Anxiety attack when trying to sleep
What is it, Causes, Symptoms & Treatment
Overview
What is sleep anxiety?
Sleep anxiety is fear or worry about going to sleep. You may be apprehensive about not falling asleep or not being able to stay asleep. Some people also have a distinct phobia, or fear, about sleep called somniphobia. They may think something bad will happen to them while they sleep, or that they shouldn’t sleep because they need to stay alert and watchful.
Sleep and psychiatric disorders, such as anxiety, often go hand in hand. If you have an anxiety disorder, you may find it hard to fall asleep or stay asleep. Similarly, if you have a sleep disorder, you might feel anxious or fearful before bed because you’re afraid you won’t get the rest you need. One condition usually makes the other worse, so it can feel like a never-ending cycle.
Who gets sleep anxiety?
Sleep anxiety can affect adults, teens and children. You may be more likely to develop anxiety at night if you have a sleep disorder such as:
- Insomnia.
- Narcolepsy.
- Restless legs syndrome (RLS).
- Sleep apnea.
- Sleepwalking.
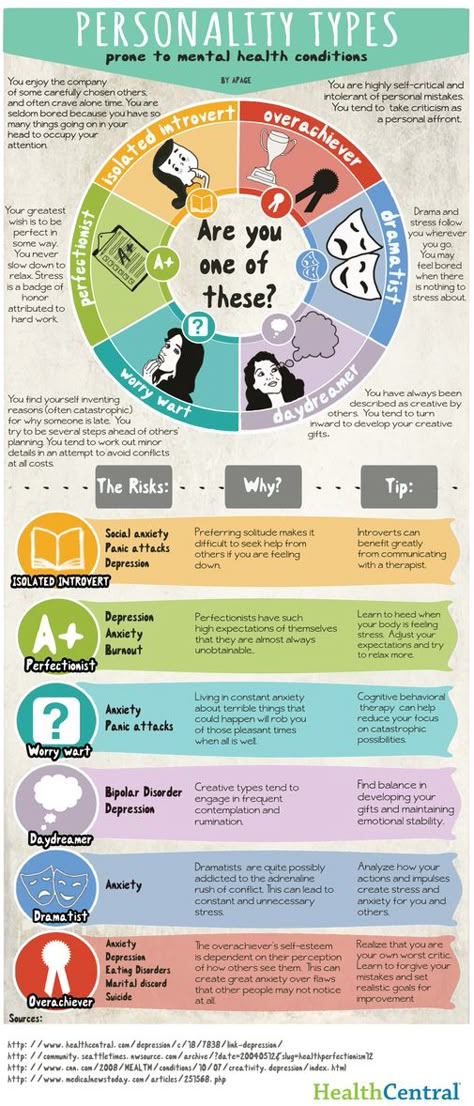
People with the following mental health disorders may also develop nighttime anxiety:
- Anxiety disorders.
- Bipolar disorder.
- Depression.
- Drug addictions or alcoholism.
- Panic disorder.
- Post-traumatic stress disorder (PTSD).
- Schizophrenia.
How common is sleep anxiety?
Anxiety is the most common mental health disorder in the U.S., affecting about 40 million people. Research suggests that most people with mental health disorders such as anxiety also have some form of sleep disruption.
Symptoms and Causes
What causes sleep anxiety?
Anxiety is a natural part of being human. We’re meant to feel afraid or worried in dangerous situations. Stress and anxiety trigger our bodies to release hormones that help us react quickly to escape harm. But if you have chronic anxiety, you might feel stress or worry all the time. You may feel fearful of everyday situations like driving to work or even falling asleep.
You may feel fearful of everyday situations like driving to work or even falling asleep.
Chronically high levels of these hormones, especially before sleep, can make it hard for your body to relax. You may have difficulty falling asleep. If you do fall asleep, you may wake up during the night with stressful or worrisome thoughts and not be able to fall asleep again.
The combination of a anxiety and insomnia can also be caused by a condition where there isn’t enough thyroid hormone in your bloodstream and your metabolism slows down (hypothyroidism).
Research suggests that anxiety can affect rapid eye movement (REM) sleep. This is the phase of sleep when you tend to have vivid dreams. If you have anxiety, the dreams may be disturbing or turn into nightmares that wake you.
Just as anxiety can affect sleep, sleep can affect anxiety. Sleep anxiety is a common characteristic of insomnia, wherein the individual begins to experience anxiety during the day and evening about poor sleep, which may help cause another night of bad sleep.
What are the symptoms of sleep anxiety?
When you can’t sleep due to anxiety, you may experience behavioral changes, including:
- Feelings of being overwhelmed.
- Inability to concentrate.
- Irritability.
- Nervousness.
- Restlessness.
- Sense of impending danger or doom.
Physical effects of anxiety before bed may include:
- Digestive problems.
- Fast heart rate.
- Rapid breathing.
- Sweating.
- Tense muscles.
- Trembling.
Some people also have nocturnal panic attacks. A panic attack is a sudden, intense burst of extreme fear. Nocturnal panic attacks only happen at night, and often wake you from sleep.
Diagnosis and Tests
How is sleep anxiety diagnosed?
Your healthcare provider performs a physical exam, reviews your medical history and evaluates your symptoms. They may ask you questions like:
- Do you eat or drink anything before bed?
- Does your anxiety always occur before bed?
- How long does it take you to fall asleep?
- How often do you wake up during the night?
- What activities do you do before bed?
What tests help confirm a sleep anxiety diagnosis?
In some cases, your provider may do a sleep study to find out if you have a sleep disorder. Also called polysomnography, a sleep study is a test where you stay overnight in a sleep lab. Your healthcare provider evaluates how your body works during sleep by checking your:
Also called polysomnography, a sleep study is a test where you stay overnight in a sleep lab. Your healthcare provider evaluates how your body works during sleep by checking your:
- Blood oxygen levels.
- Body positioning.
- Breathing.
- Electrical activity in your brain.
- Eye movements.
- Heart rates and rhythms.
- Leg movements.
- Sleep stages.
- Snoring or other noises you make during sleep.
Management and Treatment
How is sleep anxiety treated?
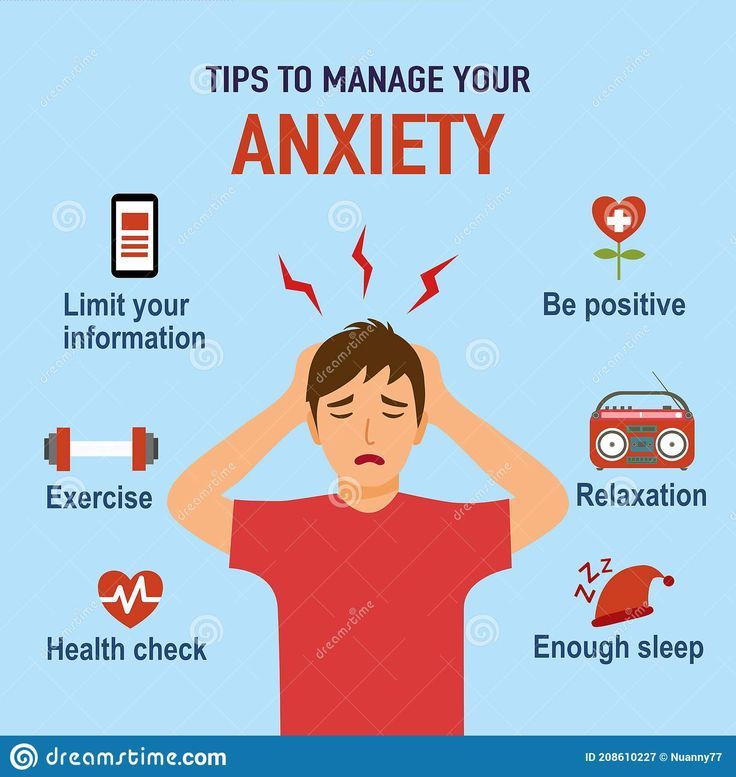
There are a variety of ways to manage sleep anxiety, including:
- Cognitive behavior therapy (CBT).
- Healthy sleep habits (sleep hygiene).
- Medication.
How does cognitive behavioral therapy treat sleep anxiety?
CBT is a form of psychotherapy, or talk therapy. It teaches you how to change your behavior by changing the way you think. It’s a common treatment for people with anxiety. A special form of CBT called cognitive behavior therapy for insomnia (CBTI) focuses on helping people who have insomnia. This therapy can take anywhere from six to 12 weeks to produce results.
This therapy can take anywhere from six to 12 weeks to produce results.
During CBT or CBTI, you may learn to:
- Avoid behaviors or environmental factors that trigger your anxiety or make sleeping difficult.
- Better understand how sleep and anxiety affect your brain and the rest of your body.
- Change negative or inaccurate thinking about bedtime or sleep.
Your therapist may teach you how to sleep with anxiety by using biofeedback. Biofeedback trains you to manage your body’s functions. You learn to relax your muscles, regulate your breathing, lower your heart rate and focus your attention. Your therapist might use special sensors to measure these bodily functions, or they may give you exercises, such as deep breathing and meditation, to do at home.
How can healthier sleep habits treat sleep anxiety?
Sleep habits, or sleep hygiene, are your routines around bedtime that can affect your sleep. Your healthcare provider may ask you to keep a sleep diary for several weeks. This is a daily log of your sleep habits. It can help identify things that might make it harder for you to fall asleep or stay asleep.
This is a daily log of your sleep habits. It can help identify things that might make it harder for you to fall asleep or stay asleep.
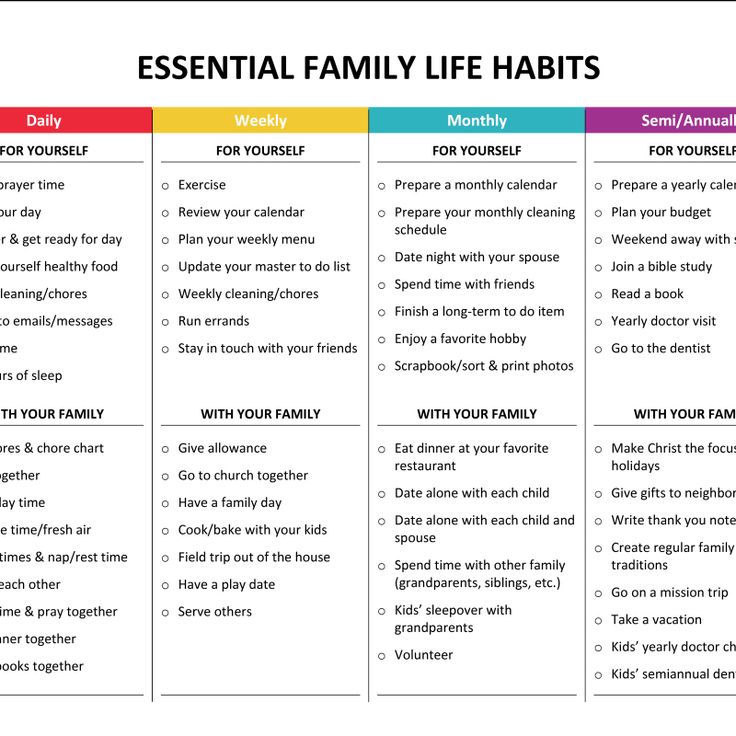
Some common ways to improve your sleep hygiene include:
- Avoid drinking lots of fluids before bed, especially alcohol.
- Do relaxing activities before bed, such as meditation or listening to soft, peaceful music.
- Don’t consume caffeine in the late afternoon or evening.
- Don’t go to bed unless you feel sleepy.
- Go to bed and wake up at the same time each day.
- If you don’t fall asleep within 20 minutes, get out of bed.
- Make sure your bedroom is comfortable, quiet and softly lit.
- Only use your bed for sleep and sex. For example, avoid watching television or doing work in bed.
- Set a goal of getting at least seven hours of sleep every night.
- Stop using electronic devices at least 30 minutes before bedtime.
- Try not to eat right before bedtime. If you’re hungry, have a light snack and not a big meal.
How can medication treat sleep anxiety?
Your healthcare provider may recommend medication to treat anxiety or other mental health disorders. Medication can also help improve the symptoms of sleep-related disorders such as restless legs syndrome or insomnia.
But some medications might actually increase your anxiety or make sleeping harder when you first start taking them. If you experience these side effects, talk to your healthcare provider. Many over-the-counter sleep aids can also be habit-forming. Don’t start any medication for anxiety or sleep without your healthcare provider’s supervision.
Prevention
How can I prevent sleep anxiety?
You may be able to reduce your risk of sleep anxiety by:
- Eating a healthy diet.
- Exercising regularly.
- Practicing good sleep hygiene.
- Taking medications for mental health disorders or sleep disorders as prescribed by your healthcare provider.
Outlook / Prognosis
What’s the prognosis (outlook) for people with sleep anxiety?
Most people can successfully manage their sleep anxiety with the right treatments.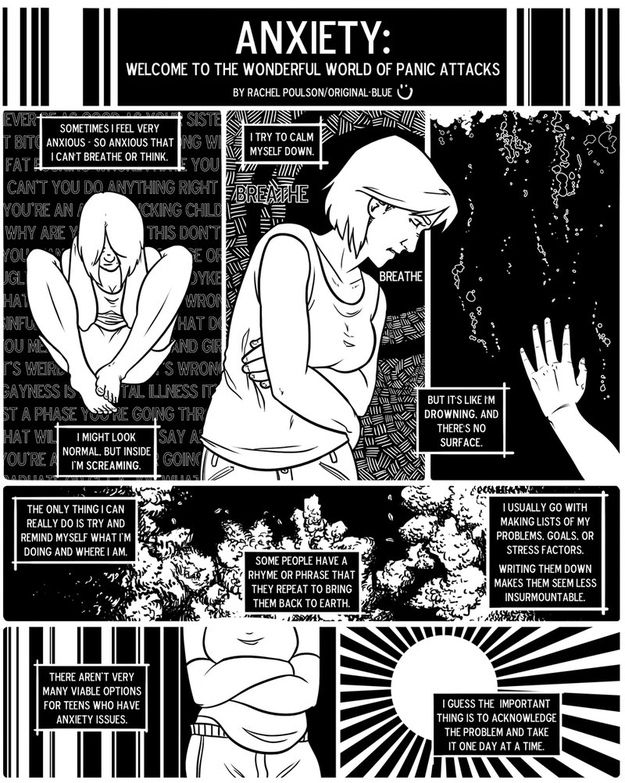 But remember that some treatments, such as medication or CBT, can take time to be effective. Don’t stop treatment prematurely if you think it isn’t working.
But remember that some treatments, such as medication or CBT, can take time to be effective. Don’t stop treatment prematurely if you think it isn’t working.
Are there long-term complications of sleep anxiety?
Prolonged anxiety or lack of sleep can affect your body in many ways. Sleep anxiety puts you at a higher risk for the following long-term complications:
- Diabetes.
- Heart attack.
- Heart disease.
- Heart failure.
- High blood pressure.
- Arrhythmia (irregular heartbeat).
- Obesity.
- Stroke.
Living With
How can I make living with sleep anxiety easier?
Anxiety or sleep problems can affect every aspect of your life, from your performance at work to your interactions with others. It may help to talk about your sleep anxiety with a therapist, co-workers, friends or loved ones. Support groups can also connect you to a community of people dealing with similar experiences.
A note from Cleveland Clinic
Sleep anxiety is a feeling of fear or stress about falling asleep or staying asleep.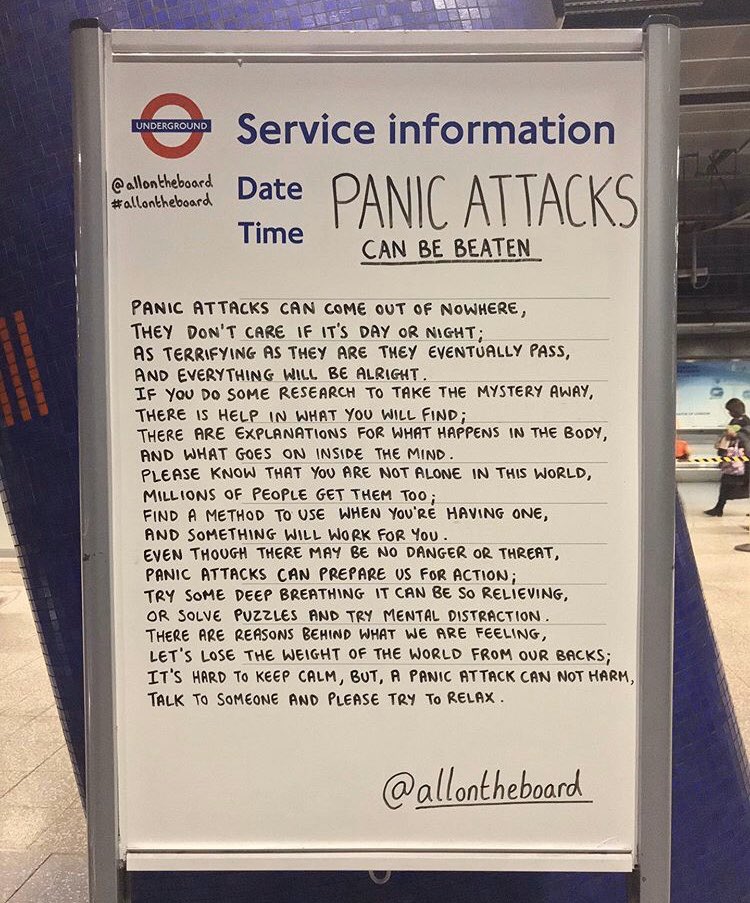 Sleep problems and mental health disorders such as anxiety are closely intertwined. One can often make the other worse, so it can feel like a never-ending cycle. But anxiety and sleep problems are both treatable. Talk to your healthcare provider about your symptoms and work together to build the right treatment plan. Common treatments include cognitive behavioral therapy (CBT), good sleep hygiene and medication.
Sleep problems and mental health disorders such as anxiety are closely intertwined. One can often make the other worse, so it can feel like a never-ending cycle. But anxiety and sleep problems are both treatable. Talk to your healthcare provider about your symptoms and work together to build the right treatment plan. Common treatments include cognitive behavioral therapy (CBT), good sleep hygiene and medication.
What is it, Causes, Symptoms & Treatment
Overview
What is sleep anxiety?
Sleep anxiety is fear or worry about going to sleep. You may be apprehensive about not falling asleep or not being able to stay asleep. Some people also have a distinct phobia, or fear, about sleep called somniphobia. They may think something bad will happen to them while they sleep, or that they shouldn’t sleep because they need to stay alert and watchful.
Sleep and psychiatric disorders, such as anxiety, often go hand in hand. If you have an anxiety disorder, you may find it hard to fall asleep or stay asleep. Similarly, if you have a sleep disorder, you might feel anxious or fearful before bed because you’re afraid you won’t get the rest you need. One condition usually makes the other worse, so it can feel like a never-ending cycle.
Similarly, if you have a sleep disorder, you might feel anxious or fearful before bed because you’re afraid you won’t get the rest you need. One condition usually makes the other worse, so it can feel like a never-ending cycle.
Who gets sleep anxiety?
Sleep anxiety can affect adults, teens and children. You may be more likely to develop anxiety at night if you have a sleep disorder such as:
- Insomnia.
- Narcolepsy.
- Restless legs syndrome (RLS).
- Sleep apnea.
- Sleepwalking.
People with the following mental health disorders may also develop nighttime anxiety:
- Anxiety disorders.
- Bipolar disorder.
- Depression.
- Drug addictions or alcoholism.
- Panic disorder.
- Post-traumatic stress disorder (PTSD).
- Schizophrenia.
How common is sleep anxiety?
Anxiety is the most common mental health disorder in the U.S., affecting about 40 million people. Research suggests that most people with mental health disorders such as anxiety also have some form of sleep disruption.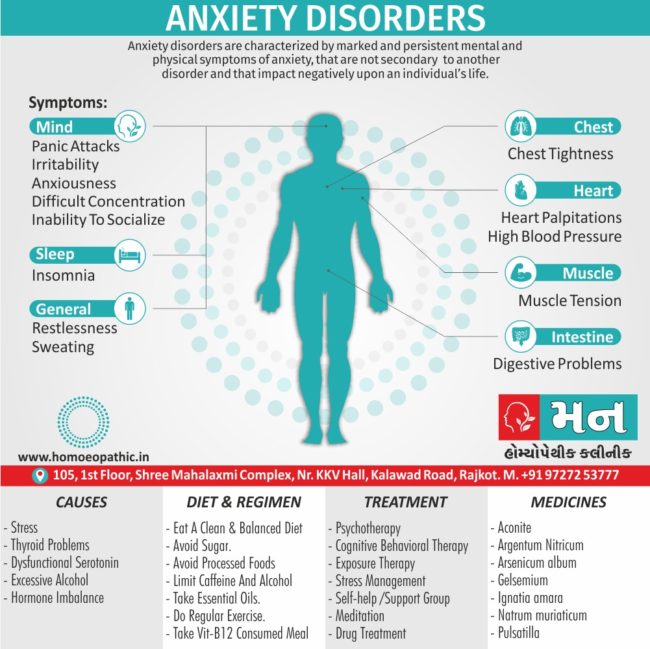
Symptoms and Causes
What causes sleep anxiety?
Anxiety is a natural part of being human. We’re meant to feel afraid or worried in dangerous situations. Stress and anxiety trigger our bodies to release hormones that help us react quickly to escape harm. But if you have chronic anxiety, you might feel stress or worry all the time. You may feel fearful of everyday situations like driving to work or even falling asleep.
Chronically high levels of these hormones, especially before sleep, can make it hard for your body to relax. You may have difficulty falling asleep. If you do fall asleep, you may wake up during the night with stressful or worrisome thoughts and not be able to fall asleep again.
The combination of a anxiety and insomnia can also be caused by a condition where there isn’t enough thyroid hormone in your bloodstream and your metabolism slows down (hypothyroidism).
Research suggests that anxiety can affect rapid eye movement (REM) sleep. This is the phase of sleep when you tend to have vivid dreams. If you have anxiety, the dreams may be disturbing or turn into nightmares that wake you.
This is the phase of sleep when you tend to have vivid dreams. If you have anxiety, the dreams may be disturbing or turn into nightmares that wake you.
Just as anxiety can affect sleep, sleep can affect anxiety. Sleep anxiety is a common characteristic of insomnia, wherein the individual begins to experience anxiety during the day and evening about poor sleep, which may help cause another night of bad sleep.
What are the symptoms of sleep anxiety?
When you can’t sleep due to anxiety, you may experience behavioral changes, including:
- Feelings of being overwhelmed.
- Inability to concentrate.
- Irritability.
- Nervousness.
- Restlessness.
- Sense of impending danger or doom.
Physical effects of anxiety before bed may include:
- Digestive problems.
- Fast heart rate.
- Rapid breathing.
- Sweating.
- Tense muscles.
- Trembling.
Some people also have nocturnal panic attacks. A panic attack is a sudden, intense burst of extreme fear. Nocturnal panic attacks only happen at night, and often wake you from sleep.
A panic attack is a sudden, intense burst of extreme fear. Nocturnal panic attacks only happen at night, and often wake you from sleep.
Diagnosis and Tests
How is sleep anxiety diagnosed?
Your healthcare provider performs a physical exam, reviews your medical history and evaluates your symptoms. They may ask you questions like:
- Do you eat or drink anything before bed?
- Does your anxiety always occur before bed?
- How long does it take you to fall asleep?
- How often do you wake up during the night?
- What activities do you do before bed?
What tests help confirm a sleep anxiety diagnosis?
In some cases, your provider may do a sleep study to find out if you have a sleep disorder. Also called polysomnography, a sleep study is a test where you stay overnight in a sleep lab. Your healthcare provider evaluates how your body works during sleep by checking your:
- Blood oxygen levels.
- Body positioning.
- Breathing.
- Electrical activity in your brain.
- Eye movements.
- Heart rates and rhythms.
- Leg movements.
- Sleep stages.
- Snoring or other noises you make during sleep.
Management and Treatment
How is sleep anxiety treated?
There are a variety of ways to manage sleep anxiety, including:
- Cognitive behavior therapy (CBT).
- Healthy sleep habits (sleep hygiene).
- Medication.
How does cognitive behavioral therapy treat sleep anxiety?
CBT is a form of psychotherapy, or talk therapy. It teaches you how to change your behavior by changing the way you think. It’s a common treatment for people with anxiety. A special form of CBT called cognitive behavior therapy for insomnia (CBTI) focuses on helping people who have insomnia. This therapy can take anywhere from six to 12 weeks to produce results.
During CBT or CBTI, you may learn to:
- Avoid behaviors or environmental factors that trigger your anxiety or make sleeping difficult.

- Better understand how sleep and anxiety affect your brain and the rest of your body.
- Change negative or inaccurate thinking about bedtime or sleep.
Your therapist may teach you how to sleep with anxiety by using biofeedback. Biofeedback trains you to manage your body’s functions. You learn to relax your muscles, regulate your breathing, lower your heart rate and focus your attention. Your therapist might use special sensors to measure these bodily functions, or they may give you exercises, such as deep breathing and meditation, to do at home.
How can healthier sleep habits treat sleep anxiety?
Sleep habits, or sleep hygiene, are your routines around bedtime that can affect your sleep. Your healthcare provider may ask you to keep a sleep diary for several weeks. This is a daily log of your sleep habits. It can help identify things that might make it harder for you to fall asleep or stay asleep.
Some common ways to improve your sleep hygiene include:
- Avoid drinking lots of fluids before bed, especially alcohol.

- Do relaxing activities before bed, such as meditation or listening to soft, peaceful music.
- Don’t consume caffeine in the late afternoon or evening.
- Don’t go to bed unless you feel sleepy.
- Go to bed and wake up at the same time each day.
- If you don’t fall asleep within 20 minutes, get out of bed.
- Make sure your bedroom is comfortable, quiet and softly lit.
- Only use your bed for sleep and sex. For example, avoid watching television or doing work in bed.
- Set a goal of getting at least seven hours of sleep every night.
- Stop using electronic devices at least 30 minutes before bedtime.
- Try not to eat right before bedtime. If you’re hungry, have a light snack and not a big meal.
How can medication treat sleep anxiety?
Your healthcare provider may recommend medication to treat anxiety or other mental health disorders. Medication can also help improve the symptoms of sleep-related disorders such as restless legs syndrome or insomnia.
But some medications might actually increase your anxiety or make sleeping harder when you first start taking them. If you experience these side effects, talk to your healthcare provider. Many over-the-counter sleep aids can also be habit-forming. Don’t start any medication for anxiety or sleep without your healthcare provider’s supervision.
Prevention
How can I prevent sleep anxiety?
You may be able to reduce your risk of sleep anxiety by:
- Eating a healthy diet.
- Exercising regularly.
- Practicing good sleep hygiene.
- Taking medications for mental health disorders or sleep disorders as prescribed by your healthcare provider.
Outlook / Prognosis
What’s the prognosis (outlook) for people with sleep anxiety?
Most people can successfully manage their sleep anxiety with the right treatments. But remember that some treatments, such as medication or CBT, can take time to be effective. Don’t stop treatment prematurely if you think it isn’t working.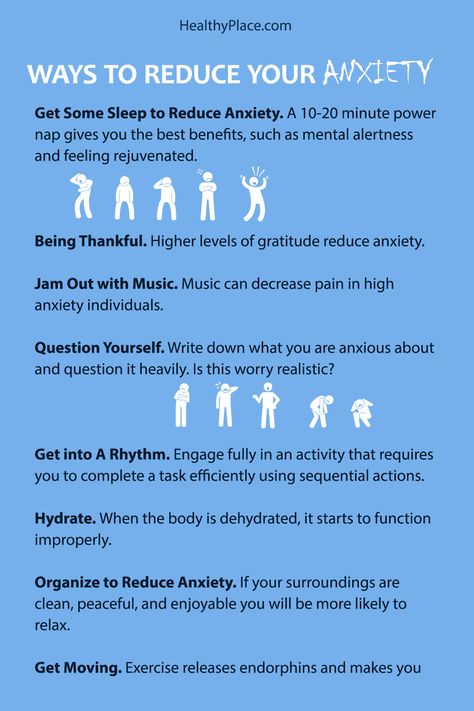
Are there long-term complications of sleep anxiety?
Prolonged anxiety or lack of sleep can affect your body in many ways. Sleep anxiety puts you at a higher risk for the following long-term complications:
- Diabetes.
- Heart attack.
- Heart disease.
- Heart failure.
- High blood pressure.
- Arrhythmia (irregular heartbeat).
- Obesity.
- Stroke.
Living With
How can I make living with sleep anxiety easier?
Anxiety or sleep problems can affect every aspect of your life, from your performance at work to your interactions with others. It may help to talk about your sleep anxiety with a therapist, co-workers, friends or loved ones. Support groups can also connect you to a community of people dealing with similar experiences.
A note from Cleveland Clinic
Sleep anxiety is a feeling of fear or stress about falling asleep or staying asleep. Sleep problems and mental health disorders such as anxiety are closely intertwined.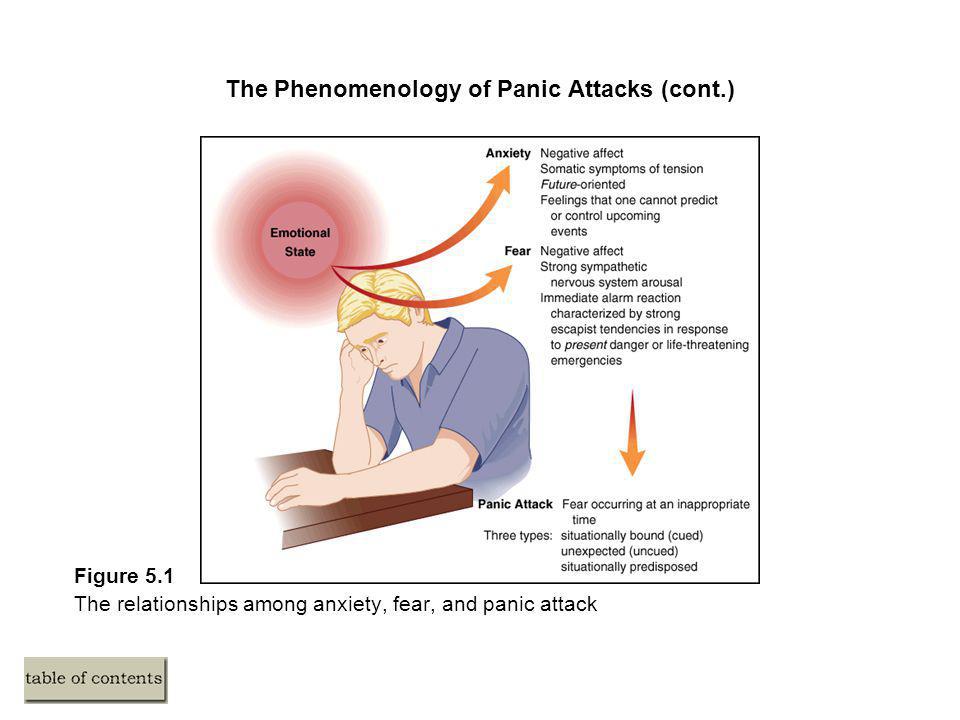 One can often make the other worse, so it can feel like a never-ending cycle. But anxiety and sleep problems are both treatable. Talk to your healthcare provider about your symptoms and work together to build the right treatment plan. Common treatments include cognitive behavioral therapy (CBT), good sleep hygiene and medication.
One can often make the other worse, so it can feel like a never-ending cycle. But anxiety and sleep problems are both treatable. Talk to your healthcare provider about your symptoms and work together to build the right treatment plan. Common treatments include cognitive behavioral therapy (CBT), good sleep hygiene and medication.
Sleep disorders in anxiety and anxiety-depressive disorders | Kovrov G.V., Lebedev M.A., Palatov S.Yu., Merkulova T.B., Posokhov S.I.
In clinical practice, sleep disorders are usually associated with anxiety and depression. Existing studies show a close relationship between sleep disorders and anxiety and depressive disorders [1, 2]. A clear dependence of the severity of the course of both groups of diseases on concomitant sleep disorders was shown [1]. In general somatic practice, the prevalence of insomnia reaches 73% [3], in borderline psychiatry, clinically defined insomnia occurs in 65%, and changes in nocturnal sleep according to polysomnography are noted in 100% of cases [4]. nine0003
nine0003
Combination of sleep disorders and anxiety disorders
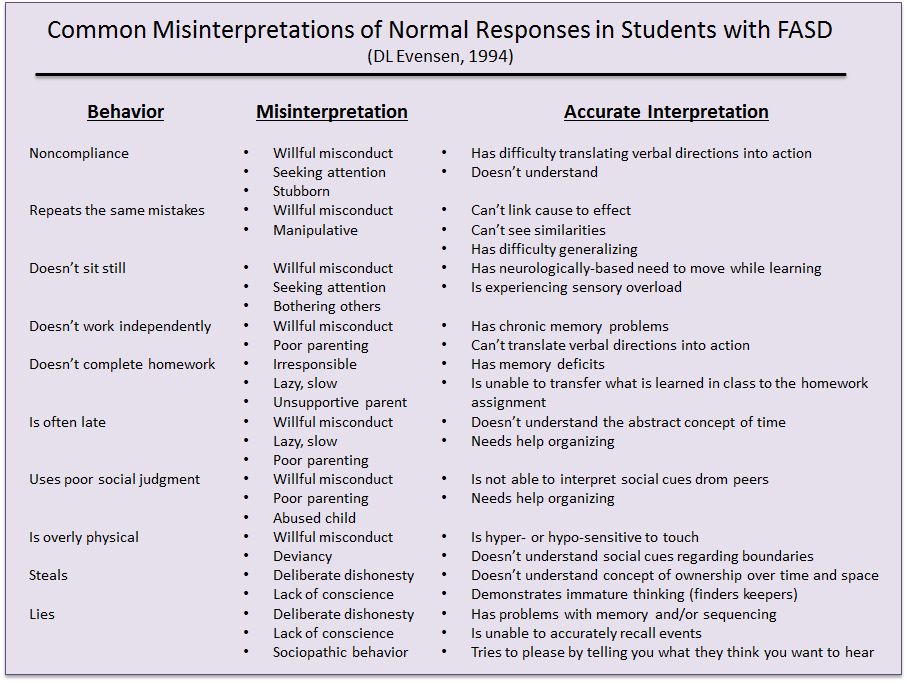
It is known that the relationship between sleep disorders and anxiety disorders is noted, on the one hand, when sleep disorders can provoke the development of anxiety disorders [5], and on the other hand, when the onset of an anxiety disorder precedes the onset of sleep disorders. Complaints about problems associated with sleep are typical for patients with all diseases included in the group of anxiety disorders. In the case of major generalized disorder and post-traumatic stress disorder (PTSD), sleep disturbances are one of the criteria required for a diagnosis. There are objective reasons for the development of sleep disorders within anxiety disorders, namely: anxiety is manifested by increased cortical activation, which entails the difficulty of falling asleep and maintaining sleep. nine0003
In the clinic, anxiety is manifested by anxiety, irritability, motor excitation, decreased concentration of attention, increased fatigue [6].
The most striking manifestation of anxiety disorders is generalized anxiety disorder (GAD), which is diagnosed on the basis of the presence of at least 3 of the following symptoms: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, sleep disturbances. The duration of the disease should be at least 6 months, the symptoms should cause psychosomatic discomfort and / or social disadaptation. nine0003
Sleep disorders in this situation are one of the 6 diagnostic criteria for GAD. The main symptom of GAD, excessive, persistent anxiety, is a major predisposing factor in the development of insomnia. Insomnia and GAD are closely related, usually comorbid disorders. The difference between insomnia in anxiety disorder and primary insomnia, not associated with other diseases, is the nature of the experiences in the process of falling asleep. In the case of GAD, the patient is concerned about current problems [7] (work, study, relationships), which hinders the process of falling asleep. In the case of primary insomnia, the anxiety itself is caused by the disease itself. nine0003
In the case of primary insomnia, the anxiety itself is caused by the disease itself. nine0003
A polysomnographic study can reveal changes characteristic of insomnia: increased time to fall asleep, frequent awakenings, reduced sleep efficiency, and a decrease in its total duration.
Another striking example of anxiety disorders is panic disorder, which is manifested by recurrent states of severe anxiety (panic). Attacks are accompanied by phenomena of depersonalization and derealization, as well as severe autonomic disorders. In the behavior of the patient, avoidance of situations in which the attack occurred for the first time is noted. There may be a fear of loneliness, a repetition of the attack. A panic attack occurs spontaneously, outside of formal situations of danger or threat. nine0003
Panic disorder is more common in women and typically begins around the age of 20. A hallmark of panic disorder are spontaneous episodes of panic attacks, characterized by bouts of fear, anxiety, and other autonomic manifestations. About 2/3 of patients with this disorder experience some form of sleep disturbance. Patients complain of difficulty falling asleep, non-restorative sleep, and characteristic nocturnal panic attacks. It should be noted that the presence of certain problems associated with sleep can lead to aggravation of anxiety disorders, including panic disorder. nine0003
About 2/3 of patients with this disorder experience some form of sleep disturbance. Patients complain of difficulty falling asleep, non-restorative sleep, and characteristic nocturnal panic attacks. It should be noted that the presence of certain problems associated with sleep can lead to aggravation of anxiety disorders, including panic disorder. nine0003
Polysomnographic examination can detect frequent awakenings, reduced sleep efficiency and a reduction in its total duration [8]. It is not uncommon to see depression coexisting with anxiety disorders, and it is possible that the presence of other changes in sleep patterns in patients with panic disorder is associated with comorbid depression, and therefore the diagnosis of depression should be ruled out in patients with similar sleep disorders.
The sleep paralysis characteristic of narcolepsy can also occur with panic disorder. It is a movement paralysis that occurs during falling asleep or waking up, during which patients experience fear, a feeling of pressure in the chest, and other somatic manifestations of anxiety.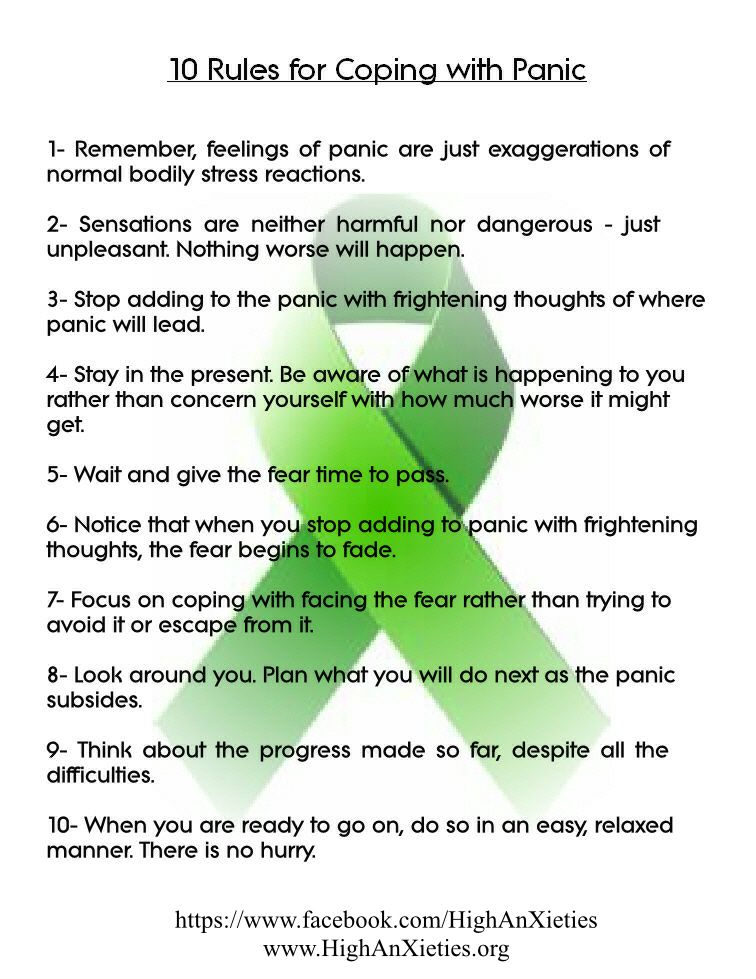 This symptom also occurs in patients with post-traumatic stress disorder.
This symptom also occurs in patients with post-traumatic stress disorder.
Nighttime panic attacks are a common occurrence in this disease [9]. They are manifested by a sudden awakening and all the symptoms characteristic of panic attacks. Awakening occurs during the phase of non-REM sleep, which most likely excludes their connection with dreams. It was also found that nocturnal attacks are an indicator of a more severe course of the disease. It must be remembered that patients, fearing the recurrence of such episodes, deprive themselves of sleep, which leads to more serious disorders and, in general, reduces the quality of life of these patients.
PTSD is a disease from the group of anxiety disorders, in which sleep disturbances are a diagnostic criterion. Sleep disorders in this disease include 2 main symptoms: nightmares and insomnia. Other phenomena inherent in PTSD and associated with sleep are: somnambulism, sleep-talking, hypnagogic and hypnopompic hallucinations. The changes detected by polysomnography are not specific and in some cases may be absent. Possible changes include: an increase in the representation of the 1st stage of sleep, a decrease in the representation of the 4th stage of sleep. Also, with PTSD, breathing disorders during sleep are often found. nine0003
The changes detected by polysomnography are not specific and in some cases may be absent. Possible changes include: an increase in the representation of the 1st stage of sleep, a decrease in the representation of the 4th stage of sleep. Also, with PTSD, breathing disorders during sleep are often found. nine0003
Agoraphobia can also be a manifestation of anxiety disorders, which is defined as anxiety that occurs in response to situations, the way out of which, according to the patient, is difficult. In the clinical picture, as a rule, there is a persistent fear of the patient to be in a crowded place, public places (shops, open squares and streets, theaters, cinemas, concert halls, workplaces), fear of independent long trips (by various modes of transport). The situational component of the agoraphobia syndrome is expressed in the confinement of phobic experiences to certain situations and in the fear of getting into situations in which, according to patients, a repetition of painful sensations is likely. Often, agoraphobic symptoms cover many fears of various situations, forming panagoraphobia - the fear of leaving the house with the development of deep social maladaptation. There are attempts by the patient to overcome their own experiences, in adverse cases, there is a restriction of social activity. nine0003
Often, agoraphobic symptoms cover many fears of various situations, forming panagoraphobia - the fear of leaving the house with the development of deep social maladaptation. There are attempts by the patient to overcome their own experiences, in adverse cases, there is a restriction of social activity. nine0003
Specific phobias are characterized by an association of anxiety with certain situations (air travel, contact with animals, the sight of blood, etc.), also accompanied by an avoidance reaction. Patients are critical of their experiences, however, phobias have a significant impact on various areas of activity of patients. There are the following forms: cardiophobia, cancerophobia, claustrophobia, etc. Sleep disturbances in these patients are non-specific, and from the point of view of the patient, they are a minor manifestation of the disease. nine0003
In general, the most common manifestations of sleep disturbances in anxiety states are presomnic disorders. The initial phase of sleep consists of 2 components: drowsiness, a kind of craving for sleep, and actually falling asleep. Often, patients have no desire to sleep, no desire to sleep, muscle relaxation does not occur, they have to perform various actions aimed at falling asleep. In other cases, there is an inclination to sleep, but its intensity is reduced, drowsiness becomes intermittent, undulating. Drowsiness occurs, the muscles relax, the perception of the environment decreases, the patient takes a comfortable position for falling asleep, and a slight drowsiness appears, but soon it is interrupted, disturbing thoughts and ideas arise in the mind. In the future, the state of wakefulness is again replaced by mild drowsiness and superficial drowsiness. Such changes in states can be repeated several times, leading to emotional discomfort that prevents the onset of sleep. nine0003
Often, patients have no desire to sleep, no desire to sleep, muscle relaxation does not occur, they have to perform various actions aimed at falling asleep. In other cases, there is an inclination to sleep, but its intensity is reduced, drowsiness becomes intermittent, undulating. Drowsiness occurs, the muscles relax, the perception of the environment decreases, the patient takes a comfortable position for falling asleep, and a slight drowsiness appears, but soon it is interrupted, disturbing thoughts and ideas arise in the mind. In the future, the state of wakefulness is again replaced by mild drowsiness and superficial drowsiness. Such changes in states can be repeated several times, leading to emotional discomfort that prevents the onset of sleep. nine0003
In a number of patients, experiences about disturbed sleep can acquire an overvalued hypochondriacal coloration and come to the fore according to the mechanisms of actualization, often there is an obsessive fear of insomnia - agripnophobia. It is usually combined with an anxious and painful expectation of sleep, certain requirements for others and the creation of the above-mentioned special conditions for sleep.
It is usually combined with an anxious and painful expectation of sleep, certain requirements for others and the creation of the above-mentioned special conditions for sleep.
Anxiety depression is characterized by the patient's constant experience of anxiety, a sense of impending danger and insecurity. Anxious experiences change: anxiety about their loved ones, fears about their condition, their actions. The structure of anxious depression, as a rule, includes anxiety, feelings of guilt, motor restlessness, fussiness, fluctuations in affect with worsening in the evening, and somatovegetative symptoms. Anxious and melancholy affects often occur simultaneously, in many cases it is impossible to determine which of them is leading in the patient. Anxiety depression is most often found in people of involutionary age and proceeds according to the type of protracted phases. In addition, it is actually the leading type of neurotic depression [10]. nine0003
The patient exhibits a variety of symptoms of anxiety and depression. Initially, one or more physical symptoms (eg, fatigue, pain, sleep disturbances) may be present. Further questioning allows us to state a depressive mood and/or anxiety.
Initially, one or more physical symptoms (eg, fatigue, pain, sleep disturbances) may be present. Further questioning allows us to state a depressive mood and/or anxiety.
Signs of anxiety depression:
- depressed mood;
- loss of interest;
- severe anxiety.
The following symptoms are also often seen: nine0003
- sleep disorders;
- physical weakness and loss of energy;
- fatigue or decreased activity;
- difficulty concentrating, fidgeting;
- impaired concentration;
- excitation or retardation of movements or speech;
- appetite disorders;
- dry mouth;
- tension and anxiety;
- irritability; nine0044
- tremor;
- heartbeat;
- dizziness;
- suicidal thoughts.
Often with anxiety depression, variants of presomnic disorders are observed, in which the desire to sleep is pronounced, drowsiness increases rapidly, and the patient falls asleep relatively easily, but wakes up suddenly after 5-10 minutes, drowsiness completely disappears, and then within 1-2 hours he does not can fall asleep. This period without sleep is characterized by unpleasant ideas, thoughts, fears, reflecting to a greater or lesser extent the experienced conflict situation and the reaction to the inability to sleep. There is also hyperesthesia to sensory stimuli. Those suffering from this form of sleep disorder react extremely painfully to the slightest sensory stimuli, up to flashes of affect. nine0003
This period without sleep is characterized by unpleasant ideas, thoughts, fears, reflecting to a greater or lesser extent the experienced conflict situation and the reaction to the inability to sleep. There is also hyperesthesia to sensory stimuli. Those suffering from this form of sleep disorder react extremely painfully to the slightest sensory stimuli, up to flashes of affect. nine0003
For disturbed falling asleep, lengthening of the drowsy period is characteristic. This drowsy state is often accompanied by motor, sensory and visceral automatisms, sharp shudders, vivid perceptions of sounds and visual images, palpitations, sensations of muscle spasms. Often these phenomena, awakening the patient, cause various painful ideas and fears, sometimes acquiring an obsessive character.
Sleep disorders and their polysomnographic manifestations among mental illnesses are the most studied for depressive disorder. Among the sleep disorders in depressive disorder, insomnia is the most common.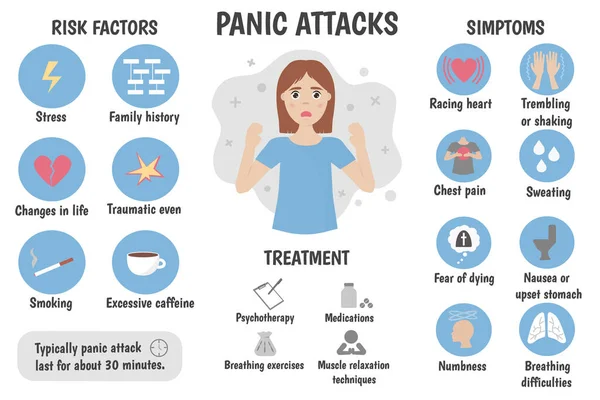 The severity and duration of insomnia are manifestations of a more severe depressive disorder, and the appearance of insomnia during remission indicates the imminent occurrence of a recurrent depressive episode [1]. In addition, sleep disorders in this disease are the most persistent symptom. The close relationship of this disorder with sleep disorders is explained by the biochemical processes characteristic of depression. In particular, in depressive disorder, there is a decrease in the level of serotonin, which plays a role in the initiation of REM sleep and the organization of delta sleep [11]. Depressive disorder is characterized by the following manifestations of sleep disturbances: difficulty falling asleep [10], non-restorative sleep, as a rule, reduced total sleep time. The most specific symptoms for depression are frequent nocturnal awakenings and early terminal awakenings. Complaints about difficulty falling asleep are more often observed in young patients, and frequent awakenings are more characteristic of the elderly [12].
The severity and duration of insomnia are manifestations of a more severe depressive disorder, and the appearance of insomnia during remission indicates the imminent occurrence of a recurrent depressive episode [1]. In addition, sleep disorders in this disease are the most persistent symptom. The close relationship of this disorder with sleep disorders is explained by the biochemical processes characteristic of depression. In particular, in depressive disorder, there is a decrease in the level of serotonin, which plays a role in the initiation of REM sleep and the organization of delta sleep [11]. Depressive disorder is characterized by the following manifestations of sleep disturbances: difficulty falling asleep [10], non-restorative sleep, as a rule, reduced total sleep time. The most specific symptoms for depression are frequent nocturnal awakenings and early terminal awakenings. Complaints about difficulty falling asleep are more often observed in young patients, and frequent awakenings are more characteristic of the elderly [12]. nine0003
nine0003
With masked depression, complaints of sleep disturbances may be the only manifestation of the disease. In depression, in contrast to primary insomnia, there are complaints of sleep disturbances typical of this disease: frequent awakenings, early morning awakening, etc. [12].
In polysomnographic study, the following changes are observed: an increase in the time to fall asleep, a decrease in sleep efficiency. The most common and depressive disorder-specific symptoms are shortened REM sleep latency and reduced delta sleep. It has been found that patients with a higher proportion of delta sleep stay in remission longer than those with a decrease in the proportion of delta sleep [13]. nine0003
Attempts have been made to explore the possibility of using depression-specific sleep disturbances as markers of depressive disorder. Due to the heterogeneity of the manifestations of sleep disorders, this issue remains not fully resolved.
The features of sleep disorders in various types of depression were also highlighted. For patients with a predominance of the anxious component, difficulty falling asleep and early awakenings are more characteristic. With this type of depression, dream plots are associated with persecution, threats, etc. In addition, in these patients, in general, there was a high level of wakefulness before falling asleep. For depressions with the leading affect of melancholy, early morning awakenings and dreams of static types of gloomy content are most characteristic. Depression with the affect of apathy is characterized by early awakenings and rare, unsaturated dreams. Also typical of depression with apathetic affect is the loss of a sense of boundaries between sleep and wakefulness. Patients with bipolar disorder have a similar polysomnographic pattern [14]. nine0003
For patients with a predominance of the anxious component, difficulty falling asleep and early awakenings are more characteristic. With this type of depression, dream plots are associated with persecution, threats, etc. In addition, in these patients, in general, there was a high level of wakefulness before falling asleep. For depressions with the leading affect of melancholy, early morning awakenings and dreams of static types of gloomy content are most characteristic. Depression with the affect of apathy is characterized by early awakenings and rare, unsaturated dreams. Also typical of depression with apathetic affect is the loss of a sense of boundaries between sleep and wakefulness. Patients with bipolar disorder have a similar polysomnographic pattern [14]. nine0003
Features of sleep disturbance in bipolar disorder are a significant decrease in the duration of sleep during a manic episode and a greater tendency of patients to hypersomnia during depressive episodes compared with the unipolar course of the disorder. Complaints of sleep disturbances during manic episodes are usually absent.
Complaints of sleep disturbances during manic episodes are usually absent.
Treatment
For the treatment of anxiety and depressive disorders, drugs of various pharmacological groups are used: tranquilizers (mainly long-acting or short-acting benzodiazepine drugs), selective serotonin reuptake inhibitors, selective serotonin reuptake stimulants, tricyclic antidepressants. All these drugs, to one degree or another, affect a person’s sleep, making it easier to fall asleep, reducing the number and duration of nocturnal awakenings, thereby affecting the recovery processes that occur during a night’s sleep. When constructing tactics for the treatment of sleep disorders associated with anxiety and depressive manifestations, it is important to remember that insomnia itself can increase anxiety, worsen well-being, mood, as a rule, in the morning hours after poor sleep [15]. In this regard, the use of hypnotics in the treatment may be promising in the presence of a predominance of insomnia symptoms in the clinical picture in order to prevent exacerbation of anxiety and depressive disorders. In this regard, the most effective helpers can be sleeping pills that affect the GABAergic (GABA - γ-aminobutyric acid) system - histamine receptor blockers (Valocordin®-Doxylamine) and melatonin preparation. The most convenient to use in the treatment of insomnia is Valocordin®-Doxylamine, which is available in drops, which allows you to select an individual dose of the drug. nine0003
In this regard, the most effective helpers can be sleeping pills that affect the GABAergic (GABA - γ-aminobutyric acid) system - histamine receptor blockers (Valocordin®-Doxylamine) and melatonin preparation. The most convenient to use in the treatment of insomnia is Valocordin®-Doxylamine, which is available in drops, which allows you to select an individual dose of the drug. nine0003
Valocordin®-Doxylamine is a unique drug used as a hypnotic. Most known hypnotic drugs (benzodiazepines, cyclopyrrolones, imidazopyridines, etc.) act on the GABAergic complex, activating the activity of somnogenic systems, while histamine receptor blockers act on wakefulness systems, not sleep ones, reducing their activation. A fundamentally different mechanism of hypnotic action makes it possible to use Valocordin®-Doxylamine more widely: when changing one drug to another, reducing the dosages of "habitual hypnotics", and also, if necessary, canceling hypnotics. nine0003
A drug study conducted on healthy subjects showed that doxylamine succinate leads to a decrease in the duration of nocturnal awakenings and stage 1 sleep and an increase in stage 2 without a significant effect on the duration of stages 3 and 4 sleep and REM sleep. There was no significant subjective effect on the reports of healthy volunteers, however, compared with placebo, doxylamine increased the depth of sleep and improved its quality [16].
There was no significant subjective effect on the reports of healthy volunteers, however, compared with placebo, doxylamine increased the depth of sleep and improved its quality [16].
In Russia, one of the first studies was carried out under the supervision of A.M. Wayne [17]. It has been shown that under the influence of doxylamine such subjective characteristics of sleep as the duration of falling asleep, the duration and quality of sleep, the number of night awakenings and the quality of morning awakenings improve. An analysis of the objective characteristics of sleep showed that while taking doxylamine, there was a reduction in the time of wakefulness during sleep, a decrease in the duration of falling asleep, an increase in the duration of sleep, the time of the REM sleep phase, and the sleep quality index. It was also shown that doxylamine did not reduce the effectiveness of other drugs in patients, such as antihypertensive, vasoactive, etc. The results of a study of the effect of doxylamine on patients with insomnia indicate the effectiveness of this drug in these patients.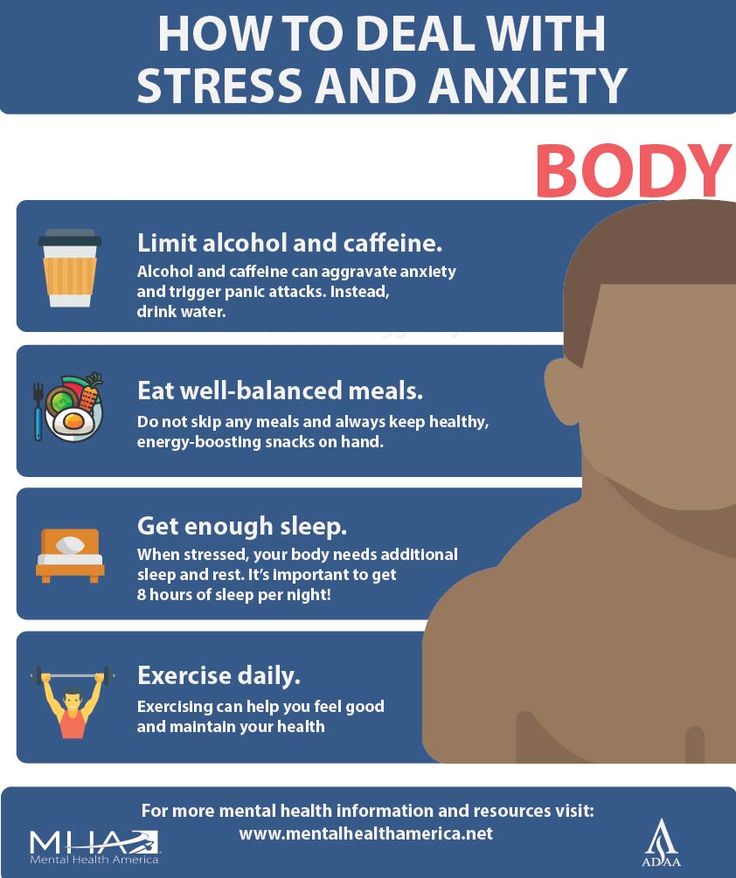 Subjective feelings of a positive effect are confirmed by objective studies of the structure of sleep, which undergoes positive shifts, which affect such indicators as sleep duration, falling asleep duration, REM sleep phase. Of great importance is also the absence of any changes in the results of personal data regarding drowsiness and sleep apnea syndrome, which indicates the absence of an aftereffect of the drug in relation to the worsening of the course of obstructive sleep apnea syndrome. However, if obstructive sleep apnea is suspected, doxylamine should be used with caution. nine0003
Subjective feelings of a positive effect are confirmed by objective studies of the structure of sleep, which undergoes positive shifts, which affect such indicators as sleep duration, falling asleep duration, REM sleep phase. Of great importance is also the absence of any changes in the results of personal data regarding drowsiness and sleep apnea syndrome, which indicates the absence of an aftereffect of the drug in relation to the worsening of the course of obstructive sleep apnea syndrome. However, if obstructive sleep apnea is suspected, doxylamine should be used with caution. nine0003
Modern clinical studies do not reveal serious side effects in the treatment of therapeutic doses of the drug, but it is always necessary to remember the possible appearance of symptoms that arise due to the individual characteristics of the body, and contraindications (glaucoma; difficulty urinating due to benign prostatic hyperplasia; age up to 15 years; increased drug sensitivity).
Simultaneous administration of the drug Valocordin®-Doxylamine and sedative drugs that affect the central nervous system (CNS): neuroleptics, tranquilizers, antidepressants, hypnotics, analgesics, anesthetics, antiepileptic drugs, may enhance their effect. Procarbazines and antihistamines should be combined with caution to minimize CNS depression and potential drug potentiation. During treatment with Valocordin®-Doxylamine, alcohol should be avoided as it may unpredictably affect the effects of doxylamine succinate. nine0003
Procarbazines and antihistamines should be combined with caution to minimize CNS depression and potential drug potentiation. During treatment with Valocordin®-Doxylamine, alcohol should be avoided as it may unpredictably affect the effects of doxylamine succinate. nine0003
During the use of this drug, it is recommended to exclude driving a car and working with mechanisms, as well as other activities accompanied by an increased risk, at least at the first stage of treatment. The attending physician is advised to evaluate the individual reaction rate when choosing a dose. It is important to consider these features of the effect of the drug in the treatment of patients with insomnia in order to increase the effectiveness of Valocordin®-Doxylamine and exclude possible undesirable effects. nine0003
Conclusion
When diagnosing a disease, it is important to remember that, as a rule, problems falling asleep indicate the presence of severe anxiety, early awakenings are a manifestation of depression. When choosing treatment tactics at all stages of the development of anxiety-depressive syndrome (ADS), the appointment of modern hypnotic drugs at the stage of unexpressed TDS is a promising tactic aimed at reducing the risk of a further increase in symptoms of anxiety and depression. nine0003
When choosing treatment tactics at all stages of the development of anxiety-depressive syndrome (ADS), the appointment of modern hypnotic drugs at the stage of unexpressed TDS is a promising tactic aimed at reducing the risk of a further increase in symptoms of anxiety and depression. nine0003
what to do, how it goes and what to do.
articles on psychology
- All articles
- Psychotherapy
- Personality
- Relationship
- Psychologist's advice
- Self-esteem
- Phobias and fears nine0043 Depression
- Insomnia
- Stress
- Contacts
- Jobs
A panic attack begins suddenly, when, it would seem, nothing foreshadows it.
The absence of a real cause is the most characteristic feature of this psychosomatic disorder. nine0123
nine0123
In this article, we will look at a problem that worries many: unexpected panic attacks during sleep or when a person wants to, but cannot sleep. Moreover, the second happens more often and is more difficult to bear, because it is at such moments that anxiety and tension reach their peak.
A panic attack at the time of insomnia can occur for the following reasons:
- conflicts, depressions , stress;
- severe mental or physical fatigue;
- excessive addiction to psychoactive substances (alcohol, cigarettes, caffeine), drug use;
- mental trauma received in childhood;
- periods of hormonal disorders;
- traumatic brain injuries and diseases of the brain;
- congenital or acquired neurasthenia; nine0044
- features of nature (tendency to anxiety, fears, suspiciousness, etc.).
Naturally, only the main factors are listed above. The reasons leading to panic attacks during moments of insomnia are very diverse. Each specific situation has its own nuances. The goal of the psychotherapist is to identify the source of the disorder and level it. Practice shows that it is the timeliness of contacting a good specialist that plays the main role in successfully getting rid of the disease. nine0003
The reasons leading to panic attacks during moments of insomnia are very diverse. Each specific situation has its own nuances. The goal of the psychotherapist is to identify the source of the disorder and level it. Practice shows that it is the timeliness of contacting a good specialist that plays the main role in successfully getting rid of the disease. nine0003
How a panic attack manifests itself
The following are considered the most characteristic symptoms of a panic attack:
- palpitations (the heart just "jumps" out of the chest), "mad" pulse;
- temperature fluctuations: fever changes to chills and vice versa;
- profuse cold sweat;
- "lump" in the throat, shortness of breath, severe shortness of breath; nine0049
- nausea;
- dizziness;
- stomach and intestinal cramps;
- upset stomach, diarrhea;
- loss of space-time perception;
- numbness and tremor of hands and feet.

- Chronic lack of sleep, which is the result of panic attacks, leads to a state of constant disharmony, weakens the body, provokes headaches and a feeling of weakness throughout the body. nine0044
- There is a danger of dysfunctions of the cardiovascular system.
- Dramatically reduced, or even completely lost performance.
- Increased irascibility, irritability, nervousness. A person begins to react sharply to literally everything.
- Fearing another panic attack, the patient delays going to bed, which only aggravates the situation.
- Each subsequent attack is more difficult to bear, as anxiety-depressive factors only intensify.
 nine0044
nine0044
Panic attacks
A panic attack is usually preceded by a person losing touch with reality. His consciousness is upset, the ability to think adequately is lost. Often this state persists even after the attack has ended, that is, in the morning and afternoon hours. Night torment, the inability to sleep normally lead to loss of strength. Even in the daytime, a person is not able to perceive reality normally, a certain “jump” from reality continues. nine0003
Regular panic attacks on the background of lack of sleep can lead to the fact that the patient will have a constant feeling of prostration, being outside of reality.
An attack can overtake a person before falling asleep, but usually this happens already in a half-asleep state. If we consider the situation as a physiological process, then panic is a spontaneous release of adrenaline into the blood. At night, the human body needs to rest, it enters a corresponding “sleepy” phase, so unexpected and untimely releases of active chemical compounds completely upset the picture. Often panic is accompanied by nightmares. It seems to a person that it is terrible dreams that provoke a panic attack, although in fact the opposite is true. nine0003
Often panic is accompanied by nightmares. It seems to a person that it is terrible dreams that provoke a panic attack, although in fact the opposite is true. nine0003
What to do if you suffer from insomnia and panic attacks
Sleep disturbance, fear, anxiety, and panic are all interconnected. Their "complex" impact is especially detrimental to both mental and physical health.
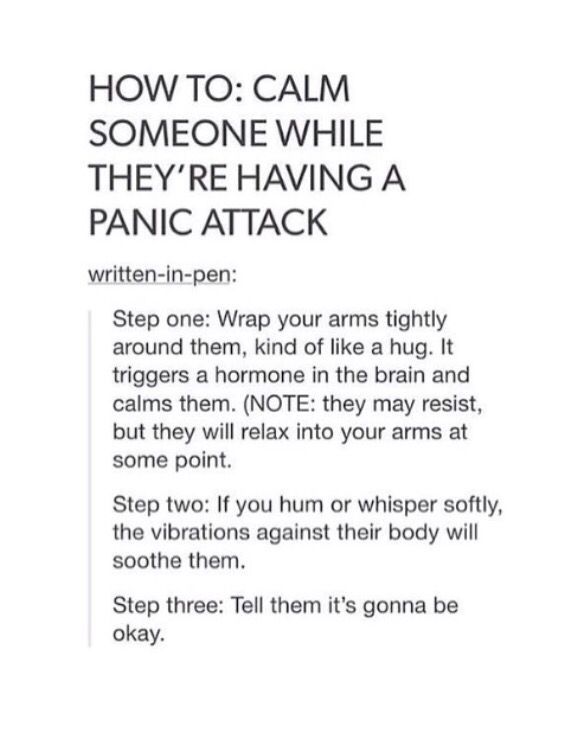
How to behave when a panic attack is approaching
In order to help yourself in time, you need to learn a few basic rules.
1. Breathe properly. Feeling alarming symptoms, in most cases a person cannot pull himself together: his breathing gets confused, becomes rapid and shallow. A significant amount of air still remains in the lungs after the previous breath, and a new portion is already entering, which provokes hyperventilation. It is hyperventilation that contributes to the onset of a panic attack. nine0003
Thus, noticing that breathing quickens, you should immediately establish control over it. After inhaling very deeply, continue to take slow breaths, not allowing yourself to stray. This should be done exclusively with the nose! The mouth must be closed. Make sure that the stomach is involved in the process, while the chest remains motionless. This method is called "belly breathing".
2. Relax your body muscles. To prevent muscle strain, do the following: sharply strain them to the limit, “shrink”, stopping breathing. Then just as sharply “throw off” tension from yourself, relax as much as possible, straighten up. Tilt your head and loosen your jaw muscles without opening your mouth. Start breathing as slowly as possible, pronouncing the sound “I” as you inhale. As you exhale, say lingeringly: "I spit ...". nine0003
To prevent muscle strain, do the following: sharply strain them to the limit, “shrink”, stopping breathing. Then just as sharply “throw off” tension from yourself, relax as much as possible, straighten up. Tilt your head and loosen your jaw muscles without opening your mouth. Start breathing as slowly as possible, pronouncing the sound “I” as you inhale. As you exhale, say lingeringly: "I spit ...". nine0003
3. Try to eliminate the tremor (shaking) of the hands and feet. A method known as "mad dance" can help here. First, with an effort of will, bring the trembling to a maximum. In other words, tremble with all your might. At the same time, many have an unexpected desire to pronounce some sounds, words or phrases, and even cry. There is no need to resist such a desire! Keep in mind only one setting: “dancing”, you will immediately fall asleep peacefully. Stop "dancing" as sharply as possible. nine0003
4. Drive away intrusive thoughts. If they “climb” into your head uncontrollably, causing torment, you can try to drive them away with the help of extraneous sounds and noises. Close your eyes and focus in turn on each, even the faintest sound that you can catch. Count all the noises you hear. The more noises and sounds your brain fixes, the faster you can “turn off” and fall asleep.
Close your eyes and focus in turn on each, even the faintest sound that you can catch. Count all the noises you hear. The more noises and sounds your brain fixes, the faster you can “turn off” and fall asleep.
5. Do not think about past and possible failures. nine0123 As soon as another terrible thought about the imminent approach of night and the likely repetition of a nightmare visits you, immediately drive it away.
Concluding our conversation, we hope that these tips will help you properly deal with panic attacks, defeat them and establish a good night's sleep. But the most effective way to get rid of insomnia, anxiety, weakness and nightmares is to seek help from a specialist.
If you find it difficult to cope with panic attacks yourself, you can always seek help from our specialists. nine0003
Our priority task is to do everything possible to bring joy, comfort and harmony back into your life!
Make an appointment with a psychologist:
tel.