Schizophrenia with multiple personality disorder
Dissociative Identity Disorder vs. Schizophrenia
Schizophrenia and DID are complex mental health conditions that people often confuse for one another. While they have some overlapping symptoms, they are different conditions.
A major difference is that someone with DID has two or more distinct identity states, sometimes known as alternate identities, or alters. This is not present in schizophrenia. DID was formerly known as multiple personality disorder or split personality disorder, but clinicians no longer use these terms.
The term “schizophrenia” is derived from the Greek words for “splitting” (schizo) and “mind” (phren), so some people have taken this to mean “split personality.” People with schizophrenia experience symptoms that affect their thoughts, behaviors, and feelings, but they don’t have multiple distinct personalities.
While there’s some overlap between the two conditions, DID and schizophrenia are different in many ways.
There are a lot of misconceptions surrounding both DID and schizophrenia. Many people inaccurately believe that people with schizophrenia have “split personalities.” This isn’t the case.
This isn’t even technically true of DID. The Sidran Institute says that, although these personalities may feel or appear different, “They’re all manifestations of a single, whole person.”
While some symptoms do overlap between DID and schizophrenia, they are different in important ways, including their causes, treatments, and age of onset.
Causes
Neither condition has one definitive cause, but DID is associated with trauma while schizophrenia is more often associated with having certain genes.
Most people with DID have a history of severe childhood trauma. An estimated 90% of people with DID have a history of neglect or abuse. The condition can arise when a child dissociates as a defense mechanism to escape an intolerable reality.
Experts believe several factors play a role in the development of schizophrenia. A main one is your genes. Your environment, brain development and chemicals, and pregnancy complications may also be involved.
Which treatments work better
The first-line treatment for schizophrenia is a second-generation antipsychotic medication. Healthcare professionals may recommend a few other types of medications as well.
Along with medication, treatments for schizophrenia often include:
- different types of psychotherapy (talk therapy)
- family support
- community-based treatment programs
On the other hand, DID doesn’t have an approved medication for treatment. People with DID may take meds to treat coexisting conditions — like antidepressants to improve symptoms of depression — but antipsychotics are unlikely to improve symptoms.
Talk therapy is the primary treatment for DID. Talk therapy helps the person to understand their symptoms and their causes, and to learn ways to manage dissociative episodes. Types include:
- cognitive behavioral therapy (CBT)
- dialectical behavioral therapy (DBT)
Age of onset
One of the major differences between DID and schizophrenia is the age when symptoms typically first begin showing up. Schizophrenia usually has a later onset — in someone’s late teens to 30s. DID symptoms, on the other hand, typically start showing up in childhood.
Schizophrenia usually has a later onset — in someone’s late teens to 30s. DID symptoms, on the other hand, typically start showing up in childhood.
According to research from 2009, dissociative symptoms usually start between ages 5 to 10 for people with DID. Someone’s first alter may appear around age 6.
Hearing voices
While people with either DID or schizophrenia may hear voices, people with DID who do are reportedly more likely to start hearing them before age 18.
People with schizophrenia don’t usually start having hallucinations until their late teens to early 20s.
Differences in “hearing voices”People with schizophrenia may experience auditory hallucinations, such as hearing voices. People with DID may hear voices too, with some differences. People with DID typically:
- begin hearing voices earlier in life
- hear more voices
- experience voices that “talk” to one another
- hear a combination of adult and child voices, whereas people with schizophrenia most often only hear adult voices
- report they would miss the voices
Prevalence
About 1% of adults around the world live with schizophrenia.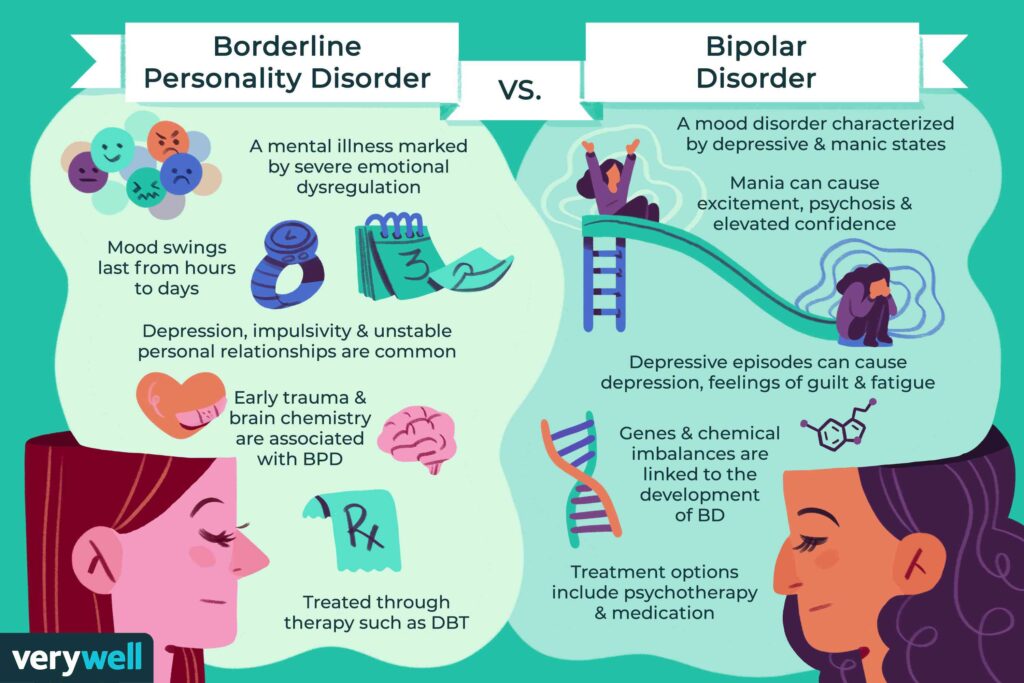 One study estimated that healthcare professionals diagnose schizophrenia in 5.1 per 1,000 people per year in the United States.
One study estimated that healthcare professionals diagnose schizophrenia in 5.1 per 1,000 people per year in the United States.
Worldwide, DID is diagnosed in about 1.5% of people. However, it’s often misdiagnosed, and some people may spend as much as 12 and a half years in treatment before they receive an accurate diagnosis.
Other notable differences
Memory loss, or amnesia, can occur in both schizophrenia and DID, but it’s more common in DID.
People with DID also have higher rates of derealization and depersonalization, according to research. For instance, if someone has “switched” to a different personality, they may look in the mirror and not recognize themselves.
People with schizophrenia may experience depersonalization and derealization, but this is less likely or happens less often.
Cognitive functioning issues and symptoms are often more common in schizophrenia than dissociative disorders.
There are a number of reasons why you might get DID and schizophrenia mixed up.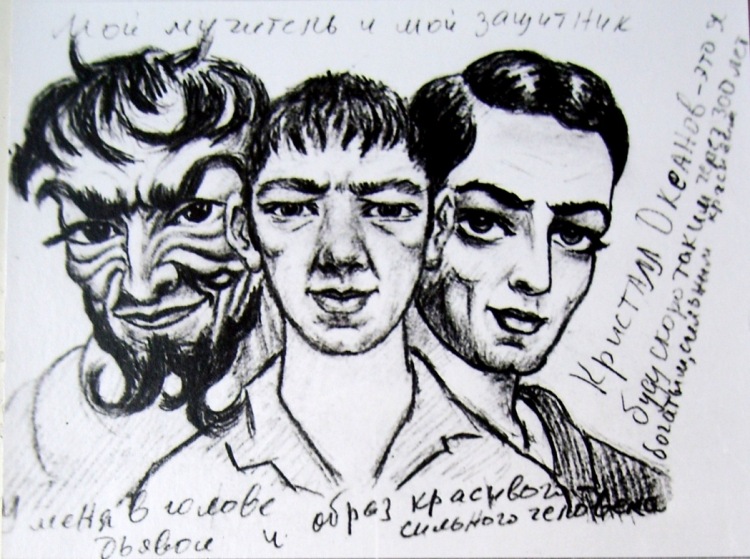
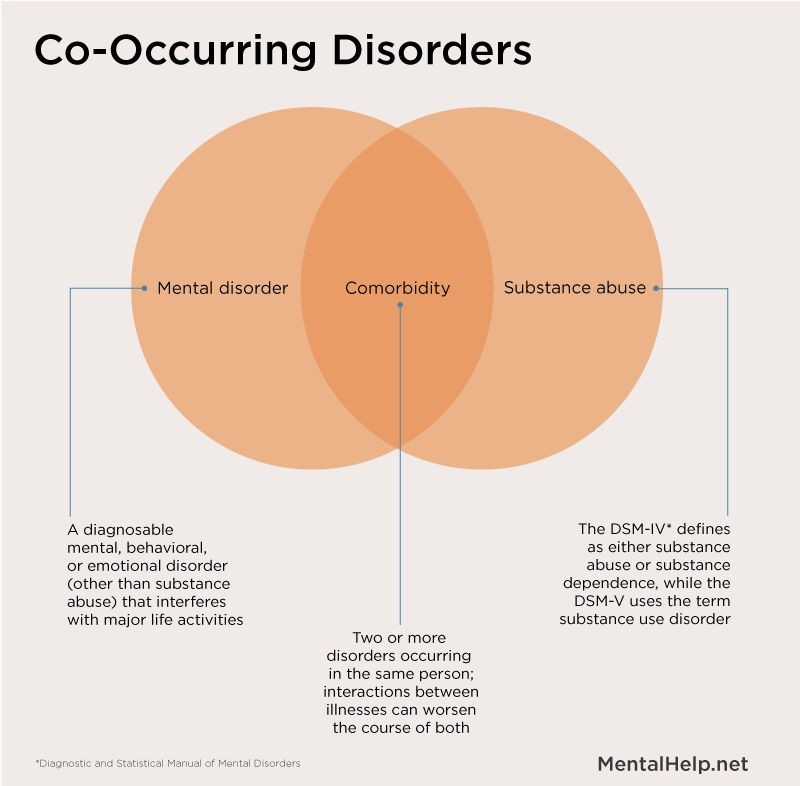
For starters, research has shown a high co-occurrence between dissociative disorders and schizophrenia spectrum disorders: Between 9% and 50% of people with schizophrenia also meet the criteria for a dissociative disorder.
They share some symptoms
One of the biggest reasons why people confuse the two conditions is their overlapping symptoms.
Popular culture portrayals may lead you to believe that hallucinations are unique to schizophrenia. However, people with DID, narcolepsy, and bipolar disorder, along with those who take certain substances, may also experience hallucinations.
Symptoms that DID and schizophrenia may have in common include:
- visual and auditory hallucinations
- issues with memory
- suicidal ideation
- difficulties sleeping
- delusions
- dissociation
Some of these symptoms are similar, so they may also be confused.
People with DID are typically more likely to have symptoms that overlap with positive symptoms of schizophrenia — the ones that involve altered perceptions, reality, and thinking. People with DID don’t often show many negative symptoms.
People with DID don’t often show many negative symptoms.
People with schizophrenia are less likely to experience dissociative symptoms. Those that do have them usually experienced some type of trauma.
DID is sometimes misdiagnosed
Healthcare professionals sometimes misdiagnose DID as schizophrenia.
It can be incredibly difficult to get a correct diagnosis of DID. According to research from 2016, only 60% of U.S. clinicians were able to accurately diagnose DID in an individual.
The clinicians misdiagnosed the condition as:
- post-traumatic stress disorder (PTSD)
- schizophrenia
- major depression
One reason for this confusion? Some clinicians might confuse someone’s belief that they have multiple identities with them experiencing delusions. The fact that both conditions can involve hearing voices and other overlapping symptoms can make diagnosis even more complex.
Other misdiagnosesThere are several conditions that can be confused with DID and schizophrenia, and possibly lead to misdiagnosis:
- borderline personality disorder
- bipolar disorder
- PTSD
- major depressive disorder
- schizoaffective disorder
- schizoid personality disorder
Multiple identities ≠ delusions or hallucinations
Some people confuse the multiple identities of DID for the delusions or hallucinations of schizophrenia, but they aren’t the same.
To break down the difference between these symptoms, let’s define them:
- Delusions. False beliefs that are not based in reality. If you have delusions, you believe them despite evidence to the contrary, even if everyone else believes otherwise. There are many types of delusions, including grandiose, bizarre, persecutory, and somatic (involving touch or sensation).
- Hallucinations. False perceptions — when someone sees, hears, or feels something that’s not actually happening. These sensory experiences feel real, but they’re not.
- Multiple identities. Also called alternate identities or “alters,” these occur when someone has more than one personality state. This alternate personality may appear to function separately from another. Alternate identities may have distinct behaviors, memories, expressions, languages, ages, and more. For instance, an alter of a 30-year-old female could be a 12-year-old male.
Coexisting conditions can complicate diagnosis
Other conditions that may simultaneously occur in people with DID and schizophrenia can complicate your symptoms and diagnosis.
People with DID, particularly, have comorbid conditions or symptoms, such as:
- PTSD
- depression
- anxiety disorders
- substance use disorder
- nonepileptic seizures
- self-harm
- a personality disorder
- eating disorders
- sleep disorders
Someone with schizophrenia may also experience:
- substance use disorder
- anxiety disorders, such as panic disorder
- obsessive-compulsive disorder (OCD)
- a personality disorder
Outdated diagnostic criteria
A lot of the confusion may also come from older diagnostic criteria. As we’ve learned more about mental health, the criteria have become more specific and clear.
Not that long ago, depersonalization was a big part of a schizophrenia diagnosis. Depersonalization is when you feel detached from yourself and your thoughts and feelings. It may feel like an “out of body” experience.
Neither condition has depersonalization listed as a necessity for diagnosis, but it’s now more commonly considered part of dissociative disorders. That said, some people with schizophrenia may still have it.
That said, some people with schizophrenia may still have it.
DID is a rare type of dissociative disorder. The main characteristic of DID is having two or more distinct personality states, also called alters or identities. People with DID may say they have more than one self in their mind or body.
The multiple identities are often distinct, with different names, mannerisms, and voices. They might have distinct histories and memories, ages, genders, sexualities, or interests. If you have DID, you might be aware of these identities or completely unaware.
Symptoms
Signs and symptoms of DID may include:
- two or more distinct personality states that affect behaviors, consciousness, memory, and more
- looking like you’re in a trance, blinking or rolling your eyes, or changing your posture when switching alters
- dissociative amnesia — big gaps in memory that are more than just forgetfulness
- dissociative fugue — losing your sense of awareness and engaging in some sort of travel away from home for a short or long period of time
- depersonalization and derealization — feeling detached or disconnected from yourself or the world
- behaviors of self-harm or suicide
- hallucinations, such as hearing voices
- sleep issues, such as insomnia or distressing dreams
For you to receive a DID diagnosis, these symptoms will affect your daily functioning and can’t be due to other causes, such as substance use or other medical conditions. However, someone with DID may use substances or have coexisting conditions.
However, someone with DID may use substances or have coexisting conditions.
In some cultures and religions, dissociation and possession or possession-like identities are an accepted norm, so dissociating in these ways wouldn’t be considered a disorder.
If you’re having thoughts of suicide or self-harm
Help is available right now.
- Call the National Suicide Prevention Lifeline anytime at 800-273-8255.
- Text “HOME” to the Crisis Text Line at 741741.
- Not in the U.S.? Find a helpline in your country with Befrienders Worldwide or the Suicide Stop International Help Center.
Causes and diagnosis
You may have a higher chance of developing DID if you experienced trauma or abuse as a child. Certain parenting styles, neglect, a lack of support or stability, and the ability to dissociate easily are also factors.
While it can be challenging to get accurately diagnosed with DID, reaching out to a mental health professional can be a positive first step.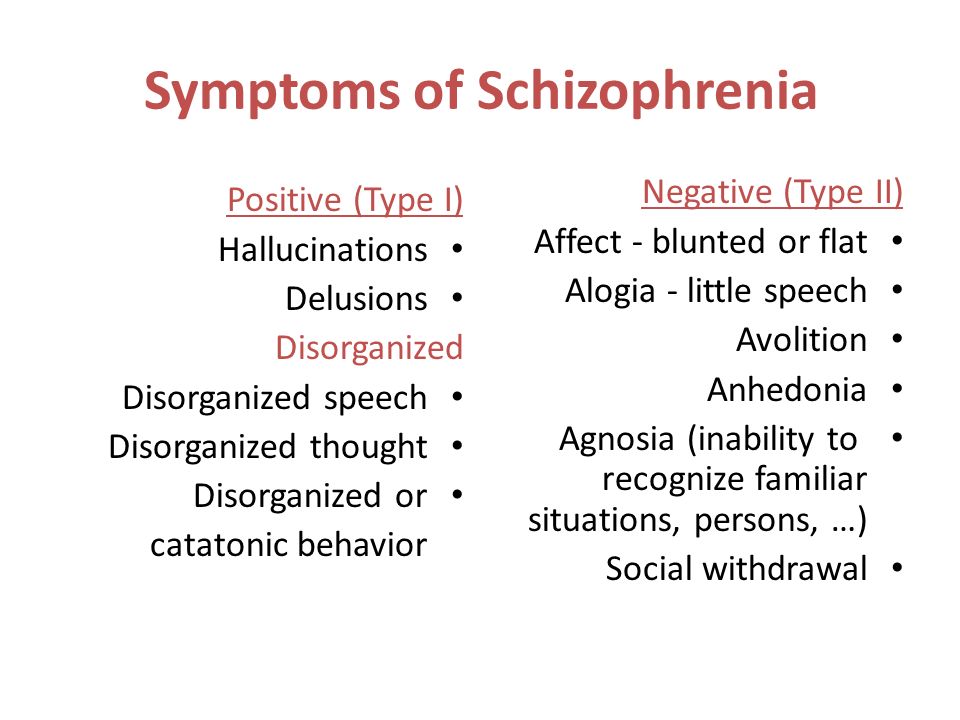 They’ll likely ask you questions about your symptoms, health history, and how you’re functioning in your day to day.
They’ll likely ask you questions about your symptoms, health history, and how you’re functioning in your day to day.
They might also use one of these evaluation tools:
- Dissociative Experiences Scale
- Dissociation Questionnaire
- Difficulties in Emotion Regulation Scale (DERS)
Treatments
While it can be a long road, treatments like talk therapy make managing and living well with DID possible. Everyone’s treatment plan will be personalized, but DID treatments typically involve:
- psychotherapy
- hypnosis
- eye movement desensitization and reprocessing (EMDR)
- coping tools to help regulate emotions, manage stress, and improve daily functioning
While no medications exist that treat DID specifically, healthcare professionals may prescribe meds to treat related symptoms or coexisting conditions.
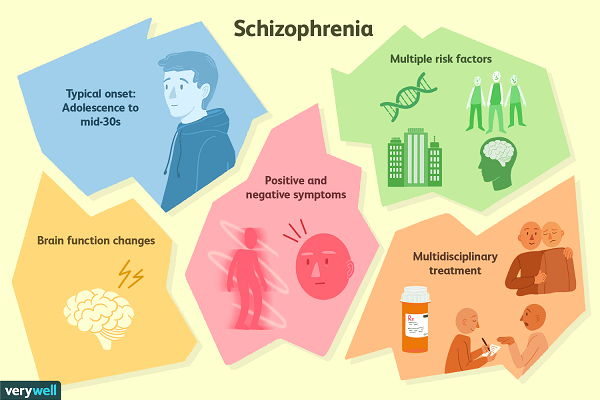
Schizophrenia is a mental health condition that affects your thoughts, behaviors, and feelings. People often feel as if they’ve lost touch with reality, usually due to hallucinations and delusions. These are some of the most well-known symptoms of schizophrenia.
These are some of the most well-known symptoms of schizophrenia.
Schizophrenia onset usually happens in your teens to 30s. This is when someone has their first episode or starts showing prominent signs. Onset tends to occur earlier in males than females.
Symptoms
Healthcare professionals often break down the symptoms of schizophrenia into three categories: positive, negative, and cognitive symptoms.
Positive symptoms involve altered perceptions or thinking. You might experience:
- delusions
- hallucinations
- disorganized thinking
- unusual body movements, such as in catatonia
- suicidal thoughts or behaviors
Negative symptoms can be considered the absence of something, such as motivation or emotional expressions. These might look like:
- low motivation
- difficulty planning or following through with activities
- flat affect — a lack of emotional expression
- speaking less
- taking less pleasure in daily life
- social withdrawal
Cognitive symptoms are those that affect your memory or attention. These symptoms can be subtle or noticeable, depending on the person. Some examples include:
These symptoms can be subtle or noticeable, depending on the person. Some examples include:
- trouble making decisions
- having a hard time paying attention or focusing
- difficulty using information that you’ve just learned
Causes and diagnosis
A number of factors may contribute to developing schizophrenia. They include:
- genetics
- environment
- brain structure and function
- changes or differences in neurotransmitters
- social stressors
If you have schizophrenia, you might have received your first evaluation for the condition after experiencing your first episode of schizophrenia or psychosis. In many people, this first episode is severe enough to warrant seeking medical help or hospitalization.
According to the DSM-5, someone must meet the below criteria to receive a diagnosis of schizophrenia:
- two or more positive or negative symptoms most of the time during a 1-month period
- daily ability to function is extremely affected
- continuous signs of issues must occur for at least 6 months
- other mental health conditions or substance use aren’t causing the symptoms
A mental health professional will often talk with you about your health history and symptoms. They may try to rule out other conditions that may be causing your symptoms. To do this, they might give you mental health assessments and physical tests.
They may try to rule out other conditions that may be causing your symptoms. To do this, they might give you mental health assessments and physical tests.
Treatments
There are many tools and treatments available to help you if you’re living with schizophrenia.
Treatment plans often involve a combo of:
- medications, specifically antipsychotics
- psychotherapy
- family education, support, and therapy
- coordinated specialty care (CSC), a treatment program aimed at recovery from your first episode of psychosis
- assertive community treatment, a multidisciplinary team aimed to decrease hospitalizations and homelessness
- coping tools
DID and schizophrenia are two mental health conditions that may be confused for each other, but they aren’t the same. It’s also possible to have both conditions at once or other overlapping conditions that make diagnosis difficult.
If you think you’re experiencing symptoms of these or another condition, consider reaching out to a mental health professional for an evaluation. If you’ve already received a diagnosis of DID or schizophrenia but don’t think it’s the right one, consider getting a second opinion.
If you’ve already received a diagnosis of DID or schizophrenia but don’t think it’s the right one, consider getting a second opinion.
Whether you have schizophrenia, DID, or another condition altogether, you can thrive with the right coping tools, treatments, and support.
If you’re looking for peer support, you can try the Connection Group or Family Support Group from the National Alliance on Mental Illness (NAMI).
Here are additional resources for DID:
- International Society for the Study of Trauma and Dissociation: Find a Therapist
- Sidran Institute: Help Desk
Here are additional resources for schizophrenia:
- Schizophrenia & Psychosis Action Alliance: Peer Support Groups
- National Institute of Mental Health (NIMH): RAISE Resources (Recovery After an Initial Schizophrenia Episode)
- Read more about the best online schizophrenia support groups.
Dissociative Identity Disorder vs. Schizophrenia
Schizophrenia and DID are complex mental health conditions that people often confuse for one another. While they have some overlapping symptoms, they are different conditions.
While they have some overlapping symptoms, they are different conditions.
A major difference is that someone with DID has two or more distinct identity states, sometimes known as alternate identities, or alters. This is not present in schizophrenia. DID was formerly known as multiple personality disorder or split personality disorder, but clinicians no longer use these terms.
The term “schizophrenia” is derived from the Greek words for “splitting” (schizo) and “mind” (phren), so some people have taken this to mean “split personality.” People with schizophrenia experience symptoms that affect their thoughts, behaviors, and feelings, but they don’t have multiple distinct personalities.
While there’s some overlap between the two conditions, DID and schizophrenia are different in many ways.
There are a lot of misconceptions surrounding both DID and schizophrenia. Many people inaccurately believe that people with schizophrenia have “split personalities.” This isn’t the case.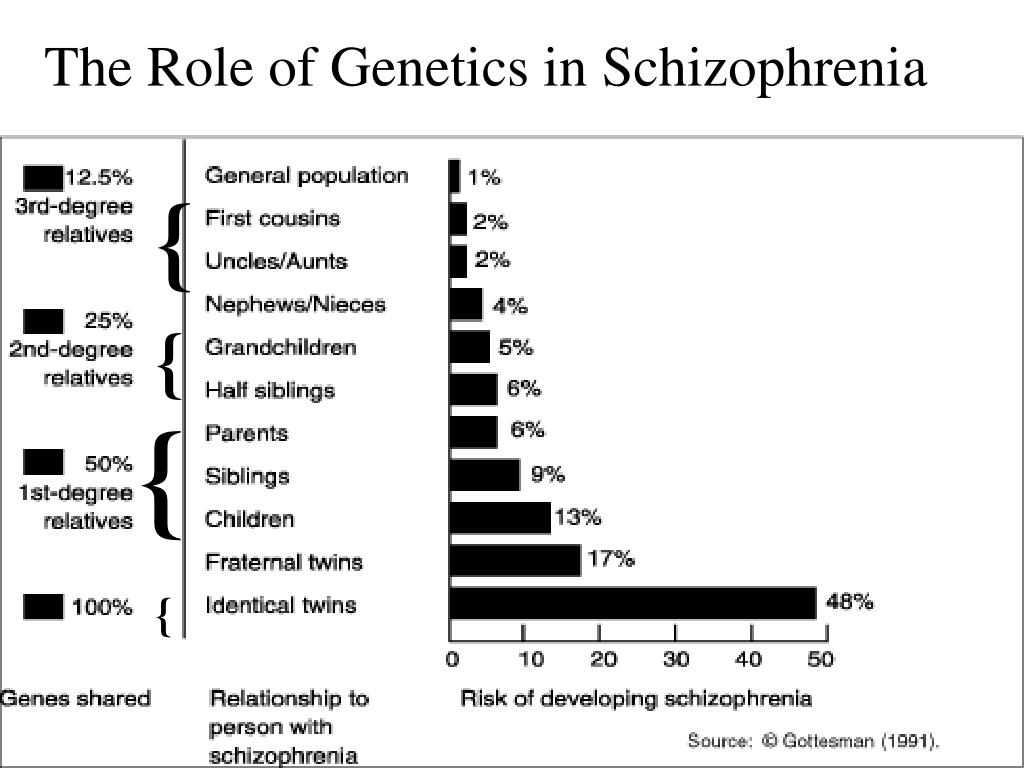
This isn’t even technically true of DID. The Sidran Institute says that, although these personalities may feel or appear different, “They’re all manifestations of a single, whole person.”
While some symptoms do overlap between DID and schizophrenia, they are different in important ways, including their causes, treatments, and age of onset.
Causes
Neither condition has one definitive cause, but DID is associated with trauma while schizophrenia is more often associated with having certain genes.
Most people with DID have a history of severe childhood trauma. An estimated 90% of people with DID have a history of neglect or abuse. The condition can arise when a child dissociates as a defense mechanism to escape an intolerable reality.
Experts believe several factors play a role in the development of schizophrenia. A main one is your genes. Your environment, brain development and chemicals, and pregnancy complications may also be involved.
Which treatments work better
The first-line treatment for schizophrenia is a second-generation antipsychotic medication.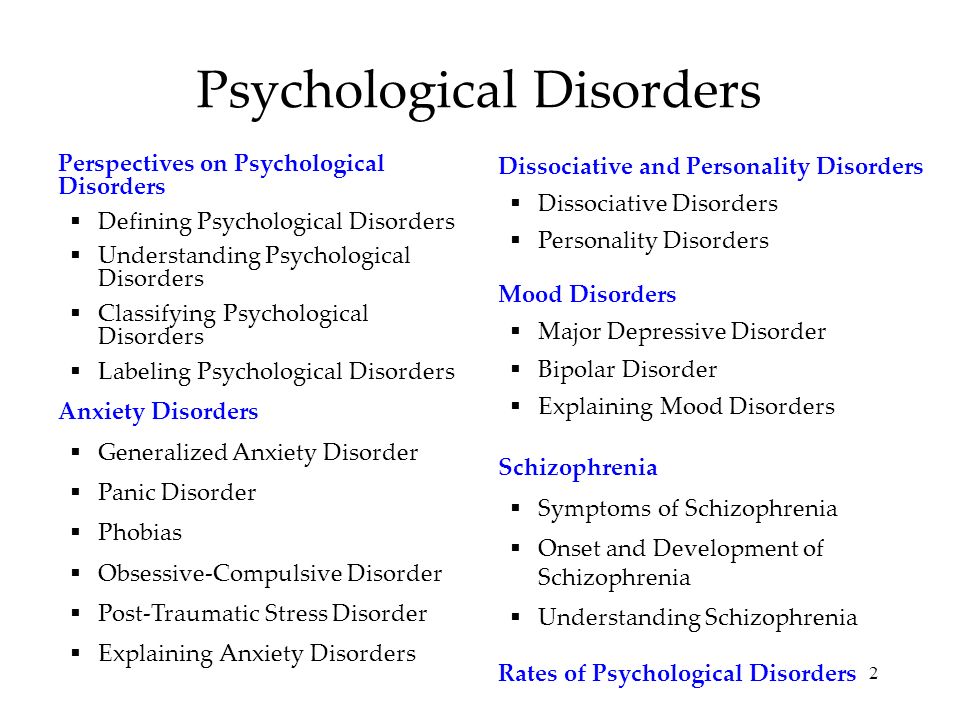 Healthcare professionals may recommend a few other types of medications as well.
Healthcare professionals may recommend a few other types of medications as well.
Along with medication, treatments for schizophrenia often include:
- different types of psychotherapy (talk therapy)
- family support
- community-based treatment programs
On the other hand, DID doesn’t have an approved medication for treatment. People with DID may take meds to treat coexisting conditions — like antidepressants to improve symptoms of depression — but antipsychotics are unlikely to improve symptoms.
Talk therapy is the primary treatment for DID. Talk therapy helps the person to understand their symptoms and their causes, and to learn ways to manage dissociative episodes. Types include:
- cognitive behavioral therapy (CBT)
- dialectical behavioral therapy (DBT)
Age of onset
One of the major differences between DID and schizophrenia is the age when symptoms typically first begin showing up. Schizophrenia usually has a later onset — in someone’s late teens to 30s. DID symptoms, on the other hand, typically start showing up in childhood.
DID symptoms, on the other hand, typically start showing up in childhood.
According to research from 2009, dissociative symptoms usually start between ages 5 to 10 for people with DID. Someone’s first alter may appear around age 6.
Hearing voices
While people with either DID or schizophrenia may hear voices, people with DID who do are reportedly more likely to start hearing them before age 18.
People with schizophrenia don’t usually start having hallucinations until their late teens to early 20s.
Differences in “hearing voices”People with schizophrenia may experience auditory hallucinations, such as hearing voices. People with DID may hear voices too, with some differences. People with DID typically:
- begin hearing voices earlier in life
- hear more voices
- experience voices that “talk” to one another
- hear a combination of adult and child voices, whereas people with schizophrenia most often only hear adult voices
- report they would miss the voices
Prevalence
About 1% of adults around the world live with schizophrenia.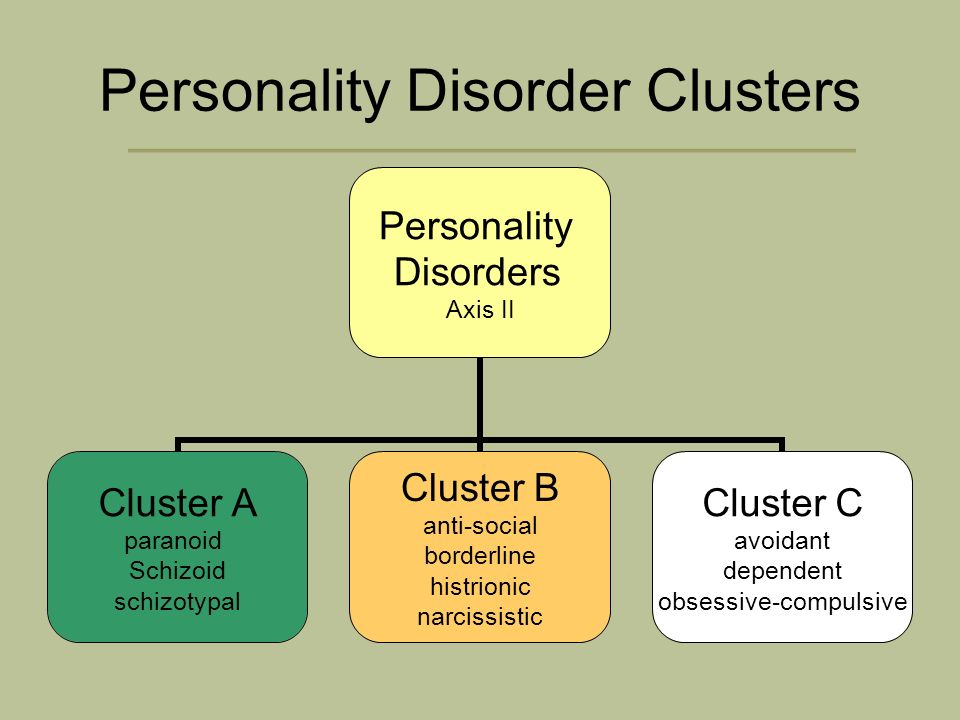 One study estimated that healthcare professionals diagnose schizophrenia in 5.1 per 1,000 people per year in the United States.
One study estimated that healthcare professionals diagnose schizophrenia in 5.1 per 1,000 people per year in the United States.
Worldwide, DID is diagnosed in about 1.5% of people. However, it’s often misdiagnosed, and some people may spend as much as 12 and a half years in treatment before they receive an accurate diagnosis.
Other notable differences
Memory loss, or amnesia, can occur in both schizophrenia and DID, but it’s more common in DID.
People with DID also have higher rates of derealization and depersonalization, according to research. For instance, if someone has “switched” to a different personality, they may look in the mirror and not recognize themselves.
People with schizophrenia may experience depersonalization and derealization, but this is less likely or happens less often.
Cognitive functioning issues and symptoms are often more common in schizophrenia than dissociative disorders.
There are a number of reasons why you might get DID and schizophrenia mixed up.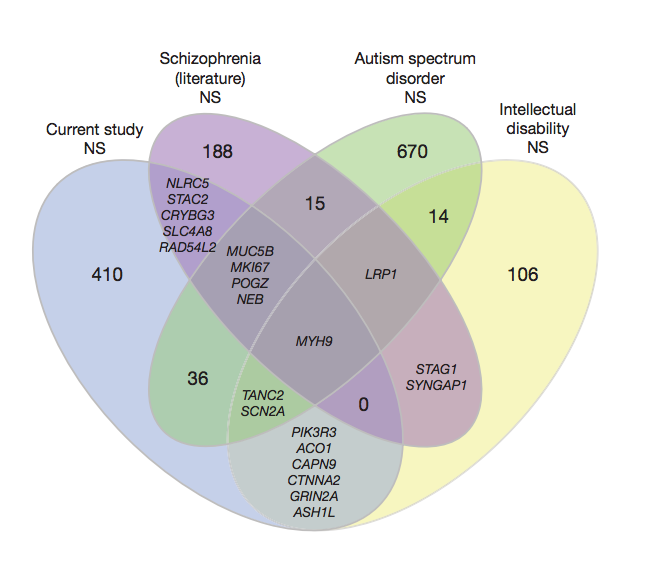
For starters, research has shown a high co-occurrence between dissociative disorders and schizophrenia spectrum disorders: Between 9% and 50% of people with schizophrenia also meet the criteria for a dissociative disorder.
They share some symptoms
One of the biggest reasons why people confuse the two conditions is their overlapping symptoms.
Popular culture portrayals may lead you to believe that hallucinations are unique to schizophrenia. However, people with DID, narcolepsy, and bipolar disorder, along with those who take certain substances, may also experience hallucinations.
Symptoms that DID and schizophrenia may have in common include:
- visual and auditory hallucinations
- issues with memory
- suicidal ideation
- difficulties sleeping
- delusions
- dissociation
Some of these symptoms are similar, so they may also be confused.
People with DID are typically more likely to have symptoms that overlap with positive symptoms of schizophrenia — the ones that involve altered perceptions, reality, and thinking. People with DID don’t often show many negative symptoms.
People with DID don’t often show many negative symptoms.
People with schizophrenia are less likely to experience dissociative symptoms. Those that do have them usually experienced some type of trauma.
DID is sometimes misdiagnosed
Healthcare professionals sometimes misdiagnose DID as schizophrenia.
It can be incredibly difficult to get a correct diagnosis of DID. According to research from 2016, only 60% of U.S. clinicians were able to accurately diagnose DID in an individual.
The clinicians misdiagnosed the condition as:
- post-traumatic stress disorder (PTSD)
- schizophrenia
- major depression
One reason for this confusion? Some clinicians might confuse someone’s belief that they have multiple identities with them experiencing delusions. The fact that both conditions can involve hearing voices and other overlapping symptoms can make diagnosis even more complex.
Other misdiagnosesThere are several conditions that can be confused with DID and schizophrenia, and possibly lead to misdiagnosis:
- borderline personality disorder
- bipolar disorder
- PTSD
- major depressive disorder
- schizoaffective disorder
- schizoid personality disorder
Multiple identities ≠ delusions or hallucinations
Some people confuse the multiple identities of DID for the delusions or hallucinations of schizophrenia, but they aren’t the same.
To break down the difference between these symptoms, let’s define them:
- Delusions. False beliefs that are not based in reality. If you have delusions, you believe them despite evidence to the contrary, even if everyone else believes otherwise. There are many types of delusions, including grandiose, bizarre, persecutory, and somatic (involving touch or sensation).
- Hallucinations. False perceptions — when someone sees, hears, or feels something that’s not actually happening. These sensory experiences feel real, but they’re not.
- Multiple identities. Also called alternate identities or “alters,” these occur when someone has more than one personality state. This alternate personality may appear to function separately from another. Alternate identities may have distinct behaviors, memories, expressions, languages, ages, and more. For instance, an alter of a 30-year-old female could be a 12-year-old male.
Coexisting conditions can complicate diagnosis
Other conditions that may simultaneously occur in people with DID and schizophrenia can complicate your symptoms and diagnosis.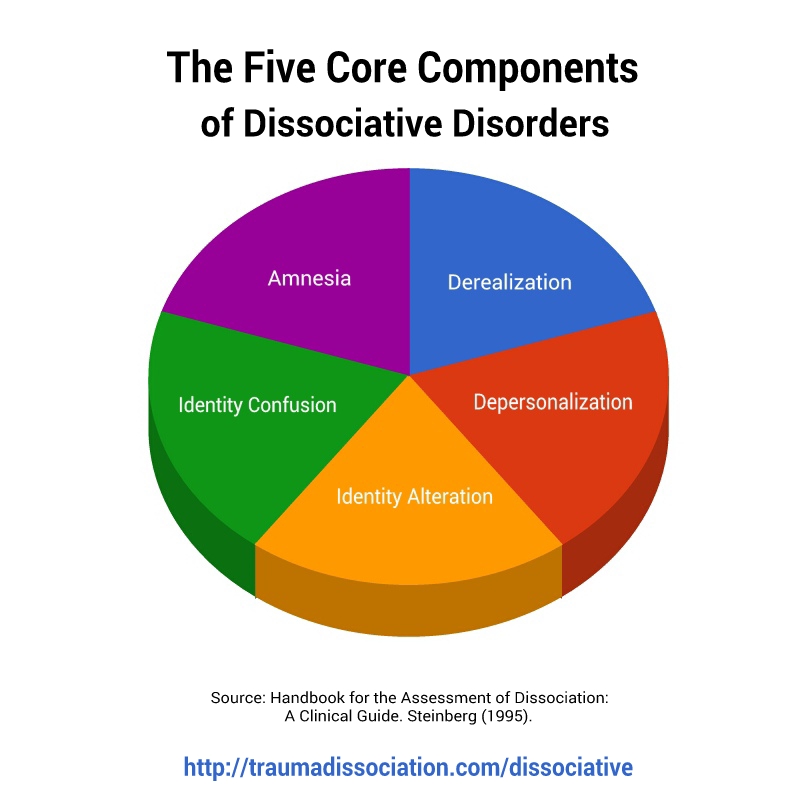
People with DID, particularly, have comorbid conditions or symptoms, such as:
- PTSD
- depression
- anxiety disorders
- substance use disorder
- nonepileptic seizures
- self-harm
- a personality disorder
- eating disorders
- sleep disorders
Someone with schizophrenia may also experience:
- substance use disorder
- anxiety disorders, such as panic disorder
- obsessive-compulsive disorder (OCD)
- a personality disorder
Outdated diagnostic criteria
A lot of the confusion may also come from older diagnostic criteria. As we’ve learned more about mental health, the criteria have become more specific and clear.
Not that long ago, depersonalization was a big part of a schizophrenia diagnosis. Depersonalization is when you feel detached from yourself and your thoughts and feelings. It may feel like an “out of body” experience.
Neither condition has depersonalization listed as a necessity for diagnosis, but it’s now more commonly considered part of dissociative disorders. That said, some people with schizophrenia may still have it.
That said, some people with schizophrenia may still have it.
DID is a rare type of dissociative disorder. The main characteristic of DID is having two or more distinct personality states, also called alters or identities. People with DID may say they have more than one self in their mind or body.
The multiple identities are often distinct, with different names, mannerisms, and voices. They might have distinct histories and memories, ages, genders, sexualities, or interests. If you have DID, you might be aware of these identities or completely unaware.
Symptoms
Signs and symptoms of DID may include:
- two or more distinct personality states that affect behaviors, consciousness, memory, and more
- looking like you’re in a trance, blinking or rolling your eyes, or changing your posture when switching alters
- dissociative amnesia — big gaps in memory that are more than just forgetfulness
- dissociative fugue — losing your sense of awareness and engaging in some sort of travel away from home for a short or long period of time
- depersonalization and derealization — feeling detached or disconnected from yourself or the world
- behaviors of self-harm or suicide
- hallucinations, such as hearing voices
- sleep issues, such as insomnia or distressing dreams
For you to receive a DID diagnosis, these symptoms will affect your daily functioning and can’t be due to other causes, such as substance use or other medical conditions.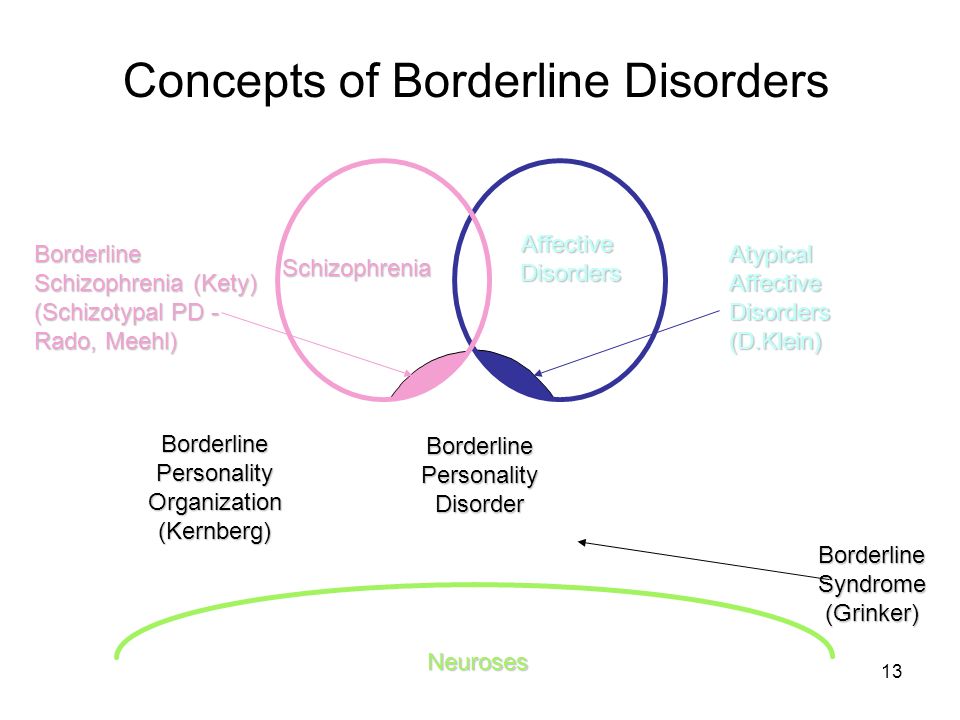 However, someone with DID may use substances or have coexisting conditions.
However, someone with DID may use substances or have coexisting conditions.
In some cultures and religions, dissociation and possession or possession-like identities are an accepted norm, so dissociating in these ways wouldn’t be considered a disorder.
If you’re having thoughts of suicide or self-harm
Help is available right now.
- Call the National Suicide Prevention Lifeline anytime at 800-273-8255.
- Text “HOME” to the Crisis Text Line at 741741.
- Not in the U.S.? Find a helpline in your country with Befrienders Worldwide or the Suicide Stop International Help Center.
Causes and diagnosis
You may have a higher chance of developing DID if you experienced trauma or abuse as a child. Certain parenting styles, neglect, a lack of support or stability, and the ability to dissociate easily are also factors.
While it can be challenging to get accurately diagnosed with DID, reaching out to a mental health professional can be a positive first step. They’ll likely ask you questions about your symptoms, health history, and how you’re functioning in your day to day.
They’ll likely ask you questions about your symptoms, health history, and how you’re functioning in your day to day.
They might also use one of these evaluation tools:
- Dissociative Experiences Scale
- Dissociation Questionnaire
- Difficulties in Emotion Regulation Scale (DERS)
Treatments
While it can be a long road, treatments like talk therapy make managing and living well with DID possible. Everyone’s treatment plan will be personalized, but DID treatments typically involve:
- psychotherapy
- hypnosis
- eye movement desensitization and reprocessing (EMDR)
- coping tools to help regulate emotions, manage stress, and improve daily functioning
While no medications exist that treat DID specifically, healthcare professionals may prescribe meds to treat related symptoms or coexisting conditions.
Schizophrenia is a mental health condition that affects your thoughts, behaviors, and feelings. People often feel as if they’ve lost touch with reality, usually due to hallucinations and delusions.![]() These are some of the most well-known symptoms of schizophrenia.
These are some of the most well-known symptoms of schizophrenia.
Schizophrenia onset usually happens in your teens to 30s. This is when someone has their first episode or starts showing prominent signs. Onset tends to occur earlier in males than females.
Symptoms
Healthcare professionals often break down the symptoms of schizophrenia into three categories: positive, negative, and cognitive symptoms.
Positive symptoms involve altered perceptions or thinking. You might experience:
- delusions
- hallucinations
- disorganized thinking
- unusual body movements, such as in catatonia
- suicidal thoughts or behaviors
Negative symptoms can be considered the absence of something, such as motivation or emotional expressions. These might look like:
- low motivation
- difficulty planning or following through with activities
- flat affect — a lack of emotional expression
- speaking less
- taking less pleasure in daily life
- social withdrawal
Cognitive symptoms are those that affect your memory or attention.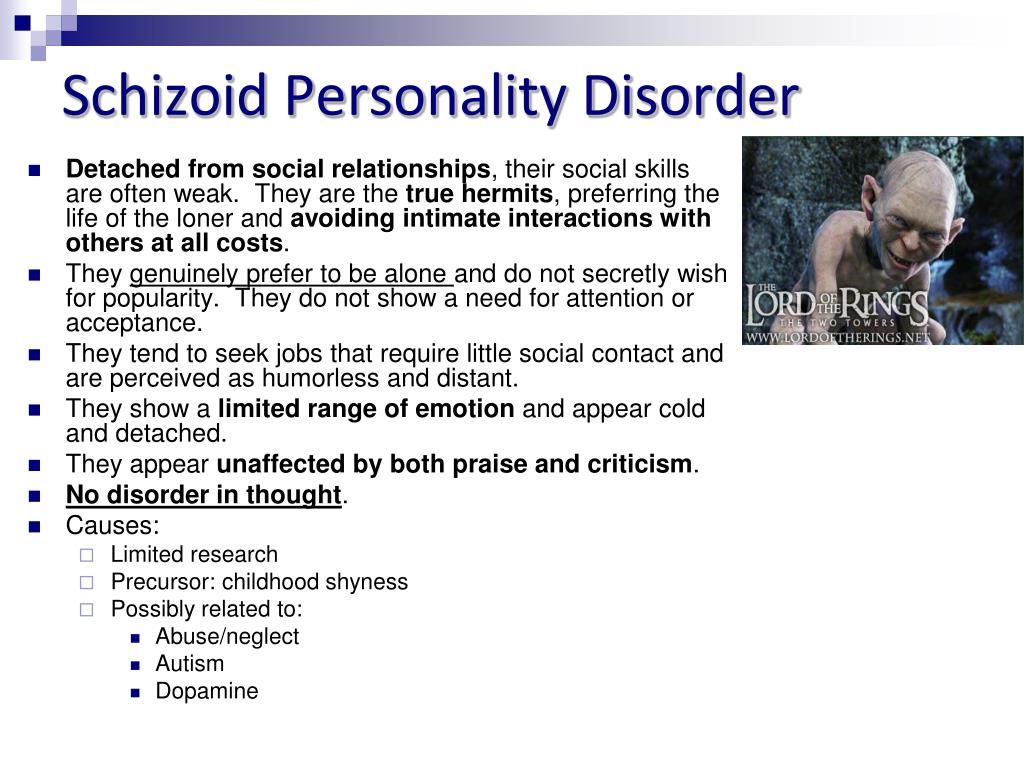 These symptoms can be subtle or noticeable, depending on the person. Some examples include:
These symptoms can be subtle or noticeable, depending on the person. Some examples include:
- trouble making decisions
- having a hard time paying attention or focusing
- difficulty using information that you’ve just learned
Causes and diagnosis
A number of factors may contribute to developing schizophrenia. They include:
- genetics
- environment
- brain structure and function
- changes or differences in neurotransmitters
- social stressors
If you have schizophrenia, you might have received your first evaluation for the condition after experiencing your first episode of schizophrenia or psychosis. In many people, this first episode is severe enough to warrant seeking medical help or hospitalization.
According to the DSM-5, someone must meet the below criteria to receive a diagnosis of schizophrenia:
- two or more positive or negative symptoms most of the time during a 1-month period
- daily ability to function is extremely affected
- continuous signs of issues must occur for at least 6 months
- other mental health conditions or substance use aren’t causing the symptoms
A mental health professional will often talk with you about your health history and symptoms. They may try to rule out other conditions that may be causing your symptoms. To do this, they might give you mental health assessments and physical tests.
They may try to rule out other conditions that may be causing your symptoms. To do this, they might give you mental health assessments and physical tests.
Treatments
There are many tools and treatments available to help you if you’re living with schizophrenia.
Treatment plans often involve a combo of:
- medications, specifically antipsychotics
- psychotherapy
- family education, support, and therapy
- coordinated specialty care (CSC), a treatment program aimed at recovery from your first episode of psychosis
- assertive community treatment, a multidisciplinary team aimed to decrease hospitalizations and homelessness
- coping tools
DID and schizophrenia are two mental health conditions that may be confused for each other, but they aren’t the same. It’s also possible to have both conditions at once or other overlapping conditions that make diagnosis difficult.
If you think you’re experiencing symptoms of these or another condition, consider reaching out to a mental health professional for an evaluation.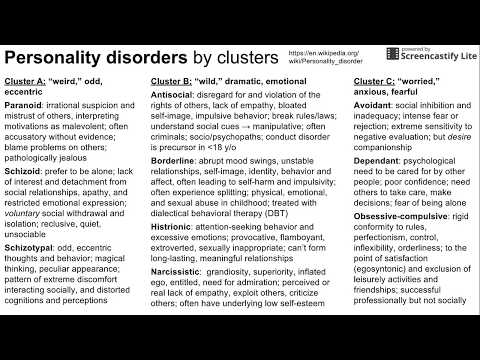 If you’ve already received a diagnosis of DID or schizophrenia but don’t think it’s the right one, consider getting a second opinion.
If you’ve already received a diagnosis of DID or schizophrenia but don’t think it’s the right one, consider getting a second opinion.
Whether you have schizophrenia, DID, or another condition altogether, you can thrive with the right coping tools, treatments, and support.
If you’re looking for peer support, you can try the Connection Group or Family Support Group from the National Alliance on Mental Illness (NAMI).
Here are additional resources for DID:
- International Society for the Study of Trauma and Dissociation: Find a Therapist
- Sidran Institute: Help Desk
Here are additional resources for schizophrenia:
- Schizophrenia & Psychosis Action Alliance: Peer Support Groups
- National Institute of Mental Health (NIMH): RAISE Resources (Recovery After an Initial Schizophrenia Episode)
- Read more about the best online schizophrenia support groups.
Split personality - is it schizophrenia or another disease?
Mental illnesses have similar symptoms and are often confused. For this reason, each of them requires differential diagnosis. However, split personality and schizophrenia have a slightly different fate. They are not just confused, but identified, taking for the same disorder. In fact, these are two completely different diseases. Consider both to understand what is the difference between them and whether there is a similarity.
For this reason, each of them requires differential diagnosis. However, split personality and schizophrenia have a slightly different fate. They are not just confused, but identified, taking for the same disorder. In fact, these are two completely different diseases. Consider both to understand what is the difference between them and whether there is a similarity.
In this article
- Reason for confusion
- Dissociative identity disorder
- Causes
- Symptoms
- ICD-10 entry
- Treatment
- About schizophrenia
- Output
Cause of confusion
First, let's try to figure out why two different diseases began to be perceived as one. This is mainly due to the etymology of the word "schizophrenia". From Greek, it literally translates as “split” or “split” “mind”, “thinking” or “thought”. This causes confusion among people who do not understand medicine and psychiatry.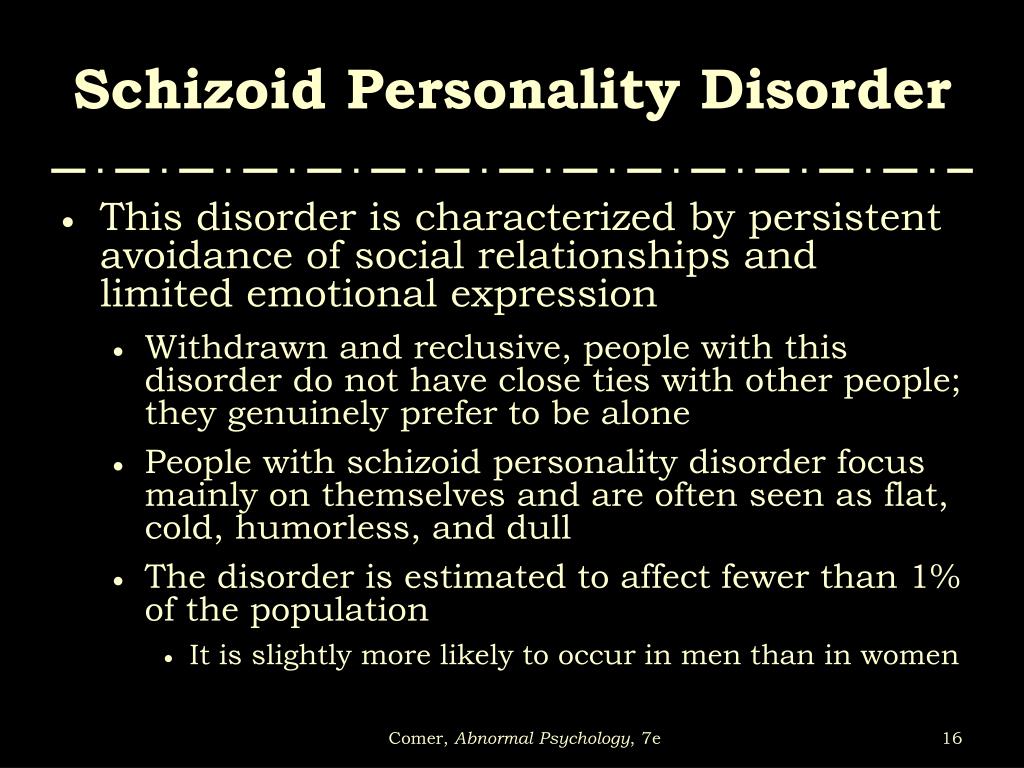
But for an experienced doctor, it is not so difficult to differentiate these diagnoses. In short, with a split personality, a person seems to have several people in one body. In schizophrenia, there is no such split or split; the patient simply inadequately evaluates himself and the surrounding reality. The differences between these diseases will be more obvious if we consider their signs. Let's start with split personality.
Dissociative identity disorder
Multiple personality disorder is the common name for the mental illness "dissociative identity disorder". The phrase "multiple personality disorder" is also sometimes used, in which a split personality occurs, resulting in the impression that several people live in one body. Periodically there is a switch from one personality to another. Moreover, each of them can be strikingly different from the first one in terms of such parameters as gender, age, education, profession, etc. After switching, one person may not remember what the other person replacing her was doing.
After switching, one person may not remember what the other person replacing her was doing.
This disease is very rare. It is included in the International Classification of Diseases, but not in all countries doctors agree to recognize it as a pathology. Disputes over its origin have been going on for more than one century, but scientists have not come to a common denominator.
For the first time, a dissociative disorder, or rather a description of the condition that we today call an identity disorder, is found in the writings of Paracelsus. He described a woman who complained that she was sometimes robbed. Observations showed that she herself spends her money, she just does not remember it after shopping, because she does not consciously participate in the process.
A split personality is rare, but interest in the disease is very high, including from people who are not related to medicine. This is due to the promotion of this topic in literature and cinema.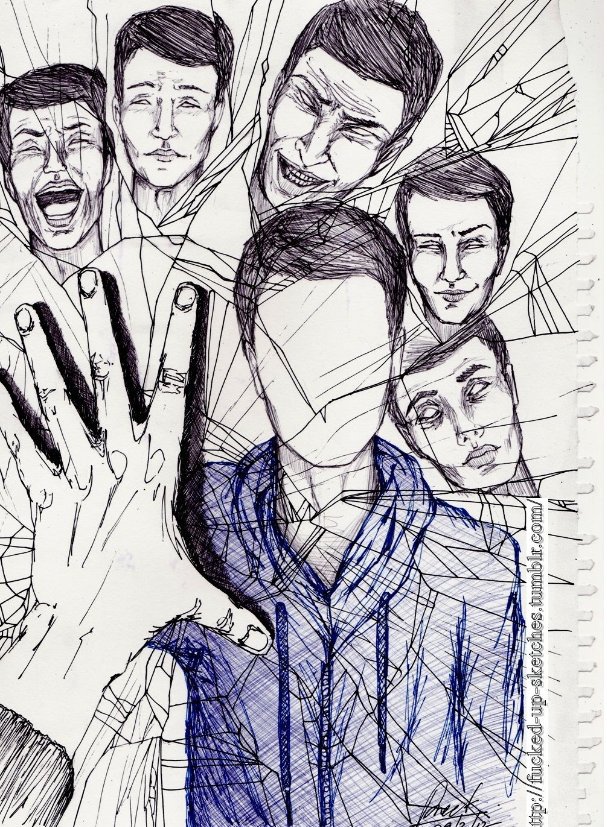 One of the most famous patients with this diagnosis is Billy Milligan. In his body, 24 personalities coexisted at once, 10 of which were the main ones.
One of the most famous patients with this diagnosis is Billy Milligan. In his body, 24 personalities coexisted at once, 10 of which were the main ones.
Some experts believe that psychiatrists artificially increase interest in this topic in order to attract new clients and make money. It is doubtful that people with this disorder often have criminal experience. When it comes to sanity, it is more profitable for them to be “crazy” than ordinary criminals who can be imprisoned for life or even sentenced to death. The same Milligan was accused of theft, robbery and rape, for which he could pay with freedom or life.
In 1981 Daniel Keyes published The Many Minds of Billy Milligan, a bestseller and translated into 14 languages.
However, most scientists still believe that dissociative identity disorder does occur, and is a very complex mental illness that leads to a split personality.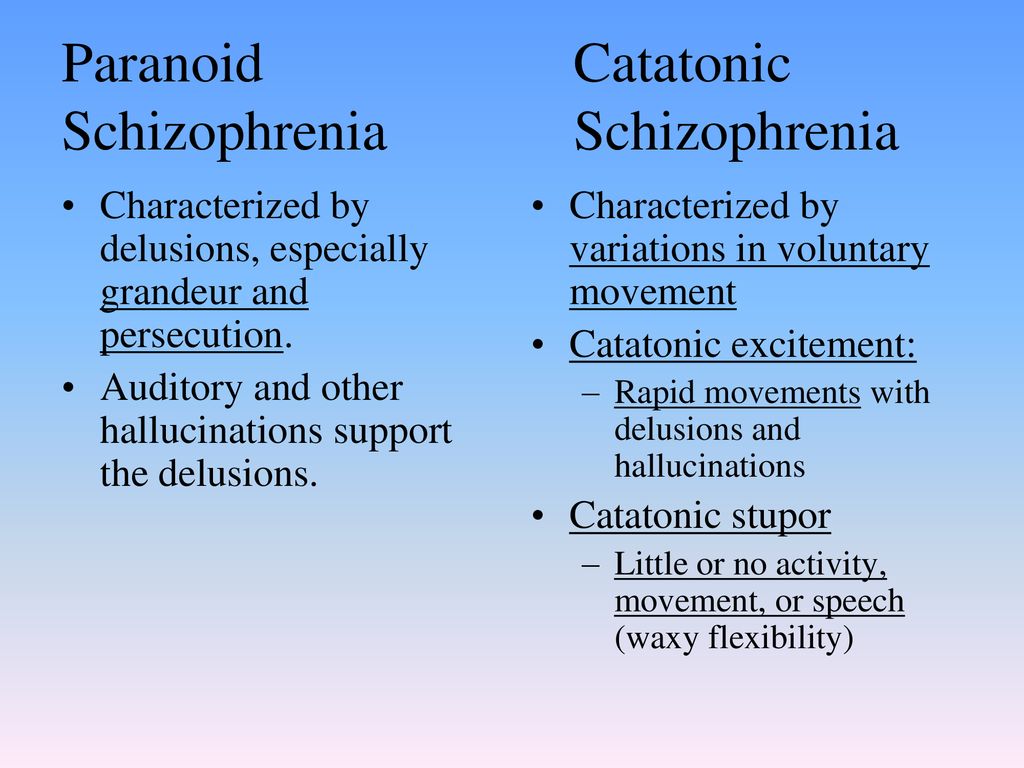
Causes
In psychology and psychiatry, the concept of "dissociation" is used as a description of a protective mechanism that is activated by the psyche in a stressful or difficult situation for a person that he does not want to experience personally. He seems to abstract and observe himself from the side, as if all this "is not happening to him."
The tendency to such behavior can act as one of the reasons for the development of dissociative identity disorder. Violence, despotic upbringing, psychological or physical trauma, etc. can provoke dissociation.
Also, genetic factors can play a big role when there are or were close relatives with similar mental illnesses in the patient's family. In general, a child is born without a coherent identity. His personality will have to be formed in the cultural environment.
If the baby is abused or left to himself and does not receive proper education, he can force the negative out of his mind. Hypothetically, this can subsequently lead to an identity disorder.
Hypothetically, this can subsequently lead to an identity disorder.
It should be understood that the versions about the causes of this mental illness are only assumptions. Science does not know exactly how childhood memories are formed and how exactly they then affect a person’s life. The same situation can affect two children differently.
Thus, a child who sees his father systematically beating his mother is also likely to beat women. However, it is possible that he will become their ardent defender. It's almost impossible to predict exactly. One way or another, people who were subjected to psychological, physical or sexual abuse in childhood are at risk for many mental pathologies. With their development, the psychiatrist necessarily studies the patient's biography.
The fact of violence is recorded in 85% of adults and 95% of children with a split personality.

Also, psychedelics can lead to a split personality. In the 50s. of the last century, scientists tried to find out the mechanism of development of schizophrenia by studying psychedelic drugs. Some of the volunteers who took part in the experiment had a split personality. Moreover, it did not work to return people to their original state, healthy.
Symptoms
There are many symptoms of dissociative identity disorder. Scientists systematized all forms of manifestation of the disease and identified key symptoms. Among them:
- Dissociative fugue, or dissociative flight reaction. In this state, a person looks healthy, but he has features that are unusual for him. He may suddenly leave or leave work, responds to different names, looks lost. As a rule, this passes quickly, but small memory lapses are possible.
- Dissociative amnesia. Usually, memory disappears for individual events that traumatize the psyche.
 A person understands this and tries to remember something, but he fails. At the same time, he learns new information well.
A person understands this and tries to remember something, but he fails. At the same time, he learns new information well. - Dissociative identity disorder. This is a form of direct split personality, when it splits into several persons, each of which has its own name, character and even nationality. The main personality does not control the transition from one character to another. Subsequently, a person cannot remember what he did and how he ended up in one place or another.
- Depersonalization disorder. It seems to the patient that he is watching his body from the side. The perception of the world changes, it becomes colorless. Lost sense of time and space. The person suffers from anxiety and depression. These signs are similar to the symptoms of some forms of schizophrenia.
- Trans. In this state, the patient does not respond to external stimuli. Children tend to behave this way in response to violence or as a result of trauma.
- Ganser syndrome (Mimorech).
 A person deliberately gives incorrect answers to the simplest questions, feigns a severe mental illness, performs actions in the reverse order, for example, lights a match with the wrong side. Often the syndrome is detected in male criminals. In such situations, it is difficult to determine whether a person is really sick, or is trying to portray the disease. After an exit from an attack comes amnesia.
A person deliberately gives incorrect answers to the simplest questions, feigns a severe mental illness, performs actions in the reverse order, for example, lights a match with the wrong side. Often the syndrome is detected in male criminals. In such situations, it is difficult to determine whether a person is really sick, or is trying to portray the disease. After an exit from an attack comes amnesia.
Any of these signs is a reason to consult a psychotherapist. If this is not done, the disease will progress, which is often accompanied by:
- suicide attempts;
- severe headaches;
- self-mutilation;
- eating problems;
- drug addiction and alcoholism;
- deviant behavior, etc.
There may be other consequences that the patient may not remember. If you believe the biography of Billy Milligan, then sexual crimes, that is, violence against women, were committed by a lesbian girl (one of his personalities), who sought physical intimacy with girls.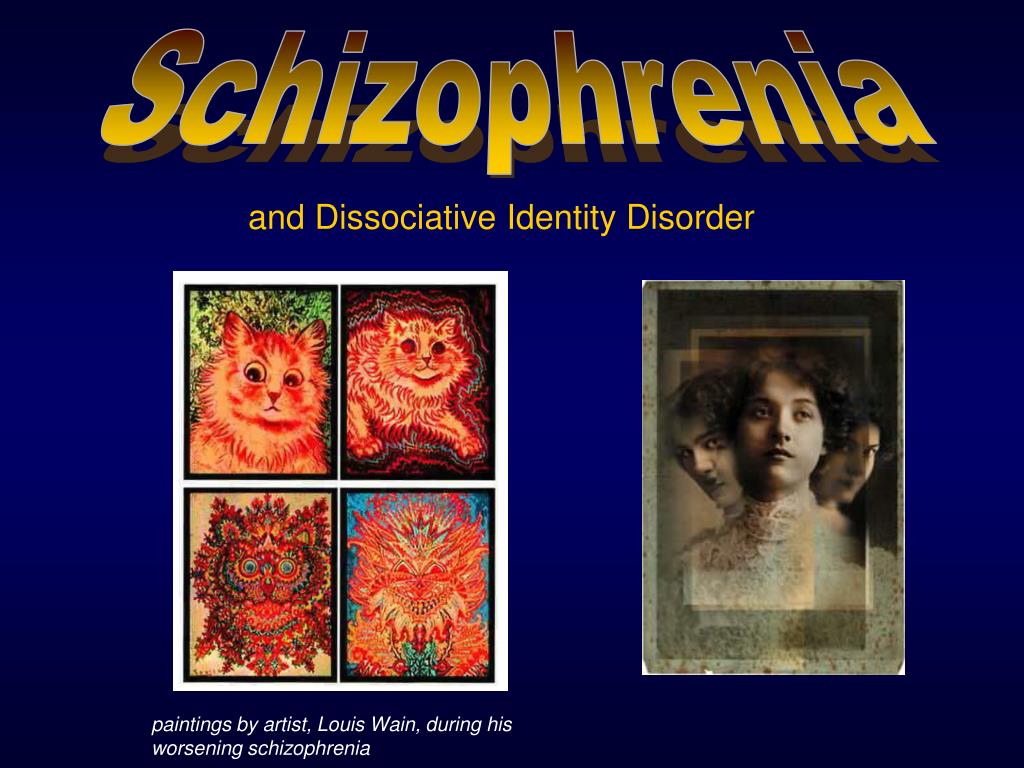
ICD-10 position
In the International Classification of Diseases, Tenth Revision (ICD-10), multiple personality disorder is classified under F44. To make such a diagnosis, it is necessary to identify four signs in the patient:
- The presence of two or more personalities, and at this particular time only one should be present.
- Each person has his own memory, preferences and behavior; at times one of them takes control of the mind.
- The patient cannot remember important information for the main personality. At the same time, memory lapses in scale exceed ordinary forgetfulness.
- Symptoms not associated with organic psychiatric disorders such as epilepsy and substance use.
The number of individuals may exceed a hundred. Their number has been growing over the years. They arise unconsciously. Most likely, the brain creates them in order to make it easier to cope with various situations. So, at the very beginning of treatment, the doctor can identify 2-4 personalities in the patient, and already in the course of communication - another 10-12. Each has its own mannerisms, gestures and even handwriting. Often they do not know that they are not the only ones in a person's head.
So, at the very beginning of treatment, the doctor can identify 2-4 personalities in the patient, and already in the course of communication - another 10-12. Each has its own mannerisms, gestures and even handwriting. Often they do not know that they are not the only ones in a person's head.
Each person can have a different IQ, and the spread can be quite significant - from 80 for one to 140 for another.
Such patients are very rare, therefore, the attitude towards this disease among specialists is different. But the world of art and commerce often exploits this topic, as it attracts the interest of the public.
Treatment
Treatment of dissociative identity disorder is carried out with the help of psychotherapy - cognitive, family, behavioral, etc. All of them are aimed at merging all personalities into one full-fledged identity. The psychiatrist also tries to identify the nature of the internal conflict, to work out situations that turned out to be traumatic for a person and caused the creation of many personalities.
The psychiatrist also tries to identify the nature of the internal conflict, to work out situations that turned out to be traumatic for a person and caused the creation of many personalities.
Medical therapy for such diseases does not help. There are no specific drugs designed to treat it. The doctor may prescribe only antidepressants if the patient is worried about anxiety and depression. But the main treatment is aimed at ensuring the harmonious coexistence of different personalities. This allows you to protect both the patient himself and those around him.
About schizophrenia
Schizophrenia is an endogenous polymorphic mental illness that affects thinking. It does not lead to a split personality. Even if the patient considers himself Napoleon, no split occurs. In this case, we are talking about the disintegration of personal characteristics, but within the framework of one identity. As a result, a person can completely lose touch with reality and remain inside their own fantasies.
The causes of schizophrenia are unknown. Like most mental disorders, it is genetically determined. Various factors can provoke it, including psychological trauma, as with a split personality.
Schizophrenia manifests itself in many ways and develops in one form or another in about 1 in 100 people.
The symptomatology of psychopathology depends on the phase. When the psyche is active, symptoms of an attack or exacerbation are observed:
- Delusional ideas (delusions of grandeur, delusions of jealousy, inventions, reformism, etc.).
- Hallucinations (often voices, but sometimes visual, tactile or even olfactory).
- Catatonic syndrome (excitement in which a person makes strange movements of the same type; or stupor, when the patient freezes for a long time in an unnatural position).
In the negative phase, the patient suffers from apathy, depression, lack of will and other symptoms that indicate the passivity of the mental apparatus.
These signs can also be observed in people with a split personality. However, delusions and hallucinations are extremely rare. Also, this disorder is not characterized by catatonia.
Treatment of schizophrenia is carried out with the help of psychotherapeutic methods and drugs. Among the latter are various kinds of antipsychotic drugs. Some of them increase the level of dopamine, while others, on the contrary, lower it. This allows you to cope with depression or delusions and hallucinations, respectively.
Output
Mental disorders only at first glance are very similar. In fact, they have a different nature of occurrence and are treated using various methods. If any of them is suspected, differential diagnosis is required. But an experienced doctor will be able to distinguish one pathology from another and develop the correct treatment regimen.
Sources:
- arbat25.
 ru
ru - chastnaya-psihiatricheskaya-klinika.ru
- matzpen.ru
how multiple personality arises - T&P
Multiple personality disorder is a bright but rather controversial disease that still causes heated discussions among doctors and scientists. Someone doubts whether it exists at all, someone doubts whether this state should be considered a deviation from the norm. "Theories and Practices" remembered how the research of this psychiatric phenomenon began and why one should not rush to evaluate it.
Dissociative identity disorder - a condition in which, in addition to the main personality, the patient has at least one (and often more) subpersonality, periodically "taking control" of the body and acting in accordance with their own ideas about life. These ideas can be very different from the habits and philosophy of the real owner of the body.
Despite the fact that some experts consider this disease iatrogenic - that is, provoked by the careless words of doctors or watching a "scientific" TV show - there is a number of evidence indicating the opposite.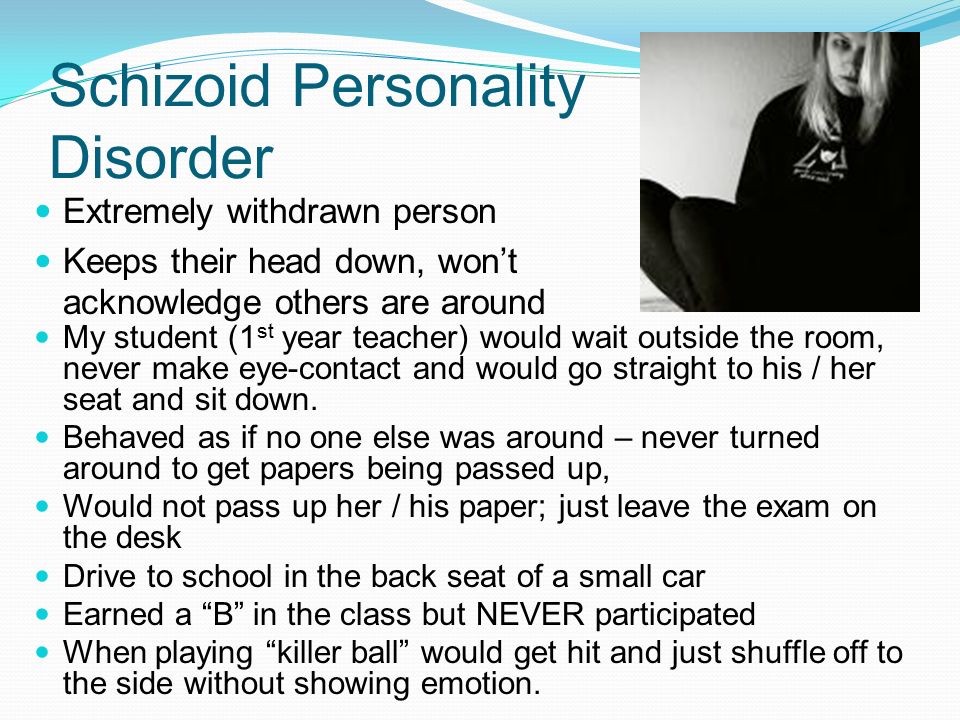 One of the most impressive is the history of the disease. Cases of dissociative disorder were also recorded when neither psychotherapists nor TV shows were in sight. However, psychiatry itself did not exist.
One of the most impressive is the history of the disease. Cases of dissociative disorder were also recorded when neither psychotherapists nor TV shows were in sight. However, psychiatry itself did not exist.
One of the first described cases of dissociative personality disorder occurred at the end of the 18th century in the German city of Stuttgart. A revolution had just taken place in France, and the aristocrats, saving their lives, fled from their native country to neighboring states, including Germany. A young resident of Stuttgart took their misfortunes too close to her heart. She suddenly had a second personality - a Frenchwoman. She not only spoke her “native language” perfectly, but also coped noticeably worse with German, she had a noticeable accent. The Frenchwoman who appeared was of aristocratic blood, and her manners and habits fully corresponded to her status. It is noteworthy that the German girl did not remember what the "Frenchwoman" was doing, and she did not know anything about the legal mistress of the body.
The young German woman was not the only person with this disease in her century, but nevertheless her illness turned out to be extremely rare - in total, 76 cases of dissociative identity disorder were documented up to the middle of the 20th century. Interestingly, in recent decades, much more of them have been described - today more than 40 thousand people with this diagnosis live in the world. However, this does not mean the beginning of an "epidemic" - psychiatry, with all its arsenal of medicines, appeared only in the middle of the last century, and, accordingly, control over the incidence of such disorders began not much earlier.
To date, quite a lot of books and articles have been written about multiple personality disorder, both popular and academic. The most interesting thing about it is, perhaps, the moment of the onset of the disease in childhood. No one is born a “ready-made”, whole person. Growing up, the child experiences many emotions and experiences that are loosely related to each other.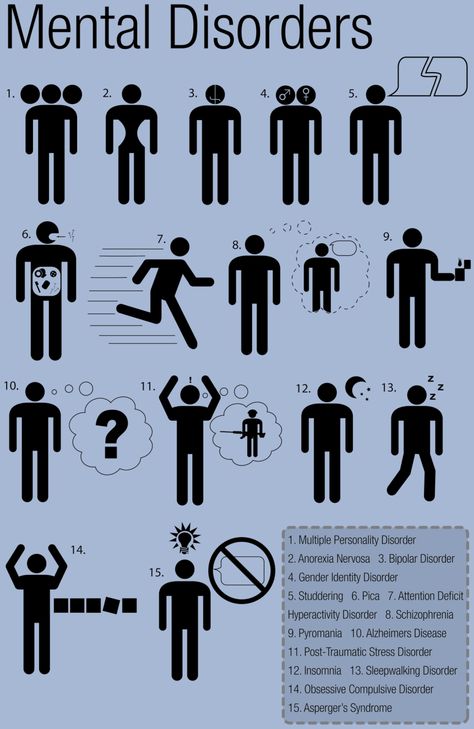 Over time, they integrate together, forming one common identity. However, the development of a child does not always go smoothly. In cases where children at an early age (about 2 years) are separated from their mother when they experience abuse or some traumatic experience, childhood experiences can remain segregated and lead to the formation of two or more personalities. Almost all patients with multiple personality disorder (more precisely, 97-98%) mention a difficult childhood with traumatic experiences.
Over time, they integrate together, forming one common identity. However, the development of a child does not always go smoothly. In cases where children at an early age (about 2 years) are separated from their mother when they experience abuse or some traumatic experience, childhood experiences can remain segregated and lead to the formation of two or more personalities. Almost all patients with multiple personality disorder (more precisely, 97-98%) mention a difficult childhood with traumatic experiences.
Dissociative identity disorder often begins in childhood, but may appear later. Over the years, patients, as a rule, have an increasing number of "tenants". Since individuals, as a rule, perform certain functions, help to cope with certain life situations, with the emergence of new tasks and problems, new residents appear who are able to cope with them. Each of the subpersonalities has its own worldview, its own habits, gestures and facial expressions, even age and intelligence. At certain moments, by the good will of the "owner" or against it, some of the personalities gain control over the body, and everything done by it during use, as a rule, is not controlled and is not remembered by the patient himself.
At certain moments, by the good will of the "owner" or against it, some of the personalities gain control over the body, and everything done by it during use, as a rule, is not controlled and is not remembered by the patient himself.
A key issue in the lives of patients with dissociative personality disorder is the relationship that has developed in the “team”. Sub-personalities may or may not be aware of each other's existence, be aggressive or silently roam museums at their own time, negotiate rental schedules with the owner of the body, or regularly stage power grabs. The treatment strategy also depends on these factors - it is based on psychotherapy, and although its ultimate goal is to come to the integration of personalities into one, an important task in the process is the "neutralization" of dangerous tenants, and the organization of harmonious relations between all subpersonalities.
More than one person in one body is unfortunately not the only symptom of dissociative identity disorder. It is often accompanied by depression, anxiety disorders, phobias, sleep and eating disorders, even hallucinations. Dissociative disorder is sometimes confused with schizophrenia, but these diseases can be distinguished - in schizophrenia, as a rule, the symptoms are perceived as enemy actions of aliens, the KGB or members of the Masonic lodge, which is not the case with dissociative disorder. In addition, splitting identities in schizophrenia is a simple separation of mental functions due to a general breakdown of personality, but with DID (Dissociative identity disorder - another name for multiple personality disorder), everything is much more complicated. Functions are not only separated, but also become full-fledged individuals: each of them has their own style of clothing, supports their football team and has their own ideas about how to spend time.
It is often accompanied by depression, anxiety disorders, phobias, sleep and eating disorders, even hallucinations. Dissociative disorder is sometimes confused with schizophrenia, but these diseases can be distinguished - in schizophrenia, as a rule, the symptoms are perceived as enemy actions of aliens, the KGB or members of the Masonic lodge, which is not the case with dissociative disorder. In addition, splitting identities in schizophrenia is a simple separation of mental functions due to a general breakdown of personality, but with DID (Dissociative identity disorder - another name for multiple personality disorder), everything is much more complicated. Functions are not only separated, but also become full-fledged individuals: each of them has their own style of clothing, supports their football team and has their own ideas about how to spend time.
Treatment of patients diagnosed with multiple personality disorder is usually long, difficult and emotionally costly. However, not everyone agrees that it should be treated at all. The American psychologist James Hillman, the founder of the school of archetypal psychology, is convinced that the position that multiple personality syndrome is considered a disorder is nothing more than a stereotype that can and should be fought, advocating the right of people with this diagnosis to be considered no less normal than others. The goal of therapy, according to Hillman, is only the creation of harmonious relations of all subpersonalities. Many patients also support his position. The ideologist of such a movement was Truddy Chase, who refused to integrate subpersonalities into a single whole and instead established mutually beneficial cooperation with them. She wrote about her experience in the book When the Rabbit Howls. Today, Truddy is far from the only one who refuses to integrate. No wonder: killing good friends and useful assistants with your own hands, albeit symbolically, is still not easy.
The American psychologist James Hillman, the founder of the school of archetypal psychology, is convinced that the position that multiple personality syndrome is considered a disorder is nothing more than a stereotype that can and should be fought, advocating the right of people with this diagnosis to be considered no less normal than others. The goal of therapy, according to Hillman, is only the creation of harmonious relations of all subpersonalities. Many patients also support his position. The ideologist of such a movement was Truddy Chase, who refused to integrate subpersonalities into a single whole and instead established mutually beneficial cooperation with them. She wrote about her experience in the book When the Rabbit Howls. Today, Truddy is far from the only one who refuses to integrate. No wonder: killing good friends and useful assistants with your own hands, albeit symbolically, is still not easy.
Flora Schreiber
A serious and very detailed book written by a doctor about her own patient who is trying to get along with her sixteen subpersonalities.