Natural prevention for migraines
15 Natural and Home Remedies for Migraine Relief
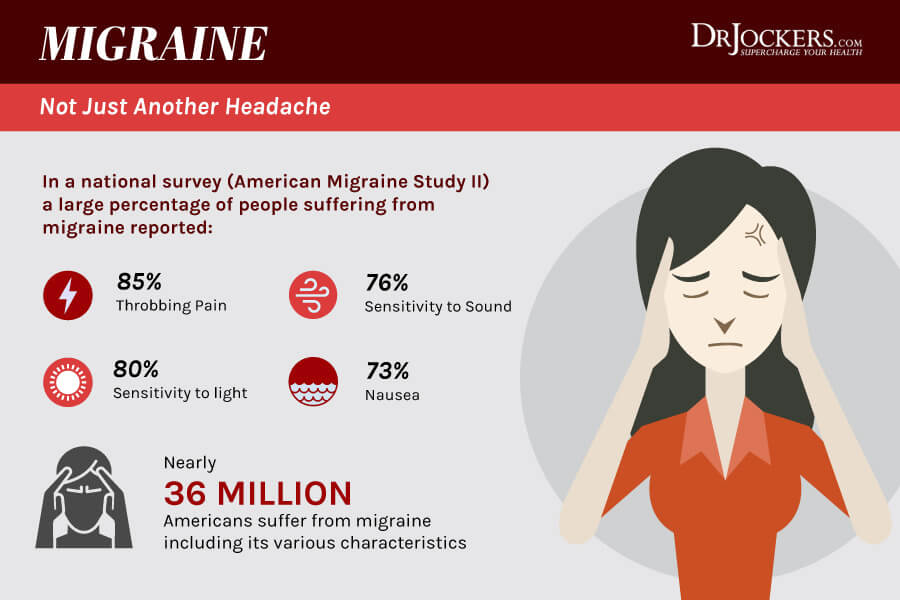
Migraine attacks aren’t typical headaches. You may experience pounding pain, nausea, and sensitivity to light and sound. When a migraine attack or episode occurs, you’ll do almost anything to make it go away.
Natural remedies are drug-free methods of reducing migraine symptoms. These at-home treatments may help prevent the onset of migraine attacks or at least help reduce their severity and duration.
Keep reading as we take a look at 15 natural remedies that may help you manage migraine symptoms.
Note that migraine attacks may require treatment with prescription or over-the-counter (OTC) medication. Speak with a doctor about a treatment plan that works for you.
Diet plays a vital role in preventing migraine attacks. Many foods and beverages may be migraine triggers, such as:
- foods with nitrates, including hot dogs, deli meats, bacon, and sausage
- chocolate
- cheese that contains the naturally occurring compound tyramine, such as blue, feta, cheddar, Parmesan, and Swiss
- alcohol, especially red wine
- foods that contain monosodium glutamate (MSG), a flavor enhancer
- foods that are very cold, such as ice cream or iced drinks
- processed foods
- pickled foods
- beans
- dried fruits
- cultured dairy products, such as buttermilk, sour cream, and yogurt
A small amount of caffeine may ease migraine pain in some people. Caffeine is also in some migraine medications. But too much caffeine may cause a migraine attack. It may also lead to a severe caffeine withdrawal headache.
To figure out which foods and beverages trigger migraine attacks for you, keep a daily food journal. Record everything you eat and note how you feel afterward.
Inhaling lavender essential oil may ease migraine pain. Lavender oil may be inhaled directly or diluted with a carrier oil and applied in small amounts to your temples.
A 2016 randomized controlled study found evidence that 3 months of lavender therapy as a prophylactic therapy, meaning taken before a migraine attack begins, reduced frequency and severity of migraine attacks. However, research is still limited.
A 2020 review of studies published in the journal Phytotherapy Research examined the ability of various herbal treatments, including lavender therapy for migraine. The authors found mixed or limited evidence to support the use of butterbur and feverfew for treating migraine but didn’t note that current research supports the use of lavender.
According to the authors, many studies had a high risk for bias, and more high quality research is needed.
Acupuncture involves injecting very thin needles into certain parts of your skin to stimulate relief from a wide variety of health conditions.
A 2020 randomized controlled study found that 20 sessions of manual acupuncture along with usual care was more effective at preventing migraine in people with a history of episodic migraine without aura than sham acupuncture along with usual care. Sham acupuncture is a treatment where the needles are not inserted as deeply.
A 2016 review of 22 studies also found moderate evidence that acupuncture may reduce headache symptoms. In the results summary, the authors explain that if people had 6 days of migraine per month before treatment, it would be expected that they would have:
- 5 days with usual care
- 4 days with fake acupuncture or prophylactic medications
- 3 1/2 days with real acupuncture
Feverfew is a flowering herb that looks like a daisy. It’s a folk remedy for migraine. It still isn’t well-studied, but there is some evidence that it may be slightly more effective than a placebo for treating migraine.
It’s a folk remedy for migraine. It still isn’t well-studied, but there is some evidence that it may be slightly more effective than a placebo for treating migraine.
In a 2015 review of studies, which is an update of a previous 2004 study, the authors concluded that larger studies are needed to support the use of feverfew for treating migraine.
The authors note that one larger study published since the 2004 review found 0.6 fewer migraine days per month in people who took feverfew versus a placebo. They describe previous studies as low quality or providing mixed evidence.
The 2020 review of studies published in Phytotherapy Researchalso summarizes the finding on feverfew as “mixed.”
The chemical menthol found in peppermint oil may help prevent migraine episodes, although there’s a very limited amount of research.
A 2019 randomized controlled study compared the effects of nasal 4 percent lidocaine with 1.5 percent peppermint essential oil and a placebo for managing migraine symptoms.
The researchers found that 40 percent of people in the lidocaine and peppermint oil groups experienced considerable improvements in their symptoms, compared with only 4.9 percent of people in the placebo group.
The National Center for Complementary and Integrative Health notes that very little research has examined peppermint leaf, but a limited amount of evidence suggests topical peppermint oil may benefit tension headaches.
Ginger is known to ease nausea caused by many conditions, including migraine. It may have pain-relieving benefits for migraine attacks. According to a 2020 review of studies, one randomized controlled study found evidence that ginger may have beneficial activity.
More research is needed to understand the extent and usefulness of ginger for treating migraine-related pain.
Yoga uses breathing, meditation, and body postures to promote health and well-being. A 2015 study found yoga may relieve the frequency, duration, and intensity of migraine attacks.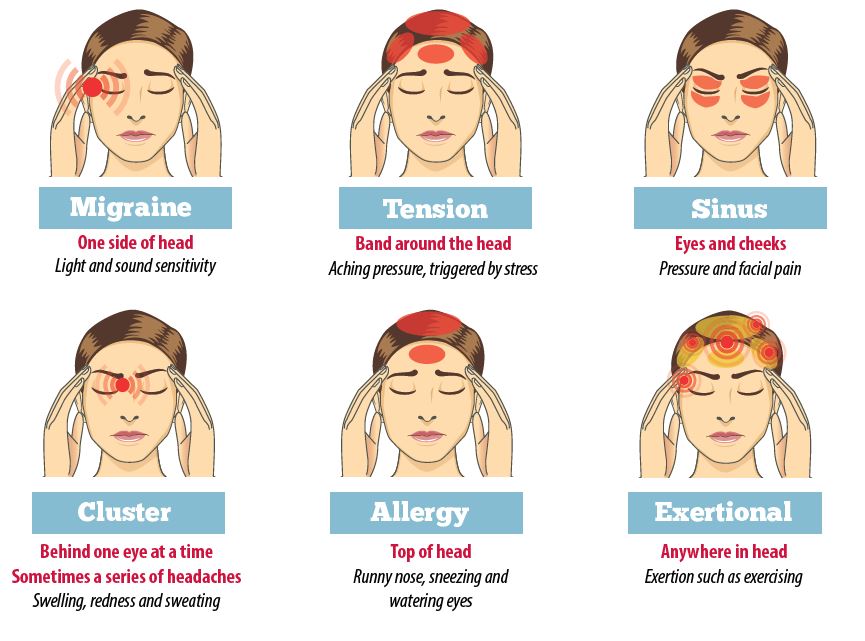 It’s thought to improve anxiety, release tension in migraine-trigger areas, and improve vascular health.
It’s thought to improve anxiety, release tension in migraine-trigger areas, and improve vascular health.
The researchers concluded that yoga could be beneficial as a complementary therapy for treating migraine.
Biofeedback is a relaxation method. It teaches you to control autonomic reactions to stress. During this therapy, electrodes are applied to your skin to monitor physiologic processes that change with stress, such as your heart rate, blood pressure, and muscle tension.
During a biofeedback session, you work with a therapist to manage stress using changes in your physiologic processes as feedback.
According to a 2019 study, there’s good evidence to support the use of mind-body interventions such as biofeedback and cognitive behavioral therapy for treating migraine. These therapies are effectively free of side effects and may make a good alternative for medication for some people.
Magnesium deficiency is linked to headaches and migraine. Magnesium oxide supplementation may help prevent migraine with aura. It may also prevent menstrual migraine (hormone headaches).
It may also prevent menstrual migraine (hormone headaches).
A 2021 study found that 500 milligrams of magnesium oxide taken twice a day for 8 weeks was as effective as the medication valproate sodium for preventing migraine without significant side effects.
You can get magnesium from foods that include:
- almonds
- sesame seeds
- sunflower seeds
- Brazil nuts
- cashews
- peanut butter
- oatmeal
- eggs
- milk
Massage may reduce migraine frequency. Migraine is associated with low serotonin in the brain, and massage has been shown to increase serotonin. There’s limited evidence to support the use of massage for migraine relief, but it’s generally safe and has a low risk of side effects.
Acupressure is the practice of applying pressure with the fingers and hands to specific points on the body to relieve pain and other symptoms.
A 2017 study found evidence that acupuncture may help manage migraine-related nausea during treatment, but that it doesn’t improve pain or quality of life.
According to the American Headache Society, more than 80 percent of people with migraine report stress being a migraine trigger. Learning how to better manage your stress may help you decrease migraine frequency.
Some commonly used stress management techniques include:
- deep breathing exercises
- mental imagery
- music therapy or listening to relaxing music
- counseling or therapy
- meditating
- progressive muscle relaxation
- improving time management
- scheduling more time for relaxing activities
According to the American Migraine Foundation, about a third of people with migraine report dehydration as a migraine trigger.
To prevent dehydration, make sure to drink plenty of water throughout the day, especially when exercising. On hot days, you may need to drink more water than usual.
The connection between sleep and migraine still isn’t entirely clear. Research from 2016 has found a correlation between high migraine frequency and poor sleep quality. This association is true in people with migraine with and without aura.
This association is true in people with migraine with and without aura.
Going to bed at the same time each night, avoiding caffeine late in the day, and avoiding stimulating activities before bed are some of the ways you can improve your sleep.
Butterbur is a plant that grows throughout Europe, Asia, and North America. Up until 2012, the American Academy of Neurology recommended using it for preventing migraine attacks. In 2015, they stopped their recommendation due to the possibility of liver toxicity.
The National Center for Complementary and Integrative Health recommends only using pyrrolizidine alkaloid-free butterbur products, as this chemical can damage the liver, lungs, and circulation. Speak with a doctor before taking butterbur.
If you have migraine, you know the symptoms can be challenging. You might miss work or not be able to participate in activities you love. But the remedies above may provide some relief.
It might also be helpful to speak with others who understand exactly what you’re going through. Our free app, Migraine Healthline, connects you with real people who experience migraine. Ask treatment-related questions and seek advice from others who get it. Download the app for iPhone or Android.
Our free app, Migraine Healthline, connects you with real people who experience migraine. Ask treatment-related questions and seek advice from others who get it. Download the app for iPhone or Android.
If your migraine attacks or episodes don’t respond to home remedies, it’s important to talk with a doctor. Visit a doctor if your symptoms are severe, frequent, or interfere with your daily life.
Migraine Herbal Remedies: Peppermint, Ginger, and More
Herbal remedies for migraines
If you’re one of the millions of Americans who experience migraines, you know they’re much more than just a headache. The intense throbbing, pulsing, and excruciating pain that accompany a migraine can be debilitating. In fact, more than 90 percent of people who get migraines can’t work or function normally during an episode, the Migraine Research Foundation reports.
Most people who experience migraines opt for medication. But many are turning to natural therapies such as relaxation techniques and herbal remedies.
Years before the introduction of modern medicine, cultures worldwide developed herbal remedies for headaches and other common migraine symptoms. Many of these herbal traditions have survived the passage of time. Although most herbal migraine remedies haven’t been thoroughly scientifically tested for their effectiveness, many are rapidly gaining the support of the modern medical community.
Always use caution when considering herbal treatments for migraines. Discuss your decision with a healthcare professional before beginning or stopping any medical or herbal treatment. Many herbs interfere with other medications.
First used in ancient Greece in as early as the fifth century B.C., feverfew (or “featherfew”) has been used to treat a variety of ailments. These include fever, swelling, and inflammation. People commonly took the herb to relieve aches and pains such as headaches in the first century.
The plant is native to the Balkan Mountains but can now be found nearly worldwide. Eastern European cultures traditionally used feverfew for headaches, insect bites, and other pain. More modern uses have extended to the treatment of:
Eastern European cultures traditionally used feverfew for headaches, insect bites, and other pain. More modern uses have extended to the treatment of:
- migraines
- dizziness
- inflammation
- breathing problems
Feverfew is usually prepared by drying the leaves, flowers, and stems. This combination is also used to make supplements and extracts. Some cultures eat the leaves raw.
A 2011 review suggests that feverfew is an effective treatment for migraines, fever, the common cold, and arthritis. However, a Cochrane review of five large clinical trials showed little to no benefit for the majority of people who experience migraines.
Feverfew may cause minor side effects such as bloating, canker sores, and nausea. You may also experience moderate side effects when discontinuing use. These side effects can include difficulty sleeping, increased headaches, and joint pain.
Pregnant women, people taking blood thinning medications, and people with allergies to the daisy family should avoid the use of feverfew.
Butterbur is found in wet, marshy areas of Europe, Asia, and North America. People once used the leaves of the plant to wrap and preserve butter during warm weather, which is how butterbur got its name. It’s been used throughout history for a variety of purposes. The Greek physician Dioscurides originally used the plant as a skin ulcer remedy. Since then, it’s been used to treat:
- headaches
- asthma
- allergies
- cough
- fever
- gastrointestinal problems
- general pain
Most butterbur herbal remedies use its purified root extract, Petasites, in pill form to treat headaches and migraines. A 2012 study published in Neurology supports conclusions from older studies that Petasites is effective for migraine prevention when taken as 50- to 75-milligram doses twice daily.
If you live in Europe, Butterbur might be hard for you to obtain — the U.K. and Germany have both banned butterbur from being sold because of safety concerns with the leading manufacturers.
A cross of spearmint and water mint, peppermint grows throughout North America, Europe, and Asia. Peppermint leaves and their essential oils are used for medicinal and culinary purposes. In addition to a headache treatment, it’s also used to relieve:
- spasms
- toothaches
- gastrointestinal problems
- nausea
Peppermint oil and its active ingredient, menthol, is available in liquid capsule form. Tea versions are also available for easy brewing.
A 2010 study published in the International Journal of Clinical Practice found that menthol was effective at stopping migraine pain and easing nausea when applied to the forehead and temples in a 10 percent solution.
Research is limited on its clinical effectiveness, but topical peppermint oil may be a good herbal option for the relief of migraine pain. Peppermint oil is one of the easiest herbal remedies to try because of its prevalence in health food stores and pharmacies.
Willow bark extract (WBE) was used in the development of aspirin, a well-known over-the-counter pain reliever, fever reducer, and anti-inflammatory drug. WBE contains an anti-inflammatory ingredient called salicin. A 2012 study suggests WBE is also an effective antioxidant.
WBE contains an anti-inflammatory ingredient called salicin. A 2012 study suggests WBE is also an effective antioxidant.
Willow is a tree found in Europe, Asia, and North America. It’s been used since the time of Hippocrates (400 B.C.), when people would chew the bark for its anti-inflammatory and fever-relieving effects. Willow was later used in China and Europe for headaches, osteoarthritis, tendonitis, and lower back pain.
Willow bark can be found in capsule form and as a chewable bark at most health food stores.
Ginger is a tropical Asian plant. It’s been used in herbal medicines in China for over 2,000 years. It’s also been popular in Indian and Arabic medicines since ancient times. Ginger has traditionally been used as a remedy for:
- headaches
- stomach pain
- nausea
- arthritis
- cold and flu symptoms
- neurological problems
Ginger has been well-documented as anti-inflammatory, antiviral, antifungal, and antibacterial. In addition, a 2014 study published in the Phytotherapy Research showed that ginger powder’s benefits were comparable to sumatriptan’s, a common prescription migraine drug, but with fewer side effects.
In addition, a 2014 study published in the Phytotherapy Research showed that ginger powder’s benefits were comparable to sumatriptan’s, a common prescription migraine drug, but with fewer side effects.
Most people can tolerate fresh or dried ginger root, supplements, or extract. Be careful not to combine ginger supplements with blood thinners because of potential drug interactions.
Ginger capsules and ginger tea are both relatively easy to obtain in almost any grocery store or pharmacy. You can also try drinking ginger water.
Caffeinated teas became common in China during the Ming Dynasty. They exploded in popularity in Europe during the 18th and 19th centuries. Green tea was used in combination with other herbs for migraine pain in traditional Chinese medicine. Coffee initially gained recognition in Arabia. Yerba mate, a less widely known caffeinated tea, originated in South America.
People in many cultures primarily consumed caffeine to help treat:
- headaches
- high blood pressure
- stomach problems
- sexually transmitted diseases
- cancer
- circulatory problems
- inflammation
- skin damage
- kidney disease
Caffeine is also found in many over-the-counter pain relievers today.
Although caffeine is frequently studied in combination with other pain relievers, it’s considered a useful and safe additive in pills for many people who experience migraines. A 2012 study found that a combination of 1,000 milligrams (mg) of acetaminophen and 130 mg of caffeine is particularly helpful. However, caffeine withdrawal and caffeine intake can also be triggers for headaches and migraines.
Valerian is native to Europe and Asia. It’s now also commonly found in North America. Use of valerian traces back to ancient Greece and Rome from the time of Hippocrates. It was recognized as a remedy for insomnia a few centuries later. Valerian was known as “all-heal” in the 1500s, as it was used to treat a multitude of ailments. These included:
- insomnia
- headaches
- heart palpitations
- tremors
- anxiety
It’s sometimes used in the modern treatment of headaches, but valerian hasn’t been researched enough to determine its usefulness in the treatment of migraine pain.
Valerian is usually taken as a supplement, tea, or tincture made from the dried roots. Liquid extract is also available in capsule form. Valerian root capsules are widely sold in the United States.
For over 7,000 years, people across cultures have used coriander seed’s healing and seasoning properties. Coriander was lauded for its ability to treat ailments that ranged from allergies to diabetes to migraines. Traditional Ayurvedic medicine used coriander to relieve sinus pressure and headaches by pouring hot water over the fresh seeds and inhaling the steam.
Research on the seed’s medicinal effects is generally focused on its potential to treat arthritis and diabetes. More studies need to be conducted to determine if it’s useful as a remedy for migraine pain. However, coriander seed’s anti-inflammatory potential may prove beneficial for some people with migraines.
Coriander seeds can be chewed and used in food or teas. Oral extracts are also available.
Hailing from the same family as carrots, parsley, and celery, dong quai root has been used as a spice, tonic, and medicinal cream for more than 1,000 years, especially in Japanese, Chinese, and Korean practices. Modern uses often mix it with other herbs to treat:
Modern uses often mix it with other herbs to treat:
- headaches
- fatigue
- inflammation
- nerve pain
Despite its history, the root hasn’t been studied enough to recommend it as an effective treatment for migraine pain.
Share on Pinterest
Known for its sweet smell, lavender oil (made from the flowers of the lavender plant) is highly fragrant and has long been used to perfume hygiene products. Lavender is indigenous to the mountainous regions surrounding the Mediterranean. It’s now widely grown throughout Europe, Australia, and North America.
Lavender oil was used in ancient Egypt during the mummification process. Because of its antimicrobial properties and clean scent, it was later added to baths in Rome, Greece, and Persia. The aromatic flowers and their oil were used to treat everything from headaches and insomnia to mental health complaints such as stress and fatigue. Many of these historical uses remain popular today.
A 2012 study suggests that inhaling lavender oil during a migraine may help relieve symptoms quickly. To use lavender oil, breathe in the oil or apply a diluted solution to the temples. If you don’t dilute it properly, the oil may irritate the skin at the application site. Lavender oil can be toxic when taken orally at certain doses.
To use lavender oil, breathe in the oil or apply a diluted solution to the temples. If you don’t dilute it properly, the oil may irritate the skin at the application site. Lavender oil can be toxic when taken orally at certain doses.
Share on Pinterest
Rosemary is native to the Mediterranean region. Medicinal uses have included the treatment of:
- muscle and joint pain
- memory problems
- concentration difficulties
- nervous disorders
- circulatory problems
- liver ailments
- migraines
Rosemary oil can be diluted and applied topically or inhaled for aromatherapeutic purposes. The plant’s leaves can be dried and ground for use in capsules. It can also be used in teas, tinctures, and liquid extracts. Rosemary is believed to have antimicrobial, antispasmodic, and antioxidant effects. Still, its ability to reduce migraine pain hasn’t been well studied.
Linden, also known as lime tree or Tilia, is a tree whose blossoms have been used in medicinal teas in European and Native American cultures.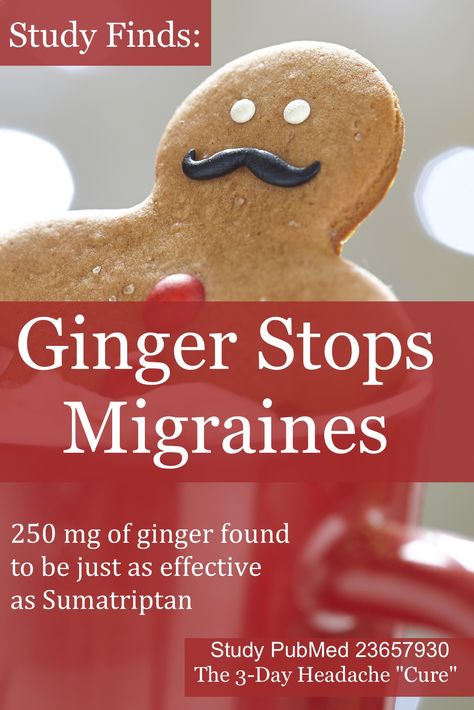 The plant has been used to calm nerves and ease anxiety, tension, and inflammatory problems, among other issues. The blossoms can also be used in tinctures, liquid extracts, and capsules.
The plant has been used to calm nerves and ease anxiety, tension, and inflammatory problems, among other issues. The blossoms can also be used in tinctures, liquid extracts, and capsules.
Linden has been shown to have sweat-inducing and sedative properties. It’s been used to relieve tension and sinus headaches, calm the mind, and induce sleep. The flowers have also been used to relieve nasal congestion and lower high blood pressure.
This tea is sometimes used in modern alternative medicine for the treatment of headaches and migraines. There currently isn’t enough research about the effect of linden tea on migraines to recommend it as an effective natural remedy.
The potato has been used in European folk medicine for over 200 years. Country folk medicine has anecdotally supported the use of thick slices of raw potato in calming migraine pain. Traditionally, the slices are cloaked in a thin cloth and wrapped around the head or rubbed directly on the temples to ease tension and pain.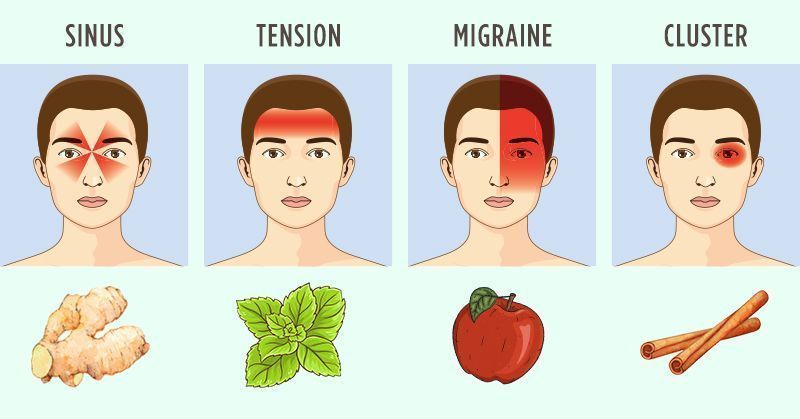 There is no current scientific research suggesting that raw potato cuttings can effectively treat migraines when applied topically.
There is no current scientific research suggesting that raw potato cuttings can effectively treat migraines when applied topically.
Share on Pinterest
Native to Europe, horseradish has been used in medicinal folk remedies as an oil extract or in dried or fresh root form. It has historically been used to treat:
- bladder infections
- kidney disease
- respiratory problems
- joint pain
- arthritis
- muscle strains
Its ability to narrow blood vessels may aid in treating migraines, but no clinical trials support the use of horseradish for migraines.
Native to Asia, the Japanese honeysuckle started taking root in North America in the 1800s. It’s been used in traditional Chinese medicine to treat:
- wounds
- fever
- colds and viruses
- inflammation
- sores
- infections
Along with honeysuckle’s anticancer and antimicrobial powers, research has also identified anti-inflammatory properties in the plant’s leaves, stems, and flowers that can provide pain relief similar to that of aspirin.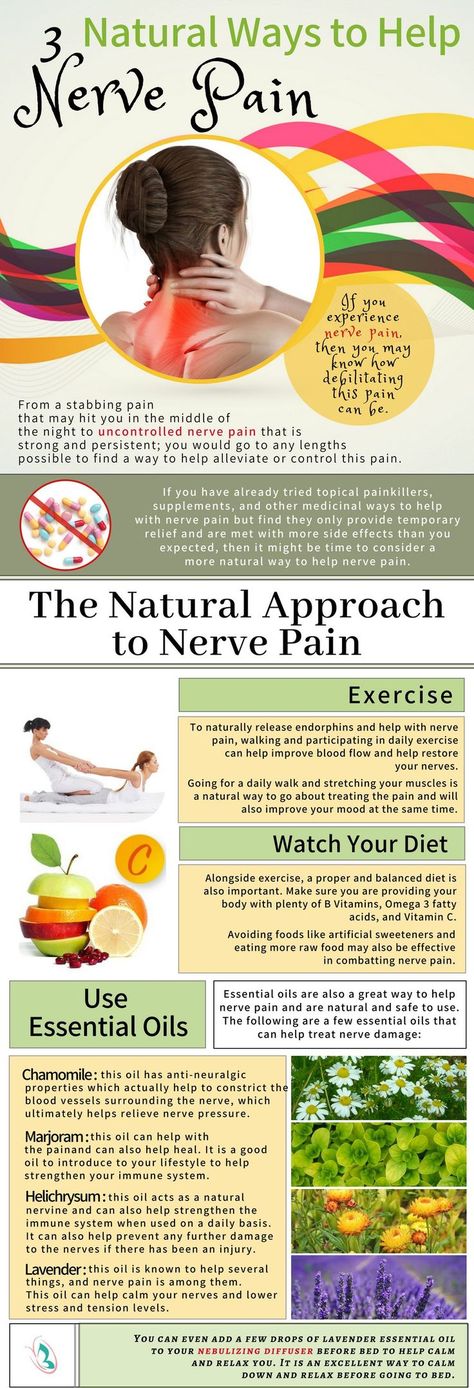 It may also be effective against migraine pain.
It may also be effective against migraine pain.
Since ancient times, people in Europe and Asia have been using mullein for medicinal purposes, treating inflammatory conditions, spasms, diarrhea, and migraines. The leaves and flowers can be used for extracts, capsules, poultices, and dried preparations. Tinctures of the plant are used in modern homeopathic therapies for migraine treatment. Research has shown that mullein has diuretic properties.
Believed to be named after Achilles, the Greek mythical hero, yarrow has historically been used to heal wounds and slow blood loss. Other folk remedies encourage the use of yarrow to treat inflammatory conditions, muscle spasms, and anxiety or insomnia. More recent folk remedies have used yarrow to relieve colds, flus, coughs, and diarrhea.
Yarrow has also been shown to have pain-relieving, anti-anxiety, and antimicrobial properties. Although more research is needed, the plant contains anti-inflammatory properties that may provide relief to people who experience migraines. Yarrow can be used in a variety of forms, including capsules and tinctures.
Yarrow can be used in a variety of forms, including capsules and tinctures.
Teaberry, popularly known as wintergreen, is native to eastern North America. This edible plant, made famous by Teaberry gum, has long held a place in folk medicine for its anti-inflammatory properties. It can be used to make teas, tinctures, and oil extracts.
Teaberry also has been used historically as an astringent and as a stimulant to fight fatigue. Most important for people who experience migraines is teaberry’s potential to treat neuralgias and headaches as well as stomach pain and vomiting.
You can brew teaberry in hot water for 3 to 4 minutes and drink the mixture to experience its healing effects.
Hops are native to Europe and western Asia and can now be found throughout North America. Once used as a food in ancient Roman culture, this flavorful plant also has significant medicinal properties. Hops have historically been used to treat:
- sleep problems
- inflammation
- infections
- neuralgia (pain from nerve damage)
- fever
- cramps
- spasms
- anxiety
Modern medicine acknowledges the sedative effect of hops, but hasn’t thoroughly studied it for its impact on migraine pain.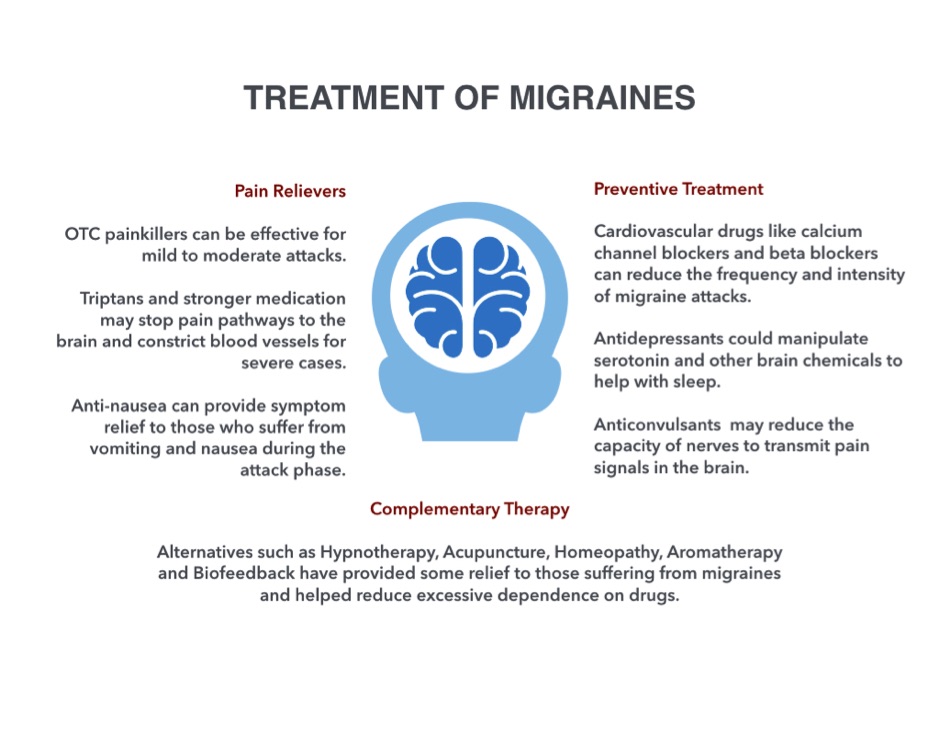
This perennial herb can be found throughout Europe and Asia. It’s been used as a medicinal plant since classical times. The plant has traditionally been used to relieve headaches and facial swelling and pain. The leaves can be used as a juice, poultice, or ointment.
The mildly sedative properties of the plant are used to treat headache and migraine pain, menstrual cramps, stress, and tension. It may help alleviate sinus headaches and congestion when used in combination with lime flowers and comfrey.
However, there have been no human clinical trials performed to demonstrate the plant’s effectiveness against migraine pain. It’s not always easy to find betony in health food stores, so you may have to grow your own or buy it online.
Betony can have a tonic effect on the body. It’s important to avoid the herb if you’re pregnant.
This deciduous tree is a native to China and has been used in Chinese medicine since the first century A.D. Evodia has traditionally been used to treat abdominal pain, headaches, diarrhea, and vomiting. The fruits of the tree may also reduce blood pressure. The anti-inflammatory and pain-reducing properties of the fruit may help ease migraine pain.
The fruits of the tree may also reduce blood pressure. The anti-inflammatory and pain-reducing properties of the fruit may help ease migraine pain.
Although many herbal remedies can be safe when used correctly, they may also have side effects like any prescription medication would. Some herbs can interact with medications, such as oral contraceptives or heart drugs. Herbs can be dangerous or even deadly when misused. Some have little research to back claims, verify toxicity levels, or identify potential side effects.
Migraine without aura
This is the most common kind of migraine headache. It builds over several hours before the pain of your migraine peaks, usually lasting up to 72 hours. People who have these kinds of migraines tend to experience them a few times per year. If they occur more often than that, the condition may be diagnosed as chronic migraine.
Migraine with aura
Some people experience disturbances of the nervous system, called aura, during their migraines.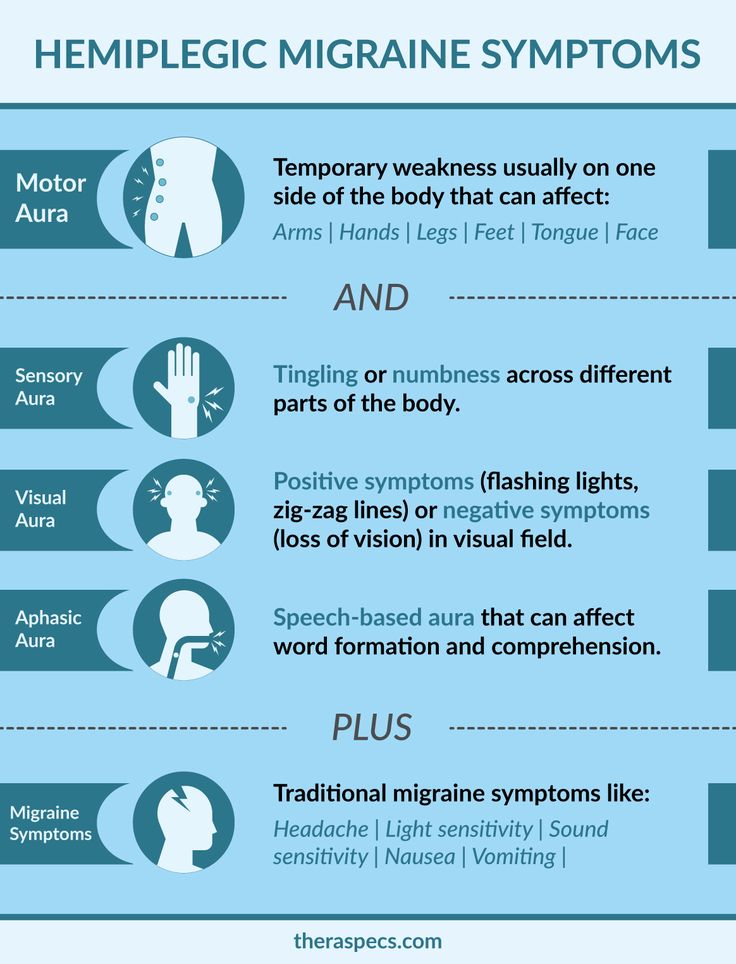 Auras can include bright spots in the field of vision, tingling sensations, vision loss, hallucinated odors, and uncontrolled movements.
Auras can include bright spots in the field of vision, tingling sensations, vision loss, hallucinated odors, and uncontrolled movements.
Retinal migraine
Retinal migraines involve vision loss in one eye. Unlike migraines with aura, the visual disturbances are usually contained to that eye.
Chronic migraine
Chronic migraine is defined as having migraines that occur on more than 15 days per month for 3 months or more. This frequency can be debilitating. Medical evaluation is required to obtain a treatment plan and to identify if something else is causing the migraines to occur so often.
Certain behaviors, emotions, hormones, and foods can trigger a migraine. Caffeine or chemical withdrawal can cause migraines, for example. Chocolate, food dyes and additives, preservatives, aspartame, and cured meats are the most common dietary triggers for migraines, according to the American Nutrition Association. Food allergies and sensitivities can also activate migraines as a symptom.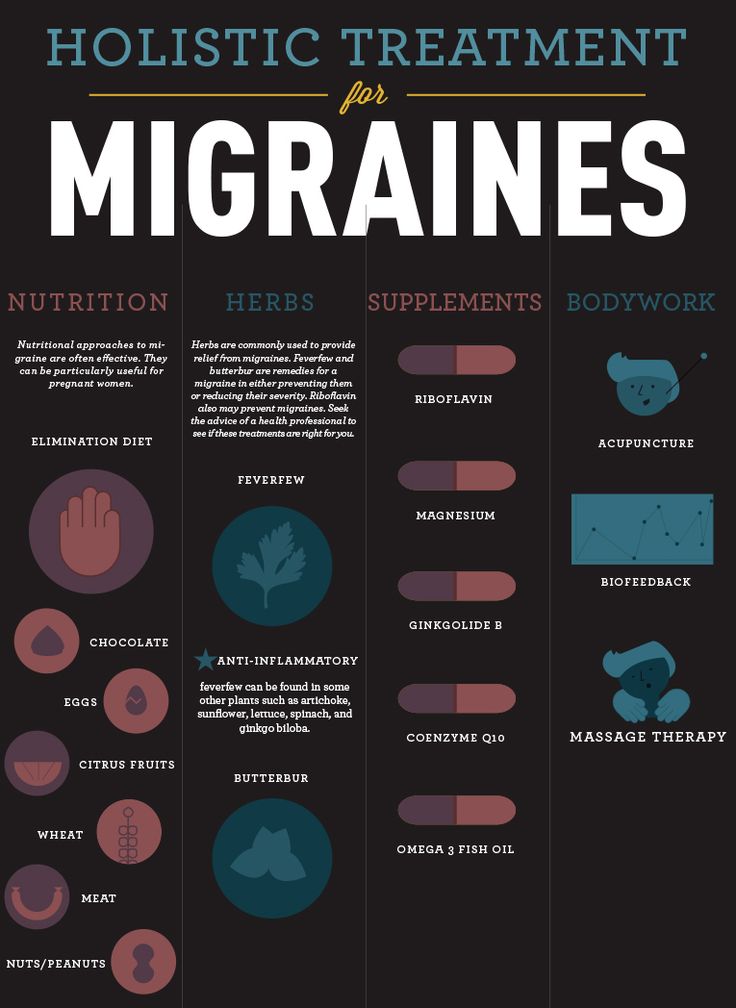
A high-stress, competitive lifestyle can sometimes lead to recurrent migraines. Emotional stress from chemicals released during emotional situations can provoke a migraine. Hormones are also a notorious migraine trigger. For women, the menstrual cycle is often connected to when their migraines occur. You may want to consider if there are migraine patterns or triggers that you can identify before you decide to try an herbal treatment.
In addition to herbal treatments, significant research shows that diet can play a major role in migraine frequency, duration, and intensity. Potential preventive measures and treatments for migraines include:
- eating a low-fat diet
- eliminating or limiting foods that show IgG antibody production
- improving gut flora content
- eating consistently to minimize low blood sugar
Just like medications, herbs can have significant side effects on the body. Some can interact with other medicines and be dangerous or even deadly when misused.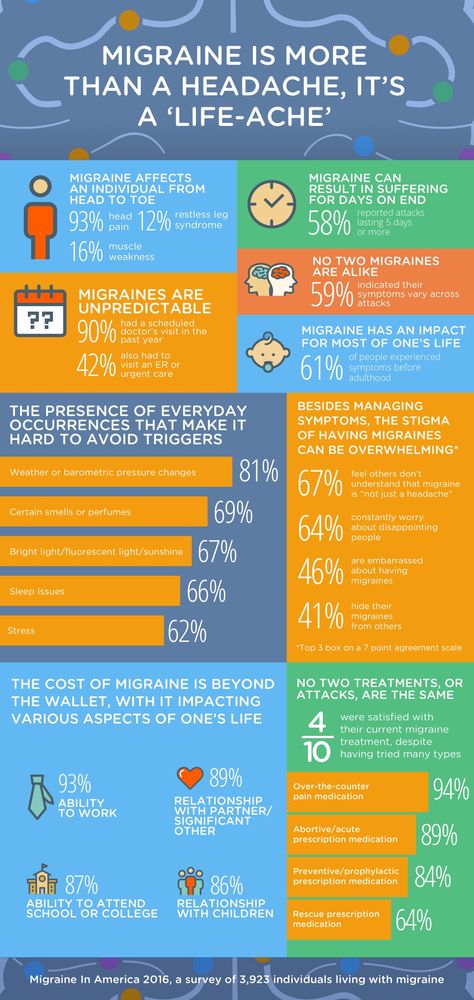 Discuss all treatment options with your doctor before use.
Discuss all treatment options with your doctor before use.
Consider tracking your triggers, symptoms, pain intensity and duration, and other related factors in a migraine journal or migraine app. Whether you choose pharmaceutical treatments, natural remedies, or a combination, having a thorough record of your experiences will help you and your doctor narrow down the best treatment options.
It might also be helpful to talk to others about their own experiences with migraines. Our free app, Migraine Healthline, connects you with real people who experience migraines. Ask treatment-related questions and seek advice from others who get it. Download the app for iPhone or Android.
Pharmacotherapy of menstrual migraine uMEDp
According to epidemiological studies, from 5 to 70% of women tell their doctors about the relationship between the occurrence of a headache attack and a certain period of the menstrual cycle (5, 6, 11). In this regard, both doctors and patients sometimes mistakenly believe that they are dealing with menstrual migraine (11). Moreover, there are works indicating a connection between changes in the level of female sex hormones and migraine (3, 6).
Moreover, there are works indicating a connection between changes in the level of female sex hormones and migraine (3, 6).
Table 1. Diagnostic criteria and characteristics of menstrual migraine
Figure 1. Algorithm for the treatment of migraine in women
Table 2. Characteristics of patients who participated in the study
Figure 2. Results of treatment of menstrual migraine with zolmitriptan and placebo
Figure 3. Number of recurrent headaches with zolmitriptan (red) and placebo (grey)
Table 3. Side effects during treatment
In childhood, migraine occurs with the same frequency in both boys and girls, but after the age of 15 it significantly predominates in women. The first migraine attacks appear with the first menarche in 33-40% of women. In the future, migraine attacks may appear a few days before menstruation, during it, in rare cases, during the period of ovulation. All of the above, plus the lack of clear diagnostic criteria, contributes to the overdiagnosis of menstrual migraine. The International Society for the Study of Headaches recommends that a migraine be called a true menstrual if an attack occurs only 2 days before or within 5 days of menstruation (Table 1). If migraine attacks occur during menstruation, but also occur on other days of the cycle, this form of the disease is called menstruation-associated migraine (table 1). nine0003
The International Society for the Study of Headaches recommends that a migraine be called a true menstrual if an attack occurs only 2 days before or within 5 days of menstruation (Table 1). If migraine attacks occur during menstruation, but also occur on other days of the cycle, this form of the disease is called menstruation-associated migraine (table 1). nine0003
The latest classification of headaches combines these two forms of migraine with the term menstrual migraine (4). Menstrual migraine differs from the usual attack in higher intensity, longer duration and more severe impairment of the woman's functional activity. In addition, an attack of menstrual migraine is much more difficult to stop even with modern treatments (5, 7).
There is still no single point of view in understanding the mechanisms of occurrence of menstrual migraine. Most researchers consider menstruation to be only a trigger that triggers the neurogenic and vascular mechanisms of migraine. It has been proven that estrogens are involved in the mechanisms of nitric monoxide and serotonin synthesis, which play an important role in the formation of vascular and neuronal processes that develop during a migraine attack (1, 2, 10, 13). nine0003
nine0003
Clinical studies have shown that increasing estrogen levels with injections of estradiol prevents the onset of menstrual migraine attacks, and reducing estrogen levels after discontinuation of the drug leads to their resumption (3, 8). Other data supporting the theory of estrogen deficiency are the occurrence of menstrual migraine in the pill-free week in women taking hormonal contraceptives, and the beneficial effect of pregnancy (high estrogen levels) on the course of migraine with the subsequent resumption of attacks after childbirth (decrease in estrogen levels). However, a number of studies have shown that menstrual migraine attacks also decrease or disappear after the use of estrogen-lowering drugs or during menopause (6). Recognizing the important role of cyclic fluctuations in estrogen levels in the formation of menstrual migraine, this mechanism should not be considered the main one, since hormone levels change in all women, and migraine occurs only in some. Probably, hormonal imbalance only facilitates the development of a migraine attack, increasing the implementation of the existing genetically determined predisposition, and menstruation is only a trigger for another attack. nine0003
nine0003
The modern algorithm for the treatment of migraine in women involves the relief of each attack of headache and the prevention of very frequent attacks in some patients. During an attack, analgesics, NSAIDs, and triptans are used (Figure 1). Currently, triptans are considered one of the most effective means for stopping a migraine attack. This class of drugs appeared at the end of the last century, and now seven triptans are registered for clinical use: almotriptan, sumatriptan, rizatriptan, eletriptan, zolmitriptan, naratriptan, frovatriptan. In Russia, sumatriptan (Imigran, Sumamigren, Amigrenin), eletriptan (Relpax) and zolmitriptan (Zomig) are used to stop a migraine attack. nine0003
All triptans are selective 5HT 1B/1D type serotonin receptor agonists located in the vascular wall and nervous system. Stimulation of these receptors blocks the main links in the pathogenesis of migraine, which leads to relief of headache, nausea, vomiting, photophobia and sound phobia. It is generally accepted that a migraine attack occurs due to the activation of the trigeminovascular system and, as a result, developing vasodilation and neurogenic perivascular inflammation. Headache after the use of triptans is relieved as a result of narrowing of excessively dilated arteries of the meninges, suppression of the release of vasoactive and inflammatory peptides, blocking the conduction of pain at the level of the brainstem. nine0003
It is generally accepted that a migraine attack occurs due to the activation of the trigeminovascular system and, as a result, developing vasodilation and neurogenic perivascular inflammation. Headache after the use of triptans is relieved as a result of narrowing of excessively dilated arteries of the meninges, suppression of the release of vasoactive and inflammatory peptides, blocking the conduction of pain at the level of the brainstem. nine0003
The high efficacy of triptans in migraine has been proven in numerous studies, but they did not reveal any obvious benefits of any of them. A small number of studies have been devoted to the study of the effectiveness of triptans in menstrual migraine (7, 9, 12). Nevertheless, a number of recent clinical studies have shown the high efficacy of zolmitriptan in menstrual migraine (9, 12). In one of them, 334 women took part, who in three months with the help of zolmitriptan tablets (2.5 mg) stopped 614 attacks of menstrual migraine (table 2).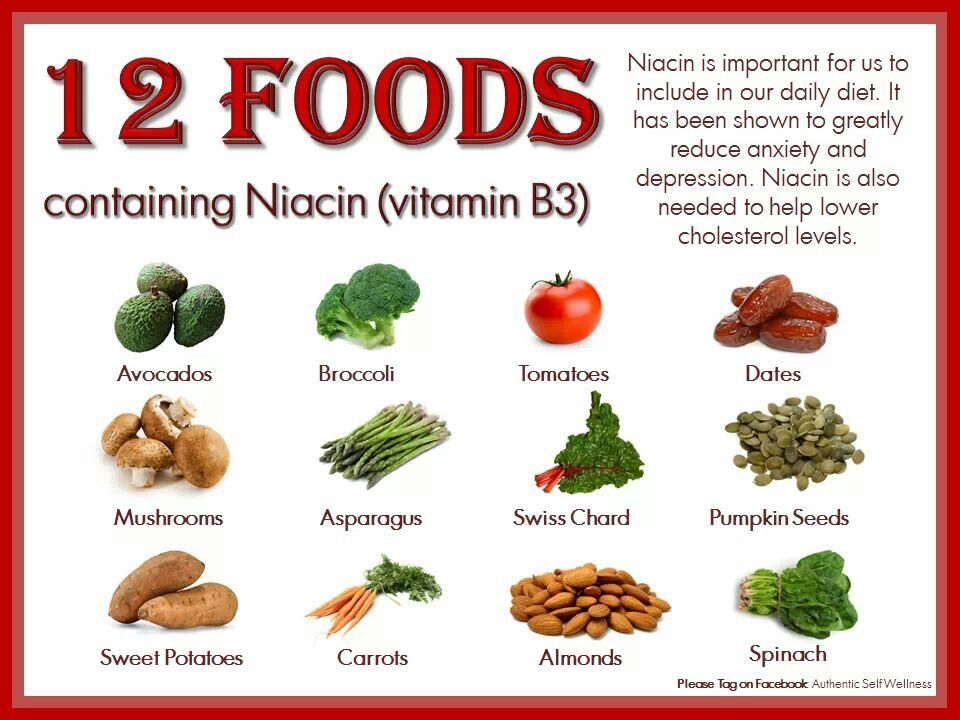 nine0003
nine0003
1 hour after taking zolmitriptan, 41% of women noted a positive result of treatment (pain relief or reduction of its intensity to insignificant), and after 2 hours this figure increased to 66% (Figure 2). Only 29% of patients noted a recurrence of a migraine attack after its successful relief (Figure 3). The good tolerability and safety of zolmitriptan was noted by the majority of women. The frequency and nature of side effects that occurred during treatment were insignificant compared with placebo (table 3). nine0003
The results of this study once again showed the high efficacy and safety of zolmitriptan in migraine, and, in particular, in one of its most severe forms - menstrual migraine.
Often, a headache that appears a few days before menstruation as part of premenstrual syndrome is mistakenly called menstrual migraine. As medical practice and the results of epidemiological studies show, headache in premenstrual syndrome often does not meet the criteria for migraine and is associated with other signs of this syndrome. These can be: dysphoria (mood changes, depression, anxiety, tension, bouts of tearfulness), feeling tired or exhausted, drowsiness, pain in the lower back, lower abdomen, edematous syndrome, constant hunger, eating too much salt, sugar or nausea. The appearance of premenstrual syndrome is associated with a lack of progesterone and, to a lesser extent, estrogen at the end of the luteal phase of the menstrual cycle, as well as an increase in the level of prostaglandins and a violation of the production of endorphins. nine0003
These can be: dysphoria (mood changes, depression, anxiety, tension, bouts of tearfulness), feeling tired or exhausted, drowsiness, pain in the lower back, lower abdomen, edematous syndrome, constant hunger, eating too much salt, sugar or nausea. The appearance of premenstrual syndrome is associated with a lack of progesterone and, to a lesser extent, estrogen at the end of the luteal phase of the menstrual cycle, as well as an increase in the level of prostaglandins and a violation of the production of endorphins. nine0003
The prevention of menstrual migraine and premenstrual syndrome is based on the principle of estrogen and progesterone replacement before menstruation and suppression of prostaglandin synthesis. Hormonal therapy for menstrual migraine and headache that occurs within the framework of premenstrual syndrome is carried out in the absence of a therapeutic effect from the use of NSAIDs and triptans or in order to enhance their action, and only after consultation with a gynecologist-endocrinologist (see Figure 1). Currently, the position is expressed that attacks of menstrual migraine can be prevented by maintaining a high level of estrogen (estrogen replacement therapy) or, conversely, by reducing it (natural/medicated menopause). Estrogen replacement therapy can reduce the frequency of menstrual migraine attacks by 3 or more times, and the low effectiveness of treatment may be associated with an incorrect definition of the type of headache or the wrong choice of hormone dose (6). nine0003
Currently, the position is expressed that attacks of menstrual migraine can be prevented by maintaining a high level of estrogen (estrogen replacement therapy) or, conversely, by reducing it (natural/medicated menopause). Estrogen replacement therapy can reduce the frequency of menstrual migraine attacks by 3 or more times, and the low effectiveness of treatment may be associated with an incorrect definition of the type of headache or the wrong choice of hormone dose (6). nine0003
Of course, menstrual migraine is one of the special and severe types of migraine, the pathogenesis of which remains insufficiently studied, and the role of female sex hormones in the origin of attacks remains unclear. Future experimental and clinical studies should be aimed at elucidating the mechanisms of menstrual migraine. We can be sure that effective relief of this severe form of migraine can be achieved with the help of modern drugs - NSAIDs and triptans (Zomig). However, the need to prescribe prophylactic treatment of menstrual migraine with the help of estrogens still needs to be investigated, especially in cases where a woman has no additional indications for hormone replacement therapy.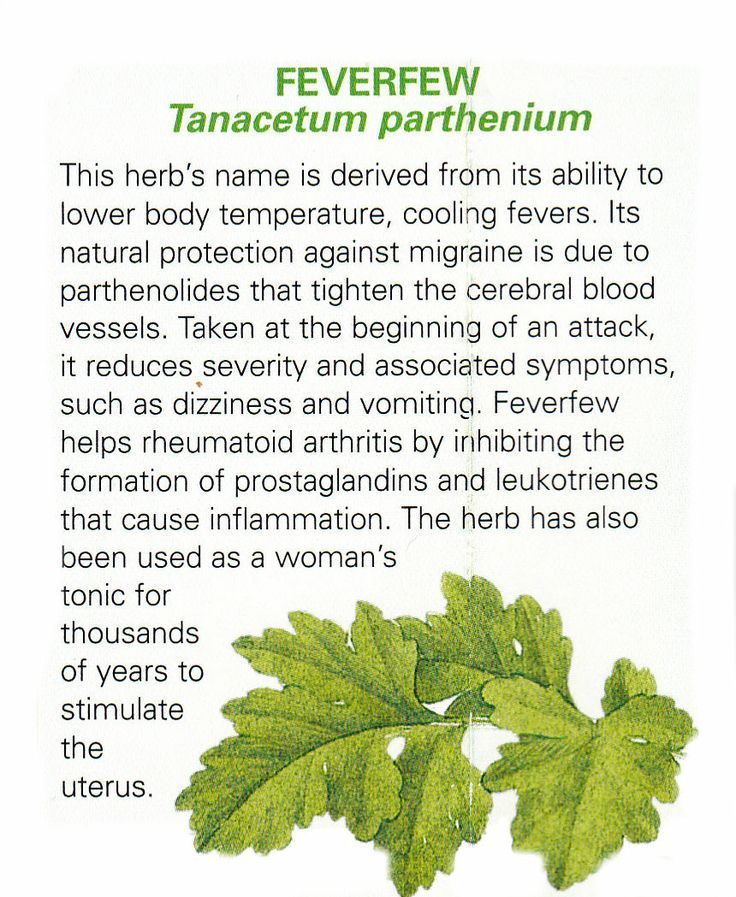 nine0003
nine0003
Headache / Diseases / Clinic EXPERT
Headache is pain in the head and/or neck. According to the latest scientific data, there are about 200 types of headache, many of which are well studied and can be both explicit and indirect signs of various diseases of the nervous system. Drinking a headache pill can only relieve the symptom, but not get rid of the cause of its occurrence.
Many people experience intermittent head and neck pain throughout their lives. According to statistics, during the year about 90% of people experience a headache at least once. Approximately 10-15% of the world's population is prone to migraine attacks, of which women are 3 times more than men. Overall, headache is 5 to 8 times more common in middle-aged men.
In most cases, such pain does not pose a threat to life, as it is a natural reaction of the body to overexertion or general overwork. But this does not mean at all that the problem can be “jammed” with pills for years without taking any measures.
nine0003
Acute pain in the head can be a terrible symptom of a stroke, traumatic brain injury, aneurysm rupture, neoplasms in the brain, meningitis, arachnoiditis, etc.
Infrequent headache attacks that are not intense, of an understandable nature and do not cause much discomfort, do not require a visit to a doctor.
Types of headaches
There is an international classification according to which all types of headaches are divided into primary and secondary (symptomatic):
- primary - an independent disease. These include migraine, tension headache, and cluster headache.
- secondary - a symptom of another organic disease.
Causes
The causes of primary headaches are not fully understood, so they are much more difficult to diagnose and treat than secondary headaches.
Causes of secondary headaches:
- dysregulation of vascular tone on the part of the autonomic nervous system (in practice, this means that the vessels cannot regulate their “adequate” diameter, i.
 e. they are either too narrowed or too widened) nine0060
e. they are either too narrowed or too widened) nine0060 - emotional or mental stress, neurosis-like and depressive conditions, inability to cope with stress and neck injuries (for example, whiplash injuries to the neck that occur during heavy braking during an accident).
- in osteochondrosis of the cervical spine and in violation of the tone of the muscles of the neck
- dental problems - from dental disease to vascular reactions in temporomandibular joint dysfunctions due to incorrect bite or prosthetics, etc.
- ENT pathology, e.g. sinusitis, both acute and indolent chronic, or inflammation of other sinuses may occur without abdominal pain, but it may be a headache that can signal it
- chronic viral infections, various intoxications, parasitic diseases
- use of birth control pills, a period of hormonal changes, long-term hormonal therapy can also be a source of headaches pain, the cause of which may be the presence of quite serious pathologies not only of the nervous system, but also of other organs and systems, require qualified medical care.
 nine0003
nine0003 Symptoms
Tension headache symptoms include:
- constant, non-throbbing pain
- feeling of tension and pressure in the head and neck
- discomfort that does not increase with physical and mental exertion or increases slightly
Symptoms of cluster headache:
- acute pain in the region of the eye of a constant nature, often recurring at the same time of the day
- redness of the eyes and swelling of the eyelids
- lacrimation
- nostril congestion on one side
Before a migraine attack, about 20% of people see flashes of light, bright spots.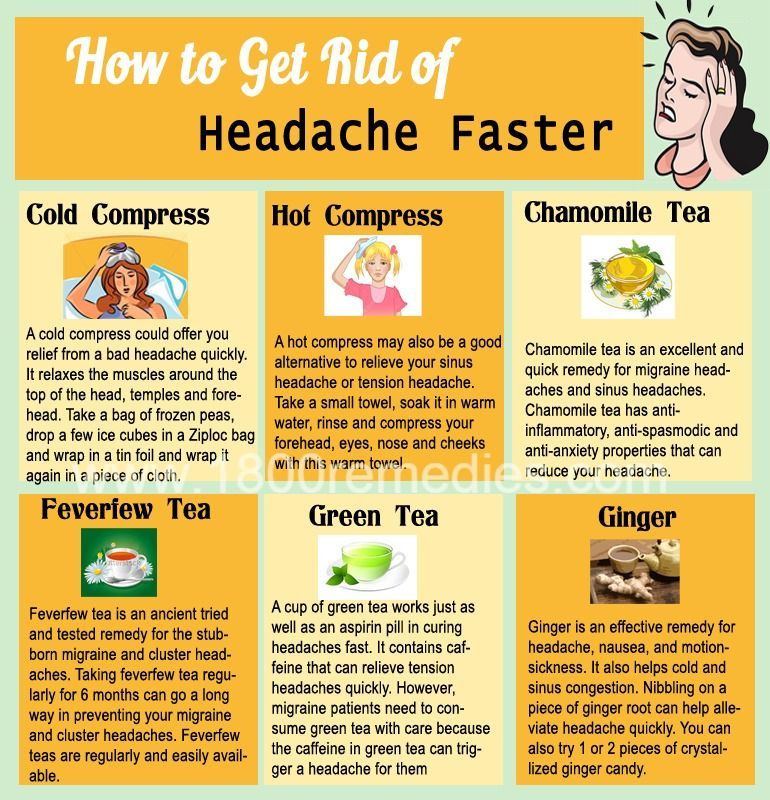 This symptom is called an aura. Some creative and active people, shortly before the onset of an attack, may have a sharp burst of vivacity.
This symptom is called an aura. Some creative and active people, shortly before the onset of an attack, may have a sharp burst of vivacity.
Any headache requires qualified diagnosis and adequate treatment. With prolonged and uncontrolled use of painkillers, serious complications arise: drug-induced hepatitis, damage to the gastrointestinal tract, kidneys, blood diseases, etc., which further aggravates the patient's condition. nine0003
In addition, uncontrolled use of painkillers can itself cause headaches.
In order to get rid of a headache without risk to health, we recommend that you consult a neurologist.
Diagnosis
In some cases, with headaches, a rather long observation of the patient is required, the use of various examination methods that depend on the symptoms identified by the neurologist:
- blood pressure measurement
- dopplerography and duplex examination of the vessels of the head and neck
- clinical, biochemical, immunological and other blood and urine tests
- ECG
- 24-hour monitoring (by Holter) of ECG and blood pressure in selected cases physician can prescribe:
- examination of the heart and other internal organs
- examination of endocrine, ENT organs, organs of vision
- electroencephalography, electroneuromyography
- X-ray examination of the spine and skull
- MRI (magnetic resonance imaging) or CT (computer tomography) of the brain and/or spine
- drug relief of pain
- individual selection of therapy based on a long-term effect
- be outdoors every day
- observe the daily regimen
- ensure good sleep
- exercise
- avoid stress and overexertion fully 90 90 massage course 90 eat
- exclude alcohol, nicotine, synthetic carbonated drinks.

other specialties (endocrinologist, cardiologist, nephrologist, gastroenterologist, gynecologist, urologist, dentist, etc. ) This allows you to reduce the number of "unnecessary" examinations and speed up the correct diagnosis, and hence the appointment of adequate treatment. nine0003
) This allows you to reduce the number of "unnecessary" examinations and speed up the correct diagnosis, and hence the appointment of adequate treatment. nine0003
Headache treatment
How to treat a headache - in this matter it is better to trust specialists. Self-medication can numb the symptoms, but not eliminate the cause. Based on the tests and conclusions of the necessary diagnostic specialists, two options for treating headaches are possible - these are:
The effectiveness of headache treatment depends on the correct identification of the cause of the headache symptom. As a rule, if a patient goes to a neurologist as soon as possible, then the likelihood of recovery is much greater. nine0003
Do not self-medicate!
The most effective complex treatment using an individual approach to each patient during the observation process, when therapeutic factors are prescribed that affect not only the mechanisms of headache, but also maintain a good functional state of the nervous system and the body as a whole.
In the conditions of the EXPERT Clinic, the attending physician can help you by prescribing treatment in the comfortable conditions of a day hospital, involving the capabilities of a psychotherapist. nine0003
Prognosis
With timely diagnosis, course of treatment and compliance with all recommendations, the prognosis is favorable.
Various types of headaches are successfully treated. Often after one course of treatment, the headache does not return.
Tips and Prevention
Never put off making an appointment with your doctor until tomorrow. It is better to complain as soon as possible than to allow the development of complications. You can not ignore the headache, which can lead to irreversible consequences. nine0003
For the prevention and treatment of headaches, the following recommendations should be observed:
FAQ
I often have headaches. Is it a migraine?
Migraines are not the only cause of headaches. The most common are tension headaches. The diagnosis can be made by a neurologist after examination and examination.
I have to take a lot of pain medication because of my headaches. It is harmful?
Uncontrolled use of analgesics can cause various complications. In addition, the likelihood of side effects increases. But the uncontrolled use of painkillers itself can be the cause of headaches - abuse headache. nine0003
What if the usual painkillers don't help my headache?
Before prescribing a drug, it is necessary to establish the cause of the headache, i.e. make the correct diagnosis. In some cases, headaches require the appointment of not painkillers, but vascular, anti-inflammatory drugs or drugs of other groups. It may be necessary to use several drugs in combination or non-drug treatment.
Treatment histories
Case #1
Patient A.