Multiple personality disorder name
Dissociative Identity Disorder (Multiple Personality Disorder): Signs, Symptoms, Treatment
Written by WebMD Editorial Contributors
In this Article
- What Is Dissociative Identity Disorder?
- Who Is At Risk for DID?
- How to Recognize Dissociative Identity Disorder and Its Associated Mental Disorders
- How Is Dissociative Identity Disorder Diagnosed?
- What Other Psychiatric Illnesses Might Occur With DID?
- Are There Famous People With Dissociative Identity Disorder?
- What's the Treatment Plan for Dissociative Identity Disorder?
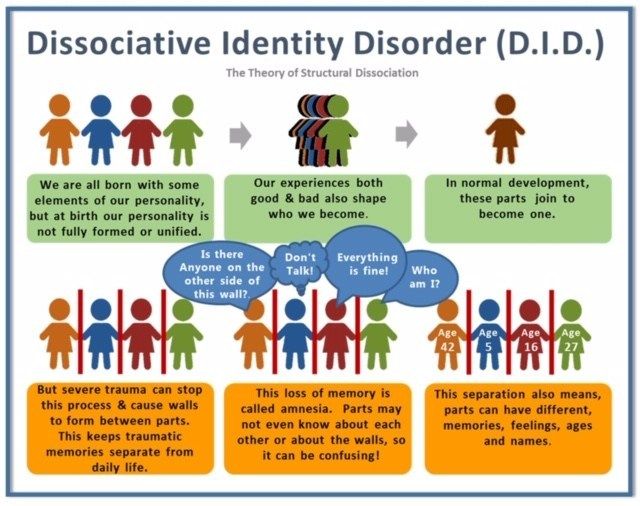
Dissociative identity disorder (previously known as multiple personality disorder) is thought to be a complex psychological condition that is likely caused by many factors, including severe trauma during early childhood (usually extreme, repetitive physical, sexual, or emotional abuse).
What Is Dissociative Identity Disorder?
Dissociative identity disorder is a severe form of dissociation, a mental process which produces a lack of connection in a person's thoughts, memories, feelings, actions, or sense of identity. Dissociative identity disorder is thought to stem from a combination of factors that may include trauma experienced by the person with the disorder. The dissociative aspect is thought to be a coping mechanism -- the person literally shuts off or dissociates themselves from a situation or experience that's too violent, traumatic, or painful to assimilate with their conscious self.
Who Is At Risk for DID?
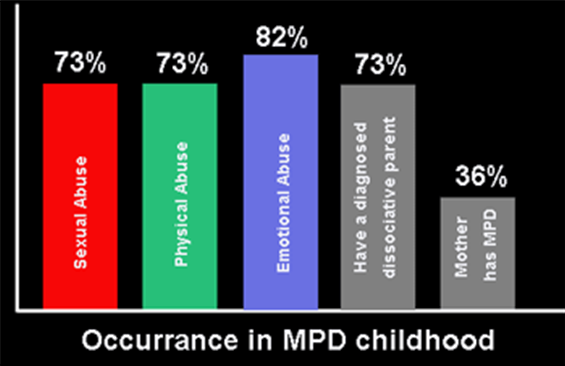
Research indicates that the cause of DID is likely a psychological response to interpersonal and environmental stresses, particularly during early childhood years when emotional neglect or abuse may interfere with personality development. As many as 99% of individuals who develop dissociative disorders have recognized personal histories of recurring, overpowering, and often life-threatening disturbances or traumas at a sensitive developmental stage of childhood (usually before age 6).
Dissociation may also happen when there has been persistent neglect or emotional abuse, even when there has been no overt physical or sexual abuse.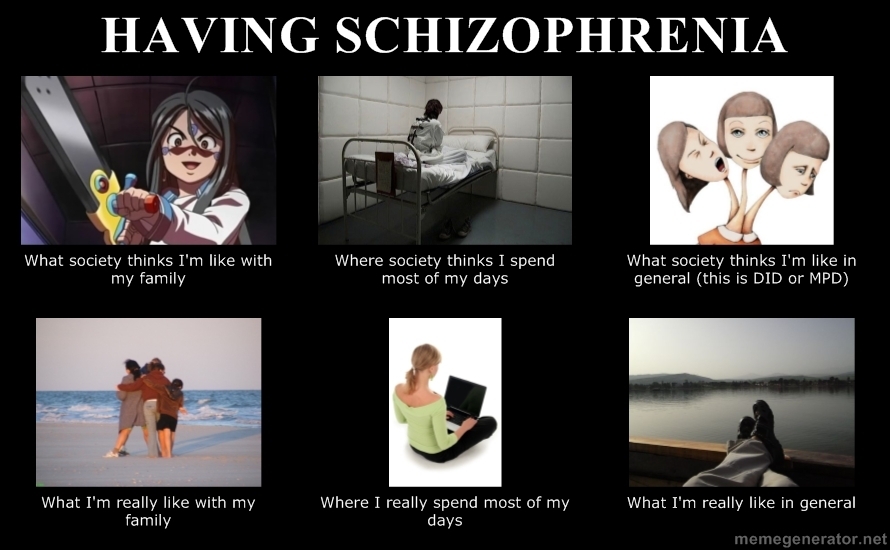 Findings show that in families where parents are frightening and unpredictable, the children may become dissociative. Studies indicate DID affects about 1% of the population.
Findings show that in families where parents are frightening and unpredictable, the children may become dissociative. Studies indicate DID affects about 1% of the population.
How to Recognize Dissociative Identity Disorder and Its Associated Mental Disorders
Dissociative identity disorder is characterized by the presence of two or more distinct or split identities or personality states that continually have power over the person's behavior. With dissociative identity disorder, there's also an inability to recall key personal information that is too far-reaching to be explained as mere forgetfulness. With dissociative identity disorder, there are also highly distinct memory variations, which may fluctuate.
Although not everyone experiences DID the same way, for some the "alters" or different identities have their own age, sex, or race. Each has their own postures, gestures, and distinct way of talking. Sometimes the alters are imaginary people; sometimes they are animals. As each personality reveals itself and controls the individuals' behavior and thoughts, it's called "switching." Switching can take seconds to minutes to days. Some seek treatment with hypnosis where the person's different "alters" or identities may be very responsive to the therapist's requests.
As each personality reveals itself and controls the individuals' behavior and thoughts, it's called "switching." Switching can take seconds to minutes to days. Some seek treatment with hypnosis where the person's different "alters" or identities may be very responsive to the therapist's requests.
Other symptoms of dissociative identity disorder may include headache, amnesia, time loss, trances, and "out of body experiences." Some people with dissociative disorders have a tendency toward self-persecution, self-sabotage, and even violence (both self-inflicted and outwardly directed). As an example, someone with dissociative identity disorder may find themselves doing things they wouldn't normally do, such as speeding, reckless driving, or stealing money from their employer or friend, yet they feel they are being compelled to do it. Some describe this feeling as being a passenger in their body rather than the driver. In other words, they truly believe they have no choice.
There are several main ways in which the psychological processes of dissociative identity disorder change the way a person experiences living, including the following:
- Depersonalization.
 This is a sense of being detached from one's body and is often referred to as an "out-of-body" experience.
This is a sense of being detached from one's body and is often referred to as an "out-of-body" experience. - Derealization. This is the feeling that the world is not real or looking foggy or far away.
- Amnesia. This is the failure to recall significant personal information that is so extensive it cannot be blamed on ordinary forgetfulness. There can also be micro-amnesias where the discussion engaged in is not remembered, or the content of a meaningful conversation is forgotten from one second to the next.
- Identity confusion or identity alteration. Both of these involve a sense of confusion about who a person is. An example of identity confusion is when a person has trouble defining the things that interest them in life, or their political or religious or social viewpoints, or their sexual orientation, or their professional ambitions. In addition to these apparent alterations, the person may experience distortions in time, place, and situation.
It is now acknowledged that these dissociated states are not fully mature personalities, but rather they represent a disjointed sense of identity. With the amnesia typically associated with dissociative identity disorder, different identity states remember different aspects of autobiographical information. There is usually a "host" personality within the individual, who identifies with the person's real name. Ironically, the host personality is usually unaware of the presence of other personalities.
How Is Dissociative Identity Disorder Diagnosed?
Making the diagnosis of dissociative identity disorder takes time. It's estimated that individuals with dissociative disorders have spent seven years in the mental health system prior to accurate diagnosis. This is common, because the list of symptoms that cause a person with a dissociative disorder to seek treatment is very similar to those of many other psychiatric diagnoses. In fact, many people who have dissociative disorders also have coexisting diagnoses of borderline or other personality disorders, depression, and anxiety.
The DSM-5 provides the following criteria to diagnose dissociative identity disorder:
- Two or more distinct identities or personality states are present, each with its own relatively enduring pattern of perceiving, relating to, and thinking about the environment and self.
- Amnesia must occur, defined as gaps in the recall of everyday events, important personal information, and/or traumatic events.
- The person must be distressed by the disorder or have trouble functioning in one or more major life areas because of the disorder.
- The disturbance is not part of normal cultural or religious practices.
- The symptoms cannot be due to the direct physiological effects of a substance (such as blackouts or chaotic behavior during alcohol intoxication) or a general medical condition (such as complex partial seizures).
The distinct personalities may serve diverse roles in helping the individual cope with life's dilemmas. For instance, there's an average of two to four personalities present when the patient is initially diagnosed. Then there's an average of 13 to 15 personalities that can become known over the course of treatment. Environmental triggers or life events cause a sudden shift from one alter or personality to another.
Then there's an average of 13 to 15 personalities that can become known over the course of treatment. Environmental triggers or life events cause a sudden shift from one alter or personality to another.
What Other Psychiatric Illnesses Might Occur With DID?
Along with the dissociation and multiple or split personalities, people with dissociative disorders may experience a number of other psychiatric problems, including symptoms:
- Depression
- Mood swings
- Suicidal tendencies
- Sleep disorders (insomnia, night terrors, and sleep walking)
- Anxiety, panic attacks, and phobias (flashbacks, reactions to stimuli or "triggers")
- Alcohol and drug abuse
- Compulsions and rituals
- Psychotic-like symptoms (including auditory and visual hallucinations)
- Eating disorders
Are There Famous People With Dissociative Identity Disorder?
Famous people with dissociative identity disorder include comedienne Roseanne Barr, Adam Duritz, and retired NFL star Herschel Walker.
Walker wrote a book about his struggles with DID, along with his suicide attempts, explaining he had a feeling of disconnect from childhood to the professional leagues. To cope, he developed a tough personality that didn't feel loneliness, one that was fearless and wanted to act out the anger he always suppressed. These "alters" could withstand the abuse he felt; other alters came to help him rise to national fame. Treatment helped Walker realize that these alternate personalities are part of dissociative identity disorder, which he was diagnosed with in adulthood.
What's the Treatment Plan for Dissociative Identity Disorder?
There are currently no formal, evidence-based guldelines to treat DID. Many treatments are based on case reports or are even controversial.
While there's also no "cure" for dissociative identity disorder, long-term treatment can be helpful, if the patient stays committed. Effective treatment includes:
- Psychotherapy: Also called talk therapy, the therapy is designed to work through whatever triggered and triggers the DID.
 The goal is to help “fuse” the separate personality traits into one consolidated personality that can control the triggers. This therapy often includes family members in the therapy.
The goal is to help “fuse” the separate personality traits into one consolidated personality that can control the triggers. This therapy often includes family members in the therapy. - Hypnotherapy. Used in conjunction with psychotherapy, clinical hypnosis can be used to help access repressed memories, control some of the problematic behaviors which accompany DID as well as help integrate the personalities into one.
- Adjunctive therapy. Therapies such as art or movement therapy have been shown to help people connect with parts of their mind that they have shut off to cope with trauma.
There are no established medication treatments for dissociative identity disorder, making psychologically-based approaches the mainstay of therapy. Treatment of co-occurring disorders, such as depression or substance use disorders, is fundamental to overall improvement. Because the symptoms of dissociative disorders often occur with other disorders, such as anxiety and depression, medicines to treat those co-occurring problems, if present, are sometimes used in addition to psychotherapy.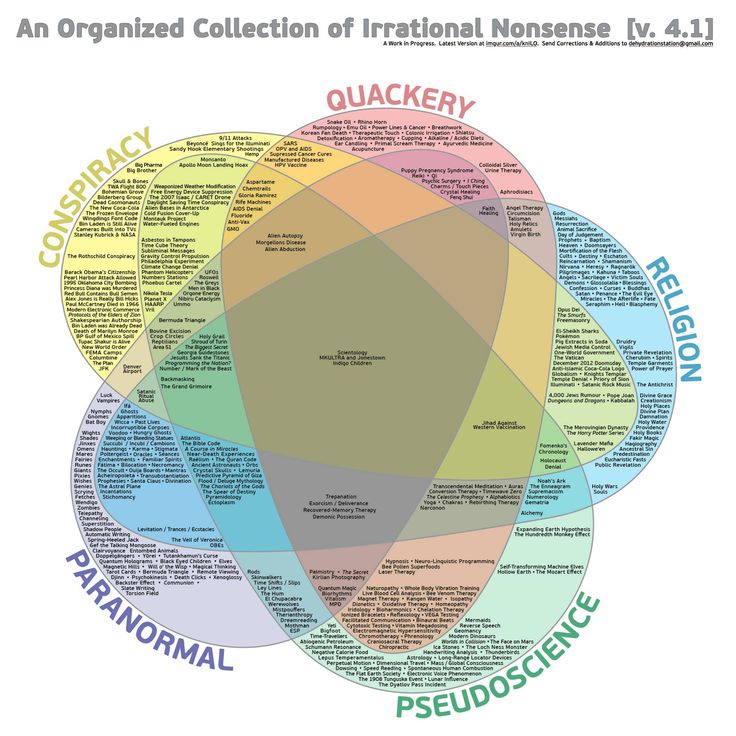
Dissociative disorders - Symptoms and causes
Overview
Dissociative disorders are mental disorders that involve experiencing a disconnection and lack of continuity between thoughts, memories, surroundings, actions and identity. People with dissociative disorders escape reality in ways that are involuntary and unhealthy and cause problems with functioning in everyday life.
Dissociative disorders usually develop as a reaction to trauma and help keep difficult memories at bay. Symptoms — ranging from amnesia to alternate identities — depend in part on the type of dissociative disorder you have. Times of stress can temporarily worsen symptoms, making them more obvious.
Treatment for dissociative disorders may include talk therapy (psychotherapy) and medication. Although treating dissociative disorders can be difficult, many people learn new ways of coping and lead healthy, productive lives.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Signs and symptoms depend on the type of dissociative disorders you have, but may include:
- Memory loss (amnesia) of certain time periods, events, people and personal information
- A sense of being detached from yourself and your emotions
- A perception of the people and things around you as distorted and unreal
- A blurred sense of identity
- Significant stress or problems in your relationships, work or other important areas of your life
- Inability to cope well with emotional or professional stress
- Mental health problems, such as depression, anxiety, and suicidal thoughts and behaviors
There are three major dissociative disorders defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association:
- Dissociative amnesia.
 The main symptom is memory loss that's more severe than normal forgetfulness and that can't be explained by a medical condition. You can't recall information about yourself or events and people in your life, especially from a traumatic time. Dissociative amnesia can be specific to events in a certain time, such as intense combat, or more rarely, can involve complete loss of memory about yourself. It may sometimes involve travel or confused wandering away from your life (dissociative fugue). An episode of amnesia usually occurs suddenly and may last minutes, hours, or rarely, months or years.
The main symptom is memory loss that's more severe than normal forgetfulness and that can't be explained by a medical condition. You can't recall information about yourself or events and people in your life, especially from a traumatic time. Dissociative amnesia can be specific to events in a certain time, such as intense combat, or more rarely, can involve complete loss of memory about yourself. It may sometimes involve travel or confused wandering away from your life (dissociative fugue). An episode of amnesia usually occurs suddenly and may last minutes, hours, or rarely, months or years. - Dissociative identity disorder. Formerly known as multiple personality disorder, this disorder is characterized by "switching" to alternate identities. You may feel the presence of two or more people talking or living inside your head, and you may feel as though you're possessed by other identities. Each identity may have a unique name, personal history and characteristics, including obvious differences in voice, gender, mannerisms and even such physical qualities as the need for eyeglasses.
 There also are differences in how familiar each identity is with the others. People with dissociative identity disorder typically also have dissociative amnesia and often have dissociative fugue.
There also are differences in how familiar each identity is with the others. People with dissociative identity disorder typically also have dissociative amnesia and often have dissociative fugue. - Depersonalization-derealization disorder. This involves an ongoing or episodic sense of detachment or being outside yourself — observing your actions, feelings, thoughts and self from a distance as though watching a movie (depersonalization). Other people and things around you may feel detached and foggy or dreamlike, time may be slowed down or sped up, and the world may seem unreal (derealization). You may experience depersonalization, derealization or both. Symptoms, which can be profoundly distressing, may last only a few moments or come and go over many years.
When to see a doctor
Some people with dissociative disorders present in a crisis with traumatic flashbacks that are overwhelming or associated with unsafe behavior. People with these symptoms should be seen in an emergency room.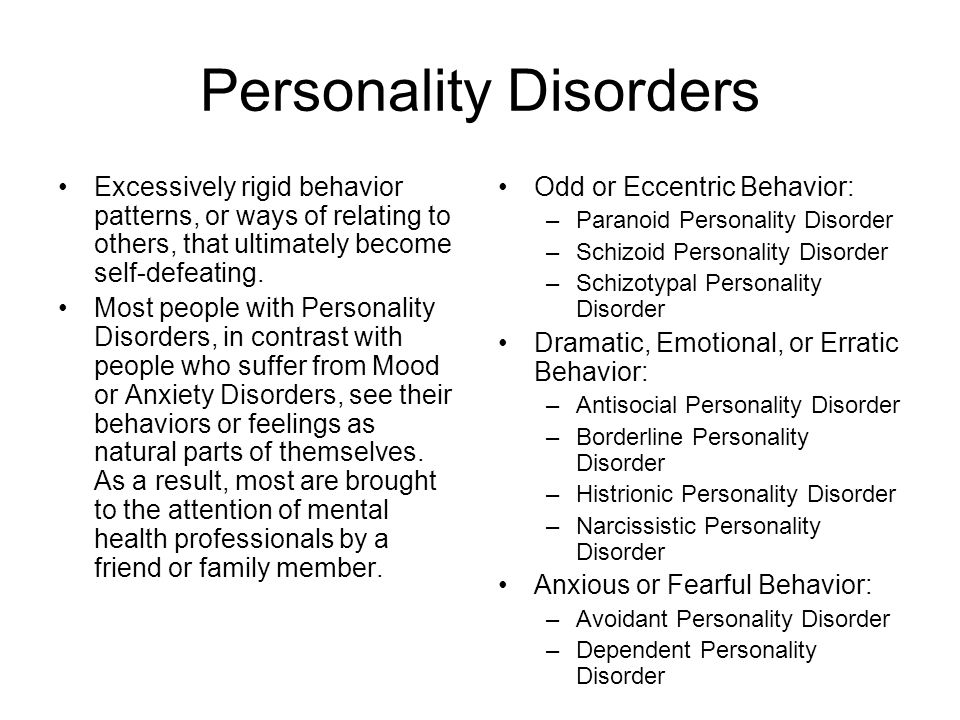
If you or a loved one has less urgent symptoms that may indicate a dissociative disorder, call your doctor.
Suicidal thoughts or behavior
If you have thoughts of hurting yourself or someone else, call 911 or your local emergency number immediately, go to an emergency room, or confide in a trusted relative or friend. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
Dissociative disorders usually develop as a way to cope with trauma. The disorders most often form in children subjected to long-term physical, sexual or emotional abuse or, less often, a home environment that's frightening or highly unpredictable. The stress of war or natural disasters also can bring on dissociative disorders.
Personal identity is still forming during childhood. So a child is more able than an adult to step outside of himself or herself and observe trauma as though it's happening to a different person. A child who learns to dissociate in order to endure a traumatic experience may use this coping mechanism in response to stressful situations throughout life.
A child who learns to dissociate in order to endure a traumatic experience may use this coping mechanism in response to stressful situations throughout life.
Risk factors
People who experience long-term physical, sexual or emotional abuse during childhood are at greatest risk of developing dissociative disorders.
Children and adults who experience other traumatic events, such as war, natural disasters, kidnapping, torture, or extended, traumatic, early-life medical procedures, also may develop these conditions.
Complications
People with dissociative disorders are at increased risk of complications and associated disorders, such as:
- Self-harm or mutilation
- Suicidal thoughts and behavior
- Sexual dysfunction
- Alcoholism and drug use disorders
- Depression and anxiety disorders
- Post-traumatic stress disorder
- Personality disorders
- Sleep disorders, including nightmares, insomnia and sleepwalking
- Eating disorders
- Physical symptoms such as lightheadedness or non-epileptic seizures
- Major difficulties in personal relationships and at work
Prevention
Children who are physically, emotionally or sexually abused are at increased risk of developing mental health disorders, such as dissociative disorders. If stress or other personal issues are affecting the way you treat your child, seek help.
If stress or other personal issues are affecting the way you treat your child, seek help.
- Talk to a trusted person such as a friend, your doctor or a leader in your faith community.
- Ask for help locating resources such as parenting support groups and family therapists.
- Look for churches and community education programs that offer parenting classes that also may help you learn a healthier parenting style.
If your child has been abused or has experienced another traumatic event, see a doctor immediately. Your doctor can refer you to a mental health professional who can help your child recover and adopt healthy coping skills.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
how multiple personality arises - T&P
Multiple personality disorder is a bright but rather controversial disease that still causes heated discussions among doctors and scientists. Someone doubts whether it exists at all, someone doubts whether this state should be considered a deviation from the norm.
 "Theories and Practices" remembered how the research of this psychiatric phenomenon began and why one should not rush to evaluate it.
"Theories and Practices" remembered how the research of this psychiatric phenomenon began and why one should not rush to evaluate it. Dissociative identity disorder is a condition in which, in addition to the main personality, the patient has at least one (and often more) subpersonality that periodically “takes control” of the body and acts in accordance with their own ideas about life. These ideas can be very different from the habits and philosophy of the real owner of the body.
Despite the fact that some experts consider this disease iatrogenic - that is, provoked by the careless words of doctors or watching a "scientific" TV show - there is a number of evidence that indicates the opposite. One of the most impressive is the history of the disease. Cases of dissociative disorder were also recorded when neither psychotherapists nor TV shows were in sight. However, psychiatry itself did not exist.
One of the first described cases of dissociative personality disorder occurred at the end of the 18th century in the German city of Stuttgart. A revolution had just taken place in France, and the aristocrats, saving their lives, fled from their native country to neighboring states, including Germany. A young resident of Stuttgart took their misfortunes too close to her heart. She suddenly had a second personality - a Frenchwoman. She not only spoke her “native language” perfectly, but also coped noticeably worse with German, she had a noticeable accent. The Frenchwoman who appeared was of aristocratic blood, and her manners and habits fully corresponded to her status. It is noteworthy that the German girl did not remember what the "Frenchwoman" was doing, and she did not know anything about the legal mistress of the body.
A revolution had just taken place in France, and the aristocrats, saving their lives, fled from their native country to neighboring states, including Germany. A young resident of Stuttgart took their misfortunes too close to her heart. She suddenly had a second personality - a Frenchwoman. She not only spoke her “native language” perfectly, but also coped noticeably worse with German, she had a noticeable accent. The Frenchwoman who appeared was of aristocratic blood, and her manners and habits fully corresponded to her status. It is noteworthy that the German girl did not remember what the "Frenchwoman" was doing, and she did not know anything about the legal mistress of the body.
The young German woman was not the only person with this disease in her century, but nevertheless her illness turned out to be extremely rare - in total, 76 cases of dissociative identity disorder were documented up to the middle of the 20th century. Interestingly, in recent decades, much more of them have been described - today more than 40 thousand people with this diagnosis live in the world. However, this does not mean the beginning of an "epidemic" - psychiatry, with all its arsenal of medicines, appeared only in the middle of the last century, and, accordingly, control over the incidence of such disorders began not much earlier.
However, this does not mean the beginning of an "epidemic" - psychiatry, with all its arsenal of medicines, appeared only in the middle of the last century, and, accordingly, control over the incidence of such disorders began not much earlier.
To date, quite a lot of books and articles have been written about multiple personality disorder, both popular and academic. The most interesting thing about it is, perhaps, the moment of the onset of the disease in childhood. No one is born a “ready-made”, whole person. Growing up, the child experiences many emotions and experiences that are loosely related to each other. Over time, they integrate together, forming one common identity. However, the development of a child does not always go smoothly. In cases where children at an early age (about 2 years) are separated from their mother when they experience abuse or some traumatic experience, childhood experiences can remain segregated and lead to the formation of two or more personalities. Almost all patients with multiple personality disorder (more precisely, 97-98%) mention a difficult childhood with traumatic experiences.
Almost all patients with multiple personality disorder (more precisely, 97-98%) mention a difficult childhood with traumatic experiences.
Dissociative identity disorder often begins in childhood, but may appear later. Over the years, patients, as a rule, have an increasing number of "tenants". Since individuals, as a rule, perform certain functions, help to cope with certain life situations, with the emergence of new tasks and problems, new residents appear who are able to cope with them. Each of the subpersonalities has its own worldview, its own habits, gestures and facial expressions, even age and intelligence. At certain moments, by the good will of the "owner" or against it, some of the personalities gain control over the body, and everything done by it during use, as a rule, is not controlled and is not remembered by the patient himself.
A key issue in the lives of patients with dissociative personality disorder is the relationship that has developed in the “team”.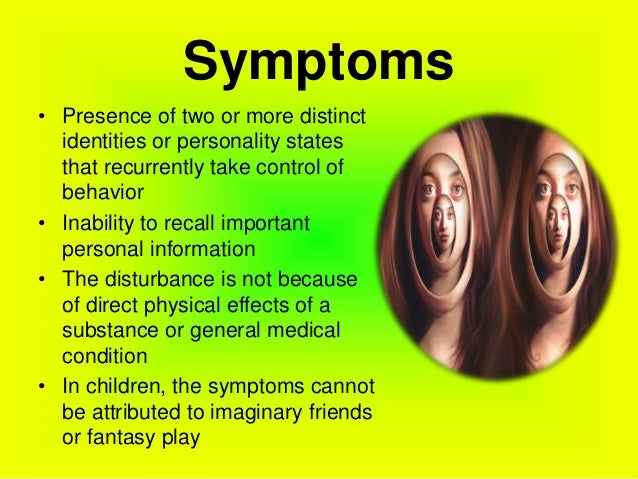 Sub-personalities may or may not be aware of each other's existence, be aggressive or silently roam museums at their own time, negotiate rental schedules with the owner of the body, or regularly stage power grabs. The treatment strategy also depends on these factors - it is based on psychotherapy, and although its ultimate goal is to come to the integration of personalities into one, an important task in the process is the "neutralization" of dangerous tenants, and the organization of harmonious relations between all subpersonalities.
Sub-personalities may or may not be aware of each other's existence, be aggressive or silently roam museums at their own time, negotiate rental schedules with the owner of the body, or regularly stage power grabs. The treatment strategy also depends on these factors - it is based on psychotherapy, and although its ultimate goal is to come to the integration of personalities into one, an important task in the process is the "neutralization" of dangerous tenants, and the organization of harmonious relations between all subpersonalities.
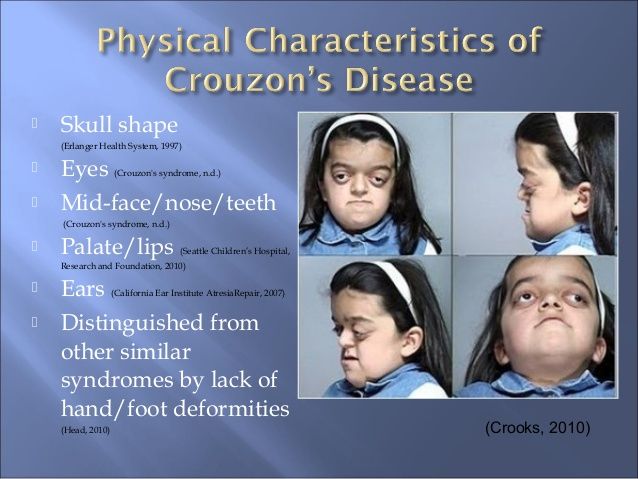
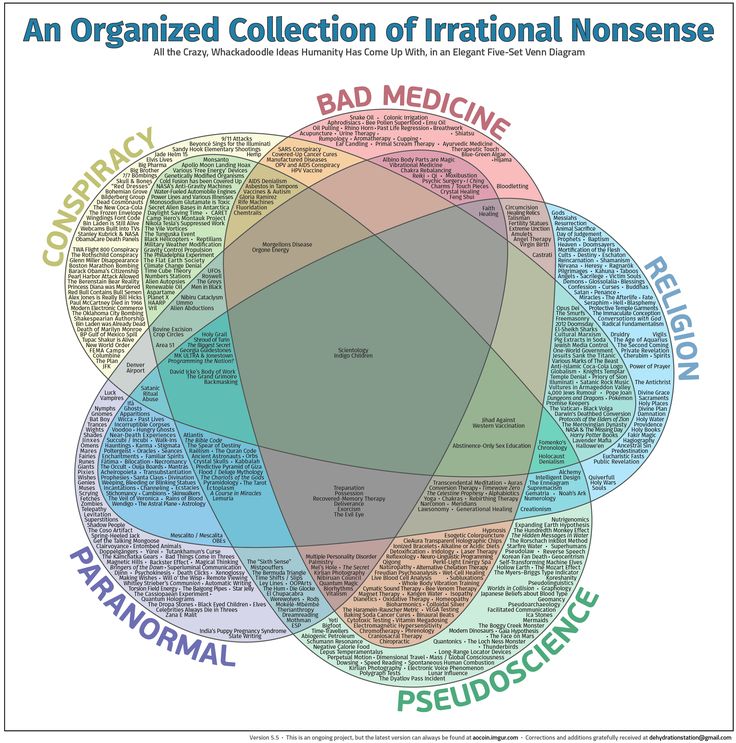
More than one person in one body is unfortunately not the only symptom of dissociative identity disorder. It is often accompanied by depression, anxiety disorders, phobias, sleep and eating disorders, even hallucinations. Dissociative disorder is sometimes confused with schizophrenia, but these diseases can be distinguished - in schizophrenia, as a rule, the symptoms are perceived as enemy actions of aliens, the KGB or members of the Masonic lodge, which is not the case with dissociative disorder. In addition, splitting identities in schizophrenia is a simple separation of mental functions due to a general breakdown of personality, but with DID (Dissociative identity disorder - another name for multiple personality disorder), everything is much more complicated. Functions are not only separated, but also become full-fledged individuals: each of them has their own style of clothing, supports their football team and has their own ideas about how to spend time.
In addition, splitting identities in schizophrenia is a simple separation of mental functions due to a general breakdown of personality, but with DID (Dissociative identity disorder - another name for multiple personality disorder), everything is much more complicated. Functions are not only separated, but also become full-fledged individuals: each of them has their own style of clothing, supports their football team and has their own ideas about how to spend time.
Treatment of patients diagnosed with multiple personality disorder is usually long, difficult and emotionally costly. However, not everyone agrees that it should be treated at all. The American psychologist James Hillman, the founder of the school of archetypal psychology, is convinced that the position that multiple personality syndrome is considered a disorder is nothing more than a stereotype that can and should be fought, advocating the right of people with this diagnosis to be considered no less normal than others.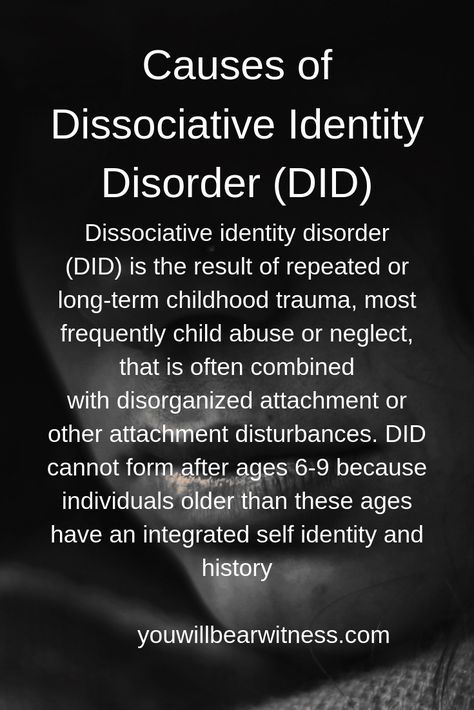 The goal of therapy, according to Hillman, is only the creation of harmonious relations of all subpersonalities. Many patients also support his position. The ideologist of such a movement was Truddy Chase, who refused to integrate subpersonalities into a single whole and instead established mutually beneficial cooperation with them. She wrote about her experience in the book When the Rabbit Howls. Today, Truddy is far from the only one who refuses to integrate. No wonder: killing good friends and useful assistants with your own hands, albeit symbolically, is still not easy.
The goal of therapy, according to Hillman, is only the creation of harmonious relations of all subpersonalities. Many patients also support his position. The ideologist of such a movement was Truddy Chase, who refused to integrate subpersonalities into a single whole and instead established mutually beneficial cooperation with them. She wrote about her experience in the book When the Rabbit Howls. Today, Truddy is far from the only one who refuses to integrate. No wonder: killing good friends and useful assistants with your own hands, albeit symbolically, is still not easy.
Flora Schreiber
A serious and very detailed book written by a doctor about her own patient who is trying to get along with her sixteen subpersonalities.
Daniel Keyes
Incredible biography of the most famous criminal diagnosed with multiple personality disorder. 24 personalities coexisted in the body of Billy Milligan, including a Yugoslav communist, a lesbian poet, and a three-year-old girl. By the way, the book has a sequel - Milligan's War.
By the way, the book has a sequel - Milligan's War.
Truddy Chase
The most interesting thing about this very positive biographical book is that it was written by Truddy Chase in collaboration with subpersonalities, and by reading it you can see from the inside the teamwork of all Truddy's alters.
Robert Oxnam
Oxnam, president of the Asia Society and well-known public figure, talks in his book about how he tried to disguise his illness with alcoholism, struggled with memory lapses and worked in a rehabilitation center to integrate his 11 sub-personalities.
Elena Foer
Tags
#Psychiatry
#Likbez
#Science
-
72 790
What is a dissociative personality disorder?
Dissociative Identity Disorder is a mental disorder characterized by either having two or more personalities, or a state of disconnection from the outside world, one's identity, and an inability to remember certain daily life events and important personal information. This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
Types of dissociative identity disorder
There are several types of dissociative disorders, which are characterized by different symptoms and manifestations. One of them is dissociative fugue, a disorder in which a person can find himself in a completely unfamiliar place and not remember how he got there. In this case, a person may forget some important information about himself and not even remember his name. At the same time, memory for some information, such as literature, science, and other things, can be preserved. In a state of fugue, a person assumes a different personality and identity with a different character, mannerisms and behavior.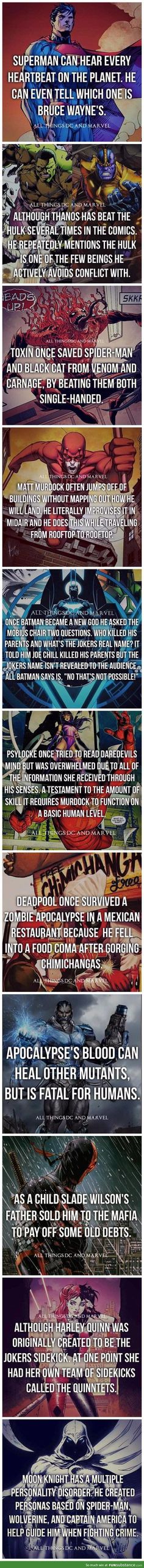 While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue.
While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue.
A person who has a dissociative disorder is actually suffering a lot from their condition.
Another type of dissociative disorder is the presence of several personalities in which a person finds himself in turn or simultaneously. At such moments, he disconnects from himself and stops feeling his own body, and also cannot see himself from the outside. Personalities within a person can have different ages, genders, nationalities, mental abilities, temperaments, and behave in completely different ways. Often these personalities can even have different physiological manifestations. For example, while in one personality, a person can see poorly and wear glasses, and in another, have excellent vision and walk without glasses or lenses (or think that he sees perfectly and does without glasses). Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Manifestations of dissociative identity disorder
This disease affects both children (adolescents) and adults and presents with similar symptoms. However, dissociative disorder with multiple personalities in adolescents is quite rare. In old age, dissociation practically does not develop. When a specialist suspects a person of dissociative identity disorder, he usually asks if it happened that the person suddenly found himself in some place and did not understand how he got there. Also, the patient may suddenly speak in a completely different voice, he may have a different handwriting. For example, a person who has one of his personalities as a child may suddenly begin to write in a child's handwriting. Such phenomenal manifestations can be evoked in a patient suffering from dissociative personality disorder, and in a state of hypnosis. That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis.
See also
Myths about hypnosis
A person who has a dissociative disorder is, in fact, very distressed by his condition. He sees the negative or dismissive attitude of those around him: they look at him strangely, they reject him, no one finds a common language with him, because of him the family can collapse, and so on. At the moment of a dissociative state, a person does not have the opportunity to critically look at himself and his own behavior. That is, in a situation where one of the alternative personalities appears, he is in an inadequate state.
The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence.
Dissociation is one of three conditions in which the patient is exempt from criminal responsibility, along with psychosis and mental retardation. There were cases when people in a dissociative state committed murder and rape. In such situations, even taking into account the severity of the crimes, patients are not sent to prison, but are sent to a psychiatric hospital or, in extreme cases, to a special ward of the psychiatric department of the prison.
Causes of dissociative identity disorder
Scientists have not yet found the genetic causes of dissociative identity disorder. The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence. However, even this theory does not explain all 100% of cases of dissociative states. There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
Diagnosis of dissociative identity disorder
Diagnosis of dissociative identity disorder is made through clinical interviews with several specialists. Sometimes the diagnosis requires not one, but several meetings with psychologists and psychiatrists, so that they have the opportunity to identify different aspects of the disorder, look at the patient's condition from several points of view and assemble a consultation. However, the specialist who identifies this disorder must have a great deal of experience and qualifications, since this disease can often be confused with others.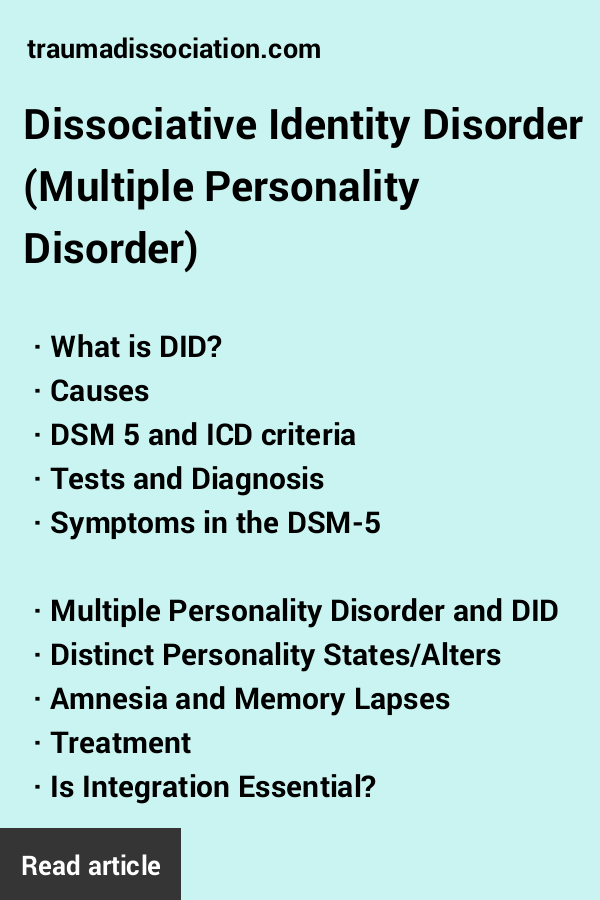 In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this condition.
In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this condition.
Medications do not cure dissociative identity disorder, but only relieve some of the symptoms.
See also
Mental norm and pathology
A separate task for a specialist in the process of diagnosing dissociation in a child is to distinguish diseases from the presence of imaginary friends in a child, which very often appear in perfectly healthy children at a certain age. To do this, a specialist must be highly qualified in the field of developmental psychology and clearly be able to recognize a dissociative disorder not only in adults, but also in children.
Treatment of dissociative identity disorder
The main treatment for dissociative personality disorder is hypnosis.