Symptoms of grief and stress
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.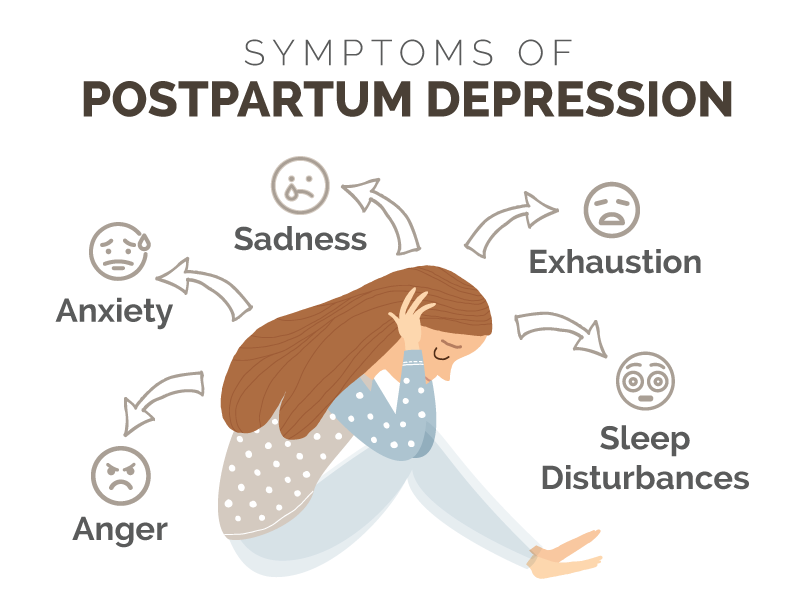
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
Phases of grief in psychology
The stages of the natural course of grief (the "work of grief") are characteristic of any phase of psychological stress, although, of course, their duration varies greatly depending on the severity of the trauma, as well as depending on other factors.
General symptoms of grief.
Somatic disorders
Psychological sphere
Specific breathing disorders (intermittent, especially when inhaling), physical fatigue, loss of appetite, sleep disturbances (nightmares, insomnia), possible symptoms of the disease from which the loved one died. nine0007
nine0007
Feeling of guilt, immersion in the image of the deceased.
Feeling of emptiness, fading, dullness of the world, irritability.
Idealization of the deceased.
Feeling abandoned, causing anger.
The conflict of this anger with idealization.
Other general symptoms of grief include specific disturbances in the sphere of meaning.
Look at everything, it seems that everything is connected with the deceased. Violated performance, attention, memory, which enhances and emphasizes the feeling of their own low value. nine0003
Phases of grief
1. Shock and numbness
Lasts from a few seconds to several weeks. The average is nine days.
A person does not suffer, his sensitivity to pain decreases, even the disturbing diseases “pass away”.
Loss of appetite, muscle weakness, immobility (sometimes replaced by fussiness). In consciousness - a feeling of unreality of what is happening, mental numbness, insensitivity, deafness.
Often afterward there are gaps in the memories of this period. The shock leaves the person in the time where the loved one was still alive. The present is accompanied by derealization and depersonalization sensations. Despite external well-being, the person is in an extremely serious condition. And his calmness can at any moment be replaced by an acute reactive state. nine0003
Help from loved ones.
It is useless to talk and console. You just have to walk with your tail.
If this is a child, it is better not to let him go to school.
Frequent tactile contact.
Serious feelings can be aroused to bring a person out of shock.
2. Phase. Suffering is disorganization.
Lasts an average of 40 days. This is the hardest period.
This phase is critical in relation to a person's further experiences, and sometimes it acquires significance for the entire life path. nine0007 Reality is, as it were, covered with a transparent muslin, through which the sensations of the presence of the deceased break through.
Persist and at first intensify bodily reactions - difficult shortened breathing, muscle weakness, asthenia - loss of energy, lump in the throat, feeling of emptiness in the stomach, tightness in the chest, increased sensitivity to odors, decrease or extreme increase in appetite, sexual dysfunction, sleep disturbances .
The period of greatest suffering, acute mental pain. These are feelings of emptiness and meaninglessness, despair, a feeling of abandonment, loneliness, fear, guilt, anxiety, helplessness. Preoccupation with the image of the deceased. Relationships with others are changing - loss of warmth, irritability, desire to retire. Daily activities change. nine0007 Sometimes there is an unconscious identification with the deceased, manifested in involuntary imitation of facial expressions, gestures, gait.
GRIEF WORK BECOMES THE MAIN ACTIVITY.
The main experience is the feeling of guilt.
A child in such a situation feels depressed, fearful.
Impaired memory (for current events) is typical.
If a person does not cope with grief, then he can forever remain in this phase of grief (pathological grief), or a victim will be formed from it. nine0007 Outwardly, in this phase, a person changes - facial expressions are smoothed out, the face takes on an expression of suffering. The man stoops, his hair grows dull. Health problems arise. At any moment a person can cry.
Help from relatives:
1. Let a person be alone if he wants to.
2. Always be at his disposal, listen and support.
3. Treat him gently.
4. Give the opportunity to cry, without interfering with "consolation".
5. At the end of the phase, gradually involve the person in socially useful activities. nine0007 6. Formation of feelings of real guilt. Demonstrate that they treat him like an ordinary person.
3. Phase of aftershocks and reorganization.
Comes after about forty days and lasts about a year.
Life returns to normal, sleep, appetite, daily activities are restored.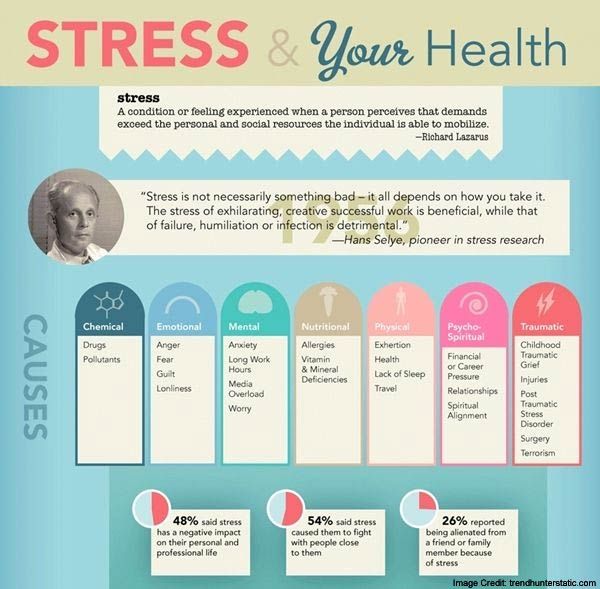 The experience of grief appears in the form of separate attacks, which, against the background of normal existence, are perceived more acutely than before. Loss gradually enters into life. Memories appear, free from pain, guilt, resentment. A person gets the opportunity to escape from the past, turns to the future - begins to plan his life without the deceased. nine0003
The experience of grief appears in the form of separate attacks, which, against the background of normal existence, are perceived more acutely than before. Loss gradually enters into life. Memories appear, free from pain, guilt, resentment. A person gets the opportunity to escape from the past, turns to the future - begins to plan his life without the deceased. nine0003
Help from loved ones:
To help turn to the future, build new life plans.
4. Completion phase
A person has to overcome some cultural barriers that make it difficult to complete the "work of grief". For example, the idea that the duration of grief is a measure of our love for the deceased.
The image of the deceased occupies a permanent place in our lives. A person, remembering the deceased, experiences not grief, but sadness that will remain forever. nine0003
Helping a child overcome grief.
It is worth observing the behavior of a child who has lost a loved one. In the first weeks, there may be a tendency to isolation, aggressiveness, anger, nervousness, isolation, inattention. We must be patient with him, do not force the child to do anything against his will.
In the first weeks, there may be a tendency to isolation, aggressiveness, anger, nervousness, isolation, inattention. We must be patient with him, do not force the child to do anything against his will.
Listen to the child, do not forget about tactile contact.
Involve the child's best friends.
Be prepared for any questions the child may have and be honest with him. nine0007 To prove to the child that crying is not a shame.
Never say to a child, "You don't think so, do you?", especially in relation to a child's fears or feelings of guilt.
Be in contact with parents.
Be especially attentive on "difficult" days (holidays, for example).
Secondary school.
1. It is recommended to have a class discussion on the topic of death.
2. The child should be able to be alone.
3. Among the comrades there should be an "assistant" who would take care of him. nine0007 4. Be patient with the forgetfulness of such a child.
5. Don't forget about your parents.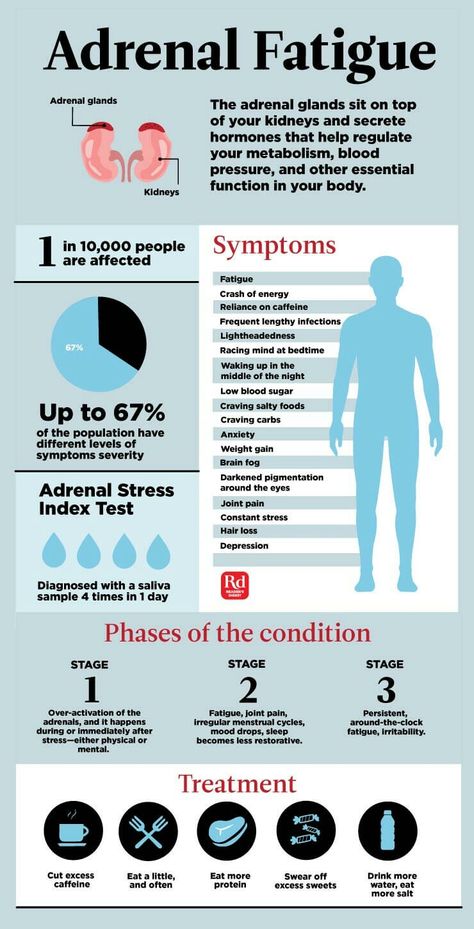 It's hard for them too.
It's hard for them too.
6. A teenager is mentally disorganized. It is worth inviting him to imagine that he is not in the classroom, but is engaged in his favorite sport. This helps the child to keep up with the class.
Pathological grief.
The normal "work of grief" can become a pathological process if a person "gets stuck" in one phase (usually in the second). All the symptoms of the second phase are intensified and emphasized, and the person develops the most severe syndrome of post-traumatic stress disorders in full. nine0003
Causes of pathological grief:
1. Conflicts or quarrels with a loved one before his death
2. Unfulfilled promises
3. Certain circumstances of the death of a loved one.
4. "The Unburied Dead" (did not attend the funeral, cannot believe in death)
ALWAYS AND IN ALL CASES THE DEATH OF A LOVED ONE SHOULD BE REPORTED.
ALWAYS, REGARDLESS OF AGE, IT IS RECOMMENDED TO TAKE CHILDREN TO THE FUNERAL OF A LOVED PERSON. nine0066
nine0066
Social programGOST Funeral services
Return to the list
Acute grief. Grief
A person in a state of acute grief.
Patient aged 60 years.
In January 2018, after a long illness, his twin brother, who suffered from glyblastoma, died. The patient has a history of the death of two children and a wife as a result of a disaster, the death of a sister due to melanoma, and the sudden death of parents. nine0003
Complaints. The status was dominated by emotional disorganization, anxiety, irritability, despair, fixation on one's state of health. Accordingly, the patient was at risk for the development of anxiety-depressive disorders.
To prevent these conditions , the patient was prescribed treatment with lithium ascorbate (Normotim) at a dose of 2 tablets 2 times a day on the third day after the death of his brother. nine0007
During the week of taking the drug , the condition stabilized, excessive anxiety stopped, fixation on various sensations in the body, but irritability, increased fatigue and drowsiness persisted.
On the second week of treatment, irritability disappeared, there were no deviations in the neurological status and hemodynamics.
In the fourth week, the transition to the 7th stage was recorded - the resolution of grief. The patient resigned himself to what happened, reconciled with it and returned to the pre-crisis state, while maintaining good working capacity and an active life position and desire to live on. nine0003
The course of treatment was 7 weeks.
Thus, the Normotim drug can be recommended as an aid to people in crisis situations, as well as for the prevention of depressive, anxiety and astheno-neurotic disorders.
Because during the year, repeated attacks of grief and despair are possible, the risk of depression, the patient was recommended to take Normotim again in 3-6 months to prevent anxiety and depressive disorders. nine0003
A bit of theory
There are 8 stages of the grief reaction, which were identified and described by A.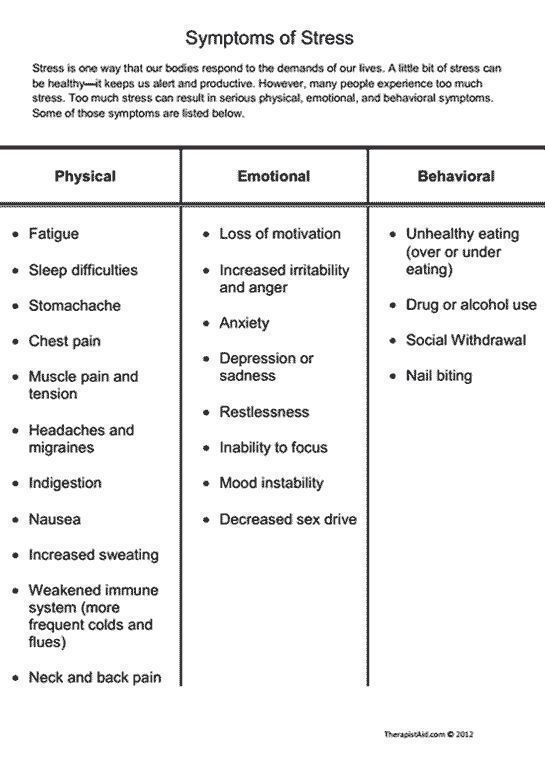 G. Ambrumova, (1983) and G.V. Starshenbaum (1994).
G. Ambrumova, (1983) and G.V. Starshenbaum (1994).
Stage 1 - with dominant emotional disorganization, which lasts from several minutes to several hours and is accompanied by an outbreak of negative feelings - panic, anger, despair. Behavior is dominated by affective disorganization with a temporary weakening of volitional control. nine0003
Stage 2 - hyperreactivity, duration 2-3 days. During this period, a person is overly active, active, prone to constant talk about the personality and deeds of the deceased. His mental status is dominated by emotional lability, dysthymia, anxiety, sometimes there is emotional dullness without fixation on the experience of grief.
Stage 3 - tension, duration - about a week. Mental status is dominated by psychophysical stress, anxiety. Outwardly, patients are constrained, their face is amimic, they are silent. Their condition is periodically interrupted by fussy activity, spasms in the throat or convulsive sighs. Often they get annoyed when trying to distract them or switch their attention to everyday topics. nine0003
nine0003
Stage 4 - the stage of search, which usually takes place in the second week after the loss of a loved one. The mental status is dominated by a dysthymic background of mood, loss of perspective and life meaning. The deceased is perceived by the patient as living: he speaks about him in the present tense, mentally talks with him, sometimes he perceives random passers-by as the deceased. During this period, illusions, hypnogagic and hypnopompic hallucinations are possible. There are two variants of the course of the fourth stage: anxious and oppositional. nine0003
Anxious option. In these persons, the mental status is dominated by anxiety, tension, concern and exaggeration of the problems that have arisen in connection with the death of a loved one. Many patients are fixated on their health and often find manifestations of the disease from which the deceased died.
opposition option. Patients are dominated by irritability, resentment, a sense of hostility and tension towards the attending physicians and relatives. As a rule, such a reaction is observed in persons who are psychologically dependent on the deceased, with a pronounced ambivalent reaction to him during his lifetime: from love to suppressed feelings of hostility and aggressiveness. nine0003
As a rule, such a reaction is observed in persons who are psychologically dependent on the deceased, with a pronounced ambivalent reaction to him during his lifetime: from love to suppressed feelings of hostility and aggressiveness. nine0003
Stage 5 - despair. This is the period of maximum mental anguish, which develops, as a rule, at 3-6 weeks after the loss of a significant loved one. The mental status of patients is dominated by complaints of insomnia, anxiety and fear, and ideas of self-blame, own low value and guilt are expressed. Patients experience loneliness, helplessness, note the loss of the meaning of life and future prospects. During this period, they are irritable, refuse to communicate with loved ones, often subjecting them to criticism. At the height of the experience, chest pain often occurs, accompanied by severe anxiety. nine0003
and anxiety.
Stage 6 - with elements of demobilization. This stage occurs in case of failure to resolve the stage of despair. The clinical picture of these individuals is dominated by neurotic syndromes (most often neurasthenic and with a predominance of vegetative-somatic disorders), masked subdepressions and depressions. During this period, people, as a rule, are uncommunicative, focused on inner experiences, they are overcome by a feeling of hopelessness, uselessness, loneliness. nine0003
The clinical picture of these individuals is dominated by neurotic syndromes (most often neurasthenic and with a predominance of vegetative-somatic disorders), masked subdepressions and depressions. During this period, people, as a rule, are uncommunicative, focused on inner experiences, they are overcome by a feeling of hopelessness, uselessness, loneliness. nine0003
Stage 7 - permission. As a rule, its duration is limited to several weeks. The patient comes to terms with what happened, comes to terms with it and begins to return to the pre-crisis state. Thoughts of loss "live in the heart." A.S. Pushkin described this state as "My sadness is light."
Stage 8 - recurrent. Within 1 year, attacks of grief and despair are possible, accompanied by depressive disorders. Provoking factors, as a rule, are certain calendar dates that are significant for the individual (birthday of the deceased, New Year and other holidays celebrated for the first time without a loved one, etc.