What is maoi in medicine
Monoamine Oxidase Inhibitors (MAOI) - StatPearls
Tahrier Sub Laban; Abdolreza Saadabadi.
Author Information
Last Update: July 19, 2022.
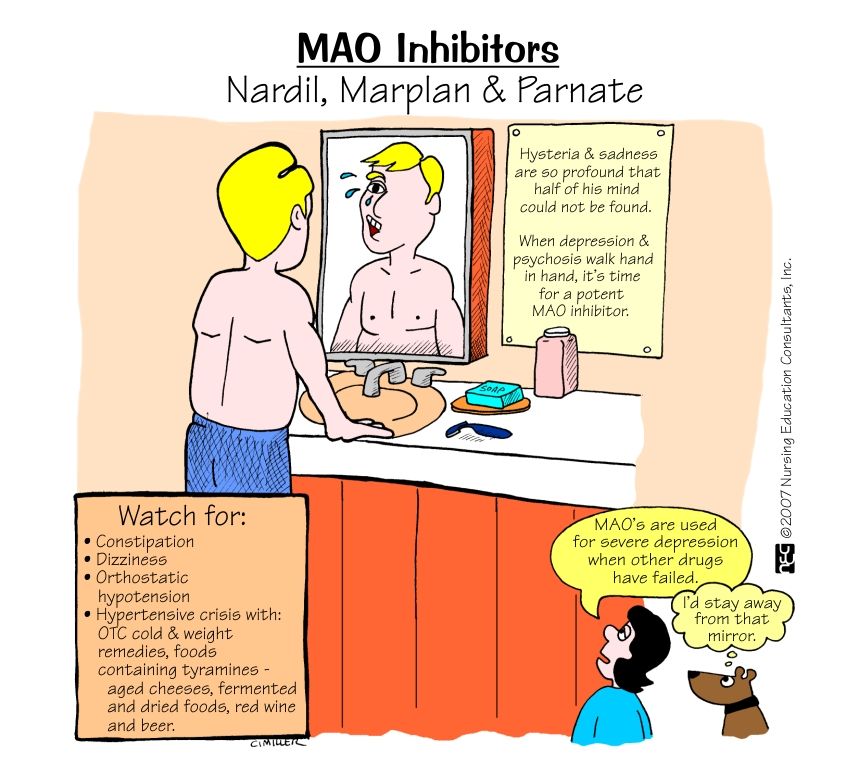
Continuing Education Activity
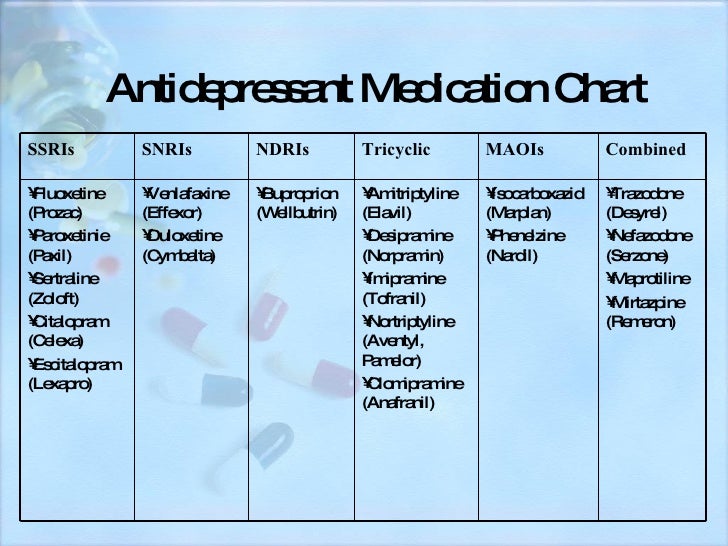
Monoamine oxidase inhibitors (MAOIs) are a separate class from other antidepressants, treating different forms of depression and other nervous system disorders such as panic disorder, social phobia, and depression with atypical features. Even though MAOIs were the first antidepressants introduced, they are not the first choice in treating mental health disorders due to several dietary restrictions, side effects, and safety concerns. MAOIs are only a treatment option when all other medications are unsuccessful. This activity will highlight the mechanism of action, adverse event profile, pharmacology, monitoring, and relevant interactions of MAOIs, pertinent for members of the interprofessional team in treating patients with conditions where this drug class has a therapeutic purpose.
Objectives:
Summarize the mechanisms of actions of the MAOI class of drugs.
Identify the approved and off-label indications for MAOI therapy.
Review the adverse event profile of MAOIs.
Outline the importance of collaboration and communication among interprofessional team members to improve outcomes and treatment efficacy for patients who might benefit from MAOI therapy.
Access free multiple choice questions on this topic.
Indications
Monoamine oxidase inhibitors (MAOIs) were first introduced in the 1950s.[1][2] They are a separate class from other antidepressants, treating different forms of depression as well as other nervous system disorders such as panic disorder, social phobia, and depression with atypical features.[3] Examples of atypical features are oversleeping and overeating. Even though MAOIs were the first antidepressants introduced, they are not the first choice in treating mental health disorders due to several dietary restrictions, side effects, and safety concerns.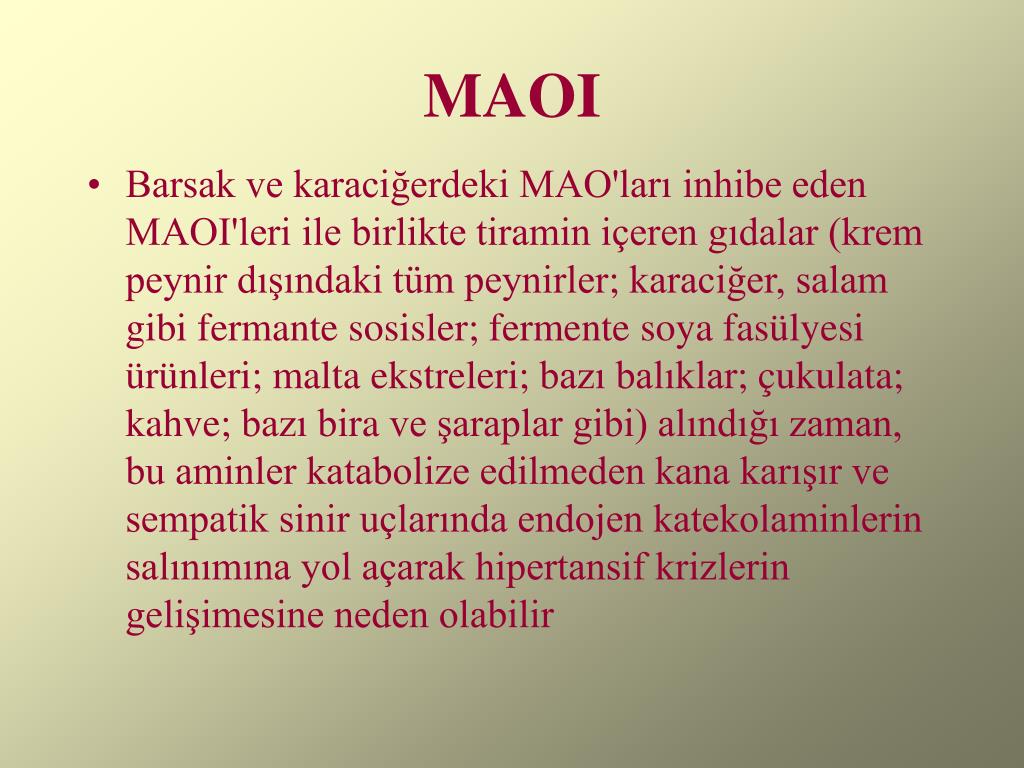 MAOIs are only a treatment option when all other medications are unsuccessful.
MAOIs are only a treatment option when all other medications are unsuccessful.
Furthermore, examples of neurological disorders that can benefit from MAOIs are patients with Parkinson disease and those diagnosed with multiple system atrophy.[4][5] Multiple system atrophy is a neurodegenerative disease that includes symptoms affecting movement as well as blood pressure.
Mechanism of Action
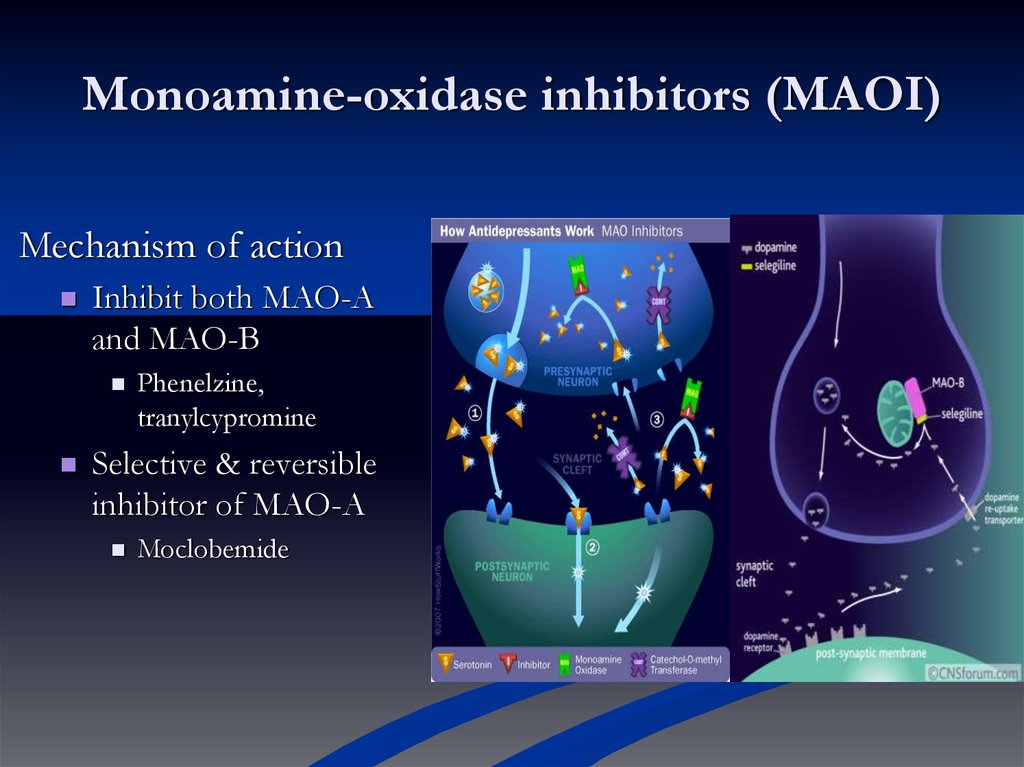
Monoamine oxidase inhibitors are responsible for blocking the monoamine oxidase enzyme. The monoamine oxidase enzyme breaks down different types of neurotransmitters from the brain: norepinephrine, serotonin, dopamine, and tyramine. MAOIs inhibit the breakdown of these neurotransmitters thus, increasing their levels and allowing them to continue to influence the cells that have been affected by depression.[6]
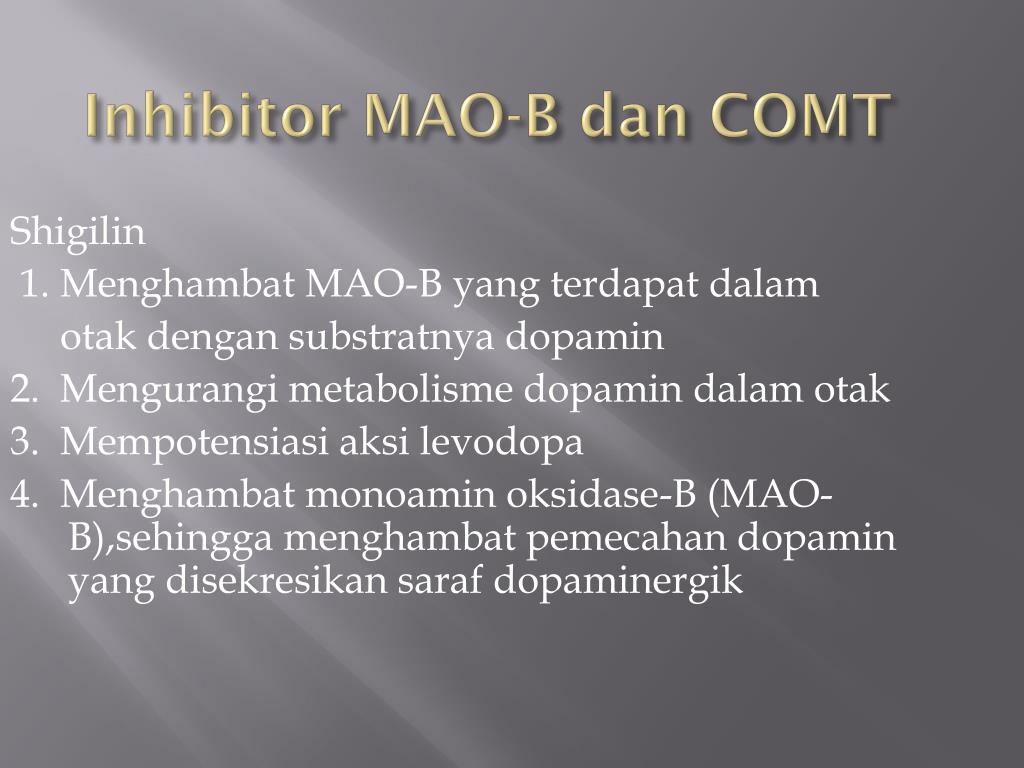
There are two types of monoamine oxidase, A and B. The MAO A is mostly distributed in the placenta, gut, and liver, but MAO B is present in the brain, liver, and platelets.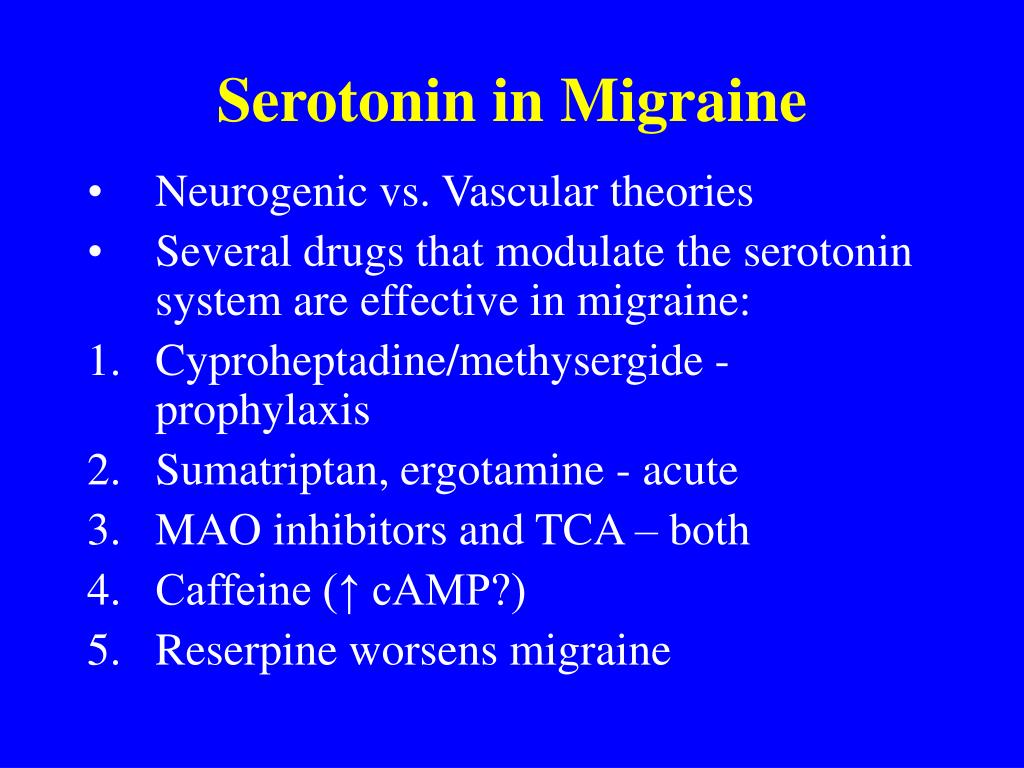 Serotonin and noradrenaline are substrates of MAO A, but phenylethylamine, methylhistamine, and tryptamine are substrates of MAO B. Dopamine and tyramine are metabolized by both MAO A and B. Selegiline and rasagiline are irreversible and selective inhibitors of MAO type B, but safinamide is a reversible and selective MAO B inhibitor.[7]
Serotonin and noradrenaline are substrates of MAO A, but phenylethylamine, methylhistamine, and tryptamine are substrates of MAO B. Dopamine and tyramine are metabolized by both MAO A and B. Selegiline and rasagiline are irreversible and selective inhibitors of MAO type B, but safinamide is a reversible and selective MAO B inhibitor.[7]
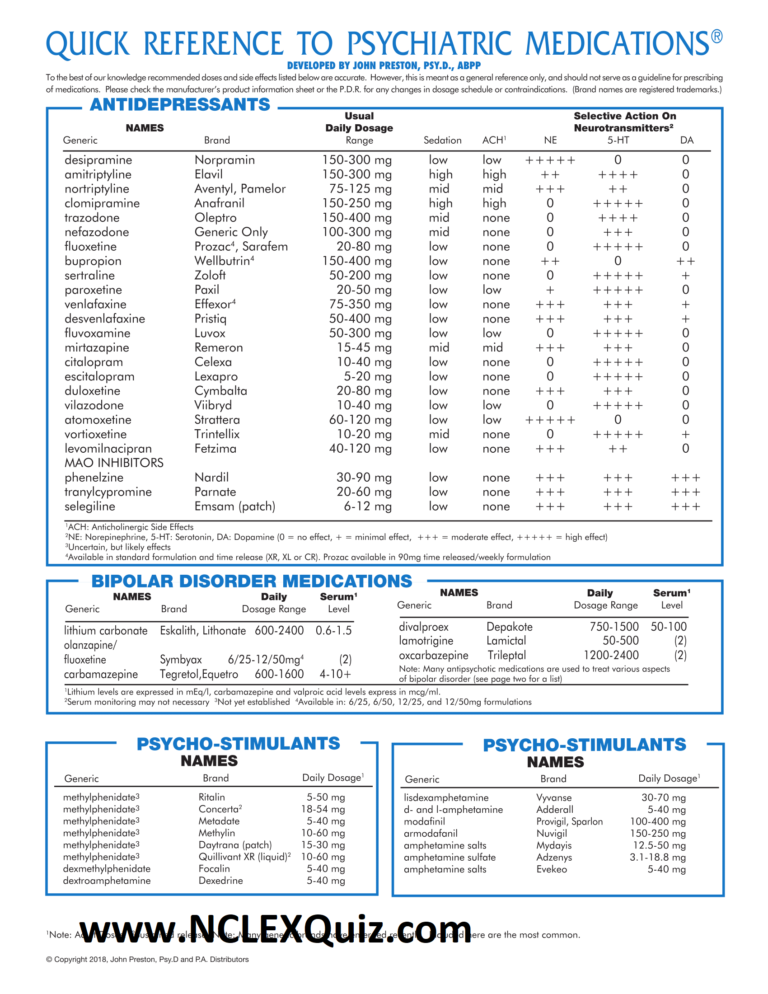
MAOIs are reversible or irreversible. Moclobemide is an example of a reversible MAOI I (RIMA), tranylcypromine, phenelzine, isocarboxazid, and selegiline irreversibly inhibit MAO. Selegiline in low doses is a selective, irreversible MAO B inhibitor, but it is no longer selective at higher doses.[8]
Administration
MAOI administration is almost always orally but sometimes comes in the form of a skin patch.[1] The skin patches were FDA approved and can be more beneficial to patients than oral dose forms. An example of this is selegiline, which can be given in a skin patch and causes fewer side effects than oral administration.[1] Patients with lower doses of MAOIs may not have to be as strict with their diet as those with higher doses.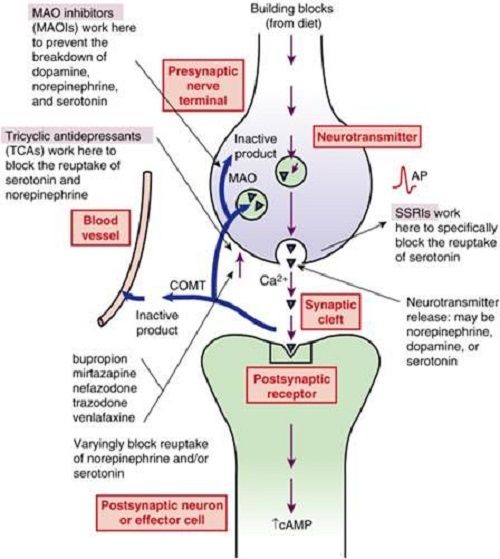
The different types of MAOIs approved by the FDA include isocarboxazid, phenelzine, selegiline, and tranylcypromine.[9] When patients are prescribed antidepressants like MAOIs, they must be aware of the time it takes to start experiencing the therapeutic effects of the drug. Usually, the medication starts to become effective within two to three weeks. However, patients should take the antidepressant for at least six months for the maximal therapeutic benefit. Patients who take an antidepressant for less than six months are shown to have a high symptomatic relapse rate.
Adverse Effects
The most frequently encountered side effects are dry mouth, nausea, diarrhea, constipation, drowsiness, insomnia, dizziness, and/or lightheadedness. Furthermore, if applied via patch, a skin reaction may occur at the patch site.[9] Recommendations are that any patient scheduled for an elective surgery that requires general anesthesia should not take MAOIs for at least ten days before the surgery to avoid any drug interaction.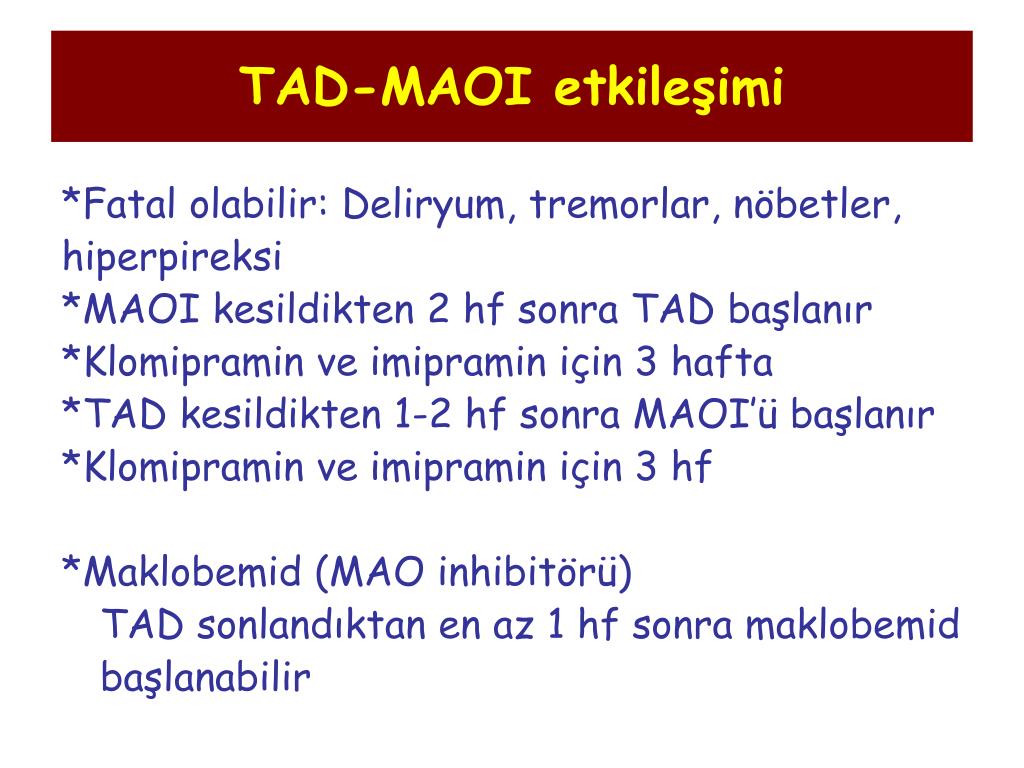 [10][11]
[10][11]
Contraindications
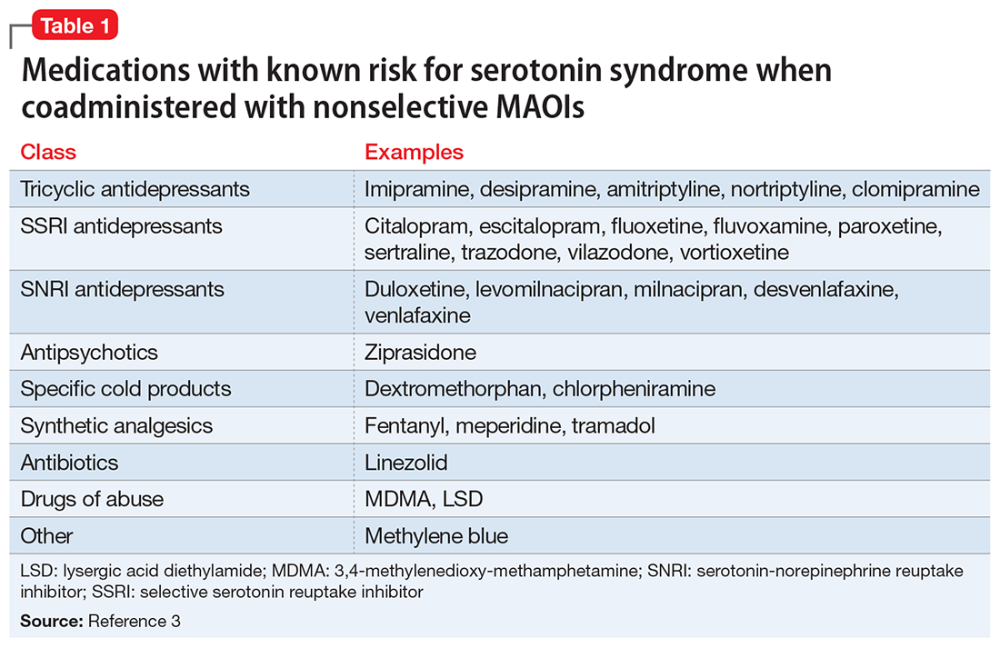
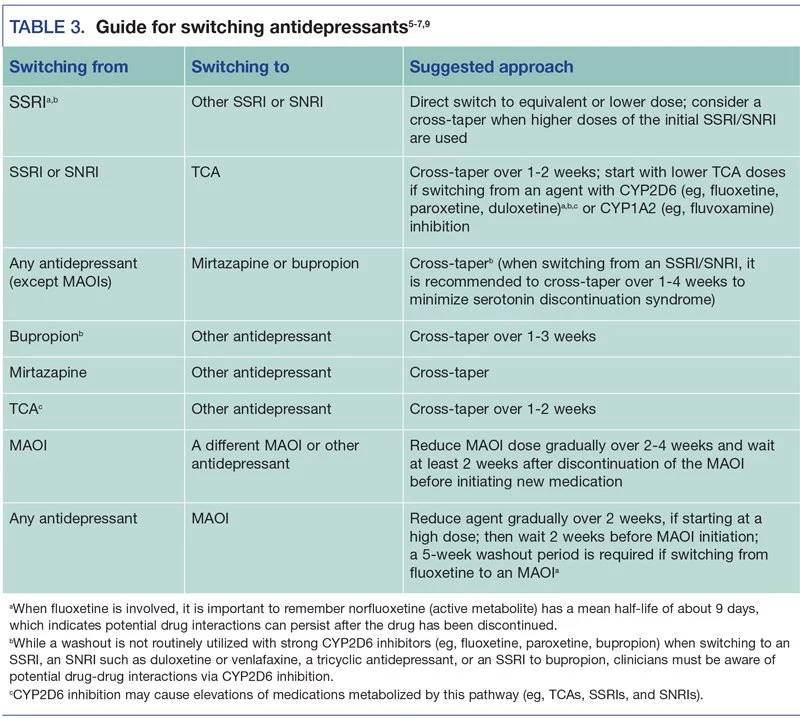
MAOIs can potentially cause drug-to-drug interactions, drug-food interaction, and overdoses, of which the patient should be aware.[9] For example, patients should not be mixing MAOIs with other antidepressants like selective serotonin reuptake inhibitors (SSRIs).[12] These two drugs combined can cause serotonin syndrome, which is potentially fatal. The first cases of serotonin syndrome were reported during the 1960s when patients were on MAOIs and tryptophan. Patients showed signs and symptoms of fever, confusion, increased perspiration, muscle rigidity, seizures, liver or kidney problems, fluctuation of heart rhythms, and blood pressure. Furthermore, when changing MAOIs to another antidepressant, patients should give themselves 14 days to pass before initiating the new treatment, to prevent any drug interaction.
MAOIs prevent the breakdown of tyramine found in the body and certain foods, drinks, and other medications. Patients that take MAOIs and consume tyramine-containing foods or drinks will exhibit high serum tyramine level.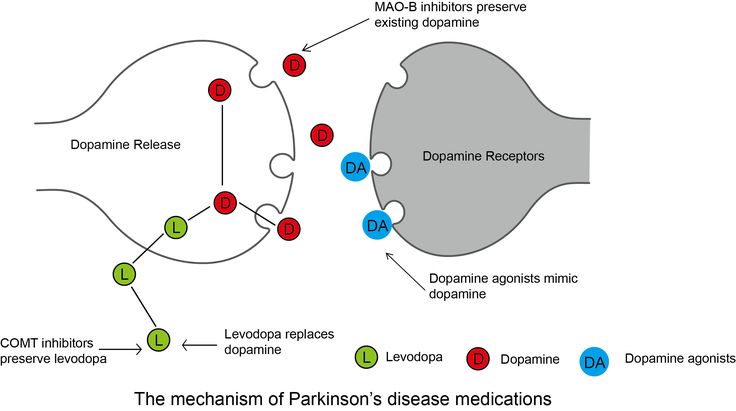 [13][14] A high level of tyramine can cause a sudden increase in blood pressure, called the tyramine pressor response.[14] Even though it is rare, a high tyramine level can trigger a cerebral hemorrhage, which can even result in death.
[13][14] A high level of tyramine can cause a sudden increase in blood pressure, called the tyramine pressor response.[14] Even though it is rare, a high tyramine level can trigger a cerebral hemorrhage, which can even result in death.
Eating foods with high tyramine can trigger a reaction that can have serious consequences.[14] Patients should know that tyramine can increase with the aging of food; they should be encouraged to have fresh foods instead of leftovers or food prepared hours earlier. Examples of high levels of tyramine in food are types of fish and types of meat, including sausage, turkey, liver, and salami.[15][16] Also, certain fruits can contain tyramine, like overripe fruits, avocados, bananas, raisins, or figs. Further examples are cheeses, alcohol, and fava beans; all of these should be avoided even after two weeks of stopping MAOIs.[16] Anyone taking MAOIs is at risk for an adverse hypertensive reaction, with accompanying morbidity.
Tramadol, meperidine, dextromethorphan, and methadone are contraindicated in patients on MAOIs as they are at high risk for causing serotonin syndrome.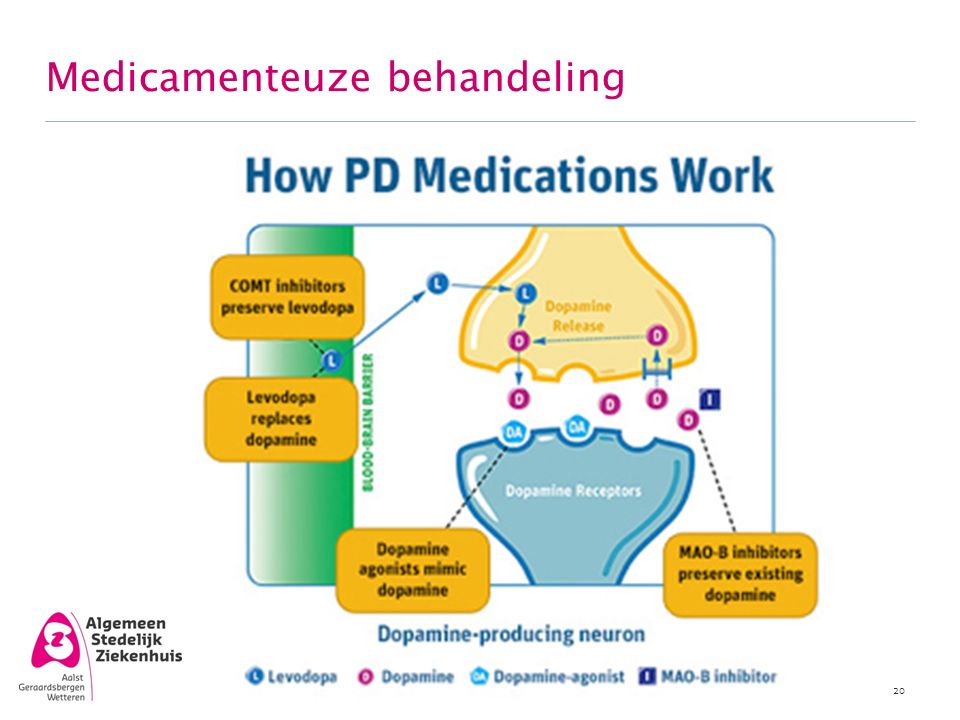 [8]
[8]
In general, SSRIs, SNRIs, TCAs, bupropion, mirtazapine, St. John's Wort and, sympathomimetic amines, including stimulants, are contraindicated with MAOIs.[8]
Monitoring
Even though MAOIs are no longer a first-line treatment option, they are still in use, and it is essential to note the precautions when initiating treatment.[12] Patients should be encouraged by health providers to carry identification cards or wear a wristband.[9] Patients always need to notify every doctor they encounter, whether dental or medical, to avoid any health consequences, especially due to the medications' influence on the vasculature.
Toxicity
Patients taking MAOIs can overdose and may show similar side effects, as stated above, except with more severe presentation.[17] Anyone on MAOIs may experience symptoms slowly within the first 24 to 48 hours. However, symptoms can be nonspecific, which range from mild to severe to even life-threatening. Depending on the MAOI prescribed, some can cause patients to go into a coma, and others (e. g., overdosing on tranylcypromine) can result in death.[9] The severity depends on the amount consumed and the type of MAOIs the patient took. For example, phenelzine and tranylcypromine being nonselective and nonreversible, increase the risk of a patient experiencing a hypertensive crisis when ingested with tyramine. However, selegiline is a selective MAO-B inhibitor with less hypertensive risk.[4] Any patient experiencing any of the following: agitation, flushing, tachycardia, hypotension or hypertension, palpations, twitching, increased deep tendon reflexes, seizures, or high fevers should immediately report to a health provider.[9]
g., overdosing on tranylcypromine) can result in death.[9] The severity depends on the amount consumed and the type of MAOIs the patient took. For example, phenelzine and tranylcypromine being nonselective and nonreversible, increase the risk of a patient experiencing a hypertensive crisis when ingested with tyramine. However, selegiline is a selective MAO-B inhibitor with less hypertensive risk.[4] Any patient experiencing any of the following: agitation, flushing, tachycardia, hypotension or hypertension, palpations, twitching, increased deep tendon reflexes, seizures, or high fevers should immediately report to a health provider.[9]
Enhancing Healthcare Team Outcomes
Safety and optimal treatment are vital to patient health. Patients with a history of seizures or epilepsy should avoid MAOIs; these medications can increase the occurrence of seizures. Also, people with a history of alcoholism, angina, severe headaches, blood vessel disease, diabetes, kidney or liver disease, history of a recent heart attack or stroke, overactive thyroid, and pheochromocytoma should not receive MAOI therapy; since this may cause a hypertensive crisis. [2] This caution is also necessary for patients with a family history of depression, any neurological disorders, or even if any family members have attempted suicide. Due to the high risks, patients must provide a complete family history. Educating the patient on the importance of possible risks and side effects of the drug is critical for their well-being. It provides them an opportunity for a better outcome.
[2] This caution is also necessary for patients with a family history of depression, any neurological disorders, or even if any family members have attempted suicide. Due to the high risks, patients must provide a complete family history. Educating the patient on the importance of possible risks and side effects of the drug is critical for their well-being. It provides them an opportunity for a better outcome.
Ads with other illnesses, depression, and other psychiatric treatment plans pose multiple dilemmas for physicians.[17] These patients may need to try various medication regimens before achieving effective treatment. Someone experiencing depression or panic attacks may have significant life changes, and usually, the family physician is aware of these changes. While a psychiatric physician is almost always involved with patients dealing with different types of mental health issues, it is important to consult with an interprofessional group specialist that includes a family physician, internal medicine, specialty-trained mental health nurse, neurologist, and pharmacist.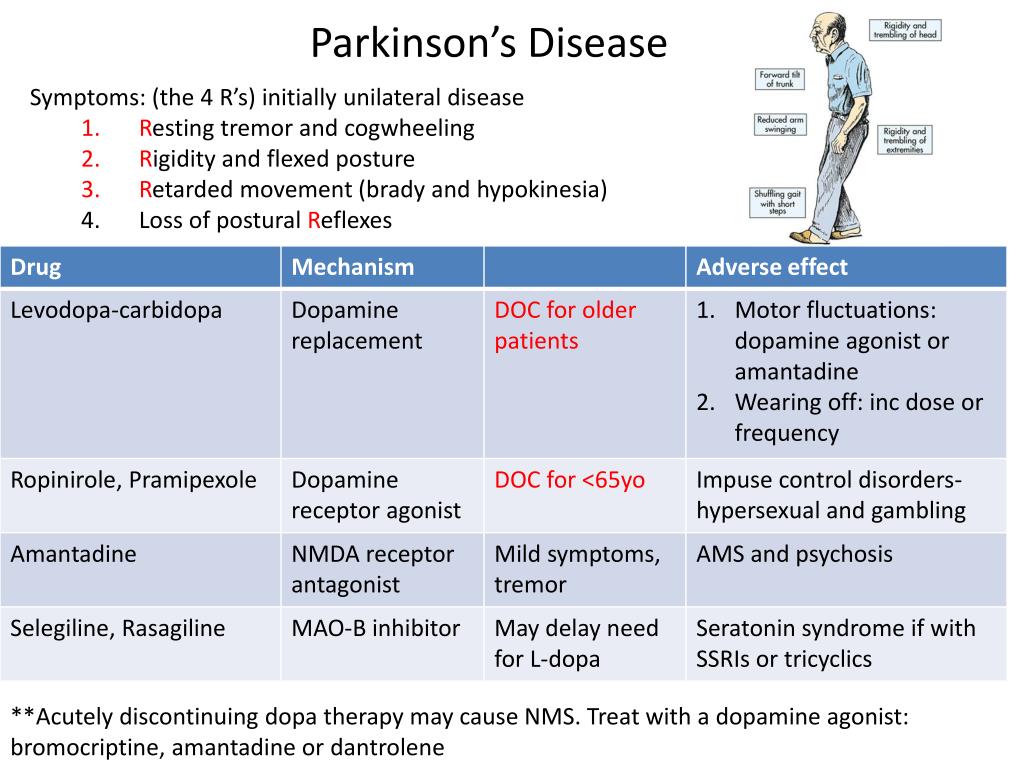 [18] Also, all other health providers involved in the patient's care are vital members of the interprofessional team, for example, other nurses and social workers. Each member provides an essential element to the patient's treatment plan. Evidence has shown that promoting interprofessional communication by consulting specialists can improve the outcome of a patient's health and their adherence to the plan.[19] [Level 5]
[18] Also, all other health providers involved in the patient's care are vital members of the interprofessional team, for example, other nurses and social workers. Each member provides an essential element to the patient's treatment plan. Evidence has shown that promoting interprofessional communication by consulting specialists can improve the outcome of a patient's health and their adherence to the plan.[19] [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Culpepper L. Reducing the Burden of Difficult-to-Treat Major Depressive Disorder: Revisiting Monoamine Oxidase Inhibitor Therapy. Prim Care Companion CNS Disord. 2013;15(5) [PMC free article: PMC3907330] [PubMed: 24511450]
- 2.
Rapaport MH. Dietary restrictions and drug interactions with monoamine oxidase inhibitors: the state of the art. J Clin Psychiatry. 2007;68 Suppl 8:42-6.
 [PubMed: 17640157]
[PubMed: 17640157]- 3.
Thase ME. MAOIs and depression treatment guidelines. J Clin Psychiatry. 2012 Jul;73(7):e24. [PubMed: 22901357]
- 4.
Volz HP, Gleiter CH. Monoamine oxidase inhibitors. A perspective on their use in the elderly. Drugs Aging. 1998 Nov;13(5):341-55. [PubMed: 9829163]
- 5.
McFarland NR. Diagnostic Approach to Atypical Parkinsonian Syndromes. Continuum (Minneap Minn). 2016 Aug;22(4 Movement Disorders):1117-42. [PMC free article: PMC5567217] [PubMed: 27495201]
- 6.
Baker GB, Coutts RT, McKenna KF, Sherry-McKenna RL. Insights into the mechanisms of action of the MAO inhibitors phenelzine and tranylcypromine: a review. J Psychiatry Neurosci. 1992 Nov;17(5):206-14. [PMC free article: PMC1188458] [PubMed: 1362653]
- 7.
Müller T, Riederer P, Grünblatt E. Determination of Monoamine Oxidase A and B Activity in Long-Term Treated Patients With Parkinson Disease. Clin Neuropharmacol.
 2017 Sep/Oct;40(5):208-211. [PubMed: 28682929]
2017 Sep/Oct;40(5):208-211. [PubMed: 28682929]- 8.
Thomas SJ, Shin M, McInnis MG, Bostwick JR. Combination therapy with monoamine oxidase inhibitors and other antidepressants or stimulants: strategies for the management of treatment-resistant depression. Pharmacotherapy. 2015 Apr;35(4):433-49. [PubMed: 25884531]
- 9.
Fiedorowicz JG, Swartz KL. The role of monoamine oxidase inhibitors in current psychiatric practice. J Psychiatr Pract. 2004 Jul;10(4):239-48. [PMC free article: PMC2075358] [PubMed: 15552546]
- 10.
Saraghi M, Golden LR, Hersh EV. Anesthetic Considerations for Patients on Antidepressant Therapy-Part I. Anesth Prog. 2017 Winter;64(4):253-261. [PMC free article: PMC5715313] [PubMed: 29200376]
- 11.
Saraghi M, Golden L, Hersh EV. Anesthetic Considerations for Patients on Antidepressant Therapy - Part II. Anesth Prog. 2018 Spring;65(1):60-65. [PMC free article: PMC5841487] [PubMed: 29509514]
- 12.
Flockhart DA. Dietary restrictions and drug interactions with monoamine oxidase inhibitors: an update. J Clin Psychiatry. 2012;73 Suppl 1:17-24. [PubMed: 22951238]
- 13.
Brown C, Taniguchi G, Yip K. The monoamine oxidase inhibitor-tyramine interaction. J Clin Pharmacol. 1989 Jun;29(6):529-32. [PubMed: 2666453]
- 14.
Sathyanarayana Rao TS, Yeragani VK. Hypertensive crisis and cheese. Indian J Psychiatry. 2009 Jan;51(1):65-6. [PMC free article: PMC2738414] [PubMed: 19742203]
- 15.
Walker SE, Shulman KI, Tailor SA, Gardner D. Tyramine content of previously restricted foods in monoamine oxidase inhibitor diets. J Clin Psychopharmacol. 1996 Oct;16(5):383-8. [PubMed: 8889911]
- 16.
Sullivan EA, Shulman KI. Diet and monoamine oxidase inhibitors: a re-examination. Can J Psychiatry. 1984 Dec;29(8):707-11. [PubMed: 6394124]
- 17.
Thorp M, Toombs D, Harmon B. Monoamine oxidase inhibitor overdose.
 West J Med. 1997 Apr;166(4):275-7. [PMC free article: PMC1304212] [PubMed: 9168689]
West J Med. 1997 Apr;166(4):275-7. [PMC free article: PMC1304212] [PubMed: 9168689]- 18.
Culpepper L. The use of monoamine oxidase inhibitors in primary care. J Clin Psychiatry. 2012;73 Suppl 1:37-41. [PubMed: 22951241]
- 19.
Agius M, Murphy CL, Zaman R. Does shared care help in the treatment of depression? Psychiatr Danub. 2010 Nov;22 Suppl 1:S18-22. [PubMed: 21057395]
Types, Side Effects, and More
Understanding MAO Inhibitors: Types, Side Effects, and MoreMedically reviewed by Alan Carter, Pharm.D. — By Brian Krans — Updated on September 29, 2018
What are MAOIs?
Monoamine oxidase inhibitors (MAOIs) are a class of medication used to treat depression. They were introduced in the 1950s as the first drugs for depression. Today, they’re less popular than other depression medications, but some people benefit from their use.
Read on to learn more about MAOIs, including how they work, who they might help, and what foods to avoid while taking them.
MAOIs work with the chemicals in your brain called neurotransmitters that allow brain cells to communicate with each other. Depression is thought to be caused by low levels of the neurotransmitters dopamine, serotonin, and norepinephrine, which collectively are called monoamines. A chemical found naturally in the body, monoamine oxidase, removes these neurotransmitters.
By inhibiting monoamine oxidase, MAOIs allow more of these neurotransmitters to remain in the brain, thus elevating mood through improved brain cell communication.
Monoamine oxidase is a type of enzyme that helps neurons fire throughout your body. It’s formed in your liver and cleans up neurotransmitters in your brain once they’ve done their jobs.
Besides neurotransmitters, monoamine oxidase cleans out tyramine, a chemical that helps regulate blood pressure. Because MAOIs inhibit monoamine oxidase from doing its job, they adversely affect blood pressure in addition to keeping neurotransmitters at optimal levels.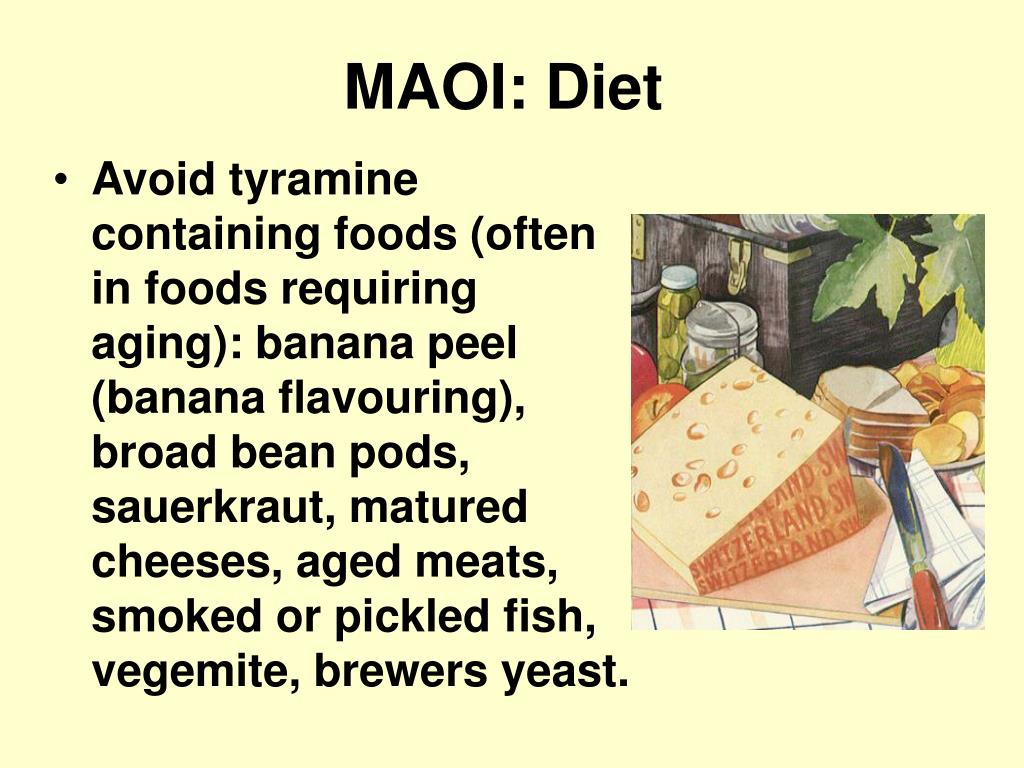 People taking MAOIs have to pay special attention to their blood pressure, including avoiding certain foods.
People taking MAOIs have to pay special attention to their blood pressure, including avoiding certain foods.
One downside to MAOIs is that they come with dietary restrictions because of the elevated tyramine levels in the blood.
When this class of drug first entered the market, no one knew about the concerns over tyramine and blood pressure. This caused a wave of deaths that prompted further research. Now we know that certain foods contain excess tyramine, and these should be avoided when taking MAOIs.
The more food ages, the more concentrated the levels of tyramine become. This is true for aged meats, cheeses, and even leftovers in your fridge. Foods with dangerously high levels of tyramine include:
- soy sauce and other fermented soy products
- sauerkraut
- salami and other aged or cured meats
Other foods that contain high levels of tyramine are:
- aged cheeses, such as Brie, cheddar, Gouda, Parmesan, Swiss, and blue cheese
- alcohol, especially chianti, vermouth, and beers
- fava beans
- raisins, dates, and other dried fruits
- tofu
- all nuts
Get more information about tyramine-free diets.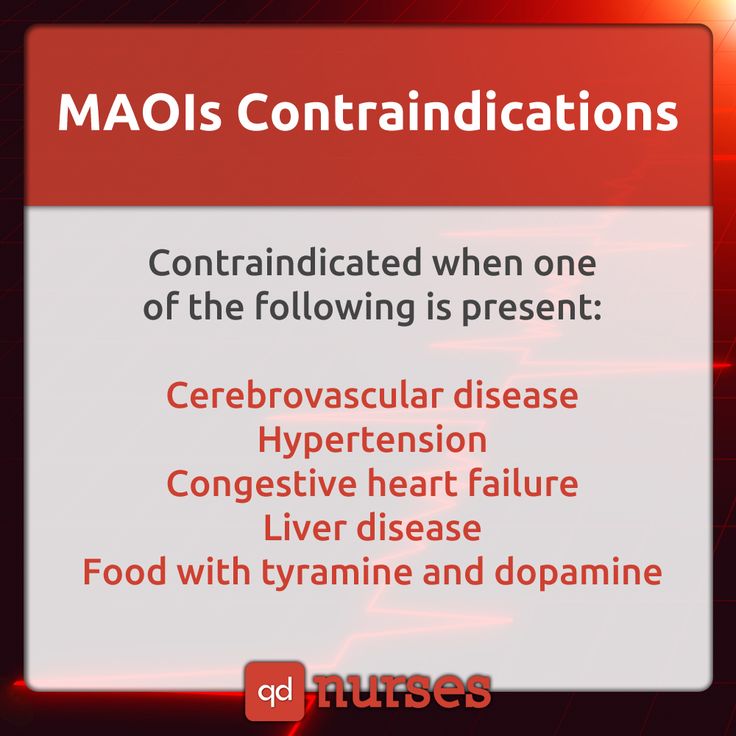
Besides blood pressure problems, people taking MAOIs should also beware of a condition called serotonin syndrome. Symptoms can include:
- confusion
- fever
- irregular or rapid heartbeat
- dilated pupils
- occasional unconsciousness
The condition can manifest if a person on MAOIs takes other antidepressants or the herbal supplement St. John’s wort.
To avoid serotonin syndrome, people taking MAOIs shouldn’t take anything for two weeks when ending MAOI treatment and starting another.
These days, MAOIs are rarely the first choice of prescription medication to treat depression. However, the U.S. Food and Drug Administration (FDA) — the regulating agency of all prescription medication — has approved the following MAOIs:
- isocarboxazid (Marplan): can take three to six weeks to fully take effect
- phenelzine (Nardil): can take up to four weeks to fully work
- tranylcypromine (Parnate): can take up to 3 weeks to achieve its desired effects
Selegiline
Selegiline (Emsam, Atapryl, Carbex, Eldepryl, Zelapar) is a newer type of MAOI. It works by selectively blocking monoamine oxidase B (MAO-B). This reduces the breakdown of dopamine and phenethylamine and means there are no dietary restrictions. It’s available in patch form. Learn about other medications used to treat depression.
It works by selectively blocking monoamine oxidase B (MAO-B). This reduces the breakdown of dopamine and phenethylamine and means there are no dietary restrictions. It’s available in patch form. Learn about other medications used to treat depression.
Aside from depression, selegiline is also prescribed for early onset Parkinson’s disease and dementia.
MAOIs carry more side effects than other antidepressants, which is why they’re often the last drug prescribed to treat depression. Some side effects of MAOIs include:
- fatigue
- muscle aches
- nervousness
- insomnia
- reduced libido
- erectile dysfunction (ED)
- dizziness
- lightheadedness
- diarrhea
- dry mouth
- high blood pressure
- tingling of the skin
- difficulty urinating
- weight gain
The FDA requires a warning on antidepressants that they may increase the risk of suicide in children and young adults. While MAOIs are rarely prescribed for children, all people beginning any kind of antidepressant therapy should be watched for changes in mood, mindset, or attitude.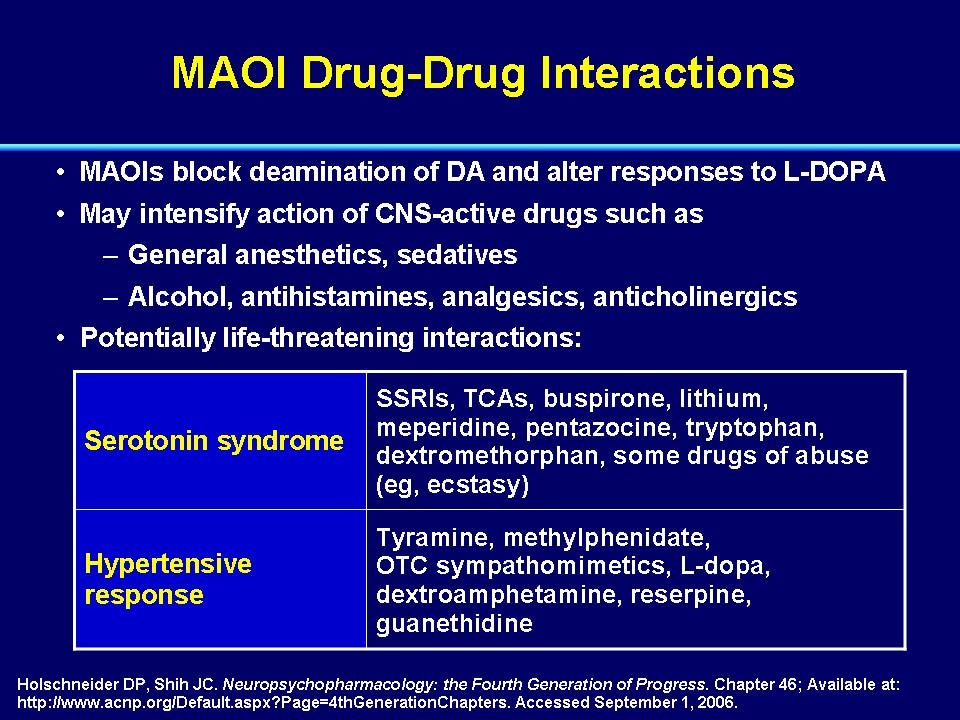 Successful antidepressant treatments should lower suicide risk by increasing mood.
Successful antidepressant treatments should lower suicide risk by increasing mood.
However, you should consult your doctor before you stop taking MAOIs or any other prescribed medication.
MAOIs are only one type of medication used to treat depression. Like most antidepressants, they may not be right for everyone and take weeks of use to reach their full effect. However, when used in combination with other therapies and lifestyle changes, they can be highly effective at combating depression symptoms. Talk to your doctor for more information to see if MAOI therapy suits your lifestyle.
Last medically reviewed on September 5, 2017
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Depression: FDA-approved medications may help.
 (2017).
(2017).
fda.gov/ForConsumers/ConsumerUpdates/ucm095980.htm - Drug approval package: Marplan/isocarboxazid 10 mg tablets. (2005).
accessdata.fda.gov/drugsatfda_docs/nda/98/11961-s017.cfm - Safety concerns with MAOIs. (2016).
mayoclinic.org/diseases-conditions/depression/in-depth/maois/art-20043992?pg=2
Share this article
Medically reviewed by Alan Carter, Pharm.D. — By Brian Krans — Updated on September 29, 2018
Read this next
How Burnout at Work May Be Causing You to Gain Weight
A demanding workload at your job or school can increase your stress level — and your waistline. Here’s how to spot the signs you’re burned out and…
READ MORE
Combination Medication Therapies for Depression
Medically reviewed by Femi Aremu, PharmD
New research is showing that combining antidepressants with medications for other mood disorders can be effective in helping people manage their…
READ MORE
Gym Anxiety: Strategies to Overcome Gymtimidation
Medically reviewed by Danielle Hildreth, RN, CPT
Gym anxiety, or "gymtimidation," is real.
 Here are some strategies to cope.
Here are some strategies to cope.READ MORE
Repetitive Transcranial Magnetic Stimulation
Medically reviewed by Timothy J. Legg, PhD, PsyD
Repetitive transcranial magnetic stimulation (rTMS) is a form of brain stimulation therapy used to treat depression. Learn more about how it works.
READ MORE
Yoga, Running, and Other Workouts Can Combat Depressive Episodes
A new study suggests that an increase in physical activity can help significantly lower the risk of depression among individuals with risk or higher…
READ MORE
What to Know About Ketamine Therapy for Depression
Medically reviewed by Nicole Washington, DO, MPH
Ketamine offers a new, fast-acting approach to relieving treatment-resistant depression. Learn the research-backed benefits and how to try it.
READ MORE
Unipolar Depression Explained — Plus Tips to Get Support
Medically reviewed by Nicole Washington, DO, MPH
Unipolar depression often refers to major depression, also called clinical depression. Learn the signs and how it compares to bipolar disorder.
READ MORE
New Study Debunks Old Theory That Depressed People Are Just More Realistic
New research raises doubts about a decades-old theory that depressed people are more realistic.
READ MORE
Task Force Recommends Depression, Anxiety Screenings for Children
A federal task force is recommending children between the ages of 8 and 18 be screened for anxiety while children 12 to 18 be screened for depression
READ MORE
More People May Experience Seasonal Affective Disorder This Year
Experts theorize that a greater number of people may experience Seasonal Affective Disorder this year.
 Here's how to spot the signs.
Here's how to spot the signs.READ MORE
Monoamine oxidase inhibitors | it's... What are Monoamine Oxidase Inhibitors?
Monoamine oxidase inhibitors (MAOIs, MAOIs) are biologically active substances capable of inhibiting the enzyme monoamine oxidase. Monoamine oxidase inhibitors include some antidepressants, as well as a number of natural substances.
|
Contents
|
IMAO classification
According to their pharmacological properties, monoamine oxidase inhibitors are divided into reversible and irreversible, selective and non-selective.
Selective MAOIs inhibit mainly one of the types of MAO, non-selective - both types.
Irreversible MAOIs interact with monoamine oxidase, forming chemical bonds with it. The enzyme is then unable to perform its functions and is metabolized, and instead the body synthesizes a new one, which usually takes about two weeks.
Reversible MAOIs bind to the active center of the enzyme and form a relatively stable complex with it. This complex gradually dissociates, releasing the MAOI, which then enters the bloodstream and is excreted from the body, leaving the enzyme intact.
Nonselective irreversible MAOIs
- Iproniazid
- Nialamide
- Isocarboxazid
- Phenelzine
- Tranylcypramine
Strictly speaking, it is not entirely correct to attribute tranylcypramine to this group, since it is a reversible inhibitor, however, it may take up to 30 days for its complex to dissociate with the enzyme and be completely eliminated from the body. In addition, it exhibits some selectivity towards MAO-A.
In addition, it exhibits some selectivity towards MAO-A.
Reversible selective MAO inhibitors A
- Moclobemide
- Pyrlindol (Pyrazidol)
- Bethol
- Metrolindole
- Beta-carboline derivatives
Reversible MAOIs do not require a diet.
Irreversible selective MAO B inhibitors
- Selegiline
Pharmacology MAOIs
General information
MAOIs, blocking the destruction of monoamines by monoamine oxidase, increase the content of one or more mediator monoamines (norepinephrine, serotonin, dopamine, phenylethylamine, etc.) in the synaptic cleft and enhance monoaminergic impulses (mediated by monoamine nerve impulses) transmission neurotransmission). For this reason, for medical purposes, these substances are used mainly as antidepressants. MAOI-Bs are also used in the treatment of parkinsonism and narcolepsy.
Interactions with drugs and certain surfactants
The combination of monoamine oxidase inhibitors with substances that affect the metabolism of monoamines can lead to an unpredictable increase in their action and be life-threatening.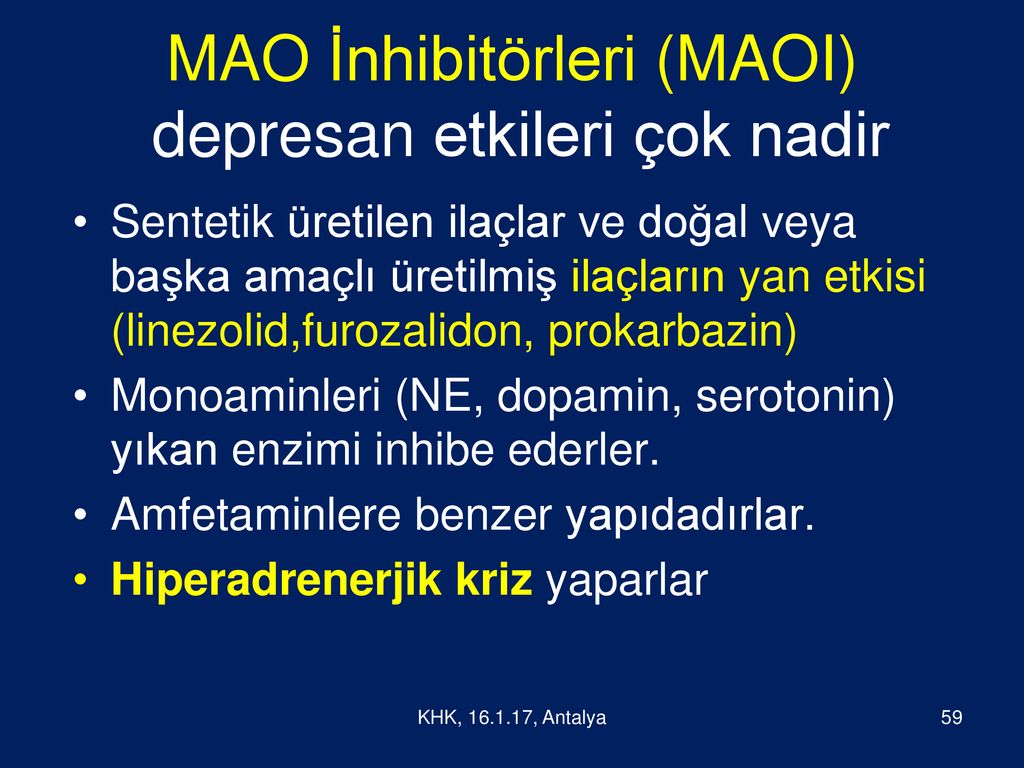
List of drugs to avoid:
- Psychostimulants of the amphetamine group, and related to them - increasing the levels of catecholamines in the synaptic cleft (amphetamine, methamphetamine, sydnocarb, etc.).
- Any entactogens
- Cold remedies containing sympathomimetics (ephedrine, pseudoephedrine, phenylpropanolamine, phenylephrine, chlorpheniramine, oxymetazoline, etc.): coldrex teraflu, rinza, etc., sprays and nasal drops such as naphthyzinum.
- Slimming aids
- Monoamine reuptake inhibitors:
- Cocaine
- Tricyclic antidepressants (amitriptyline, desipramine, imipramine, etc.)
- Serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac)
- Dextromethorphan (DXM)
- Metabolic precursors of monoamines: DOPA, methyldopa, 5-hydroxytryptophan
- Reserpine
- Antihistamines [ source not specified 122 days ]
- Barbiturates [ source not specified 122 days ]
- Anticholinergics [ source not specified 122 days ]
- Pethidine (Demerol) and other opiates (risk of respiratory depression) [ source unspecified 122 days ] .
Foods incompatible with MAOIs
A significant hazard when using MAOIs is the consumption of foods containing various monoamines and their metabolic precursors. First of all, it is tyramine and its metabolic precursor amino acid tyrosine, as well as tryptophan. Tyramine, like amphetamine psychostimulants, causes the release of catecholamines from nerve endings. Its joint intake with MAOIs is fraught with a hypertensive crisis. Tryptophan is used by the body to produce serotonin, and eating foods high in tryptophan can lead to serotonin syndrome.
Foods to avoid:
- Cheeses, especially aged
- Red wine, beer, especially dark (including non-alcoholic), ale, liqueurs, whiskey.
- Smoked meats, sausages and any products of stale meat
- Marinated, smoked and dried fish (fresh fish is relatively safe)
- Yeast extracts and brewer's yeast (regular baker's yeast is safe)
- Protein supplements
- Legumes (beans, lentils, beans, soybeans)
- Sauerkraut
Foods to be handled with care:
- White wine, port
- Strong alcoholic drinks (risk of depression of the respiratory center)
- Certain fruits such as bananas, avocados, figs, raisins, prunes, raspberries, pineapple, coconut
- Dairy products (yogurt, kefir, yogurt, sour cream)
- Chocolate
- Soy sauce
- Peanut
- Caffeine, theobromine, theophylline (coffee, tea, mate, cola)
- Spinach
Irreversible non-selective MAOIs require avoidance of the aforementioned substances and products during their use and for two weeks after the end of use.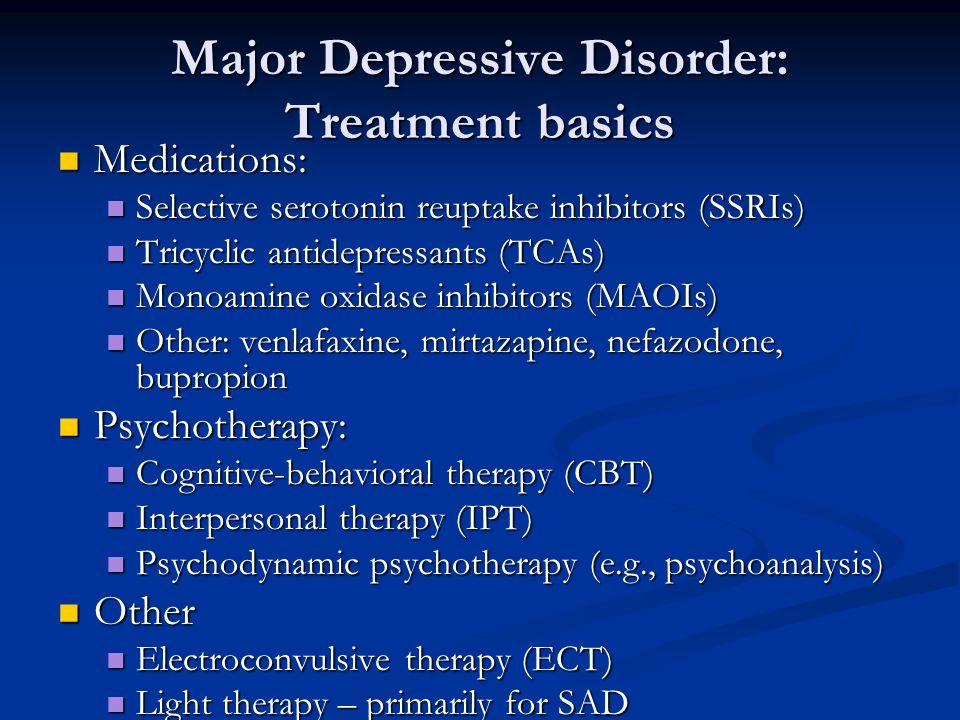 In the case of reversible MAOIs, dietary restrictions are usually less severe and apply to the time that the substance remains in the body (no more than a day). The use of drugs and surfactants listed in the list together with reversible MAOIs should also be avoided until they are completely eliminated.
In the case of reversible MAOIs, dietary restrictions are usually less severe and apply to the time that the substance remains in the body (no more than a day). The use of drugs and surfactants listed in the list together with reversible MAOIs should also be avoided until they are completely eliminated.
Interaction with phenethylamine and tryptamine psychedelics
Most tryptamines are good substrates for MAO-A. DMT and 5-MeO-DMT, when taken orally, are metabolized by it already in the gastrointestinal tract and liver, without having time to get into the blood, so they are inactive when taken orally. 4-hydroxy-DMT (psilocin) is less susceptible to degradation by MAO, since its hydroxyl group in the 4th position makes it difficult for it to bind to the active site of the enzyme, as a result of which it is orally active. Alkyl substituents on the amino group that are bulkier than methyl (ethyl, propyl, cyclopropyl, isopropyl, allyl, etc.) also make it difficult for tryptamines with such substituents to be metabolized by MAO, so all such tryptamines are active when taken orally. The alpha-methyl in tryptamines such as AMT and 5-MeO-AMT significantly impairs their metabolism by MAO, and turns them, de facto, from substrates into weak inhibitors of this enzyme.
The alpha-methyl in tryptamines such as AMT and 5-MeO-AMT significantly impairs their metabolism by MAO, and turns them, de facto, from substrates into weak inhibitors of this enzyme.
Inhibition of peripheral MAO-A - in the gastrointestinal tract and liver by strong MAOIs can make tryptamines such as DMT and 5-MeO-DMT orally active, as well as enhance and prolong the action of other tryptamines such as psilocin and DET. On the other hand, long-term use of MAOIs as antidepressants significantly weakens the effects of psychedelics. This is apparently due to changes in the monoaminergic systems of the brain caused by increased levels of monoamines. The nature of this phenomenon is currently unclear, and is not explained by a simple desensitization of the serotonin receptors with which psychedelics interact.
Thus, the use of MAOIs with tryptamines or immediately before the use of tryptamines prolongs and, in some cases, enhances the effect of the latter, and also allows the use of oral tryptamines such as DMT.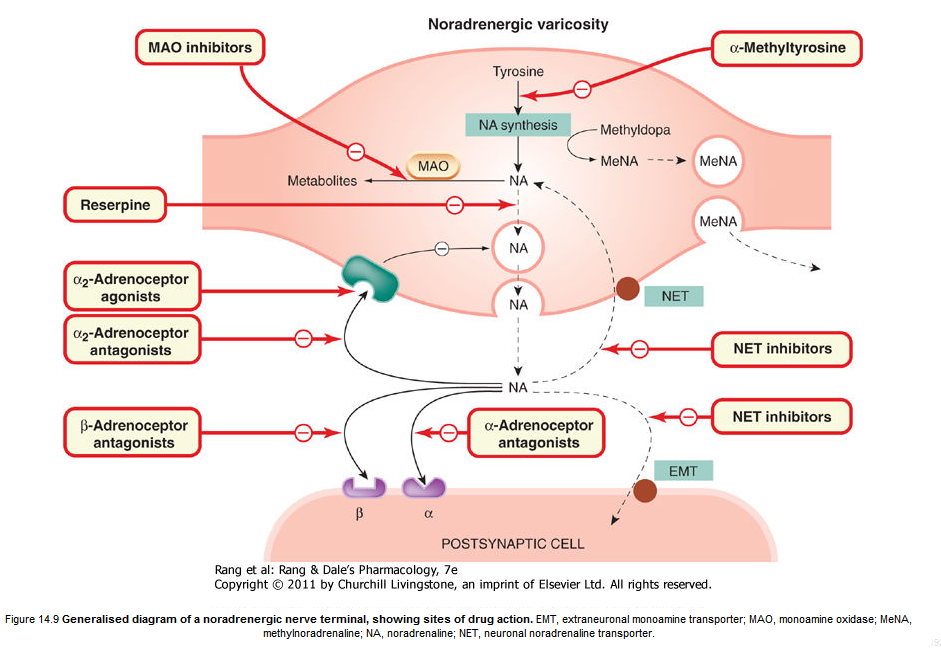 This is the basis of the principle of action of ayahuasca, and similar mixtures, including the so-called pharmahoasca, in which pure DMT is used instead of plant components, and both traditional Banisteriopsis Caapi and Peganum Harmala seeds, or their extracts, can be used as MAOIs, or even moclobemide (Aurorix). At the same time, taking irreversible MAOIs a few days before taking a psychedelic will weaken its effect. The same will happen with long-term use of both irreversible and reversible MAOIs before a psychedelic is taken.
This is the basis of the principle of action of ayahuasca, and similar mixtures, including the so-called pharmahoasca, in which pure DMT is used instead of plant components, and both traditional Banisteriopsis Caapi and Peganum Harmala seeds, or their extracts, can be used as MAOIs, or even moclobemide (Aurorix). At the same time, taking irreversible MAOIs a few days before taking a psychedelic will weaken its effect. The same will happen with long-term use of both irreversible and reversible MAOIs before a psychedelic is taken.
It is not safe to use 5-MeO-DMT with MAOIs. Many note the strong and unpleasant side effects of this combination, up to serotonin syndrome. In addition, such an experience for many people is psychologically extremely difficult, and can be a serious danger to mental health.
Tryptamines that significantly increase synaptic monoamine levels, such as AMT, 5-MeO-AMT, and AET, can be deadly when combined with MAOIs. There is some concern about the safety of using MAOIs with tryptamines such as DPT.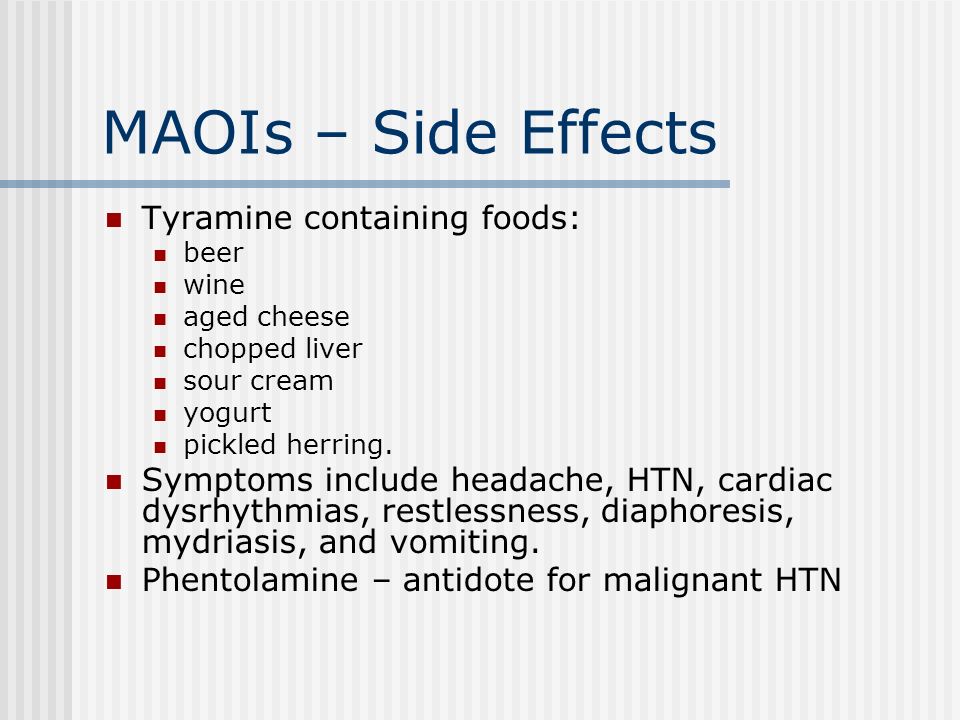
The metabolism of LSD is currently not well understood, but MAO does not appear to play any role in it. However, according to some participants, when used in conjunction with harmala, its effects are enhanced and prolonged. The same applies to other ergolines.
MAO plays a minor role, or even practically does not participate in the metabolism of phenylethylamine psychedelics. Therefore, taking MAOIs together with them is devoid of practical meaning. Although some users report that both harmala and moclobemide increase the effect of some PEAs, such as 2C-B. In most cases, the use of MAOIs with phenylethylamine psychedelics does not pose a serious health hazard. However, the use of MAOIs with sulfur containing phenethylamines such as 2C-T-7 and Aleph-7 should be avoided due to their controversial and little-studied effects on brain monoamine levels and high toxicity. Combinations of MAOIs with TMA-6 and TMA-2 may also be unsafe.
Other MAOIs
Amphetamines and alpha-methyltryptamines
Nicotiana Rustica
Notes
References
- Erowid MAOI Vault
- Pharmahuasca: On Phenethylamines and Potentiation, by Jonathan Ott
See also
- Monoamine oxidase
- Psychoactive substances
Monoamine oxidase inhibitors | it's.
 .. What are Monoamine Oxidase Inhibitors?
.. What are Monoamine Oxidase Inhibitors? Monoamine oxidase inhibitors (MAOIs, MAOIs) - biologically active substances capable of inhibiting the enzyme monoamine oxidase. Monoamine oxidase inhibitors include some antidepressants, as well as a number of natural substances.
|
Contents
|
IMAO classification
According to their pharmacological properties, monoamine oxidase inhibitors are divided into reversible and irreversible, selective and non-selective.
Selective MAOIs inhibit mainly one of the types of MAO, non-selective - both types.
Irreversible MAOIs interact with monoamine oxidase, forming chemical bonds with it. The enzyme is then unable to perform its functions and is metabolized, and instead the body synthesizes a new one, which usually takes about two weeks.
Reversible MAOIs bind to the active center of the enzyme and form a relatively stable complex with it. This complex gradually dissociates, releasing the MAOI, which then enters the bloodstream and is excreted from the body, leaving the enzyme intact.
Nonselective irreversible MAOIs
- Iproniazid
- Nialamide
- Isocarboxazid
- Phenelzine
- Tranylcypramine
Strictly speaking, it is not entirely correct to attribute tranylcypramine to this group, since it is a reversible inhibitor, however, it may take up to 30 days for its complex to dissociate with the enzyme and be completely eliminated from the body.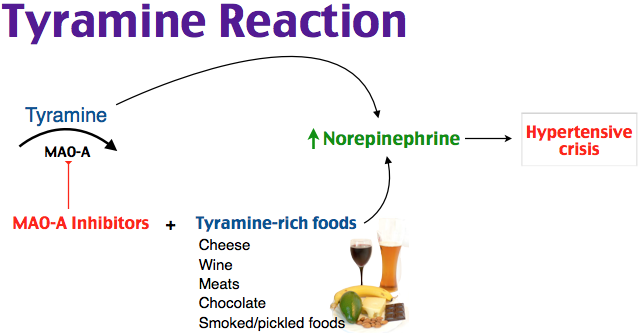 In addition, it exhibits some selectivity towards MAO-A.
In addition, it exhibits some selectivity towards MAO-A.
Reversible selective MAO inhibitors A
- Moclobemide
- Pyrlindol (Pyrazidol)
- Bethol
- Metrolindole
- Beta-carboline derivatives
Reversible MAOIs do not require a diet.
Irreversible selective MAO B inhibitors
- Selegiline
Pharmacology MAOIs
General information
MAOIs, blocking the destruction of monoamines by monoamine oxidase, increase the content of one or more mediator monoamines (norepinephrine, serotonin, dopamine, phenylethylamine, etc.) in the synaptic cleft and enhance monoaminergic impulses (mediated by monoamine nerve impulses) transmission neurotransmission). For this reason, for medical purposes, these substances are used mainly as antidepressants. MAOI-Bs are also used in the treatment of parkinsonism and narcolepsy.
Interactions with drugs and certain surfactants
The combination of monoamine oxidase inhibitors with substances that affect the metabolism of monoamines can lead to an unpredictable increase in their action and be life-threatening.
List of drugs to avoid:
- Psychostimulants of the amphetamine group, and related to them - increasing the levels of catecholamines in the synaptic cleft (amphetamine, methamphetamine, sydnocarb, etc.).
- Any entactogens
- Cold remedies containing sympathomimetics (ephedrine, pseudoephedrine, phenylpropanolamine, phenylephrine, chlorpheniramine, oxymetazoline, etc.): coldrex teraflu, rinza, etc., sprays and nasal drops such as naphthyzinum.
- Slimming aids
- Monoamine reuptake inhibitors:
- Cocaine
- Tricyclic antidepressants (amitriptyline, desipramine, imipramine, etc.)
- Serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac)
- Dextromethorphan (DXM)
- Metabolic precursors of monoamines: DOPA, methyldopa, 5-hydroxytryptophan
- Reserpine
- Antihistamines [ source not specified 122 days ]
- Barbiturates [ source not specified 122 days ]
- Anticholinergics [ source not specified 122 days ]
- Pethidine (Demerol) and other opiates (risk of respiratory depression) [ source unspecified 122 days ] .
Foods incompatible with MAOIs
A significant hazard when using MAOIs is the consumption of foods containing various monoamines and their metabolic precursors. First of all, it is tyramine and its metabolic precursor amino acid tyrosine, as well as tryptophan. Tyramine, like amphetamine psychostimulants, causes the release of catecholamines from nerve endings. Its joint intake with MAOIs is fraught with a hypertensive crisis. Tryptophan is used by the body to produce serotonin, and eating foods high in tryptophan can lead to serotonin syndrome.
Foods to avoid:
- Cheeses, especially aged
- Red wine, beer, especially dark (including non-alcoholic), ale, liqueurs, whiskey.
- Smoked meats, sausages and any products of stale meat
- Marinated, smoked and dried fish (fresh fish is relatively safe)
- Yeast extracts and brewer's yeast (regular baker's yeast is safe)
- Protein supplements
- Legumes (beans, lentils, beans, soybeans)
- Sauerkraut
Foods to be handled with care:
- White wine, port
- Strong alcoholic drinks (risk of depression of the respiratory center)
- Certain fruits such as bananas, avocados, figs, raisins, prunes, raspberries, pineapple, coconut
- Dairy products (yogurt, kefir, yogurt, sour cream)
- Chocolate
- Soy sauce
- Peanut
- Caffeine, theobromine, theophylline (coffee, tea, mate, cola)
- Spinach
Irreversible non-selective MAOIs require avoidance of the aforementioned substances and products during their use and for two weeks after the end of use.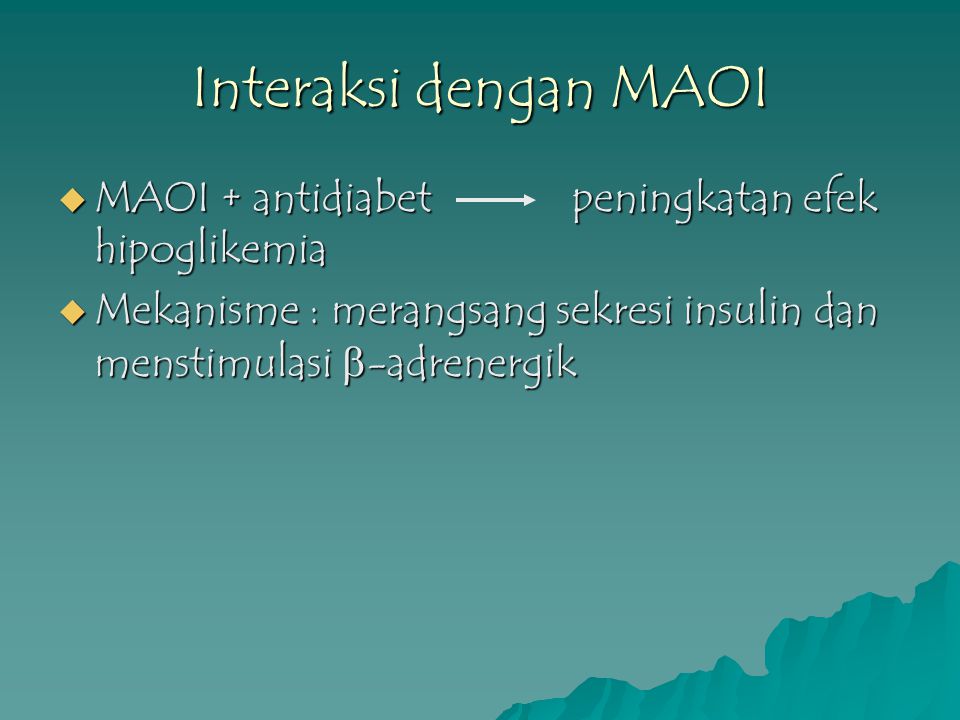 In the case of reversible MAOIs, dietary restrictions are usually less severe and apply to the time that the substance remains in the body (no more than a day). The use of drugs and surfactants listed in the list together with reversible MAOIs should also be avoided until they are completely eliminated.
In the case of reversible MAOIs, dietary restrictions are usually less severe and apply to the time that the substance remains in the body (no more than a day). The use of drugs and surfactants listed in the list together with reversible MAOIs should also be avoided until they are completely eliminated.
Interaction with phenethylamine and tryptamine psychedelics
Most tryptamines are good substrates for MAO-A. DMT and 5-MeO-DMT, when taken orally, are metabolized by it already in the gastrointestinal tract and liver, without having time to get into the blood, so they are inactive when taken orally. 4-hydroxy-DMT (psilocin) is less susceptible to degradation by MAO, since its hydroxyl group in the 4th position makes it difficult for it to bind to the active site of the enzyme, as a result of which it is orally active. Alkyl substituents on the amino group that are bulkier than methyl (ethyl, propyl, cyclopropyl, isopropyl, allyl, etc.) also make it difficult for tryptamines with such substituents to be metabolized by MAO, so all such tryptamines are active when taken orally. The alpha-methyl in tryptamines such as AMT and 5-MeO-AMT significantly impairs their metabolism by MAO, and turns them, de facto, from substrates into weak inhibitors of this enzyme.
The alpha-methyl in tryptamines such as AMT and 5-MeO-AMT significantly impairs their metabolism by MAO, and turns them, de facto, from substrates into weak inhibitors of this enzyme.
Inhibition of peripheral MAO-A - in the gastrointestinal tract and liver by strong MAOIs can make tryptamines such as DMT and 5-MeO-DMT orally active, as well as enhance and prolong the action of other tryptamines such as psilocin and DET. On the other hand, long-term use of MAOIs as antidepressants significantly weakens the effects of psychedelics. This is apparently due to changes in the monoaminergic systems of the brain caused by increased levels of monoamines. The nature of this phenomenon is currently unclear, and is not explained by a simple desensitization of the serotonin receptors with which psychedelics interact.
Thus, the use of MAOIs with tryptamines or immediately before the use of tryptamines prolongs and, in some cases, enhances the effect of the latter, and also allows the use of oral tryptamines such as DMT.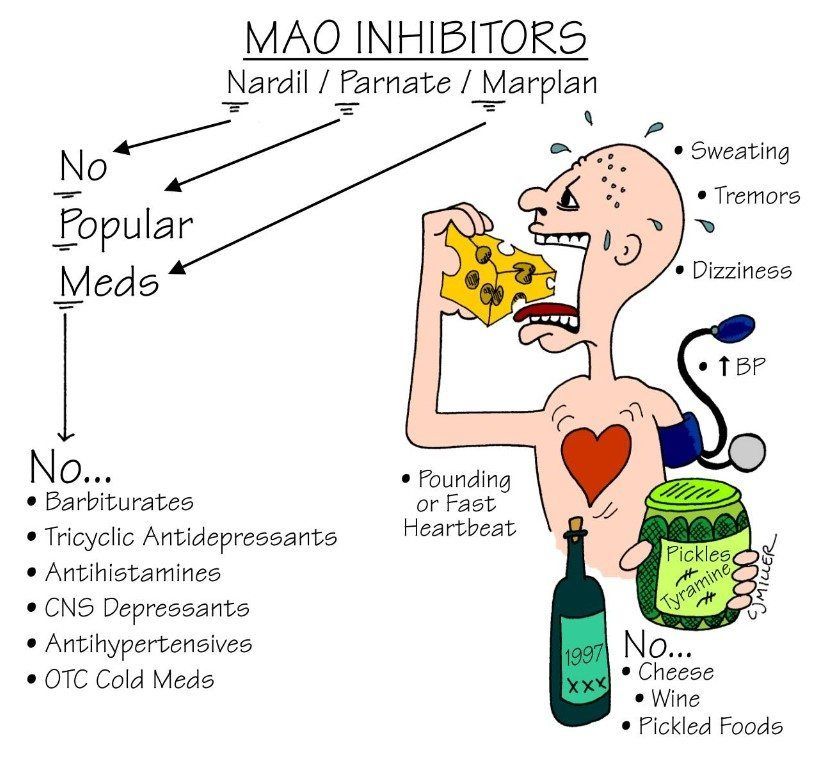 This is the basis of the principle of action of ayahuasca, and similar mixtures, including the so-called pharmahoasca, in which pure DMT is used instead of plant components, and both traditional Banisteriopsis Caapi and Peganum Harmala seeds, or their extracts, can be used as MAOIs, or even moclobemide (Aurorix). At the same time, taking irreversible MAOIs a few days before taking a psychedelic will weaken its effect. The same will happen with long-term use of both irreversible and reversible MAOIs before a psychedelic is taken.
This is the basis of the principle of action of ayahuasca, and similar mixtures, including the so-called pharmahoasca, in which pure DMT is used instead of plant components, and both traditional Banisteriopsis Caapi and Peganum Harmala seeds, or their extracts, can be used as MAOIs, or even moclobemide (Aurorix). At the same time, taking irreversible MAOIs a few days before taking a psychedelic will weaken its effect. The same will happen with long-term use of both irreversible and reversible MAOIs before a psychedelic is taken.
It is not safe to use 5-MeO-DMT with MAOIs. Many note the strong and unpleasant side effects of this combination, up to serotonin syndrome. In addition, such an experience for many people is psychologically extremely difficult, and can be a serious danger to mental health.
Tryptamines that significantly increase synaptic monoamine levels, such as AMT, 5-MeO-AMT, and AET, can be deadly when combined with MAOIs. There is some concern about the safety of using MAOIs with tryptamines such as DPT.
 2 Nicotiana Rustica
2 Nicotiana Rustica