you have new/worsening symptoms of depression, sadness, loss of interest in activities you used to enjoy, suicidal thoughts/attempts, or other mental/mood/behavior changes (such as new/worsening anxiety, panic attacks, trouble sleeping, irritability, hostile/angry feelings).
... Show More
Uses
Deutetrabenazine is used to decrease involuntary movements (chorea) caused by Huntington's disease. It is also used to treat involuntary movements of the face, tongue, or other body parts (tardive dyskinesia). However, it is not a cure for the Huntington's disease or tardive dyskinesia. Reducing involuntary movements will help you take part in more of your normal daily activities. This medication is thought to work by decreasing the amount of certain natural substances in the brain that affect how your nerves and muscles work (monoamines such as dopamine, serotonin, and norepinephrine).
It is also used to treat involuntary movements of the face, tongue, or other body parts (tardive dyskinesia). However, it is not a cure for the Huntington's disease or tardive dyskinesia. Reducing involuntary movements will help you take part in more of your normal daily activities. This medication is thought to work by decreasing the amount of certain natural substances in the brain that affect how your nerves and muscles work (monoamines such as dopamine, serotonin, and norepinephrine).
How to use Austedo
Read the Medication Guide provided by your pharmacist before you start using deutetrabenazine and each time you get a refill. If you have any questions, ask your doctor or pharmacist.
Take this medication by mouth with food as directed by your doctor, usually once or twice a day. The manufacturer directs not to chew, crush or break the tablet before taking it. However, many similar drugs (immediate-release tablets) can be chewed, crushed or split. To reduce your risk of side effects, your doctor may direct you to start this medication at a low dose and gradually increase your dose. Follow your doctor's instructions carefully.
Follow your doctor's instructions carefully.
The dosage is based on your medical condition, response to treatment, and other medications you may be taking. Be sure to tell your doctor and pharmacist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).
Take this medication regularly to get the most benefit from it. To help you remember, take it at the same time(s) each day. If you stop taking this medication for more than 1 week, do not take another dose until you talk to your doctor. You may need to restart your medication at a lower dose.
Tell your doctor if your condition does not get better or if it gets worse.
Side Effects
See also Warning section.
Drowsiness, trouble sleeping, tiredness, dizziness, nausea, and vomiting may occur. If any of these effects last or get worse, tell your doctor or pharmacist promptly. Your doctor may need to adjust your dose to reduce these side effects.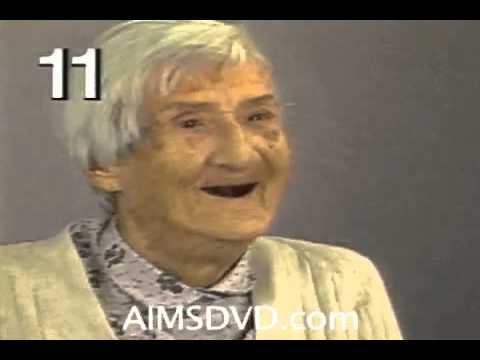
To reduce the risk of dizziness and lightheadedness, get up slowly when rising from a sitting or lying position.
Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.
Tell your doctor right away if you have any serious side effects, including: agitation/restlessness, Parkinson's disease symptoms (such as shaking/tremors, slowed movement, loss of balance).
Sometimes deutetrabenazine can cause side effects that are similar to the symptoms of worsening Huntington's disease. Your doctor may need to adjust your dose to see if these side effects are due to the drug or to the disease. Tell your doctor right away if any of these serious side effects occur: mental/mood changes (such as new/worsening depression, suicidal thoughts/attempts, problems with thinking), trouble swallowing, uncontrolled muscle movements of the face (such as lip smacking, unusual tongue movements), signs of increased prolactin hormone (such as enlarged breasts, abnormal breast milk production, decreased sexual ability, a change in menstrual cycle).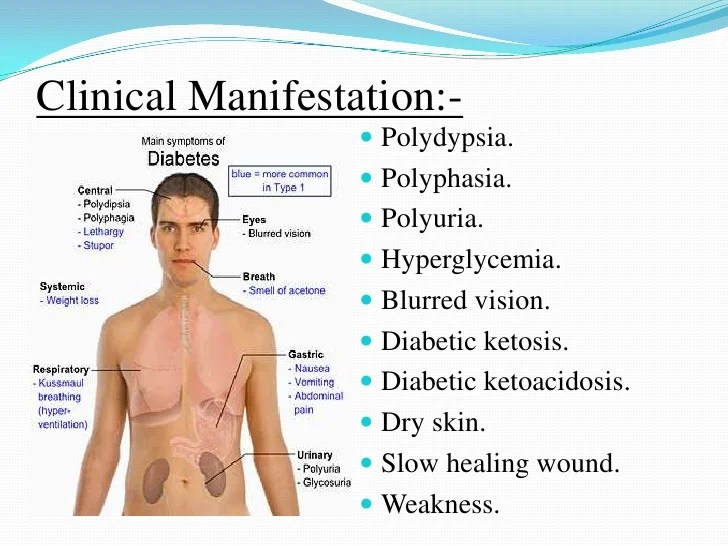
This medication may rarely cause a very serious condition called neuroleptic malignant syndrome (NMS). Get medical help right away if you have any of the following symptoms: fever, muscle stiffness/pain/tenderness/weakness, severe tiredness, severe confusion, sweating, fast/irregular heartbeat, dark urine, signs of kidney problems (such as change in the amount of urine).
A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.
This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.
In the US - Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.
In Canada - Call your doctor for medical advice about side effects.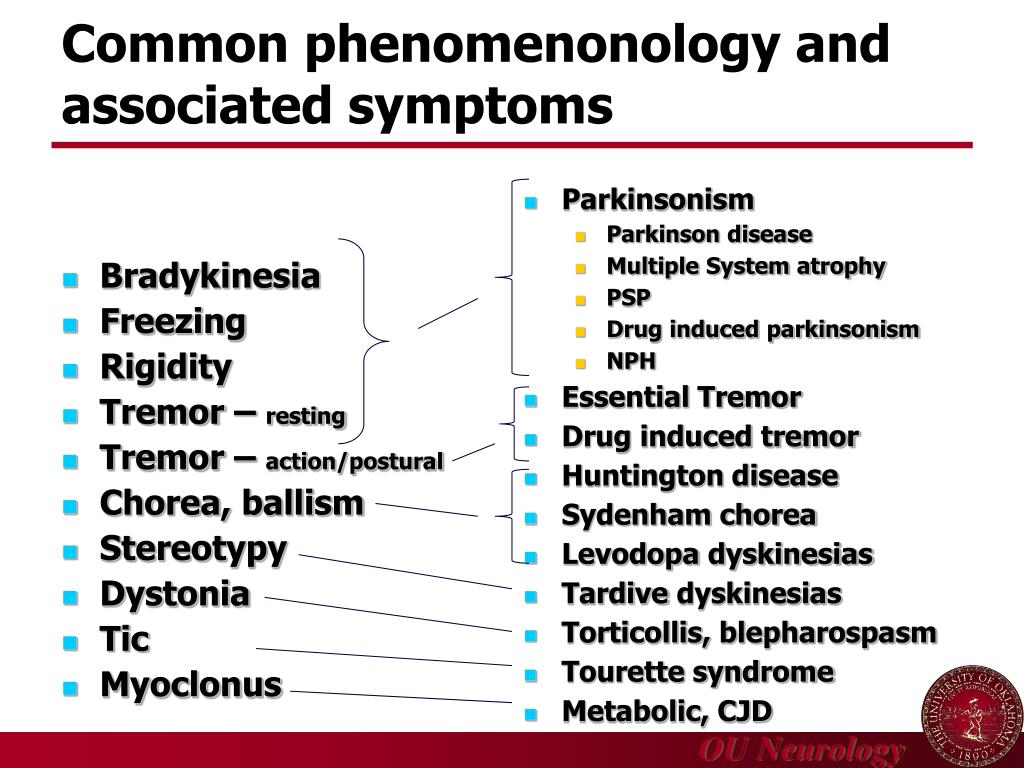 You may report side effects to Health Canada at 1-866-234-2345.
You may report side effects to Health Canada at 1-866-234-2345.
Precautions
See also Warning section.
Before taking deutetrabenazine, tell your doctor or pharmacist if you are allergic to it; or to tetrabenazine; or if you have any other allergies. This product may contain inactive ingredients, which can cause allergic reactions or other problems. Talk to your pharmacist for more details.
Before using this medication, tell your doctor or pharmacist your medical history, especially of: breast cancer, liver problems, certain heart problems (fast/slow/irregular heartbeat, QT prolongation in the EKG).
This drug may make you dizzy or drowsy. Alcohol or marijuana (cannabis) can make you more dizzy or drowsy. Do not drive, use machinery, or do anything that needs alertness until you can do it safely. Limit alcoholic beverages. Talk to your doctor if you are using marijuana (cannabis).
Before having surgery, tell your doctor or dentist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).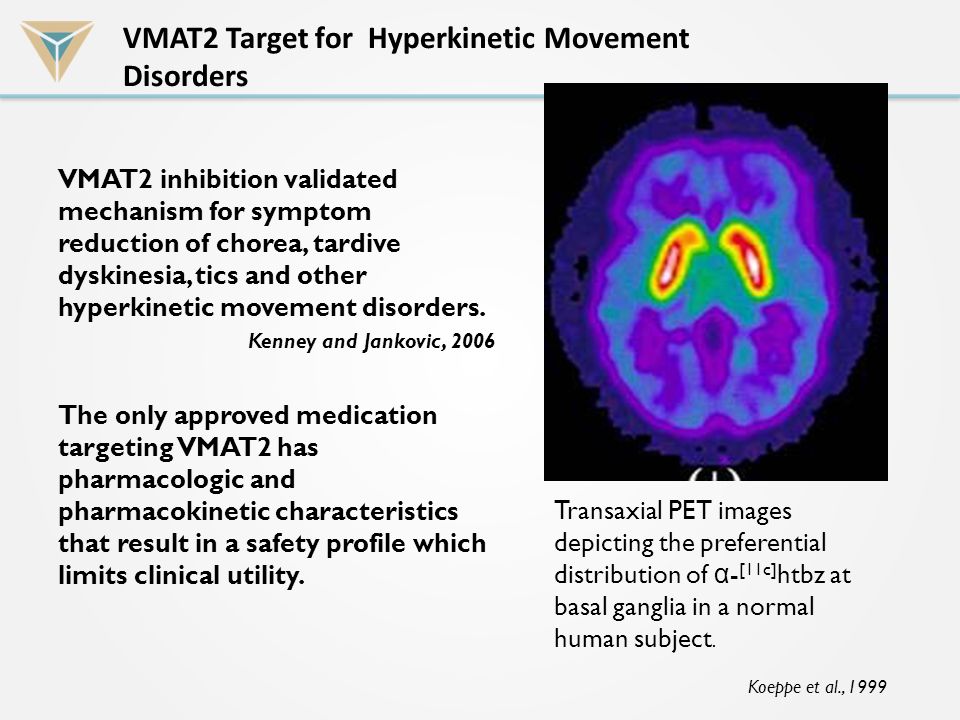
During pregnancy, this medication should be used only when clearly needed. Discuss the risks and benefits with your doctor.
It is unknown if this drug passes into breast milk. Consult your doctor before breast-feeding.
Interactions
Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.
Some products that may interact with this drug are: valbenazine.
Taking MAO inhibitors with this medication may cause a serious (possibly fatal) drug interaction. Do not take any MAO inhibitors (isocarboxazid, linezolid, metaxalone, methylene blue, moclobemide, phenelzine, procarbazine, rasagiline, safinamide, selegiline, tranylcypromine) during treatment with this medication.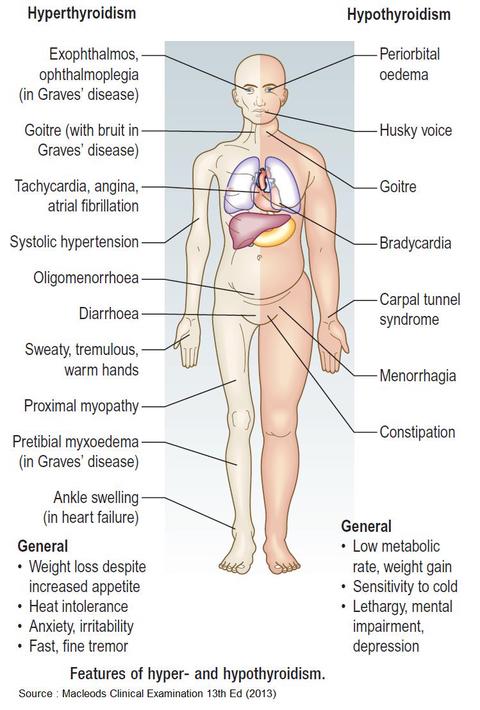 Most MAO inhibitors should also not be taken for two weeks before and after treatment with this medication. Ask your doctor when to start or stop taking this medication.
Most MAO inhibitors should also not be taken for two weeks before and after treatment with this medication. Ask your doctor when to start or stop taking this medication.
Deutetrabenazine is very similar to tetrabenazine. Do not use medications containing tetrabenazine while using deutetrabenazine.
Does Austedo interact with other drugs you are taking?
Enter your medication into the WebMD interaction checker
Overdose
If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call their local poison control center at 1-800-222-1222. Canada residents can call a provincial poison control center. Symptoms of overdose may include: muscle stiffness/pain, fixed upward position of the eyeballs, sweating, dizziness, severe drowsiness.
Do not share this medication with others.
If you miss a dose, take it as soon as you remember.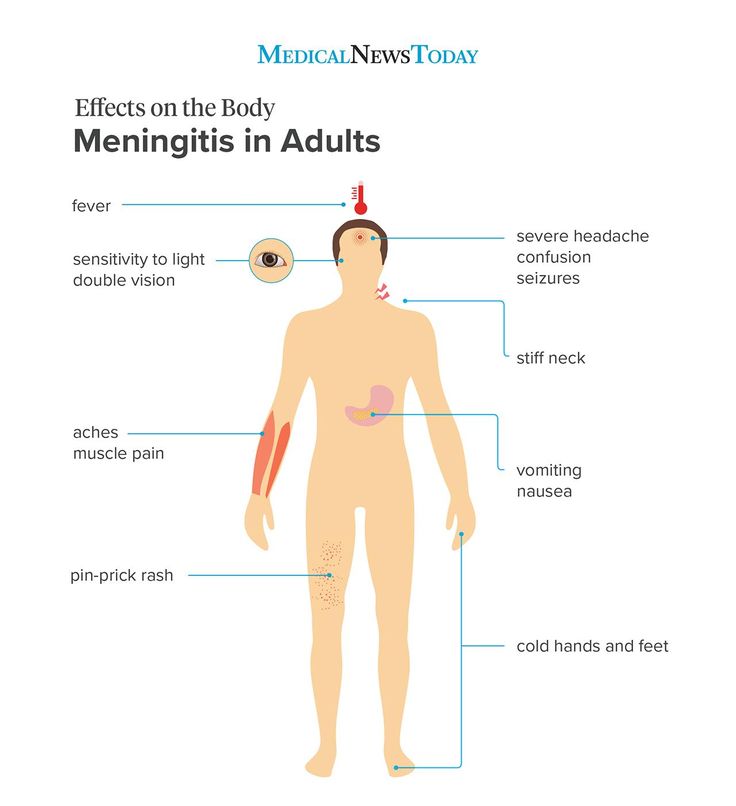 If it is near the time of the next dose, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up.
If it is near the time of the next dose, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up.
Store at room temperature away from light and moisture. Do not store in the bathroom. Keep all medications away from children and pets.
Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
Selected from data included with permission and copyrighted by First Databank, Inc. This copyrighted material has been downloaded from a licensed data provider and is not for distribution, except as may be authorized by the applicable terms of use.
CONDITIONS OF USE: The information in this database is intended to supplement, not substitute for, the expertise and judgment of healthcare professionals. The information is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects, nor should it be construed to indicate that use of a particular drug is safe, appropriate or effective for you or anyone else. A healthcare professional should be consulted before taking any drug, changing any diet or commencing or discontinuing any course of treatment.
A healthcare professional should be consulted before taking any drug, changing any diet or commencing or discontinuing any course of treatment.
Extrapyramidal symptoms and tardive dyskinesia in neuroleptic treatment
Although antipsychotics have become the cornerstone of the treatment of schizophrenia in recent decades, a number of motor disorders are associated with their use, which can be divided into two main groups: extrapyramidal symptoms (EPS) and tardive dyskinesia (TD).
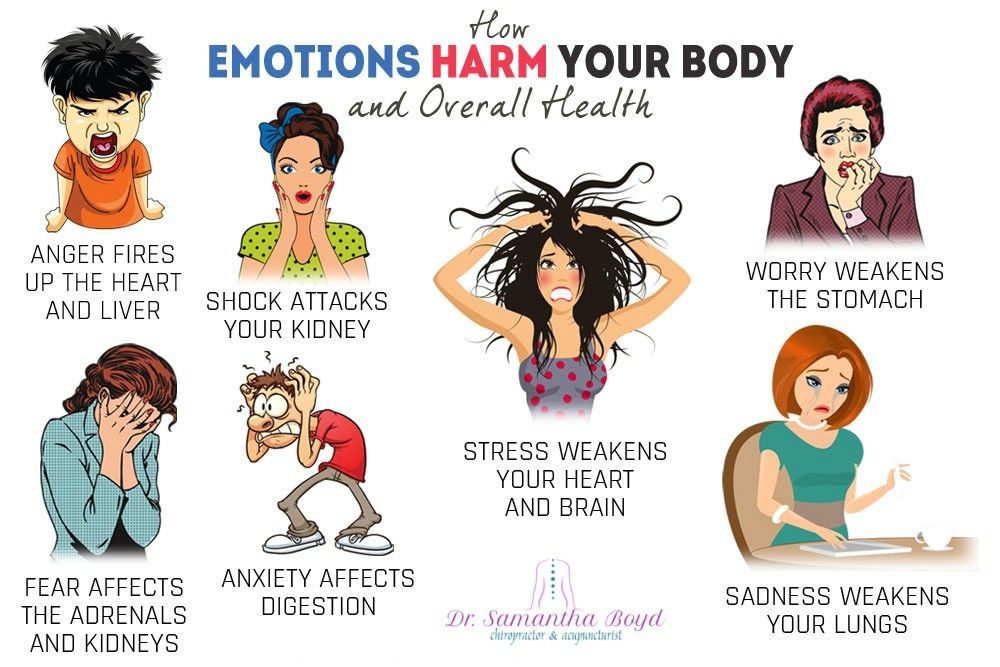
Extrapyramidal symptoms include akathisia, dystonia, drug-induced parkinsonism and may occur during the first days (weeks) after the appointment of an antipsychotic or increase in its dose, and later. Depending on their severity and persistence, EPS can cause discomfort, impaired functioning, stigmatization, reduced adherence to antipsychotics, and somatic complications (eg, injuries due to falls due to parkinsonism). nine0004
A recent meta-analysis of double-blind, randomized controlled trials comparing atypical antipsychotics to conventional antipsychotics, including CATIE (Clinical Antipsychotic Trials of Intervention Effectiveness), showed that all atypical antipsychotics have a lower risk of developing EPS than haloperidol.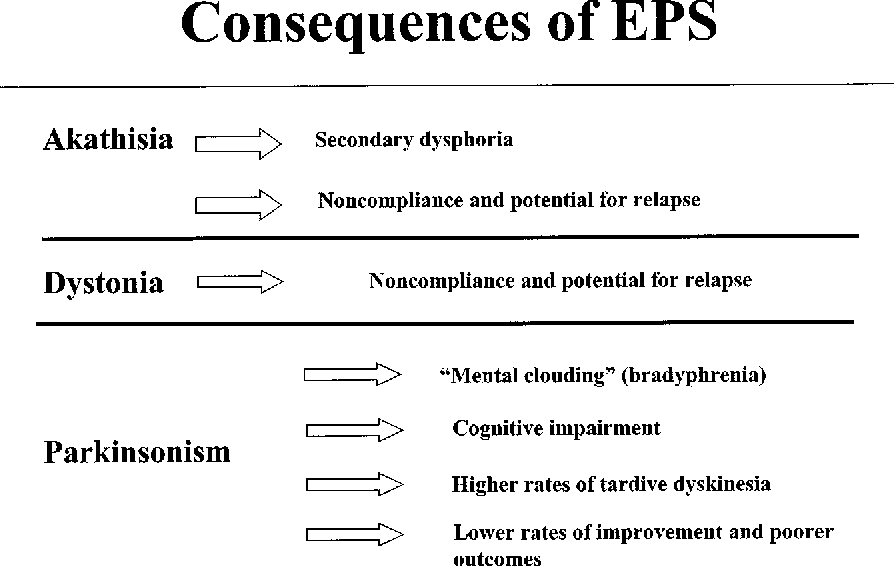 However, only patients treated with olanzapine, clozapine, and risperidone had a lower risk of EPS than patients treated with low-potency typical antipsychotics. These results are consistent with the individual profile of typical and atypical drugs in relation to EPS, which emphasizes the need to take into account the tolerability of individual drugs rather than entire classes of psychotropic drugs. So, young people, apparently, are more susceptible to the development of acute dystonia, and elderly patients - drug-induced parkinsonism. Differences between antipsychotics in the EPS profile are attributed to differing mechanisms of action, including the degree of binding to D2-dopamine and serotonin type 2 receptors, as well as M-cholinergic receptors. The relative importance of these mechanisms may vary from drug to drug. nine0004
However, only patients treated with olanzapine, clozapine, and risperidone had a lower risk of EPS than patients treated with low-potency typical antipsychotics. These results are consistent with the individual profile of typical and atypical drugs in relation to EPS, which emphasizes the need to take into account the tolerability of individual drugs rather than entire classes of psychotropic drugs. So, young people, apparently, are more susceptible to the development of acute dystonia, and elderly patients - drug-induced parkinsonism. Differences between antipsychotics in the EPS profile are attributed to differing mechanisms of action, including the degree of binding to D2-dopamine and serotonin type 2 receptors, as well as M-cholinergic receptors. The relative importance of these mechanisms may vary from drug to drug. nine0004
Tardive dyskinesia (TD) is a persistent motor disorder that can be not only severe but also irreversible. It is believed that the risk of developing PD and the likelihood of its persistence increase as the duration of treatment and the total dose of the antipsychotic increase.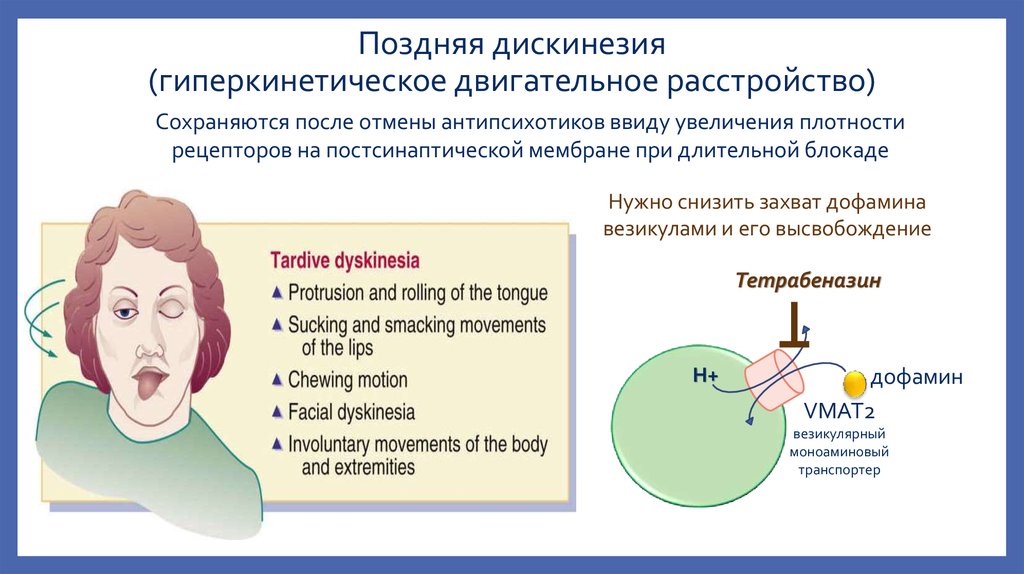 In addition, PD may develop, although rather rarely, after a relatively short period of treatment at low doses or after discontinuation of the drug. Tardive dyskinesia usually begins with abnormal movements of the lips and tongue, but may progress to involve other parts of the body, as well as manifest a wide range of involuntary movements. DD is a stigmatizing phenomenon. In its severe form, pronounced maladaptation is observed, associated with difficulties in eating, articulation, movement and breathing. Many risk factors contribute to the development of PD, including long-term use of antipsychotics and advanced age, as well as female sex in the elderly, comorbid affective disorders, acute EPS, race, and diabetes mellitus. The mechanism supposedly underlying tardive dyskinesia is due to prolonged blockade of postsynaptic dopamine receptors, dopamine hypersensitivity, damage during neuroleptic therapy of striatal interneurons mediated by gamma-aminobutyric acid or acetylcholine. One meta-analysis found that patients treated with atypicals had a lower risk of PD compared with patients treated with haloperidol.
In addition, PD may develop, although rather rarely, after a relatively short period of treatment at low doses or after discontinuation of the drug. Tardive dyskinesia usually begins with abnormal movements of the lips and tongue, but may progress to involve other parts of the body, as well as manifest a wide range of involuntary movements. DD is a stigmatizing phenomenon. In its severe form, pronounced maladaptation is observed, associated with difficulties in eating, articulation, movement and breathing. Many risk factors contribute to the development of PD, including long-term use of antipsychotics and advanced age, as well as female sex in the elderly, comorbid affective disorders, acute EPS, race, and diabetes mellitus. The mechanism supposedly underlying tardive dyskinesia is due to prolonged blockade of postsynaptic dopamine receptors, dopamine hypersensitivity, damage during neuroleptic therapy of striatal interneurons mediated by gamma-aminobutyric acid or acetylcholine. One meta-analysis found that patients treated with atypicals had a lower risk of PD compared with patients treated with haloperidol. It is assumed that this is due to a less pronounced blockade of D2 receptors in the basal ganglia, as well as a low probability of postsynaptic dopaminergic hypersensitivity. Atypical antipsychotics also differ in their ability to cause PD. So, according to the results of a prospective, observational study of outcomes in patients with schizophrenia, performed by D.Novick et al. (2010), patients treated with typical antipsychotics (oral or depot), amisulpride, risperidone, or clozapine were more likely to develop EPS than those treated with olanzapine. The severity of disease at the first visit (as measured by the Global Clinical Assessment Scale) was associated with a higher risk of developing EPS during the follow-up period. The authors of the study found that, compared with olanzapine as a reference drug, when taking risperidone and typical antipsychotics (oral or in depot form), the risk of developing PD is also higher. Factors associated with the risk of developing PD at baseline were age, EPS, a higher negative score on the global clinical assessment scale, and gynecomastia.
It is assumed that this is due to a less pronounced blockade of D2 receptors in the basal ganglia, as well as a low probability of postsynaptic dopaminergic hypersensitivity. Atypical antipsychotics also differ in their ability to cause PD. So, according to the results of a prospective, observational study of outcomes in patients with schizophrenia, performed by D.Novick et al. (2010), patients treated with typical antipsychotics (oral or depot), amisulpride, risperidone, or clozapine were more likely to develop EPS than those treated with olanzapine. The severity of disease at the first visit (as measured by the Global Clinical Assessment Scale) was associated with a higher risk of developing EPS during the follow-up period. The authors of the study found that, compared with olanzapine as a reference drug, when taking risperidone and typical antipsychotics (oral or in depot form), the risk of developing PD is also higher. Factors associated with the risk of developing PD at baseline were age, EPS, a higher negative score on the global clinical assessment scale, and gynecomastia.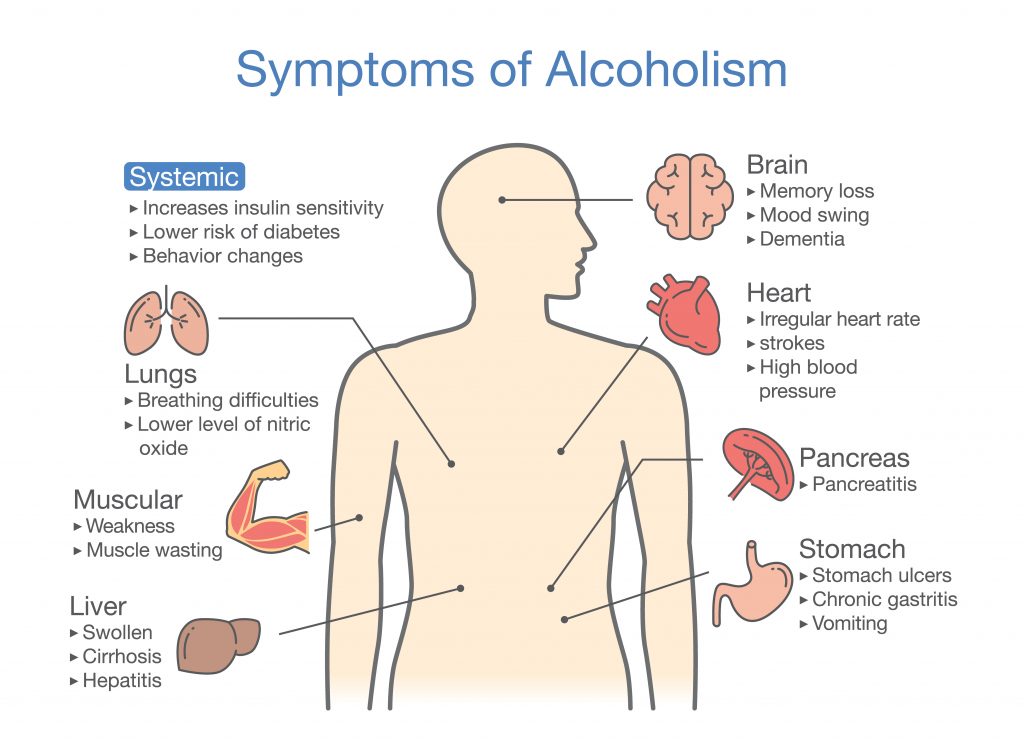 nine0004
nine0004
more details in the article " Drug dyskinesias " O.S. Levin, Department of Neurology, RMAPE, Center for Extrapyramidal Diseases (Journal "Modern Therapy in Psychiatry and Neurology" No. 3, 2014) [read]
Phoenix
The involuntary facial expressions and awkward movements caused by tardive dyskinesia keep many people with this disease behind closed doors. In addition, DYSKINESIA can also affect breathing and nutrition. Let's consider in more detail. nine0004
Tardive dyskinesia is a disease caused by the use of antipsychotics or neuroleptics.
These drugs are used primarily to treat symptoms associated with serious mental illness such as schizophrenia and bipolar disorder, but are also used to treat nervous system disorders, allergies, seizures, anxiety, and gastrointestinal problems.
Movement disorders are difficult to live with and are becoming more common as the drugs that cause them are prescribed to a growing number of children and the elderly, two groups particularly vulnerable to complex side effects. nine0004
nine0004
Various movement disorders have been associated with dopamine receptor blocking drugs, also known as neuroleptics, ranging from mildly embarrassing facial tics and/or unpleasant seizures to life-threatening respiratory dyskinesia and associated eating problems that can potentially have catastrophic consequences for patients.
Dyskinesia affects the nervous system, causing involuntary and sometimes painful movements that can be felt as excruciating spasms. Also, this disorder can lead to protruding tongue, wrinkling of the mouth and smacking of the lips. Rapid twitching of the arms, legs, and feet is another unwanted side effect. In the most advanced cases, it can also affect speech and lead to restless sleep with frequent awakenings. nine0038 The embarrassment experienced by people with dyskinesia can be a very heavy burden, as can uncontrolled physical movements, it can lead to social isolation and depression.
Impact of tardive dyskinesia on respiratory function and nutrition
Tardive dyskinesia occurs in 20-50% of patients receiving antipsychotics.
What is known is that the risk increases with the age of the person taking the medication and with the duration of the medication. The risk of dyskinesia is also high in older female patients. Breathing and eating problems can lead to severe disability and negatively affect a person's quality of life. nine0004
More than 27% of patients surveyed who had symptoms consistent with dyskinesia reported that uncontrolled movements made it difficult to eat.
And almost 9% said that the symptoms affect their breathing.
Drinking diet and other difficulties
Patients describe the effect of dyskinesia on eating as if the muscles involved in swallowing are not as coordinated as they used to be. From dyskinesia, the neck is compressed, but internal discomfort is also felt. There are malfunctions in the gastrointestinal system. Eating with dyskinesia is a real test. nine0004
Extreme care must be taken to avoid suffocation. You need to eat very slowly and not swallow too large pieces. Drinking diets are sometimes prescribed for people with dyskinesia difficulties. Swallowing problems can cause aspiration, the potentially dangerous result of food or liquid getting into the lungs (where it can cause infection) rather than into the esophagus and stomach, where they belong. Aspiration pneumonia is another ongoing concern because, in severe cases, it can lead to long-term lung damage. nine0004
Drinking diets are sometimes prescribed for people with dyskinesia difficulties. Swallowing problems can cause aspiration, the potentially dangerous result of food or liquid getting into the lungs (where it can cause infection) rather than into the esophagus and stomach, where they belong. Aspiration pneumonia is another ongoing concern because, in severe cases, it can lead to long-term lung damage. nine0004
Patients also sometimes experience severe nausea and intestinal cramps, which are prominent in the first years after diagnosis but are still present over time.
Problems with eating and swallowing are usually not chronic and resolve over time.
Respiratory problems with dyskinesia
From time to time, patients experience unpleasant spasms in the diaphragm at the most unexpected moments. Ironically, painful spasms can happen when a person is as relaxed as possible. For example, when a person is just resting or even during sleep. It's usually just one spasmodic inhalation and exhalation, but it can lead to serious anxiety.