Fastest acting antidepressant
FDA Approves First Fast-Acting Drug for Clinical Depression
- The FDA just approved the first-ever “fast-acting” drug to treat clinical depression.
- The drug, Auvelity, from Axsome Therapeutics claims to start working within one week.
- Clinical trials have found the drug to be safe and quickly effective in helping patients experiencing depression.
A new medication called Auvelity was just FDA-approved to treat major depressive disorder (MDD), also known as clinical depression, in as little as one week. The new “fast-acting” oral drug for clinical depression, from Axsome Therapeutics, could change the way we treat mental health.
The medication is the first of its kind and was granted Breakthrough Therapy Designation by the FDA. Auvelity is an N-methyl D-aspartate (NMDA) receptor antagonist, marking the first new type of medication to be approved for clinical depression in 60 years.
We chatted with experts to break down what makes this drug different than the rest of the SSRIs on the market—and why it’s such a game-changer.
What is Auvelity?Auvelity is the first and only fast-acting oral treatment approved for statistically significant improvement in depressive symptoms in just one week compared to a placebo. The new medication is comprised of the two drugs dextromethorphan and bupropion, and should be available this year, but the price has yet to be announced.
In short, most antidepressant drugs work on the same neurotransmitters like dopamine and serotonin, but Auvelity focuses on glutamate receptors instead, Dan V. Iosifescu, M.D., professor of psychiatry at NYU Langone Health, a co-author on both the studies for Auvelity, and on the advisory board for this new drug tells Prevention.
He explains that for nearly 50 years there was nothing different in the science when it came to combating depression with medication. Then, there was a breakthrough with a medication called ketamine, which was able to work on a different mechanism within the brain to act as an antidepressant. The issue was that ketamine is somewhat addictive, and an FDA-approved version of it was only available in doctor’s offices with many restrictions.
Then, there was a breakthrough with a medication called ketamine, which was able to work on a different mechanism within the brain to act as an antidepressant. The issue was that ketamine is somewhat addictive, and an FDA-approved version of it was only available in doctor’s offices with many restrictions.
Researchers set out to find a pill people could take at home that was safer but acted on the same receptor, says Dr. Iosifescu. That’s when they started looking at dextromethorphan, an older drug that works similarly but was metabolized in the body very quickly. He explains that if researchers could pair the drug with something that stayed it in the body longer, they could harness the brain benefits and use it to improve depressive symptoms. That’s when doctors paired it with bupropion, an existing antidepressant, which was able to allow dextromethorphan to metabolize slower in the body.
This new drug comes just after research indicated depression may not be a chemical imbalance at all—or as closely linked to serotonin as we once thought.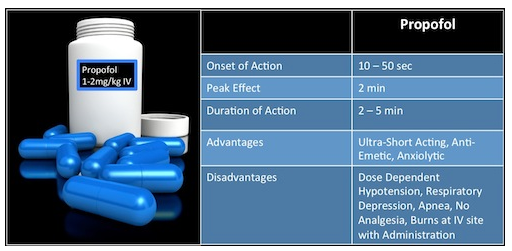 “We see depression to be much more complicated than a chemical imbalance, but involving neuroplastic changes—the ability for the brain to rewire itself and change pathways,” explains Tracey Marks, M.D., a general and forensic psychiatrist and owner of Marks Psychiatry.
“We see depression to be much more complicated than a chemical imbalance, but involving neuroplastic changes—the ability for the brain to rewire itself and change pathways,” explains Tracey Marks, M.D., a general and forensic psychiatrist and owner of Marks Psychiatry.
Dr. Marks suggests that current medications work as a “band-aid” by replacing serotonin levels instead of working on the problem itself. This new medication uses newer information to work similarly to ketamine but in a fast, well-tolerated manner, she says.
What does the research say?Research published in the Journal of Clinical Psychiatry found in a double-blind phase three clinical trial, 163 patients taking Auvelity said their feelings of depression significantly improved within a week compared to those taking a placebo. Another double-blind study found patients who took the drug felt a reduction in depressive symptoms compared to those taking doses of sustained-released bupropion (an existing antidepressant) alone.
For many people who experience clinical depression, commonly used antidepressants don’t work. These “treatment-resistant” patients need an alternative option, and that’s where this new drug comes in, Dr. Iosifescu explains to Prevention. He says that this new treatment option may be key in helping those patients who don’t respond to existing depression medications.
“Nearly two-thirds of patients treated with currently available antidepressants do not adequately respond, and those that do may not achieve clinically meaningful responses for up to six to eight weeks,” Maurizio Fava, M.D., psychiatrist-in-chief of the department of psychiatry at the Massachusetts General Hospital, said in a press release. “Given the debilitating nature of depression, the efficacy of Auvelity observed at one week and sustained thereafter may have a significant impact on the current paradigm for this condition.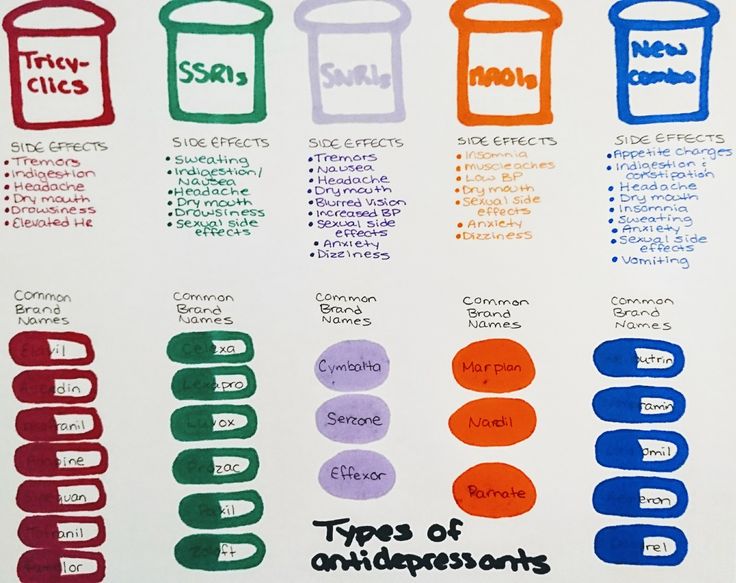 ”
”
Additionally, many current drugs on the market take at least six weeks to see results, which can be far too long for someone looking to function properly. This new medication has the speed of ketamine, without the barriers and restrictions that come along with it, Dr. Marks says. “It opens the door for more people to get treatment without hesitancy,” she adds. “To have an option that’s supposed to work within a week is a huge intervention that will be very transformative.”
Dr. Iosifescu says that Auvelity doesn’t have the same safety or addictive restrictions as ketamine, making it a much safer alternative. In general, it has similar side effects and warnings to existing antidepressant medications.
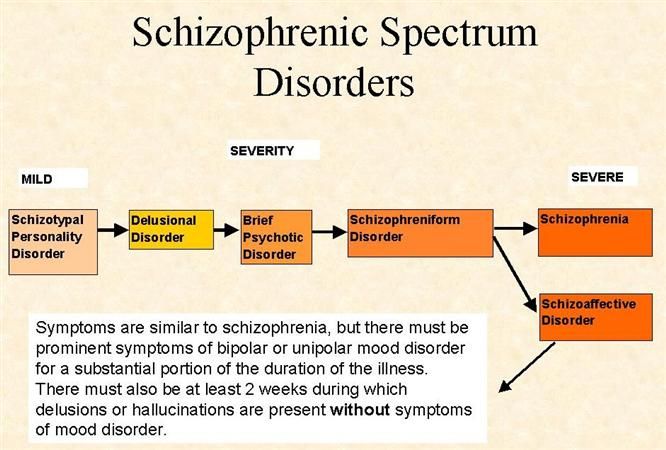
The medication information notes that Auvelity and other antidepressants may increase suicidal thoughts and actions in young adults, adolescents, and children.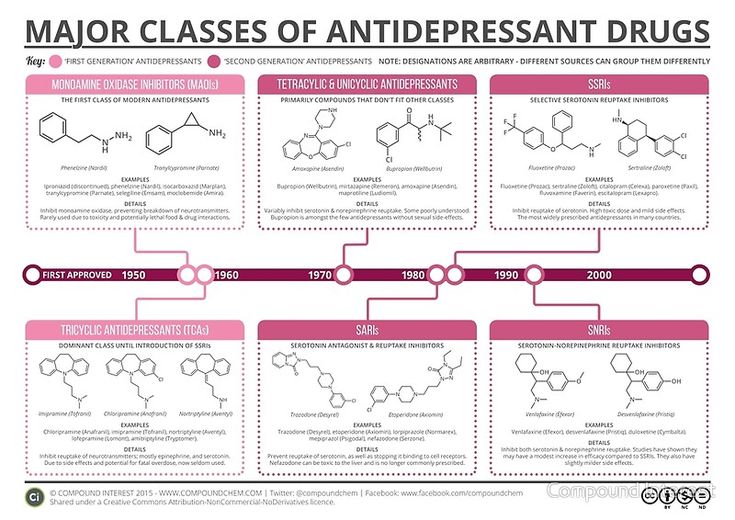 It’s essential to keep close attention to new or sudden changes in mood, behavior, thoughts, feelings, or suicidal thoughts when taking new medications of this nature.
It’s essential to keep close attention to new or sudden changes in mood, behavior, thoughts, feelings, or suicidal thoughts when taking new medications of this nature.
Additionally, Auvelity is not for those with seizure disorders, eating disorders, or those taking certain medications like monoamine oxidase inhibitors, benzodiazepines, barbiturates, or anti-seizure medicines. Check with your healthcare provider about additional risks or side effects of the drug before taking it.
Symptoms of depressionAccording to the National Alliance of Mental Illness (NAMI), about 21 million U.S. adults had at least one major depressive episode in 2020. The mental health disorder impacts people of all ages, races, ethnicities, or socioeconomic backgrounds. If a person experiences depressive symptoms for more than two weeks, they can be diagnosed with depression. Common symptoms of depression include:
- Changes in appetite
- Changes in sleep
- Lack of concentration
- Loss of energy
- Lack of interest in activities
- Hopelessness or guilty thoughts
- Less activity
- Physical aches and pains
- Suicidal thoughts
Dr. Marks says that if your depressive symptoms are getting in the way of your day-to-day life, it’s time to speak to a medical professional about treatment options.
Marks says that if your depressive symptoms are getting in the way of your day-to-day life, it’s time to speak to a medical professional about treatment options.
In addition to this new drug, people experiencing depression have many options for finding the best treatment that works for them. Additional antidepressants, mood stabilizers, and antipsychotic medications are available and can be prescribed by your healthcare provider. Psychotherapy (most often cognitive-behavioral therapy) with a therapist can also be done on its own or in tandem with medications, but this option requires time and commitment, Dr. Marks notes.
If you or someone you know is at risk, call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255) or text HOME to 741741 to message a trained crisis counselor from the Crisis Text Line for free.
Arielle Weg
Arielle Weg is the associate editor at Prevention and loves to share her favorite wellness and nutrition obsessions. She previously managed content at The Vitamin Shoppe, and her work has also appeared in Women’s Health, Men’s Health, Cooking Light, MyRecipes, and more. You can usually find her taking an online workout class or making a mess in the kitchen, creating something delicious she found in her cookbook collection or saved on Instagram.
She previously managed content at The Vitamin Shoppe, and her work has also appeared in Women’s Health, Men’s Health, Cooking Light, MyRecipes, and more. You can usually find her taking an online workout class or making a mess in the kitchen, creating something delicious she found in her cookbook collection or saved on Instagram.
Types, Time Frames, and More
It takes time before any antidepressant kicks in. But some medications relieve your symptoms faster than others.
Waiting for medication to work can be challenging. And if you’re having to try various options that don’t provide relief, finding a drug that does improve your symptoms can take a lot of time and effort.
Other options, such as ketamine and newer antidepressants, may help provide faster relief, reducing symptoms in days instead of weeks.
With the most common antidepressants, people usually start to feel the antidepressant effects after 1 to 2 weeks of taking the medication.
According to a 2008 review, you might notice the effects of selective serotonin reuptake inhibitors (SSRI) after a week of use, with symptoms continuing to improve for at least 6 weeks. The time frame varies based on each person’s circumstances.
The time frame varies based on each person’s circumstances.
Common antidepressants include:
- SSRIs such as fluoxetine (Prozac), citalopram (Celexa), and sertraline (Zoloft)
- serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine (Effexor), desvenlafaxine (Pristiq), and duloxetine (Cymbalta)
While these antidepressants work for many people, some other medication options have faster action and might be useful when a person doesn’t respond to other antidepressants (treatment-resistant depression) or needs relief right away to keep them safe.
Ketamine
Ketamine is a medication originally used for anesthesia and pain relief, but medical professionals also use it to help people with treatment-resistant depression.
Unlike other antidepressants, ketamine can improve depression symptoms in just a few hours. A 2018 clinical trial found that intravenous ketamine significantly and quickly reduced suicidal ideation in people with depression.
The Food and Drug Administration (FDA) approved a ketamine-derived drug called esketamine in 2019 for treatment-resistant depression. Esketamine comes in the form of a nasal spray.
Esketamine is part of a new class of antidepressant drugs called N-methyl-d-aspartate (NMDA) receptor blockers.
By blocking NMDA brain receptors, esketamine (and other NDMA receptor blockers) stimulate the release of the neurotransmitter glutamate, which helps create new neural connections. Experts believe that stimulating new brain connections can improve depression symptoms.
A 4-week study from 2015 of 30 people found that treatment involving ketamine and an SSRI (escitalopram )was well-tolerated and helped with severe depression symptoms, compared with those who took only the SSRI.
Ketamine and ketamine-derived products come with potential side effects, including:
- sedation
- dissociation
- dizziness
- nausea
- vertigo
- anxiety
- increased blood pressure
- vomiting
Because of the potential for severe side effects, a healthcare professional will need to monitor you for at least 2 hours after taking your first dose. And while the prescription nasal spray is easy to administer, you’ll need to take it in a doctor’s office and not at home.
And while the prescription nasal spray is easy to administer, you’ll need to take it in a doctor’s office and not at home.
The FDA warns that esketamine (brand name Spravato) can cause dissociation and sedation. There’s also the potential for misuse, so it’s listed as a schedule 3 drug on the Drug Enforcement Administration (DEA) list of controlled substances.
Other fast-acting medications
While esketamine is the only FDA-approved fast-acting antidepressant, research is ongoing to find new depression medications that offer faster relief than traditional options.
A 2021 clinical trial of a drug called zuranolone found that the drug significantly reduced symptoms in people with postpartum depression compared to the control group.
The FDA approved another drug called brexanolone in 2019, also for postpartum depression. Brexanolone is administered via infusion, unlike zuranolone, an oral drug.
Some antidepressant medications may also help quickly address anxiety symptoms.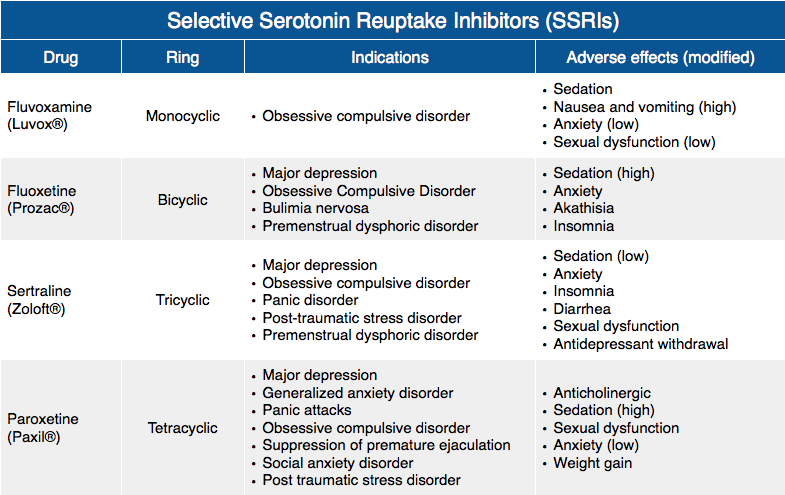 Still, they may not have the same effect on depression symptoms.
Still, they may not have the same effect on depression symptoms.
For example, a 2019 placebo-controlled trial found that sertraline, a type of SSRI medication, weakly improved depression symptoms within 12 weeks but reduced anxiety in half that time.
The gold standard treatment for depression involves therapy, medication, or both. But not everyone has access to treatments. Checking out affordable treatment options and learning to cope with the symptoms daily is helpful.
You might consider trying these coping tips:
- Make quality time for yourself. Whether that involves relaxing with your favorite book or soaking in a bubble bath after a long day, setting aside time for self-care may help provide some relief.
- Go for a walk. Being outdoors and getting exposure to sunlight can help boost vitamin D levels and improve your mood.
- Do something active. It can be hard to find the energy to move when feeling depressed, but even a short burst of exercise could release feel-good endorphins.

- Call up a friend. If talking on the phone isn’t appealing, send a text message or set up a video meeting to catch up. Depression can make you feel isolated, so setting aside time to be with others, whether online or in person, may help you feel less alone.
Looking for more tips? You can check out Psych Central’s article on how to feel better fast when you have depression.
Whether you’re trying a new depression medication for the first time or are curious about other options, finding the right antidepressant can take some time.
Learning about the options and talking about them with a doctor may help you feel better equipped to choose an antidepressant that’s right for your needs.
And while medication is often an important part of treating depression, therapy and self-care strategies are also valuable tools to consider.
Are you thinking about talking with someone about your depression symptoms but aren’t sure where to start? Consider checking out Psych Central’s How to Find Mental Health Support resource for more information.
A new class of fast-acting antidepressants discovered? — PCR News
Major depressive disorder is one of the most common mental disorders, affecting hundreds of millions of people. Antidepressants are prescribed for this condition, but they have significant drawbacks - withdrawal syndrome, delayed onset of action, increased risk of suicide or schizophrenia. A new solution was proposed by scientists from the Nanjing Medical University (China). The results of their work were published in Science .
Most modern antidepressants target the serotonin transporter SERT (aka 5-HTT), a membrane protein that reuptakes the neurotransmitter serotonin, that is, transports it from the synaptic cleft back to the presynaptic neuron. Selective serotonin reuptake inhibitors include fluoxetine, clomipramine, and other popular drugs. The authors of the new work found another promising way to influence SERT. In experiments on mice, they found that depression is inhibited by the dissociation of the serotonin transporter from NO synthase in the neurons of the dorsal raphe nucleus. They have developed a small molecule that acts on this target and could give rise to a new class of fast-acting antidepressants. nine0005
They have developed a small molecule that acts on this target and could give rise to a new class of fast-acting antidepressants. nine0005
Brainstem structures called raphe nuclei are one of the main sources of serotonin in the brain, both in humans and mice. The authors focused on the processes in the dorsal raphe nucleus. Activation of serotonin receptors in this structure has the opposite effect compared to the cortex or hippocampus - it does not excite, but suppresses the signals of serotonergic neurons and reduces the release of serotonin in other brain structures, causing a lack of this neurotransmitter. In depression, serotonin receptors in the dorsal raphe nucleus are overactive. nine0005
This is one of the problems in the treatment of depression - serotonin reuptake inhibitors activate, among other things, serotonin receptors of the raphe nuclei; this disturbs the balance of serotonin metabolism, and the response does not develop until a few weeks later, when the receptors in the dorsal nucleus lose their sensitivity.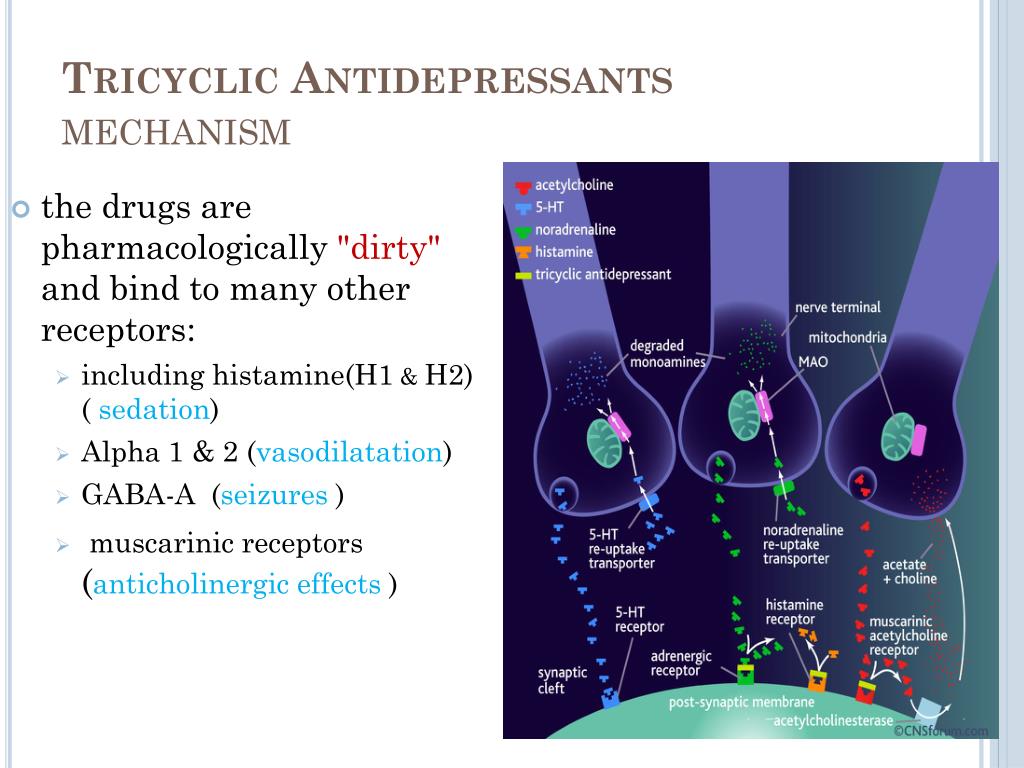
But blockers of the interaction between SERT and neuronal synthase (nNOS) can provide a rapid antidepressant effect. The formation of the nNOS-SERT complex in neurons of the dorsal raphe nucleus prevents translocation of the SERT transporter to the membrane, which leads to the accumulation of extracellular serotonin. The authors of the study developed a small molecule, SNIB ZZL-7, which interferes with the interaction of SERT with nNOS, and was convinced of its antidepressant effect. nine0005
To study the role of the SERT-nNOS complex in the development of depression, the scientists subjected mice to chronic uncontrolled stress for four weeks. The experimental animals demonstrated depressive behavior and increased the content of the SERT-nNOS complex in the neurons of the dorsal raphe nucleus. In mice with a knockout of the gene for neuronal NO synthase nNos , on the contrary, under chronic stress, behavioral tests showed antidepressant behavior, and the amount of SERT embedded in the neuronal membrane also increased. nine0005
nine0005
In addition, the scientists found in their earlier group of compounds based on short peptides called Sakura some molecules that can interact with NO synthase and facilitate the association of nNOS and SERT. In animals microinjected with these substances into the dorsal raphe nucleus, depressive behavior was observed, the level of the SERT-nNOS complex increased, and the amount of the SERT transporter on the membrane decreased. The same effects were observed in animals with recombinant NO synthase, which was unable to synthesize NO, but formed stronger complexes with the transporter. The researchers hypothesized that emotional stress may contribute to the association of SERT-nNOS, thereby leading to depression. nine0005
Using optogenetic methods, it was found that the destruction of the SERT-nNOS complex and the translocation of SERT to the membrane increases the activity of neurons and promotes the release of serotonin in the medial prefrontal cortex, and hence the development of a rapid antidepressant effect.
Finally, by studying the chemical mechanisms of SERT and nNOS binding, the scientists synthesized the small molecule ZZL-7, which reduced depression in experimental animals as early as two hours after intravenous administration. Additional tests showed that the compound did not affect memory, cognition, or aggression, but also did not cause abnormal brain activity. nine0005
The list of researchers studying fast-acting antidepressants is growing, notes Fierce Biotech. In August, Axsome Therapeutics Auvelity's NMDA receptor antagonist received FDA approval for use in major depressive disorder. Depressive symptoms improved in one week, complete remission was achieved in the second week. Johnson & Johnson's Spravato nasal spray, aka esketamine, a ketamine derivative, was approved by the FDA in 2019 for the rapid treatment of episodes of severe depression or suicidal thoughts. nine0005
Major depressive disorder accelerates cellular aging by years
New fast-acting class of antidepressants discovered
News > A new fast-acting class of antidepressants has been discovered
| Studies by American scientists have shown that selective suppression of a certain type of serotonin receptors produces a fast-acting antidepressant effect. Scientists note that it usually takes weeks, and sometimes months, for patients to take antidepressants to begin to show a therapeutic effect and relieve symptoms of the disease. To date, only preparations containing ketamine and scopolamine can have a fairly rapid effect on the human body, however, due to the presence of many serious side effects, none of them is suitable for adequate therapy. nine0005 Researchers at the University of Chicago have studied various receptors and signaling pathways for serotonin (5-hydroxytryptamine, or 5-HT), a neurotransmitter that affects mood, memory, and appetite. As a result, it was found that the 2c subtype was distinguished from all serotonin receptors in terms of the rate of manifestation of therapeutic effects. Blocking the 5-HT2c subtype of serotonin receptors is associated with the action of antidepressants such as mianserin, imipramine, maprotiline, desipramine and agomelatine. These drugs help improve sleep and suppress anxiety, fear and emotional stress. nine0005 Now, however, for the first time, scientists have shown that by selectively downregulating the 2c receptor subtype in mice with modeled depression, the condition of the animals improved significantly in as little as five days, while the usual minimum time for antidepressants to show their effects is about two weeks. "After administering to animals substances that selectively block the 2c subtype of serotonin receptors, we observed a rapid onset of therapeutic effect, which manifested itself in behavioral tests," Mark Opal, lead author of the study, was quoted by Medical Xpress as saying. nine0005 This serotonin receptor subtype inhibits the release of dopamine, another neurotransmitter associated with mood. |
 The results of the work, according to the authors, open up opportunities for the development of a potentially new class of therapeutic agents for the treatment of depression. Research data published 29October in the journal Molecular Psychiatry.
The results of the work, according to the authors, open up opportunities for the development of a potentially new class of therapeutic agents for the treatment of depression. Research data published 29October in the journal Molecular Psychiatry.