Winter depression syndrome
Seasonal affective disorder (SAD) - Symptoms and causes
Overview
Seasonal affective disorder (SAD) is a type of depression that's related to changes in seasons — SAD begins and ends at about the same times every year. If you're like most people with SAD, your symptoms start in the fall and continue into the winter months, sapping your energy and making you feel moody. These symptoms often resolve during the spring and summer months. Less often, SAD causes depression in the spring or early summer and resolves during the fall or winter months.
Treatment for SAD may include light therapy (phototherapy), psychotherapy and medications.
Don't brush off that yearly feeling as simply a case of the "winter blues" or a seasonal funk that you have to tough out on your own. Take steps to keep your mood and motivation steady throughout the year.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
In most cases, seasonal affective disorder symptoms appear during late fall or early winter and go away during the sunnier days of spring and summer. Less commonly, people with the opposite pattern have symptoms that begin in spring or summer. In either case, symptoms may start out mild and become more severe as the season progresses.
Signs and symptoms of SAD may include:
- Feeling listless, sad or down most of the day, nearly every day
- Losing interest in activities you once enjoyed
- Having low energy and feeling sluggish
- Having problems with sleeping too much
- Experiencing carbohydrate cravings, overeating and weight gain
- Having difficulty concentrating
- Feeling hopeless, worthless or guilty
- Having thoughts of not wanting to live
Fall and winter SAD
Symptoms specific to winter-onset SAD, sometimes called winter depression, may include:
- Oversleeping
- Appetite changes, especially a craving for foods high in carbohydrates
- Weight gain
- Tiredness or low energy
Spring and summer SAD
Symptoms specific to summer-onset seasonal affective disorder, sometimes called summer depression, may include:
- Trouble sleeping (insomnia)
- Poor appetite
- Weight loss
- Agitation or anxiety
- Increased irritability
Seasonal changes and bipolar disorder
People who have bipolar disorder are at increased risk of seasonal affective disorder. In some people with bipolar disorder, episodes of mania may be linked to a specific season. For example, spring and summer can bring on symptoms of mania or a less intense form of mania (hypomania), anxiety, agitation and irritability. They may also experience depression during the fall and winter months.
In some people with bipolar disorder, episodes of mania may be linked to a specific season. For example, spring and summer can bring on symptoms of mania or a less intense form of mania (hypomania), anxiety, agitation and irritability. They may also experience depression during the fall and winter months.
When to see a doctor
It's normal to have some days when you feel down. But if you feel down for days at a time and you can't get motivated to do activities you normally enjoy, see your health care provider. This is especially important if your sleep patterns and appetite have changed, you turn to alcohol for comfort or relaxation, or you feel hopeless or think about suicide.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The specific cause of seasonal affective disorder remains unknown. Some factors that may come into play include:
- Your biological clock (circadian rhythm). The reduced level of sunlight in fall and winter may cause winter-onset SAD. This decrease in sunlight may disrupt your body's internal clock and lead to feelings of depression.
- Serotonin levels. A drop in serotonin, a brain chemical (neurotransmitter) that affects mood, might play a role in SAD. Reduced sunlight can cause a drop in serotonin that may trigger depression.
- Melatonin levels. The change in season can disrupt the balance of the body's level of melatonin, which plays a role in sleep patterns and mood.
Risk factors
Seasonal affective disorder is diagnosed more often in women than in men. And SAD occurs more frequently in younger adults than in older adults.
Factors that may increase your risk of seasonal affective disorder include:
- Family history. People with SAD may be more likely to have blood relatives with SAD or another form of depression.

- Having major depression or bipolar disorder. Symptoms of depression may worsen seasonally if you have one of these conditions.
- Living far from the equator. SAD appears to be more common among people who live far north or south of the equator. This may be due to decreased sunlight during the winter and longer days during the summer months.
- Low level of vitamin D. Some vitamin D is produced in the skin when it's exposed to sunlight. Vitamin D can help to boost serotonin activity. Less sunlight and not getting enough vitamin D from foods and other sources may result in low levels of vitamin D in the body.
Complications
Take signs and symptoms of seasonal affective disorder seriously. As with other types of depression, SAD can get worse and lead to problems if it's not treated. These can include:
- Social withdrawal
- School or work problems
- Substance abuse
- Other mental health disorders such as anxiety or eating disorders
- Suicidal thoughts or behavior
Prevention
There's no known way to prevent the development of seasonal affective disorder. However, if you take steps early on to manage symptoms, you may be able to prevent them from getting worse over time. You may be able to head off serious changes in mood, appetite and energy levels, as you can predict the time of the year in which these symptoms may start. Treatment can help prevent complications, especially if SAD is diagnosed and treated before symptoms get bad.
However, if you take steps early on to manage symptoms, you may be able to prevent them from getting worse over time. You may be able to head off serious changes in mood, appetite and energy levels, as you can predict the time of the year in which these symptoms may start. Treatment can help prevent complications, especially if SAD is diagnosed and treated before symptoms get bad.
Some people find it helpful to begin treatment before symptoms would normally start in the fall or winter, and then continue treatment past the time symptoms would normally go away. Other people need continuous treatment to prevent symptoms from returning.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
NIMH » Seasonal Affective Disorder
What is seasonal affective disorder?
Many people go through short periods of time where they feel sad or not like their usual selves. Sometimes, these mood changes begin and end when the seasons change. People may start to feel “down” when the days get shorter in the fall and winter (also called “winter blues”) and begin to feel better in the spring, with longer daylight hours.
Sometimes, these mood changes begin and end when the seasons change. People may start to feel “down” when the days get shorter in the fall and winter (also called “winter blues”) and begin to feel better in the spring, with longer daylight hours.
In some cases, these mood changes are more serious and can affect how a person feels, thinks, and handles daily activities. If you have noticed significant changes in your mood and behavior whenever the seasons change, you may be suffering from seasonal affective disorder (SAD), a type of depression.
In most cases, SAD symptoms start in the late fall or early winter and go away during the spring and summer; this is known as winter-pattern SAD or winter depression. Some people may experience depressive episodes during the spring and summer months; this is called summer-pattern SAD or summer depression and is less common.
What are the signs and symptoms of SAD?
SAD is not considered a separate disorder but is a type of depression characterized by its recurrent seasonal pattern, with symptoms lasting about 4 to 5 months per year. Therefore, the signs and symptoms of SAD include those associated with major depression, and some specific symptoms that differ for winter-pattern and summer-pattern SAD. Not every person with SAD will experience all of the symptoms listed below.
Therefore, the signs and symptoms of SAD include those associated with major depression, and some specific symptoms that differ for winter-pattern and summer-pattern SAD. Not every person with SAD will experience all of the symptoms listed below.
Symptoms of major depression may include:
- Feeling depressed most of the day, nearly every day
- Losing interest in activities you once enjoyed
- Experiencing changes in appetite or weight
- Having problems with sleep
- Feeling sluggish or agitated
- Having low energy
- Feeling hopeless or worthless
- Having difficulty concentrating
- Having frequent thoughts of death or suicide
For winter-pattern SAD, additional specific symptoms may include:
- Oversleeping (hypersomnia)
- Overeating, particularly with a craving for carbohydrates
- Weight gain
- Social withdrawal (feeling like “hibernating”)
Specific symptoms for summer-pattern SAD may include:
- Trouble sleeping (insomnia)
- Poor appetite, leading to weight loss
- Restlessness and agitation
- Anxiety
- Episodes of violent behavior
Get Immediate Help
If you or someone you know is in immediate distress or is thinking about hurting themselves, call the National Suicide Prevention Lifeline toll-free at 1-800-273-TALK (8255). You also can text the Crisis Text Line (HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website.
You also can text the Crisis Text Line (HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website.
How is SAD diagnosed?
If you think you may be suffering from SAD, talk to your health care provider or a mental health specialist about your concerns. They may have you fill out specific questionnaires to determine if your symptoms meet the criteria for SAD.
To be diagnosed with SAD, a person must meet the following criteria:
- They must have symptoms of major depression or the more specific symptoms listed above.
- The depressive episodes must occur during specific seasons (i.e., only during the winter months or the summer months) for at least 2 consecutive years. However, not all people with SAD do experience symptoms every year.
- The episodes must be much more frequent than other depressive episodes that the person may have had at other times of the year during their lifetime.
Who develops SAD?
Millions of American adults may suffer from SAD, although many may not know they have the condition. SAD occurs much more often in women than in men, and it is more common in those living farther north, where there are shorter daylight hours in the winter. For example, people living in Alaska or New England may be more likely to develop SAD than people living in Florida. In most cases, SAD begins in young adulthood.
SAD is more common in people with major depressive disorder or bipolar disorder, especially bipolar II disorder, which is associated with recurrent depressive and hypomanic episodes (less severe than the full-blown manic episodes typical of bipolar I disorder). Additionally, people with SAD tend to have other mental disorders, such as attention-deficit/hyperactivity disorder, an eating disorder, an anxiety disorder, or panic disorder. Learn more about these disorders by visiting the NIMH Mental Health Information page.
SAD sometimes runs in families. SAD is more common in people who have relatives with other mental illnesses, such as major depression or schizophrenia.
SAD is more common in people who have relatives with other mental illnesses, such as major depression or schizophrenia.
What causes SAD?
Scientists do not fully understand what causes SAD. Research indicates that people with SAD may have reduced activity of the brain chemical (neurotransmitter) serotonin, which helps regulate mood. Research also suggests that sunlight controls the levels of molecules that help maintain normal serotonin levels, but in people with SAD, this regulation does not function properly, resulting in decreased serotonin levels in the winter.
Other findings suggest that people with SAD produce too much melatonin—a hormone that is central for maintaining the normal sleep-wake cycle. Overproduction of melatonin can increase sleepiness.
Both serotonin and melatonin help maintain the body’s daily rhythm that is tied to the seasonal night-day cycle. In people with SAD, the changes in serotonin and melatonin levels disrupt the normal daily rhythms. As a result, they can no longer adjust to the seasonal changes in day length, leading to sleep, mood, and behavior changes.
As a result, they can no longer adjust to the seasonal changes in day length, leading to sleep, mood, and behavior changes.
Deficits in vitamin D may exacerbate these problems because vitamin D is believed to promote serotonin activity. In addition to vitamin D consumed with diet, the body produces vitamin D when exposed to sunlight on the skin. With less daylight in the winter, people with SAD may have lower vitamin D levels, which may further hinder serotonin activity.
Negative thoughts and feelings about the winter and its associated limitations and stresses are common among people with SAD (as well as others). It is unclear whether these are "causes" or "effects" of the mood disorder, but they can be a useful focus of treatment.
How is SAD treated?
Treatments are available that can help many people with SAD. They fall into four main categories that may be used alone or in combination:
- Light therapy
- Psychotherapy
- Antidepressant medications
- Vitamin D
Talk to your health care provider about which treatment, or combination of treatments, is best for you. For tips for talking with your health care provider, refer to the NIMH fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
For tips for talking with your health care provider, refer to the NIMH fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
Light Therapy
Since the 1980s, light therapy has been a mainstay for the treatment of SAD. It aims to expose people with SAD to a bright light every day to make up for the diminished natural sunshine in the darker months.
For this treatment, the person sits in front of a very bright light box (10,000 lux) every day for about 30 to 45 minutes, usually first thing in the morning, from fall to spring. The light boxes, which are about 20 times brighter than ordinary indoor light, filter out the potentially damaging UV light, making this a safe treatment for most. However, people with certain eye diseases or people taking certain medications that increase sensitivity to sunlight may need to use alternative treatments or use light therapy under medical supervision.
Psychotherapy or “Talk Therapy”
Cognitive behavioral therapy (CBT) is a type of talk therapy aimed at helping people learn how to cope with difficult situations; CBT also has been adapted for people with SAD (CBT-SAD). It is typically conducted in two weekly group sessions for 6 weeks and focuses on replacing negative thoughts related to the winter season (e.g., about the darkness of winter) with more positive thoughts. CBT-SAD also uses a process called behavioral activation, which helps individuals identify and schedule pleasant, engaging indoor or outdoor activities to combat the loss of interest they typically experience in the winter.
It is typically conducted in two weekly group sessions for 6 weeks and focuses on replacing negative thoughts related to the winter season (e.g., about the darkness of winter) with more positive thoughts. CBT-SAD also uses a process called behavioral activation, which helps individuals identify and schedule pleasant, engaging indoor or outdoor activities to combat the loss of interest they typically experience in the winter.
When researchers directly compared CBT with light therapy, both treatments were equally effective in improving SAD symptoms. Some symptoms seemed to get better a little faster with light therapy than with CBT. However, a long-term study that followed SAD patients for two winters found that the positive effects of CBT seemed to last longer over time.
Medications
Because SAD, like other types of depression, is associated with disturbances in serotonin activity, antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are also used to treat SAD when symptoms occur. These agents can significantly enhance patients' moods. Commonly used SSRIs include fluoxetine, citalopram, sertraline, paroxetine, and escitalopram.
These agents can significantly enhance patients' moods. Commonly used SSRIs include fluoxetine, citalopram, sertraline, paroxetine, and escitalopram.
The U.S. Food and Drug Administration (FDA) also has approved another type of antidepressant, bupropion, in an extended-release form, that can prevent recurrence of seasonal major depressive episodes when taken daily from the fall until the following early spring.
All medications can have side effects. Talk to your doctor about the possible risk of using these medications for your condition. You may need to try several different antidepressant medications before finding one that improves your symptoms without causing problematic side effects. For basic information about SSRIs, bupropion, and other mental health medications, visit the NIMH Mental Health Medications page. Also, visit the FDA website for the most up-to-date information on medications, side effects, and warnings.
Vitamin D
Because many people with SAD often have vitamin D deficiency, nutritional supplements of vitamin D may help improve their symptoms. However, studies testing whether vitamin D is effective in SAD treatment have produced mixed findings, with some results indicating that it is as effective as light therapy but others detecting no effect.
However, studies testing whether vitamin D is effective in SAD treatment have produced mixed findings, with some results indicating that it is as effective as light therapy but others detecting no effect.
Can SAD be prevented?
Because the timing of the onset of winter pattern-SAD is so predictable, people with a history of SAD might benefit from starting the treatments mentioned above before the fall to help prevent or reduce the depression. To date, very few studies have investigated this question, and existing studies have found no convincing evidence that starting light therapy or psychotherapy ahead of time could prevent the onset of depression. Only preventive treatment with the antidepressant bupropion prevented SAD in study participants, but it also had a higher risk of side effects. Therefore, people with SAD should discuss with their health care providers if they want to initiate treatment early to prevent depressive episodes.
Are there clinical trials studying SAD?
NIMH supports a wide range of research, including clinical trials that look at new ways to prevent, detect, or treat diseases and conditions—including SAD. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct clinical trials with patients and healthy volunteers. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information about clinical research and how to find clinical trials being conducted around the country, visit the NIMH Clinical Trials page.
Reprints
This publication is in the public domain and may be reproduced or copied without permission from NIMH. Citation of NIMH as a source is appreciated. To learn more about using NIMH publications, refer to our reprint guidelines.
For More Information
MedlinePlus (En español)
ClinicalTrials. gov (En español)
gov (En español)
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 20-MH-8138
What is winter depression and how to deal with it
In winter, people often experience a bad mood, apathy, drowsiness and increased appetite - these are manifestations of seasonal affective disorder, or winter depression. "Gazeta.Ru" understood what signs winter depression has and how to deal with it.
In winter, many people lose their vitality, mood, desire to engage in vigorous activity, and, conversely, the need for food and sleep increases. I want to hibernate like a bear and not wake up until spring. These are manifestations of winter depression, which experts consider as a kind of seasonal depression. Often this condition does not begin in winter, but in late autumn, when daylight hours are greatly reduced.
"Magnetic storm? And I thought it was old age!
Even a healthy body can react negatively to weather disasters. About what modern science knows...
About what modern science knows...
November 19 11:13
Scientifically, experts call it Seasonal Affective Disorder (SAD).
Scientists identify seven symptoms of this disorder. One of them is emotional disturbances: low mood, inability to experience positive emotions, apathy, increased irritability, decreased self-esteem. The other is cognitive impairment: difficulty concentrating, memory loss, decreased intellectual activity.
Also criteria are fatigue, increased fatigue and drowsiness, increased need for sleep, in which a person does not get enough sleep, wakes up with difficulty in the morning.
The remaining three criteria are an increased need for food, cravings for flour and sweets, which leads to a set of extra pounds; reduced immunity, which increases the frequency of colds and other diseases; avoidance of social contacts, reduced need for communication, desire to stay at home. In winter, in severe frosts, it can also rise weather sensitivity to which people are exposed in any season.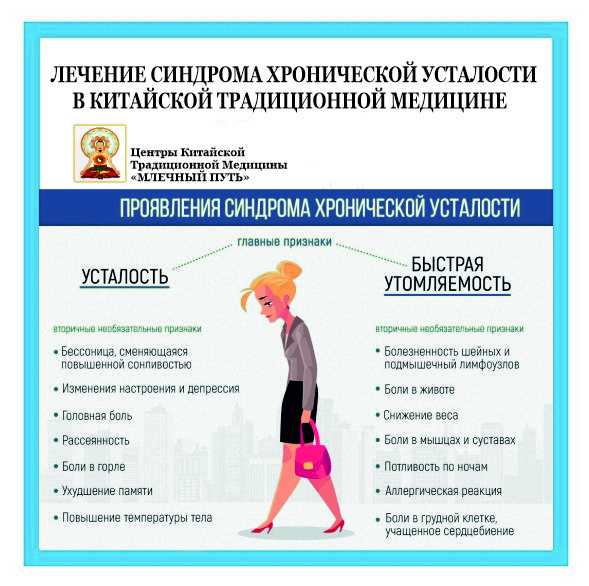
However, according to the specialists of the Scientific Center for Mental Health of the Russian Academy of Medical Sciences, investigating this problem under the guidance of Dr. Vladimir Medvedev , to make a diagnosis of “seasonal depression”, it is necessary that depressive attacks recur for three years in the same season and exactly same took place with the onset of the next season.
If you are cold - check your thyroid gland
Scientists have found out why people with impaired thyroid function are more sensitive to temperature...
September 17 2:16 pm
Women are much more likely to suffer from this condition than men, at least in the sample of subjects suffering from SAD, which the researchers studied, there were 76 women and 21 men. The symptom complex observed in most included "increased appetite with cravings for sweet and other carbohydrate-rich foods, weight gain, increased sleep duration, and daytime sleepiness with no sense of rest.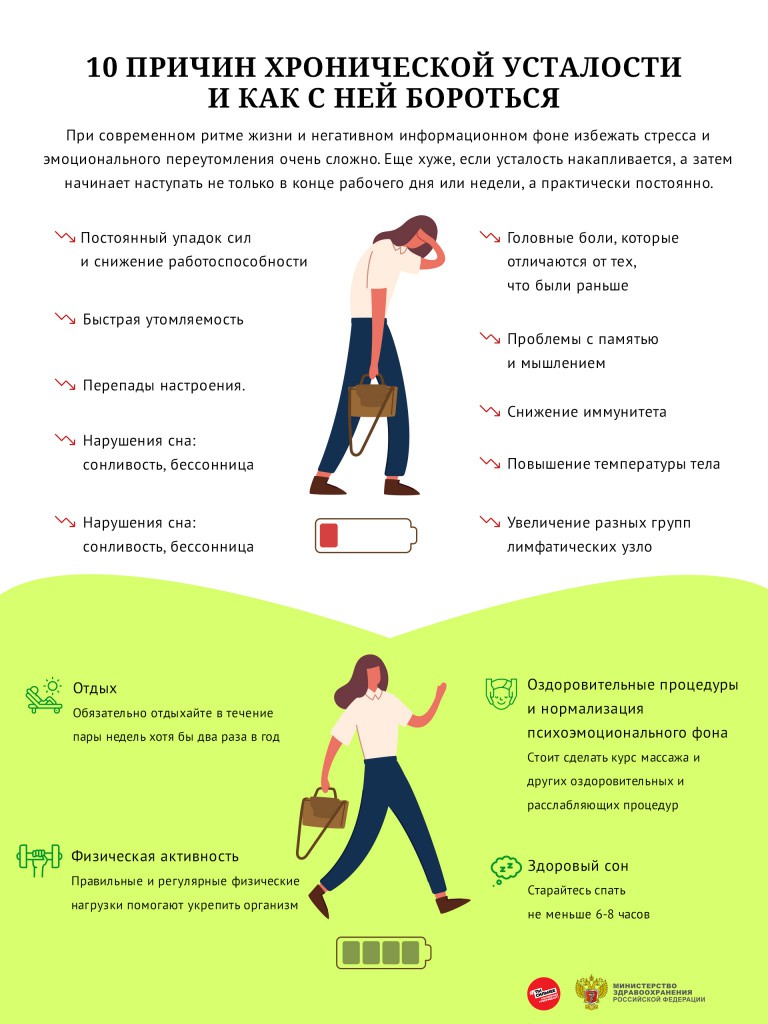 " At the same time, there were also atypical forms of SAD, in which appetite and sleep were reduced, and body weight fell. Moreover, these atypical forms were the most severe forms of depression.
" At the same time, there were also atypical forms of SAD, in which appetite and sleep were reduced, and body weight fell. Moreover, these atypical forms were the most severe forms of depression.
Experts believe that the main causes of winter depression are hormonal changes under the influence of reduced daylight hours.
Because of this, the circadian, circadian, rhythms of the body disagree with external conditions. In winter, the secretion of melatonin (a hormone that is produced at night) is disrupted and less serotonin is produced (a neurotransmitter that greatly affects our emotions and mood).
It is believed that up to 10% of people in the population are affected by seasonal depression, and it usually appears after 18 years of age.
Women suffer from it more often than men due to increased emotionality.
According to specialists from the Belarusian State Medical University, who studied this problem among medical students, SAD was observed in 16% of girls and another 23% had a mild (subsyndromal) form of its manifestation.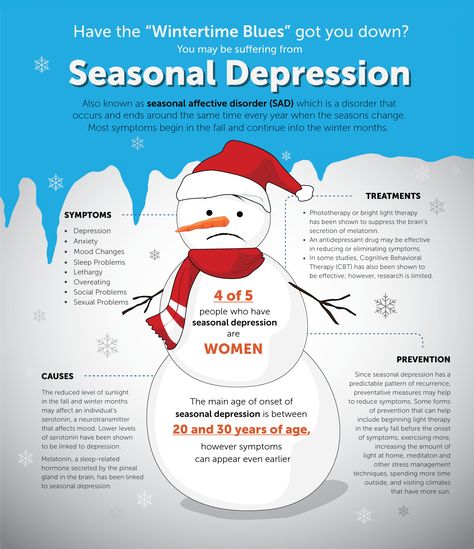 Among male students, only 6% had a mild form of SAD. Interestingly, winter depression was more pronounced in students living in a hostel than in students living at home.
Among male students, only 6% had a mild form of SAD. Interestingly, winter depression was more pronounced in students living in a hostel than in students living at home.
Untreated depression is a life lost
Depressive disorders are one of the main causes of disability and a factor that increases the risk of developing ...
07 November 11:46
The influence of personality type on predisposition to seasonal mood swings was recently studied by Polish specialists from the Institute of Applied Psychology in Krakow. They argue that winter depression is more typical for women. This state is facilitated by a greater neuroticism of the individual, as well as a quality that psychologists call harm avoidance. This refers to the type of person who avoids dangers and unpleasant situations and prefers to behave passively in response to a threat. More often, less socially active individuals, introverts, suffer from winter depression.
The most important question is how to deal with winter depression?
According to the majority of experts, Russian and foreign, the best way to treat her is light.
Light therapy can be carried out in clinics, in special boxes in which patients are irradiated with high-intensity visible light.
But you can fight winter depression on your own. To do this, experts give some advice.
Spend more time outside, even on cloudy days. Even when there is no sun, the light level outside is higher than indoors.
Eat a balanced diet. Eat more complex carbohydrates and cut down on sugary foods, and remember to take vitamins, especially C, A, and D.
Red-colored vegetables and fruits (dried apricots, red peppers, beetroots) are useful, containing nutrients that help overcome depression . Dark chocolate can help boost serotonin levels.
Find time for physical activity. Exercise for at least 30 minutes three times a week, but more is better.
Lead an active social life , keep in touch with people, diversify daily activities.
Doctors strongly do not recommend alcohol as a means of combating the autumn-winter melancholy.
This will bring only a temporary improvement in mood, but not a lasting effect. And long-term abuse will result in serious health problems.
Seasonal affective disorder - what to look out for
Also known as SAD, this is a seasonal affective disorder often seen during the winter months that mimics symptoms of depression.
What is seasonal affective disorder
Seasonal affective disorder, or "SAD", is a type of depression that occurs when the seasons change. Seasonal affective disorder may be more commonly known as seasonal depression, winter depression, or the winter blues. Seasonal affective disorder causes significant changes in mood and behavior.
SAD is most common in winter when daylight hours are getting shorter. Seasonal affective disorder rarely affects people during the spring and summer months. In winter and summer seasonal affective disorder, symptoms come and go at about the same time each year. Symptoms usually begin as mild at the beginning of the season change, such as autumn, and then become most severe in the middle of the season, such as winter.
What are the symptoms of SAD?
In both summer and winter seasonal affective disorder, the symptoms follow a seasonal pattern, so they appear at the beginning of the season and subside at the end of it.
With winter seasonal affective disorder (the most common SAD), people often begin to feel low and lack energy in late fall or early winter. People may begin to sleep more and experience more fatigue during the day. Other symptoms include sadness and crying more than usual, feelings of hopelessness, and suicidal thoughts. People may feel less interested in activities they used to enjoy and may begin to drift away from friends and family. Other symptoms are weight gain, overeating, especially starchy and sugary foods, and carbohydrate cravings. The symptoms of winter SAD often begin to disappear in the spring or early summer.
People with seasonal affective disorder during the summer months may have different symptoms than those with seasonal affective disorder during the winter months. These symptoms may include increased anxiety or irritability, irritability, sleep problems and insomnia, and weight loss.
These symptoms may include increased anxiety or irritability, irritability, sleep problems and insomnia, and weight loss.
What are the causes of seasonal affective disorder?
For winter seasonal affective disorder, the most common cause is reduced sunlight due to shorter daylight hours. Decreased exposure to sunlight can cause chemical changes in the brain that can lead to symptoms of SAD. Decreased exposure to sunlight can affect the activity of serotonin, leading to symptoms of depression. Serotonin is a brain chemical that affects mood, digestion, sleep, bone health, and other bodily functions. Low serotonin has been linked to mood disorders and mental illness, including depression and anxiety, as well as sleep and digestive problems.
A shorter day can also cause disturbances in sleep patterns (circadian rhythm) and changes in the levels of melatonin your body produces. An overproduction of melatonin due to reduced sunlight can cause increased drowsiness and drowsiness.
In summer SAD, symptoms may begin in early spring or summer. During the summer months, the body may not produce enough melatonin. Decreased melatonin levels can cause the symptoms of insomnia, restlessness, and irritability that are seen with summer seasonal affective disorder. Other symptoms include high stress levels and decreased appetite.
Risk factors for seasonal affective disorder
Having another affective disorder, such as major depressive disorder or bipolar disorder, may increase the risk of seasonal affective disorder. Also, having family members with seasonal affective disorder or other affective disorders can make you more susceptible to seasonal affective disorder.
Living farther from the equator may also play a role, as there are more dramatic changes between seasons and daylight hours. Daylight hours become much shorter in winter and much longer in summer. Also, living further away from the equator means there is less sunshine during the winter months.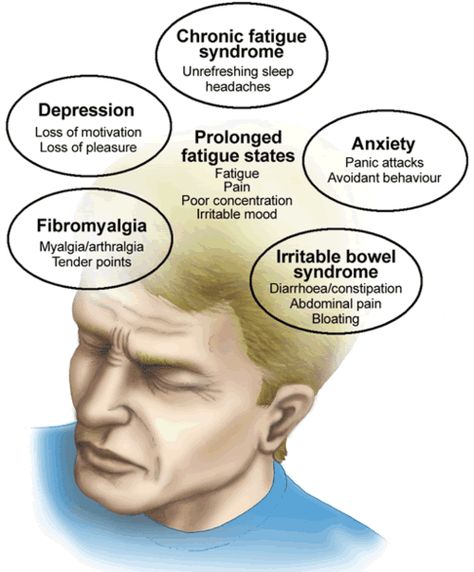 Finally, living in a cloudy climate with limited exposure to direct sunlight can also increase the likelihood of seasonal affective disorder.
Finally, living in a cloudy climate with limited exposure to direct sunlight can also increase the likelihood of seasonal affective disorder.
What are the treatments for seasonal affective disorder?
One treatment option for seasonal affective disorder in the winter is bright light therapy. Light therapy involves daily exposure to bright artificial light. Special lamps and equipment have been developed for light therapy, such as the light therapy box.
It is also beneficial to get as much natural light as possible during the winter months. Sunlight helps our bodies produce vitamin D. Therefore, people living in climates with limited sun exposure may benefit from taking vitamin D supplements.
A balanced diet and regular exercise can also help manage symptoms of seasonal affective disorder. To maintain a normal sleep cycle, it is important to ensure that you get enough sleep.
Other treatments may include yoga, meditation, or mindfulness exercises.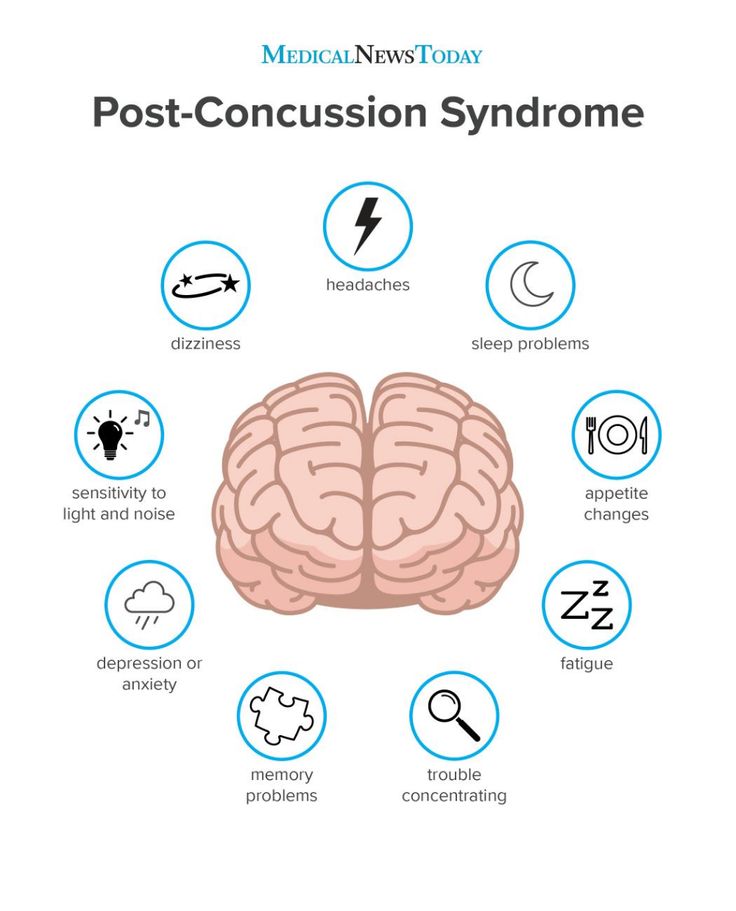 Meditation and mindfulness exercises can help you recognize and understand your feelings and emotions. Meditation can also help increase serotonin levels. Yoga will help you connect your mind and body and recognize the changes that come with the change of seasons. Yoga and meditation can also help manage stress and become a form of physical activity that can help manage SAD symptoms.
Meditation and mindfulness exercises can help you recognize and understand your feelings and emotions. Meditation can also help increase serotonin levels. Yoga will help you connect your mind and body and recognize the changes that come with the change of seasons. Yoga and meditation can also help manage stress and become a form of physical activity that can help manage SAD symptoms.
Psychotherapy, a form of talking therapy, can also help people with seasonal affective disorder. Finally, some people may find that antidepressant medications, such as selective serotonin reuptake inhibitors, can help with seasonal affective disorder.
Frequently Asked Questions about Seasonal Affective Disorder
How do I know if I have SAD?
- Practicing mindfulness and controlling your moods and emotions can help you understand your moods and feelings and how they change throughout the year.
- Notice if you experience significant mood swings at certain times of the year.