Ocd asking questions
Reassurance Seeking OCD | Is Seeking Reassurance Good Or Bad For OCD?
Reassurance (noun): the action of removing someone’s doubts or fears; a statement or comment that removes someone’s doubts or fears.
What is reassurance?
You’re walking around and you see a kid riding a bike. The kid falls over, and someone who seems to be the mother runs over and scoops them up, saying things like, “It’s okay. You’re going to be okay. It’s just a scratch.”
Or maybe you’re sitting in a coffee shop when you hear someone at the next table telling their friends about a recent breakup, listing all the reasons life will never be good again. The friends swoop in and say, “You can’t think like that. You’re just in a lot of pain right now. It wasn’t even that great of a relationship anyways.”
These are examples of people giving reassurance to someone else. And they’re so recognizable because reassurance is an everyday part of social interaction: someone expresses a doubt or fear, and you help them feel better by negating that doubt or fear. This happens in infinitely many ways each day. In fact, it’s hard to imagine how one would get through life without reassurance when things get really tough.
Is it normal to want reassurance?
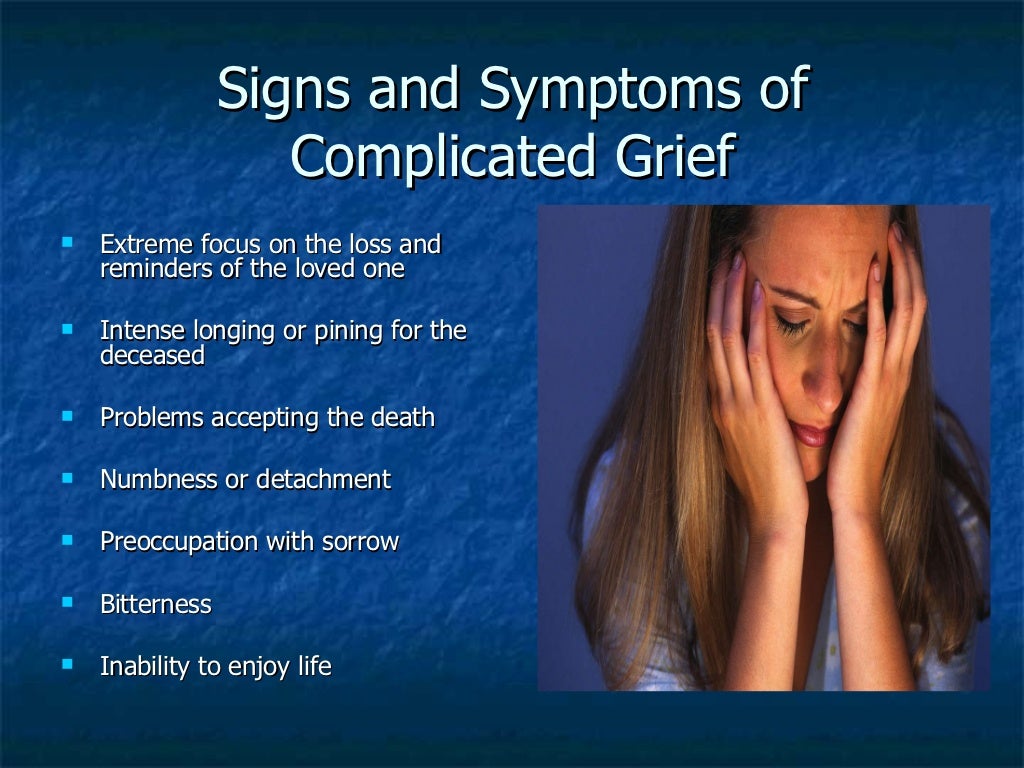
Everybody– from newborn infants to the oldest and wisest adults– feels a strong need to be reassured in situations that provoke fear, guilt, anxiety, stress, sadness, and so on. These tend to be unpleasant feelings, so we usually want to get rid of them. Reassurance often helps, at least in the short term, but it’s not always effective. Someone in grief, for example, is probably not going to hear They’re in a better place now and feel much better.
Barring a huge life change like illness or death, people also tend to learn other responses to stressful situations after some experience with them. After enough trips down the big slide at the park, most kids will stop asking whether or not it will be okay. By testing the world, we learn what is safe and what we should probably avoid. (Even this learning can be skewed by a bunch of factors, but let’s get into that another time.)
(Even this learning can be skewed by a bunch of factors, but let’s get into that another time.)
Reassurance, like most things we do, isn’t exactly good or bad. It’s certainly normal, and makes up a sizable portion of all the social interactions you’ll observe on a given day. For most people, especially adults, the need for reassurance is strong at times, but not persistently strong. And even when it is strong, it might seem plausible that there are other ways to proceed, besides temporarily getting rid of unpleasant feelings. But excessive reassurance seeking is associated with a number of mental health conditions, including depression, obsessive-compulsive disorder (OCD), and anxiety disorders.
Recovery from OCD requires habituation to the distress caused by uncertainty. And habituation cannot occur when reassurance keeps the person from getting exposure to uncertainty.
What does reassurance have to do with OCD?
Because we keep talking about most people, there’s clearly a group that doesn’t fit within some of the above statements. That would be people with OCD, health anxiety, and a few other psychiatric conditions. Let’s have a look at a 2017 paper written by Drs. Brynjar Halldorsson and Paul Salkovskis:
That would be people with OCD, health anxiety, and a few other psychiatric conditions. Let’s have a look at a 2017 paper written by Drs. Brynjar Halldorsson and Paul Salkovskis:
Excessive reassurance seeking (ERS) is particularly prominent in people who suffer from obsessive-compulsive disorder (OCD) and health anxiety… reassurance seeking functions in a similar way to compulsive checking in OCD with the added potential of transferring ‘responsibility’ for the feared harm to another person (Rachman 2002; Salkovskis 1985, 1999). However, it could also be seen as being a supportive maneuver, and is often considered in this way by sufferers and their loved ones.
They introduce the central complication of reassurance in OCD: on the one hand, reassurance seeking is a compulsive response to the distress caused by obsessions; on the other hand, it’s a very normal way to seek support from others. It’s what everyone else is doing, in other words. But the need for reassurance isn’t a passing thing for people with OCD.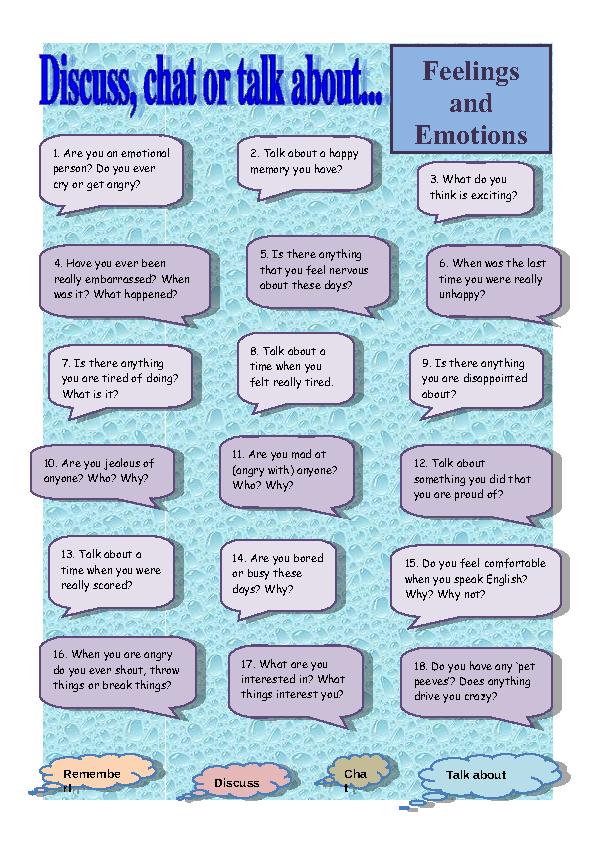
It might help for a little bit, but the urge tends to return quickly. As a result, people with OCD tend to ask for reassurance more often, and with more urgency, than others. And they may feel unable to proceed without it. The distinguishing factor for people with OCD isn’t that they seek reassurance; it’s that their reassurance seeking behaviors get out of their control quickly.
Why do people with OCD seek reassurance?
Because researchers haven’t found a definite cause of OCD, attempts to explain this on a neurological level aren’t going to satisfy. From a psychological perspective, ocd reassurance-seeking behaviors are another attempt by people with OCD to get rid of the uncertainty at the core of the condition. If you feel unsure about something, you might check it repeatedly- or you might try to get someone else to tell you that things will work out just fine.
When you ask for reassurance, you’re basically asking someone else to neutralize the distress of confronting uncertainty, by presenting a different way of viewing the situation.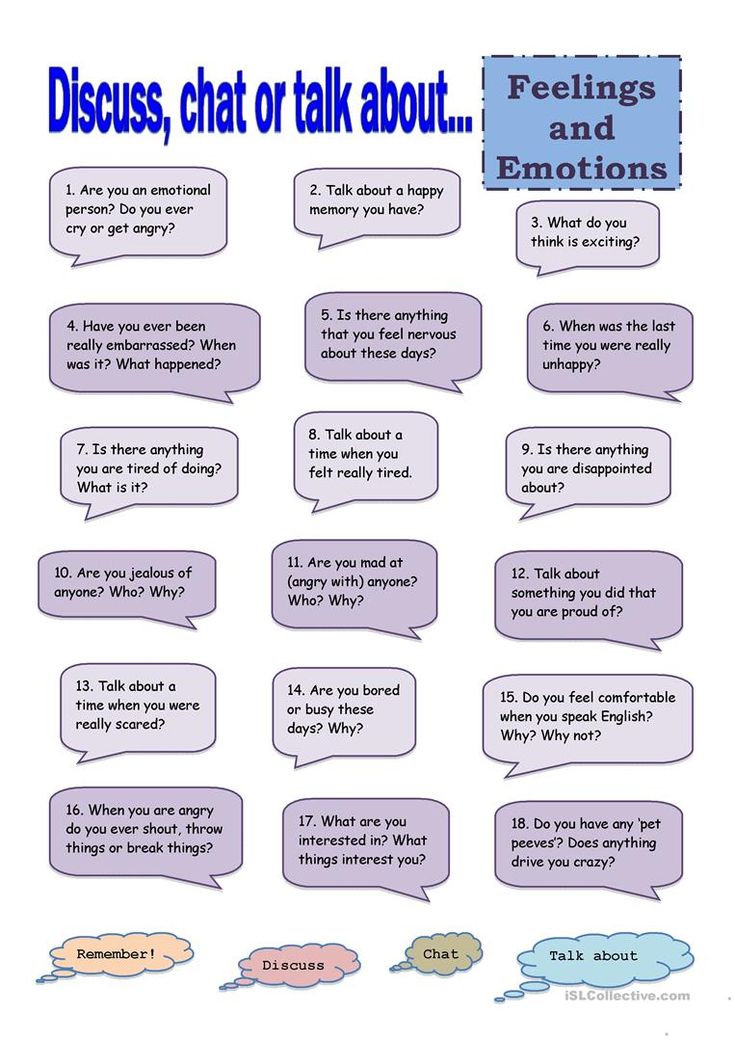 It feels like a big relief to have this distress taken away, but in the long term it guarantees that you won’t learn how to tolerate uncertainty (or even learn that you
can tolerate it). You’ll be stuck in a loop of perceiving uncertainty, growing distressed, seeking reassurance. In this way, reassurance-seeking is both a compulsion (a repetitive behavior meant to minimize distress) and a form of avoidance.
It feels like a big relief to have this distress taken away, but in the long term it guarantees that you won’t learn how to tolerate uncertainty (or even learn that you
can tolerate it). You’ll be stuck in a loop of perceiving uncertainty, growing distressed, seeking reassurance. In this way, reassurance-seeking is both a compulsion (a repetitive behavior meant to minimize distress) and a form of avoidance.
Let’s use a metaphor that’s imperfect but hopefully instructive. There are two people next to each other lifting weights. They’re of equal strength, but only one is confident. The other is so full of doubt that– as the more confident one keeps trying, failing, adjusting, even succeeding– they keep calling a friend over to help. After a few months of this, the confident one has grown much stronger. But the less confident one has only become more and more convinced that they need help, and hasn’t become able to lift anything on their own.
Does reassurance keep people from getting better?
People with OCD seem particularly bothered by not having absolute certainty, at least in a few key areas depending on one’s specific symptoms. As countless research papers and personal stories tell us, recovery from OCD requires habituation to the distress caused by uncertainty. And habituation– the lessening of a physiological or emotional response after repeated exposure to a stimulus– cannot occur when reassurance keeps the person from getting that exposure to uncertainty.
Some research suggests that people get worse when they’re getting reassurance because the feared stimulus grows even more fearsome as others help them avoid it. At the very least, getting reassurance doesn’t help people get better. Like other compulsions, reassurance seeking works by negative reinforcement: because it gets rid of an unpleasant feeling, the behavior is strengthened. The result? We just want more and more reassurance.
The insatiable desire for reassurance, always increasing due to operant conditioning, combines with the impossibility of certainty to lock people into the endless quest of trying to make sure things will be alright. Unsurprisingly, this can result in all kinds of unfortunate situations where other people end up resenting the person who is constantly asking for reassurance. Because friends and family might pull away, it’s common for people to end up lonely just because they didn’t know how to avoid asking too much of loved ones.
Unsurprisingly, this can result in all kinds of unfortunate situations where other people end up resenting the person who is constantly asking for reassurance. Because friends and family might pull away, it’s common for people to end up lonely just because they didn’t know how to avoid asking too much of loved ones.
What can we do instead of reassurance?
Remember that research paper that we discussed above? Later they bring up an interesting concept: reassurance-seeking versus support-seeking.
Here’s how they define
reassurance-seeking:Verbal and/or non-verbal interaction with someone, who you perceive has access to potentially threat relieving information, with the intention of increasing your perceived sense of certainty of safety from harm.
And this is
support-seeking:Interpersonal behaviour, verbal or non-verbal, that is intended to get encouragement, confidence, or assistance to cope with feelings of distress.

The difference is subtle, which points to the confusion most of us face when trying to decide how to help someone. But remember the chain of events: uncertainty -> distress -> behavior. Reassurance-seeking is an attempt to get rid of the distress by getting rid of the uncertainty that underlies it. Support-seeking, however, is an attempt to have someone encourage you while you deal with the distress caused by your uncertainty. It means allowing the uncertainty and distress to exist while also acknowledging that it’s easier to succeed with the support of others.
If we think now of the person on the other end of these interactions, the one offering either reassurance or support, the distinction can be even more subtle. Because of this subtlety, it might require saying something as direct as, “It seems like you’re looking for reassurance, which I understand because you’re dealing with difficult feelings right now. But I know you can get through this, as you have so many times before, and I also know it’s important for you to get through these situations so you can learn to trust yourself and the world a little more. I’m here with you, but I can’t tell you whether or not things will be fine.”
I’m here with you, but I can’t tell you whether or not things will be fine.”
Even better, whether you’re struggling with OCD or want to help someone else stop relying on reassurance, we’d strongly suggest you look into exposure and response prevention (ERP) therapy. Conducted by a licensed OCD therapist, ERP is the best way to recover from OCD and unlearn reassurance-seeking behaviors. This unique therapy is specifically designed to help people face their obsessions and resist compulsions in healthy and productive ways.
ERP is most effective when practiced with a therapist who has received specialized training in OCD treatment. They know what to anticipate when you describe your thoughts and behaviors, and how to build your personalized treatment program. Their expertise is in teaching you how to manage your OCD so you don’t feel stuck trying to “get rid of” the unpleasant feelings caused by disturbing thoughts.
This is the same important training all of our NOCD Therapists receive. The goal of NOCD is to reduce your OCD symptoms within just a few weeks of live one-on-one video therapy. You’ll be welcomed into our supportive peer community, with 24/7 access to personalized self-management tools built by people who have been through OCD and successfully recovered.
The goal of NOCD is to reduce your OCD symptoms within just a few weeks of live one-on-one video therapy. You’ll be welcomed into our supportive peer community, with 24/7 access to personalized self-management tools built by people who have been through OCD and successfully recovered.
Did you now that ERP is most effective when the therapist conducting the treatment has experience with OCD and training in ERP.? At NOCD, all therapists specialize in OCD and receive ERP-specific training. Schedule a free call today with a member of the NOCD clinical team to learn more about how a licensed OCD therapist can help you get better. This consultation is free and doesn’t take very long—and it could be one of the most important calls you ever make.
How to Stop the Cycle
Anna knew Taylor would find her text annoying, but she sent it anyway. “Does this sound right?” she wrote, pasting her drafted email response to a speaking panel she’d been asked to attend. It was a straightforward confirmation, but Anna, 28, still struggled with it. Should she add an exclamation mark after the first sentence? Was it too formal? Anna was convinced her email needed to be worded perfectly — or else her speaking opportunity might fall through. The only way she could make sure was to ask her friend for a second (and third) opinion.
Should she add an exclamation mark after the first sentence? Was it too formal? Anna was convinced her email needed to be worded perfectly — or else her speaking opportunity might fall through. The only way she could make sure was to ask her friend for a second (and third) opinion.
Taylor, 29, knew Anna needed her, but she couldn’t understand why she felt this much anxiety about something so inconsequential. “Can’t she just figure it out herself?” she thought. She had tried encouragement (“Don’t worry too much; it’s just an email!”) and a harsh-but-loving approach (“You really don’t need my help with this”). She’d also tried avoiding Anna’s requests, but she felt too guilty to give her friend the cold shoulder. Sometimes, it seemed to Taylor that no matter how many times she reassured her, Anna wouldn’t be able to send an email on her own.
What she didn’t know was that this behavior is indicative of just right obsessive-compulsive disorder (OCD), an OCD subtype that causes people to feel an incredible amount of distress if something feels “off. ” According to OCD expert and licensed professional counselor Davida Vaughn, M.S., Ed.S., an ongoing need for reassurance can be a sign that a person is resorting to reassurance seeking as a compulsion. Continual texts like Anna’s may be part of an OCD cycle.
” According to OCD expert and licensed professional counselor Davida Vaughn, M.S., Ed.S., an ongoing need for reassurance can be a sign that a person is resorting to reassurance seeking as a compulsion. Continual texts like Anna’s may be part of an OCD cycle.
OCD is a prevalent chronic mental health condition that affects millions of adults in the United States alone. It’s been ranked by the World Health Organization as a top 10 most disabling condition. There are many different subtypes of OCD, but the OCD cycle is generally the same: an intrusive thought leads to anxiety or distress, leading to a compulsive behavior. The symptoms of OCD can range from minor disturbances to a person’s daily tasks, to obsessive rituals that completely take over a person’s life.
It’s normal to want to make sure a professional email is worded properly, especially when stakes are high. But for Anna, the stress could feel insurmountable. Without a second opinion, she’d often leave an email in her draft folder for weeks. The consequences of sending an email that wasn’t “just right” were so terrifying, Anna would rather not send any messages at all.
Without a second opinion, she’d often leave an email in her draft folder for weeks. The consequences of sending an email that wasn’t “just right” were so terrifying, Anna would rather not send any messages at all.
Without a second opinion, Anna would often leave an email in her draft folder for weeks. The consequences of sending an email that wasn’t “just right” were terrifying.
Reassurance seeking is one of the more common OCD compulsions. When someone is not yet diagnosed, the constant need to hear others’ opinions can feel disorienting. “Especially before I knew I had OCD, I couldn’t understand why I couldn’t make a decision without getting someone else’s reassurance. I needed someone else to tell me it was right,” Casie David, a peer advocate at NOCD, tells me. “It got very bad to the point where I needed someone there to make a decision.”
To Anna, Taylor’s reassurance felt urgent. In the moment, it seemed like the only thing that would calm her down. Taylor, meanwhile, was strengthening Anna’s dependence on her response. “The hard thing about reassurance is that for most people, [reassurance] would help, but it feeds into the OCD,” David says. “You have an intrusive thought, you ask someone for reassurance, and you might feel better for some time, but then the OCD keeps cycling through. It comes back.”
Taylor, meanwhile, was strengthening Anna’s dependence on her response. “The hard thing about reassurance is that for most people, [reassurance] would help, but it feeds into the OCD,” David says. “You have an intrusive thought, you ask someone for reassurance, and you might feel better for some time, but then the OCD keeps cycling through. It comes back.”
OCD is often nicknamed the “doubting disease.” It latches on to any ounce of uncertainty and starts spinning endless what-if scenarios. When people with OCD become overwhelmed with the stress of obsessive thoughts, it often feels like reassurance from a loved one is the only thing that can calm them down. They might ask questions like:
- “Are you sure you washed your hands?”
- “Is this food fresh? When did you buy it?”
- “Do you think I would ever harm someone?”
- “Do you think I’m a bad person for getting upset with my friend?”
For the person on the receiving end, it’s natural to want to help by answering. (“Of course you would never harm someone.” “Yes, I washed my hands.” “I just bought the food yesterday; don’t worry, it’s fresh.”) But this reinforces the idea that the OCD compulsions were helpful and necessary. (“See, I knew I needed to ask. I would have been in danger otherwise.”)
(“Of course you would never harm someone.” “Yes, I washed my hands.” “I just bought the food yesterday; don’t worry, it’s fresh.”) But this reinforces the idea that the OCD compulsions were helpful and necessary. (“See, I knew I needed to ask. I would have been in danger otherwise.”)
Providing support to someone with OCD can be a difficult balance. You want to make someone feel better, but you don’t want to make their condition worse. “I think it can be very taxing on other people because it probably feels like you can’t give someone the right answer enough times,” David says.
Providing support to someone with OCD can be a difficult balance. You want to make someone feel better, but you don’t want to make their condition worse.
Seeking reassurance doesn’t always provide short-term relief. Sometimes it simply isn’t reassuring. “It’s hard when you ask someone for reassurance and they don’t give you the answer you’re expecting — it sends you down a whole other spiral,” David says. For people with OCD, reassurance-seeking can turn into a never-ending cycle. They might start doubting the responses they get, wondering, “What if Taylor is wrong?” or “What if she was busy when she responded and didn’t look over my email properly?” They might then seek reassurance from more people — and feel even more anxious if their answers don’t line up.
For people with OCD, reassurance-seeking can turn into a never-ending cycle. They might start doubting the responses they get, wondering, “What if Taylor is wrong?” or “What if she was busy when she responded and didn’t look over my email properly?” They might then seek reassurance from more people — and feel even more anxious if their answers don’t line up.
Underneath the need for reassurance is discomfort with uncertainty. Anna wants to know with 100% confidence that her emails are perfectly worded, but of course she’ll never know with absolute confidence. That can leave someone with OCD in a perpetual cycle of anxiety as they seek an unattainable level of perfection.
How to respond to reassurance seekingLoved ones may find it difficult to know how to help someone with OCD, but when it comes to reassurance, mental health professionals say there’s a better way to respond. “The best and most helpful thing for families to do is not provide reassurance,” says Vaughn. Instead, she advises friends and family to respond with phrases such as “I’m here for you, but I can’t answer that for you,” or “I can’t tell you whether things will turn out OK,” or “Is this part of reassurance seeking?”
“The best and most helpful thing for families to do is not provide reassurance,” says Vaughn. Instead, she advises friends and family to respond with phrases such as “I’m here for you, but I can’t answer that for you,” or “I can’t tell you whether things will turn out OK,” or “Is this part of reassurance seeking?”
In OCD therapy, patients learn how to prevent themselves from engaging in the compulsions they’ve been dependent on. “Once you get to the point where you’re in recovery, I think it’s a lot easier to tell people, ‘I might ask for reassurance, but don’t give it to me. I need to figure this out on my own,’” David says. “It’s frustrating, but at the end of the day it’s better, because it’s forcing you to deal with it on your own and accept that you might not have the right answer.”
It can also be difficult for friends and family to spot the difference between OCD-driven reassurance and a well-meaning question. David says to consider how reassurance seeking falls under specific OCD subtypes: “If someone has harm OCD and they’re asking for reassurance, like, ‘Do you think I hurt this person?’ ‘Do you think I would ever hurt this person?,’ that reassurance is different from ‘Do you think I parked here OK?’”
During recovery, people with OCD often find that when they stop themselves from asking for reassurance, their intrusive thoughts become less intense. As part of Anna’s treatment process, she began sending an email without asking Taylor for reassurance. It was scary at first, but eventually she discovered she was capable of writing without her fears becoming a reality. “It’s dealing with uncertainty,” David describes: “‘I don’t know if I did this right. I don’t know if this is correct, but I need to be able to live with that.’”
As part of Anna’s treatment process, she began sending an email without asking Taylor for reassurance. It was scary at first, but eventually she discovered she was capable of writing without her fears becoming a reality. “It’s dealing with uncertainty,” David describes: “‘I don’t know if I did this right. I don’t know if this is correct, but I need to be able to live with that.’”
It wasn’t that Anna’s emails were “perfect.” It was that she became OK with the fact that they wouldn’t be. And she discovered an exclamation mark didn’t make or break her speaking opportunity.
If you or someone you know is struggling with OCD, you can schedule a free call today with the NOCD clinical team to learn more about how a licensed therapist can help. At NOCD, all therapists specialize in OCD and receive ERP-specific training. ERP is most effective when the therapist conducting the treatment has experience with OCD and training in ERP.
5 questions about OCD and obsessions
Medical psychologist and psychoanalyst Lesya Loriashvili answers 5 questions about obsessive-compulsive disorder and obsessions. What is the difference between OCD and obsessiveness, how do I know if I or a loved one needs help, and why it is important to share my worries with others or a therapist.
What is the difference between OCD and obsessiveness, how do I know if I or a loved one needs help, and why it is important to share my worries with others or a therapist.
What is the difference between OCD and obsession?
OCD is considered a mental illness because there are certain neural connections that organically make a person do these rituals. This is not just a psychological symptom, it is already a psychiatric symptom that requires treatment. Obsessive states, obsessions are psychological symptoms, it does not require medical treatment, but it requires more awareness of why this happens, especially if it interferes with a person. And then another question: perhaps this does not interfere? There are rituals, they suit a person, define and somehow structure life. And in general, everything, a person is fine with this, it does not interfere with loved ones - why not? nine0003
How can I figure out what I might have?
I would say that there are different levels: there is just anxiety that does not result in this type of behavior, there is anxiety that results in ritual - rituals, for example, are ordinary, normal, they do not turn into obsession. The next level of obsession is when these rituals are very important, they are very important and it is difficult to live without them. There is an obsessive state when a person practically cannot refuse these rituals, and he already experiences them as obsessive, they begin to seriously interfere with his life in everyday life. But there is OCD - when a person is practically filled, filled and absorbed by these incessant rituals, and he cannot live, work, build relationships, sex life normally. It almost completely absorbs all spheres of his life and limits him very much. nine0003
The next level of obsession is when these rituals are very important, they are very important and it is difficult to live without them. There is an obsessive state when a person practically cannot refuse these rituals, and he already experiences them as obsessive, they begin to seriously interfere with his life in everyday life. But there is OCD - when a person is practically filled, filled and absorbed by these incessant rituals, and he cannot live, work, build relationships, sex life normally. It almost completely absorbs all spheres of his life and limits him very much. nine0003
How obsession works, is there an example?
For example, a woman checks her iron or kettle all the time before going out, can't go to work, to some extent this is already beginning to interfere with her life. She is critical of this, realizing that she turned off this iron, but still comes back several times to double-check. This does not mean that the iron is not really turned off, but that she has a high level of anxiety, which makes her calm down. This ritual is actually a calming ritual. The ritual always has such a logical explanation: if the iron is not turned off, the house will burn down, if you do not wash your hands, there will be bacteria. There is always some logic to obsessions, but behind that logic there is always a feeling, a very strong feeling, and one is not necessarily linked to the other. That is, anxiety may be about a divorce from her husband, and it results in the ritual turning off the iron or kettle ten times and rechecking the doors. And it doesn't have to be directly related. It is precisely the task of psychotherapy to reveal what exactly the feelings are connected with, realizing that the logical part, the external part is not necessarily connected with real anxiety. But there was always some event, some event that led to the appearance of rituals. Almost always a person remembers when, from what moment it started for him. nine0003
This ritual is actually a calming ritual. The ritual always has such a logical explanation: if the iron is not turned off, the house will burn down, if you do not wash your hands, there will be bacteria. There is always some logic to obsessions, but behind that logic there is always a feeling, a very strong feeling, and one is not necessarily linked to the other. That is, anxiety may be about a divorce from her husband, and it results in the ritual turning off the iron or kettle ten times and rechecking the doors. And it doesn't have to be directly related. It is precisely the task of psychotherapy to reveal what exactly the feelings are connected with, realizing that the logical part, the external part is not necessarily connected with real anxiety. But there was always some event, some event that led to the appearance of rituals. Almost always a person remembers when, from what moment it started for him. nine0003
How do you know when a loved one needs specialist help?
If a person is not critical of this, but everyone around them sees and understands that this is not the norm, this is already quite serious - and you need to go to the doctors, because the person is not critical of his behavior, and it clearly interferes with him. Most likely, you need to contact a psychiatrist, up to taking medications, since you need to extinguish these symptoms. It can only grow.
Most likely, you need to contact a psychiatrist, up to taking medications, since you need to extinguish these symptoms. It can only grow.
There are obsessive states that a person perceives critically: he understands that there are too many of them, that there are too many of these rituals, that they already interfere with him, but he can cope with them one way or another, he does not go into continuous repetition, continuous rituals, there are improvements and deteriorations in it - depending on the anxiety, on the situation in life. There is enough psychotherapy and self-awareness, reflection, and the help of loved ones. There is nothing too serious in this, it is rather a psychological experience. nine0003
What to do about OCD and obsessions?
People are embarrassed to talk about their symptoms because they think they will be thought badly of them, that they are not normal. It's such a level of shame and fear that they'd rather hide than talk about it. At best, they will turn to a specialist, where it is normal to talk about it. At worst, they will not turn to a specialist and will not tell anyone about it, but then most likely the symptoms will increase, the ritual will become more frequent, increase, they will become worse. The sooner they turn to a specialist or the sooner they can share this with their friends, acquaintances, the better, because they can be a little more critical of this, and their anxiety, which actually lies under these rituals, will result in talk. If a person shares his anxiety, yes, it will decrease. nine0003
At worst, they will not turn to a specialist and will not tell anyone about it, but then most likely the symptoms will increase, the ritual will become more frequent, increase, they will become worse. The sooner they turn to a specialist or the sooner they can share this with their friends, acquaintances, the better, because they can be a little more critical of this, and their anxiety, which actually lies under these rituals, will result in talk. If a person shares his anxiety, yes, it will decrease. nine0003
call to serve with neuroses
About 70% of Russians suffer from neurosis, and the number of patients is only growing every year. Chronic stress, high fatigue, trauma, infectious diseases are just some of the reasons that can lead to a neurotic or borderline mental disorder. Therefore, more and more young men of military age are wondering whether citizens with neuroses are recognized as fit for service and are obsessive-compulsive disorder (OCD) and the army compatible? Let's explore these issues together. nine0003
nine0003
What is the diagnosis
OCD is a mental illness that manifests itself in the form of thoughts and fears that are constantly present in a person, leading to cyclic actions of a pathological nature. Obsessive-compulsive disorder leaves a negative imprint on a person’s entire life, since he cannot cope with his phobias on his own, therefore, he begins to avoid people, things that can exacerbate his fears. nine0003
Main causes of OCD
According to official data, the following factors can lead to the disease:
- hereditary predisposition. If one of the close family members suffers from OCD, then the risks of passing on a pathological phobia to a child increase many times over.
- Brain diseases. Some patients who suffer from this disorder have evidence of changes in brain function. nine0042
- Stress. Traumatic events can lead to the development of OCD.
- The presence of concomitant mental disorders, for example, substance abuse, depression.
Important! The first symptoms of OCD begin to appear during adolescence. The older a person becomes, the more pronounced will be the fears and phobias. The increase in symptoms occurs with stress, so the exacerbation of a mental disorder can be due to any factor. nine0003
What symptoms accompany the disease
To understand whether people diagnosed with OCD are eligible for draft, it is important to understand what symptoms accompany the patient and how this can affect his life. All signs can be divided into two large groups.
The symptoms of obsession are:
- suspiciousness;
- excessive craving for order, intolerance if things are out of place; nine0042
- fear of soiling clothes or touching a dirty surface with your hands;
- intrusive sexual thoughts;
- fear of losing control over one's own actions, which will lead to a possible risk of harm to oneself or others, etc.
Signs of OCD can be the actions of a person aimed at constantly disinfecting an object before touching it. In addition, the constant fear of getting into an accident indicates a mental disorder, which does not allow driving a vehicle, or, for example, a desire to do obscene things in the presence of "spectators", etc. nine0003
In addition, the constant fear of getting into an accident indicates a mental disorder, which does not allow driving a vehicle, or, for example, a desire to do obscene things in the presence of "spectators", etc. nine0003
Compulsiveness symptoms are actions that help a person reduce the anxiety that comes with a flare-up:
- feverish cleaning;
- solving examples in the mind;
- pronunciation of a certain sequence of numbers until the moment of calm;
- double-checking how objects lie;
- repetition of prayers, etc.
Pay attention! Obsessive-compulsive disorder can lead to numerous complications, both physically and psychologically. For example, such patients often develop contact dermatitis due to constant cleaning with disinfectants. In the most difficult cases, a complication of the mental state is possible - patients with OCD have thoughts of suicide.
Neurosis in the Schedule of Diseases
Obsessive-compulsive disorder is one of the types of neuroses. Therefore, in order to answer the question of whether they are recruited for mobilization with OCD, and whether recruits with this diagnosis are called up for military service, one should refer to the Schedule of Diseases (Appendix No. 1 to Decree of the Government of the Russian Federation No. 565). nine0003
Therefore, in order to answer the question of whether they are recruited for mobilization with OCD, and whether recruits with this diagnosis are called up for military service, one should refer to the Schedule of Diseases (Appendix No. 1 to Decree of the Government of the Russian Federation No. 565). nine0003
In general, if we analyze section 5 "Mental disorders", then the only disease for which a valid category of fitness cannot be set is schizophrenia. In schizoid disorders within the framework of the IHC, category "D" is assigned. With other deviations, it is possible to recognize a conscript: fit, limited fit and unfit for the army.
Medical examination of ROC recruits is carried out in accordance with Art. 17 Schedules of diseases. This disease belongs to the category of neurotic, stress-related and somatoform disorders. According to this article, it is possible to assign 3 categories of validity: nine0003
- "B" (fit with minor restrictions for service).
 This health group is assigned to conscripts who, as part of the examination, will have a mild illness that lasts a short period of time. This takes into account the fact that the disorder was successfully treated before the time of the call.
This health group is assigned to conscripts who, as part of the examination, will have a mild illness that lasts a short period of time. This takes into account the fact that the disorder was successfully treated before the time of the call. - "B" (limited fit for service). Mental disorder is of moderate severity. The duration of the disease is short. There is no talk of a complete cure of the patient from OCD, but in order to put down this category of suitability, the disease must be in the stage of stable compensation. In other words, the patient's organism must adapt to the effects of the neurosis. In addition, this category includes neuroses that are difficult to treat, and after the end of the course, an exacerbation occurs. If in everyday life it is possible to cope with symptoms, then in the army a conscript will not be able to follow orders with neuroses. nine0042
- "D" (not good). Mental disorders that are not treatable fall under this category. If the symptoms of OCD do not disappear even after the patient has received psychotherapeutic and drug therapy.

The concept of suitability and unfitness in patients with OCD when called up for military service or as part of mobilization has very blurred boundaries. Doctors must carefully diagnose recruits in order to have an objective idea of whether the mental disorder is in the stage of compensation or, for example, long-term remission. If your rights within the framework of the military medical examination have been violated, our experts will help you file a complaint. We work remotely 24/7. nine0003
Whether they take for mobilization with OKR
How are ROC and mobilization related? This question is asked by both the conscripts themselves, who are faced with neurosis, and their relatives. Consider two situations:
- Can they recruit people who were released from the army in connection with the ROC as part of the recruitment process.
- Are persons subject to mobilization who did military service in the army, but after demobilization faced OCD.
 nine0042
nine0042
In the first case, it depends on what category of fitness was set for the conscript. If he was found to be partially fit for military service (health group "B"), then they can be recruited as part of mobilization. However, in the first place, the call will be extended to those liable for military service with a category of fitness "A" or "B".
As for diagnosing OCD after the end of military service, such a citizen can be given a summons, but during the medical examination, a decision can be made to assign the reservist an unfit category for military service ("D"). In such situations, he is commissioned. nine0003
Example
The reserve officer received a summons from the military commissariat about his arrival at the military commissariat as part of mobilization measures. Since in recent years he suffered from neurosis, during the VVK he provided certificates from a psychiatrist, in which the diagnosis was indicated - OCD. By decision of the draft commission, he was assigned an unsuitable category of fitness, and he was discharged from the military service.
By decision of the draft commission, he was assigned an unsuitable category of fitness, and he was discharged from the military service.
Litigation
nine0002 Gamov A.N., sent an administrative claim to the court through his representative Prozorova L.A. to the military commissariat for the Maloyaroslavetsky district of the Kaluga region with a request to recognize the decision of the draft board to assign him a category of fitness "D" in accordance with Art. 17 Schedules of diseases - illegal.In 2011, the recruit underwent a military medical examination, according to the results of which he was commissioned with category “D” (unfit for military service). The plaintiff believes that the representatives of the VVK did not have any legal or medical grounds for this. nine0003
In the summer of 2011, due to great mental overload, the plaintiff Gamov applied for help to a specialized clinic, where he underwent the necessary therapy. The discharge summary indicates that he has been fully recovered and can begin further education.
As part of the draft board, the plaintiff was consulted by a psychiatrist and, on the basis of an extract from the recruit's personal card, he was assigned category "D" (unfit for military service). The plaintiff believes that this health group was established in direct contradiction to the medical documentation, which was drawn up by the doctors at the Clinic of Neurosis. He has never been registered with a psychiatrist. In addition, according to the results of an examination in a psycho-neurological dispensary in 2021, no mental disorders were identified in him. nine0139In considering the case, the court took into account both the arguments of the plaintiff and the defendant. Thus, according to the data received, conscript Gamov did not use his legal right to challenge the decision of the draft commission. The plaintiff did not indicate good reasons for the deadlines for appeal officially fixed by law. Gamow went to court only 7 years later, after he had reached the age of 27.

Guided by articles 175-180 of the Code of Administrative Procedure of the Russian Federation, the court ruled: Gamow’s claims to invalidate the decision of the military commissariat for the Maloyaroslavetsky district of the Kaluga region to assign a category of fitness “D” (unfit for the army) to a conscript should be dismissed. nine0003
FAQ
Why can't conscripts with OCD serve if the disease is compensated?
+
Military conditions are unfavorable for individuals suffering from OCD. This can cause a significant progress of neurosis: a soldier may have suicidal thoughts, unmotivated aggression against other soldiers. Therefore, such a conscript who has access to weapons poses a potential threat to others. That is why the medical commission in most cases recognizes people with OCD as unfit for the army. nine0003
Is it possible to hide a neurosis while passing the VVK in order to get a suitable category?
+
During the medical examination, the passage of a psychiatrist is a mandatory procedure.