Lamotrigine missed dose
How and when to take lamotrigine
Dosage
For epilepsy, the usual dose of lamotrigine is:
- adults and older children (aged 12 years and over) – 100mg to 700mg a day, taken as 1 or 2 doses
- younger children (aged 2 to 11 years) – the dose will vary depending on their weight
For bipolar disorder, the usual dose for adults is:
- between 200mg and 400mg a day, taken as either 1 or 2 doses
Changes to your dose
When you start taking lamotrigine, it's important to increase the dose slowly as this will help reduce or stop side effects.
Once you find a dose that suits you, it'll usually stay the same.
How to take it
You'll usually take lamotrigine once or twice a day. You can take it with or without food.
If you take it twice a day, try to space your doses evenly through the day. For example, take it first thing in the morning and in the evening.
If you're taking standard tablets, swallow them whole with a drink of water. Do not chew them.
If you're taking chewable or dispersible tablets, you can swallow them whole with a drink of water, or chew them or mix them with water or juice to make a drink.
How long to take it for
If you have epilepsy, it's likely that once your condition is under control you'll still need to take lamotrigine for many years.
If you have bipolar disorder, it's likely that you'll take lamotrigine for at least 6 months, but possibly much longer.
Important: Important
Do not stop taking lamotrigine without speaking to your doctor first.
If you forget to take it
If you take lamotrigine once a day and forget your dose, take the missed dose as soon as you remember, unless it's less than 12 hours until your next dose is due. In this case, leave out the missed dose and take your next dose at the usual time.
If you take it twice a day, take the missed dose as soon as you remember, unless it's less than 8 hours before the next dose is due. In this case, leave out the missed dose and take your next dose at the usual time.
Do not take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you have epilepsy, it's important to take this medicine regularly. Missing doses may trigger a seizure.
If you forget to take your tablets for more than 5 days in a row, speak to your doctor, as you'll need to start on a low dose again and gradually increase to your usual dose.
If you forget doses often, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
If you take too much
Taking too much lamotrigine can lead to symptoms such as:
- rapid, uncontrollable eye movements
- feeling clumsy or losing your balance
- feeling a change in the rhythm of your heartbeat
- having a seizure (fit)
- passing out
Urgent advice: Contact 111 for advice now if:
- you take more than your prescribed dose of lamotrigine
Go to 111.nhs.uk or call 111. If you need advice for a child under the age of 5 years, call 111.
If you have to go to A&E, do not drive yourself. Get someone else to drive you or call for an ambulance.
Get someone else to drive you or call for an ambulance.
Take the lamotrigine packet or the leaflet inside it, plus any remaining medicine, with you.
Stopping lamotrigine
Do not stop taking lamotrigine without talking to your doctor.
If you're taking lamotrigine for epilepsy, stopping it suddenly can cause seizures. Coming off lamotrigine should be done very slowly and might take a few months.
If you're taking lamotrigine for bipolar disorder, it's usually safe to stop taking it without having to reduce your dose first.
If you get a serious side effect, such as a severe skin rash, your doctor may tell you to stop taking lamotrigine straight away, even if you have epilepsy.
Page last reviewed: 20 May 2022
Next review due: 20 May 2025
I've Missed a Dose; What Should I Do?
Published: May 2003
Information on this subject
has been updated. Read the most recent information.
Read the most recent information.
Prescriber Update 24(1): 14
May 2003
Andrew Gilbert, Libby Roughead and Lloyd Sansom, Quality Use of Medicines and Pharmacy Research Centre, University of South Australia, Adelaide
Reprinted from Australian Prescriber 2002;25(1):16-18 with permission.
More than 80% of patients occasionally miss a dose of their medication. Health practitioners ought to plan with their patients what to do if a dose is missed. Patients believe that this plan should be a required part of the information received when a medication is prescribed and dispensed. Consumer Medicine Information sheets, which are available for most commonly prescribed medications, contain a section on what to do if a dose is missed. The routine use of these sheets or similar advice may help patients to know what to do when they miss a dose.
Introduction
Why don't consumers know what to do when they miss a
dose of their medication? As health professionals we know that the
vast majority of patients occasionally miss a dose of their medication.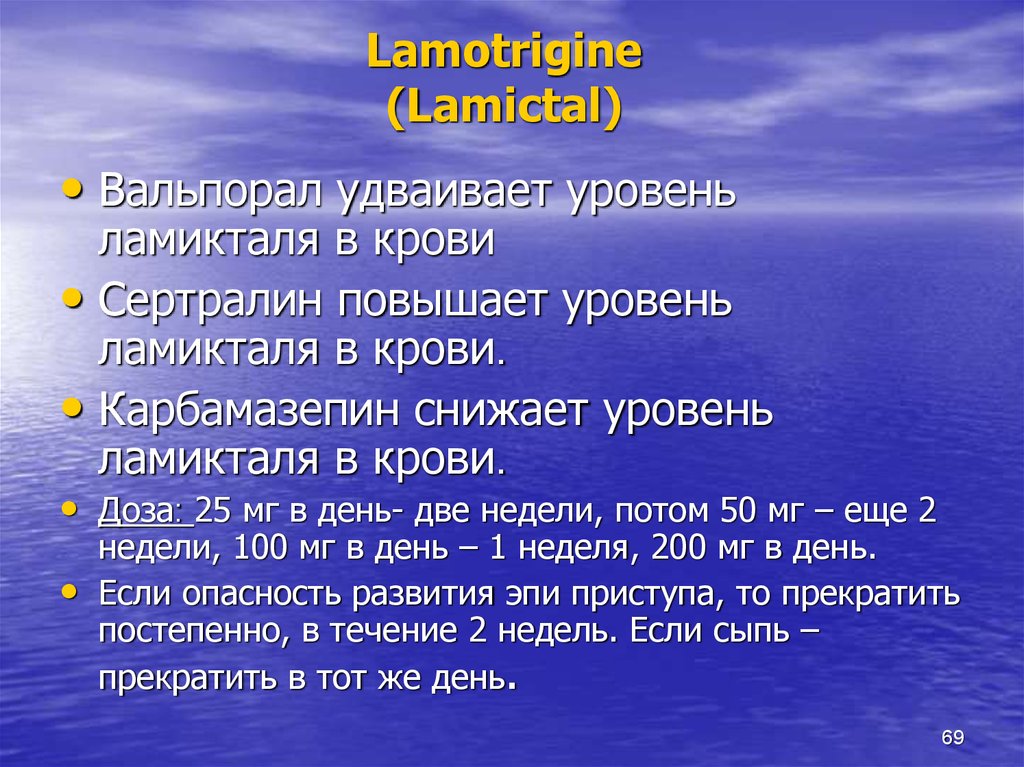 This unintentional non-compliance, and request for advice after the event,
is very common in practice. In a study of 205 people, 90% rated having information
on 'what to do if a dose is missed' as very important or important and only
1.5% did not want information on this topic.1
A USA study2 found that less than 50% of patients
received this information.
This unintentional non-compliance, and request for advice after the event,
is very common in practice. In a study of 205 people, 90% rated having information
on 'what to do if a dose is missed' as very important or important and only
1.5% did not want information on this topic.1
A USA study2 found that less than 50% of patients
received this information.
Given our understanding of the difficulties around compliance with medication regimens, it must be our expectation that many patients will miss doses. Informing them about what to do about a missed dose at the time of prescribing, dispensing and administration would seem to be a logical step towards improved compliance.
Pre-emptive advice
Missed doses could be viewed within the framework of patient non-compliance,
however the problems which arise often result because health professionals
do not give enough information to allow the patient to safely use the medication. Teaching a patient what to do if a dose is missed and providing strategies
to minimise the number of missed doses appears a sensible approach.3
Providing written information, that includes what to do if a dose is missed,
improves people's self-administration of medicines, including corrective
action when a dose is missed.4
Teaching a patient what to do if a dose is missed and providing strategies
to minimise the number of missed doses appears a sensible approach.3
Providing written information, that includes what to do if a dose is missed,
improves people's self-administration of medicines, including corrective
action when a dose is missed.4
In practice, giving information on what to do if a dose is missed should
not be too onerous a task for medical practitioners or pharmacists.
Most of the commonly prescribed medications in Australia come with, or have
available, a Consumer Medicine Information (CMI) sheet.a
All CMI sheets have a section entitled 'What to do if you miss a dose'.
Giving patients a CMI sheet the first time they receive a medication, and
using this material in discussion with patients at the time of prescribing
and dispensing would prepare them for this eventuality.
Assessing the importance of a missed dose (Table 1)
The severity of the patient's condition, whether clinically significant breakthrough effects are likely to be observed, and the characteristics of the medication should be considered when deciding the most appropriate strategy following a missed dose. Vulnerable patients are easily recognisable in any practice and include those on medications of low therapeutic index,b or suffering from conditions which require constant maintenance of therapeutic concentrations (for example epilepsy and thromboembolic diseases requiring anticoagulation). On the other hand, for most people with hypertension or hypercholesterolaemia a single missed dose will be of little consequence.
The patients should be informed at the time of prescribing and dispensing,
of strategies to minimise missed doses and to redeem the situation when
a dose is missed.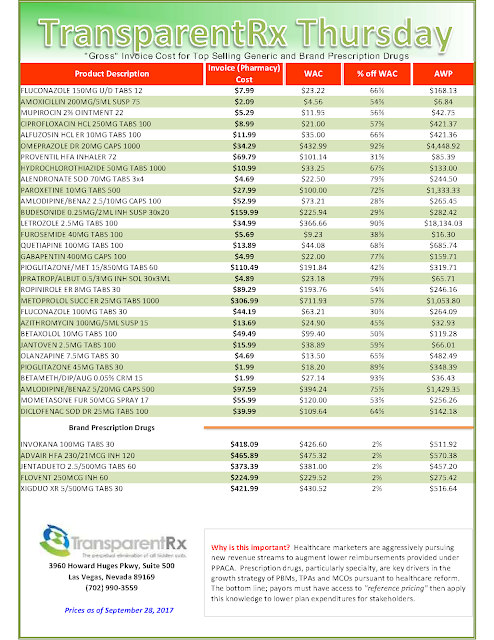 Highlighting the strategy as it appears on the CMI
or writing out an action plan as a reminder to the patient may prove very
useful.
Highlighting the strategy as it appears on the CMI
or writing out an action plan as a reminder to the patient may prove very
useful.
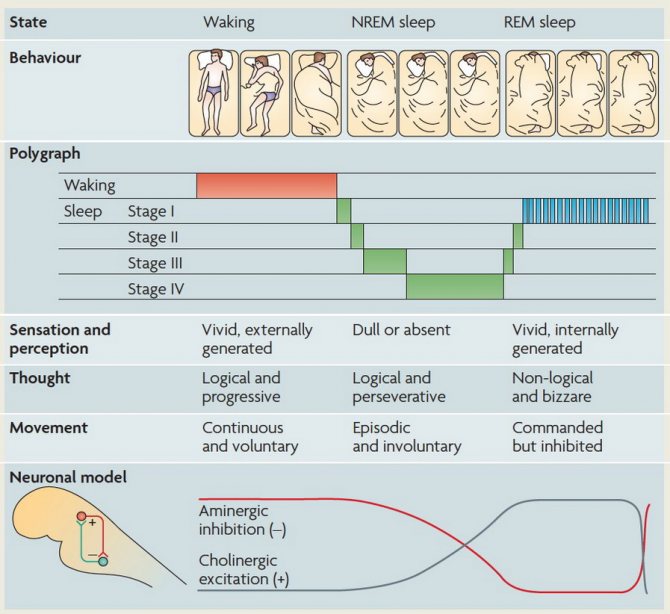
While a pre-emptive approach is ideal it is recognised that requests for information about missed doses are common. Knowledge of a drug's half-life, a major determinant of the fluctuation in interdose concentrations at steady state, is useful for making recommendations on what to do if a dose is missed. Upon cessation of therapy, it takes four to five half-lives for the drug to be completely eliminated.
In general, medications, or their active metabolites, with a long half-life
tend to create less problems when a dose is missed than medications with
a short half-life. However, the clinical effect of some drugs is not
related to the half-life. This usually occurs when the drug is acting
via an irreversible mechanism (for example aspirin's effect on platelets),
via an indirect mechanism (for example the effect of warfarin on blood coagulation),
when the drug is a pro-drug (in which case it is the half-life of the active
species that is important) or when the drug is converted to an active metabolite
which has a long half-life. 5
5
Missing several consecutive doses raises additional problems. For example, for drugs with long half-lives it can take a significant time to re-establish therapeutic concentrations when regular dosing resumes unless loading doses are given (for example digoxin). Drugs with short half-lives will lose therapeutic effect rapidly. Further, drugs with first-dose effects, for example an ACE inhibitor in combination with diuretics, may also present clinical problems when normal dosing is resumed. Overall, surprisingly few studies have examined the clinical significance of a missed dose.
Missed doses of the oral contraceptive pill have been well studied.
Women taking the pill need to be aware of the risk associated with missed
doses and of what to do when a dose is missed (Table
1). Given the complexity of this information, and the risk of
an unwanted pregnancy, it is important that any verbal counselling is supported
with appropriate written material. Where a CMI sheet is available
this can be used during the consultation. If no CMI sheet is available
for the prescribed product, written notes based on the recommendations in
the Australian Medicines Handbook are useful.6
Where a CMI sheet is available
this can be used during the consultation. If no CMI sheet is available
for the prescribed product, written notes based on the recommendations in
the Australian Medicines Handbook are useful.6
Conclusion
For the vast majority of patients an occasional missed dose will have little impact on the outcome of therapy. Most CMI sheets include statements such as:
- If you forget to take one or more doses: take your next dose at the normal time and in the normal amount. Do not take any more than your doctor prescribed.
- If you miss one dose, skip it and continue with your normal schedule.
Having this knowledge when starting therapy may be a simple way to alleviate much patient anxiety and in some cases avoid unwanted clinical consequences.
a In New Zealand, CMI fact sheets are available for
some medicines. These CMI can be freely accessed from the Medsafe web site:
www.medsafe.govt.nz/Medicines/infoSearch.asp
These CMI can be freely accessed from the Medsafe web site:
www.medsafe.govt.nz/Medicines/infoSearch.asp
b The therapeutic index reflects the range of concentrations between the drug concentration which produces toxic effects and the drug concentration required for therapeutic effects. A narrow therapeutic index means only small increases in concentration can cause toxicity and small decreases in concentration can result in loss of efficacy.
Conflict of interest: none declared
References
- Howard J, Wildman K, Blain J, Wills S, Brown D. The importance of drug information from a patient perspective. J Soc Admin Pharm 1999;16:115-26.
- Lyons RF, Rumore MM, Merola MR. An analysis of drug information desired by the patient. J Clin Pharm Ther 1996;21:221-8.
- Zind R, Furlong C, Stebbins M. Educating patients about missed
medication doses.
 J Psychosoc Nurs Ment Health Serv 1992;30:10-4.
J Psychosoc Nurs Ment Health Serv 1992;30:10-4.
- Paulson PT, Bauch R, Paulson ML, Zilz DA. Medication data sheets - an aid to patient education. Drug Intell Clin Pharm 1976;10:448-53.
- Sansom L, editor. Australian Pharmaceutical Formulary and Handbook. 17th ed. Canberra: Pharmaceutical Society of Australia; 2000.
- Australian Medicines Handbook 2000. 2nd ed. Adelaide: Australian Medicines Handbook Pty Ltd.; 2000. p. 17-9.
Table 1
Examples of medications for which missed doses may be clinically important, and information for patients on what to do if a dose is missed
| Medication | Information for consumers |
|---|---|
| Oral contraceptives | |
| Combined oral contraceptives | If one or more tablets are missed from the inactive tablets,
no additional contraceptive precautions are necessary, and tablet
taking should be recommenced ignoring the missed tablet or tablets. However, if all the inactive tablets are missed and then the next pack is not started on time, start as soon as it is remembered. Additional contraception (such as a condom or a diaphragm) must be used for the next 7 days. If an active tablet is forgotten take it as soon as it is remembered, within 12 hours after the time that it is normally taken. Then take the next and subsequent tablets at the usual time. If there is a delay of more than 12 hours after the time that the tablet is normally taken, contraceptive protection in this cycle may be reduced. There is more risk in becoming pregnant if tablets are missed during the first week, or at the end of the current pack. Take the missed tablet as soon as it is remembered, even if this means taking two tablets at the same time. Any earlier missed tablets are left in the pack. Continue taking a daily tablet as usual, and use additional contraceptive precautions (except for the rhythm or temperature method) for the next 7 days.  If these 7 days extend
into the inactive section, skip the inactive section and start a
new pack in the active area on the next day instead If these 7 days extend
into the inactive section, skip the inactive section and start a
new pack in the active area on the next day instead |
| Progestogen-only oral contraceptives | For women using the progestogen-only pill the recommendation for the use of other methods of contraception is extended to 14 days if the dose is delayed by three hours or more. |
| Anticonvulsants | |
| Acetazolamide Carbamazepine Ethosuximide Phenytoin Tiagabine Topiramate Vigabatrin |
If it is almost time for next dose (within 4 hours), skip the
missed dose and take the next dose when it is due. Otherwise, take
it as soon as it is remembered, and then go back to taking the medicine
as usual. Do not take a double dose to make up for the missed dose. This may increase the chance of you getting an unwanted adverse
effect.
This may increase the chance of you getting an unwanted adverse
effect. |
| Lamotrigine Sodium valproate |
Do not take a double dose to make up for the dose that you missed. (This drug has a long half-life.) |
| Digoxin Warfarin |
If it is almost time for the next dose, skip the missed dose and take the next dose when it is due. Otherwise, take it as soon as it is remembered, and then go back to taking the medicine as usual. Do not take a double dose to make up for the dose that you missed. |
| Psychotropics | |
| Lithium | If it is almost time for the next dose (within 2 hours), skip
the missed dose and take the next dose when it is due. Otherwise,
take it as soon as it is remembered, and then go back to taking
the medicine as usual.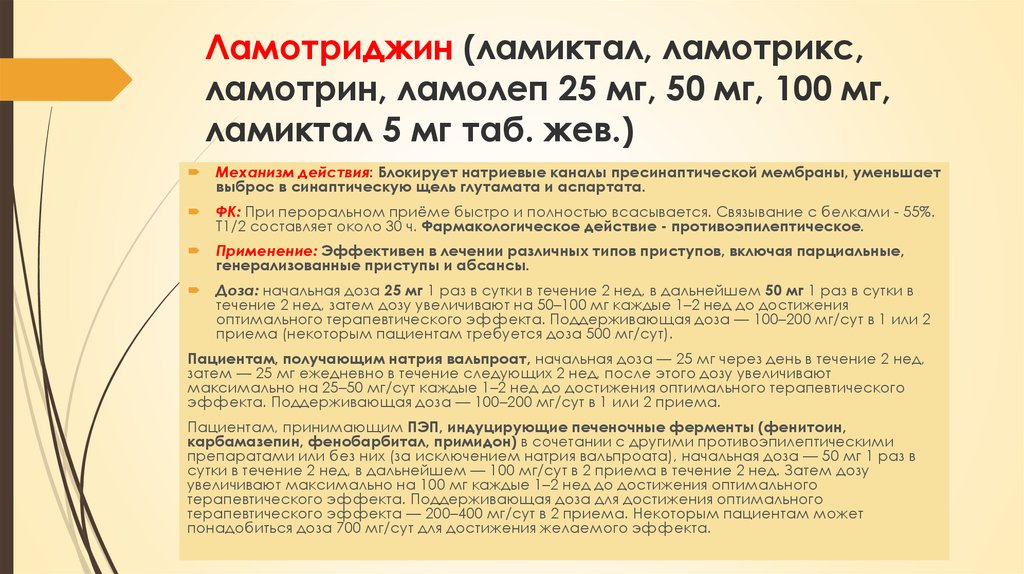 Do not take a double dose to make up for
the dose that you missed. Do not take a double dose to make up for
the dose that you missed. |
| Antidepressants other than monoamine oxidase
inhibitors Monoamine oxidase inhibitors |
If it is almost time for the next dose, skip the missed dose and take the next dose when it is due. Otherwise, take it as soon as it is remembered, and then go back to taking the medicine as usual. Do not take a double dose to make up for the dose that you missed. |
| Phenelzine Tranylcypromine | Do not take an extra dose. Wait until the next day and take the normal dose then. |
Media Publications
- Home
- Press Center
- Media Publications
(Lamoiriginum) INN
Synonyms. Lamictal.
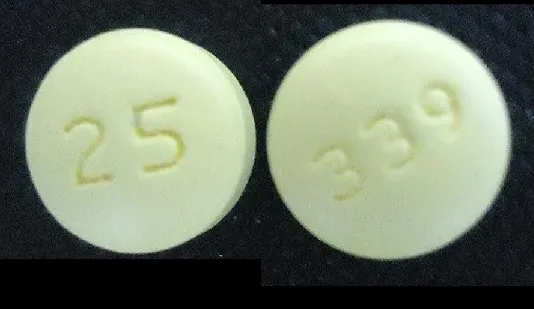
Composition and form of release. Lamotrigine 0. 025, 0.05 and 0.1 g tablets.
025, 0.05 and 0.1 g tablets.
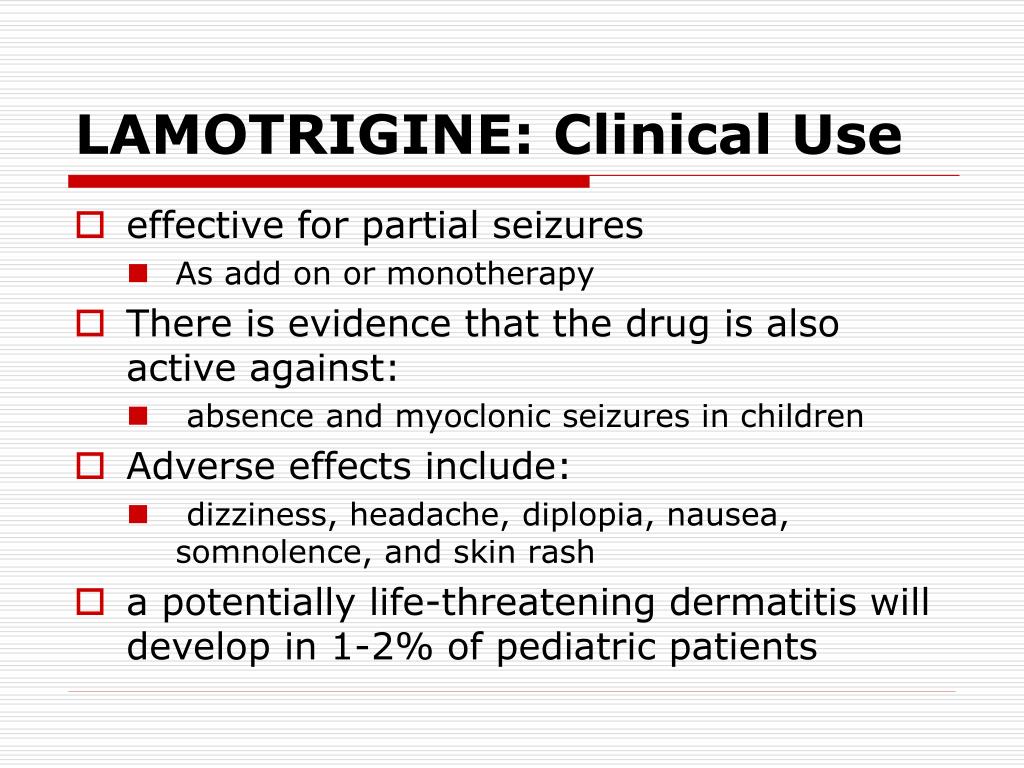
Indications. Epilepsy (mono- and adjuvant therapy for partial and generalized seizures).
Pharmacological action. Lamotrigine is an anticonvulsant drug capable of blocking the action of excitatory neurotransmitter amino acids (glutamate and aspartate). Blockade of voltage-dependent sodium channels, prevention of the release of excitatory amino acids, and stabilization of presynaptic neuronal membranes provide its anticonvulsant effect. Lamotrigine realizes its action through NMDA receptors of excitatory amino acids.
Pharmacokinetics. The drug, when taken orally, is absorbed quickly and completely from the gastrointestinal tract into the blood; the bioavailability of lamotrigine is 98%; food intake does not affect bioavailability. The volume of distribution is 1.2 l/kg. Peak plasma concentration is observed on average 2.5 hours after ingestion. Contacts proteins of plasma for 55%.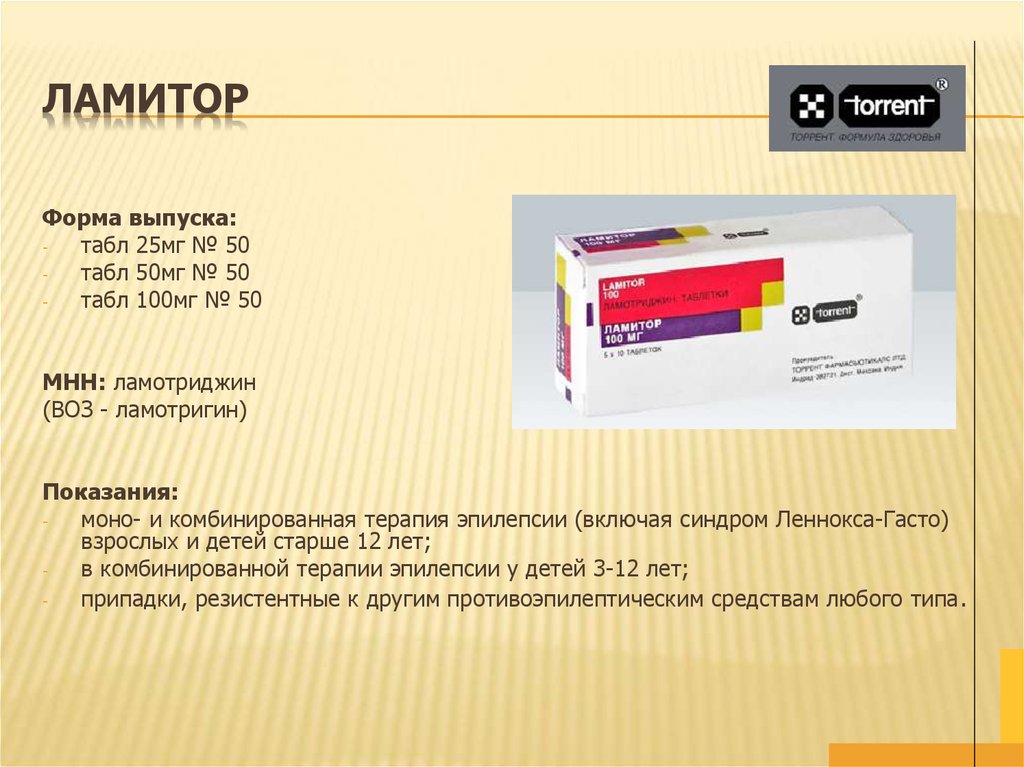 The drug is almost completely metabolized in the liver with the formation of the main metabolite - N-glucuronide. T1 / 2 is 29 hours. It is excreted mainly in the urine as the main metabolite and, partially, unchanged.
The drug is almost completely metabolized in the liver with the formation of the main metabolite - N-glucuronide. T1 / 2 is 29 hours. It is excreted mainly in the urine as the main metabolite and, partially, unchanged.
Side effects . Nausea, vomiting; feeling tired, headache, dizziness, irritability, drowsiness, tremor; blurred vision, diplopia; allergic reactions; lymphadenopathy.
Contraindications. Severe diseases of the liver, kidneys; hypersensitivity to the drug.
Adverse reactions when interacting with other drugs. The drug is not recommended to be taken simultaneously with drugs that depress the central nervous system, and with alcohol because of the dangerous potentiation of effects. Valproic acid, chloramphenicol, cimetidine inhibit the metabolism of lamotrigine and may increase its side effects. Carbamazepine, when taken simultaneously with lamotrigine, causes dizziness, diplopia, visual disturbances in the form of a veil before the eyes. The clearance of lamotrigine increases when it is taken simultaneously with carbamazepine or phenobarbital, or phenytoin, or primidone, which leads to a decrease in its T1 / 2.
The clearance of lamotrigine increases when it is taken simultaneously with carbamazepine or phenobarbital, or phenytoin, or primidone, which leads to a decrease in its T1 / 2.
Information for the patient. Lamotrigine is prescribed for adults and children 0.05 g 2 times a day 30-40 minutes before meals or after meals to avoid irritation of the gastric mucosa. If necessary, the daily dose can be increased. Alcohol and other CNS depressants should not be used during treatment with lamotrigine. Be careful when driving. Lamotrigine should be avoided during pregnancy. Cancellation of the drug is carried out gradually in order to avoid a sharp exacerbation of the disease. Missed dose: take the missed dose as soon as possible; if there is no time left to take the missed dose, then do not take it; do not take double doses.
Embed code
(Lamoiriginum) INN
Synonyms.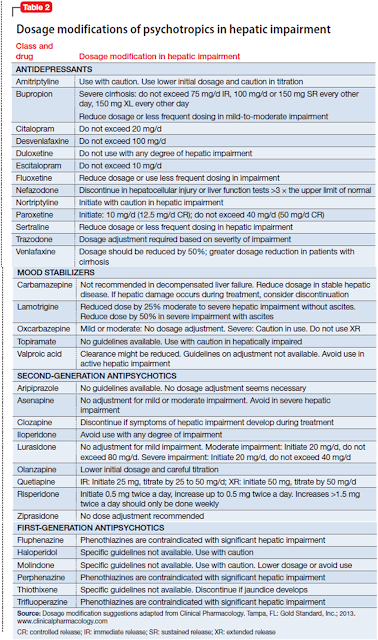 Lamictal.
Lamictal.
Composition and dosage form. Tablets of 0.025, 0.05 and 0.1 g of lamotrigine.
Indications. Epilepsy (mono- and auxiliary therapy of partial and generalized seizures).
Pharmacological action. Lamotrigine is an anticonvulsant drug capable of blocking the action of excitatory neurotransmitter amino acids (glutamate and aspartate). Blockade of voltage-dependent sodium channels, prevention of the release of excitatory amino acids, and stabilization of presynaptic neuronal membranes provide its anticonvulsant effect. Lamotrigine realizes its action through the NMDA receptors of excitatory amino acids.
Pharmacokinetics. When taken orally, the drug is absorbed quickly and completely from the gastrointestinal tract into the blood; the bioavailability of lamotrigine is 9eight%; food intake does not affect bioavailability. The volume of distribution is 1.2 l/kg. Peak plasma concentration is observed on average 2. 5 hours after ingestion. Contacts proteins of plasma for 55%. The drug is almost completely metabolized in the liver with the formation of the main metabolite - N-glucuronide. T1 / 2 is 29 hours. It is excreted mainly in the urine as the main metabolite and, partially, unchanged.
5 hours after ingestion. Contacts proteins of plasma for 55%. The drug is almost completely metabolized in the liver with the formation of the main metabolite - N-glucuronide. T1 / 2 is 29 hours. It is excreted mainly in the urine as the main metabolite and, partially, unchanged.
Side effects. Nausea, vomiting; feeling tired, headache, dizziness, irritability, drowsiness, tremor; blurred vision, diplopia; allergic reactions; lymphadenopathy.
Contraindications. Severe diseases of the liver, kidneys; hypersensitivity to the drug.
Adverse reactions when interacting with other drugs. The drug is not recommended to be taken simultaneously with drugs that depress the central nervous system, and with alcohol because of the dangerous potentiation of effects. Valproic acid, chloramphenicol, cimetidine inhibit the metabolism of lamotrigine and may increase its side effects. Carbamazepine, when taken simultaneously with lamotrigine, causes dizziness, diplopia, visual disturbances in the form of a veil before the eyes. The clearance of lamotrigine increases when it is taken simultaneously with carbamazepine or phenobarbital, or phenytoin, or primidone, which leads to a decrease in its T1 / 2.
The clearance of lamotrigine increases when it is taken simultaneously with carbamazepine or phenobarbital, or phenytoin, or primidone, which leads to a decrease in its T1 / 2.
Information for the patient. Lamotrigine is prescribed for adults and children 0.05 g 2 times a day 30-40 minutes before meals or after meals to avoid irritation of the gastric mucosa. If necessary, the daily dose can be increased. Alcohol and other CNS depressants should not be used during treatment with lamotrigine. Be careful when driving. Lamotrigine should be avoided during pregnancy. Cancellation of the drug is carried out gradually in order to avoid a sharp exacerbation of the disease. Missed dose: take the missed dose as soon as possible; if there is no time left to take the missed dose, then do not take it; do not take double doses.
(Lamoiriginum) INN
Synonyms. Lamictal.
Composition and form of release. Lamotrigine 0. 025, 0.05 and 0.1 g tablets.
025, 0.05 and 0.1 g tablets.
Indications. Epilepsy (mono- and adjuvant therapy for partial and generalized seizures).
Pharmacological action. Lamotrigine is an anticonvulsant drug capable of blocking the action of excitatory neurotransmitter amino acids (glutamate and aspartate). Blockade of voltage-dependent sodium channels, prevention of the release of excitatory amino acids, and stabilization of presynaptic neuronal membranes provide its anticonvulsant effect. Lamotrigine realizes its action through NMDA receptors of excitatory amino acids.
Pharmacokinetics. The drug, when taken orally, is absorbed quickly and completely from the gastrointestinal tract into the blood; the bioavailability of lamotrigine is 98%; food intake does not affect bioavailability. The volume of distribution is 1.2 l/kg. Peak plasma concentration is observed on average 2.5 hours after ingestion. Contacts proteins of plasma for 55%. The drug is almost completely metabolized in the liver with the formation of the main metabolite - N-glucuronide. T1 / 2 is 29 hours. It is excreted mainly in the urine as the main metabolite and, partially, unchanged.
The drug is almost completely metabolized in the liver with the formation of the main metabolite - N-glucuronide. T1 / 2 is 29 hours. It is excreted mainly in the urine as the main metabolite and, partially, unchanged.
Side effects . Nausea, vomiting; feeling tired, headache, dizziness, irritability, drowsiness, tremor; blurred vision, diplopia; allergic reactions; lymphadenopathy.
Contraindications. Severe diseases of the liver, kidneys; hypersensitivity to the drug.
Adverse reactions when interacting with other drugs. The drug is not recommended to be taken simultaneously with drugs that depress the central nervous system, and with alcohol because of the dangerous potentiation of effects. Valproic acid, chloramphenicol, cimetidine inhibit the metabolism of lamotrigine and may increase its side effects. Carbamazepine, when taken simultaneously with lamotrigine, causes dizziness, diplopia, visual disturbances in the form of a veil before the eyes.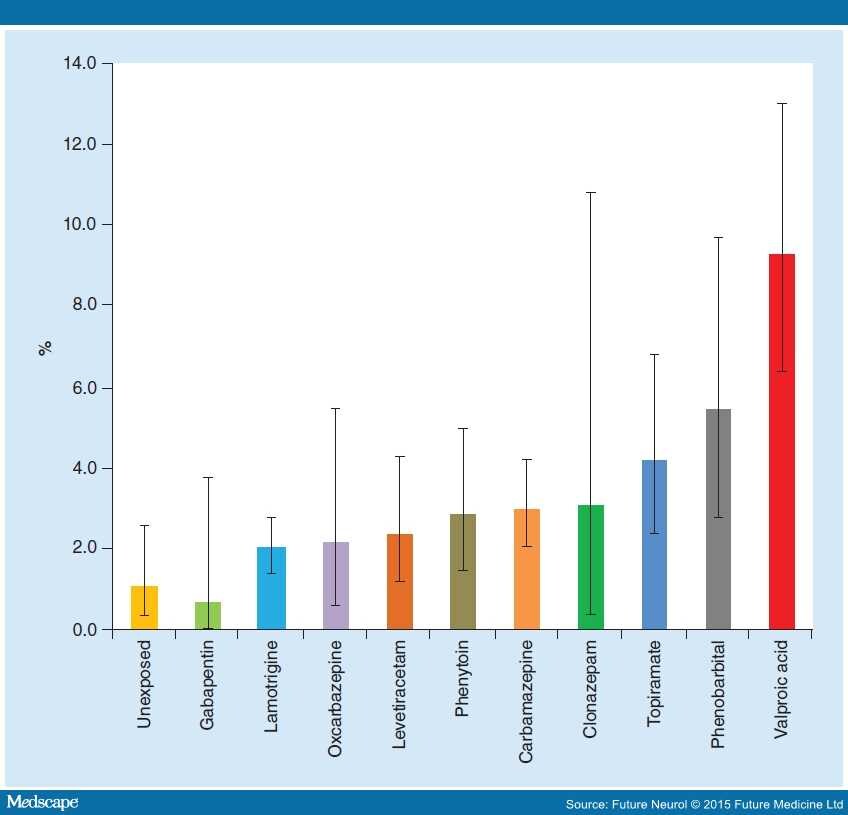 The clearance of lamotrigine increases when it is taken simultaneously with carbamazepine or phenobarbital, or phenytoin, or primidone, which leads to a decrease in its T1 / 2.
The clearance of lamotrigine increases when it is taken simultaneously with carbamazepine or phenobarbital, or phenytoin, or primidone, which leads to a decrease in its T1 / 2.
Information for the patient. Lamotrigine is prescribed for adults and children 0.05 g 2 times a day 30-40 minutes before meals or after meals to avoid irritation of the gastric mucosa. If necessary, the daily dose can be increased. Alcohol and other CNS depressants should not be used during treatment with lamotrigine. Be careful when driving. Lamotrigine should be avoided during pregnancy. Cancellation of the drug is carried out gradually in order to avoid a sharp exacerbation of the disease. Missed dose: take the missed dose as soon as possible; if there is no time left to take the missed dose, then do not take it; do not take double doses.
Go to section:
- News
- Events
- Video
- Photo gallery
- Library
- Newspaper "Sechenovskiye Vesti"
- Journal of National Health
- Website Terms of Use
| 💊 Composition of the drug Lamotrigine ✅ Use of the drug Lamotrigine Save Search for analogues Interaction Description of the active ingredients of the preparation Lamotrigine (Lamotrigine) The scientific information provided is general and cannot be used to make decisions. decisions about the use of a particular drug. Update date: 2020. Marketing authorization holder:ATOLL, OOO (Russia)
Produced:OZON, OOO (Russia) ATX code: N03AX09 (Lamotrigine) Active substance: lamotrigine (lamotrigine) Rec.INN WHO registered Dosage form
Release form, packaging and composition drug LamotrigineTablets white or white with a yellowish tint, round, flat-cylindrical, notched on one side and chamfered on both sides.
Excipients : lactose monohydrate (milk sugar) - 167.8 mg, microcrystalline cellulose - 76 mg, povidone K-25 - 19 mg, sodium carboxymethyl starch - 11.4 mg, magnesium stearate - 38 mg colloidal dioxide - 2 mg. 10 pcs. - cellular contour packings (1) - packs of cardboard. Clinical and pharmacological group: Antiepileptic drug Pharmacotherapeutic group: Antiepileptic Pharmacological actionAnticonvulsant. The mechanism of action is associated with the effect on voltage-dependent sodium channels of the presynaptic membrane. This leads to a decrease in the release of mediators into the synaptic cleft, primarily glutamate, an excitatory amino acid that plays an important role in the formation of epileptic discharges in the brain. Pharmacokinetics Following oral administration, lamotrigine is rapidly and completely absorbed from the gastrointestinal tract. T 1/2 in adults is an average of 29 hours Excreted by the kidneys mainly as a metabolite; about 8% of the active substance is excreted unchanged. T 1/2 less in children than in adults. Indications of the active substances of the drug LamotriginePartial and generalized tonic-clonic seizures (more often in cases of resistance to treatment with other anticonvulsants). Open list of ICD-10 codes
Dosing regimen The route of administration and dosing regimen of a particular drug depends on its form of release and other factors. When taken orally for adults and children over 12 years of age, the initial single dose is 25-50 mg, maintenance doses are 100-200 mg / day. In rare cases, doses of 500-700 mg / day may be required. For children aged 2 to 12 years, the initial dose is 0.2-2 mg/kg/day, the maintenance dose is 1-15 mg/kg/day. The maximum daily dose of for children aged 2 to 12 years, depending on the treatment regimen used, is 200-400 mg. The frequency of administration, the intervals between doses with increasing doses depend on the treatment regimen used, the patient's response to the treatment. Side effectsFrom the side of the central nervous system: headache, dizziness, drowsiness, sleep disturbances, fatigue, aggressiveness, confusion. From the digestive system: nausea, liver dysfunction. From the hematopoietic system: leukopenia, thrombocytopenia. Allergic reactions: skin rash (usually maculo-papular), angioedema, Stevens-Johnson syndrome, toxic epidermal necrolysis, lymphadenopathy. Contraindications for useSevere hepatic impairment, hypersensitivity to lamotrigine. Use in pregnancy and lactationClinical data on the safety of the use of lamotrigine during pregnancy and lactation are insufficient. When deciding on the need for use during pregnancy, the expected benefit of therapy for the mother and the potential risk to the fetus should be compared. Preliminary data show that lamotrigine passes into breast milk at a concentration of 40-45% of the plasma concentration. A small number of infants whose mothers received lamotrigine did not experience side effects. Use in hepatic impairmentContraindicated in severe hepatic impairment. Use in impaired renal function Use with caution in patients with renal insufficiency. Use in childrenDo not use lamotrigine in children under 2 years of age. Elderly useDo not use lamotrigine in elderly patients. PrecautionsUse with caution in patients with renal insufficiency. Lamotrigine should not be used in elderly patients. If severe allergic skin reactions occur, lamotrigine should be discontinued. With the sudden withdrawal of lamotrigine, the manifestations of epilepsy may increase, so it is necessary to gradually stop treatment, reducing the dose over 2 weeks. When used simultaneously with carbamazepine, dizziness, diplopia, ataxia, visual disturbances, nausea are possible. These phenomena, as a rule, disappear with a decrease in the dose of carbamazepine. Do not use lamotrigine in children under 2 years of age. Influence on the ability to drive vehicles and mechanisms During the treatment period, a slowdown in the speed of psychomotor reactions is observed. |
 100 mg: 10, 20, 25, 30, 40, 50, 60, 75, 90, 100, 125, 150, 250, 300 or 500 pcs. (46102)
100 mg: 10, 20, 25, 30, 40, 50, 60, 75, 90, 100, 125, 150, 250, 300 or 500 pcs. (46102) 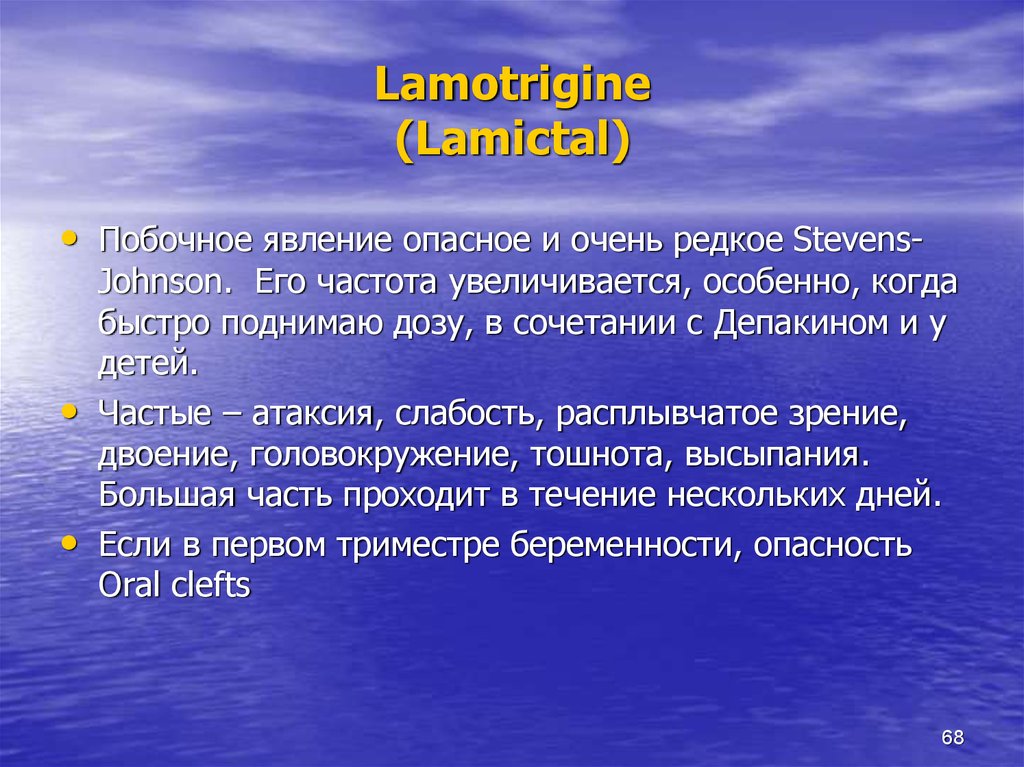 04.27
04.27  01.17 - Current
01.17 - Current 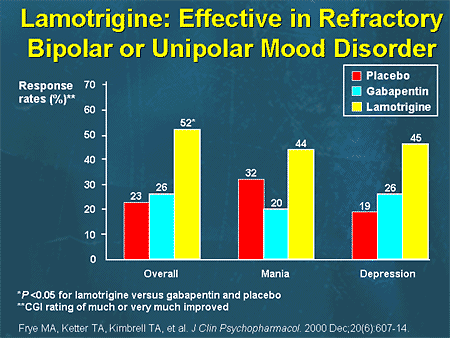

 C max in plasma is reached after about 2.5 hours. Plasma protein binding is 55%. It undergoes intensive metabolism with the formation of the main metabolite N-glucuronide.
C max in plasma is reached after about 2.5 hours. Plasma protein binding is 55%. It undergoes intensive metabolism with the formation of the main metabolite N-glucuronide.  The optimal dosage regimen is determined by the doctor. Compliance of the dosage form of a particular drug with indications for use and dosing regimen should be strictly observed.
The optimal dosage regimen is determined by the doctor. Compliance of the dosage form of a particular drug with indications for use and dosing regimen should be strictly observed.