Obsessive compulsive reading
Reading OCD: A Confession of Why I'm Not Reading
mental health | OCD | trouble reading
ByLucy Last updated on
A quick note that some of my posts contain Amazon affiliate links. When you buy through these links, I may earn a commission.
Yesterday evening I was planning to wind down with my Kindle and a cup of my ‘buenas noches’ tea. I’ve been looking forward to reading Brené Brown’s Daring Greatly for a long time now, ever since I first watched her TED talks, and I think it’s the perfect time for me to learn from her lessons on vulnerability. I’ve also been wanting to get on with other books that are in varying states of progress.
There’s just one problem: my mind is doing everything it can to stop me from reading.
Last night, I settled down with the Brené Brown book readily downloaded on my Kindle and I read the first sentence. I wasn’t sure I had read it properly, so I read it again. I moved on to the next sentence, but then I couldn’t remember what happened in the sentence before, so I went back to the beginning. I moved on to the next sentence, then the whole process repeated again.
With each sentence the tightness in my chest grew stronger, alongside the growing panic that I hadn’t understood it properly or read it correctly. This isn’t the first time it’s happened by any means: the last few months I’ve experienced it almost every moment I’ve spent reading. I know it doesn’t make sense at all and it sounds really pathetic, but I’m struggling to work out how to control it. And it’s intensely painful.
Perhaps now it makes sense to you why I’ve only read five books since the start of August. I’ve been reluctant to admit that I’ve been facing this problem, and I haven’t really let myself think about it, let alone tell anyone else. I can tell that it’s bad because I’ve only just Googled it: normally I’m the first person to type my symptoms into a search engine and become paranoid about all the possible problems.
I can tell that it’s bad because I’ve only just Googled it: normally I’m the first person to type my symptoms into a search engine and become paranoid about all the possible problems.
Google provides the following answer by Jonathan Grayson, Ph.D., as outlined on a a blog by someone who seems to be experiencing exactly the same thing as me:
“The core of the problem is having the feeling that you don’t understand what you read. As a result, you reread a sentence or a word over and over before going on to the next sentence. Unfortunately, this contributes to destroying the flow of what you are reading, so the feeling of understanding becomes even more unattainable. Generally, the more important the material, the greater the anxiety. Schoolwork becomes torture.”
Now that sounds familiar.
I’ve never really talked about my mostly mild OCD much here on the blog (update: other than in this list of books to read if you have OCD). I’ve also never pursued dedicated help for it, apart from being diagnosed a few years ago. My anxiety and PTSD have felt like bigger issues, and I feel like working on these in therapy should also help my OCD.
I’ve also never pursued dedicated help for it, apart from being diagnosed a few years ago. My anxiety and PTSD have felt like bigger issues, and I feel like working on these in therapy should also help my OCD.
In my early teenage years, it was a need for neatness and order that affected me. I’d spend hours arranging drawers and smoothing the creases from my bed. I’d be on the verge of tears if someone moved my pencil case from how I’d put it on my desk. It was absolutely the stereotypical ‘OCD’ behaviour that the media usually jumps to, which I know isn’t accurate for many others. But things were out of control, and I was desperate to control what I could. I really needed to read Marcus Aurelius and his Meditations back then.
At university, I became terrified that I’d sleepwalk and end up outside my halls of residence. I’d spend way too much time before bed putting my desk chair in front of my door and something in front of the window to stop me from going near it.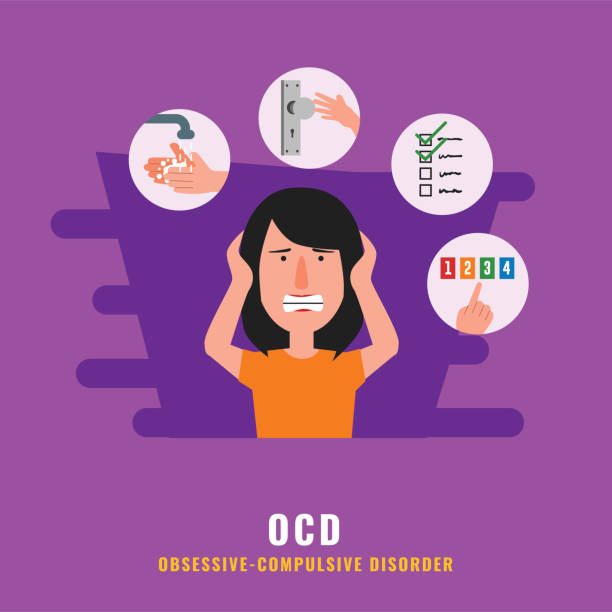 I would check the doors and windows again and again. It was almost laughably bad luck that I dropped the window key out the window and into a drain underneath.
I would check the doors and windows again and again. It was almost laughably bad luck that I dropped the window key out the window and into a drain underneath.
These habits persisted throughout both my first and second years of university, and my nighttime anxiety developed into fears that people I loved were in danger. If I didn’t count in a certain way (usually groups of four), a family member would fall sick. And I couldn’t just do it once and everything would be ok: I’d have to repeat the counting until it felt right. That could take a while.
About a year ago I started needing to tap my forehead in groups of four a certain amount of times whenever bad thoughts came to me. If you ever met me and saw me tapping my forehead and trying my hardest to make it look like I was scratching an itch or moving my hair, that’s what was going on. I’m embarrassed to say it still happens quite a lot.
It’s fairly easy to understand why I keep all of this quiet from people. The tidiness and the furniture rearranging and the bad thoughts and the head tapping have all been – and often still are – very hard to deal with, but not being able to read is by far the worst-case scenario
for me.
The tidiness and the furniture rearranging and the bad thoughts and the head tapping have all been – and often still are – very hard to deal with, but not being able to read is by far the worst-case scenario
for me.
Unlike my other compulsions, I don’t get any sense of order or relief from giving in and reading sentences over and over again. The stress just gets higher the longer I spend with the book, and I’m so angry with myself that I’ve let this develop into a ritual. But the thing is, by the time I realise that something has become a ritual, it’s already a full-blown problem.
I’m looking into solutions, and particularly into whether this is something I can deal with on my own. I know that I’m going to have push myself and go ahead with what scares me. I’m aware that it’s going to be challenging, and probably exhausting too. Even writing this post has made me feel incredibly vulnerable, and it’s going to take a lot of courage to press ‘publish’.
I know I’m going to have to dare greatly, and so I might as well start by reading the Brené Brown book.
Enjoy more from me
- Retreat into my new book, Your Life in Bloom: Finding Your Path and Your Courage, Grounded in the Wisdom of Nature.
- I'm also the author of Mountain Song: A Journey to Finding Quiet in the Swiss Alps, a book about my time living alone by the mountains.
- If you love books, are feeling a little lost right now, and would love some gentle comfort and guidance, join The Sanctuary, my seven-day course to rebalance your life.
Lucy
It's good to meet you! I started Tolstoy Therapy back in 2012 to share my healing journey through anxiety and PTSD with books. I also climb mountains, go on solo adventures, and write over at livewildly.co. In 2020, I published Mountain Song: A Journey to Finding Quiet in the Swiss Alps.
Reading with OCD - Dealing with Disorder
Share This Post
Reading with OCD can pose a challenge. It could be the need to go back and read sections again or read in a particular way. Perfectionism may lead to starting over if mistakes are made.
The following article is anonymous. Our aim is to help people understand how normal certain thoughts are, and to know that professional help can improve daily life.
As a child I loved escaping into a book. Reading with OCD however made this process a lot more complicated than it should have been.
There was a specific routine I had to do every single time I bought a new book.
I have to read books in a particular order
As a child I had to read a book in the following order:
- Front Cover
- Back Cover Blurb
- The pages before the first chapter (foreword, who the book is dedicated to or in memory of etc)
- Introduction
- First Chapter
If I missed one part of the routine, I had to start again.
If I made a mistake such as mispronounce a word, back to the start. If someone interrupted me, back to the start too.
I would have a strange feeling inside that wouldn’t go away if I didn’t start the book in this exact order, or if I made a mistake.
My earliest memories of reading books are full of these behaviors. Although I loved nothing more than finding a good book (Goosebumps and Horrible Histories were some my fave series), the fun never lasted too long.
This order was vital for me to keep reading. There wasn’t another way I could read that I would be happy with. The book felt dirty.
Obsessive-compulsive behavior was, and still is, a problem for me.
I would make up 'checkpoint's' in my mind that I had to reach
If I could make it to the first chapter without making a mistake or messing up the order of things, I hit my first ‘checkpoint‘.
I would create checkpoints in both reading and gaming. Once reached, I could start from this point if I made any further mistakes.
Once reached, I could start from this point if I made any further mistakes.
I think deep down even my OCD knew that having to start again every time I made an error would mean it would be almost impossible to finish a book.
Any mistakes after that would mean I start from this new checkpoint, although the compulsion to do so would ease as I progressed through the book.
Usually by the time I got into the second or third chapter, I wouldn’t feel these compulsions so strongly.
I could often relax after mistakes and have little to no desire to start from the last checkpoint, which would tend to be the beginning of that chapter.
I would keep going back to make sure I didn't miss something
Although I knew deep down that any text before the introduction was not important, I would worry about missing something vital if I didn’t check anyway.
What if I miss something in the cover art? Who is the author dedicating the book to?
I know I’m not the only one to read these pages in-between, but I could not skip them.
I would just feel uncomfortable if I didn’t read every single word before the introduction. Going back later was not an option due to the order of things.
This constant feeling that something wasn't right
This ‘feeling’ I have after making a mistake is pretty hard to describe.
I wasn’t feeling a lot of anxiety taking over, it was more like a low-key alarm bell that was going off in my mind. I couldn’t ignore it. That off switch wasn’t there.
Also, if I was to finish the book with this mistake being made, the book would always seem dirty to me. I wouldn’t be able to look back at it with joy, even if I knew it was a great read.
Throughout my twenties I rarely picked up a book, mainly for this reason. However ADHD also made it very difficult to concentrate, and now I usually listen to podcasts.
I find it easier to take in audio without having to read words from a page. I can also listen on the move.
Share This Post
Needing support? Click here to be directed to the support finder, wherever you are in the world.
More reads:
Music OCD: Obsessions with songs and listening routines
Do you feel music is only enjoyable if listened to in a very specific way? You may have songs you have to
Read More »
Understanding Transgender OCD
Transgender OCD involves intrusive thoughts around gender identity. Examples of this subtype include the worry that one is secretly transgender and denying
Read More »
Door checking OCD
Door and lock checking can be an exhausting compulsion, usually done when leaving the home or going to bed. Intrusive thoughts about
Read More »
Thank you for your support
Support on Patreon
symptoms, how to get rid of and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, it all came to naught, and as a teenager, I decided that it was just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is Obsessive-Compulsive Disorder - Mayo Clinic
Obsessive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed. Do I have OCD?
Sergey Divisenko
psychotherapist
If a person's condition does not interfere with himself or others, then everything is in order, if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasurable. The fact that an action will help reduce anxiety is not considered pleasant in this sense.
- Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number.
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other drugs: tranquilizers, neuroleptics or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive behavioral therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16, 2003 No. 438 "On psychotherapeutic care"
Psychiatrists, psychotherapists and psychologists are involved in the treatment of OCD in Russia. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn.:strip_icc():format(jpeg)/kly-media-production/medias/3650367/original/050840200_1638416728-obsessive-compulsive-disorder-concept-illustration_114360-3650.jpg) I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
My young man, seeing all this, insisted that we try to see a psychologist.
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
How a visit to a neuropsychiatric dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons.
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalization My condition worsened, I tried to ignore obsessive thoughts.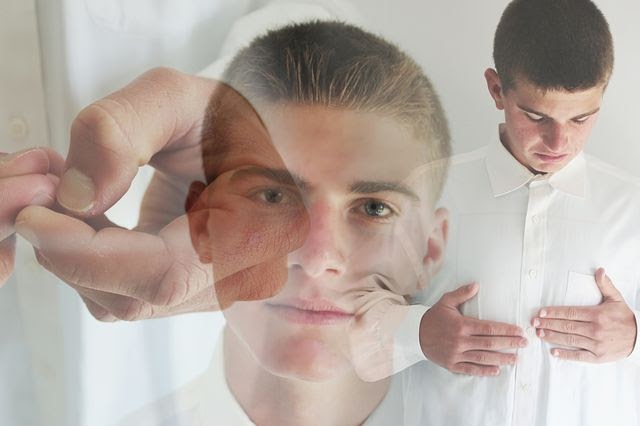 But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital.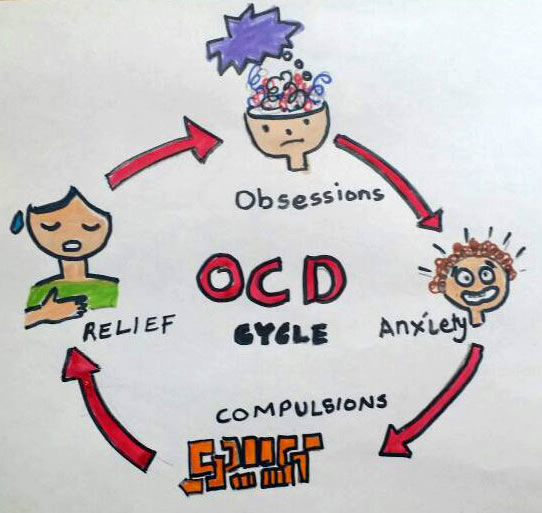 But there was no strength to argue with the psychiatrist.
But there was no strength to argue with the psychiatrist.
The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription.
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them.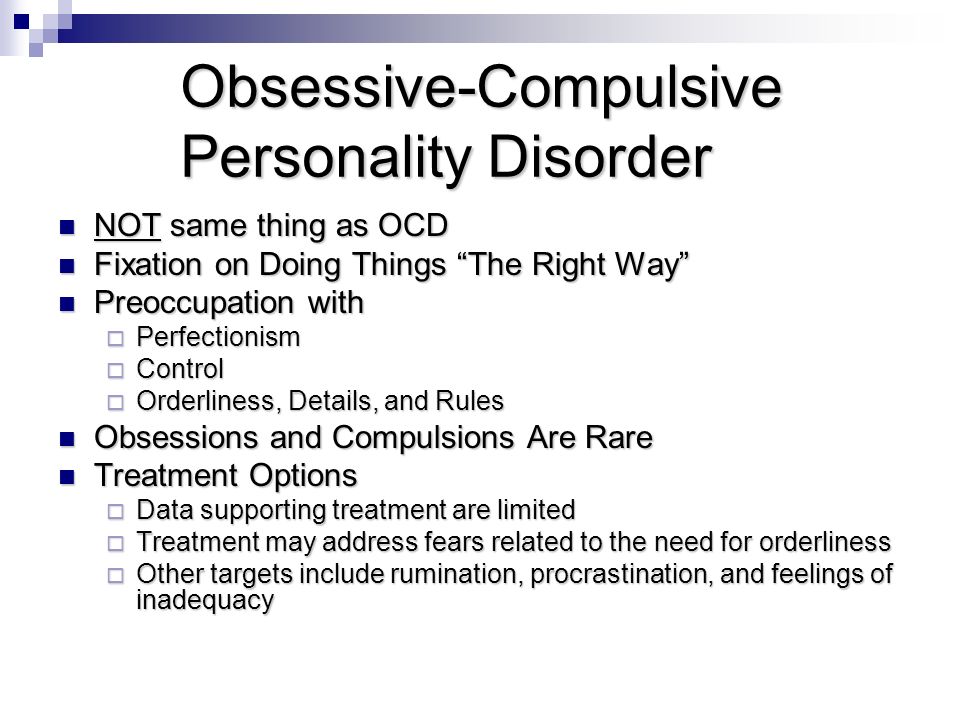 Usually the registrar complied with my request.
Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 R |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refused
When I wanted to buy one more to have a supply, the pharmacist refused Treatment
Second hospitalization and psychotherapyAfter six months of outpatient treatment, the district psychiatrist recommended to be treated again in the hospital. Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
/psychotherapy-search/
How to choose a psychotherapist
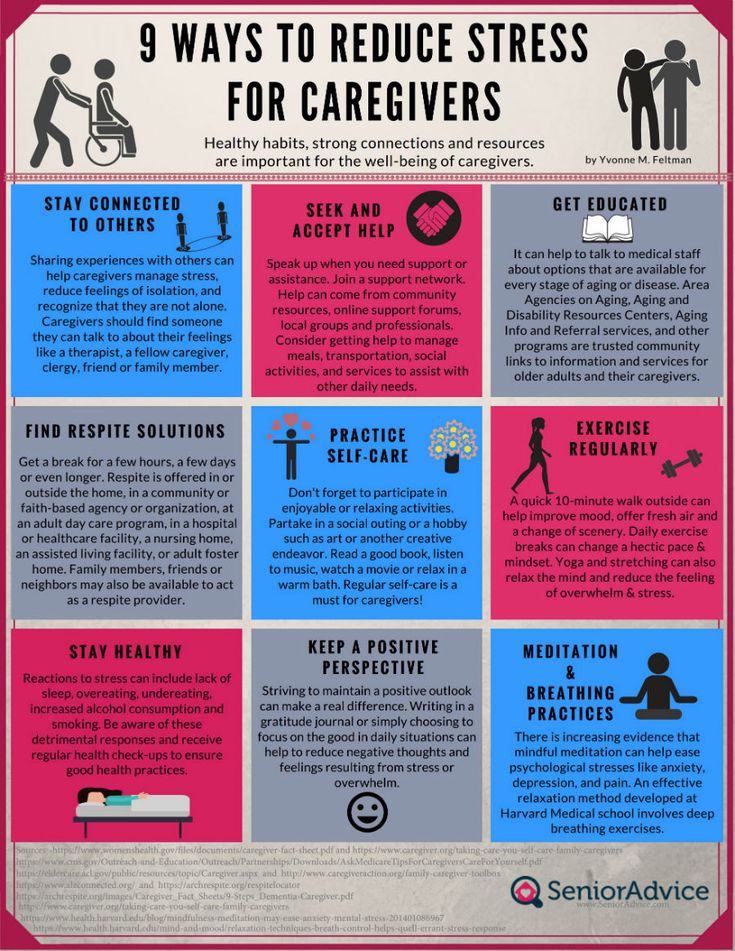
We agreed that I would try to keep the number of compulsive acts to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How much does psychotherapy cost? Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary.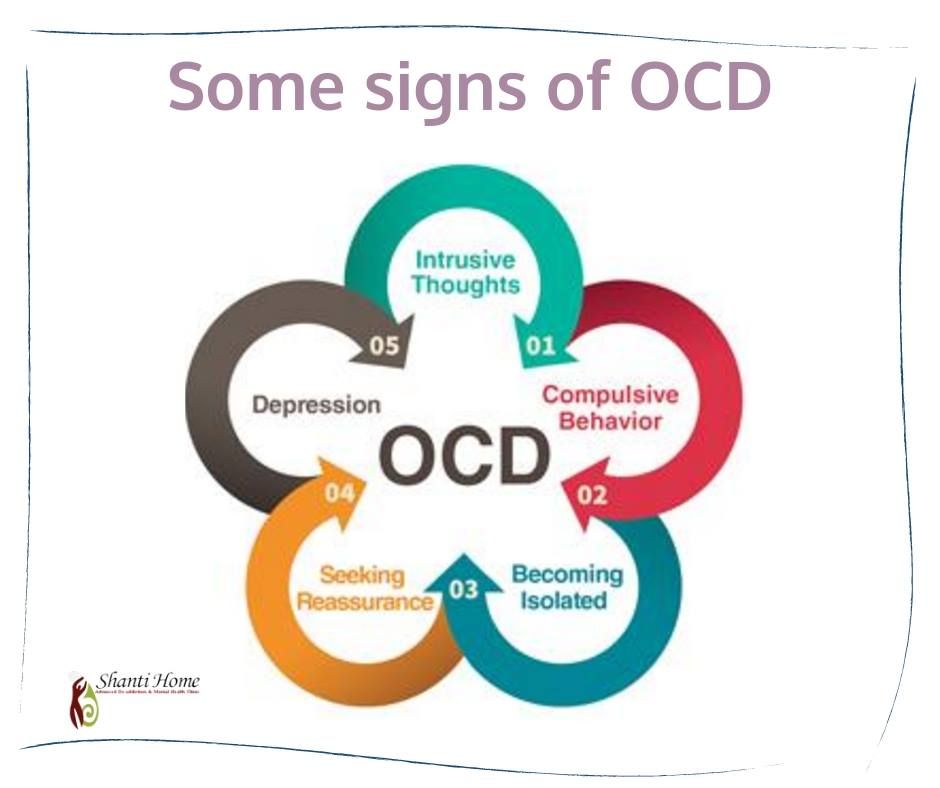 Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenditures | Spending |
|---|---|
| Antidepressants | 2422 P |
| Transport | 780 Р |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis.
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenditures | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
| Transport during hospitalization | 1380 Р |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
- OCD is considered a lifelong disorder, but remission can be achieved with the help of psychotherapy and drugs.
- OCD is treated in Russia by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
- A visit to a neuropsychiatric dispensary will not prevent people with OCD from moving freely, driving a car, using weapons, or getting a job.
- Patients with OCD can receive care free of charge in state neuropsychiatric dispensaries or at their own expense in private clinics.
Did you also have an illness that affected your lifestyle or attitude? Share your story.
Tell
Obsessive Compulsive Disorder | Blog 4brain
Obsessive Compulsive Disorder (OCD) is a mental illness that occurs when a person enters a cycle of obsession and obsessions. Obsessions or obsessions are intrusive thoughts and urges that cause intense distress. Compulsive behavior is defined as behavior by which a person tries to get rid of obsessions or reduce suffering.
Compulsive behavior is defined as behavior by which a person tries to get rid of obsessions or reduce suffering.
Most people experience obsessions or compulsive behaviors periodically throughout their lives. However, this does not mean that they suffer from OCD. For a diagnosis to be made, the cycle must be extreme, last for a significant period, and interfere with important activities the person is engaged in. That is, if obsessions or compulsive behaviors last more than one hour a day, then this can be considered alarming signals. Let's take a closer look at OCD. You will learn how the disease appeared, what its symptoms are and how to deal with it.
The Self-Knowledge online program will help you get to know yourself, your strengths and weaknesses.
Discovery of the disease
In the fourth century BC, Hippocrates coined the term melancholy. With it, he characterized those people who faced unfavorable living conditions and entered into an uncontrollable emotional state of alienation. Such people experienced mental anguish and were obsessed with an idea, thought, memory, or desire. In the Middle Ages, such people were considered possessed.
Such people experienced mental anguish and were obsessed with an idea, thought, memory, or desire. In the Middle Ages, such people were considered possessed.
Beginning in the seventeenth century AD, scientific papers began to appear in publications on various types of obsessive-compulsive disorders. At first, an obsessive fear of death and various forms of religious insanity were described. After obsessive-compulsive disorders became too much and in the 19th century they all fell into the category of "neurosis". Further, from the neurosis, the “disease of doubt” was singled out - an obsessive state that simultaneously influenced the will and intellect of a person.
By the 20th century, the “disease of doubt” included a long list of disorders that received different names in different countries. In France and Russia, the "disease of doubt" began to be called psychasthenia, in Great Britain and Germany - obsessive-compulsive disorder, and in the USA - obsessive-compulsive neurosis. Further, depending on the type of disorder, many classifiers were created, and now such a disease is commonly called obsessive-compulsive disorder or OCD. We are talking about it in the article.
Further, depending on the type of disorder, many classifiers were created, and now such a disease is commonly called obsessive-compulsive disorder or OCD. We are talking about it in the article.
Obsessions
OCD sufferers do not want to face intrusive thoughts and find them disturbing. In most cases, patients realize that these thoughts do not make any sense. Intrusive thoughts are usually accompanied by uncomfortable feelings such as fear, disgust, doubt, or a feeling that everything should be “right.”
In the context of obsessive-compulsive personality disorder, obsession is time-consuming and falls into the category of important activities that are valued by patients. This last part is important to remember as it determines if someone has OCD - a psychological disorder, not an obsessive personality trait.
Unfortunately, "possession" is a common term in everyday language. This use of the word means that someone is preoccupied with a topic, an idea, or even a person. "Possessed" in this everyday sense has no problems in everyday life and even has a pleasant component. A person may be "obsessed" with a new song, but it does not prevent him from living his daily life.
"Possessed" in this everyday sense has no problems in everyday life and even has a pleasant component. A person may be "obsessed" with a new song, but it does not prevent him from living his daily life.
In fact, studies have shown that most people have "unwanted thoughts" from time to time, but in the context of OCD they occur frequently and cause extreme anxiety that interferes with daily functioning. Let's single out the main groups of obsessions from which OCD patients suffer:
- Contamination or fear of infection through contact with something. It can be natural human secretions, various liquids, microbes, household chemicals, dirt, or anything else.
- Thoughts about losing control. Fear of harming oneself and others, fear of violent or horrific images, fear of insults, etc.
- Thoughts about the harm done and its consequences. Fear of starting a fire, stealing, dropping something, damaging or injuring someone.
- Obsessive perfectionism.
 Concern about evenness or accuracy, anxiety with the need to know or remember something, fear of losing or forgetting important information when throwing something away, inability to decide to keep or abandon the subject, fear of losing the thing.
Concern about evenness or accuracy, anxiety with the need to know or remember something, fear of losing or forgetting important information when throwing something away, inability to decide to keep or abandon the subject, fear of losing the thing. - Unwanted sexual thoughts and various forms of religious obsession.
OCD provokes too many different obsessions, so it will not be possible to define them in some general classification. There are people who constantly live in fear of getting cancer, at the sight of black they prepare for death, and at the appearance of the number six they sell everything and go on the run. These are all special cases.
Compulsions
Compulsions (compulsions) are the second part of OCD. These are the repetitive actions or thoughts that a person uses to neutralize, counter or eliminate their obsessions. People with OCD understand that this is only a temporary solution, but, having no better way to cope with their condition, they rely on compulsive behavior as a temporary salvation. Compulsions may also include avoiding situations that trigger obsessions. Compulsions are time-consuming and interfere with a person's important daily activities.
Compulsions may also include avoiding situations that trigger obsessions. Compulsions are time-consuming and interfere with a person's important daily activities.
Like obsessions, not all repetitive actions or "rituals" are compulsion. It is necessary to consider the function and context of behavior. For example, bedtime routines, religious practices, and learning a new skill all require some level of exercise repetition, but are usually a positive and functional part of everyday life.
The behavior depends on the context. Ordering books for eight hours a day is the norm if a person works in a library. Similarly, there may be "obsessive" behaviors that do not fall under OCD if the person is a detail lover or likes to arrange things neatly. In this case, "obsession" refers to personality traits. In OCD, compulsive behavior is carried out with the intent to avoid or reduce anxiety, to get rid of obsessions.
Consider a few examples of how compulsions can manifest themselves:
- Hygiene.
 Unnecessarily frequent showering, bathing, brushing teeth, grooming or going to the toilet. Cleaning household items or other activities to prevent or remove exposure to contaminants.
Unnecessarily frequent showering, bathing, brushing teeth, grooming or going to the toilet. Cleaning household items or other activities to prevent or remove exposure to contaminants. - Checks. Excessive control over the fact that the patient does not harm himself or someone else. Checking the position of certain parts of the body.
- Repeating the actions taken. Doing a task three times, because three is a “good”, “correct”, “safe” number.
There are as many variants of compulsions as there are obsessions. Some people will deal with the arrangement of things until it becomes "right." Others will seek reassurance that the other person will not take some action. Still others will make every effort to avoid situations in which obsessions may form. The fourth will come up with a more unusual option, the manifestation of which will depend entirely on the personality of the patient.
Symptoms
OCD affects men, women and children equally. Race, nationality and other ethnographic features of origin do not matter. OCD can start at any time, from preschool to adulthood. Doctors distinguish two age ranges when the disease first appears. The first range falls on the age of 8 to 12 years. The second range occurs between late adolescence and early adulthood.
OCD can start at any time, from preschool to adulthood. Doctors distinguish two age ranges when the disease first appears. The first range falls on the age of 8 to 12 years. The second range occurs between late adolescence and early adulthood.
Scientists still do not know the exact cause of OCD. There is an assumption that everything depends on the structure of the brain and heredity:
- If we talk about the brain, here scientists see a problem in the disruption of communication between the front of the brain and its deeper structures. Pictures were taken, and when OCD patients took medication, the brain circuits were partially restored and the person became better.
- If we talk about genes, they probably play a role in the development of the disorder: a relative suffered OCD → harmful chromosomes got to the receiver → the receiver is nine times more likely to get OCD than an ordinary person. This conclusion was made by an American research team that published their data in the Archives of General Psychiatry.

Almost nothing is known about the presence of other disease catalysts. It can be common illnesses and even normal life stresses that can trigger the activity of genes associated with OCD symptoms.
Treatment
Only qualified therapists can diagnose the disease, which requires a special psychological test and analysis to confirm. A self-diagnosis will almost always be erroneous and a person will not be able to deal with the problem. It usually only gets worse.
The most effective treatments for OCD include cognitive behavioral therapy (CBT) and medication. In some cases, treatment for obsessive-compulsive disorder may require other forms of therapy, including surgery.
The care you need is usually provided by a mental health professional on an outpatient basis. This means that the patient visits their therapist's office at the scheduled time one or more times a week. Medications may only be administered by qualified healthcare professionals who will work with a physician to develop a treatment plan.
When you can do without a psychotherapist
OCD is a serious mental illness that people often confuse with temporary and obsessive or compulsive tendencies. Trends are safe and affect most people from time to time. To cope with them, try to adhere to the following recommendations:
- Accept that you are unable to control the thoughts that come to mind. The more you try to get away from something, the more it haunts you. Stop and try to focus on some work.
- If the work did not help, switch to visualization. Imagine yourself on the platform with many trains. Each train is some kind of obsessive thought that is going to take you in an unnecessary direction. Watch these trains, but don't get on any of them. By doing this, you will strengthen your inner confidence and make sure that you can decide for yourself what thought and how to respond.
- Perform a written analysis after visualization. Write down what thoughts are bothering you and why.