How to handle schizophrenia family members
How to Care for Your Loved One
Written by WebMD Editorial Contributors
Giving support to a family member or friend with schizophrenia means helping them get the medical and psychological treatment they need. But it also means taking care of yourself at the same time.
Use these suggestions to make an action plan that works for both of you.
Educate Yourself
Schizophrenia is a difficult mental illness to understand. So learn as much as you can. The more information you have, the better prepared you will be to deal with it.
You’ll also be better able to support your friend or family member who has schizophrenia. And that can boost the odds that they will stick with their treatment, even when things get tough.
Be Goal-Oriented
A doctor will set up a wellness plan with your loved one that will include specific goals. If you’re not sure who to call to get treatment started, try your family doctor, who may refer you to a psychiatrist.
Your job as a caregiver is to remind your loved one how important it is to stick to their goals, and to encourage them to stay on their medication. They need to follow their treatment plan to help prevent the disease from coming back and keep their symptoms from getting worse.
Keep Track of Details
Go to all doctor appointments with your loved one. It will make it easier for you to help them with their treatment plan. Ask their doctor as many questions as you need, and keep details. Remember: The doctor is there to help both of you.
Also, take notes to every appointment. Some things to include are:
- Your loved one’s recent symptoms (what they are and when they started)
- Any other medical conditions they may have
- New sources of stress (These can include major life changes.)
- Medications, vitamins, herbs, or any other supplements that they have taken, as well as the dosage
Join Support Groups
Encourage your family member or friend to join a group, and make sure they get to the meetings. In these support groups, they will be among other people with schizophrenia who will share their experiences. It may help them feel less alone.
It may help them feel less alone.
The Schizophrenia and Related Disorders Alliance of America (SARDAA) and National Alliance on Mental Illness (NAMI) offer support.
Learn How to Manage Stress
Activities like yoga, tai chi, and meditation can make both of you feel more relaxed. Try to do them regularly so you can use them in a crisis.
Learn How to Respond
When someone with schizophrenia has hallucinations (hears or sees things that aren’t there) or delusions (believes things that aren’t true, even when they get proof that they’re false), they believe they are real. It doesn’t help them to challenge their beliefs by saying they’re not.
Instead, tell them that you each see things in your own way. Be respectful, kind, and supportive, and call their doctor if needed.
If they are acting out hallucinations, stay calm, call 911, and tell the dispatcher they have schizophrenia. While you wait for paramedics, don’t argue, shout, criticize, threaten, block the doorway, touch them, or stand over them. Also avoid direct eye contact, which could make them feel threatened.
Also avoid direct eye contact, which could make them feel threatened.
Be Ready to Respond
If a person with schizophrenia has a psychotic episode, which means their hallucinations or delusions become a lot worse and more severe, you need to size up the situation quickly and decide who to call. If another person is available, ask them to stay with your loved one while you contact the doctor or call 911.
If your loved one threatens suicide, don’t leave them alone. If their behavior becomes dangerous, immediately call 911 and ask for police. Tell them they have schizophrenia and explain the situation, but let them handle it. Police should be trained to evaluate and manage people with psychotic disorders and other types of emotional distress. Call their doctor to let them know what’s going on as well.
On your smartphone, you can also download the Psychiatric Crisis Resources Kit app (from the Treatment Advocacy Center). It has state-specific standards on emergency hospitalization and can be useful in a crisis.
Know the Signs of Suicide
Most people with schizophrenia are harmless to others. They’re more likely to hurt themselves than anybody else. Sometimes that includes trying to take their own life. You should take any suicidal talk seriously, and pay attention to poems, notes, or any other things your loved one creates that are about death.
Also, be suspicious if they suddenly go from depressed to cheerful. This change could mean they are thinking about suicide. For help on the spot, call your doctor and the National Suicide Prevention Lifeline at 800-273-8255.
Stay in Touch
When a person with schizophrenia feels alone, their suicidal thoughts may increase. If you don’t live close by, you can help by staying in touch via telephone, text, email, and mail. Sending short notes like postcards and greeting cards can remind them how much you care.
Take Care of Yourself
It can be draining to look after someone with schizophrenia. You need to make nurturing yourself a top priority every day. It’s common for caregivers to feel sad, angry, alone, or afraid of what others will think.
It’s common for caregivers to feel sad, angry, alone, or afraid of what others will think.
Reach out to friends and family, and tell them what you need. They can:
- Listen to you without judging you
- Find information and doctors
- Share hopeful stories, moral support, and spiritual guidance
- Offer financial assistance
- Do your housework and babysit your kids
Most of all, eat well, get enough sleep, exercise, and take part in fun activities. You can’t be “on call” 24 hours a day. So schedule guilt-free vacations and give yourself a complete break from time to time.
Learn About the Stigma of Mental Illness
The stigma of mental illness still exists, even though society has become more accepting and understanding of mental health issues in recent years.
Families of people who have a mental illness can take certain steps to cope with it:
- Remember that you and your loved ones have choices. Mental and physical illnesses are private, personal information.
 You can decide who to tell about the mental illness and what to tell them.
You can decide who to tell about the mental illness and what to tell them. - Remember that you are not alone. Mental health problems can be more common than you might think. One in four people in the United States has some form of mental illness at some point in their lives. Many other people cope with similar situations. People commonly struggle with depression, anxiety, substance abuse, and other mental health disorders.
- Stay hopeful, and remember that treatment works. Safe and effective medications and psychosocial treatments are available, and newer treatments are being developed. As a result, many people who have a mental illness enjoy productive lives.
- Praise your loved one for seeking help. Mental health treatment can be difficult, as people often need to be patient in trying new medications, coping with side effects, and learning new behaviors. Helping your loved one to feel good about them or themselves is important.
- Stay active, and surround yourself with supportive people. Social isolation can be a negative side effect of the stigma linked to mental illness. Isolating yourself and not doing the things you enjoy put you at high risk for depression and burnout. Take a risk, and try new activities in your community.
Someone I love has been diagnosed with schizophrenia. How can I help?
Author: Canadian Mental Health Association, BC Division
We naturally want to help a loved one who isn’t feeling well. How we can or should help may seem fairly obvious when a loved one experiences a physical health problem, but many people say they’re not sure how to best help when a loved one experiences a mental illness like schizophrenia. Here are some tips:
Educate yourself
You don’t have to be an expert in schizophrenia, but learning more can help you understand what’s going on. There are a lot of myths about schizophrenia, so it’s a good idea to find some trustworthy resources. Our Schizophrenia info sheet is a great place to start. You can also find a lot of information from the BC Schizophrenia Society.
Our Schizophrenia info sheet is a great place to start. You can also find a lot of information from the BC Schizophrenia Society.
Listen
Sometimes talking about problems or concerns can really help. It’s important to understand that talking about something difficult like experiences of schizophrenia can be very hard for your loved one—and the symptoms of schizophrenia can also make conversations difficult. If a loved one opens up to you, listen actively—that is, without distractions like your phone or the TV. Really pay attention to what they have to say. Give them time to finish their thoughts, even if it takes a bit longer than usual. Listen with empathy and without judgement. Even if you don’t understand the problem or you see the problem in a different way, your main concern is the distress or difficult feelings your loved one is experiencing. You can find in-depth tips on listening and communicating well in Module Three of the Family Toolkit. Some people are not ready to talk about everything at once, or at all. That’s okay! Respect your loved one’s boundaries and let them tell you when they’re ready to talk.
That’s okay! Respect your loved one’s boundaries and let them tell you when they’re ready to talk.
Use empathy, not arguments.
Symptoms of schizophrenia like hallucinations (sensations that aren’t real, like hearing voices) or delusions (beliefs that can’t be true, like believing that you are being followed by a spy) can take some time to stop even when people are receiving treatment and following their treatment plan. As a group, these very distressing symptoms are called psychosis. Many people have a hard time responding to a loved one’s hallucinations or delusions. It’s best to avoid arguing about these experiences. Remember that delusion are symptoms of schizophrenia—they are not thoughts that you can talk someone out of. Telling someone that their experiences aren’t real or aren’t true doesn’t help when the experiences feel very real to that person! A better approach is to empathize with the feelings that hallucinations or delusions bring up—without confirming or denying the hallucination or delusion. For example, if a loved one is frustrated or upset when they hear voices, it isn’t helpful to say something like, “You’re okay! It isn’t real. I don’t hear anything.” Instead, you might say, “I can only image how upsetting that voice must be. I can see the voice makes you feel scared.” Know that with good treatment and support, symptoms like hallucinations and delusions become much easier for people to manage and lose importance.
For example, if a loved one is frustrated or upset when they hear voices, it isn’t helpful to say something like, “You’re okay! It isn’t real. I don’t hear anything.” Instead, you might say, “I can only image how upsetting that voice must be. I can see the voice makes you feel scared.” Know that with good treatment and support, symptoms like hallucinations and delusions become much easier for people to manage and lose importance.
Ask how you can help. When people experience a serious mental illness like schizophrenia, they may want to plan how they can take action if they start to feel unwell again, especially if they have dependent children. These plans, such as advanced directives or Ulysses Agreements, are made when a person feels well and are meant to communicate their wishes to loved ones and their care team. Ask your loved one if they have a plan in place so you know what they need if they need help. If you’d like to learn more about planning for care, see the BC Schizophrenia Society.
If a loved one is experiencing an episode of psychosis or is recovering for an episode of psychosis, they might need extra help. For example, people who are actively experiencing hallucinations or delusions might need a lot of personal space and feel uncomfortable being around a lot of people or even making eye contact. When people are recovering from an episode of psychosis, they may need a quiet space and a lot of rest. Sometimes people can get back into their usual routines fairly quickly, while other times it may take a lot of time (and effort) to get back into routines. Keep in mind that too much help can be a bit counterproductive. It may well be faster and easier for you to take care of your loved one’s tasks or chores yourself, but rebuilding activity and confidence are a big part of recovery. Encourage and support your loved one as they take on daily responsibilities, and let them tell you when they need extra help.
Don’t take it personally
Schizophrenia can be a difficult illness—for everyone. During episodes of psychosis, your loved one may experience frightening sensations that you can’t understand. They may act in ways that you don’t understand. Other symptoms of schizophrenia can make it hard for people to express emotions or feelings, communicate clearly, or seem interested in others. It’s important to know that these are symptoms of an illness. They are no one’s fault, but they can still be hard to cope with. Consider reaching out to a family and friends support group for your own support. The BC Schizophrenia Society has a directory of groups around BC at www.bcss.org/monthly-meetings-calendar/.
During episodes of psychosis, your loved one may experience frightening sensations that you can’t understand. They may act in ways that you don’t understand. Other symptoms of schizophrenia can make it hard for people to express emotions or feelings, communicate clearly, or seem interested in others. It’s important to know that these are symptoms of an illness. They are no one’s fault, but they can still be hard to cope with. Consider reaching out to a family and friends support group for your own support. The BC Schizophrenia Society has a directory of groups around BC at www.bcss.org/monthly-meetings-calendar/.
Take care of yourself, too
As a family member, it’s important to take care of yourself. Try to maintain your regular schedule and activities, such as your exercise routine and hobbies. Ask another family member or good friend to provide help with caregiving, especially in the early days of your loved one's illness. If you need help balancing time for self-care with caregiving duties, check out the BC Schizophrenia Society’s Family Respite Program.
Maintain your social network
Try to maintain your friendships or the network of people that you have in your life. These will later become important supports as your loved one recovers. Educate them and update them on your loved one's recovery. People are sometimes afraid to ask questions about schizophrenia and this will put them at ease.
Encourage your loved one to keep up with their treatment and recovery plan
This is very important! You are not responsible for your loved one’s treatment (unless your loved one is your child under 19), but you can support them. Schizophrenia can make it difficult for people to make and go to appointments and follow their treatment plan. With your loved one’s permission, you may choose to help by reminding them of appointments, taking them to appointments, or whatever helps in your situation. If your loved one isn’t happy with their treatment or would like to try a new approach, you can encourage them to talk with their care team, like their doctor or mental health team—it can be dangerous to stop or change a treatment without a doctor’s support.
Treatment can be a difficult area for loved ones. It’s hard to see someone you love in pain. You might be scared of the things your loved one is experiencing. You want to help. But in order for any treatment to work, your loved one needs to be active in their care. Forcing or threatening treatment generally doesn’t work (or if it does, in the case of an emergency, only for a short time) and can often hurt everyone involved. In most cases, anyone 19 years of age and older and not at risk of harm is free to make their own choices. And their choices may include refusing treatment or choosing a treatment that you disagree with. It helps everyone if you can be respectful and keep honest communication open between you. You can learn more about dealing with this situation in Q&A: An adult in my life seems ill and won’t find help. What can I do?.
Take action if you think you or your loved one is in danger
If you think your loved one is at risk of harming themselves or others and they refuse help, it is possible to have them evaluated by a psychiatrist under the Mental Health Act. This process may involve police and other first responders, and it can be a difficult and stressful process for everyone. But it can also be a necessary step if someone is in danger. You can learn more about the Mental Health Act in the info sheet Families Coping with a Crisis and you can find the Guide to the Mental Health Act at www.health.gov.bc.ca/library/publications/year/2005/MentalHealthGuide.pdf. For a more in-depth discussion of the Mental Health Act, see a video with lawyer and health law consultation Gerrit Clements.
This process may involve police and other first responders, and it can be a difficult and stressful process for everyone. But it can also be a necessary step if someone is in danger. You can learn more about the Mental Health Act in the info sheet Families Coping with a Crisis and you can find the Guide to the Mental Health Act at www.health.gov.bc.ca/library/publications/year/2005/MentalHealthGuide.pdf. For a more in-depth discussion of the Mental Health Act, see a video with lawyer and health law consultation Gerrit Clements.
If your loved one says that they have thoughts of ending their life, it’s important to take action. Call 1-800-SUICIDE (1-800-784-2433) at any time or message online at www.crisiscentrechat.ca between noon and 1am. If you think your loved one is in immediate danger, you can always call 911 or go to a hospital emergency room.
Where can I learn more?
- Dealing with Psychosis: A Toolkit for Moving Forward with Your Life is aimed at people experiencing schizophrenia, but it has good information on symptoms and strategies for managing the illness.
 There is also a chapter for support people
There is also a chapter for support people - Helping a Friend You're Worried About info sheet
- Supporting a Friend or Family Member with a Mental Illness info sheet
- The Family Toolkit workbook—it has good information for anyone who is supporting someone they care about
- Family Self-Care and Recovery from Mental Illness workbook
- Preventing Relapse of a Mental Illness info sheet
About the author
The Canadian Mental Health Association promotes the mental health of all and supports the resilience and recovery of people experiencing a mental illness through public education, community-based research, advocacy, and direct services. Visit www.cmha.bc.ca.
© 2016 | Back to Q&A | Email us a question
Communication in schizophrenia //Psychological newspaper
The description of schizophrenia, like any other mental illness, is a description of its symptoms that develop into their more complex complexes - syndromes that follow each other with a certain sequence, giving us the opportunity to talk about a particular diagnosis. It is possible to talk about certain objectively detectable symptoms of mental disorders by describing the patient's behavior in the context of a particular situation, communication with a particular person. From the point of view of communication theory, communication can be recognized as a symptom of a mental disorder if two criteria are met: a) the person's behavior must be unusual in a given situation for a given culture, and b) it occurs involuntarily. It should also be noted that in any act of communication there is both a verbal component (what is specifically said) and a non-verbal component - facial expressions, gestures, features of voice intonation, as well as the context of communication, and information about the content of communication is transmitted simultaneously through all these channels. Of great importance in communication is the fact whether the information transmitted through all these channels is uniform (for example: a girl who invited a young man to her home greets him with an affectionate voice, smiles, and in response to his hug clings to him) - this the option is called congruent communication, in which the attitude towards the interlocutor is determined unambiguously, or different (in response to the young man's attempt to hug the girl in this situation, she says that she does not want this, but does it in a gentle voice and her body rushes to him).
It is possible to talk about certain objectively detectable symptoms of mental disorders by describing the patient's behavior in the context of a particular situation, communication with a particular person. From the point of view of communication theory, communication can be recognized as a symptom of a mental disorder if two criteria are met: a) the person's behavior must be unusual in a given situation for a given culture, and b) it occurs involuntarily. It should also be noted that in any act of communication there is both a verbal component (what is specifically said) and a non-verbal component - facial expressions, gestures, features of voice intonation, as well as the context of communication, and information about the content of communication is transmitted simultaneously through all these channels. Of great importance in communication is the fact whether the information transmitted through all these channels is uniform (for example: a girl who invited a young man to her home greets him with an affectionate voice, smiles, and in response to his hug clings to him) - this the option is called congruent communication, in which the attitude towards the interlocutor is determined unambiguously, or different (in response to the young man's attempt to hug the girl in this situation, she says that she does not want this, but does it in a gentle voice and her body rushes to him). The second option is called incongruent communication, and the young man has to guess what is really meant: whether to accept the girl’s verbal message that she does not want more intimate communication as truth, or, neglecting her words, behave even more insistently, considering that it is the intonation and movement of the body, as well as the context of the situation - after all, the girl herself invited him to visit - are more significant (118). nine0003
The second option is called incongruent communication, and the young man has to guess what is really meant: whether to accept the girl’s verbal message that she does not want more intimate communication as truth, or, neglecting her words, behave even more insistently, considering that it is the intonation and movement of the body, as well as the context of the situation - after all, the girl herself invited him to visit - are more significant (118). nine0003
It should be emphasized here that no kind of communication occurs by chance. In psychology, as in economics, only those processes are preserved that bring some kind of, way and perverted, benefit. Both congruent and incongruent communication pursue their goals to achieve some specific behavior from the interlocutor (even if this intention is not realized by the person himself). For example, it can be assumed that in the second case, the true goal of the girl is to inflame the feelings of the young man. In addition, in the process of communication, information about the internal state of a person is always transmitted - valuable feedback, without which no systematic interaction is possible. Working with severe personality disorders and schizophrenia, we very often see how the whole process of intra-family communication is permeated with “double binds”. Selvini Palazzolli described the style of communication in such families as follows: “Everyone is desperate to seize the right to define relationships, and everyone keeps testing their position again and again, thus constantly putting themselves at risk of defeat. However, arrogance, this hypertrophied pride, nests in each of the spouses and cannot accept defeat. Failure (or even the possibility of it) is utterly unbearable and must be prevented at all costs. Avoiding the conflict does not solve the problem in itself, in this case it is tantamount to admitting defeat. The fight must continue, but without risk to the opponents. And they find the only way out - avoiding any definition of relationships. Each must disqualify his definition of relationship before the other gets a chance to do so.”(122).
Working with severe personality disorders and schizophrenia, we very often see how the whole process of intra-family communication is permeated with “double binds”. Selvini Palazzolli described the style of communication in such families as follows: “Everyone is desperate to seize the right to define relationships, and everyone keeps testing their position again and again, thus constantly putting themselves at risk of defeat. However, arrogance, this hypertrophied pride, nests in each of the spouses and cannot accept defeat. Failure (or even the possibility of it) is utterly unbearable and must be prevented at all costs. Avoiding the conflict does not solve the problem in itself, in this case it is tantamount to admitting defeat. The fight must continue, but without risk to the opponents. And they find the only way out - avoiding any definition of relationships. Each must disqualify his definition of relationship before the other gets a chance to do so.”(122).
Thus, any psychiatric symptom that manifests itself in any behavior can also be considered as a way of unconscious manipulation of others. Neurotic symptoms in this respect are built more simply, and it is not for nothing that one of the signs of neurosis is the situational secondary benefit from neurotic behavior that is relatively easily detected by a psychiatrist (for example, the widespread headache of wives, which helps, while maintaining their status as a wife, to avoid intimate relationships with an unloved husband). With schizophrenic symptoms, the situation is more complicated. nine0003
Neurotic symptoms in this respect are built more simply, and it is not for nothing that one of the signs of neurosis is the situational secondary benefit from neurotic behavior that is relatively easily detected by a psychiatrist (for example, the widespread headache of wives, which helps, while maintaining their status as a wife, to avoid intimate relationships with an unloved husband). With schizophrenic symptoms, the situation is more complicated. nine0003
J. Haley described the essence of schizophrenic behavior as the avoidance of a clear definition of one's behavior and intentions in order, on the one hand, to make one's communication more effective using unconscious mechanisms, on the other hand, to avoid responsibility for one's actions and in any case remain innocent and good for all.
Any appeal of one person to another can be schematically described as follows:
1. I am
2. report something
3. you
4. in this situation
There are many ways to avoid defining your behavior when addressing someone. For example:
For example:
1. In order to deny that it is this person who is addressing the interlocutor, you can call yourself by some other name, for example, introduce yourself as Stalin or a Martian, or say that God (and not himself) speaks through his mouth. It can also be said that the statement was made involuntarily when a person could not control himself - under the influence of alcohol or by order of "voices". In addition, the conversion can be performed in the form of some symbolic physiological action (for example, urination, defecation, or yawning), as if in fact it was not a conversion at all, but the manifestation of some physiological process. nine0003
2. The easiest way to deny that a person said something is amnesia. In addition, for this it can be stated that he misunderstood the interlocutor and had in mind something completely different. It is also possible to invent your own language, or communicate in such a way that verbal and non-verbal communication contradict each other (for example, saying "I'm glad to see you" in a dull tone with a wistful expression). In addition, to deny your behavior, you can plunge into a trance state. When a hypnotic in a trance is suggested that his hand becomes lighter and begins to rise higher and higher on its own, and this happens, then later on the question of how this happened, the patient will answer with sincere surprise that the hand really did rise on its own in addition to his will. However, on the other hand, who could raise a hand except the patient himself? nine0003
In addition, to deny your behavior, you can plunge into a trance state. When a hypnotic in a trance is suggested that his hand becomes lighter and begins to rise higher and higher on its own, and this happens, then later on the question of how this happened, the patient will answer with sincere surprise that the hand really did rise on its own in addition to his will. However, on the other hand, who could raise a hand except the patient himself? nine0003
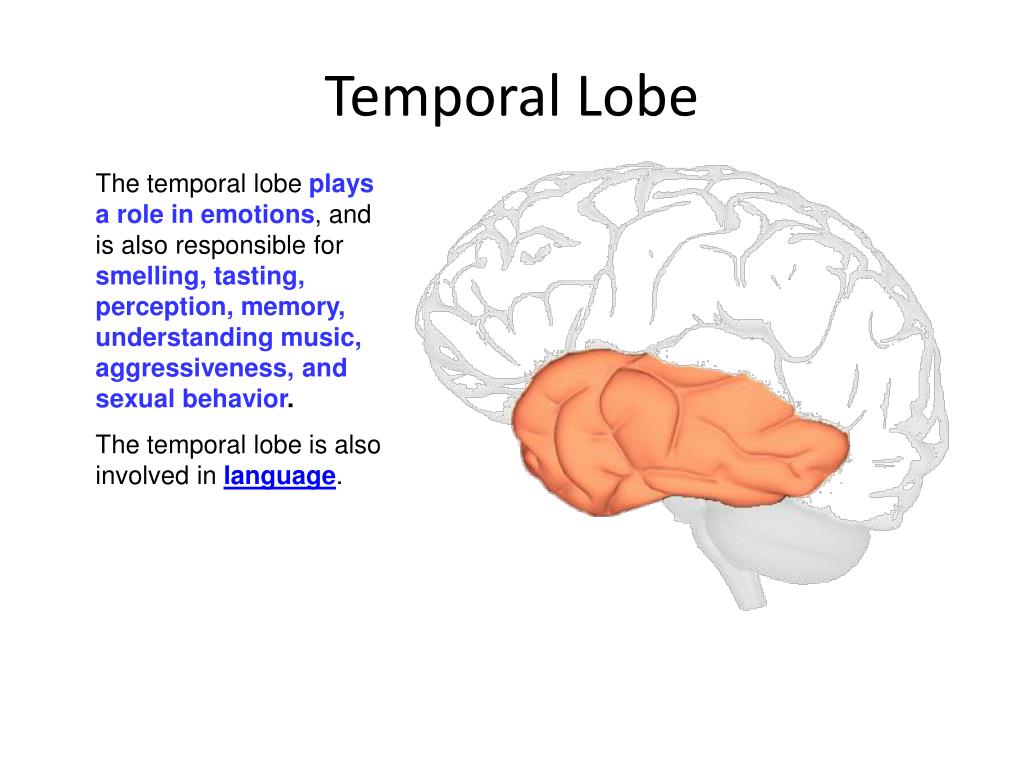
Similar phenomena occur in schizophrenia. Even Pavlov, in his article "A Trial Excursion of a Physiologist into the Field of Psychiatry", noted the extreme similarity from the point of view of physiologists between schizophrenic psychosis and hypnotic trance: "it can hardly be doubted that schizophrenia in certain variations and phases really represents chronic hypnosis" (167 ). The same point of view is expressed by Ericksonian hypnotherapists, for example, M. Erickson (9), S. Gilligan (10). It is worth remembering that the hypnotic trance differs from the waking state precisely in the focus of consciousness. In the waking state, it is focused outward, and in trance it is focused on the inner world of a person, his feelings, sensations and visual images. Deep, persistent withdrawal into oneself, one's experiences during the devaluation (i.e., refusal to define the relationship) of the real things of the outside world is one of the characteristic signs of schizophrenia. nine0003
In the waking state, it is focused outward, and in trance it is focused on the inner world of a person, his feelings, sensations and visual images. Deep, persistent withdrawal into oneself, one's experiences during the devaluation (i.e., refusal to define the relationship) of the real things of the outside world is one of the characteristic signs of schizophrenia. nine0003
3. In order to deny that a person is addressing any particular interlocutor, you can start talking aloud to yourself, or call the interlocutor by a different name. In addition, you can say that the interlocutor (let's say a neighbor) is not the one he claims to be, but a secret FSB officer, and, accordingly, start talking to him not as a neighbor, but as a secret FSB officer, which, again However, it excludes the possibility of determining the true nature of the relationship. nine0003
4. You can deny the situation in which the conversation is being conducted by violating the orientation in place, time and situation. In addition, you can begin to transfer past experiences into the present and future ("no one could help me - and you will not help").
In addition, you can begin to transfer past experiences into the present and future ("no one could help me - and you will not help").
In studies by G. Bateson's group (46), this kind of communication, built according to the type of "double bind" (double bind), was qualified as "schizophrenogenic". For this kind of relationship, G. Bateson identified three qualifying signs:
1. Communication should be important for this person.
2. During communication, two contradictory messages are simultaneously transmitted (the term “incongruence” was used to define this - for example, words and facial expressions, pantomime, intonation do not correspond to each other).
3. It is forbidden by the rules of communication to clarify what exactly is meant.
It was found that schizophrenogenic communication itself is often found not only in patients with schizophrenia. However, in other cases, it is temporary - alcohol is excreted from the body, headache and anger pass, the traumatic situation ends, and the person begins to communicate congruently. The fundamental difference in communication between patients with schizophrenia and neuroses, as Jung and Haley (118) pointed out, is quantitative - how consistently a person communicates incongruently and how deep this incongruence goes. The pathopsychologists come to the same conclusions: it is important not only that in the experiment, in principle, there are slips of thinking or the patient's lack of interest in performing one or another test, but how often these phenomena occur in various tests (168). While the neurotic simply uses incongruence to deny his message (for example, annoyedly says "Sit down!" to an unwanted visitor at the end of the working day - this still allows the visitor to guess that he is not particularly welcome here), the schizophrenic patient strengthens his incongruence to such an extent that the very fact of denying the definition of one’s behavior is denied in behavior: for example, when an unwanted visitor enters the room, the patient not only remains silent and pretends not to notice him - this is already, albeit incongruently, but would already show an attitude towards a person, but begins to behave as if he is extremely busy with something in the room or in his thoughts - this allows him to avoid communication and at the same time not define his behavior as avoidant.
The fundamental difference in communication between patients with schizophrenia and neuroses, as Jung and Haley (118) pointed out, is quantitative - how consistently a person communicates incongruently and how deep this incongruence goes. The pathopsychologists come to the same conclusions: it is important not only that in the experiment, in principle, there are slips of thinking or the patient's lack of interest in performing one or another test, but how often these phenomena occur in various tests (168). While the neurotic simply uses incongruence to deny his message (for example, annoyedly says "Sit down!" to an unwanted visitor at the end of the working day - this still allows the visitor to guess that he is not particularly welcome here), the schizophrenic patient strengthens his incongruence to such an extent that the very fact of denying the definition of one’s behavior is denied in behavior: for example, when an unwanted visitor enters the room, the patient not only remains silent and pretends not to notice him - this is already, albeit incongruently, but would already show an attitude towards a person, but begins to behave as if he is extremely busy with something in the room or in his thoughts - this allows him to avoid communication and at the same time not define his behavior as avoidant. The same purpose is served by symbolic statements, actions, as well as the expression of one's true feelings as metaphors - in words and behavior. In a lighter version, this will be a statement: “I feel as if the world has collapsed and everyone has betrayed me” - with the corresponding suicidal behavior, in a more difficult version - sewing up the mouth with threads in protest that the patient’s opinion was not heeded, even more severe - the fragmentation of speech and thinking as an expression of fear of life, which allows you to safely hide from this life behind the walls of a psychiatric clinic. nine0003
The same purpose is served by symbolic statements, actions, as well as the expression of one's true feelings as metaphors - in words and behavior. In a lighter version, this will be a statement: “I feel as if the world has collapsed and everyone has betrayed me” - with the corresponding suicidal behavior, in a more difficult version - sewing up the mouth with threads in protest that the patient’s opinion was not heeded, even more severe - the fragmentation of speech and thinking as an expression of fear of life, which allows you to safely hide from this life behind the walls of a psychiatric clinic. nine0003
In addition, the refusal to clearly define one's intentions guarantees the absence of defeats, because whoever does nothing never loses. And this circumstance for our patient, brought up in the spirit of the double bind: “you must always be a winner and make only accurate decisions, but at the same time you are forbidden in the fight to cause inconvenience to others and make mistakes, gaining experience through them” turns out to be extremely important. After all, it is possible to clearly fulfill this parental instruction only by going into a schizophrenic type of reaction: “I am generally good and talented, but I could not fulfill everything entrusted to me because I fell ill with an incurable disease, which is also complicated by the fact that I cannot realize what I am ill, and I am not capable of purposeful actions in order to cope with the disease. Now, if someone (God forbid!) cured me, I would certainly be able to justify my parental hopes. nine0003
After all, it is possible to clearly fulfill this parental instruction only by going into a schizophrenic type of reaction: “I am generally good and talented, but I could not fulfill everything entrusted to me because I fell ill with an incurable disease, which is also complicated by the fact that I cannot realize what I am ill, and I am not capable of purposeful actions in order to cope with the disease. Now, if someone (God forbid!) cured me, I would certainly be able to justify my parental hopes. nine0003
In the Old Testament, it was established: “If your brother, a Jew, or a Jewess, sells himself to you, then for six years he should be your slave, and in the seventh year let him go free from you ... If he says to you: “I will not go away from you, because I love you and your house”, because it is good for him with you, then take an awl and pierce his ear to the door; and he will be your servant forever” (Deuteronomy 15:12-17). Why was the share of a slave so pleasant that Moses had to specifically prescribe such a law? Only one: the slave is spared the burden of taking responsibility. How sweet, despite the constant humiliation and obligation to do the hardest work, is the share of an irresponsible person that even his own ears turned out to be not a pity! nine0003
How sweet, despite the constant humiliation and obligation to do the hardest work, is the share of an irresponsible person that even his own ears turned out to be not a pity! nine0003
In the same way, a person who avoids determining his behavior, attitudes and intentions through unconscious mechanisms also avoids responsibility, falling under the category of insanity.
Certainly, a significant role in the patient's transition to a schizophrenic style of response is also played by the specific vulnerability of the personality, which, as modern studies show, is based on a decrease in the function of the frontal cortex against the background of autoimmune, toxic and mediator disorders. It is erroneous to oppose the biological and psychological mechanisms of pathogenesis to each other. nine0003
They, as practice shows, always go hand in hand, and the strengthening of biological disorders always leads to aggravation of psychological and family problems. At the same time, regular stresses to which patients are exposed due to the psychological weakness and vulnerability of their personality, as well as constant family problems, according to all the laws of the development of stress reactions, are guaranteed to lead to a violation of the biological functioning of the brain. Therefore, in parallel with the described psychological methods of influence, and often ahead of them, scientifically based biological therapy should always be carried out. nine0003
Therefore, in parallel with the described psychological methods of influence, and often ahead of them, scientifically based biological therapy should always be carried out. nine0003
Another weighty reason to use a schizophrenic type of communication for a patient is narcissistic rage - a powerful charge of destructive negative emotions that invariably manifests itself in the psyche of a patient with schizophrenia during psychoanalytic therapy.
It arises as a reactive formation due to a deep sense of one's own weakness, the inferiority of the patient and the corresponding fear of annihilation by the outside world. This rage is restrained by libido - the energy of love for loved ones. Spotnitz describes this process as follows: “The integrity of the psyche and the fate of the external object become the stake in the battle between the aggressive object cathexis, fighting for motor control, and the libidinal cathexis, controlling motor skills to prevent aggressive actions.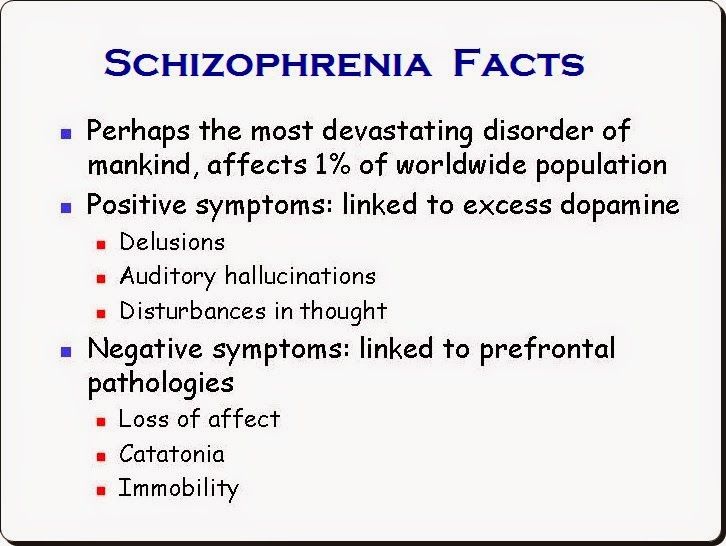 In these states of high tension, the energy of the libido is sufficient to restrain hostile behavior, but not enough to be the organizing force of the psychic apparatus. The outcome of this battle is a foregone conclusion in favor of a more powerful opponent. nine0003
In these states of high tension, the energy of the libido is sufficient to restrain hostile behavior, but not enough to be the organizing force of the psychic apparatus. The outcome of this battle is a foregone conclusion in favor of a more powerful opponent. nine0003
The patterning of the schizophrenic reaction reduces the tension sufficiently to preserve the object, but disorganizes the psychic apparatus, resulting in psychosis... To clarify the unconscious operation, I will emphasize again that the patient is constantly under the pressure of a strong desire to kill and defends himself from it by deducing out of order their mental apparatus with its high potential for destructive actions.
To destroy a potentially destructive self in order to prevent dangerous actions directed against other people is like smashing a rifle to smithereens so as not to pull the trigger” (1). nine0003
Going into the world of symbols, the patient must spend somewhere the energy that should have been spent on social adaptation and development of his personality, and also at least somehow explain to himself the meaning of what is happening (despite the fact that the true goals of his behavior, according to the rules of the subconscious games are not subject to clarification). This is where initiation comes to the rescue using the endogenous mechanisms of the myth-ritual complex "death-rebirth", described by Zaitseva-Pushkash and other authors who studied traditional cultures (2) (39). The patient does not just move away from communication with people and work - he is busy comprehending important, unknown to the uninitiated knowledge and performing actions under the guidance of higher forces that capture his will. After that, a completely new life awaits him - sometimes filled with a new meaning, incomprehensible to others, and sometimes just living out his life exhausted and weak-willed, like a squeezed lemon. But now this lack of will has an explanation: “Everything that happened completely exhausted me, it’s not me running away from life, it’s my illness. I can’t do anything myself, but I hope that everything will work out somehow (that is, someone will solve my problems for me).” In both of these cases, as Yalom shows, a person refuses to take responsibility for his actions and his life, entrusting it to the "ultimate savior" (40).
This is where initiation comes to the rescue using the endogenous mechanisms of the myth-ritual complex "death-rebirth", described by Zaitseva-Pushkash and other authors who studied traditional cultures (2) (39). The patient does not just move away from communication with people and work - he is busy comprehending important, unknown to the uninitiated knowledge and performing actions under the guidance of higher forces that capture his will. After that, a completely new life awaits him - sometimes filled with a new meaning, incomprehensible to others, and sometimes just living out his life exhausted and weak-willed, like a squeezed lemon. But now this lack of will has an explanation: “Everything that happened completely exhausted me, it’s not me running away from life, it’s my illness. I can’t do anything myself, but I hope that everything will work out somehow (that is, someone will solve my problems for me).” In both of these cases, as Yalom shows, a person refuses to take responsibility for his actions and his life, entrusting it to the "ultimate savior" (40).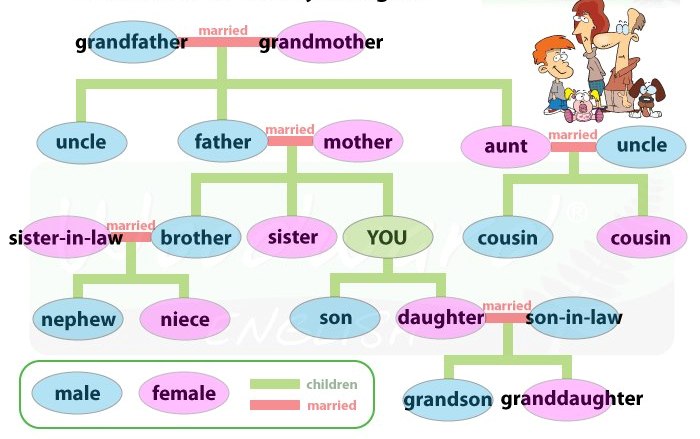 nine0003
nine0003
In addition, we constantly see that communication in the families of patients with schizophrenia, as noted above, is built on "double binds". The difference between the patient and his family members is that, firstly, they use "double binds" periodically, refusing them where it interferes with social and labor adaptation, and, secondly, the patient is a less important member of the family, than one of the parents or siblings, and despite the fact that this other family member turns out to be even more mentally ill than our patient, the latter, according to the unconscious mechanisms of the functioning of the family system, is sacrificed to family stability. Declaring him sick allows others to sigh sadly: “Oh, how good we would live if Vasya did not suffer from schizophrenia,” and calm down, forgetting about their own intrapsychic problems and difficulties in communication. The love of the parents is gone (or it never was), and it’s scary to get a divorce and start life over again. To realize this for them is to plunge into the abyss of despair, and here again Vasya's illness comes to the rescue: “We are honest, decent, responsible people. How can we part when our son is so seriously ill! We are together to save him." Experienced psychiatrists know that often the biggest problems in a family begin when a mentally ill family member suddenly goes into pure remission. nine0003
To realize this for them is to plunge into the abyss of despair, and here again Vasya's illness comes to the rescue: “We are honest, decent, responsible people. How can we part when our son is so seriously ill! We are together to save him." Experienced psychiatrists know that often the biggest problems in a family begin when a mentally ill family member suddenly goes into pure remission. nine0003
However, to go into pure remission does not mean to recover forever. After all, our patient spent his whole life in the little world of his family, who communicated in “double bonds” and hid their true feelings and intentions from themselves and from each other. And to recover means to enter the big world, where people communicate in a completely different way and where “double binds” are used relatively rarely, and successful people (oh, horror!) openly tell each other about their feelings, desires and intentions, and at the same time are not afraid make new mistakes, guided by the dictum of W.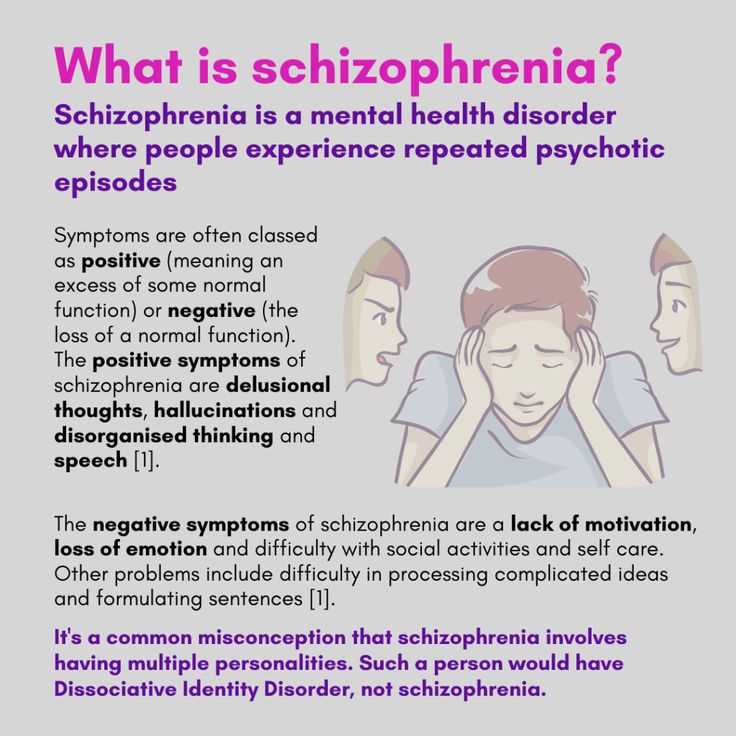 Churchill: “Success is the ability to go from defeat to defeat without losing optimism!” Our patient has never lived in such conditions, and, in the absence of psychosocial rehabilitation, he simply does not know how to act in such a way. He tries, with the best of intentions, to communicate the way he learned in his family, but he is not understood and rejected, considering him a ridiculous eccentric. Social and labor maladaptation is growing, and soon, like a prisoner released after a long term of imprisonment and unable to adapt to the freedom that he dreamed of for so long, our patient returns to the world of his family, which causes him the most negative feelings, but the style of communication which is more familiar to him. And to start communicating differently usually means becoming a stranger to your parental family in conditions where new social ties are made with great difficulty and, due to the inability to develop them, are not stable, which is fraught with chronic loneliness.
Churchill: “Success is the ability to go from defeat to defeat without losing optimism!” Our patient has never lived in such conditions, and, in the absence of psychosocial rehabilitation, he simply does not know how to act in such a way. He tries, with the best of intentions, to communicate the way he learned in his family, but he is not understood and rejected, considering him a ridiculous eccentric. Social and labor maladaptation is growing, and soon, like a prisoner released after a long term of imprisonment and unable to adapt to the freedom that he dreamed of for so long, our patient returns to the world of his family, which causes him the most negative feelings, but the style of communication which is more familiar to him. And to start communicating differently usually means becoming a stranger to your parental family in conditions where new social ties are made with great difficulty and, due to the inability to develop them, are not stable, which is fraught with chronic loneliness.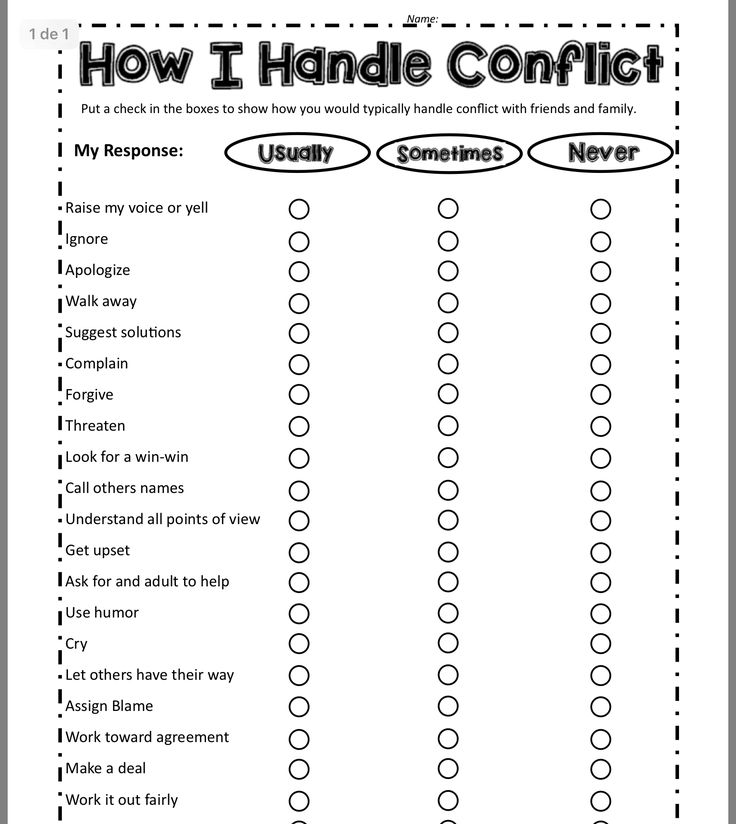 nine0003
nine0003
Thus, the refusal to define one's relationship and the withdrawal into a schizophrenic style of response has a number of great advantages for the patient:
1. Avoiding leaving for an independent life and taking responsibility for your actions.
2. Keeping your loved ones safe by keeping them from venting their narcissistic rage.
3. Stabilization of the mental state of their loved ones and relationships in the parental family. nine0003
4. Avoiding mistakes and defeats.
5. Maintaining relationships with parents.
6. Prevention of complete loneliness.
7. Finding the meaning of one's life through the development of the mythological-ritual complex "death-rebirth".
As pointed out by N.P. Bekhterev (116), any long-term neurological or psychiatric disease leads to the formation of a stable pathological state of the brain, in which the psyche resists doctors' attempts to cure the patient, and exit from which is possible only through the decompensation phase (if possible, controlled). Psychoanalysis also affirms the same, one of the most important tools of which is work with the patient's unconscious resistance. Therefore, as Hayley (118), Minukhin (121), Whitaker (50), Selvini Pallazzolli (122) and others rightly pointed out, the first step in working with a patient with schizophrenia is “uprooting” him from the “ecological niche” occupied by him, refusing to relationship definitions. This can be done in two ways. The first is the most common way of a direct attack, when the patient is removed from his intra-family environment to a psychiatric hospital, where his relationships are determined by the directive of the medical staff (and therefore it is impossible to avoid their definition), and the symptoms of mental disorders, with the help of which the patient manipulated the environment, are cut off with the help of psychopharmacotherapy or comatose treatments, forcing the patient to look for other ways of communicating and behaving in the world. However, the results of using this method are reminiscent of the situation common in modern politics, when a major developed power undertakes to urgently civilize a neighboring country that is in a barbaric state, using the method of a major military operation, hoping that in the future the neighbors will hold civilized democratic elections and finally live as people.
Psychoanalysis also affirms the same, one of the most important tools of which is work with the patient's unconscious resistance. Therefore, as Hayley (118), Minukhin (121), Whitaker (50), Selvini Pallazzolli (122) and others rightly pointed out, the first step in working with a patient with schizophrenia is “uprooting” him from the “ecological niche” occupied by him, refusing to relationship definitions. This can be done in two ways. The first is the most common way of a direct attack, when the patient is removed from his intra-family environment to a psychiatric hospital, where his relationships are determined by the directive of the medical staff (and therefore it is impossible to avoid their definition), and the symptoms of mental disorders, with the help of which the patient manipulated the environment, are cut off with the help of psychopharmacotherapy or comatose treatments, forcing the patient to look for other ways of communicating and behaving in the world. However, the results of using this method are reminiscent of the situation common in modern politics, when a major developed power undertakes to urgently civilize a neighboring country that is in a barbaric state, using the method of a major military operation, hoping that in the future the neighbors will hold civilized democratic elections and finally live as people.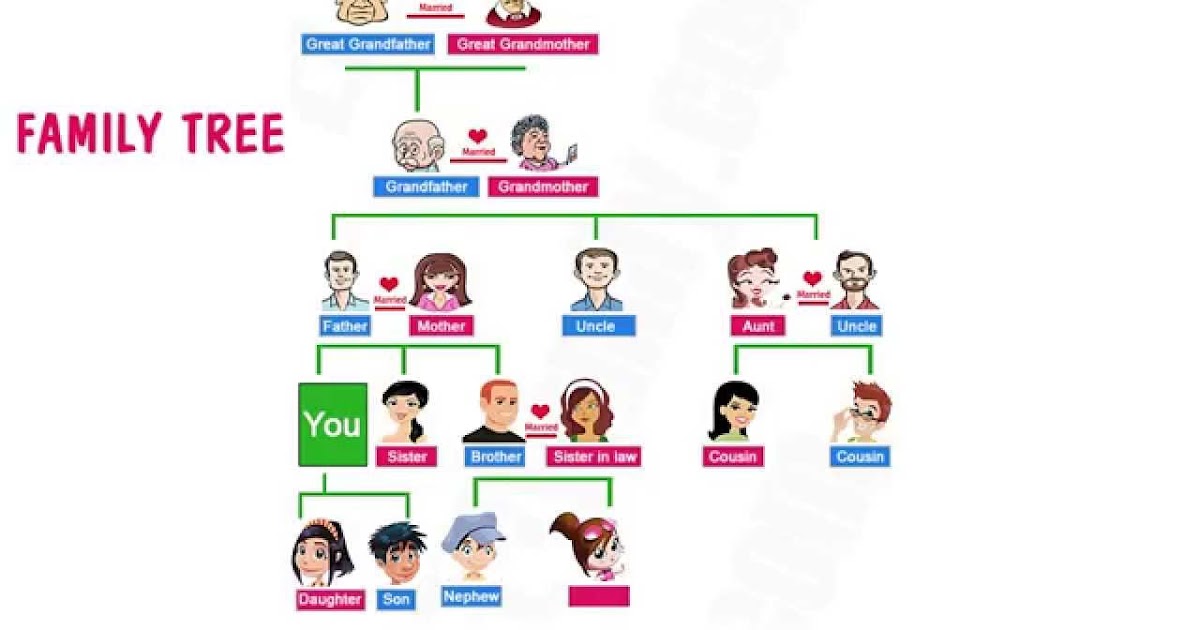 At first, everything goes brilliantly: the neighboring country is quickly occupied, all its leaders swear allegiance to the democratic ideals of their pale-faced brothers, humanitarian aid is sent to the country in a wide stream. However, the latter is quickly being stolen, which for some reason is only helped by democratically elected authorities, in the poor provinces the guerrilla movement is rearing its head and strengthening, which is becoming increasingly difficult to cope with, new and new military operations bring less and less results at ever greater costs, and gradually a major developed power is discovering that the cost of keeping its barbarian neighbors from ultimate chaos is getting ever higher. At a certain moment, a major developed country develops a syndrome of psychotherapeutic burnout, it spits on the problems of its neighbors and leaves, having come to terms with all the reputational and economic losses, regarding the situation as incurable in principle, when the best way would be to isolate yourself from your neighbors with the highest possible fence in order to never see them again.
At first, everything goes brilliantly: the neighboring country is quickly occupied, all its leaders swear allegiance to the democratic ideals of their pale-faced brothers, humanitarian aid is sent to the country in a wide stream. However, the latter is quickly being stolen, which for some reason is only helped by democratically elected authorities, in the poor provinces the guerrilla movement is rearing its head and strengthening, which is becoming increasingly difficult to cope with, new and new military operations bring less and less results at ever greater costs, and gradually a major developed power is discovering that the cost of keeping its barbarian neighbors from ultimate chaos is getting ever higher. At a certain moment, a major developed country develops a syndrome of psychotherapeutic burnout, it spits on the problems of its neighbors and leaves, having come to terms with all the reputational and economic losses, regarding the situation as incurable in principle, when the best way would be to isolate yourself from your neighbors with the highest possible fence in order to never see them again. Will it just work? nine0003
Will it just work? nine0003
Wise politicians know that in order to cultivate a barbarian country, one should first of all establish close ties with the ruling elites and, first of all, slowly cultivate them by educating the rulers and their children in their universities, providing these elites with military and economic assistance so that they themselves bring order, and to create economic conditions so that it would be more profitable and easier for the inhabitants of the country to engage in peaceful labor than to rob. Then begins delicate diplomatic work, full of cunning, imperceptible from the outside, but accurately calculated moves. This process turns out to be much longer and less brilliant at the beginning than the frontal attack method described earlier, but it gives much better and more stable long-term results. nine0003
In a similar way, the principle of community-based treatment of mental illness, which has recently become increasingly popular, operates when the goals of a team of specialists working with the patient and his relatives is to build an adequate hierarchical structure among the latter, trained to independently successfully cope with all emerging problems.
There is another important point that is characteristic not only for patients with schizophrenia, but for personally immature people in general. If for a mature person the words that he speaks and which are spoken to him are important (the second signal system according to Pavlov), then for an immature person words in themselves are unimportant and significant are the external expressions of mental life: actions and gestures (the first, phylogenetically older signal system ). Humanity faced this even during the collapse of Ancient Rome, when the coherent system of Roman laws, based on the logic and evidence of the word, gave way to the laws of gestures and actions. Instead of a speech or a logically composed statement, the Frankish legislation "Salic Truth" (169) to lay part of his debt on relatives, he ordered to invite 12 jurors - witnesses from the closest relatives, go out onto the porch of his house, stand facing inside the house - civilization of the gesture, stand up like that, then it will be according to the law - and throw this handful with your right hand, necessarily right, over their shoulders to the next three relatives, on the father, then on the mother, etc. , and then they must pay half of what is not enough to pay the fine. If these next of kin have already paid - even for the next relatives. Then he must, without shoes, without a belt, with a stake in his hand, jump over the wattle fence, and then the requirement of the law to pay relatives for the debtor came into force. If, on the contrary, a person wanted to renounce kinship in order not to pay off other people's debts, then he had to come to the judge and there scatter sticks a cubit long over his head to all parts of the world. Among immature people, it was the act, the gesture that reigned and reigns, and it is on them that the psychotherapist should rely in the first stages of his work, paying more attention to working with action and experiencing feelings than with a logical discussion of what is happening, the turn of which comes much later. This idea is one of the core ones in justifying the use of body-oriented psychotherapy for schizophrenia, based on the use of dance, gestures, and movement.
, and then they must pay half of what is not enough to pay the fine. If these next of kin have already paid - even for the next relatives. Then he must, without shoes, without a belt, with a stake in his hand, jump over the wattle fence, and then the requirement of the law to pay relatives for the debtor came into force. If, on the contrary, a person wanted to renounce kinship in order not to pay off other people's debts, then he had to come to the judge and there scatter sticks a cubit long over his head to all parts of the world. Among immature people, it was the act, the gesture that reigned and reigns, and it is on them that the psychotherapist should rely in the first stages of his work, paying more attention to working with action and experiencing feelings than with a logical discussion of what is happening, the turn of which comes much later. This idea is one of the core ones in justifying the use of body-oriented psychotherapy for schizophrenia, based on the use of dance, gestures, and movement. K.-H. Leiner, in turn, describing his method of symbol-drama (42), emphasized that at the first stages of working with visualized images, their analysis and interpretation are possible, but undesirable, which also reflects the difficulties of our patients in logical comprehension of the world and the greater importance of action. and experiences, even imaginary ones. nine0003
K.-H. Leiner, in turn, describing his method of symbol-drama (42), emphasized that at the first stages of working with visualized images, their analysis and interpretation are possible, but undesirable, which also reflects the difficulties of our patients in logical comprehension of the world and the greater importance of action. and experiences, even imaginary ones. nine0003
In the practice of a psychiatrist, periodically there are patients whose thinking and emotional-volitional response, according to the data of an experimental psychological study (EPI), are greatly altered by the current endogenous process, while these patients turn out to be remarkably adapted in society, have good families or personal relationships, and come to the attention of a psychiatrist about moderately severe problems of a neurotic nature. An important question for us was: what exactly compensatory mechanisms help them, with a sufficiently pronounced schizophrenic pathological symptom complex, to avoid social and labor maladjustment and live a fairly happy, full life? nine0003
For this purpose, we conducted clinical examinations in combination with EPI of 32 similar patients. All of them showed signs of a schizophrenic pathopsychological symptom complex from mild to moderate severity with a change in both the motivational and operational spheres of thinking according to the schizophrenic type. At the same time, clinically, it was impossible to confidently speak about the presence of the current endogenous process in its progredient form: structurally and dynamically, they were confidently kept at the neurotic level, neither autism nor social and labor maladaptation was noted. The reason for visiting a psychiatrist was moderate anxiety and psychosomatic disorders. nine0003
All of them showed signs of a schizophrenic pathopsychological symptom complex from mild to moderate severity with a change in both the motivational and operational spheres of thinking according to the schizophrenic type. At the same time, clinically, it was impossible to confidently speak about the presence of the current endogenous process in its progredient form: structurally and dynamically, they were confidently kept at the neurotic level, neither autism nor social and labor maladaptation was noted. The reason for visiting a psychiatrist was moderate anxiety and psychosomatic disorders. nine0003
In the process of studying compensation mechanisms, it was noted that this group of patients was characterized by high intelligence and high values on the scales of "hysteria" and "psychopathy" in SMIL (i.e., personality traits that compensate for schizoid and depressive traits gradually developing against the background of the disease, thanks to which, at some stages of the disease, they themselves and their relatives sometimes noted that their character had become even better than before the disease). To a lesser extent than in other patients, they had facial expression disorders; they were able to understand quite well the true meaning of the mimic reactions of the interlocutors. All of them, thanks to their high intelligence and ability to establish harmonious object relations, managed to develop an interesting way of adaptation: in the conditions of the unevenness and inconsistency of the process of generalization with the equalization of the significance of the main and secondary features of objects and concepts, they were trained to solve these issues by asking interlocutors in detail about about what exactly should be done and according to what criteria the right decision should be made, after which, having received the necessary instructions and following them exactly, they acted very effectively, including during testing. If, during the EPI, they were given a test with a “deaf” instruction (when the psychologist refused to give detailed explanations on how to perform the test correctly, limiting himself to the standard setting of the task), significant thinking disorders were immediately reflected in the results in the form of a tendency to equalize the significance of the main and secondary signs of objects and concepts, semantic slips with the actualization of non-standard properties and relationships, a clear tendency to overgeneralize when defining concepts, manifestations of diverse thinking.
To a lesser extent than in other patients, they had facial expression disorders; they were able to understand quite well the true meaning of the mimic reactions of the interlocutors. All of them, thanks to their high intelligence and ability to establish harmonious object relations, managed to develop an interesting way of adaptation: in the conditions of the unevenness and inconsistency of the process of generalization with the equalization of the significance of the main and secondary features of objects and concepts, they were trained to solve these issues by asking interlocutors in detail about about what exactly should be done and according to what criteria the right decision should be made, after which, having received the necessary instructions and following them exactly, they acted very effectively, including during testing. If, during the EPI, they were given a test with a “deaf” instruction (when the psychologist refused to give detailed explanations on how to perform the test correctly, limiting himself to the standard setting of the task), significant thinking disorders were immediately reflected in the results in the form of a tendency to equalize the significance of the main and secondary signs of objects and concepts, semantic slips with the actualization of non-standard properties and relationships, a clear tendency to overgeneralize when defining concepts, manifestations of diverse thinking. nine0003
nine0003
In addition, well-established object relations were also a source of motivation for constructive activity for patients. At the same time, it should be emphasized once again that personal relationships in all examined patients of this group were quite structurally clearly built, with an established intra-family hierarchy and feedback. All of them worked and were valued as specialists or even heads of organizations, and the occasional emotional and volitional decompensation was quickly smoothed out by those around them who knew the personal characteristics of the patients well: “The boss is not in a good mood today, come tomorrow or let us decide everything ourselves.” nine0003
Often, to solve their problems, patients in this group spontaneously used the method of image visualization: “I work somehow at the machine, and then “voices” appear. Well, I understand that this is a potentially dangerous business, I turn off the machine, sit next to me and imagine a beautiful garden, apple trees, a stream, how I relax there - the voices gradually disappear. I'll take a break and get back to work."
I'll take a break and get back to work."
In this way, the main mechanisms of spontaneous personal compensation that prevent the development of social and labor maladjustment and reduce the severity of emotional and volitional disorders in patients with schizophrenia turned out to be high intelligence, the severity of excitable and hysterical radicals in the personality, clearly structurally built, with an established intra-family hierarchy and feedback, object relationships (which, in turn, is impossible without sufficient integration of the Super-Ego, the ability to take responsibility for oneself and one's life) and the ability to overcome decompensation with the help of visualization of images. These observations of ours confirm Kernberg's opinion that the prognosis of psychotherapeutic treatment for severe personality disorders largely depends not on the severity of the disease, but on the quality of object relations and the degree of Super-Ego integration (20). nine0003
What should be the strategy for solving the problems of a patient with schizophrenia and his microsocial environment? As we have already shown above, it should be based on moves that render ineffective the usual strategy of the patient's problem-solving behavior, based on the manipulation of the environment with the help of his symptoms, disguised as a refusal to determine his behavior and intentions. These moves fall into a number of categories:
These moves fall into a number of categories:
1. Creation in the microsocial environment of the patient of a harmonious hierarchical structure with clearly defined rights and obligations of all its members, responsibility for failure to fulfill their duties, and a head capable of enforcing all these laws, as well as a working feedback that allows each family member to correctly understand the consequences of their actions. In such a structure, there is no room for the uncertainty of relations. nine0003
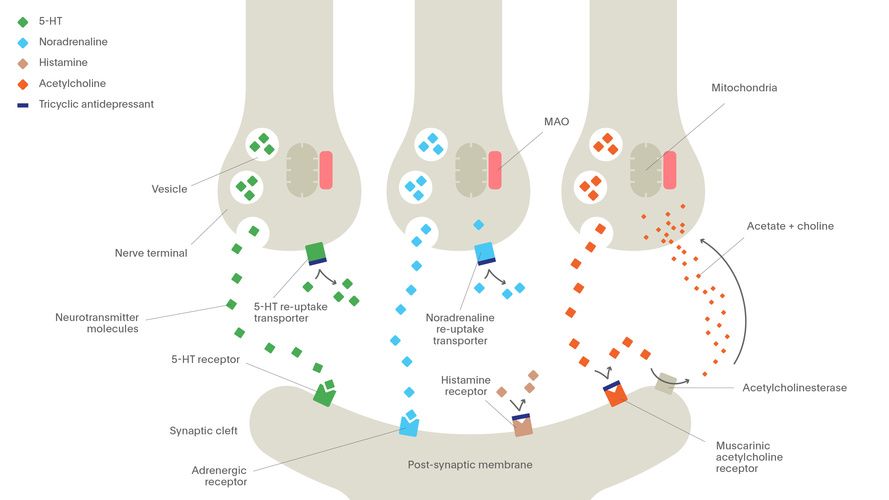
2. Effective biological therapy aimed at correcting mediator, toxic and autoimmune disorders leading to a specific schizophrenic vulnerability of the individual and the development of psychosis. In addition, biological therapy leads to a limitation of the patient's ability to maintain the previous style of intra-family response, which also creates conditions for changing the nature of intra-family relations and the patient's search for new opportunities for self-realization in the outside world. nine0003
nine0003
3. Contrasting communication based on "double binds" with the psychotherapist's paradoxical actions aimed at prescribing the patient in a disguised form of his own schizophrenic style of response. It also destroys the unconscious game of the patient and his loved ones: the continuation of the previous behavior and response now begins to mean submission to the psychotherapist and, accordingly, a clear definition of the relationship.
4. Given the inclination of patients with schizophrenia to trance functioning, hypnotherapy can also be used to gain access to their experiences and correct their personality, which, among other things, has a pronounced positive effect on biological processes that are also the driving forces of the disease - intoxication, autoimmune disorders, mediator metabolism disorders. However, most of these patients are less receptive to conventional hypnotic induction techniques due to negativism, impaired concentration, and thought disorders. Therefore, in these cases, hypnotic work should be preceded by cognitive training aimed at correcting these problems. nine0003
Therefore, in these cases, hypnotic work should be preceded by cognitive training aimed at correcting these problems. nine0003
5. The schizophrenic initiation of the myth-ritual complex "death-rebirth" (35) with the shifting of all one's problems and responsibility to the "ultimate savior" (40) should be replaced with the initiation of the development of a mature, a successful person, strong enough to, unlike many other people, successfully cope with all his difficulties both in the internal and external world (the script of his own exceptionalism) (40). This is especially necessary because schizophrenic patients, due to the dysfunctionality of their families, have many more examples of life failures and dead ends around them than successes, and in order to win, they often really need to become an exception to the general rule of life failures established in their family. nine0003
6. At the first stages of work with the patient, priority should be given not to the logical analysis of existing difficulties, but, first of all, to the patient's relatives performing specific actions demonstrating compliance with the new laws based on the principles of hierarchy and feedback.
These actions lead to the destruction of previous stereotypes in relationships, response style and behavior. But for the final solution of the issue, the patient and his relatives must be trained to act differently and accumulate sufficient experience in the harmonious expression of their feelings and problem-solving behavior both in matters of internal and external life. This also turns out to be important goals for further individual and family psychotherapy, as well as social and labor readaptation. This book "Practical Psychotherapy of Schizophrenia" is devoted to the presentation of practical ways to achieve these goals. nine0003
“This book is not a textbook. These are rather travel notes of a person who for 13 years, together with his colleagues, explored the field at the intersection of psychiatry and psychology, which seemed interesting to him - psychotherapy and rehabilitation of patients with schizophrenia.
We cannot say that we were the first here. Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as: People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills. At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms. nine0003 Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease. nine0003 Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life. Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment. nine0003 Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, cause isolation and disrupt health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder. At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals. Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education). steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care. nine0003 The WHO Mental Health Gap Action Program (mhGAP) is developing evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities. The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities. nine0003 (1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Many have worked here before us, and in many ways we have tried to follow in their footsteps. Some of what was described turned out to be true in our experience, something was not - and our experience will not be true in everything and not for everyone. Trying different things, we tried to systematize a variety of approaches, assuming that in all of them - such dissimilar methods of work of classical psychiatrists, psychoanalysts, cognitive-behavioral psychotherapists, NLP-ditch, hypnotists, family therapists, supporters of creative therapy - there is something general, which helps to defeat this terrible disease, which until recently was considered incurable. Madorsky V.V. nine0139
Many have worked here before us, and in many ways we have tried to follow in their footsteps. Some of what was described turned out to be true in our experience, something was not - and our experience will not be true in everything and not for everyone. Trying different things, we tried to systematize a variety of approaches, assuming that in all of them - such dissimilar methods of work of classical psychiatrists, psychoanalysts, cognitive-behavioral psychotherapists, NLP-ditch, hypnotists, family therapists, supporters of creative therapy - there is something general, which helps to defeat this terrible disease, which until recently was considered incurable. Madorsky V.V. nine0139
Key Facts
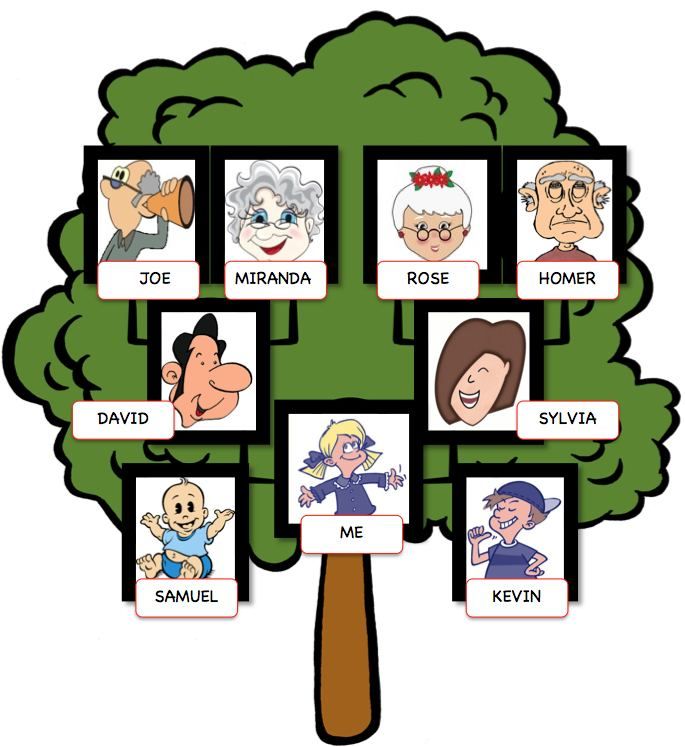
Symptoms
Scope and impact
 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.  nine0003
nine0003
Causes of schizophrenia
Assistance services  Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities. nine0003
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities. nine0003
Schizophrenia management and care  The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0003
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0003
WHO action 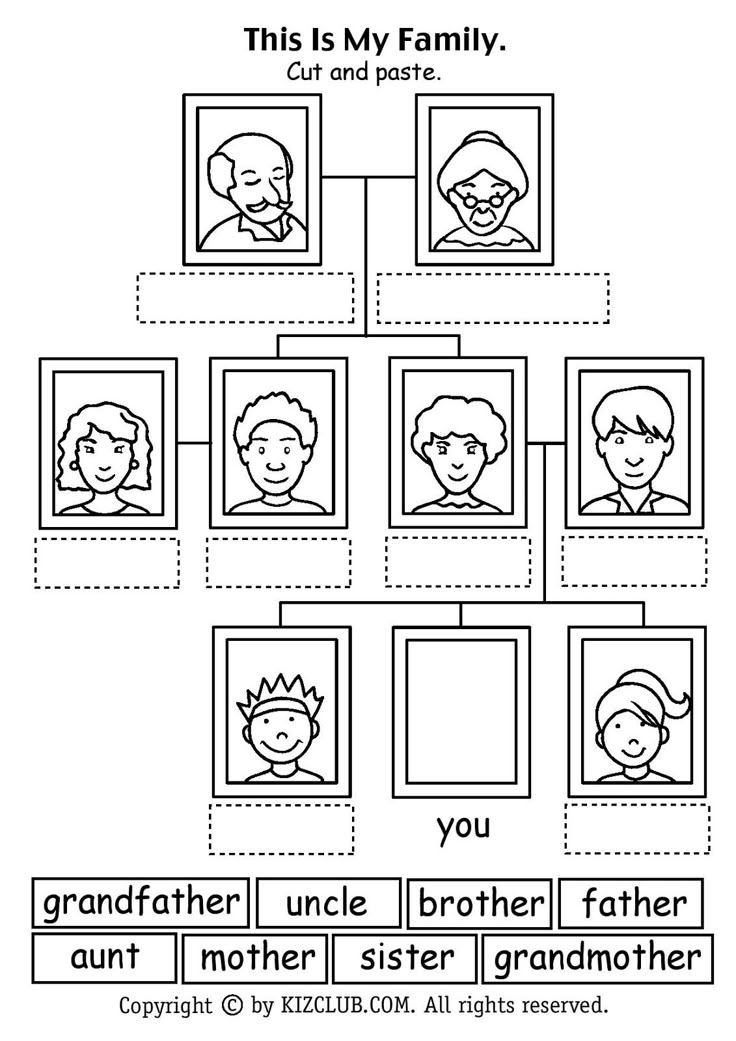 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0003
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0003 Bibliography