Lithium vs. depakote
Efficacy of divalproex vs lithium and placebo in the treatment of mania. The Depakote Mania Study Group
Clinical Trial
. 1994 Mar 23-30;271(12):918-24.
C L Bowden 1 , A M Brugger, A C Swann, J R Calabrese, P G Janicak, F Petty, S C Dilsaver, J M Davis, A J Rush, J G Small, et al.
Affiliations
Affiliation
- 1 Department of Psychiatry, University of Texas Health Science Center, San Antonio.
- PMID: 8120960
Clinical Trial
C L Bowden et al. JAMA. 1994 Mar 23-30.
. 1994 Mar 23-30;271(12):918-24.
Authors
C L Bowden 1
, A M Brugger, A C Swann, J R Calabrese, P G Janicak, F Petty, S C Dilsaver, J M Davis, A J Rush, J G Small, et al.
Affiliation
- 1 Department of Psychiatry, University of Texas Health Science Center, San Antonio.
- PMID: 8120960
Abstract
Objective: To compare the effectiveness of divalproex sodium with that of lithium and placebo in patients with acute mania.
Design: Randomized, double-blind, parallel-group study of treatment outcomes in patients with manic-depressive illness.
Patients: A total of 179 hospitalized, acutely manic patients meeting the Research Diagnostic Criteria for manic disorder, approximately half of whom had been nonresponsive to lithium previously, were studied at nine university-affiliated hospitals.
Interventions: After a minimum 3-day washout period, random assignment for 21 days to divalproex, lithium, or placebo in a 2:1:2 ratio. Dosage of divalproex and lithium was increased if tolerated to a target concentration of 1041 mumol/L (150 micrograms/mL) or 1.5 mmol/L (conventionally expressed as milliequivalents per liter), respectively.
Main outcome measures: Primary outcome measures were changes in the Mania Rating scale derived from the Schedule for Affective Disorders and Schizophrenia.
Results: Intent-to-treat analysis for efficacy was based on data from 68, 35, and 73 patients in the divalproex, lithium, and placebo groups, respectively. Groups were initially comparable except that all eight patients with four or more manic episodes in the previous year were in the divalproex group.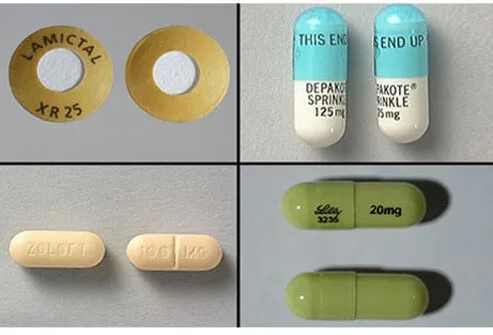 In 30%, 33%, and 51% of the above groups, treatment was prematurely terminated due to lack of efficacy, with fewer premature terminations from divalproex than placebo (P = .017). The proportions of patients improving at least 50% were higher for divalproex and lithium groups than for the placebo group: 48% for divalproex (P = .004) and 49% for lithium (P = .025) vs 25% for placebo. Divalproex was as effective in rapid-cycling manic patients as in other patients.
In 30%, 33%, and 51% of the above groups, treatment was prematurely terminated due to lack of efficacy, with fewer premature terminations from divalproex than placebo (P = .017). The proportions of patients improving at least 50% were higher for divalproex and lithium groups than for the placebo group: 48% for divalproex (P = .004) and 49% for lithium (P = .025) vs 25% for placebo. Divalproex was as effective in rapid-cycling manic patients as in other patients.
Conclusions: Both divalproex and lithium were significantly more effective than placebo in reducing the symptoms of acute mania. The efficacy of divalproex appears to be independent of prior responsiveness to lithium.
Similar articles
-
Combination of a mood stabilizer with risperidone or haloperidol for treatment of acute mania: a double-blind, placebo-controlled comparison of efficacy and safety.

Sachs GS, Grossman F, Ghaemi SN, Okamoto A, Bowden CL. Sachs GS, et al. Am J Psychiatry. 2002 Jul;159(7):1146-54. doi: 10.1176/appi.ajp.159.7.1146. Am J Psychiatry. 2002. PMID: 12091192 Clinical Trial.
-
Relationship of mania symptomatology to maintenance treatment response with divalproex, lithium, or placebo.
Bowden CL, Collins MA, McElroy SL, Calabrese JR, Swann AC, Weisler RH, Wozniak PJ. Bowden CL, et al. Neuropsychopharmacology. 2005 Oct;30(10):1932-9. doi: 10.1038/sj.npp.1300788. Neuropsychopharmacology. 2005. PMID: 15956987 Clinical Trial.
-
A randomized, placebo-controlled, multicenter study of divalproex sodium extended-release in the acute treatment of mania.
Hirschfeld RM, Bowden CL, Vigna NV, Wozniak P, Collins M.
 Hirschfeld RM, et al. J Clin Psychiatry. 2010 Apr;71(4):426-32. doi: 10.4088/JCP.08m04960yel. Epub 2010 Mar 9. J Clin Psychiatry. 2010. PMID: 20361904 Clinical Trial.
Hirschfeld RM, et al. J Clin Psychiatry. 2010 Apr;71(4):426-32. doi: 10.4088/JCP.08m04960yel. Epub 2010 Mar 9. J Clin Psychiatry. 2010. PMID: 20361904 Clinical Trial. -
Rationale for using lithium in combination with other mood stabilizers in the management of bipolar disorder.
Goodwin FK. Goodwin FK. J Clin Psychiatry. 2003;64 Suppl 5:18-24. J Clin Psychiatry. 2003. PMID: 12720480 Review.
-
Divalproex sodium versus placebo in the treatment of acute bipolar depression: a systematic review and meta-analysis.
Bond DJ, Lam RW, Yatham LN. Bond DJ, et al. J Affect Disord. 2010 Aug;124(3):228-34. doi: 10.1016/j.jad.2009.11.008. Epub 2009 Dec 30. J Affect Disord. 2010. PMID: 20044142 Review.
See all similar articles
Publication types
MeSH terms
Substances
Valproic Acid: Overused in Bipolar Disorder?
David N. Osser, MD
Psychiatric Times, Vol 37, Issue 7, Volume 37, Issue 7
Valproate/divalproex appears to be considerably overused in the US; the use of lithium, second-generation antipsychotics, and carbamazepine should be more prominent in treatment decisions for patients with bipolar mania.
BIPOLAR UPDATE
Valproate/divalproex appears to be considerably overused in the US; the use of lithium, second-generation antipsychotics, and carbamazepine should be more prominent in treatment decisions for patients with bipolar mania.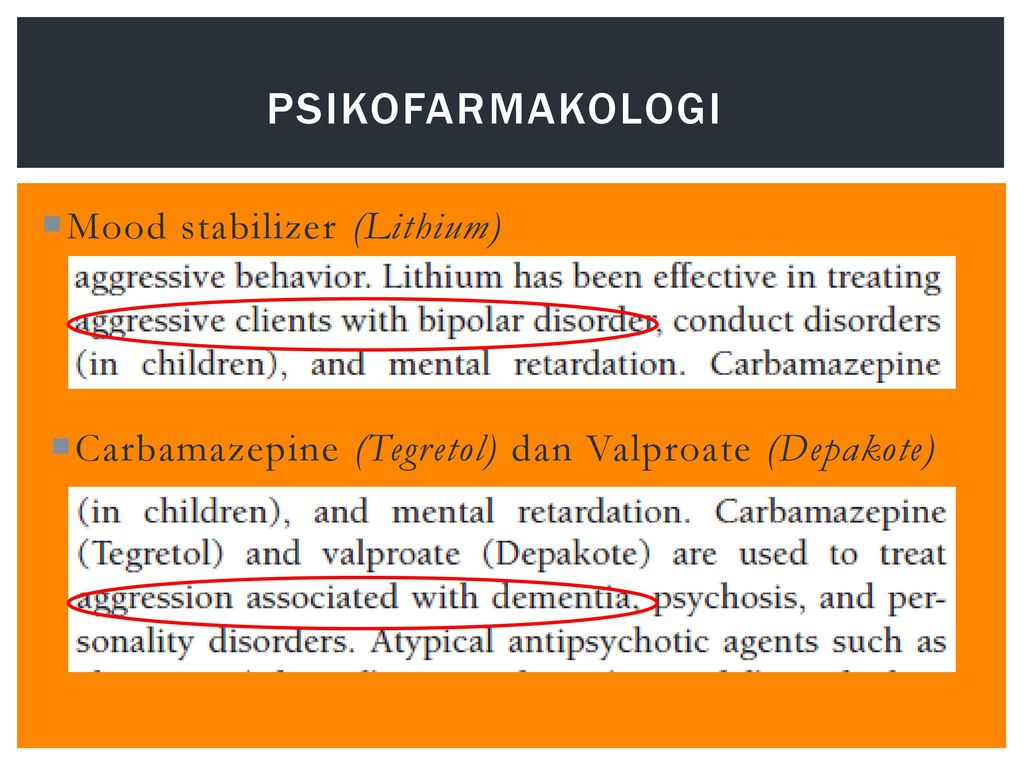
Valproate/divalproex was approved by the FDA for use in bipolar mania with the publication of a major study in 1994 that showed efficacy. It was heavily marketed and entered the mainstream practice in the US. It has been used less in Europe and even less in Japan where carbamazepine is more popular as an alternative to lithium. In the 1970s, Japanese researcher Teruo Okuma, MD, PhD, was the first to demonstrate the effect of carbamazepine in mania.
As there have been more studies, the evidence base for the efficacy of this product has become less and less impressive. In the last 2 published placebo-controlled trials of divalproex in acute mania (1 in adults, 1 in adolescents and young adults), there were no differences from placebo; and, in the study published just before those, the effects were statistically significant but quite small.1 Meta-analyses of controlled studies of medications for acute mania find it to have a smaller effect size than lithium, carbamazepine, and antipsychotics. 2
2
Maintenance trials have not shown efficacy, and the medication does not have FDA approval as a maintenance treatment for bipolar disorder. Its use for that purpose, although common, is off-label. Valproate/divalproex is also not approved for treatment of acute bipolar depression nor for prevention of depressive episodes. However, there are a few small studies that suggest that it could work for bipolar depression; larger studies are needed.3
One group of patients with bipolar disorder that seem to fare better on valproate includes those with acute mixed mania (ie, meeting full criteria for mania but having 3 or more symptoms of depression concomitantly). Valproate may be preferred over lithium for such patients.1
Clinicians often choose valproate because of a perception that it has a milder adverse effect profile than other bipolar medications. However, head-to-head studies indicate that 1 very important adverse effect—weight gain—is greater with valproate than with lithium, olanzapine, and quetiapine. 1 The risk of suicidal behaviors is twice as high on anticonvulsants such as valproate compared with controls, whereas substantial evidence finds reduced risk of suicidality on lithium. Liver dysfunction and, less commonly, pancreatitis, thrombocytopenia, and polycystic ovaries are other significant adverse effect issues with valproate. It has the most teratogenicity of any medication used in bipolar disorder and has been declared by experts to be a last resort medication for any woman of child-bearing potential.2
1 The risk of suicidal behaviors is twice as high on anticonvulsants such as valproate compared with controls, whereas substantial evidence finds reduced risk of suicidality on lithium. Liver dysfunction and, less commonly, pancreatitis, thrombocytopenia, and polycystic ovaries are other significant adverse effect issues with valproate. It has the most teratogenicity of any medication used in bipolar disorder and has been declared by experts to be a last resort medication for any woman of child-bearing potential.2
In conclusion, valproate/divalproex appears to be considerably overused in the US. Clinicians should think of lithium, second-generation antipsychotics, and carbamazepine more prominently in selecting medication for patients with bipolar mania. Patients should be informed of the evidence-base for efficacy and FDA approval status before being prescribed valproate for acute illness and especially for maintenance usage.
Dr Osser is Associate Professor of Psychiatry, Harvard Medical School, and Consulting Psychiatrist, US Department of Veterans Affairs, National Telemental Health Center, Bipolar Disorders Telehealth Program, Brockton, MA.
This article was posted ahead of print on June 16, 2020, under the title "Valproic Acid: Its Role in Bipolar Disorder," and has since been updated. -Ed
References
1. Mohammad O, Osser DN. The psychopharmacology algorithm project at the Harvard South Shore Program: an algorithm for acute mania. Harvard Rev Psychiatry. 2014;22:274-294.
2. Cipriani A, Barbui C Salanti G, et al. Comparative efficacy and acceptability of antimanic drugs in acute mania: a multiple-treatments meta-analysis. Lancet. 2011;378:1306-1315.
3. Osser DN, Wang D. The psychopharmacology algorithm project at the Harvard South Shore Program: an update on bipolar depression. Bipolar Disord. 2019; DOI: 10.1111/bdi.12860.
4. Balon R, Riba M. Should women of childbearing potential be prescribed valproate? A call to action. J Clin Psychiatry. 2016:77:525-526.
5. Sher J, Frank JW, Doi L, de Caestecker L. Failures in reproductive health policy: overcoming the consequences and causes of inaction. J Pub Health. 2019;41:e209-e215.
J Pub Health. 2019;41:e209-e215.
Download Issue: Vol 37, Issue 7
Treatment of Bipolar Disorder - Bipolar.su
With the right treatment, most patients with bipolar disorder - even in its most severe forms - can stabilize mood swings and other symptoms of the disease. Because bipolar disorder is relapsing, preventive treatment is not only indicated but strongly recommended. Treatment that combines medication and psychotherapy is optimal to keep the disease under control.
In most cases, bipolar disorder is controlled much more effectively if the patient does not interrupt the course of treatment, but continues to follow it. But even in these cases, episodes of mood swings are quite likely. In such cases, you must definitely notify the attending physician. A timely change in the course of treatment by a doctor can prevent a full-blown episode.
Treatment will be more effective if you openly discuss all doubts and proposed treatment options with your doctor.
In addition, if the patient himself and his relatives fill out a daily schedule of symptoms of mood, medication, sleep patterns, events of the day, then they begin to better understand the disease. Such graphs also help the attending physician to more effectively monitor the progress of the disease and treatment.
Medications
Medications for bipolar disorder are prescribed by registered psychiatrists-Doctors of Medicine (MD), specialists in the diagnosis and treatment of mental illness. Although a therapist can also prescribe medication, it is highly recommended that people with bipolar disorder be seen and treated by a psychiatrist.
So-called "mood stabilizers" are usually prescribed for bipolar disorder. There are several types of them. Usually people with bipolar disorder continue to take mood stabilizers for a long period of time (years). Other drugs are added as needed, usually for a shorter period of time, to relieve episodes of mania or depression that can occur intermittently, even with mood stabilizers.
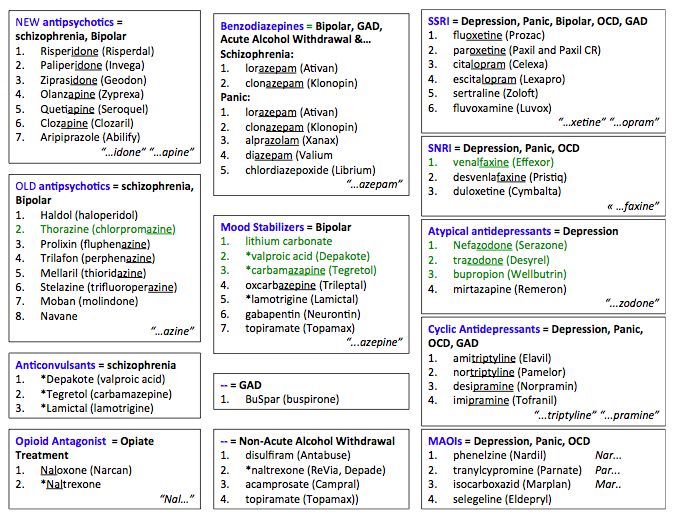
Lithium is the first mood-stabilizing drug approved by the US Food and Drug Administration (FDA) for the treatment of mania. This medicine is effective in controlling mania or preventing recurrence of both manic and depressive episodes.
Anticonvulsants such as valproate (Depakote®) or carbamazepine (Tegretol®) also have a mood-stabilizing effect and can be used in particularly difficult to treat cases of bipolar disorder. The FDA approved the use of valproate for the treatment of mania at 19
New anticonvulsants such as lamotrigine (Lamictal®), gabapentin (Neurontin®), and topiramate (Topamax®) are under study to determine how well they work to stabilize mood cycles
To achieve maximum effect, several anticonvulsants can be prescribed at once or they can be used in combination with lithium.
Children and adolescents with bipolar disorder are usually treated with lithium, but valproate and carbamazepine are also used.![]() Scientists are evaluating the safety and effectiveness of these and other psychotropic drugs in children and adolescents. Studies have shown that valproate can lead to hormonal changes in adolescent girls and to polycystic ovary syndrome in young women who start taking this drug before the age of 20 years. .
Scientists are evaluating the safety and effectiveness of these and other psychotropic drugs in children and adolescents. Studies have shown that valproate can lead to hormonal changes in adolescent girls and to polycystic ovary syndrome in young women who start taking this drug before the age of 20 years. .
Patients with bipolar disorder who want to become pregnant or are already pregnant face a difficult choice because mood stabilizers can have negative effects on the fetus or on the breastfed infant. pros and cons of various treatments. Currently, new drugs are being tested that significantly reduce the risk during pregnancy or breastfeeding.
Studies have shown that patients with bipolar disorder treated with antidepressants are at risk of developing mania, hypomania, or a rapidly circulating form of the disease.
Mood stabilizing drugs, either in combination with antidepressants or on their own, are usually required to protect patients with bipolar disorder from such consequences. Currently, lithium and valproate are the most commonly used mood-stabilizing drugs. However, trials are ongoing to evaluate the effectiveness of new drugs to stabilize mood.
Currently, lithium and valproate are the most commonly used mood-stabilizing drugs. However, trials are ongoing to evaluate the effectiveness of new drugs to stabilize mood.
Atypical antipsychotics including clozapine (Clozaril®), olanzapine (Zyprexa®), risperidone (Rispendal®), quetipine (Seroquel®), and ziprasidone (Geodon®) are being studied for use in the treatment of bipolar disorder. There is evidence that clozapine may help patients who do not respond to lithium or anticonvulsant therapy.
Other studies have confirmed that olanzapine is effective in acute mania and has recently been approved by the FDA for this use.17 Olanzapine is also helpful in the treatment of psychotic depression.18
Aripiprazole (Abilify®) is another atypical antipsychotic used to treat symptoms of schizophrenia and manic or mixed (manic and depressive) episodes of bipolar I disorder. It is available in both tablets and liquid form. The injections are used to treat the symptoms of agitation in schizophrenia and manic or mixed episodes of bipolar I disorder.
If insomnia is a problem, high-potency benzodiazepine drugs such as clonazepam (Klonopin®) or lorazepam (Ativan®) may help. However, because these drugs are addictive, they are only prescribed for a short time. In some cases, sedatives such as zolpidem (Ambien®) are prescribed instead.
During the course of treatment for bipolar disorder, medications must be changed many times in order to achieve the most effective treatment. All drug changes and dose changes must occur as directed by the treating psychiatrist.
Be sure to tell your psychiatrist about all medications you take, including over-the-counter medicines, homeopathic remedies, vitamins, and other supplements. This is very important as some medications and supplements are incompatible and may cause adverse reactions.
To avoid a relapse or a new episode, the treatment plan must be strictly adhered to. Talk to your doctor about any questions you have about medications.
Thyroid function
Thyroid dysfunction is common in patients with bipolar disorder. Elevated or decreased levels of thyroid hormones in themselves can have an impact on changes in mood and energy levels. Therefore, it is very important that the thyroid gland indicators are under the constant supervision of the attending physician.
Elevated or decreased levels of thyroid hormones in themselves can have an impact on changes in mood and energy levels. Therefore, it is very important that the thyroid gland indicators are under the constant supervision of the attending physician.
The rapidly circulating form of bipolar disorder is often associated with thyroid disease. In such cases, along with medications for bipolar disorder, it is necessary to take thyroid medications. It should also be borne in mind that in some patients, lithium can cause a decrease in thyroid activity. In this case, it is necessary to introduce medications into the course of treatment to regulate the function of the thyroid gland.
Side effects of drugs
Always talk to your psychiatrist and/or pharmacist about possible side effects before starting new medicines. Depending on the drug, side effects may include weight gain, nausea, tremors, decreased sexual activity or ability, anxiety, hair loss, difficulty moving, and dry mouth. Be sure to tell your doctor about any side effects that occur while taking this or that medication. To remove or reduce side effects, the doctor may change the dosage of the drug or change it to another. Do not change medications or stop taking them without consulting a psychiatrist.
Be sure to tell your doctor about any side effects that occur while taking this or that medication. To remove or reduce side effects, the doctor may change the dosage of the drug or change it to another. Do not change medications or stop taking them without consulting a psychiatrist.
Psychosocial methods
Psychosocial methods, including certain forms of psychotherapy (or "talk" therapy), are recommended along with medication. Such methods help patients with bipolar disorder and their families to understand the specifics of the disease and obtain the necessary information. The results of studies have shown that psychosocial therapy helps to stabilize mood, reduce the number of hospitalizations and improve life in various areas of human activity.
This therapy is usually administered by licensed psychologists and social workers, coordinating with the attending psychiatrist and jointly monitoring the progress of the patient's health. The number of sessions, their frequency and duration depend on the individual needs of each patient.
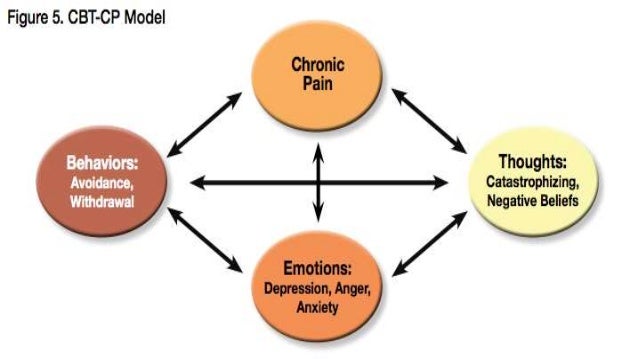
Psychosocial interventions for bipolar disorder include cognitive behavioral therapy, psychological education, family therapy, and a new approach, interpersonal and sociorhythmic therapy. Researchers at the National Institute of Mental Health (NIMH) are studying and comparing the effectiveness of these methods in combination with various drugs for the treatment of bipolar disorder:
Cognitive Behavioral Therapy helps people with bipolar disorder understand and change negative or distorted thought patterns and behaviors associated with the disorder.
Psychological education provides patients with information about the disease and its treatment methods, and helps them learn to recognize the signs of relapse, which allows them to seek help early and prevent a full-blown episode. Psychic education is also useful for family members of the patient.
Family therapy uses a strategy to reduce the level of tension in the family, which can aggravate the symptoms of the disease or provoked by them.
Interpersonal and socio-rhythmic therapy helps patients with bipolar disorder improve interpersonal relationships and organize their daily routine. A regular schedule and regular sleep patterns help prevent manic episodes.
As with drug treatment, adherence to the prescribed course of treatment is essential to achieve successful results in psychosocial therapy.
Other treatments
Electroconvulsive therapy (ECT/ECT) is used when medications, psychosocial therapies, or a combination of both do not work or are too slow to treat serious symptoms such as psychosis or suicidality. The use of ECT may also help during acute episodes when the patient's physical condition (including pregnancy) does not allow the use of drugs. ECT is highly effective in the treatment of severe depression, manic and/or mixed episodes. The possibility of long-term memory problems as a result of ECT, which until recently was a serious cause for concern, is now significantly reduced thanks to the latest methods of ECT.
However, the pros and cons of using ECT and other alternative treatments should be discussed in advance with the patient and, if necessary, with family members or friends.
Herbal medicines and natural supplements such as St. John's wort (Hypericum perforatum) are not yet well understood and there is little information available about their impact on bipolar disorder. Since FDA regulations do not apply to such products, different manufacturers of these supplements use different amounts of active ingredients. Before you start taking herbal medicines or natural supplements, you should consult with your doctor. There is evidence that St. John's wort can reduce the effectiveness of certain drugs (see: www.nimh.nih.gov/events/stjohnwort.cfm) by leaving the OMH site. 20 In addition, like prescription antidepressants, St. John's wort can induce mania in some patients with bipolar disorder, especially when the patient is not taking mood stabilizers.
Studies are being conducted on the effectiveness of using omega-3 fatty acids (found in fish oil) in the treatment of bipolar disorder in combination with conventional medicines or alone.
A chronic disease with very effective treatment
Although episodes of mania and depression tend to come and go, it must always be remembered that bipolar disorder is a chronic disease that currently has no cure. The only way to keep this disease under control is to take medicine constantly, even when you feel well. Only in this case it is possible to reduce the chance of relapses and deterioration.
Comorbidities
Alcoholism and drug addiction are very common among patients with bipolar disorder. Studies have shown that there are a number of reasons for this, including self-medication, mood swings from alcohol or drug abuse, and risk factors that affect both the development of bipolar disorder and drug addiction.
Treatment for alcoholism or drug addiction is an important part of the overall course of treatment.
Anxiety disorders such as post-traumatic stress disorder or obsessive-compulsive disorder (OCD) are also common in bipolar disorder.
Comorbid anxiety disorders can sometimes be managed with the same tools as bipolar disorder, but in some cases special treatment is required.
Help for people with bipolar disorder and their families
People with bipolar disorder should be managed by an experienced psychiatrist who specializes in diagnosing and treating the condition. Psychologists, mental health social workers, and psychiatric nurses help provide various aspects of treatment and care for patients and their families.
Help is available at the following locations:
- University or medical school treatment programs
- Hospital psychiatric departments
- Private psychiatric offices and clinics
- Community health care organizations (HMOs) 9010 or HMOs 9010 Pediatric doctors
- Community mental health centers
- People with bipolar disorder may need help to get help
People with bipolar disorder often do not realize how sick they are, or they see the cause of their illness not in a mental disorder, but in something else.
People with bipolar disorder may need encouragement and support from family and friends to seek medical help. The therapist can play an important role in insisting on consultation with a psychiatrist.
It is sometimes necessary to have a family member or friend accompany a person with bipolar disorder to medical appointments and treatment.
Sometimes a patient who is in the stage of an acute attack needs to be hospitalized for his/her own safety and to ensure the necessary treatment. In some cases, it is necessary to hospitalize the patient against his/her will and without consent.
It is necessary to constantly support and encourage the patient, after the start of treatment, because in some cases it may take quite a long time to find the right course of treatment.
In some cases, patients with bipolar disorder in remission may agree on a specific course of action in the event of a future manic or depressive relapse.
Like other serious illnesses, bipolar disorder is hard on spouses, family members, friends, and employers.
It is not uncommon for family members of a person with bipolar disorder to deal with serious behavioral problems, such as spending money recklessly during manic episodes or withdrawing during depression, and the long-term consequences of such behavior.
Many people with bipolar disorder are helped by support groups supported by organizations such as the National Depressive and Manic-Depressive Research Association (NDMDA), the National Mental Health Alliance (NAMI), and the National Mental Health Association (NMHA). These support groups also help the families and friends of people with bipolar disorder. You can find contact information for these organizations in the Useful Information section of our brochure.
Source: http://www.omh.ny.gov/omhweb/russian/booklets/bipolar.html
Mental health care, drugs | PsyQ.ru Psychological Center
Psychiatric drugs
Psychiatric drugs first appeared in the early 1950s in the form of the antipsychotic drug chlorpromazine. Subsequently, a huge number of other drugs appeared. These drugs have changed the lives of people with mental disorders for the better.
Subsequently, a huge number of other drugs appeared. These drugs have changed the lives of people with mental disorders for the better.
Psychotropic drugs can accompany psychotherapy treatment and make it more effective. For example, a patient who is chronically depressed may experience communication difficulties during psychotherapy and counseling, and proper drug treatment will help relieve negative symptoms and the patient will be able to adequately respond to therapy. For many patients, a combination of psychotherapy and medication can be an effective treatment.
When combined with medication, psychotherapy can relieve symptoms of many disorders such as psychosis, depression, anxiety, obsessive-compulsive disorder, and panic disorder.
Just as aspirin reduces fever without treating the infection that causes it, psychotropic drugs work by relieving symptoms. Psychotropic medications do not cure mental illness, but in many cases, they can help a person function despite some ongoing mental anguish and psychological problems. For example, narcotic drugs such as chlorpromazine can "turn off" the "inner voice" that some people with mental disorders hear and help them see reality more clearly. Antidepressants can help relieve the gloomy mood in severe depression.
For example, narcotic drugs such as chlorpromazine can "turn off" the "inner voice" that some people with mental disorders hear and help them see reality more clearly. Antidepressants can help relieve the gloomy mood in severe depression.
How long a patient should take medication depends on the individual. Many depressed and anxious people will take medication for a period, perhaps a few months, and go off medication afterwards. People with conditions such as schizophrenia and bipolar disorder (also known as manic-depressive disorder), or those for whom depression or anxiety is chronic or recurrent, may take medication indefinitely.
Like any drug, psychotropic drugs do not give the same effect in each case. There is a difference in the tolerability of one or other drugs, their effectiveness, dosage, the presence of side effects in some patients and the absence of others. Age, sex, weight, body chemistry, physical diseases and their treatment, diet, and habits such as smoking are just a few of the factors that can affect the effect of a remedy.
Antipsychotics
People with psychotic disorders are out of touch with reality. People with psychosis may hear "voices" and may have intrusive, strange, and illogical ideas (eg, that others may be hearing their thoughts, or trying to harm them, or that they are the president or some other famous person). They may become agitated or angry for no apparent reason, sleeping during the day and awake at night. The person may not pay attention to their appearance, not bathe or change their clothes, they may have difficulty speaking or saying things that do not make sense. Such people often do not know that they are sick.
This type of behavior is a symptom of a psychotic illness such as schizophrenia. Antipsychotic medications work for these symptoms. These drugs cannot "cure" the disease, but they can relieve most symptoms or make them milder. In some cases, they can shorten the duration of an episode of illness.
There are a number of antipsychotic (neuroleptic) medications available. These drugs affect the neurotransmitters that form connections between nerve cells.
These drugs affect the neurotransmitters that form connections between nerve cells.
The first antipsychotic drugs were invented in the 1950s. Antipsychotic drugs have helped many patients with psychosis lead more normal and fulfilling lives by relieving symptoms such as hallucinations, both visual and auditory, and eliminating paranoid thoughts. However, in the beginning, antipsychotic medications often had serious side effects such as muscle stiffness, tremors, and abnormal movements.
In the 1990s, a number of new drugs for the treatment of schizophrenia, called "atypical antipsychotics", were developed. These days, they are prescribed as a course of treatment in the first place, since they have fewer side effects. The first atypical antipsychotic drug, clozapine (Clozaril), was invented in the United States in 1990 year. In clinical trials, treatment with this drug has proven to be more effective than conventional or "typical" antipsychotic medications. However, because of the potential side effect of the blood disorder agranulocytosis (loss of white blood cells that fight infection), patients taking clozapine need a blood test every 1 or 2 weeks. Clozapine, however, is still the mainstay of treatment for resistant patients with schizophrenia.
Clozapine, however, is still the mainstay of treatment for resistant patients with schizophrenia.
Several other atypical antipsychotics have been developed since clozapine. The first of these is risperidone (Risperdal), followed by olanzapine (Zyprexa), quetiapine (Seroquel), and Ziprasidone (Geodon). Each of them has its own side effects, but in general, these drugs are better tolerated than early narcotic drugs.
Preparations for the treatment of bipolar disorder
Bipolar disorder is characterized by a spontaneous change in mood, from extremely elated (mania) to downright depressed (depression). Episodes may be predominantly manic or depressive, with normal mood between episodes. Mood swings can follow each other very often, within a few days, or they can recur in intervals of a month to several years. "Highs" and "lows" can vary in intensity and severity and co-exist in "mixed" episodes.
Lithium
Lithium treatment is most commonly used to treat bipolar disorder. Lithium smoothes mood swings in both directions from mania to depression and vice versa, it is used not only for manic states or flare-ups of the disease, but also as an ongoing supportive form of therapy for bipolar disorder.
Lithium smoothes mood swings in both directions from mania to depression and vice versa, it is used not only for manic states or flare-ups of the disease, but also as an ongoing supportive form of therapy for bipolar disorder.
Although lithium relieves symptoms in about 5 to 14 days, it may take several weeks to several months before the patient's condition is fully controlled.
Antidepressants may be added to lithium during the depressive phase of bipolar disorder. If lithium or another mood stabilizer is not taken, antidepressants can induce mania in people with bipolar disorder.
Anticonvulsants
Some people with manic symptoms would prefer to avoid lithium and take anticonvulsant medicines that are commonly used to treat seizures. The use of the anticonvulsant drug valproic acid (Depakote, divalproex sodium) is the main alternative therapy for bipolar disorder. It is just as effective as lithium.
Other anticonvulsants used for bipolar disorder:
carbamazepine (Tegretol), lamotrigine (Lamictal), gabapentin (Neurontin) and topiramate (Topamaxom). Anticonvulsants have been shown to be more effective in relieving acute mania than in the long-term treatment of bipolar disorder.
Anticonvulsants have been shown to be more effective in relieving acute mania than in the long-term treatment of bipolar disorder.
Antidepressants
Depression to be treated with medication must be sufficiently severe . This is a condition that lasts for 2 weeks or more and manifests itself in a violation of a person's ability to solve everyday tasks and enjoy life. There is an opinion that depression is associated with improper functioning of the brain. The interaction between genetic predisposition and life history is decisive in the development of depressive states in a person. Episodes of depression can be triggered by stress, difficult life events, side effects of medications, or even viral infections that can affect the brain.
Depression can vary in intensity, from mild to severe. Depression can coexist with other non-mental illnesses such as cancer, heart disease, stroke, Parkinson's disease, Alzheimer's disease, and diabetes.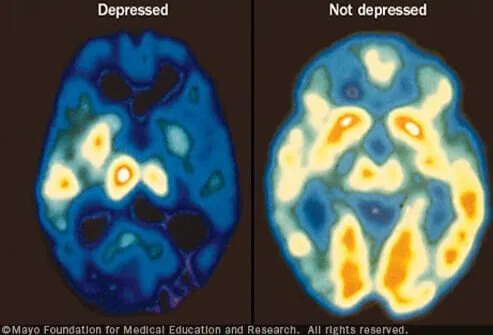 In such cases, depression is often overlooked and untreated. If depression is diagnosed and treated, a person's quality of life can be greatly improved.
In such cases, depression is often overlooked and untreated. If depression is diagnosed and treated, a person's quality of life can be greatly improved.
Antidepressants are most commonly used for severe depression, but they may also be helpful for some forms of mild depression. Antidepressants are not a cure, they only relieve the symptoms of depression and help depressed people feel the way they did before they became depressed.
Early Antidepressants
From the 1960s to the 1980s, tricyclic antidepressants (named for their chemical structure) were the first drugs to treat severe depression. Most of these drugs work through two chemical messengers, norepinephrine and serotonin. Although tricyclic antidepressants are effective in the treatment of depression, as well as newer antidepressants, they tend to have more pronounced side effects, so today tricyclic antidepressants such as imipramine, amitriptyline, nortriptyline and desipramine are used only after the second or third visit for help.
Other antidepressants that appeared during this period were monoamine oxidase inhibitors (MAOIs). MAOIs are effective in treating some people with severe depression who do not respond to other antidepressants. They are also effective in treating panic disorder and bipolar depression.
MAOIs used to treat depression: phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan).
Many new antidepressants have been developed in the last ten years, they work just like the old ones, but have fewer side effects. Some of these drugs primarily target one neurotransmitter, serotonin, and are called serotonin reuptake inhibitors (SSRIs). These include fluoxetine (Prozac), sertraline (Zoloft), fluvoxamine (Luvox), paroxetine (Paxil), and citalopram (Celexa).
In the late 1990s, new drugs are invented that, like tricyclics, affect both norepinephrine and serotonin, but have fewer side effects.
These include: venlafaxine (Effexor) and nefazadone (Serzone).
There are also new drugs that are not chemically related to antidepressants, in fact they are sedatives.
Among them: mirtazepine (Remeron) and stronger bupropion (SR).
All questions about the use of any antidepressant, or problems that may be associated with treatment, should be discussed with a doctor and / or psychiatrist.
Anxiety medications
Everyone experiences anxiety at some point or another, such as shaky speech or sweaty palms during an interview are common symptoms.
There are other symptoms such as irritability, restlessness, tremors, fear, palpitations, abdominal pain, nausea, dizziness and trouble breathing.
Anxiety, usually manageable and mild, can sometimes lead to serious problems. A high level or prolonged state of anxiety can interfere with daily activities and make it difficult or impossible. People with generalized anxiety disorder or other anxiety disorders such as panic, phobias, obsessive-compulsive disorder, or post-traumatic stress disorder (PTSD) have severe limitations in life and work.
Antidepressants are also widely used to treat anxiety disorders. Most broad spectrum antidepressants are effective in treating anxiety disorders and depression.
Most broad spectrum antidepressants are effective in treating anxiety disorders and depression.
The first drug specifically designed for the treatment of obsessive-compulsive disorder was the tricyclic antidepressant clomipramine (Anafranil). Fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft) are also approved to treat people with obsessive-compulsive disorder. Paroxetine was also effective in treating patients with social phobia (social phobia), and panic disorders.
Anxiety medications include benzodiazepines, which can relieve symptoms in a short time. They have relatively few side effects: drowsiness and loss of coordination are the most common.
Benzodiazepines commonly used include clonazepam (Klonopin), alprazolam (Xanax), diazepam (Valium), and lorazepam (Ativan). The only drug developed specifically for the treatment of anxiety disorders other than benzodiazepines is buspirone (BuSpar). Unlike benzodiazepines, buspirone must be taken consecutively for at least 2 weeks to have a beneficial effect.