How much does a lobotomy cost
What is a Lobotomy? Risks, History and Why It’s Rare Now
What is a Lobotomy? Risks, History and Why It’s Rare NowMedically reviewed by Alana Biggers, M.D., MPH — By Daniel Yetman on April 28, 2022
Few medical procedures in history have garnered as much controversy as the lobotomy. Tens of thousands of lobotomies were performed in the United States in the mid-1900s, often leading to devastating outcomes.
A lobotomy, also called a leucotomy, is a type of psychosurgery that was used to treat mental health conditions such as mood disorders and schizophrenia. Psychosurgeries are procedures that involve the physical removal or alteration of part of the brain.
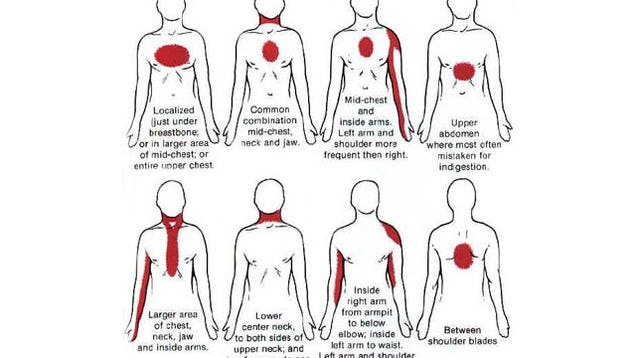
Lobotomies involved separating tissue in an area called the prefrontal cortex in one of two primary ways:
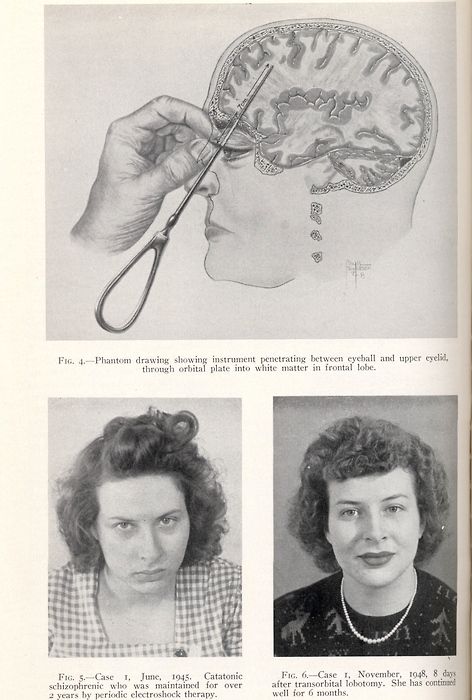
- Frontal lobotomy. A surgeon drilled a hole into each side of the skull and cut through brain tissue with an instrument resembling an ice pick called a leucotome.
- Transorbital lobotomy.
A surgeon inserted a leucotome through the eye socket and drove it through a thin layer of bone with a mallet to access the brain.
These procedures are no longer performed in the United States, but some other types of psychosurgery are still performed when other treatments have failed. Read on to learn more about why lobotomies were traditionally performed and why psychosurgery is used today.
Lobotomies are no longer performed in the United States. They began to fall out of favor in the 1950s and 1960s with the development of antipsychotic medications. The last recorded lobotomy in the United States was performed by Dr. Walter Freeman in 1967 and ended in the death of the person on whom it was performed.
In Europe, the Soviet Union banned lobotomies in 1950, a year after inventor Dr. Egas Moniz won the Nobel Prize for medicine. They persisted into the 1970s in the rest of Europe and into the 1980s in Scandinavia.
Some other types of psychosurgeries are still used today, such as:
- cingulotomy
- anterior capsulotomy
- subcaudate tractotomy
- limbic leucotomy
- corpus callosotomy
With advancements in medications, psychosurgeries are rarely performed. Surgery is usually only used when all other treatment options have failed. Surgical techniques still in use today include:
Surgery is usually only used when all other treatment options have failed. Surgical techniques still in use today include:
Cingulotomy
Cingulotomy is the most commonly performed psychosurgery in North America. It’s a type of surgery that involves altering tissue in the anterior cingulate region associated with feeling chronic pain. It’s sometimes used to manage symptoms of:
- chronic and severe anxiety disorders, such as obsessive-compulsive disorder (OCD)
- severe mood disorders, such as treatment-resistance depression or bipolar disorder
- heroin addiction
- chronic pain syndromes that don’t respond to other treatments
- severe schizophrenia with aggressive behavior
Anterior capsulotomy
An anterior capsulotomy is a potential treatment for severe OCD that doesn’t respond to psychotherapy and medications. It involves altering the part of the brain that carries information from the thalamus and brainstem to the prefrontal region.
In a 2019 review, researchers found that of 512 people who received treatment from 1961 to 2018, 73 percent responded to the surgery and 24 percent saw their symptoms resolve.
Subcaudate tractotomy
A subcaudate tractotomy may be used to treat delusions and hallucinations in people with severe schizophrenia with aggressive symptoms. It involves cutting connections between the limbic system and a part of the prefrontal lobe called the orbitofrontal cortex.
Limbic leucotomy
Limbic leucotomy is a combination of the subcaudate tractotomy and cingulotomy. It’s been performed since the 1970s to treat mood disorders and OCD.
Corpus callosotomy
Corpus callosotomy involves severing the corpus callosum, a bundle of nerves that connect your left and right brain hemispheres. In a 2017 study, researchers found that corpus callosotomy is a potentially effective treatment for generalized epilepsy in people with drug-resistant epilepsy.
Lobotomies were considered experimental even at the height of their popularity. Although some people did see improvements in their conditions, many other people experienced life-alternating side effects, or even died.
Although some people did see improvements in their conditions, many other people experienced life-alternating side effects, or even died.
One of the highest-profile cases of a failed lobotomy was that of Rosemary Kennedy, younger sister of John F. Kennedy. After undergoing a lobotomy in 1941 to treat seizures and extreme shifts in mood, she lost her ability to walk or talk. Her personality was permanently altered, and she was left with physical disability.
Risks of psychosurgeries include the risk of death and:
- seizures
- loss of bladder control or bowel control
- changes in appetite
- weakness
- changes in language ability
- brain infection
- cognitive impairment
- changes in personality and emotion
António Egas Moniz and his colleague Almeida Lima are credited with the development of the lobotomy in 1935. They promoted their frontal lobotomy procedure across Europe, despite keeping poor patient records and lacking evidence of effectiveness. The procedure quickly gained popularity, despite thousands of people experiencing severe side effects and outcomes, such as seizures, infections, and death.
The procedure quickly gained popularity, despite thousands of people experiencing severe side effects and outcomes, such as seizures, infections, and death.
American neurologist Walter Freeman and surgeon James Watts championed the procedure in America. Influenced by an Italian colleague, Freeman eventually switched to the transorbital method, in which an icepick-like instrument was inserted through the eye socket to reach the brain. He passionately spread the surgery across North America, despite haphazardly performing surgeries without proper sterilization.
Tens of thousands of lobotomies were performed in the United States between the 1930s and 1960s, often without informed consent. Eventually, lack of evidence supporting the procedure finally caught up with it, and it was largely abandoned once the medication chlorpromazine was developed.
Despite a risk of severe side effects and outcomes, lobotomies were once used to treat many mental health conditions, including schizophrenia, depression, and bipolar disorder. Nowadays, treatment for mental health conditions largely consists of medication and psychotherapy.
Nowadays, treatment for mental health conditions largely consists of medication and psychotherapy.
Antipsychotics and other medications
Antipsychotics are often the initial treatment for acute schizophrenic episodes. They block the effects of the neurotransmitter dopamine on your brain to reduce feelings of anxiety or aggression as well as hallucinations and delusional thoughts.
Many other types of medications are also used to treat mental health conditions, including:
- antidepressants
- anti-anxiety medications
- stimulants
- mood stabilizers
Psychotherapy
Psychotherapy, also called talk therapy, is a common type of mental health treatment. It may be administered alone or in combination with medication. There are many types of psychotherapy used to treat mental health conditions. They include:
- cognitive behavioral therapy
- dialectical behavioral therapy
- interpersonal therapy
- psychodynamic therapy
- psychoanalysis
Hospitalization
Some people with severe mental health conditions may need to be admitted to a medical facility. Laws vary by state, but in most states, a person can be held in facility involuntarily if they pose a danger to themselves or others.
Laws vary by state, but in most states, a person can be held in facility involuntarily if they pose a danger to themselves or others.
Lobotomies were surgeries that involved altering a part of the brain called the prefrontal cortex. Sometimes these surgeries were performed without consent and without proper sterilization, despite a lack of evidence for their effectiveness.
Lobotomies are no longer performed and have largely been replaced by medications. Some other types of psychosurgeries are performed in very rare circumstances to treat conditions such as severe depression or OCD that doesn’t respond to other treatments. These surgeries are considered last resorts.
Last medically reviewed on April 28, 2022
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Caruso JP, et al. (2017). Psychosurgery, ethics, and media: A history of Walter Freeman and the lobotomy.
thejns.org/focus/view/journals/neurosurg-focus/43/3/article-pE6.xml - Gallea MA. (2017). A brief reflection on the not-so-brief history of the lobotomy.
bcmj.org/mds-be/brief-reflection-not-so-brief-history-lobotomy - Lovell B. (2015). Frontal lobotomy: A vanishing but important radiological finding.
ncbi.nlm.nih.gov/pmc/articles/PMC4533630/ - Luat AF, et al. (2017). Corpus callosotomy for intractable epilepsy revisited: The Children’s Hospital of Michigan series.
ncbi.nlm.nih.gov/pmc/articles/PMC5436305/ - Manjila S, et al. (2019). Minimally invasive bilateral anterior cingulotomy via open minicraniotomy using a novel multiport cisternoscope: A cadaveric demonstration.
ncbi.nlm.nih.gov/pmc/articles/PMC6215753/ - Pepper J, et al. (2019). Anterior capsulotomy for obsessive-compulsive disorder: A review of old and new literature.
:origin()/pre08/0f68/th/pre/f/2017/032/c/e/lobotomy_girls_by_skullbow09-daxjio6.png)
thejns.org/view/journals/j-neurosurg/133/5/article-p1595.xml - Rosemary Kennedy, the eldest Kennedy daughter. (2021).
nps.gov/articles/000/rosemary-kennedy-the-eldest-kennedy-daughter.htm - Sinha S, et al. (2015). Ablative limbic system surgery: Review and future directions.
link.springer.com/article/10.1007/s40473-015-0038-1 - Staudt MD, et al. (2019). Evolution in the treatment of psychiatric disorders: From psychosurgery to psychopharmacology to neuromodulation.
ncbi.nlm.nih.gov/pmc/articles/PMC6384258/ - Treatment — Schizophrenia. (2019).
nhs.uk/mental-health/conditions/schizophrenia/treatment/ - Tuft M, et al. (2017). Post-lobotomy epilepsy illustrated by the story of Ellinor Hamsun, the daughter of the famous Norwegian author Knut Hamsun.
ncbi.nlm.nih.gov/pmc/articles/PMC5633827/ - Vilela-Filho O, et al. (2021). The impact of subcaudate tractotomy on delusions and hallucinations in psychotic patients.

ncbi.nlm.nih.gov/pmc/articles/PMC8492415/ - Zajicek B. (2017). Banning the Soviet lobotomy: Psychiatry, ethics, and professional politics during late Stalinism.
pubmed.ncbi.nlm.nih.gov/28366896/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Apr 28, 2022
By
Daniel Yetman
Edited By
Roman Gokhman
Medically Reviewed By
Alana Biggers, MD, MPH
Copy Edited By
Christina Baswell
Share this article
Medically reviewed by Alana Biggers, M.D., MPH — By Daniel Yetman on April 28, 2022
Read this next
What Part of the Brain Controls Speech?
Medically reviewed by Nancy Hammond, M.D.
Researchers have studied what part of the brain controls speech, and now we know much more. The cerebrum, more specifically, organs within the…
READ MORE
Everything You Need to Know About Hallucinations
Medically reviewed by Timothy J.
 Legg, PhD, PsyD
Legg, PhD, PsyDHallucinations are sensations that appear real but are created by your mind. They can affect all of your senses. Learn about the types, causes, and…
READ MORE
Is Shock Therapy Being Underutilized in Treating Depression?
In a new study, some experts recommend that electroconvulsive therapy be used more often and earlier to help people with depression.
READ MORE
Can Zapping People’s Brains Really Reduce Violent Behavior?
A controversial new study found a noninvasive form of brain stimulation may reduce a person’s likelihood to engage in aggressive acts. But should it…
READ MORE
Vagotomy
Medically reviewed by Saurabh Sethi, M.D., MPH
A vagotomy is a procedure that removes part of your vagus nerve, which plays an important role in the functioning of your digestive system.
 It used to…
It used to…READ MORE
Your Old iPhone Might Save Lives During Brain Surgery
Researchers have found that old iPhones could replace expensive surgical equipment. In some ways, the devices are easier to use, too.
READ MORE
‘Musical Brain Surgery’ Part of a New Trend
Brain mapping is allowing surgeons to perform operations where the patient plays music or performs tasks to make sure the surgery is going well.
READ MORE
Awake Brain Surgery Isn't Just on ‘Grey's Anatomy’
Performing brain surgery on patients who are awake allows surgeons to map — and preserve — areas of the brain that are vital to a patient’s…
READ MORE
Atrial Fibrillation: Ablation Surgery May Be More Effective for AFib Than Drugs
Researchers say ablation surgery appears to be more effective than drugs in both the short-term and the long-term for treating atrial fibrillation
READ MORE
Lobotomy: The brain op described as ‘easier than curing a toothache’
Published
Image source, Wellcome Collection
Image caption,Lobotomy instruments that once belonged to Walter Freeman
There was a time when people with severe mental illness might be given an operation to sever connections in the brain. Lobotomy became one of the most notorious surgical procedures of the 20th Century, writes Claire Prentice, but retired neurosurgeon, Henry Marsh, who once carried out a modified version of the operation, tells her it's wrong to divide doctors into heroes and villains.
It seems incredible today, but lobotomy was once hailed as a miracle cure, portrayed by doctors and the media as "easier than curing a toothache".
More than 20,000 lobotomies were performed in the UK between the early 1940s and the late '70s. They were typically carried out on patients with schizophrenia, severe depression or Obsessive Compulsive Disorder (OCD) - but also, in some cases, on people with learning difficulties or problems controlling aggression.
While a minority of people saw an improvement in their symptoms after lobotomy, some were left stupefied, unable to communicate, walk or feed themselves. But it took years for the medical profession to realise that the negative effects outweighed the benefits - and to see that drugs developed in the 1950s were effective and much safer.
Writers and film directors have not been kind to the doctors who carried out lobotomies. From One Flew Over the Cuckoo's Nest and the Netflix spin-off series, Ratched, to Suddenly Last Summer, they portray sadistic surgeons preying on the vulnerable and leaving dead-eyed patients in their wake.
Image source, Getty Images
Image caption,Jack Nicholson as Randle McMurphy being restrained in One Flew Over The Cuckoo's Nest
Image source, Alamy
Image caption,Sarah Paulson as Nurse Ratched (right) in a scene from Ratched
The truth is more complex. Lobotomists were often progressive reformers, driven by a desire to improve the lives of their patients.
In the 1940s, there were no effective treatments for the severely mentally ill. Doctors had experimented with insulin shock therapy and Electro-Convulsive Therapy with limited success and asylums were filled with patients, including shell-shocked soldiers, who had no hope of a cure, or of going home.
It was against this background that Portuguese neurologist Egas Moniz developed the lobotomy - or leucotomy as he called it - in 1935. His procedure involved drilling a pair of holes into the skull and pushing a sharp instrument into the brain tissue. He then swept it from side to side to sever the connections between the frontal lobes and the rest of the brain.
"It was based on this terribly crude, simplistic view of the brain, that the brain was a simple mechanism, and you could just sort of stick things into it. The idea was that you had these thoughts running round and round and by interrupting the circuit you would stop these distressing, obsessional thoughts," says the neurosurgeon and writer, Henry Marsh.
"In reality the brain is utterly complicated and we don't even begin to understand how it all interconnects."
- Listen to Archive on 4: Easier Than Curing A Toothache? The Story of Lobotomy on BBC Radio 4 at 20:00 on Saturday 30 January
- Explore previous episodes of Archive on 4
Moniz claimed that his first 20 patients had experienced a dramatic improvement - and a young American neurologist, Walter Freeman, was greatly impressed. With his operating partner, James Watts, he carried out the first lobotomy in the US in 1936; the following year, the New York Times referred to the operation as "the new 'surgery of the soul'". But to begin with it was complicated and time-consuming.
While working at St Elizabeths Hospital in Washington DC, the largest mental hospital in the country, Freeman had been horrified by "the waste of manpower and woman power" he witnessed there. He was keen to help patients get out of hospital, and set himself the goal of making lobotomy quicker and cheaper.
In 1946 he devised the "transorbital lobotomy" in which steel instruments resembling ice picks were hammered into the brain through the fragile bones at the back of the eye sockets. The operating time was drastically reduced, and patients did not need an anaesthetic - they were knocked out before the operation using a portable "Electro-Shock" machine.
Image source, Getty Images
Image caption,Walter Freeman demonstrating his transorbital lobotomy technique in 1949
Freeman would drive across America during the long summer holidays to conduct his "ice-pick lobotomies" - sometimes taking his children along.
Initially described as a surgery of last resort for psychiatric patients for whom all other treatments had failed, Freeman began to promote lobotomy as a cure for everything from serious mental illness to post-natal depression, severe headaches, chronic pain, nervous indigestion, insomnia and behavioural difficulties.
Image source, Getty Images
Image caption,Freeman's colleague, Dr James Shanklin, uses electrical apparatus to prepare a patient for transorbital lobotomy
Many patients and their families were grateful to Freeman, who kept boxes filled with the letters of thanks and Christmas cards they sent him. But in other cases the results were disastrous.
But in other cases the results were disastrous.
Freeman's patients included Rosemary Kennedy, sister of the future US president John F Kennedy. She was left incontinent and unable to speak clearly after a lobotomy at the age of 23.
Over the course of his career, Freeman conducted lobotomies on 3,500 patients, including 19 children, the youngest just four years old.
Freeman's counterpart in the UK was the neurosurgeon, Sir Wylie McKissock, who carried out his own variation of the lobotomy on about 3,000 patients.
"This is not a time-consuming operation. A competent team in a well-organised mental hospital can do four such operations in two to two-and-a-half hours," he boasted. "The actual bilateral prefrontal leucotomy can be done by a properly trained neurosurgeon in six minutes and seldom takes more than 10 minutes."
Thanks in large part to McKissock, more lobotomies were carried out in the UK, per head of population, than in the US.
As a medical student in the 1970s, Henry Marsh took a job as a psychiatric nursing auxiliary in a mental hospital, on what he describes as "the end-stage ward where the burnt-out cases went to die". There he saw first-hand the devastating effects of lobotomy. "It was painfully apparent to me that there was no proper follow up of these patients at all," he says. "The patients who were the worst, most apathetic, sort of ruined patients were the ones who had been lobectomised."
There he saw first-hand the devastating effects of lobotomy. "It was painfully apparent to me that there was no proper follow up of these patients at all," he says. "The patients who were the worst, most apathetic, sort of ruined patients were the ones who had been lobectomised."
They had all been operated on by McKissock and his assistants.
Later, after Marsh had qualified as a neurosurgeon, a modification of the procedure, known as a limbic leucotomy, was still in use. Marsh describes it as "a sort of microscopic version, much more refined, of the sort of lobectomies people had been carrying out many years earlier".
I didn't like doing them, and I was rather glad to give up the practice fairly shortly after I became a consultant
Henry Marsh
Neurosurgeon
He himself performed this operation on a dozen patients with severe OCD until as recently as 1990.
"They were all suicidal, they had failed all other treatments, so you know I didn't feel particularly anguished about it, but I preferred not to do it," he says.
"I didn't see the patients afterwards, I was purely a technician. I was assured by the psychiatrists involved that the operations were a success."
Image source, Alamy
Image caption,Neurosurgeon Henry Marsh in 2015
I ask him how he feels about these operations now. "I didn't like doing them, and I was rather glad to give up the practice fairly shortly after I became a consultant."
In the early 1960s, about 500 lobotomies were carried out each year in the UK, down from 1,500 at its peak. By the mid-1970s this number had dropped to around 100-150 a year, nearly always involving smaller cuts and more precise targeting.
The introduction of the 1983 Mental Health Act introduced tighter controls and more oversight. Today psychosurgical operations are rarely carried out.
Howard Dully, who was given a lobotomy by Walter Freeman at the age of 12, says he tries to avoid thinking about how different his life might have been if he hadn't had it, for fear that anger would overwhelm him.
To me it's insane. I mean you're talking about a brain. Shouldn't there be some precision involved?
Howard Dully
Child lobotomy patient
"I've tried to piece my life together. It took a long time," he says. "I got into a lot of trouble as a young adult — drugs, and alcohol and criminal activity, trying to steal and make money and make a living. It's very hard to do."
Dully feels that the operation, carried out because he had been clashing with his stepmother, cast a shadow over every aspect of his life.
"You don't walk up to people and say, 'Hi, I had a lobotomy,' because if you do they ain't going to be around you long," he says.
Sixty years on, he can remember the operation in vivid detail.
"They lifted up the eye and went into the corner and tapped it through and wiggled it around with this egg beater thing," he says.
"To me it's insane. I mean you're talking about a brain. Shouldn't there be some precision involved?
This video can not be played
To play this video you need to enable JavaScript in your browser.
 Media caption,
Media caption, Howard Dully on recovery from 'ice-pick' lobotomy
Lobotomy had had its critics from the outset, and the chorus of opposition grew louder as the poor results became apparent.
Walter Freeman, who initially claimed to have a success rate of 85%, was discovered to have a fatality rate of 15%. And when doctors investigated long-term outcomes for his patients they found that just one-third could be regarded as experiencing some improvement, while another third were significantly worse off.
One former advocate for lobotomy in America stated: "Lobotomy was really no more subtle than a gunshot to the head."
Fifteen years ago, a group of doctors and lobotomy victims and their families campaigned to have Egas Moniz stripped of the Nobel Prize for Medicine he won in 1949 for devising lobotomy. But the Nobel Foundation, whose charter states that its awards may not be withdrawn, refused to comply.
Looking back, how should we view the people who carried out this most controversial medical procedure?
"This business of dividing doctors into heroes and villains is wrong. We are all a mix of both, we are a product of our time, of our culture, of our training," says Henry Marsh.
We are all a mix of both, we are a product of our time, of our culture, of our training," says Henry Marsh.
"The generation of surgeons who trained me had, I wouldn't say god-like powers, but they had enormous authority, nobody questioned them or queried them and I can think of some of the people who trained me who were essentially decent people who had been corrupted by this power and became a little bit monstrous as a result."
Follow Claire Prentice on Twitter
You may also be interested in:
Image source, Carol Boyce Heinisch
For years doctors in the US made little attempt to save the lives of premature babies, but there was one place distressed parents could turn for help - a sideshow on Coney Island. Here one man saved thousands of lives, writes Claire Prentice, and eventually changed the course of American medical science.
How one man saved a generation of premature babies
- Mental health
- Long Reads
Facts about the terrible operation - lobotomy
History remembers many barbaric practices in medicine, but lobotomy is the most frightening. Today, this operation can only be seen in the cinema, but in the middle of the last century, you could well be forced to undergo a lobotomy for your wayward character.
Today, this operation can only be seen in the cinema, but in the middle of the last century, you could well be forced to undergo a lobotomy for your wayward character.
Alisa Gorbunova
1. Lobotomy, or leucotomy is an operation in which one of the lobes of the brain is separated from the rest of the areas, or completely excised. It was believed that this practice could treat schizophrenia.
2. The method was developed by the Portuguese neurosurgeon Egas Moniz in 1935, and a trial lobotomy took place in 1936 under his supervision. After the first hundred operations, Moniz observed the patients and made a subjective conclusion about the success of his development: the patients calmed down and became surprisingly submissive.
3. The results of the first 20 operations were as follows: 7 patients recovered, 7 patients showed improvement, and 6 people remained with the same illness. But the lobotomy continued to cause disapproval: many of Moniz's contemporaries wrote that the actual result of such an operation was the degradation of the personality.
But the lobotomy continued to cause disapproval: many of Moniz's contemporaries wrote that the actual result of such an operation was the degradation of the personality.
4. The Nobel Committee considered the lobotomy a discovery that was ahead of its time. Egas Moniz received the Nobel Prize in Physiology and Medicine in 1949. Subsequently, the relatives of some patients requested that the award be canceled, since lobotomy causes irreparable harm to the patient's health and is generally a barbaric practice. But the request was rejected.
5. If Egas Moniz argued that leucotomy is a last resort, then Dr. Walter Freeman considered lobotomy a remedy for all problems, including willfulness and aggressive character. He believed that lobotomy eliminates the emotional component and thereby "improves the behavior" of patients. It was Freeman who introduced the term "lobotomy" in 1945 year. Throughout his life, he operated on about 3,000 people . By the way, this doctor was not a surgeon.
By the way, this doctor was not a surgeon.
6. Freeman once used an ice pick from his kitchen for an operation. Such a “necessity” arose because the previous instrument, the leukote, could not withstand the load and broke in the skull of patient .
7. Subsequently, Freeman realized that ice pick is great for lobotomy. Therefore, the doctor designed a new medical instrument based on this model. The orbitoclast had a pointed end on one side and a handle on the other. A division was applied to the tip to control the depth of penetration.
8. By the middle of the last century lobotomy had become an incredibly popular procedure : it was practiced in Great Britain, in Japan, in the USA and in many European countries. In the United States alone, about 5,000 operations were performed per year.
9. In the USSR, the new method of treatment was used relatively rarely, but it was improved. The Soviet neurosurgeon Boris Grigoryevich Egorov proposed the use of osteoplastic trepanation instead of access through the orbit. Egorov explained that trepanation would allow more precise orientation in determining the area of surgical intervention.
The Soviet neurosurgeon Boris Grigoryevich Egorov proposed the use of osteoplastic trepanation instead of access through the orbit. Egorov explained that trepanation would allow more precise orientation in determining the area of surgical intervention.
10. Lobotomy was practiced in the USSR for 5 years, but was banned at the end of 1950. It is generally accepted that the decision was dictated by ideological considerations , because this method is most widely used in the United States. By the way, in America, lobotomy continued to be practiced until the 70s. However, there is also an opposite point of view: the ban on lobotomy in the USSR was due to the lack of scientific data and the questionable method in general.
"For now, you just need to work with your head, and your brain will become beautiful" - neurosurgeon Alexei Tomsky
In the last century, brain surgery was often perceived as a punitive measure by a totalitarian state against its out-of-the-box thinking citizens.
Head of the Functional Neurosurgery Group of the Federal State Agrarian University of the N.N. N. N. Burdenko Aleksey Alekseevich Tomsky discusses the evolution of domestic neurosurgery, new developments, and why he still prefers a saw to a laser.
How narrow is your specialization?
Quite narrow. There are many different areas in neurosurgery - oncology, vascular surgery, spinal, pediatric, we will not talk about everything, besides, I am not an expert in all these areas, I can say something wrong. I do surgery for neuroleptic extrapyramidal disorders.
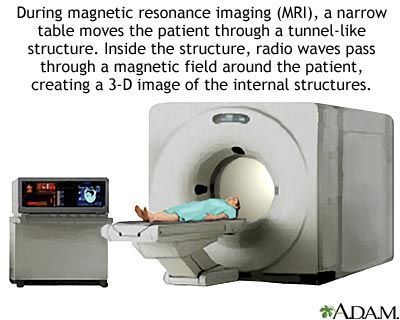
How accurate is magnetic resonance imaging (MRI) today in showing the picture of brain disease?
MRI will not show you any picture of the disease. For example, MRI does not show Parkinson's disease or early dementia at all, the tumor can be seen. But the question immediately arises, what. You need to do verification. Of course, devices are becoming more accurate, and over time, MRI will determine the nature of the tumor. MRI shows plaques in multiple sclerosis, aneurysm, vascular changes, congenital pathologies or spinal stenosis can be seen.
Of course, devices are becoming more accurate, and over time, MRI will determine the nature of the tumor. MRI shows plaques in multiple sclerosis, aneurysm, vascular changes, congenital pathologies or spinal stenosis can be seen.
I understand correctly that neurosurgeons do not make a diagnosis, are you already working with the diagnosis?
There is an emergency neurosurgery, where they bring patients with craniocerebral injuries, they immediately decide what to do with the patient. And so usually the patient already has a diagnosis, and we solve tactical problems.
And how many operations do you do per week?
It depends on different points. In our country, for example, one operation to implant a system for neurostimulation lasts more than six hours, so we will not do many of them in a week. Secondly, they are very expensive and are financed by the city budget, so it also depends on how many quotas we have been allocated for surgical treatment.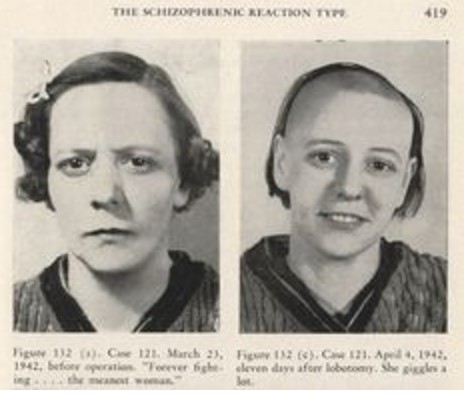 This is a complex multicomponent operation with mathematical calculations, MRI control, a whole team of doctors is working. These operations differ from standard neurosurgical operations, where a simple incision, craniotomy and removal of, for example, a tumor. As there is a pacemaker, so we have - neurostimulator, an electronic device that delivers electrical current to the brain with the given parameters and depending on where it will be implanted. This, in turn, depends on the disease (Parkinson's disease, dystonia, Tourette's syndrome or severe pain neuropathic syndromes).
This is a complex multicomponent operation with mathematical calculations, MRI control, a whole team of doctors is working. These operations differ from standard neurosurgical operations, where a simple incision, craniotomy and removal of, for example, a tumor. As there is a pacemaker, so we have - neurostimulator, an electronic device that delivers electrical current to the brain with the given parameters and depending on where it will be implanted. This, in turn, depends on the disease (Parkinson's disease, dystonia, Tourette's syndrome or severe pain neuropathic syndromes).
When did such technological operations become possible?
They have been carried out in the world for about 50 years, we have - since the 1990s. At first there were domestic systems, then more modern imported ones appeared.
What did they do in the USSR?
Destructive operations - is when certain parts of the brain were destroyed, now, by the way, they are also sometimes performed. The council of doctors decides which ones.
The council of doctors decides which ones.
Like Jack Nicholson's character in One Flew Over the Cuckoo's Nest?
Jack Nicholson's character in this film had a completely different operation - lobotomy. They were done before to correct mental disorders. They were used quite often abroad, in the USSR there was also experience in using them, but then repressions against doctors began, and the USSR Ministry of Health banned these operations. But in Europe and America they continued to make them for a long time.
Do you think it's bad that they banned it?
Of course, bad. This significantly set the country back in the development of this topic. Another thing, when it all started, there were too wide indications for a lobotomy and the methods were different.
Someone turned into a vegetable, and someone experienced a lobotomy and lived normally.
Of course, when surgeons massively performed these operations on everyone, this, of course, was wrong. But Egash Moniz, who first developed the lobotomy technique, and under his leadership the first operations and observations were carried out, at 1949th received the Nobel Prize in Physiology or Medicine.
But Egash Moniz, who first developed the lobotomy technique, and under his leadership the first operations and observations were carried out, at 1949th received the Nobel Prize in Physiology or Medicine.
This is a very fine line… Who decides whether a person needs such an operation or not? She's irreversible.
In the 1940s, when this operation first appeared in America, it was done by everyone: soldiers returning from the war, housewives, even to correct the behavior of children. Psychiatrists and neurosurgeons decided, at that time it was the development of neurosurgery. As far as I know, it has never been done for political reasons. And so ... Imagine a very serious mental patient, he is absolutely inadequate, it is not clear what to expect from him. This operation was a way out, it appeared even before antipsychotics, by the way.
How does this operation help? It simply turns a person into a vegetable…
Someone turned into a vegetable, and someone survived it and lived normally. In America, a book was published by a former patient, Howard Dally, who suffered a lobotomy as a child. It is called - "My Lobotomy". If a person wrote it, then he is far from a vegetable. But, of course, there are many questions and nuances. Today, the approach to this topic, fortunately, is completely different.
In America, a book was published by a former patient, Howard Dally, who suffered a lobotomy as a child. It is called - "My Lobotomy". If a person wrote it, then he is far from a vegetable. But, of course, there are many questions and nuances. Today, the approach to this topic, fortunately, is completely different.
Do similar operations exist? Removal of some part of the brain?
There are a number of diseases, including psychiatric ones, and if patients are resistant to all types of treatment... In Europe and America they do it, but there is a very strict protocol, of course, and there are many ethical issues. Operations are done rarely and according to very strict indications. This issue is always resolved collegially and discussed with relatives.
Don't they ask the person himself?
Well, it's hard to say... It's clear that people with schizophrenia are not operated on, there are drugs for that. But there are disorders such as obsessive-compulsive syndrome (obsessive-compulsive disorder). Howard Hughes, played by Leonardo DiCaprio in the movie The Aviator, had a mild form of this syndrome, but there are very severe obsessive states when a person, for example, washes his hands around the clock - he will have nothing left of his hands. Or, for example, a person always checks whether the front door is closed, and now he closes and opens it all day long. Such conditions interfere with life, they develop and further lead to disability. In such cases, operations are performed, but nothing is removed from patients, but simply a piece of the brain is destroyed or electronic systems are implanted.
Howard Hughes, played by Leonardo DiCaprio in the movie The Aviator, had a mild form of this syndrome, but there are very severe obsessive states when a person, for example, washes his hands around the clock - he will have nothing left of his hands. Or, for example, a person always checks whether the front door is closed, and now he closes and opens it all day long. Such conditions interfere with life, they develop and further lead to disability. In such cases, operations are performed, but nothing is removed from patients, but simply a piece of the brain is destroyed or electronic systems are implanted.
I read somewhere that gambling addiction can be treated in this way.
Oh no. Gambling is just one type of addiction. And dependencies - are not approved readings. It can be corrected with medication, sometimes electroconvulsive therapy was used. Today, such therapy is done only under anesthesia. Previously, it was performed live, and such therapy actually gives a very good result.
Do you still use such a terrible saw in operations? Or have you come up with something else?
Of course, they use a saw, but how to cut? Of course, there are laser techniques, there is an X-ray method, when parts of the brain are irradiated, there are ultrasound technologies that allow you to destroy a small area of the brain without an incision. Well, what's the difference0007 - sawing with a laser or a saw?
There is no sound so disgusting…
(Laughs.) What do dentists drill their teeth with? Why not laser? Why is everyone attached to this laser? The possibilities of the laser are very limited and exaggerated, it cannot do much. The saw is still more convenient, I prefer to work with a saw. Another thing to consider is the cost of the equipment. Lasers and other technologies are very expensive. If their use is expedient and necessary, if the laser will be much safer, then this is one thing, but just indulge .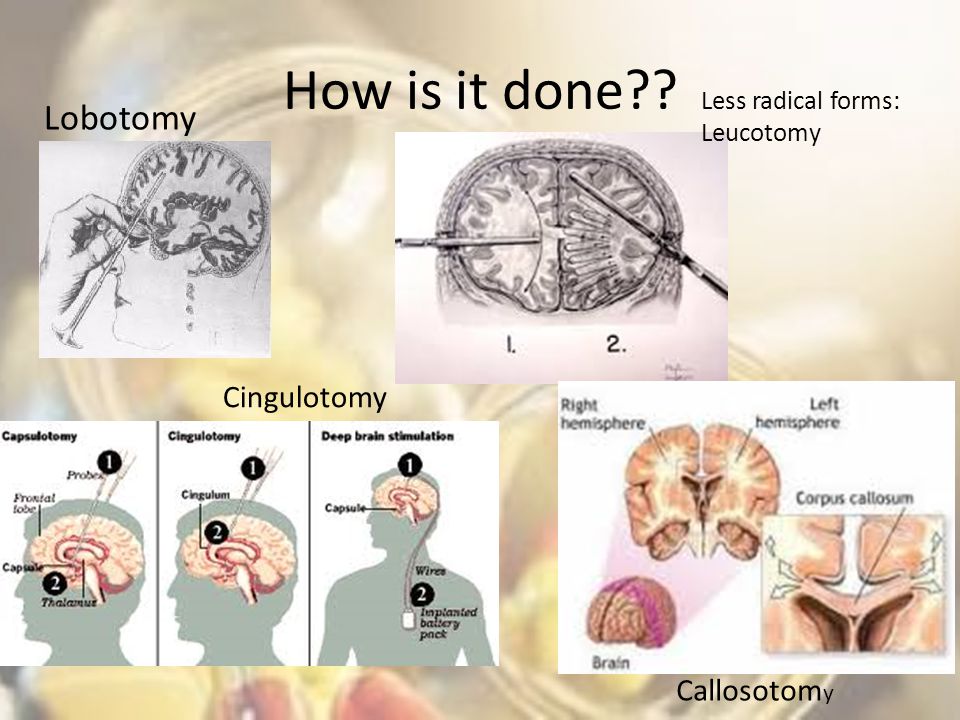 .. and cut what can be done in a simple way - why?
.. and cut what can be done in a simple way - why?
Which operation is considered easy in terms of patient safety, and which is difficult?
Operations on the brain stem are complex. Trunk - is a small structure, vital centers are concentrated there, all this requires special training and special equipment. And the manipulations are more subtle. And a simple one... Sew up the wound on the head after the brick fell on the head.
Can the brain be sewn up?
The brain is not sutured. If a piece of the brain has died, then it cannot be replaced or sewn up. If there is an open wound on the head, it is treated so that there is no inflammation, and it is sewn up ... If, for example, a damaged part of the brain can lead to infection or disability, if it is aggressive, then it can be removed. If he just died, then no one does anything with him, they just leave him.
Some South American neurosurgeon was going to transplant a whole head of one Russian patient, and he was ready.

The brain is not replaced. You can restore the integrity of the layers of the skin, shell, bone. There is very little that can be done with the brain, it does not like to be interfered with in its life and work. This is an integral system, the most conservative part of the body, one might say.
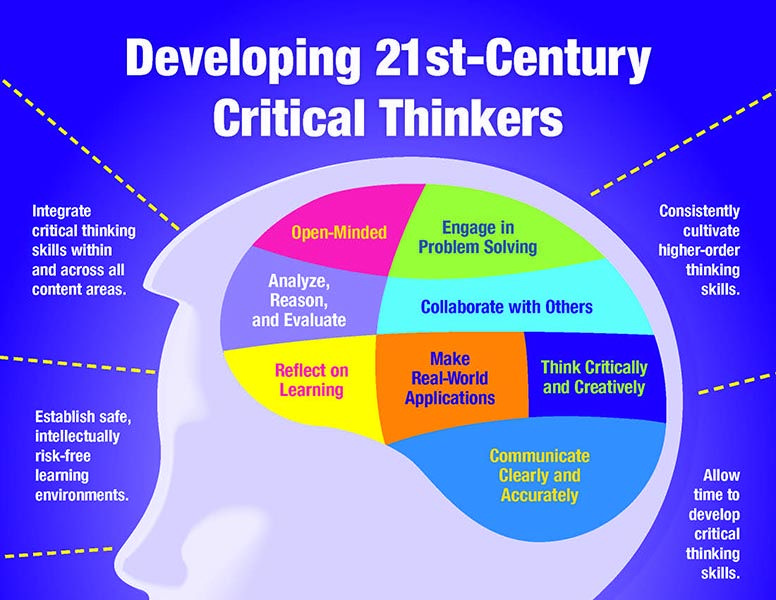
And if a person wants to improve his memory, increase IQ , he is healthy, but wants to improve, can this be solved with the help of neurosurgery? In a word, is brain plastic surgery possible? I think people will come to this.
We'll be waiting. In the meantime, you just need to work with your head, and your brain will become beautiful. You can learn foreign languages. No, surgeons don't do that yet. Uploading the contents of a book into the brain is not yet possible, you can only develop it from within. The brain is not yet grown and transplanted in test tubes, but perhaps something like this will happen later.
Why is a brain transplant still impossible?
This is a complex mechanism that is very sensitive to hypoxia, it will simply die during transplantation. Well, brain - is a personality, a soul, how can you transplant it? Today there are no methods to do this, even a small part of the brain cannot be transplanted. Some neurosurgeon from South America was going to transplant the whole head of one Russian patient, and he was already ready, he was diagnosed with cerebral palsy. But while this story did not end with anything, they abandoned this idea. Although head transplants were performed on dogs... Nothing good ended there either.
Yes, we remember Sharikov... It's just that we're already used to transplanting the liver, kidneys and heart.
Well, they're just organs. And the brain works with the help of multi-million connections, and it is not yet possible to somehow legalize them, transplant even a very similar piece. There are a lot of patients with disorders and injuries of the spinal cord, and the spinal cord is a more primitive structure. But today no one can put it all together to make it work. The nerve must sprout, and it grows very slowly.
There are a lot of patients with disorders and injuries of the spinal cord, and the spinal cord is a more primitive structure. But today no one can put it all together to make it work. The nerve must sprout, and it grows very slowly.
What can be considered a breakthrough in neurosurgery over the past ten years?
Neurosurgery is developing very rapidly, first of all, it is new equipment that is constantly being improved. For example, a navigation system that allows you to find a small area in the brain, accurately approach it and not get lost in your head. These are very important developments.
There are neurosurgical robots that allow implantation into a deep point of the brain. In this case, it is not necessary to cut the entire head, but it is enough to make a small trajectory without damaging the brain. This is one of the trends in neurosurgery - in situations where possible, to minimize injury. For this, endoscopes, stereotaxic technologies, a lot of MRI studies are used, which allow you to build a picture of the brain and bypass vital areas in order to approach the right place more sparingly.
There are virtual models of the brain. They are not yet made for each patient, they are based on MRI, they can be modeled like on a computer, only in 3D. A lot of work is being done on the genetics of tumors. Computer programming is actively developing. For example, we implant a system for neurostimulation to a patient, there are developments that allow us to understand what kind of field is formed around this electrode, and what effect it can potentially have. For example, we set a picture where we have an electrode in the brain, and the program calculates what will happen, with what degree of probability and what will be the result, depending on the electric field that we intend to set. So far, such programs exist at the level of experimental developments, but if they are confirmed in reality, this will greatly facilitate our work.
What do you think are the trends in the future? The future of implantation?
I think so. There is a lot of work in the field of exoskeletons, but so far everything is experimental. Imagine a person who cannot move his arms or legs. He is implanted with a chip, his hand is on the table, it is connected to him, and he controls it. He can still perform simple manipulations, but the first attempts are already possible. In Russia, unfortunately, such work is not carried out at all, this requires serious laboratories and funding. We have a number of institutions that are very successful in prosthetics.
Imagine a person who cannot move his arms or legs. He is implanted with a chip, his hand is on the table, it is connected to him, and he controls it. He can still perform simple manipulations, but the first attempts are already possible. In Russia, unfortunately, such work is not carried out at all, this requires serious laboratories and funding. We have a number of institutions that are very successful in prosthetics.
What do we ourselves need to do to influence the anatomical structure of our brain?
Any learning - is the accumulation of neural connections. The more you rehearse in any area, the faster you will do it. But anatomically, the brain does not change in any way, the player's brain will look like any other. Although there are anatomical features. What is a genius? Who is it? This is a person with the anatomical features of the brain, which converged in some direction, and something is realized in him much better than in other people.