Ocd and controlling others
OCD vs OCPD: Symptoms and Treatments
OCD vs OCPD
Their abbreviated names sound very similar: OCD and OCPD. But in fact, OCD (obsessive-compulsive disorder) and OCPD (obsessive-compulsive personality disorder) are two very different conditions, each with their own symptoms and treatment plans. The good news for individuals who have either one is that with appropriate treatment, they can be well managed to the point that the disruption to one’s life is minimized.
“Although some people may have a tough time distinguishing OCD and OCPD from each other by name, they’re quite distinct in the nature of what they are,” says Simon Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine in New York City.
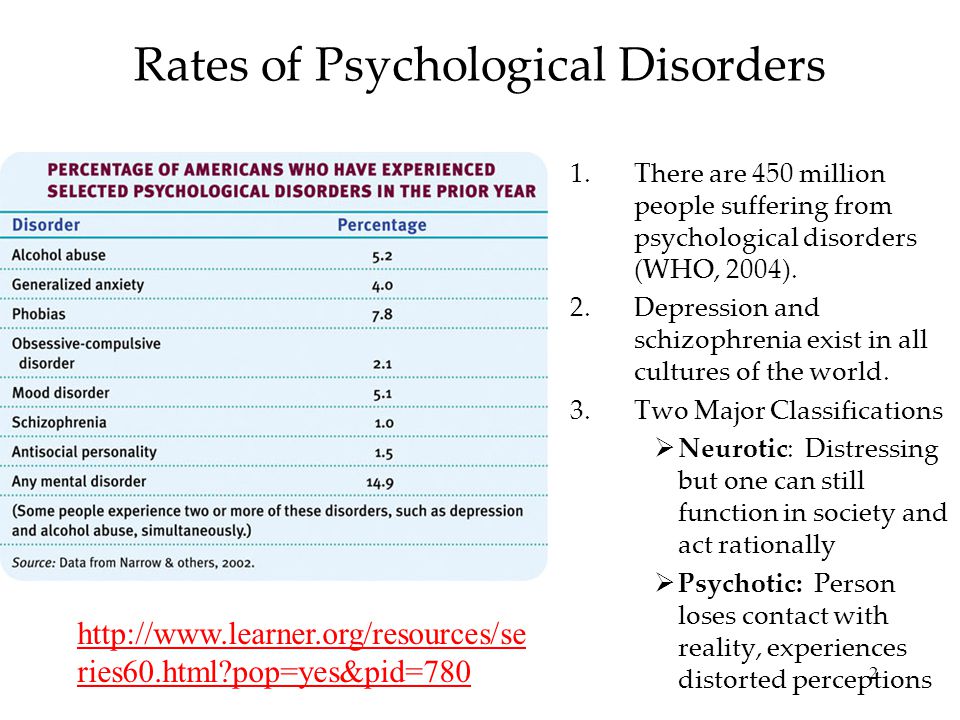
When it comes to OCD, the lifetime prevalence is about 2.5%, Dr. Rego explains. It’s estimated that about 2 to 8% of people have OCPD, and it’s believed to be twice as common in men as in women. ² Additionally, many people exhibit some of the signature traits and behaviors of OCPD, such as self-limiting perfectionism and rigidity, but don’t have the fully diagnosed personality disorder.²
Here’s the rundown on these two mental health conditions.
An individual with OCD has frequent, upsetting thoughts (obsessions) that she tries to control by repeating particular behaviors (compulsions). The obsessions spark a great deal of anxiety because they are not only intrusive and unwanted but also recurrent, Dr. Rego says. “People with OCD will do anything to combat or escape the obsessions and therefore they resort to extensive compulsions and avoidance,” he explains.
Those with OCD are aware that their obsessions are unreasonable, and they can feel tortured by both the obsessions and compulsive behavior. Typically, OCD starts to develop in later childhood or during adolescence.¹ Symptoms can wax and wane, with symptoms getting better at times and worse at others. “It’s not typical for OCD to start later in life,” Dr. Rego says. “But without treatment, the condition becomes chronic and worsens.”
Rego says. “But without treatment, the condition becomes chronic and worsens.”
OCD tends to be distressing because the person may realize that her symptoms are impairing her life but still feels compelled to do her compulsions, says Scott Krakower, DO, assistant unit chief of psychiatry at Zucker Hillside Hospital in Glen Oaks, New York.
“For example, someone with obsessive symptoms of germs and contamination may be doing unwanted rituals to stay clean,” he says. “This may ultimately worsen to where it begins to impact relationships and other functioning.”
Selective serotonin reuptake inhibitors (SSRIs) are commonly used in the treatment of OCD. The most effective form of psychotherapy for OCD is a type of cognitive behavioral therapy (CBT) called exposure and response prevention, says Anthony Pinto, PhD, director of the Northwell Health OCD Center, located at Zucker Hillside Hospital. “In this form of therapy, the patient works closely with the therapist to gradually approach a situation that the patient finds terrifying, and then the patient learns to cope with their anxiety without relying on their compulsions or avoidance,” Dr. Pinto says. “Touching surfaces in a public restroom and then not washing is an example.”
Pinto says. “Touching surfaces in a public restroom and then not washing is an example.”
The goal of this treatment is not to limit having the intrusive thoughts, but instead to learn, over time, to be open to them and not react to them in fear. Both in session and through homework assignments, the person learns to notice and acknowledge the intrusive thoughts without responding with compulsions and, through this process, the person reclaims her life since her routine and functioning are no longer disrupted.
Individuals with OCPD tend to think their way of doing things is the “right and best way,” and they are fixated with following set procedures or routines in their work or daily living, even when these routines are inefficient. These individuals tend to be overly controlling of their environments or relationships, wanting others to conform to the strict rules they set.
This personality disorder includes maladaptive traits and behaviors, including perfectionism that interferes with completing tasks, rigid following of moral or ethical codes, hoarding behaviors, and an excessive fixation with lists and rules·² A person with OCPD has an overwhelming need for order, a strong sense of “how things should be done,” and a rigidity when it comes to following rules. “For someone with OCPD, it’s all about rules and orderliness,” Dr. Rego says. “The person believes there is a certain right way of doing things, and that is how things should be done even at the expense of relationships.”
“For someone with OCPD, it’s all about rules and orderliness,” Dr. Rego says. “The person believes there is a certain right way of doing things, and that is how things should be done even at the expense of relationships.”
A person with OCPD can be successful in work life, he says. “Their perfectionism keeps them at a high standard,” Dr. Rego explains. “That said, others may find the individual with OCPD is difficult to work or live with because of their style of operating.”
The individual with OCPD is preoccupied with perfectionism at the expensive of openness, flexibility, and efficiency, Dr. Krakower says.
Treating OCPD may involve a combination of psychotherapy, medication, and mindfulness techniques. The SSRIs may be helpful because they can make the person feel less distressed and bogged down by minor things.
CBT can be effective for treating OCPD because it targets the individual’s quest for perfectionism and rigidity in thinking and helps focus on the stress that is causing the need to be perfect and organized.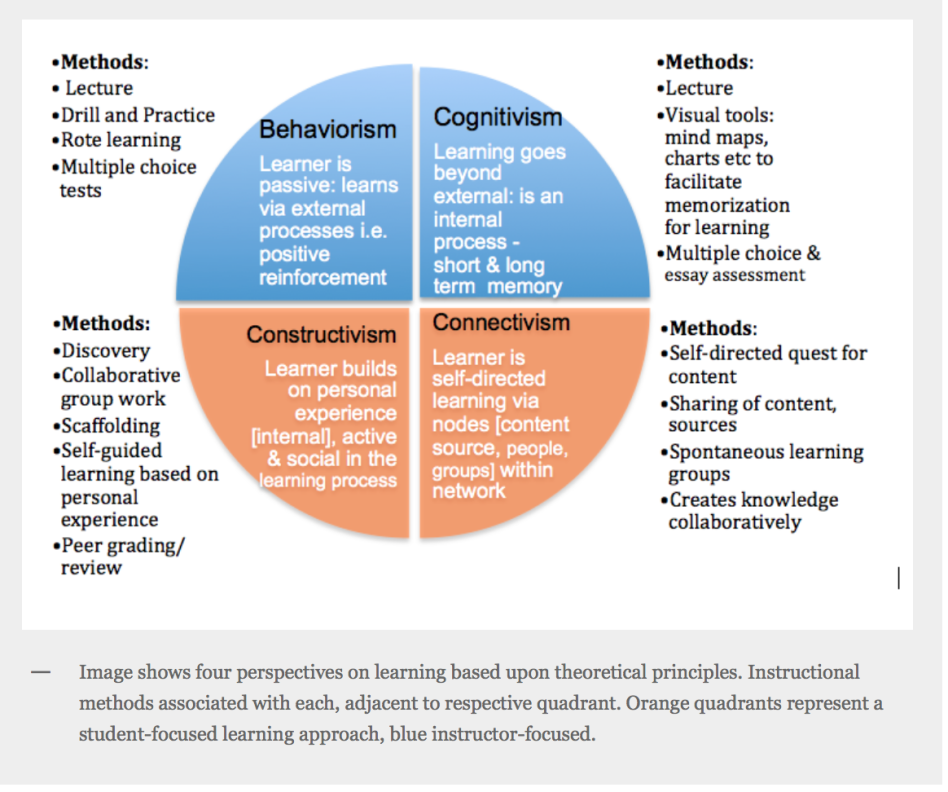 “It helps the person identify the distress that is driving her to be so perfect and organized,” Dr. Rego says.
“It helps the person identify the distress that is driving her to be so perfect and organized,” Dr. Rego says.
“CBT also helps the person to identify the unattainable standards and rigid rules they are living by and to understand how these things get in their way,” Dr. Pinto says. “I work with patients to test these standards and rules so that they can come up with more flexible and time-efficient ways of living. In the process, we also aim to reduce self-criticism and broaden how the person evaluates herself to be based on various life areas rather than being just based on achievement.”
- “What is OCD?” National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/what-is-ocd.shtml
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Washington, D.C.: American Psychiatric Publishing; 2013.
Rosemary Black
Rosemary Black is a veteran journalist who has written about food, health, fitness, and parenting for more than 25 years.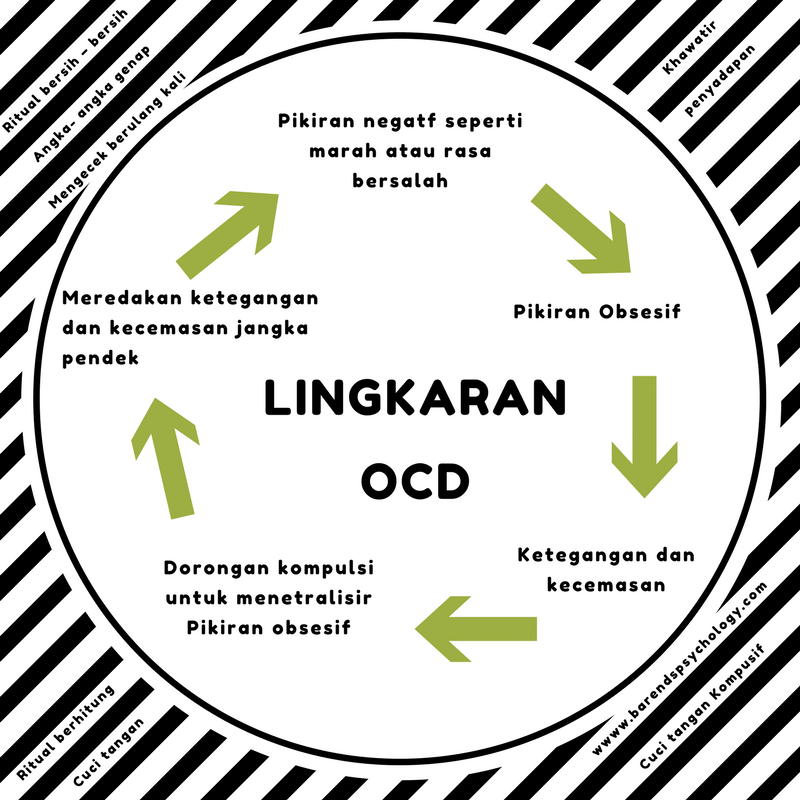 A former senior editor at Everyday Health, she was food editor for the New York Daily News and Parade's Dash magazine. Rosemary, the author of four cookbooks, has written for QualityHealth.com and various other websites and magazines. The mom of 7 lives with her family in Westchester County, New York.
A former senior editor at Everyday Health, she was food editor for the New York Daily News and Parade's Dash magazine. Rosemary, the author of four cookbooks, has written for QualityHealth.com and various other websites and magazines. The mom of 7 lives with her family in Westchester County, New York.
OCD and the Need to Be in Control
In my previous post, I discussed 6 common themes in obsessive-compulsive disorder. Starting with todays entry, in a series of 5 posts, I will be discussing additional aspects of obsessive-compulsive disorder, and will end with reviewing one of the most effective treatments for this condition.
Let me begin with defining obsessive-compulsive disorder.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder (OCD) is a psychological disorder consisting of obsessions and compulsions.
Obsessions are recurrent impulses, images, and thoughts which cause anxiety. Compulsions are repetitive behaviors or mental rituals performed in response to obsessions.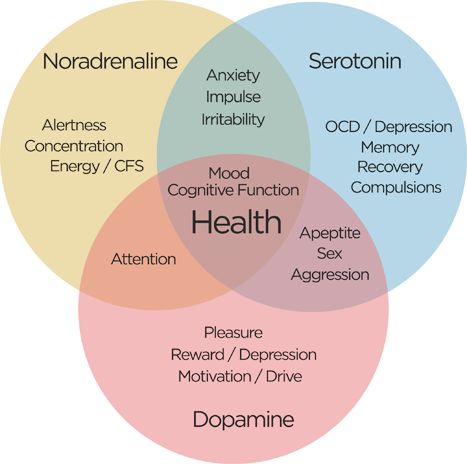
An example of an obsession is having the impulse to scream obscenities in church.
An example of a compulsion is saying 77 Hail Marys to undo the urge to shout obscenities.
The relationship between obsessions and compulsions
Sometimes compulsions are directly related to obsessions.
For instance, a certain individual obsessed with the possibility of catching a fatal disease takes a shower each time she comes home, even if having gone out only for a few minutes. This behavior is obviously excessive, but does it make sense? Yes, because we can see the logical connection between fears of catching an illness and compulsive need for cleanliness.
Sometimes compulsions are not directly related to obsessions. For instance, I once read about a young man who, fearing he would die in a car accident, would try to neutralize these fears by counting from 1 to 26. How does counting prevent accidents? And why up to 26? I could see no clear logical connection in this case.
Consequences of obsessions and compulsions
People with OCD often experience high levels of impairment. There are different reasons for that. For instance:
1. The time taken up by obsessions and compulsions. A person with OCD might spend hours obsessing and performing compulsive rituals; this leaves her little time and energy to initiate or maintain relationships, hold a job, and engage in other activities or hobbies.
2. Avoiding circumstances that may provoke obsessions or compulsions. An individual who worries about contamination might refuse to work in settings where he could be exposed to germs. Or he may avoid going to the hospital to get a much-needed medical treatment for fear of catching a rare and dangerous illness when in the hospital.
Need for control
I like to talk about three additional aspects of OCD, but due to limited space, I will explain the first aspect (i.e. lack of control) in this post and leave the other two for the following posts in this series.
So let me consider humans need for control.
Life can be unpredictable. Despite all precautions taken, we (or people we love) are sometimes severely or irreversibly harmed.
While the possibility of a specific terrible thing happening to you (or your loved ones) is extremely small, the likelihood that something terrible will happen is high because even small odds can add up to a big number.
This is the reality we all need to face. We can do everything right and yet be harmed (or harm others). For instance, sometimes religious people commit sins, loving parents harm their children, caring doctors harm their patients, and careful people hurt themselves.
OCD and control
People with obsessive-compulsive disorder find it more difficult to accept the reality of lifes unpredictability. Why? They might feel a lower sense of control or have a greater desire for control.
Here is an example. A person once told me about her sister, whose OCD had worsened after she gave birth. She constantly worried she would accidentally make her infant ill (e.g., by not washing her hands often enough). One day, when she got home, she left the baby on the table and rushed to the bathroom to wash her hands. Her baby fell off the table.
She constantly worried she would accidentally make her infant ill (e.g., by not washing her hands often enough). One day, when she got home, she left the baby on the table and rushed to the bathroom to wash her hands. Her baby fell off the table.
Luckily, the baby received only minor injuries. But had this person been less preoccupied with certain prevention of only one kind of harm (from dirty hands), she might have been able to prevent her babys fall.
The problem is that some power, predictability, or control, is rarely enough for a person with obsessive-compulsive disorder. Nothing short of full certainty will do. Clean enough, or safe enough is no good. God-like perfection feels like a necessity.
However, that is impossible. We are human beings. Which means demanding perfection in one area of harm prevention means we may not have the time, attention, or energy, to prevent other kinds of harm.
I hope the person above learned the incident, and can have more control in focusing on what matters the most. From what her sister was telling me, she was a great mother. What she experienced (the worsening of her OCD symptoms) after the birth of her child is not unusual. Many people with OCD react to stressful situations with a greater attempt at gaining control. If you have OCD, it helps to be mindful of that, and to seek support during such times.
From what her sister was telling me, she was a great mother. What she experienced (the worsening of her OCD symptoms) after the birth of her child is not unusual. Many people with OCD react to stressful situations with a greater attempt at gaining control. If you have OCD, it helps to be mindful of that, and to seek support during such times.
References
1. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
2. Moulding, R., & Kyrios, M. (2007). Desire for control, sense of control and obsessive-compulsive symptoms. Cognitive Therapy and Research, 31, 759772.
Is there a way out of the inner prison? — Monoclair
Headings : Latest articles, Psychology
Did you find something useful here? Help us stay free, independent, and free by making any donation or purchasing some of our literary merchandise.
Magical thinking as an attempt to control reality arose in primitive times.
 Then, not knowing the laws of the objective world, people tried to protect themselves from the blows of fate with specific rituals. Surprisingly, today, in the 21st century, during the heyday of science and free access to knowledge, many still obsess over "magic rituals" in an attempt to influence the ever-changing world. What is magical thinking, why is it dangerous and what is obsessive-compulsive disorder, we understand together with practicing psychologists and leading researchers. nine0009
Then, not knowing the laws of the objective world, people tried to protect themselves from the blows of fate with specific rituals. Surprisingly, today, in the 21st century, during the heyday of science and free access to knowledge, many still obsess over "magic rituals" in an attempt to influence the ever-changing world. What is magical thinking, why is it dangerous and what is obsessive-compulsive disorder, we understand together with practicing psychologists and leading researchers. nine0009 Each new century sets conditions for humanity that it was not ready for: the First and Second World Wars struck the world with their unprecedented cruelty and broke the psyche of entire generations, and the relatively stable XXI fell upon us with the daily variability of reality. Being in the so-called information society, we daily receive information flows of very different, sometimes polar content, we are forced to master new programs and techniques, regularly improve our skills in order to maintain a source of income, rethink social processes and, most importantly, come to terms with the absolute instability of everyday life.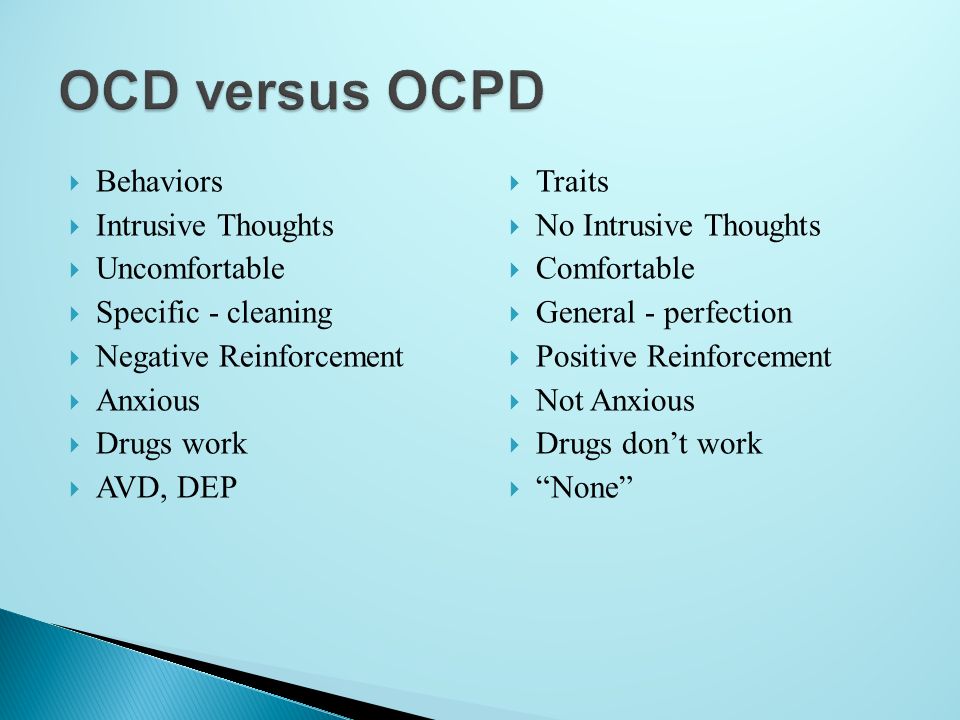 nine0003
nine0003
The demands that modernity imposes on us affect a huge amount of mental resources. Meanwhile, the need for stability is still one of the basic ones for us. Reality is accelerating, and in these difficult conditions, more and more people resort to the so-called "magical thinking". Its essence lies in the fact that a person begins to think that his thoughts, actions or words have a certain impact on the reality around him.
It is worth noting that Ivan Petrovich Pavlov, who studied the human tendency to try to program the surrounding reality, was also engaged in the study of this phenomenon. nine0003
As modern experts note, such a habit can develop into addiction, and in this case, the person will explain all his victories and defeats by the fact that he “was rude to someone in public transport”, “didn’t borrow money for a friend”, “didn’t listen to the annoying him a comrade”, etc. Variants of "magical actions" are deeply individual and diverse.
In addition, according to Doctor of Sociology V.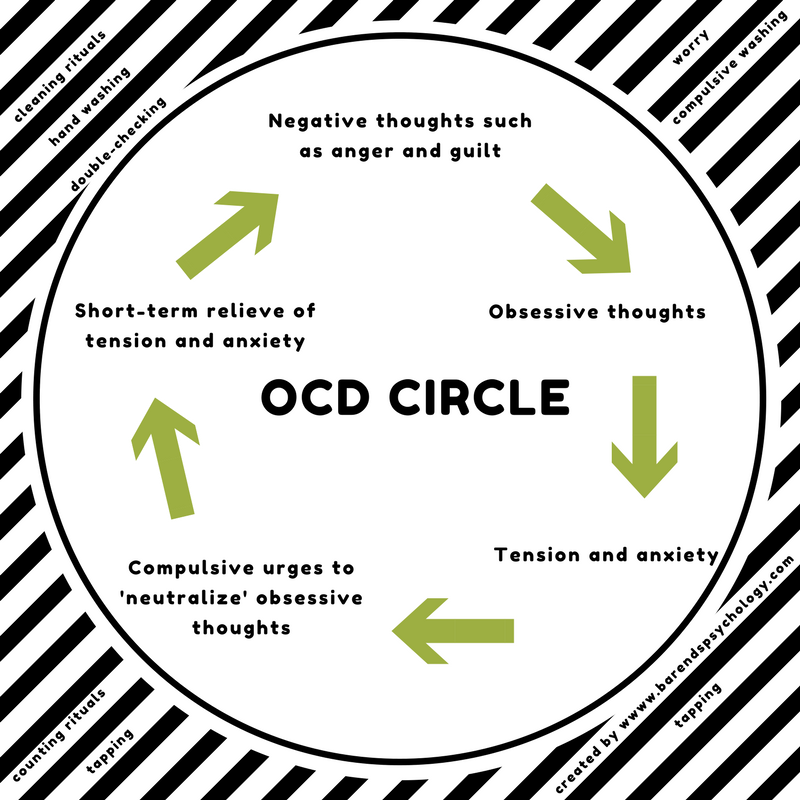 S. Svechnikov and the competitor of the Department of Cultural Studies of the SSTU L.N. Chevtaeva, myths about magic are firmly rooted in the collective unconscious. They note:
S. Svechnikov and the competitor of the Department of Cultural Studies of the SSTU L.N. Chevtaeva, myths about magic are firmly rooted in the collective unconscious. They note:
Sane citizens of Russia, businessmen, politicians, doctors, scientists understand that any mysterious phenomena are always of interest to the masses and are the basis for various kinds of speculation.
This was especially noticeable in the 90s. In a period of absolute instability, people with particular zeal turned to all kinds of magicians, fortune-tellers and psychics. During this time, and later in the 2000s. television, radio and other media supported the interest of the masses in everything “mysterious”: A. Kashpirovsky’s programs, shows with psychics, calls to the studio to “magicians” who “resolved” any problems at a distance were especially popular - from husband’s alcoholism to serious diseases. nine0003
In this regard, the Russian Academy of Sciences even created a special Commission to combat pseudoscience and falsification of scientific research.
At the same time, it is interesting that many understand the illogicality of "magical thinking" and speak out against such a method of controlling reality. However, a study conducted in the UK by psychologist E. Subbotsky showed the opposite. One of the experiments is described as follows:
Adult subjects were asked to imagine their future life. After that, they were told that a) a magic spell cast on their future life would change this life for better or worse (mythical suggestion), and b) changing the numbers on the computer screen would change their future life for better or worse (ordinary suggestion). All subjects denied that changing the numbers on the computer screen could affect their future lives, but in their actions they demonstrated their belief in this possibility. nine0003
Thus, it can be said that mentally healthy people are aware of the absurdity of "magic spells", however, an irrational grain deeply embedded in the unconscious, in some cases associated with childhood trauma, as well as with culture (tales, myths, tales, sayings and local superstitions) prevents them from thinking rationally and greatly increases anxiety levels.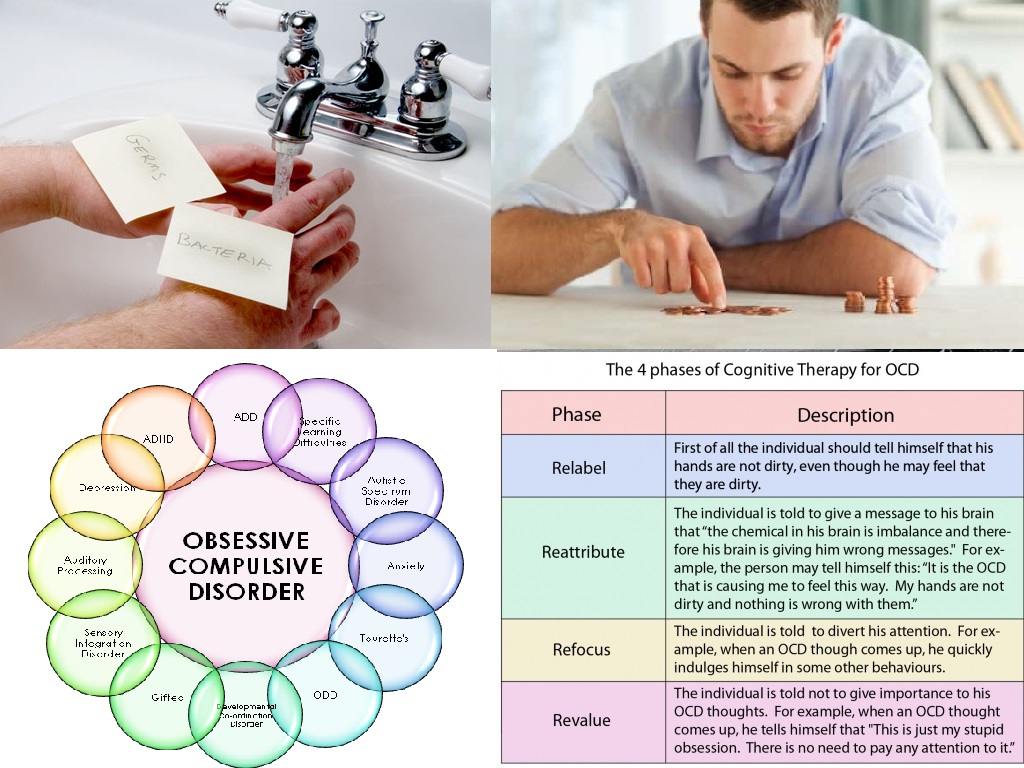
This is precisely what "magical thinking" is dangerous for. Getting the illusion of control over the world, a person begins to strive for "absolute omnipotence" and tries to program the uncontrollable. In cases where his actions coincide with obtaining the expected result, he increasingly believes that he has found a "magic way" to control the environment. Otherwise, he blames himself for supposedly “wrong” thoughts or actions. nine0003
The habit of thinking "magically" is fraught with the fact that seemingly harmless actions quickly progress into a real mental illness - obsessive-compulsive disorder (hereinafter - OCD), bringing severe, sometimes unbearable suffering to a person.
OCD is an obsessive condition characterized by obsessions and compulsions, where an obsession is a persistent, highly frightening or unpleasant thought that comes into the mind of the patient against his will, and a compulsion is a special, deeply individual ritual that helps to temporarily get rid of obsessive thoughts.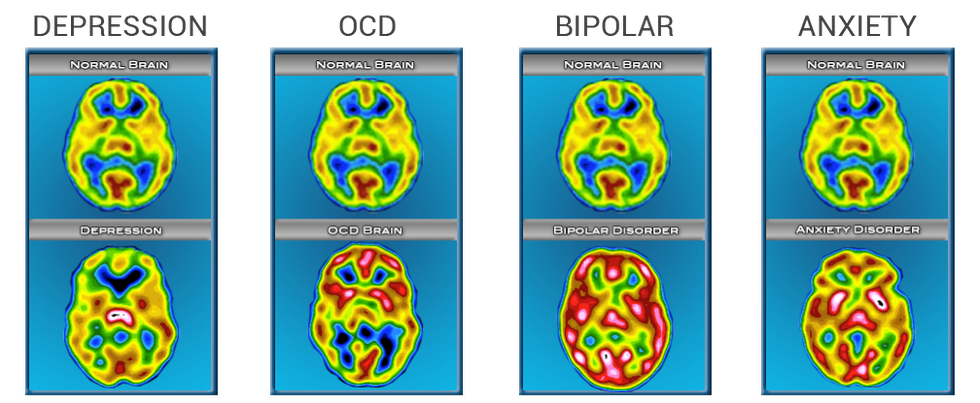 nine0003
nine0003
Thus, the consciousness of a person with varying degrees of frequency is visited by phobic, sometimes disgusting, thoughts unusual for the individual. Among the most common are the fear of contracting a dangerous, incurable disease, catching a virus, failing at work or school, losing a loved one, etc. Sometimes the patient is faced with nasty and unusual images of violence, cruelty, sexual perversion, intentions to cause someone moral or physical harm.
nine0002 Thoughts that have nothing to do with the patient's personality drive him crazy, drive him into a panic. To get rid of them, he tries to perform absurd rituals invented by him. The most frequent ones are constant washing of hands, avoiding stepping on certain steps of stairs, arranging books and other objects in the “right” order, etc. Rituals can be very different. For example, some people are afraid to repost or like on social media simply because they think “something bad” might happen. nine0003 Psychologist-consultant A.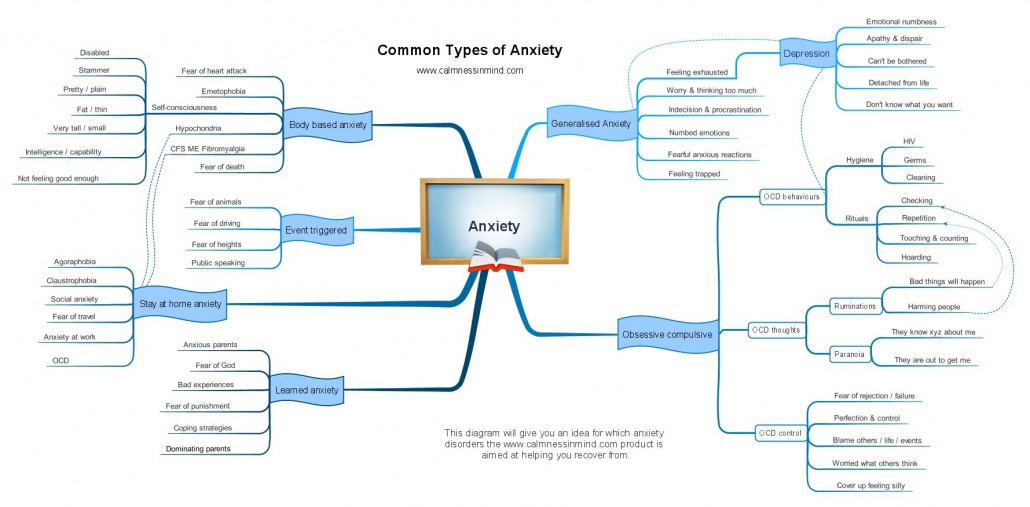 V. Duhareva notices:
V. Duhareva notices:
A person believes that the repetition of certain actions can protect him from the vicissitudes of fate. Often from such clients you can hear phrases like: “if I do everything right, then nothing will happen”, “the main thing is to turn off the light with the right / good thought”, “if I made a mistake in the sequence of actions, then it is important to start all over again”, etc. P.
OCD usually occurs for a variety of reasons. This can be both a consequence of a passion for magical thinking, and childhood trauma, stress, moral and physical exhaustion, heavy workload at work, instability in professional activities. nine0003
The danger lies in the fact that in reality there are no "magic" rituals. But sincerely believing in their power, the patient can spend hours just washing their hands, turning door handles a certain number of times, rewriting social media messages, choosing the “correct word order”, etc. The fear behind each ritual varies significantly each individual person. For example, people with anorexia may forbid themselves from saying certain words or letters for fear of gaining weight. At the same time, rituals bring only temporary relief, forcing a person to independently immerse himself in an inner prison full of unbearable suffering. nine0003
For example, people with anorexia may forbid themselves from saying certain words or letters for fear of gaining weight. At the same time, rituals bring only temporary relief, forcing a person to independently immerse himself in an inner prison full of unbearable suffering. nine0003
Interestingly, most OCD sufferers really understand the absurdity of the situation, but can't fix anything. As a rule, they hide their illness, fearing condemnation and ridicule. According to WHO, in 2013, 1 to 3% of the population suffered from OCD. However, according to experts, this figure is greatly underestimated.
It is also important that, in addition to most people who are aware of the illogicality of their actions, patients with a "psychopathic level of organization will believe that rituals really save them from fatal consequences." nine0003
The good news is that this disease is curable. The advice of psychiatrists is universal. A person should carefully monitor his condition and effort of will, try to break the chain of his own “cause and effect relationship”, trying to identify in the cause of success or failure not a sign of “correct performance of magical actions”, but a real act, to realize the level of anxiety that interferes with a full life, for example, in the form of relationship problems, an eating disorder, a stressful job, an unstable business.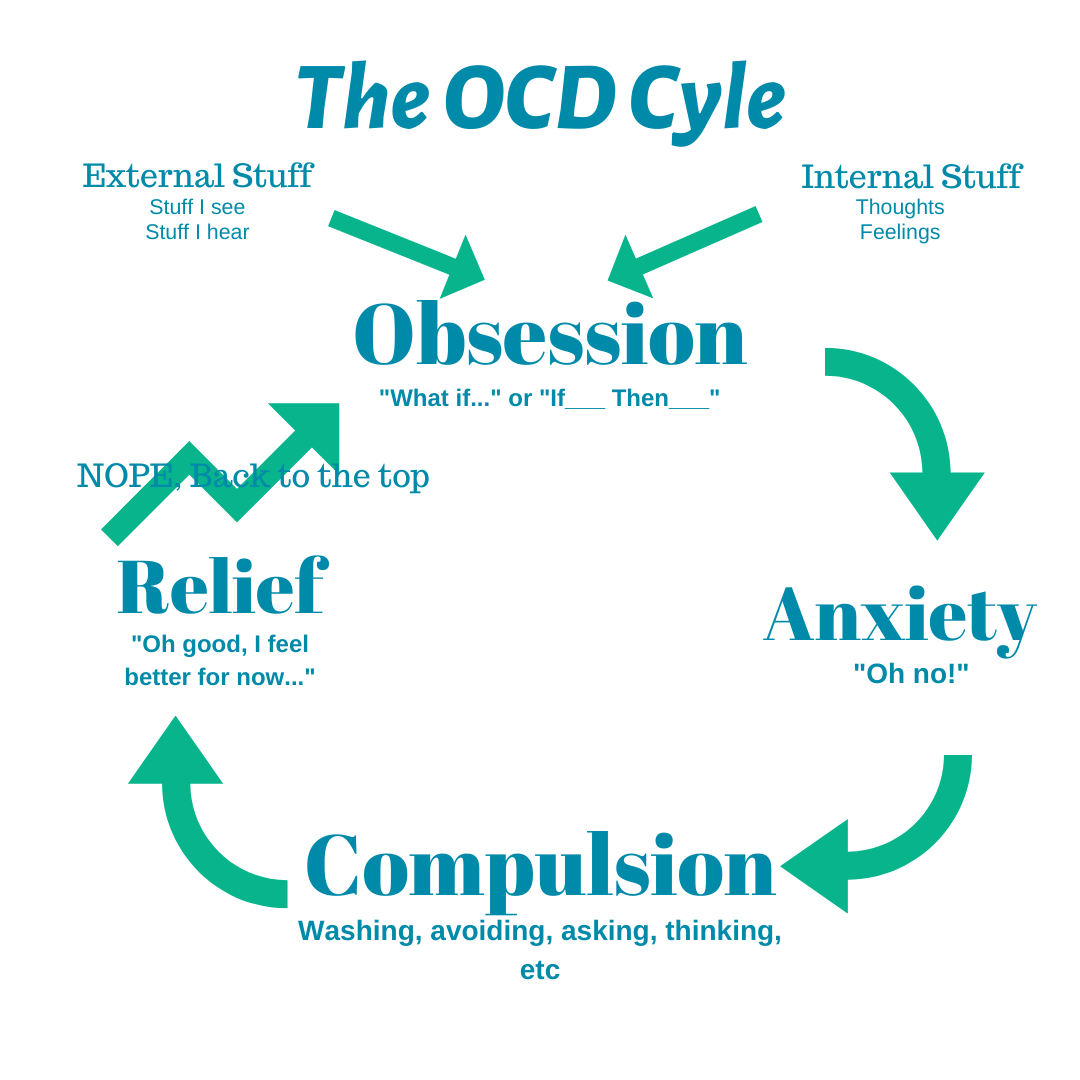 Psychotherapists also offer to bring rituals to the point of absurdity, that is, for example, to close and open doors until the moment when a person simply gets tired and realizes the meaninglessness of this action. Moreover, doctors recommend visualizing my fears, imagining what would happen if I “lost my job”, “gained weight”, “broke up with a toxic partner”, etc. In this case, the patient, albeit with more discomfort and high anxiety, works out alternative options that help him remove fatal scenarios from his life. nine0003
Psychotherapists also offer to bring rituals to the point of absurdity, that is, for example, to close and open doors until the moment when a person simply gets tired and realizes the meaninglessness of this action. Moreover, doctors recommend visualizing my fears, imagining what would happen if I “lost my job”, “gained weight”, “broke up with a toxic partner”, etc. In this case, the patient, albeit with more discomfort and high anxiety, works out alternative options that help him remove fatal scenarios from his life. nine0003
As a rule, patients diagnosed with obsessive-compulsive disorder undergo both drug therapy (usually with the help of antidepressants and tranquilizers) and visit a psychotherapist who not only helps to get rid of obsessive thoughts, but also tries to help the client find and neutralize reason for his anxiety. After all, everything that happens to us, be it OCD or a panic attack, is, in fact, a signal that something is going wrong in our lives. And our psyche begins to rebel, demanding a more careful attitude towards ourselves and our lives. Reviewing the life script, realizing that the patient may not be going his own way or taking on too much, helps him return to a healthy life. nine0003
Reviewing the life script, realizing that the patient may not be going his own way or taking on too much, helps him return to a healthy life. nine0003
In addition, it is important to remember that life has always been, is and will be a changeable substance. This is its value and beauty. We do not have the right to "concrete" the present, but we have a unique opportunity to live without fear, enjoying every day, with all its amazing surprises or troubles, which, in the end, save us from infantilism and make us stronger.
Related selection
- "Primitive Thinking": Lucien Levy-Bruhl on the prelogical ideas of the ancients
- Diogenes Syndrome: why do we collect trash
- Political Myth: How Basic Archetypes Became Manipulation Weapons
Cover: René Magritte, detail from The Heart of the Matter (1937)
If you want to help Monocler, make a monthly payment on Patreon or support us with a one-time donation:
Patreon
YuMoney
If you find an error, please highlight the text and press Ctrl+Enter .
Psychiatriyapsychology psychology
Similar obsessive-compulsive disorder in children and adolescents. Inclusion of the family in the treatment process
Source: Collection of scientific articles. VIII International Congress of the CPT Association (CBTFORUM)
Key words: OCD, CBT, method of exposure and reaction prevention, obsessions in children and adolescents, obsessions, compulsions, reassuring behavior
The body of scientific evidence on OCD has grown exponentially in recent years, and these studies have shown that cognitive behavioral therapy (CBT) is the most effective and evidence-based treatment for OCD. The EX/RP treatment program, exposure and reaction prevention, received the most scientific evidence.
It is important to answer the question: what is obsessive-compulsive disorder (OCD)? This problem is characterized by the presence of obsessions and compulsions.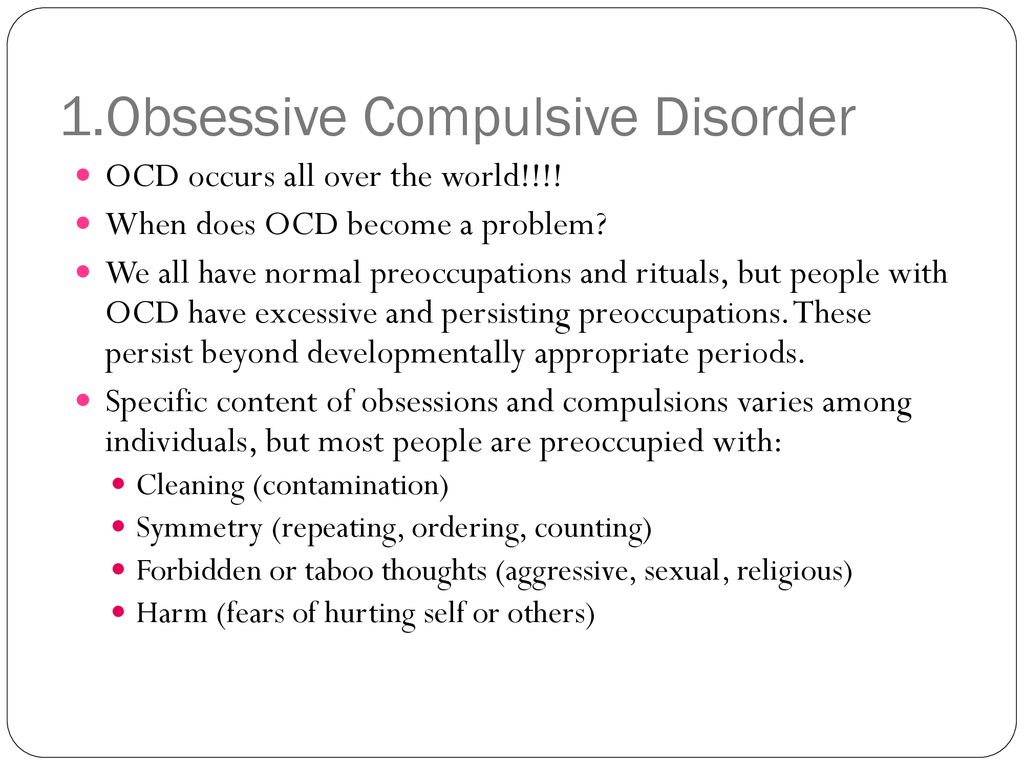 The former consist of unwanted intrusive thoughts (“I can’t touch the table because I will pollute myself”), terrible and disgusting images (“I can’t stand this image, the picture that comes to my mind is disgusting”) or urges (“ I look like I'm going to get naked in front of people"), which are usually described as being rejected by a child or teenager. These thoughts cause great anxiety and discomfort and are very difficult or impossible to suppress. The most common are intrusive thoughts. The child may have recurring thoughts about problems related to danger or harm to self or parents, germs and disease, cleanliness, housework, sex, etc.
The former consist of unwanted intrusive thoughts (“I can’t touch the table because I will pollute myself”), terrible and disgusting images (“I can’t stand this image, the picture that comes to my mind is disgusting”) or urges (“ I look like I'm going to get naked in front of people"), which are usually described as being rejected by a child or teenager. These thoughts cause great anxiety and discomfort and are very difficult or impossible to suppress. The most common are intrusive thoughts. The child may have recurring thoughts about problems related to danger or harm to self or parents, germs and disease, cleanliness, housework, sex, etc.
Compulsions are not about getting pleasure, but about preventing or reducing discomfort. Usually these are motor or mental reactions, which are characterized by high repetition and even severity. For example, the fear of infection leads to a reluctance to touch objects, wash hands, force mom to wash them, etc. Obsession with not making mistakes leads to having to reread school homework, recheck it again and again, erase and rewrite.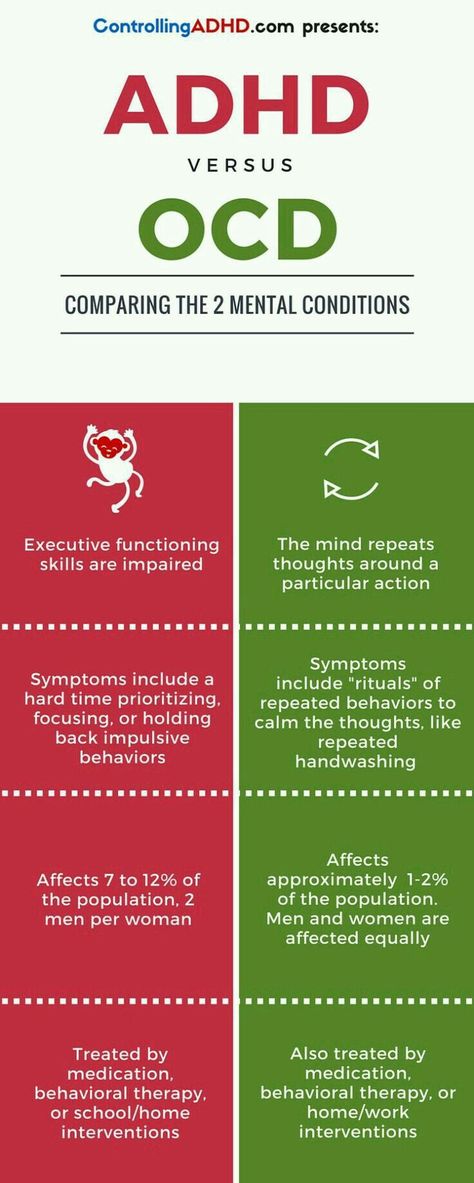 nine0003
nine0003
Childhood obsessive-compulsive disorder
Different obsessive themes may occur or change over the course of the disorder in the same child. This sense of loss of control over one's own behavior is felt very strongly, although this does not mean that the fearful behavior is eventually carried out. At an early age, children often do not know how to recognize or explain what their obsessions are, and sometimes they can even describe them as voices in their heads. The most obvious are the compulsions or rituals they perform that they can force others to perform. nine0003
How does OCD affect the family?
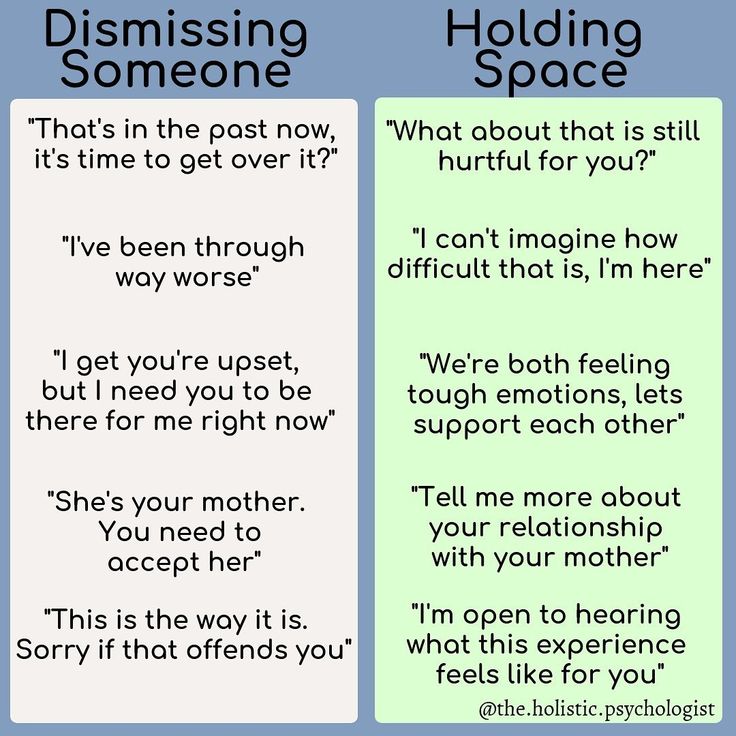
If a child has OCD, it affects daily life. At first, strange behavior can be embarrassing or frustrating for parents. They may panic if the child is naughty and cannot complete the rituals. Children with OCD can make family members part of OCD in a variety of ways: in an effort to gain reassurance, they constantly ask their parents the same question and each time demand an answer.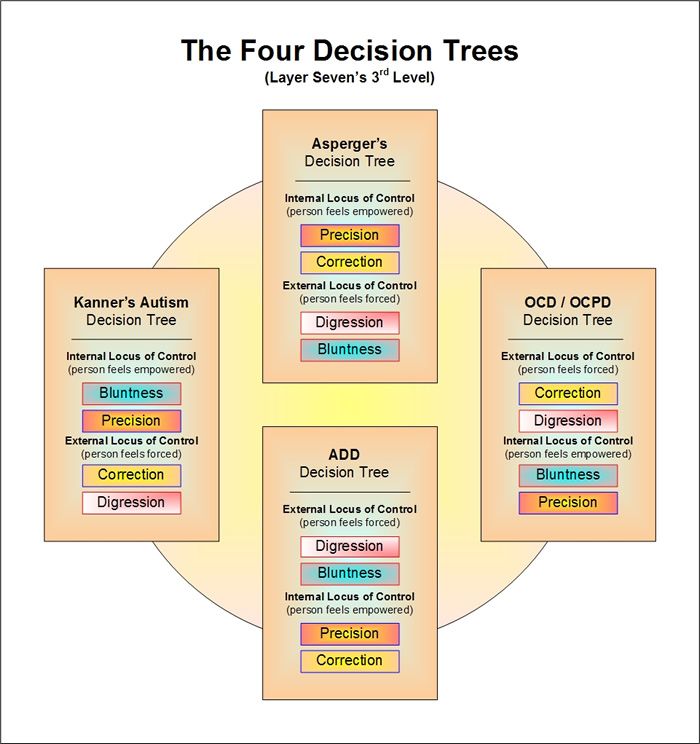
They may insist that parents and siblings perform OCD rituals. They may become frustrated if they fail to complete them, and this is very stressful for the family, who feel they cannot relax and that family life is becoming dysfunctional. Parents may feel that they have to change their daily routine or give in to the child's demands to avoid his child's anxiety. Parents experience a variety of emotional states, including fear, frustration, irritability, guilt, and sadness. They often wonder if the child will recover or what the future will be like. nine0003
Keys to Communication
The more information parents have in OCD psychoeducation sessions, the easier it will be for them to talk about it with their child. Parents can help boost their child's self-esteem by letting them know that the problem is with the illness, not with them. Criticism only increases the child's anxiety and makes OCD much more difficult to overcome.
On the other hand, when parents approach any problem without judgment, they communicate to the child that they understand what he is going through and that they are always ready to help.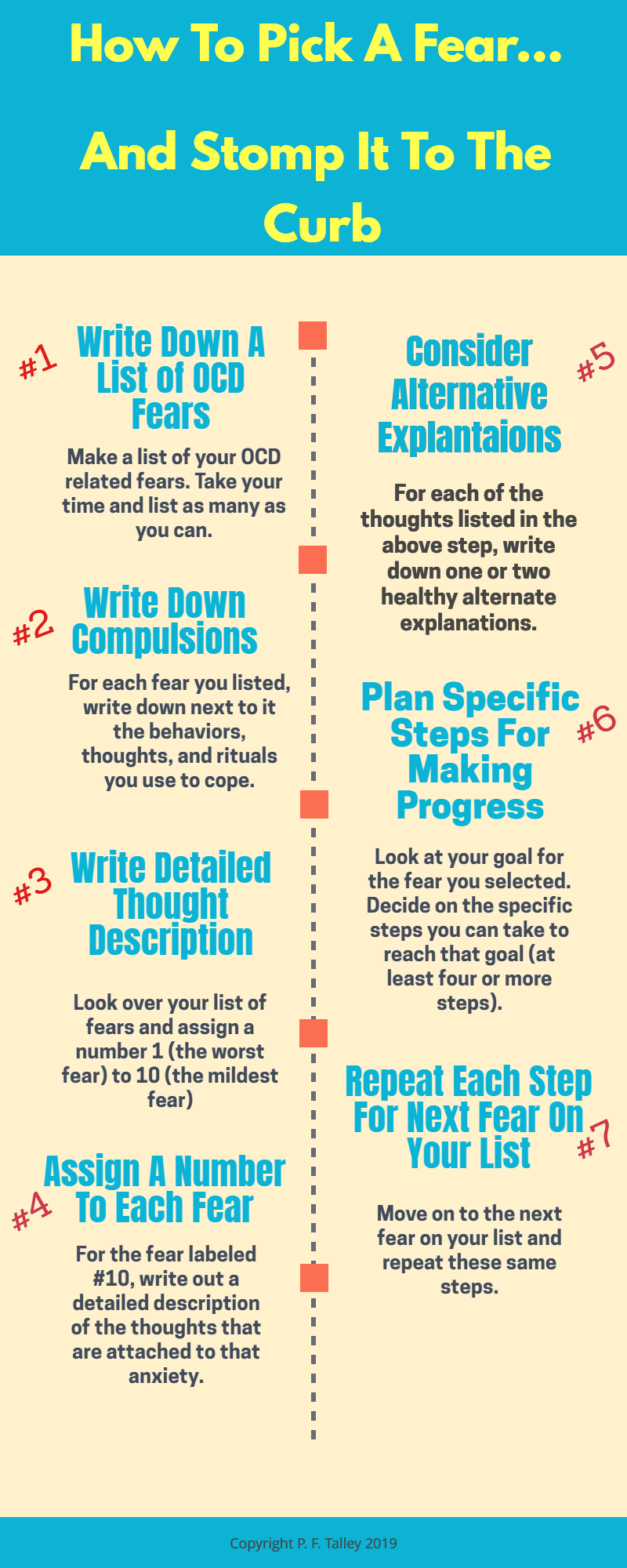 Children and adolescents with OCD often hide their symptoms due to inappropriate feelings of shame or guilt. nine0003
Children and adolescents with OCD often hide their symptoms due to inappropriate feelings of shame or guilt. nine0003
How to keep stress out of control:
- Seek help from family and friends who are willing to support.
- Contact a professional support group in person or online.
- Remember: the initial period is the most difficult, and it seems that everything is hopeless when therapy still does not help, but it is like a storm before the calm. Once the child, with the help of the parents at home and with the therapist in the sessions, overcomes this obstacle, everything becomes much better. nine0168
- Seek therapy if parents need it. Parents must be calm in order to create a favorable climate for the recovery of the child.
- Parents can encourage communication, but not insist that their child tell more than is comfortable for him.
 Over time, as the treatment begins to take effect, the child will be able to speak more frankly—and when this happens, it is best for parents to listen with an open mind to whatever they have to say.
Over time, as the treatment begins to take effect, the child will be able to speak more frankly—and when this happens, it is best for parents to listen with an open mind to whatever they have to say. - Let the child know that it is okay to talk about unpleasant thoughts or feelings, as well as pleasant ones. Do not give simplistic advice such as "Don't worry!" or "Stop." No one is more affected by OCD than the child himself. If it were easy to stop, he would no doubt have already done so. Instead, it is better for parents to let their child know that they are aware of how difficult it is, but are confident that he will be able to overcome the disease. nine0168
Assertive actions
Sometimes parents start doing things that the child avoids due to obsessions. They think that in this way they can help him. They alleviate the child's anxiety for only a short period of time, helping to maintain avoidance behavior, which ultimately harms him. As well as the desire to help, the negative behavior of the close environment contributes to the reinforcement of obsessions and compulsions.
As well as the desire to help, the negative behavior of the close environment contributes to the reinforcement of obsessions and compulsions.
It happens that close people are indignant and try to prevent the performance of a ritual action. Sometimes this leads to a delay in the rituals that the child will make up for when he is not seen. A child with OCD will accumulate significant stress during this time, in part due to being rejected, and will perform rituals longer and more intensely. nine0003
Parents trying to help can make a child or teenager very unhappy if they constantly tell him what to do and what to avoid. Sometimes some members of the family engage in rituals or, conversely, leave the child alone to repeat their compulsive actions over and over again because they feel helpless about what is happening. It is best not to lose control of yourself and try to remember that parents and family members are not the only ones who suffer from this disorder. nine0003
Can children overcome OCD?
Cognitive Behavioral Therapy (CBT) can help a child learn the skills needed to overcome this problem.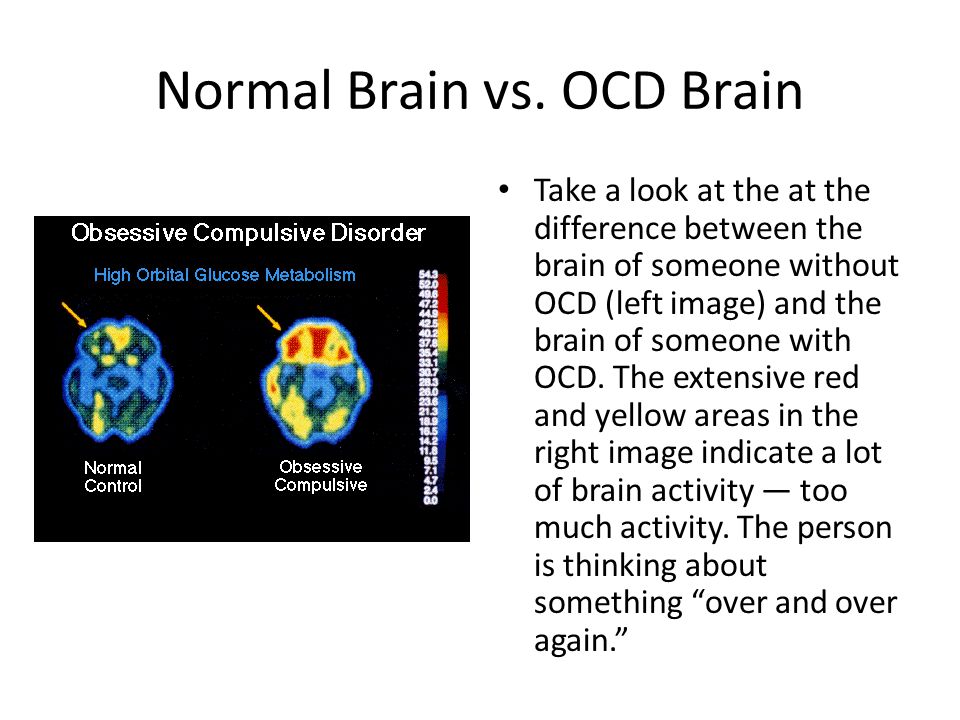 When thinking about taking control of OCD rather than letting the disorder control the child, it is important to remember that the right treatment helps.
When thinking about taking control of OCD rather than letting the disorder control the child, it is important to remember that the right treatment helps.
How to indicate that the problem is not in the child, but in the OCD?
One way to do this is to call OCD a derogatory or obnoxious nickname of the child's choice. Criticism and other forms of punishment hinder the healing process. This is why working on generosity, kindness, and patience as the child works with a psychologist to apply EX/PR therapy strategies will reduce OCD symptoms in the long term. nine0003
It is preferable not to give advice. Most kids already know that OCD doesn't make sense, so reminding a child that their behavior is pointless or stupid usually makes them feel really bad. Similarly, giving advice like "Stop it" has the same meaning; no one hates OCD more than a child with OCD. Showing a neutral, supportive and reassuring stance can help reduce a child's anxiety during exposure tasks.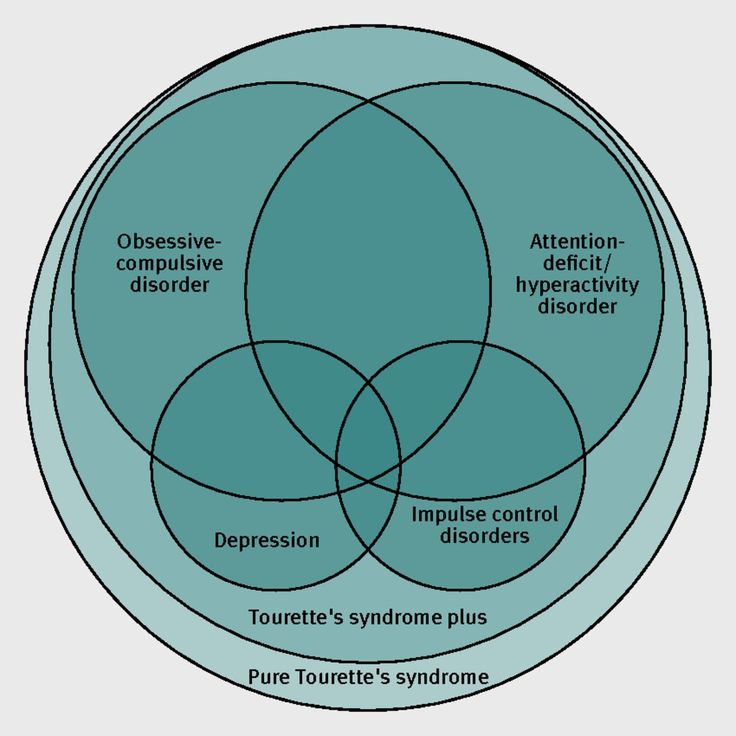 Criticism or punishment not only aggravates OCD, but also reduces motivation to undergo CBT. nine0003
Criticism or punishment not only aggravates OCD, but also reduces motivation to undergo CBT. nine0003
Examples of reassurance within the family:
- Wash clothes with special soap.
- Help check if everything is turned off properly.
- Wait for the child to complete the hand washing ritual.
- Wait until the child has finished putting certain things in a certain order in his room before leaving the house, etc.
Another important requirement for the family is not to give the child reassurance. A large number of children ask for reassurance from both a psychologist and loved ones. These requests should not be granted. To the question "Are you sure that nothing will happen?" or “Are you sure everything will be okay?” the patient's family members should respond as follows:
- We agreed not to talk about this, right?
- Don't forget that your psychologist forbade me to answer such questions.
- I understand that you are going through a difficult period, I am here, I am with you.
- I love you, but I won't help you if I answer this question.
- I'm afraid my answer won't help you, so I won't answer.
Explaining OCD with metaphors
When a student is about to take a very important exam at school, they get nervous. The teacher starts handing out exam papers, and the student's anxiety grows, he becomes more nervous, afraid that he will not be able to answer the questions, he wants to run away from the class, but he sits and waits. Then, when the child reads the ticket questions, the anxiety subsides because he knows the answers to them. It is the same as if the child had an obsession; the difference is that in a school situation he accepts it as the norm and puts up with discomfort, however, when obsessions come, the child immediately seeks and takes measures to reduce his level of anxiety - he does not wait until it passes by itself. nine0003
nine0003
Sometimes we wake up in the morning singing a song, after a while we get tired of constantly singing it, and we try to get the tune out of our head, but it goes over and over in our head. If we put in a lot of effort, confrontation, and try to forget the song, we find that it has stuck and stays in our head. The same thing happens with intrusive thoughts. They appear, and the more your child tries to put them out of his mind, the more they are repeated and reinforced. nine0003
The basic idea is simple: OCD is just a hiccup in the brain that comes and goes like a cloud in the sky.
Thus, working with OCD involves teaching the child four simple phrases.
- First : something like "It's OCD again." Sometimes a friendly “hello+ nickname” can help reduce a child’s tendency to react emotionally to OCD symptoms.
- Second : "My brain is hiccuping again" - explicitly acknowledging that what we call OCD is due to a malfunction in the circuitry of the central nervous system.
 nine0168
nine0168 - Third : "The hiccups don't matter" suggests no response other than patience, since OCD doesn't make sense.
- Fourth (aimed at downplaying symptoms that will go away on their own if nothing is done): "I'd rather do something enjoyable while the OCD goes away." Cultivating detachment will help your child not worry about their OCD. Parents can do something interesting with their child (for example, read a fairy tale, take a walk or play). nine0168
Anxiety thermometer
Anxiety thermometer can be used to check the level of anxiety, which will measure the temperature of discomfort and range from 0 (no anxiety) to 10 degrees (very strong or extreme anxiety).
Let's see what we can say to a child: “Look at this thermometer, can you tell us: if you are very nervous at the sight of cutlery on the table, are you very ill or not very ill? It's like a thermometer: how bad or scared are you when you see them? The worse it gets, the more the temperature rises.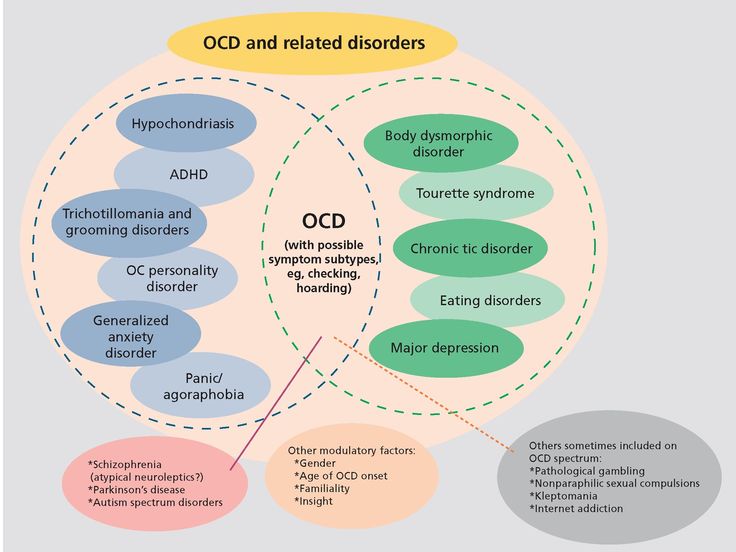 ” nine0003
” nine0003
It is necessary to praise and encourage the child if refusal to participate in the ritual does not cause him anxiety. Parents should not abruptly stop affirmative actions and refuse to participate in rituals. Abrupt cessation will not help, as the child will not develop strategies to cope with the resulting distress; it will not reduce those symptoms that are "out of sight" and, most importantly, will not help the child learn strategies for coping with OCD symptoms in the long term. nine0003
It is normal for parents to have doubts and concerns about the effectiveness of treatment. In this case, it is recommended to discuss all emerging questions and concerns with the doctor, psychologist and all family members.
If there is a feeling that the treatment does not help at all or causes discomfort, the psychiatrist must be informed immediately. OCD is difficult to control, so there is a risk of relapse by stopping treatment without first consulting a doctor or psychologist. nine0003
nine0003
Post-treatment follow-up
At the start of treatment, many families see their doctor at least once a week to monitor symptoms, medication dosage, and side effects. As the child recovers, contact becomes less frequent at the discretion of the doctor. After recovery, the child is encouraged to visit their doctor for a short check-up regularly for the first year and then once a year. A doctor should be consulted if parents notice the following in their child:
- severe and recurrent OCD symptoms;
- worsening of OCD symptoms that do not "respond" to the strategies taught in CBT;
- changes in how drugs work;
- new symptoms of another disorder, such as panic disorder or depression;
- problems at school that can exacerbate OCD.
The future of children with OCD
While the child is in therapy and working towards recovery, it is preferable for parents to allow their child to accept life as he can and not pressure him. High expectations should be avoided: support from the family is important, not criticism. Perhaps the child's performance at school will drop - a patient attitude on the part of parents is important. If necessary, the psychologist will help to work with the school to make it part of the treatment team. nine0003
What to do if the child does not go to the dialogue?
If a child perceives parental involvement as interference and does not want to talk to them about OCD, it is important to remember that this does not indicate parental rejection, but only the presence of a disorder. Also, such behavior may indicate the next stage of development through which children go, in which case parents have nothing to worry about.
Distinguish between a bad day and OCD and don't attribute everything that goes wrong to the disorder.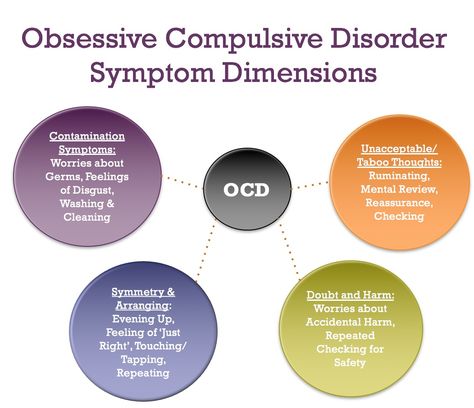 Parents need to take care of themselves. If there is a child with a severe form of OCD in the house, then if possible, it is worth taking turns with other family members to meet the needs of the child so that OCD does not "burn out" someone alone. nine0003
Parents need to take care of themselves. If there is a child with a severe form of OCD in the house, then if possible, it is worth taking turns with other family members to meet the needs of the child so that OCD does not "burn out" someone alone. nine0003
Treatment can often be provided through parents, especially in very young children. The state of mind of the parents, discomfort about what is happening to their child, poor relations between parents and children make the psychologist intervene directly in the work with the child. If one of the two partners does not participate in the treatment, then it is possible to agree that he/she does not interfere and invite him/her to cooperate after a while.
Acceptance principles
One of the tools for acquiring emotional self-regulation skills is the “STOP” skill:
- C (stop) : stop, freeze, do not react and do not move. Emotions can prompt you to do or say something without thinking it through.

- R (now take a break) : take a deep breath, step back from the situation and control emotions.
- O (look around) : identify and become aware of what is happening inside and outside of us: what is happening here and now, what thoughts and feelings I have, what am I being told to do or say? nine0168
- P (continue with mindfulness) : to make a wise decision, we must integrate our emotions and thoughts, as well as our goals, objectives and values, and ask ourselves what action will make the situation better and what will make the situation worse?
People avoid painful thoughts, feelings, and situations where they feel fear, anger, shame, sadness, because they think they can't do anything to change it, and that they can't stand this feeling at the moment.
Acceptance is the acceptance of facts as they are.