Male dependency disorder
Dependent Personality Disorder | Mental Health Treatment MI
Mental health experts describe personality as characteristic patterns of thinking, feeling, and behaving that make us unique individuals. Personality characteristics tend to remain consistent over time. A personality disorder affects how a person thinks or acts, resulting in behavior that deviates from cultural norms and impairs healthy functioning. Individuals with personality disorders experience severe dysfunction in most areas of life, mainly with interpersonal relationships. Rose Hill Center is a top-rated mental health treatment facility offering various services, including personality disorder treatment.
Individuals with personality disorders often struggle with other mental health issues, including anxiety and depression. When your mental health is compromised, you can feel lost and alone, but help is available. Call the Rose Hill Center team at 866.367.0220.
What Is Dependent Personality Disorder (DPD)?
There are ten types of personality disorders, of which dependent personality disorder, DPD, is among the most commonly diagnosed. DPD occurs in men and women equally and usually develops in young adulthood. DPD involves a pervasive need to be taken care of that causes feelings of helplessness and submissiveness. People with DPD have an excessive fear of abandonment and difficulty making everyday decisions. They are often described as needy and clingy. Their reliance on others to fulfill their emotional and physical needs frequently leads to them being involved in physically and emotionally abusive relationships.
DPD may be due to a mixture of genetic, developmental, and environmental factors. DPD is more common in individuals with particular life experiences, including:
- Childhood trauma
- Severe childhood illness
- History of abusive relationships
- Family history of anxiety or personality disorders
- Religious, cultural, or family behavior that emphasizes reliance on authority
People with DPD want someone to take care of them, and they have great anxiety about caring for themselves.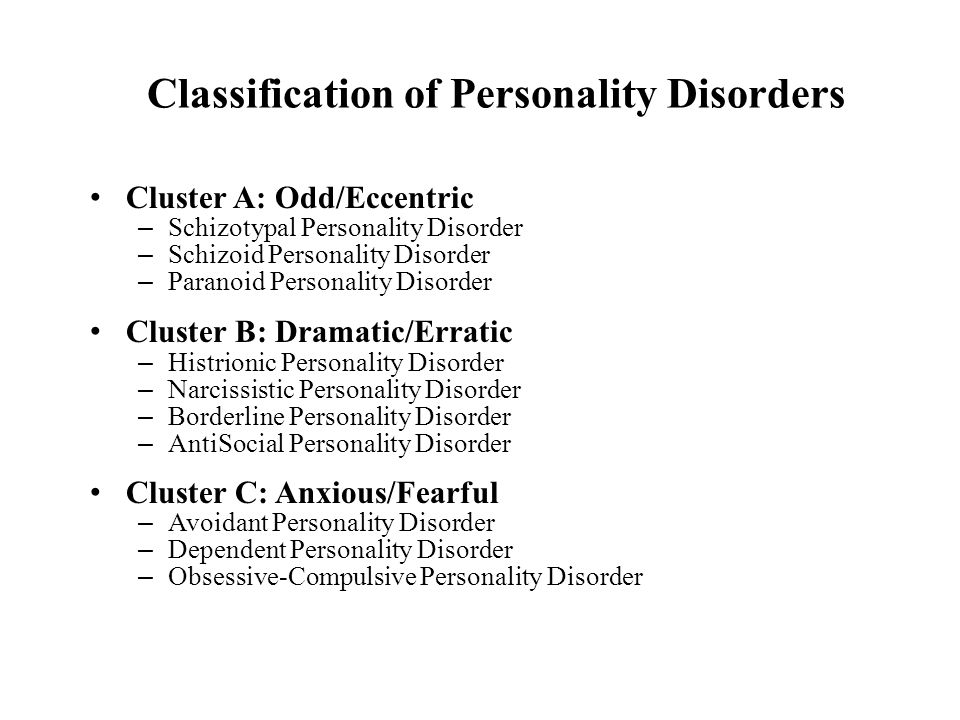 They give up their interests and independence to get the care they crave.
They give up their interests and independence to get the care they crave.
Do You Have Dependent Personality Disorder (DPD) Symptoms?
Overall, those with dependent personality disorder are overdependent on others and will do anything to please them. In addition to being extremely needy, clingy, passive, and fearful of abandonment, common symptoms of DPD include:
- Inability to make everyday decisions without advice and reassurance from others
- Avoidance of responsibilities by acting helpless and passive
- Oversensitivity to criticism
- Extreme pessimism and lack of self-confidence
- A tendency toward fantasy and naivety
- Willingness to tolerate negative behavior, mistreatment, and abuse from others
- Placing the needs of others before their own
Though people with DPD fear being alone, their behaviors often sabotage relationships. While the end of a relationship devastates them, they quickly jump into a new one. Some treatment experts may confuse DPD with borderline personality disorder (BPD), as they share many common symptoms. If you think you or a loved one has DPD, reach out to your doctor. Following an accurate diagnosis, dependent personality disorder treatment can help you manage symptoms and learn how to develop healthy relationships.
Some treatment experts may confuse DPD with borderline personality disorder (BPD), as they share many common symptoms. If you think you or a loved one has DPD, reach out to your doctor. Following an accurate diagnosis, dependent personality disorder treatment can help you manage symptoms and learn how to develop healthy relationships.
What to Expect from Dependent Personality Disorder (DPD) Treatment
As with many personality disorders, those with dependent personality disorder usually seek help when life becomes overwhelming due to their symptoms, specifically those of anxiety and depression. Psychotherapy is the main form of treatment for DPD, where the goals are to help patients:
- Become more actively involved in decision-making
- Develop independence
- Improve self-esteem and self-confidence
- Develop coping skills
- Learn to form healthy relationships
People with DPD often have a history of trauma, so trauma therapy is a standard part of treatment for many. In working with patients with DPD, therapists are careful to monitor the therapeutic relationship so that the patient does not form an unhealthy bond in treatment. Medication does not treat the core problems that DPD causes. However, we may use it to help you manage anxiety or depression associated with DPD.
In working with patients with DPD, therapists are careful to monitor the therapeutic relationship so that the patient does not form an unhealthy bond in treatment. Medication does not treat the core problems that DPD causes. However, we may use it to help you manage anxiety or depression associated with DPD.
Find Dependent Personality Disorder Treatment at Rose Hill Center
At Rose Hill Center, we understand that dependent personality disorder can feel like a scary diagnosis. Education about DPD helps to alleviate your fears. You will learn the skills and tools to manage your DPD symptoms and regain control of your life through inpatient dependent personality disorder treatment. To learn more about how we can help, contact our team today at 866.367.0220.
Dependent Personality Disorder
Written by WebMD Editorial Contributors
In this Article
- What Are the Symptoms of DPD?
- What Causes DPD?
- How Is DPD Diagnosed?
- How Is DPD Treated?
- What Are the Complications of DPD?
- What Is the Outlook for People With DPD?
- Can DPD Be Prevented?
Dependent personality disorder (DPD) is one of the most frequently diagnosed personality disorders. It causes feelings of helplessness, submissiveness, a need to be taken care of and for constant reassurance, and an inability to make everyday decisions without an excessive amount of advice and reassurance from others.
It causes feelings of helplessness, submissiveness, a need to be taken care of and for constant reassurance, and an inability to make everyday decisions without an excessive amount of advice and reassurance from others.
This personality disorder occurs equally in men and women and usually becomes apparent in young adulthood or later as important adult relationships form.
What Are the Symptoms of DPD?
People with DPD become emotionally overdependent on other people and spend great effort trying to please others. People with DPD tend to display needy, passive, and clinging behavior, and have a fear of separation. Other common characteristics of this personality disorder include:
- Inability to make decisions, even everyday decisions like what to wear, without the advice and reassurance of others
- Avoidance of adult responsibilities by acting passive and helpless; dependence on a spouse or friend to make decisions like where to work and live
- Intense fear of abandonment and a sense of devastation or helplessness when relationships end; a person with DPD often moves right into another relationship when one ends.
- Oversensitivity to criticism
- Pessimism and lack of self-confidence, including a belief that they are unable to care for themselves
- Avoidance of disagreeing with others for fear of losing support or approval
- Inability to start projects or tasks because of a lack of self-confidence
- Difficulty being alone
- Willingness to tolerate mistreatment and abuse from others
- Placing the needs of their caregivers above their own
- Tendency to be naive and to fantasize
What Causes DPD?
Although the exact cause of DPD is not known, it most likely involves a combination of biological, developmental, temperamental, and psychological factors. Some researchers believe an authoritarian or overprotective parenting style can lead to the development of dependent personality traits in people who are susceptible to the disorder.
How Is DPD Diagnosed?
A diagnosis of DPD must be distinguished from borderline personality disorder, as the two share common symptoms.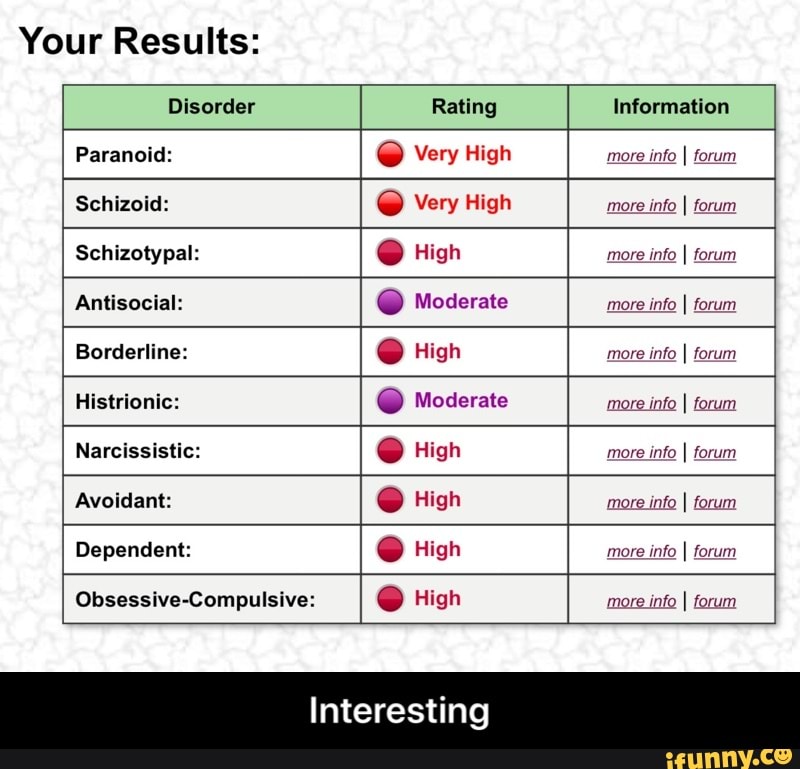 In borderline personality disorder, the person responds to fears of abandonment with feelings of rage and emptiness. With DPD, the person responds to the fear with submissiveness and seeks another relationship to maintain their dependency.
In borderline personality disorder, the person responds to fears of abandonment with feelings of rage and emptiness. With DPD, the person responds to the fear with submissiveness and seeks another relationship to maintain their dependency.
If most or all the (above) symptoms of DPD are present, the doctor will begin an evaluation by taking a thorough medical and psychiatric history and possibly a basic physical exam. Although there are no laboratory tests to specifically diagnose personality disorders, the doctor might use various diagnostic tests to rule out physical illness as the cause of the symptoms.
If the doctor finds no physical reason for the symptoms, they might refer the person to a psychiatrist, psychologist, or other health care professional trained to diagnose and treat mental illnesses. Psychiatrists and psychologists use specially designed interview and assessment tools to evaluate a person for a personality disorder.
How Is DPD Treated?
As is the case with many personality disorders, people with DPD generally do not seek treatment for the disorder itself. Rather, they might seek treatment when a problem in their lives -- often resulting from thinking or behavior related to the disorder -- becomes overwhelming, and they are no longer able to cope. People with DPD are prone to developing depression or anxiety, symptoms that might prompt the individual to seek help.
Rather, they might seek treatment when a problem in their lives -- often resulting from thinking or behavior related to the disorder -- becomes overwhelming, and they are no longer able to cope. People with DPD are prone to developing depression or anxiety, symptoms that might prompt the individual to seek help.
Psychotherapy (a type of counseling) is the main method of treatment for DPD. The goal of therapy is to help the person with DPD become more active and independent, and to learn to form healthy relationships. Short-term therapy with specific goals is preferred when the focus is on managing behaviors that interfere with functioning. It is often useful for the therapist and patient together to pay attention to the role of therapist in order to recognize and address ways in which the patient may form the same kind of passive reliance in the treatment relationship that happens outside of treatment. Specific strategies might include assertiveness training to help the person with DPD develop self-confidence and cognitive-behavioral therapy (CBT) to help someone develop new attitudes and perspectives about themselves relative to other people and experiences. More meaningful change in someone's personality structure usually is pursued through long-term psychoanalytic or psychodynamic psychotherapy, where early developmental experiences are examined as they may shape the formation of defense mechanisms, coping styles, and patterns of attachment and intimacy in close relationships.
More meaningful change in someone's personality structure usually is pursued through long-term psychoanalytic or psychodynamic psychotherapy, where early developmental experiences are examined as they may shape the formation of defense mechanisms, coping styles, and patterns of attachment and intimacy in close relationships.
Medication might be used to treat people with DPD who also suffer from related problems such as depression or anxiety. However, medication therapy in itself does not usually treat the core problems caused by personality disorders. In addition, medications should be carefully monitored, because people with DPD become dependent on them or misuse certain prescription drugs.
What Are the Complications of DPD?
People with DPD are at risk for depression, anxiety disorders, and phobias, as well as substance abuse. They are also at risk for being abused because they may find themselves willing to do virtually anything to maintain the relationship with a dominant partner or person of authority.
What Is the Outlook for People With DPD?
With psychotherapy (counseling), many people with DPD can learn how to make more independent choices in their lives.
Can DPD Be Prevented?
Although prevention of the disorder might not be possible, treatment of DPD can sometimes allow a person who is prone to this disorder to learn more productive ways of dealing with situations.
The development of personality structure is a complex process that begins from an early age. Psychotherapy aimed at modifying personality may be more successful when begun early, when the patient is highly motivated for change, and when there is a strong working relationship between the therapist and patient.
Anxiety & Panic Disorders Guide
- Overview
- Symptoms & Types
- Treatment & Care
- Living & Managing
Disorders of sexual behavior in men
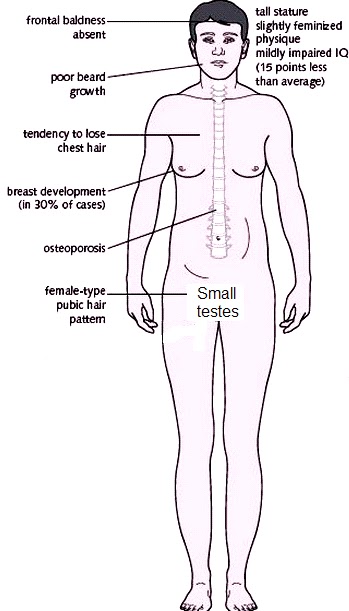
Disorders of sexual behavior have an extremely negative impact on the psycho-emotional state of a person. Violations in the sexual sphere in men usually manifest themselves in the form of a lack of sexual desire, erectile dysfunction, lack of ejaculation, as well as premature ejaculation and pain in the genitals during an erection. A person who does not have a regular sexual relationship or has no sexual experience at all, having problems in sexual behavior, may withdraw into himself, develop depression, anxiety disorder and avoid potential partners, thereby reinforcing the course of the disorder. nine0003
Violations in the sexual sphere in men usually manifest themselves in the form of a lack of sexual desire, erectile dysfunction, lack of ejaculation, as well as premature ejaculation and pain in the genitals during an erection. A person who does not have a regular sexual relationship or has no sexual experience at all, having problems in sexual behavior, may withdraw into himself, develop depression, anxiety disorder and avoid potential partners, thereby reinforcing the course of the disorder. nine0003
Causes of sexual behavior disorders
According to statistics, 80% of men with problems of sexual intercourse to psychologists, sexologists or psychiatrists are associated with organic disorders. Such patients either did not pay enough attention to checking their physical health, or rushed to contact a sexologist or psychologist. Such patients need to make an appointment from the very beginning, for example, with a urologist or undergo an MRI examination. Therefore, when a person turns to a specialist with problems in sexual behavior, first of all it is necessary to make sure that the patient has at least been checked by a urologist. Sometimes treatment by a psychotherapist does not bring any results, because the cause of the disturbances is in an organic problem. This is very critical in this area. nine0003
Therefore, when a person turns to a specialist with problems in sexual behavior, first of all it is necessary to make sure that the patient has at least been checked by a urologist. Sometimes treatment by a psychotherapist does not bring any results, because the cause of the disturbances is in an organic problem. This is very critical in this area. nine0003
Sexual behavior disorders, which are symptoms of severe mental illness, are often the result of side effects from medications.
In the field of sexual dysfunction, experts do not find a genetic predisposition. Usually the causes are either organic or psychological. For example, the cause may be anxiety, which has developed into psychosomatics, for example, in the form of impotence. Psychological reasons may be related to sexual trauma that occurred to the patient in the past. The most popular problems that have non-organic causes are impotence and early ejaculation. It can appear due to anxiety, psychotrauma or natural aging of the body. In some cases, problems with potency can also be caused by systematic violations of the physiological cycle of sexual intercourse. This form of sexual dysfunction develops over time, beginning to manifest as orgasm blunting, premature ejaculation, or inability to ejaculate. Such patients can be treated for a long time and in vain by urologists with a diagnosis of chronic prostatitis, which subsequently forms neurotic manifestations. nine0003
In some cases, problems with potency can also be caused by systematic violations of the physiological cycle of sexual intercourse. This form of sexual dysfunction develops over time, beginning to manifest as orgasm blunting, premature ejaculation, or inability to ejaculate. Such patients can be treated for a long time and in vain by urologists with a diagnosis of chronic prostatitis, which subsequently forms neurotic manifestations. nine0003
See also
Mental norm and pathology
Sexual behavior disorders, which are symptoms of severe mental illness, are often the result of side effects from medications. For example, impotence appears due to the use of antipsychotic drugs, which are prescribed, for example, for psychosis during schizophrenia or bipolar disorder. In this case, the level of prolactin rises in a person. An increase in prolactin levels leads to a decrease in sexual appetite, weakening of erection and early ejaculation.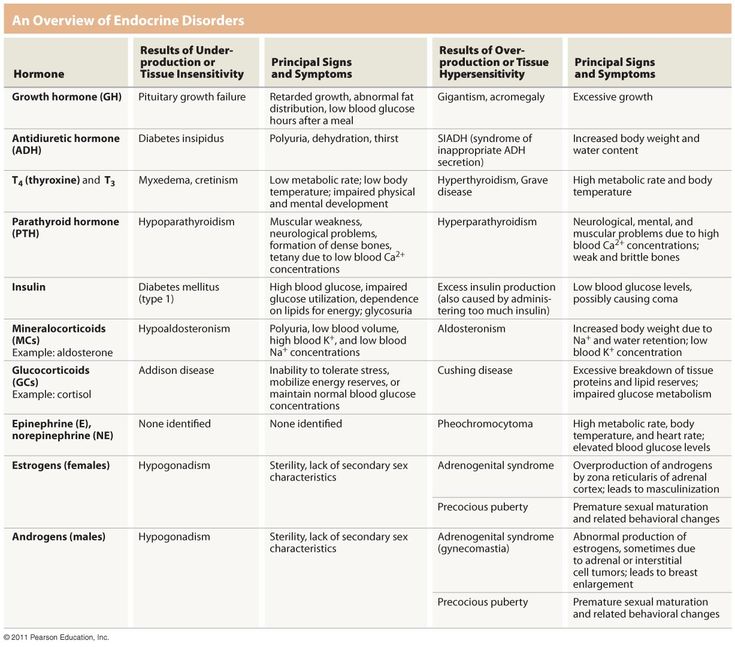 When a person with schizophrenia or bipolar disorder complains of impotence, doctors first check the effect of drugs, and if necessary, change the dosage and frequency of taking the drugs. After all, mental disorders already violate a person’s life comfort, and a decrease in sexual appetite can bring even greater inconvenience. nine0003
When a person with schizophrenia or bipolar disorder complains of impotence, doctors first check the effect of drugs, and if necessary, change the dosage and frequency of taking the drugs. After all, mental disorders already violate a person’s life comfort, and a decrease in sexual appetite can bring even greater inconvenience. nine0003
Types of sexual behavior disorders
Disorders of sexual behavior are divided into organic and inorganic disorders of sexual intercourse. If we divide sexual intercourse into four stages, then for each of them we can distinguish separate disorders of sexual behavior. The first stage is preparation for sexual intercourse, when there is no sexual desire for a woman or a man. The second is the presence of problems with potency. At the third stage, pain in the genitals may be present, and at the fourth stage, premature ejaculation is possible. According to these stages, certain sexual dysfunctions may appear. For disorders of each stage, special psychotherapy is prescribed. nine0003
nine0003
Diagnostics and treatment of sexual disorders
Before the advent of drugs such as Viagra, Levitra and others, such disorders were treated exclusively with sexual therapy. At the very beginning, various sexual dysfunctions were tried to be treated with the help of psychoanalysis. Very quickly, the physiologist Ivan Pavlov, and later the psychologist Burres Frederick Skinner, developed a behavioral theory that in the 60s, thanks to William Masters and Virginia Johnson, developed into a very coherent therapy for the treatment of sexual disorders. Thanks to this therapy, many sexual disorders in men began to be treated very effectively and quickly. nine0003
Psychotherapy is usually prescribed as a treatment for sexual behavior disorders in men.
Until Viagra appeared, there were no options for effective drug treatment, but only behavioral therapy, sometimes combined with cognitive techniques. Occasionally, medications were added to the treatment, which were prescribed by psychiatrists to reduce stress and anxiety. As soon as drugs like Viagra and Cialis appeared, they helped to solve the problem of the second stage of sexual behavior, but still did not solve the problem of the first - the lack of urge or sexual desire.
As soon as drugs like Viagra and Cialis appeared, they helped to solve the problem of the second stage of sexual behavior, but still did not solve the problem of the first - the lack of urge or sexual desire.
See also
Myths about psychotherapy
Working with a psychotherapist
After the patient has been ruled out for organic causes of the sexual behavior disorder, he is referred for a clinical interview with a psychiatrist. The specialist collects a detailed history of the patient's sexual life and, if necessary, prescribes additional instrumental checks. Psychotherapy is usually prescribed as a treatment for sexual behavior disorders in men. As a rule, this is a combination of two approaches: behavioral therapy and interpersonal therapy. The therapist discusses with the patient every aspect of his sexual behavior, considering all the feelings, thoughts, reactions and sensations in the body at every stage. It also studies interpersonal behavior and finds out at which stage of interaction with a partner a problem appears and the process is disrupted. After that, the patient is offered various behavioral-communicative tools. nine0003
It also studies interpersonal behavior and finds out at which stage of interaction with a partner a problem appears and the process is disrupted. After that, the patient is offered various behavioral-communicative tools. nine0003
It happens that a patient has problems at the first stage of sexual intercourse, that is, a lack of sexual appetite, as well as impotence - and this is all against the background of increased shyness towards women.
The patient is then taught to apply these techniques in real life, in real interpersonal relationships, and determine what needs to be changed with the help of communicative behavioral therapy. This type of therapy was developed in the 70s by several very famous American psychotherapists: Virginia Satir, Jay Haley, Paul Watzlawick and others. Communicative behavioral therapy is used in the treatment of sexual disorders to this day. nine0003
When it comes time to apply these techniques in life, it is necessary that the patient had a partner or partner.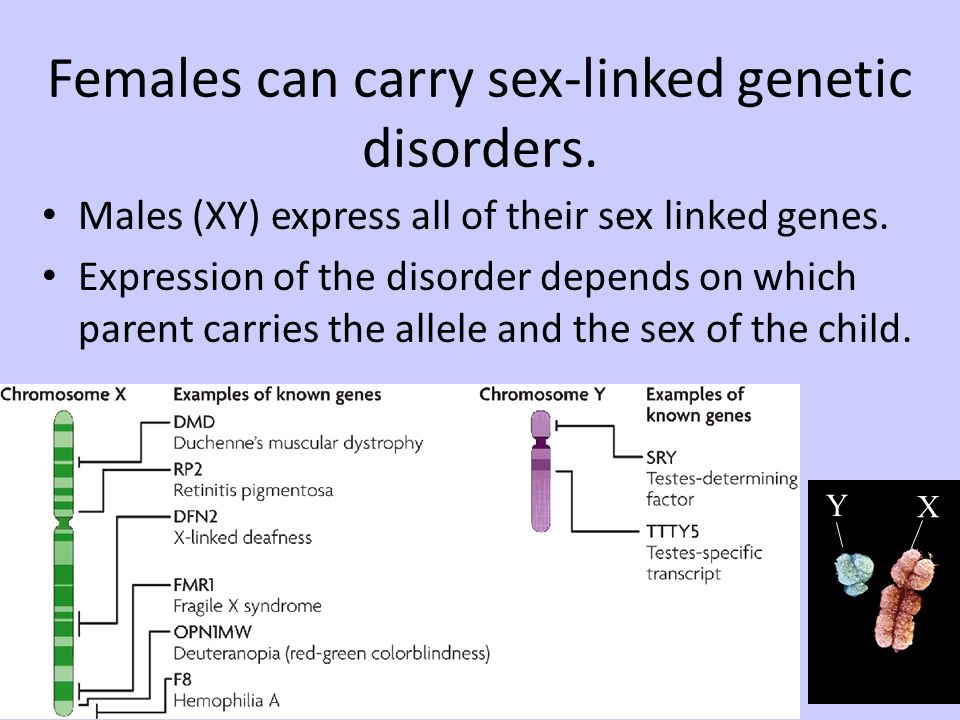 Serious work is also taking place in this direction. It happens that a patient has problems at the first stage of sexual intercourse, that is, a lack of sexual appetite, as well as impotence - and this is all against the background of increased shyness towards women. A psychotherapist also works with these problems so that the patient can meet with a woman or a man and apply new techniques for himself. For this, there is a direction in treatment, in which specially trained people - serogates - portray pseudo-partners. nine0003
Serious work is also taking place in this direction. It happens that a patient has problems at the first stage of sexual intercourse, that is, a lack of sexual appetite, as well as impotence - and this is all against the background of increased shyness towards women. A psychotherapist also works with these problems so that the patient can meet with a woman or a man and apply new techniques for himself. For this, there is a direction in treatment, in which specially trained people - serogates - portray pseudo-partners. nine0003
The main difficulties usually occur in patients before sexual intercourse, during courtship and flirting. The patient learns how to give flowers, how to look a partner or partner in the eye, how to give compliments, and how to use proper body language on dates. This is a type of behavioral therapy when, with the help of special behavioral techniques, sexual interaction is built on the example of a living relationship.
nine0061Share:
Sexual dysfunctions in men with depressive disorders
Depression is the most common mental disorder, and its prevalence rate has grown rapidly in recent decades [1]. The incidence of depression is approaching 3%, and the risk of getting sick during life is 20% [2]. The prevalence of depressive disorders among men is 4-10%.
The incidence of depression is approaching 3%, and the risk of getting sick during life is 20% [2]. The prevalence of depressive disorders among men is 4-10%.
The relationship of depressive states with pathology in the sexual sphere has been the subject of attention of many generations of domestic and foreign researchers. R. Krafft-Ebing [3, 4] wrote that a patient in a depressed state ceases to experience desires, since any goal seems unattainable to him and that "the mind and mood of melancholics are unfavorable for the awakening of sexual desire." S. Freud [5] noted: "A particularly powerful asthenic factor in affective disorders with sexual disorders is the switching of the entire mental register of the individual to the area of extreme anxiety about the reduction or loss of one's masculinity." Speaking about the relationship between depression and sexual dysfunction, it should be noted that at the dawn of sexological research, more importance was attached to sexual disorders themselves, and mood disorders were considered their consequence. And only by the end of the 19th century, violations in the sexual sphere began to be considered not as a cause, but as a consequence of mental illness [6-8]. This began to concern, first of all, works devoted to the psychosomatic aspects of depressive disorders, masked depressions and somatic equivalents of depressions, in which sexual disorders were described as manifestations of dysfunctions of the autonomic nervous system. nine0003
And only by the end of the 19th century, violations in the sexual sphere began to be considered not as a cause, but as a consequence of mental illness [6-8]. This began to concern, first of all, works devoted to the psychosomatic aspects of depressive disorders, masked depressions and somatic equivalents of depressions, in which sexual disorders were described as manifestations of dysfunctions of the autonomic nervous system. nine0003
Prevalence of sexual dysfunctions in depressive disorders
Data on the prevalence of sexual disorders in the population vary greatly from 2 to 50% in various forms depending on sex and age [9]. In this regard, it should be noted that epidemiological studies in the field of sexopathology encounter certain difficulties. The fact is that information, both obtained from direct examination of patients and from various medical institutions, is not reliable enough. This is due to the fact that, firstly, patients often hide their sexual disorders, secondly, the data obtained depend on the clinical qualifications and orientation of the researcher, and thirdly, there are serious discrepancies in diagnostic issues among sexologists belonging to different schools , and there are also significant differences in research methods [10]. nine0003
nine0003
In general, the frequency of sexual problems in patients with depression is about 2-3 times higher than in the general population - 50% compared to 24% [11]. According to a number of authors [12-14], 5% of men with depression experience difficulties due to reduced sexual desire, 21-38% suffer from premature ejaculation, and 4-10% suffer from orgasmic disorders. The data presented in the study by N.Sh. Tatlaev [15], indicate a significant prevalence of disorders of libido, erection, ejaculation, orgasm and the level of sexual activity in general in depressive patients. According to the literature, libido to some extent decreases in 100% of cases, the level of sexual activity - in 99%, erection - 98%, and orgasm - 82%. However, as mentioned above, there is a fairly large scatter of indicators, which is explained by the vagueness of patients seeking sexological help, which does not reflect the true prevalence of disorders in the population [16]. Only very degraded patients with a "complete lack of modesty" can bring to the attention of the doctor the details of their intimate life [7].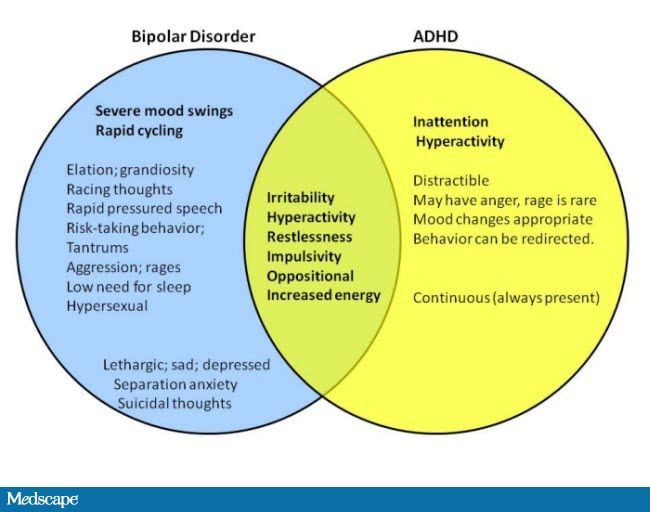 For the majority, communication with a doctor on this topic presents great difficulties. This is evidenced by the fact that among the 6,000 West Germans who attempted suicide, more than ½ had some kind of sexual problems, with 21% having them as the main motive, and 32% as one of the important ones. J. Hempel et al. [17] reported that impotence ranks second among the motives for suicide. It can be added to the above that the patient's sexual problems turn out to be a very unpleasant topic for doctors, especially women. nine0003
For the majority, communication with a doctor on this topic presents great difficulties. This is evidenced by the fact that among the 6,000 West Germans who attempted suicide, more than ½ had some kind of sexual problems, with 21% having them as the main motive, and 32% as one of the important ones. J. Hempel et al. [17] reported that impotence ranks second among the motives for suicide. It can be added to the above that the patient's sexual problems turn out to be a very unpleasant topic for doctors, especially women. nine0003
Modern understanding of the relationship between sexual and depressive disorders
It is known that depression is characterized by a number of somatic disorders, biochemical changes, and hormonal changes. There are no exceptions and violations in the sexual sphere. According to some foreign authors [18-20], in those suffering from depression, sexual desire is noticeably reduced, erection and ejaculation disorders occur, and the ability to enjoy sexual fantasies is lost.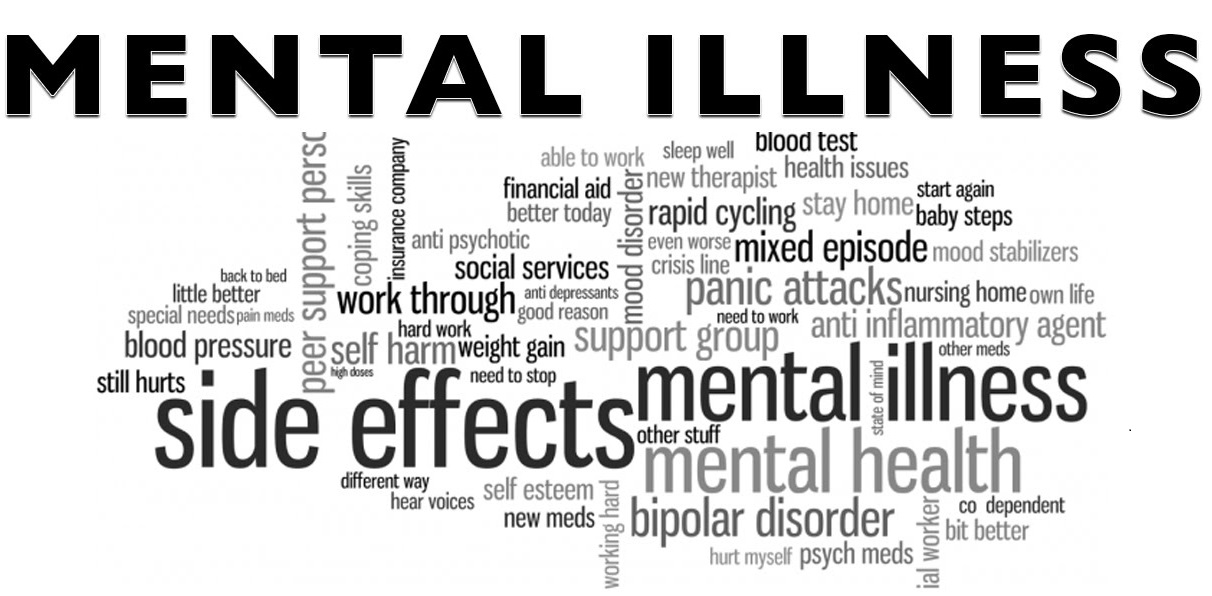 V.D. Topolyansky [21] emphasizes that functional sexual disorders are one of the almost indispensable components of depression. It is no coincidence that a noticeable decrease in potency is considered as almost its most important sign (“symptom of symptoms”), which is detected during a targeted study in almost any emotionally unstable patient. It is no coincidence that "impotence" as such sometimes turns out to be one of the most frequent erroneous diagnoses [21]. G.S. Vasilchenko [22] also noted that most often a persistent fear of impotence is a symptom of a depressive circle. According to O.P. Vertogradov et al. [23], “a decrease in drives (food, sexual, etc.), characteristic of a depressive syndrome, is most pronounced in melancholy and apathetic depression, however, in anxious depression, on the contrary, there may be an increase in drives (increased thirst, appetite, sexual desire) ". Research by N.Sh. Tatlaeva [15] showed that the clinical picture of sexual disorders is determined by the depth and psychopathological structure of the depressive state.
V.D. Topolyansky [21] emphasizes that functional sexual disorders are one of the almost indispensable components of depression. It is no coincidence that a noticeable decrease in potency is considered as almost its most important sign (“symptom of symptoms”), which is detected during a targeted study in almost any emotionally unstable patient. It is no coincidence that "impotence" as such sometimes turns out to be one of the most frequent erroneous diagnoses [21]. G.S. Vasilchenko [22] also noted that most often a persistent fear of impotence is a symptom of a depressive circle. According to O.P. Vertogradov et al. [23], “a decrease in drives (food, sexual, etc.), characteristic of a depressive syndrome, is most pronounced in melancholy and apathetic depression, however, in anxious depression, on the contrary, there may be an increase in drives (increased thirst, appetite, sexual desire) ". Research by N.Sh. Tatlaeva [15] showed that the clinical picture of sexual disorders is determined by the depth and psychopathological structure of the depressive state.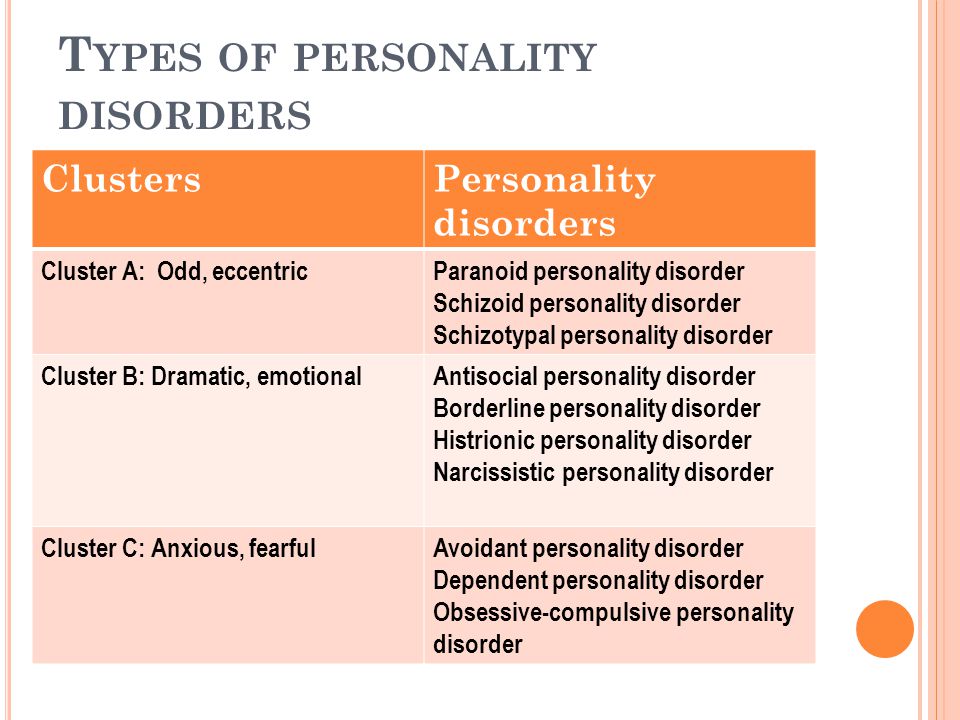 Libido, the level of sexual activity, the quality of erection and orgasm decreased in parallel with the deepening of depressive affect, and this decrease was more pronounced in melancholy and apathetic rather than anxious variants of depressive disorder. In anxiety-depressive states, in contrast to dreary and apathetic, short-term episodes of increased sexual desire are observed. nine0003
Libido, the level of sexual activity, the quality of erection and orgasm decreased in parallel with the deepening of depressive affect, and this decrease was more pronounced in melancholy and apathetic rather than anxious variants of depressive disorder. In anxiety-depressive states, in contrast to dreary and apathetic, short-term episodes of increased sexual desire are observed. nine0003
Most modern authors [11, 22-29] confirm that classical (vital) depression is characterized by pronounced somatovegetative manifestations, including sexual dysfunctions. However, sexual disorders also come to the fore in mild forms of depression (masked, erased, larvated) [30—32].
It is known that somatovegetative disorders can be the main complaints of a patient with affective pathology [23, 24, 29, 33, 34]. Therefore, with depression masked by somatovegetative disorders, from 1/3 to 2/3 of patients are observed in general practitioners, as well as narrow non-psychiatric specialists [9]. Some authors [35] indicate that latent depression can be manifested not only by a decrease in sexual functions, but also by hypersexuality, promiscuity and homosexual tendencies of patients. So, D. Renshaw [13] attributed masturbation to the manifestations of "latent" depression. V.S. Rotenberg and V.V. Andrianov [36] also regarded intermittent nocturnal priapism as a sign of latent depression.
Some authors [35] indicate that latent depression can be manifested not only by a decrease in sexual functions, but also by hypersexuality, promiscuity and homosexual tendencies of patients. So, D. Renshaw [13] attributed masturbation to the manifestations of "latent" depression. V.S. Rotenberg and V.V. Andrianov [36] also regarded intermittent nocturnal priapism as a sign of latent depression.
Depression is a multi-link disorder, the stages of development of which are clinically manifested not only by the deepening of the main symptoms, but also by the modification of self-awareness and self-esteem of patients [25]. The most important criterion for the diagnosis of sexual dysfunction (according to ICD-10 heading F52) is the subjective feeling of dissatisfaction, depression, anxiety, guilt that occurs in an individual in a situation of sexual intercourse [37]. In this case, the patient may present complaints that are not really confirmed. When depression is masked by sexological complaints, they are often perceived as purely evaluative disturbances of the type of imaginary sexual ones. Another typical option is that sexological complaints can dominate, masking affective manifestations. Consequently, the affective disorder itself can manifest itself as sexological dysfunctions. Such depression masked by sexological complaints may not be recognized, while sexual disorders may be regarded as an independent disorder or a symptom of another disease [38]. nine0003
Another typical option is that sexological complaints can dominate, masking affective manifestations. Consequently, the affective disorder itself can manifest itself as sexological dysfunctions. Such depression masked by sexological complaints may not be recognized, while sexual disorders may be regarded as an independent disorder or a symptom of another disease [38]. nine0003
It is important that any resulting sexual disturbance in itself negatively affects the patient, since the inability to have a full sexual life is one of the strongest emotional traumas for a man of any age. Painful personal reactions occur in the form of a depressive affect, which aggravates existing affective disorders and complicates the behavior of therapeutic measures [39].
The above is strong evidence that in depressive disorders there is a biological two-way relationship between depression and sexual disturbances, and psychosexual-related problems may be a psychogenic factor in both the development and maintenance of pre-existing depression. nine0003
nine0003
Pathogenesis of sexual dysfunctions in depressive disorders
The lack of knowledge of general practitioners about the diagnosis and course of affective disorders leads to prolonged ineffective therapy, as a result of which depression becomes chronic with a noticeable decrease in the level of socio-psychological functioning and the quality of life of the patient and his family. Another no less significant side of this problem [22, 29, 40] is the insufficient attention of psychiatrists to the somatovegetative symptoms of depression, especially at the stage of its reverse development and the formation of drug remission, which increases the likelihood of relapse. In the light of the foregoing, it is important to analyze the relationship between somatovegetative (in our case, sexual) and depressive disorders in the pathogenetic aspect.
If we turn to the pathogenesis of depression itself, then it is currently considered from a systemic standpoint, including morphofunctional (neuroanatomical, neurophysiological, neurochemical) and pathopsychological components.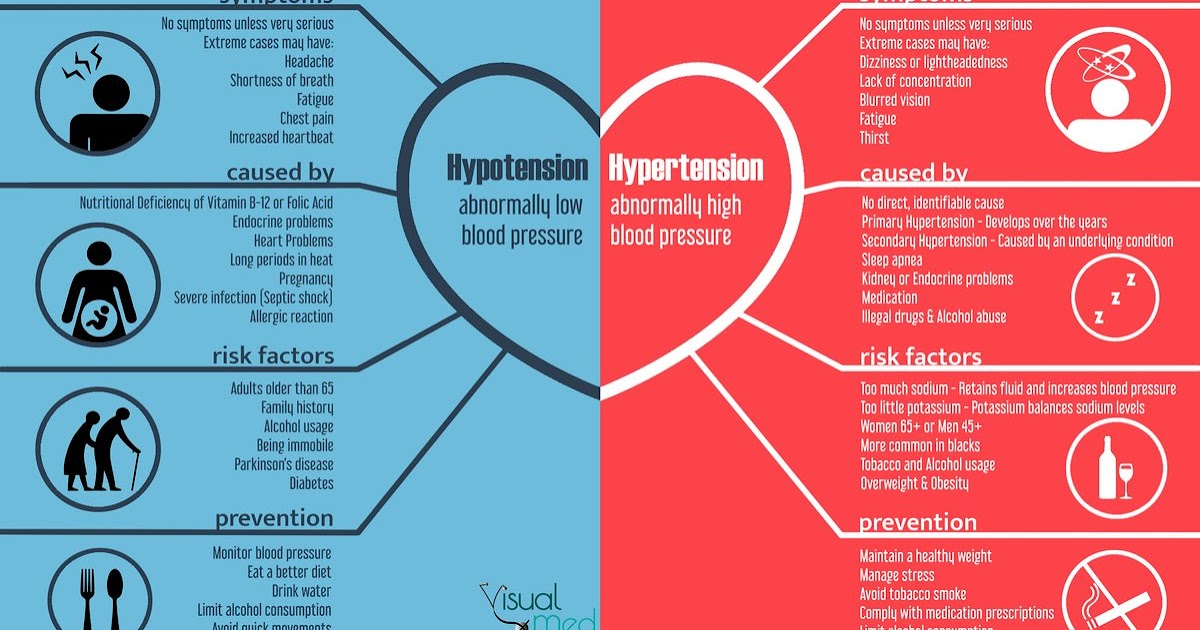 Within the framework of the first, much attention is paid to the pathological functioning of brain structures, in particular, the limbic-thalamic and hypothalamic-pituitary regions. It has now been established that in depressive disorders, disturbances in the production of neuropeptides - hypothalamus-releasing factors - are detected. Through the pituitary gland, they affect various hormonal functions of the body, causing, in particular, the phenomenon of hypercortisolism revealed in depression. If normally the ratio of the secretion of glucocorticosteroids and the function of the monoamine neurotransmitter system is determined by the nature of the feedback (an excess of cortisol in the blood inhibits the release of the hypothalamic corticotropin-releasing factor and, accordingly, the pituitary adrenocorticotropic hormone), then with depression, their relationship changes significantly. At the same time, norepinephrine and serotonin have a direct regulatory effect on the secretion of corticotropin-releasing factor.
Within the framework of the first, much attention is paid to the pathological functioning of brain structures, in particular, the limbic-thalamic and hypothalamic-pituitary regions. It has now been established that in depressive disorders, disturbances in the production of neuropeptides - hypothalamus-releasing factors - are detected. Through the pituitary gland, they affect various hormonal functions of the body, causing, in particular, the phenomenon of hypercortisolism revealed in depression. If normally the ratio of the secretion of glucocorticosteroids and the function of the monoamine neurotransmitter system is determined by the nature of the feedback (an excess of cortisol in the blood inhibits the release of the hypothalamic corticotropin-releasing factor and, accordingly, the pituitary adrenocorticotropic hormone), then with depression, their relationship changes significantly. At the same time, norepinephrine and serotonin have a direct regulatory effect on the secretion of corticotropin-releasing factor.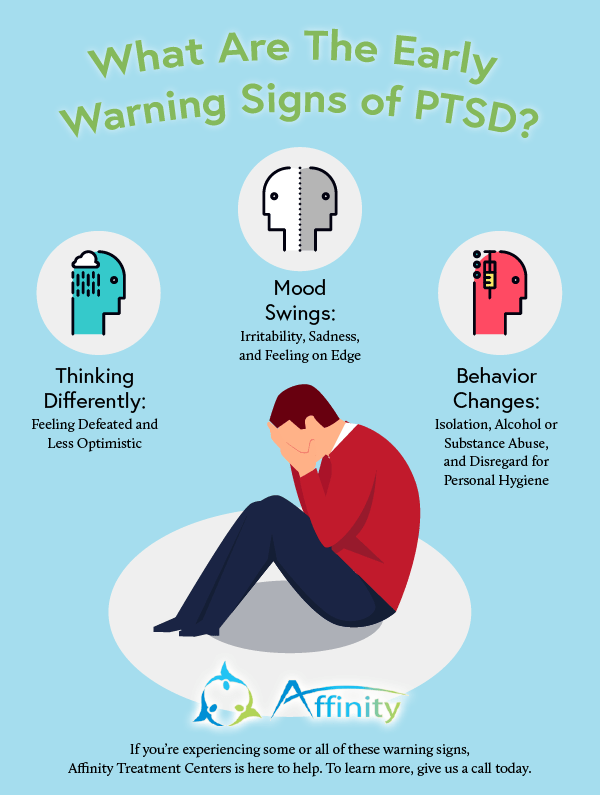 Deficiency of adrenergic neurotransmitters and the associated hypercortisolism contribute to the onset of depressive disorders by forming a "pathological circle" in the hypothalamic-pituitary-adrenal system with positive feedback. At the same time, the limbic system is the main coordinator, forming an integrative circuit through which the cortical emotion regulation centers send impulses to the hypothalamus, and the hypothalamic impulses are transmitted to the hippocampus. Dysfunction of the reticular formation as an activating system of the brain causes an “energy defect”, a decrease in the “biotonicity” of brain mechanisms, which affects the energy component of libido, causing it to decrease, and, as a result, affects the entire copulative cycle. nine0003
Deficiency of adrenergic neurotransmitters and the associated hypercortisolism contribute to the onset of depressive disorders by forming a "pathological circle" in the hypothalamic-pituitary-adrenal system with positive feedback. At the same time, the limbic system is the main coordinator, forming an integrative circuit through which the cortical emotion regulation centers send impulses to the hypothalamus, and the hypothalamic impulses are transmitted to the hippocampus. Dysfunction of the reticular formation as an activating system of the brain causes an “energy defect”, a decrease in the “biotonicity” of brain mechanisms, which affects the energy component of libido, causing it to decrease, and, as a result, affects the entire copulative cycle. nine0003
Constitutional or acquired disorders in the hypothalamic-pituitary-adrenal system are reflected in the clinic of depression, which is confirmed by the phenomenon of neuroendocrine disinhibition. Depletion of the central mediator noradrenergic structures reciprocally causes an increase in peripheral hormonal adrenomedullary activity [28]. Thus, a somatic sympathetic-tonic syndrome is formed, which causes an inhibitory effect of higher centers on the spinal center of the erectile reflex, blocking the parasympathetic impulses necessary for expanding the vessels of the penis, as well as increased sympathetic tone, leading to an increase in the tone of the smooth muscles of the penis, causing difficulty blood flow and, as a result, erectile dysfunction. This affects the neurohumoral component and the copulative cycle. All together causes erectile dysfunction of varying severity, and also leads to ejaculation disorders (acceleration or deceleration, up to absence). nine0003
Thus, a somatic sympathetic-tonic syndrome is formed, which causes an inhibitory effect of higher centers on the spinal center of the erectile reflex, blocking the parasympathetic impulses necessary for expanding the vessels of the penis, as well as increased sympathetic tone, leading to an increase in the tone of the smooth muscles of the penis, causing difficulty blood flow and, as a result, erectile dysfunction. This affects the neurohumoral component and the copulative cycle. All together causes erectile dysfunction of varying severity, and also leads to ejaculation disorders (acceleration or deceleration, up to absence). nine0003
In the pathogenesis of depression, disorders of activity and the pineal gland play a certain role, which lead to the so-called low melatonin syndrome [41]. A deficiency of melatonin produced by the pineal gland disrupts the circadian rhythm of cortisol secretion, explaining the circadian dynamics of the mental state in depressive disorders (deterioration of the mental state in the morning and its improvement in the evening, and this also corresponds to the patients' sexual complaints: increased sexual activity in the evening and a decrease or absence in morning).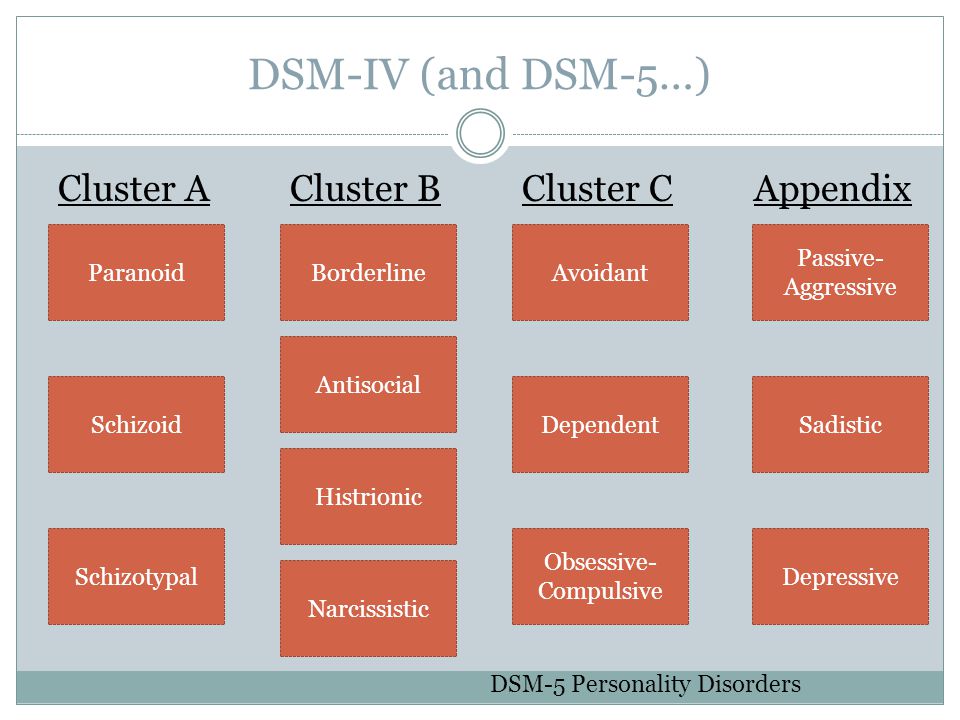 nine0003
nine0003
Normal sexual activity is currently defined as an extremely complex psychophysiological function localized along the hypothalamus-pituitary-gonadal axis, on the one hand, and having representation in higher cortical centers, on the other, not to mention the involvement of the limbic system. Sexual dysfunctions in mental disorders have a complex pathogenesis, since they are associated not only with the neurodynamic shifts discussed above, but also with previously formed behavioral conditioned reflex stereotypes of sexual behavior relating to all its manifestations - attraction, arousal, orgasm, ejaculation [42]. nine0003
The nervous regulation of sexual function is understood as a dynamic functional system that combines the cellular structures of different levels of the nervous system into a single regulatory mechanism [21]. The combination of cerebral and humoral components in it in the functional structure of libido determines the extraordinary lability of the latter under the influence of not only the general vitality and purely situational factors, but above all the emotional state of the individual. Erections, along with ejaculation, are characteristic phenomena of male sexuality and are mainly regulated by the autonomic nervous system. With affective disorders, regardless of the rhythm of sexual activity, there is always a vegetative imbalance of regulation: either the predominance of sympathicotonia (tachycardia, mydriasis, constipation, etc.), accompanied, as a rule, by an acceleration of ejaculation up to ejaculation ante portas ; or parasympathicotonia (bradycardia, low blood pressure, sweating, lacrimation, hypersalivation, etc.), accompanied by a slowdown in ejaculation up to anejaculation.
Erections, along with ejaculation, are characteristic phenomena of male sexuality and are mainly regulated by the autonomic nervous system. With affective disorders, regardless of the rhythm of sexual activity, there is always a vegetative imbalance of regulation: either the predominance of sympathicotonia (tachycardia, mydriasis, constipation, etc.), accompanied, as a rule, by an acceleration of ejaculation up to ejaculation ante portas ; or parasympathicotonia (bradycardia, low blood pressure, sweating, lacrimation, hypersalivation, etc.), accompanied by a slowdown in ejaculation up to anejaculation.
Systemic sexology explains orgasm as the result of a complex interaction of a number of structural formations located at different levels (pelvic, spinal, diencephalic and cortical). For the convenience of analysis, the system concept allows for a conditional separation from the considered functional unity of two levels - cerebral and segmental. Cerebral - unites all cortical conditioned reflex complexes of the genital area.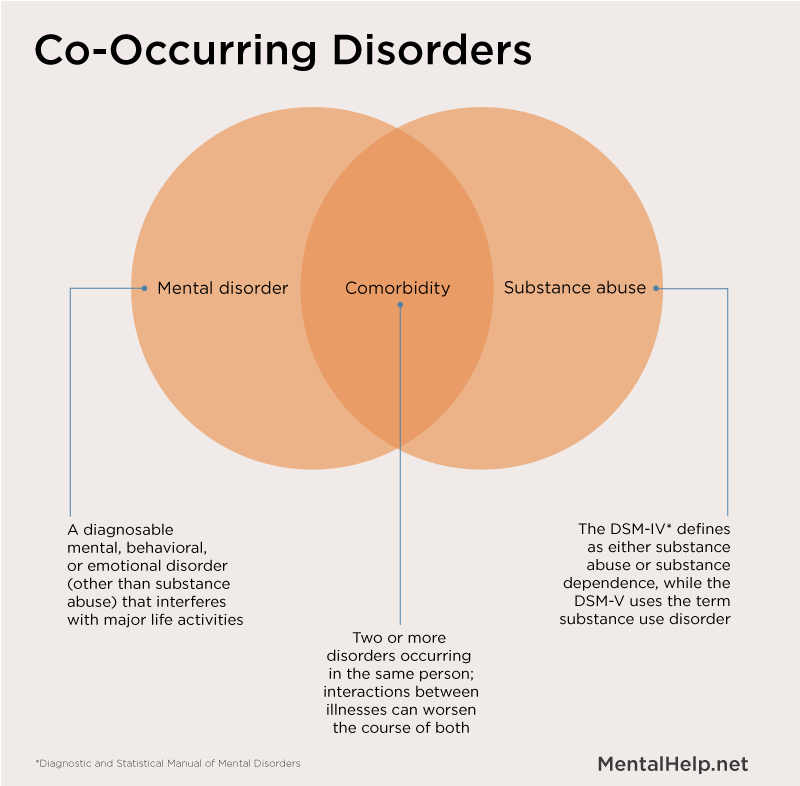 It includes the cerebral cortex and the parts of the diencephalon connected with the sexual sphere, including the visual tubercle. The segmental level includes the lumbar and sacral sections of the spinal centers of ejaculation with their extraspinal, including organ support. In the formation of a man's sexual desire, the same levels take part as orgasm, but the degree of participation of each of them is different. If in orgasm supraspinal (cerebral) mechanisms play the role of instances that mainly carry out sensory perception of the final phases of orgasm and their evaluation, then in the formation of libido, it is cerebral formations that perform all the main tasks throughout the entire life cycle [43]. nine0003
It includes the cerebral cortex and the parts of the diencephalon connected with the sexual sphere, including the visual tubercle. The segmental level includes the lumbar and sacral sections of the spinal centers of ejaculation with their extraspinal, including organ support. In the formation of a man's sexual desire, the same levels take part as orgasm, but the degree of participation of each of them is different. If in orgasm supraspinal (cerebral) mechanisms play the role of instances that mainly carry out sensory perception of the final phases of orgasm and their evaluation, then in the formation of libido, it is cerebral formations that perform all the main tasks throughout the entire life cycle [43]. nine0003
An important aspect of the violations under consideration is that superstrong conditioned reflex complexes formed during the pathological process are superimposed on their physiological basis. Natural sexual stimuli turn into a conditional brake, for example, in an altered physiological state, an attempt made under unfavorable conditions gives rise to a fear of repeating failure and leads to the fact that each subsequent attempt, with steadily increasing anxiety, first becomes less and less likely, and then completely excludes a favorable completion of intimacy. This in itself, in the final stages, intensifies existing affective disorders and forms already new and persistent reactive depressions. nine0003
This in itself, in the final stages, intensifies existing affective disorders and forms already new and persistent reactive depressions. nine0003
Thus, the pathogenesis of sexual disorders in depression, considered from a systemic standpoint, includes both morphofunctional (neuroanatomical, neurophysiological, neurochemical) and pathopsychological components. The mechanisms of suppression of sexuality with reduced affect are due to a violation of the mental and neuroendocrine components of the copulative cycle. Also, the pathological genesis of sexual dysfunctions is based on changes primarily at the level of neurotransmitter systems, and subsequently - autonomic, vascular and endocrine levels. nine0003
Summarizing the above, we can say that the pathogenesis of affective disorders and sexual dysfunctions is a single and multilevel process. Accumulating evidence suggests that there is a biological two-way relationship between depression and many sexual disorders, and psychosexual-related problems may be a psychogenic factor in the development and maintenance of an already existing depressive disorder.