How do mood stabilizers work in the brain
Mood stabilizers - Fraser Health Authority
Mood stabilizers are a group of medications used to reduce or relieve symptoms of mood swings in bipolar disorder and other mental disorders.
What are mood stabilizers commonly prescribed for?
Mood stabilizers are used mainly to treat bipolar disorder, mood swings associated with other mental disorders, and in some cases, to enhance the effect of other medications used to treat depression.
How do mood stabilizers work?
Mood stabilizers work by decreasing abnormal activity in the brain. These medications can help reduce mood swings and prevent manic and depressive episodes.
What mood stabilizers are currently available?
Commonly prescribed mood stabilizers include:
- Lithium
- Carbamazepine
- Lamotrigine
- Oxcarbazepine
- Valproic acid
- Divalproex sodium
What can I expect from mood stabilizers?
Signs that the medication may be helping can include:
- Reduced mood swings
- Relief of symptoms
How long do mood stabilizers take to work?
There can be signs of improvement early on in treatment but it may take up to several months to experience the full effect of the medication and determine whether it is working.
Everybody is different including the way each person’s brain is wired, therefore medications may work differently in each person.
Finding the right mood stabilizer is a process of trial and error. Some people may have to try several different medications before they find one that works.
What are the common side effects of mood stabilizers?
Not everyone will experience side effects. People who experience some side effects may find that many of these side effects go away with time as their body gets used to the medication.
Some common side effects may include:
- Itchy skin, rashes
- Increased thirst
- Frequent urination (peeing too often)
- Nausea and vomiting (stomach upset)
- Slurred speech (difficulty saying words clearly)
- Blackouts (not knowing where you are for brief moments)
- Changes in vision (unable to see things clearly or the way you normally would)
- Seizures (periods of body spasms or jerking movements that cannot be controlled)
- Loss of coordination (for example, some difficulty placing fork to mouth when eating)
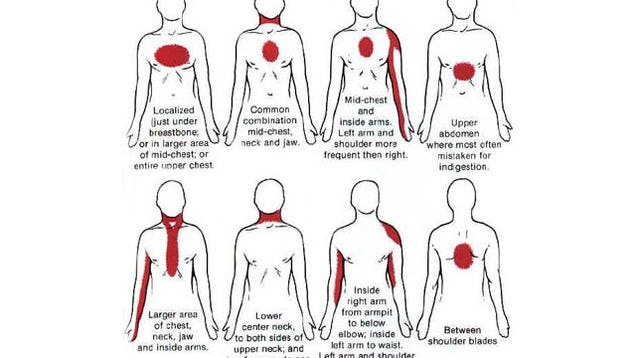
If at any time you develop a sudden rash, have any trouble with breathing, sudden pain in any part of the body (e. g. chest, muscles), sudden muscle stiffness, any involuntary movements, trouble staying awake during the day, confusion or difficulty peeing or peeing too much, contact your doctor immediately.
g. chest, muscles), sudden muscle stiffness, any involuntary movements, trouble staying awake during the day, confusion or difficulty peeing or peeing too much, contact your doctor immediately.
Some side effects may go away over time but you should always report to your doctor any symptoms that you feel are bothersome and/or have become worse.
Some suggestions to help reduce risk and/or severity of side effects can include:
- Balanced diet, adequate fluids, daily activity or exercise
- Report any weight gain greater or equal to five per cent (approximately two to 25 lbs)
- Limit excess intake of caffeinated products and sodium
- Decrease smoking
Sometimes a change in the dose and schedule may help manage some side effects. You should follow up with your doctor as there may be other treatments that could help.
Your doctor may also ask you to go for lab work or other tests to make sure you are tolerating the medication and watch for any concern of side effects.
How can I safely use my mood stabilizer?
- Do not take any other medication that is not prescribed by your doctor (e.g. over the counter products, vitamins, herbal supplements) without checking if it is safe to combine with your mood stabilizer. Check with your pharmacist before deciding to take anything new.
- All mood stabilizers should be taken regularly, preferably at around the same time every day. If you miss a dose do not double up, take your next dose at the regularly scheduled time. If you miss more than one dose please contact your doctor to discuss.
- Do not stop taking your mood stabilizers until you have spoken with your doctor to avoid any severe withdrawal effects. If there is a need to stop taking the medication the dose should be gradually reduced.
Resources
- HealthLink BC: Mood-stabilizing medicines
General information about mood-stabilizing medicines. - Centre for Addiction and Mental Health: Mood stabilizers
Learn more about mood stabilizers.
Mood Stabilizing Medications | CAMH
Overview
Mood stabilizers are medications used in the treatment of bipolar disorder, where a person’s mood changes from a depressed feeling to a high “manic” feeling or vice versa. These drugs can help reduce mood swings and prevent manic and depressive episodes.
Mood stabilizers can take up to several weeks to reach their full effect. Because of this, other psychiatric medications such as antipsychotics; are often used in the early stages of treatment to treat acute mania.
Depression in bipolar disorder can be hard to distinguish from other forms of depression. Antidepressant medications can be effective; however, they must never be used alone with bipolar disorder as they can also cause a person who is depressed to switch into mania. Antidepressants may also lead to more frequent mood episodes, known as rapid cycling. This risk is lessened if the person is also taking a mood stabilizer.
Do I need this treatment?
The term “bipolar” refers to the two extremes of mood: mania and depression. People with bipolar disorder usually experience these extremes at different times, although the two mood states can occur together (known as a mixed state). With bipolar disorder, people can also have periods where their mood is balanced. Mood stabilizers can help to keep the mood of a person with bipolar disorder within this balanced range.
People with bipolar disorder usually experience these extremes at different times, although the two mood states can occur together (known as a mixed state). With bipolar disorder, people can also have periods where their mood is balanced. Mood stabilizers can help to keep the mood of a person with bipolar disorder within this balanced range.
Treatment with mood stabilizers can reduce symptoms of bipolar disorder and increase people’s ability to pursue their interests and participate more fully in their relationships.
Medication is generally considered to be the cornerstone of treatment for bipolar disorder; however, combining medication with other types of therapy and support can help you to get and stay well. Forms of talk therapy that have been shown to help with bipolar disorder are interpersonal and social rhythm therapy, cognitive-behavioural therapy and family-focused education about bipolar disorder. Other aids can include peer support, school and job counselling, and housing and employment support. Eating a nutritious diet, exercising regularly and getting enough sleep are also important, as are minimizing your use of alcohol and caffeine and avoiding street drugs.
Eating a nutritious diet, exercising regularly and getting enough sleep are also important, as are minimizing your use of alcohol and caffeine and avoiding street drugs.
What does Mood Stabilizing Medication do?
How mood stabilizers work is not fully understood. It is thought that the drugs work in different ways to bring stability and calm to areas of the brain that have become overstimulated and overactive, or to prevent this state from developing.
Side effects of Mood Stabilizing Medication
The side-effects of mood stabilizers vary depending on the type of medication. With some medications, side-effects are kept to a minimum through regular monitoring of the level of the drug in the blood. Some people experience no side-effects. Others may find the side-effects distressing. Side-effects usually lessen as treatment continues.
Check the information given to you by your doctor or pharmacist on the specific effects of any drug you have been prescribed.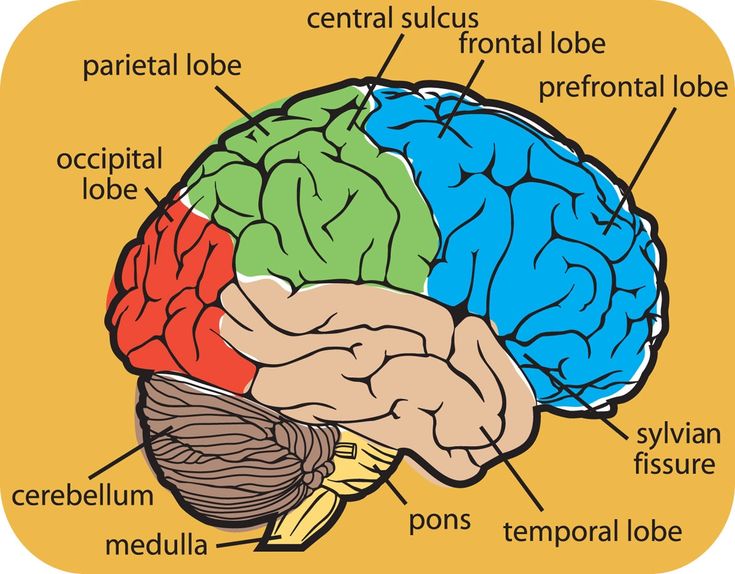 If side-effects are not mild and tolerable, let your doctor know as soon as possible. Your doctor may:
If side-effects are not mild and tolerable, let your doctor know as soon as possible. Your doctor may:
- adjust your dose
- suggest you take the medication at a different time of day
- suggest you take your medication with food
- prescribe other medications to help control side-effects
- change your medication.
More information on side-effects is included for each type of mood stabilizer.
Getting the right doseWith lithium, carbamazepine and divalproex, the dose is based on how much of the drug is in your blood and how you respond to treatment. This means that the dose differs for everyone who takes it. Blood samples are taken regularly to make sure that the dose is neither too high nor too low. Taking less may not be effective, and taking more can make you physically sick.
The right dose is within a range, rather than a precise point. It may change over time, depending on whether the medication is being used to treat active symptoms of mania or depression or to help prevent symptoms from returning.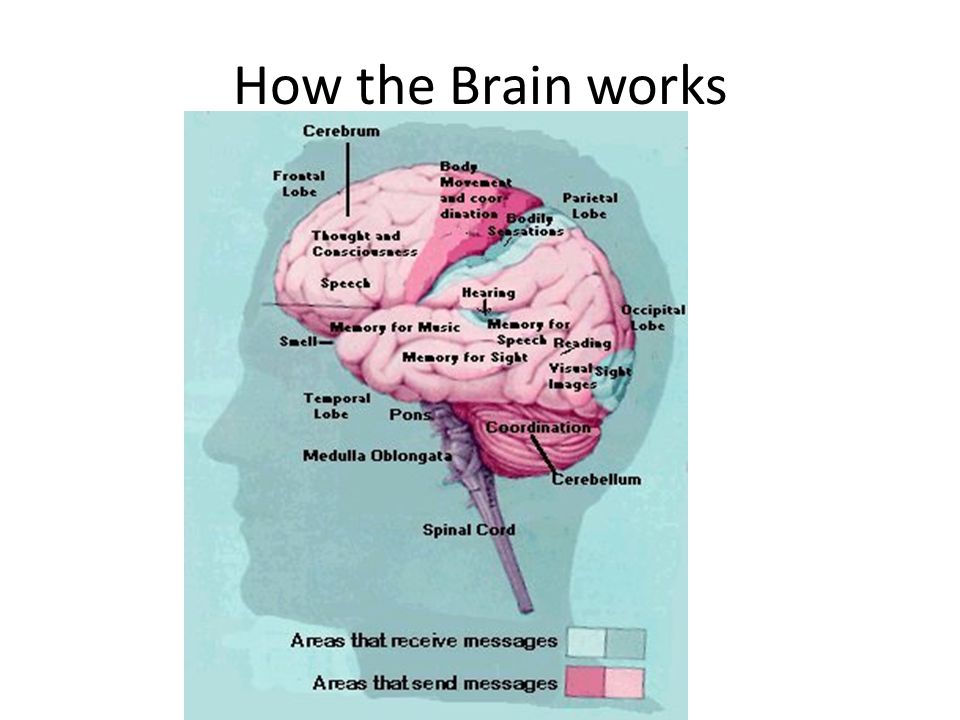 On days that you are scheduled to have your blood level tested, wait until after the test to take your morning dose to avoid inaccurate results.
On days that you are scheduled to have your blood level tested, wait until after the test to take your morning dose to avoid inaccurate results.
If you are taking carbamazepine, avoid grapefruit juice as it can raise the level of this drug in your body.
Controlling side-effects- Mood stabilizers can increase your sensitivity to the sun: wear sunscreen when outdoors to prevent burning.
- To reduce stomach upset, take your dose with food or milk.
- If your medication makes you feel drowsy, check with your doctor to see if you can take it at bedtime.
- Taking mood stabilizers can cause weight gain. Getting regular exercise and eating a low-fat, low-sugar, high-fibre diet (e.g., bran, fruits and vegetables) can help prevent weight gain.
- If side-effects are troublesome or severe, you may do better on a lower dose. Talk to your doctor.
Types of Mood Stabilizing Medication
The oldest and most studied of mood stabilizers is lithium. However, many drugs that were first developed as anticonvulsants to treat epilepsy also act as mood stabilizers. These include carbamazepine, divalproex and lamotrigine. Gabapentin and topiramate are also anticonvulsants that may act as mood stabilizers, but they are usually given in addition to other medications.
However, many drugs that were first developed as anticonvulsants to treat epilepsy also act as mood stabilizers. These include carbamazepine, divalproex and lamotrigine. Gabapentin and topiramate are also anticonvulsants that may act as mood stabilizers, but they are usually given in addition to other medications.
Lithium (Carbolith, Duralith, Lithane) is found in nature in some mineral waters and is also present in small amounts in the human body.
Lithium is used to treat mania and to prevent further episodes of mania and depression.
Common side-effects of lithium include increased thirst and urination, nausea, weight gain and a fine trembling of the hands. Less common side-effects can include tiredness, vomiting and diarrhea, blurred vision, impaired memory, difficulty concentrating, skin changes (e.g., dry skin, acne) and slight muscle weakness. These effects are generally mild and fade as treatment continues. If, however, any of these effects are severe, they should be reported to your doctor immediately. Thyroid and kidney function can be affected by lithium in some people and must be monitored regularly by your doctor.
If, however, any of these effects are severe, they should be reported to your doctor immediately. Thyroid and kidney function can be affected by lithium in some people and must be monitored regularly by your doctor.
Signs of lithium overdose: Lithium blood levels can increase to dangerous levels when a person becomes severely dehydrated. Remember to drink eight to 12 cups of fluid per day, especially when it’s hot or when you’re exercising. Severe vomiting, diarrhea or a fever can also cause dehydration. If you have these symptoms, stop taking lithium and see your doctor as soon as possible.
Changing the amount of salt you use can also affect lithium levels: avoid switching to low- or no-salt diets.
Signs that the amount of lithium in the body is higher than it should be include severe nausea, vomiting and diarrhea, shaking and twitching, loss of balance, slurred speech, double vision and weakness.
If you experience any of these effects, see your doctor as soon as possible.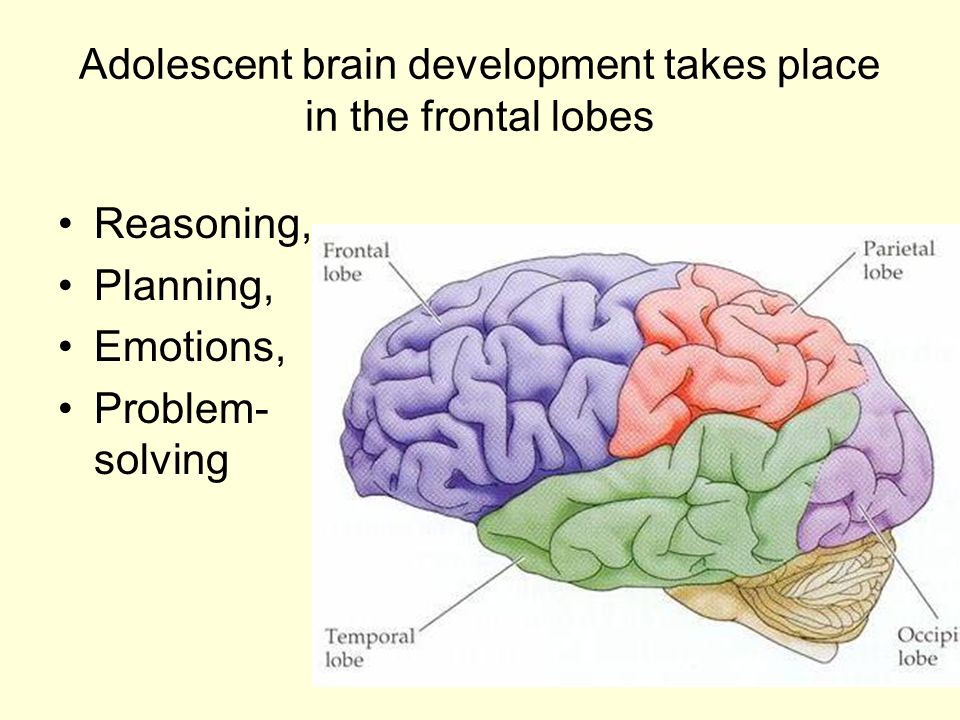 In the meantime, stop taking lithium and drink plenty of fluids. If you cannot reach your doctor and the symptoms do not clear up, go to the nearest hospital emergency department.
In the meantime, stop taking lithium and drink plenty of fluids. If you cannot reach your doctor and the symptoms do not clear up, go to the nearest hospital emergency department.
The differing names for this anticonvulsant medication reflect the various ways it is formulated. Divalproex (and its various forms) is used for acute manic episodes. Brand names include Depakene and Epival.
Common side-effects of divalproex include drowsiness, dizziness, nausea and blurred vision. Less common side-effects are vomiting or mild cramps, muscle tremor, mild hair loss, weight gain, bruising or bleeding, liver problems and, for women, changes in the menstrual cycle.
CarbamazepineCarbamazepine (Tegretol) is another anticonvulsant. It is used for mania and mixed states that do not respond to lithium or when the person is irritable or aggressive.
Common side-effects of carbamazepine include dizziness, drowsiness, blurred vision, confusion, muscle tremor, nausea, vomiting or mild cramps, increased sensitivity to sun, skin sensitivity and rashes, and poor co-ordination.
A rare but dangerous side-effect of carbamazepine is reduced blood cell counts. People who take this drug should have their blood monitored regularly for this effect. Soreness of the mouth, gums or throat, mouth ulcers or sores, and fever or flu-like symptoms can be a sign of this effect and should be reported immediately to your doctor. If carbamazepine is the cause of these symptoms, they will go away when the medication is stopped.
Oxcarbazepine (Trileptal), a closely related drug, may have less side-effects and drug interactions than carbamazepine, but is not as well studied for bipolar disorder.
LamotrigineLamotrigine (Lamictal) may be the most effective mood stabilizer for depression in bipolar disorder, but is not as helpful for mania.
The starting dose of lamotrigine should be very low and increased very slowly over four weeks or more. This approach decreases the risk of a severe rash—a potentially dangerous side-effect of this drug.
Common side-effects of lamotrigine include fever, dizziness, drowsiness, blurred vision, nausea, vomiting or mild cramps, headache and skin rash. Although it is rare, a severe skin rash can occur with lamotrigine. Any rashes that begin in the first few weeks of treatment should be reported to your doctor.
* Medications are referred to in two ways: by their generic name and by their brand or trade names. Brand names available in Canada appear here in brackets.
Frequently Asked Questions
How long should I take mood stabilizers? When you start taking mood stabilizers, it may be two weeks or more before you notice their effect and four to six weeks before they reach their full effect. It’s important to give them time to work. Once your symptoms are under control, you will be encouraged to continue to take mood stabilizers for at least six months and probably longer. How much longer varies from person to person.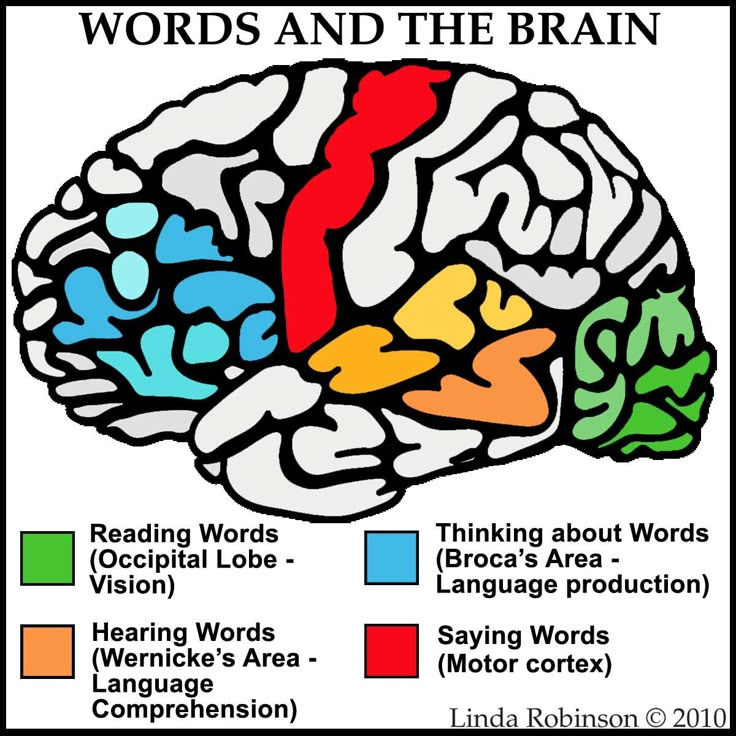
Mood stabilizers can help prevent further episodes of mania or depression. In other words, staying on these medications for the long term can help to keep you well. Going off mood stabilizers, on the other hand, can greatly increase your chances of having another episode.
Once you have been taking mood stabilizers for a while and you are feeling well, you may do fine on a lower “maintenance” dose. Talk to your doctor if you would like to try this.
Are mood stabilizers addictive?Drugs that are addictive produce a feeling of euphoria, a strong desire to continue using the drug, and a need to increase the amount used to achieve the same effect. Mood stabilizers do not have these effects.
While mood stabilizers are not addictive, when you take them (or any drug) over months or years, your body adjusts to the presence of the drug. If you then stop using the drug, especially if you stop suddenly, the absence of the drug may result in withdrawal effects or in return of symptoms.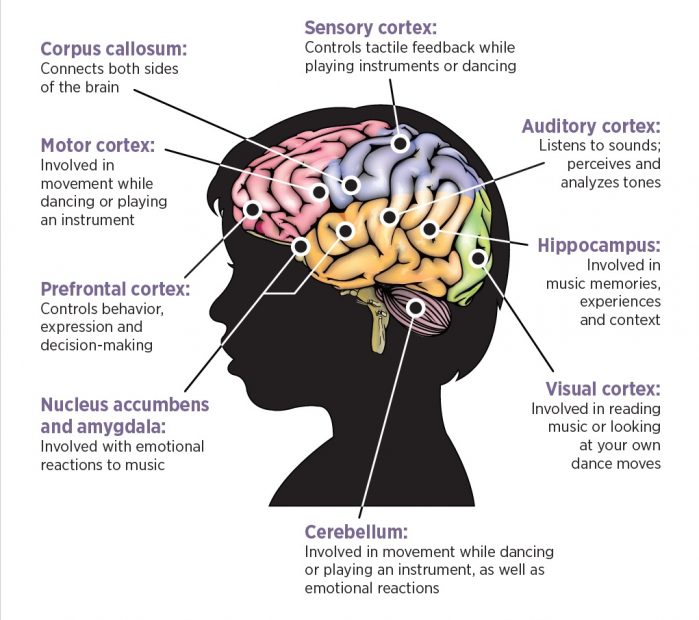 With mood stabilizers, the withdrawal effects are generally mild; the greatest risk with stopping these drugs is the return of symptoms.
With mood stabilizers, the withdrawal effects are generally mild; the greatest risk with stopping these drugs is the return of symptoms.
Whether you want to cut down your dose or stop taking a medication, the same rule applies: go slowly. Sudden changes in your dose can greatly increase your risk of having another mood episode.
The first step is to ask yourself if this is the right time. Are you feeling well? Is the level of stress in your life manageable? Do you feel supported by your family and friends?
If you think you’re ready, talk to your doctor. If your doctor doesn’t agree, find out why. If you are not satisfied with his or her reasons, you may want to see another doctor for a second opinion.
If your doctor does agree, he or she will advise you not to skip doses but to reduce your dose gradually over a four to six week period. This process of cutting back will take several months.
If you want to stop taking more than one medication, your doctor will usually suggest that you lower the dose of one drug at a time.
As you cut down, if you start to feel unwell, let your doctor know. You may want to go back up with your dose. Find the dose that works best for you.
Will mood stabilizers interact with other medications?Some medications can affect the blood levels of mood stabilizers, meaning your dose of mood stabilizer may have to be adjusted while you are taking the other medication. Mood stabilizers, especially carbamazepine, may also reduce the effectiveness of some other drugs. Always make sure your doctor or dentist knows about any drugs you are taking when he or she prescribes another medication. It’s also important to check with your pharmacist before using any over-the-counter medication, including pain medications, herbal remedies, cold or allergy tablets, or cough syrups.
What if I drink coffee or alcohol while taking mood stabilizers? Drinking coffee or other beverages that contain caffeine can lower lithium levels and increase tremor. If you want to dramatically change how much caffeine you have in a day (e.g., cutting back from four cups to one cup of coffee a day), check with your doctor or pharmacist first to see if your mood stabilizer dose should be adjusted.
If you want to dramatically change how much caffeine you have in a day (e.g., cutting back from four cups to one cup of coffee a day), check with your doctor or pharmacist first to see if your mood stabilizer dose should be adjusted.
People with bipolar disorder are generally advised to avoid alcohol. This is recommended because:
- Drinking alcohol can worsen depressive episodes and further impair judgment in mania.
- Many people with bipolar disorder develop addiction problems with alcohol and other drugs, especially when they use these substances to “take the edge off” their symptoms or to offset the effects of medication.
- Combining mood stabilizers with alcohol tends to enhance the negative effects of both drugs, such as drowsiness, nausea and poor co-ordination.
While avoiding alcohol is the best choice for many people with bipolar disorder, having a drink or two on occasion should be okay for those who are stable, feeling well and who have not had a substance use problem.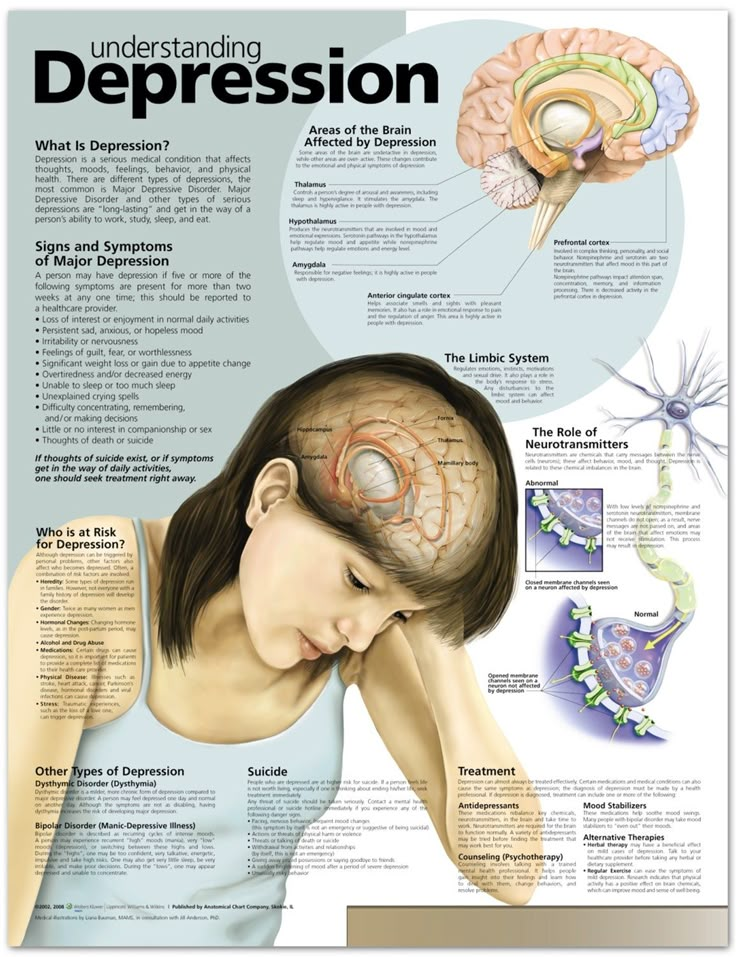
Street drugs can complicate your situation and create problems. Cocaine and amphetamines, for example, can trigger an episode of mania or depression. Marijuana could lift you up or it could bring you down; its effects on mood can be unpredictable, especially when combined with bipolar disorder. Using any street drugs (or alcohol) regularly to modify your mood increases your risk of addiction.
Will mood stabilizers affect my ability to drive safely?Mood stabilizers, especially early in treatment, may delay your reaction time. This effect could impair your ability to drive a car or operate other machinery. Avoid these activities until you adjust to the medication or if you feel slowed down.
Will mood stabilizers affect my sex drive and function? Taking lithium may reduce your interest in sex. This can be a good thing for some people and not so good for others.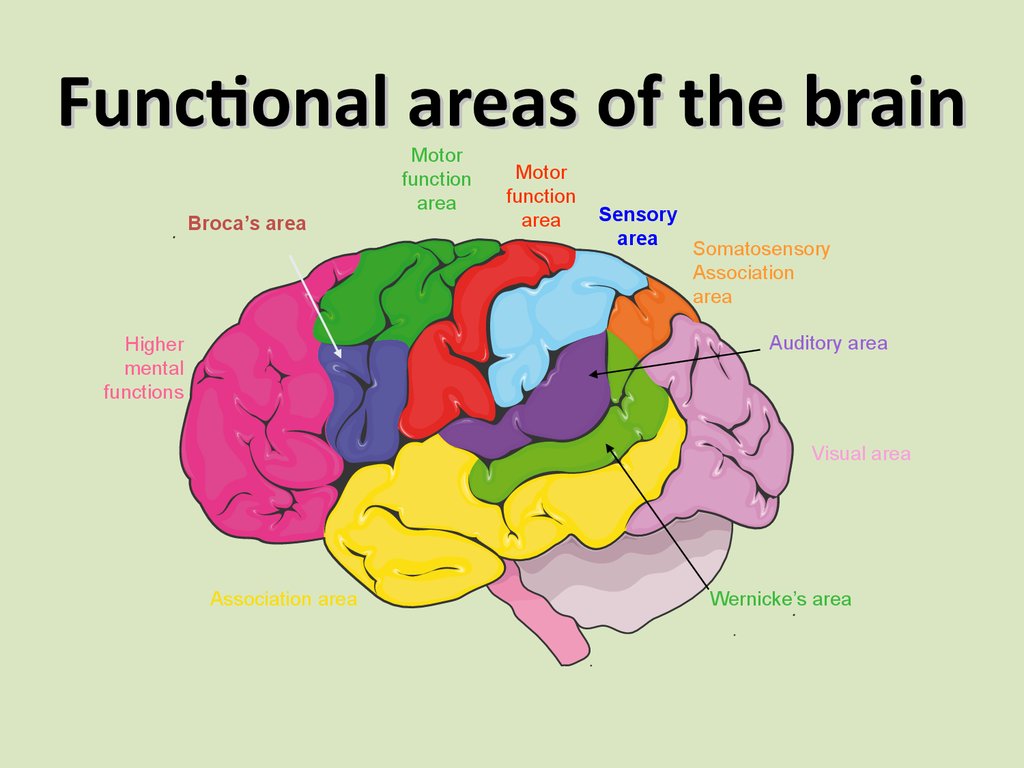 If you feel your interest in sex is too low, talk to your doctor about it. Sometimes an adjustment in dose can help.
If you feel your interest in sex is too low, talk to your doctor about it. Sometimes an adjustment in dose can help.
Although not common, some men who take lithium report a decreased ability to maintain an erection or to ejaculate. With bipolar disorder, many complex factors other than medication may contribute to sexual difficulties.
In women, mood stabilizers may cause changes in the menstrual cycle. Carbamazepine and other anticonvulsants may reduce the effectiveness of birth control pills.
Is it safe to take mood stabilizers while pregnant or breastfeeding? Each woman’s situation is unique and should be discussed with her doctor. For any pregnant woman with a history of bipolar disorder, the question of taking mood stabilizers during pregnancy usually comes down to a risk-benefit analysis. All mood stabilizers carry some risk—some more than others; however, episodes of depression or mania can affect prenatal care and a mother’s ability to parent her newborn child. When treatment with a mood stabilizer helps to avoid a relapse or to reduce distress, the benefits may outweigh the risks.
When treatment with a mood stabilizer helps to avoid a relapse or to reduce distress, the benefits may outweigh the risks.
Taking lithium during the first trimester in pregnancy is believed to slightly increase the risk of a heart defect in the baby. This risk has been shown to be .05-.1 per cent (i.e., one in 2,000). Newborns must be monitored for possible toxic effects of lithium; these effects usually resolve within one to two weeks.
Divalproex increases the risk of spinal defects in the developing baby by approximately five to nine per cent. Divalproex is also related to developmental delays and cognitive problems in children. Carbamazepine increases the risk of spinal defects by approximately one per cent. Lamotrigine is associated with a potential increased risk for cleft palate.
Lithium can be passed to the baby through breast milk; however, the amount varies greatly from woman to woman. Some women may be able to breastfeed with close monitoring of lithium levels in the mother’s milk and the baby’s blood.
The amount of anticonvulsant mood stabilizers passed through breast milk is very small and is not considered to be a risk to the baby, especially when weighed against the benefits of breastfeeding.
If you decide to stop taking medications during pregnancy or while breastfeeding, it is a good idea to see your doctor more often to help you monitor for a return of symptoms.
Can children and teens use mood stabilizers?The first signs of bipolar disorder can appear in childhood, usually as depression or behaviour problems. Early substance use problems or petty crime can also be signs. When bipolar disorder in childhood is misdiagnosed as attention-deficit/hyperactivity disorder or unipolar depression, treatment with stimulants or antidepressants can worsen symptoms.
Mood stabilizers were developed and tested on adults. While most of these drugs are not officially approved for use by children and teens, professional guidelines direct their use in this age group.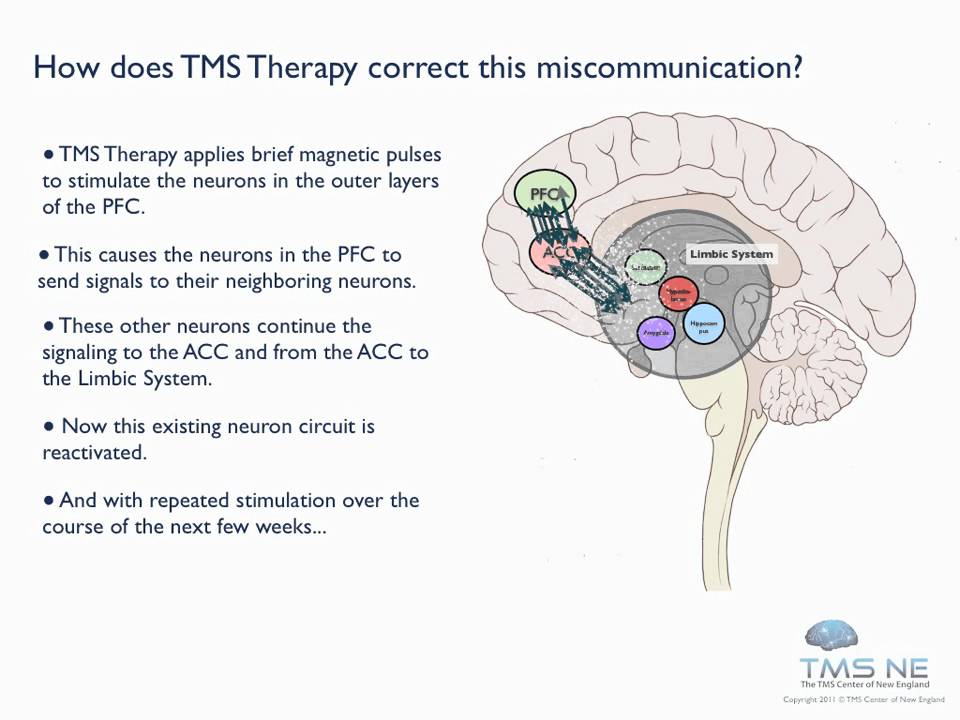 Lithium is approved for treating manic symptoms in children aged 12 and older.
Lithium is approved for treating manic symptoms in children aged 12 and older.
Children and teens may be more prone to the side-effects of these drugs and should be monitored by their doctor regularly for side-effects.
Can older adults use mood stabilizers?As people age into their 60s and older, their bodies become less able to eliminate medications. This means that older people who take mood stabilizers need to have the drug levels in their blood measured more often than younger people. Those taking lithium also need to have their kidney and thyroid function and heart rate monitored more frequently.
As people get older, they also become more sensitive to medications and may require a lower dose. Mood stabilizers can increase the risk of falls, especially when taken with other drugs.
Copyright © 2009, 2012 Centre for Addiction and Mental Health
Related Programs & Services
- Treatment at CAMH: Access CAMH
- Help for families from CAMH
- ConnexOntario
- For information on using medications while pregnant or breastfeeding, contact MotherRisk at 416 813-6780 or visit www.
 motherisk.org.
motherisk.org.
Additional Resources
- When a parent has bipolar disorder - What kids want to know
- Bipolar Disorder: An Information Guide (PDF)
- A free tutorial on bipolar disorder is available on the Mental Health 101 page.
Unnecessary happiness
Bipolar affective disorder. Accompanied deviations in the biochemical processes of the brain. Word "bipolar" means two extremes - mania and depression replace each other while the person is just trying to live.
“Fifteen years ago I wrote a book about my struggle with mania and depression, about a suicide attempt that almost became for me fatal, about a stubborn unwillingness to take the medicines that I were needed. It was a heavy book, plunging into a heavy the reality of bipolar disorder. But it was also a story. about the saving power of love, friendship, family, about the gift of a doctor, able to heal, ”so begins the afterword of the clinical psychologist Kay Jamison to his book on bipolar disorder.
This afterword to A Restless Mind reflects both pain and the hope of people suffering from bipolar affective disorder. AT The world of such people is approximately from 1% to 4%. Of course, count impossible, but even 4% is 320 million people. This is despite that BAD is difficult to diagnose and not everyone goes to the doctor. On the in fact, this number could be much higher.
The words "depression" and "bipolar disorder" only in March 2021 years searched in Yandex about a million times. For the same period in 2020 - 700,000 times, and in 2019year - 500,000. And although the tendency to take care of oneself and one's health, including psychological, recently gaining momentum - mental diseases are still shrouded in a fog of obscurity for many, myths, rumors and stereotypes.
Terminology.
BAD - bipolar affective disorder, pathology, accompanied by deviations in the biochemical processes of the brain brain. This disease is chronic, and life expectancy in people with bipolar disorder by an average of 9years less.
This disease is chronic, and life expectancy in people with bipolar disorder by an average of 9years less.
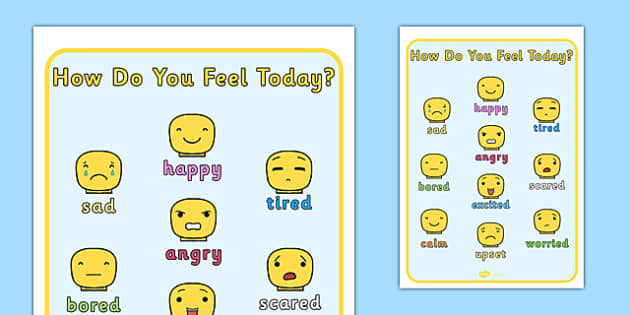
The word "bipolar" means two extremes. Disorder manifests itself in sudden changes in emotions, mood and level energy. These changes do not happen all at once, they usually last for several days or weeks.
In general characteristics, suppressed depressive state - depressive episode . He identical to the condition in the associated disorder - unipolar depression. People feel despair, despondency, lack of energy and mental concentration. This condition may appear physically - in lack or excess of sleep or food.
They also distinguish an elevated state, which replaces depressive - manic episode . In that difference between bipolar disorder and unipolar depression. AT in this state, a person feels full of energy, happiness and optimism. Euphoria and high self-esteem are also companions of this stages.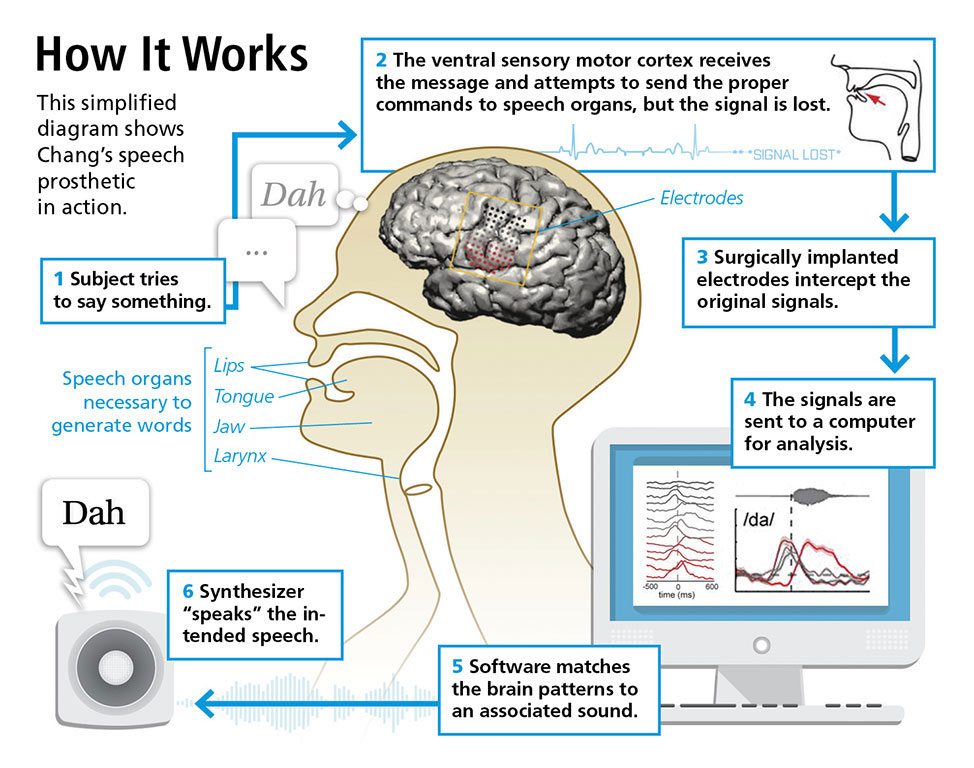
In depression, suicidal thoughts come to a person, he is gnawing feeling of guilt, self-flagellation begins, certain addictions – food cravings, for example. And in mania people don't just feel good, they feel good literally invincible, in every way. Can invest everything savings in a risky business, carelessly engage in dangerous sports. At this stage, the person may become delirious or manifestations of megalomania - to feel like a messenger of God or with supernatural powers.
Classification
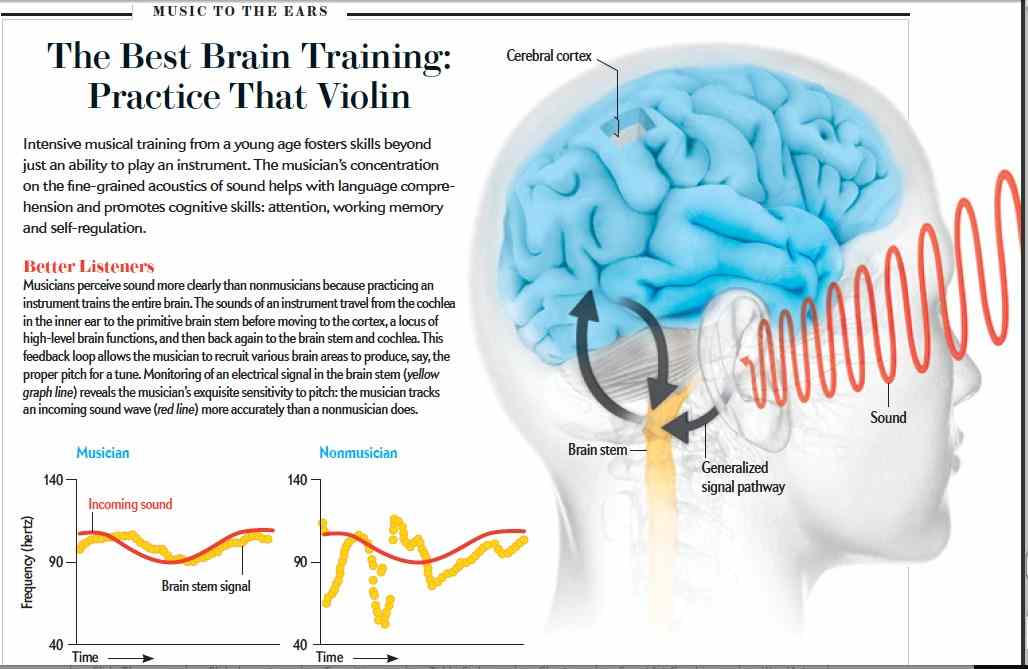
Yes, we all go through certain stages in the "middle" intensity, even when healthy people. In case of bipolar disorder to describe these episodes fit the word "too". Classification disorder depends on the nature of its manifestation. (Fig. 1)
Fig. 1. Classification of disorders and the nature of their manifestations in comparison
A person suffering from unipolar depression may have "average" ups but downs can be crushing and last long enough for a long time. People with bipolar disorder-1 experience severe downturns that last at least two weeks, and then - a steep climb that lasts at least a week. If such manic episodes are not treated, they can last from 3 to 6 months. Bipolar disorder-2 is different from type 1 that a person does not reach such a high level instability in the stage of mania. This is called hypomania. And it can last at least four days, but, as a rule, such episodes last weeks or months. With cyclothymia, ups and downs less peak, but they continue alternately for at least for two years.
People with bipolar disorder-1 experience severe downturns that last at least two weeks, and then - a steep climb that lasts at least a week. If such manic episodes are not treated, they can last from 3 to 6 months. Bipolar disorder-2 is different from type 1 that a person does not reach such a high level instability in the stage of mania. This is called hypomania. And it can last at least four days, but, as a rule, such episodes last weeks or months. With cyclothymia, ups and downs less peak, but they continue alternately for at least for two years.
There are also other options. For example, sometimes a person may experience symptoms characteristic of both stages at the same time. Or these phases can change very often - 4 or more episodes depression or mania during the year.
Causes
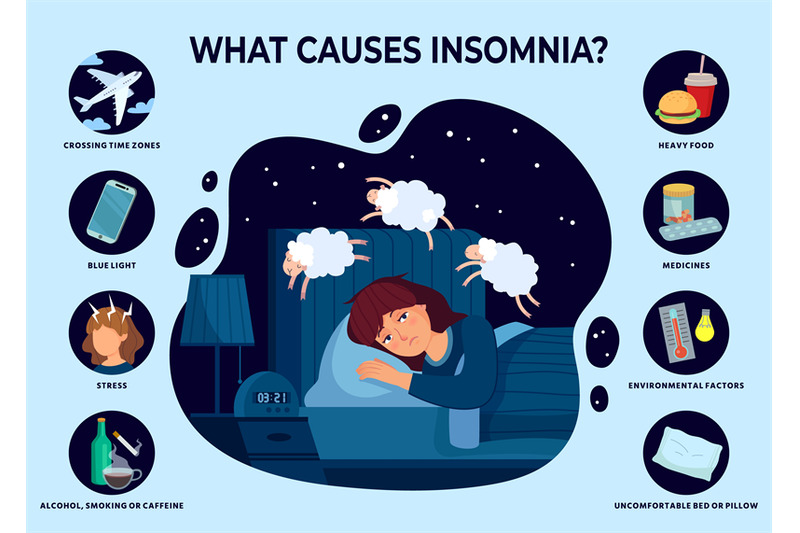
The cause of bipolar disorder is not yet known, as is the case with many other mental illnesses. However, scientific research has achieved some results.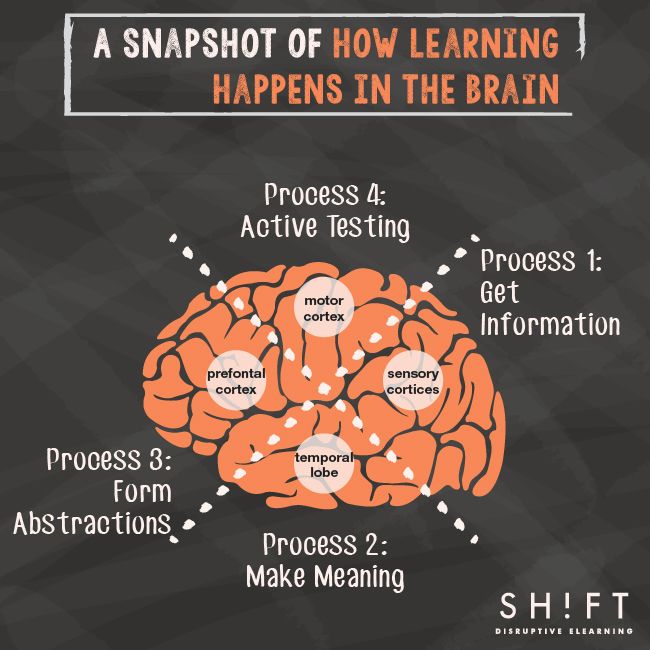 Was found, that the dynamic interplay between genetic, neurochemical and environmental factors play a role in the onset and progression of BAD. (Fig. 2)
Was found, that the dynamic interplay between genetic, neurochemical and environmental factors play a role in the onset and progression of BAD. (Fig. 2)
Fig. 2. Causes of Bipolar Disorder
It is assumed that the level of heredity is approximately 70-80%. Scientists explain such high numbers by two factors: genetic transmission and "inherited" family environment, which potentially impaired if parents have psychopathology. "Bipolar gene" was not found, but found that some interaction between certain genes affects the likelihood of developing disorders.
A genome-wide association study conducted in 2019, found 30 locations on the chromosome - loci that contain genes encoding ion channels, transporters neurotransmitters and synaptic components. Their analysis revealed nine highly enriched sets of genes that affect BAR development. According to the results of the study, scientists found that bipolar disorder-1 is highly genetically correlated with schizophrenia due to psychosis, while bipolar disorder-2 is more strongly correlated with major depressive disorder disorder.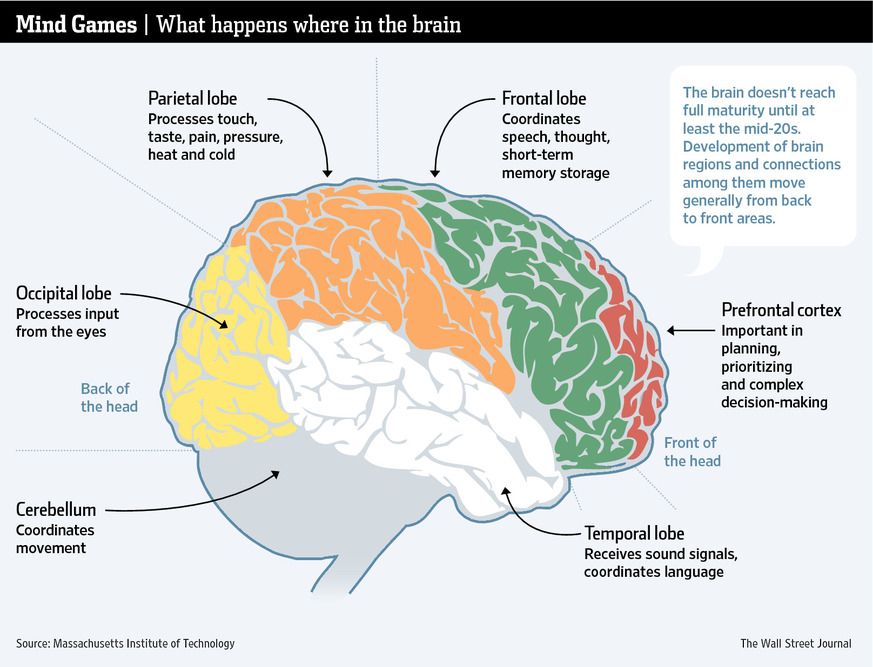
Another study of the DNA genome in the post-mortem hippocampus in humans revealed a decrease in the number of copies of mitochondrial DNA (mtDNA), which are located in the mitochondria. Mitochondria are like "energy" stations for all body cells - including and brain. Scientists believe that the preservation of mitochondria and their proper work affects life expectancy. Many research over the past 50 years has proven mitochondrial dysfunction in people with bipolar disorder and this is considered a pathological factor.
In the same study, researchers found a strong correlation between the number of mtDNA copies and the length of telomeres, which are the "tips" chromosomes, and their length is closely related to the duration life. They also found a significant correlation between acceleration epigenetic aging and telomere length. So the scientists proved accelerated biological aging of the hippocampus in people with bipolar disorder. By According to the same scientists, it may underlie neurocognitive dysfunctions in people with bipolar disorder.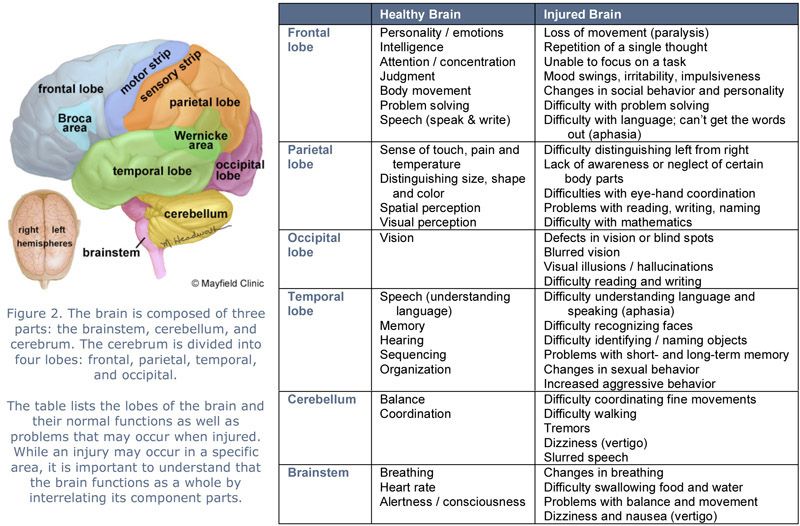
Scientists have repeatedly proven that a person in one way or another At the stage of disorder, the brain works differently.
In a healthy brain, strong relationship, there is a constant process of renewal. Unnecessary connections that a person does not use are erased, and new ones - grow up. In patients with bipolar disorder, the ability updated is broken, there are too many connections and the brain is already unable to navigate them. And since he cannot to navigate, people have abnormal thoughts or behavior.
Neurotrophin BDNF, which is involved in all processes preservation of neuronal cells and the creation of synapses, is considered the most studied in bipolar disorder. Such an interest in him and also in several neutrophins due to the discovery that antidepressants and mood stabilizers can act on these molecules, modulating their signaling pathways.
The amount of BDNF neutrophin in patients with bipolar disorder is underestimated in brain and blood, and preclinical studies have shown that chronic use of certain antidepressants and mood stabilizers such as lithium and valproic acid can increase its level in the brain of rats.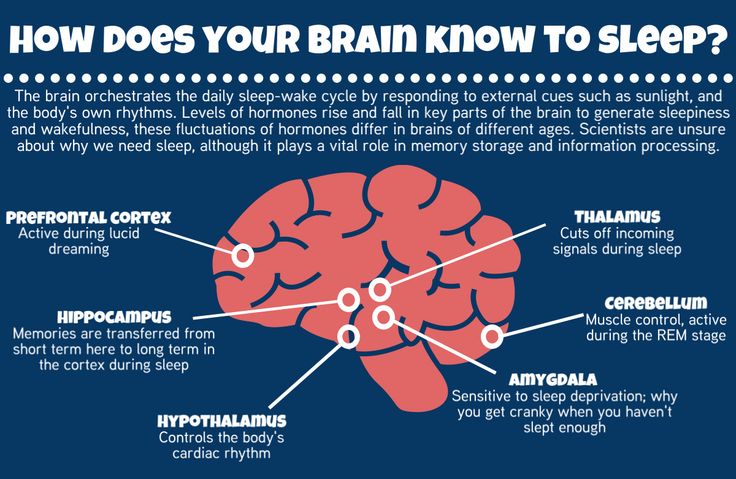 There are studies which confirm the underestimation of the level of nerve growth factor NGF in plasma in patients with bipolar disorder. Lithium also increases NGF and GDNF - glial neurotrophic factor in hippocampus, frontal cortex, occipital region and striatum. The neutrophins NGF and GDNF promote survival, regeneration of neurons and the emergence of new neural connections.
There are studies which confirm the underestimation of the level of nerve growth factor NGF in plasma in patients with bipolar disorder. Lithium also increases NGF and GDNF - glial neurotrophic factor in hippocampus, frontal cortex, occipital region and striatum. The neutrophins NGF and GDNF promote survival, regeneration of neurons and the emergence of new neural connections.
Fig. 3. Brain reactions during risky decision making in patients with mania, patients with depression and healthy people.
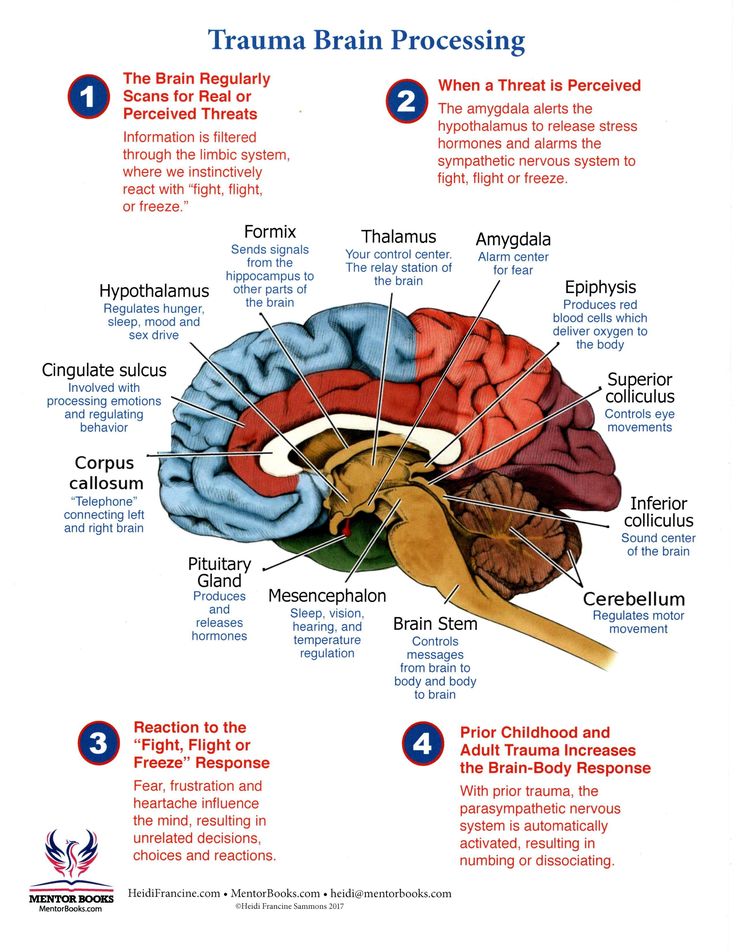
In 2001, scientists conducted an experiment where they asked people to decide neuropsychological task (Fig. 3). The people were divided into three groups - patients with mania, patients with depression and healthy people. We watched the reaction of the brain when making risky decisions. The subjects were told that there was a token that was hidden under one of six boxes, which are presented in different colors. The subjects had to guess whether the token was hidden under the red or blue box to win points.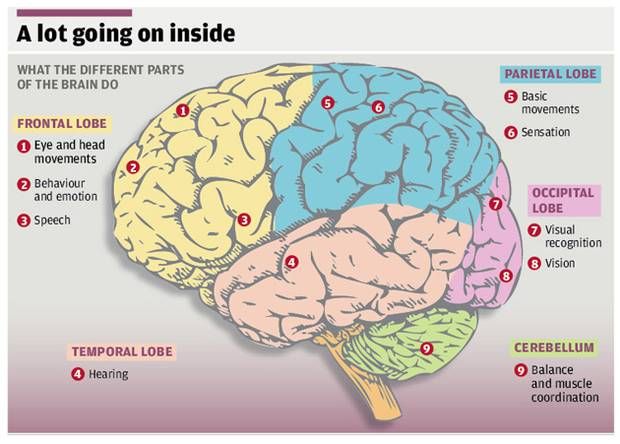 Less likely option blue in this example is also associated with a higher value gain to create conflict between reward and uncertainty.
Less likely option blue in this example is also associated with a higher value gain to create conflict between reward and uncertainty.
Patients with mania had increased activity in the area of the brain which is responsible for emotionality, and in the area that participates in strategic processes and management functions – on the contrary, it is underestimated. Patients with depression did not have significant differences in the activation of brain regions.
It is also known that psychosocial stress can also provoke the development of bipolar disorder.
With the clinical course of BAD, scientists have identified abnormalities in the axis hypothalamic-pituitary-adrenal (HPA), which is major mediator of the biological response to stress. This system releases hormones such as glucocorticoids and epinephrine. Glucocarticoids are steroid hormones that are released adrenal glands in response to any stress. Their production is strictly controlled and they affect all three neurotransmitter systems brain - serotonin, norepinephrine and dopamine, which are considered "depressive triad". The production of these hormones affects the synthesis neurotransmitters, their breakdown, the number of receptors (which convert neurotransmitters into a nerve impulse) and their correct work.
The production of these hormones affects the synthesis neurotransmitters, their breakdown, the number of receptors (which convert neurotransmitters into a nerve impulse) and their correct work.
In response to stress, the brain sends a command: to work out some kind of glucocorticoid that prepares the body for counter this stress by stimulating the production of neurotransmitters. To do this, in response to stress, the hypothalamus uses corticotropin-releasing hormone. That one is sent to the pituitary gland, where it causes it to produce adrenocorticotropic a hormone that is already sent to the adrenal glands for increased production of glucocorticoids. And glucocorticoids are already in in turn stimulate the production of the desired neurotransmitter. On the this stage, as soon as the body feels that the glucocorticoid got into the blood, the hypothalamus and pituitary stop working, the body comes to a state of rest and the production of a neurotransmitter stops.
Anomalies occur when the negative feedback of the glucocorticoid cortisol to the hypothalamus and pituitary gland, which leads to permanent activation of the HPA axis and excessive release of cortisol. Violation of the negative feedback means that cortisol is not produced stops, its receptors become resistant to constant signals, which leads to an increase in the activity of pro-inflammatory immune mediators and downregulation of neurotrophic factors such as BDNF. The brain simply does not receive information about the fact that cortisol has developed and does not stop sending “impulses stress."
This process is also considered one of the theories of the origin clinical depression. Failures in this system lead to deterioration in sleep patterns, impaired fat burning, disruption in emotions and mood, decreased production of sex hormones, imbalance neurotransmitters, increased inflammation, and many other consequences. (fig.4)
Fig. 4. Visual reflection of the totality of recent studies of the neurobiological mechanisms of bipolar disorder. Biochemical pathways causing cell damage.
4. Visual reflection of the totality of recent studies of the neurobiological mechanisms of bipolar disorder. Biochemical pathways causing cell damage.
Resume
There is a lot of research in the field of neurobiological mechanisms of bipolar disorder, but it is still not clear what is the root cause and what is consequence. Several biochemical processes, not all of which shown in the figure above, interact at the same time, causing cell damage. A vicious circle in which numerous systems and mechanisms exacerbate and accelerate cell damage, synoptic dysfunction and impaired neurogenesis. It leads to progressive structural changes in the brain and cognitive decline, which scientists believe contributes to neuroprogression of bipolar disorder.
Bipolar affective disorder is not just the inability to take self-control or excessive emotionality. Like depression is mental illness that affects the work of everything organism.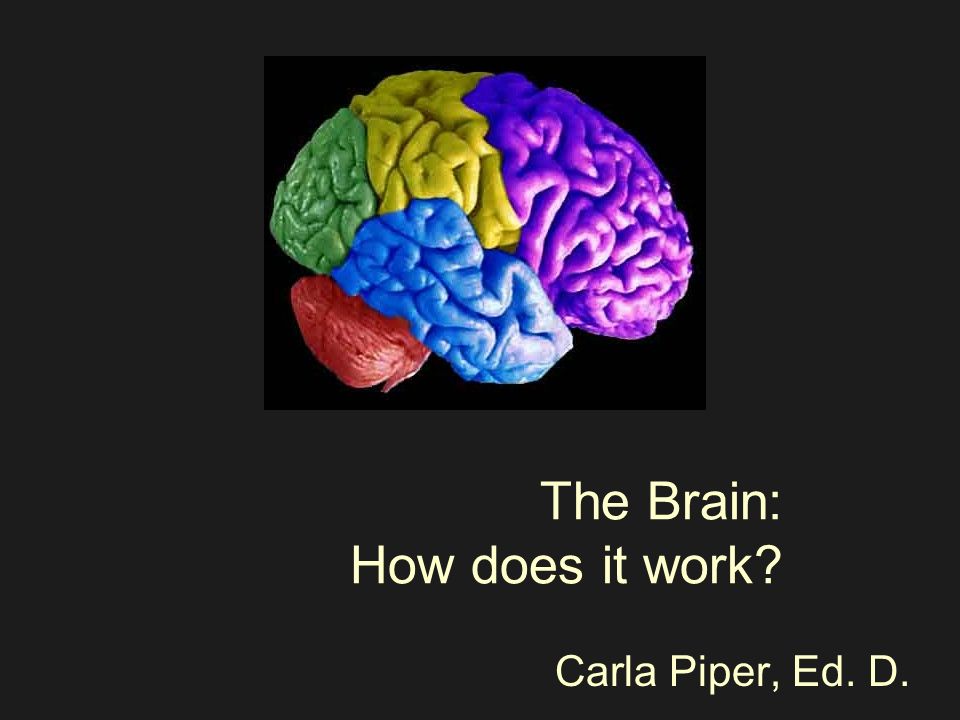
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6282906/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7524405/#B18
- https://pubmed.ncbi.nlm.nih.gov/31746071/
- https://pubmed.ncbi.nlm.nih.gov/31043756/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181872/
- https://pubmed.ncbi.nlm.nih.gov/11701607/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6489983/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4552246/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1525098/
- https://ironman.ru/news.php?id=5692
- https://www.youtube.com/watch?v=ShsJ6Jr53JI
- https://www.youtube.com/watch?v=RrWBhVlD1H8
Illustrations:
- https://www.healthshots.com/mind/mental-health/what-is-bipolar-disorder/
- https://www.
 ncbi.nlm.nih.gov/pmc/articles/PMC7524405/figure/f01/
ncbi.nlm.nih.gov/pmc/articles/PMC7524405/figure/f01/ - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7524405/figure/f02/
- https://www.youtube.com/watch?v=KSvk8LLBo2g
Inside Bipolar Disorder: What's Wrong with Your Brain and How to Fix It
We've translated for you a chapter from Living a Productive Life with Depression and Bipolar Disorder by John McManamy. The author himself is ill with bipolar disorder, and at the same time he is sure that a successful and meaningful life with this diagnosis is possible. He devoted years to studying the disease and how to deal with it.
In this chapter, the author has collected up-to-date scientific data on how nerve cells function, what is wrong with them in a person with bipolar disorder, and how this can be corrected with medication. Here are scientific answers to the questions: why do antidepressants begin to work after a few weeks, do nerve cells recover, and how exactly do serotonin reuptake inhibitors work?
The material is quite complex - for those who really want to understand how everything works.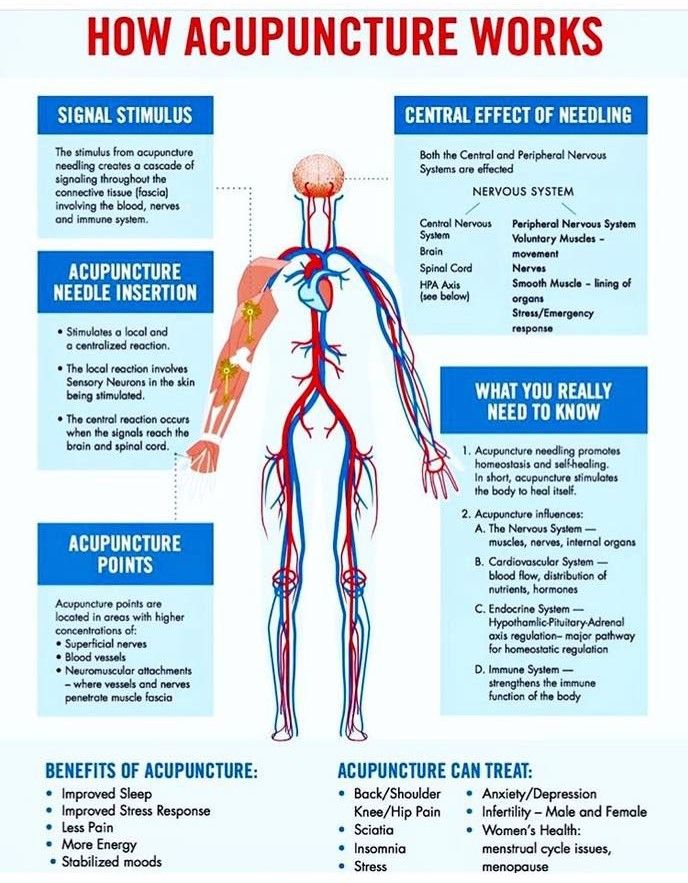 Download chapter in pdf.
Download chapter in pdf.
Translation of a chapter from the book "Productive Life with Depression and Bipolar Disorder" by John McManami, 2006. (John McManamy, Living Well with Depression and Bipolar Disorder)
Neurotransmitters, neurons, and things your psychiatrist doesn't know about
Introduction
“The brain is the great synthesizer of many biological, psychological and sociocultural phenomena that makes us who we are. It is the result of our genes and our experience working together.”
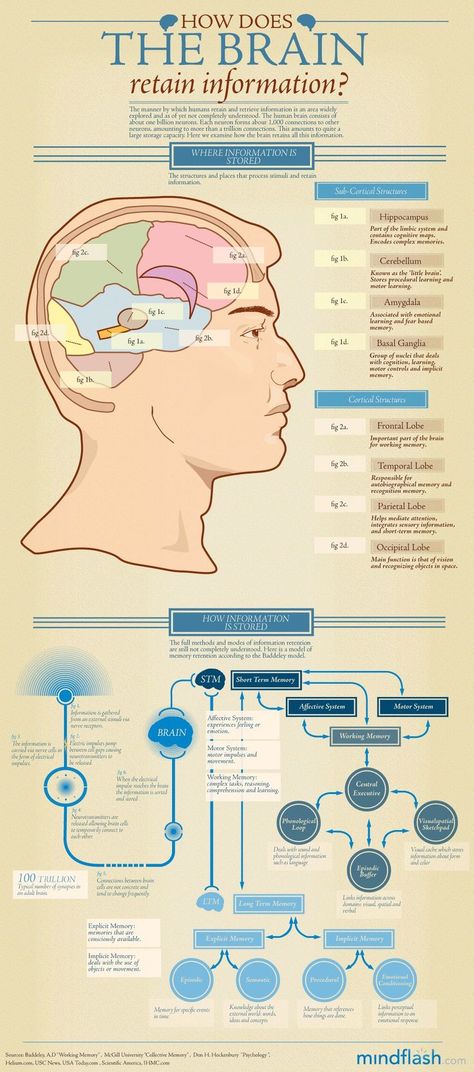
What Woody Allen called his "second favorite organ" is nothing more than a mass of 1.3 kilograms containing about 100 billion nerve cells (neurons). They are divided into thousands of different types, each of which in turn forms thousands of connections with other neurons (synapses). In total, there are between 100 trillion and a quadrillion synapses organized in intricate networks, which is the reason for the endless complexity and intricacies of the structure of the brain. More than half of the 25 thousand genes of the human genome are also responsible for its structure.
More than half of the 25 thousand genes of the human genome are also responsible for its structure.
So what happens when the brain receives a signal? Initially, signals are transmitted from a neuron along a section called an axon, which can terminate in several terminal sections (terminals). These signals are then picked up by processes (dendrites) coming from other neurons.
Communication between neurons is carried out along countless synapses (gaps) that separate axons from dendrites. In these end sections of the neuron that send an impulse, special messenger molecules called neurotransmitters are formed. They pass through the synapse and "bind" to receptors on the surface of the neuron receiving the impulse. The task of the neurotransmitter is completed when its "message" is delivered through the opening of the membrane into the interior of the neuron.
Neurotransmitters
About a hundred neurotransmitters are produced in the brain. The three most well-known, serotonin, norepinephrine, and dopamine, are chemically classified as monoamines.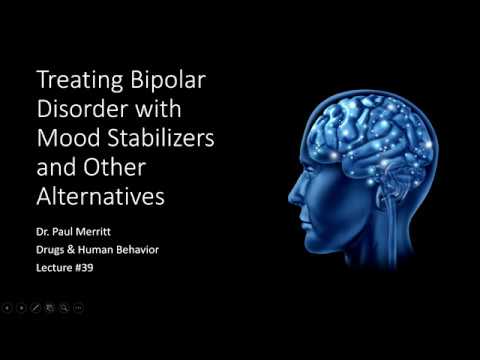 The monoamine hypothesis states that mood disorders are caused by the depletion of one or more neurotransmitters. But this theory is reminiscent of the "flat earth" theory: after all, it does not make any mention of the latest achievements in genetics, neuroscience and brain imaging.
The monoamine hypothesis states that mood disorders are caused by the depletion of one or more neurotransmitters. But this theory is reminiscent of the "flat earth" theory: after all, it does not make any mention of the latest achievements in genetics, neuroscience and brain imaging.
Neurotransmitters are just the first step in the relationship between biological processes and mood. In a 2004 American Psychological Association lecture, Jack Barchas, M.D., Cornell University, a pioneer in the field of
brain biochemistry and behavioral research, recounted how, half a century ago, while still a student, he proposed studying neurotransmitters. They answered him: “If you want to study biochemistry, study the liver. Years will pass before the processes occurring in the brain are discovered.
Psychiatry at that time was so far removed from medicine that his mentor challenged these ideas, saying, "How does that prove Freud's teachings?" Fortunately, Dr. Barkas paid no attention to these words.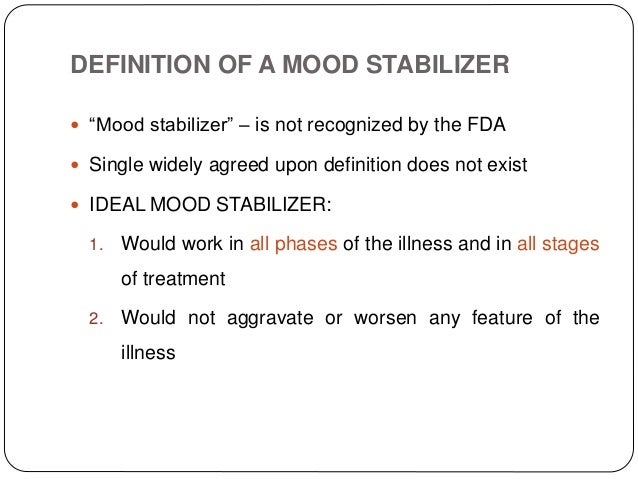
Norepinephrine
Norepinephrine (also called norepinephrine) is produced in neurons from the amino acid tyrosine. Tyrosine is converted to DOPA (dihydroxyphenylalanine) and then to dopamine (see below). Some dopamine is then converted to norepinephrine; it is "packaged" and stored in "packages" called synaptic vesicles (vesicles). Once norepinephrine is formed by the action of one enzyme, it is in danger of being destroyed by others: for example, monoamine oxidase (MAO), which also destroys serotonin and dopamine. Monoamine oxidase inhibitors (MAOIs), which inhibit this enzyme and thus prevent the destruction of monoamines, were the first antidepressants created.
When a neuron is functioning normally, it releases norepinephrine into the synaptic cleft (the space between two neurons). Norepinephrine binds to α1, α2, and β1 receptors on the postsynaptic membrane, the membrane of the neuron on the other side of the synapse. This binding is passed on to the cell, which activates certain genes that regulate the activity of proteins, which in turn determine the entire activity of the neuron.
Norepinephrine is most active in a certain part of the brainstem known as the coeruleus (locus coeruleus). It "monitors" external stimuli affecting the body, as well as physiological responses to external stimuli (for example, pain, the fight-or-flight response, etc.). Norepinephrine and the locus coeruleus are also believed to play a role in cognition, mood, emotions, movement, and blood pressure maintenance. Difficulty concentrating, fatigue, apathy, and depression are just some of the problems that result from disruptions in norepinephrine.
After norepinephrine is released into the synapse and binds to receptors on the postsynaptic membrane, the presynaptic neuron "sucks" some of the remaining neurotransmitter into the cell through a reuptake carrier protein for further packaging into vesicles and subsequent reuse. Tricyclic antidepressants (TCAs) bind to reuptake carrier proteins, preventing the neurotransmitter from being "absorbed" and prolonging its circulation and action at the synapse.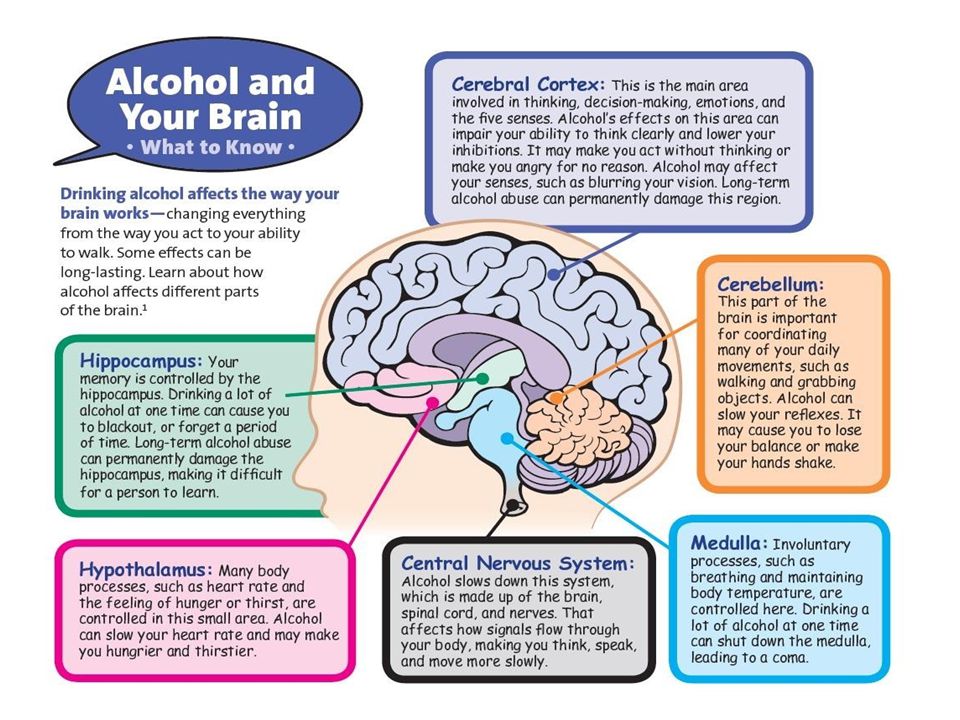 They also attach to certain serotonin receptors. New antidepressants, reuptake inhibitors, have a similar mechanism of action.
They also attach to certain serotonin receptors. New antidepressants, reuptake inhibitors, have a similar mechanism of action.
Serotonin
Serotonin, or 5-hydroxytryptamine (5-HT), is synthesized in neurons from the amino acid tryptophan, which is converted to 5-hydroxytryptophan (5-HTP) and then to serotonin. Serotonin is released into the synaptic cleft in the same way as norepinephrine. There are 17 different types of receptors for serotonin, highlighting its importance as a neurotransmitter.
Serotonin is released from the so-called. nuclei of the brain stem, spreading to other formations - the basal ganglia, the cortex of the frontal lobes, the hypothalamus, the limbic system, the spinal cord. Serotonin is also found in the gastrointestinal tract. No wonder this neurotransmitter is responsible for everything from mood, anxiety levels, sleep, sex drive, to digestion and hunger. Unfortunately, antidepressants of the SSRI group (selective serotonin reuptake inhibitors) increase serotonin concentrations in all synapses.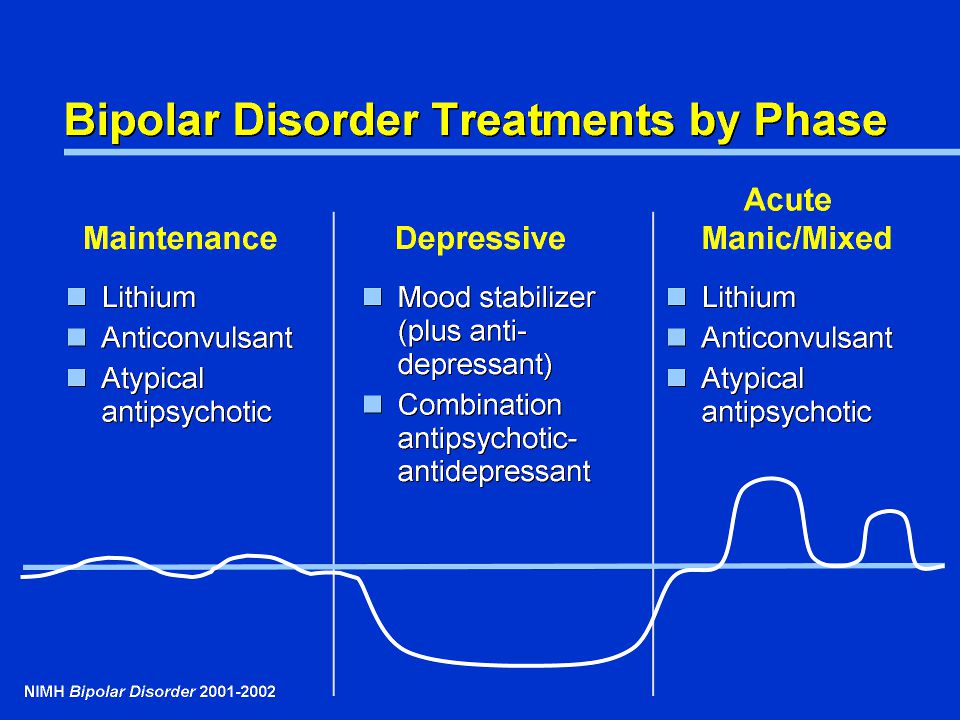 They do not take into account one fact: what has a good effect on mood can negatively affect libido and other bodily functions. Thus, the word "selective" (that is, acting selectively) in the name of this group of drugs is a complete distortion of the truth.
They do not take into account one fact: what has a good effect on mood can negatively affect libido and other bodily functions. Thus, the word "selective" (that is, acting selectively) in the name of this group of drugs is a complete distortion of the truth.
As with norepinephrine, the presynaptic reuptake carrier protein "pulls" excess serotonin from the synapse for release. Both TCAs and new antidepressants of the SSRIs and SNRIs (selective serotonin and norepinephrine reuptake inhibitors) block this protein, leaving more serotonin circulating. However, if this were true, antidepressants would have an immediate effect. In fact, for the first two weeks, they only "make an impression"; the disclosure of the full clinical effect requires another 2 to 6 weeks of continuous use.
One explanation could be that blockade of the reuptake protein desensitizes neurons, impairing normal neurotransmitter release for 4 weeks. Another possible reason is that antidepressants also affect the downstream cascade of intracellular processes (see below).
Dopamine
Dopamine is to the brain what nuclear power plants are to electrical grids. We all need energy, but sometimes it can be disastrous. Not surprisingly, several classes of drugs used in psychiatry and neurology target this neurotransmitter.
For example, antipsychotics (neuroleptics), which work like fire extinguishers, or drugs that "start the engine." The older generation of MAOIs did not directly increase dopamine (as well as other monoamines) concentrations, while the atypical antidepressant bupropion does so in a different way.
Dopamine is formed from norepinephrine, which in turn is formed from tyrosine. There are several dopaminergic neural pathways in the brain.
The mesolimbic pathway, which runs from the midbrain to the nucleus accumbens, is thought to be involved in pleasure processes and is also responsible for the development of delirium, psychotic states, and addiction to drugs. Cocaine is just notorious for increasing the production of dopamine, while antipsychotics bind to dopamine D2 receptors, preventing excessive psychoproduction (delusions, hallucinations). Unfortunately, antipsychotics are not limited to D2 receptors in the mesolimbic pathway, which leads, as Dr. Steven Stahl said in his book Essential Psychopharmacology of Antipsychotics and Mood Stabilizers, to "too much of a cost to do business."
Unfortunately, antipsychotics are not limited to D2 receptors in the mesolimbic pathway, which leads, as Dr. Steven Stahl said in his book Essential Psychopharmacology of Antipsychotics and Mood Stabilizers, to "too much of a cost to do business."
Dopamine receptor stimulants (agonists) (such as the drug pramipexole for Parkinson's disease) mimic the action of natural dopamine. They bind to D2 and D3 receptors in the nigrostriatal dopaminergic pathway from the substantia nigra of the brainstem to the basal ganglia and striatum. The above drug is clinically tested in patients with depression. A new generation of drugs that stimulate D1 receptors is under development. Dopamine receptor agonists are expected to counteract apathy and cognitive dulling.
Glutamate
Glutamate and GABA (γ-aminobutyric acid) are a yin-yang pair, as Darryle Schoepp, PhD, explained at the 2003 American Psychiatric Association meeting. Both of these neurotransmitters regulate almost all functions synapses throughout the brain, with glutamate being an "excitatory" neurotransmitter and GABA being an "inhibitory" neurotransmitter.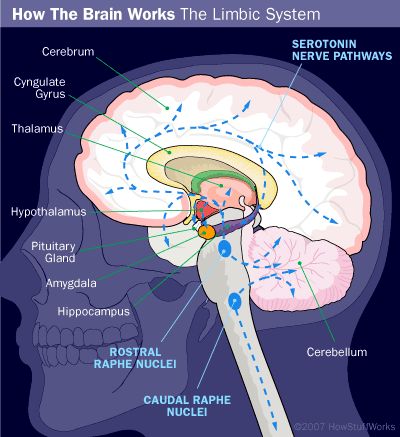 It is believed that mood stabilizers (normothymics) act on either one or the other, or both of them.
It is believed that mood stabilizers (normothymics) act on either one or the other, or both of them.
There are 2 types of glutamate receptors - ionotropic (iGluR), which include NMDA-, AMPA-, and kainate receptors, and metabotropic (mGluR), which control numerous chemical reactions.
When the NMDA receptor is functioning correctly, glutamate and glycine attach to it, which "opens" the ion channel within the receptor, allowing calcium ions to enter the neuron. This triggers an intracellular cascade of signaling reactions necessary for cell adaptation and survival.
However, too much glutamate can lead to disaster. The mood stabilizer lamotrigine, which has been shown to be effective in the treatment of bipolar depression, is an anti-glutamate drug.
GABA
GABA (γ-aminobutyric acid) is formed in the brain from glutamate, glucose and glutamine. It attaches to one of two receptors on the postsynaptic membrane, GABA or GABA.
GABA receptors regulate excitability, anxiety, panic and stress.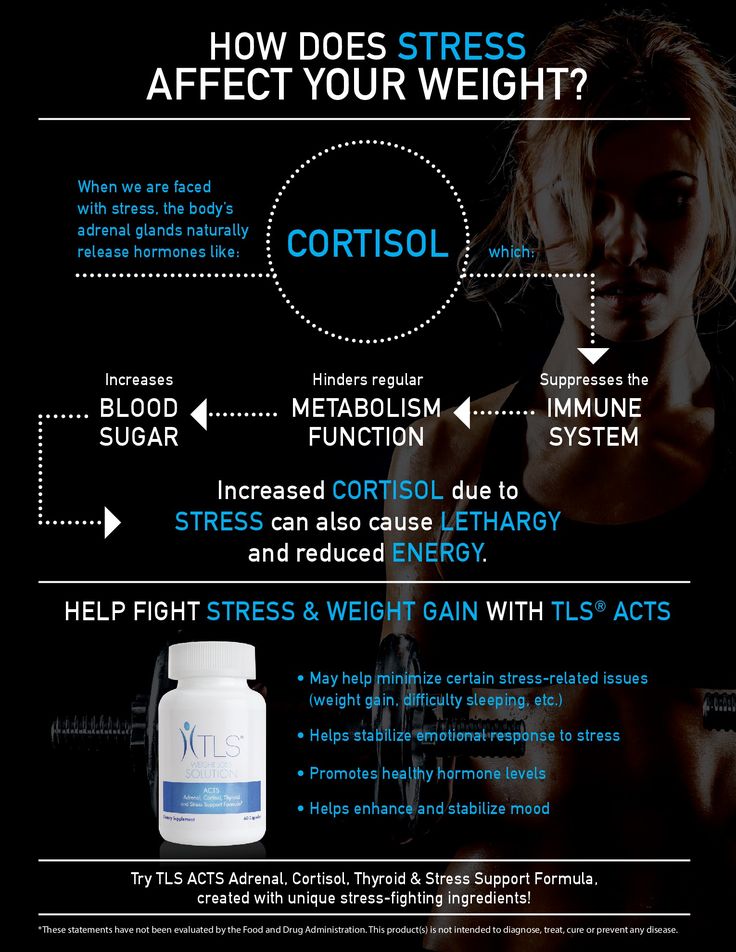 They are application point
They are application point
benzodiazepine tranquilizers (such as diazepam), barbiturates, and alcohol. In persons with depression, the level of GABA in the cerebrospinal fluid and blood plasma is reduced.
Gerard Sanacora, MD Yale, used magnetic resonance spectroscopy to measure GABA levels in the brain. He found that people with mild depression have low concentrations of GABA in the occipital cortex, but the depletion of GABA is not as pronounced as in people with atypical depression. This indicates the possibility of a more detailed approach in the diagnosis of depression. Dr. Sanacora also compared before and after scans, revealing that patients treated with antidepressants or electroconvulsive therapy had significantly increased GABA levels.
Inside a neuron
Until recently, it was believed that new neurons could not form in the brain. In terms of mood disorders, this is a sad fact. Imaging of the brain and examination of the bodies of the deceased revealed that in people with depression and bipolar disorder, there is a decrease in the volume of the prefrontal cortex, as well as atrophy of nerve cells and their death.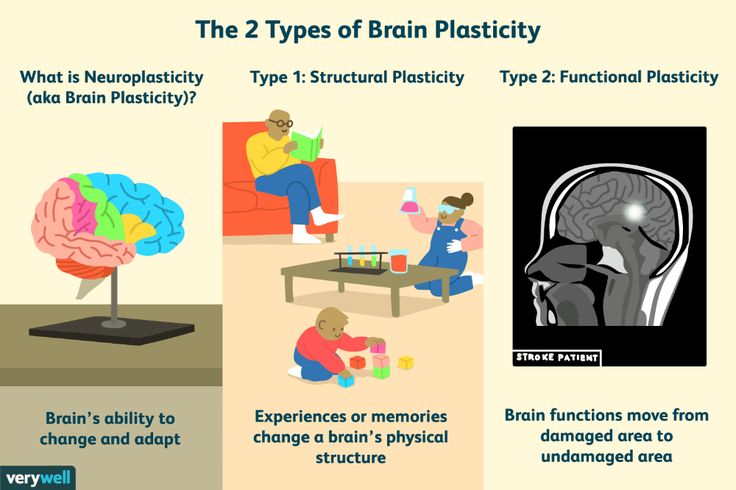 In a classic study in 1997, Dr. Wayne Drevets (National Institute of Mental Health, USA) found that the popliteal prefrontal cortex was 38% smaller than normal in patients with bipolar disorder and 48% in those with depression, regardless of their mental health and treatment.
In a classic study in 1997, Dr. Wayne Drevets (National Institute of Mental Health, USA) found that the popliteal prefrontal cortex was 38% smaller than normal in patients with bipolar disorder and 48% in those with depression, regardless of their mental health and treatment.
In experiments conducted by Robert Sapolsky (Stanford University), exposure of animals to stress factors led to the death or atrophy of neurons in the hippocampus.
Some neurons were also at risk, being more likely to die when exposed to other stressors.
One of the components of the brain that is deficient during stress is brain-derived neurotrophic factor (BDNF). It is a neuropeptide that plays a key role in the survival and growth of neurons.
Stress increases cortisol levels, which in turn increase the excitatory neurotransmitter glutamate. This increases the chance of calcium getting inside the neuron and activates certain calcium-dependent "death enzymes". Cortisol can also reduce the neuron's ability to store glucose, which supports energy metabolism in the cell.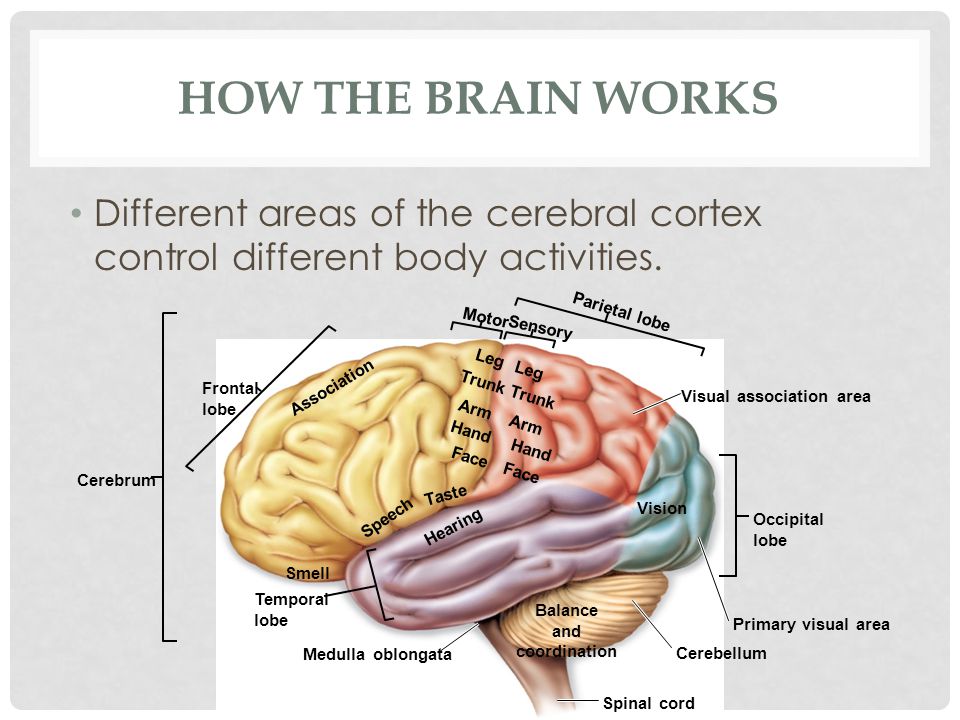 Thus, the cell may not have enough strength to cope with the subsequent crisis.
Thus, the cell may not have enough strength to cope with the subsequent crisis.
“Put simply, the cell can't handle the load,” Dr. Husseini Manji, head of the National Institute of Mental Health's Anxiety and Mood Disorders Program, explained in a 2003 lecture. Atrophy and death of neurons follows, which reduces their ability to communicate with each other and transmit signals to other cells.
Back in the 1960s. it became known that nerve cells do recover: under favorable conditions, new cells can grow in the brain of animals, and compressed, shrunken brain cells can return to their normal size and create new intercellular connections - a process called neurogenesis. Most of it takes place in the hippocampus. In 2000, Fred Gage (PhD, Salk Institute) discovered that neurogenesis can also occur in humans.
In 2000, Ron Duman (PhD) and his team at Yale University, using rats, discovered that antidepressants promote the growth of new cells in the hippocampus. A year later, he published a hypothesis that the same effect might also occur in humans.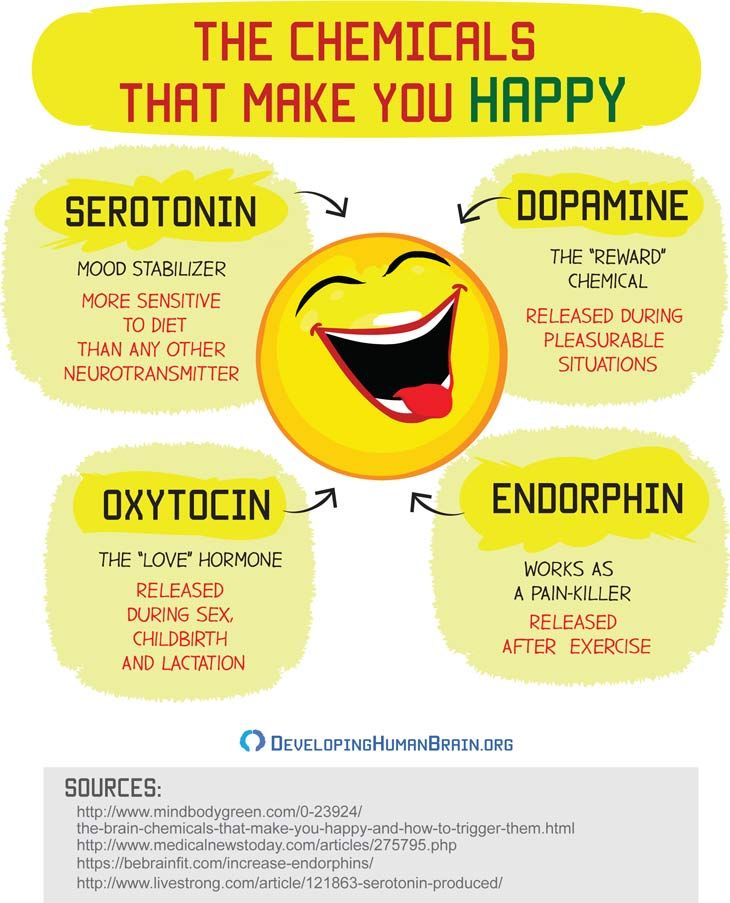 Dr. Dyuman and colleagues were the first to discover that repeated antidepressant treatment stimulates a process known as the cAMP-CREB cascade. CAMP (cyclic adenosine monophosphate) is a signaling molecule found in the DNA sequence of the CREB protein (closer to the 5' end of the DNA). CREB controls the activity of certain genes, including BDNF. It is important that CREB and BDNF play critical roles in neuroplasticity — that is, in the ability of the brain to constantly redistribute memory, “reshape itself” by memorizing new information and retaining it.
Dr. Dyuman and colleagues were the first to discover that repeated antidepressant treatment stimulates a process known as the cAMP-CREB cascade. CAMP (cyclic adenosine monophosphate) is a signaling molecule found in the DNA sequence of the CREB protein (closer to the 5' end of the DNA). CREB controls the activity of certain genes, including BDNF. It is important that CREB and BDNF play critical roles in neuroplasticity — that is, in the ability of the brain to constantly redistribute memory, “reshape itself” by memorizing new information and retaining it.
The cAMP-CREB cascade also appears in neurogenesis. Dr. Dyuman and his team shocked the paws of rats to induce behavioral helplessness, which led to long-term inhibition of neurogenesis. But when the animals were treated with antidepressants, their behavior returned to normal.
Approximately 9,000 new cells form in the hippocampus of an adult rodent every day. Of these, 75–80% become neurons, of which only half survive after 4 weeks. It is estimated that in humans, the rate of new cell growth is only 10–20% of that in rodents. According to Dr. Dyuman, this is still enough to affect the functions of the hippocampus.
It is estimated that in humans, the rate of new cell growth is only 10–20% of that in rodents. According to Dr. Dyuman, this is still enough to affect the functions of the hippocampus.
Meanwhile, a study led in 2000 by Dr. Manji found that lithium "significantly increases total brain gray matter volume in people with bipolar disorder."
Using a gene microchip (microarray) - a process that allows researchers to record the interactions of thousands of genes at once - Dr. Manji and his colleagues began to experiment with lithium and valproate on brain cells. To their surprise, they found that two completely different drugs affected the same cell signaling pathways associated with cell survival or cell death. In one experiment, the level of a protective protein involved in these signaling pathways (Bcl-2) doubled after administration of lithium and valproate. Subsequent experiments in rats revealed that lithium mitigated the effects of artificially induced stroke and increased the growth of new neurons in the hippocampus.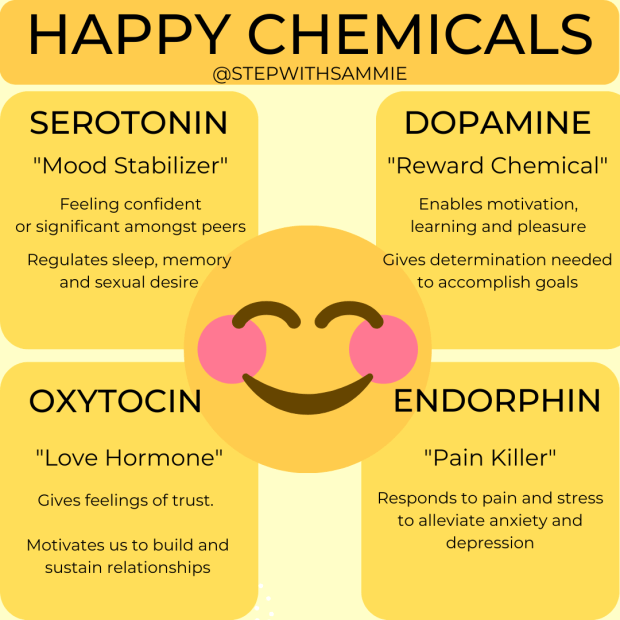 When Dr. Manji asked Dr. Drewetz to review his study, it was found that patients who took lithium or valproate showed no signs of brain atrophy.
When Dr. Manji asked Dr. Drewetz to review his study, it was found that patients who took lithium or valproate showed no signs of brain atrophy.
The growth of new cells in the brain is just one side of the coin, and most likely not the main one. “More important is the ability to protect and repair damaged brain cells and help them re-create intercellular connections,” said Dr. Manji. To fully appreciate the potential of lithium, we must understand that both depression and bipolar disorder are more than just mood disorders. Cognitive and behavioral impairment can last much longer than a normal affective episode. Although major depressive disorder and bipolar disorder are not the "classic" neurodegenerative (i.e., brain-destroying) diseases such as Alzheimer's and Parkinson's, they are nevertheless accompanied by a decrease in the number and shrinkage of brain cells.
"Impressively, the Bcl-2 protein protects against the effects of free radicals that can damage brain cells, as well as against the development of Parkinson's disease, and the possibly damaging effects of mood disorders," Dr.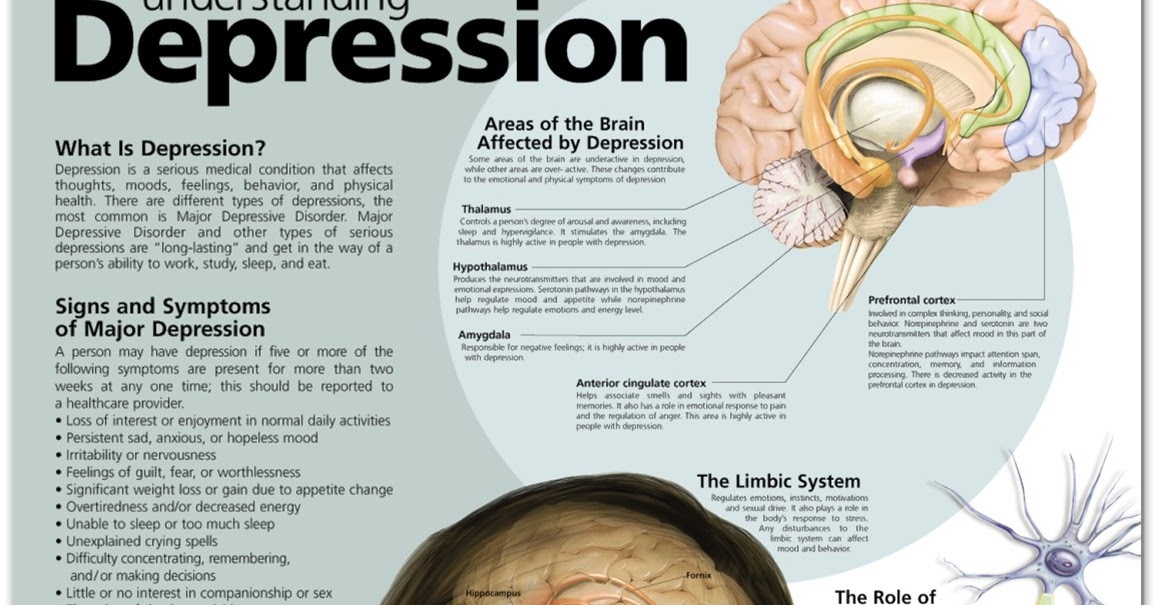 Manji informed the annual conference of the National Alliance on Mental Health. (NAMI) in 2002.
Manji informed the annual conference of the National Alliance on Mental Health. (NAMI) in 2002.
Dr. Manji explained that over the past three decades, mental health research has primarily focused on neurotransmitters. But recently, scientists have begun to realize that mental disorders are more complex than thought. Nerve cells communicate with each other through neurotransmitters, but they do not travel directly from one cell to another. More precisely, they are simply keys that can open the way to what happens inside neurons, where all processes take place.
According to Dr. Manji, there are about 10 different potential targets within the nerve cell that we didn't even know existed 10 years ago.
One of the possible intracellular targets is the protein kinase C (PKC) enzyme involved in the signaling pathway responsible for neuronal excitability. Dr. Manji's team found that both lithium and valproate had a similar effect on the PKC systems, and that their action began days to weeks later. Inhibition of protein kinase C, however, can be done directly. One small study used tamoxifen, an anticancer drug used for breast cancer. It inhibited (suppressed) protein kinase C. It was found that its use significantly reduced the severity of mania. Trials are planned with a larger sample of patients at the National Institute of Mental Health and Harvard University. “If they are successful,” said Dr. Manji, “we can develop a PKC inhibitor with better properties.”
Inhibition of protein kinase C, however, can be done directly. One small study used tamoxifen, an anticancer drug used for breast cancer. It inhibited (suppressed) protein kinase C. It was found that its use significantly reduced the severity of mania. Trials are planned with a larger sample of patients at the National Institute of Mental Health and Harvard University. “If they are successful,” said Dr. Manji, “we can develop a PKC inhibitor with better properties.”
A review article by Dr. Manji and colleagues at the National Institute of Mental Health (Biological Psychiatry May 2003) states that the main problem with antidepressant use is the mistaken assumption that our intracellular cascades are intact and will accurately redirect drug-enhanced neurotransmitter activity to the right points. In fact, quite the opposite is found: some brain cells mistake the “bombardment” of neurotransmitters for a kind of violence that forces them to develop “both trophic and neurochemical support” in order to restore neuronal connectivity and molecular signaling.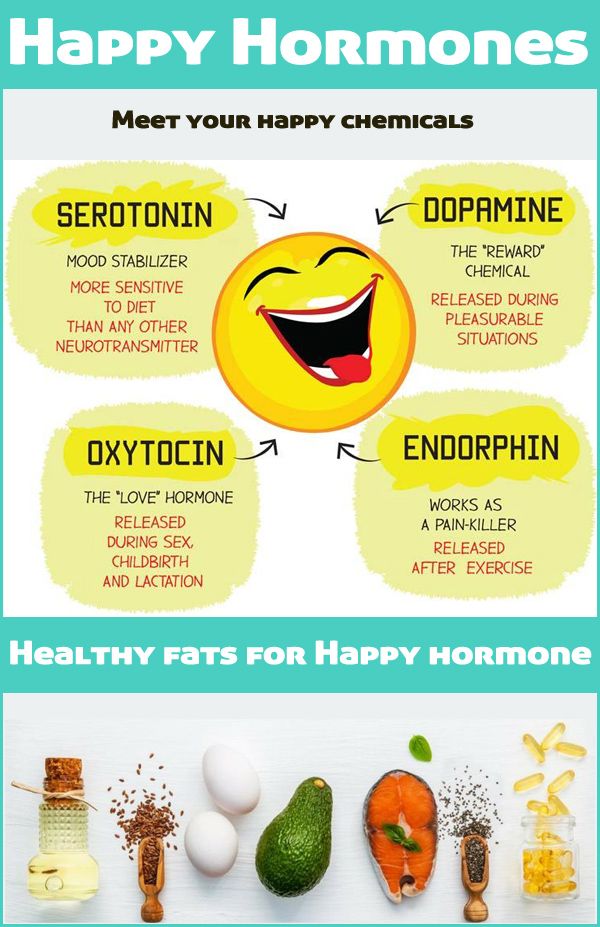
Someday cAMP, Bcl-2, BDNF and other targets may become as widely known as serotonin is today, not only in academia, but also as entry points for new drugs designed to improve our lives.
Other brain cells
There are two fundamentally different groups of brain cells - neurons and glial cells (neuroglia, or simply glia). “Brain glue” was the unpretentious term German scientists called this substance (the word “glia” means “glue” in Greek). As researchers began studying this structure, slowly but surely, these "other brain cells" gained their respect.
The story began in the early 1960s, when scientists discovered that the cerebral cortex of rat pups living in an enriched environment (nutrition, light, etc.) contained more glial cells per neuron than those of rat pups growing up in debilitating conditions . Apparently, more active cortical neurons required a larger "support network". As a rule, we stay with the neurons with which we were born for life (these cells do not divide).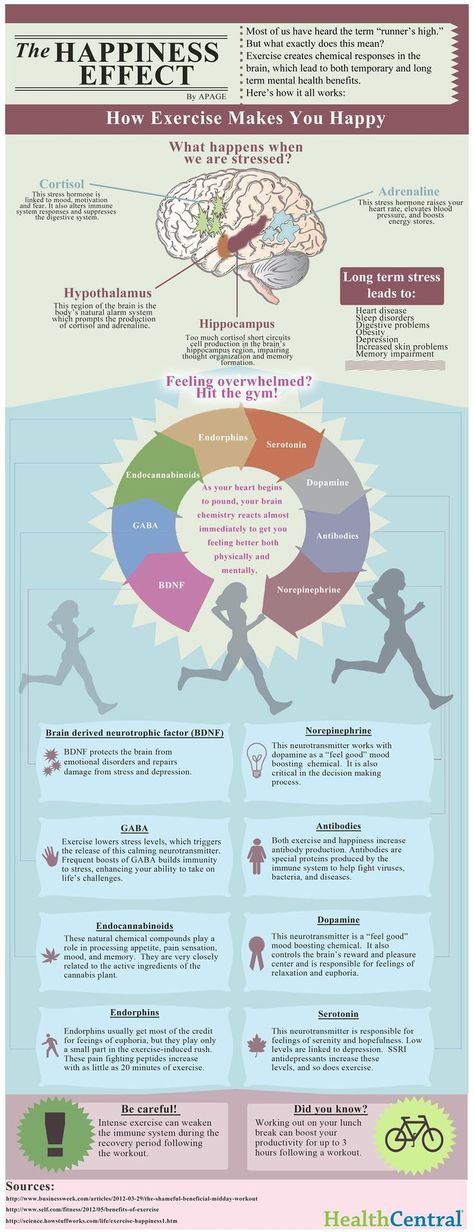 But glia is capable of this. In humans, the number of glial cells and neurons is in the ratio of about 9to 1. This is more than in the lower animals.
But glia is capable of this. In humans, the number of glial cells and neurons is in the ratio of about 9to 1. This is more than in the lower animals.
Two decades after research on rat brains, 4 pieces of Albert Einstein's brains, each the size of a sugar cube, arrived by mail to one of the researchers, Marian Diamond (PhD, from the University of California at Berkeley). When Dr. Diamond compared regions of the cerebral cortex associated with active cognitive processes with similar regions of 11 control samples, she found that Einstein's brain was literally "filled" to the brim with glial cells.
Advanced neuroimaging has confirmed that glia should not be ignored. Our knowledge was far from perfect, but now it turned out that the glia is in constant, ongoing "dialogue" with the neuron.
Astrocytes are a type of glia that surrounds the synapses between neurons. Of particular interest is the neurotransmitter glutamate, which binds to receptors on the downstream neuron and opens the channels of the cell membrane.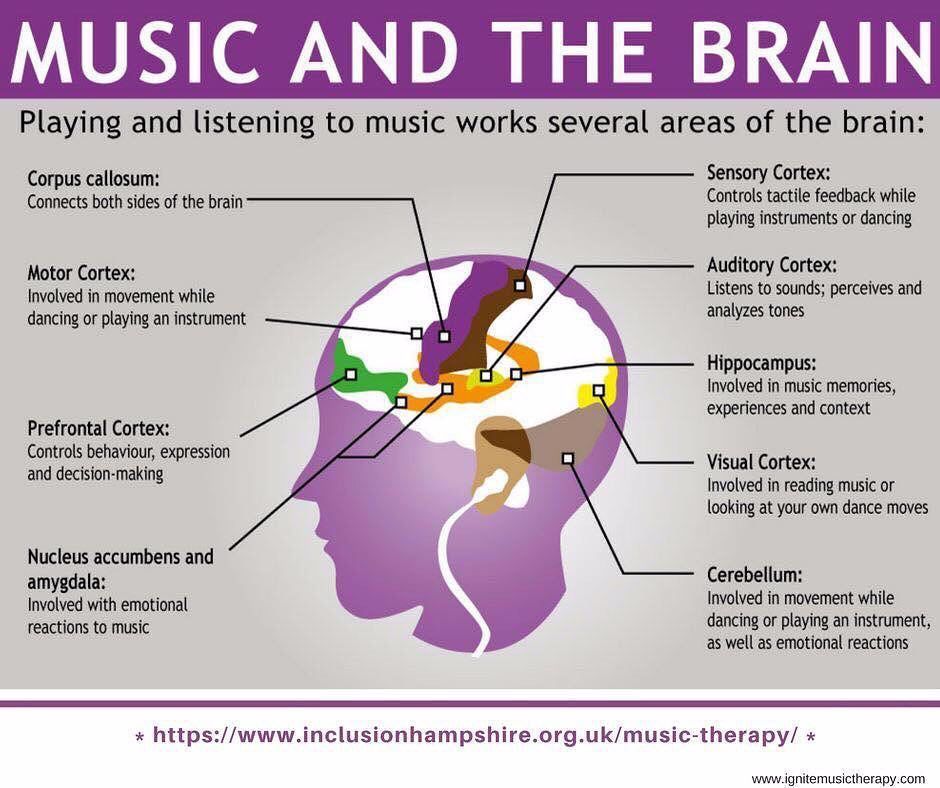 This allows calcium ions to get in and alert the entire "chemical population" inside the cell. Through a series of chemical interactions, astrocytes are able to enhance signaling with the help of glutamate, releasing it from themselves, or, conversely, weaken it, removing this neurotransmitter from the synapse.
This allows calcium ions to get in and alert the entire "chemical population" inside the cell. Through a series of chemical interactions, astrocytes are able to enhance signaling with the help of glutamate, releasing it from themselves, or, conversely, weaken it, removing this neurotransmitter from the synapse.
Glutamate (in partnership with GABA) is an essential ingredient in mood regulation. When something doesn't go according to plan, glia always stays in place. Some studies on the brains of deceased people who suffered from major depressive disorder or bipolar disorder during life showed that they had lower than normal levels of glia in certain regions of the brain. Without glia, the neuron remains practically defenseless, it is unable to resist the “bombardment” by glutamate and the subsequent negative effects of calcium ions.
In a 2004 article in the journal Neuroscientist, Bernhard Mitterauer (MD, University of Salzburg) proposed the neuronal-glial imbalance hypothesis to explain bipolar affective disorder.