What is a psychiatric hospital
Psychiatric hospitals | Your Health in Mind
Private psychiatric hospitals admit a really broad range of people.
They range from adolescents, through to adults through to elderly people, with a whole range of mental health problems.
Common problems like depression and anxiety, drug and alcohol problems.
Even less common things like schizophrenia.
One of the reasons people come into hospital is things like suicidal ideas where there's a real risk and danger.
And clearly in hospital we can observe people and support them during those difficult times.
The treatment of a person is tailored to what they need and will usually involve a close discussion between them and their psychiatrist.
Almost all patients will be involved in therapy, both group and individual.
There'll be other group activities involving things like art therapy, yoga or exercise - all of which we know can be beneficial to the treatment of mental health problems.
There's also some treatments like ECT that we utilise for some of the most serious conditions. They also have lots of opportunities to have one-on-one discussions with their nurse.
In hospital you will be greeted at a reception desk.
They'll help you get to the ward and find your way around.
Usually a nurse will greet you, take some admission details and show you around the place - so you know where to go for various things.
Your psychiatrist is responsible for leading your care. That means your psychiatrist will meet with you most days, review how things are going and what you need to work on next.
Your psychiatrist will also meet regularly with the rest of the team. That means nurses, psychologists, occupational therapists or whoever else in hospital is there to help you.
The average length of stay in a psychiatric hospital now, is about two to three weeks. Many people worry about - what's it going to be like with the other people in hospital.
For many people, having a mental health problem can be quite isolating. Remember that these people are more likely to understand what it's like than most people you meet every day.
People get better in hospital.
They usually need ongoing support afterwards, and your psychiatrist is likely to continue to be part of that care team.
How long will I be in hospital?
The length of time you’ll be in hospital really depends on why you’re there, the treatments you need and how you’re responding.
Some people only stay a day or two. Others may stay for 2–3 weeks or longer.
People who haven’t been in a psychiatric ward before sometimes worry they may never be able to leave. That never happens these days.
What happens after I leave hospital?
Being in hospital is just one part of your recovery.
Before and after you’re in hospital you might have home visits, telephone or internet case-management and appointments for psychological and medical treatment.
A social worker can help if you're worried about accommodation after you leave hospital.
Can I be treated without my consent?
Sometimes a mental illness can become so severe that the person with the illness may not even realise they are unwell.
If someone is so sick they don’t understand they need treatment, and if not having the treatment would put them (or others) in danger, the law allows that person to be treated involuntarily.
This means they can be kept in hospital (if necessary) and treated, even though they say they don’t agree to it.
To make sure this only happens when it’s absolutely necessary, the law requires that doctors present a case for this in front of a tribunal (or, in New Zealand, a judge).
The law also protects your rights. You have the right to legal representation and in some cases this is provided for free. (In New Zealand all cases under mental health compulsory treatment orders receive free legal representation.)
You have the right to be seen regularly by your psychiatrist and to have contact with family/whānau.
Each Australian state and territory and New Zealand have their own mental health acts, which set out these rights and the other rules that doctors must obey.
Seclusion and restraint
Seclusion or restraint may be used when a person is acting violently and the person, other patients or staff members are at risk.
Seclusion is where a person is kept alone in a room or area where they are unable to leave.
Restraint is where a person is physically restricted from moving around, for example by someone holding them, through medication, or by being strapped down.
Seclusion and restraint are a last resort where all other options to keep people safe have been tried or considered. Both should be very rare.
The RANZCP’s position is that the use of seclusion and restraint should be reduced and where possible removed entirely.
RANZCP Position statement on seclusion and restraint [PDF; 305 KB]
Your rights in hospital
Tell hospital staff if you are uncomfortable with any part of your treatment or are unsure of anything.
While in hospital, you have the right to:
- privacy
- safety
- respect for your cultural identity
- ask questions about your treatments and medications and their side effects
- know your diagnosis, and disagree with it
- get a second opinion (this could be at your own cost)
- refuse treatment (though if you are under an involuntary order your doctors may end up insisting on some medications)
- make a complaint
- have a family/whānau member, friend, family consultant or anyone you choose to help you ask questions.
Help for families/whānau
If you have a family member or friend who is in hospital, you can be involved in the person’s treatment, with their permission.
Most hospitals will have workers whose main job is to help families learn about the person’s illness, find community supports and work out how to best use the health-care system.
What Is an Acute Psychiatric Hospital?
Psychiatric hospitals are a place for people in crisis who may need safety monitoring and assessment as well as therapy and medication management. As being in the hospital interrupts daily life and is expensive, it should only be used when you need 24-hour care to keep you safe.
As being in the hospital interrupts daily life and is expensive, it should only be used when you need 24-hour care to keep you safe.
For more information, please call us at 512-324-2039 or contact us online.
How will I get there and what will happen when I do?
- You may be brought to the hospital or a psychiatric emergency room by a friend or family member, by an ambulance or mental health deputy, or you may be able to drive yourself to the hospital
- DO NOT drive yourself if you have been using drugs or alcohol; get a ride with a family member, friend or cab
- Some psychiatric hospitals require you to go to a psychiatric emergency department first
- When you arrive you will go through a process called “intake” in which you will meet with hospital staff such as nurses, social workers and doctors or other medical providers
- You will be asked to place your belongings in a secure place for safety reasons so you should write down important phone numbers and keep your driver’s license/ID card and insurance cards with you
- You will be asked to fill out different types of paperwork including:
- Medical history forms
- Consent for treatment forms (so the hospital can care for you)
- Release of information forms (so the hospital staff can talk to your family and friends or your doctor or therapist)
- Insurance and billing forms
- These forms can be confusing so feel free to ask questions
- If you do not need acute psychiatric hospitalization, the staff will give you information on other treatment options before you leave
What will my stay in the hospital be like?
- There will be visiting hours
- You will have access to a phone to make and receive calls
- Most hospitals will give you a code for your family and friends to use when calling and visiting to protect your privacy
- You will be included in creating your treatment plan, determining what your goals are while in the hospital and how the staff will help you meet those goals
- The psychiatrist may prescribe new medication or adjust the dosage of your current medication; medication cannot be given to you without your permission unless it is an emergency
- You will have access to therapy groups and other types of treatment as well
- Before you leave the hospital a social worker will meet with you to make a plan and additional appointments for continuing your treatment when you get home
How long does a stay in a psychiatric hospital last?
- Most hospital stays are only long enough to resolve the most urgent issues, and usually last from a few days to a few weeks
- The average psychiatric inpatient stay is three to five days
Treatment in a psychiatric hospital | SKKSPB №1
Hospitalization in a psychiatric hospital, contrary to popular stereotypes, is not always due to the fact that someone sees hallucinations or runs after people, brandishing an axe.
Placement in a psychiatric hospital indicates that the patient's mental state has deteriorated and it is impossible to help him at home. At the same time, a person can adequately perceive reality and give an account of his actions. Some forms of depression, for example, require hospital care. Sometimes a patient is admitted to the hospital to clarify his diagnosis or prescribe a more effective treatment. In any case, you should not be afraid of hospitalization. A stay in a psychiatric hospital is not much different from treatment in any other hospital.
Who makes the decision on admission to a psychiatric hospital?
It happens in different ways. For convenience, it is worth separating voluntary and involuntary hospitalization (a lot of social prejudices and fears are associated with it). First of all, consider situations where a person ends up in the hospital against their will. Indications for involuntary hospitalization are stipulated by the Russian law “On Psychiatric Care and Guarantees of the Rights of Citizens in its Provision”. The patient may be admitted to the hospital without his consent in the following cases:
The patient may be admitted to the hospital without his consent in the following cases:
- When, due to his mental condition, he can harm (himself or another person) or tries to take his own life.
- When he is helpless in front of daily household tasks (cook his own food, go to the grocery store, follow the basic rules of personal hygiene).
- When not providing mental health care will lead to even more serious health problems.
- When the decision on hospitalization is made by the court, this is the topic of a separate long conversation
Is it possible to go to a psychiatric hospital voluntarily?
Yes, if a person feels the need for inpatient care, he or she has the right to go to the hospital and ask to be hospitalized or tell the attending psychiatrist about his desire. The psychiatrist also, if he sees the need for this, suggests that his patient go to the hospital for a while, explains why this is necessary and how long the hospitalization will approximately last. But the decision on hospitalization still remains with the patient.
But the decision on hospitalization still remains with the patient.
It is important to remember that the mere fact of being admitted to a psychiatric hospital does not mean negative social consequences or restrictions on rights for the patient. Some patients refuse to apply for a sick leave during their hospitalization, as they are afraid that they will find out at work in which hospital they were treated. These fears are also unfounded. The sick leave does not indicate the diagnosis, and besides, psychiatric hospitals and narcological clinics have separate stamps for disability certificates (the profile of the institution is not indicated on the stamp).
To sum up : it is not the fact of hospitalization that matters, but the state of your mental health. If it requires inpatient treatment, then you need to discard fears and follow the doctor's recommendations.
According to the WHO, taking care of your mental health reduces your risk of developing suicidal tendencies and premature death from suicide, and improves your overall quality of life. Timely detection of mental illness in the early stages of its development makes it possible to stop or significantly slow down its progressive course. If you notice signs of disorder in yourself or your family, we urge you to seek help from a psychologist or psychiatrist in a timely manner.
Timely detection of mental illness in the early stages of its development makes it possible to stop or significantly slow down its progressive course. If you notice signs of disorder in yourself or your family, we urge you to seek help from a psychologist or psychiatrist in a timely manner.
Read our other articles
Follow and follow us on social networks
The illustration for this publication is taken from the public image library https://www.freepik.com/ and from open sources.
You can read more about the use of images from the Freepik library here
Psychiatric hospital: history, modernity and perspectives
The role of psychiatric hospitals in the overall mental health care system has been a subject of discussion since their inception. Famous psychiatrists G. Tornicroft and M. Tansella [1] divide the process of development of the system of hospital psychiatric care into three conditional historical periods: 1) the development of psychiatric hospitals; 2) denial of their necessity; 3) the balance of hospital and community-oriented (out-of-hospital) psychiatric care.
The psychiatric hospital, which initially served as a charity for the mentally ill, later began to play the role of the main clinical structure in which patients were examined, methods of their treatment were developed and implemented, and ideas about mental illness were formed.
By the beginning of the last century, a wide network of psychiatric hospitals had been created in many countries of the world, which not only provided the population with various types of psychiatric care, but also served as the basis for serious theoretical developments. Over time, psychiatric hospitals began to perform the functions of educational centers.
The development in our country and abroad of dispensary and other forms of out-of-hospital psychiatric care, the formation in Western countries of the anti-psychiatric movement, which led to the process of deinstitutionalization in psychiatry (reducing the number of hospitals and withdrawing hospitals from them into the "society"), initiated a wide wave of professional and public discussions about the justification for reducing inpatient types in the general system of psychiatric care and shifting the emphasis to out-of-hospital, community-oriented types. And although psychiatrists in most countries of the world recognize that the hospital link has been and remains an integral component of the overall system of psychiatric care and the treatment of patients in a psychiatric hospital is the main one [2-5], the discussion on this problem continues in modern psychiatry.
And although psychiatrists in most countries of the world recognize that the hospital link has been and remains an integral component of the overall system of psychiatric care and the treatment of patients in a psychiatric hospital is the main one [2-5], the discussion on this problem continues in modern psychiatry.
The assertion of the role of community-oriented psychiatry was reflected in the decline in research interest in the problems of the inpatient link. This can be evidenced by the dynamics of the number of publications devoted to topical problems of inpatient psychiatric care. As an example, the ratio of the number of publications devoted to issues of inpatient and outpatient care in the materials of congresses of psychiatrists in Russia from 1990 to 2010 can be given: 1990 (VI Congress) - 1:1.1; 2000 (XIII Congress) - 1: 1.2; 2010 (XV Congress) - 1:2.8. At the same time, the number of detailed publications covering the features of the work and way of psychiatric hospitals has always remained relatively small in psychiatry [2-4, 6-9].
This article reflects an attempt to discuss the activities of psychiatric hospitals in the aspect of the problems existing in modern psychiatry and the prospects for improving inpatient psychiatric care.
Development and current state of hospital care
Given the complex, interdisciplinary nature of the problems associated with the peculiarities of the activities of psychiatric hospitals, it is advisable to analyze and evaluate the formation of the system of inpatient psychiatric care, taking into account their scientific, clinical, organizational, social and economic aspects, based on existing historical experience .
Scientific and clinical aspect
According to A.V. Snezhnevsky [4], in psychiatry, unlike all other medical disciplines, the topic of organizing medical care in a psychiatric hospital turned out to be most connected with theoretical, therapeutic and organizational issues. Similar views are shared by other domestic psychiatrists [2, 3, 6-8, 10, 11], who noted that throughout the history of its existence, a psychiatric hospital (hospital) has remained the main base in which scientific schools were formed and theoretical developments were carried out. primary training of young doctors and advanced training of specialists working in psychiatry and testing of new methods of treatment. In turn, the development of hospital care itself was largely determined by the theoretical concepts that existed in various psychiatric schools. Differences in scientific views on the nature of mental illness, methods of their treatment, which existed among domestic and foreign psychiatrists, also formed different approaches to the arrangement of psychiatric hospitals, their way of life and way of life, and features of work. The nosological concept adopted in domestic psychiatry and the recognition of the biological nature of mental illness led to the creation in psychiatric hospitals of conditions for a comprehensive not only psychiatric, but also general somatic examination of patients and the implementation of active drug and other methods of biological treatment.
primary training of young doctors and advanced training of specialists working in psychiatry and testing of new methods of treatment. In turn, the development of hospital care itself was largely determined by the theoretical concepts that existed in various psychiatric schools. Differences in scientific views on the nature of mental illness, methods of their treatment, which existed among domestic and foreign psychiatrists, also formed different approaches to the arrangement of psychiatric hospitals, their way of life and way of life, and features of work. The nosological concept adopted in domestic psychiatry and the recognition of the biological nature of mental illness led to the creation in psychiatric hospitals of conditions for a comprehensive not only psychiatric, but also general somatic examination of patients and the implementation of active drug and other methods of biological treatment.
The introduction of neuroleptics into psychiatric practice had a great influence on the development of hospital psychiatric care and attitudes towards it. It is generally recognized that they have changed the stereotype of the course of many mental illnesses, reducing their severity and reducing the length of stay of patients in the hospital. According to the recognition of psychiatrists in many countries, the use of antipsychotics contributed to the removal of many patients from psychiatric hospitals, and for those who remained, there were opportunities to create more favorable conditions for effective therapy and social rehabilitation measures. However, in this regard, different approaches to the organization of care for patients have come to light.
It is generally recognized that they have changed the stereotype of the course of many mental illnesses, reducing their severity and reducing the length of stay of patients in the hospital. According to the recognition of psychiatrists in many countries, the use of antipsychotics contributed to the removal of many patients from psychiatric hospitals, and for those who remained, there were opportunities to create more favorable conditions for effective therapy and social rehabilitation measures. However, in this regard, different approaches to the organization of care for patients have come to light.
According to the socio-psychological concept of the etiology of mental illness accepted in Anglo-American psychiatry, many types of mental abnormalities are regarded as the result of a violation of interpersonal relations in a microsociety. This contributed to the development and implementation in hospital practice of various types of sociotherapeutic influences (open door system, family, group therapy, therapeutic communities, environmental therapy, etc. ), which took the main place in the treatment of patients. Drug treatments in these and some other countries have almost faded into the background, and psychiatrists and other medical personnel have largely been replaced by psychologists and social workers. Moreover, low-skilled doctors and nurses began to work in state psychiatric hospitals in some Western countries [9].
), which took the main place in the treatment of patients. Drug treatments in these and some other countries have almost faded into the background, and psychiatrists and other medical personnel have largely been replaced by psychologists and social workers. Moreover, low-skilled doctors and nurses began to work in state psychiatric hospitals in some Western countries [9].
In domestic psychiatric hospitals in the situation under consideration, it was possible to maintain an integrated approach to the treatment of patients, which ensured a balance of medical and socio-rehabilitation measures. As an example in this regard, hospitals in a number of cities (St. Petersburg, Tomsk, Kaluga, Moscow, etc.) can be cited, where rehabilitation measures have received the greatest development.
Organizational aspect
An important achievement of Russian psychiatry, according to R.A. Nadzharova [3] is the creation of a unified accessible system of psychiatric care, in which the psychiatric hospital will take one of the leading places.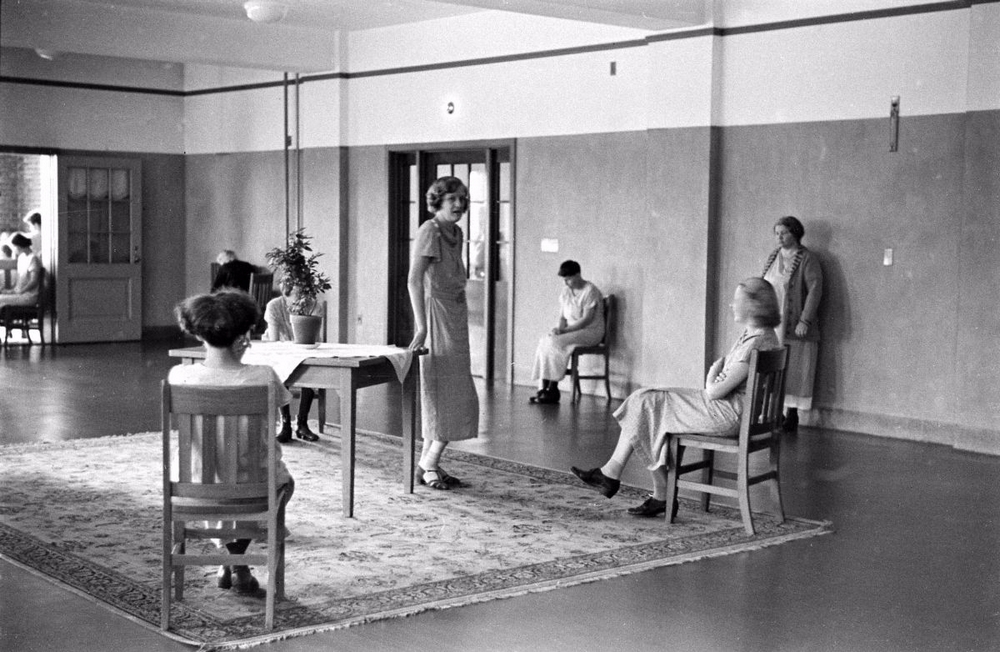 Unlike the system of psychiatric care in many foreign countries, the hospital sector of the domestic psychiatric service remains the largest and most significant to date [2, 7].
Unlike the system of psychiatric care in many foreign countries, the hospital sector of the domestic psychiatric service remains the largest and most significant to date [2, 7].
With the development of psychiatric science and practice, there was a specialization of hospital types of care, which began to differentiate according to age, nosological and other principles. To a large extent, this was facilitated in the 60-70s of the last century by an active discussion at conferences, meetings, and other issues of improving inpatient psychiatric care. There was an active discussion on the issues of reprofiling the medical departments of hospitals, replacing acute restless, semi-restless psychiatric departments with mixed, general psychiatric ones, etc. Thanks to the success of psychopharmacotherapy, it became possible to provide differentiated psychiatric care in psychiatric hospitals: along with territorial general psychiatric departments, a number of specialized departments were created ( children, adolescents, geriatric psychiatric, sanatorium, tuberculosis, forensic psychiatric, psychosomatic profile, etc. ).
).
In one of our previous publications [12], we presented the dynamics of individual indicators of the psychiatric service in the new Russia. In this article, we have the opportunity to provide updated indicators relating to hospital psychiatry 1991-2010.
Currently, the psychiatric service in Russia, unlike many other countries, remains centered on hospitals. Over the 20 years of the post-Soviet period (from 1991 to 2010), the number of psychiatric hospitals decreased from 288 to 234, although in some regions this reduction was indirect due to the merger of several hospitals into larger psychiatric hospitals with branches. The number of neuropsychiatric dispensaries with inpatient departments decreased from 9,eight%). The level of hospitalization of children (0-14 years old) with mental disorders increased by 70.1%.
The proportion of rehospitalizations decreased slightly (from 21.6 to 20.1%), while there is also an increase in rehospitalizations of patients with non-psychotic mental disorders and mental retardation.
The average duration of inpatient treatment over 20 years decreased by 23.6% (from 98.0 to 74.9 days). However, this concerned mainly groups of patients with psychoses and/or dementia, mental retardation. The terms of treatment of patients with non-psychotic mental disorders, on the contrary, have increased.
The diagnostic structure of the contingent of mental patients who were in hospitals also underwent changes: the proportion of patients with non-psychotic mental disorders (from 11.9 to 19.1%) and mental retardation (from 8.9 to 12.0%) increased. The change in these indicators was due to a decrease in the proportion of patients with psychoses and/or dementia (from 79.2 to 68.9%). The most problematic group of the hospital contingent is still patients who have been in the hospital for more than 1 year and, in fact, “block” 1/5 of the bed fund: if in 1991, their share was 22.9%, then in 2010 - 21.3%.
Thus, over the past 20 years, the proportion of the inpatient link in the structure of the psychiatric service has decreased, but the scale of the changes that have occurred compared to many other countries turned out to be much smaller.
Social and psychological aspect
The well-known German psychiatrist M. Angermeyer [13] noted that the degree of readiness of the population to seek psychiatric help is largely determined by the image of psychiatry that has developed in society, which is formed by psychiatric hospitals, which are associated among the population with restriction of freedom, repressive measures, etc. The correctness of this statement confirms the situation in our country.
According to domestic works [14], these ideas are supported by myths that have existed for a long time about the mentally ill and psychiatric hospitals in which these patients are located (“if a person ends up in a psychiatric hospital, then the road is closed to him everywhere”, “in psychiatric hospitals they use barbaric methods of treatment, etc.).
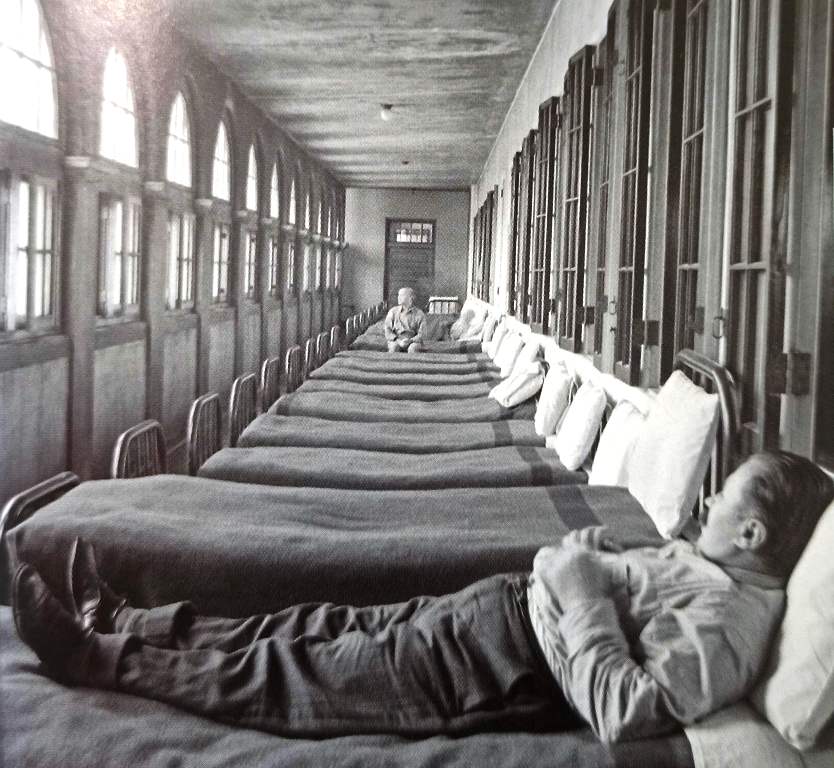
In many ways, the mass media contribute to the maintenance of these myths and negative stereotypes of society about psychiatry and psychiatric hospitals [15].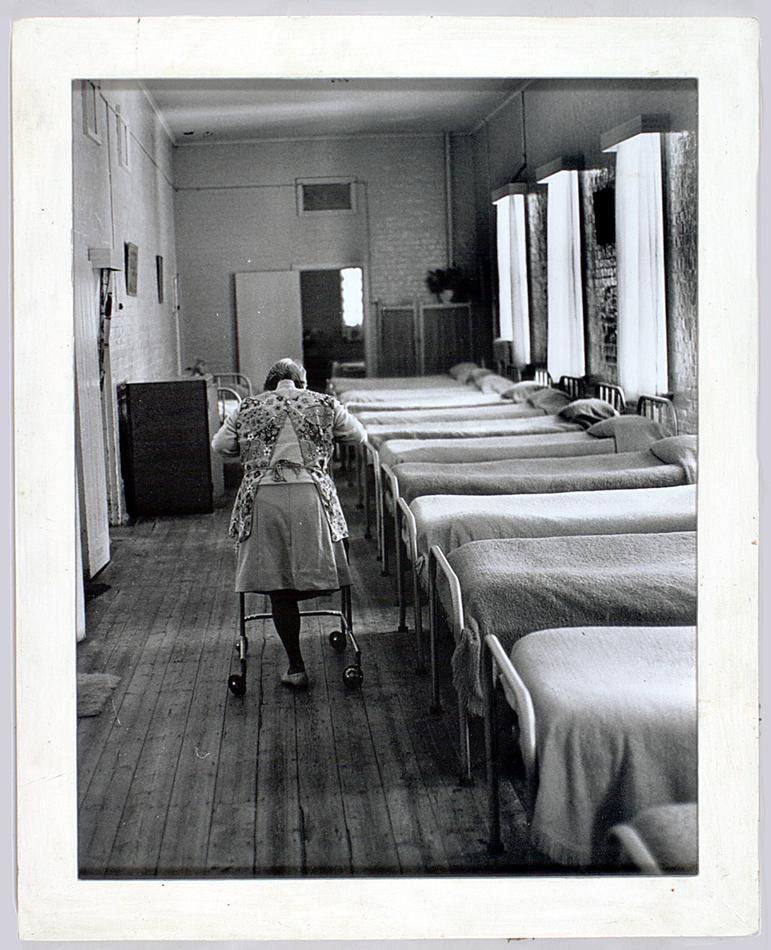 When describing the atmosphere of psychiatric hospitals, an analogy is often made with a prison, and the mentally ill with prisoners. In some newspaper publications, an “exposing” of the true state of the internal life of the hospital with “prison” orders in the departments, and the arbitrariness of the staff is presented. The emphasis is on the insufficient funding of the psychiatric service, due to which it is not able to provide either proper treatment, or even a decent maintenance of the mentally ill. In the relevant materials, stigmatizing terminology is usually used, when instead of the term “psychiatric hospital”, different sources use “fool” (4%), “madhouse” (29%), "psychiatric hospital" (67% of cases). It seems that the reader is deliberately transferred to the atmosphere of insane asylums of the end of the century before last - the beginning of the last century, the permanent inhabitants of which were patients with personality regression, its complete ruin, patients with hospital dementia, symptoms of hospitalism and social degradation [16].
When describing the atmosphere of psychiatric hospitals, an analogy is often made with a prison, and the mentally ill with prisoners. In some newspaper publications, an “exposing” of the true state of the internal life of the hospital with “prison” orders in the departments, and the arbitrariness of the staff is presented. The emphasis is on the insufficient funding of the psychiatric service, due to which it is not able to provide either proper treatment, or even a decent maintenance of the mentally ill. In the relevant materials, stigmatizing terminology is usually used, when instead of the term “psychiatric hospital”, different sources use “fool” (4%), “madhouse” (29%), "psychiatric hospital" (67% of cases). It seems that the reader is deliberately transferred to the atmosphere of insane asylums of the end of the century before last - the beginning of the last century, the permanent inhabitants of which were patients with personality regression, its complete ruin, patients with hospital dementia, symptoms of hospitalism and social degradation [16].
Meanwhile, in accordance with the current legislative national acts, documents of WHO and other international and national organizations, the observance of the rights and interests of patients is one of the most important tasks of the management of psychiatric hospitals. In practice, the implementation of these provisions is expressed in the organization of a therapeutic environment in the hospital, an open door regime, a system of home holidays, transfer of patients to a semi-stationary regime, etc. the architecture of psychiatric hospitals has a huge rehabilitative and destigmatizing effect. The question of the influence of architecture on mental health was discussed in the early 1980s [17]. It is noteworthy that by this time in some rehabilitation-oriented psychiatric hospitals in our country (Kaluga, Tomsk, etc.) a comfortable environment for the stay of patients had already been created. The thoughtful design of medical departments could serve as an example not only for general hospitals, but also for many sanatoriums and rest homes. It is obvious that this type of psychiatric departments, hospitals radically changed the traditional idea of the average person about a psychiatric hospital as a "house for the mad", intended for isolation and maintenance of its inhabitants. Ensuring the listed conditions, according to A.V. Snezhnevsky [4], reflects the "general culture" of the psychiatric hospital, helps to increase its prestige and authority among the population, helps to overcome its negative stereotypical images in society.
It is obvious that this type of psychiatric departments, hospitals radically changed the traditional idea of the average person about a psychiatric hospital as a "house for the mad", intended for isolation and maintenance of its inhabitants. Ensuring the listed conditions, according to A.V. Snezhnevsky [4], reflects the "general culture" of the psychiatric hospital, helps to increase its prestige and authority among the population, helps to overcome its negative stereotypical images in society.
To date, more and more data is accumulating, indicating that it is effective to reduce the duration of hospital treatment, reduce the level of repeated, prolonged and frequent hospitalizations, is the inclusion of psychosocial interventions and measures for the rehabilitation of patients in the system of inpatient treatment [7]. The departments of the first psychotic episode opened in Moscow, St. Petersburg, Orenburg, Nizhny Novgorod, Omsk and other cities can serve as an example of this kind. In these departments, the organization of complex treatment, including active pharmacotherapy and a variety of psychosocial interventions, allows achieving high quality remissions and maintaining the social functioning of patients at the highest possible level.
In these departments, the organization of complex treatment, including active pharmacotherapy and a variety of psychosocial interventions, allows achieving high quality remissions and maintaining the social functioning of patients at the highest possible level.
In a number of regions (St. Petersburg, Tambov, Omsk, Kaluga, etc.), on the basis of psychiatric hospitals, rehabilitation departments-hostels for patients who have been in hospital for a long time (over 1 year) have been opened. The system of complex psychosocial treatment (social rehabilitation work, training of cognitive and social skills) makes it possible to successfully rehabilitate and discharge up to 35-40% of such patients.
According to the existing tradition, in the Russian Federation, mental patients with concomitant pulmonary tuberculosis receive inpatient treatment in psychiatric hospitals. However, in a number of regions (Leningrad region, Vologda), the provision of this assistance was transferred to the TB service, which significantly reduced the stigmatization of such patients. Complex therapy in the created phthisio-psychiatric departments includes phthisiatric treatment, psychopharmacotherapy and psychosocial rehabilitation at the level of approved standards.
Complex therapy in the created phthisio-psychiatric departments includes phthisiatric treatment, psychopharmacotherapy and psychosocial rehabilitation at the level of approved standards.
In recent years, many psychiatric hospitals have opened day hospitals, geriatric psychiatric departments for social rehabilitation, and departments for social rehabilitation. Operating in a number of regions (St. Petersburg, Moscow, etc.), sanatorium-rehabilitation departments with an open regimen are designed to treat borderline mental disorders and maintain a good quality of remission in treated patients with psychoses.
Economic aspect
The activities of psychiatric hospitals and inpatient psychiatric units have been covered in some detail in our previous publications [12, 18, 19]. Here we only emphasize that in the new socio-economic conditions, the issues of the future development of inpatient psychiatric care, its structural reorganization should be addressed on the basis of a systematic approach, which should include improving the quality of inpatient types of psychiatric care, including its specialized types, introducing resource-saving forms of work in psychiatric hospitals , the maximum possible social integration of the mentally ill, the use of economic and financial mechanisms that contribute to the improvement of the entire system of inpatient psychiatric care. In practical terms, this can be reflected in the form of the restructuring of some hospital units into semi-inpatient units, specialized departments for patients with borderline, gerontopsychiatric and other profiles, boarding houses for patients who have lost their homes and social ties, the introduction of community-oriented forms of work (clubs, rehabilitation centers, groups of mutual support and self-support of patients, public associations for the implementation of public support programs for the mentally ill and their families, etc.). However, an important condition for the ongoing reorganization should be the preservation of the material, financial and human resources released by the psychiatric hospital when the bed fund is reduced, the use of financial mechanisms to increase motivation and stimulate the work of psychiatric hospital employees.
In practical terms, this can be reflected in the form of the restructuring of some hospital units into semi-inpatient units, specialized departments for patients with borderline, gerontopsychiatric and other profiles, boarding houses for patients who have lost their homes and social ties, the introduction of community-oriented forms of work (clubs, rehabilitation centers, groups of mutual support and self-support of patients, public associations for the implementation of public support programs for the mentally ill and their families, etc.). However, an important condition for the ongoing reorganization should be the preservation of the material, financial and human resources released by the psychiatric hospital when the bed fund is reduced, the use of financial mechanisms to increase motivation and stimulate the work of psychiatric hospital employees.
Prospects for the development of inpatient care
In foreign works concerning the prospects of inpatient psychiatric care [5, 9, 13, 20, 21], the issues of the future of state psychiatric hospitals are mainly discussed, which, according to the authors, will exist for many more years, and their differences will largely be determined by local conditions, the position of the psychiatrists working in them, the attitude to stationary types of care of the whole society.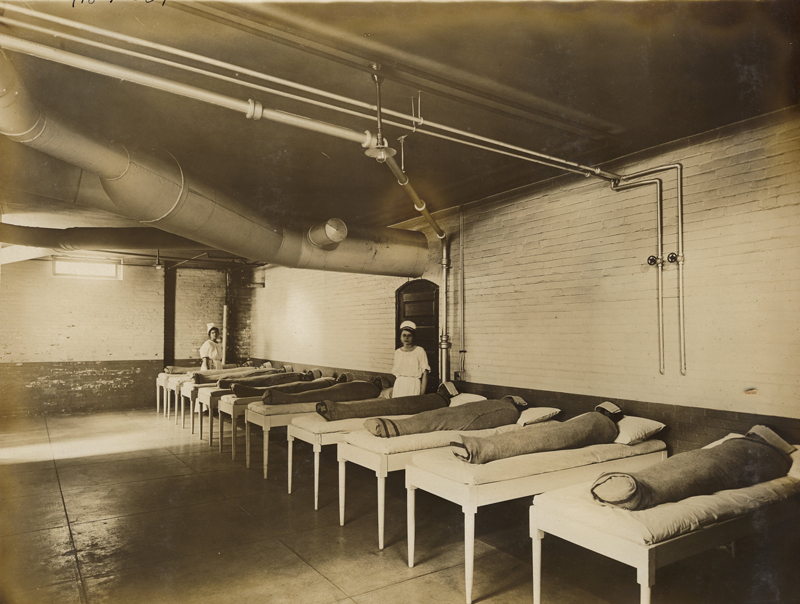 It is noted that the main contingent in these hospitals will be patients with a chronic course of the disease. However, it is emphasized that the psychiatric hospital will continue to be an institution that provides the most qualified types of care that the community mental health service will not be able to provide.
It is noted that the main contingent in these hospitals will be patients with a chronic course of the disease. However, it is emphasized that the psychiatric hospital will continue to be an institution that provides the most qualified types of care that the community mental health service will not be able to provide.
Discussion of the issues of the future development of the domestic system of psychiatric care, including inpatient care, should be carried out taking into account several fundamental circumstances. The first and most important thing is that when creating a promising model of care, domestic experience and the best traditions that were created by our predecessors, representatives of zemstvo psychiatry, and later by well-known scientists and organizers of psychiatric care, should be taken into account. The second circumstance boils down to building a strategy for the development of hospital care based on the general concept of psychiatric care, which in our country has not yet been fully developed. And finally, when developing a further strategy for the development of the psychiatric service, it is necessary to take into account the realities of today, the available financial, material and other possibilities of the service, department, and the state as a whole.
And finally, when developing a further strategy for the development of the psychiatric service, it is necessary to take into account the realities of today, the available financial, material and other possibilities of the service, department, and the state as a whole.
One of the most pressing issues of the modern psychiatric service, which is very significant for the domestic system of care, is the ratio of the volume, types and forms of care provided in the conditions of out-of-hospital and inpatient links. From the above data it follows that in modern conditions this ratio is subject to revision. Another question is how and in what terms this revision can be carried out.
From our point of view, the restructuring of the current system of out-of-hospital and inpatient care should be carried out in stages and in several directions. Serious preparatory work is required for the transition to a system of preferential treatment of patients in out-of-hospital settings.
At the first stage, it is necessary to strengthen the network of non-hospital institutions, improve their forms of assistance, develop socially oriented types of care, and create a developed network of communities into which patients could be integrated. At the same time, neuropsychiatric dispensaries should remain the main institutions that create the necessary conditions for the provision of complex types of assistance on their territory, provide it themselves and coordinate the work of social, public, and other interacting institutions and services. Ultimately, the out-of-hospital psychiatric service of the municipality, the territory whose population it serves, should provide patients with the necessary amount of diagnostic, therapeutic and socio-rehabilitation care [1, 22]. Only then can we talk about the readiness of outpatient services to take over part of the treatment, diagnostic and rehabilitation care that patients currently receive in psychiatric hospitals and which the outpatient psychiatric service should provide in accordance with modern trends.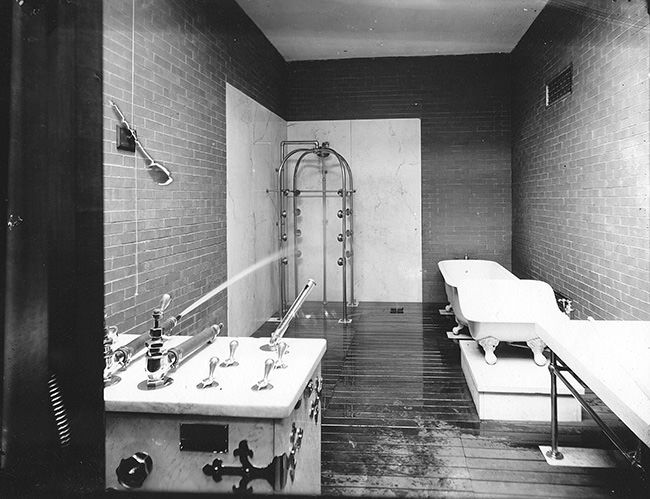
Psychiatric hospitals at the first, "transitional" stage should also change the volume and types of care, adding alternative forms of care to traditional ones. Here, first of all, we can talk about the introduction of resource-saving organizational and medical technologies. The staff of a psychiatric hospital can more effectively use the accumulated intra-institutional resources aimed at more intensive methods of work (reducing the time for examining patients, improving the work of paraclinical and housekeeping services, etc.). On the basis of this approach, the average duration of a patient's stay in a bed can be reduced without harm to the patient, which, as noted above, is one of the highest in our country in comparison with other countries.
Due to the unused bed fund and the re-profiling of beds in a psychiatric hospital, it is possible to develop types of care replacing the hospital - semi-inpatient and outpatient. It is known that at the moment the provision of mentally ill places in day hospitals does not exceed 30% of the need for them. In the setting of psychiatric hospitals, as already noted, community-oriented forms of care should be widely adopted. From the point of view of internal sources of saving resources, it is preferable to convert underutilized beds into beds for medical and social assistance to the elderly, the disabled and other groups of patients who need it.
In the setting of psychiatric hospitals, as already noted, community-oriented forms of care should be widely adopted. From the point of view of internal sources of saving resources, it is preferable to convert underutilized beds into beds for medical and social assistance to the elderly, the disabled and other groups of patients who need it.
In this regard, the positive experience accumulated on the territory of our country deserves attention.
The activities of the second stage of the restructuring of out-of-hospital and inpatient psychiatric care can be implemented after the implementation of the activities of the first stage and the accumulation of relevant work experience. Thus, a staged restructuring of the inpatient and outpatient mental health care network will help to avoid the negative consequences that many patients experienced in different countries when they were transferred from hospitals to the community.
To successfully solve these problems, it will be necessary to improve the system of training young and advanced training of specialists working in psychiatry, in accordance with which they could use new technologies for diagnosing, treating and rehabilitating patients.
Let us emphasize that the implementation of the above measures to improve inpatient psychiatric care can have not only a clinical, economic, but also an important social effect, according to which many contingents of patients at different stages will be able to receive comprehensive types of care, including psychosocial, and psychiatric hospitals themselves - improve their social role and image.
An undoubted condition for the implementation of the listed activities of the long-term plan is a change in the relevant regulatory framework, a number of departmental and interdepartmental documents that would give regional health authorities, heads of psychiatric institutions the right to carry out the necessary restructuring in accordance with the need for certain types of assistance, without fear of changing the staffing structure and the number of personnel, other restrictions that are provided for by the current regulatory documents. Since this is mainly about the regulatory framework at the federal level, it should be developed by the relevant structures of the Ministry of Health of the Russian Federation, regional health authorities, and the Institute of Chief Psychiatrists.
Discussing the issues of the future development of inpatient psychiatric care, we consider it appropriate to dwell on a brief description of the reorganization of the Moscow city psychiatric service carried out in 2012, according to which neuropsychiatric dispensaries were subordinated to the territorial psychiatric hospitals of the capital. From our point of view, which is also shared by many heads of psychiatric institutions and services, the restructuring of the service in Moscow contradicts the fundamental principle of domestic and foreign psychiatry - the maximum approximation of psychiatric care to the mentally ill, their place of residence, their family and other environment. One of the serious shortcomings of the introduced structure of the psychiatric service is the deprivation of the legal independence of neuropsychiatric dispensaries. Restriction of the legal, administrative, economic, financial and other rights of the dispensary greatly complicates its ability to independently resolve a wide range of issues related to the conduct of medical diagnostic and rehabilitation work, the solution of many social problems of patients, interaction with territorial bodies of social protection, law enforcement, education , manufacturing enterprises, etc.
In conclusion, inpatient care remains an integral part of the overall mental health care system. The psychiatric hospital is an important institution that provides specialized care, improves methods of diagnosis and treatment of mental disorders, while still playing the role of clinical, scientific and educational base at the same time.
The treatment and diagnostic, rehabilitation process, the structure of a psychiatric hospital should be organized in accordance with modern achievements in psychiatric science and practice. The volume of therapeutic measures in it should be based on a combination of drug methods and psychosocial effects.
The appearance and way of life of a psychiatric hospital should be built on the principle of the least stigmatizing impact.
The solution to the issue of restructuring the inpatient service and changing the emphasis in the types and volumes of care provided by it should be based on an appropriate national mental health program that determines the optimal and effective model of a modern service.