Motor disorders dsm 5
Motor Disorders | Abnormal Psychology
Learning Objectives
- Describe the characteristics and etiology of motor disorders
Motor Disorders
The DSM-5 motor disorders include developmental coordination disorder; stereotypic movement disorder; and the tic disorders of Tourette’s Disorder, persistent (chronic) motor or vocal tic disorder, and provisional tic disorder.
Motor disorders are malfunctions of the nervous system that cause involuntary or uncontrollable movements or actions of the body. These disorders can cause lack of intended movement or an excess of involuntary movement. Symptoms of motor disorders include tremors, jerks, twitches, spasms, contractions, or gait problems.
Causes of Motor Disorders
Pathological changes of certain areas of the brain are the main causes of most motor disorders. Causes of motor disorders by genetic mutation usually affect the cerebellum. The way humans move requires many parts of the brain to work together to perform a complex process. The brain must send signals to the muscles instructing them to perform a certain action. There are constant signals being sent to and from the brain and the muscles that regulate the details of the movement such as speed and direction, so when a certain part of the brain malfunctions, the signals can be incorrect or uncontrollable causing involuntary or uncontrollable actions or movements.
Developmental Coordination Disorder
Figure 1. Some possible signs of dyspraxia.
Developmental coordination disorder (DCD), also known as developmental motor coordination disorder, developmental dyspraxia, or simply dyspraxia, is a chronic neurological disorder beginning in childhood. It is also known to affect planning of movements and coordination as a result of brain messages not being accurately transmitted to the body. Impairments in skilled motor movements per a child’s chronological age interfere with activities of daily living.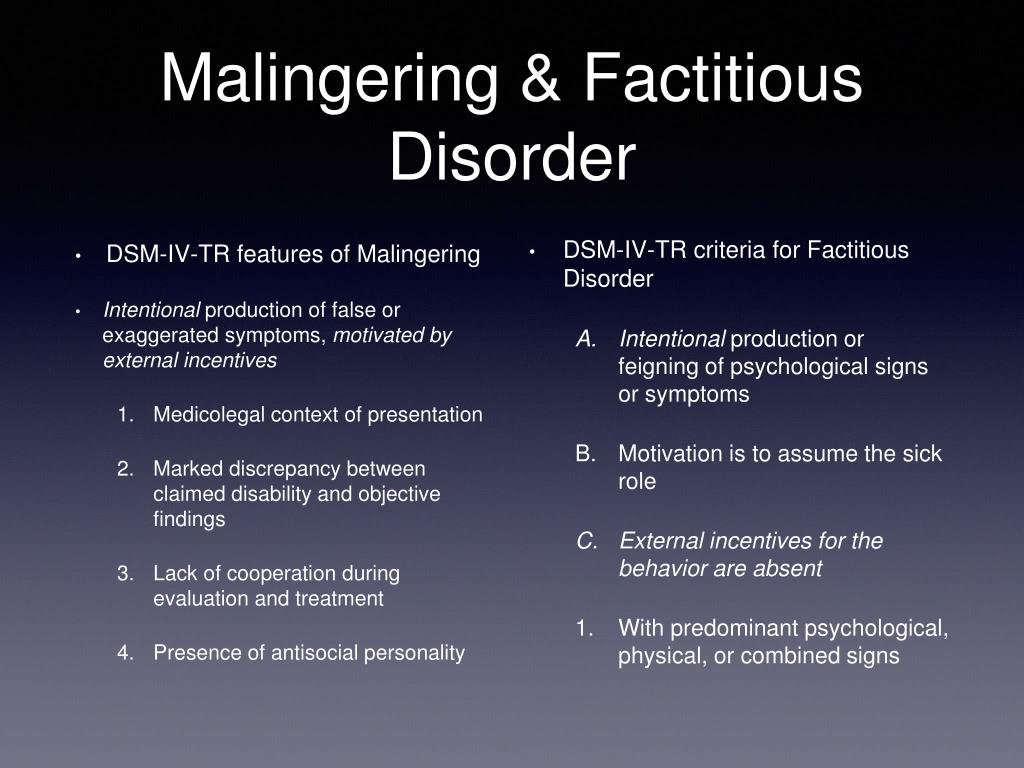 A diagnosis of developmental coordination disorder (DCD) is then reached only in the absence of other neurological impairments like cerebral palsy, multiple sclerosis, or Parkinson’s disease.
A diagnosis of developmental coordination disorder (DCD) is then reached only in the absence of other neurological impairments like cerebral palsy, multiple sclerosis, or Parkinson’s disease.
The DSM-5 criteria are as follows:
- Motor coordination will be greatly reduced, although the intelligence of the child is normal for the age.
- The difficulties the child experiences with motor coordination or planning interfere with the child’s daily life.
- The difficulties with coordination are not due to any other medical condition
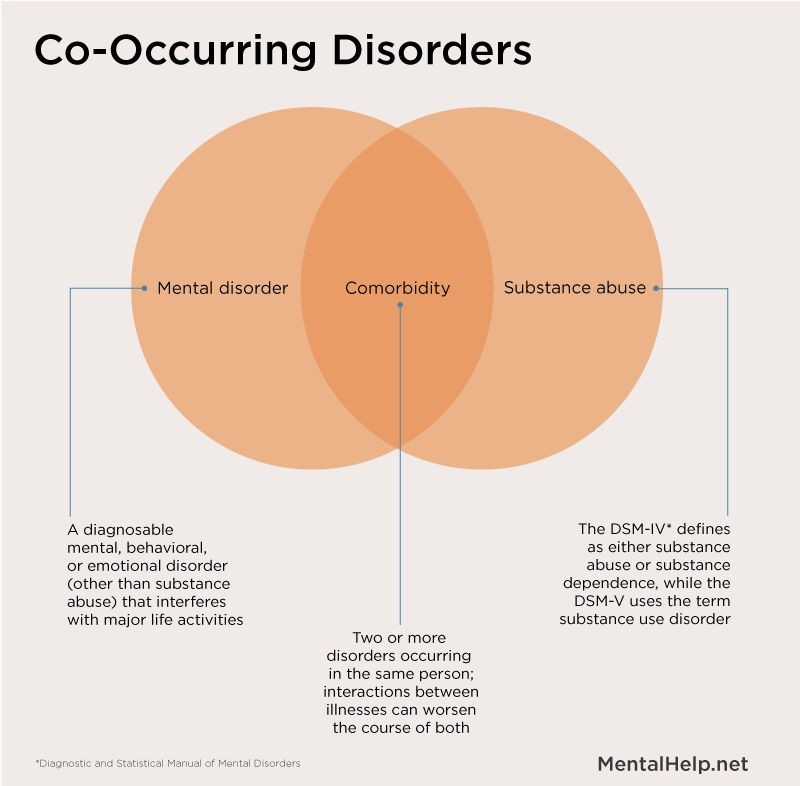
- If the child also experiences comorbidities such as intellectual or other developmental disorder; motor coordination is still disproportionally affected.
Management
There is no cure for the condition. Instead, it is managed through therapy. Physical therapy or occupational therapy can help those living with the condition.
Some people with the condition find it helpful to find alternative ways of carrying out tasks or organizing themselves, such as typing on a laptop instead of writing by hand or using diaries and calendars to keep organized.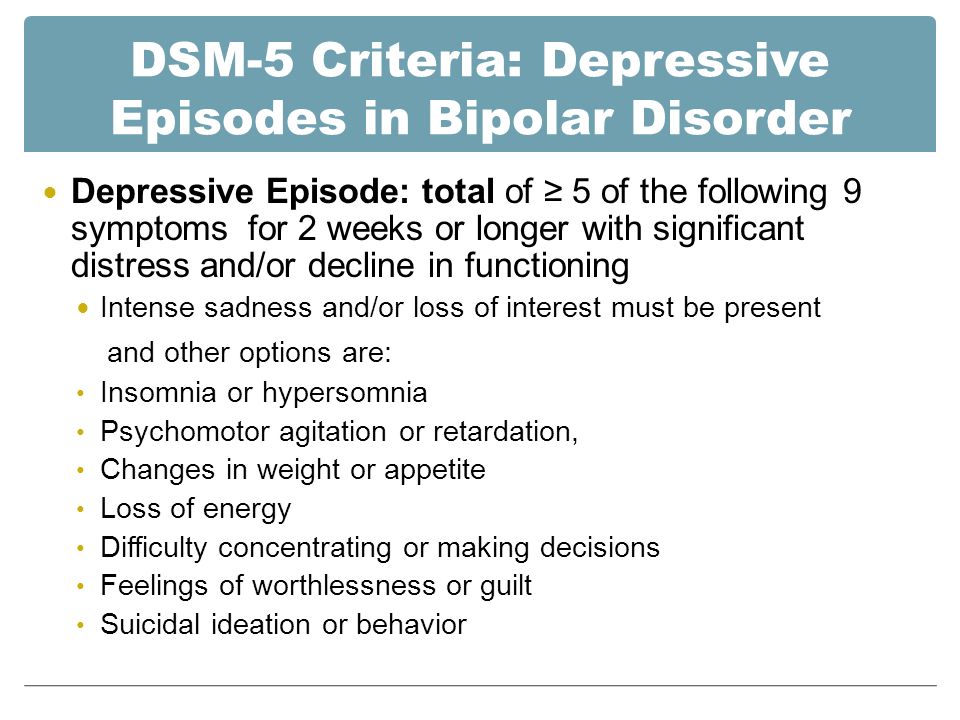 A review completed in 2017 by Cochrane of task-oriented interventions for developmental coordination disorder (DCD) resulted in inconsistent findings and a call for further research and randomized controlled trials.
A review completed in 2017 by Cochrane of task-oriented interventions for developmental coordination disorder (DCD) resulted in inconsistent findings and a call for further research and randomized controlled trials.
Epidemiology
DCD is a lifelong neurological condition that is more common in males than in females, with a ratio of approximately four males to every female. The exact proportion of people with the disorder is unknown since the disorder can be difficult to detect due to a lack of specific laboratory tests, thus making diagnosis of the condition one of elimination of all other possible causes/diseases. Approximatelyfive to 6% of children are affected by this condition.
Watch it
Watch this video to get a better understanding of DCD and measures taken to learn more about the disorder:
You can view the transcript for “Understanding DCD (Developmental Coordination Disorder)” here (opens in new window).
Stereotypic Movement Disorder
Stereotyped movements are common in infants and young children; if the child is not distressed by movements and daily activities are not impaired, diagnosis is not warranted. When stereotyped behaviors cause significant impairment in functioning, an evaluation for stereotypic movement disorder is needed. There are no specific tests for diagnosing this disorder, although some tests may be ordered to rule out other conditions. Stereotyped movement disorder (SMD) may occur with Lesch–Nyhan syndrome, intellectual development disorder (intellectual disability), and fetal alcohol exposure or as a result of amphetamine intoxication.
When stereotyped behaviors cause significant impairment in functioning, an evaluation for stereotypic movement disorder is needed. There are no specific tests for diagnosing this disorder, although some tests may be ordered to rule out other conditions. Stereotyped movement disorder (SMD) may occur with Lesch–Nyhan syndrome, intellectual development disorder (intellectual disability), and fetal alcohol exposure or as a result of amphetamine intoxication.
When diagnosing stereotypic movement disorder, DSM-5 calls for specification of
- with or without self-injurious behavior,
- association with another known medical condition or environmental factor, and
- severity (mild, moderate, or severe).
Common repetitive movements of stereotyped movement disorder (SMD) include head banging, arm-waving, hand-shaking, rocking and rhythmic movements, self-biting, self-hitting, and skin-picking; other stereotypies are thumb-sucking, nail-biting, trichotillomania, bruxism, and abnormal running or skipping.
Epidemiology
Stereotyped movement disorder (SMD) occurs in about 3%-4% of children.[1] Stereotypies often represent a physiological and transient finding, up to 60% of neurologically typical children showing some stereotypic movements or behaviors between two and five years. Therefore, SMD are classified as primary, indicating their presence in an otherwise typically developing child, or secondary, if another of the above-mentioned neuropsychiatric disorders is present.[2] Although not necessary for the diagnosis, individuals with intellectual development disorder (intellectual disorder) are at higher risk for SMD. It is more common in boys and can occur at any age.
Management
Though we have yet to find a cure for these disorders, some studies have looked at the effectiveness of medication therapy but thus far (based on parent reports of medication trials) there haven’t been any medication therapy identified to be effective in treating symptoms.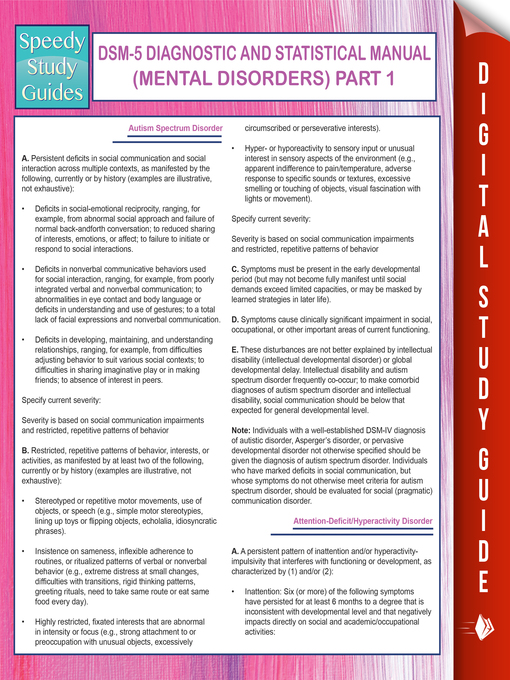 However, behavioral therapy appears to be beneficial for those with primary SMD. Researchers found that therapy that focuses on a mix of awareness and reinforcement of other behaviors helped reduce unwanted movement. Additionally, another study looked at the effectiveness of home-based, parent-administered behavioral therapy and this assessment showed significant improvement compared to the baseline.[3]
However, behavioral therapy appears to be beneficial for those with primary SMD. Researchers found that therapy that focuses on a mix of awareness and reinforcement of other behaviors helped reduce unwanted movement. Additionally, another study looked at the effectiveness of home-based, parent-administered behavioral therapy and this assessment showed significant improvement compared to the baseline.[3]
Tic Disorders
Tourette Syndrome (TS or Tourette’s)
To be diagnosed with Tourette syndrome (TS or Tourette’s), a person must have
- two or more motor tics (for example, blinking or shrugging the shoulders) and at least one vocal tic (for example, humming, clearing the throat, or yelling out a word or phrase), although they might not always happen at the same time.
- had tics for at least a year. The tics can occur many times a day (usually in bouts) nearly every day or off and on.
- tics that begin before age 18 years.
- symptoms that are not due to taking medicine or other drugs or due to having another medical condition (for example, seizures, Huntington disease, or postviral encephalitis).
Figure 2. Coughing is a common tic.
Tourette syndrome or Tourette’s syndrome (TS or Tourette’s) is a common neurodevelopmental disorder that begins in childhood or adolescence. It is characterized by multiple movement (motor) tics and at least one vocal (phonic) tic. Common tics are blinking, coughing, throat clearing, sniffing, and facial movements. These are typically preceded by an unwanted urge or sensation in the affected muscles, can sometimes be suppressed temporarily, and characteristically change in location, strength, and frequency. Tourette’s is at the more severe end of a spectrum of tic disorders. The tics often go unnoticed by casual observers.
Tourette’s was once regarded as a rare and bizarre syndrome and has popularly been associated with coprolalia (the utterance of obscene words or socially inappropriate and derogatory remarks). It is no longer considered rare; about 1% of school-age children and adolescents are estimated to have Tourette’s, and coprolalia occurs only in a minority.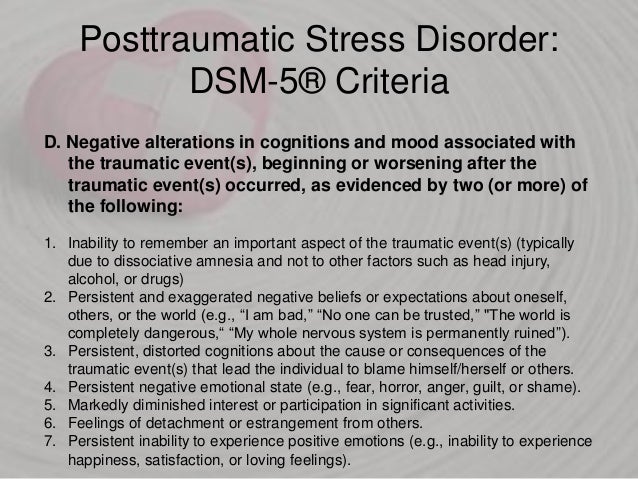 There are no specific tests for diagnosing Tourette’s; it is not always correctly identified because most cases are mild and the severity of tics decreases for most children as they pass through adolescence. Therefore, many go undiagnosed or may never seek medical attention. Extreme Tourette’s in adulthood, though sensationalized in the media, is rare, but for a small minority, severely debilitating tics can persist into adulthood. Tourette’s does not affect intelligence or life expectancy.
There are no specific tests for diagnosing Tourette’s; it is not always correctly identified because most cases are mild and the severity of tics decreases for most children as they pass through adolescence. Therefore, many go undiagnosed or may never seek medical attention. Extreme Tourette’s in adulthood, though sensationalized in the media, is rare, but for a small minority, severely debilitating tics can persist into adulthood. Tourette’s does not affect intelligence or life expectancy.
Tourette syndrome was named by French neurologist Jean-Martin Charcot for his intern, Georges Gilles de la Tourette, who published in 1885 an account of nine patients with a “convulsive tic disorder.” While the exact cause is unknown, it is believed to involve a combination of genetic and environmental factors. The mechanism appears to involve dysfunction in neural circuits between the basal ganglia and related structures in the brain.
Persistent (Chronic) Motor or Vocal Tic Disorder
To be diagnosed with a persistent tic disorder, a person must
- have one or more motor tics (for example, blinking or shrugging the shoulders) or vocal tics (for example, humming, clearing the throat, or yelling out a word or phrase), but not both.
- have tics that occur many times a day nearly every day or on and off throughout a period of more than a year.
- have tics that start before age 18 years.
- have symptoms that are not due to taking medicine or other drugs or due to having a medical condition that can cause tics (for example, seizures, Huntington disease, or postviral encephalitis).
- not have been diagnosed with Tourette’s.
Provisional Tic Disorder
To be diagnosed with a provisional tic disorder, a person must
- have one or more motor tics (for example, blinking or shrugging the shoulders) or vocal tics (for example, humming, clearing the throat, or yelling out a word or phrase).
- have been present for no longer than 12 months in a row.
- have tics that start before age 18 years.
- have symptoms that are not due to taking medicine or other drugs or due to having a medical condition that can cause tics (for example, Huntington disease or postviral encephalitis).
- not have been diagnosed with Tourette’s or persistent motor or vocal tic disorder.
Epidemiology
Tic disorders are more common among males than females. At least one in five children experience some form of tic disorder, most frequently between the ages of seven and twelve. As many as one in 100 people may experience some form of tic disorder, usually before the onset of puberty.
Treatment of Tic Disorders
There is no cure for Tourette’s and no single most effective medication. In most cases, medication for tics is not necessary, and behavioral therapies are the first-line treatment. Education is an important part of any treatment plan, and explanation alone often provides sufficient reassurance that no other treatment is necessary. Among those who are referred to specialty clinics, other conditions like ADHD and OCD are more likely than in the broader population of persons with Tourette’s. These co-occurring diagnoses often cause more impairment to the individual than the tics; hence it is important to correctly distinguish co-occurring conditions and treat them.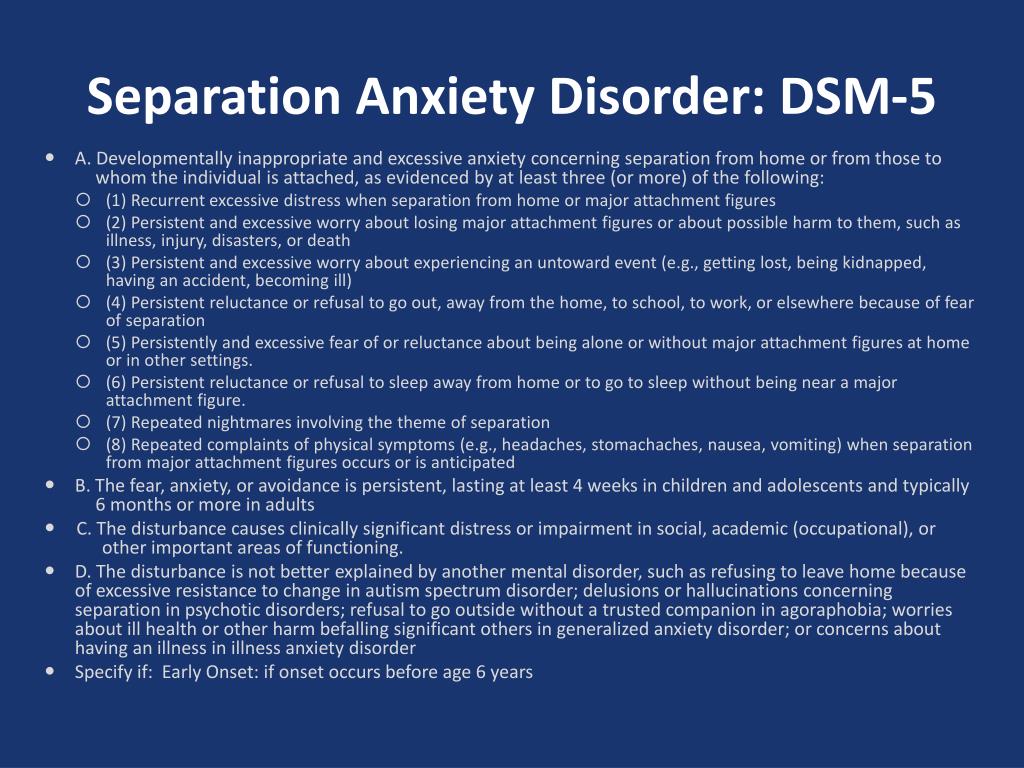
Watch It
Watch this video to learn more about Tourette’s and tic disorders.
You can view the transcript for “Tourette’s syndrome & tic disorders – definition, symptoms, diagnosis, treatment” here (opens in new window).
Key Takeaways: Motor Disorders
| Disorder | Diagnostic Criteria | Prevalence |
| Developmental coordination disorder |
| The exact proportion of people with the disorder is unknown since the disorder can be difficult to detect. Approximately 5%-6% of children are affected by this condition. |
| Stereotypic movement disorder |
| SMD occurs in about 3%-4% of children. Stereotypies often represent a physiological and transient finding, up to 60% of neurologically typical children showing some stereotypic movements or behaviors between two and five years.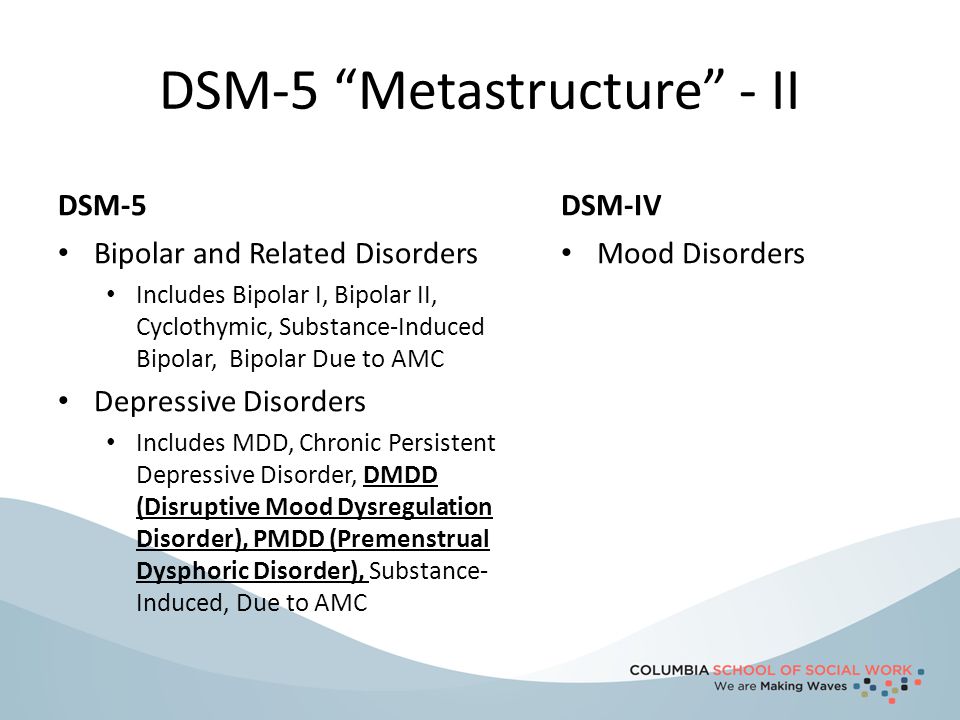 |
| Tourette’s Disorder |
| Tic disorders are more common among males than females. At least one in five children experience some form of tic disorder, most frequently between the ages of seven and twelve. |
| Persistent (chronic) motor or vocal tic disorder |
| Tic disorders are more common among males than females. At least one in five children experience some form of tic disorder, most frequently between the ages of seven and 12. |
| Provisional tic disorder |
| Tic disorders are more common among males than females. At least one in five children experience some form of tic disorder, most frequently between the ages of seven and 12. |
Try It
Glossary
developmental coordination disorder: a chronic neurological disorder beginning in childhood also known to affect planning of movements and co-ordination as a result of brain messages not being accurately transmitted to the body
motor disorders: malfunctions of the nervous system that cause involuntary or uncontrollable movements or actions of the body and can cause lack of intended movement or an excess of involuntary movement
stereotypic movement disorder: a motor disorder with onset in childhood involving repetitive, nonfunctional motor behavior (e.g., hand waving or head banging), that markedly interferes with normal activities or results in bodily injury
tic disorders: a motor disorder that can involve motor tics (e.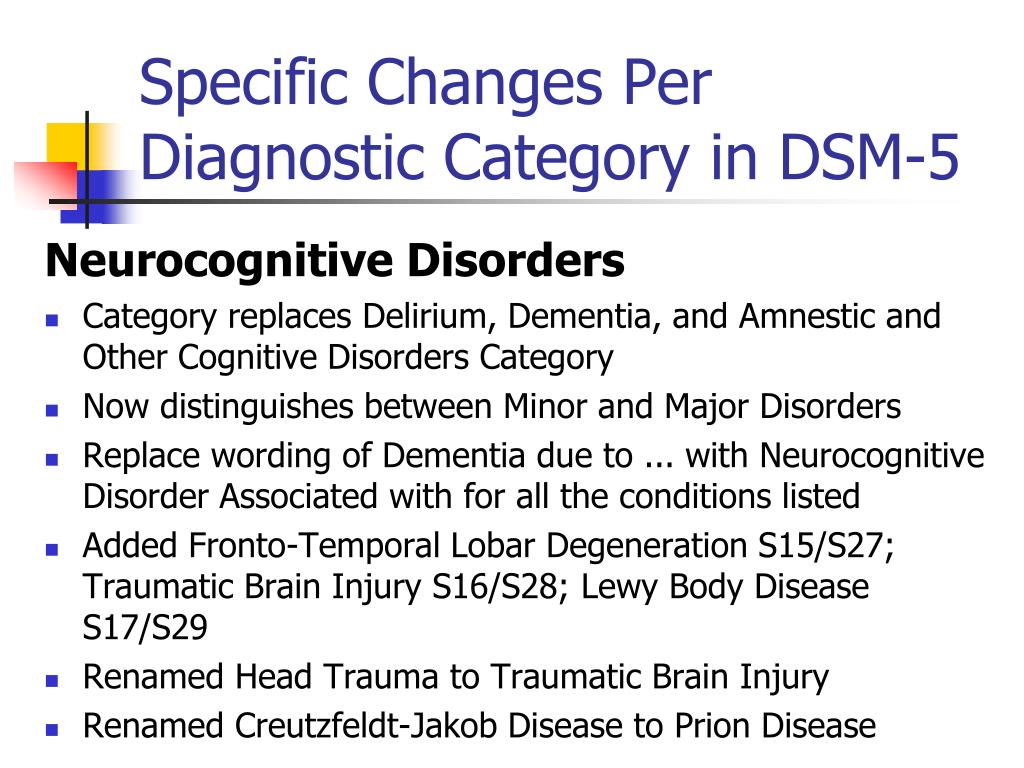 g., blinking or shrugging the shoulders) or vocal tics (e.g., humming, clearing the throat, or yelling out a word or phrase), although they might not always happen at the same time
g., blinking or shrugging the shoulders) or vocal tics (e.g., humming, clearing the throat, or yelling out a word or phrase), although they might not always happen at the same time
- “Stereotypic Movement Disorder." Psychology Today. Accessed November 10, 2020. https://www.psychologytoday.com/us/conditions/stereotypic-movement-disorder. ↵
- Valente, F., Pesola, C., Baglioni, V., Teresa Giannini, M., Chiarotti, F., Caravale, B., & Cardona, F. (2019). Developmental Motor Profile in Preschool Children with Primary Stereotypic Movement Disorder. BioMed research international, 2019, 1427294. https://doi.org/10.1155/2019/1427294 ↵
- Singer, H. S., Rajendran, S., Waranch, H. R., & Mahone, E. M. (2018). Home-Based, Therapist-Assisted, Therapy for Young Children With Primary Complex Motor Stereotypies. Pediatric neurology, 85, 51–57. https://doi.org/10.1016/j.pediatrneurol.2018.05.004 ↵
What are Motor Disorders? Signs, Symptoms, Causes, Treatments
Tic disorders appear in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as motor disorders listed in the neurodevelopmental disorder category.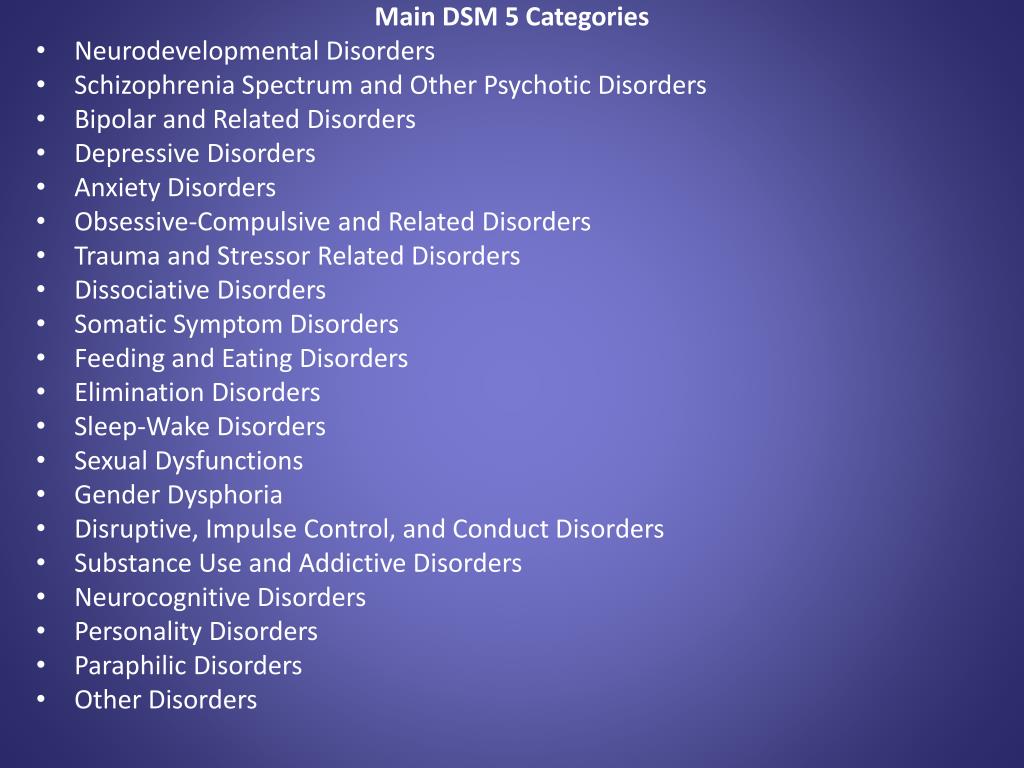 The DSM-5 replaces the term transient tic disorder with provisional tic disorder, but made few other significant changes.
The DSM-5 replaces the term transient tic disorder with provisional tic disorder, but made few other significant changes.
The term, tics, refers to sudden movements, twitches, or sounds that people perform repetitively. People with tic or motor disorders cannot refrain from doing these things or uttering the sounds. An individual with a motor tic disorder may blink repeatedly. Someone with a vocal tic might unwillingly make a grunting sound over and over.
The DSM-5 Motor Disorders
The various motor disorders differ in relation to the type of tic present and the duration of symptoms. People with tic disorders can have motor, vocal, or a combination of the two types of tics. The seven motor disorders listed in the DSM-5 include:
- Developmental Coordination Disorder
- Stereotypic Movement Disorder
- Tourette Syndrome (also called Tourette's disorder)
- Persistent (chronic) vocal or motor tic disorder
- Provisional tic disorder
- Other Specified Tic Disorder
- Unspecified Tic Disorder
Symptoms, Causes, and Treatment of Motor Disorders
Knowing the symptoms, causes, and treatment of motor disorders, as well as their impact and prognosis, can assist with early identification and help you obtain effective treatment.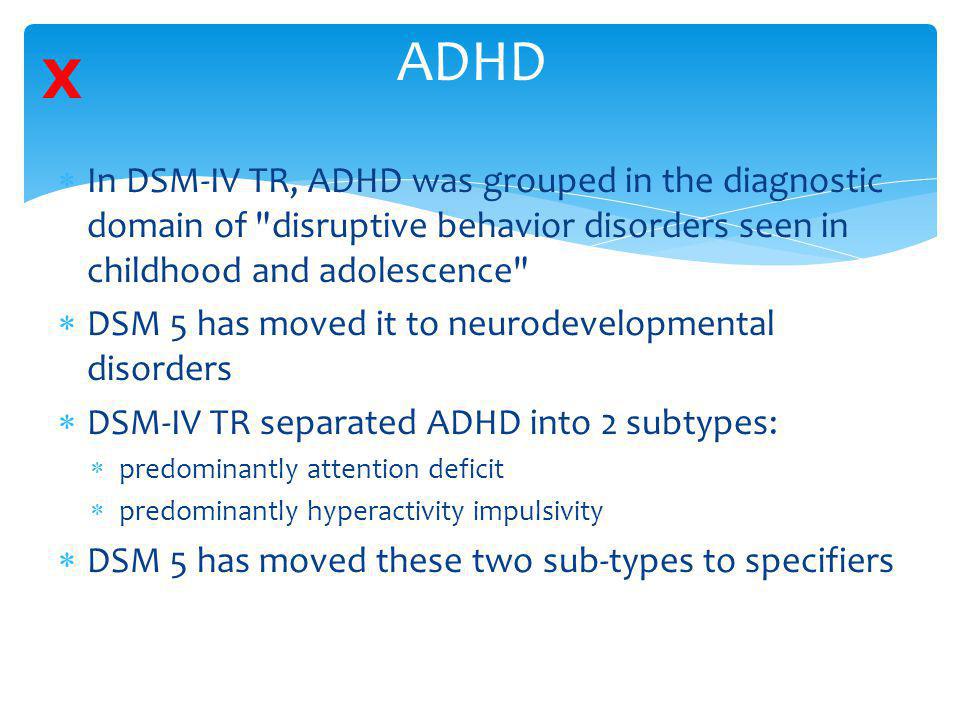 Each disorder has its own characteristics and issues.
Each disorder has its own characteristics and issues.
Developmental Coordination Disorder
Developmental coordination disorder (DCD) begins in childhood and leads to clumsiness and impaired coordination. Children with the disorder have impaired motor coordination compared to others in their age group. Symptoms include:
- Clumsiness
- Problems suckling and swallowing during the first 12 months of life
- Delayed sitting, crawling, and walking
- Difficulties with gross motor skills (i.e. jumping, hopping, and standing on one foot)
- Difficulties with fine motor skills (i.e. writing, cutting with scissors, tying shoes)
Experts have many theories, but still don't have a clear idea about what causes DCD. Children with DCD frequently have other difficulties in association with their motor problems, making it unlikely that a single factor causes the coordination issues in this group of children. Some research suggests a link between the cerebellum in the brain and DCD, since this brain structure has a critical role in developing movement control and other aspects of movement.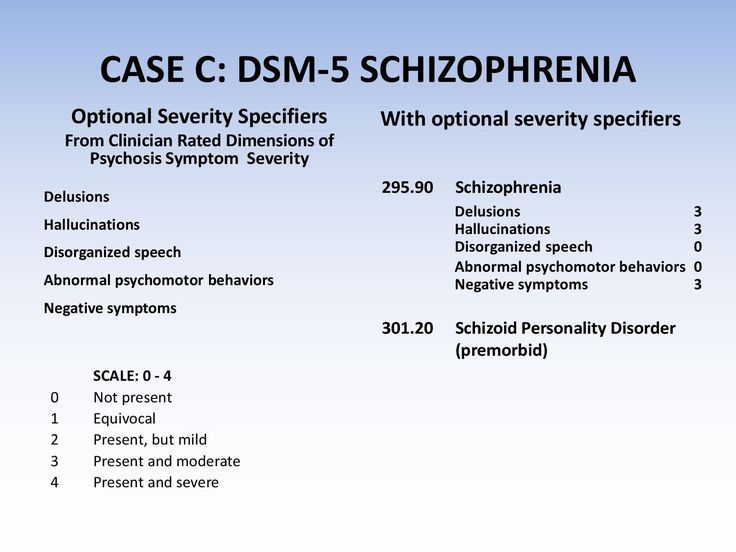
Treatment of developmental coordination disorder involves perceptual motor training and physical education. Children with DCD may overcome their writing issues by taking notes using a computer. Prognosis depends on the severity of the DCD. It typically does not worsen over time, but continues into adulthood.
Stereotypic Movement Disorder
The term, stereotypic movement disorder, refers to a movement or motor disorder characterized by repetitive movements, such as head banging or body rocking, for over four weeks. The movements tend to increase or intensify with elevated levels of stress or boredom.
These purposeless movements impede normal daily activity and could cause physical harm to the mover or those around him. Symptoms include repetitive and excessive:
- Head banging (against a wall or other solid form)
- Rocking back and forth
- Shaking or waving hands for no reason
- Nail biting
- Biting of self
- Hitting self
More boys than girls present with stereotypic movement disorder in childhood, however it can develop in adults too. Experts don't know the cause of this disorder when it occurs without the presence of other associated conditions. Abuse of stimulants like cocaine or amphetamines can cause a rapid onset, but short-lived period of stereotypic movement disorder. Head injuries may cause these stereotypical movements as well.
Experts don't know the cause of this disorder when it occurs without the presence of other associated conditions. Abuse of stimulants like cocaine or amphetamines can cause a rapid onset, but short-lived period of stereotypic movement disorder. Head injuries may cause these stereotypical movements as well.
Treatment of motor disorders depends on the possible causes, individual's age, and symptoms. Behavioral modification techniques and psychotherapy represent the most effective treatments. The prognosis for individuals with stereotypic movement disorder depends on the underlying cause, if identifiable. If drug-induced, the condition typically resolves on its own after the drug leaves the body. Stereotypic movements resulting from a head injury may remain indefinitely.
Tourette's Disorder
Tourette's disorder, also called Tourette syndrome, is a tic disorder that starts in childhood. It involves involuntary tics, which include purposeless movements or undesired sounds. Individuals with tic disorders, like Tourette syndrome, may blink their eyes excessively, constantly shrug shoulders up and down, or jerk the head. They may also grunt repetitively or randomly blurt out offensive words and phrases. People with this disorder can't control their movements or sounds. Signs typically appear between the ages of 2 and 12 years. Boys develop Tourette syndrome four times as often as girls. Symptoms of Tourette's disorder include:
Individuals with tic disorders, like Tourette syndrome, may blink their eyes excessively, constantly shrug shoulders up and down, or jerk the head. They may also grunt repetitively or randomly blurt out offensive words and phrases. People with this disorder can't control their movements or sounds. Signs typically appear between the ages of 2 and 12 years. Boys develop Tourette syndrome four times as often as girls. Symptoms of Tourette's disorder include:
- Simple tics – sudden, brief, and repetitive small movements
- Complex tics – coordinated strings of larger, more complex movements
- Vocal tics – short, random sounds or words
Motor tics usually appear before vocal tics, but not always. Symptoms range anywhere from very mild to severe. Severe symptoms interfere with communication and quality of life. As with many neurodevelopmental disorders, experts don't know the exact cause of Tourette syndrome. Many researchers believe that both genetics and the environment play a role in its development. Some evidence suggests that abnormal levels of certain brain chemicals may contribute to the development of the disorder.
Some evidence suggests that abnormal levels of certain brain chemicals may contribute to the development of the disorder.
Since there's no cure for Tourette's disorder, treatment focuses on controlling the tics that interfere with everyday life. Some success has been found with psychotherapy, behavior modification therapy, and deep brain stimulation. No psychiatric medication helps everyone with Tourette syndrome, but some are prescribed to reduce symptoms of adjunct or related conditions, such as ADHD or obsessive-compulsive disorder. Possible medications used to minimize symptoms include: antidepressants, stimulants (i.e. Ritalan and Adderall), or dopamine blockers.
Tics typically lessen in intensity and frequency with age. It's important for those dealing with tic disorders to reach out to others to help them cope and give support.
Persistent (chronic) Vocal or Motor Tic Disorder
Chronic vocal or motor tic disorder involves brief, repetitive movements or unwanted vocal sounds, but not both.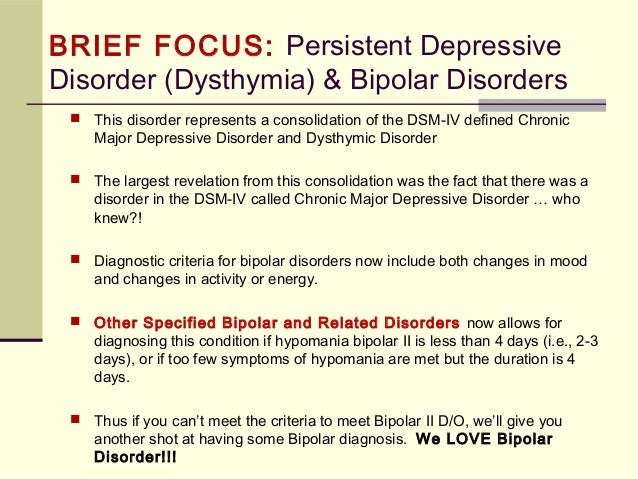 It's more common than Tourette syndrome, but less common than provisional tic disorder. Researchers do not know the cause of this disorder, but some theorize that chronic tics are forms of Tourette syndrome. Symptoms of chronic motor or vocal tic disorder include chronic and excessive:
It's more common than Tourette syndrome, but less common than provisional tic disorder. Researchers do not know the cause of this disorder, but some theorize that chronic tics are forms of Tourette syndrome. Symptoms of chronic motor or vocal tic disorder include chronic and excessive:
- Eye blinking
- Facial grimaces
- Jerking of the arms, legs, or head
- Vocal sounds (grunting, throat clearing)
People with chronic motor disorder report that they feel a sense of relief when making these movements or sounds. They can refrain from carrying them out for a brief period, but not for long. When asked, people describe their movements or sounds as in response to an intense inner urge. The tics often continue while the person sleeps and may worsen with fatigue, stress, frustration, or excitement.
Treatments focus on reducing symptoms, since there is no known cure. Doctors only prescribe psychotherapy and medications when the tics significantly impact daily activities and quality of life.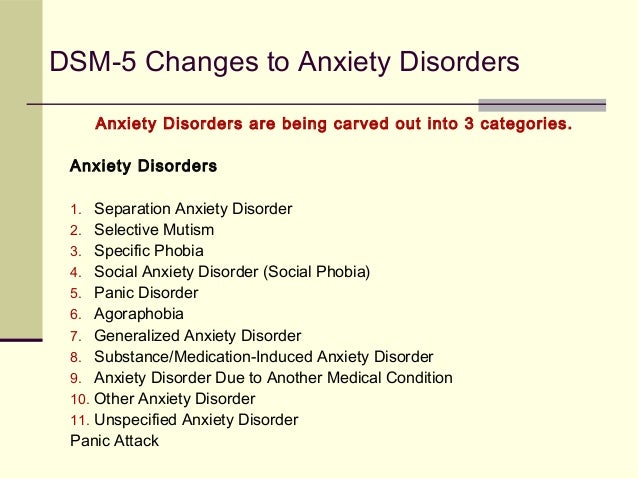 Drugs used to treat symptoms of tic disorders have negative side effects that must be weighted against any benefit. Children who develop chronic motor disorder before the age of 8 usually find that the symptoms stop once they reach puberty. But when older children or adults develop the disorder, the symptoms may last a lifetime.
Drugs used to treat symptoms of tic disorders have negative side effects that must be weighted against any benefit. Children who develop chronic motor disorder before the age of 8 usually find that the symptoms stop once they reach puberty. But when older children or adults develop the disorder, the symptoms may last a lifetime.
Provisional Tic Disorder
Formerly called transient tic disorder, provisional tic disorder involves the presence of one or more motor tics or vocal tics that occur several times a day. This is a temporary condition and people with this disorder make one or many quick, repetitive movements or noises. Provisional tic disorder develops before the age of 18. Symptoms include:
- Repetitive, non-rhythmic movements
- Intense urge to make the movement
- Quick movements that include:
- Eye blinking
- Fist clenching
- Toe curling
- Nostril flaring
- Facial grimaces
- Jerking of arms or legs
- Eyebrow raising
- Shoulder shrugging
- Other brief, purposeless movements
- Vocal tics may include:
- Grunting
- Moaning
- Sniffing
- Throat clearing
- Clicking
- Hissing
- Snorting
Health care experts recommend that family members avoid calling attention to the tics because this attention may increase stress levels, causing tics to worsen.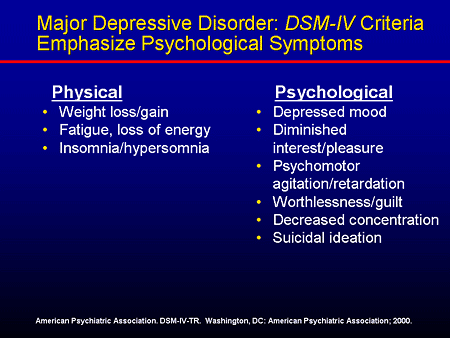 These simple childhood tics typically disappear over a few months.
These simple childhood tics typically disappear over a few months.
Other Specified Tic Disorder and Unspecified Tic Disorder
Other specified tic disorders are those in which the tics don't meet the diagnostic standards for a particular, specific tic disorder. This diagnosis might involve tics that last less than a month, or tics that begin and persist after the age of 18. The clinician will list the reason the tics don't meet this criteria. An unspecified tic disorder is the same thing; except the clinician does not list the reason the tics don't meet criteria for a specific diagnosis.
Coping with Motor Disorders
Motor disorders are most often conditions that occur in childhood and they can cause great shame and embarrassment in the individuals who have them. Dwelling on the tics and exaggerating their appearance to others can cause extreme anxiety and stress, actually making the tics worse. People with motor disorders or tic disorders should educate themselves about their condition so they can inform others about it.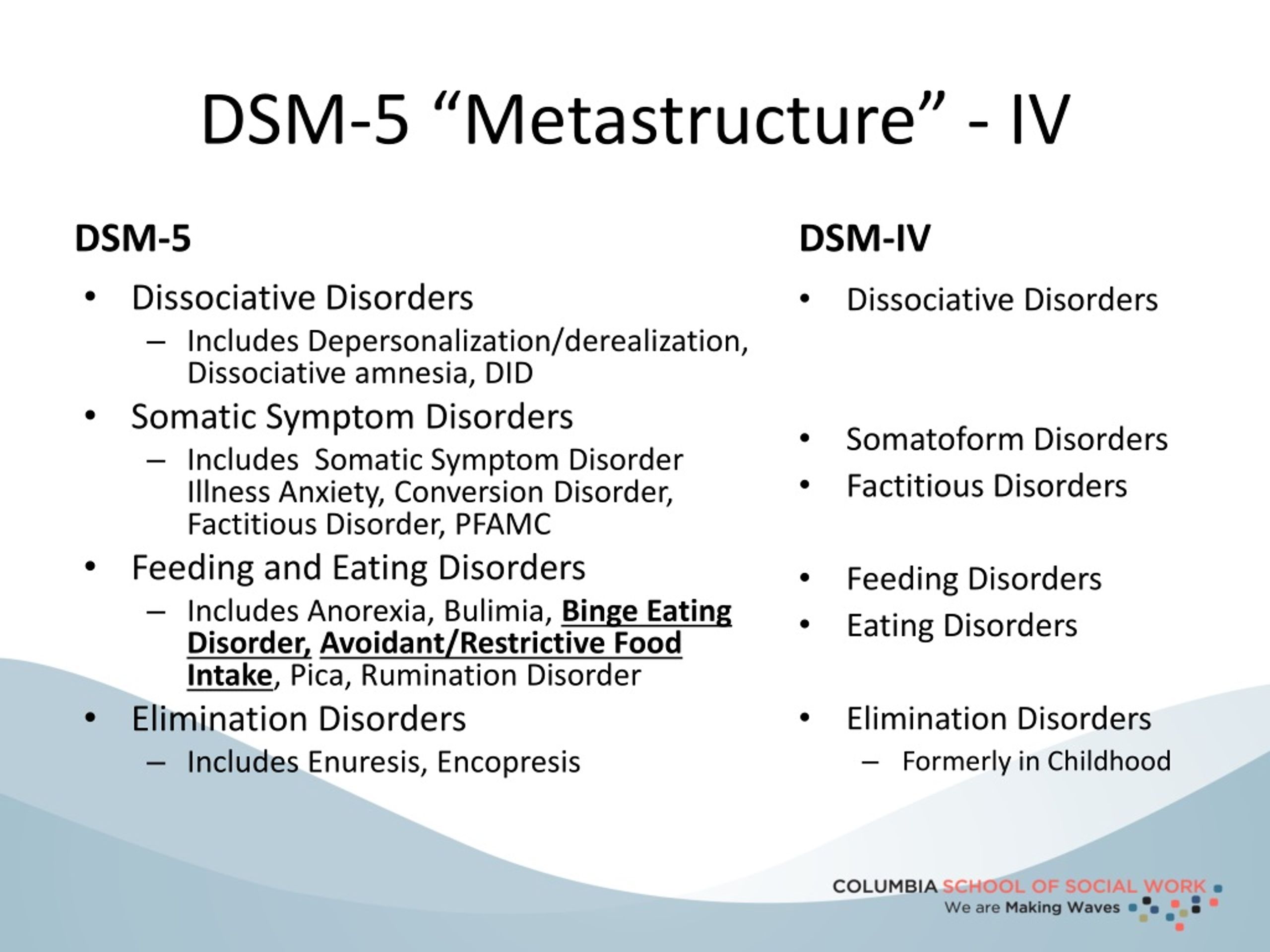 Joining a support group with others dealing with motor disorders helps too. Motor disorders are not something you can control, so there's no reason to be embarrassed. Avoiding stressful situations and getting plenty of rest can reduce symptoms of motor disorders too.
Joining a support group with others dealing with motor disorders helps too. Motor disorders are not something you can control, so there's no reason to be embarrassed. Avoiding stressful situations and getting plenty of rest can reduce symptoms of motor disorders too.
article references
APA Reference
Gluck, S. (2014, May 21). What are Motor Disorders? Signs, Symptoms, Causes, Treatments, HealthyPlace. Retrieved on 2022, November 3 from https://www.healthyplace.com/neurodevelopmental-disorders/motor-disorders/what-are-motor-disorders-signs-symptoms-causes-treatments
New American classification of mental disorders DSM-5 released to the world
Home > News > The new American classification of mental disorders DSM-5 is released to the world
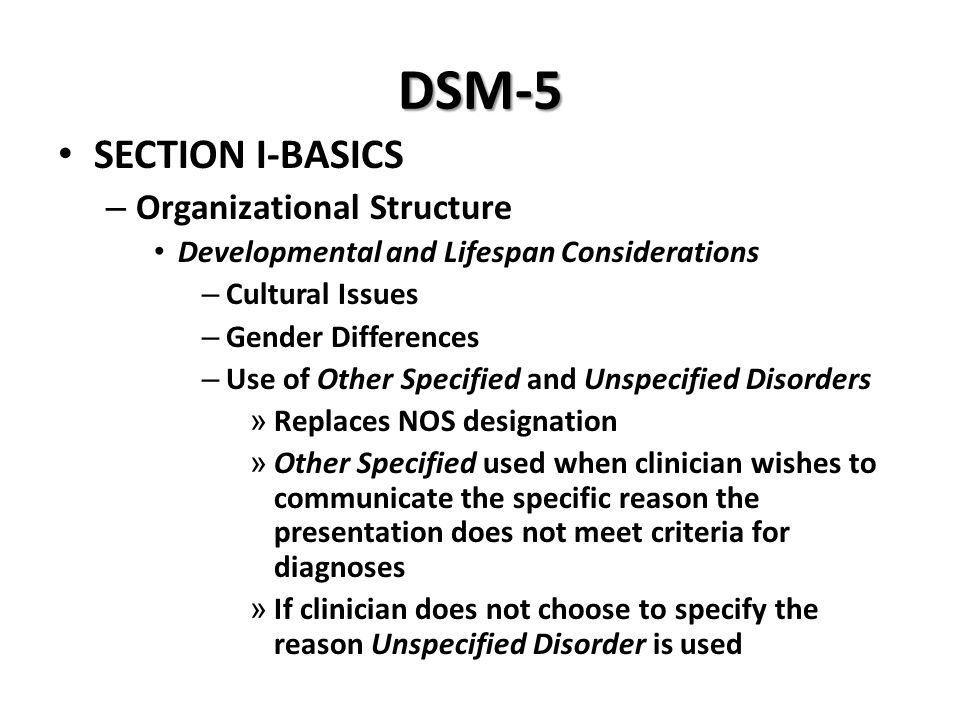
| DSM-5 consists of three sections: it is (1) an introductory part with instructions for use and a warning about the forensic psychiatric use of the DSM-5; (2) diagnostic criteria and codes for routine clinical use; and (3) tools and techniques to inform clinical decision making. Major changes:
The severity of the disorder is not determined by IQ, but by the level of adaptive functioning. Speech disorders have entered the new category "social communication disorder", in which some of the syndromes coincide with "autism spectrum disorder". The category "Autism Spectrum Disorders" replaces the DSM-4 diagnoses of autism, Asperger's syndrome, childhood disintegrative disorder, and an unspecified general developmental disorder, all of which cease to exist as separate diagnoses. ADHD can start later (before 12) and is treated differently in different areas. Learning disorders and movement disorders are organized differently in this chapter and somewhat combined.
For the diagnosis of schizophrenia, symptoms of the first Schneider rank lose their special weight. One positive symptom is required for a diagnosis to be made.
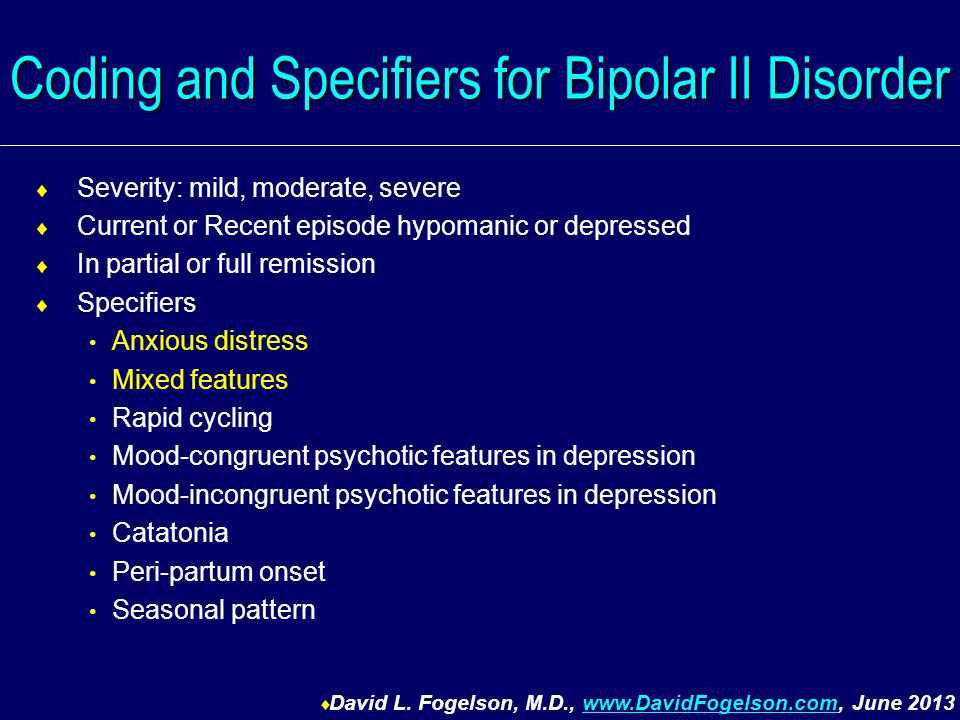
Bipolar and related disorders are now separated from depressive disorders and placed in a separate category. A clearer definition of mania is given and refinements for mixed episodes are introduced, which lowers the threshold for disorder. Added a residual subcategory ""other"" and a qualifying score for anxiety symptoms.
Disruptive mood dysregulation disorder and premenstrual dysphoric disorder added. Chronic depression and dysthymia are combined into one diagnosis, now it is ""persistent depressive disorder (dysthymia)"" with a number of clarifying indicators.
|
ISSN 2588-0519 (Print)
ISSN 2618-8473 (Online)
Autism spectrum disorders in children
home
Articles
Diseases
Dmitry Alpatsky Neurologist, epileptologist, EEG doctor
07.12.2015
Often, mothers come to the doctor with complaints of delayed speech development in a child. But in some children, with a close look, the specialist, in addition to this, sees the features of the child's behavior that differ from the norm and alarm .
Consider a clinical example:
Boy S. Age 2 years 9 months. According to the mother, the child's vocabulary is no more than 20 separate words, consisting of two or three syllables.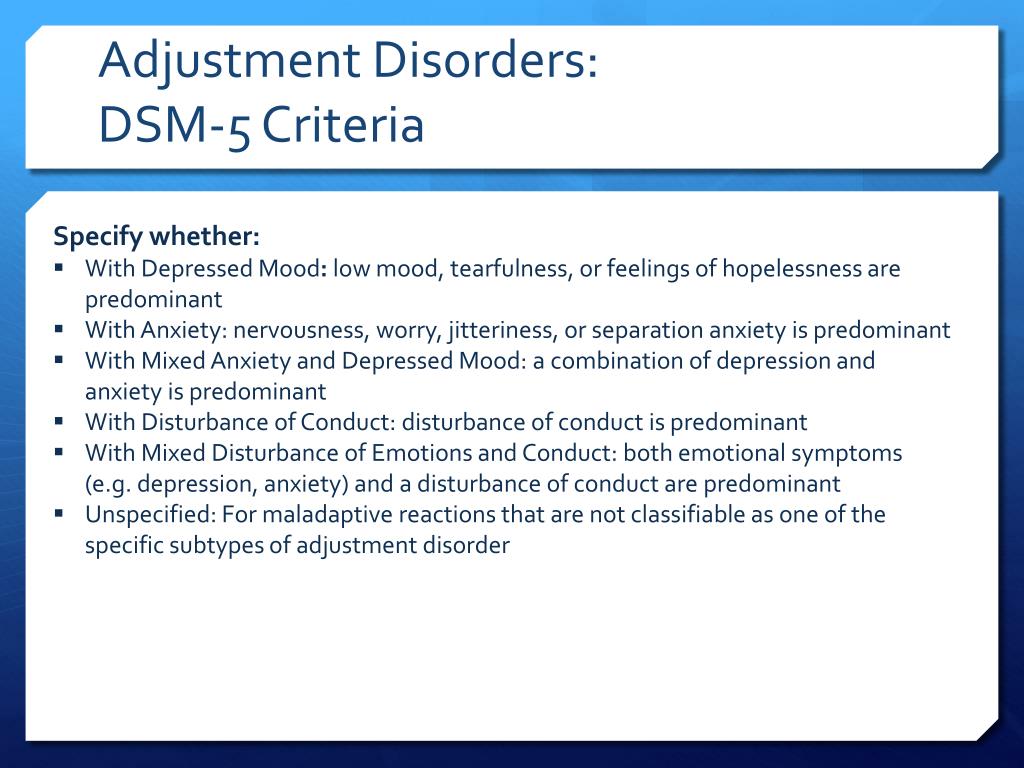 There are no phrases. Mom says that the child often has tantrums, is restless, it is difficult to fall asleep. The child's mother has no other complaints. On examination, the doctor notices that the child does not look into the eyes, is constantly in motion, reacts with a cry if something is not given or forbidden to him. You can calm the child only by giving him a mobile phone or tablet. Shows interest not in children's toys, but more in shiny pieces of furniture and interior. Starting to play something, quickly loses interest and switches to something else. Asking the mother, it turns out that the child is very selective in food. Not accustomed to the potty, defecation only in a diaper in a standing position. Difficulty falling asleep and waking up during sleep. The child underwent Electroencephalography and consultations with a clinical psychologist and a speech therapist. Based on the results of the diagnosis and the clinical picture, the diagnosis was made - Autism Spectrum Disorder.
There are no phrases. Mom says that the child often has tantrums, is restless, it is difficult to fall asleep. The child's mother has no other complaints. On examination, the doctor notices that the child does not look into the eyes, is constantly in motion, reacts with a cry if something is not given or forbidden to him. You can calm the child only by giving him a mobile phone or tablet. Shows interest not in children's toys, but more in shiny pieces of furniture and interior. Starting to play something, quickly loses interest and switches to something else. Asking the mother, it turns out that the child is very selective in food. Not accustomed to the potty, defecation only in a diaper in a standing position. Difficulty falling asleep and waking up during sleep. The child underwent Electroencephalography and consultations with a clinical psychologist and a speech therapist. Based on the results of the diagnosis and the clinical picture, the diagnosis was made - Autism Spectrum Disorder.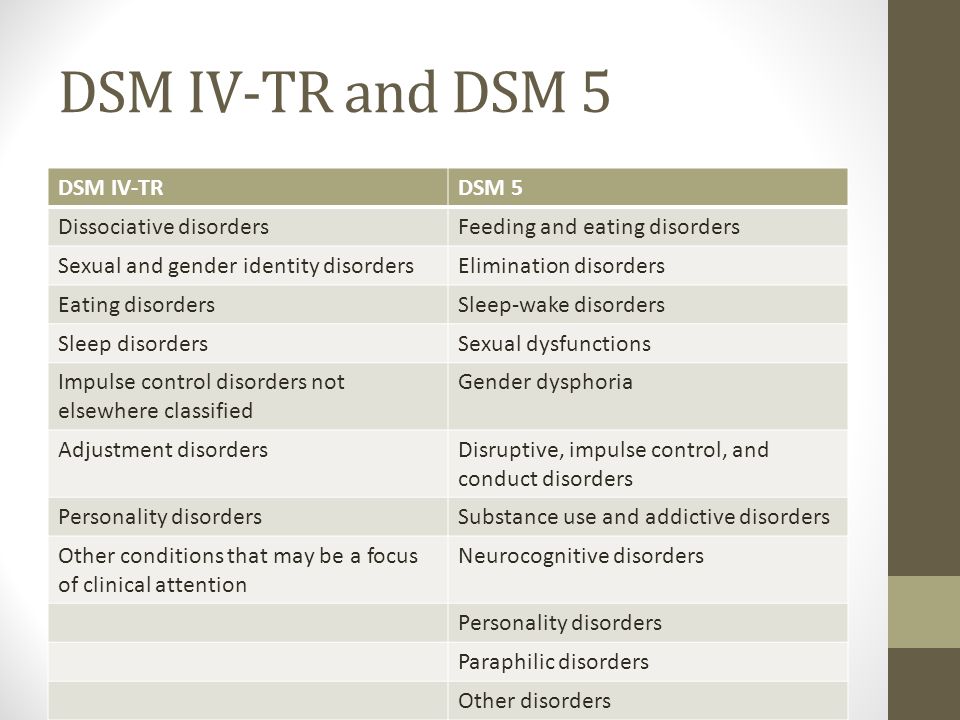
Autism Spectrum Disorders (ASD) are complex disorders of mental development that are characterized by social maladaptation and inability to social interaction, communication and behavioral stereotypy (multiple repetitions of monotonous actions).
Back in the middle of the last century, autism was a fairly rare disease. But over time, more and more children suffering from this disorder began to appear. Statistics show that the incidence of ASD in children over the past 30-40 years in countries where such statistics are carried out has risen from 4-5 people per 10,000 children to 50-116 cases per 10,000 children. At the same time, boys are more susceptible to this disease than girls (approximately 4:1 ratio).
Causes of RAS.
All over the world, until today, scientists studying the causes of autism have not come to a consensus. Many assumptions are put forward. Among the possible factors for the appearance of this disorder in children are some hypotheses:
- genetic predisposition hypothesis
- a hypothesis based on disorders of the development of the nervous system (autism is considered as a disease caused by disorders of brain development in the early stages of a child's growth).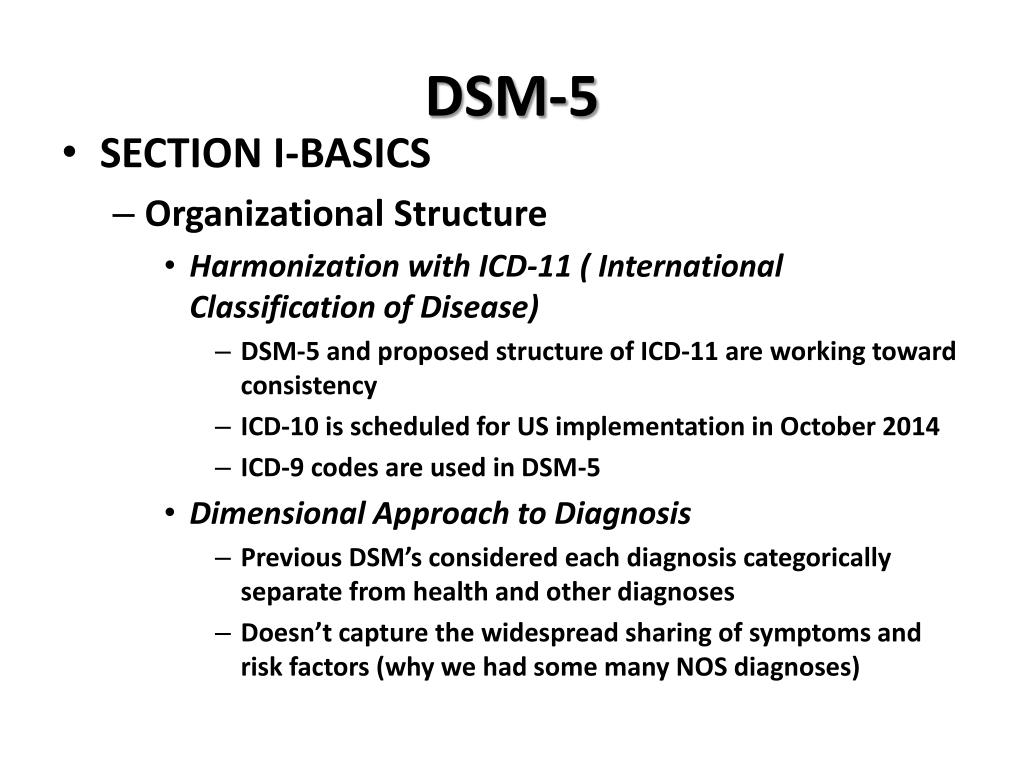
- hypotheses about the influence of external factors: infections, chemical effects on the mother's body during pregnancy, birth trauma, congenital metabolic disorders, the influence of certain drugs, industrial toxins.
But whether these factors really can lead to the appearance of autism in children has not yet been clarified.
Features of the mental development of children with ASD.
To understand and recognize the presence of autism in a child, parents need to carefully monitor the behavior of the child, notice unusual signs that are not characteristic of the age norm. Most often, these signs can be detected in children under the age of 3 years.
Childhood autism is considered as a developmental disorder that affects all areas of the child's psyche: intellectual, emotional, sensitivity, motor sphere, attention, thinking, memory, speech.
Disorders of speech development : absent or weak cooing and babbling may be noted at an early age.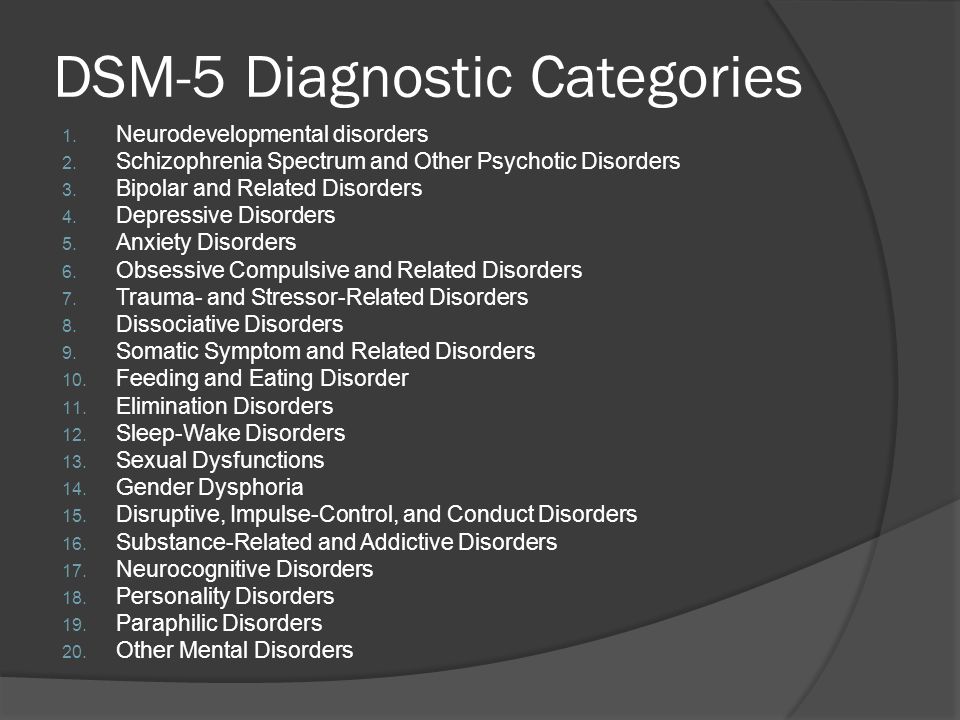 After a year, it becomes noticeable that the child does not use speech to communicate with adults, does not respond to a name, and does not follow verbal instructions. By the age of 2, children have a very small vocabulary. By the age of 3 they do not build phrases or sentences. At the same time, children often stereotypically repeat words (often incomprehensible to others) in the form of an echo. Some children have a lack of speech development. For others, speech continues to develop, but there are still communication impairments. Children do not use pronouns, address, speak about themselves in the third person. In some cases, there is a regression of previously acquired speech skills.
After a year, it becomes noticeable that the child does not use speech to communicate with adults, does not respond to a name, and does not follow verbal instructions. By the age of 2, children have a very small vocabulary. By the age of 3 they do not build phrases or sentences. At the same time, children often stereotypically repeat words (often incomprehensible to others) in the form of an echo. Some children have a lack of speech development. For others, speech continues to develop, but there are still communication impairments. Children do not use pronouns, address, speak about themselves in the third person. In some cases, there is a regression of previously acquired speech skills.
Difficulties in communication and lack of emotional contact with others: Such children shy away from tactile contact, eye contact is almost completely absent, there are inadequate facial reactions and difficulties in using gestures. Children most often do not smile, do not reach out to their parents and resist attempts by adults to take them in their arms. Children with autism lack the ability to express their emotions, as well as to recognize them in the people around them. There is a lack of empathy for other people. The child, along with the adult, does not focus on one activity. Children with autism do not make contact with other children or avoid it, they find it difficult to cooperate with other children, most often they tend to retire (difficulties in adapting to the environment).
Children with autism lack the ability to express their emotions, as well as to recognize them in the people around them. There is a lack of empathy for other people. The child, along with the adult, does not focus on one activity. Children with autism do not make contact with other children or avoid it, they find it difficult to cooperate with other children, most often they tend to retire (difficulties in adapting to the environment).
H violation of exploratory behavior: children are not attracted by the novelty of the situation, are not interested in the environment, are not interested in toys. Therefore, children with autism most often use toys in an unusual way, for example, a child may not roll the whole car, but turn one of its wheels monotonously for hours. Or not understanding the purpose of the toy to use it for other purposes.
Eating disorders : a child with autism can be extremely selective in the offered products, food can cause the child to be disgusted, dangerous, often children begin to sniff food.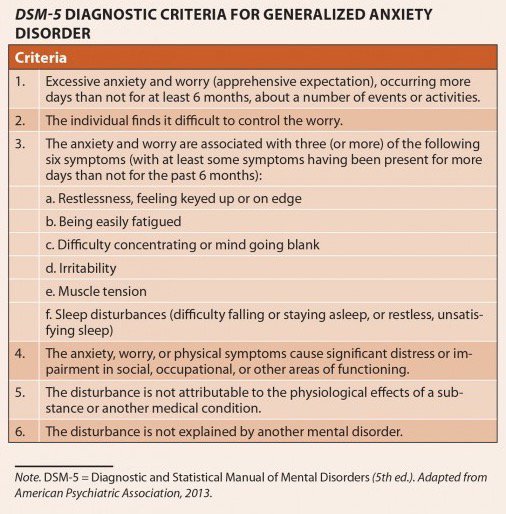 But along with this, children may try to eat an inedible thing.
But along with this, children may try to eat an inedible thing.
Violation of self-preservation behavior: due to a large number of fears, the child often finds himself in a situation that is dangerous for himself. The cause can be any external stimulus that causes an inadequate reaction in the child. For example, a sudden noise may cause a child to run in a random direction. Also, the reason is ignoring real threats to life: a child can climb very high, play with sharp objects, cross the road without looking.
Disturbance of motor development: as soon as the child begins to walk, he is noted for clumsiness. Also, some children with autism are inherent in walking on their toes, a very noticeable violation of the coordination of hands and feet. It is very difficult for such children to teach everyday actions, it is rather difficult for them to imitate. Instead, they develop stereotypical movements (performing the same actions for a long time, running in circles, swinging, flapping “like wings” and circular movements with their arms), as well as stereotypical manipulations with objects (tweaking small details, lining them up).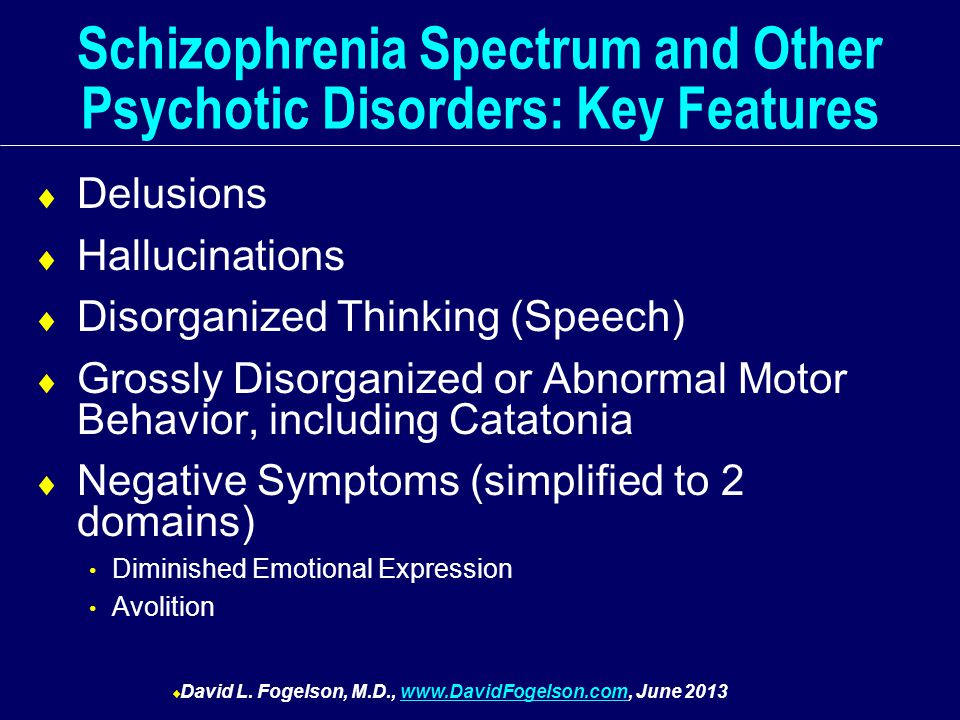 Children with autism have significant difficulty in learning self-care skills. Pronounced motor awkwardness.
Children with autism have significant difficulty in learning self-care skills. Pronounced motor awkwardness.
Perception disorders: difficulties in orientation in space, fragmentation in the perception of the environment, distortion of a holistic picture of the objective world.
Difficulty in concentrating: children have difficulty concentrating on one thing, there is high impulsivity and restlessness.
Poor memory: both parents and professionals often notice that children with autism are good at remembering things that are meaningful to them (this may cause them pleasure or fear). Such children remember their fear for a long time, even if it happened a very long time ago.
Features of thinking: experts note difficulties in arbitrary learning. Also, children with autism do not focus on understanding the cause-and-effect relationships in what is happening, there are difficulties in transferring the acquired skills to a new situation, the concreteness of thinking.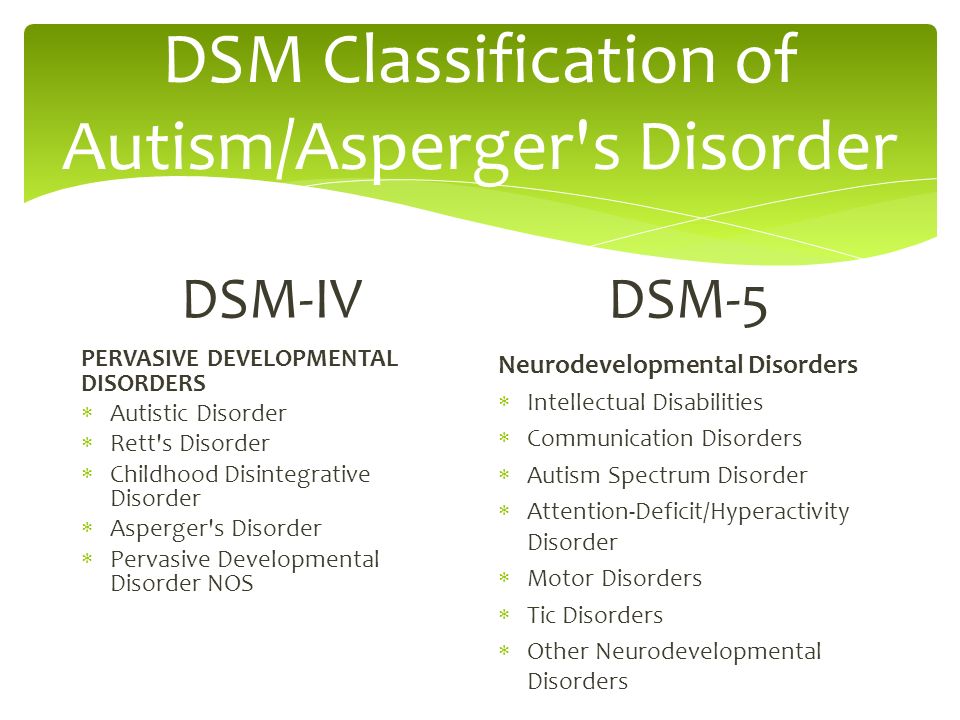 It is difficult for a child to understand the sequence of events and the logic of another person.
It is difficult for a child to understand the sequence of events and the logic of another person.
Behavioral problems: negativism (refusal to listen to instructions from an adult, to perform joint activities with him, avoiding a learning situation). Often accompanied by resistance, screams, aggressive outbursts. A huge problem is the fears of such children. Usually they are incomprehensible to others, because often children cannot explain them. The child may be frightened by sharp sounds, some specific actions. Another behavioral disorder is aggression. Any disorder, violation of a stereotype, interference of the outside world in a child's life can provoke aggressive (hysteria or physical attack) and auto-aggressive outbursts (damage to oneself).
Each case of the disease is very individual: autism can have most of the listed signs in an extreme degree of manifestation, and it can manifest itself only in some barely noticeable features.
Diagnosis of Autism Spectrum Disorders
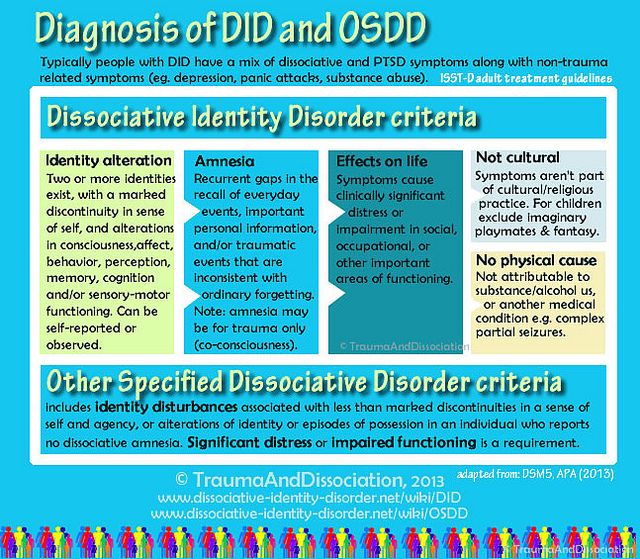
To diagnose autism, specialists use the criteria of 2 international classifications: ICD-10 and DSM-5.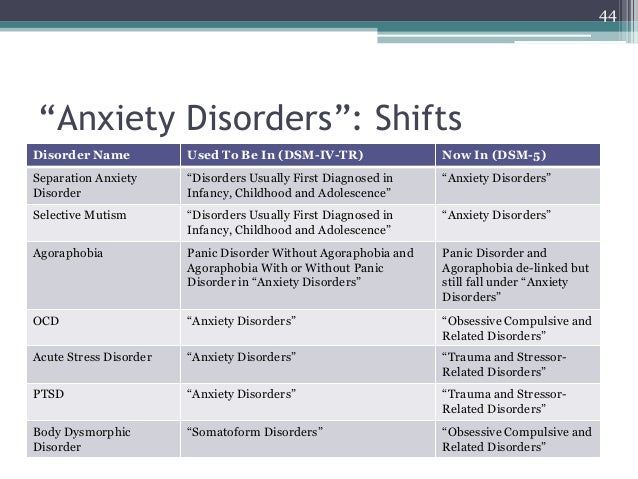
But the main three criteria (“triad” of violations) that can be distinguished are:
- violation of social adaptation
- violations in the communication sphere
- stereotypical behavior
The main diagnostic steps include:
- examination of the child by a psychiatrist, neurologist, psychologist
- observation of the child and filling out the "Autism Rating Scale", which can be used to determine the severity of the disorder
- conversation with parents
- filling in questionnaires by parents - "Questionnaire for the diagnosis of autism"
Species PAC
There are several existing classifications of ASD, and the separation often occurs on completely different grounds, which, of course, can bring some inconvenience to a person who is initially little familiar with medicine or psychology; therefore, the most basic and frequently encountered types of ASD will be highlighted below: - Kanner's syndrome (Early childhood autism) - characterized by a "triad" of the main violations: difficulty in establishing contacts with the outside world, stereotypical behavior, as well as a delay or violation of the communicative functions of speech development . It is also necessary to note the condition of the early onset of these symptoms (up to about 2.5 years)
It is also necessary to note the condition of the early onset of these symptoms (up to about 2.5 years)
It manifests itself in children in 4 forms, depending on the degree of fencing off from the outside world:
Complete detachment from what is happening. This group is characterized by the absence of speech and the inability to organize the child (to establish eye contact, to achieve the implementation of instructions and assignments). When trying to interact with the child, he shows the greatest discomfort and impaired activity.
Active rejection. It is characterized by more active contact with the environment than the first group. There is no such detachment, but there is rejection of a part of the world that is unacceptable to the child. The child shows selective behavior (in communication with people, in food, in clothes)
Preoccupation with autistic interests. It is characterized by the formation of overvalued addictions (for years a child can talk on the same topic, draw the same plot).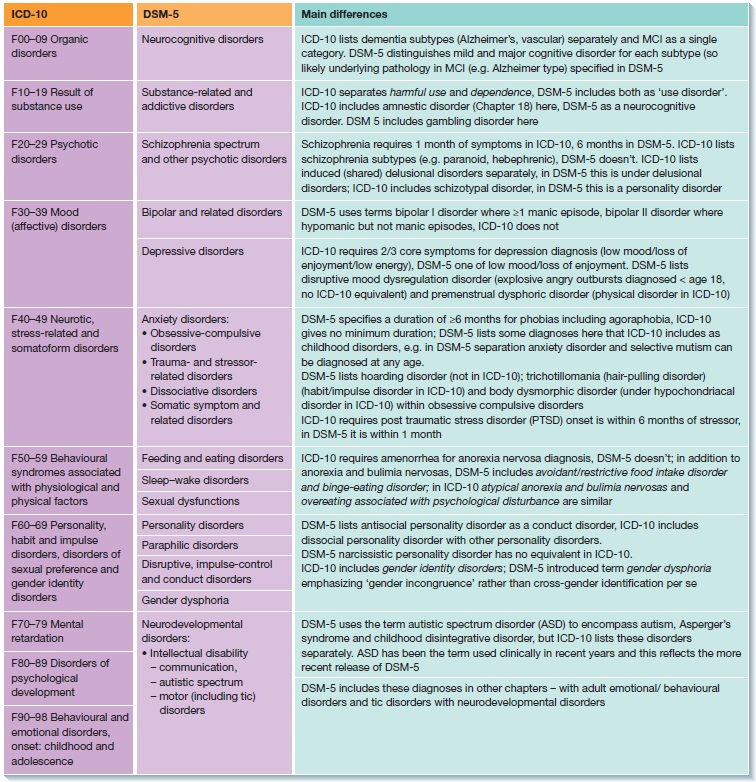 The gaze of such children is directed at the face of a person, but they look "through" this person. Such children enjoy the stereotyped reproduction of individual impressions.
The gaze of such children is directed at the face of a person, but they look "through" this person. Such children enjoy the stereotyped reproduction of individual impressions.
Extreme difficulty in organizing communication and interaction. Autism at its mildest. Children are characterized by increased vulnerability, contact with the world stops at the slightest sensation of obstacles. These children can make eye contact.
- Asperger's Syndrome. Formed from birth. Children have an early onset of speech development, a rich vocabulary, developed logical thinking, and there are no disorders in mental development. But at the same time, the communicative side of speech suffers: such children do not know how to establish contact with other people, do not listen to them, can talk to themselves, do not keep a distance in communication, and do not know how to empathize with other people.
- Rett syndrome. Its peculiarity lies in the fact that the development of a child up to 1-1.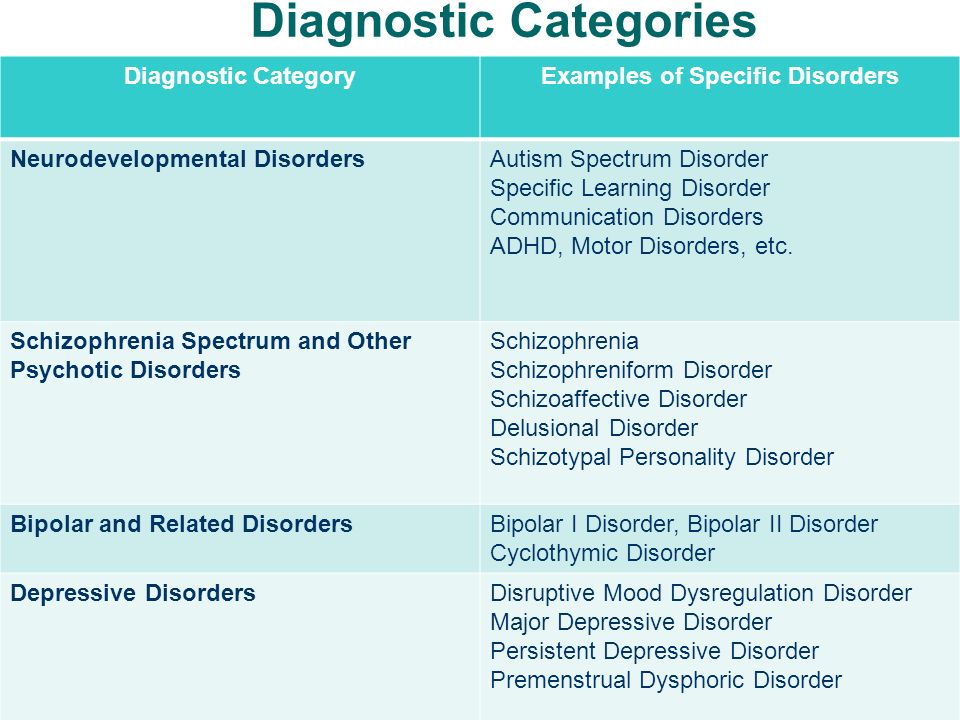 5 years proceeds normally, but then the newly acquired speech, motor and subject-role skills begin to disintegrate. Characteristic for this condition are stereotypical, monotonous movements of the hands, rubbing, wringing, while not carrying a purposeful character. The rarest of the presented diseases, occurring almost always only in girls.
5 years proceeds normally, but then the newly acquired speech, motor and subject-role skills begin to disintegrate. Characteristic for this condition are stereotypical, monotonous movements of the hands, rubbing, wringing, while not carrying a purposeful character. The rarest of the presented diseases, occurring almost always only in girls.
- Childhood psychosis. The first manifestation of symptoms before 3 years of age. It is characterized by violations of social behavior, communication disorders. There are stereotypes in behavior (children run in a monotonous circle, sway while standing and sitting, fingering their fingers, shaking their hands). These children have eating disorders: they can swallow food without chewing. Their unclear speech can sometimes be an incoherent set of words. There are times when children freeze in place, like dolls.
- Atypical autism. It differs from autism in terms of age manifestation and the absence of one criterion from the “triad” of major disorders.
Correction of patients with ASD
One of the most important sections of habilitation for children with ASD is undoubtedly the provision of psycho-correctional and social rehabilitation assistance, with the formation of social interaction and adaptation skills. Comprehensive psycho-correctional work, which includes all sections and types of rehabilitation assistance, which will be described below, is, along with drug therapy, an effective means of stopping the negative symptoms of ASD, and also contributes to the normal inclusion of the child in society. Types of RAS correction:
1) Psychological correction - the most common and well-known type; It is characterized by a fairly wide range of methods, of which the TEACCH and ABA-therapy programs are most widely used and recognized in the world.
The first program is based on the following principles:
- The characteristics of each individual child are interpreted on the basis of observations of him, and not from theoretical ideas;
- increasing adaptation is carried out both by learning new skills and by adapting existing ones to the environment;
- Creation of an individual training program for each child; use of structured learning; holistic approach to intervention.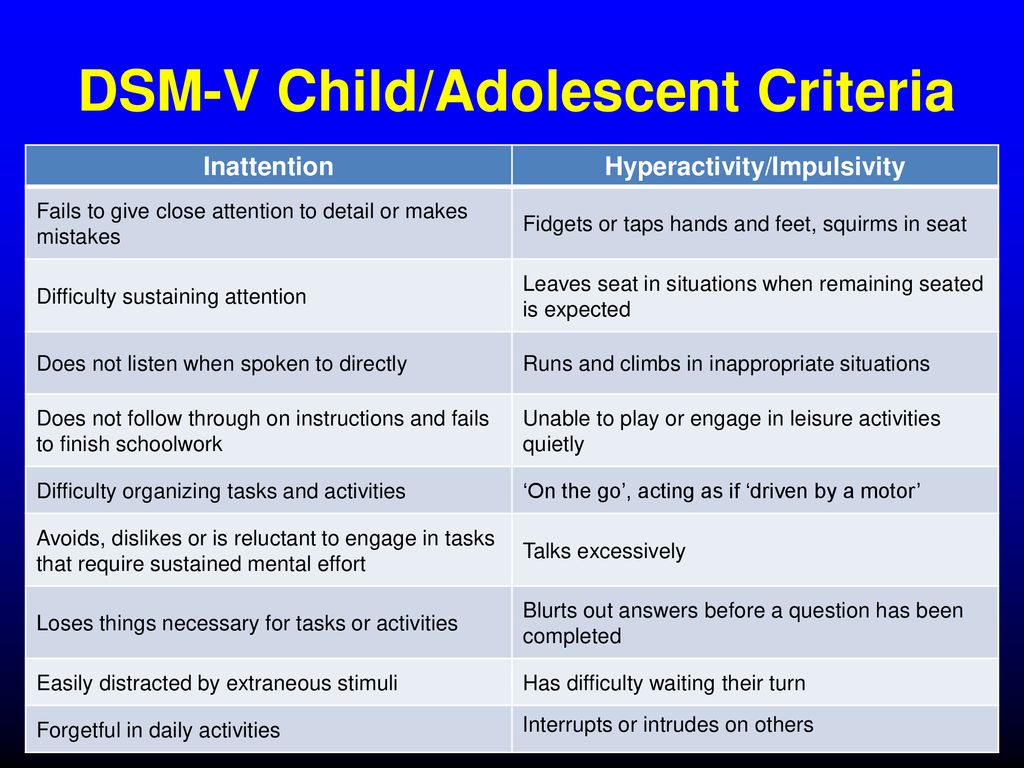
The second program is largely based on learning, which depends on the consequences that have arisen after the behavior. Consequences can be in the form of punishment or reward. In this model, it is necessary to highlight the main methods, such as the procedure for creating a contour and reinforcing behavior similar to the target; method of teaching chains of behavior; method of teaching discrimination of stimuli.
2) Neuropsychological correction - this type includes a set of exercises consisting of stretching, breathing, oculomotor, facial and other exercises for the development of the communicative and cognitive sphere, and the exercises themselves differ markedly in time and quantity.
3) Work with the child's family and environment - first of all, this type of correction is aimed at alleviating emotional tension and anxiety among family members, since parents of children with ASD often also need help, including psychotherapeutic support and training programs (such programs are mainly aimed at developing feelings of understanding of the problem, the reality of its solution and the meaningfulness of behavior in the current family situation).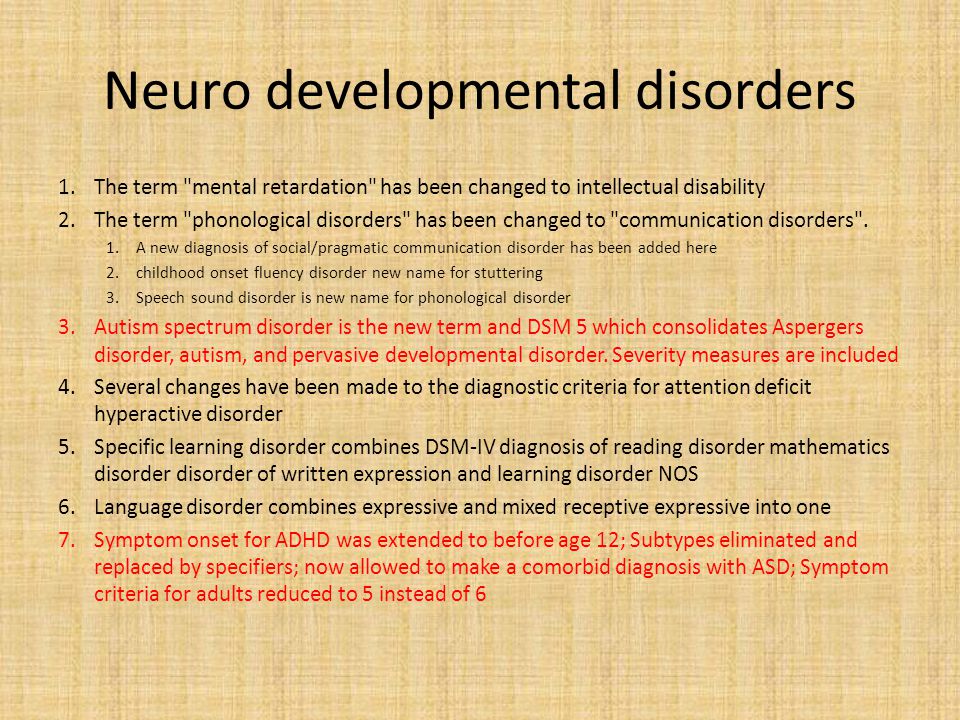
4) Psychosocial therapy - in fact, work with the child himself to form the cognitive, emotional and motivational-volitional resources of the individual for the possibility of further social adaptation, the need for which becomes more pronounced as the child with ASD grows older.
5) Logopedic correction - given the fact that speech development disorder is one of the cardinal manifestations of ASD, this type of work with a child will be an integral part of the correction program. It is characterized by a focus on the formation of vocabulary, the development of auditory attention, as well as phonetic and speech hearing.
6) Medical correction of RAS. In some forms of autism, medication is needed for the child. For example, to improve concentration and perseverance, a doctor may prescribe vitamins and nootropic drugs that improve thinking processes and stimulate speech development. And with high impulsivity, aggression, negativism, pronounced signs of "withdrawal into oneself", psychotropic drugs can help.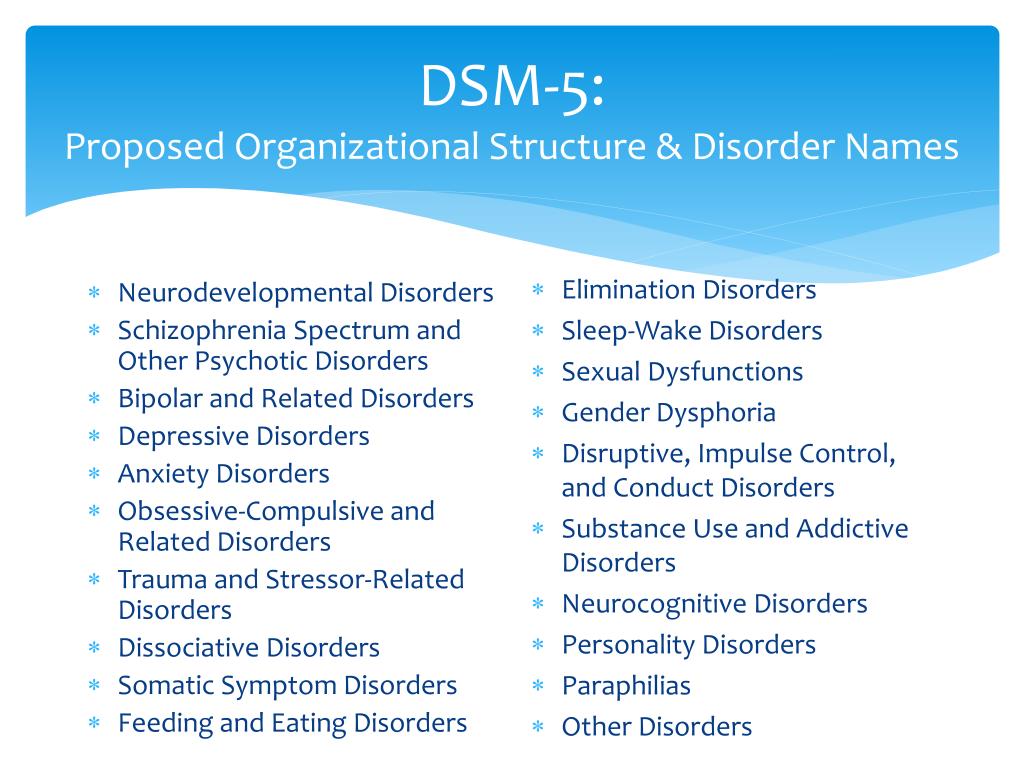
 Subtypes are removed - in favor of the dimensional indicator of severity. For schizoaffective disorder, the mood aspect is emphasized, and for delusional disorder, frivolous content is no longer excluded – although it is evaluated separately. The "catatonia" section has been expanded: this code can now be entered as an adjacent diagnosis (specifying indicator) for depressive, bipolar and psychotic disorders.
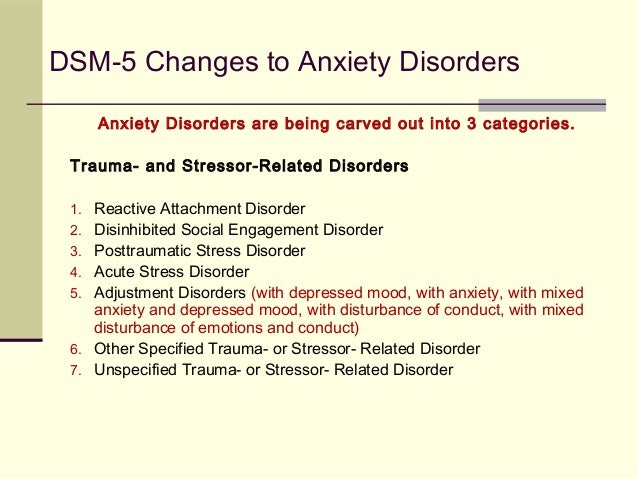
Subtypes are removed - in favor of the dimensional indicator of severity. For schizoaffective disorder, the mood aspect is emphasized, and for delusional disorder, frivolous content is no longer excluded – although it is evaluated separately. The "catatonia" section has been expanded: this code can now be entered as an adjacent diagnosis (specifying indicator) for depressive, bipolar and psychotic disorders. 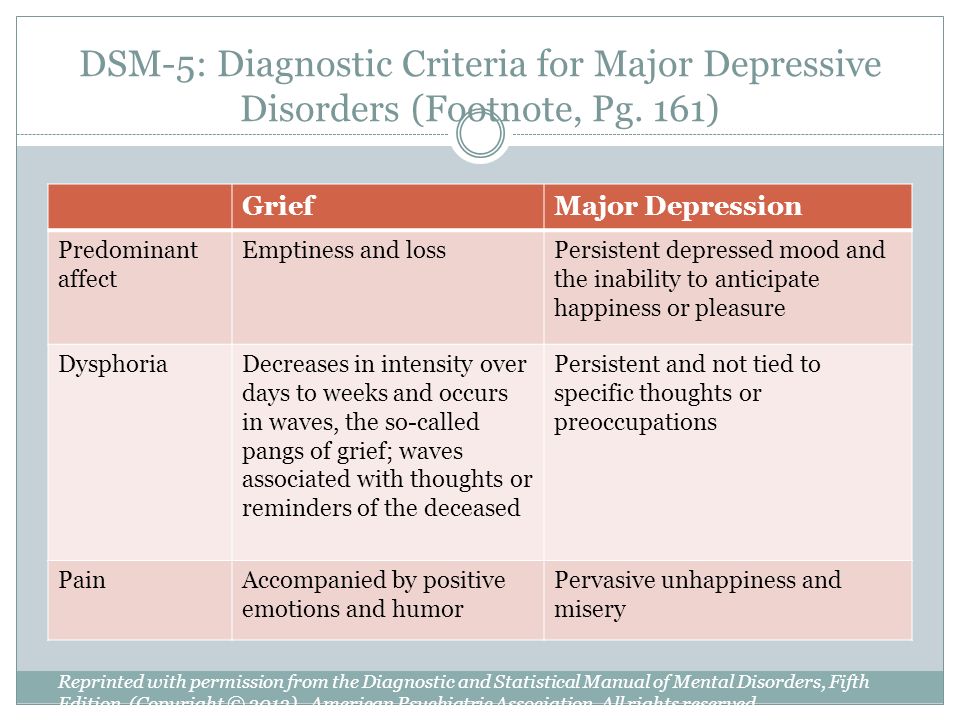 Major depressive disorder remained virtually unchanged, however, for "subthreshold" symptoms, a clarifying indicator ""mixed manifestations"" was introduced. A clarifying indicator for anxious distress has also been introduced. Removed grounds for exclusion for grief. 9(see below) Various phobia criteria are slightly adapted, and agoraphobia and panic are decoupled. Panic attacks can act as a clarifying indicator for other diagnoses. The diagnoses of separation anxiety disorder and selective mutism are no longer specific "childhood" diagnoses.
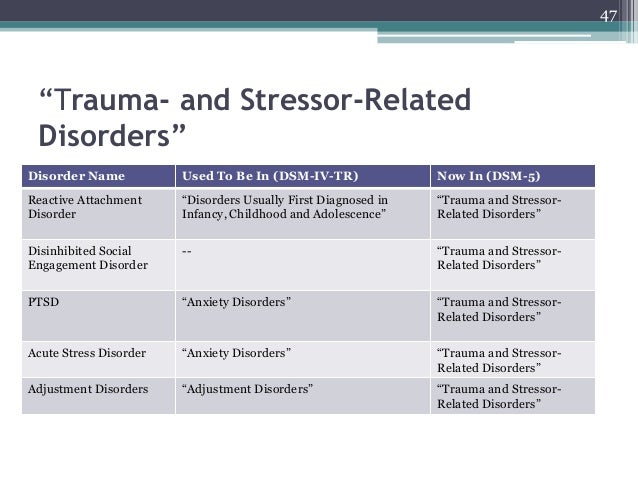
Major depressive disorder remained virtually unchanged, however, for "subthreshold" symptoms, a clarifying indicator ""mixed manifestations"" was introduced. A clarifying indicator for anxious distress has also been introduced. Removed grounds for exclusion for grief. 9(see below) Various phobia criteria are slightly adapted, and agoraphobia and panic are decoupled. Panic attacks can act as a clarifying indicator for other diagnoses. The diagnoses of separation anxiety disorder and selective mutism are no longer specific "childhood" diagnoses. 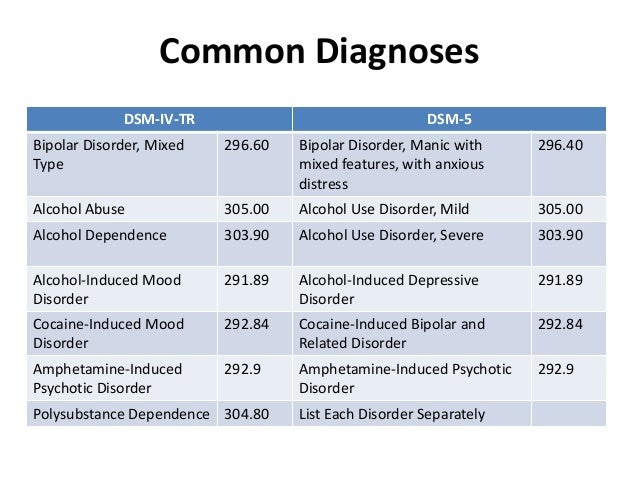 Also ruled out is the requirement to directly experience fear, horror, or feelings of helplessness. Avoidance and emotional flattening are separated, and at the same time, emotional flattening is added, incl. persistent depressed mood. Recklessness, (auto) destructive behavior, irritability and aggression are added to the already known symptoms of arousal. For children and adolescents in puberty, lower diagnostic thresholds are used. The adjustment disorder remained unchanged. Reactive attachment disorder has been moved to this chapter.
Also ruled out is the requirement to directly experience fear, horror, or feelings of helplessness. Avoidance and emotional flattening are separated, and at the same time, emotional flattening is added, incl. persistent depressed mood. Recklessness, (auto) destructive behavior, irritability and aggression are added to the already known symptoms of arousal. For children and adolescents in puberty, lower diagnostic thresholds are used. The adjustment disorder remained unchanged. Reactive attachment disorder has been moved to this chapter. 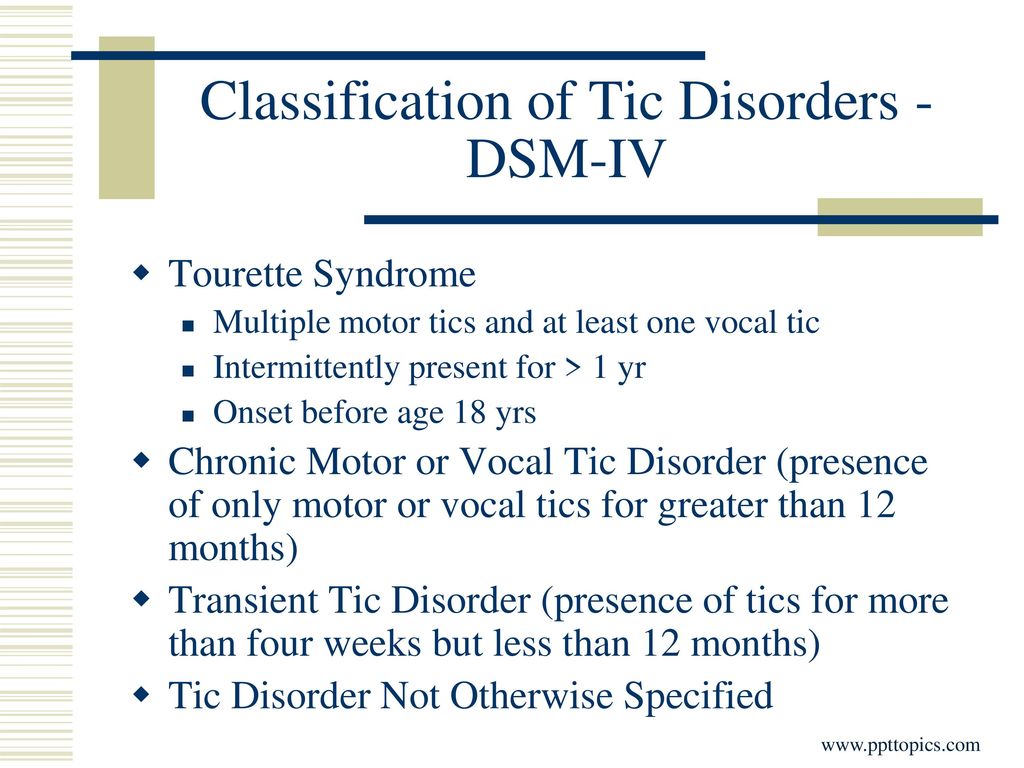 Removed somatization disorder, hypochondriasis, pain disorder, and unspecified somatoform disorder from DSM. A diagnosis of a "disorder with somatic symptoms" can be made on par with a diagnosis from another medical specialty only if the somatic symptoms are associated with abnormal thoughts, feelings, and behaviors. Unexplained medical symptoms play a decisive role only in false pregnancy and conversion (i.e. functional disorder with neurological symptoms). In other cases, positive symptoms should be sought in this group.
Removed somatization disorder, hypochondriasis, pain disorder, and unspecified somatoform disorder from DSM. A diagnosis of a "disorder with somatic symptoms" can be made on par with a diagnosis from another medical specialty only if the somatic symptoms are associated with abnormal thoughts, feelings, and behaviors. Unexplained medical symptoms play a decisive role only in false pregnancy and conversion (i.e. functional disorder with neurological symptoms). In other cases, positive symptoms should be sought in this group.  The chapter presents a large number of sleep disorders described in terms of physical characteristics in relation to circadian rhythms and respiratory disorders. This group includes Restless legs syndrome and REM Sleep Behavior Disorder. A large diagnostic choice predisposes to move away from the use of "unspecified" diagnoses.
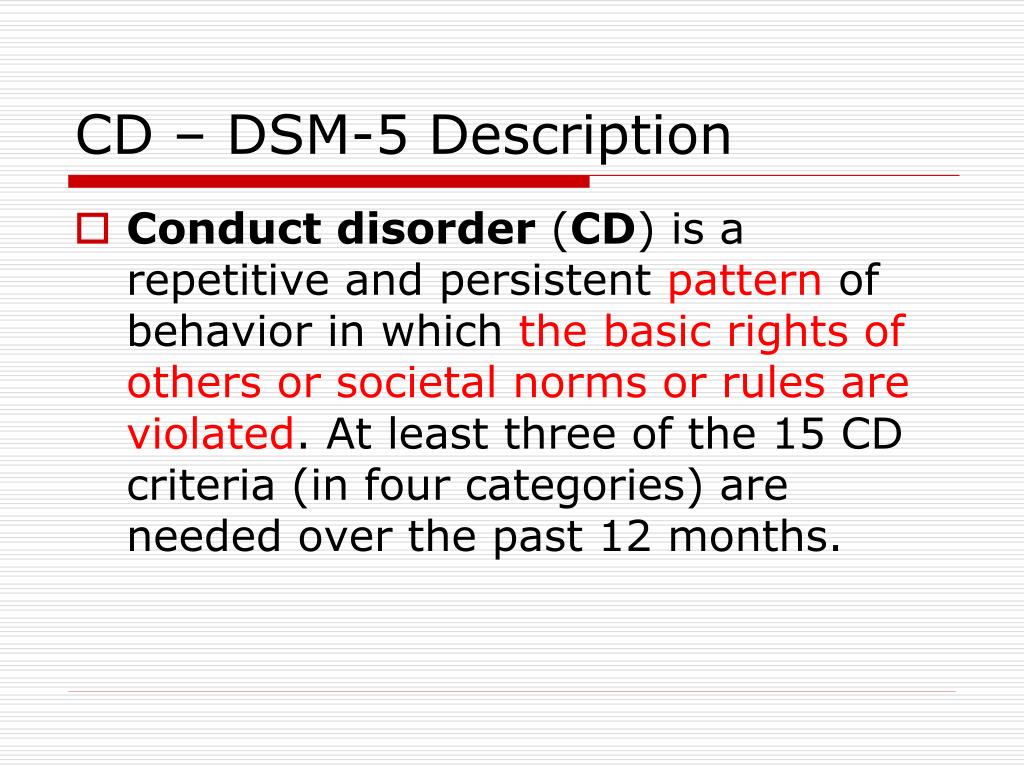
The chapter presents a large number of sleep disorders described in terms of physical characteristics in relation to circadian rhythms and respiratory disorders. This group includes Restless legs syndrome and REM Sleep Behavior Disorder. A large diagnostic choice predisposes to move away from the use of "unspecified" diagnoses.  In addition to a variety of impulse control disorders, antisocial personality disorder, dubbed from the chapter on personality disorders, also got here. The criteria for oppositional defiant disorder have been revised and weighted. In conduct disorder (Conduct Disorder), the grounds for excluding the diagnosis have been removed, but the clarifying indicator “callous-unemotional” has been added. Intermittent Explosive Disorder can now be verbal, and the rest of the criteria for this disorder are much more refined.
In addition to a variety of impulse control disorders, antisocial personality disorder, dubbed from the chapter on personality disorders, also got here. The criteria for oppositional defiant disorder have been revised and weighted. In conduct disorder (Conduct Disorder), the grounds for excluding the diagnosis have been removed, but the clarifying indicator “callous-unemotional” has been added. Intermittent Explosive Disorder can now be verbal, and the rest of the criteria for this disorder are much more refined.