How long does liletta last
Exciting News—LILETTA now approved for use up to 6 years!
SHOP TALK /
The FDA has extended approval of LILETTA IUDs for up to 6 years of use, research shows they are safe and effective for up to 7 years.
by Robin Watkins, CNM, WHNP-BC
published 11/14/19
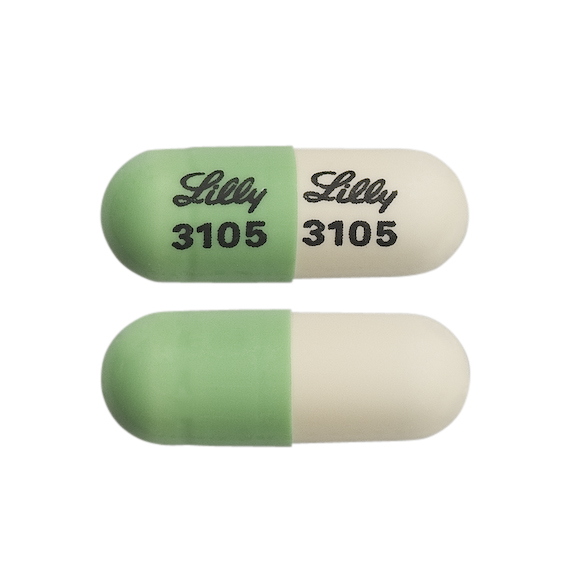
On October 28, based on the research from the manufacturer, the FDA was able to approved LILETTA, a 52mg levonorgestrel-releasing intrauterine device (IUD) for up to 6 years of use, making it the longest approval for any levonorgestrel-releasing IUD in the US. Here is what you need to know.
LILETTA: the background
There are currently four levonorgestrel-releasing IUDs on the market: LILETTA (52mg), Mirena (52mg), Skyla (13.5mg) and Kyleena (19.5mg). Both LILETTA and Mirena have 52mg of levonorgestrel, making them very similar in practice. However, LILETTA is unique in that it was brought to market in 2015 and manufactured by Medicines360, a non-profit pharmaceutical company working to improve access to the IUD for everyone who wants one, regardless of socioeconomic status or geographic location.
Clinics with 340B designation are able to purchase LILETTA for a discounted rate in order to make it accessible to more people who need it. You can find more information about LILETTA [here](https://www.lilettahcp.com/, sign up for updates here, and find updated Bedsider materials for patients here.
Why the change to 6 years?
Current research shows that an IUD with 52mg of levonorgestrel, like LILETTA, is effective and safe to use beyond the original FDA approval. The science showing that IUDs are effective beyond the original FDA approval continues to improve as time passes and it is possible to study them for longer periods of time. Additional evidence suggests that IUDs with 52mg of levonorgestrel, like LILETTA and Mirena, are effective for at least 7 years, but the FDA approval of Mirena has not changed. The manufacturers of LILETTA designed their clinical trial testing effectiveness to extend through 7 years and that research is ongoing through 2020.
Counseling patients who are having LILETTA placed
When you are placing IUDs and implants, a conversation about the discrepancy between the FDA approval and the evidence can be potentially long-winded or even unnecessary. While these methods are shown to be effective beyond the FDA approval and patients may desire to use them up to the maximum, evidence shows that the average duration of use tends to be much shorter.
While these methods are shown to be effective beyond the FDA approval and patients may desire to use them up to the maximum, evidence shows that the average duration of use tends to be much shorter.
So, if you already know from previous conversations with a patient what is most important to them about their birth control method and how long they plan on using it, you may not need to share all of the details of the FDA approval process. This is a great opportunity to engage your patient in shared decision-making about their birth control.
Here are some general points to cover when counseling patients about LILETTA and FDA approval:
- All LILETTA IUDs are now FDA approved for 6 years. This new approval doesn’t just apply to new ones that are placed going forward. If a patient already has the LILETTA IUD, it’s good for 6 years.
- Good evidence shows that an IUD with 52mg levonorgestrel is safe and effective for at least 7 years.
- Printed package materials may not match current FDA approval and/or current research.
- Patients can always come in to have their IUD strings checked, discuss satisfaction, ask about the latest FDA approval, and talk about how long they plan to use their IUD.
Counseling patients who already have a LILETTA
You may have anticipated expanded FDA approval and therefore had this conversation with your patients about LILETTA when placing it. Patients presenting for removal of LILETTA IUDs after 3 or 4 years may not feel comfortable continuing to use their method beyond the previously FDA approved maximum. If they don’t feel comfortable continuing with their IUD after you’ve explained the new FDA approval, you should replace it.
Stay tuned—we anticipate that LILETTA will get FDA approval for 7 years!
Robin Watkins is the Sr. Director, Health Care at Power to Decide. Robin is a midwife and women’s health nurse practitioner focused on expanding provider capacity to offer equitable, resonant, and high-quality sexual and reproductive health care. Robin provides clinical care in Washington, DC. When she is not talking sex, placing IUDs, or asking One Key Question, you can find her riding her bike on the streets of DC or eating ice cream for dinner.
Robin provides clinical care in Washington, DC. When she is not talking sex, placing IUDs, or asking One Key Question, you can find her riding her bike on the streets of DC or eating ice cream for dinner.
read more about:birth control,LARC,shoptalk,public policy
read our commenting policy »
What makes the Liletta IUD different from Mirena?
SHOPTALK /
Here’s what you and your patients should know about these two (very similar) hormonal IUDs.
by Jessica Morse, MD, MPH
published 02/12/19
Many of you are likely already stocking and placing Liletta, the levonorgestrel intrauterine system (IUS, a.k.a. IUD) introduced in 2015. But you and your patients may still be trying to sort out how Liletta is different from—or very similar to—another IUD that’s been out there for years, the Mirena. Here are the details.
How long does Liletta actually last?
As of late 2018, the official word from the FDA is that Liletta effectively prevents pregnancy for up to five years. But that’s just a start. Liletta was designed to last seven years, and the study testing its effectiveness will be ongoing through 2020. To date, the study has shown that the pregnancy rate is very low (0.55%) for up to five years of use. Another study looking at the amount of levonorgestrel released by the IUS through five years of use suggests that it’s on track for a seven-year lifespan.
But that’s just a start. Liletta was designed to last seven years, and the study testing its effectiveness will be ongoing through 2020. To date, the study has shown that the pregnancy rate is very low (0.55%) for up to five years of use. Another study looking at the amount of levonorgestrel released by the IUS through five years of use suggests that it’s on track for a seven-year lifespan.
So what can you tell your patients now? You can reassure them that if they reach the three or five-year mark (depending on the what information was available when it was placed) and want to keep their Liletta, the FDA will likely have approved a longer lifespan by that time. Check out this article to read more about talking to your patients about the updated FDA approval.
How easy is Liletta to place?
The early adopters out there may remember that the original Liletta inserter was a bit clunky—sort of a hybrid between other inserters we love or hate. The current inserter, now widely available, is remarkably similar to the inserters you’re used to with other hormonal IUDs. Liletta’s inserter even has numbers on it to remind you of the steps for placement. Although the slider is a bit stiff, the placement process will be very familiar to anyone who has placed a hormonal IUD in the past. It’s also reloadable and easily learned by a new health care provider.
Liletta’s inserter even has numbers on it to remind you of the steps for placement. Although the slider is a bit stiff, the placement process will be very familiar to anyone who has placed a hormonal IUD in the past. It’s also reloadable and easily learned by a new health care provider.
How should I counsel my patients about Mirena versus Liletta?
In terms of the patient experience of the device, the truth is that they are likely the same. Both are excellent at preventing pregnancy, and both are likely to cause noticeable decreases in menstrual bleeding or even complete cessation. The amount of levonorgestrel delivered is basically the same over the first five years, resulting in similar side effect and benefit profiles. Even the inserters and placement processes are now similar. From your patient’s perspective, the biggest difference between the two may be the cost.
How much will my patient pay for a Liletta?
Cost is the only place where there may be a profound difference between the two devices. Liletta is the result of a unique partnership with women’s health advocates, researchers, and a not-for-profit drug company to develop an affordable IUD. Throughout the process, Liletta’s makers have been committed to ensuring the device is broadly accessible, even to those without health insurance and those with high deductibles. Their goal is that no one will ever have to pay more than $150 for a Liletta.
Liletta is the result of a unique partnership with women’s health advocates, researchers, and a not-for-profit drug company to develop an affordable IUD. Throughout the process, Liletta’s makers have been committed to ensuring the device is broadly accessible, even to those without health insurance and those with high deductibles. Their goal is that no one will ever have to pay more than $150 for a Liletta.
How do I get reimbursed for Liletta?
If your practice should be reimbursed by a third-party payer for a Liletta, there is a J-code specific to this IUD. For additional tips on reimbursement and coding, check out this comprehensive resource: Intrauterine Devices & Implants: a Guide to Reimbursement.
Overall, Liletta is a welcome option for patients interested in hormonal contraception. As a provider, I feel good about being able to offer patients who want an IUD an effective, safe, and affordable option—regardless of their health care coverage.
Jessica Morse is an ob/gyn at Duke University where she works with residents providing a full spectrum of reproductive health care. Her main research interest is increasing the number of women who know about long-acting reversible contraceptives (IUDs and implants), in the U.S., Uganda, Rwanda and Honduras. She lives in Durham, NC, with her husband and silly 3-year-old son, where they spend weekends hiking, hanging out at playgrounds, and exploring the Bull City.
Her main research interest is increasing the number of women who know about long-acting reversible contraceptives (IUDs and implants), in the U.S., Uganda, Rwanda and Honduras. She lives in Durham, NC, with her husband and silly 3-year-old son, where they spend weekends hiking, hanging out at playgrounds, and exploring the Bull City.
read more about:how to,LARC,cost,birth control,shoptalk
read our commenting policy »
How does the IUD work? - September 8, 2020
Sep 08, 2020
How does the IUD work? – September 8, 2020
Posted at 2:14 AM in Pregnancy Prevention, Women's Health to Andrew Thorne
The IUD is not a new method of birth control, but it has become more popular in recent years. Demand for IUDs has skyrocketed since 2016, according to Planned Parenthood statistics. A common question we get from our patients at One Community Health is, "How does the IUD work?" Read on to learn more about this popular contraceptive.
What is an IUD?
IUD stands for intrauterine device. It is a long-term, highly effective contraceptive option. The device itself is a small "T" shaped piece of plastic that is placed in the uterus. Depending on the specific device, IUDs last from 3 to 12 years if they have not been removed before.
How does the IUD work?
As we mentioned above, there are different types of IUDs, and each one works a little differently. Some are copper coated and some are hormone coated. Copper is toxic to spermatozoa, and if it enters the uterus, it acts as a spermicide, preventing fertilization.
IUDs coated with the hormone progestin thicken cervical mucus so sperm cannot reach the egg. In some cases, it stops ovulation - the release of an egg during a woman's monthly menstrual cycle. If the egg is not released, pregnancy is not dangerous.
How effective are IUDs?
IUDs are 99% effective in preventing pregnancy, making them one of the most effective forms of birth control available today. One of the reasons why they are so effective is that they are practically reliable, which means you cannot forget to take them or misuse them, as is possible with pills and condoms.
One of the reasons why they are so effective is that they are practically reliable, which means you cannot forget to take them or misuse them, as is possible with pills and condoms.
IUD benefits
- Comfortable
- 99% effective
- Can be removed at any time if you want to get pregnant
- Hormonal IUDs can relieve heavy periods
- Non-hormonal option available for people who prefer (copper IUDs)
- Copper IUDs can serve as emergency contraception if inserted within 5 days of unprotected intercourse.
Reverse
Some people experience minor side effects, including:
- Irregular bleeding in the first few months
- More heavy periods and more severe cramps (copper IUD)
- Menses lighter/shorter or no menses (some progestin IUDs)
- PMS-like symptoms such as mood swings, headaches, acne, nausea, and breast tenderness (progestin IUDs)
In rare cases, there may be more serious side effects. Another disadvantage of IUDs is that they do not protect against STDs.
Another disadvantage of IUDs is that they do not protect against STDs.
Different types of IUDs
Four types of hormonal IUDs are available. They all work in the same way, but last for a different amount of time.
- Mirena - lasts up to 7 years
- Kailina - lasts up to 5 years
- Liletta - lasts up to 7 years
- Skyla - lasts up to 3 years
The only type of non-hormonal or copper IUD available in the US is the Paragard. This IUD is valid up to 12 years.
Sacramento IUD
If you have additional questions about how the IUD works or which option is right for you, be sure to speak with your One Community Health doctor. Learn more about our comprehensive women's health service and how to become a patient by calling 916-443-3299.
photo Reproductive Health Providers Coalition on Hide
Breaking news
Everything you were afraid to ask about the IUD - GlagoL - Dec 11 - 43582727403
photo: look4ward. co.uk
co.uk
becomes smaller. While there are many excellent resources on the Internet, it is extremely difficult to find a comprehensive guide to help deal with the anxiety of many girls and women. But it is better not to look for answers using Google, but to ask all the questions of interest to professionals - doctors and experts. Especially if the spiral is installed for the first time.
For starters, the IUD is safe and more than 99 percent effective in preventing pregnancy.
“IUD (intrauterine device) is a safe and highly effective birth control option for most people of all ages, from young people who have never had children to people in their 50s who have not yet reached menopause ,” says Dr. Gillian Dean, senior director of medical services, in a statement to the Planned Parenthood Federation of America. - An IUD can even be inserted if you have never had vaginal sex before. Your sexual history should not affect the method of birth control you choose to use. "
"
So what is the difference between all IUDs and how do they work to prevent pregnancy?
Dr. Katherine O'Connell White, Director of Family Planning Scholarships, Boston University/Boston Medical Center:
So there are five different IUDs on the market. Four of them are hormonal - that is, they contain the hormone progestin, and one of them is non-hormonal, that is, it uses copper wire as a method of birth control. All five IUDs work locally, which means that the biggest impact on preventing pregnancy comes from its effect on the lining of the uterus. Hormonal IUDs carry a small amount of progestin into your bloodstream, but in general, especially when compared to other forms of hormonal birth control, your blood levels of hormones are much lower. Most of it stays in your uterus.
All hormonal IUDs contain the same progestin hormone, but it has different levels of progestin. Therefore, they last a different number of years and affect your period in different ways. The hormonal IUD with the lowest dose is Skyla, and the woman usually has lighter but fairly regular periods—very similar to those that occur while taking birth control pills. The highest doses of the progestin IUDs - Mirena and Liletta - very often result in women having incredibly light periods, often only intermittently or not at all. (Note: the fourth hormonal IUD - Kyleena - is installed for five years. The fifth IUD is non-hormonal copper, ParaGard (ParaGard) - in the US market, in Russia - Nova-T).
The hormonal IUD with the lowest dose is Skyla, and the woman usually has lighter but fairly regular periods—very similar to those that occur while taking birth control pills. The highest doses of the progestin IUDs - Mirena and Liletta - very often result in women having incredibly light periods, often only intermittently or not at all. (Note: the fourth hormonal IUD - Kyleena - is installed for five years. The fifth IUD is non-hormonal copper, ParaGard (ParaGard) - in the US market, in Russia - Nova-T).
Some birth control pills are based on estrogen while others are based on progestin. What are the differences between what these two hormones can do to the body?
Dr. White: Estrogen and progestin can prevent pregnancy, although they work in slightly different ways. The biggest difference between the two is that estrogen-containing methods tend to have more predictable bleeding patterns—that is, fewer spots and more regular, lighter periods. Methods with progestin are known to cause new breakthrough bleeding and irregularity. Therefore, if you do not have any medical conditions that prevent you from getting an estrogen contraceptive method, these methods may have a better effect on your menstrual cycle. But there are some women who can't take estrogen because of a chronic condition, which would be unsafe and could lead to high blood pressure or migraines.
Therefore, if you do not have any medical conditions that prevent you from getting an estrogen contraceptive method, these methods may have a better effect on your menstrual cycle. But there are some women who can't take estrogen because of a chronic condition, which would be unsafe and could lead to high blood pressure or migraines.
Copper IUDs are said to make the uterus toxic to sperm - is that true?
It's true, but most women prefer not to think about anything toxic inside their bodies. I tend to describe it more like inflammation in the lining of the uterus, which turns out to be toxic to the sperm, it's true.
Could you explain how the IUD insertion process works, especially if the girl hasn't had sex at all?
The first thing your doctor does is put a speculum in your vagina, and it's an instrument that just holds up the walls of your vagina so the doctor can see your cervix. So if you've never had penetrative sex, it might already be a little uncomfortable.
Then, once your doctor has cleaned your cervix, he often puts a stabilization instrument on your cervix - sometimes putting this instrument on can cause a slight spasm. I describe the IUD process as a series of three seizures. A cramp, a cramp, then a big cramp, and then everything is ready. So it's not five minutes of constant excruciating pain, but just little bursts of pain.
The doctor will then see how deep your uterus is, place an incredibly thin instrument inside it called a "sound" that shows the depth of your uterus so the doctor knows exactly where to place the IUD inside. And then the last step is the insertion of the IUD itself. The IUD is screwed into what looks like a very thin straw and it goes through the hole in your cervix and the IUD pops out at the other end. Therefore, the doctor does not need to make any incisions or incisions on your body at all. The doctor may use the natural opening of your cervix, which leads to the uterus where blood flows, to place an IUD. "
"
For those not familiar with anatomy, is this near the hymen area?
The dilator actually goes into the vagina and the hymen covers the entrance to the vagina. It is very rare for women to reach adolescence without a natural opening of the hymen. I hate to use the word "tear" because it sounds very traumatic, but usually with various exercises (not special), natural movements and play, it opens even before the first intercourse. In some girls, however, there is still no opening, so the hymen still completely blocks the entrance to the vagina, which complicates the installation of the IUD.
But a girl whose hymen is intact can have an IUD inserted if she wants to?
Yes, absolutely. It will be just a process of cutting through the hymen.
Why are some doctors hesitant to give IUDs to virgins?
Moreover, looking in the mirror itself can be really uncomfortable if the girl has not had penetrative sex. Much depends on the size of the mirror used by the doctor, how slowly he inserts it, and how much the girl can relax the muscles in the pelvic area. It does not require special knowledge of yoga or any special techniques, but when you are nervous, you tense up. And this must be fought to relax enough to allow the mirror to enter.
Much depends on the size of the mirror used by the doctor, how slowly he inserts it, and how much the girl can relax the muscles in the pelvic area. It does not require special knowledge of yoga or any special techniques, but when you are nervous, you tense up. And this must be fought to relax enough to allow the mirror to enter.
Being sexually active is not a requirement for an IUD, so it's kind of an old school mentality surrounding an IUD. There will definitely be those who will discourage you, and a lot of that has to do with their own level of comfort with the procedure itself. Therefore, it is important that a person knows that, regardless of their sexual activity, they are eligible to have an IUD inserted.
How to deal with nervousness before the procedure?
First, you have a doctor you really trust, feel comfortable with and always be honest about your sexual activity. If you've never had penetrative sex, you should tell the doctors because they're going to use different sized speculums and they need to be slower in wielding those speculums. Another trick that works for some women is that they position the mirror themselves so you can control how fast you insert it. Therefore, if you feel that the doctor is going to do it quickly, you can ask him to stop and place this mirror himself. (Note: Dr. White also said that you can always ask your doctor to use smaller speculums if others are too painful).
Another trick that works for some women is that they position the mirror themselves so you can control how fast you insert it. Therefore, if you feel that the doctor is going to do it quickly, you can ask him to stop and place this mirror himself. (Note: Dr. White also said that you can always ask your doctor to use smaller speculums if others are too painful).
Are there any medicines you can ask your doctor to make the process less painful?
Dr. Pari Ghodsi, LA-based OB/GYN: The only thing we generally recommend is taking pain medication before the procedure. You can simply take a high dose of medication that helps you relieve pain, such as 800 mg of ibuprofen about 30-60 minutes before the procedure (this will help reduce some of the spasms).
But what about the anesthesia, cervical dilation pills or spray that some doctors say they use to relieve pain?
Dr. White on the injection and spray: Studies of local anesthesia, such as that used by a dentist to numb the mouth, do not show a significant difference in pain reduction, so this is not standard practice for all physicians. The reason I don't think this will work for some women is that most of the pain isn't really in the cervix - it's in the uterus itself. Because when the instruments touch the top of the uterus, it causes spasms and localized blockage around the cervix. For some women, para-cervical blockade is very painful.
The reason I don't think this will work for some women is that most of the pain isn't really in the cervix - it's in the uterus itself. Because when the instruments touch the top of the uterus, it causes spasms and localized blockage around the cervix. For some women, para-cervical blockade is very painful.
Spray (Lidocaine 10%), (another method some doctors use to reduce pain during the procedure), only works on the instrument on the cervix. And it doesn't work on any of the remaining procedures. But each doctor has his own technique and what they have achieved good results with.
Dr. White on the expansion pill: The evidence against this is really strong - the pills don't make any difference in facilitating the procedure. This pill causes an increase in cramps, nausea and diarrhea, which is why we don't really use it.
photo: wikipedia.org
Why does the IUD cause spasms in the first couple of months after insertion (both copper and other types)?
Dr. White: There is an exchange going on in the womb (with IUD insertion) that has predictable "responses" from the womb, and the first is determination. Cramps are more severe with hormonal IUDs, to be honest, than with copper ones, but this can happen with copper as well, as the body sort of adapts to this new “inhabitant”.
White: There is an exchange going on in the womb (with IUD insertion) that has predictable "responses" from the womb, and the first is determination. Cramps are more severe with hormonal IUDs, to be honest, than with copper ones, but this can happen with copper as well, as the body sort of adapts to this new “inhabitant”.
But the release of the hormone progestin in the hormonal IUD tends to counteract spasms; in fact, hormonal IUDs are used for chronic pelvic pain, they are very effective in reducing pain and cramping in the uterus.
The copper IUD, due to the inflammation caused by the way it works, can lead to very intense or painful periods in some women. This is due to the inflammatory response, which is how copper works. Things will get better after the first 3-6 months, and women who have difficulty with seizures can get a prescription for an anti-inflammatory.
When should stains on laundry be a concern?
Dr. White: Heavy bleeding, for example, which you don't have even with very "heavy" periods, and which continues for several weeks when you change several pads or tampons a day is probably a lot, but this is not a common occurrence. Spots are annoying, can be a real nuisance, but are a very common side effect. I sometimes joke that a Navy starter pack should come with a box of pads and 12 sets of underwear.
Spots are annoying, can be a real nuisance, but are a very common side effect. I sometimes joke that a Navy starter pack should come with a box of pads and 12 sets of underwear.
Dr. Ghodsi: After a few months with any type of IUD, if you have any concerns, you should see a doctor.
What to expect after the first six months?
Dr. Ghodsi: If you have a copper IUD, there are probably no stains by now. You may just notice that your periods are heavier than before. But you shouldn't bleed between cycles. People who have a hormonal IUD, unfortunately, sometimes experience this problem (bleeding between cycles). That's why I said it matters if it's a worries you - because some women don't care, they just know that it can be. And some women don't menstruate at all, but of course there's always a risk factor for spotting.
How do you know if the IUD has moved or something has happened after insertion, especially if you don't feel anything after a few weeks after insertion?
Dr. White: That's exactly what you should feel - that is, nothing. We've talked about all the side effects that can happen, but the bottom line is that everyone feels fine after having an IUD inserted. But, if this question bothers you, then you can check the IUD yourself. Place one finger in the vagina up to the cervix and you will feel the strings - this indicates that the IUD is still in place. If you can't feel the strings, or if you're too uncomfortable doing this check, you can always see a doctor and they'll do a quick check.
White: That's exactly what you should feel - that is, nothing. We've talked about all the side effects that can happen, but the bottom line is that everyone feels fine after having an IUD inserted. But, if this question bothers you, then you can check the IUD yourself. Place one finger in the vagina up to the cervix and you will feel the strings - this indicates that the IUD is still in place. If you can't feel the strings, or if you're too uncomfortable doing this check, you can always see a doctor and they'll do a quick check.
Many young women, especially those who have not been very sexually active, may not know how to check their cervix. Do you have any advice for this?
Dr. White: The vagina is longer than you think. I always say have a glass of wine, lie down in bed with your knees bent, and then try to get your finger in as far as you can. And if you come across something that looks like your nose, it's your cervix. In fact, this is how your cervix will feel. And then you will feel yourself in this area. But a lot of women who try to do it don't go far enough because it's either weird or uncomfortable or they just don't want to do it. But, if you have a partner, you can also ask him to help you.”
And then you will feel yourself in this area. But a lot of women who try to do it don't go far enough because it's either weird or uncomfortable or they just don't want to do it. But, if you have a partner, you can also ask him to help you.”
For young women who may not have had any sexual experience, is it more painful to have an IUD or lose your virginity?
Dr. White: I think it depends on the woman. When you lose your virginity, this does not mean that you will necessarily be hurt during the first sexual intercourse. Where "legs grow" is unknown, but everyone believes that it will definitely hurt. It may be uncomfortable, but it shouldn't hurt. Because there must first be a fairly long foreplay (during which a sufficient amount of lubrication will be released) - before letting someone inside you for the first time. Your first time is not a time for quick sex - it's a time when you want to "play" before getting to the actual intercourse.
And sex is only in the vagina, it doesn't go all the way to the womb, so the IUD can hurt people whether they've lost their virginity or not. But IUD placement lasts much less time than sex. Most people have sex for more than three minutes. Maybe not if their partner is a teenager, but it usually takes a little longer.
But IUD placement lasts much less time than sex. Most people have sex for more than three minutes. Maybe not if their partner is a teenager, but it usually takes a little longer.
If you become sexually active for the first time within the first 3-6 months after insertion, is it normal to expect bleeding?
Dr. White: In most cases, sex itself does not cause bleeding, even if it is dry. It hurts, but it doesn't bleed - you can't cut yourself from it. Sometimes sex can cause bleeding if a woman is about to start her period. I've heard women talk about post-sex spots (with an IUD), especially in the first few months. And I see this as a kind of “loosening” of what would have happened anyway (spots can be without sex). But if it continues after the first few months, then it's probably worth talking to your doctor, because postpartum hemorrhage can also be a sign of an infection not related to the IUD (if it's placed right after delivery) but related to your vagina and cervix. .
.
McLean: Every time something is inserted into the vagina for the first time, be it a sex toy, a penis, or even fingers, there may be blood. The blood should not be "heavy" - it will be bright red blood. And typically, what comes out of the uterus as a result of an IUD insertion will be a little darker and a little more than menstrual blood (because it has a longer travel path). There should not be much bleeding during sex and an IUD. And if after the first time you feel uncomfortable inserting something into your vagina, you should talk to your doctor about it, because sex should always be consensual, sex should always be pleasant.
What side effects can be expected if a woman is considering giving up birth control pills in favor of an IUD?
Dr. White: Birth control pills that could give you good, regular periods that are very predictable, with few cramps, you can "trade" for the irregular bleeding and increased cramps we talked about. Birth control pills also have a good effect on our skin, helping to reduce acne. So your skin can actually change, not because the IUD has damaged it, but because you've lost the protective effect of birth control. I think there are three main things: bleeding, spasms and pimples.
So your skin can actually change, not because the IUD has damaged it, but because you've lost the protective effect of birth control. I think there are three main things: bleeding, spasms and pimples.
Dr. Ghodsi: Every time you go from one birth control to another, you may have some adjustment period. Again, this can last for more than a couple of months, but after 2-3 months, if it's something irregular and bothers you, you should call your doctor.
Can some hormonal IUDs cause cystic acne?
Dr. White: For women who are incredibly hormonally sensitive, this can make things worse. In most cases where I have seen severe acne with IUDs in women, they started taking birth control pills. So it's really hard to know what their skin would look like without the pills. But it's true - if you have acne problems and the pills control them, then the acne situation can get worse if you stop taking birth control pills. Some girls use copper IUDs and pills - they use copper IUDs for better birth control and pills for their skin. And there is nothing wrong with that.
And there is nothing wrong with that.
But would you use birth control pills with one of the hormonal IUDs?
Dr. White: It's really contradictory because there is no research. It's one of the things I would say, "you should talk to your doctor."
If something is wrong with the IUD after insertion, how can you find out?
Dr. White: A visit to the doctor six weeks after insertion is standard procedure, but this check is mainly to make sure two things: first, that the IUD did not accidentally enter your abdomen, but Secondly, just to check everything. After that, you typically only check your IUD once a year. This is because once we know that the IUD is in your uterus, the only place it will go if it's going to move is out of your body: that is, through the cervix into the vagina and out.
You'll notice this - it won't happen quietly. You will usually suddenly experience more cramping, bleeding, or both. Therefore, I always advise my patients that if suddenly the bleeding really changes, do not just accept it and be cold-blooded, but come to me.