Manic behaviors examples
Symptoms - Bipolar disorder - NHS
Bipolar disorder is characterised by extreme mood swings. These can range from extreme highs (mania) to extreme lows (depression).
Episodes of mania and depression often last for several weeks or months.
Depression
During a period of depression, your symptoms may include:
- feeling sad, hopeless or irritable most of the time
- lacking energy
- difficulty concentrating and remembering things
- loss of interest in everyday activities
- feelings of emptiness or worthlessness
- feelings of guilt and despair
- feeling pessimistic about everything
- self-doubt
- being delusional, having hallucinations and disturbed or illogical thinking
- lack of appetite
- difficulty sleeping
- waking up early
- suicidal thoughts
Mania
The manic phase of bipolar disorder may include:
- feeling very happy, elated or overjoyed
- talking very quickly
- feeling full of energy
- feeling self-important
- feeling full of great new ideas and having important plans
- being easily distracted
- being easily irritated or agitated
- being delusional, having hallucinations and disturbed or illogical thinking
- not feeling like sleeping
- not eating
- doing things that often have disastrous consequences – such as spending large sums of money on expensive and sometimes unaffordable items
- making decisions or saying things that are out of character and that others see as being risky or harmful
Patterns of depression and mania
If you have bipolar disorder, you may have episodes of depression more regularly than episodes of mania, or vice versa.
Between episodes of depression and mania, you may sometimes have periods where you have a "normal" mood.
The patterns are not always the same and some people may experience:
- rapid cycling – where a person with bipolar disorder repeatedly swings from a high to a low phase quickly without having a "normal" period in between
- mixed state – where a person with bipolar disorder experiences symptoms of depression and mania together; for example, overactivity with a depressed mood
If your mood swings last a long time but are not severe enough to be classed as bipolar disorder, you may be diagnosed with a mild form of bipolar disorder called cyclothymia.
Living with bipolar disorder
Bipolar disorder is a condition of extremes. A person with bipolar disorder may be unaware they're in the manic phase.
After the episode is over, they may be shocked at their behaviour. But at the time, they may believe other people are being negative or unhelpful.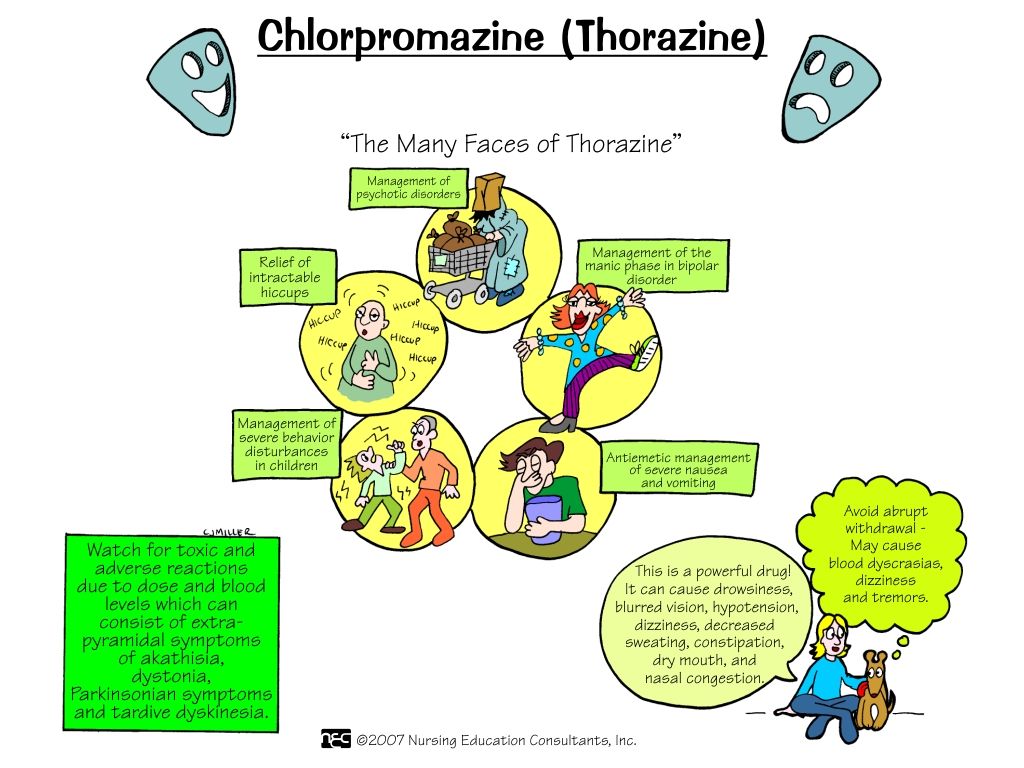
Some people with bipolar disorder have more frequent and severe episodes than others.
The extreme nature of the condition means staying in a job may be difficult and relationships may become strained. There's also an increased risk of suicide.
During episodes of mania and depression, someone with bipolar disorder may experience strange sensations, such as seeing, hearing or smelling things that are not there (hallucinations).
They may also believe things that seem irrational to other people (delusions). These types of symptoms are known as psychosis or a psychotic episode.
Find out more about living with bipolar disorder
Page last reviewed: 14 March 2019
Next review due: 14 March 2022
What Is It, Causes, Triggers, Symptoms & Treatment
Overview
What is mania?
Mania is a condition in which you have a period of abnormally elevated, extreme changes in your mood or emotions, energy level or activity level.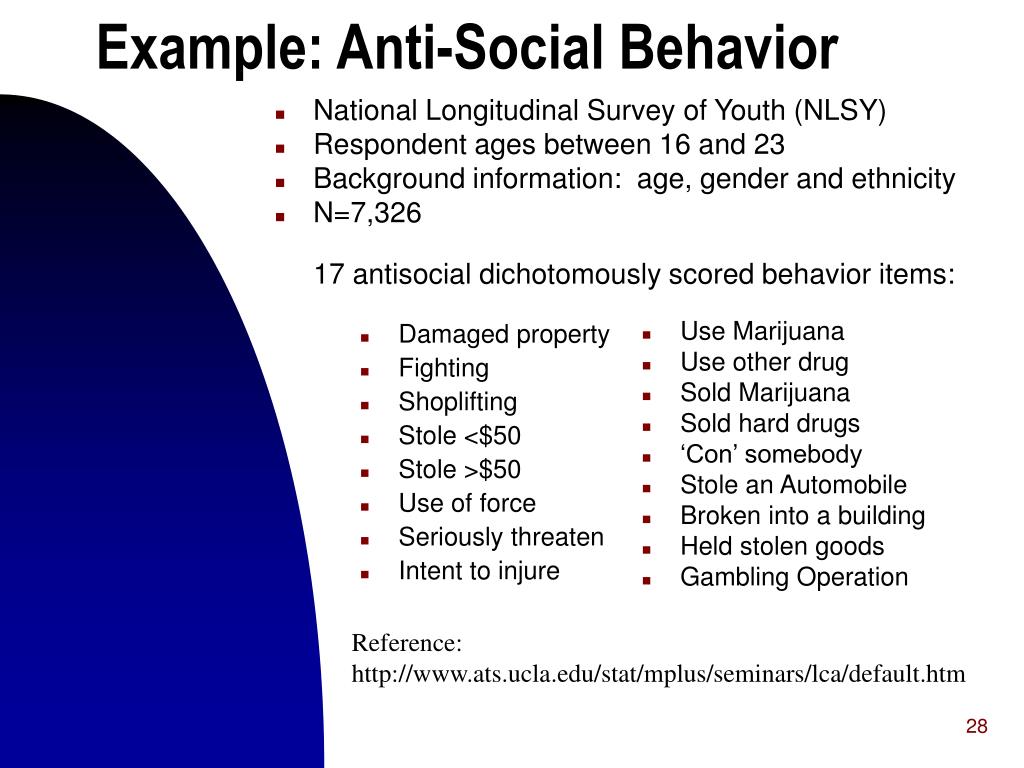 This highly energized level of physical and mental activity and behavior must be a change from your usual self and be noticeable by others.
This highly energized level of physical and mental activity and behavior must be a change from your usual self and be noticeable by others.
What's considered an “abnormal,” extreme change in behavior and what does it look like?
Abnormal manic behavior is behavior that stands out. It’s over-the-top behavior that other people can notice. The behavior could reflect an extreme level of happiness or irritation. For example, you could be extremely excited about an idea for a new healthy snack bar. You believe the snack could make you an instant millionaire but you’ve never cooked a single meal in your life, don’t know a thing about how to develop a business plan and have no money to start a business. Another example might be that you strongly disagree with a website “influencer” and not only write a 2,000 word post but do an exhaustive search to find all the websites connected to the influencer so you can post your letter there too.
Although these examples may sound like they could be normal behavior, a person with mania will expend a great deal of time and energy including many sleepless nights working on projects such as these.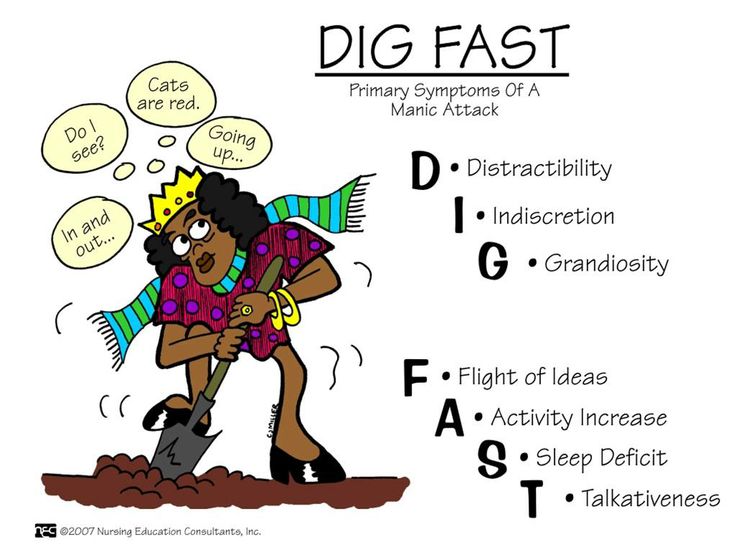
What is a manic episode?
A manic episode is a period of time in which you experience one or more symptoms of mania and meet the criteria for manic episode (see “symptoms” and “diagnosis” sections). In some cases, you may need to be hospitalized.
Can I have a manic episode as its own condition or is it always part of another mental health condition?
Technically if you have a manic episode, you have a mental health condition. Mania can be a part of several mental health conditions including:
- Bipolar I disorder (most common condition for mania to occur).
- Seasonal affective disorder.
- Postpartum psychosis.
- Schizoaffective disorder.
- Cyclothymia.
What is bipolar I disorder?
Bipolar I disorder is a mental health illness in which a person has major high and low swings in mood, activity, energy and ability to think clearly. To be diagnosed with bipolar I disorder, you have to have at least one episode of mania that lasts for at least seven days or have an episode that is so severe that it requires hospitalization.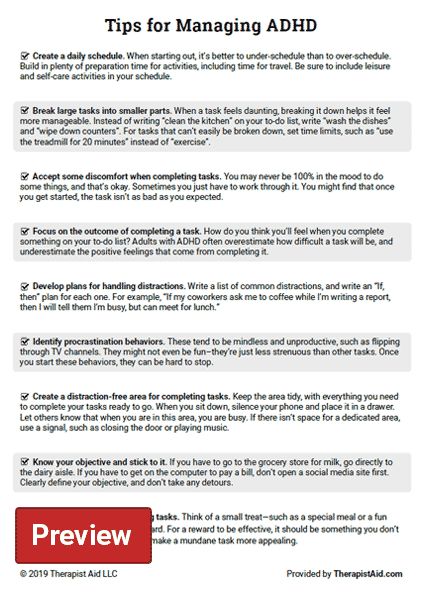
Most people have both episodes of both mania and depression, but you don’t have to have depression to be diagnosed with mania. Many people with a bipolar I disorder diagnosis have recurring, back-to-back manic episodes with very few episodes of depression.
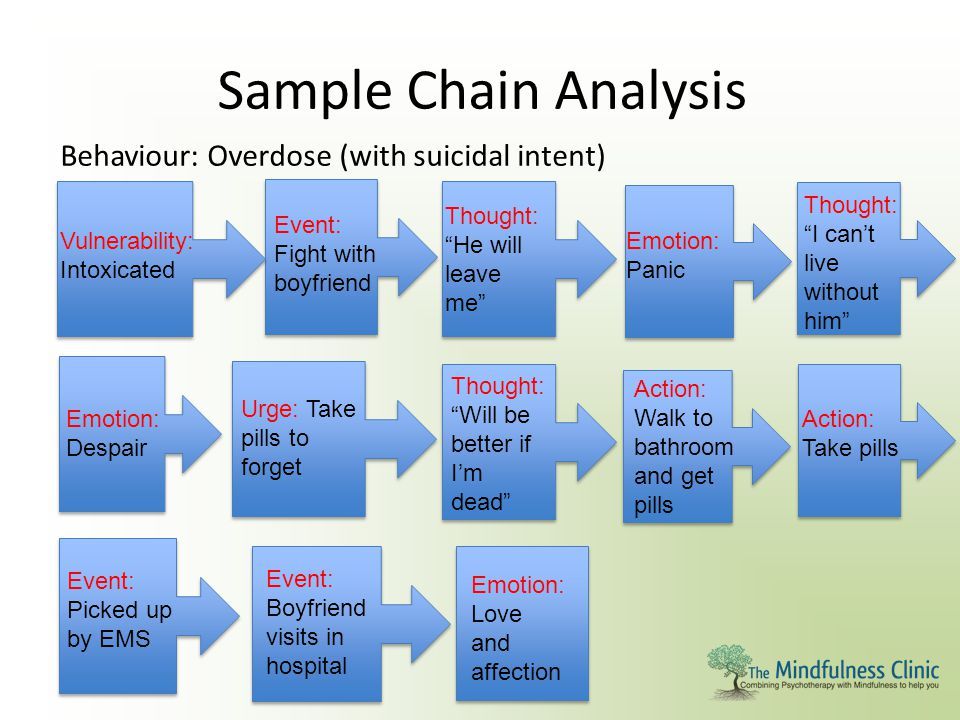
What are the triggers of manic episodes?
Manic episode triggers are unique to each person. You’ll have to become a bit of a detective and monitor your mood (even keeping a “mood diary”) and start to track how you feel before an episode and when it occurs. Ask family and close friends who you trust and have close contact with to help identify your triggers. As outside observers, they may notice changes from your usual behavior more easily than you do.
Knowing your triggers can help you prepare for an episode, lessen the effect of an episode or prevent it from happening at all.
Common triggers to be aware of include:
- A highly stimulating situation or environment (for example, lots of noise, bright lights or large crowds).
- A major life change (such as divorce, marriage or job loss).
- Lack of sleep.
- Substance use, such as recreational drugs or alcohol.
What happens after a manic episode?
After a manic episode you may:
- Feel happy or embarrassed about your behavior.
- Feel overwhelmed by all the activities you’ve agreed to take on.
- Have only a few or unclear memories of what happened during your manic episode.
- Feel very tired and need sleep.
- Feel depressed (if your mania is part of bipolar disorder).
Symptoms and Causes
What are the symptoms of mania?
Symptoms of a manic episode
- Having an abnormally high level of activity or energy.
- Feeling extremely happy or excited — even euphoric.
- Not sleeping or only getting a few hours of sleep but still feeling rested.
- Having an inflated self-esteem, thinking you’re invincible.
- Being more talkative than usual.
 Talking so much and so fast that others can’t interrupt.
Talking so much and so fast that others can’t interrupt. - Having racing thoughts — having lots of thoughts on lots of topics at the same time (called a “flight of ideas”).
- Being easily distracted by unimportant or unrelated things.
- Being obsessed with and completely absorbed in an activity.
- Displaying purposeless movements, such as pacing around your home or office or fidgeting when you’re sitting.
- Showing impulsive behavior that can lead to poor choices, such as buying sprees, reckless sex or foolish business investments.
Psychotic symptoms of a manic episode
- Delusions. Delusions are false beliefs or ideas that are incorrect interpretations of information. An example is a person thinking that everyone they see is following them.
- Hallucinations. Having a hallucination means you see, hear, taste, smell or feel things that aren’t really there. An example is a person hearing the voice of someone and talking to them when they’re not really there.
How long does a manic episode last?
Early signs (called “prodromal symptoms”) that you’re getting ready to have a manic episode can last weeks to months. If you’re not already receiving treatment, episodes of bipolar-related mania can last between three and six months. With effective treatment, a manic episode usually improves within about three months.
What causes mania?
Scientists aren’t completely sure what causes mania. However, there are several factors that are thought to contribute. Causes differ from person to person.
Causes may include:
- Family history. If you have a family member with bipolar illness, you have an increased chance of developing mania. This isn't definite though. You may never develop mania even if other family members have.
- A chemical imbalance in the brain.
- A side effect of a medication (such as some antidepressants), alcohol or recreational drugs.
- A significant change in your life, such as a divorce, house move or death of a loved one.
- Difficult life situations, such as trauma or abuse, or problems with housing, money or loneliness.
- A high level of stress and an inability to manage it.
- A lack of sleep or changes in sleep pattern.
- As a side effect of mental health problems including seasonal affective disorder, postpartum psychosis, schizoaffective disorder or other physical or neurologic condition such as brain injury, brain tumors, stroke, dementia, lupus or encephalitis.
Diagnosis and Tests
How is mania diagnosed?
Your healthcare provider will ask about your medical history, family medical history, current prescriptions and non-prescription medications and any herbal products or supplements you take. Your provider may order blood tests and body scans to rule out other conditions that may mimic mania. One such condition is hyperthyroidism. If other diseases and conditions are ruled out, your provider may refer you to a mental health specialist
To be diagnosed with mania, your mental health specialist may follow the criteria of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, DSM-5.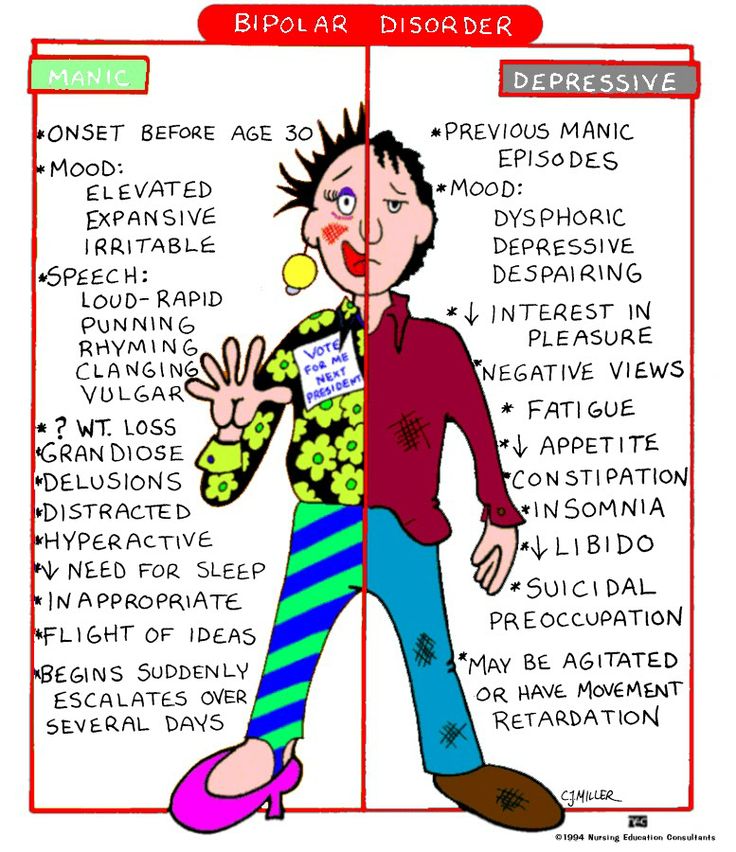 Their criteria for manic episode is:
Their criteria for manic episode is:
- You have an abnormal, long-lasting elevated expression of emotion along with a high degree of energy and activity that lasts for at least one week and is present most of the day, nearly every day.
- You have three or more symptoms to a degree that they’re a noticeable change from your usual behavior (four symptoms if mood is only irritable). (See the symptoms section of this article for a list of the symptoms used as criteria.)
- The mood disturbance is severe enough to cause significant harm to your social, work or school functioning or there’s a need to hospitalize you to prevent you from harming yourself or others, or you have psychotic features, such as hallucinations or delusions.
- The manic episode can’t be caused by the effects of a substance (medications or drug abuse) or another medical condition.
Management and Treatment
How is mania treated?
Mania is treated with medications, talk therapy, self-management and family and friends support.
Medications
If you have mania only, your healthcare provider may prescribe an antipsychotic medication, such as ariprazole (Abilify®), lurasidone (Latuda®), olanzapine (Zyprexa®), quetiapine (Seroquel®) or risperridone (Risperdal®).
If you have mania as part of a mood disorder, your provider may add a mood stabilizer. Some examples include lithium, valproate (Depakote®) and carbamazepine (Tegretol®). (If you’re pregnant or plan to become pregnant, let your provider know. Valproate can increase the chance of birth defects and learning disabilities and shouldn’t be prescribed to individuals who are able to become pregnant.)
Sometimes antidepressants are also prescribed.
Talk therapy (psychotherapy)
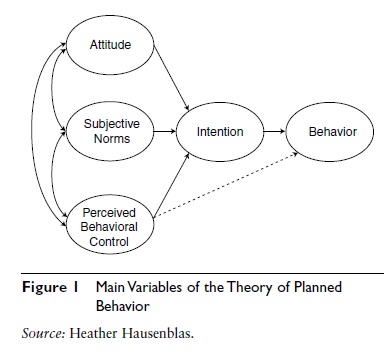
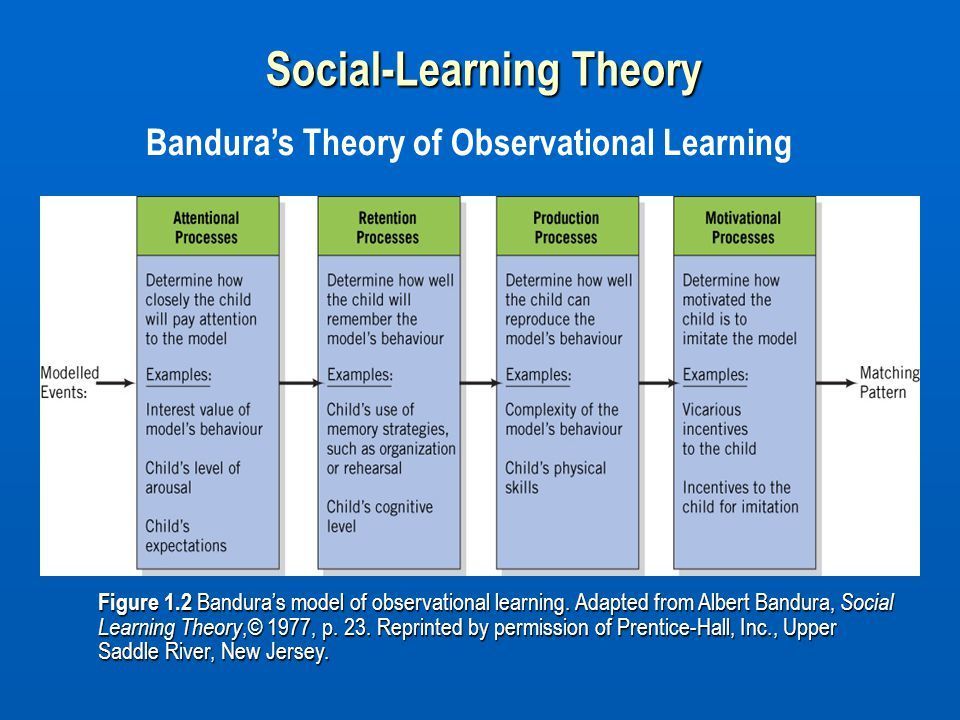
- Psychotherapy involves a variety of techniques. During psychotherapy, you’ll talk with a mental health professional who'll help you identify and work through factors that may be triggering your mania and/or depression (if you’re diagnosed with bipolar I disorder).
- Cognitive behavioral therapy can be useful in helping you change inaccurate perceptions that you have about yourself and the world around you.
- Family therapy is important since it’s very helpful for your family members to understand your behavior and what they can do to help.
Ask your provider for contact information for local support groups. You might find it helpful to talk with other people who have similar medical experiences and share problems, ideas for coping and strategies for living and caring for yourself.
Other treatments
Electroconvulsant therapy (ECT) may be considered in rare cases in individuals who have severe mania or depression (if bipolar). ECT involves applying brief periods of electric current to your brain.
Prevention
What steps can I take to better cope with or manage my mania?
Although episodes of mania can’t always be prevented, you can make a plan to better manage your symptoms and prevent them from getting worse when you feel a manic episode may be starting.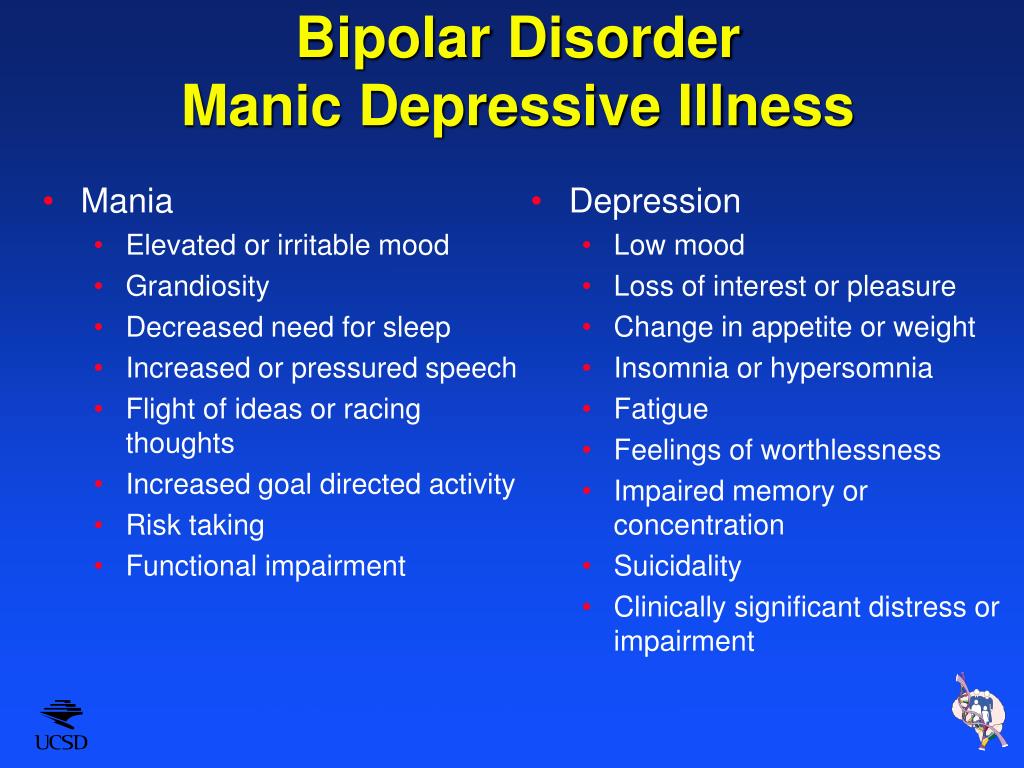
Some ideas to try during this time include:
- Avoid stimulating activities and environment – such as loud or busy places or bright places. Instead choose calm and relaxing activities and environments.
- Stick to routines. Go to bed at a set time, even if you’re not tired. Also, stick to the same times for eating meals, taking medications and exercising.
- Limit the number of social contacts to keep you from getting too stimulated and excited.
- Postpone making any major life decisions and big purchases.
- Avoid people and situations that might tempt you to make poor or risky choices, such as taking recreational drugs or drinking alcohol.
- Consider selecting someone to manage your finances during a manic episode.
If you ever have thoughts of harming yourself, tell family or friends, call you healthcare provider or contact the National Suicide Prevention Lifeline at 800-273-(TALK) (1-800-273-8255). Counselors are available 24/7.
Outlook / Prognosis
What outcome can I expect if I’ve been diagnosed with mania?
If your mania is related to a diagnosis of bipolar I disorder, this is a lifelong disease. Although there’s no cure for mania, medication and talk therapy (psychotherapy) can manage your condition in most cases.
Living With
How can I involve family and friends in understanding my mania?
It’s important to have an honest conversation with your family and closest friends.
- Let your family and friends know what you do and don’t find helpful. For example, if you’d appreciate a friendly reminder about taking your daily medications or a question about if you are getting enough sleep, let them know. On the other hand, if you don’t like always being asked if your current state of happiness is a sign you’re having a manic episode, discuss this.
- Ask your family and friends if they can help identify your triggers if you can’t. They may be able to spot triggers that you can’t spot yourself.
 Ask what they’ve noticed or any patterns they may see around the times of your episodes. As soon as you recognize an early sign, make an appointment to see your healthcare provider. You may or may not need a medication adjustment. However, it’s good to be on the alert since your symptoms could rapidly change.
Ask what they’ve noticed or any patterns they may see around the times of your episodes. As soon as you recognize an early sign, make an appointment to see your healthcare provider. You may or may not need a medication adjustment. However, it’s good to be on the alert since your symptoms could rapidly change. - Describe how your symptoms feel to you. Your family and friends will have a better understanding of your condition.
- Let family and friends know what type of help you’d like from them and when you’d like it. There may be times when you feel you can cope on your own. Knowing the difference will be helpful for everyone.
Frequently Asked Questions
What is acute mania?
Acute mania is the manic phase of bipolar I disorder. It is defined as an extremely unstable euphoric or irritable mood along with excess activity or energy level, excessively rapid thought and speech, reckless behavior and feeling of invincibility.
What is unipolar mania?
Unipolar mania is a disorder in which only excitement, excess activity or energy level and euphoric symptoms are seen. This is a rare condition.
What’s the difference between mania and hypomania?
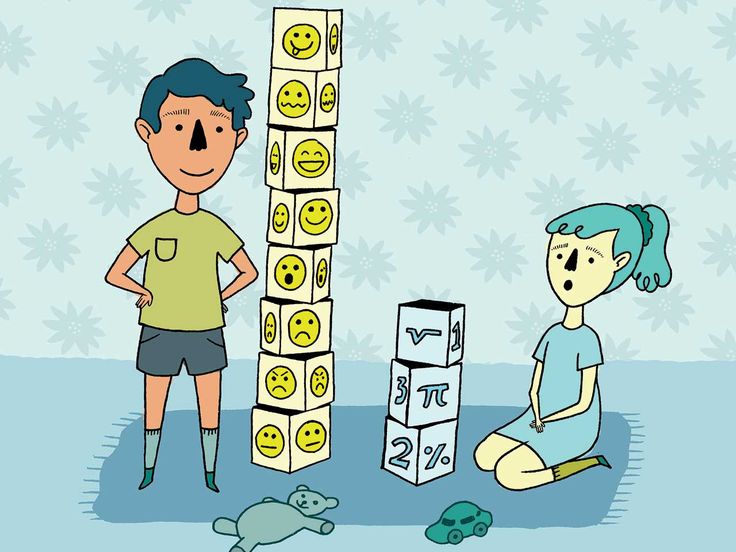
Hypomania is a less severe form of mania. The criteria that healthcare professionals use to make the diagnosis of either hypomania or mania is what sets them apart. The differences between these two conditions is as follows:
| Mania | Hypomania | |
|---|---|---|
| How long the episode lasts. | At least one week. | At least four consecutive days. |
| Severity of episode. | Causes severe impact on social or work/school functioning. | Not severe enough to significantly affect social or work/school functioning. |
| Need for hospitalization. | Possibly. | No. |
| Psychotic symptoms present (delusions or hallucinations). | Is among possible symptoms. | Can’t be present for a diagnosis of hypomania. |
Can my diagnosis change between bipolar I disorder and bipolar II disorder?
No. Once you have a diagnosis of bipolar I disorder — even if you never have another manic episode or a psychotic event (delusions or hallucinations) — your diagnosis can never be changed to bipolar II disorder. You’ll always have a bipolar I disorder diagnosis.
A note from Cleveland Clinic
Problems can develop in your social life, work/school functioning and home life when you have symptoms of mania, which include mood swings and an abnormal level of energy and activity. You may require hospitalization if you have severe hallucinations or delusions, or to prevent you from harming yourself or others. It’s important to have a good understanding of mania, mania symptoms, your particular triggers and ways to better manage your manic episodes. Medications, talk therapy and support groups as well as support from your family and friends can help manage your mania.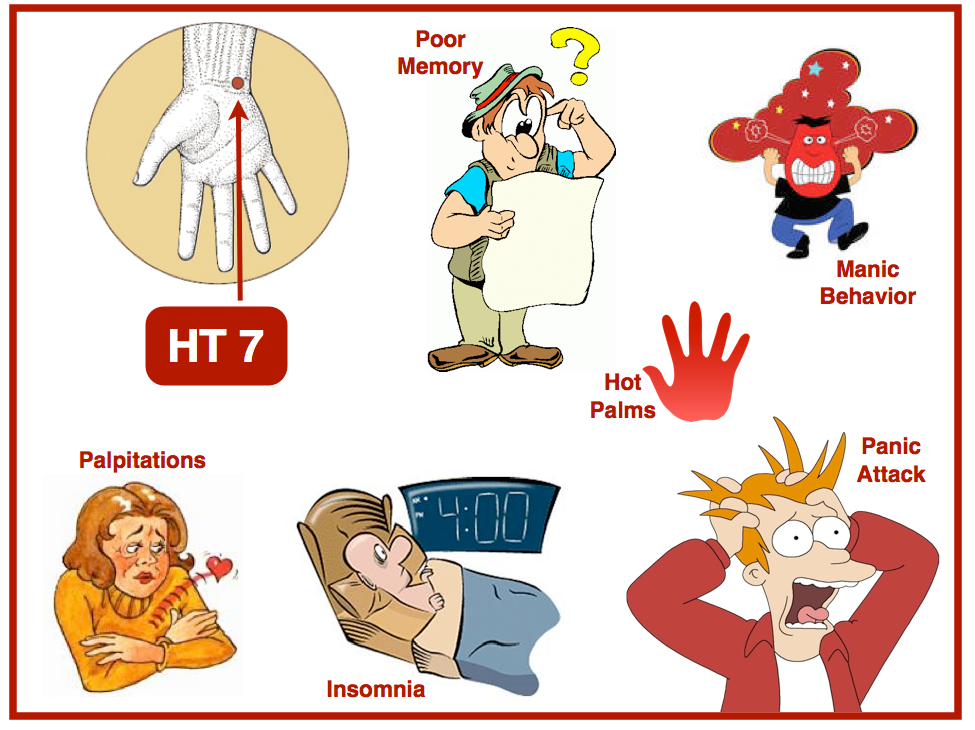 Stay in close contact with all your healthcare providers, especially during times of manic episodes. Your provider will want to see you and may need changes to your medications or dose.
Stay in close contact with all your healthcare providers, especially during times of manic episodes. Your provider will want to see you and may need changes to your medications or dose.
Manic syndrome - good mood or mania?
Inadequately elevated mood is a state that is exactly the opposite of depression. If it haunts a person for a sufficiently long time and is accompanied by other inadequate or illogical manifestations, then it is considered a mental disorder. This condition is referred to as manic and requires special treatment. Depending on the severity of the symptoms, consultation with a psychotherapist or psychiatrist may be required.
Features of the development of mania
In some cases, a tendency to mania can be a character trait, as well as a tendency to apathy. Increased activity, constant mental agitation, inappropriately high spirits, outbursts of anger or aggression are all symptoms of a manic syndrome. This is the name for a whole group of conditions that have different causes and sometimes different symptoms.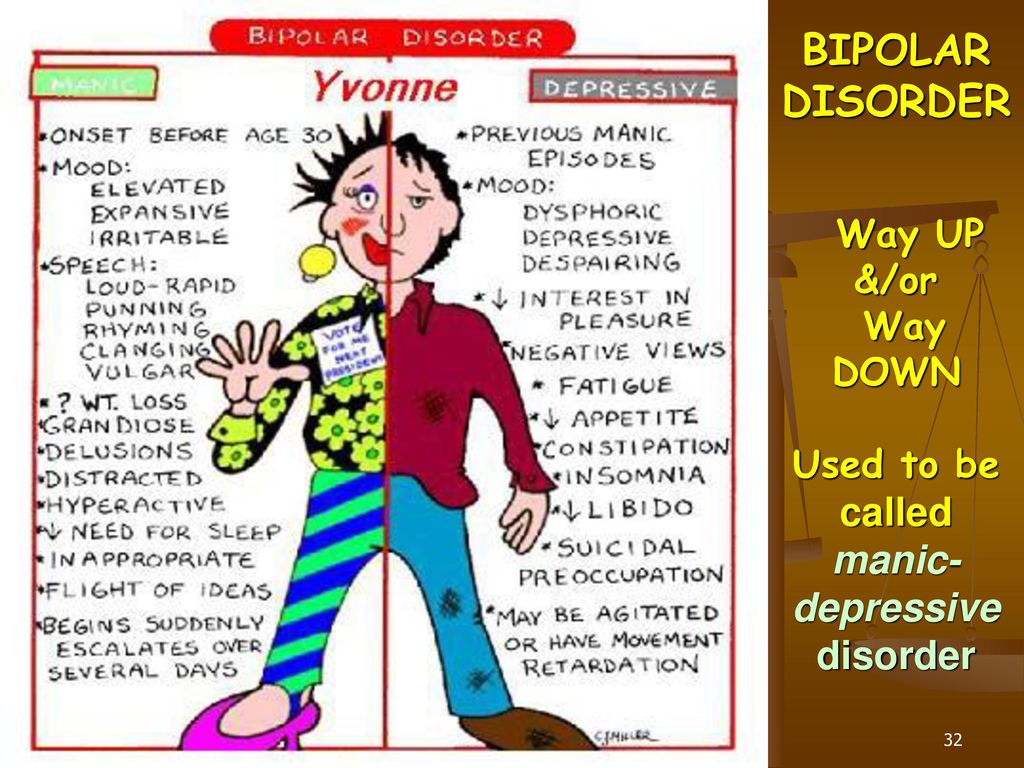
Both various life situations and incidents and uncorrected pathological character traits lead to the development of mania. A person prone to manic behavior is very often obsessed with an idea, he strives to realize it, even if it is unrealistic. Often patients are driven by theories that have political, religious or scientific justifications. Quite often, patients show a tendency to active social and social activities.
A significant proportion of manic patients have so-called overvalued thoughts and ideas. Sometimes they can be global, sometimes they are ideas of the household level. From the outside, the behavior of patients talking about their ideas sometimes looks quite comical. If the overvalued thought is of a global nature, the patient, on the contrary, seems thoughtful and enthusiastic to those around him. Especially if he has enough education and erudition to justify his beliefs.
This condition is not always a pathology, it can be individual mental characteristics.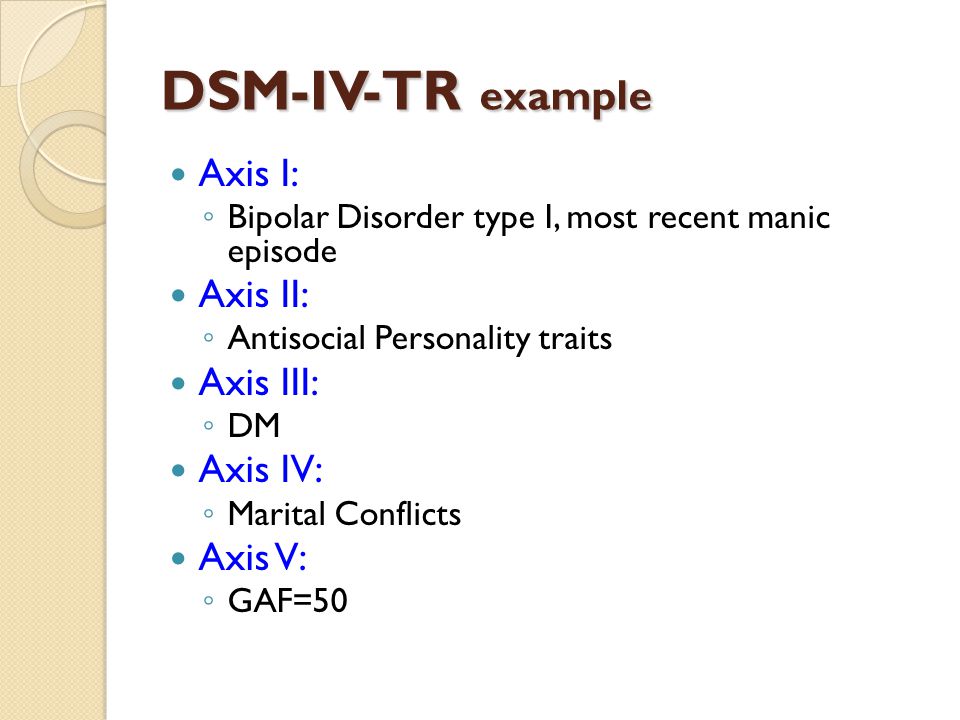 Treatment is necessary if overvalued thoughts and ideas get out of control and absorb the entire life of the patient, in other words, they prevent him or others from living.
Treatment is necessary if overvalued thoughts and ideas get out of control and absorb the entire life of the patient, in other words, they prevent him or others from living.
When do you need medical attention?
Manic syndrome is already a deviation from the norm, which is characterized by a number of symptoms that are more unpleasant for others than for the patient himself. This disease is manifested by disturbances in mental activity and the emotional sphere.
Usually the behavior of a manic patient is incomprehensible to others and looks at least strange.
There are certain symptoms that indicate the need for medical attention:
- Extremely high spirits, up to constant mental excitement and euphoria.
- Inappropriate optimism, the patient does not notice real problems and is not inclined to experience a bad mood appropriate to the occasion.
- Accelerated speech, accelerated thinking, lack of concentration on objects and phenomena that the patient is not interested in.
 Therefore, in mania, learning is often difficult when you have to pay attention to rather boring things.
Therefore, in mania, learning is often difficult when you have to pay attention to rather boring things. - Increased mobility, active gestures and hyperbolic facial expressions.
- Extravagance, pathological generosity. The patient can spend all the savings in a minute, not realizing the responsibility for his actions.
- Insufficient control over behavior. The patient does not realize that his high spirits are not appropriate everywhere.
- Hypersexuality, often with promiscuity (for example, a person who has never been prone to cheating before suddenly begins to flirt “indiscriminately”, enters into close relationships that he would never have dared to before, to the point that he starts several novels in parallel or embarks on a series of "short non-committal relationships", about which later, after the episode of mania has passed, he will repent and feel shame and even disgust, sincerely not understanding "how this could happen").
Treatment is complicated by the fact that the patient himself often does not recognize himself as ill.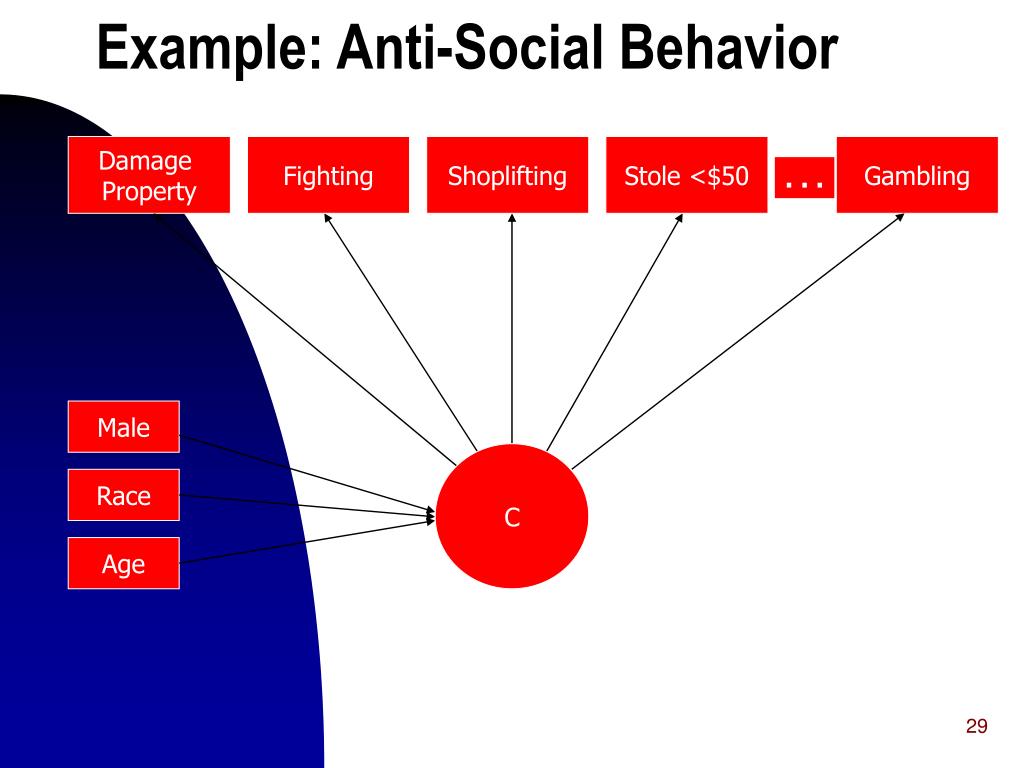 He considers his condition normal, subjectively pleasant and does not understand why others do not like his behavior: after all, he feels good, like never before. It is difficult to send such a patient to see a doctor and persuade him to therapy.
He considers his condition normal, subjectively pleasant and does not understand why others do not like his behavior: after all, he feels good, like never before. It is difficult to send such a patient to see a doctor and persuade him to therapy.
Our doctors
Valeria Lastovkina
Psychiatrist
Experience 4 years
Make an appointment
Gravolatova Elena Nikolaevna
Psychiatrist, Candidate of Medical Sciences
Great Boles 32 years
Sign up for an appointment
Bogdanova Natalia Ivanovna
Psychiatrist,
Years 20000
Psychiatrist, doctor of the highest category
Experience 26 years
Make an appointment0003
Experience 47 years
Make an appointment
Symptoms and signs of the disease
In addition to the above signs, there are several characteristic symptoms that unite almost all manic states:
- Tendency to thoughtlessly waste money.
- Tendency to unprofitable transactions, gambling.
- Frequent violation of the law.
- Tendency to provoke fights and conflicts.
- Excessive consumption of alcohol or addiction to other bad habits.
- Promiscuous sexual behavior.
- Pathological sociability - the patient often meets strange, suspicious personalities and spends time in a variety of companies.
If these signs get out of hand, seek medical attention. It is important to understand that such behavior is not promiscuity, but symptoms of a disease that needs to be treated. Appeal to common sense is useless.
In some cases, the patient has a specific mania - for example, a mania for a specific purpose. Then the patient is sincerely confident in his special mission and tries to fulfill it with all his might, despite the skepticism of those around him.
Varieties of manic states
There are several classifications according to the manifestations of mania and according to their content.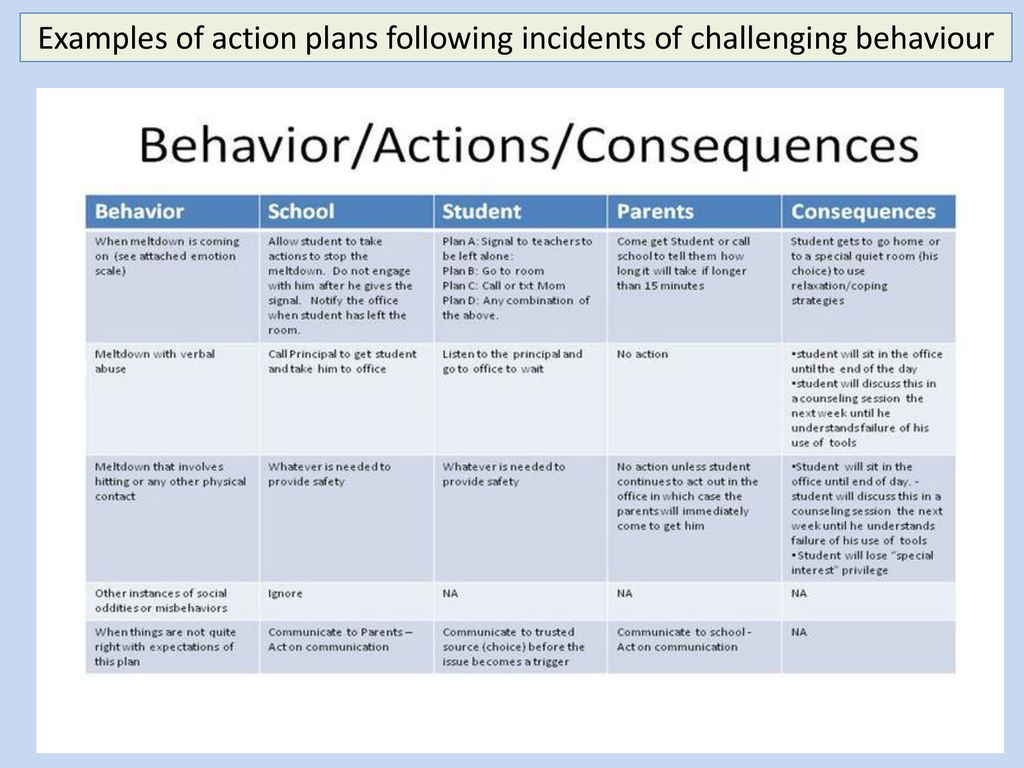
According to the content, the following types are distinguished:
- Mania of persecution - accompanied by paranoia. The patient is convinced that he is being persecuted, anyone can act as a persecutor - from relatives and friends to special services.
- Mania for a special purpose - the patient is sure that he needs to create a new religion, make a scientific discovery, save humanity.
- Megalomania - similar to the previous one. The main difference is that the patient does not have a goal, he simply considers himself the chosen one - the most intelligent, beautiful, rich.
- Mania of guilt, politeness, self-destruction, nihilistic - more rare situations. In patients prone to alcohol abuse, jealousy mania is often noted.
According to the emotional state, manic syndrome can be:
- Joyful mania - excitement, unreasonably elevated mood.
- Angry - irascibility, tendency to create conflict situations.
- Paranoid - manifested by paranoia of persecution, paranoia of relationships.
- Oneiroid - accompanied by hallucinations.
- Manic-depressive syndrome is characterized by alternating mania and depression.
In manic-depressive disorder, intervals may alternate at equal intervals, or one type of behavior predominates. Sometimes the next phase may not come for years.
Treatment of manic states
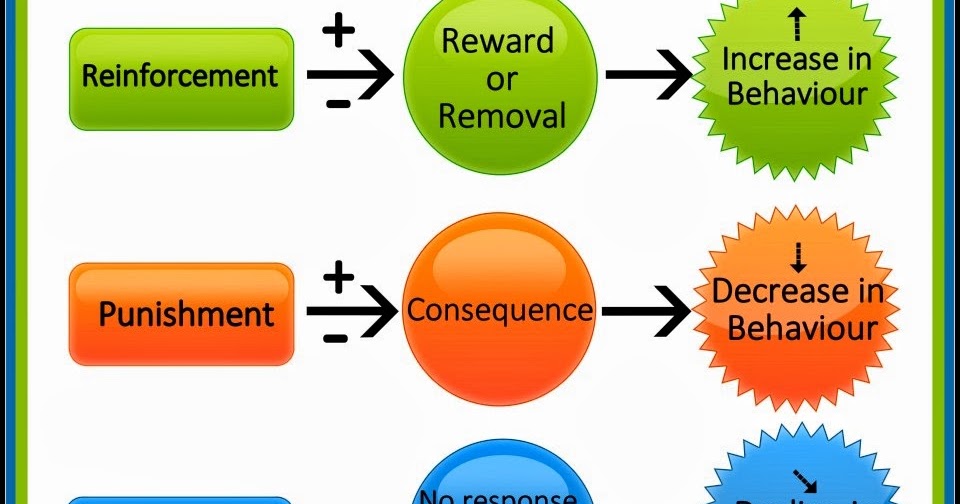
Diagnosed mania is a condition that requires mandatory treatment. It is customary to carry out complex therapy: pharmacological and psychotherapeutic. Pharmaceutical preparations are selected to relieve symptoms: for example, a patient with increased excitability will receive a prescription for sedatives, antipsychotics help to relieve concomitant symptoms, and to prevent the development of the next phase - normotimics.
With regard to psychotherapeutic treatment, usually work with a specialist goes in the direction of cognitive and cognitive-behavioral therapy, as well as psychoeducation (targeted informing the patient about the disease and learning to recognize early signs (“markers”) of the phase change and respond quickly to them in order to prevent the development of the next full-fledged depression or mania). In the course of psychotherapy, one can find and eliminate the cause of the disease, correct the behavior and way of thinking of the patient. On average, treatment takes about a year, but after improvement, dynamic monitoring is required, since the manic syndrome can recur.
In the course of psychotherapy, one can find and eliminate the cause of the disease, correct the behavior and way of thinking of the patient. On average, treatment takes about a year, but after improvement, dynamic monitoring is required, since the manic syndrome can recur.
If the patient is in serious condition, hospitalization is recommended. Usually it is prescribed in order to protect others and the patient himself.
Regardless of the patient's condition, it is important to start treatment as soon as symptoms appear. Psychotherapists of the CELT clinic also work with manic states. Thanks to their serious experience and high qualifications, they will help restore mental health.
Manic disorders
Classification of manic episodes according to severity includes hypomania, mania without psychotic episodes, and mania with psychotic episodes.
Under hypomania understand a mild degree of mania, in which changes in mood and behavior are long-term and pronounced, not accompanied by delusions and hallucinations. An elated mood manifests itself in the sphere of emotions as a joyful cloudlessness, irritability, in the sphere of speech - as increased talkativeness with ease and superficial judgments, increased contact. In the field of behavior, there is an increase in appetite, sexuality, distractibility, a decrease in the need for sleep, and individual actions that go beyond morality. Ease of associations, increase in working capacity and creative productivity are subjectively felt. Objectively, the number of social contacts and success increase. At the same time, there are episodes of reckless or irresponsible behavior, increased sociability or familiarity.
An elated mood manifests itself in the sphere of emotions as a joyful cloudlessness, irritability, in the sphere of speech - as increased talkativeness with ease and superficial judgments, increased contact. In the field of behavior, there is an increase in appetite, sexuality, distractibility, a decrease in the need for sleep, and individual actions that go beyond morality. Ease of associations, increase in working capacity and creative productivity are subjectively felt. Objectively, the number of social contacts and success increase. At the same time, there are episodes of reckless or irresponsible behavior, increased sociability or familiarity.
The main criterion for diagnosis is an elevated or irritable mood that is abnormal for the individual, persists for at least several days, and is accompanied by the above symptoms.
It should be noted that hypomanic episodes are possible in some somatic and psychiatric disorders. For example, with hyperthyroidism, anorexia or therapeutic starvation in the phase of food arousal; with intoxication with certain psychoactive substances - PAS (amphetamines, alcohol, marijuana, cocaine), however, there are other manifestations of somatic and mental pathology and PAS intoxication.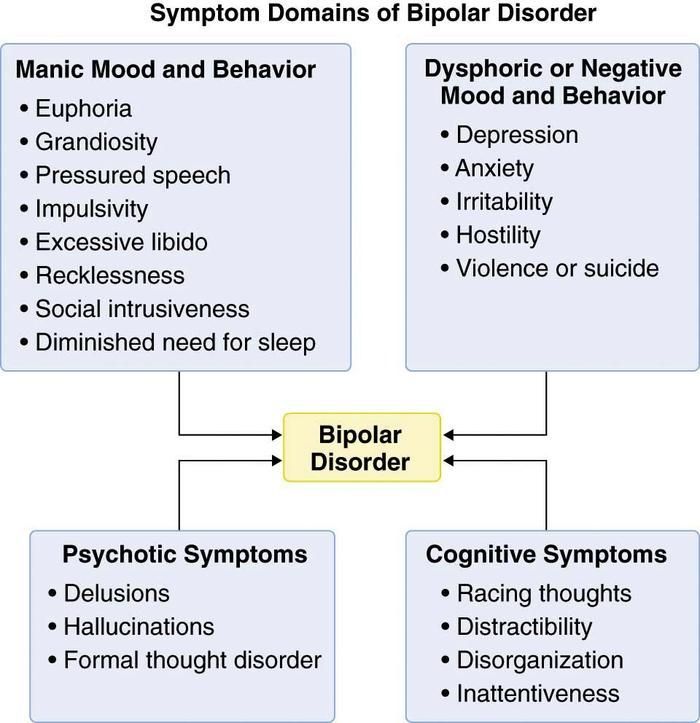
In a typical form , an extended manic state is manifested by the so-called manic triad: a painfully elevated mood, an accelerated flow of thoughts, and motor excitation. The leading sign of a manic state is a manic affect, manifested in an elevated mood, a feeling of happiness, contentment, well-being, an influx of pleasant memories and associations. It is characterized by an aggravation of sensations and perceptions, an increase in mechanical and some weakening of logical memory, superficial thinking, lightness and unproductiveness of judgments and conclusions, ideas of reassessment of one's own personality , up to delusional ideas of greatness, disinhibition of inclinations and weakening of higher feelings, instability, ease of switching attention.
Mania without psychotic symptoms. The main difference from hypomania is that elevated mood affects the change in the norms of social functioning, manifests itself in inadequate actions that are not controlled by the patient.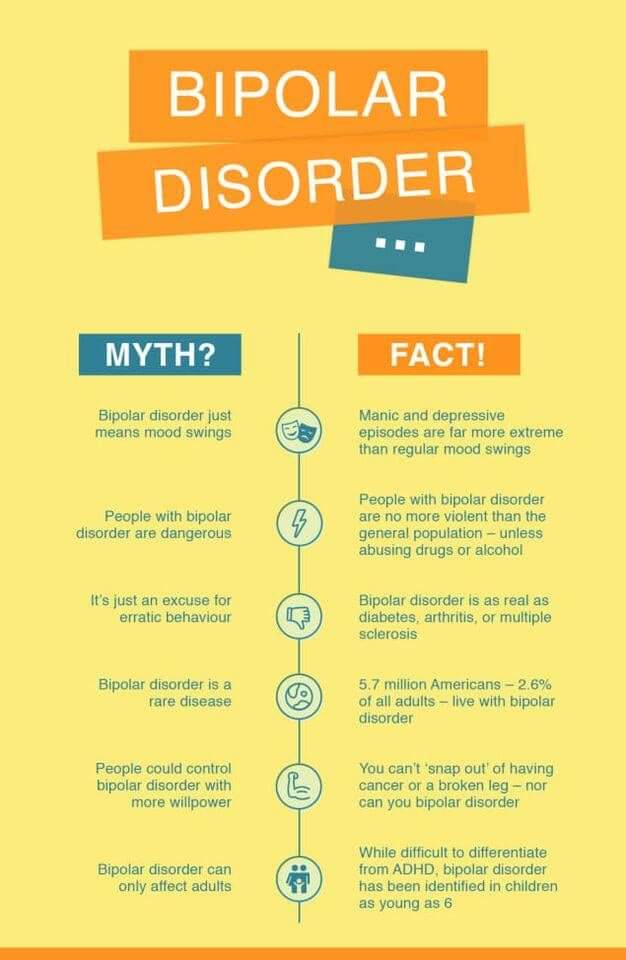 The pace of the passage of time accelerates and the need for sleep is significantly reduced. Tolerance and need for alcohol increase, sexual energy and appetite increase, there is a craving for travel and adventure. Thanks to the leap of ideas, many plans arise, the implementation of which is not carried out. The patient strives for bright and flashy clothes, speaks in a loud voice, incurs a lot of debt and gives money to people he hardly knows. He easily falls in love and is sure of the love of the whole world for himself. Gathering a lot of random people, he arranges holidays on credit. There is reckless driving, a marked increase in sexual energy, or sexual promiscuity. There are no hallucinations or delusions, although there may be perceptual disturbances (eg, subjective hyperacusis, vivid color perception).
The pace of the passage of time accelerates and the need for sleep is significantly reduced. Tolerance and need for alcohol increase, sexual energy and appetite increase, there is a craving for travel and adventure. Thanks to the leap of ideas, many plans arise, the implementation of which is not carried out. The patient strives for bright and flashy clothes, speaks in a loud voice, incurs a lot of debt and gives money to people he hardly knows. He easily falls in love and is sure of the love of the whole world for himself. Gathering a lot of random people, he arranges holidays on credit. There is reckless driving, a marked increase in sexual energy, or sexual promiscuity. There are no hallucinations or delusions, although there may be perceptual disturbances (eg, subjective hyperacusis, vivid color perception).
The main symptom is an elevated, expansive, irritable (angry) or suspicious mood, which is not characteristic of this individual. The change in mood should be distinct and persist throughout the week.
Mania with psychotic symptoms. It is a pronounced mania with a bright jump of ideas and manic excitement, to which secondary crazy ideas of greatness, high origin, hypereroticity, value join. There may be hallucinatory hails confirming the significance of the person, or "voices" telling the patient about emotionally neutral things, or delusions of meaning and persecution. The greatest difficulty lies in the differential diagnosis with schizoaffective disorders, however, with these disorders, there should be symptoms characteristic of schizophrenia, and delusions with them are less consistent with mood. However, the diagnosis can be considered as the starting point for the assessment of schizoaffective disorder (first episode).
Mental disorder formerly referred to as manic-depressive psychosis (MDP). It is characterized by repeated (at least two) manic, depressive and mixed episodes that alternate without a definite sequence. A feature of this psychosis is the presence of light interphase gaps (intermissions), in which all signs of the disease disappear, a complete restoration of a critical attitude to the transferred painful condition is observed, premorbid characterological and personal properties, professional knowledge and skills are preserved.