Is depression a disability under ada
Is Depression Covered Under the Americans with Disabilities Act?
See New Jersey Disclaimer Page - Award Methodology
According to the Americans with Disabilities Act (ADA), a disability is defined as any physical or mental impairment that limits a major life activity. While physical disabilities are much easier to define, mental disabilities can be difficult to understand. Clinical depression is considered a disability under the ADA, but not everyone who suffers from it is protected. In general, the ADA is used on a case-by-case basis. Because no two people are the same, no two disabilities are either. There are many misconceptions about what depression is and how it affects people. Depression is not considered a disability by many, which means that people who suffer from it often face workplace discrimination. However, depression is a serious mental condition that can affect how a person functions in their daily life. In order for a person to be protected under the ADA, they must have at least one of the following:
- A physical or mental impairment that prevents them from performing a major life activity
- A medical history of suffering from a physical or mental ailment
- The perception that you suffer from a physical or mental impairment
While a person with clinical depression may fall under any of these categories, they still might not be protected by the ADA. In order to be protected by the act, the person with depression must be able to prove that their condition hinders their job performance. A factor that may contribute to a person with depression not being protect under the ADA is drug or alcohol abuse. Sometimes people with depression self-medicate, and the ADA does not protect people with substance abuse problems. You employer can only make reasonable accommodations for you if they are aware of your depression. You cannot file an ADA claim against your employer for discrimination if your employer had no way of knowing you were suffering from depression. The ADA does recognize that clinical depression is a permanent and serious condition, but if it does not affect your ability to perform major life activities or do your job, you will not be protected under the act. If you believe that you have been discriminated against, contact the Arcè Law Group today to schedule a free initial consultation. Our employment law attorneys can help you determine if your depression falls under the ADA and then guide you through the process of filing a claim in New York, New Jersey or Philadelphia.

By Bryan Arcé | Published January 10, 2016
Client Reviews
★★★★★
Gregory Kirschenbaum is an awesome attorney. He helps and understands clients need. He was very helpful and attentive towards me. I'll recommend him and the Arce Law Group, P.C. to anybody who needs legal assistance. Hector R.
★★★★★
Bryan and Greg, I am very pleased and satisfied in the manner that my case was conducted by you two lawyers. I appreciated you all very much. Thanks for a job well done. Ishmael C.
★★★★★
Arce Law Group was there for me during a trying time with my former employer the firm resolved my case to my satisfaction. Elijah C.
View More
Submit a Law Firm Client Review
Is Depression a Disability Under the ADA?
Depression and other mental conditions often qualify as disabilities under the ADA, for which you can get a reasonable accommodation.

Free evaluation for disability benefits. Get up to $3,345 per month.
Free evaluation for disability benefits. Get up to $3,345 per month.
Answer a few questions to check your eligibility.
How old are you?
Select an answer181920212223242526272829303132333435363738394041424344454647484950515253545556575859606162636465Select an answer181920212223242526272829303132333435363738394041424344454647484950515253545556575859606162636465
BackNext
Depression and other mental or emotional conditions can qualify as disabilities under the Americans with Disabilities Act (ADA). In fact, according to the Equal Employment Opportunity Commission (EEOC), the federal agency that enforces the ADA, depression is the impairment claimed in 6% to 7% of charges of disability discrimination that employees file each year.
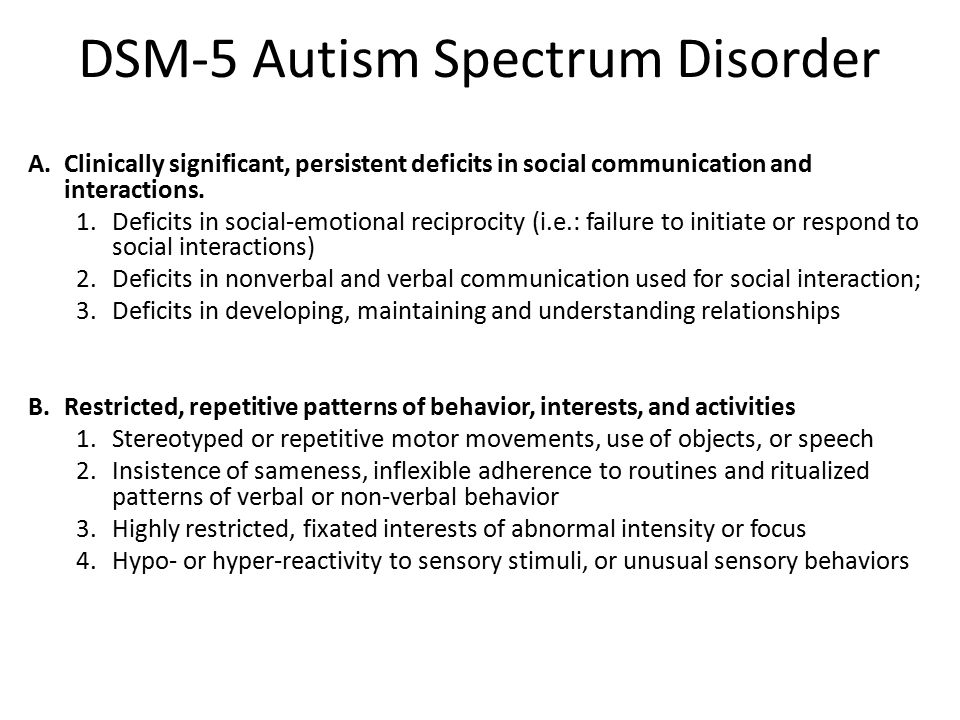
Not all impairments qualify as disabilities. The ADA doesn't include a list of conditions that always (or never) count as disabilities. Instead, the ADA counsels employers and courts to consider how the condition affects the individual employee. If depression substantially limits an employee's ability to perform major life activities, then it is a disability. And, if you have a disability, your employer must provide reasonable accommodations that will allow you to do your job.
Instead, the ADA counsels employers and courts to consider how the condition affects the individual employee. If depression substantially limits an employee's ability to perform major life activities, then it is a disability. And, if you have a disability, your employer must provide reasonable accommodations that will allow you to do your job.
How Does Depression Affect Daily Life?
The Mayo Clinic defines depression as a mood disorder that creates a "persistent feeling of sadness and loss of interest." According to the National Alliance on Mental Illness (NAMI), major depression is persistent and can significantly interfere with someone's moods, thoughts, activities, and behavior. Depression is more than a temporary case of the blues or the blahs: It can significantly disrupt daily life and cause serious symptoms such as sleep disturbances, loss of appetite, feelings of hopelessness and despair, suicidal thoughts, trouble with thinking, concentration, and memory, lack of energy, and loss of interest in normal activities, from exercise to socializing to sex.
When Depression Is a Disability
The ADA defines a disability as a physical or mental impairment that substantially limits a major life activity. Depression counts as a mental impairment, but it must substantially limit a major life activity to qualify as a disability that your employer must accommodate. Here's how the law defines these terms.
What Are Major Life Activities?
Tasks and functions that are basic to our everyday lives qualify as major life activities. For example, seeing, walking, hearing, and standing are major life activities that might be impaired by physical disabilities, such as paralysis, blindness, or back injuries. Major life activities that are often impaired by mental conditions, including depression, include sleeping, concentrating, thinking, communicating, interacting with others, eating, taking care of yourself, and regulating your emotions and thoughts.
Major bodily functions are also considered major life activities. If, for example, your depression affects the proper functioning of your neurological system, that would qualify as a limitation on a major bodily function.
What Is a Substantial Limitation?
You don't have to be completely incapable of sleeping, concentrating, or thinking, for example, to be substantially limited in performing these major life activities. Under the ADA, you are substantially limited if your ability to perform these tasks is limited in comparison to the general population. In making this determination, your employer should consider the manner, duration, and condition in which you can perform the activity. For example, if you can sleep for only a few hours a night, your ability to sleep is substantially limited. If it's very difficult for you to concentrate, and you can't focus for more than short periods of time, your ability to think is substantially limited.
The ADA does not consider "mitigating measures"—medication or other devices or assistance you might use to ameliorate the effects of your disability—when determining whether you are substantially limited. For example, if you have suffered several episodes of major depression, but your condition is currently controlled with medication, you still have a disability even though you may show no signs of impairment. The key is how your condition affects you when it is active and untreated.
The key is how your condition affects you when it is active and untreated.
Requesting an Accommodation for Depression
If you suffer from depression and you believe you need a reasonable accommodation, speak to your employer. Legally, you are entitled to a reasonable accommodation—a change to the job or the workplace—that will allow you to do your job with your disability, unless providing it would cause your employer undue hardship. Reasonable accommodations for depression might include scheduling changes, time off work to attend therapy appointments or for hospitalization, or changes in the way work is assigned, among other things. For more information, see the EEOC's guidance on depression, PTSD, and other mental health conditions.
Personal experience: how disability changes lives
October 19, 2019LifeColumn
The tragedy of a person who finds himself in difficult circumstances is that he does not yet realize that he has lost along with physical health.
Share
0Sergey Balashov
Web developer. In 2007 he received a disability of group I, paralyzed.
Everyone who supports the household knows the importance of well-being. As soon as some kind of illness or ailment appears, the list of important things that are waiting in the wings begins to grow rapidly.
This mostly applies to people with disabilities. Even the solution of ordinary everyday issues requires considerable effort, and the realization comes that you are no longer able to cope with the problem on your own.
What you need to be prepared for
1. Initially, you have someone to turn to for help: family, friends, good acquaintances, people who owe you something. At first, the problems are solved little by little.
2. Then the list of friends thins out: someone stops answering calls, someone promises to help, but does not help, someone “helps” so that they no longer contact him. Good friends disappear, and even more so everyone else is lost. But if you can still be useful to society, there are people who begin to use your resources. The more hopeless the situation you are in, the more arrogant these people are.
Good friends disappear, and even more so everyone else is lost. But if you can still be useful to society, there are people who begin to use your resources. The more hopeless the situation you are in, the more arrogant these people are.
Of course, there are those who sincerely want to help and offer a person with a disability a job that could well be entrusted to a healthy performer. But someone simply takes the opportunity to pay pennies for a voluminous task, knowing that a disabled person has little choice. Some descend to deceit. Such are people, and their weaknesses are so strong.
3. In the meantime, a person with a disability is losing faith in humanity. “He is honest, he won’t do that”, “We are a family!”, “How can a person forget how much I have done for him?” and many other beliefs are destroyed one by one.
4. “Wishlists” disappear from the overgrown to-do list: you need to at least save what you have. You could blow dust off your car and handle power tools and other valuables with care. When you have a disability, these things pass into the hands of other family members - often inexperienced - or even strangers. Often there is more breakage than repair, and you can only observe and give advice, which sooner or later leads to tension on both sides and even quarrels.
When you have a disability, these things pass into the hands of other family members - often inexperienced - or even strangers. Often there is more breakage than repair, and you can only observe and give advice, which sooner or later leads to tension on both sides and even quarrels.
5. At the next stage, a person begins to give up excess. When you sell your personal car to get rid of the cost of maintaining it, the ability to travel outside the house suffers. Initially, it seems that if there are several cars in a large family, then you can ask relatives to take them to a pension fund or bank. But over the years it turns out that this is not possible. Add to this the lack of an “accessible environment”, and it turns out that life will now take place within the apartment. For wheelchair users, this zone is even smaller - up to the first threshold or a bottleneck in the room.
The word "zone" is not accidental here: over time, the life of a paralyzed person is perceived in this way - as a prison sentence.
In a comfortable solitary cell with internet, music and TV.
Life imprisonment is perceived as very painful. I knew people who committed suicide while realizing how they were going to live.
6. A year later, the long-awaited humility appears. Good phrase, right? You have to forcefully humble yourself, otherwise the question is already whether you can bear the responsibility of a spouse and parent. You begin to equip your life and adapt yourself. You order other furniture: a suitable bed, a table. Thinking about how to decorate the room so that it is easier to keep positive in it.
However, he is lost, this positive. There are physical consequences that threaten a recumbent person. Amputation? Easily! Death from curvature of the spine? Easy!
7. The word "depression" is getting more and more serious. “What depression? I don't have time for this! I work two jobs in order to have time to make repairs, repay debts and loans, ”I said to disability, chuckling. Now depression is serious. The world turns away from you, your loved ones betray you, you are destroyed physically - how can you maintain an optimistic mood?
Now depression is serious. The world turns away from you, your loved ones betray you, you are destroyed physically - how can you maintain an optimistic mood?
This is another dangerous period. Some become addicted to alcohol or drugs. Someone, having gone through the most difficult time of the first acceptance of their disability, right now is taking their own lives.
8. Then the uphill road begins. We no longer rely on anyone, only on ourselves and our pension.
But what is this pension? It’s good if you have worked in a significant sector before and your actions were judged on merit. In my work book, continuous experience is noted: from 1992 to 2007, but my pension was lower than the social one. If I didn’t work a day all this time, and then became disabled, I would receive the same amount!
And when this miserable pension is not enough even to pay for utilities and maintain a life, a person thinks about a side job. What I could do before, now I can’t do it, so a new life makes me learn new professions.
You could end on a positive note and talk about how New Vasyuki blossomed, but in fact you get even more problems. In the labor market you are superfluous.
You offer your services to acquaintances, spam on social networks, call former employers, but in essence you are just wasting time that is so necessary for physical recovery and household chores. No one is going to pay you for work as much as a healthy employee: you cannot be present in the office or be constantly in touch.
A paralyzed person needs a total of about 4 hours of exercise therapy per day. Add here the time for hygiene and medical procedures - it will turn out to be almost 6 hours, and this is not taking into account household chores. Physiotherapy exercises have another important plus: it gives energy and helps to cope with depression. And if you decide to do something at the expense of training, it will not lead to anything good for you.
What to do to alleviate the situation
1. Place exercise therapy as efficiently as possible in your schedule. It is useful to allocate 1–1.5 hours for classes in the morning and the same amount closer to 4–5 pm. I also recommend doing a 5-minute workout every hour - it is very useful to combine it with the habit of drinking water.
Place exercise therapy as efficiently as possible in your schedule. It is useful to allocate 1–1.5 hours for classes in the morning and the same amount closer to 4–5 pm. I also recommend doing a 5-minute workout every hour - it is very useful to combine it with the habit of drinking water.
2. Keep a list of household chores. I would recommend using Todoist: it allows you to break down tasks into specializations and share the list with people who could do the work (for money or as a help). Before turning to specialists, try to accumulate an impressive list of tasks so that the cost of a home visit will pay off (of course, if we are not talking about urgent problems).
3. Don't whine, they don't like whiners. They are much more willing to help people who steadfastly meet life circumstances. And it also happens that among those whom you don’t even think about, there are people with problems even worse than yours.
4. Once you have become accustomed to your schedule and training, identify your options and think about what you could do in your circumstances. Start with creative attempts: if you find some talent, it will be much easier for you to master your niche in the future. If creative activities are not for you, choose options from those on the market. For example, you can try yourself in specialties related to the Internet or calls. Keep in mind that almost everyone will try to take advantage of your no-win situation, so don't talk about your situation, just look for a part-time job.
Once you have become accustomed to your schedule and training, identify your options and think about what you could do in your circumstances. Start with creative attempts: if you find some talent, it will be much easier for you to master your niche in the future. If creative activities are not for you, choose options from those on the market. For example, you can try yourself in specialties related to the Internet or calls. Keep in mind that almost everyone will try to take advantage of your no-win situation, so don't talk about your situation, just look for a part-time job.
The short conclusion is simple: moderate your ambitions, do everything possible for your recovery in your conditions, and do not count on the state or outside help.
Read also 🧐
- Cheat sheet: how to communicate with a child with a disability
- What rights do people with disabilities have in Russia and how to defend them
- What sex can teach if your partner has a disability
FGBNU NTSPZ.
 ‹‹Depression in General Medicine: A Guide for Physicians››
‹‹Depression in General Medicine: A Guide for Physicians›› Depressive states are the most common form of mental pathology in patients seeking help in general medical institutions, both outpatient and hospital networks.
According to modern estimates, the proportion of depression in patients of this contingent ranges from 10 [Katon W., Sulliven M. D., 1990] to 22-33% [Shmaonova L. M., Bakalova E. A., 1998; Ustun T. V., Sartorius N., 1995; Lyketsos C. G. et al, 1999].
Among elderly and senile patients who visit the territorial polyclinic, patients with depression make up 17.4% [Zozulya T.V., 1998].
Among the outpatients of the neurological clinic, as evidenced by the data of S. Kirk and M. Saunders (1997) when examining 2716 patients, affective disorders are found in 17% of cases.
When studying an approximately equal sample size (1927 patients of a psychiatric office of one of the territorial polyclinics of Moscow), the proportion of depressive disorders was 38. 2% of the identified mental pathology. Reactive depressions predominate - 28.1% (of which 18.9% are mild and 9.2% are moderately severe), the remaining 10.1% are shallow endogenous depressions within the framework of cyclothymia [Shmaonova L.M., Bakalova E.A. , 1998].
2% of the identified mental pathology. Reactive depressions predominate - 28.1% (of which 18.9% are mild and 9.2% are moderately severe), the remaining 10.1% are shallow endogenous depressions within the framework of cyclothymia [Shmaonova L.M., Bakalova E.A. , 1998].
As a result of our [Smulevich A. B. et al., 1999] on the basis of a territorial polyclinic of a continuous clinical and epidemiological examination of 495 patients who applied to a local therapist, it was found that depressive disorders in the aggregate occur in 21.5% of cases.
In economically developed countries (Sweden, Spain, USA, Australia, Japan, etc.), the frequency of depressive states in patients in a somatic hospital who applied for psychiatric counseling is comparable to the above indicator and reaches 20-29% [Ruskin P. E., 1985; Pauser H. et al., 1987; Al-Ansari E. A. et al., 1990; Hattori T. et al., 1990; Bertolo L D. et al., 1996].
Endogenous depressions (38.5%) and dysthymia (33. 8%) predominate, accounting for 2/3 of depressive disorders (72.3%).
8%) predominate, accounting for 2/3 of depressive disorders (72.3%).
The third place in frequency is occupied by vascular depressions - 16.9%, which coincides with the data of T. M. Siryachenko and N. M. Mikhailova (1998), according to which the frequency of vascular depressions in geriatric outpatient practice (specialized psychiatric office of the Moscow polyclinic) is 14 %.
Psychogenic depressions account for 10.8% (of which 6.2% are nosogenic and 4.6% are reactive).
According to the data of a continuous clinical and epidemiological survey of 921 patients of a large multidisciplinary hospital in Moscow [Smulevich A. B. et al., 1999], the frequency of depressive disorders approximately corresponds to the indicators obtained in the territorial polyclinic: every fifth (20.5%) patient suffers from depression.
In contrast to the outpatient contingent, psychogenic depressions are most common here. Their share is more than half (59.3%) of all depressive states. This part of depressive disorders is represented mainly by nosogenic depressions (45%), while reactive depressions associated with other psycho-traumatic effects were detected in 14.3% of patients.
This part of depressive disorders is represented mainly by nosogenic depressions (45%), while reactive depressions associated with other psycho-traumatic effects were detected in 14.3% of patients.
Dysthymia accounts for about 1/5 of cases of depressive states (21.2%).
Endogenous depressions (cyclothymia) are much less common - 13.8%, and vascular depressions are at least - only 5.7%.
Analysis of the ratio of depressive disorders of various origins with somatic diseases reveals the following dependencies (Table 4).
Table 4
Correlation between the form (nosological affiliation) of depression and the diagnosis of a somatic disease
| Nosological affiliation of depression | Diagnosis of a somatic disease | Patients with depression (% of the total number of patients diagnosed with this disease) |
| Psychogenic nosogenic* | myocardial infarction | 39 |
| eye injury | 38. | |
| Mallory-Weiss syndrome | 38 | |
| Acute peritonitis | 37 | |
| Systemic scleroderma | 34 | |
| Lung cancer | 33 | |
| Pancreas cancer | 33 | |
| primary tuberculosis | 33 | |
| Severe concomitant injury | 27 | |
| ENT Cancer | 33 | |
| Rectal cancer | 25 | |
| prostate cancer | 25 | |
| Chronic circulatory failure | 17 | |
| Chronic ischemic heart disease | 7 | |
| chronic colitis | 43 | |
| Osteochondrosis of the thoracic spine | 27 | |
| Osteochondrosis of the cervical spine | eighteen | |
| Type II diabetes | fourteen | |
| Chronic gastritis | 12 | |
| Cholelithiasis | 7 | |
| Residual effects after cerebrovascular accident | eight | |
| Congestive chronic circulatory failure | 7 | |
| chronic pneumonia | 7 | |
| Emphysema | 7 | |
| Encephalopathy | b |
* Reactive depressions due to other (non-nosogenic) psychotraumatic effects are evenly distributed across all categories of somatic diseases .
Among psychogenic depressions, nosogenic depressions (45% of all depressive disorders) are significantly more common in patients with severe, life-threatening or disabling somatic diseases. Such depressions are detected in more than 30 patients who have had a myocardial infarction, patients with oncological pathology (lung cancer, pancreatic cancer) and systemic connective tissue diseases, as well as in people with primary tuberculosis. The frequency of nosogenic depressions is quite high (37.5%) in patients with acute surgical pathology requiring urgent surgical intervention (acute peritonitis, Mallory-Weiss syndrome), as well as in patients with severe concomitant trauma (27%) and traumatic lesions of the organs of vision ( 38.5%).
At the same time, reactive depressions, which make up 14.3% of all depressions in the studied sample, do not show preference in relation to any individual forms of pathology of the internal organs. This, apparently, is explained by the fact that, unlike nosogenic depressions, reactive depressions are not directly related to somatic suffering and are caused by events related to family life or work.
Dysthymic disorder, which occurs in 22.1% of patients suffering from depression in a somatic hospital, is associated with protracted somatic diseases and occurs with a frequency of up to 25-30% in cancer patients (cancer of the rectum, ENT organs, prostate), less often (17 %) in chronic circulatory failure and even less frequently (7%) in chronic ischemic heart disease.
Endogenous depressions (13.8% of all depressions in the study sample) show a significant relationship with gastroenterological and neurological pathology. This type of depressive disorder is more common in patients with the main diagnoses of chronic colitis (43%), chronic gastritis (12%), cholelithiasis (7%). The frequency of endogenous depressions in patients diagnosed with osteochondrosis of the thoracic and cervical spine is 27 and 18%, respectively. Similar indicators for this pathology are also given by other researchers. Some authors believe that these calculations reflect an inadequately broad diagnosis of somatic pathology (osteochondrosis, colitis), but in reality we are talking about symptoms of depression that occurs with somatic algic and functional disorders. In our opinion, it is more adequate to consider the discussed ratios in connection with the negative impact of an affective disorder on the somatic state of the patient - with the manifestation of depression, the symptoms of diseases such as chronic gastritis, chronic colitis worsen, pain in patients with spinal osteochondrosis aggravates, which necessitates more intensive care and, accordingly, seeking inpatient care.
In our opinion, it is more adequate to consider the discussed ratios in connection with the negative impact of an affective disorder on the somatic state of the patient - with the manifestation of depression, the symptoms of diseases such as chronic gastritis, chronic colitis worsen, pain in patients with spinal osteochondrosis aggravates, which necessitates more intensive care and, accordingly, seeking inpatient care.
Vascular depressions (5.7% of all depressions in the studied sample) are significantly more often associated with diseases associated with impaired blood supply to the brain (residual effects after acute disorders of cerebral circulation - 8%, dyscirculatory encephalopathy - 6%, congestive chronic circulatory failure - 7% ). Vascular depression has a similar frequency (7%) also in patients with chronic lung diseases (chronic pneumonia, emphysema) accompanied by cerebral hypoxia. It should also be emphasized that vascular depressions are more common in neurological and cardiological clinics.
The data obtained generally confirm the results of other studies. The calculations given by the authors depend on the nature of the clinical manifestations and the characteristics of the course of the disease. It has been shown that with a high frequency of depression, reaching 20-25%, in patients with oncological diseases, in general [Plumb B., Holland J., 1977; Kathol R. et al, 1990] this indicator depends on the localization of the malignant neoplasm: with the greatest frequency, depressive disorders are detected in patients with pancreatic cancer and lung cancer [Holland J. C., 1986; Green A., Austin S., 1993; Passik S. D., Breitbart W., 1996; Zabora J. R. et al., 1996]. According to the results of our own study [Smulevich A. B. et al., 1999], in these forms of cancer, nosogenic depression prevails, the frequency of which reaches 33%, while dysthymic depressions are more typical for patients with prostate and colon cancer (25% ). The risk of developing depression increases in proportion to the duration of the oncological disease, the degree of maladjustment, the severity of the pain syndrome and other symptoms of cancer [Derogatis L.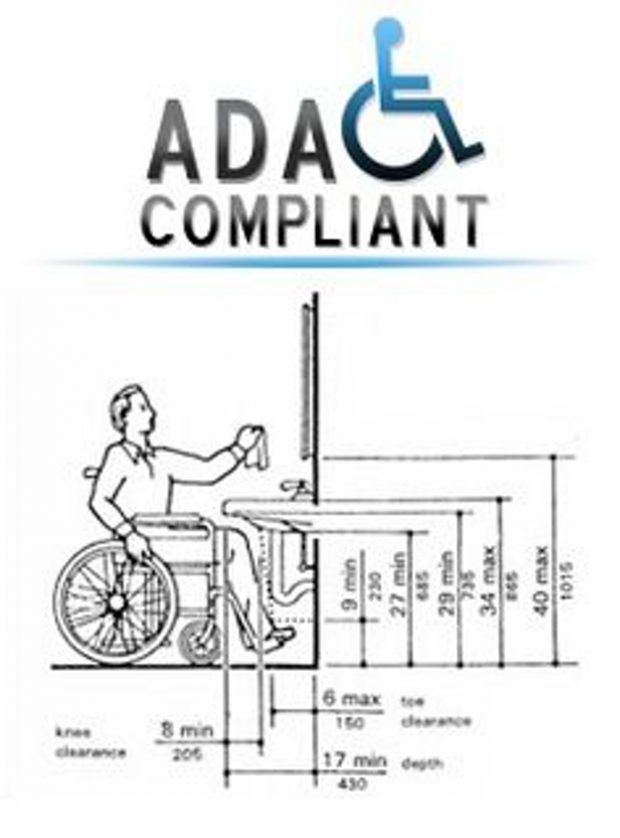 R. et al., 1983; Bukberg J. et al., 1984]. If the prevalence of depression in women is revealed in the population (in a ratio of 2: 1), then in oncological practice these disorders are approximately equally distributed among both sexes [DeFlorio M. L, Massie M. J., 1995].
R. et al., 1983; Bukberg J. et al., 1984]. If the prevalence of depression in women is revealed in the population (in a ratio of 2: 1), then in oncological practice these disorders are approximately equally distributed among both sexes [DeFlorio M. L, Massie M. J., 1995].
A number of diseases of the digestive system are also associated with an increased frequency of depressive disorders. These include, in particular, Crohn's disease and ulcerative colitis [Addolorato G. et al, 1997]. The highest frequency of comorbid depressive states in the so-called functional gastrointestinal disorders. Thus, in irritable bowel syndrome, the lifetime prevalence of depression reaches 60-70% [Walker E. et al., 1990; Tollefson G. et al., 1991]. A high frequency of depressive disorders has also been established for other variants of functional disorders of the gastrointestinal tract (GIT) - functional dyspepsia, gallbladder dysfunction, etc. [Drossman A. D. et al., 1994]. In such cases, endogenous (cyclothymic) and chronic (dysthymia) depressions predominate, the frequency of which reaches 60% (a joint study of the Department for the Study of Borderline Mental Pathology and Psychosomatic Disorders of the RAMS Scientific Center for Health and Psychology and the Laboratory of Chronobiology and Clinical Gastroenterology of the Russian Academy of Medical Sciences) [Komarov F. I. et al. ., 1999].
I. et al. ., 1999].
The frequency of depressive disorders in patients with acquired immunodeficiency syndrome (AIDS), as already mentioned, is at least 20% of the number of corporatized [May M., 1996]. The value of this indicator may depend on several factors (the psycho-traumatic content of information about the incurability of the infection, its progressive, disabling course), the importance of which increases due to the young age of patients and the negative attitude towards the AIDS patient of family members, colleagues and society as a whole.
We have received statistically significant confirmation of the adverse effect of depression of various origins on the adaptation of somatically ill patients, as already partly discussed in the introduction. The proportion of disabled people of groups I and II in terms of somatic disease with comorbid depression significantly exceeds the corresponding indicator for the studied sample as a whole.
Given in table. 5 differentiated data make it possible to verify that relatively more severe and prolonged vascular and endogenous depressions are especially unfavorable for the patient's adaptation to the manifestations of a somatic disease: when they are added to a somatic disease, the probability of disability in group 2 almost doubles (45.5 and 46.2% respectively, against 20.4% of patients of group 2 in the studied sample as a whole). The least favorable prognosis for working capacity in vascular depression, when almost 9times more often disability of the 1st group is registered (9.1% versus 0.9% in the general sample).
5 differentiated data make it possible to verify that relatively more severe and prolonged vascular and endogenous depressions are especially unfavorable for the patient's adaptation to the manifestations of a somatic disease: when they are added to a somatic disease, the probability of disability in group 2 almost doubles (45.5 and 46.2% respectively, against 20.4% of patients of group 2 in the studied sample as a whole). The least favorable prognosis for working capacity in vascular depression, when almost 9times more often disability of the 1st group is registered (9.1% versus 0.9% in the general sample).
Table 5. Correlation of depression with disability due to somatic disease in patients of a large multidisciplinary hospital, % ( n = 921)
| Physical disability | The proportion of disabled people with depression of various origins | For the entire sample | ||||
| Psychogenic | Vascular | Endogenous | Dysthymia | |||
| nosogenic | reactive | |||||
| I group | 1. | 3.7* | 9.1* | 0 | 2.5* | 0.9 |
| II group | 31.8* | 37.0* | 45.5* | 46.2* | 17.5 | 20.4 |
* Significantly higher than in the studied sample as a whole (p < 0.05) .
It can also be seen that reactive depressions also have a negative impact on the performance and adaptation of somatic patients.
.jpg) 5
5  2
2