Cognitive behavioural therapy for schizophrenia
Cognitive Behavioral Therapy (CBT) for Schizophrenia
Diagnosis: Schizophrenia and Other Severe Mental Illnesses
Treatment: Cognitive Behavioral Therapy (CBT) for Schizophrenia
Brief Summary
Cognitive Behavioral Therapy (CBT) for Schizophrenia
Status: Strong Research Support
What does this mean?
Description
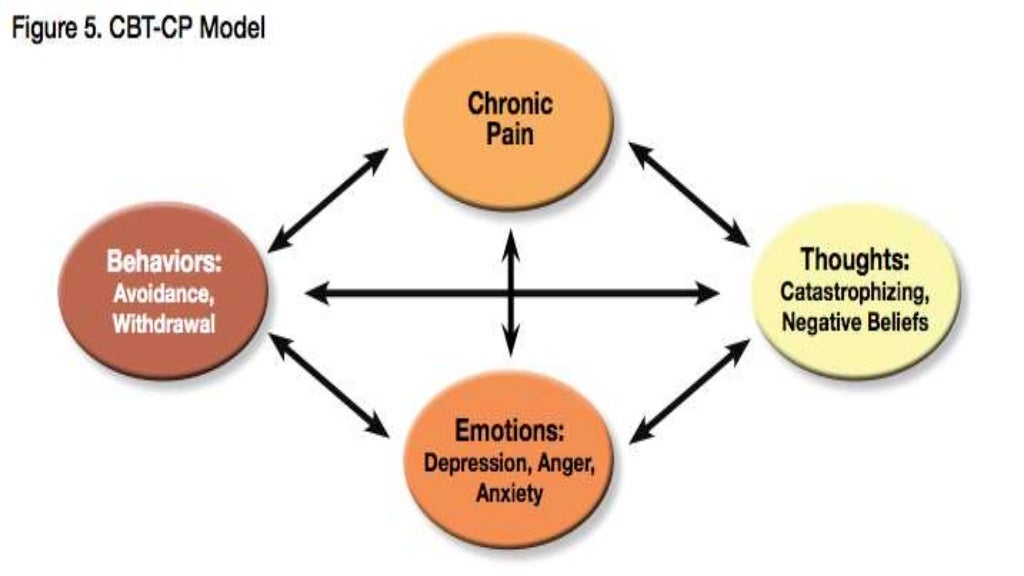
Similar to Cognitive-Behavioral Therapy (CBT) for other types of problems, CBT for schizophrenia involves establishing a collaborative therapeutic relationship, developing a shared understanding of the problem, setting goals, and teaching the person techniques or strategies to reduce or manage their symptoms. Therapy is usually conducted in individual sessions and is time-limited (typically several months). The goal is not to “cure” schizophrenia, but rather to improve the person’s ability to function independently, manage their schizophrenia, and to reduce the distress they experience in their daily life.
Specific CBT approaches used in treating schizophrenia include cognitive restructuring, behavioral experiments / reality testing, self-monitoring and coping skills training. Unique considerations in treating schizophrenia include emphases on being non-confrontational and on normalizing psychotic experiences insomuch as they are on a continuum with non-psychotic experiences. CBT for schizophrenia can focus specifically on psychotic symptoms (i.e. hallucinations or delusional beliefs) but has also been shown to be helpful for addressing depression and / or anxiety associated with psychotic symptoms and their impact on the person’s life.
Key References (in reverse chronological order)
- Dickerson, F.B. (2004). Update on cognitive behavioral psychotherapy for schizophrenia: Review of recent studies. Journal of Cognitive Psychotherapy: An International Quarterly.
- Rector, N.A.; Seeman, M.V.; and Segal, Z.V. Cognitive therapy for schizophrenia: A preliminary randomized controlled trial.
 Schizophrenia Research, 63:1-11, 2003.
Schizophrenia Research, 63:1-11, 2003. - Rector, N.A. & Beck, A.T. (2001). Cognitive Behavioral Therapy for schizophrenia: An empirical review. The Journal of Nervous and Mental Disease, 189 (5) 278-287.
- Barrowclough, C.; Haddock, G.; Tarrier, N.; Lewis, S.W.; Moring, J.; O’Brien, R.; Schofield, N.; and McGovern, J. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. American Journal of Psychiatry, 158: 1706-13, 2001.
- Pinto, A.;La Pia, S.; Menella, R.; Giorgio, D.; and DeSimone, L. Cognitive-behavioral therapy and clozapine for clients with treatment-refractory schizophrenia. Psychiatric Services, 50: 901-4, 1999.
- Dickerson, F.B. (2000) Cognitive behavioral psychotherapy for schizophrenia: A review of recent empirical studies. Schizophrenia Research, 16:71-90.
- Sensky, T.; Turkington, D.
 ; Kingdon, D.; Scott, J.L.; Scott, J.; Siddle, R.; O’Carroll, M.; and Barnes, T.R.E. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Archives of General Psychiatry, 57: 165-72, 2000.
; Kingdon, D.; Scott, J.L.; Scott, J.; Siddle, R.; O’Carroll, M.; and Barnes, T.R.E. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Archives of General Psychiatry, 57: 165-72, 2000. - Wykes, T.; Parr, A.; and Landau, S. Group treatment of auditory hallucinations: Exploratory study of effectiveness. British Journal of Psychiatry, 175: 180-5, 1999.
- Tarrier, N., L.; Yusupoff, L.; Kinney, C.; McCarthy, E.; Gledhill, A.; Haddock, G.; and Morris, J. Randomised controlled trial of intensive cognitive behaviour therapy for patients with chronic schizophrenia. British Medical Journal, 317: 303-7, 1998.
- Tarrier, N.; Beckett, R.; Harwood, S.; Baker, A; Yusupoff, L.; and Ugarteburu, I. A trial of two cognitive-behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients: I. Outcome. British Journal of Psychiatry, 162: 524-32, 1993.
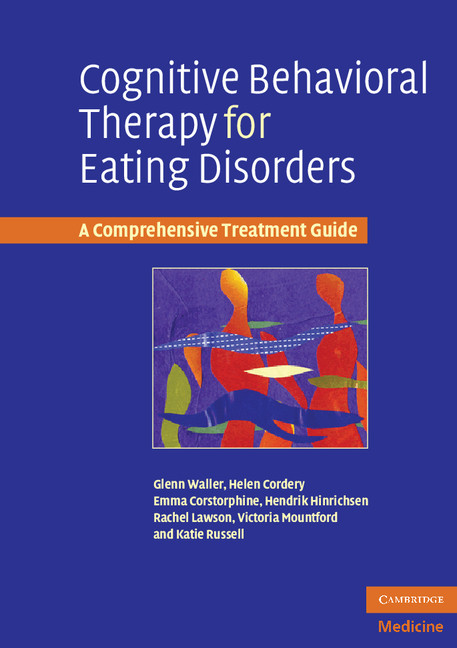
Clinical Resources
- Kingdon, D.G. & Turkington, D. (2005). Cognitive Therapy of Schizophrenia. Guilford, New York.
- Chadwick, P., Birchwood, M.J., & Trower, P. (1999). Cognitive Therapy for Delusions, Voices and Paranoia (Wiley Series in Clinical Psychology). Wiley.
- Kingdon, D.G. & Turkington, D. (1994). Cognitive-Behavioral Therapy of Schizophrenia. Guilford Press, New York.
Training Opportunities
| Beck Institute for Cognitive Therapy and Research One Belmont Avenue, Suite 700 Bala Cynwyd, PA 19004-1610 Phone: 610-664-3020 http://www.beckinstitute.org | Center for Cognitive Therapy Mary Anne Layden, Ph.D. Director of Education Center for Cognitive Therapy 3535 Market Street, 2nd Floor Philadelphia, PA 19104-3309 http://www.uphs.upenn.edu/psycct |
Treatment Resources
Note: The resources provided below are intended to supplement not replace foundational training in mental health treatment and evidence-based practice
Treatment Manuals Training Resources Measures, Handouts and Worksheets Self-help Books Smartphone Apps Video Demonstrations Video Descriptions Clinical Trials Meta-Analyses and Systematic Reviews Other Treatment Resources
Cognitive Behavioral Therapy for Schizophrenia
- Cognitive behavioral therapy is a limited-term talk therapy technique.
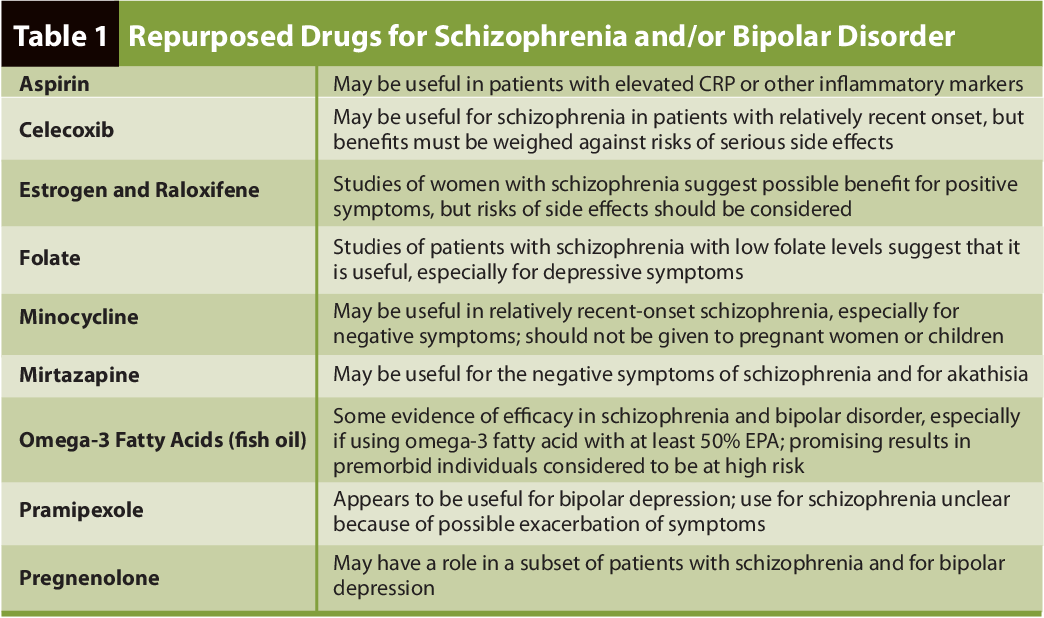
- This type of therapy is often used along with medications for schizophrenia as part of a treatment plan.
- Cognitive behavioral therapy may help those with schizophrenia manage their symptoms.
Cognitive behavioral therapy (CBT) is a type of talk therapy used to treat a variety of mental health conditions, including schizophrenia.
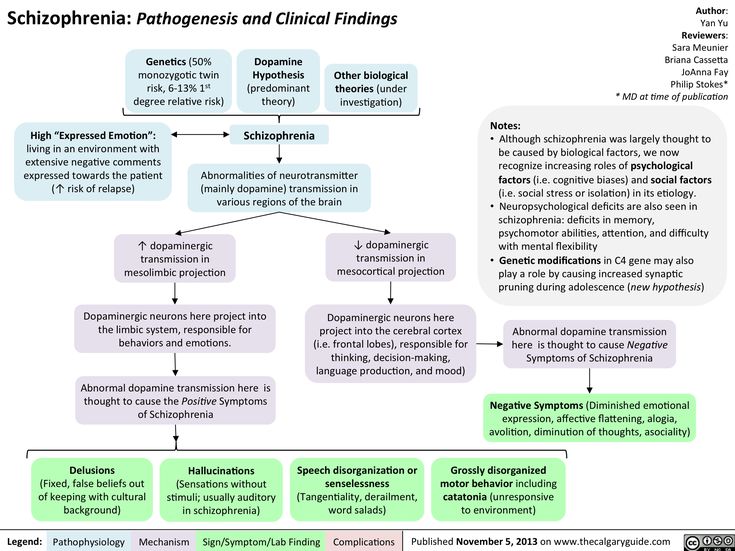
Schizophrenia is complex and lasts a lifetime. You may experience symptoms that include an inability to think clearly, have emotional regularity, interact with others, or make decisions.
Often medication is the first line of treatment for this condition. CBT may be useful as an additional therapy, though.
So, if you’re living with schizophrenia, CBT may help you manage your symptoms.
According to a 2014 review, studies have found that CBT for psychosis is most effective for reducing positive (presenting) symptoms like:
- hallucinations
- delusions
- confused thoughts
- altered speech
- difficulty focusing
- altered movement
Research from 2018 suggests that CBT may help moderate these symptoms in addition to medication. It may also help if the medication alone doesn’t improve symptoms.
It may also help if the medication alone doesn’t improve symptoms.
CBT may also help with negative (absent) symptoms like blank facial expressions, withdrawn speech, and disinterest, according to some clinical practice guidelines. It could help you adhere to other treatments and understand your condition better too.
Newer research from 2020 is even examining using CBT through group therapy paired with an app to address negative symptoms with positive results. More research is needed in this area.
Cognitive behavioral therapy and medication
Many studies suggest that CBT is a useful additional treatment for schizophrenia. In general, the first line of treatment is medication. These can be medications you take daily or less regularly, depending on the type.
Medication and CBT can help someone with this condition adhere to treatment, improve functioning, and avoid relapse. Support from family and peers can also help with this condition.
There is a lack of research on the effectiveness of CBT for schizophrenia without medication.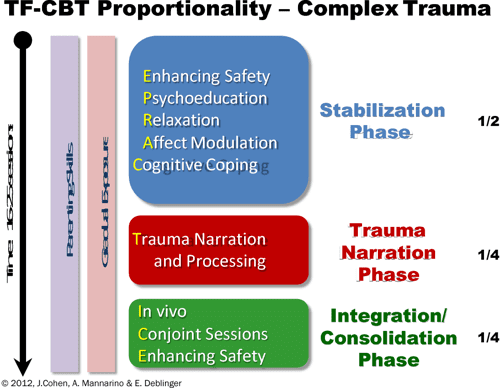
This is because most people with the condition require medication for treatment. Withholding medication to treat the condition to study the effectiveness of CBT alone may be considered unethical.
CBT occurs when a trained professional like a therapist, counselor, or social worker uses specific talk therapy to work through mental health concerns with you.
These concerns may involve:
- your inner thoughts
- your emotional responses
- your actions surrounding them
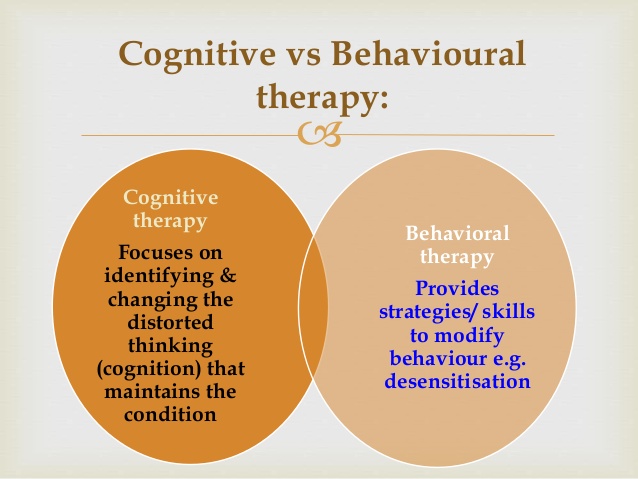
The cognitive part of the therapy relates to your thoughts and emotions. The behavioral part relates to your actions.
A facilitator listens as you speak and asks questions that push you past limiting and self-destructive thoughts so you can achieve personal goals. The process may even involve activities outside of one-on-one sessions that you try and then report back to your facilitator.
CBT can work for people with many types of mental health conditions. Researchers continue to develop studies examining the effectiveness of CBT and schizophrenia.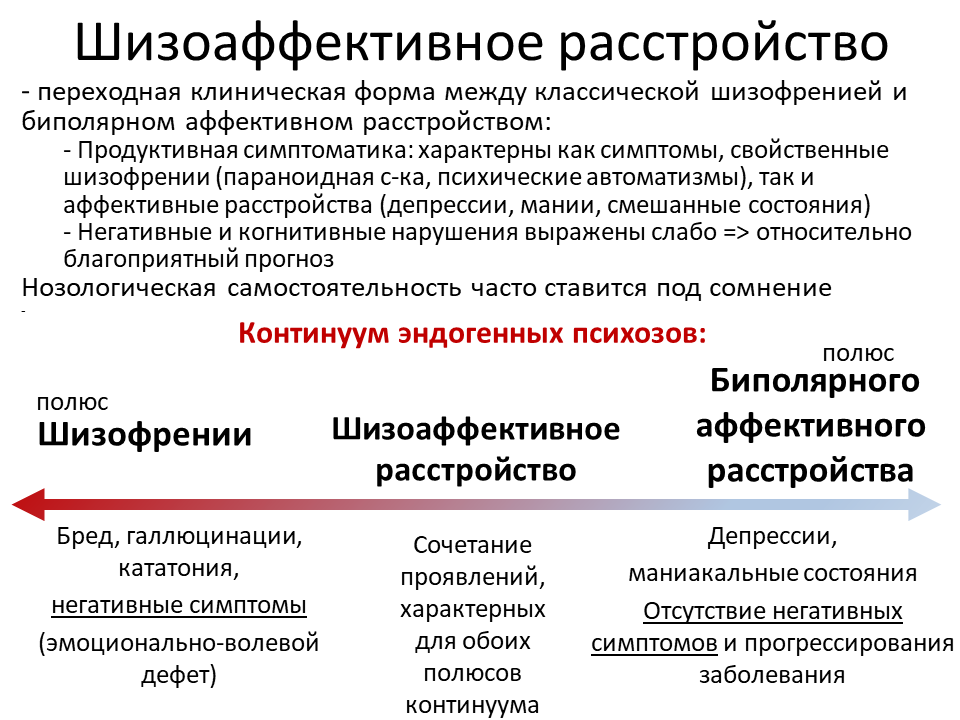
CBT may involve several objectives. You and your facilitator should identify these together.
Objectives may include:
- reducing symptoms
- working through the stigma of the condition
- avoiding relapse
- managing other conditions that may occur, like depression and anxiety
- accepting the condition
- acknowledging that symptoms like hallucinations and delusions are from the condition
It’s important that you and the facilitator create a trusting relationship, with boundaries and general rules established, before you begin treatment.
CBT may last between 6 and 9 months for about 20 sessions in total. These often last for an hour and are generally one-on-one sessions between you and the facilitator.
CBT can occur in person as in-patient or out-patient care. You can even try it via telemedicine through a computer or smartphone.
You may also benefit from CBT with another person. For example, you may want to include a family member.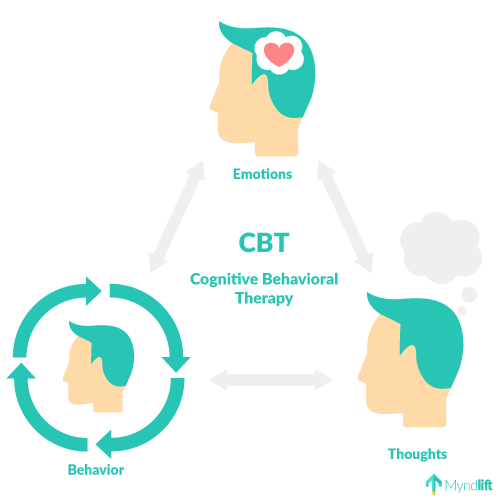
Your first sessions will explore your condition and your general outlook. The facilitator will suggest ways to reframe your thinking with new behaviors.
Over time, you’ll evaluate the issues you’ve been working on and determine whether you’re now responding to them differently.
The facilitator will also work with you at the end of your CBT timeline to make sure you keep applying new ways of thinking to future situations.
A typical CBT session might look like:
- check-in about current mental outlook
- discussion of current medication status
- follow-up on topics discussed in previous sessions
- discussion as set by an agenda for the session
- reflections from you
- feedback and active listening from the facilitator
- instructions for how to introduce changes in behavior
- homework assignments to test these behavioral modifications
- overview of how to journal outside of the session to record negative thoughts or symptoms
The facilitator may also engage you in several exercises during the feedback stage of the session. These may include:
These may include:
- identifying your thoughts and beliefs
- challenging your thoughts
- conducting behavioral experiments
- suggesting imagery
- making pro and con lists
- scheduling your activities
- engaging in role plays
These are just some of the facilitator’s options for helping you work through your thoughts.
Here are some ways you can find a facilitator for CBT:
- Talk with your doctor, who can give you a referral.
- Conduct internet searches.
- Ask for a referral from someone you know.
- Post a question on a social media community site for recommendations.
- Contact your insurance provider for therapists covered by your plan.
CBT is one way to help treat the symptoms of schizophrenia. It’s often combined with medications.
In CBT, you’ll work with a facilitator to discuss negative thoughts and change your behaviors and mindset.
This can help you cope with symptoms, accept your diagnosis, and adhere to your broader treatment plan.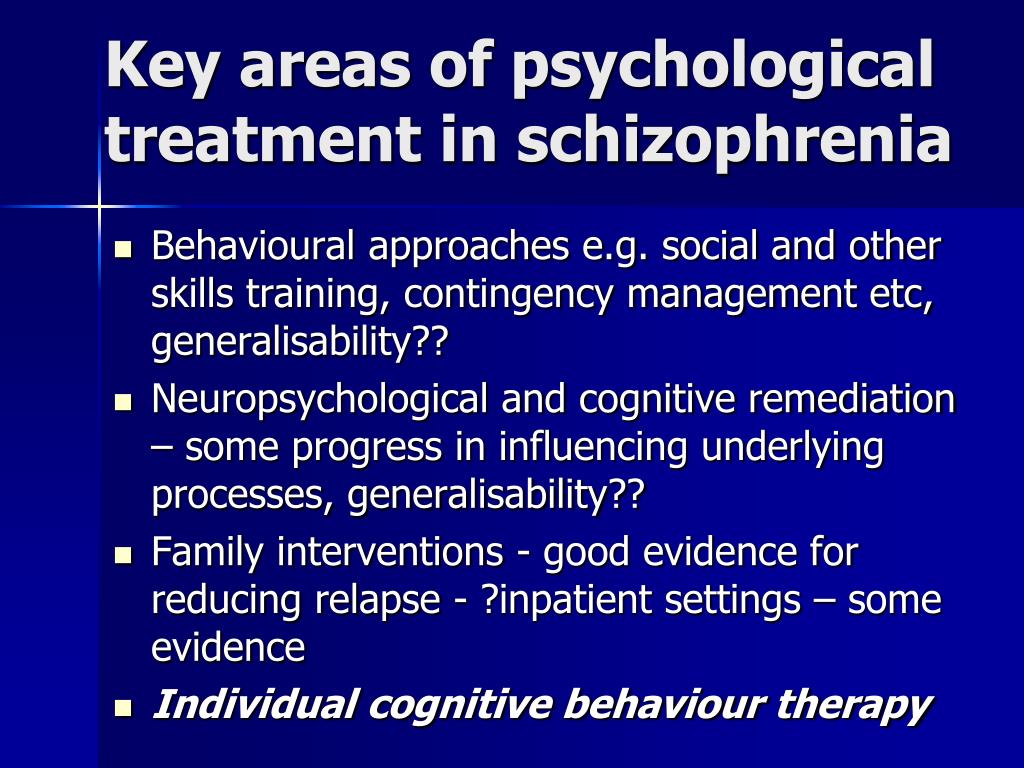
Cognitive Behavioral Therapy for Schizophrenic Patients
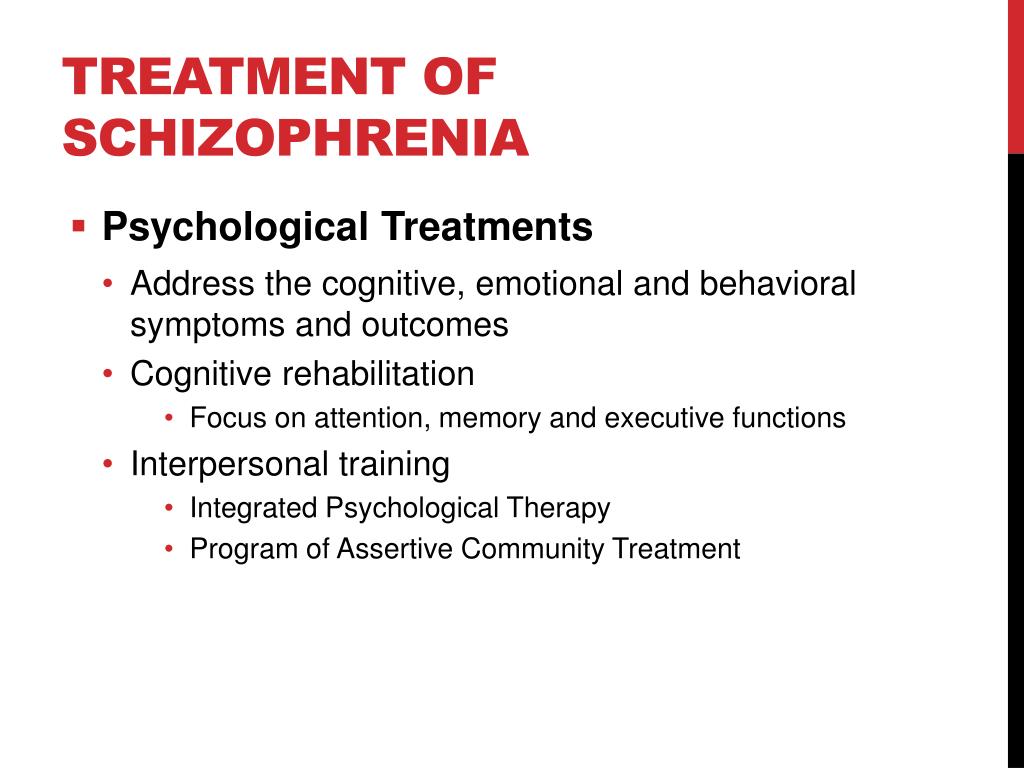
Cognitive Behavioral Therapy (CBT) is predominantly used in our clinic for schizophrenia. It is CBT that is recommended by most European and American societies as a proven and effective type of psychotherapy for schizophrenia. Cognitive behavioral therapy is a method that combines a cognitive and behavioral approach.
Cognitive psychotherapy is aimed at changing the processes of perception and thinking. During the sessions, patients clarify the relationship between their thoughts and emotions, analyze the most common cognitive errors and form thinking control skills. nine0004
Behavioral psychotherapy deals with the relationship between behavior, emotions and thinking. In behavioral psychotherapy, the patient's behavior is analyzed in various situations, after which the psychotherapist gives recommendations for its adjustment. The combination of these areas provides the most effective psychotherapeutic work with schizophrenia.
The main tasks of cognitive-behavioral psychotherapy in schizophrenia:
1. Formation of a critical assessment of delusional ideas
Psychotherapy is aimed at reducing the severity of delusions and developing a critical attitude towards delusional ideas. To solve this problem, metacognitive trainings are used (method of Stefan Moritz, University Hospital Hamburg-Eppendorf). Thanks to these trainings, a schizophrenic patient begins to realize errors in thinking that lead to delirium.
2. Work on the awareness of the disease and the formation of motivation for treatment.
As the psychosis emerges, the patient gradually becomes aware that he was ill and that his distorted perceptions and unusual thoughts were due to the illness. Some patients deny their illness, consider it "a special condition that allows you to see the world differently", or a manifestation of extrasensory abilities, or associate it with religion.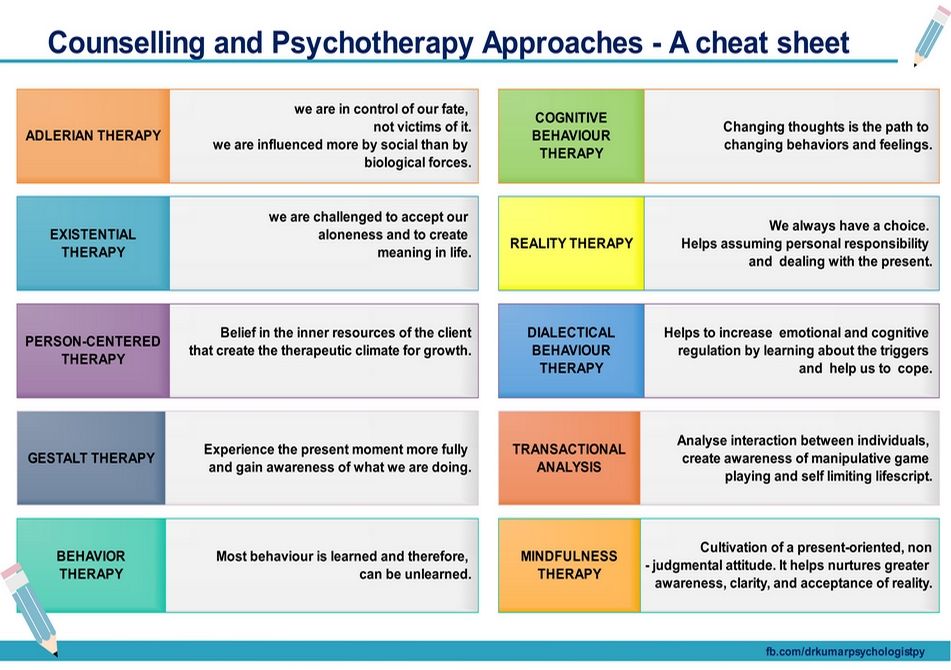 nine0003 If the patient does not understand that he is sick, he will not be treated, and he will develop exacerbations again and again.
nine0003 If the patient does not understand that he is sick, he will not be treated, and he will develop exacerbations again and again.
To understand the disease, it is necessary to show the patient that his case is not unique: other patients have similar symptoms that can be treated. Also, the patient must receive full information about the disease and its manifestations - this happens in psychoeducational classes.
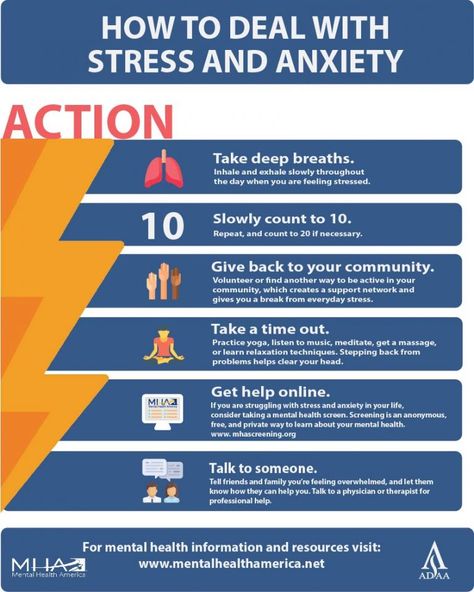
3. Stress and Emotion Management Training
Stress is one of the risk factors for relapse of schizophrenia, so it is important for the patient to learn how to manage their stress levels. During psychotherapeutic sessions, the patient develops a certain strategy of behavior in the event of difficult situations. At the same time, various techniques of cognitive-behavioral therapy, role-playing games, modeling situations, and relaxation trainings are used. nine0004
4. Training in planning skills, time management.
Problems of planning, forecasting and organizing one's time is a typical picture for schizophrenia.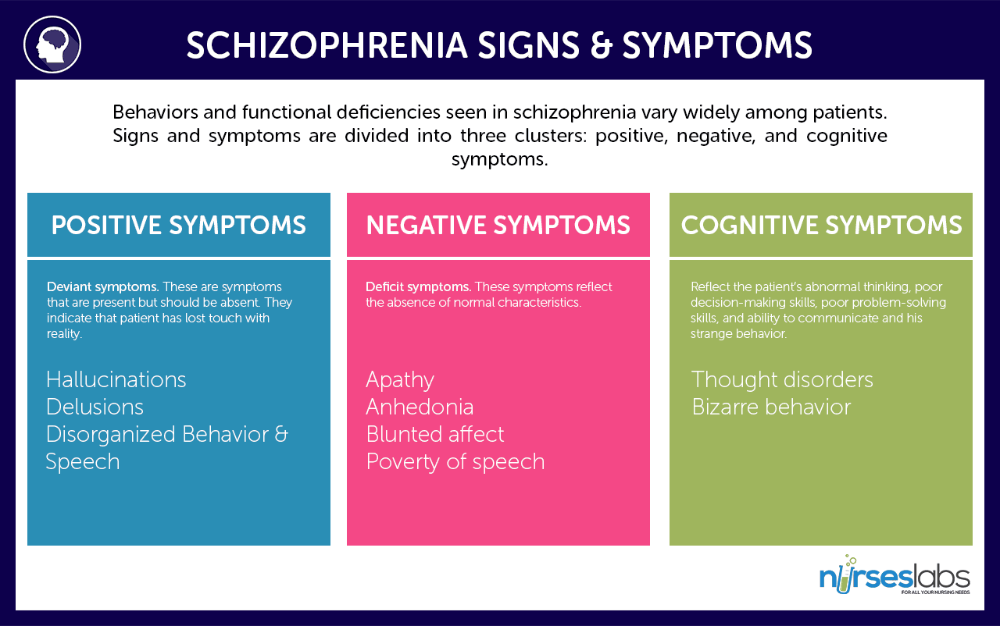 These problems are partly due to negative symptoms, partly due to the position of relatives who do not insist on the patient's employment, and in some cases seek to save the patient even from household chores. It is not uncommon for patients to sit at home and not do even simple household work. This negatively affects the sphere of thinking and the emotional-volitional sphere. nine0004
These problems are partly due to negative symptoms, partly due to the position of relatives who do not insist on the patient's employment, and in some cases seek to save the patient even from household chores. It is not uncommon for patients to sit at home and not do even simple household work. This negatively affects the sphere of thinking and the emotional-volitional sphere. nine0004
Training in planning and time management skills is important as part of social and labor rehabilitation - a process that allows the patient to return to a full life as much as possible.
5. Harmonization of relationships in the family
Difficult relationships with relatives and close people are also often a risk factor for exacerbation. Family psychotherapy in a cognitive-behavioral way allows you to reduce the level of stress in the family and improve relationships between its members. Also, relatives of the patient begin to better understand the features of the course of the disease, learn to recognize the symptoms of exacerbation and learn how to behave in this case.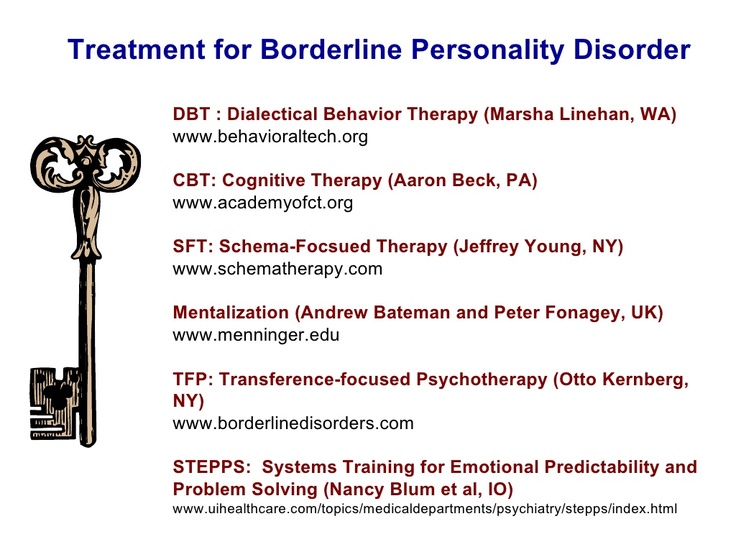 This type of psychotherapy makes it possible to build harmonious relationships without overprotection in the patient's family and reduce the risk of subsequent exacerbations. nine0004
This type of psychotherapy makes it possible to build harmonious relationships without overprotection in the patient's family and reduce the risk of subsequent exacerbations. nine0004
How does cognitive behavioral therapy work?
Psychotherapy is prescribed by a psychiatrist, who also controls the intermediate results and corrects the psychotherapy process if necessary.
In our clinic, cognitive-behavioral psychotherapy aimed at understanding the disease, working with delusions and overcoming stress is carried out by a clinical psychologist. A social psychologist works with families, organizational skills, conducts social trainings.
Cognitive Behavioral Therapy provides a psychotherapeutic contract that outlines the goals and timing of the therapy. In most cases, the psychologist gives homework for the next session. To get the result of therapy, you must complete these tasks. nine0004
Why psychotherapy may not help?
Clinical evidence has proven the effectiveness of CBT in all stages of schizophrenia.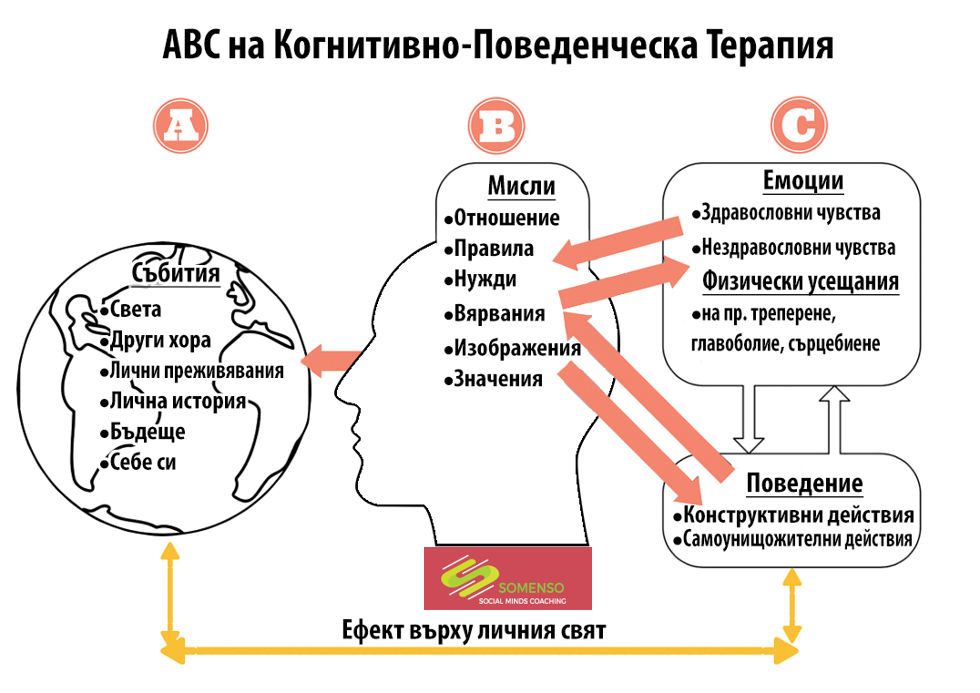 But in some cases, patients quit CBT after a few sessions. This happens if the expectations of the patient and his relatives do not correspond to reality.
But in some cases, patients quit CBT after a few sessions. This happens if the expectations of the patient and his relatives do not correspond to reality.
Firstly, no method of psychotherapy can completely correct the situation in a couple of sessions. In most cases, 15 to 30 sessions are needed to achieve results. nine0003 Secondly, the effectiveness of psychotherapy strongly depends on the position of the patient. It is important to understand that psychotherapy is, first of all, work on oneself, often difficult and painstaking. Without the intention to change and the effort to make that change, psychotherapy will only be a waste of time and money. The psychologist can show the way and give the tools to use in the process of therapy, but the very application of these tools is up to the client.
Do you need advice? nine0011 We know how to help! Call us
Tags:
Schizophrenia
Is CBT as effective as standard care for people with schizophrenia
Relevance
People with serious mental illness, such as schizophrenia, may experience severe disturbances in thought processes that can lead to perceptual delusions (beliefs that are not based on reality) and hallucinations (things the person sees or hears but is not aware of). actually no). The main (providing major support for the condition) treatment for schizophrenia is antipsychotic medication, but these are not always effective on their own, so complementary therapies such as psychosocial therapy (including cognitive behavioral therapy (CBT)) are also recommended for people with schizophrenia. The goal of CBT is for patients to rethink their view of symptoms. This therapy is believed to help reduce stress and change behavior. It is often used to help people who are prone to anxiety and depression. However, CBT is costly and its effectiveness has not yet been clearly proven, especially when used to treat people with schizophrenia. nine0004
actually no). The main (providing major support for the condition) treatment for schizophrenia is antipsychotic medication, but these are not always effective on their own, so complementary therapies such as psychosocial therapy (including cognitive behavioral therapy (CBT)) are also recommended for people with schizophrenia. The goal of CBT is for patients to rethink their view of symptoms. This therapy is believed to help reduce stress and change behavior. It is often used to help people who are prone to anxiety and depression. However, CBT is costly and its effectiveness has not yet been clearly proven, especially when used to treat people with schizophrenia. nine0004
Searches
Information Officer Cochrane Schizophrenia searched a specialized registry for trials where people with schizophrenia received CBT or standard care (the care a participant usually receives for their condition in the region where the clinical trial is conducted) up to March 2017. Total found 1730 entries. The reviewers reviewed and verified these records.
The reviewers reviewed and verified these records.
Main results
After the initial search, we were able to include 60 trials with 5992 participants. In these studies, people with schizophrenia were randomly assigned to either CBT added to standard care or to standard care only. The quality of the evidence for the main outcomes we are interested in was generally very low, or low at best. The results showed that adding CBT to standard care had no effect on the long-term risk of relapse. Only two clinical trials (82 participants) provided useful data for long-term health; these data indicated that CBT may be better for long-term improvement in general condition than standard care alone. The addition of CBT to standard care may reduce the risk of adverse events but does not appear to be superior to standard care for improving long-term mental status. Whether adding CBT to standard care improves a patient's quality of life or social functioning also remains unclear.