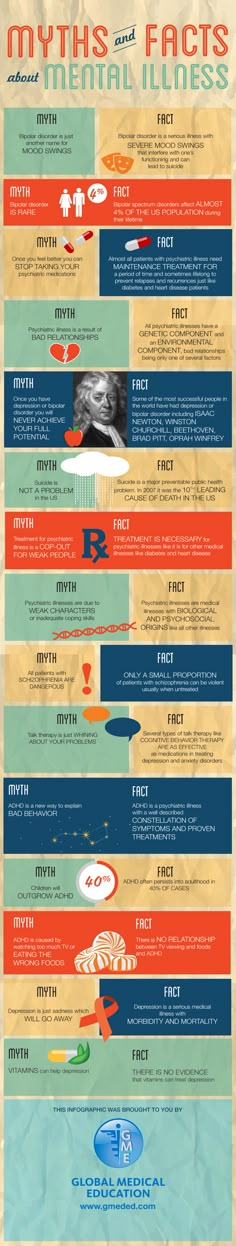
Most effective bipolar treatment
The Most Effective Treatment for Severe Bipolar Disorder & Addiction
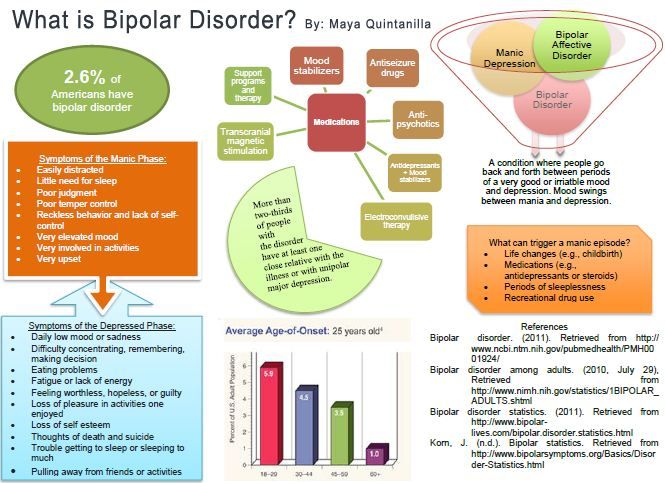
Extreme fluctuations in mood and energy levels are the hallmark signs of bipolar disorder, a form of mental illness that causes severe psychological instability.
Bipolar disorder involves more than just typical mood swings; it causes dramatic changes in emotional states, cognitive functioning, judgment, and behavior. People with bipolar disorder can veer from a depressed state to a manic high in a matter of weeks or even days, depending on the type of the disorder and the nature of their episodes. The effects of bipolar disorder are wide-ranging, causing relationship conflicts, occupational difficulties, an increased risk of suicide, and an overall decline in quality of life.
The incidence of substance abuse is higher among individuals with bipolar disorder than among the population as a whole. The National Alliance on Mental Illness states that over half of people with bipolar disorder (56 percent) have a history of illicit drug abuse, while 44 percent have abused or are dependent on alcohol. When severe bipolar disorder co-occurs with drug or alcohol addiction, the potential for negative outcomes increases. A combination of therapies — including psychiatric medications, individual and group therapy, and intensive substance abuse treatment — can help these clients achieve a sense of inner balance and create more satisfying, productive lives.
Detecting the Signs of Bipolar Disorder
Bipolar disorder can be difficult to identify, especially in people who abuse drugs or alcohol. The extreme mood swings caused by this psychiatric disorder can resemble the highs and lows that individuals experience during periods of intoxication or withdrawal from substances. By the same token, substance abuse can intensify the highs and lows of bipolar disorder, making it hard to know whether these mood swings are chemically or psychologically induced.
The changes caused by bipolar disorder are much more drastic than the mood swings that average adults experience throughout their lives.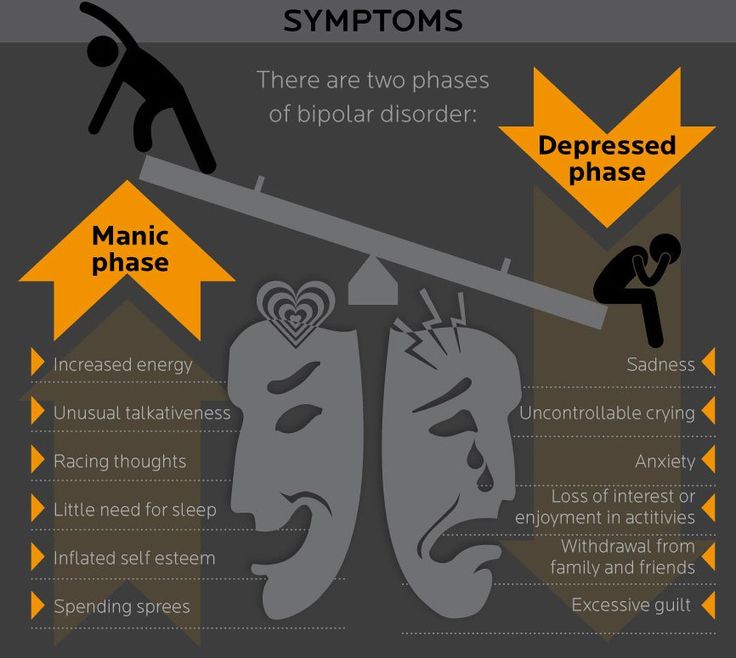 Although these fluctuations may follow certain patterns, they often strike in unpredictable ways, leaving the individual feeling out of control. Similarly, loved ones, coworkers, or acquaintances may feel helpless when confronted by these dramatic changes in the individual’s personality. The red flags of bipolar disorder can be divided into depressive and manic symptoms:
Although these fluctuations may follow certain patterns, they often strike in unpredictable ways, leaving the individual feeling out of control. Similarly, loved ones, coworkers, or acquaintances may feel helpless when confronted by these dramatic changes in the individual’s personality. The red flags of bipolar disorder can be divided into depressive and manic symptoms:
Symptoms of bipolar disorder can vary from one individual to another.
Substance abuse may occur in either a manic or depressive state. When individuals are in a manic phase, they may use stimulants like methamphetamine or cocaine to prolong this high-energy period or depressants like alcohol or tranquilizers to calm down. In a depressive phase, sedatives or depressants may be used to calm feelings of hopelessness, while stimulants may be used to elevate mood.
Addiction and Bipolar Disorder
In an attempt to regulate these changes in mood and energy, individuals with bipolar disorder may abuse drugs or alcohol. According to the Journal of Clinical Psychiatry, up to 70 percent of people who meet the criteria for bipolar disorder also have a history of substance abuse — a percentage that far exceeds the general population. Substance abuse affects the outcomes of bipolar disorder in several ways:
According to the Journal of Clinical Psychiatry, up to 70 percent of people who meet the criteria for bipolar disorder also have a history of substance abuse — a percentage that far exceeds the general population. Substance abuse affects the outcomes of bipolar disorder in several ways:
- Intensification of symptoms (mood swings, poor judgment, impulsivity, hostility, and irritability)
- Longer episodes of emotional instability
- Increased number of suicide attempts
- Diminished quality of life
Treating bipolar disorder and substance abuse can be complex, requiring intensive attention to the symptoms of mental illness as well as the behaviors associated with addiction. The results of treatment for individuals with dual diagnoses, or a mental illness co-occurring with a substance use disorder, are generally much better if both conditions are treated at the same time, within the same program. In order to provide the most effective care, staff should be cross-trained in mental health care and substance abuse treatment.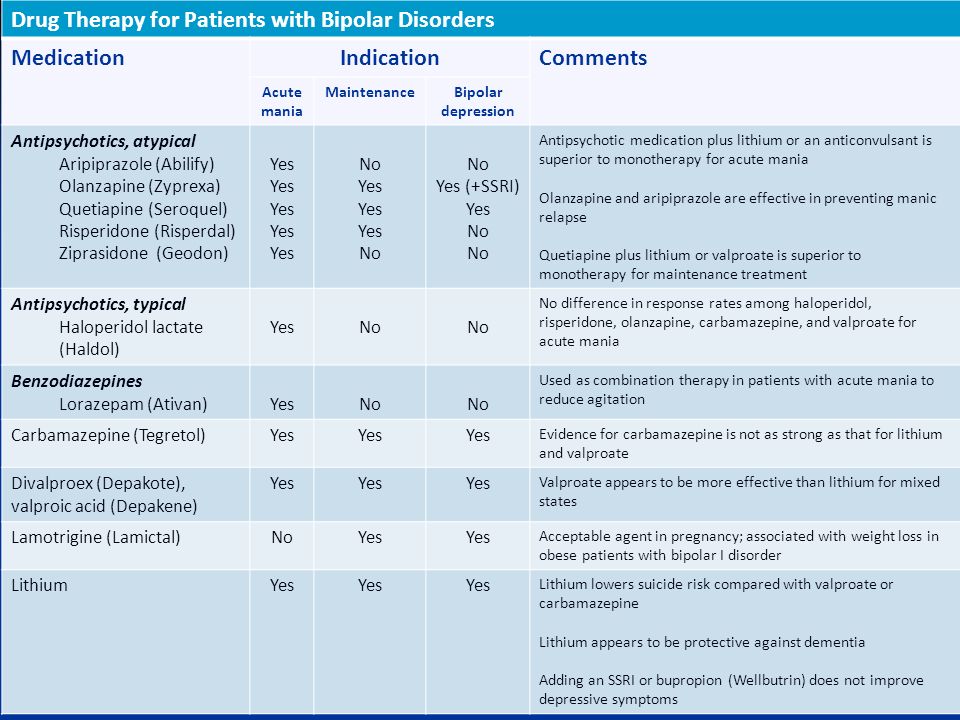
Addressing Addiction and Bipolar
The Centers for Disease Control and Prevention notes that the psychological and physical impairment caused by bipolar disorder make it the most expensive behavioral health diagnosis, both in terms of health care costs and loss of quality of life. Individuals with bipolar disorder may feel misunderstood, stigmatized, or isolated because of their illness. The disorder can have a negative impact on all aspects of a person’s life, from occupational functioning to the quality of relationships. Having the support and concern of a close friend or family member can make a significant difference in the outcome of treatment.
Many people feel uncomfortable about broaching the subjects of mental illness and addiction with a loved one. However, it is important to remember that the course of addiction and bipolar disorder will rarely improve without professional intervention. Expressing concern to a loved one may feel awkward or embarrassing at first, but this conversation could make a significant difference in the outcome of the disease.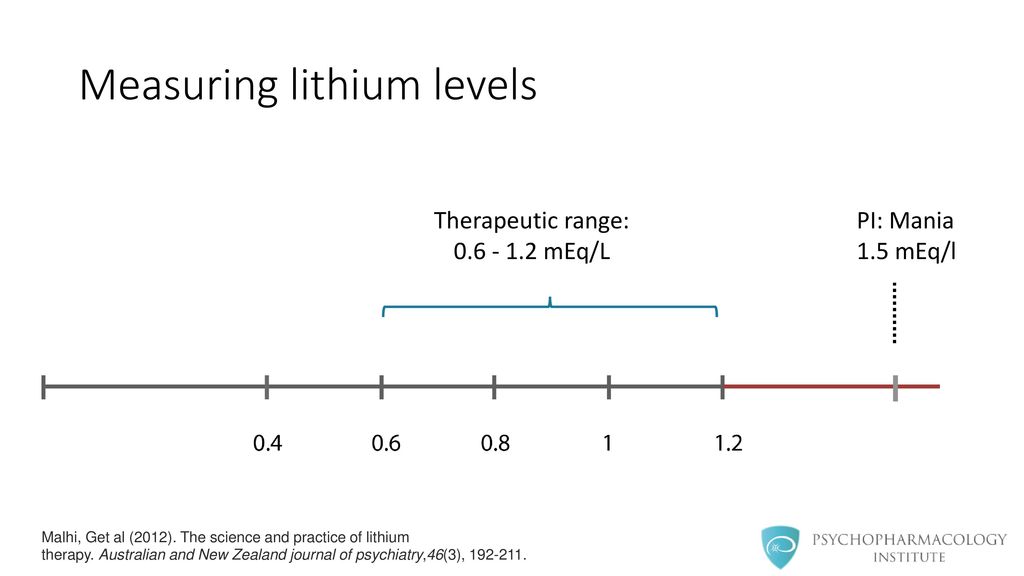
Too often, the official diagnosis of bipolar disorder comes years after the individual has first experienced symptoms. The Journal of Clinical Psychiatry states that most people with the disorder do not receive treatment until at least six years after having their first episode. Because of this delay, symptoms tend to be more extreme and relapse is more common in the early stages of treatment. Intervening on behalf of a loved one who is displaying the signs of bipolar disorder and substance abuse could prevent these unnecessary delays and expedite the process of recovery.
Exploring Treatment Options
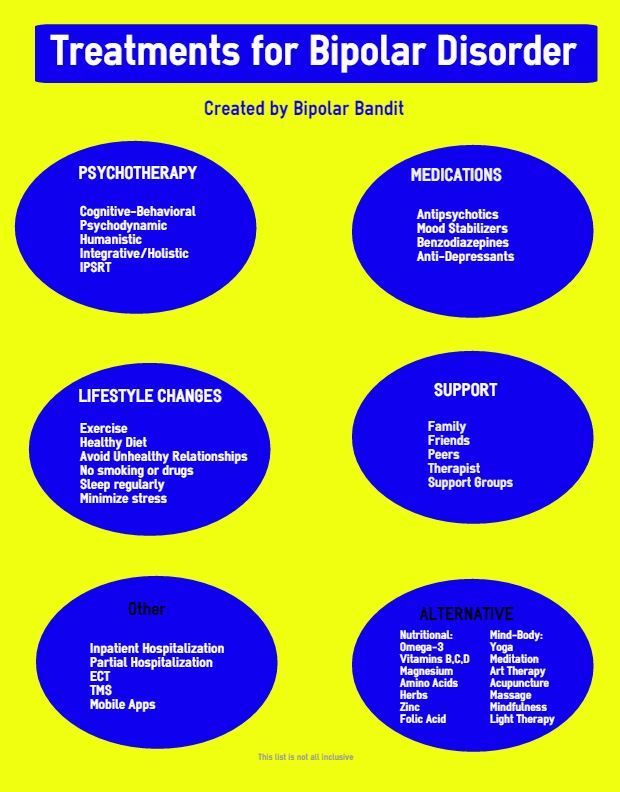
Bipolar disorder is a complex psychiatric condition, especially when combined with a substance use disorder. Treatment should draw from multiple modalities and disciplines to address the client’s neurological, psychological, physical, and psychosocial needs. In addition to intensive individual therapy, clients with dual diagnoses of bipolar disorder and addiction can benefit from the following research-based interventions:
- Motivational Interviewing (MI): Motivational Interviewing is a collaborative approach in which the therapist and client become partners in helping the client define sources of motivation and achieve self-defined goals.
 This positive, client-centered approach is especially useful in treating individuals who are working to recover from the effects of addiction. A study published in Issues in Mental Health Nursing showed that MI can help clients with bipolar disorder overcome ambivalent feelings about taking psychiatric medication.
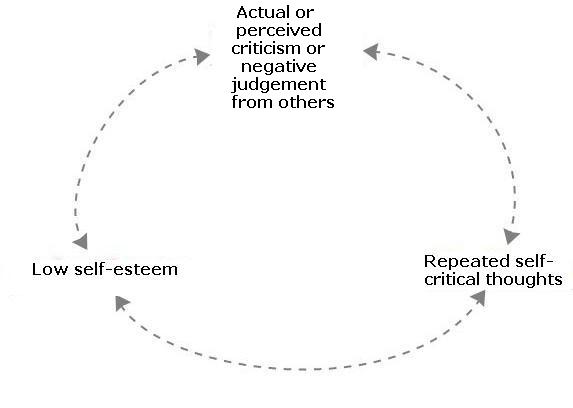
This positive, client-centered approach is especially useful in treating individuals who are working to recover from the effects of addiction. A study published in Issues in Mental Health Nursing showed that MI can help clients with bipolar disorder overcome ambivalent feelings about taking psychiatric medication. - Cognitive Behavioral Therapy (CBT): CBT addresses the learned thought patterns and destructive behaviors that contribute to addiction, depression, and anxiety. Clients learn to identify self-defeating thoughts and actions, and replace them with more positive, self-affirming coping strategies.
- Solution-Focused Therapy (SFT): This practical, client-centered modality helps individuals with mental illness and addiction set and achieve specific goals. Rather than delving deeply into the origins of mental health issues or substance abuse, SFT focuses on measurable outcomes of therapy.
- Trauma therapies: A history of trauma, childhood abuse, violence, or chaotic living environments can increase the severity of bipolar disorder.
 Trauma therapies such as Seeking Safety and Eye Movement Desensitization Reprocessing (EMDR) target the unprocessed memories and internalized fears that can intensify anxiety or depression.
Trauma therapies such as Seeking Safety and Eye Movement Desensitization Reprocessing (EMDR) target the unprocessed memories and internalized fears that can intensify anxiety or depression.
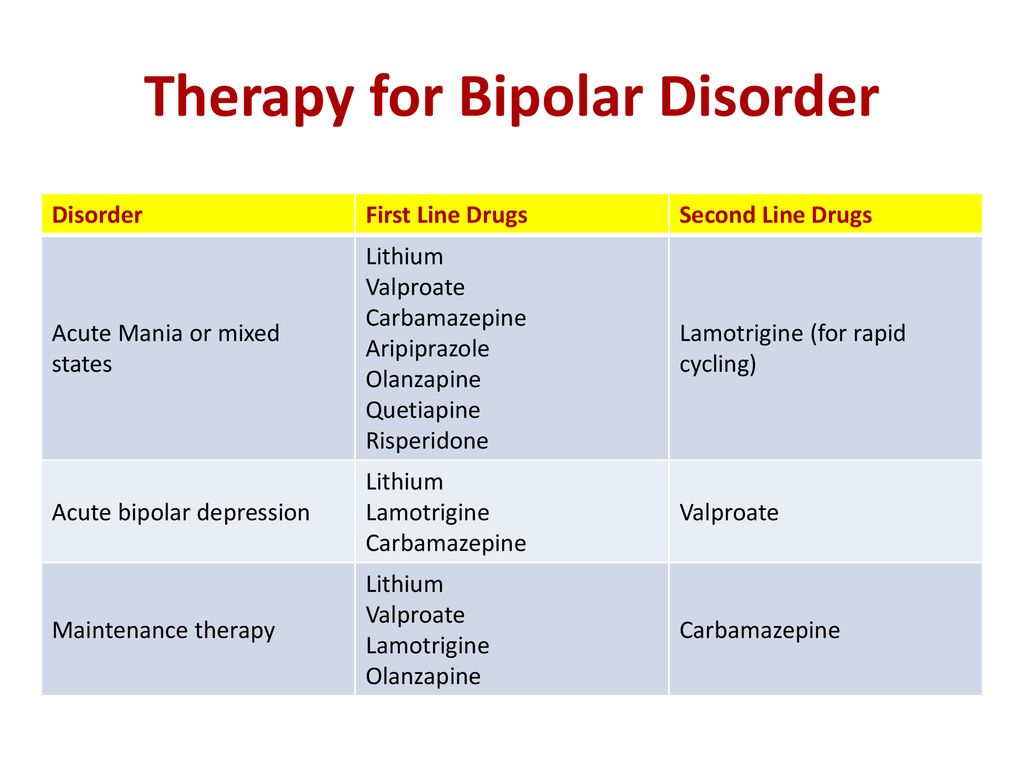
For many individuals with bipolar disorder, medication therapy is highly effective at controlling symptoms. By stabilizing moods and restoring balance to energy levels, psychiatric medications can also help to curb the impulse to abuse alcohol or drugs. Medications must be selected and adjusted carefully, as certain types of drugs can trigger manic episodes or worsen depression. The antidepressants that are used successfully to treat major depression, for example, may not be effective at treating bipolar depression and can actually induce a manic phase in bipolar patients, especially if they are used without other medications. The most common drugs used to treat bipolar disorder fall into the following categories:
- Mood stabilizers: Lithium is the most widely prescribed mood-stabilizing medication for bipolar disorder.
 Lithium is most effective at preventing or reducing the severity of manic episodes and may be prescribed in combination with other medications.
Lithium is most effective at preventing or reducing the severity of manic episodes and may be prescribed in combination with other medications. - Anticonvulsant drugs: Anti-seizure medications such as divalproex (Depakote), lamotrigine (Lamictal), carbamazepine (Tegretol), and topiramate (Topamax) are also prescribed to prevent mood instability in individuals with bipolar disorder. These drugs are especially useful at reducing the frequency and severity of depressive episodes.
- Antipsychotic medications: Quetiapine (Seroquel), risperidone (Risperdal), olanzapine (Zyprexa), and aripiprazole (Abilify) are some of the most common antipsychotic medications used to treat the effects of bipolar disorder. These medications help to minimize the delusional thought patterns and erratic moods that characterize manic phases.
- Additional medications: In addition to psychiatric medications, pharmacologic treatment for bipolar disorder may involve medications that address the physical symptoms that can contribute to bipolar symptoms.
 These include certain blood pressure medications that slow down the activity of the central nervous system and medications that help to correct hormonal imbalances.
These include certain blood pressure medications that slow down the activity of the central nervous system and medications that help to correct hormonal imbalances.
In order to provide comprehensive care for a client with a dual diagnosis, substance abuse treatment should occur at the same time, through the same program.
This integrated approach to treatment represents a departure from older schools of thought, which maintained that substance abuse treatment and mental health were separate, distinct fields. Today, integrated rehabilitation programs incorporate therapy for bipolar disorder and other forms of mental illness with addiction treatment. Addiction treatment services include:
- Medical detox (inpatient or outpatient)
- Inpatient treatment
- Residential services
- Partial hospitalization programs
- Outpatient programs
In the early stages of rehab, many clients need the structure and supervision of an inpatient or residential treatment program. After establishing a foundation for recovery and completing the intensive, initial work of rehab, clients may make the transition to outpatient services, which provide more flexibility and autonomy.
After establishing a foundation for recovery and completing the intensive, initial work of rehab, clients may make the transition to outpatient services, which provide more flexibility and autonomy.
Find Dual Diagnosis Treatment Near You
Seeking Help
Both bipolar disorder and addiction are complex, multifaceted conditions that affect all aspects of the individual’s life. Like bipolar disorder, addiction is a progressive illness that increases in severity if left untreated. In order to provide comprehensive care and maximize the outcomes of therapy, a rehab program should offer services for both substance abuse and mental health treatment. With a combination of research-based therapeutic modalities, pharmaceutical interventions, and psychosocial services, the outcomes of bipolar disorder and addiction can improve significantly.
Treatment - Bipolar disorder - NHS
Treatment for bipolar disorder aims to reduce the severity and number of episodes of depression and mania to allow as normal a life as possible.
Treatment options for bipolar disorder
If a person is not treated, episodes of bipolar-related mania can last for between 3 and 6 months.
Episodes of depression tend to last longer, often 6 to 12 months.
But with effective treatment, episodes usually improve within about 3 months.
Most people with bipolar disorder can be treated using a combination of different treatments.
These can include 1 or more of the following:
- medicine to prevent episodes of mania and depression – these are known as mood stabilisers, and you take them every day on a long-term basis
- medicine to treat the main symptoms of depression and mania when they happen
- learning to recognise the triggers and signs of an episode of depression or mania
- psychological treatment – such as talking therapies, which help you deal with depression and provide advice on how to improve relationships
- lifestyle advice – such as doing regular exercise, planning activities you enjoy that give you a sense of achievement, and advice on improving your diet and getting more sleep
Most people with bipolar disorder can receive most of their treatment without having to stay in hospital.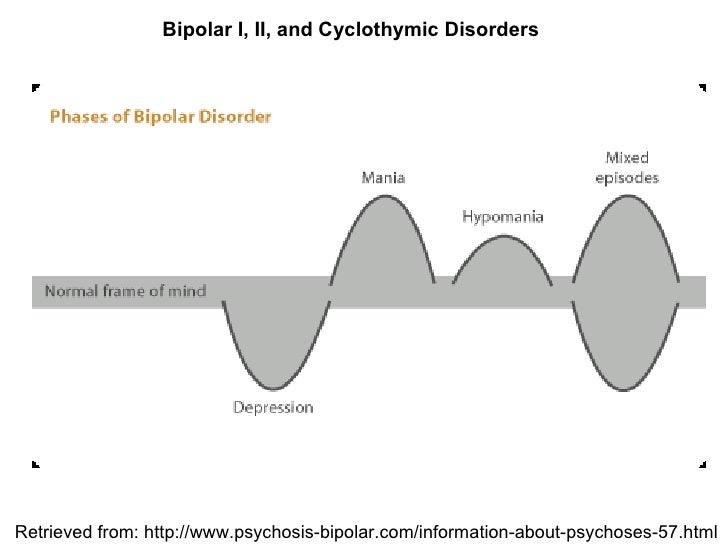
But hospital treatment may be needed if your symptoms are severe or you're being treated under the Mental Health Act, as there's a danger you may self-harm or hurt others.
In some circumstances, you could have treatment in a day hospital and return home at night.
Medicines for bipolar disorder
Several medicines are available to help stabilise mood swings.
These are commonly called mood stabilisers and include:
- lithium
- anticonvulsant medicines
- antipsychotic medicines
If you're already taking medicine for bipolar disorder and you develop depression, your GP will check you're taking the correct dose. If you're not, they'll change it.
Episodes of depression are treated slightly differently in bipolar disorder, as taking antidepressants alone may lead to a relapse.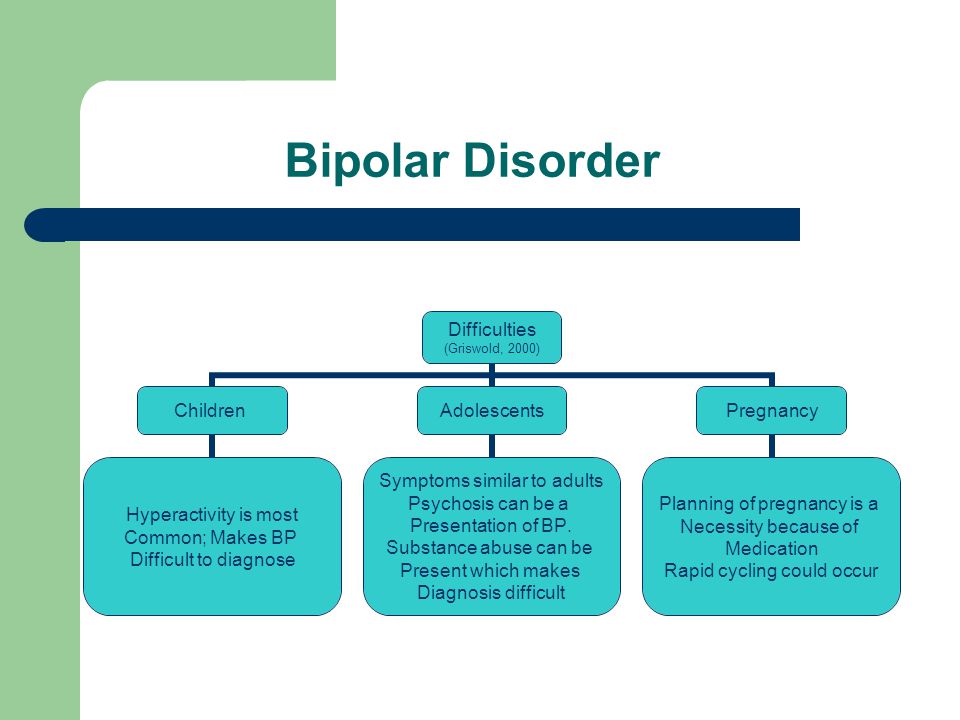
Most guidelines suggest depression in bipolar disorder can be treated with just a mood stabiliser.
But antidepressants are commonly used alongside a mood stabiliser or antipsychotic.
Find out more about antidepressants
If your GP or psychiatrist recommends you stop taking bipolar disorder medicine, the dose should be gradually reduced over at least 4 weeks, and up to 3 months if you're taking an antipsychotic or lithium.
If you have to stop taking lithium for any reason, talk to your GP about taking an antipsychotic or valproate instead.
Lithium
In the UK, lithium is the main medicine used to treat bipolar disorder.
Lithium is a long-term treatment for episodes of mania and depression. It's usually prescribed for at least 6 months.
If you're prescribed lithium, stick to the prescribed dose and do not stop taking it suddenly unless told to by your doctor.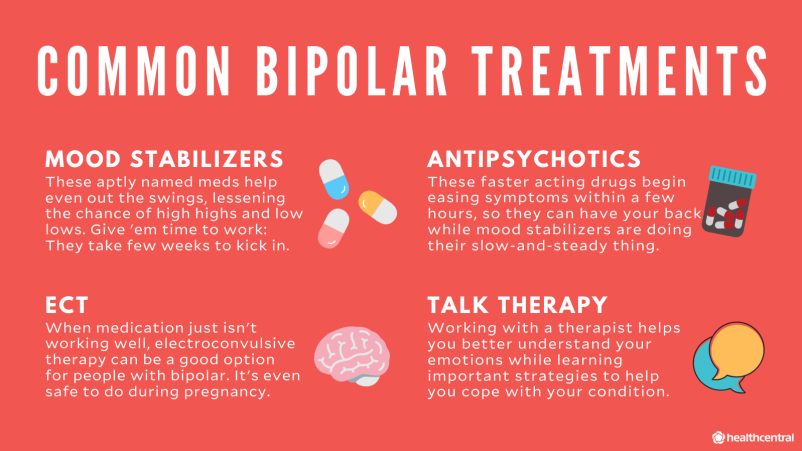
For lithium to be effective, the dosage must be correct. If it's incorrect, you may get side effects such as diarrhoea and getting sick.
Tell your doctor immediately if you have side effects while taking lithium.
You'll need regular blood tests at least every 3 months while taking lithium. This is to make sure your lithium levels are not too high or too low.
Your kidney and thyroid function will also need to be checked every 2 to 3 months if the dose of lithium is being adjusted, and every 12 months in all other cases.
While you're taking lithium, avoid using non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, unless they're prescribed by your GP.
In the UK, lithium and the antipsychotic medicine aripiprazole are currently the only medicines that are officially approved for use in teenagers with bipolar disorder.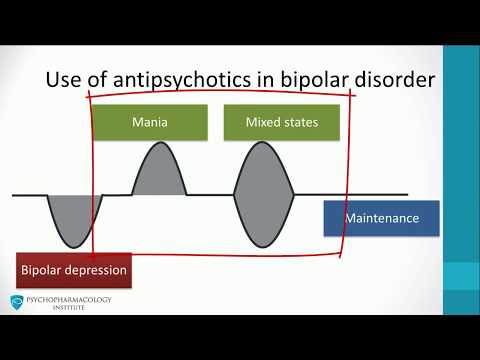
But the Royal College of Paediatrics and Child Health says that other bipolar medicines may be prescribed for children if recommended by their doctor.
Anticonvulsant medicines
Anticonvulsant medicines include:
- valproate
- carbamazepine
- lamotrigine
These medicines are sometimes used to treat episodes of mania. They're also long-term mood stabilisers.
Anticonvulsant medicines are often used to treat epilepsy, but they're also effective in treating bipolar disorder.
A single anticonvulsant medicine may be used, or they may be used in combination with lithium when bipolar disorder does not respond to lithium on its own.
Valproate
Valproate is not usually prescribed for women of childbearing age because there's a risk of physical defects in babies, such as spina bifida, heart abnormalities and cleft lip.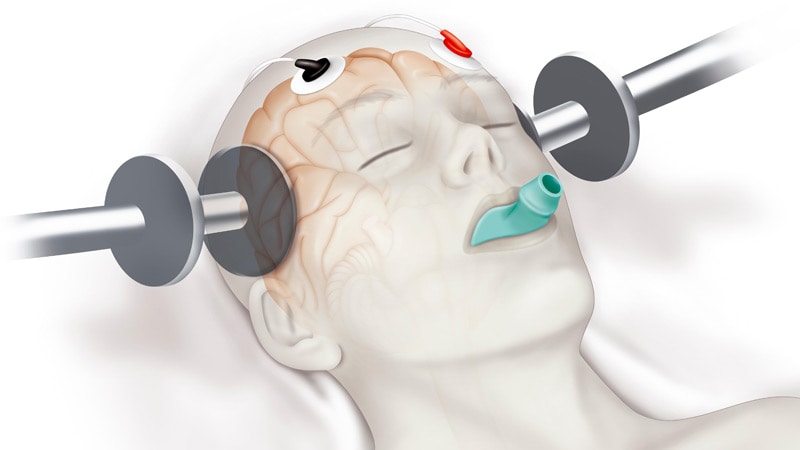
There may also be an increased risk of developmental problems, such as lower intellectual abilities, poor speaking and understanding, memory problems, autistic spectrum disorders, and delayed walking and talking.
Learn more about the risks of valproate medicines during pregnancy
In women, your GP may decide to use valproate if there's no alternative or you have been assessed and it's unlikely you'll respond to other treatments.
They'll need to check you're using a reliable contraception and will advise you on the risks of taking the medicine during pregnancy.
Find out more about pregnancy and taking medicine for a mental health condition
Carbamazepine
Carbamazepine is usually only prescribed on the advice of an expert in bipolar disorder. To begin with, the dose will be low and then gradually increased.
Your progress will be carefully monitored if you're taking other medication, including the contraceptive pill.
Blood tests to check your liver and kidney function will be carried out when you start taking carbamazepine and again after 6 months.
You'll also need to have a blood count at the start and after 6 months, and you may also have your weight and height monitored.
Lamotrigine
If you're prescribed lamotrigine, you'll usually be started on a low dose, which will be increased gradually.
See your GP straight away if you're taking lamotrigine and develop a rash. You'll need to have an annual health check, but other tests are not usually needed.
Women who are taking the contraceptive pill should talk to their GP about switching to a different method of contraception.
Antipsychotic medicines
Antipsychotic medicines are sometimes prescribed to treat episodes of mania.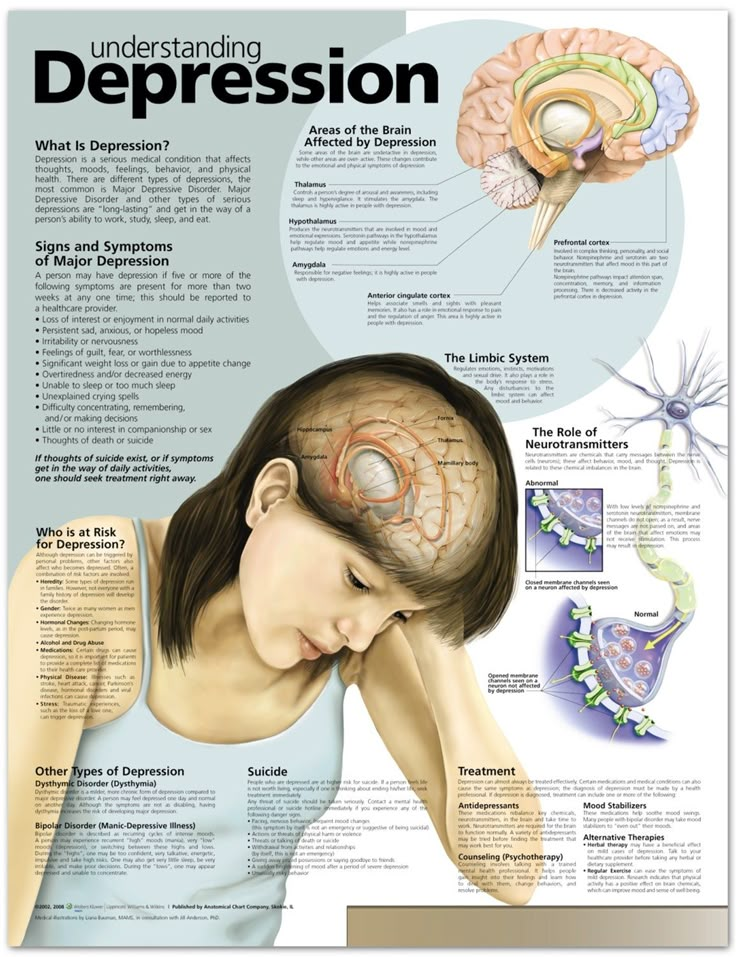
They include:
- aripiprazole
- olanzapine
- quetiapine
- risperidone
They may also be used as a long-term mood stabiliser. Quetiapine may also be used for long-term bipolar depression.
Antipsychotic medicines can be particularly useful if symptoms are severe or behaviour is disturbed.
As antipsychotics can cause side effects, such as blurred vision, a dry mouth, constipation and weight gain, the initial dose will usually be low.
If you're prescribed an antipsychotic medicine, you'll need to have regular health checks at least every 3 months, but possibly more often, particularly if you have diabetes.
If your symptoms do not improve, you may be offered lithium and valproate as well.
Rapid cycling
You may be prescribed a combination of lithium and valproate if you experience rapid cycling, where you quickly change from highs to lows without a "normal" period in between.
If this does not help, you may be offered lithium on its own, or a combination of lithium, valproate and lamotrigine.
But you will not usually be prescribed an antidepressant unless an expert in bipolar disorder has recommended it.
Learning to recognise triggers
If you have bipolar disorder, you can learn to recognise the warning signs of an approaching episode of mania or depression.
A community mental health worker, such as a psychiatric nurse, may be able to help you identify your early signs of relapse from your history.
This will not prevent the episode occurring, but it'll allow you to get help in time.
This may mean making some changes to your treatment, perhaps by adding an antidepressant or antipsychotic medicine to the mood-stabilising medication you're already taking.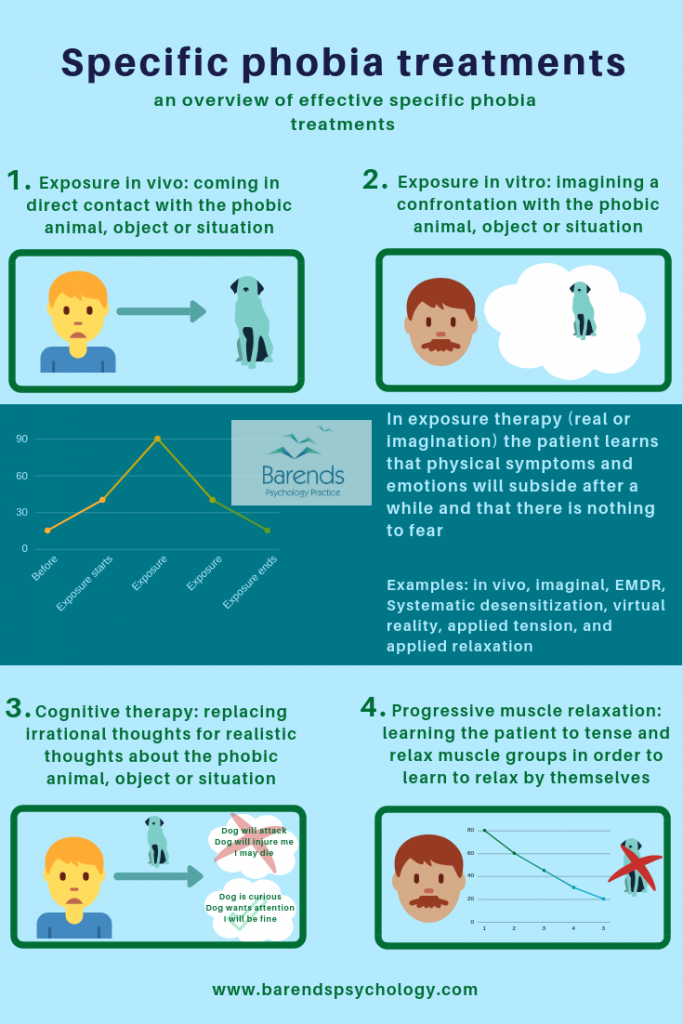
Your GP or specialist can advise you on this.
Psychological treatment
Some people find psychological treatment helpful when used alongside medicine in between episodes of mania or depression.
This may include:
- psychoeducation – to find out more about bipolar disorder
- cognitive behavioural therapy (CBT) – this is most useful when treating depression
- family therapy – a type of talking therapy that focuses on family relationships (such as marriage) and encourages everyone within the family or relationship to work together to improve mental health
Psychological treatment usually consists of around 16 sessions. Each session lasts an hour and takes place over a period of 6 to 9 months.
Pregnancy and bipolar medicines
One of the main problems is that the risks of taking bipolar medicines during pregnancy are not well understood.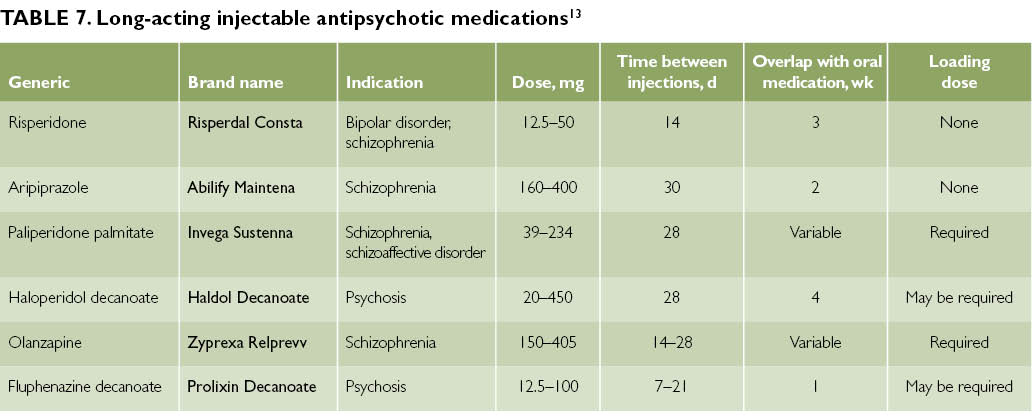
If you're pregnant and you have bipolar disorder, a written plan for your treatment should be developed as soon as possible.
The plan should be drawn up with you, your partner, your obstetrician (pregnancy specialist), midwife, GP and health visitor.
The following medicines are not routinely prescribed for pregnant women with bipolar disorder, as they may harm the baby:
- valproate
- carbamazepine
- lithium
- lamotrigine
- paroxetine
- benzodiazepines (tranquillisers), such as diazepam (Valium) and lorazepam (Ativan)
If you become pregnant while taking medicine that's been prescribed for bipolar disorder, it's important that you do not stop taking it until you have discussed it with your doctor.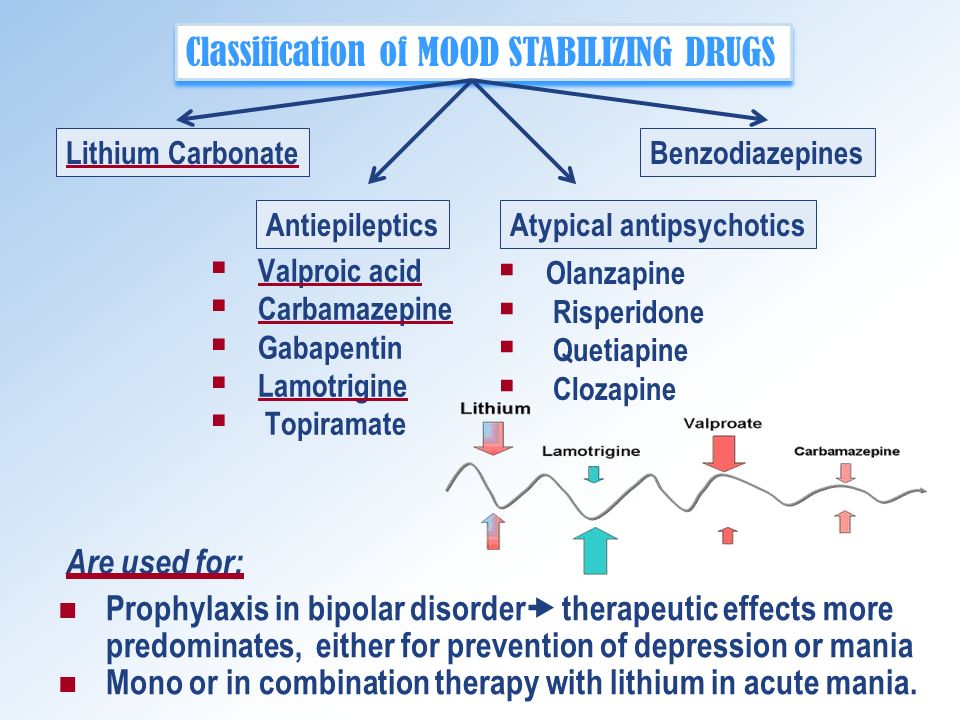
If bipolar medicine is prescribed for bipolar disorder after the baby's born, it may also affect your decision whether to breastfeed.
Your pharmacist, midwife or mental health team can give you advice based on your circumstances.
What is the treatment for bipolar disorder? - Bipolar.su
Translation of a chapter from the book “Life with Bipolar Disorder. A guide for people with bipolar disorder and their families”
This chapter will discuss medications that are commonly used to treat bipolar disorder.
It is important for you, as an active participant in the treatment, to know the purpose of the therapy, the effect of the drugs, the appropriate dosage of the drug, possible side effects, as well as how and at what time to take the drugs (dosing regimen). This information will help you and your psychiatrist find the drugs that are best for you. Please discuss your concerns about medications with your doctor.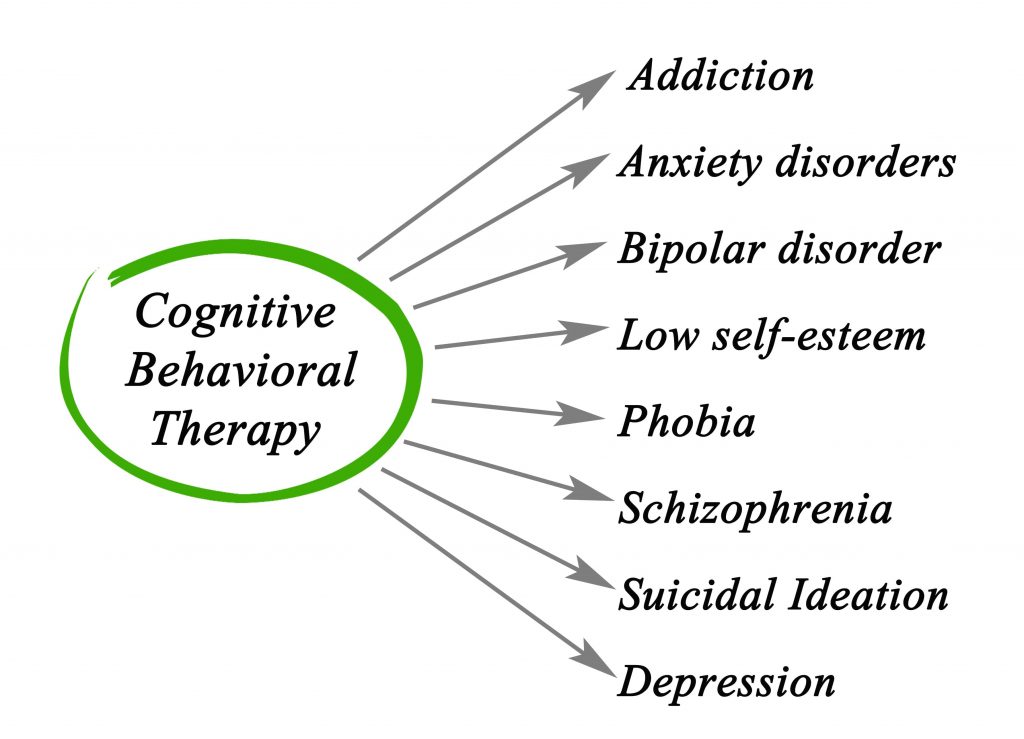 He will dispel your fears and, if necessary, help you cope with the side effects of therapy or find an alternative method of treatment.
He will dispel your fears and, if necessary, help you cope with the side effects of therapy or find an alternative method of treatment.
Do I need to take medication?
Many people have mixed feelings about taking medication; in an ideal world, they would prefer not to accept them. However, numerous studies have proven the beneficial effects of medications in the treatment and prevention of depressive and manic episodes. You can think of drugs like mood stabilizers and antidepressants as things that can help you feel better and take control of your life.
What is the treatment for bipolar disorder?
The following sections describe four types of medications used to treat bipolar disorder: mood stabilizers (normothymics), antidepressants, antipsychotics (neuroleptics), and tranquilizers (anxiolytics, anti-anxiety drugs). These drugs represent the main groups of drugs for the control of bipolar disorder, they are used individually or in combination.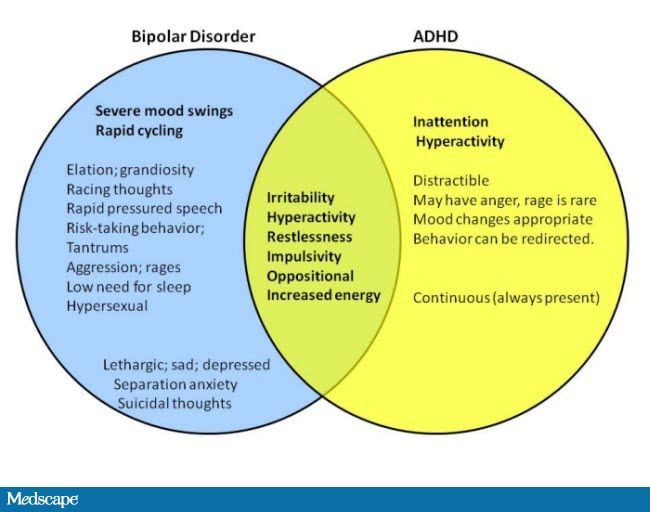 Other medications may also be used to treat other symptoms.
Other medications may also be used to treat other symptoms.
Before we describe these groups of drugs, their purposes and side effects in more detail, we would like to share information about the names of these drugs.
Drugs are often classified according to the purpose for which they were first approved (licensed) for use in the US, although many drugs have many additional uses in addition to those already approved. For example, doctors use antidepressants to treat anxiety disorders and tranquilizers to treat insomnia. For this reason, it is very important to understand the purpose of prescribing a medication, and not just know its name. This makes it easier to see the situation when you are asked about your medicines, because people only see and understand the names. For example, a family member may ask why you are taking medication for an anxiety disorder if you have bipolar disorder. Similar questions may arise when you order medicines at a pharmacy, when you communicate with friends or relatives, when you just meet with a doctor.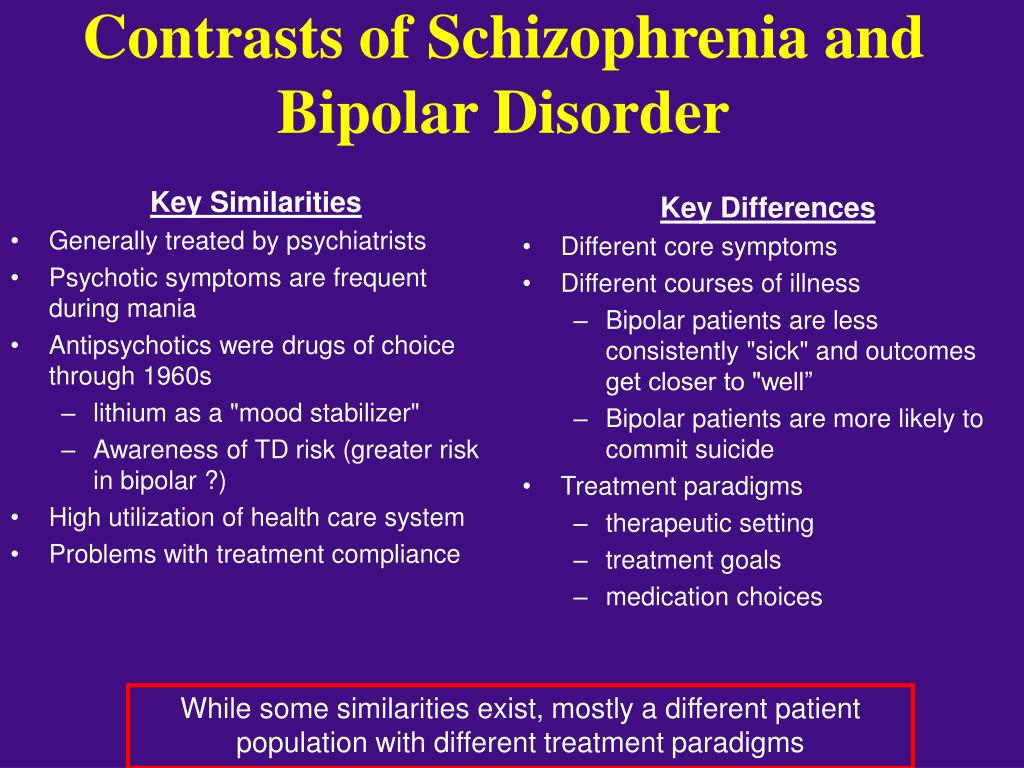 If you have questions about medications, be sure to talk to your psychiatrist before changing anything.
If you have questions about medications, be sure to talk to your psychiatrist before changing anything.
Mood Stabilizers (Mood Stabilizers)
The purpose of using mood stabilizers is to keep your mood within the normal range. While experts believe that mood stabilizers are the best group of medications for treating bipolar disorder, the term "mood stabilizer" is scientifically ambiguous. There is a mutual agreement among experts that lithium (trade name Sedalite), valproic acid + sodium valproate (Depakine), lamotrigine (Lamiktal), carbamazepine (Tegretol) and olanzapine (Zyprexa) are stabilizers moods. Each of these drugs has been shown to be effective in treating and/or preventing mania and/or depression in two or more studies. There are many studies showing that lithium is effective both in treating manias and depressions and in preventing their relapses. Several studies have proven the effectiveness of lamotrigine for the treatment of bipolar disorder and two studies have shown its ability to prevent relapses, especially in recurrent (repeated) depressive phases. Olanzapine has shown excellent ability in combating acute mania and also has some antidepressant effect and is particularly useful in preventing relapse of mania.
Olanzapine has shown excellent ability in combating acute mania and also has some antidepressant effect and is particularly useful in preventing relapse of mania.
Other medicines also have mood stabilizing properties.
To be called a mood stabilizer, a drug must: (1) work for mania, depression, or prevent relapse, and (2) not cause mood swings or abrupt transitions from one state to another. Drugs occasionally used by doctors as mood stabilizers also include verapamil (Isoptin), oxcarbazepine (Trileptal), and ω-3-polyunsaturated fatty acids (PUFAs), however, the benefits of their use are considered to be not fully proven. None of these medicines have been studied in bipolar disorder or received approval from the main regulatory body in the United States, the Food and Drug Administration (FDA).
All medicines can cause side effects. Your goal is to work with a psychiatrist to find the mood stabilizer that will best protect you or help you recover from an episode of depression or mania without uncomfortable side effects.
Antidepressants
A wide range of antidepressants can be used to control depressive episodes of bipolar disorder. However, their use should be monitored very carefully, as some patients go from depression to mania (so-called "phase inversion") when treated with antidepressants. In other words, an antidepressant used to control depression can cause mania. In contrast, some bipolar patients who take antidepressants do not experience a switch to mania, but instead suffer from worsening depression or more depressive episodes. For this reason, regular and ongoing communication with your doctor is essential to ensure that the prescribed treatment does not worsen your general condition. Your psychiatrist will watch for manic symptoms, but he/she will not be able to do his job without your help and members of your support group.
Talk to your doctor about how you feel. If during treatment with antidepressants you feel restless, excessive talkativeness, have trouble sleeping, and have a rush to run, "jump" thoughts - immediately report these symptoms to your psychiatrist. While the mood swings can be pleasant, you don't want these symptoms to turn into a full-blown mania. Remember that mania is a disease that causes problems in your life. To keep your life and your ability to achieve your goals under control, report early symptoms of mania or hypomania to your doctor. Through monitoring, antidepressant treatment can be a valuable addition to your recovery.
While the mood swings can be pleasant, you don't want these symptoms to turn into a full-blown mania. Remember that mania is a disease that causes problems in your life. To keep your life and your ability to achieve your goals under control, report early symptoms of mania or hypomania to your doctor. Through monitoring, antidepressant treatment can be a valuable addition to your recovery.
Table 3.1 lists some antidepressants. You will notice that some antidepressants are listed first because these drugs were originally developed to treat depression specifically in bipolar disorder and reduce the possibility of mania, unlike older drugs.
Antipsychotics (neuroleptics)
Antipsychotics were originally developed as a treatment for hallucinations and delusions in schizophrenia. However, antipsychotics have been shown to have specific anti-manic properties even in patients without evidence of psychosis. Antipsychotics are often prescribed for a manic episode and may be helpful in cases of disorganized behavior, confused thinking, as well as hallucinations.
A common property of these drugs is the ability to block the receptors of a neurotransmitter called dopamine. Too much dopamine in the brain can contribute to manic symptoms. You will often hear the term "neuroleptics" from doctors - this is an outdated name for antipsychotics.
Older antipsychotics, also called “typical antipsychotics,” include chlorpromazine (Aminazine), haloperidol, zuclopenthixol (Clopixol), flupentixol (Fluanxol), trifluoperazine (Triftazine), and a lot others. They are powerful blockers of dopamine receptors. They are useful in cases of acute mania. Unfortunately, they can often cause side effects that worsen their tolerability. At the beginning of the course of treatment with such drugs, patients may experience muscle stiffness, tremors in the limbs, sometimes restlessness, restlessness and agitation. Long-term use of typical antipsychotics is often associated with a potentially irreversible side effect known as tardive dyskinesia (TD), a disorder characterized by repetitive, involuntary, purposeless muscle contractions, especially of the tongue and facial muscles.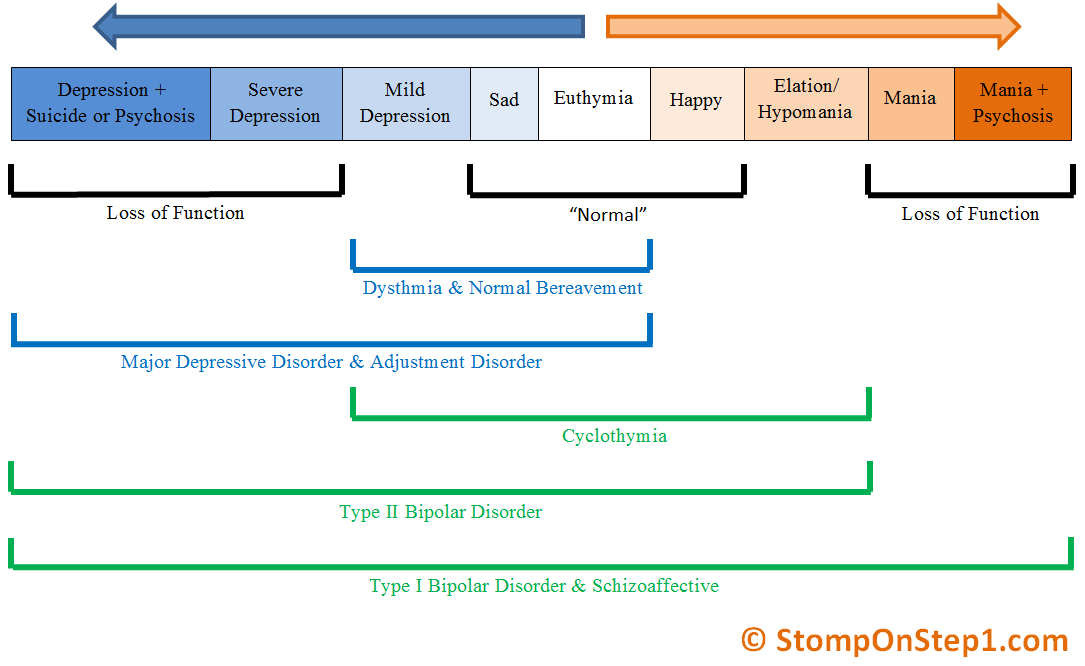
Newer antipsychotic drugs are now available for the treatment of mania, called atypical antipsychotics. Clozapine ("Azaleptin", "Klozasten") was the first synthesized drug of this class. This class also includes risperidone (Rispolept), ziprasidone (Zeldox), olanzapine (Zyprexa), quetiapine (Seroquel), aripiprazole (Abilify), asenapine (Safris) and some others. Like the older drugs, they also block dopaffin receptors, but are less powerful than typical antipsychotics. Atypical antipsychotics also block certain receptors on another neurotransmitter called serotonin. Antipsychotics with a combination of dopamine and serotonin blockade generally cause fewer side effects and are better tolerated by patients. They are often used in combination with mood stabilizers to treat acute mania.
Standard practice after recovery is to reduce the dose of the antipsychotic. Be that as it may, some patients begin to experience manic symptoms soon after the dosage is reduced. In this case, they are prescribed antipsychotics on an ongoing basis to contain the relapse of mania.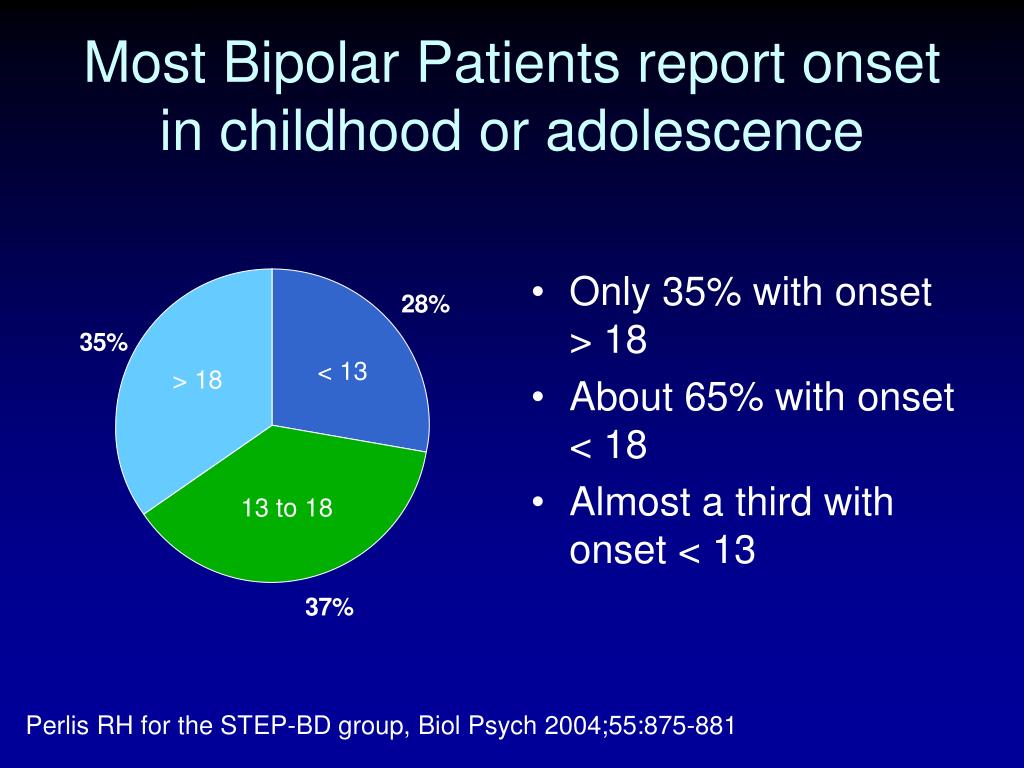 Therefore, antipsychotic drugs can be considered as the drugs of choice for the treatment of acute mania, as well as drugs for the prevention of mania and psychotic symptoms.
Therefore, antipsychotic drugs can be considered as the drugs of choice for the treatment of acute mania, as well as drugs for the prevention of mania and psychotic symptoms.
Tranquilizers (anxiolytics, anti-anxiety agents)
Anxiety is a symptom that often accompanies episodes of depression and mania. In addition, sleep problems are also common in depression, hypomania, and mania. Benzodiazepines are the most commonly used tranquilizers. These include lorazepam (Lorafen), clonazepam, diazepam (Relium, Sibazon), alprazolam, chlordiazepoxide (Elenium), and phenazepam. They are used to quickly reduce anxiety and insomnia. Benzodiazepines may also control early symptoms of hypomania. All these drugs can cause addiction, physical and psychological dependence, especially when taken uncontrolled. The potential for abuse is greater for potent drugs that are rapidly absorbed into the bloodstream, such as alprazolam. The incidence of abuse is somewhat less with the milder, longer-acting benzodiazepines (eg, chlordiazepoxide, diazepam).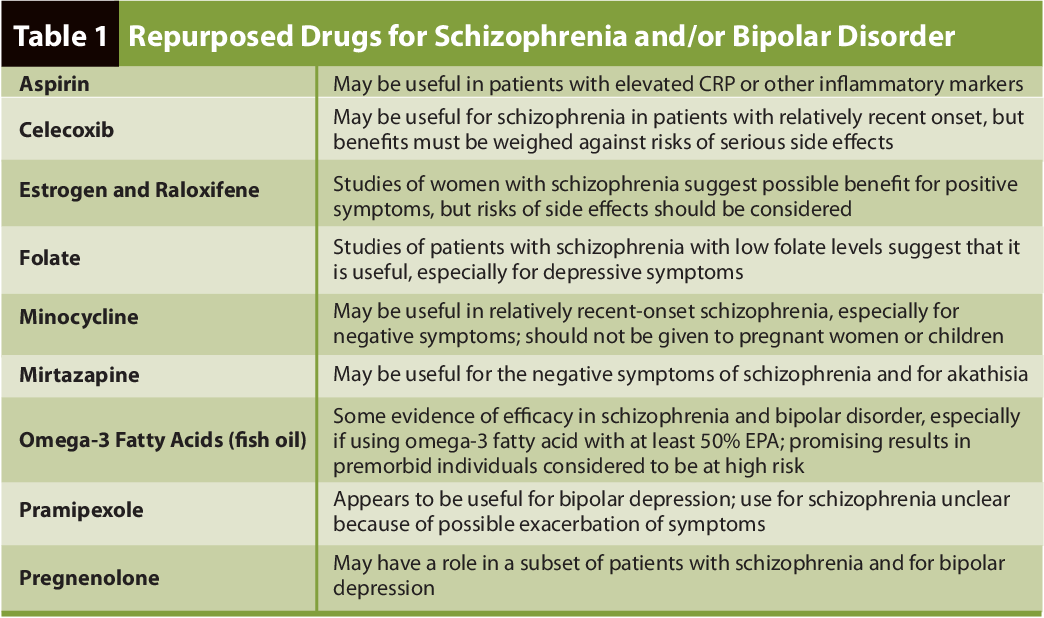
See also: How Bipolar Disorder Is Treated: Questions for a Psychiatrist
Most antidepressants can also reduce anxiety, but this usually takes several weeks of continuous use. In addition, as discussed earlier, they may cause worsening of bipolar disorder in some patients.
Finding the right dosage
The effectiveness of treatment depends on the correct selection of drugs and finding the right dosage for you. Finding the right dose for you will be easier if you are taking your medications as prescribed by your doctor and regularly informing him of the effect of medicines on your body. Tables 3.1, 3.2, and 3.3 provide information on approximate dosages for mood stabilizers, antidepressants, and antipsychotics. Only the original trade names of the drugs are indicated (many of the drugs have analogues containing the same active substance). Please note that depending on your condition, your doctor may prescribe dosages outside of those listed in the table.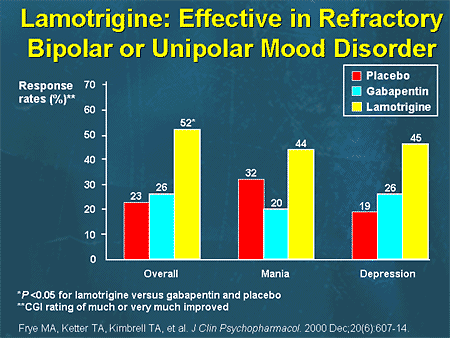 These limits are indicative so that you can take an active part in the discussion of dosages with your doctor.
These limits are indicative so that you can take an active part in the discussion of dosages with your doctor.
Download the whole chapter
Summary
Treatment of bipolar affective disorder (BAD) in Israel
Home
Services and treatment
Bipolar affective disorder treatment in Israel
Bipolar affective disorder (BAD) is a severe mental illness caused in 50% of cases at the genetic level. Previously, bipolar disorder was called manic-depressive psychosis (MDP). A person suffering from bipolar disorder is subject to sudden mood swings from overly agitated, irritable (manic) to depressed and hopelessly helpless (depressive). Such moods, as a rule, can change with a frequency of several weeks to several months.
Bipolar affective disorder affects millions of people worldwide. BAD is an insidious disease that can last a lifetime. If you do not turn to specialists or self-medicate, the disease tends to worsen.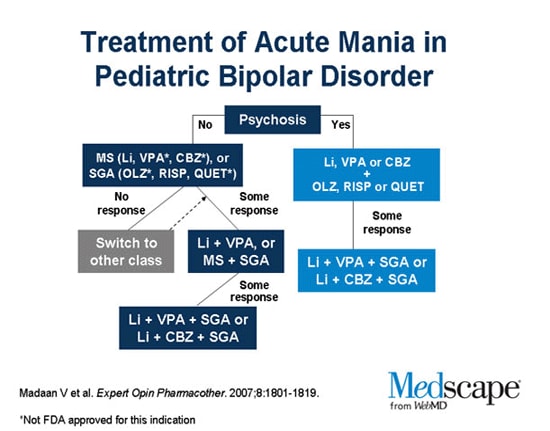 Over time, episodes of depression and mania in the patient become more frequent, the symptoms become brighter and more severe and finally tear the patient away from normal life.
Over time, episodes of depression and mania in the patient become more frequent, the symptoms become brighter and more severe and finally tear the patient away from normal life.
- Article "Description of Bipolar Affective Disorder"
Method of treatment
1 Cognitive behavioral therapy
In the center "Matspen" in the treatment of bipolar affective disorder, preference is given to the most modern and effective method - cognitive-behavioral therapy. This method is aimed at developing the patient's ability to control negative or inappropriate thoughts and behavior, regulate mood, thereby influencing the pathological affect.
Cognitive behavioral therapy can prevent relapse, both manic and depressive. In the process of communicating with a psychotherapist, the patient's way of thinking and behavior changes, which reflects a change in the functioning of the brain. These changes relieve the patient of the symptoms of the disease that interfere with a full life and perception of the world around.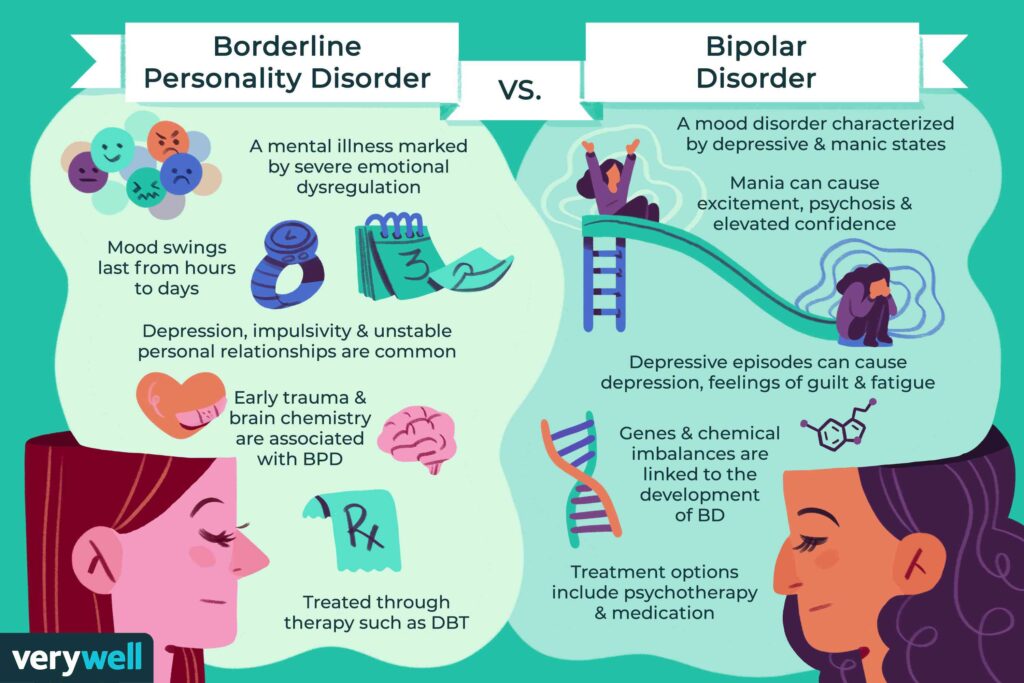
The psychotherapist in sessions of cognitive behavioral therapy helps the patient understand the nature of the disease so that in the future he can notice and, accordingly, prevent relapses at an early stage. The patient learns to avoid risk factors that can lead to relapse.
The patient learns to recognize risk factors in the development of their disease, control negative thoughts and thus prevent relapse.
2 Family therapy
In order to normalize relations in the family, as well as to teach the rules of behavior with the patient and the correct reaction in case of relapses and stressful situations, the Matspen Center conducts family therapy with members of the patient's family.
Family therapy can reduce stress on the patient in various family situations. Relatives learn to control and timely prevent the symptoms of an exacerbation of the disease. They also learn to make adequate demands on the patient.
The behavior of loved ones plays an important role in the treatment of bipolar affective disorder.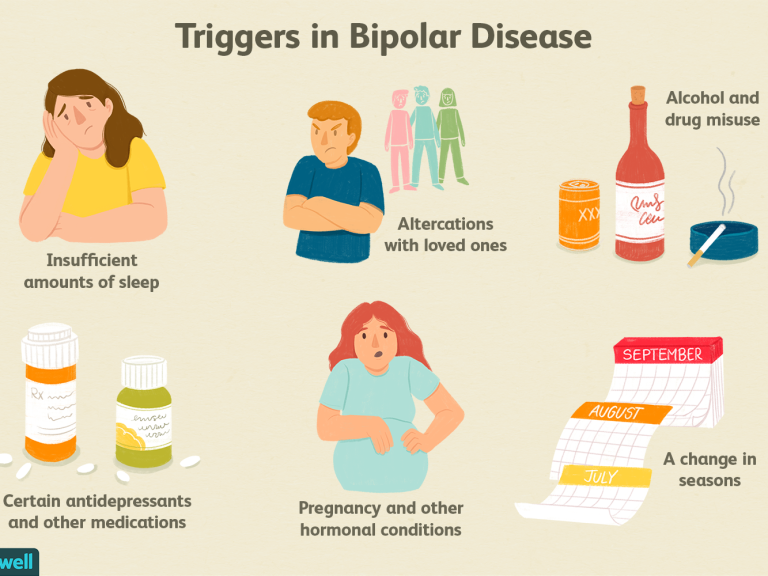 Family members learn to adequately respond to the patient's behavior and reduce the stress load on him.
Family members learn to adequately respond to the patient's behavior and reduce the stress load on him.
3 Drug treatment
The key treatment for bipolar affective disorder is drug therapy.
In the Matspen Center, a psychiatrist works with a patient and selects exclusively individual drug treatment regimens. Typically, drugs called mood stabilizers are used. In some cases, they can be combined with antidepressants.
Drug treatment most often eliminates all signs of the disease, and after the first stage of treatment, people can lead an absolutely full life.
Drug treatment of bipolar affective disorder in the center "Matspen" is divided into two stages.
First, intensive treatment is carried out, the purpose of which is to rid the patient of all the symptoms of the disease. A noticeable effect occurs after 2-3 weeks, and after a month, many symptoms disappear completely.
The second stage is maintenance therapy. It is important to continue drug treatment despite the absence of any symptoms, because. refusal to take medication can provoke a return (relapse) of the disease. The terms of taking the drugs and the dosage are also determined by the psychiatrist. The dosage is certainly different from the intensive phase of drug treatment.
It is important to continue drug treatment despite the absence of any symptoms, because. refusal to take medication can provoke a return (relapse) of the disease. The terms of taking the drugs and the dosage are also determined by the psychiatrist. The dosage is certainly different from the intensive phase of drug treatment.
Medications are selected individually, and the entire course of medication is divided into 2 stages: intensive (to relieve current symptoms of the disease) and maintenance (reduced regular dosage to avoid relapse).
Total
At the Matzpen Center, patients with bipolar affective disorder receive professional diagnosis of the disease, support and effective comprehensive treatment, the result of which is the ability to live a healthy and productive life.
- The course of treatment for bipolar affective disorder depends on the degree of the disease and can last from 1 month.
- Treatment for bipolar disorder starts at $3,000 per month.
-
It should be taken into account that we start treatment only after the diagnosis.
Specialists
-
- Dr. Vitaly Finkelstein
Head of the Neurological Department of the Matspen Center
-
- Dr. Yana Beitelman
Head of the Psychiatric Department of the Matzpen Center
Patient testimonials
-
“What many doctors in our city could not do in 4 months, they did it here in 1 month ... Miracles really work here.”
-
“He did what no doctor in Russia could do.
 Finally, our family found peace for our child.”
Finally, our family found peace for our child.” -
"A change of scenery, a change in life events, a new approach to treatment had a positive effect on health ..."
-
????“We saw your sincere desire to help us and were able to get qualified advice on our problem…”
-
"In a month and a half, we achieved a result that we never hoped to get."
-
“Thanks to the high professionalism of the doctors, we were correctly diagnosed.
 .. The iridescent atmosphere is conducive to pleasant communication and patients' trust in doctors and sets them up for treatment.”
.. The iridescent atmosphere is conducive to pleasant communication and patients' trust in doctors and sets them up for treatment.” -
“At Matspen they opened my eyes to the problem with the child much more seriously. Specialists in sufficient detail and very clearly conveyed to me what needs to be done and how to try to bring the child to the approximate level of his age.
-
“Most importantly, the diagnosis that was made before coming to Israel was rejected.”
-
"We say special thanks for your humanity, kindness and decency."
-
“Now I have a completely different life.