Can mental disorders be cured
Mental illness - Diagnosis and treatment
Diagnosis
To determine a diagnosis and check for related complications, you may have:
- A physical exam. Your doctor will try to rule out physical problems that could cause your symptoms.
- Lab tests. These may include, for example, a check of your thyroid function or a screening for alcohol and drugs.
- A psychological evaluation. A doctor or mental health professional talks to you about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
Determining which mental illness you have
Sometimes it's difficult to find out which mental illness may be causing your symptoms. But taking the time and effort to get an accurate diagnosis will help determine the appropriate treatment. The more information you have, the more you will be prepared to work with your mental health professional in understanding what your symptoms may represent.
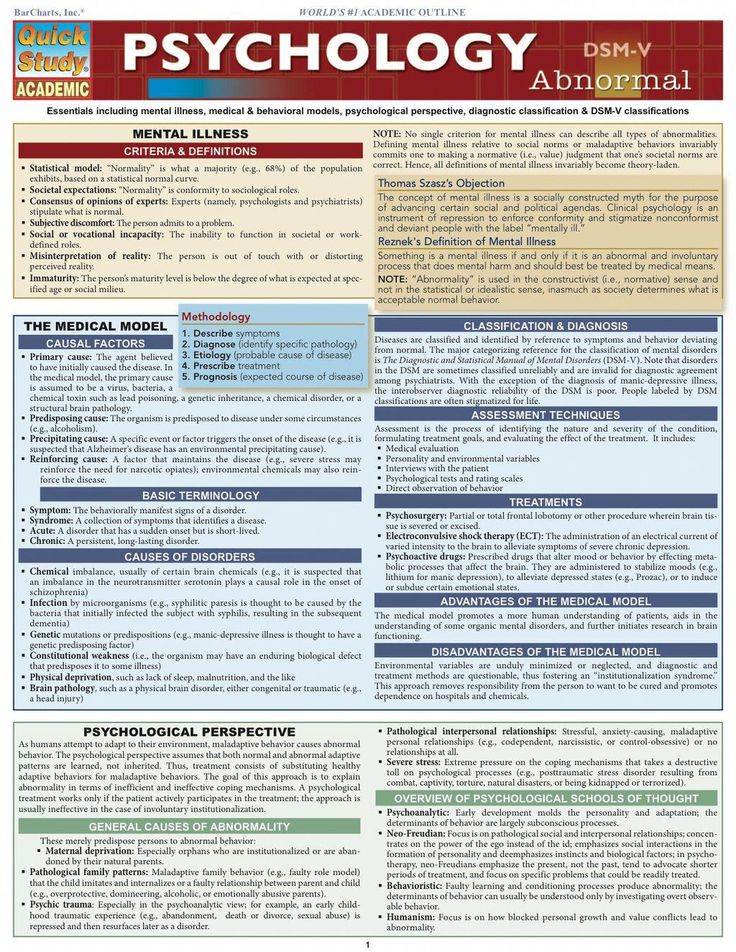
The defining symptoms for each mental illness are detailed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. This manual is used by mental health professionals to diagnose mental conditions and by insurance companies to reimburse for treatment.
Classes of mental illness
The main classes of mental illness are:
- Neurodevelopmental disorders. This class covers a wide range of problems that usually begin in infancy or childhood, often before the child begins grade school. Examples include autism spectrum disorder, attention-deficit/hyperactivity disorder (ADHD) and learning disorders.
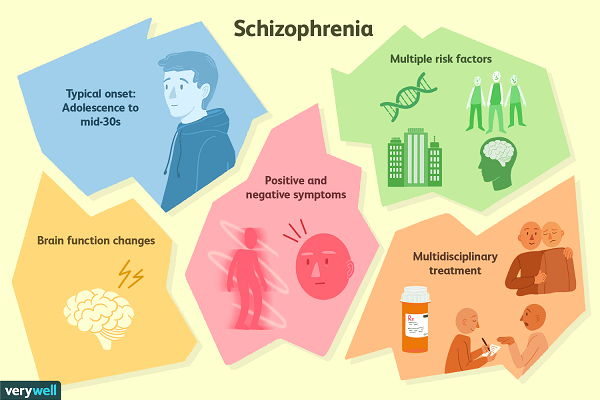
- Schizophrenia spectrum and other psychotic disorders. Psychotic disorders cause detachment from reality — such as delusions, hallucinations, and disorganized thinking and speech. The most notable example is schizophrenia, although other classes of disorders can be associated with detachment from reality at times.
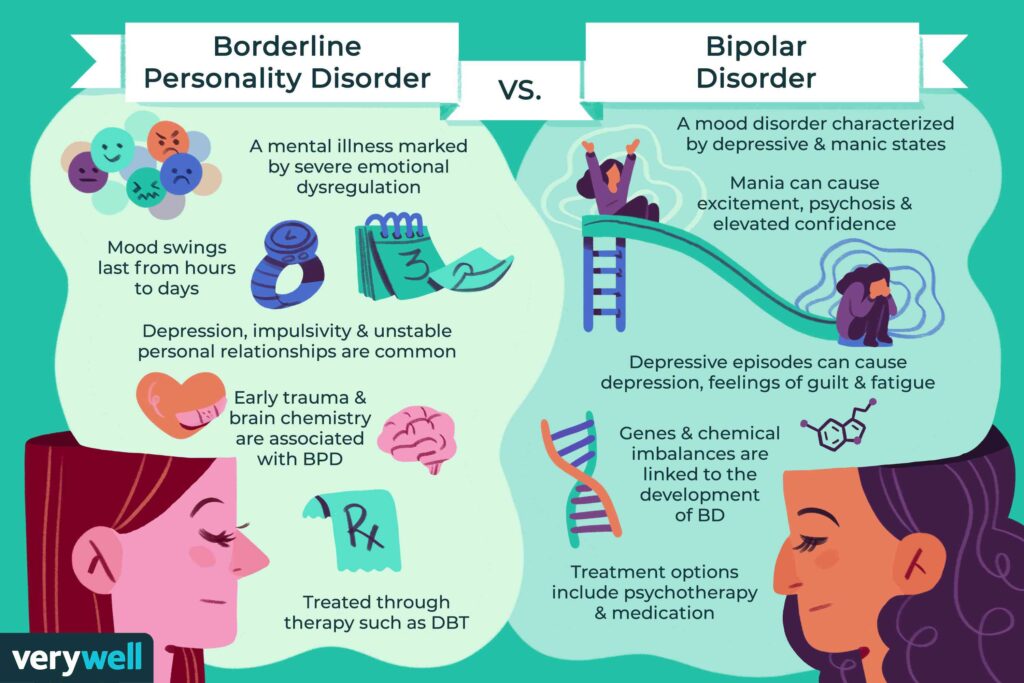
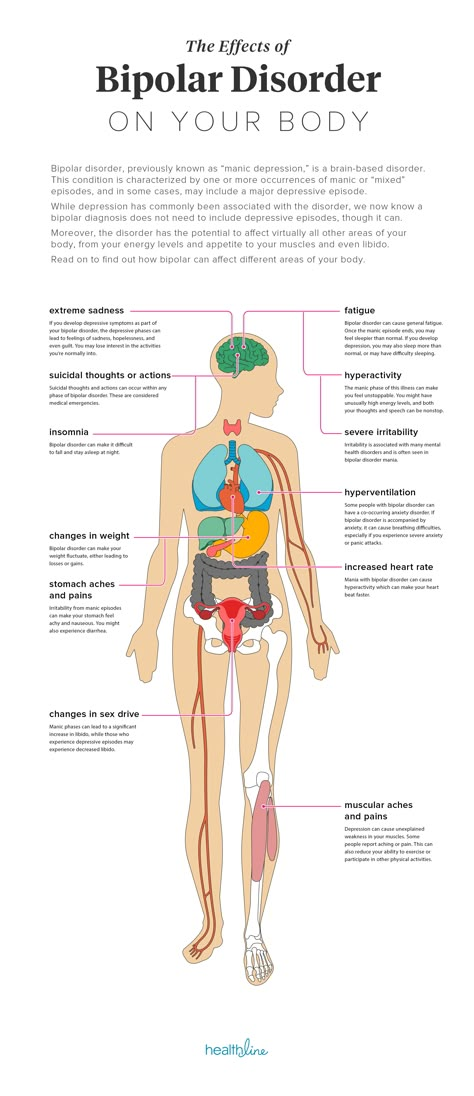
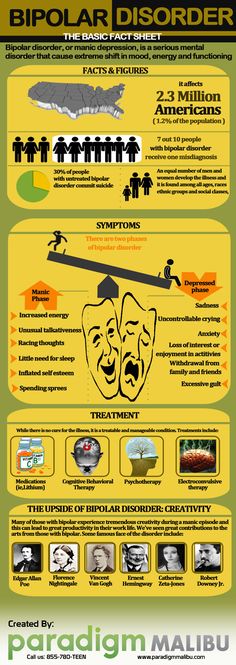
- Bipolar and related disorders. This class includes disorders with alternating episodes of mania — periods of excessive activity, energy and excitement — and depression.
- Depressive disorders. These include disorders that affect how you feel emotionally, such as the level of sadness and happiness, and they can disrupt your ability to function. Examples include major depressive disorder and premenstrual dysphoric disorder.
- Anxiety disorders. Anxiety is an emotion characterized by the anticipation of future danger or misfortune, along with excessive worrying. It can include behavior aimed at avoiding situations that cause anxiety. This class includes generalized anxiety disorder, panic disorder and phobias.
- Obsessive-compulsive and related disorders. These disorders involve preoccupations or obsessions and repetitive thoughts and actions. Examples include obsessive-compulsive disorder, hoarding disorder and hair-pulling disorder (trichotillomania).
- Trauma- and stressor-related disorders. These are adjustment disorders in which a person has trouble coping during or after a stressful life event. Examples include post-traumatic stress disorder (PTSD) and acute stress disorder.
- Dissociative disorders. These are disorders in which your sense of self is disrupted, such as with dissociative identity disorder and dissociative amnesia.
- Somatic symptom and related disorders. A person with one of these disorders may have physical symptoms that cause major emotional distress and problems functioning. There may or may not be another diagnosed medical condition associated with these symptoms, but the reaction to the symptoms is not normal. The disorders include somatic symptom disorder, illness anxiety disorder and factitious disorder.
- Feeding and eating disorders. These disorders include disturbances related to eating that impact nutrition and health, such as anorexia nervosa and binge-eating disorder.
- Elimination disorders. These disorders relate to the inappropriate elimination of urine or stool by accident or on purpose. Bed-wetting (enuresis) is an example.
- Sleep-wake disorders. These are disorders of sleep severe enough to require clinical attention, such as insomnia, sleep apnea and restless legs syndrome.
- Sexual dysfunctions. These include disorders of sexual response, such as premature ejaculation and female orgasmic disorder.
- Gender dysphoria. This refers to the distress that accompanies a person's stated desire to be another gender.
- Disruptive, impulse-control and conduct disorders. These disorders include problems with emotional and behavioral self-control, such as kleptomania or intermittent explosive disorder.
- Substance-related and addictive disorders. These include problems associated with the excessive use of alcohol, caffeine, tobacco and drugs.
 This class also includes gambling disorder.
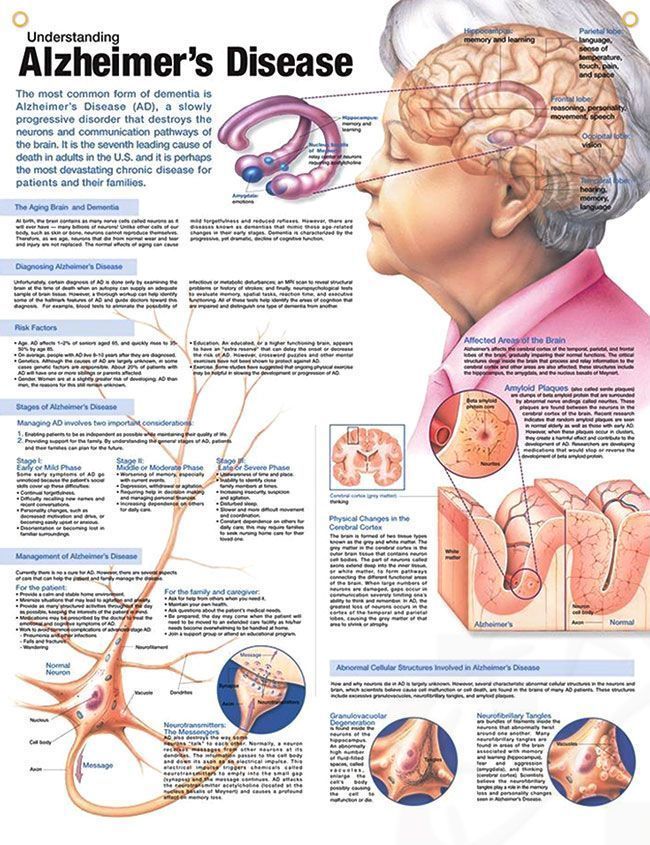
This class also includes gambling disorder. - Neurocognitive disorders. Neurocognitive disorders affect your ability to think and reason. These acquired (rather than developmental) cognitive problems include delirium, as well as neurocognitive disorders due to conditions or diseases such as traumatic brain injury or Alzheimer's disease.
- Personality disorders. A personality disorder involves a lasting pattern of emotional instability and unhealthy behavior that causes problems in your life and relationships. Examples include borderline, antisocial and narcissistic personality disorders.
- Paraphilic disorders. These disorders include sexual interest that causes personal distress or impairment or causes potential or actual harm to another person. Examples are sexual sadism disorder, voyeuristic disorder and pedophilic disorder.
- Other mental disorders. This class includes mental disorders that are due to other medical conditions or that don't meet the full criteria for one of the above disorders.
Treatment
Your treatment depends on the type of mental illness you have, its severity and what works best for you. In many cases, a combination of treatments works best.
If you have a mild mental illness with well-controlled symptoms, treatment from your primary care provider may be sufficient. However, often a team approach is appropriate to make sure all your psychiatric, medical and social needs are met. This is especially important for severe mental illnesses, such as schizophrenia.
Your treatment team
Your treatment team may include your:
- Family or primary care doctor
- Nurse practitioner
- Physician assistant
- Psychiatrist, a medical doctor who diagnoses and treats mental illnesses
- Psychotherapist, such as a psychologist or a licensed counselor
- Pharmacist
- Social worker
- Family members
Medications
Although psychiatric medications don't cure mental illness, they can often significantly improve symptoms.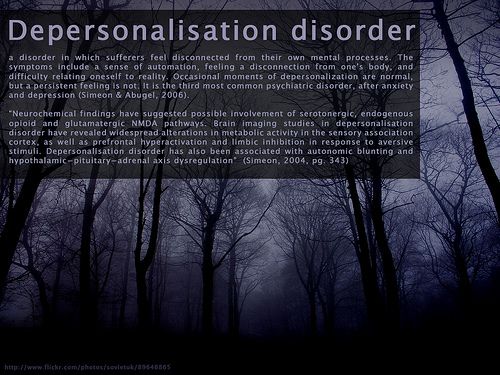 Psychiatric medications can also help make other treatments, such as psychotherapy, more effective. The best medications for you will depend on your particular situation and how your body responds to the medication.
Psychiatric medications can also help make other treatments, such as psychotherapy, more effective. The best medications for you will depend on your particular situation and how your body responds to the medication.
Some of the most commonly used classes of prescription psychiatric medications include:
- Antidepressants. Antidepressants are used to treat depression, anxiety and sometimes other conditions. They can help improve symptoms such as sadness, hopelessness, lack of energy, difficulty concentrating and lack of interest in activities. Antidepressants are not addictive and do not cause dependency.
- Anti-anxiety medications. These drugs are used to treat anxiety disorders, such as generalized anxiety disorder or panic disorder. They may also help reduce agitation and insomnia. Long-term anti-anxiety drugs typically are antidepressants that also work for anxiety. Fast-acting anti-anxiety drugs help with short-term relief, but they also have the potential to cause dependency, so ideally they'd be used short term.
- Mood-stabilizing medications. Mood stabilizers are most commonly used to treat bipolar disorders, which involves alternating episodes of mania and depression. Sometimes mood stabilizers are used with antidepressants to treat depression.
- Antipsychotic medications. Antipsychotic drugs are typically used to treat psychotic disorders, such as schizophrenia. Antipsychotic medications may also be used to treat bipolar disorders or used with antidepressants to treat depression.
Psychotherapy
Psychotherapy, also called talk therapy, involves talking about your condition and related issues with a mental health professional. During psychotherapy, you learn about your condition and your moods, feelings, thoughts and behavior. With the insights and knowledge you gain, you can learn coping and stress management skills.
There are many types of psychotherapy, each with its own approach to improving your mental well-being. Psychotherapy often can be successfully completed in a few months, but in some cases, long-term treatment may be needed. It can take place one-on-one, in a group or with family members.
Psychotherapy often can be successfully completed in a few months, but in some cases, long-term treatment may be needed. It can take place one-on-one, in a group or with family members.
When choosing a therapist, you should feel comfortable and be confident that he or she is capable of listening and hearing what you have to say. Also, it's important that your therapist understands the life journey that has helped shape who you are and how you live in the world.
Brain-stimulation treatments
Brain-stimulation treatments are sometimes used for depression and other mental health disorders. They're generally reserved for situations in which medications and psychotherapy haven't worked. They include electroconvulsive therapy, repetitive transcranial magnetic stimulation, deep brain stimulation and vagus nerve stimulation.
Make sure you understand all the risks and benefits of any recommended treatment.
Hospital and residential treatment programs
Sometimes mental illness becomes so severe that you need care in a psychiatric hospital. This is generally recommended when you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else.
This is generally recommended when you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else.
Options include 24-hour inpatient care, partial or day hospitalization, or residential treatment, which offers a temporary supportive place to live. Another option may be intensive outpatient treatment.
Substance misuse treatment
Problems with substance use commonly occur along with mental illness. Often it interferes with treatment and worsens mental illness. If you can't stop using drugs or alcohol on your own, you need treatment. Talk to your doctor about treatment options.
Participating in your own care
Working together, you and your primary care provider or mental health professional can decide which treatment may be best, depending on your symptoms and their severity, your personal preferences, medication side effects, and other factors. In some cases, a mental illness may be so severe that a doctor or loved one may need to guide your care until you're well enough to participate in decision-making.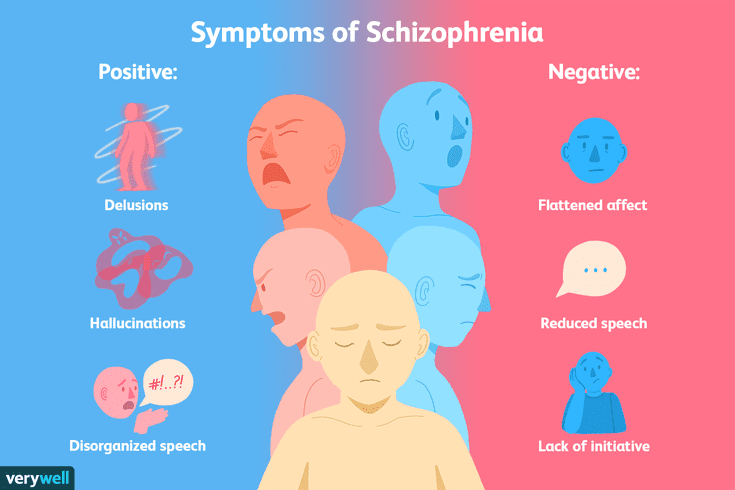
More Information
- Mental health providers: Tips on finding one
- Deep brain stimulation
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.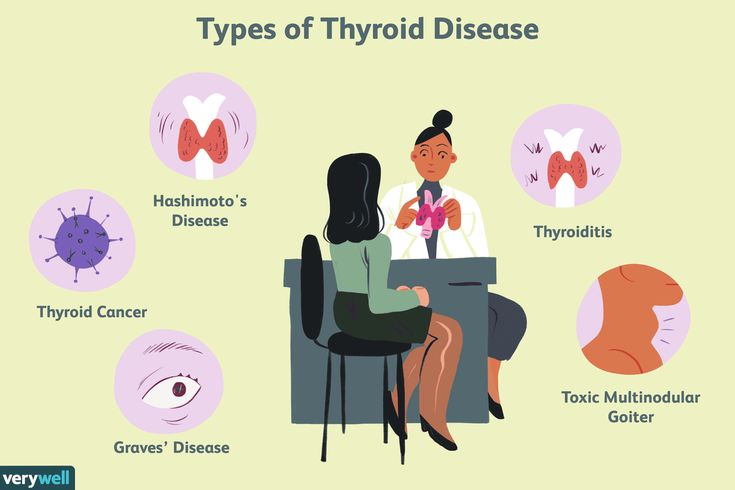 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Lifestyle and home remedies
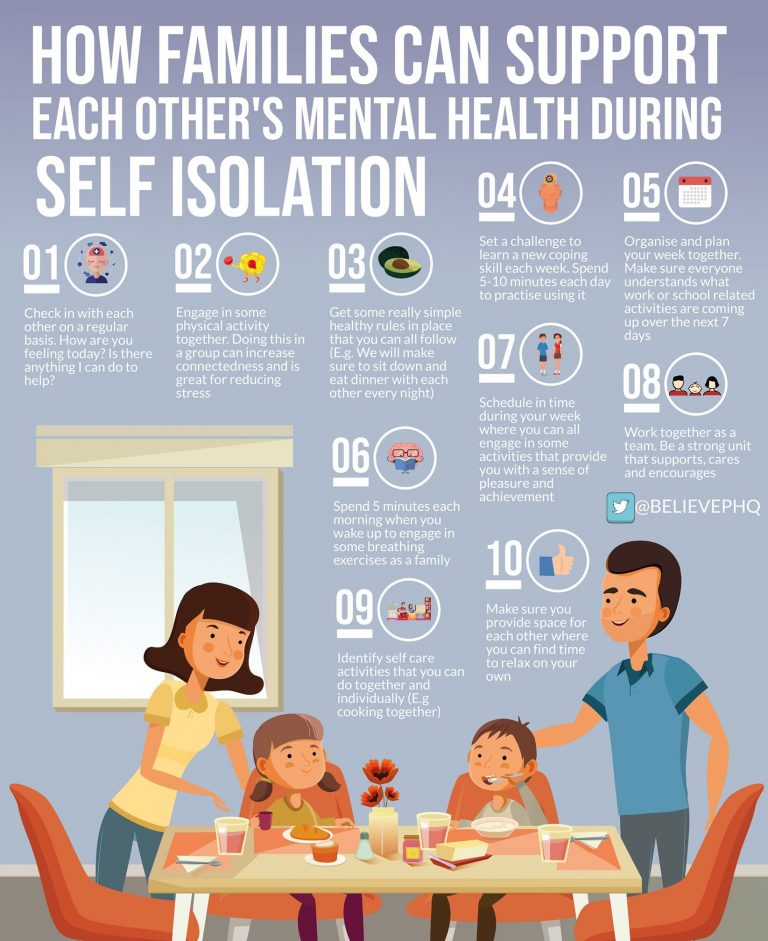
In most cases, a mental illness won't get better if you try to treat it on your own without professional care. But you can do some things for yourself that will build on your treatment plan:
- Stick to your treatment plan. Don't skip therapy sessions. Even if you're feeling better, don't skip your medications. If you stop, symptoms may come back. And you could have withdrawal-like symptoms if you stop a medication too suddenly. If you have bothersome drug side effects or other problems with treatment, talk to your doctor before making changes.
- Avoid alcohol and drug use. Using alcohol or recreational drugs can make it difficult to treat a mental illness. If you're addicted, quitting can be a real challenge. If you can't quit on your own, see your doctor or find a support group to help you.

- Stay active. Exercise can help you manage symptoms of depression, stress and anxiety. Physical activity can also counteract the effects of some psychiatric medications that may cause weight gain. Consider walking, swimming, gardening or any form of physical activity that you enjoy. Even light physical activity can make a difference.
- Make healthy choices. Maintaining a regular schedule that includes sufficient sleep, healthy eating and regular physical activity are important to your mental health.
- Don't make important decisions when your symptoms are severe. Avoid decision-making when you're in the depth of mental illness symptoms, since you may not be thinking clearly.
- Determine priorities. You may reduce the impact of your mental illness by managing time and energy. Cut back on obligations when necessary and set reasonable goals. Give yourself permission to do less when symptoms are worse.
 You may find it helpful to make a list of daily tasks or use a planner to structure your time and stay organized.
You may find it helpful to make a list of daily tasks or use a planner to structure your time and stay organized. - Learn to adopt a positive attitude. Focusing on the positive things in your life can make your life better and may even improve your health. Try to accept changes when they occur, and keep problems in perspective. Stress management techniques, including relaxation methods, may help.
Coping and support
Coping with a mental illness is challenging. Talk to your doctor or therapist about improving your coping skills, and consider these tips:
- Learn about your mental illness. Your doctor or therapist can provide you with information or may recommend classes, books or websites. Include your family, too — this can help the people who care about you understand what you're going through and learn how they can help.
- Join a support group. Connecting with others facing similar challenges may help you cope.
 Support groups for mental illness are available in many communities and online. One good place to start is the National Alliance on Mental Illness.
Support groups for mental illness are available in many communities and online. One good place to start is the National Alliance on Mental Illness. - Stay connected with friends and family. Try to participate in social activities, and get together with family or friends regularly. Ask for help when you need it, and be upfront with your loved ones about how you're doing.
- Keep a journal. Or jot down brief thoughts or record symptoms on a smartphone app. Keeping track of your personal life and sharing information with your therapist can help you identify what triggers or improves your symptoms. It's also a healthy way to explore and express pain, anger, fear and other emotions.
Preparing for your appointment
Whether you schedule an appointment with your primary care provider to talk about mental health concerns or you're referred to a mental health professional, such as a psychiatrist or psychologist, take steps to prepare for your appointment.
If possible, take a family member or friend along. Someone who has known you for a long time may be able to share important information, with your permission.
What you can do
Before your appointment, make a list of:
- Any symptoms you or people close to you have noticed, and for how long
- Key personal information, including traumatic events in your past and any current, major stressors
- Your medical information, including other physical or mental health conditions
- Any medications, vitamins, herbal products or other supplements you take, and their dosages
- Questions to ask your doctor or mental health professional
Questions to ask may include:
- What type of mental illness might I have?
- Why can't I get over mental illness on my own?
- How do you treat my type of mental illness?
- Will talk therapy help?
- Are there medications that might help?
- How long will treatment take?
- What can I do to help myself?
- Do you have any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
During your appointment, your doctor or mental health professional is likely to ask you questions about your mood, thoughts and behavior, such as:
- When did you first notice symptoms?
- How is your daily life affected by your symptoms?
- What treatment, if any, have you had for mental illness?
- What have you tried on your own to feel better or control your symptoms?
- What things make you feel worse?
- Have family members or friends commented on your mood or behavior?
- Do you have blood relatives with a mental illness?
- What do you hope to gain from treatment?
- What medications or over-the-counter herbs and supplements do you take?
- Do you drink alcohol or use recreational drugs?
Your doctor or mental health professional will ask additional questions based on your responses, symptoms and needs. Preparing and anticipating questions will help you make the most of your time with the doctor.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
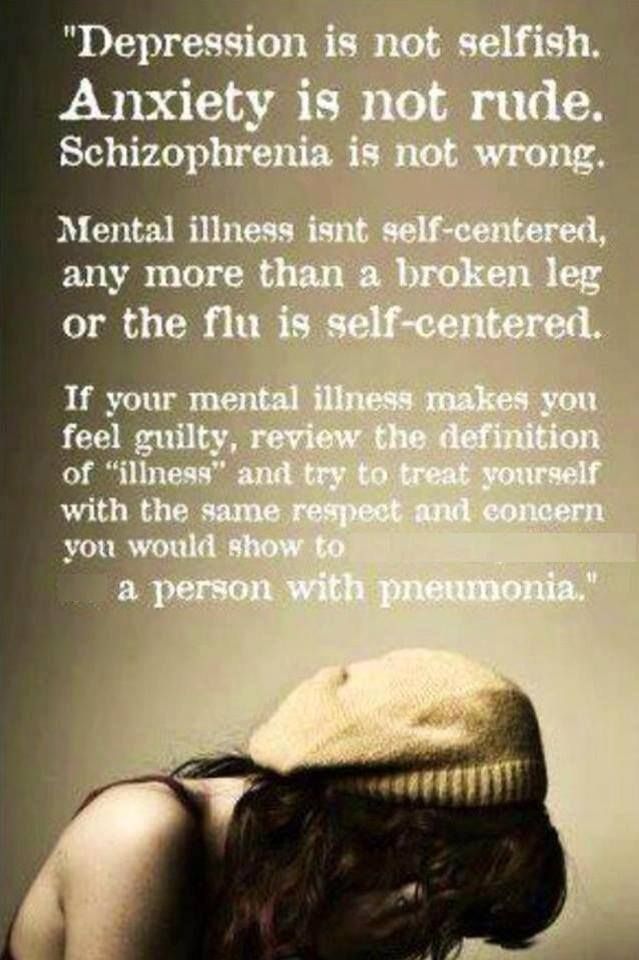
9 Damaging Myths about Mental Illness
Thanks to news stories, books, and movies, the terms “mentally ill” and “crazy” can be used interchangeably in the minds of far too many people. However, nothing could be further from the truth. Mental illness encompasses a vast array of disorders including ADHD, depression, and anxiety – the vast majority of which respond very well to proper treatment and are rarely associated with “insanity”. So if you or someone you love has just been diagnosed with a mental disorder and dread any potential stigma (which is often due to myths), it’s time to arm yourself with the facts. Following are 9 of the most common – and often damaging – myths about mental illness, and the reality behind them:
- People with mental illness just need to “get a grip”. This is one of the most common mental health myths that prevents people from getting the help they need.
 Think of it this way: when you break a bone, chances are good you’re not going to set it yourself and go on with life, hoping it heals correctly. Instead you’ll visit a medical professional with the know-how and tools to help your body recover properly. Doesn’t your mind deserve the same care?
Think of it this way: when you break a bone, chances are good you’re not going to set it yourself and go on with life, hoping it heals correctly. Instead you’ll visit a medical professional with the know-how and tools to help your body recover properly. Doesn’t your mind deserve the same care? - Mental illness has no cure. While there are some disorders that are considered life-long – even with treatment, many can be effectively treated and overcome. People living with a mental disorder, whether it’s anorexia nervosa, obsessive-compulsive disorder (OCD), or even schizophrenia, have far more available and beneficial treatment options today than in years past. A mental health professional will work with you to create an effective treatment plan that typically includes one or more of these options:
- Therapy: Say therapy and many of us envision lying on a couch talking to a note-taking Freud-type. In fact, there are many different types and modalities of therapy used by professionals to treat mental illness.
 For example, some individuals will gain the most benefit from a longer-term insight-oriented type of therapy, while others do best with a short-term type of therapy that focuses on solutions. Additionally, one-on-one talk therapy may be best for some individuals, while a group therapy setting might be more appropriate for others. Therapy for a serious, treatment-resistant condition may also involve undergoing a medical procedure such as electroconvulsive therapy (ECT).
For example, some individuals will gain the most benefit from a longer-term insight-oriented type of therapy, while others do best with a short-term type of therapy that focuses on solutions. Additionally, one-on-one talk therapy may be best for some individuals, while a group therapy setting might be more appropriate for others. Therapy for a serious, treatment-resistant condition may also involve undergoing a medical procedure such as electroconvulsive therapy (ECT). - Medication: Prescription drugs can go a long way towards helping someone with mental illness live a full and normal life. Certain anxiety disorders, attention deficit hyperactivity disorder (ADHD), bipolar disorder, severe depression, and schizophrenia are just some of the conditions that are often treated using a combination of medication and therapy. As with any prescription drugs, psychotropic medications have both limitations and side effects, so they may not be the right choice in some cases.
- Support Groups: A supportive shoulder and empathetic ear can play an important role in managing mental illness.
 Support groups, which can be led by a group member or a mental health professional, allow people living with mental illness (and, perhaps, their family or friends) to connect with others who share many of the same struggles and experiences.
Support groups, which can be led by a group member or a mental health professional, allow people living with mental illness (and, perhaps, their family or friends) to connect with others who share many of the same struggles and experiences.
- Therapy: Say therapy and many of us envision lying on a couch talking to a note-taking Freud-type. In fact, there are many different types and modalities of therapy used by professionals to treat mental illness.
- Mental illness makes people violent. The vast majority of individuals who suffer from a mental illness are not violent. While a small percentage of people with serious mental illnesses can become violent towards others, the violence that is most often committed is against themselves – in the form of suicide. Experts estimate about 90% of suicide victims have a diagnosable mental illness. The reality is that people with a severe mental disorder are 11 times more likely to be the victim of violence than those without one. [2]
- Mental illness is a sign of weakness. Most psychiatric disorders develop, at least in part, to an underlying genetic predisposition and / or a chemical imbalance within the brain. Others are the result of a traumatic event such as being raped or living through a natural disaster.
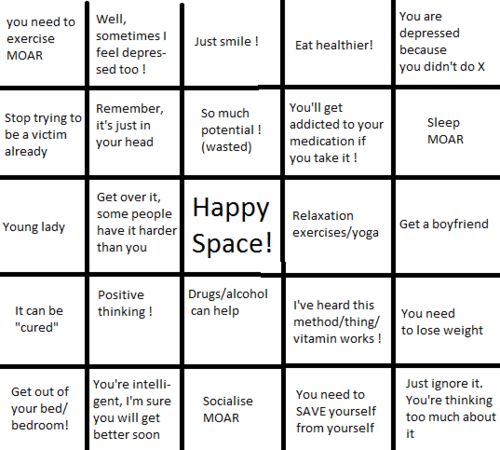 Regardless of the origin, mental illness is a genuine health problem that requires professional medical attention. Just as you can’t beat cancer by simply “being strong,” you can’t beat mental illness through the power of your will or by ignoring the problem.
Regardless of the origin, mental illness is a genuine health problem that requires professional medical attention. Just as you can’t beat cancer by simply “being strong,” you can’t beat mental illness through the power of your will or by ignoring the problem. - If I have a mental illness, I’ll never be able to hold a job. Living with an untreated mental condition can definitely make it very difficult to go about daily activities, including holding a job. With proper treatment, however, most people who have a mental illness can and do go to work every day. The key to living a normal life is to recognize the problem and then tap the resources that help you manage or overcome it.
- Real mental disorders are rare. Chances are good that you already know someone with a mental illness. It could be the girl who sits next to you at school, your neighbor across the street, or your coworker just down the hall. These disorders affect nearly 58 million Americans every year, which means approximately 1 in every 4 adults has struggled with mental illness in the past 12 months.
 Mental illness knows no boundaries; it can strike family members, friends, and co-workers – and you may not even know it.
Mental illness knows no boundaries; it can strike family members, friends, and co-workers – and you may not even know it. - My family doctor can just prescribe a drug to make me feel better. Popping a pill seems like a simple way to cure anything. But medication is often only one part of managing mental illness, and in many cases medication is not the primary form of treatment. Becoming healthy often involves a combination of treatments that may – or may not – include prescription drugs.
- Bad parenting triggers mental illness. Childhood experience is just one of the many factors that may contribute to a psychiatric disorder. Genetics, biology, and environmental influences almost always play a role in whether a person develops a mental illness. In fact, most experts agree that a person’s mental condition is often the result of many factors coming together.
- Mental illnesses are all alike…crazy is crazy. This is one of the most harmful myths about mental illness. As mentioned above, the term mental illness describes a dizzying range of disorders that affects many different people in many different ways.
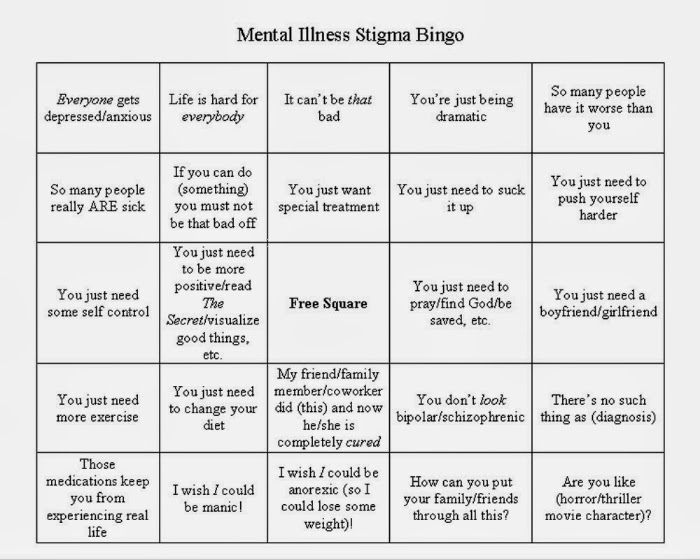 Those with mental illness might have one of dozens of disorders, from ADHD to bipolar disorder. Some people have obvious symptoms, while others are much more subtle. Still others are affected by only one episode during their lifetime while some live with their illness for decades. For some, the illness is debilitating, while others are able to live a highly productive life both during and after treatment.
Those with mental illness might have one of dozens of disorders, from ADHD to bipolar disorder. Some people have obvious symptoms, while others are much more subtle. Still others are affected by only one episode during their lifetime while some live with their illness for decades. For some, the illness is debilitating, while others are able to live a highly productive life both during and after treatment.
Mental illness does not equal crazy. In fact, many who live with these disorders learn to manage their symptoms and go on with life. Others will even recover completely. Don’t let myths about mental illness prevent you or a loved one from getting the treatment you need and deserve. If you suspect you’re battling a mental disorder, set up an appointment for an evaluation by a qualified mental health professional. The sooner you take action, the sooner you can get back to living your life as fully as possible.
SIGNS OF MENTAL DISORDERS (WHEN TO SEE A DOCTOR)
Signs of mental disorders, and also the frequency of their occurrence is a common question, exciting people in recent years. This is especially true in connection with the fact that the pace of life is steadily growing, and the resources of human nervous system remain unchanged. Very often mental violations develop gradually, stepwise, introducing features into the psyche a person who was previously not peculiar to him, respectively, there are good chances to notice them in time and provide proper medical care.
This is especially true in connection with the fact that the pace of life is steadily growing, and the resources of human nervous system remain unchanged. Very often mental violations develop gradually, stepwise, introducing features into the psyche a person who was previously not peculiar to him, respectively, there are good chances to notice them in time and provide proper medical care.
According to the latest data, mental disorders are detected in 25-30% of the population, that is, one in four in the world. However, it is noteworthy that while 75-80% are sick non-psychotic, mild mental disorders. serious mental illnesses such as schizophrenia occur in 6-17% cases. Alcoholism - in 60%.
It must be remembered that mental disorder is not a sentence, because with sufficient and timely treatment by a specialist, as well as a responsible attitude and attention to their condition, the symptoms of mental disorders can be stopped, (and often the disorder itself can be completely cured), which will help to maintain the former social, professional status and quality of life.
SIGNS
Asthenic syndrome.
This condition may accompany any mental disorders and many of the somatic diseases. Asthenia expressed in weakness, low performance, mood swings, increased sensitivity. A person starts crying easily, instantly gets irritated and loses his temper. Often asthenia is accompanied sleep disturbances, feeling of weakness, increased fatigue, inability to cope with the usual workload, study.
Obsessive states.
A wide range of obsessions includes many manifestations: from constant doubts, unpleasant thoughts, "stuck, spinning in the head", fears with which a person does not able to cope, to an irresistible desire for purity or performing certain unusual actions. Under the control of the obsessive state, a person can return home several times in order to check whether he turned off the iron, gas, water, whether he closed the door with a key. An obsessive fear of an accident can force the patient to perform some rituals that, according to the sufferer, can avert trouble. If you notice that your friend or relative washes his hands for hours, became overly squeamish and is always afraid of getting infected with something - this also obsession. The desire not to step on cracks in the asphalt, joints tiles, avoidance of certain modes of transport or people in clothing a certain color or type is also an obsessive state.
If you notice that your friend or relative washes his hands for hours, became overly squeamish and is always afraid of getting infected with something - this also obsession. The desire not to step on cracks in the asphalt, joints tiles, avoidance of certain modes of transport or people in clothing a certain color or type is also an obsessive state.
Mood changes.
It is especially important to pay attention not to how much for short-term changes under the influence of momentary factors, how much for mood changes that were not previously characteristic a person, long-term, from 2 weeks or more.
- Longing, depression, longing for self-accusations, talk about their own worthlessness, sinfulness, about death, lack of future, hope for the best, etc.
- Unnatural frivolity, carelessness.
- Foolishness, not characteristic of age and character.
- Euphoric state, optimism without any basis.
- Apathy, painful feeling of lack of emotions.
- Fussiness, talkativeness, inability to concentrate, confused thinking.
- Irritability, anger, aggressiveness
- Inability to control emotions, tearfulness, slight breakdowns in conversation natural bashfulness, inability to restrain sexual desires or vice versa, the disappearance of libido, the absence of a morning erection in men
Unusual sensations in the body.
Stinging, burning in the skin, sensations burning, “twisting” pressure in the body, stirring “something inside”, "rustling in the head", the presence of foreign objects in the body - can signal disturbances in the nervous system.
Hypochondria.
Expressed in an obsessive, obsessive search for themselves of serious illnesses and disorders, painful "listening" to the slightest change in the state of your body. At the same time, the patient often does not trust doctors, requires repeated and deeper research, completely focused on finding difficult diseases, requires to be treated as a patient.
Appetite disorders.
It is important to note how sudden increased appetite - "wolfish appetite", and its sharp decrease and perversion of taste preferences. The reason may be as in the disease gastrointestinal tract, and in the general depression of the state, or painful conviction of excessive fullness in its absence. Also it is important if previously tasty food has lost its taste, has become bland, tasteless, "like cardboard."
Illusions
Do not confuse illusions with hallucinations. Illusions force a person to perceive real objects and phenomena in distorted form, while in hallucinations a person feels something that in reality does not exist.
Examples of illusions:
- the pattern on the wallpaper seems to be an interweaving of snakes or worms;
- sizes of objects are perceived in a distorted form;
- the sound of raindrops on the windowsill seems to be the careful steps of someone terrible;
- the shadows of the trees turn into terrible creatures crawling up with frightening intentions, etc.
Hallucinations not guess, then susceptibility to hallucinations can manifest itself more noticeable. Hallucinations can affect all the senses, that is be visual and auditory, tactile and gustatory, olfactory and common, as well as combined in any combination. To the sick all he is sees, hears and feels, seems completely real. He may not believe that all this is not felt, not heard, not seen by others. Them he can perceive bewilderment as a conspiracy, deceit, mockery, get irritated at not being understood.
- Auditory hallucinations human hears various kinds of noise, fragments of words or coherent phrases. Voices can give commands or comment on every action of the patient, laugh at him or discuss his thoughts.
- Taste and olfactory hallucinations often cause a sensation of an unpleasant quality: a disgusting taste or smell.
- For tactile hallucinations, the patient it seems that someone is biting him, touching him, strangling him, that they are crawling on him insects that some creatures are introduced into his body and there move or eat the body from the inside.
- Outwardly subject to hallucinations expressed in conversations with an invisible interlocutor, sudden laughter or constant intense listening to something. The patient can always to shake off something, to cry out, to examine oneself with preoccupied look or ask others if they see something on his body or in the surrounding space.
Changes in thinking
Previously uncharacteristic overestimation own abilities or abilities, confidence in one's own exclusivity, passion for esotericism, magic, suddenly appeared belief in the supernatural. The rate at which thoughts flow in the head can also change, or become uncomfortably slow, or so fast that sometimes it is very difficult to concentrate on one thought.
Delusional thoughts.
Delusional states often accompany psychoses. Delusion is based on erroneous judgments, and the patient stubbornly maintains its false belief, even if there are obvious contradictions with reality. Crazy ideas acquire significance that determines everything behavior. Delusional disorders can be expressed in an erotic form, or in the conviction of one's great mission, in descent from a noble kind or aliens. It may seem to the patient that someone is trying to kill or poison, rob or kidnap. Sometimes the development of delusional state is preceded by a feeling of unreality of the surrounding world or own personality.
Crazy ideas acquire significance that determines everything behavior. Delusional disorders can be expressed in an erotic form, or in the conviction of one's great mission, in descent from a noble kind or aliens. It may seem to the patient that someone is trying to kill or poison, rob or kidnap. Sometimes the development of delusional state is preceded by a feeling of unreality of the surrounding world or own personality.
Desocialization.
There are people who are unsociable and unsociable in strength of his character. This is normal and should not arouse suspicion. mental disorders. But if a born merry fellow, the soul company, a family man and a good friend suddenly begins to destroy social connections, becomes unsociable, shows coldness towards those who have recently was dear to him - this is a reason to worry about his mental health. A person becomes sloppy, stops taking care of himself, maybe quit your job for no good reason, abandon your career, former goals and interests, in society can begin to behave shockingly - commit acts that are considered indecent and unacceptable.
Gathering or excessive generosity
Yes, any collector can be suspicion. Especially in cases where the gathering becomes obsession, subjugates the whole life of a person. It may expressed in the desire to drag into the house things found in the garbage, hoarding products without paying attention to expiration dates, or pick up stray animals in numbers that exceed the ability provide them with proper care and maintenance.
Desire to distribute all one's property, excessive spending can also be regarded as suspicious symptom. Especially in the case when a person was not different before generosity or altruism. Particular attention should be paid to this a condition, especially when a person begins to unexpectedly actively attend banks and make loans.
Mental disorders that are difficult to treat
Since the world was first concerned with the diagnosis and treatment of mental disorders, science has advanced a lot. Many drugs have been developed that stop and reduce the symptoms of diseases. Modern methods of psychotherapy were also proposed that correct the emotional state of patients and allow them to live a full life. But, unfortunately, not all diseases can be cured with the help of modern psychotherapy and medicines. The causes of many disorders remain unknown, and the problems of their treatment remain unresolved. Below we will talk about several mental illnesses that are still difficult to treat.
Modern methods of psychotherapy were also proposed that correct the emotional state of patients and allow them to live a full life. But, unfortunately, not all diseases can be cured with the help of modern psychotherapy and medicines. The causes of many disorders remain unknown, and the problems of their treatment remain unresolved. Below we will talk about several mental illnesses that are still difficult to treat.
Why drugs and psychotherapy don't work?
Beginning in the 1980s, scientists began to actively conduct research to understand which types of psychotherapy work for certain diseases. Cognitive behavioral therapy has been shown to work best for panic attacks, anxiety disorders, phobias, and mild depression, and modern dynamic psychotherapy has been shown to work best for personality disorders. Unfortunately, researchers have not found answers to all questions, and have not developed effective methods for treating certain disorders, so psychotherapy works selectively and does not always help.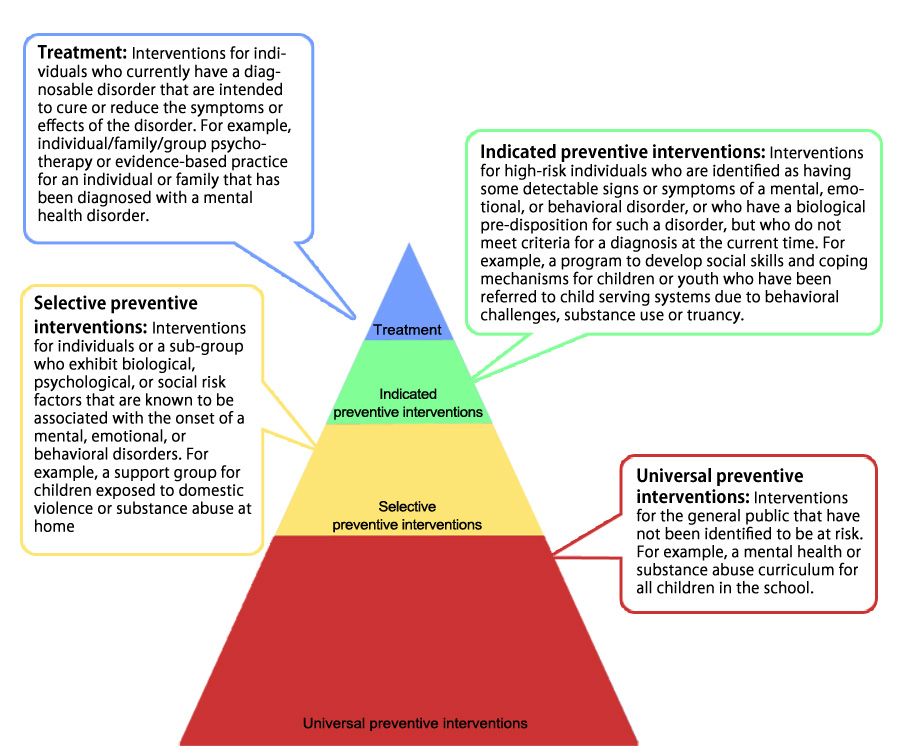
There are conditions that do not require medication, such as personality disorders, mild anxiety disorders, and mild depression.
Modern science does not know enough how the biochemistry of the brain works. This makes it difficult to develop drugs to treat psychiatric disorders. For those diseases that are not treated properly, most likely, they simply have not yet picked up effective drugs. Specialists do not know which biochemical processes are disturbed in certain diseases. There are conditions that do not require medication, such as personality disorders, mild anxiety disorders, and mild depression. In these cases, it is sufficient to use psychotherapy for treatment. But it also happens that psychotherapy is chosen only because there is simply no medical treatment for a mental disorder. In such situations, the psychologist, if not helping to treat the disorder itself, then at least provides psychological support to the patient and human participation in his condition.
One of the most important factors in effective treatment is the motivation of the patient and the environment in which he lives. After all, the patient works with a psychotherapist once or twice a week, and between sessions he is not always in an atmosphere where he is supported and helped to cope with his illness. The most important condition for effective treatment is the desire of the patient and a supportive, positive atmosphere around him.
Why is depression so difficult to cure?
There are many different types of depression: mild depression, clinical depression, recurrent depression, postpartum depression, and so on. Studies show that one of the main reasons for the development of almost all types of depression is a genetic predisposition. Scientists achieve more and more new results, pointing to some genes, then to others, then to entire commonwealths of genes that can cause depressive states. However, at the moment it has not been possible to reach a general conclusion about which genes or set of genes are responsible for depression.
See also
Myths about psychotherapy
Depression appears to be biochemically distinct, which is why treatment for one depression cannot be applied to all others. The stronger the symptoms of the disease, the more difficult it is to treat, and this is due to biological factors and the work of the brain. In a person prone to depression, certain processes occur in the brain, and only by understanding and studying these processes can effective treatment be found.
Why are mental disorders in the elderly difficult to treat?
The main reason for the development of mental disorders in old age is the peculiarities of changes in biochemical processes in the brain. This is also associated with a decrease in cognitive functions and emotional detachment from society. Science does not fully understand the biochemical structure of the brain, so at the moment there are no effective drugs in the field of psychogerontology. The most important part of the treatment of such disorders is psychotherapy, but finding the right specialist is not easy. It is important to contact a qualified psychotherapist who specializes specifically in working with older people. This is a completely separate area of specialization, working with a worldview and values that are different from young people and middle-aged patients. But if you manage to meet such a specialist, psychotherapy works in almost all cases. The exception is when an elderly patient lives outside of psychotherapy sessions in an atmosphere where he is not supported. Or if a person is lonely and his loneliness exacerbates the disease. In such cases, it is very important to work not only with the patient himself, but also with his family and environment.
The most important part of the treatment of such disorders is psychotherapy, but finding the right specialist is not easy. It is important to contact a qualified psychotherapist who specializes specifically in working with older people. This is a completely separate area of specialization, working with a worldview and values that are different from young people and middle-aged patients. But if you manage to meet such a specialist, psychotherapy works in almost all cases. The exception is when an elderly patient lives outside of psychotherapy sessions in an atmosphere where he is not supported. Or if a person is lonely and his loneliness exacerbates the disease. In such cases, it is very important to work not only with the patient himself, but also with his family and environment.
Why is it difficult to treat delusions and hallucinations?
About 10-15% of patients suffering from hallucinations and delusions cannot be cured. For example, often such a stable mental state is characteristic of patients with paranoia. Such conditions are extremely difficult to treat, again due to the fact that they are caused by biological processes.
Such conditions are extremely difficult to treat, again due to the fact that they are caused by biological processes.
People suffering from hypochondria are completely concentrated on themselves and their bodily sensations, which are constantly looking for confirmation. In a normal situation, a person usually focuses on what is happening around him and on other people.
All specialists can do is reduce the intensity of delusions or hallucinations and help the person learn the rules of behavior in society. In fact, the patient continues to believe in what he thinks, but at the same time he learns to interact with others and behave adequately in society. Such a person ceases to prove his case to everyone around and convince others that his delusions and hallucinations are real, and in this case he can continue to live a normal life, but the disease itself will not go anywhere.
Why is hypochondria difficult to treat?
People suffering from hypochondria are completely concentrated on themselves and their bodily sensations, for which they are constantly looking for confirmation.