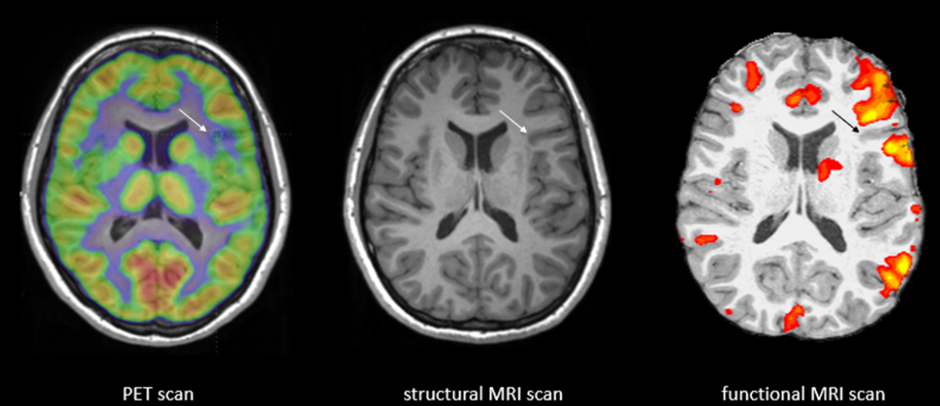
Imaging techniques pet cat mri fmri
Brain Imaging Techniques: Types and Uses
Many brain imaging techniques are used today, each one visualizing your brain in a unique way.
If your doctor has recently ordered a brain imaging scan, you might wonder what your upcoming session will be like or what types of brain imaging techniques might be used.
Experts have gradually improved techniques throughout the years to map out different parts of the brain and various brain functions.
There’s a lot that your doctor can learn from brain imaging, and the information that these scans provide can be helpful in forming a diagnosis and building a treatment plan.
While it may seem stressful to go in for brain imaging, you can take comfort in knowing that this is a safe and painless procedure.
The year 1924 marked the first human electroencephalography (EEG), recorded by German psychiatrist Hans Berger. This early EEG was able to detect electrical waves in the brain that would rise and fall as different brain cells communicated with each other.
Since then, neuroimaging techniques have gotten increasingly more sophisticated, and are an important tool for neurology and mental health specialists.
Commonly used brain imaging techniques are:
- functional magnetic resonance imaging (fMRI)
- computerized tomography (CT)
- positron emission tomography (PET)
- electroencephalography (EEG) and magnetoencephalography (MEG)
- functional near-infrared spectroscopy (fNIRS)
One of the benefits of brain imaging is how easily it can be performed. It doesn’t require invasive steps and often simply involves laying down and being still while the scan takes place around you.
These modern brain imaging techniques enable doctors to map out the regions and functions of your brain in a non-invasive way.
Brain imaging has many roles in health care and makes the jobs of diagnosticians easier. Some uses of brain imaging techniques include:
- identifying the effects of a stroke
- locating cysts and tumors
- finding swelling and bleeding
Doctors use a particular type of imaging method based on what they need to see in your brain.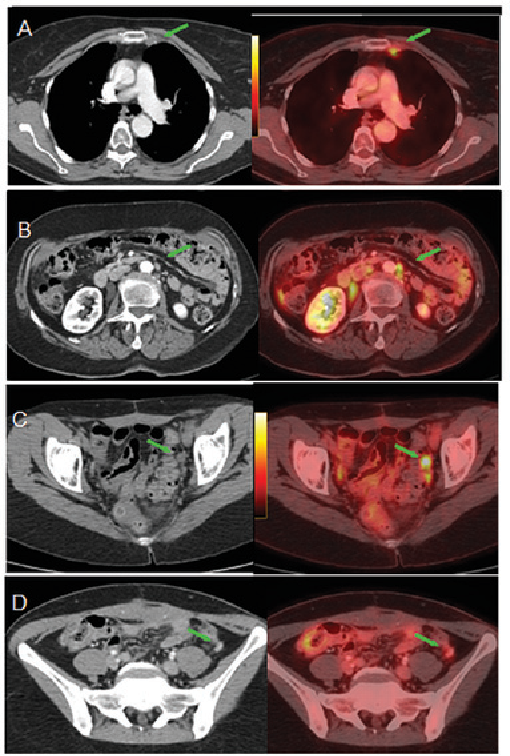 For example, if you are experiencing symptoms of multiple sclerosis (MS), your doctor can order an MRI scan to detect or rule out MS lesions. On the other hand, if you want to check for broken bones, they are more visible on a CT scan.
For example, if you are experiencing symptoms of multiple sclerosis (MS), your doctor can order an MRI scan to detect or rule out MS lesions. On the other hand, if you want to check for broken bones, they are more visible on a CT scan.
Brain imaging can also connect certain mental health issues to biological causes as well. According to a 2020 study, people with high levels of anxiety also displayed differences in brain connectivity when compared to people without anxiety. In addition, brain imaging can detect conditions such as early-stage psychosis.
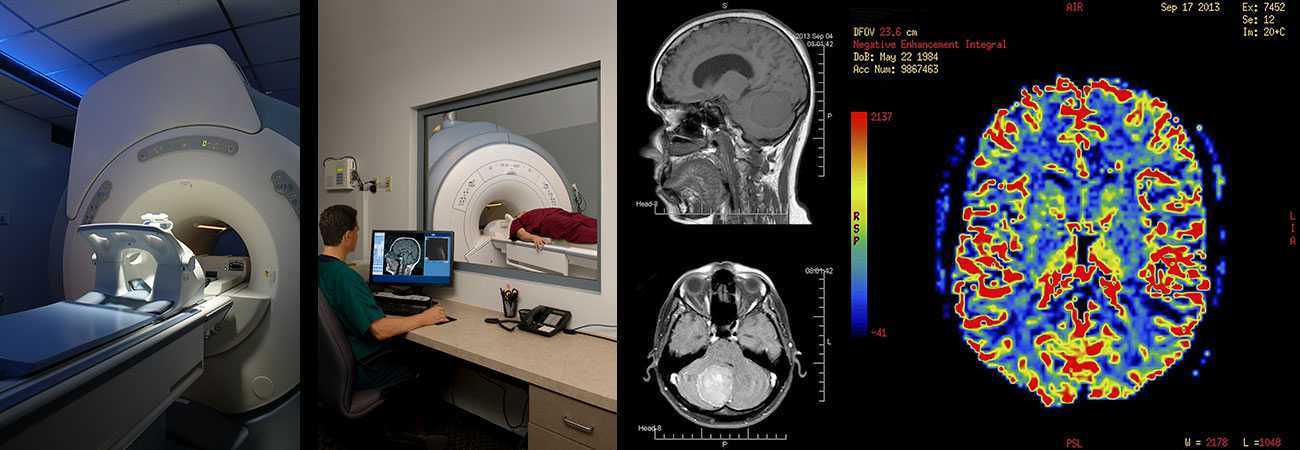
fMRI
Functional magnetic resonance imaging (fMRI) can detect changes in blood flow and oxygen levels that result from your brain’s activity. It uses the magnetic field of the scanner to affect the magnetic nuclei of hydrogen atoms, so they can be measured and converted into images.
MRIs display anatomic structure and fMRIs measure metabolic function.
fMRIs have many uses, such as:
- assessing brain activity
- finding brain abnormalities
- creating pre-surgical brain maps
CT
A computerized tomography (CT) scan is a series of X-ray images converted into cross-sectional images of your brain.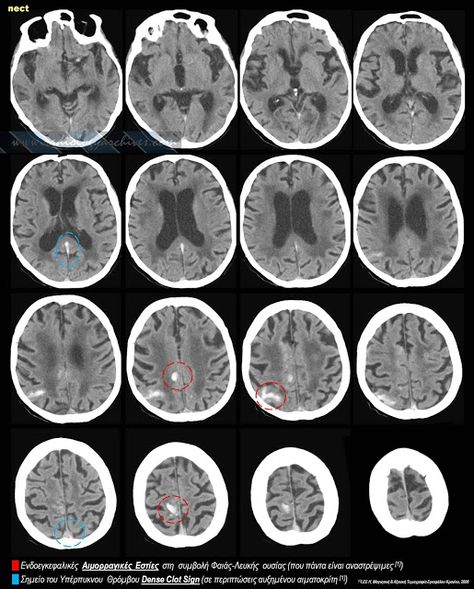 These X-rays are combined to form cross-sectional slices or even a 3-D model of your brain. The results of a CT scan can also provide more detail than a standard X-ray.
These X-rays are combined to form cross-sectional slices or even a 3-D model of your brain. The results of a CT scan can also provide more detail than a standard X-ray.
CT scans can:
- find certain types of brain injuries
- identify cancer
- locate brain swelling or bleeding
- reveal structural brain changes from schizophrenia
PET
A positron emission tomography (PET) scan uses a radioactive tracer that attaches to the glucose in your bloodstream. Since your brain uses glucose as its primary fuel source, the tracer accumulates in areas of higher brain activity.
A PET scan is able to see these tracers and observe how they move and accumulate in your brain. This allows doctors to see trouble spots where glucose isn’t moving correctly.
PET scans can evaluate:
- seizures
- Alzheimer’s
- tumors
EEG
An electroencephalography (EEG) test measures your brain waves. Before the scan, clinicians will attach small electrodes to your scalp that are attached to wires.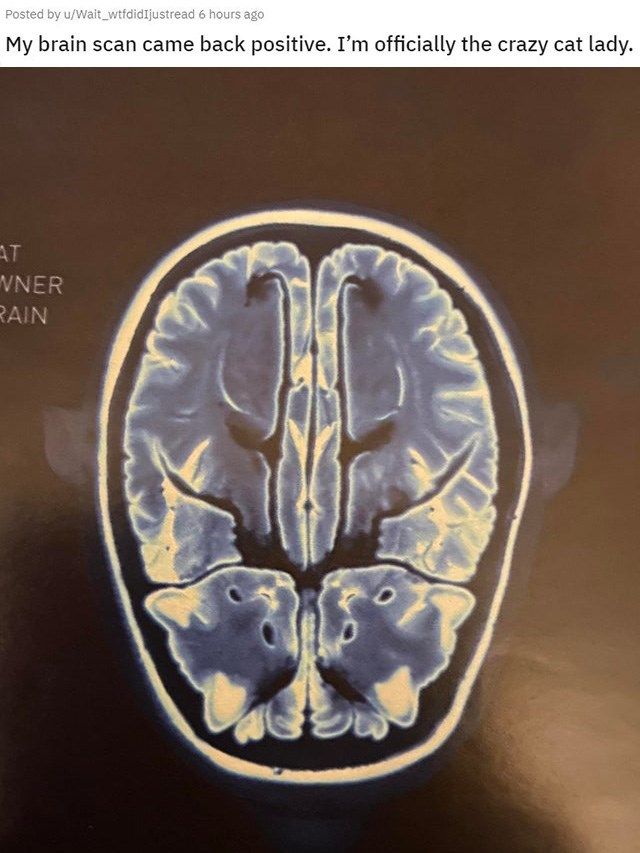 These electrodes detect electrical activity in your brain and send it to a computer where it creates a graph-like image. Each type of frequency appears on its own line and gives your doctor information about your brain activity.
These electrodes detect electrical activity in your brain and send it to a computer where it creates a graph-like image. Each type of frequency appears on its own line and gives your doctor information about your brain activity.
EEG can detect issues such as:
- anxiety
- head injuries
- epilepsy
- sleep disruption
MEG
Magnetoencephalography (MEG) measures the magnetic field from neuron electrical activity. This type of scan can locate and identify malfunctioning neurons in your brain. Doctors use MEG to evaluate both spontaneous brain activity, as well as neuronal responses triggered by stimuli.
MEG allows doctors to assess areas such as:
- epilepsy sources
- motor areas
- sensory areas
- language and vision
NIRS
Near-infrared spectroscopy (NIRS) monitors your brain’s oxygen saturation. It uses infrared light to detect variations in hemoglobin oxygen levels in your blood. Since oxygen is critical for your brain to function properly, NIRS can assist doctors in any clinical setting where brain oxygen levels may fluctuate.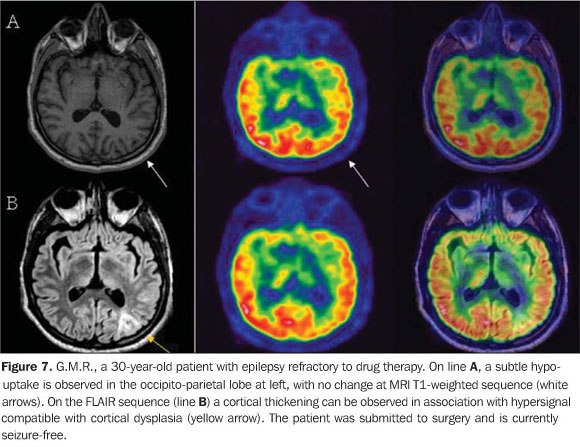
NIRS is used to monitor:
- brain oxygen levels during cardiac surgery
- brain function and oxygenation levels in preterm infants in a neonatal intensive care unit (NICU) setting
Brain imaging methods offer medical professionals a view of your brain to see if it’s structurally and functionally typical. There are several different brain scan types that map out different parts of your brain, but your specialist will know which one to use for the issue they’re investigating.
Brain imaging techniques do more than simply find medical issues, though. They can also identify brain differences associated with certain mental health conditions, such as schizophrenia, early-stage psychosis, and anxiety disorders.
If your doctor is sending you in for brain imaging, remember that this is a non-invasive procedure that will help your doctor have a clearer understanding of how your brain is functioning. After they receive the results, they can create the best and most accurate treatment plan specific to your needs.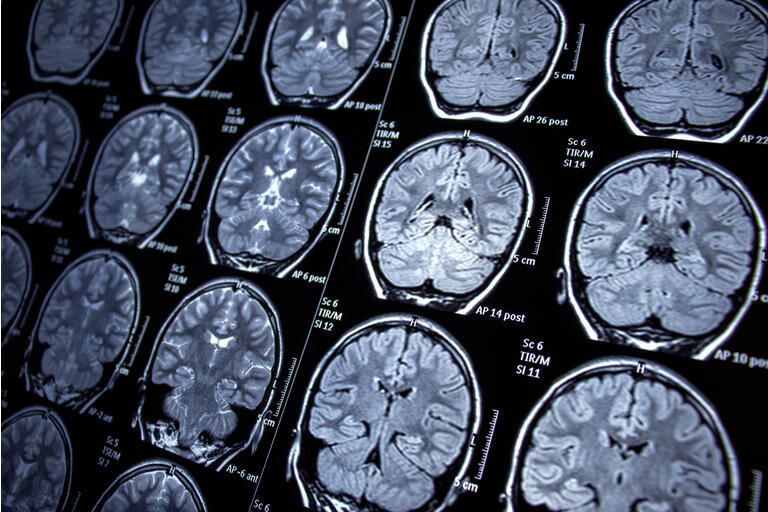
Brain Imaging Techniques: Types and Uses
Many brain imaging techniques are used today, each one visualizing your brain in a unique way.
If your doctor has recently ordered a brain imaging scan, you might wonder what your upcoming session will be like or what types of brain imaging techniques might be used.
Experts have gradually improved techniques throughout the years to map out different parts of the brain and various brain functions.
There’s a lot that your doctor can learn from brain imaging, and the information that these scans provide can be helpful in forming a diagnosis and building a treatment plan.
While it may seem stressful to go in for brain imaging, you can take comfort in knowing that this is a safe and painless procedure.
The year 1924 marked the first human electroencephalography (EEG), recorded by German psychiatrist Hans Berger. This early EEG was able to detect electrical waves in the brain that would rise and fall as different brain cells communicated with each other.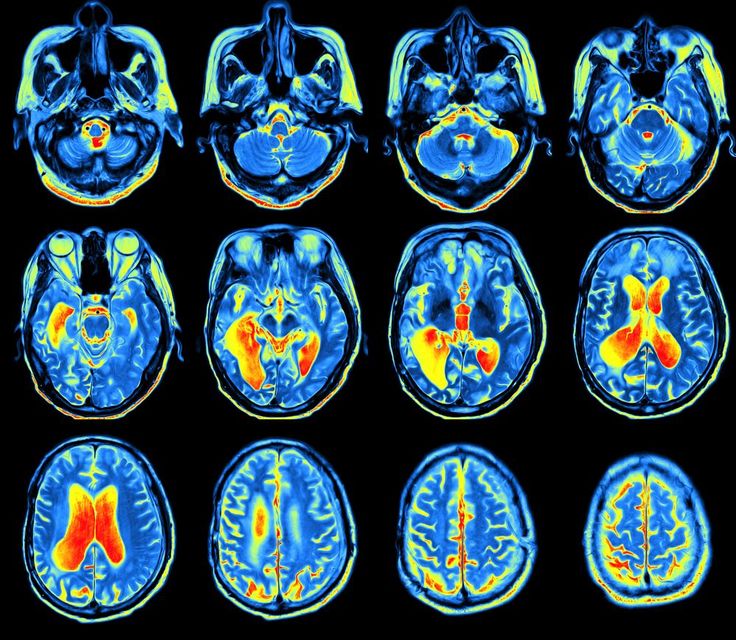
Since then, neuroimaging techniques have gotten increasingly more sophisticated, and are an important tool for neurology and mental health specialists.
Commonly used brain imaging techniques are:
- functional magnetic resonance imaging (fMRI)
- computerized tomography (CT)
- positron emission tomography (PET)
- electroencephalography (EEG) and magnetoencephalography (MEG)
- functional near-infrared spectroscopy (fNIRS)
One of the benefits of brain imaging is how easily it can be performed. It doesn’t require invasive steps and often simply involves laying down and being still while the scan takes place around you.
These modern brain imaging techniques enable doctors to map out the regions and functions of your brain in a non-invasive way.
Brain imaging has many roles in health care and makes the jobs of diagnosticians easier. Some uses of brain imaging techniques include:
- identifying the effects of a stroke
- locating cysts and tumors
- finding swelling and bleeding
Doctors use a particular type of imaging method based on what they need to see in your brain.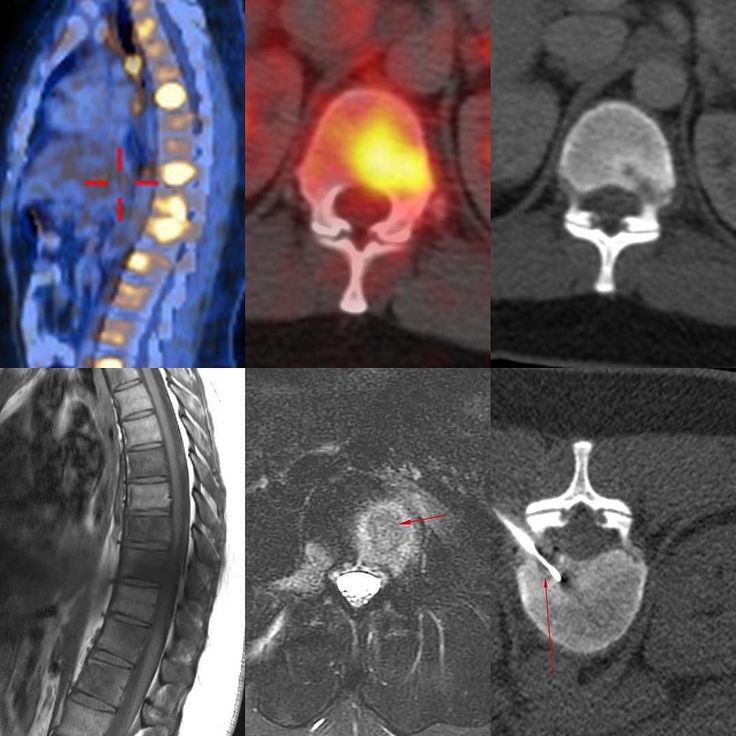 For example, if you are experiencing symptoms of multiple sclerosis (MS), your doctor can order an MRI scan to detect or rule out MS lesions. On the other hand, if you want to check for broken bones, they are more visible on a CT scan.
For example, if you are experiencing symptoms of multiple sclerosis (MS), your doctor can order an MRI scan to detect or rule out MS lesions. On the other hand, if you want to check for broken bones, they are more visible on a CT scan.
Brain imaging can also connect certain mental health issues to biological causes as well. According to a 2020 study, people with high levels of anxiety also displayed differences in brain connectivity when compared to people without anxiety. In addition, brain imaging can detect conditions such as early-stage psychosis.
fMRI
Functional magnetic resonance imaging (fMRI) can detect changes in blood flow and oxygen levels that result from your brain’s activity. It uses the magnetic field of the scanner to affect the magnetic nuclei of hydrogen atoms, so they can be measured and converted into images.
MRIs display anatomic structure and fMRIs measure metabolic function.
fMRIs have many uses, such as:
- assessing brain activity
- finding brain abnormalities
- creating pre-surgical brain maps
CT
A computerized tomography (CT) scan is a series of X-ray images converted into cross-sectional images of your brain.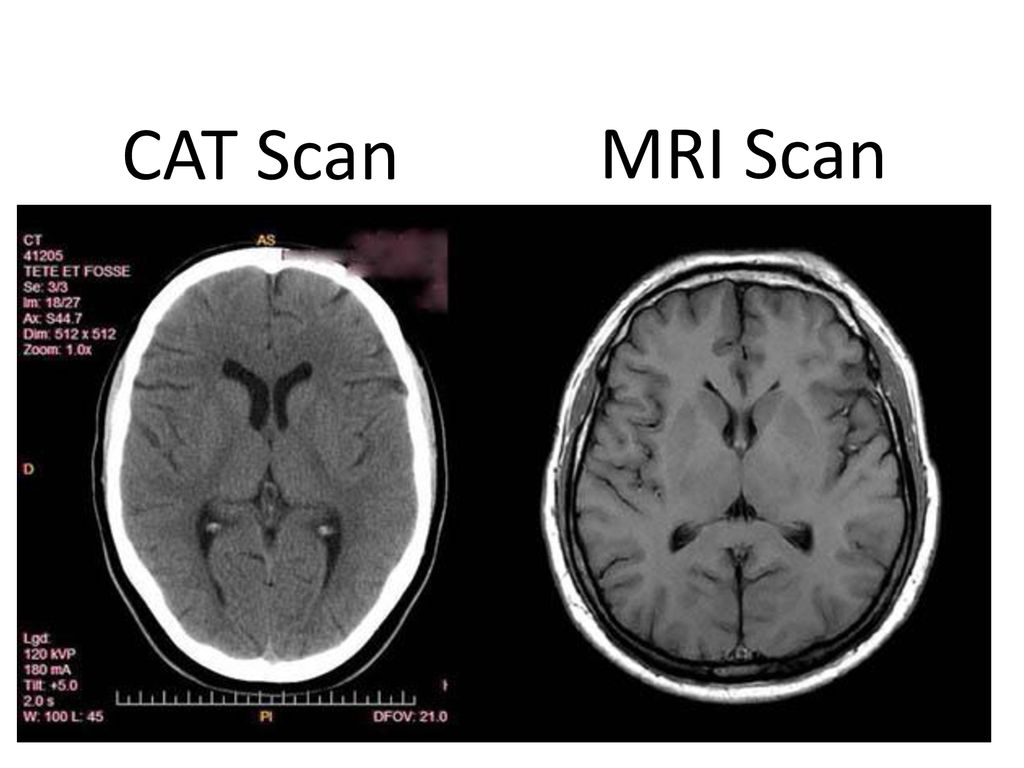 These X-rays are combined to form cross-sectional slices or even a 3-D model of your brain. The results of a CT scan can also provide more detail than a standard X-ray.
These X-rays are combined to form cross-sectional slices or even a 3-D model of your brain. The results of a CT scan can also provide more detail than a standard X-ray.
CT scans can:
- find certain types of brain injuries
- identify cancer
- locate brain swelling or bleeding
- reveal structural brain changes from schizophrenia
PET
A positron emission tomography (PET) scan uses a radioactive tracer that attaches to the glucose in your bloodstream. Since your brain uses glucose as its primary fuel source, the tracer accumulates in areas of higher brain activity.
A PET scan is able to see these tracers and observe how they move and accumulate in your brain. This allows doctors to see trouble spots where glucose isn’t moving correctly.
PET scans can evaluate:
- seizures
- Alzheimer’s
- tumors
EEG
An electroencephalography (EEG) test measures your brain waves. Before the scan, clinicians will attach small electrodes to your scalp that are attached to wires. These electrodes detect electrical activity in your brain and send it to a computer where it creates a graph-like image. Each type of frequency appears on its own line and gives your doctor information about your brain activity.
These electrodes detect electrical activity in your brain and send it to a computer where it creates a graph-like image. Each type of frequency appears on its own line and gives your doctor information about your brain activity.
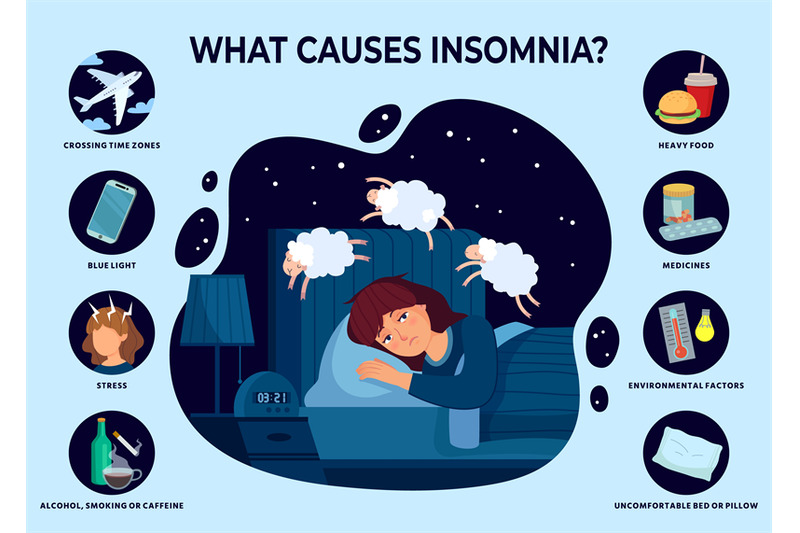
EEG can detect issues such as:
- anxiety
- head injuries
- epilepsy
- sleep disruption
MEG
Magnetoencephalography (MEG) measures the magnetic field from neuron electrical activity. This type of scan can locate and identify malfunctioning neurons in your brain. Doctors use MEG to evaluate both spontaneous brain activity, as well as neuronal responses triggered by stimuli.
MEG allows doctors to assess areas such as:
- epilepsy sources
- motor areas
- sensory areas
- language and vision
NIRS
Near-infrared spectroscopy (NIRS) monitors your brain’s oxygen saturation. It uses infrared light to detect variations in hemoglobin oxygen levels in your blood. Since oxygen is critical for your brain to function properly, NIRS can assist doctors in any clinical setting where brain oxygen levels may fluctuate.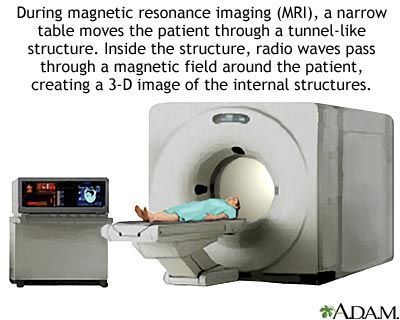
NIRS is used to monitor:
- brain oxygen levels during cardiac surgery
- brain function and oxygenation levels in preterm infants in a neonatal intensive care unit (NICU) setting
Brain imaging methods offer medical professionals a view of your brain to see if it’s structurally and functionally typical. There are several different brain scan types that map out different parts of your brain, but your specialist will know which one to use for the issue they’re investigating.
Brain imaging techniques do more than simply find medical issues, though. They can also identify brain differences associated with certain mental health conditions, such as schizophrenia, early-stage psychosis, and anxiety disorders.
If your doctor is sending you in for brain imaging, remember that this is a non-invasive procedure that will help your doctor have a clearer understanding of how your brain is functioning. After they receive the results, they can create the best and most accurate treatment plan specific to your needs.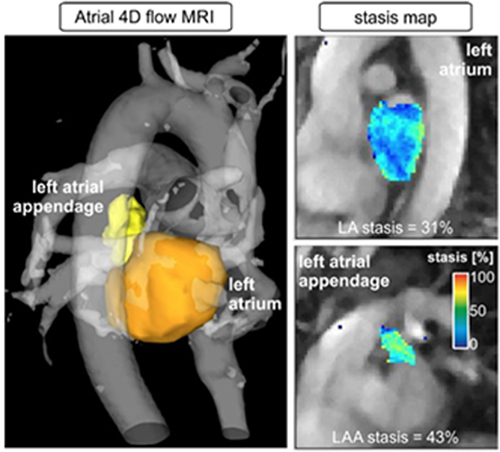
Visualization methods of diagnostics
The term “visualization” (from Latin visualis, “visual”) implies the presentation of any information in a form convenient for visual perception and analysis.
Medical imaging is a set of methods for obtaining an image of the internal structure of the body. Unlike invasive diagnostics (diagnostic operations), medical imaging does not imply a violation of the integrity of the skin or cavities of the human body.
The purpose of visualization is to diagnose pathological conditions or prepare for medical intervention, and sometimes to represent the functions of individual organs or tissues.
Medical imaging methods can be divided into several groups:
- radiological methods: fluorography, mammography, classical radiography (X-ray), computed tomography (CT), angiography and some others;
- ultrasound research methods: ultrasound, dopplerography;
- methods based on nuclear magnetic resonance phenomena : magnetic resonance imaging (MRI), MR diffusion, MR perfusion, MR angiography, MR spectroscopy, functional MRI (fMRI).
- radioisotope examinations: scintigraphy, positron emission tomography (PET)
- combined techniques: single photon emission computed tomography (SPECT), PET/CT, PET/MRI.
Almost all of the methods listed above can be used in oncology in various clinical situations and at various stages of diagnosis and treatment.
Instrumental examinations are prescribed in the following situations:
- in case of primary diagnosis of cancer to determine the size of the tumor and the spread of its foci throughout the body;
- when performing a biopsy as an auxiliary method to clarify the localization of the focus;
- during drug treatment to evaluate the effectiveness of treatment;
- when monitoring a patient after radical treatment (surgical, radiation, drug, or combinations thereof).
The first medical imaging technique invented. The method is based on the attenuation of X-ray radiation emitted by an X-ray tube when passing through various tissues of the human body with its subsequent registration on a special film or as an image on a computer.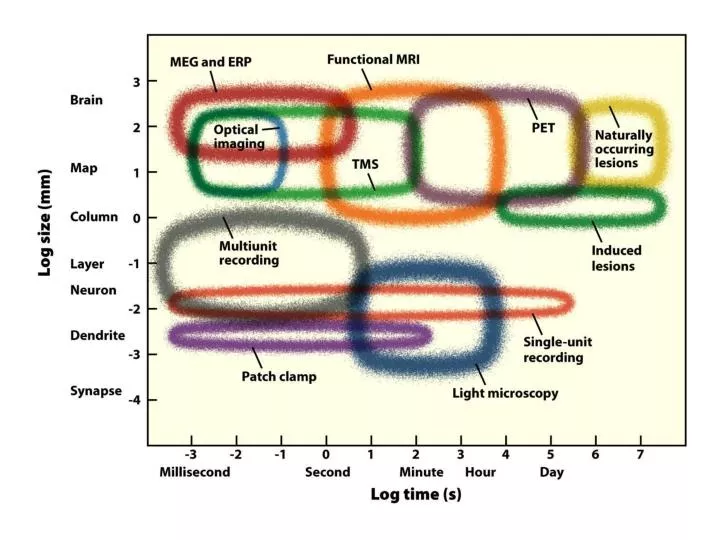
Examination is carried out in the supine or standing position for a few seconds. Sometimes you may need several studies at different intervals. At this time, you need to remain in one position motionless and sometimes hold your breath at the request of the X-ray technician. Also, the administration of a contrast agent (a liquid that is clearly visible on the obtained images) may also be prescribed. The contrast may be given by mouth, rectum, less commonly intravenously, or by other means.
As more efficient diagnostic methods have become available, the use of radiography in oncology is currently limited. However, this method is still applicable to assess bone tumors and bone tissue in general, to assess the mammary glands (mammography), as well as in some other (including emergency) situations.
The method is based on the use of ultrasonic waves emitted by an ultrasound machine. Depending on the density of the tissues under the sensor, the reflection of the waves changes, which is taken into account by the device and visualized as an image of the internal organs.
The examination takes 10-15 minutes, most often in the supine position. The ultrasound doctor will ask you to remove clothing that covers the skin in the projection of the organ under study and apply a special gel to the skin and to the sensor of the device, which improves sound transmission. From time to time it is required to change the position of the body, hold your breath. Sometimes, with the peculiarities of the location of the internal organs or the pronounced thickness of the subcutaneous fat layer, the doctor can press the sensor, trying to bring it closer to the organ under study. This may cause some discomfort for a short time. The applied gel can be wiped off at the end of the study.
In oncology, the use of ultrasound, as well as x-rays, is limited. The method is used to assess pathological processes in the mammary gland, to assess the volume of fluid in the pleural or abdominal cavity in case of a metastatic lesion, and also as an auxiliary method for biopsy.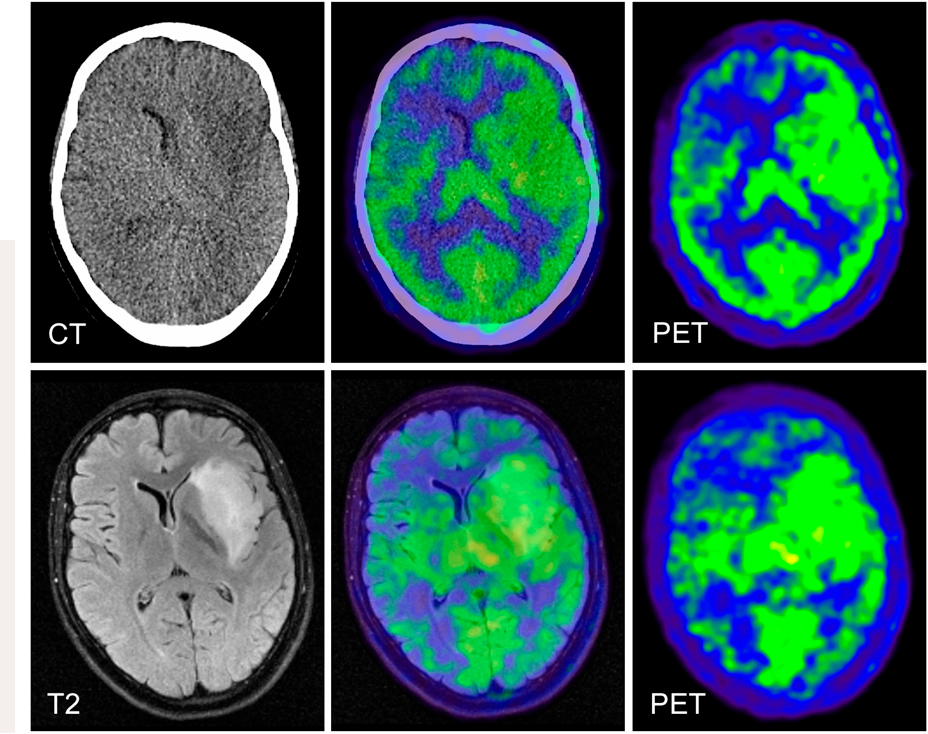 However, like x-rays, ultrasound is not recommended for detecting distant metastasis, dynamic monitoring, or monitoring the effectiveness of treatment.
However, like x-rays, ultrasound is not recommended for detecting distant metastasis, dynamic monitoring, or monitoring the effectiveness of treatment.
The principle of operation of CT consists in layer-by-layer examination of the body with an X-ray beam, followed by a computer analysis of tissue density in the area of study and the construction of a model of the human body.
The CT machine looks like a cylindrical tunnel with a movable table on which the patient is positioned.
Typically, an examination takes 5-20 minutes, depending on the number of areas to be examined. The patient lies on the table in a certain position and takes a comfortable position. A comfortable position on the table is important so that the patient can lie still on the table during the examination. Stillness is necessary to get high-quality pictures.
Sometimes the doctor prescribes contrast, which makes the study more informative. Most often, intravenous contrast is used, which is administered using special devices (infusion pumps, injectors) or manually by a laboratory assistant.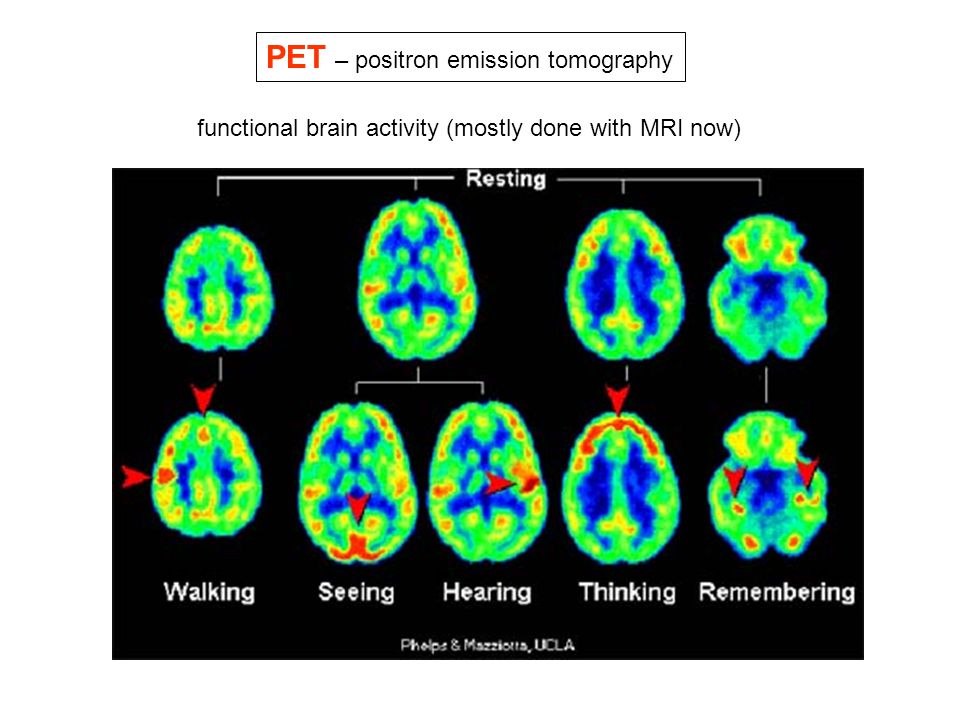 Some tests require holding your breath for a few seconds.
Some tests require holding your breath for a few seconds.
CT is one of the most commonly used imaging modalities in oncology and is used for all of the indications mentioned above.
The principle of operation of MRI also consists in the layer-by-layer study of the human body, but not with the help of X-rays, but with the phenomenon nuclear magnetic resonance.
The MRI machine is similar in appearance to the CT machine, but with a longer tunnel. Also, the device is different in that it constantly emits various sounds and noises. The study is similar to CT, but usually longer (up to 60-90 minutes), and also more sensitive to the patient's movements.
MRI is less commonly used in oncology due to technical limitations of the method, but is recommended for examining the brain and spinal cord, pelvic organs, soft tissue tumors, and certain abdominal organs.
This method, unlike those described above, is used to assess not the structure, but the function of human organs and tissues.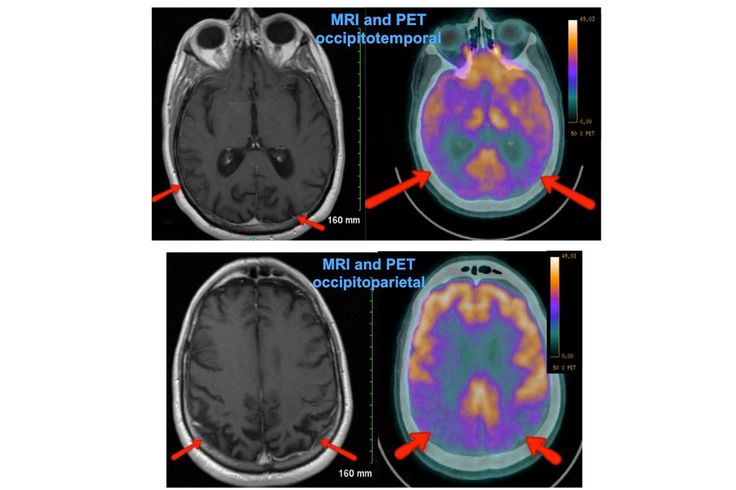 The essence of the method is the introduction of radioactive substances into the body, followed by an assessment of the foci of their maximum accumulation. When these substances are administered intravenously, they mainly accumulate in tissues that are well supplied with blood, or in cells that selectively accumulate this substance, which makes it possible to identify tumor foci.
The essence of the method is the introduction of radioactive substances into the body, followed by an assessment of the foci of their maximum accumulation. When these substances are administered intravenously, they mainly accumulate in tissues that are well supplied with blood, or in cells that selectively accumulate this substance, which makes it possible to identify tumor foci.
Externally, the scintigraphy machine is similar to an X-ray, but unlike it does not emit radiation, but captures the radiation of a radioactive substance from the patient's body.
The procedure may take several hours. First of all, a radioactive isotope is injected intravenously, after which it is necessary to wait 1-2 hours until it is distributed throughout the body, after which the study itself is carried out for about an hour.
In oncology, scintigraphy is used to diagnose primary bone tumors and bone metastases (osteoscintigraphy). There is also a combined method of scintigraphy together with CT, called SPECT.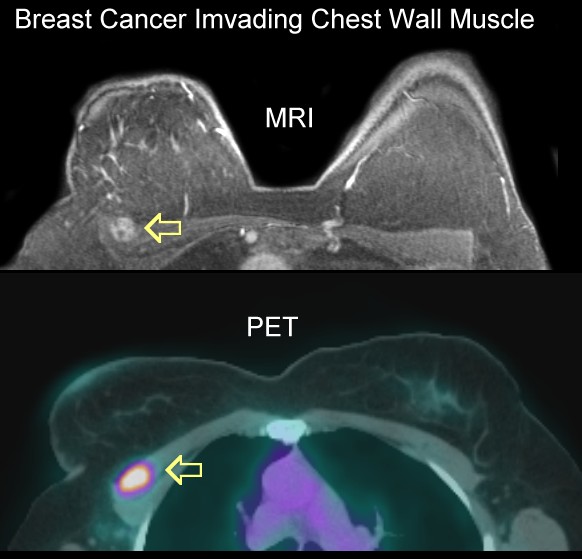 It allows you to simultaneously evaluate both the structure and function of organs and tissues.
It allows you to simultaneously evaluate both the structure and function of organs and tissues.
PET CT is a combined method that combines CT and radioisotope examination.
PET CT technique is generally similar to scintigraphy, but may take longer (up to 5-6 hours).
PET CT is an important diagnostic tool in oncology, combining the advantages of CT and radioisotope studies, and can be used, like CT, in many clinical situations.
Most of the described diagnostic methods do not require special training. Most often, before examining the organs of the gastrointestinal tract, it is required to exclude from the diet products that increase gas formation (onions, garlic, bread, apples, cabbage, milk and sour-milk products, legumes and nuts). When examining the pelvic organs, sometimes the patient may be asked to fill, or, conversely, empty the bladder and rectum.
If intravenous contrast is scheduled for CT, MRI, PET/CT, your doctor may recommend that you check your blood creatinine and urea levels. These indicators allow you to evaluate the work of the kidneys. If their function is impaired, some side effects from contrast agents will appear. You will also need to stop taking Metformin 48 hours before the scheduled injection of contrast.
These indicators allow you to evaluate the work of the kidneys. If their function is impaired, some side effects from contrast agents will appear. You will also need to stop taking Metformin 48 hours before the scheduled injection of contrast.
PET/CT requires more preparation. 24 hours before the study, it is recommended to exclude pronounced physical activity, hypothermia, foods high in carbohydrates or sugar, as all this can change the redistribution of the radiopharmaceutical throughout the body and distort the results. Also, in the presence of diabetes, it will be necessary to change the time of insulin administration.
To carry out the examination with you, it is important to have conclusions and disks with previous completed examinations. This will help the doctor track the dynamics of the disease.
There are no absolute contraindications for most investigations, however, due to radiation exposure, X-ray, CT scan, scintigraphy, or PET/PT is not recommended for pregnant women unless the risk is justified by clinical necessity (emergencies, suspected cancer) and examination cannot be replaced by a similar one (MRI, ultrasound).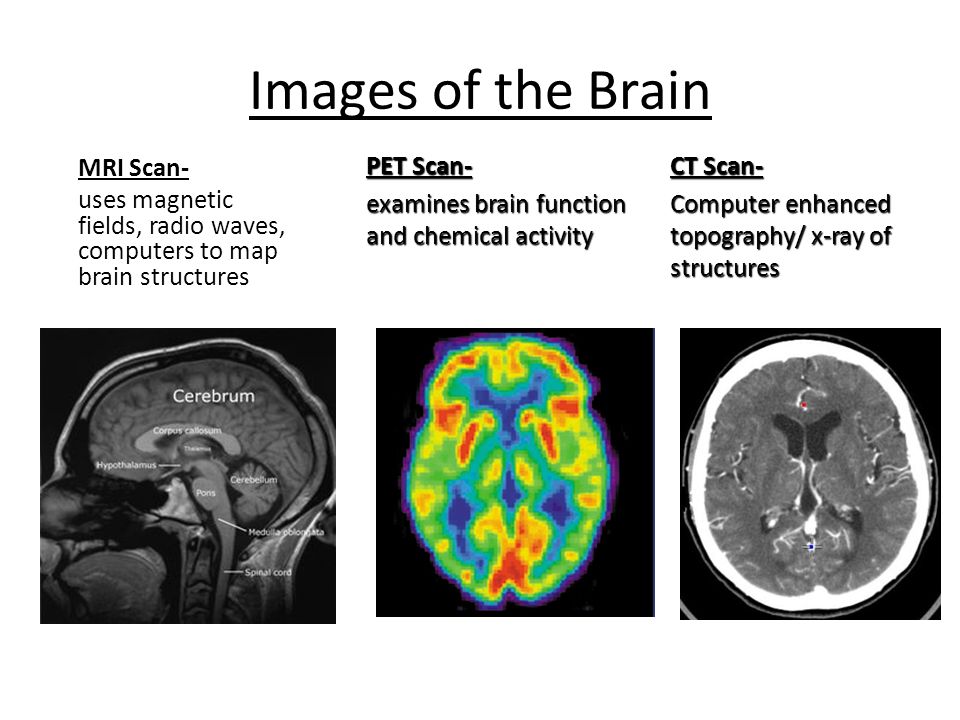
MRI is contraindicated by the presence in the human body of cardio-, neurostimulators, endoprostheses, cochlear implants (an electronic medical device that is installed for deafness), braces or other metal structures in the body. The possibility of an MRI in each case should be discussed with the radiologist. This can also be clarified in the instructions for the device or from the doctor who installed it.
Contraindications for intravenous contrast are, first of all, disorders of the kidneys, as well as allergic reactions to previous injections of contrast agents.
By themselves, the procedures described do not usually cause complications. But sometimes adverse reactions can cause injected contrast agents. The most common side effects in this case are discomfort in the injection area, an unpleasant aftertaste in the mouth, and headache. They usually go away on their own.
Rarely, nausea and allergic reactions may occur. Very rarely, serious complications develop, for example, anaphylaxis, kidney damage (more often in patients who have previously had cases of severe allergies or had impaired kidney function).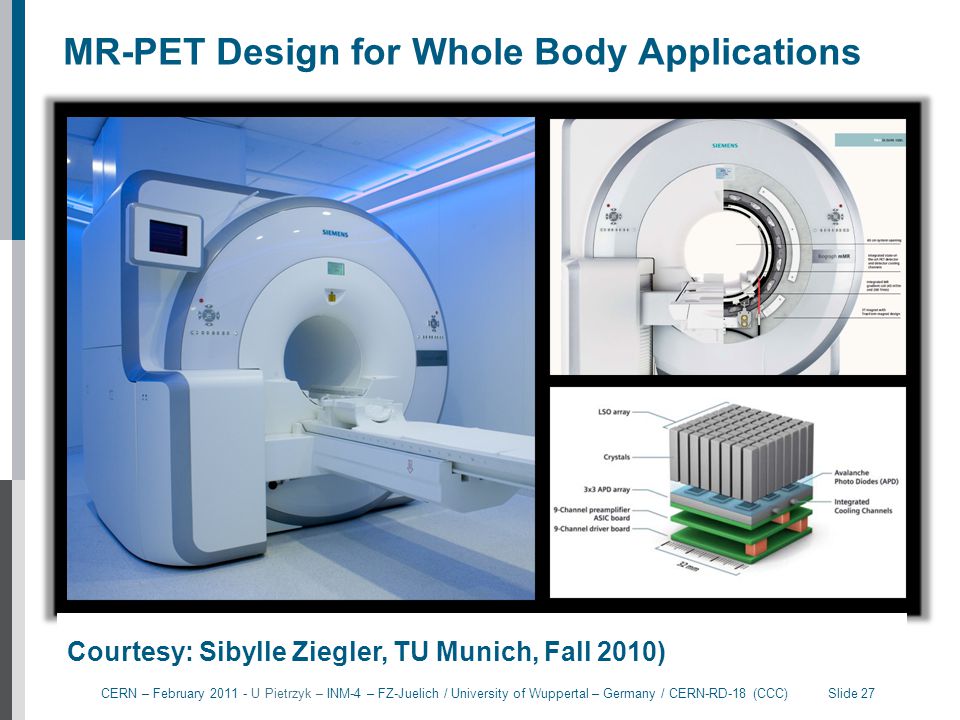
- There are many medical imaging techniques based on different physical principles.
- The choice of method depends on the specific clinical situation.
- Most imaging techniques do not require special training, have no absolute contraindications, and do not cause complications.
UK Cancer Awareness Charity Cancer Portal (in English).
Alexander Kulyabin
Resident oncologist, resident of the Higher School of Oncology
April 19, 2022
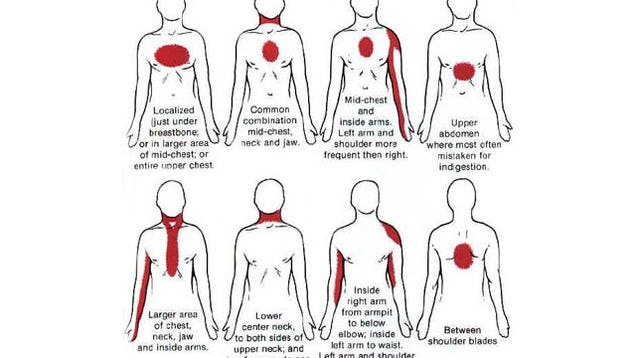
New DIANA fMRI method traces the neuronal activity of mice with an accuracy of five milliseconds
Korean engineers have developed a new method for functional magnetic resonance imaging, which allows you to directly visualize the neural activity of the brain with an accuracy of five milliseconds, while maintaining a high spatial resolution of 0.22 millimeters. A description of the new approach, which the authors called DIANA, was published in Science.
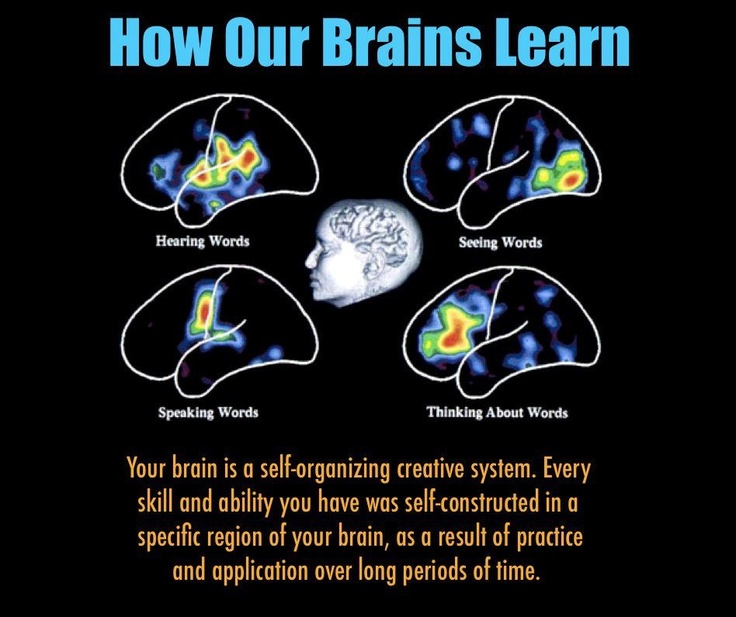
Modern science uses many methods to study the brain activity of animals and humans, but each method has its limitations.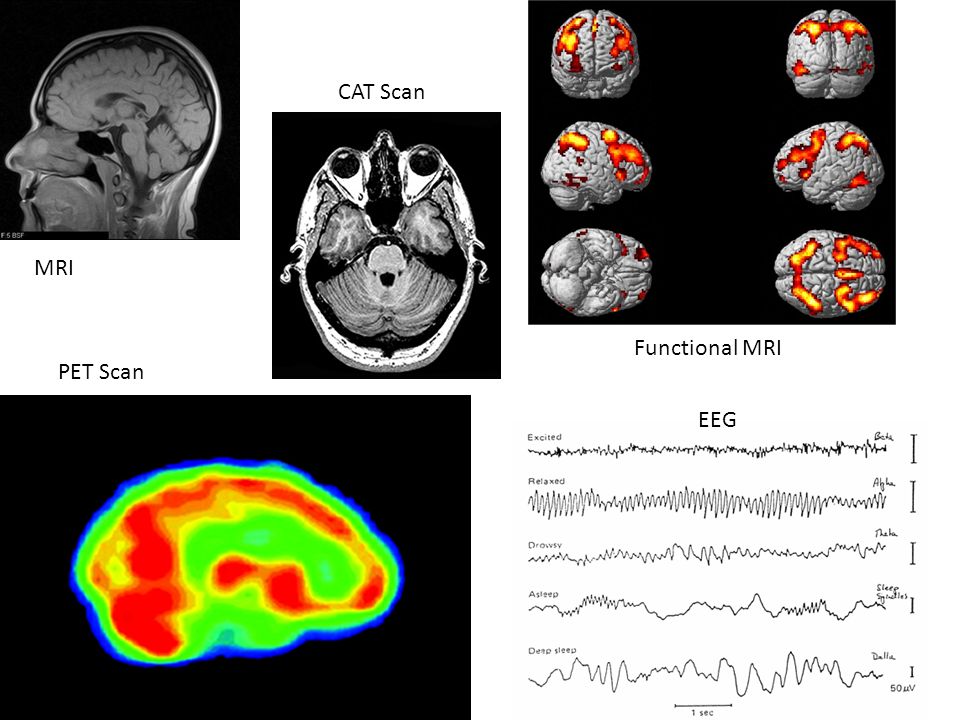 For example, electroencephalography measures electrical waves by recording voltage fluctuations that depend on the ionic current in neurons. Despite the fact that this method has good temporal resolution, the EEG recording can be highly distorted due to physical and physiological interference (surrounding tissues or movement). But functional magnetic resonance imaging (fMRI), which can be used to visualize brain activity, more accurately shows a picture of what is happening in it, but, basically, it does not work directly - using a magnetic field, fMRI captures changes in blood flow when structures are activated brain, so the response to a stimulus can be known only seconds after its appearance.
For example, electroencephalography measures electrical waves by recording voltage fluctuations that depend on the ionic current in neurons. Despite the fact that this method has good temporal resolution, the EEG recording can be highly distorted due to physical and physiological interference (surrounding tissues or movement). But functional magnetic resonance imaging (fMRI), which can be used to visualize brain activity, more accurately shows a picture of what is happening in it, but, basically, it does not work directly - using a magnetic field, fMRI captures changes in blood flow when structures are activated brain, so the response to a stimulus can be known only seconds after its appearance.
Although fMRI remains one of the most popular methods for non-invasive imaging of brain activity, the use of an indirect way of fixing parameters greatly affects the accuracy of experimental results. Therefore, scientists are constantly looking for ways to improve research methods.
A team of Korean engineers, with the participation of Phan Tan Toi from the Department of Biomedical Engineering at Sungkyunkwan University, has developed an fMRI method that can directly capture neuronal activity.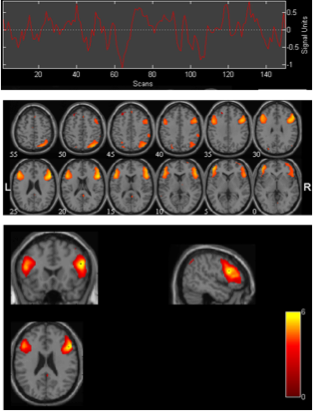 The main advantage of the new imaging method, which the authors called DIANA (direct imaging of neuronal activity), is that it allows you to maintain the spatial accuracy (resolution) of the functional MRI method and at the same time increase the temporal resolution: DIANA can dynamically visualize neuronal impulses with an accuracy of milliseconds using the 2D fast line-scan approach.
The main advantage of the new imaging method, which the authors called DIANA (direct imaging of neuronal activity), is that it allows you to maintain the spatial accuracy (resolution) of the functional MRI method and at the same time increase the temporal resolution: DIANA can dynamically visualize neuronal impulses with an accuracy of milliseconds using the 2D fast line-scan approach.
The new method was tested on mice using a 9.4 Tesla MRI scanner. The imaging focus was a one-millimeter area of the primary somatosensory cortex. During the scanning process, the researchers applied an electrical pulse every 200 milliseconds with a frequency of five hertz and a duration of 0.5 milliseconds to the whisker pads of mice that were under anesthesia.
The results showed that electrical stimulation provoked a significant increase in the signal in the contralateral primary somatosensory cortex, compared with the signal level before the stimulus (p < 0.001). The delay in the peak increase in the DIANA signal was 25 milliseconds from the moment of stimulation.