How long for latuda to work
How fast does Latuda work?
Medically reviewed by Leigh Ann Anderson, PharmD. Last updated on July 11, 2022.
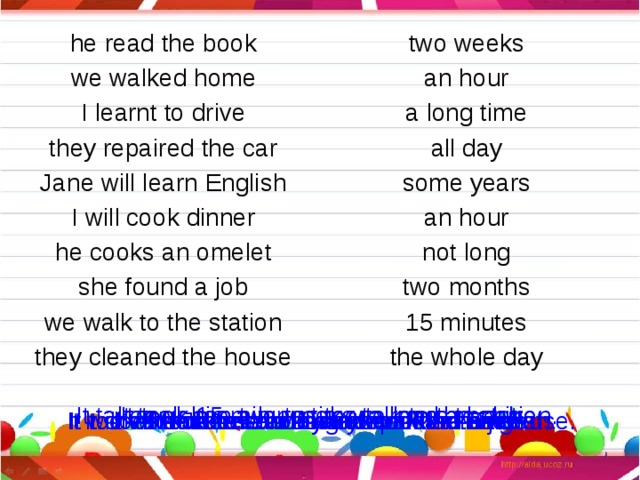
Latuda (generic name: lurasidone) works in most patients within 6 weeks or sooner at an appropriate dose, although results can vary between patients. Latuda is an atypical antipsychotic approved for patients with schizophrenia or bipolar depression. Some patients may respond as early as 1 to 3 weeks; however, some patients may not respond at all or have side effects that interrupt treatment.
It is important that you take your Latuda with food that contains at least 350 calories. Taking Latuda with food will greatly help to increase the absorption of the medicine into your body. Better absorption can increase the effectiveness of Latuda.
In randomized, placebo-controlled clinical studies conducted by the manufacturer in patients with either schizophrenia or bipolar depression, significant results of the primary endpoint were seen at 6 weeks in various age groups.
Latuda is approved in the U.S. for the treatment of:
- Schizophrenia in adults and adolescents (13 to 17 years)
- Bipolar depression (depressive episode associated with bipolar I disorder) in adults and children (10 to 17 years) as monotherapy (used alone)
- Bipolar depression in adults when used in combination with lithium or valproate.
The effectiveness of Latuda for longer than 6 weeks has not been evaluated in controlled clinical studies. However, your doctor will periodically reevaluate your response to the long-term use of Latuda if you remain on treatment for longer than 6 weeks.
Schizophrenia
Latuda is an oral prescription medicine that is given once a day. It can help keep the symptoms of schizophrenia under control in people 13 years of age or older.
Latuda was evaluated in many studies of adults living with schizophrenia and in one study of adolescents 13–17 years of age. These studies looked at how well Latuda works, how safe it is, and how well people tolerated it.
- In adult patients with schizophrenia, Latuda was shown to be safe and effective. In the trials, patients treated with Latuda had fewer symptoms of schizophrenia than those taking an inactive pill (placebo) at the end of the 6-week studies. Some patients saw significant results as early as the first week.
- In adolescent patients with schizophrenia, one study showed that Latuda was associated with improvements in symptoms of schizophrenia compared to a placebo (inactive) treatment at the end of 6 weeks. However, some patients did show significant reduction in symptoms as early as the first week.
Bipolar depression (depressive episode associated with bipolar I disorder)
Latuda has been studied in 6-week studies in adult patients with bipolar depression using it as monotherapy (used alone) or in combination with other agents such as lithium or valproate.
- A significant reduction in adult symptoms was seen at 6 weeks. Some patients had an effect as early as the second week when looking at the monotherapy study (Latuda used alone).
 A 44% greater reduction in bipolar depressive symptoms was seen at week 6 with Latuda when compared to an inactive treatment.
A 44% greater reduction in bipolar depressive symptoms was seen at week 6 with Latuda when compared to an inactive treatment. - In the combination studies with lithium or valproate, a significant reduction in symptoms was seen as early as 3 weeks for some patients. A 27% greater reduction in depressive symptoms was seen with Latuda at week 6 when compared to treatment with lithium or valproate treatment plus an inactive treatment.
In children and adolescents 10 to 17 years of age with bipolar depression, Latuda was associated with statistically significant and clinically meaningful improvement in bipolar depression symptoms compared to placebo in 6-week studies.
- Some patients experienced a significant reduction in symptoms by week 2 of the study.
- A 37% greater reduction in depressive symptoms was seen at week 6 with Latuda when compared to an inactive treatment.
To learn more about Latuda dosing in adults and children, visit: Latuda Dosing
Bottom Line
- Latuda is an atypical antipsychotic approved in the U.
 S. for patients with schizophrenia or bipolar depression. In many clinical studies, symptoms were found to have improved by 6 weeks of treatment, but some patients saw earlier results.
S. for patients with schizophrenia or bipolar depression. In many clinical studies, symptoms were found to have improved by 6 weeks of treatment, but some patients saw earlier results. - Patients with schizophrenia receiving Latuda may begin to see improvements in their symptoms as early as the first week of treatment; however, studies evaluated full effects at 6 weeks.
- In patients with bipolar depression, significant treatment results with Latuda may start as soon as the second or third week of treatment in some patients. These studies also evaluated overall results at 6 weeks.
- Some patients may not have an adequate response to treatment with Latuda, or may need to stop treatment due to side effects.
This is not all the information you need to know about Latuda for safe and effective use. Review the full Latuda prescribing information here, and discuss this information with your doctor or other health care provider.
References- Latuda (lurasidone) [prescribing information].
 Sunovion Pharmaceuticals Inc. December 2019. Accessed July 20, 2020 at https://www.latuda.com/LatudaPrescribingInformation.pdf
Sunovion Pharmaceuticals Inc. December 2019. Accessed July 20, 2020 at https://www.latuda.com/LatudaPrescribingInformation.pdf - Loebel A, Cucchiaro J, Silva S, et al. Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. 2013;171(2):160-168.
- DelBello MP, Goldman R, Phillips D, et al. Efficacy and safety of lurasidone in children and adolescents with bipolar I depression: a double-blind, placebo-controlled study. J Am Acad Child Adolesc Psychiatry. 2017;56(12):1015-1025.
- Loebel A, Cucchiaro J, Silva S, et al. Lurasidone as adjunctive therapy with lithium or valproate for the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. 2013;171(2):169-177.
- Meltzer HY, Cucchiaro J, Silva R, et al. Lurasidone in the treatment of schizophrenia: a randomized, double-blind, placebo- and olanzapine-controlled study.
 Am J Psychiatry. 2011;168:957-967.
Am J Psychiatry. 2011;168:957-967. - Goldman R, Loebel A, Cucchiaro J, Deng L, Findling RL. Efficacy and safety of lurasidone in adolescents with schizophrenia: a 6-week, randomized placebo-controlled study. J Child Adolesc Psychopharmacol. 2017;27:1-10.
Related medical questions
- Can you drink alcohol on Latuda?
- Why do you have to avoid grapefruit when taking Latuda?
- Does Latuda increase prolactin levels?
- Why do you need to take Latuda with food?
- Can you stop taking Latuda immediately?
- Does Latuda make you sleepy?
- Is Latuda a mood stabilizer or an antipsychotic?
- Does Latuda cause weight gain?
- Can Latuda be cut in half or split?
- Is Latuda a controlled substance?
- Klonopin vs Xanax - How are they different?
Drug information
- Latuda
- Lurasidone
Related support groups
- Latuda (68 questions, 326 members)
- Lurasidone (8 questions, 16 members)
- Bipolar Disorder (463 questions, 3,116 members)
- Schizophrenia (84 questions, 314 members)
Medical Disclaimer
Lurasidone (Latuda) | NAMI: National Alliance on Mental Illness
Download PDF
Generic name: Lurasidone (loo RAS I done)
Brand name: Latuda®
- Oral tablet: 20 mg, 40 mg, 60 mg, 80 mg, 120 mg
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
Please review before taking this medication.
What is lurasidone and what does it treat?
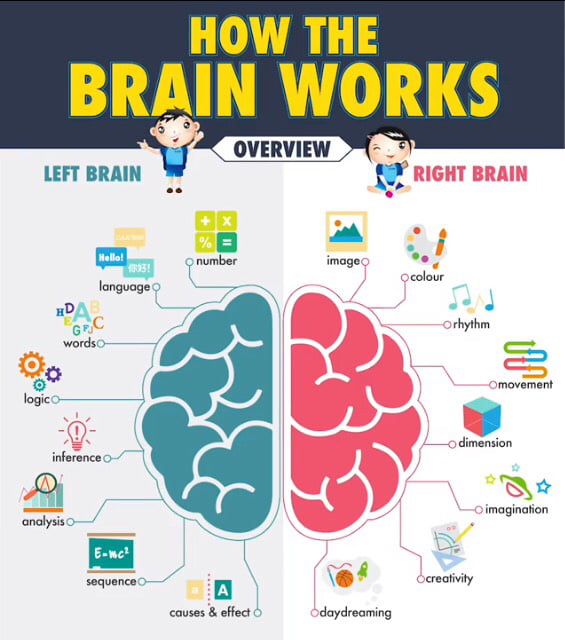
Lurasidone is a medication that works in the brain to treat schizophrenia. It is also known as a second generation antipsychotic (SGA) or atypical antipsychotic. Lurasidone rebalances dopamine and serotonin to improve thinking, mood, and behavior.
Symptoms of schizophrenia include:
- Hallucinations – imagined voices or images that seem real
- Delusions - beliefs that are not true (e.g., other people are reading your thoughts)
- Disorganized thinking or trouble organizing your thoughts and making sense
- Little desire to be around other people
- Trouble speaking clearly
- Lack of motivation
Lurasidone may help some or all of these symptoms.
Lurasidone is also FDA approved for the treatment of depressive phases of bipolar disorder.
This medication sheet will focus primarily on schizophrenia. You can find more information about bipolar disorder here.
Lurasidone may also be helpful when prescribed “off-label” for major depressive disorder or other mental health conditions. “Off-label” means that it has not been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending an “off-label” treatment. They should be clear about the limits of the research around that medication and if there are any other options.
What is the most important information I should know about lurasidone?
Schizophrenia requires long-term treatment. Do not stop taking lurasidone, even when you feel better.
With input from you, your health care provider will assess how long you will need to take the medication.
Missing doses of lurasidone may increase your risk for a relapse in your symptoms.
Do not stop taking lurasidone or change your dose without talking with your health care provider first.
For lurasidone to work properly, it should be taken every day as ordered by your health care provider.
Are there specific concerns about lurasidone and pregnancy?
If you are planning on becoming pregnant, notify your health care provider to best manage your medications. People living with schizophrenia who wish to become pregnant face important decisions. This is a complex decision since untreated schizophrenia has risks to the fetus, as well as the mother. It is important to discuss the risks and benefits of treatment with your doctor and caregivers.
Antipsychotic use during the third trimester of pregnancy has a risk for abnormal muscle movements (extrapyramidal symptoms [EPS]) and/or withdrawal symptoms in newborns following delivery. Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.
Caution is advised with breastfeeding since it is not known if lurasidone passes into breast milk.
What should I discuss with my health care provider before taking lurasidone?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you ever had muscle stiffness, shaking, tardive dyskinesia, neuroleptic malignant syndrome, or weight gain caused by a medication
- If you experience side effects from your medications, discuss them with your provider.
 Some side effects may pass with time, but others may require changes in the medication.
Some side effects may pass with time, but others may require changes in the medication. - Any psychiatric or medical problems you have, such as heart rhythm problems, long QT syndrome, heart attacks, diabetes, high cholesterol, or seizures
- If you have a family history of diabetes or heart disease
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment. Your provider can explain how these different treatments work with the medication.
- If you are pregnant, plan to become pregnant, or are breastfeeding
- If you smoke, drink alcohol, or use illegal drugs
How should I take lurasidone?
Lurasidone is usually taken 1 time per day with food (at least 350 calories).
Typically patients begin at a low dose of medication and the dose is increased slowly over several weeks.
For schizophrenia, the dose usually ranges from 40 mg to 160 mg. Only your health care provider can determine the correct dose for you.
For acute treatment of depressive episodes of bipolar disorder (when used alone or with lithium or valproate), the dose usually ranges from 20 mg to 120 mg. Only your health care provider can determine the correct dose for you.
Use a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member or a friend to remind you or check in with you to be sure you are taking your medication.
What happens if I miss a dose of lurasidone?
If you miss a dose of lurasidone, take it as soon as you remember, unless it is closer to the time of your next dose. Discuss this with your health care provider. Do not double your next dose or take more than what is prescribed.
What should I avoid while taking lurasidone?
Avoid drinking alcohol or using illegal drugs while you are taking lurasidone. They may decrease the benefits (e.g., worsen your confusion) and increase adverse effects (e.g., sedation) of the medication.
They may decrease the benefits (e.g., worsen your confusion) and increase adverse effects (e.g., sedation) of the medication.
What happens if I overdose with lurasidone?
If an overdose occurs call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of lurasidone does not exist.
What are the possible side effects of lurasidone?
Common side effects
Extrapyramidal symptoms, drowsiness, restlessness, insomnia, increased glucose, cholesterol abnormalities, nausea
Rare/serious side effects
Lurasidone may increase the blood levels of a hormone called prolactin. Side effects of increased prolactin levels include females losing their period, production of breast milk and males losing their sex drive or possibly experiencing erectile problems. Long term (months or years) of elevated prolactin can lead to osteoporosis, or increased risk of bone fractures.
Some people may develop muscle related side effects while taking lurasidone. The technical terms for these are “extrapyramidal symptoms” (EPS) and “tardive dyskinesia” (TD). Symptoms of EPS include restlessness, tremor, and stiffness. TD symptoms include slow or jerky movements that one cannot control, often starting in the mouth with tongue rolling or chewing movements.
Temperature regulation: Impaired core body temperature regulation may occur; caution with strenuous exercise, heat exposure, and dehydration.
Second generation antipsychotics (SGAs) increase the risk of weight gain, high blood sugar, and high cholesterol. This is also known as metabolic syndrome. Your health care provider may ask you for a blood sample to check your cholesterol, blood sugar, and hemoglobin A1c (a measure of blood sugar over time) while you take this medication.
- Information on healthy eating and adding exercise to decrease your chances of developing metabolic syndrome may be found at the following sites:
- https://www.
 helpguide.org/articles/healthy-eating/healthy-eating.htm
helpguide.org/articles/healthy-eating/healthy-eating.htm - http://www.helpguide.org/home-pages/exercise-fitness.htm
- https://www.
SGAs have been linked with higher risk of death, strokes, and transient ischemic attacks (TIAs) in elderly people with behavior problems due to dementia.
All antipsychotics have been associated with the risk of sudden cardiac death due to an arrhythmia (irregular heart beat). To minimize this risk, antipsychotic medications should be used in the smallest effective dose when the benefits outweigh the risks. Your doctor may order an EKG to monitor for irregular heartbeat.
Neuroleptic malignant syndrome is a rare, life threatening adverse effect of antipsychotics which occurs in <1% of patients. Symptoms include confusion, fever, extreme muscle stiffness, and sweating. If any of these symptoms occur, contact your health care provider immediately.
All antipsychotics can cause sedation, dizziness, or orthostatic hypotension (a drop in blood pressure when standing up from sitting or lying down). These side effects may lead to falls which could cause bone fractures or other injuries. This risk is higher for people with conditions or other medications that could worsen these effects. If falls or any of these symptoms occur, contact your health care provider.
These side effects may lead to falls which could cause bone fractures or other injuries. This risk is higher for people with conditions or other medications that could worsen these effects. If falls or any of these symptoms occur, contact your health care provider.
Are there any risks for taking lurasidone for long periods of time?
Tardive dyskinesia (TD) is a side effect that develops with prolonged use of antipsychotics. Medications such as lurasidone have been shown to have a lower risk of TD compared to older antipsychotics, such as Haldol® (haloperidol). If you develop symptoms of TD, such as grimacing, sucking, and smacking of lips, or other movements that you cannot control, contact your health care provider immediately. All patients taking either first or second generation antipsychotics should have an Abnormal Involuntary Movement Scale (AIMS) completed regularly by their health care provider to monitor for TD.
Second generation antipsychotics (SGAs) increase the risk of diabetes, weight gain, high cholesterol, and high triglycerides. (See “Serious Side Effects” section for monitoring recommendations).
(See “Serious Side Effects” section for monitoring recommendations).
What other medications may interact with lurasidone?
The following medications may increase the levels and effects of lurasidone: diltiazem (Cardizem®), erythromycin (Ery-Tab®), and fluconazole (Diflucan®). Grapefruit juice may also increase levels of lurasidone.
The following medications may decrease the levels and effects of lurasidone: carbamazepine (Tegretol®) and phenobarbital.
How long does it take for lurasidone to work?
It is very important to tell your doctor how you feel things are going during the first few weeks after you start taking lurasidone. It will probably take several weeks to see big enough changes in your symptoms to decide if lurasidone is the right medication for you.
Antipsychotic treatment is generally needed lifelong for persons with schizophrenia. Your doctor can best discuss the duration of treatment you need based on your symptoms and illness.
- Hallucinations, disorganized thinking, and delusions may improve in the first 1-2 weeks
- Sometimes these symptoms do not completely go away
- Motivation and desire to be around other people can take at least 1-2 weeks to improve
- Symptoms continue to get better the longer you take lurasidone
- It may take 2-3 months before you get the full benefit of lurasidone
Summary of FDA Black Box Warnings
Increased Mortality in Elderly Patients with Dementia Related Psychosis
- Both first generation (typical) and second generation (atypical) antipsychotics are associated with an increased risk of mortality in elderly patients when used for dementia related psychosis.
- Although there were multiple causes of death in studies, most deaths appeared to be due to cardiovascular causes (e.g., sudden cardiac death) or infection (e.g., pneumonia).
- Antipsychotics are not indicated for the treatment of dementia-related psychosis.
Suicidal Thoughts or Actions in Children and Adults
- Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide.
- Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking medications. This risk may persist until significant remission occurs.
- Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional.
- All patients being treated with this medication for depression should watch for and notify their health care provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment
Provided by
(January 2023)
©2022 The American Association of Psychiatric Pharmacists (AAPP) and the National Alliance on Mental Illness (NAMI). AAPP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
AAPP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the American Association of Psychiatric Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The American Association of Psychiatric Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
which ones can be broken and which ones can’t and why, how to properly divide pills in half and into parts
Daniil Davydov
medical journalist
Author’s profile
This is true, but there are nuances.
There are several groups of tablets that must not be divided. Other pills can be divided - but it is important to do it correctly.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What you need to know about tablets
Like all other forms of medicine, tablets consist of a carefully measured dose of an active ingredient that has a biological effect on the body, and excipients that give the drug volume.
What Drugs Are Made of - Bulletin of the Australian Department of Health
What are Drug Delivery Systems - Bulletin of the National Institute for Biomedical Imaging and Bioengineering
Excipients are not only dyes, flavors, sweeteners and stabilizers that protect the drug from oxidation and degradation, but also drug delivery vehicles that allow you to control the properties of the drug.
Delivery systems are either incorporated into the tablet itself or the contents of the capsule, or form its shell. They determine exactly where the tablet will dissolve - in the stomach or in the intestines, and the speed with which it will do it. The delivery method used in a particular tablet or capsule determines whether it can be divided into parts or not.
What pills that can be divided look like
All pills can be roughly divided into two groups: those that can be divided without loss of effectiveness, and those that, after division, become less effective or even dangerous. Sometimes they can be distinguished by their appearance, but you should not count on it.
What to consider when splitting pills - British Ministry of Health Bulletin
What pills that can be split should look like - FDAPDF guidelines, 55.6 KB
For example, the US Food and Drug Administration (FDA) recommends that drug companies leave tips for patients. Tablets that can be divided, the department advises making flattened and notching them to make it easier to gently break them in half.
However, no one requires strict compliance with these rules from drug manufacturers either in our country or abroad. Therefore, in the pharmacy you can find tablets with notches that are not worth dividing, and tablets without notches that can be divided.
Tablets that can be divided, usually white, most often uncoated and scored. Source: Triff / ShutterstockWhich pills can not be divided
In order not to get confused, it makes sense to focus not on the appearance of the pill, but on the instructions. There are only two types of tablets and capsules that most pharmacological experts advise against separating.
Enteric-coated tablets and capsules . This is a shell that does not allow the tablet to dissolve in the stomach, so the drug is absorbed only in the intestines. Such coverage:
- Protects drugs that become unstable in acidic gastric juices. These are, for example, the antibiotic erythromycin and the digestive enzyme pancreatin.
 If you divide the pills from this group into parts, they will either work weaker than they should, or they will not work at all.
If you divide the pills from this group into parts, they will either work weaker than they should, or they will not work at all. - Protects drugs working in the stomach from premature activation. For example, proton pump inhibitors like omeprazole, pantoprazole, and esomeprazole are activated in an acidic environment. But for some people with digestive disorders, acidic stomach juices can get into the mouth or into the esophagus. The coating prevents the drugs from "turning on" in the mouth or esophagus, where they are of no use. If it is destroyed, the medicine will work worse.
- Protects the stomach from the harmful effects of the drug.
Examples of Pills Not to be Divided - New Zealand Guidelines for Older PatientsPDF, 301KB
What is Enteric Coating - An International Textbook for Drug Manufacturers
Things to Know When Prescribing a Proton Pump Inhibitor - British Medical Journal
Peptic Ulcers and Non Steroids Anti-Inflammatory Drugs - Australian Prescription Medicines Magazine
These are primarily non-steroidal anti-inflammatory drugs that damage the gastric mucosa when taken regularly. Some of these drugs, such as aspirin, are enteric-coated to dissolve in the intestines. If you split the pill, the aspirin will still work, but the coating will no longer protect the stomach. After taking a divided tablet, you may experience the same side effects as when taking uncoated aspirin, i.e. nausea or heartburn.
Some of these drugs, such as aspirin, are enteric-coated to dissolve in the intestines. If you split the pill, the aspirin will still work, but the coating will no longer protect the stomach. After taking a divided tablet, you may experience the same side effects as when taking uncoated aspirin, i.e. nausea or heartburn.
According to the Russian pharmacological standard, in the instructions for the drug in the "Dose form" section, the manufacturer must write that the tablet or capsule is coated with a shell that prevents the drug from dissolving in the stomach. Typically, manufacturers write that tablets or capsules are enteric-coated or enteric-coated.
/fuflomizin-ili-net/
Do you know which drugs are not worth spending money on?
The hint can also be encrypted in the appearance of the drug. As a rule, such tablets are round or oval in shape, without notches, with a gleaming shell of white, orange, yellow or red. Both capsules and tablets can have letters and numbers.
Modified release tablets. Medicines have different characteristics of action. This means that the active ingredient from different tablets can be released:
- immediately - the tablets begin to act as soon as they dissolve;
- extended release - tablets dissolve gradually, gradually releasing the active ingredient. As a result, such a drug lasts longer than an immediate release drug;
- slow - the tablets begin to dissolve after a specified time after the person has drunk them, and then they work as prolonged medicines. That is, a person can take a pill at night so that it starts working in the morning, even before he wakes up, and works until the evening.
What are the characteristics of the action of drugs - the national standard of the Russian Federation GOST R ISO 11239-2014
Another drug may have a modified effect. For example, the first dose of a drug may be released immediately, while the second dose may be released after some time.
All tablets, except those from which the active ingredient is released immediately, are called modified release drugs. If you divide such medicines into parts, all their advantages are lost.
For example, the prolonged form of ibuprofen "Brufen SR" works up to 24 hours. If you split this pill, it will work like regular ibuprofen immediate release. And since the concentration of the active substance in preparations with prolonged and delayed action is usually higher than in immediate-release preparations, the risk of overdose arises even if you take half a tablet.
What can the splitting of a pill with modified action lead to - French scientific journal "Recipe"
In the instructions for the drug in the section "Dosage form" the manufacturer is obliged to indicate the characteristics of the drug. For example, in the instructions for "Brufen SR" it is written that these are prolonged release tablets.
Modified-release drugs are similar in appearance to enteric tablets - they are also usually round or oval, without notches, with shiny multi-colored shells.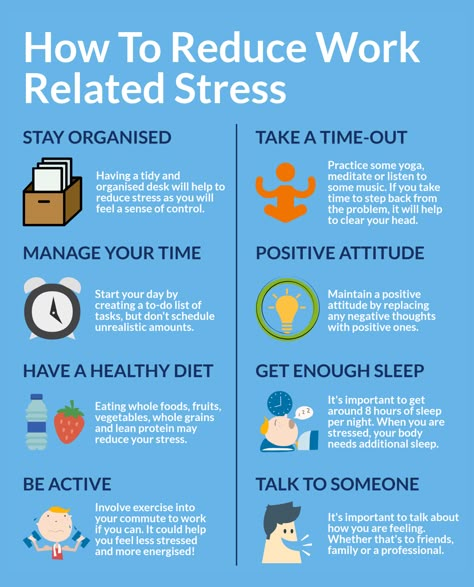
Which tablets can be divided
If the characteristic of action is not indicated in the "Dose form" section, this is not a modified release drug. Even if it says that these are film-coated tablets, such tablets can still be divided into parts. But it is important to consider that there are several important nuances in the separation of tablets.
Not all tablets are easy to split exactly in half. This is the reason doctors all over the world don't like it too much when patients share medicines. After all, if the contents of the capsule wake up or the tablet breaks unevenly, there is a risk that the patient will receive either too high or too low a dose of the drug.
Why splitting pills isn't a good idea - Bulletin on the international site for pharmacists
Or, a person may forget that the pill had to be split and take a double dose. To avoid this, those who can afford it are advised to buy tablets and capsules immediately in the dosage prescribed by the doctor.
Separation of some tablets produces caustic powder. Tablet is a compressed powder intended for oral administration. Chemotherapy drugs, antibiotics, and hormone pills break down into a corrosive powder. If it gets on hands or eyes, it can cause irritation. At the same time, separation does not affect the medicinal properties of these drugs.
Why Hormones, Steroids, Antibiotics and Cytostatics Should Not Be Divided - Greater Manchester Medicines Management Group Clinical GuidelinesPDF, 302KB
Sugar or film-coated tablets will become unpalatable. For example, the prescription drug Midantan, which is used to treat Parkinson's disease, becomes bitter after separation. But separation does not affect its effectiveness.
How to divide tablets correctly
There are situations when you cannot do without dividing a tablet. For example, some patients may require the antidepressant Mirtazapine at a dosage that is less than the standard minimum dose.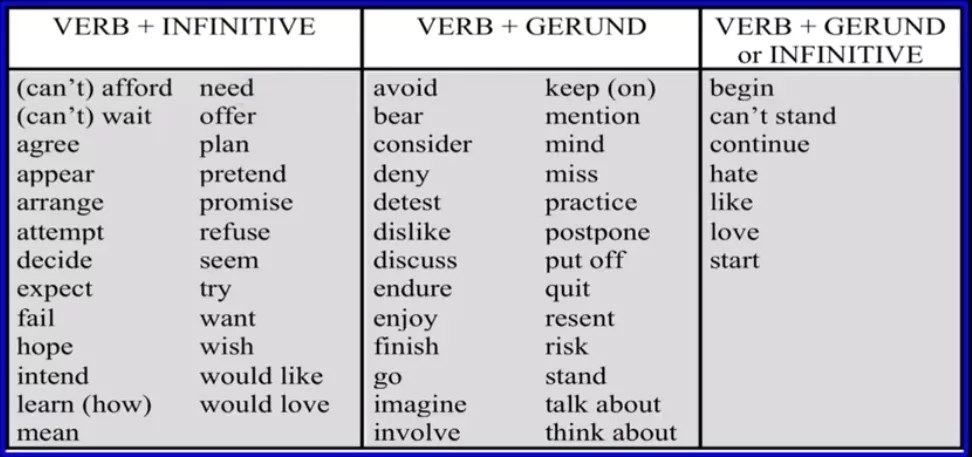 And if the medicine is expensive and needs to be taken for a long time, some patients may decide to save money.
And if the medicine is expensive and needs to be taken for a long time, some patients may decide to save money.
In this situation, you need to follow the rules for the safe separation of tablets:
- Make sure that the tablet is not intended to dissolve in the intestines and does not belong to modified release drugs. This information should be in the instructions, in the "Dosage Form" section. If you still have doubts, it makes sense to consult with the doctor who prescribed the medicine.
- Do not divide the entire supply of tablets at one time. Divided tablets have a shorter shelf life because whole shells protect them from dampness, oxidation and damage. Before splitting a new pill, you should make sure that there is not a half left from the last time.
- Some tablets are very difficult to separate because they are too hard or crumble. If this medicine is to be taken for a long time, it makes sense to purchase a separator - a guillotine for tablets, which neatly divides them into two parts.
 Guillotines work well even with tablets without notches.
Guillotines work well even with tablets without notches.
Rules for Safe Separation of Tablets - FDA Bulletin
Latuda Side Effects and How to Avoid Them | SingleCare - Product Information
Home >> Product Information >> Side effects of Latuda and how to avoid them
Information about the drug
Side effects of Latuda | Weight gain | Conclusion | How long do side effects last? | Warnings | Interactions | How to avoid side effects
Latuda (active ingredient: lurasidone hydrochloride) is a branded atypical antipsychotic approved for the treatment of schizophrenia in adolescents and adults and for the treatment of depression in adults and children 10 years of age and older diagnosed with bipolar disorder. It can also be combined with lithium or valproate to treat bipolar depression in adults. Lurasidone, the active ingredient in Latuda, affects the activity of dopamine and serotonin, chemicals that help transmit signals between nerves. Like all drugs that change brain chemistry, Latuda can cause side effects, make certain conditions worse, and interact with other drugs.
Like all drugs that change brain chemistry, Latuda can cause side effects, make certain conditions worse, and interact with other drugs.
RELATED: Find out more about Latuda | Get Discounts Latuda
Common Side Effects Latuda
Like all medicines, Latuda may cause minor or temporary side effects. More than 1 in 20 people will experience side effects such as drowsiness, nausea, restlessness, indigestion, or involuntary movements.
In patients taking Latuda, the most common side effects are:
- Nausea
- Acatisia (insurmountable desire to move)
- Extrapyramidal symptoms (tremor, tremors, involuntary movements, salivation)
- Difficulties in movement or slow movements
- Dreamy
- Sucle
- Diarrhea
- Upset stomach
- Vomiting
- Anxiety
- Agitation
- Nasal congestion
- Blurred vision
Many side effects are dose proportional - the higher the dose, the greater the risk and severity of minor side effects. Seek medical attention if you experience any minor side effects while taking Latuda.
Seek medical attention if you experience any minor side effects while taking Latuda.
Serious side effects Latuda
All antipsychotics can cause serious and long-term side effects. Serious side effects of Latuda include:
- Metabolic changes leading to high blood sugar, high triglycerides, high cholesterol, low blood sodium, or diabetes.
- hyperthermia
- Excess prolactin
- decrease in leukocytes
- Problems with swallowing
- neuroleptic malignant syndrome
- Late dyskinesia
- Mania
- Suicidal thoughts and behavior
- cramps
- Stroke
- Death
Like other antipsychotics, Latuda can cause metabolic changes and weight gain, although this is less likely and less pronounced than with similar drugs. Latuda may not be an appropriate drug for people with a family history of diabetes or metabolic syndrome.
All antipsychotics interfere with the body's ability to regulate body temperature. As a result, people taking Latuda are at an increased risk of heat stroke (hyperthermia), a potentially life-threatening health condition. Care must be taken to avoid hot weather or overexertion while taking Latuda.
As a result, people taking Latuda are at an increased risk of heat stroke (hyperthermia), a potentially life-threatening health condition. Care must be taken to avoid hot weather or overexertion while taking Latuda.
Latuda increases the risk of suicidal thoughts and behavior in children, adolescents, and young adults treated for bipolar depression. When prescribing Latuda from depression, it is important to monitor the signs of suicidality, including:
- Suicidal thoughts or comments
- Suicide attempts
- Changes in mood
- Anger, irritability or aggression
- Determining depress
- Painting
- Pranic0003
Finally, Latuda increases the risk of stroke and death in patients over 65 with dementia-related psychosis. For this reason, Latuda is not approved for the treatment of psychosis associated with dementia.
Weight Gain Latuda
Antipsychotic drugs usually cause metabolic changes and weight gain as unwanted side effects, but the degree of weight gain depends on the drug.
 However, according to the same clinical trial listed above, Latuda scores low, resulting in an average weight gain of about one pound in the short term and about two pounds in the long term (one year). About 4.8% of patients in this study gained more than 7% of their body weight compared to about 3.3% who took placebo.
However, according to the same clinical trial listed above, Latuda scores low, resulting in an average weight gain of about one pound in the short term and about two pounds in the long term (one year). About 4.8% of patients in this study gained more than 7% of their body weight compared to about 3.3% who took placebo. All this means that the risk of weight gain with Latuda is lower than with other antipsychotics. This is due to Latuda's weak effect on certain types of nerve receptors that other antipsychotic drugs interact with. As a result, side effects such as weight gain, tremors, and orthostatic hypotension are less common and less severe than with other antipsychotics. However, the manufacturer advises to carefully monitor the weight when taking Latuda.
Latuda Withdrawal
There are no studies or clinical trials on Latuda withdrawal syndrome, although there are reports of Latuda withdrawal syndrome. Neither the manufacturer nor the physician's handbook list drug withdrawal as a side effect or recommend a dosing regimen when stopping Latuda.

However, antipsychotics that work in a similar way to latuda, called dopamine antagonists, can cause withdrawal symptoms when they stop taking them, but not all patients will experience withdrawal effects when they stop taking atypical antipsychotics. Those who do may experience mild or severe withdrawal symptoms. However, the American Psychiatric Association recommends reducing the dose by 10% every month when stopping antipsychotics to reduce the risk of withdrawal or recurrence of symptoms.
The most common symptom of withdrawal upon discontinuation of antipsychotics is the return of symptoms. If the patient has been asymptomatic for some time, the return of symptoms may seem worse than before treatment. Other symptoms of antipsychotic withdrawal include involuntary movements, twitching, slow movements, compulsion to move, nausea, vomiting, diarrhea, and abdominal pain. Your doctor may prescribe Parkinson's disease medications to help with neuroleptic withdrawal symptoms.
How long do the side effects of Latuda last?
Side effects may last as long as Latuda is taken, but some minor side effects may decrease over time. After a long treatment, Latuda will take about two to four days to completely clear from the body. Around this time, the most minor and some serious side effects will begin to disappear. Unfortunately, some serious side effects may take longer to resolve, while others, such as tardive dyskinesia, may be irreversible.
Latuda contraindications and warnings
Latuda comes with a black box FDA warning not to be used to treat dementia-related psychosis due to the risk of death or stroke. Latuda should also not be taken:
- People who are allergic to lurasidone or any of its inactive ingredients.
- People taking medications or substances that greatly affect the metabolism of lurasidone in the body.
Other warnings include:
- Neuroleptic malignant syndrome
- Late discinesia
- Low amount of leukocytes
- Ortostatic hypotension
- Suicidal thoughts or behavior
- Leading, fat or cholesterol
2 13 years and older for schizophrenia and children and adolescents over 10 years of age for bipolar depression.
 The safety of Latuda in children under 10 years of age has not been studied.
The safety of Latuda in children under 10 years of age has not been studied. When used to treat bipolar depression, Latuda significantly increases the risk of suicidal thoughts and behavior in children and adolescents. Children and young patients should be monitored for worsening depression or signs of suicidality.
Pregnancy and lactation
There are no studies on the safety of using Latuda in pregnant or breastfeeding women. There is anecdotal evidence of newborns who experience movement disorders and withdrawal symptoms when taking antipsychotics in the third trimester of pregnancy. Latuda can be excreted in breast milk, but the exact amount has not been established. As with any antipsychotic drug, women should discuss the pros and cons of taking latuda while pregnant or breastfeeding.
Elderly
The safety of Latuda in people over 65 years of age has not been thoroughly studied, and prescribing information cautions when prescribing for the elderly (age 65 and over).
 Thus, the decision to prescribe this medication to people aged 65 years and older diagnosed with schizophrenia or bipolar depression is made on an individual basis after consultation with a doctor. Latuda does increase the risk of stroke and death in older patients with dementia-related psychosis, which is why Latuda is not approved for these patients.
Thus, the decision to prescribe this medication to people aged 65 years and older diagnosed with schizophrenia or bipolar depression is made on an individual basis after consultation with a doctor. Latuda does increase the risk of stroke and death in older patients with dementia-related psychosis, which is why Latuda is not approved for these patients. Latuda interactions
For drugs like Latuda, drug interactions are complex and confusing. To facilitate Latuda interactions, other drugs should not be taken or taken with caution as they may:
- Interfere with the body's ability to break down lurasidone, the active ingredient in Latuda or
- Worse side effects
CYP3A4 inducers and inhibitors
with drugs that are strong inducers and inhibitors of CYP3A4. Simply put, these drugs either speed up the breakdown of lurasidone by the body (CYP3A4 inducers) or prevent and slow down the breakdown of lurasidone (CYP3A4 inhibitors).
Drugs that only moderately or slightly accelerate the breakdown of lurasidone can be taken, but doctors may need to change therapy or dosage.
However, drugs and products that slow down the metabolism of lurasidone in the body increase the concentration of latuda in the blood and thus increase the risk of side effects. Strongest inhibitors not to be taken with Latuda include:
- Grapefruit, Curcumin and Goldenseal
- Some types of anticancer drugs that modulate the immune system such as Tasigna (nilotinib), Kiskali (ribociclib), Zidelig (idelicib), and Ridapt (midostaurin)
- Ergotamine, terfenadine, nefazodone, loperamide, cobicistat, vaprisol, diacomite (styripentol), naloxone, danazol and lonafarnib
There are substances in grapefruit that are also inhibitors of CYP3A4. However, these substances do not affect the body's ability to absorb lurasidone in the body, but rather block the same process in the gut. This means that the body absorbs more lurasidone than usual, which increases the risk of side effects. Grapefruit's effect on intestinal cells can last up to 24 hours, so grapefruit should be completely avoided while taking latuda.
Depressants
Latuda is a central nervous system depressant. It slows down the brain. These effects will be enhanced if Latuda is taken with other central nervous system depressants. The consequences can be physically dangerous. Otherwise, fatigue and loss of motor control may increase the risk of an accident or injury. Other CNS depressants should be avoided or used with caution while taking Latuda, including:
- Alcohol, marijuana, cannabinoids, ginseng or gota cola
- Antihistamines such as Benadryl (Difenhydramin), Doxylamine and Feniramin Drugs such as Codeine, Morphine or Tramadol of 5 . like midazolam or estazolam
- Anxiety medicines such as buspirone or diazepam
- Nerve pain medicines , such as gabapentin, gabapentin Enakarbil or pregabalin
- Preparations against nausea such as metocloplapramide or ondansetron
- Distribution preparations such as carbamazepine (contraindicated), phenytin, lapreidine or levateracetes not but all should be taken with great care and after consultation with your doctor or other health care provider.
 Avoid driving, operating machinery, or engaging in risky activities when two or more CNS depressants are combined.
Avoid driving, operating machinery, or engaging in risky activities when two or more CNS depressants are combined. Seizures
Seizures are uncontrolled, random and repetitive firing of nerve circuits in the brain. They can range from barely noticeable thoughts to full body spasms. In clinical trials, seizures were a side effect of Latuda at the same rate as placebo, making Latuda a relatively safe antipsychotic drug. However, Latuda and all other antipsychotics lower the seizure threshold, increasing the risk of seizures in patients. For this reason, healthcare professionals will avoid combining Latuda with drugs that can cause seizures, including Firdapse (amifampridine), Wellbutrin (bupropion), and certain types of drugs used for x-rays or other imaging.
Latuda may interact with other drugs and conditions such as:
- Parkinson's medicines
- Hyperglycemia
- Heatstroke
How to avoid the side effects of Latuda
Sometimes these side effects cause patients to stop taking the drug.
 Keep in mind that all antipsychotics are a compromise between their often significant benefits and sometimes just as significant side effects.
Keep in mind that all antipsychotics are a compromise between their often significant benefits and sometimes just as significant side effects. Follow these tips when taking Latuda to minimize the risk of side effects from Latuda while getting the most out of your drug:
1. Take Latuda as directed.
Take your daily dose as directed. Do not increase or decrease the dose. First of all, do not take a one- or two-day break in taking the drug. It must be taken daily for a long time to fully realize its benefits. If the medicine is not working or the side effects are difficult to manage, talk to your doctor about changing your dose or switching to a new medicine.
2. Take Latuda with food.
Latuda should be taken with meals. In fact, it should be taken with a meal containing at least 350 calories. Although this may not prevent side effects, it ensures that you get the maximum benefit from taking the drug.
3. Tell your doctor about all your illnesses and medications.
Due to the risk of side effects, you should tell your doctor about:
- Any physical condition you may have,
- High level of blood sugar, diabetes or metabolic syndrome
- Low amount of leukocytes
- History of convulsions or epilepsy
- Problems with thyroid gland
- History of Prolantin
- Parkinson disease or symptoms
- Problems with
- Problems with problems with problems with problems liver
- Any use of alcohol, recreational drugs or substance abuse.
- All medications you currently take
- All over-the-counter medications and supplements you usually take
prescription.
4. Avoid alcohol, antihistamines, and depressants.
Any substance that slows the brain, such as alcohol, marijuana, antihistamines, and sedatives, will exacerbate Latuda's sedative and cognitive effects, increasing the risk of accidents or injury. While taking Latuda, do not drive, operate machinery, or engage in risky activities until you know how the drug affects you.
 It is also recommended to take CNS depressants such as Latuda to clear obstacles and hazards around the home to reduce the risk of accidental injury.
It is also recommended to take CNS depressants such as Latuda to clear obstacles and hazards around the home to reduce the risk of accidental injury. 5. Do not eat grapefruit or drink grapefruit juice.
Grapefruit and grapefruit juice are prohibited when taking Latuda. Grapefruit contains substances that increase the amount of lurasidone absorbed by the body, increasing the risk and severity of Latuda side effects. Other medications and substances can also increase the levels of latuda in the body, so be sure to discuss any medications, supplements, and herbal medicines you take with your prescribing physician.
6. Avoid overheating.
Latuda and other antipsychotic drugs interfere with the body's ability to regulate temperature, creating a potential risk of overheating. Avoid overheating or dehydration:
- Staying indoors in hot weather
- Avoid overexertion or overexertion
- Avoid prolonged sun exposure
- Drink plenty of water
- Avoid alcohol - it also affects the body's ability to regulate body temperature.