Schizophrenia is said to be acute when
Symptoms - Schizophrenia - NHS
Schizophrenia changes how a person thinks and behaves.
The condition may develop slowly. The first signs can be hard to identify as they often develop during the teenage years.
Symptoms such as becoming socially withdrawn and unresponsive or changes in sleeping patterns can be mistaken for an adolescent "phase".
People often have episodes of schizophrenia, during which their symptoms are particularly severe, followed by periods where they experience few or no symptoms. This is known as acute schizophrenia.
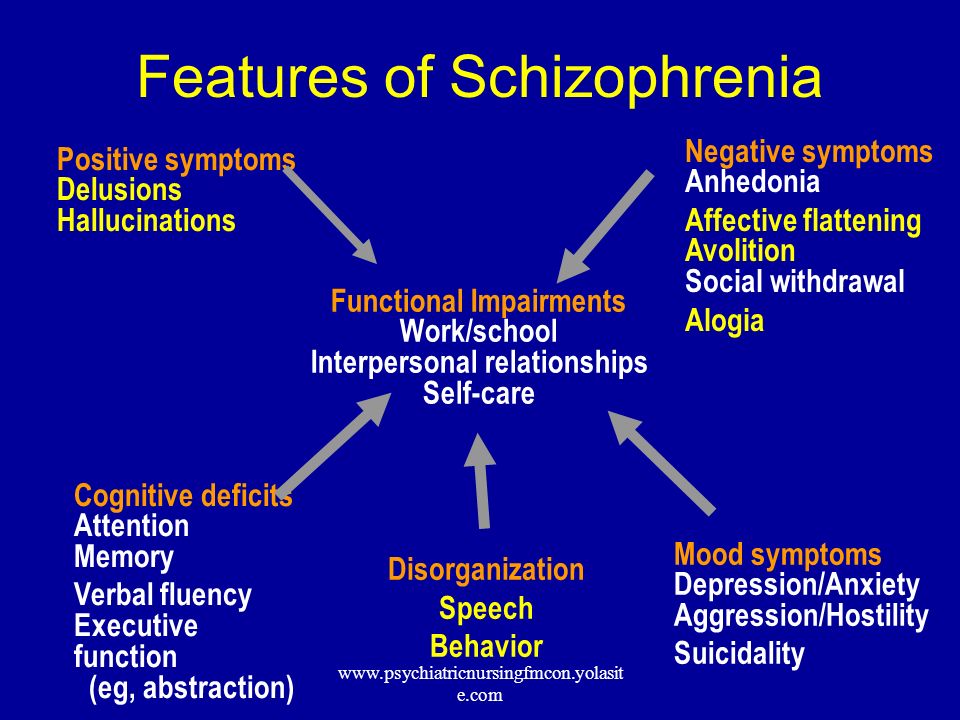
Positive and negative symptoms
The symptoms of schizophrenia are usually classified into:
- positive symptoms – any change in behaviour or thoughts, such as hallucinations or delusions
- negative symptoms – where people appear to withdraw from the world around then, take no interest in everyday social interactions, and often appear emotionless and flat
Hallucinations
Hallucinations are where someone sees, hears, smells, tastes or feels things that do not exist outside their mind. The most common hallucination is hearing voices.
Hallucinations are very real to the person experiencing them, even though people around them cannot hear the voices or experience the sensations.
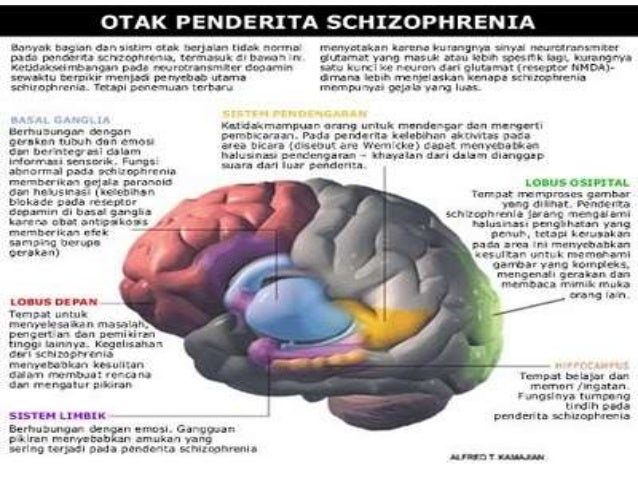
Research using brain-scanning equipment shows changes in the speech area in the brains of people with schizophrenia when they hear voices. These studies show the experience of hearing voices as a real one, as if the brain mistakes thoughts for real voices.
Some people describe the voices they hear as friendly and pleasant, but more often they're rude, critical, abusive or annoying.
The voices might describe activities taking place, discuss the hearer's thoughts and behaviour, give instructions, or talk directly to the person. Voices may come from different places or 1 place, such as the television.
Delusions
A delusion is a belief held with complete conviction, even though it's based on a mistaken, strange or unrealistic view. It may affect the way the person behaves.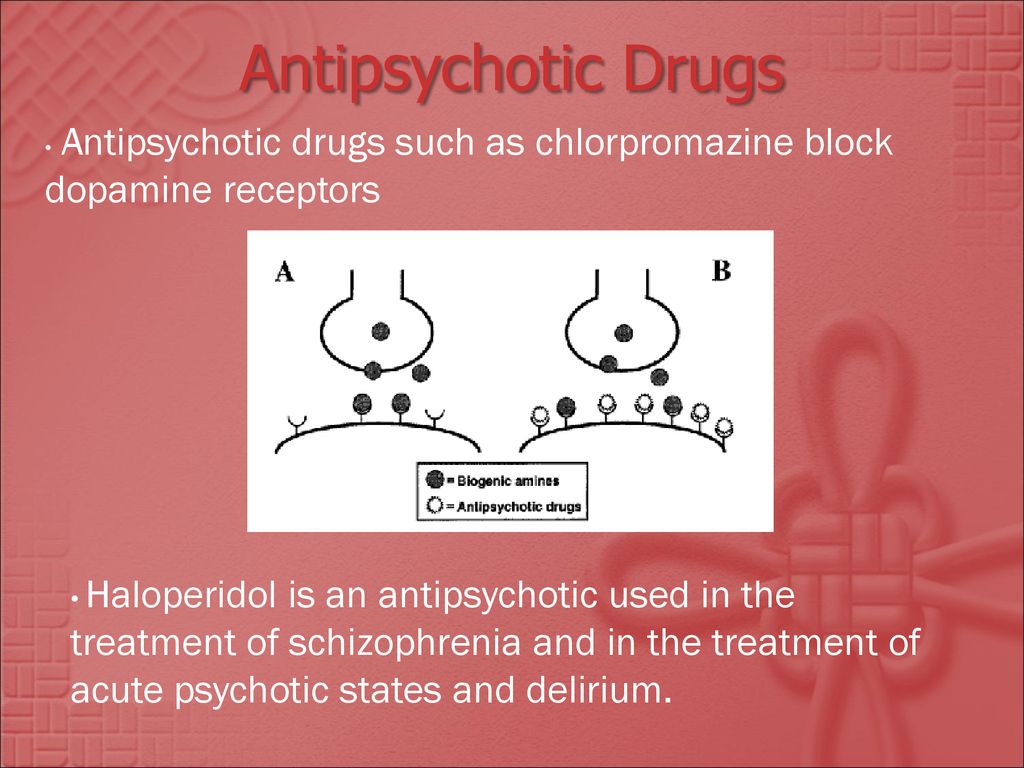 Delusions can begin suddenly or may develop over weeks or months.
Delusions can begin suddenly or may develop over weeks or months.
Some people develop a delusional idea to explain a hallucination they're having. For example, if they have heard voices describing their actions, they may have a delusion that someone is monitoring their actions.
Someone experiencing a paranoid delusion may believe they're being harassed or persecuted. They may believe they're being chased, followed, watched, plotted against or poisoned, often by a family member or friend.
Some people who experience delusions find different meanings in everyday events or occurrences.
They may believe people on TV or in newspaper articles are communicating messages to them alone, or that there are hidden messages in the colours of cars passing on the street.
Confused thoughts (thought disorder)
People experiencing psychosis often have trouble keeping track of their thoughts and conversations.
Some people find it hard to concentrate and will drift from one idea to another.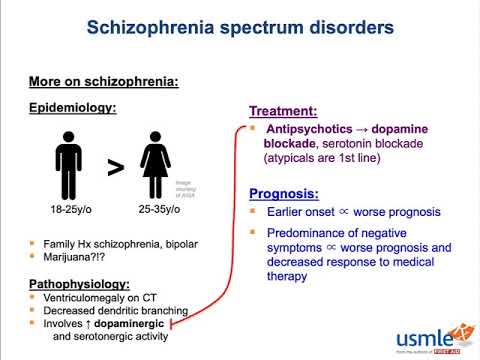 They may have trouble reading newspaper articles or watching a TV programme.
They may have trouble reading newspaper articles or watching a TV programme.
People sometimes describe their thoughts as "misty" or "hazy" when this is happening to them. Thoughts and speech may become jumbled or confused, making conversation difficult and hard for other people to understand.
Changes in behaviour and thoughts
A person's behaviour may become more disorganised and unpredictable.
Some people describe their thoughts as being controlled by someone else, that their thoughts are not their own, or that thoughts have been planted in their mind by someone else.
Another feeling is that thoughts are disappearing, as though someone is removing them from their mind.
Some people feel their body is being taken over and someone else is directing their movements and actions.
Negative symptoms of schizophrenia
The negative symptoms of schizophrenia can often appear several years before somebody experiences their first acute schizophrenic episode.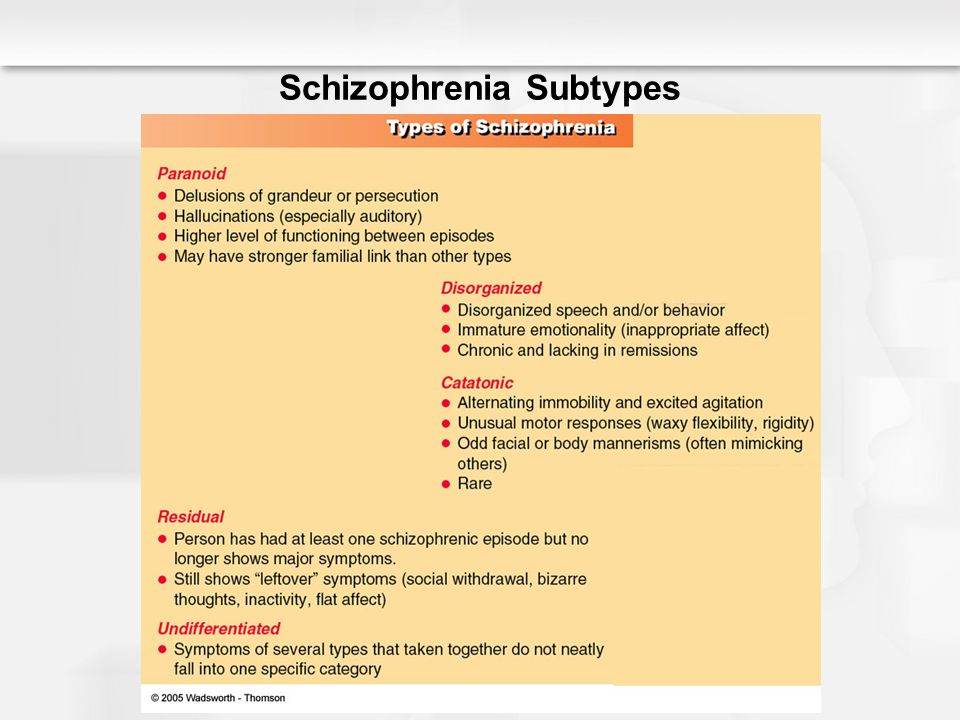
These initial negative symptoms are often referred to as the prodromal period of schizophrenia.
Symptoms during the prodromal period usually appear gradually and slowly get worse.
They include the person becoming more socially withdrawn and increasingly not caring about their appearance and personal hygiene.
It can be difficult to tell whether the symptoms are part of the development of schizophrenia or caused by something else.
Negative symptoms experienced by people living with schizophrenia include:
- losing interest and motivation in life and activities, including relationships and sex
- lack of concentration, not wanting to leave the house, and changes in sleeping patterns
- being less likely to initiate conversations and feeling uncomfortable with people, or feeling there's nothing to say
The negative symptoms of schizophrenia can often lead to relationship problems with friends and family as they can sometimes be mistaken for deliberate laziness or rudeness.
Psychosis
Schizophrenia is often described by doctors as a type of psychosis.
A first acute episode of psychosis can be very difficult to cope with, both for the person who is ill and for their family and friends.
Drastic changes in behaviour may occur, and the person can become upset, anxious, confused, angry or suspicious of those around them.
They may not think they need help, and it can be hard to persuade them to visit a doctor.
Read more about understanding psychotic experiences.
Acute schizophrenia: Definition, symptoms, treatments
Schizophrenia is a chronic mental health condition that can affect a person’s perceptions, cognition, and behavior. The condition has three distinct phases, which doctors refer to as “prodromal,” “acute,” and “residual.” Acute schizophrenia is the phase in which a person shows obvious signs of the condition, such as hallucinations, delusions, and disordered thoughts and behavior.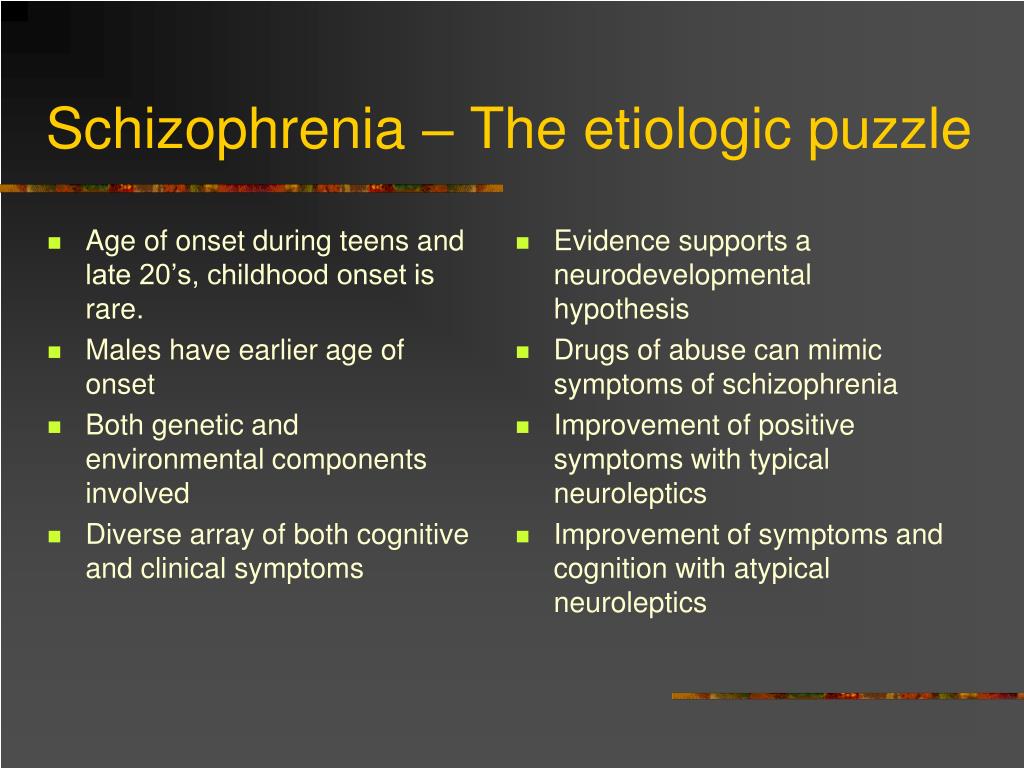
Treatments, such as medications, psychological therapies, and lifestyle changes can help manage and alleviate the symptoms of schizophrenia. In many cases, these treatments improve a person’s functioning and quality of life.
This article gives a definition of acute schizophrenia, and lists the symptoms. We also list the possible causes of schizophrenia and the treatment options available. Finally, we provide general tips and advice for people experiencing acute schizophrenia.
Schizophrenia is a type of psychosis, meaning it causes significant changes to a person’s perceptions, thoughts, beliefs, and behaviors.
The condition has three phases:
- Prodromal phase: This is the earliest phase, in which a person begins to experience changes within themselves. However, they are not yet experiencing obvious symptoms of psychosis.
- Acute or “active” phase: This is when a person experiences obvious and typically distressing symptoms of psychosis.
- Residual or “recovery” phase: This is the recovery phase, in which a person experiences fewer or no obvious symptoms of psychosis.
Symptoms a person may experience during the acute phase of schizophrenia include:
- hallucinations
- delusions
- disordered thoughts
- disorganized speech
- disorganized behavior
- lack of motivation
Schizophrenia symptoms will differ according to the phase of psychosis a person is experiencing.
According to the American Psychiatric Association (APA), the symptoms a person experiences during the acute phase of schizophrenia fall into the following three categories:
- Positive symptoms: These include thoughts and behaviors that do not normally occur in the person’s day-to-day life, such as:
- exaggerated or distorted perceptions, beliefs, or behaviors
- visual or auditory hallucinations
- paranoia
- Negative symptoms: These are thoughts and behaviors that used to be typical for the person but no longer occur.
 Examples include a loss or decrease in the following:
Examples include a loss or decrease in the following:- ability to speak or express emotions
- ability to find pleasure
- ability to make plans with others
- Disorganized symptoms: These are thoughts and behaviors that are unusual for the person, such as:
- confused and disordered thinking and speech
- abnormal movements
- bizarre behavior
Schizophrenia is a chronic condition that consists of several phases, one of which is the “acute” phase. This simply means that the person is experiencing a flare-up of symptoms following a period when their symptoms were less severe.
Sometimes, the acute phase occurs when the person stops taking their medication, while other times, it may occur for no apparent reason.
However, it is possible for a person to develop what doctors refer to as brief psychotic disorder. A person living with this condition typically develops schizophrenia symptoms that remain stable but last no longer than 1 month.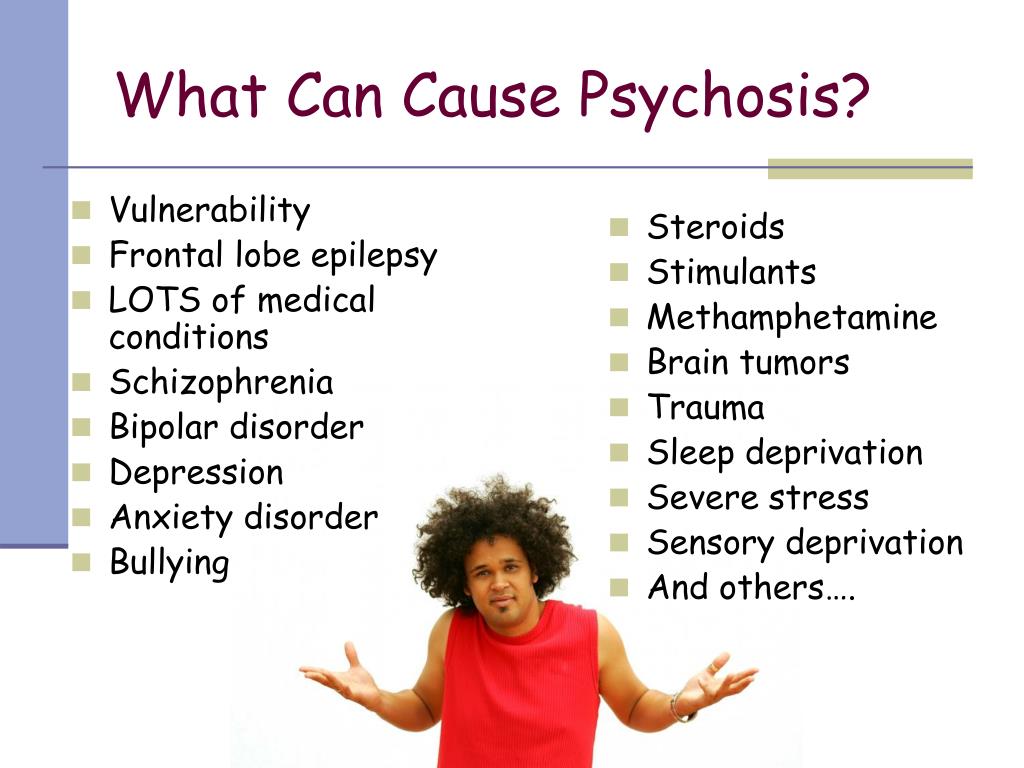
If symptoms persist for 1–6 months, a doctor will typically change the diagnosis to schizophreniform disorder. If symptoms persist beyond 6 months, the diagnosis will be schizophrenia.
Schizophrenia typically develops slowly over time. However, during the initial or “prodromal” phase, a person may not display any obvious signs of the condition. As such, it is possible that a doctor will fail to notice or diagnose the condition until the symptoms have become more evident.
In some cases, a doctor may mistake the symptoms of schizophrenia for typical developmental issues, as is often the case when a teenager develops the condition.
Experts have not identified the exact cause of schizophrenia. However, some possible explanations include:
- Genetics: Schizophrenia can run in families. However, having a parent or relative living with the condition does not mean that a person will automatically develop the condition themselves.
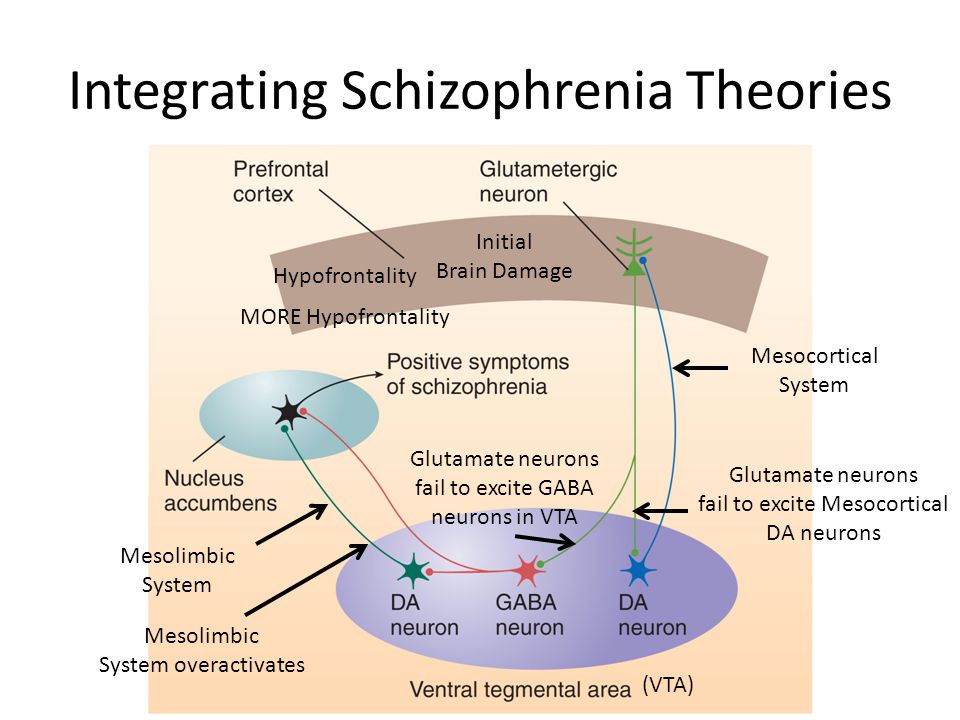
- Differences in brain chemistry: People with schizophrenia may have neurotransmitters that work differently.
- Substance use or misuse: Cannabis use may increase a person’s risk of developing schizophrenia.
- Environmental factors: Exposure to infections or malnutrition in utero may contribute to the development of schizophrenia.
There is no cure for schizophrenia. However, treatments are available that can help a person with schizophrenia live a productive and fulfilling life.
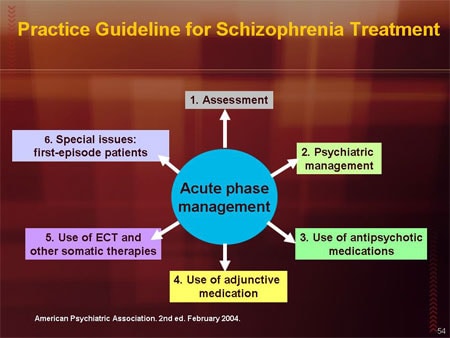
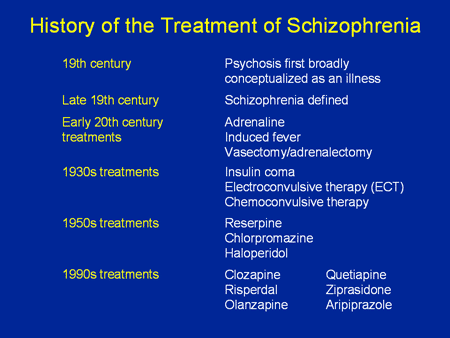
Doctors may recommend several treatment methods to help a person with schizophrenia achieve symptom remission. Common treatment methods include:
- antipsychotic medications, such as risperidone, aripiprazole, and olanzapine
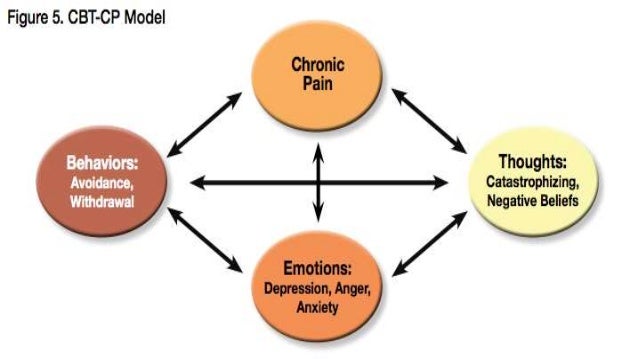
- behavioral therapies, such as cognitive behavioral therapy or cognitive enhancement therapy
- group therapies and support groups
- complementary therapies, such as:
- omega-3 supplementation
- acupuncture
- meditation
In addition, doctors often monitor a person living with schizophrenia for signs of substance use or misuse.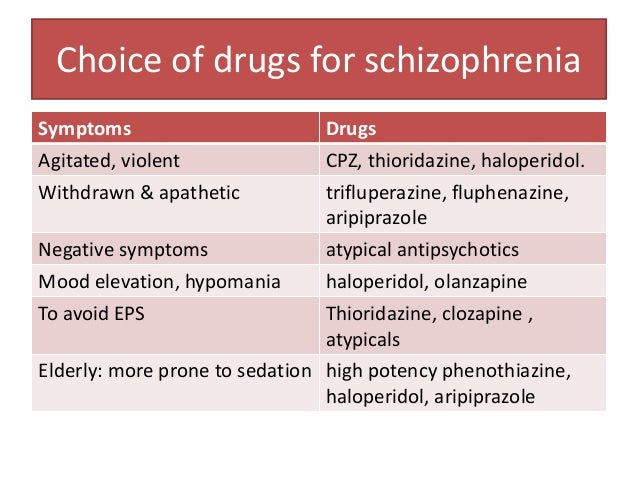 If a person uses or misuses drugs or medications, a doctor will likely take steps to treat addiction.
If a person uses or misuses drugs or medications, a doctor will likely take steps to treat addiction.
In addition to therapies and medications, a person can take steps in their everyday life to manage schizophrenia and help prevent acute phases of the condition.
The Substance Abuse and Mental Health Services Administration provides a list of daily habits that could help ease the challenges of schizophrenia. Examples include:
- learning the warning signs of an acute episode, and seeking help as soon as possible
- staying committed to the treatment plan, and letting the doctor know if symptoms are worsening
- staying focused on treatment goals and sharing those goals with family and friends
- talking with a doctor about social assistance for living and working in the community
- joining a support group
- avoiding drinking alcohol, smoking, and taking drugs recreationally
- practicing relaxation and stress management techniques daily
Acute schizophrenia typically refers to the active phase of schizophrenia, in which a person shows signs and symptoms of the mental health disorder.
However, In some cases, a doctor may use the term “acute schizophrenia” to refer to an acute schizophrenia-like disorder. This is a short-lived mental health condition with schizophrenia-like symptoms. However, it is not the same as schizophrenia.
While there is no cure for schizophrenia, treatments are available to help manage and lessen the symptoms. Certain lifestyle changes may also help to keep the condition under control.
A person who is experiencing symptoms of schizophrenia should talk with their doctor for further advice and treatment.
PKB No. 5 - Schizophrenia
Moscow State Budgetary Institution of Healthcare
Psychiatric Clinical Hospital No. 5 of the Moscow City Health Department
+7 (495) 445-55-25, +7 (496) 724-33 -33
Moscow region, Chekhov, s. Troitskoe, 5
Medical Tourism
Site search
Schizophrenia is a chronic mental illness, which is characterized by a violation of the unity of thought processes, with a relatively intact intellect, which is combined with significant emotional impoverishment and a decrease in will.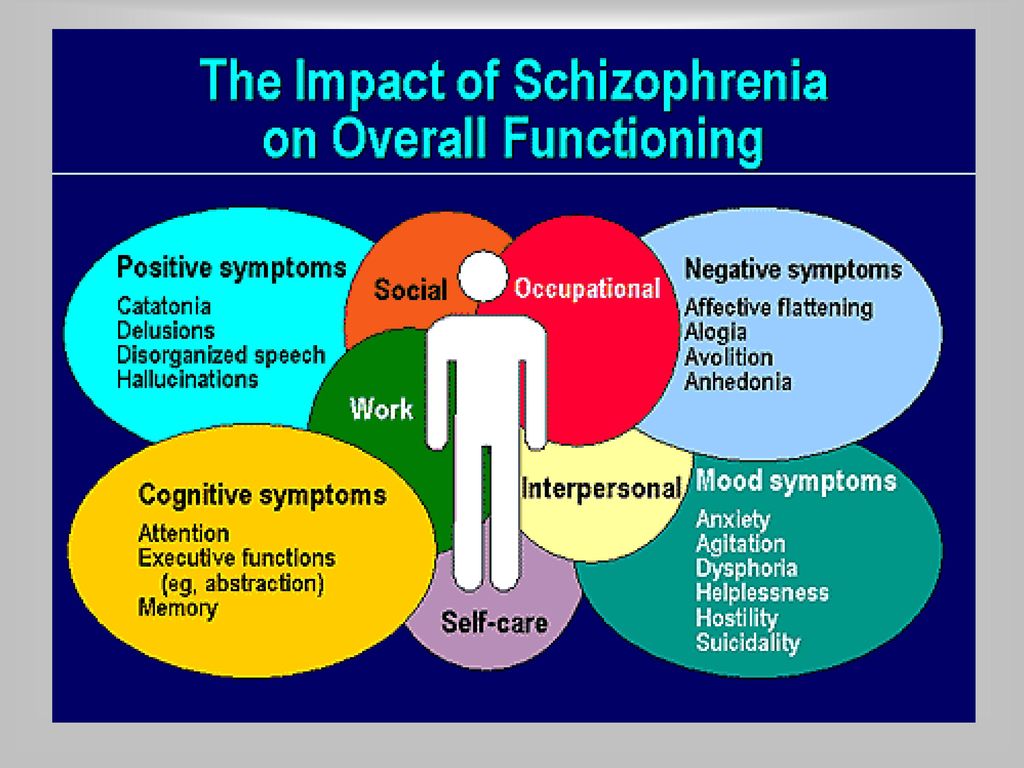 Often hallucinatory and delusional disorders join.
Often hallucinatory and delusional disorders join.
The term "schizophrenia" itself is made up of two Greek words - "schizo" - splitting and "freni" - mind reason.
This term was first used by the Swiss psychiatrist Eigen Bleuler in 1908y. Schizophrenia, of course, existed before, but only by the beginning of the 20th century did the idea of it as a special kind of psychosis mature.
In the mass consciousness there is an unreasonable identification of schizophrenia with a "split personality" - that is, in fact, with a very rare mental disorder in which different "I"s are alternately activated in one person.
Schizophrenia, unfortunately, is quite common. Its prevalence among the Russian population is 35 per 10,000 people, with no significant difference between the sexes. Thus, in Russia there are at least half a million patients with this serious pathology.
Schizophrenia refers to endogenous mental illness, which means that it is an internal breakdown of the psyche.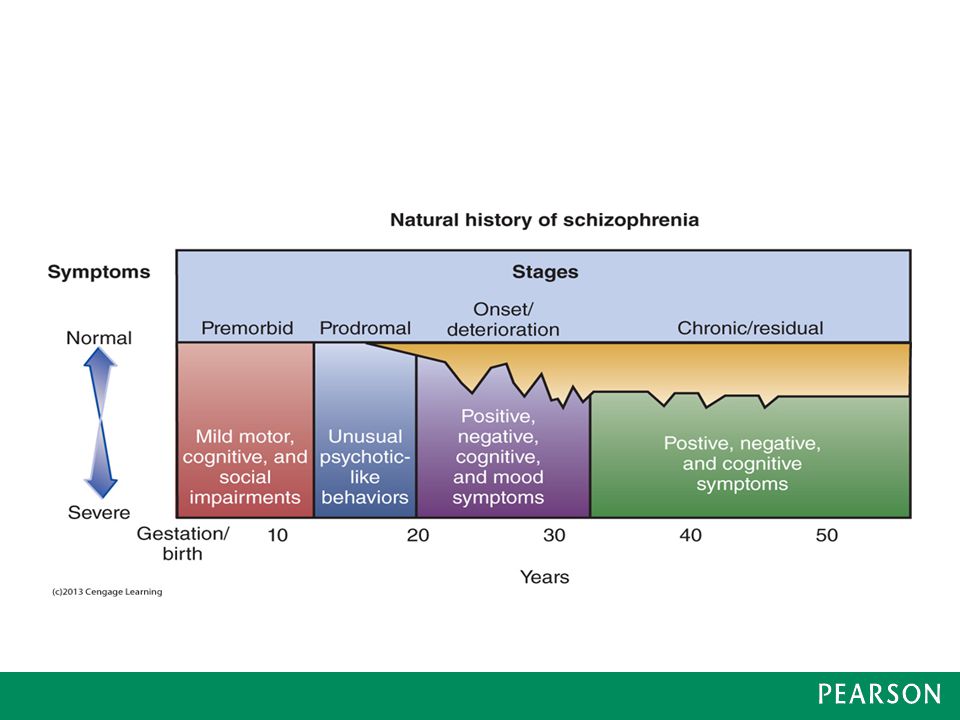 It cannot be caused by any factors acting on the brain from the outside (trauma, intoxication, severe stress). Of course, these factors can affect the rate of development of schizophrenia, but not its occurrence. However, the mechanism of development of the schizophrenic process has not yet been established with certainty. There are several hypotheses about this. Thus, there is evidence of a relationship between schizophrenia and a violation of the distribution of dopamine in the central nervous system.
It cannot be caused by any factors acting on the brain from the outside (trauma, intoxication, severe stress). Of course, these factors can affect the rate of development of schizophrenia, but not its occurrence. However, the mechanism of development of the schizophrenic process has not yet been established with certainty. There are several hypotheses about this. Thus, there is evidence of a relationship between schizophrenia and a violation of the distribution of dopamine in the central nervous system.
The role of heredity is very great. So, if one of the twins fell ill with schizophrenia, then the risk of getting sick for the other twin is 17% in a fraternal couple and 48% in an identical one. However, it is believed that in half of the cases of schizophrenia arises from a random mutation, that is, on the basis of genetic changes that were absent in the parents and appeared after conception.
Symptoms can develop at any age (possibly even in utero), but usually its onset is timed to coincide with the third pubertal crisis, that is, by the age of 12-18 years or several years later (up to about 30 years).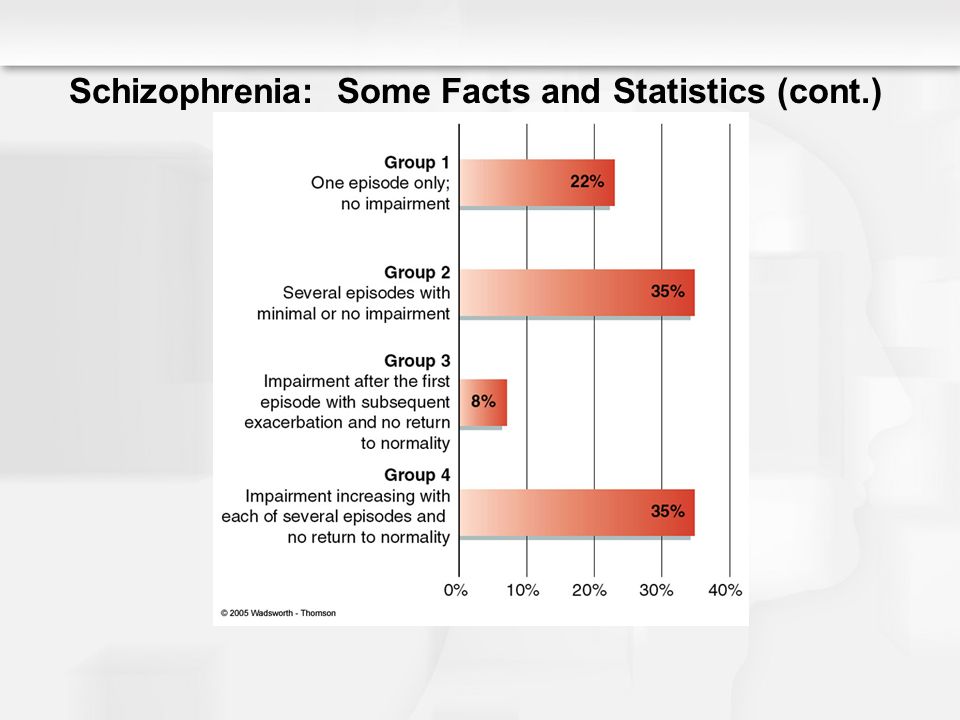
Most often, the disease begins with negative symptoms associated with the loss of normal functioning - a person changes in character for no apparent reason, becomes closed, fenced off, loses social contacts, emotional warmth in relation to relatives disappears. Former interests disappear, school or university performance drops sharply, or official duties are not fulfilled. Thus, from the very beginning of clinical manifestations there is a very high risk of disability. In the most unfavorable variant, which is designated as simple schizophrenia, the patient can lie for days on end, staring at the ceiling, and with a clear mind and normal physical strength, he is not able to simply serve himself. Even with more favorable options, thinking disorders increase, which are expressed in the influx of thoughts or in the feeling that there are no thoughts at all. Reasoning becomes unproductive, unfocused, an ambivalent attitude to life phenomena (ambivalence) is formed. Speech is distinguished by ornateness, sometimes with neologisms that the patient himself comes up with. During the conversation, there are distractions from his topic (sliding), and not to specific details and circumstances, but to the “bad” attitude of certain characters towards the patient, or to global philosophical topics. People with schizophrenia tend to be somewhat cynical about many aspects of their environment.
During the conversation, there are distractions from his topic (sliding), and not to specific details and circumstances, but to the “bad” attitude of certain characters towards the patient, or to global philosophical topics. People with schizophrenia tend to be somewhat cynical about many aspects of their environment.
Patients have a painful feeling that everything around is somehow changed, devoid of naturalness, harmony (- derealization), the same feelings can arise in relation to their personality (- depersonalization). With depersonalization, the consciousness (but not the personality!) seems to split in two: one part of it looks at what is happening from the side, and the other is horrified by the realization of the loss of control over oneself.
One's own thoughts and ideas begin to be perceived as alien. According to modern views, this is why schizophrenia has verbal hallucinations (“voices”), and it is not surprising that the sound of “voices” inside the head is typical for this disease. For the same reason, it seems to the patient that someone controls him from the outside, up to the control of movements and the work of internal organs. Visions are less common.
For the same reason, it seems to the patient that someone controls him from the outside, up to the control of movements and the work of internal organs. Visions are less common.
Such a growing wave of unusual sensations is very painful. In many cases, internal tension is somewhat relieved by the formation of delusional ideas (quickly - like an insight - the crystallization of delirium occurs). It suddenly becomes “clear” to the patient that what is happening to him is, for example, the “intrigues” of some “organization”, which, with the help of modern equipment, “influences” him from the outside (delusions of persecution, influence). There is also delusions of jealousy, damage. It is clear that the plot of experiences is influenced by the level of development of society, including the plots of popular works of literature and cinema.
This whole clinical picture often develops acutely, in the form of an attack that lasts from several days to several months, and then may recur.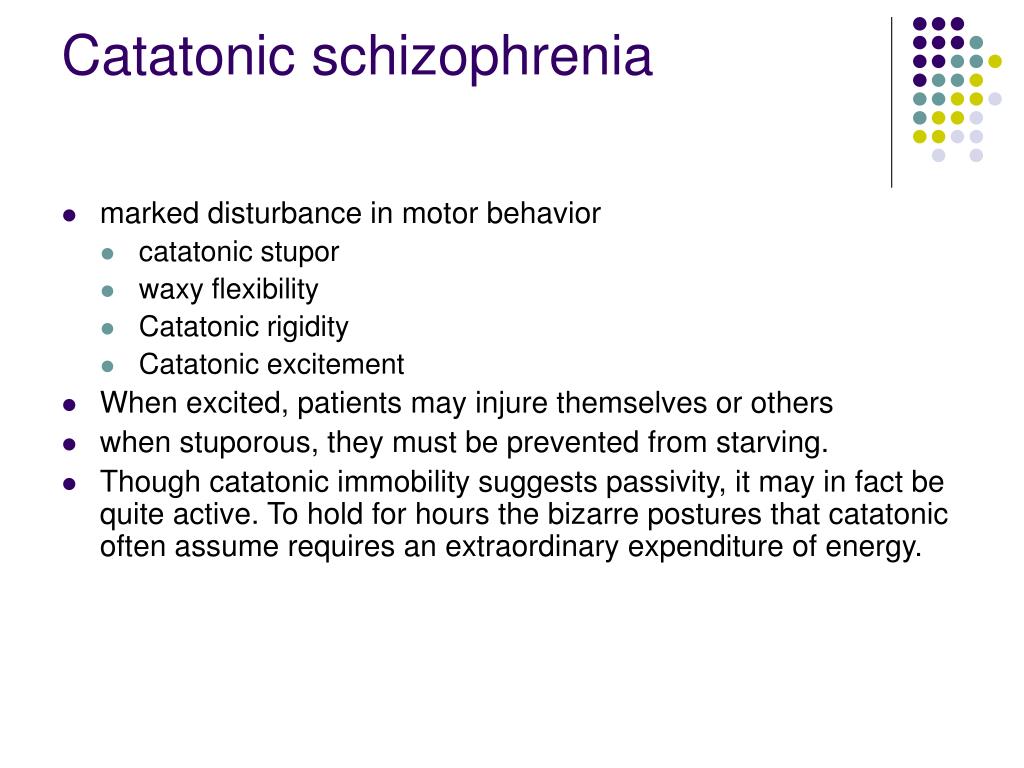 Attack-like forms of schizophrenia are more favorable, in terms of prognosis, than continuous ones. The intervals between attacks are very long (sometimes - tens of years), and between them the person looks almost the same as before, before the illness. But this is rather an exception. Much more often, exacerbations of symptoms are repeated annually or several times a year, and after each new attack, it turns out that the will has become even weaker and emotions have faded even more. Gradually, over many years, hallucinatory experiences become less relevant. Parallel, but also very slowly, delirium is falling apart as a system of pseudo-logical conclusions - separate fragments of delirium remain. As a result, a state of defect develops, which resembles simple schizophrenia.
Attack-like forms of schizophrenia are more favorable, in terms of prognosis, than continuous ones. The intervals between attacks are very long (sometimes - tens of years), and between them the person looks almost the same as before, before the illness. But this is rather an exception. Much more often, exacerbations of symptoms are repeated annually or several times a year, and after each new attack, it turns out that the will has become even weaker and emotions have faded even more. Gradually, over many years, hallucinatory experiences become less relevant. Parallel, but also very slowly, delirium is falling apart as a system of pseudo-logical conclusions - separate fragments of delirium remain. As a result, a state of defect develops, which resembles simple schizophrenia.
Patients either do not recognize themselves as ill or have conflicting thoughts about it. As a rule, they negatively meet the persuasion of relatives about the need to contact a psychiatrist. There are attempts to alleviate their condition with alcohol and drugs, which only complicates the clinical picture and leads to further social maladaptation.
Under the influence of orders "voices" and against the background of delusional experiences, the risk of socially dangerous actions of patients increases. For example, cases of attacks on imaginary "persecutors" are known. But much more often, patients with endogenous mental pathology commit OOD through other mechanisms, including when their behavior is influenced by alcohol or drug intoxication, which is superimposed on negative symptoms.
Schizophrenia is the most common disease among patients in the Clinical Hospital No. 5 in Moscow.
Common diagnosis: Paranoid schizophrenia, episodic course with progressive defect, incomplete remission. The clinical picture with this diagnosis includes delusions and hallucinations (usually delusions of persecution and verbal hallucinations - "voices").
Treatment of schizophrenia includes antipsychotics, antidepressants, nootropics. The leading role belongs to antipsychotics, the action of which is aimed primarily at combating delusions and hallucinations.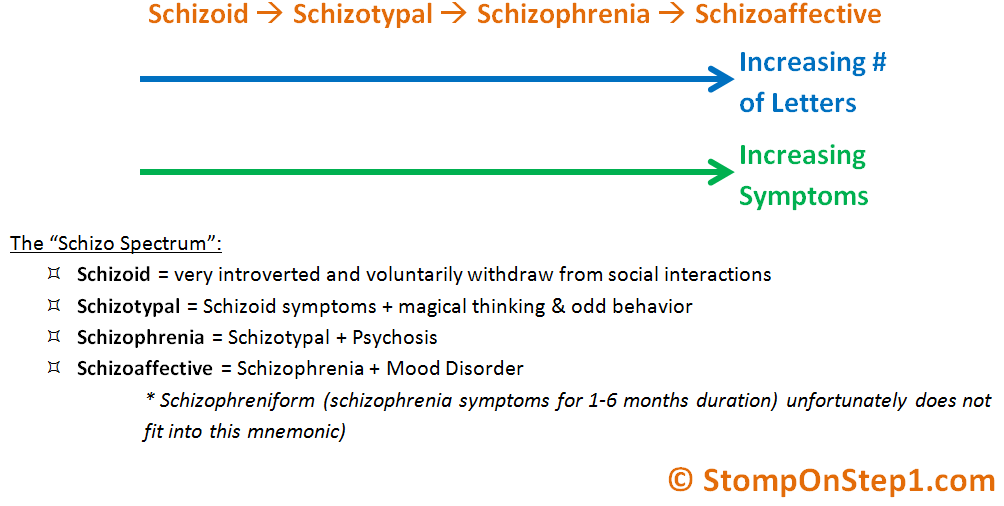 Against the background of treatment, at first, as a rule, the patient's affective reaction to his own experiences is dulled - he becomes calmer, psychomotor agitation passes. Then the hallucinations decrease in intensity or completely disappear. All these positive changes become noticeable already in the first days of the use of neuroleptics. But the plot (that is, the plot) of delirium can linger for a long time, although in the picture of internal experiences it fades significantly in relevance. After the relief of acute symptoms, the task comes to the fore: how to reduce negative symptoms and eliminate psychopathic (that is, as in psychopathy) behavioral disorders. This is helped by neuroleptics of the latest generations, such as olanzapine, paliperidone, risperidone. Already at this stage, it is worth thinking about the rehabilitation of the patient. Contrary to the earlier opinion, psychotherapy is indicated for these patients, and it helps to strengthen remission and resocialization.
Against the background of treatment, at first, as a rule, the patient's affective reaction to his own experiences is dulled - he becomes calmer, psychomotor agitation passes. Then the hallucinations decrease in intensity or completely disappear. All these positive changes become noticeable already in the first days of the use of neuroleptics. But the plot (that is, the plot) of delirium can linger for a long time, although in the picture of internal experiences it fades significantly in relevance. After the relief of acute symptoms, the task comes to the fore: how to reduce negative symptoms and eliminate psychopathic (that is, as in psychopathy) behavioral disorders. This is helped by neuroleptics of the latest generations, such as olanzapine, paliperidone, risperidone. Already at this stage, it is worth thinking about the rehabilitation of the patient. Contrary to the earlier opinion, psychotherapy is indicated for these patients, and it helps to strengthen remission and resocialization.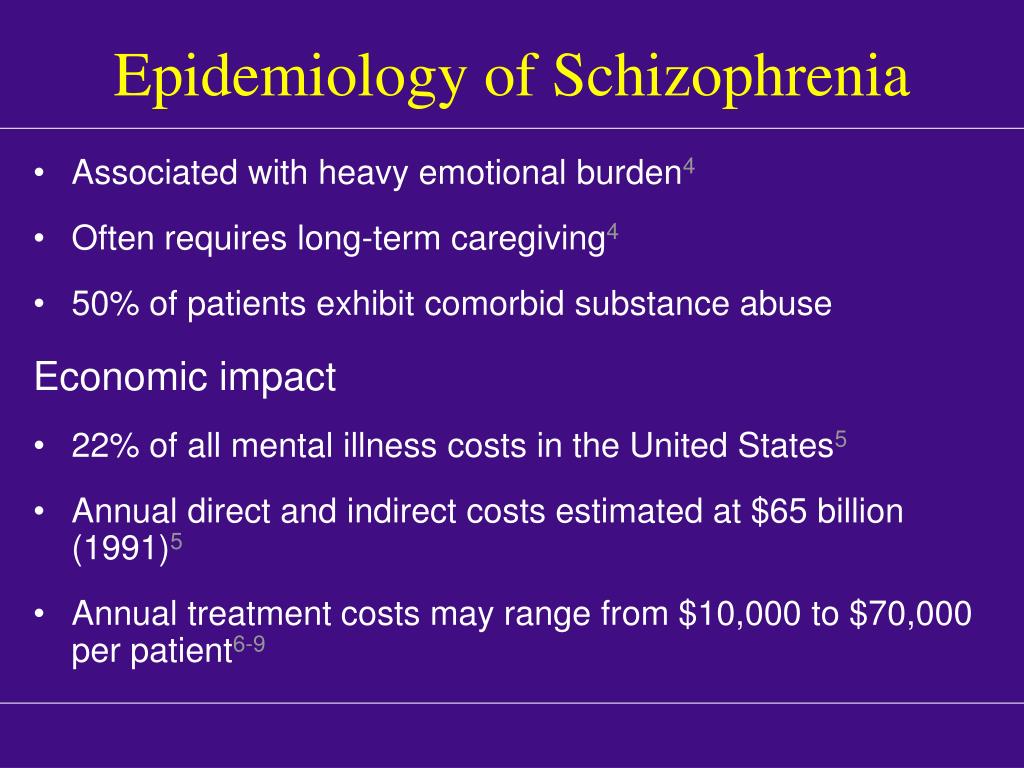 A good prognostic sign is the participation of the patient in physical labor, which, in itself, brings a significant therapeutic effect.
A good prognostic sign is the participation of the patient in physical labor, which, in itself, brings a significant therapeutic effect.
Although schizophrenia is a very formidable disease, it is not a death sentence. Due to the partial preservation of certain abilities (especially intellectual ones) and non-standard thinking, many of these patients have significant creative potential, which can be seen, among other things, from the works presented at the Ariadne's Thread festival of arts.
- Back
- Forward
- Are you here:
- Main page GBUZ "PKB No. 5 DZM" /
- For visitors /
- About mental disorders /
- Schizophrenia
Schizophrenia
Schizophrenia- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find the country »
- A
- B
- B
- g
- D
- ё
- and
- I
- К
- Л
- М
- Н
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective options for helping patients with schizophrenia, which can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in the perception of reality and behavioral changes, such as:
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Magnitude of the problem and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.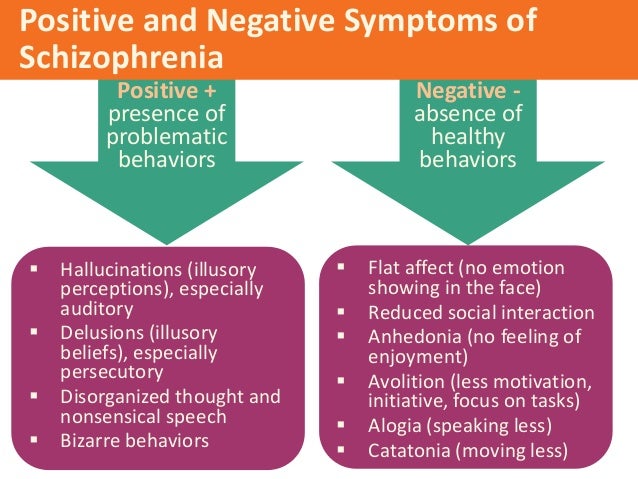
People with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause severe stress and fear, disrupt social support mechanisms, cause isolation and disrupt health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease.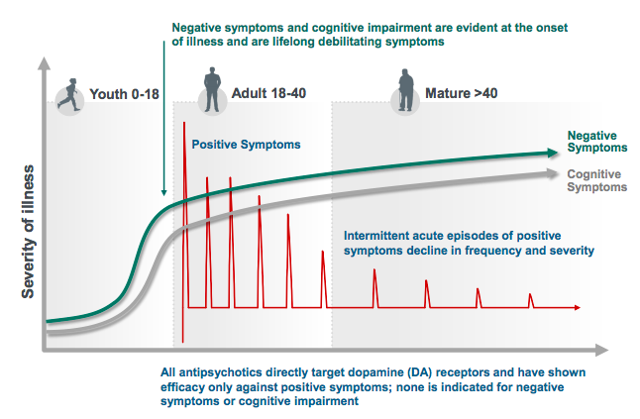 People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.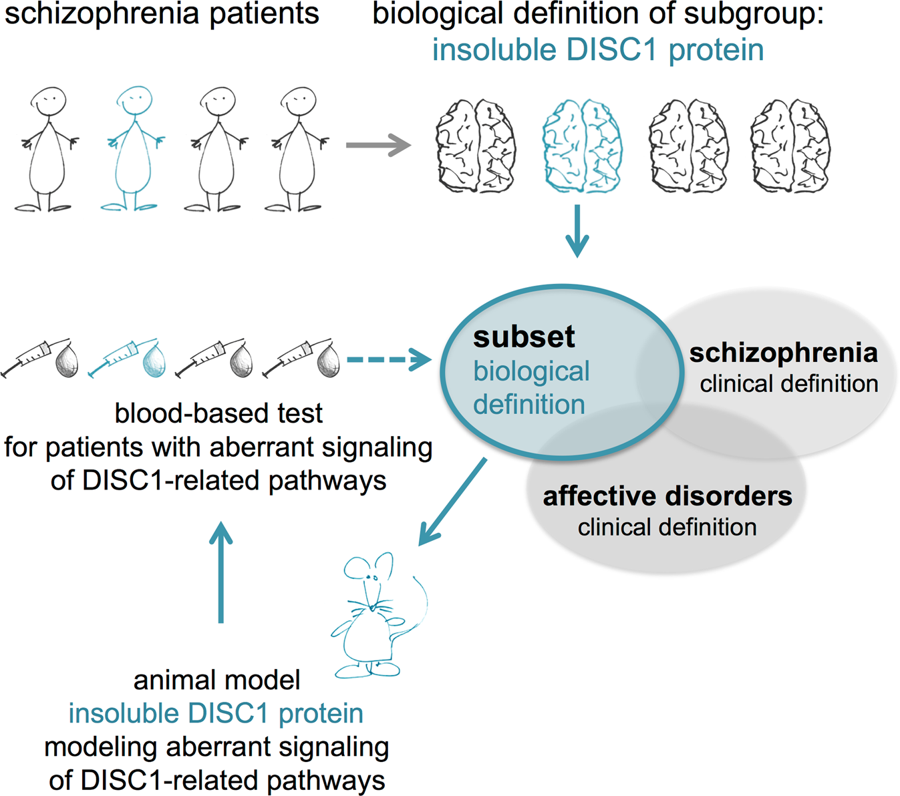
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).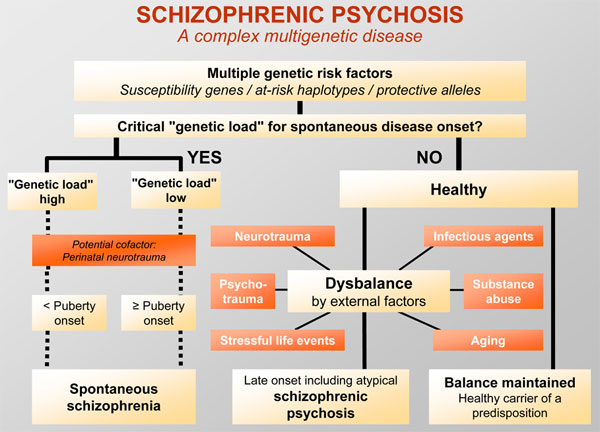 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.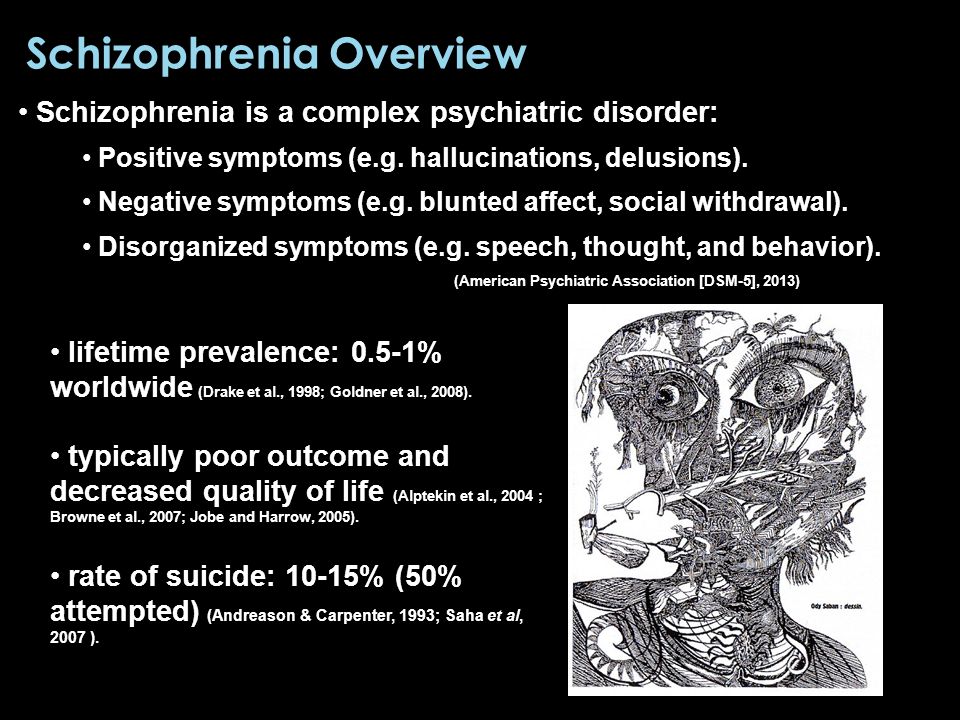 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.