How do you spell paranoid schizophrenia
Paranoid Schizophrenia: Symptoms (Delusions, Hallucinations), Treatments
Written by Terri D'Arrigo
Paranoid schizophrenia, or schizophrenia with paranoia as doctors now call it, is the most common example of this mental illness.
Schizophrenia is a kind of psychosis, which means your mind doesn't agree with reality. It affects how you think and behave. This can show up in different ways and at different times, even in the same person. The illness usually starts in late adolescence or young adulthood.
People with paranoid delusions are unreasonably suspicious of others. This can make it hard for them to hold a job, run errands, have friendships, and even go to the doctor.
Although it's a lifelong illness, you can take medicines and find help to stop symptoms or make them easier to live with.
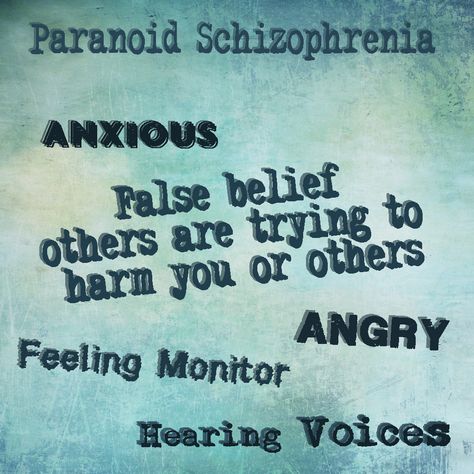
Paranoid Symptoms
Delusions are fixed beliefs that seem real to you, even when there's strong evidence they aren't. Paranoid delusions, also called delusions of persecution, reflect profound fear and anxiety along with the loss of the ability to tell what's real and what's not real. They might make you feel like:
- A co-worker is trying to hurt you, like poisoning your food.
- Your spouse or partner is cheating on you.
- The government is spying on you.
- People in your neighborhood are plotting to harass you.
These beliefs can cause trouble in your relationships. And if you think that strangers are going to hurt you, you may feel like staying inside or being alone.
People with schizophrenia aren't usually violent. But sometimes, paranoid delusions can make them feel threatened and angry. If someone is pushed over the edge, their actions usually focus on family members, not the public, and it happens at home.
You could also have related hallucinations, in which your senses aren’t working right. For example, you may hear voices that make fun of you or insult you. They might also tell you to do harmful things. Or you might see things that aren’t really there. Learn more about the symptoms of paranoia.
Medication
Your doctor may prescribe an antipsychotic drug to make the delusions go away. It could be pills, a liquid, or shots. It can take a few weeks for these drugs to work fully, but you could start to feel a little calmer quickly. You might need to try more than one to find a medication or combination that's right for you.
It could be pills, a liquid, or shots. It can take a few weeks for these drugs to work fully, but you could start to feel a little calmer quickly. You might need to try more than one to find a medication or combination that's right for you.
Even when you feel better, keep taking your medicine. If you stop, your delusions will probably come back.
Avoid using marijuana, alcohol, nicotine, cocaine or other stimulants, and street drugs. They can keep antipsychotic drugs from working well. They can also cause paranoia or make it worse.
You might have to take different kinds of drugs for other symptoms, too. Get more information about medications used to treat schizophrenia.
Counseling
Once your delusions are under control, counseling can help you get along with others, hold a job, go to school, take care of yourself, and have friends.
People with schizophrenia who get counseling are also more likely to stick with their medications.
A kind of counseling called cognitive behavioral therapy can teach you how to manage symptoms that don't go away, even when you take your medicine. You'll learn to test whether you're having delusions and how to ignore voices inside your head.
You'll learn to test whether you're having delusions and how to ignore voices inside your head.
Positive, encouraging support from family and friends really helps, too.
Because some antipsychotic drugs can make you gain weight, you might also want to get help with diet and exercise. Read more on the different types of therapy for schizophrenia.
Hospitalization
There might be times when your paranoid delusions or other symptoms are so severe that you have to go to the hospital. You'll be cared for so you and your loved ones stay safe.
If you recognize that you're having trouble, you can be admitted voluntarily. But if you think you don't need help when you really do, the law may allow a doctor or other mental health professional to admit you involuntarily if you are unable to care for yourself or may be dangerous to yourself or someone else. Know when to call the doctor or 911 for severe psychosis symptoms with schizophrenia.
What It Is, Symptoms & Treatment
Overview
What is paranoid schizophrenia?
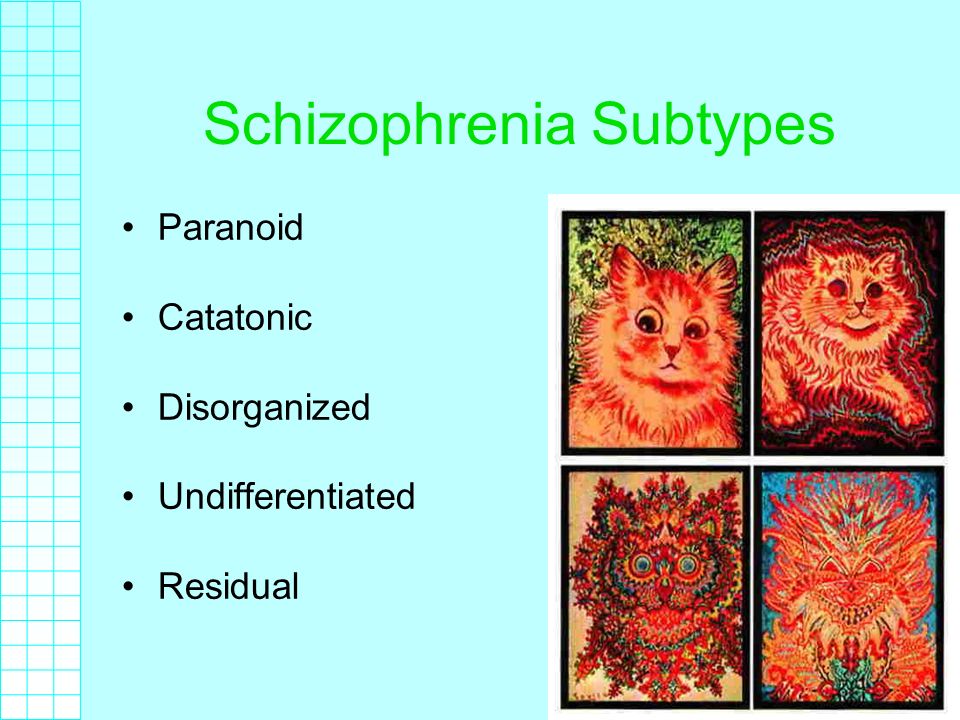
The term “paranoid schizophrenia” is an outdated name for a subtype of schizophrenia.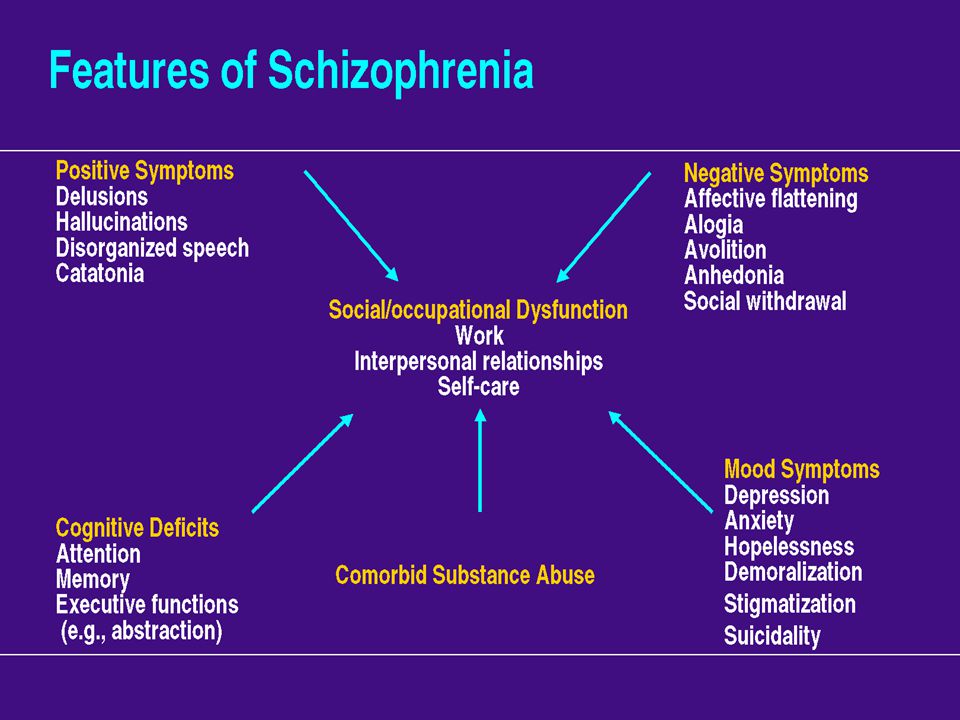 Experts no longer use or recognize this term. Instead, experts recognize schizophrenia as a specific disease, which is part of a spectrum of related conditions that involve psychosis.
Experts no longer use or recognize this term. Instead, experts recognize schizophrenia as a specific disease, which is part of a spectrum of related conditions that involve psychosis.
The American Psychiatric Association removed paranoid schizophrenia from the list of official diagnoses when updating the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5), published in 2013. The World Health Organization removed paranoid schizophrenia from the International Classification of Diseases when updating to the 11th edition (ICD-11) in 2019.
What is the difference between paranoid schizophrenia and schizophrenia?
The term “paranoid schizophrenia” is obsolete. It previously described schizophrenia with very noticeable paranoia and delusions.
Who does it affect?
Schizophrenia usually happens at different ages depending on biological sex, but it doesn't happen at different rates. It usually starts between ages 15 and 25 for people assigned male at birth and between 25 and 35 for people assigned female at birth. Schizophrenia in children is rare but possible, and these cases are usually much more severe.
Schizophrenia in children is rare but possible, and these cases are usually much more severe.
How common is this condition?
Schizophrenia is an uncommon — but widely known — condition. Experts estimate about 85 people out of every 10,000 will develop this condition at some point in their lifetime. Worldwide, there are about 2.77 million new cases each year.
How does this condition affect my body?
Schizophrenia is a mental health condition that disrupts several different areas of your brain. This condition typically affects your thinking abilities, memories .and senses. People with schizophrenia commonly struggle to tell what's real and what isn't. They often have hallucinations and delusions (see below to learn more about these symptoms) and struggle with disorganized thinking.
Symptoms and Causes
What are the symptoms?
Schizophrenia typically happens in three stages. The active stage of schizophrenia is when symptoms are at their worst. The key symptoms of schizophrenia are:
The key symptoms of schizophrenia are:
- Delusions.
- Hallucinations.
- Disorganized or incoherent speech.
- Disorganized or unusual behavior.
- Negative symptoms.
Paranoia and what it looks like
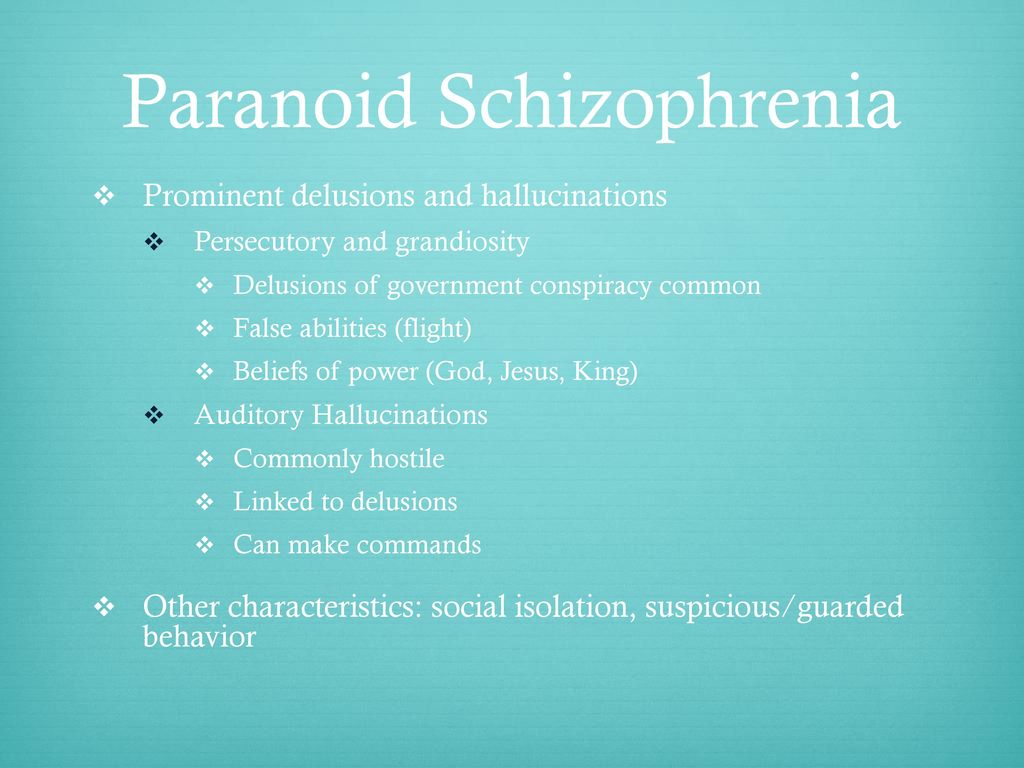
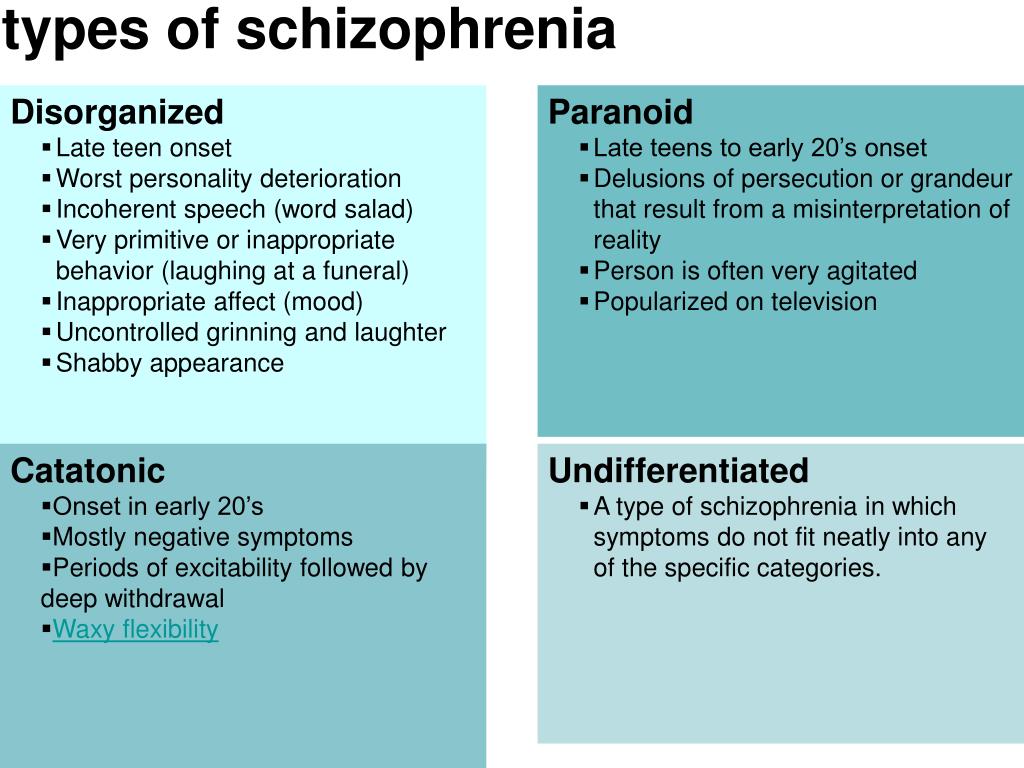
Paranoid schizophrenia was once a subtype of this condition because paranoia commonly happens with schizophrenia. Paranoia is a pattern of behavior where a person feels distrustful and suspicious of other people and acts accordingly.
Delusions and hallucinations are the two symptoms that can involve paranoia.
- Delusions. These are persistent false beliefs. A person who has a delusional belief usually won't change their mind even if faced with strong evidence. Delusions involving paranoia are often "persecutory," which means a person believes that someone is trying to harm them or negatively affect their life.
- Hallucinations. These are events a person imagines (usually in the form of something that a person hears or sees).
 A person who has a hallucination typically can't tell that what they're experiencing isn't real. These commonly feed into delusions by giving the person additional "evidence" to confirm that someone is trying to harm or upset them.
A person who has a hallucination typically can't tell that what they're experiencing isn't real. These commonly feed into delusions by giving the person additional "evidence" to confirm that someone is trying to harm or upset them.
Lack of insight
A common feature of schizophrenia is a symptom known as anosognosia. This condition, often described as “lack of insight,” means that a person’s brain can’t recognize any signs, symptoms or other evidence of a medical condition that they have. This lack of insight is very common with schizophrenia, which is why people with schizophrenia often don't believe that they have the condition and are more likely to resist treatment.
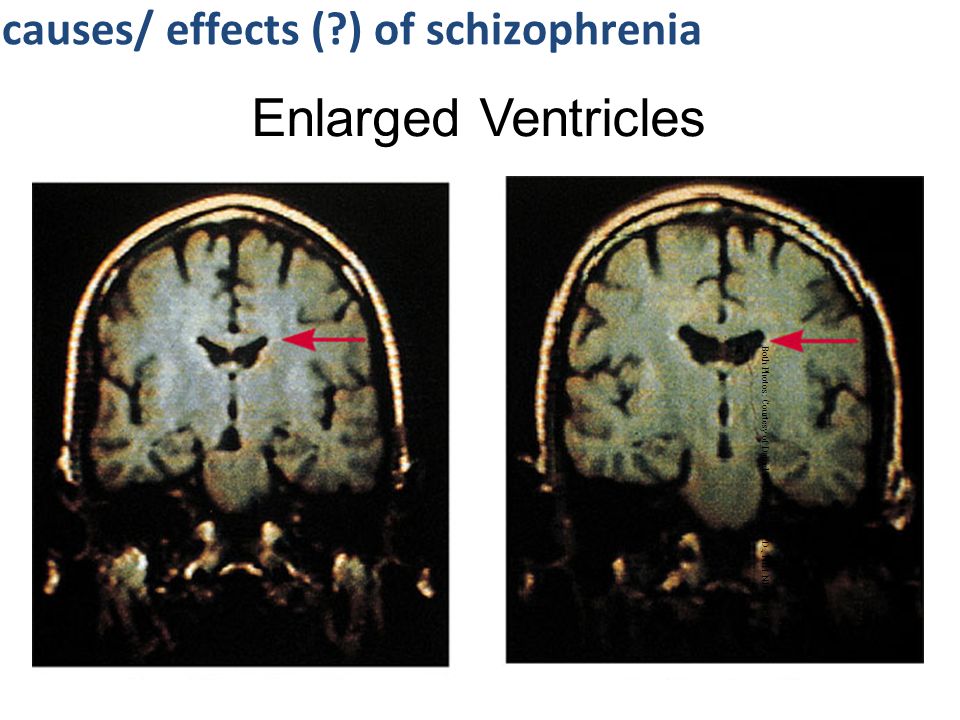
What causes schizophrenia, and does it have any triggers?
Schizophrenia doesn't have a single confirmed cause. Experts suspect that several factors play a role, but none of these guarantees that you'll develop schizophrenia. The three main reasons that schizophrenia happens include:
- Chemical imbalances in your brain.
 The chemicals involved are those that your brain uses to communicate between brain cells.
The chemicals involved are those that your brain uses to communicate between brain cells. - Congenital brain problems. These are problems that affect your brain’s development before you're born.
- Communication disruptions between areas of the brain. Your brain relies on intricate networks of connections between its various areas. Experts suspect that schizophrenia happens because those connections deteriorate.
Experts believe several risk factors contribute to developing schizophrenia. Those risk factors include genetic mutations you inherit from one or both parents, exposure to certain chemicals or substances, complications during pregnancy and recreational drug use. However, experts have yet to uncover any confirmed triggers or causes for this condition.
Is it contagious?
Schizophrenia isn't contagious. It doesn’t spread from person to person.
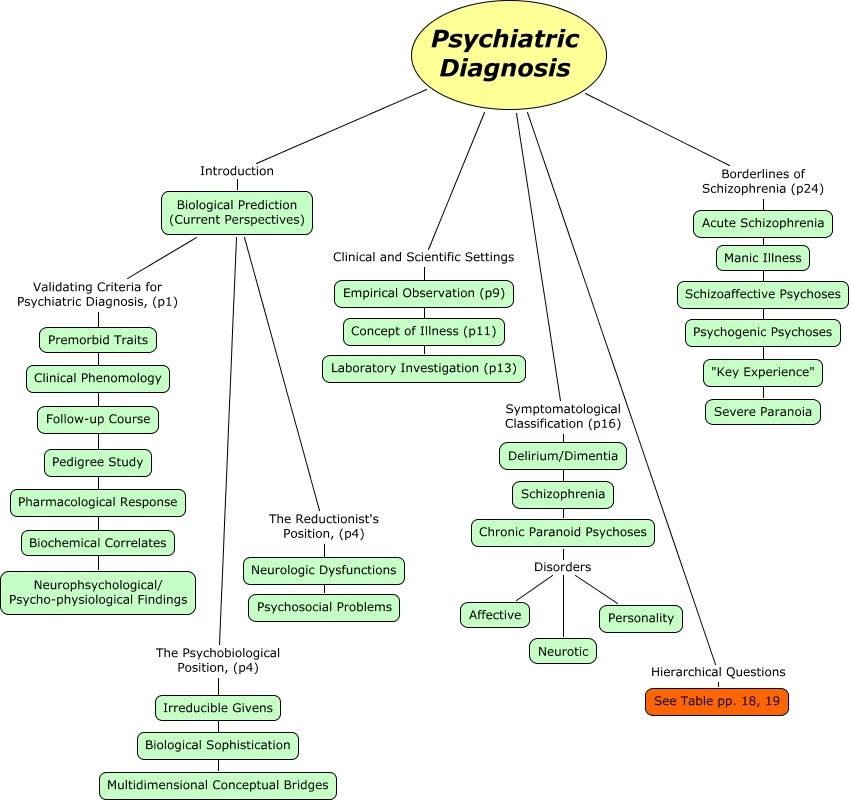
Diagnosis and Tests
How is it diagnosed?
A healthcare provider, usually a mental health specialist like a psychiatrist, diagnoses schizophrenia using a combination of tools and techniques.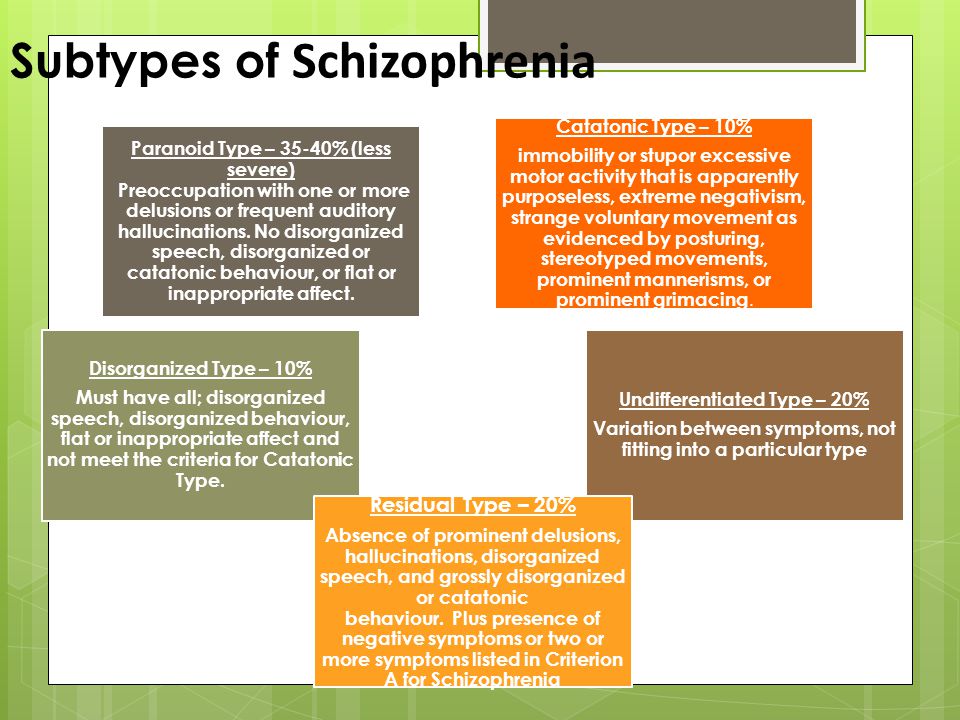 Some of the techniques involve analyzing your medical and personal history, asking you questions about your experiences and symptoms, and observing your behavior and actions.
Some of the techniques involve analyzing your medical and personal history, asking you questions about your experiences and symptoms, and observing your behavior and actions.
Combining those methods is necessary because diagnosing schizophrenia requires the following:
- At least two of the five main symptoms.
- Main symptoms that have lasted at least one month, and overall effects that have lasted at least six months.
- Disruption in your social or work life.
What tests will be done to diagnose this condition?
Many possible tests can happen with schizophrenia. While none can diagnose the condition directly, they can rule out other conditions and problems that cause similar symptoms.
The possible tests include:
- Imaging tests. These can include computerized tomography (CT) scans, magnetic resonance imaging (MRI) scans and other imaging tests.
- Blood, urine and cerebrospinal fluid (spinal tap) tests.
 These tests look for chemical changes in bodily fluids, as well as heavy metal poisoning, infections and more.
These tests look for chemical changes in bodily fluids, as well as heavy metal poisoning, infections and more. - Brain activity testing. An electroencephalogram (EEG) analyzes and records the electrical activity in your brain, which can rule out seizures or epilepsy.
Management and Treatment
How is it treated, and is there a cure?
Schizophrenia is almost always treatable, but it isn’t curable. Some people can recover from schizophrenia entirely and never have it return. However, experts consider people in that situation “in remission” because there’s no way to predict if it will or won’t return.
Treating schizophrenia generally involves multiple methods applied in sequence or at the same time. Medication, therapy and self-management techniques are common, and all three can help treat this condition when applied consistently and effectively. Diagnosing and treating this condition sooner rather than later also increases the likelihood of a good outcome.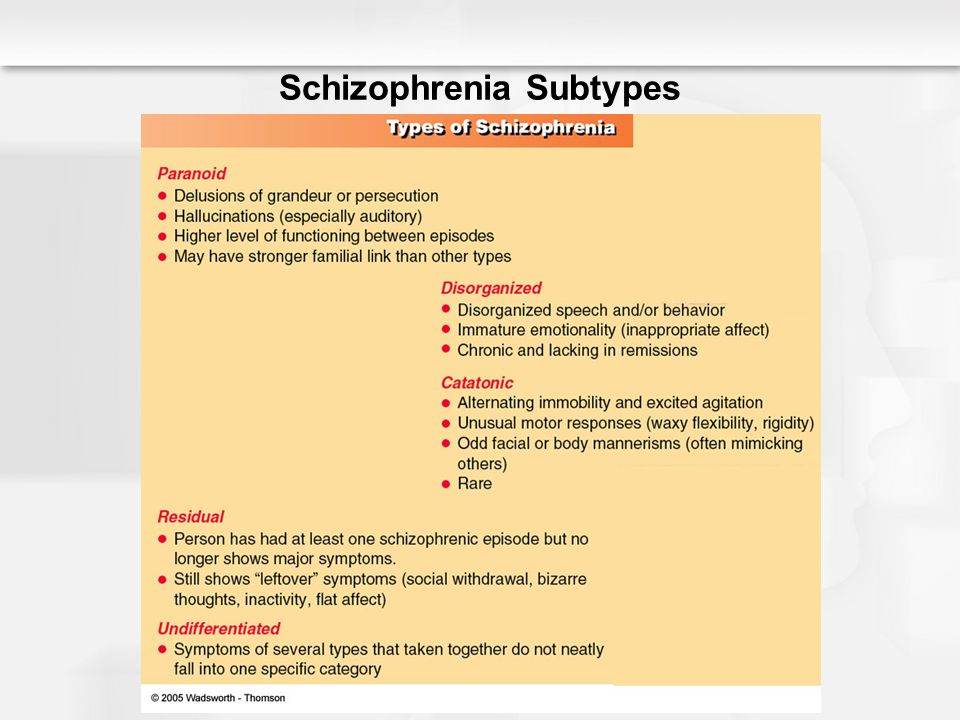
What medications or treatments are used?
Medication is a cornerstone of most treatment plans for schizophrenia. People with schizophrenia often undergo other treatments that complement or enhance the effects of medications.
There are two main types of medications that treat schizophrenia, typical antipsychotic medications and atypical antipsychotic medications. Other medications may also help treat schizophrenia directly or help reduce the side effects of antipsychotic medications.
Other treatments or techniques that may help include:
- Psychotherapy: Mental health therapy can help people with schizophrenia understand their condition and adapt to it better. It can also help them manage mental health concerns that may happen with or because of schizophrenia.
- Electroconvulsive therapy (ECT): This is especially helpful when schizophrenia resists medications, or a person has such severe psychosis symptoms that they are a danger to themselves or others.

How do I take care of myself or manage the symptoms?
You should never try to self-diagnose schizophrenia or diagnose it in a loved one. Schizophrenia isn't always an easy condition to diagnose, and it takes training and experience to diagnose it accurately. This condition also involves symptoms that can happen with other conditions, such as paranoid personality disorder or delusional disorder. Because of all these factors, a healthcare provider should be the one to diagnose this condition.
How soon after treatment will I feel better?
If you have questions about how long it will take before you notice the effects of your treatments, the best source of information is your healthcare provider. Your provider is the most accurate source of information because they can consider the factors in your life that might affect when you notice the effects of treatments. They can also talk to you about other available treatment options when initial treatments aren't effective.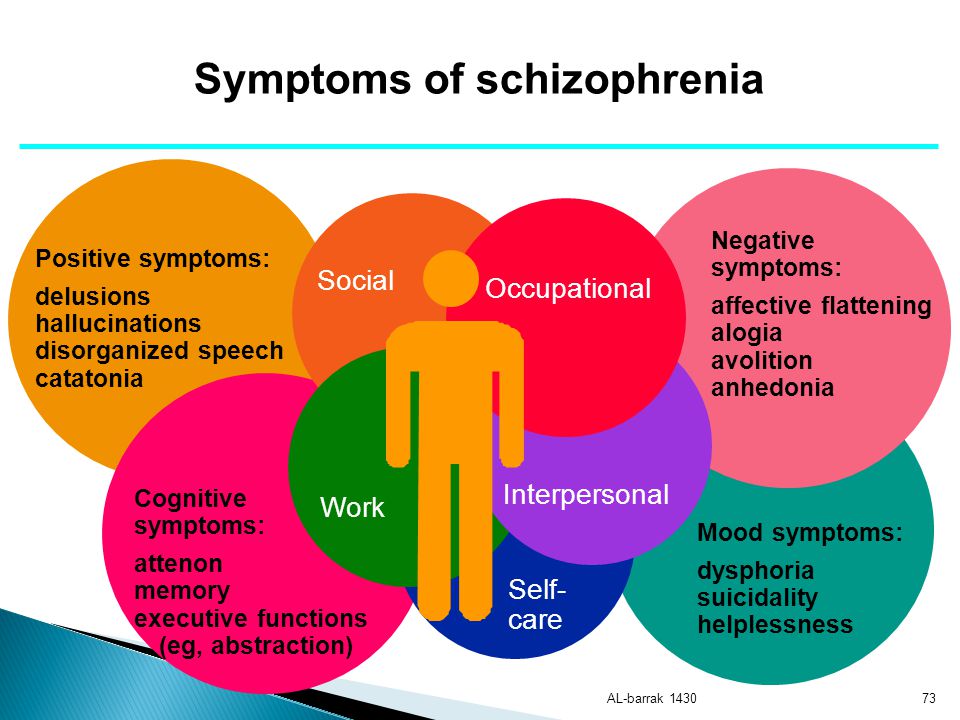
Prevention
How can I reduce my risk or prevent this condition?
Schizophrenia happens unpredictably, so it's impossible to prevent it or reduce your chances of developing it.
Outlook / Prognosis
What can I expect if I have this condition?
Schizophrenia is a condition that can cause severe disruptions in a person’s life because it affects their connection to reality. That means a person with schizophrenia has trouble knowing what’s real and what isn’t. That can be a scary and very disorienting feeling.
When a person experiences paranoia that feeds into delusions and hallucinations, it’s common for them to feel afraid and unable to trust others. A person with schizophrenia may see others trying to help them and mistake their efforts as attempts to cause harm.
With treatment, schizophrenia is often manageable. Without treatment, or if there are long delays or gaps in treatment, people with schizophrenia are more likely to struggle with the effects of this condition.
This can have severe or even dangerous impacts on a person’s life, increasing the risk of problems with maintaining relationships and holding a job. That can lead to problems like housing insecurity or social isolation. People with schizophrenia also have a higher risk of dying by suicide, which means treatment can be life-saving, not just helpful.
How long does schizophrenia last?
Schizophrenia is a lifelong, incurable condition. Some people may have only one episode of schizophrenia in their lifetime. However, healthcare providers consider these cases “in remission” instead of cured or resolved because the symptoms can return unpredictably.
Living With
How do I take care of myself?
Taking care of yourself and managing schizophrenia is possible, especially when people with this condition build a strong, trusting relationship with a healthcare provider and their loved ones. Some of the most important things you can do to take care of yourself include:
- Take your medication as prescribed (and don’t stop taking it without first talking to your provider).
- See your provider as recommended (these visits can help with adjusting medication or treatment plans to help you best).
- Don’t ignore or avoid your symptoms.
- Avoid alcohol and recreational drug use (these can worsen your symptoms or cause other problems).
- Consider seeking support.
- Build relationships with people you trust — especially loved ones and your healthcare provider — and don’t isolate yourself from them.
When should I see my healthcare provider?
You should see your healthcare provider as recommended, or if you notice a change in your symptoms or the effectiveness of your medication(s).
When should I go to ER?
You should go to the ER or call 911 (or your local emergency services number) if you have thoughts about harming yourself, including thoughts of suicide or about harming others. If you have thoughts like this, you can call any of the following:
- National Suicide Prevention Lifeline (United States).
 To call this line, dial 1-800-273-TALK (1-800-273-8255).
To call this line, dial 1-800-273-TALK (1-800-273-8255). - Local crisis lines. Mental health organizations and centers in your area may offer resources and help through crisis lines.
- 911 (or your local emergency services number): You should call 911 (or the local emergency services number) if you feel like you’re in immediate danger of harming yourself. Operators and dispatchers for 911 lines can often help people in immediate danger because of a severe mental crisis and send first responders to assist.
Frequently Asked Questions
What can I do if a loved one shows signs of schizophrenia or a similar condition?
Because people with schizophrenia often can't recognize their symptoms or condition, they often don't believe they need medical care or treatment. That can be frustrating or frightening for both the person with the symptoms and those who care about them.
If you notice a loved one showing signs of schizophrenia or a related condition, you can try to help them by doing the following:
- Ask how you can help.
 Listening and offering your help keeps a line of communication open and helps them feel connected to others.
Listening and offering your help keeps a line of communication open and helps them feel connected to others. - Encourage them to see someone who can help. Treatment for schizophrenia, especially medication, can improve a person's symptoms. In many cases, that's enough to help them recognize that they have a medical condition that needs care.
- Don’t judge or argue. People with schizophrenia have trouble recognizing what’s real and what isn’t. Avoid judging them or trying to convince them that they’re experiencing hallucinations or delusions. That may cause them to lose trust or fuel feelings of paranoia.
- Stay calm. Anger and frustration can negatively affect your relationship with a loved one who has schizophrenia. It's also easy for them to feel overwhelmed in noisy or hectic environments. Try to pick quiet and calming environments, and do what you can so they feel as safe and comfortable as possible.
- Get help in emergencies.
 If someone with schizophrenia talks about harming themselves or others, or if they show severe paranoia, agitation or act violently, you should call your local emergency services immediately.
If someone with schizophrenia talks about harming themselves or others, or if they show severe paranoia, agitation or act violently, you should call your local emergency services immediately.
A note from Cleveland Clinic
Paranoid schizophrenia is an outdated term for the condition schizophrenia, but paranoia is still a common part of the symptoms that people experience. Schizophrenia is a disorienting and often frightening condition for people who have it, causing them to lose touch with reality and their ability to tell what’s real and what isn’t.
When people experience paranoia, they may struggle to trust people who want to help. That can make diagnosing and treating this condition very difficult. However, with medical care, especially medications, people with schizophrenia can avoid severe complications and can live fulfilling lives.
FGBNU NTsPZ. ‹‹Endogenous mental illness››
Paranoid schizophrenia occurs most often at the age of 30-35 years (sometimes earlier) and occurs mainly with delusional and hallucinatory disorders.
In the development of the disease, a number of clear stages are noted, described at the end of the last century by V. Magnan (1891) and characterizing the picture of chronic delirium. In the stereotype of the development of delusional syndromes, in typical cases, there is a stage of delirium that is not accompanied by hallucinations and phenomena of mental automatism - paranoid syndrome, stages of paranoid delirium - Kandinsky-Clerambault syndrome and fantastic delirium - paraphrenic syndrome [Kurashev S.V., 1955; Elgazina L. M., 1958; Shumsky N. G., 1958].
Depending on the predominance of delusional disorders or hallucinations in the picture of the disease, delusional and hallucinatory (pseudo-hallucinatory) variants of the course of paranoid schizophrenia are distinguished.
The disease develops gradually, the manifestations of the initial period are diverse: obsessions, psychopathic disorders, depersonalization phenomena, senesto-hypochondriac pictures. Against their background, at first unstable episodic, and later recurring delusional ideas of various content arise.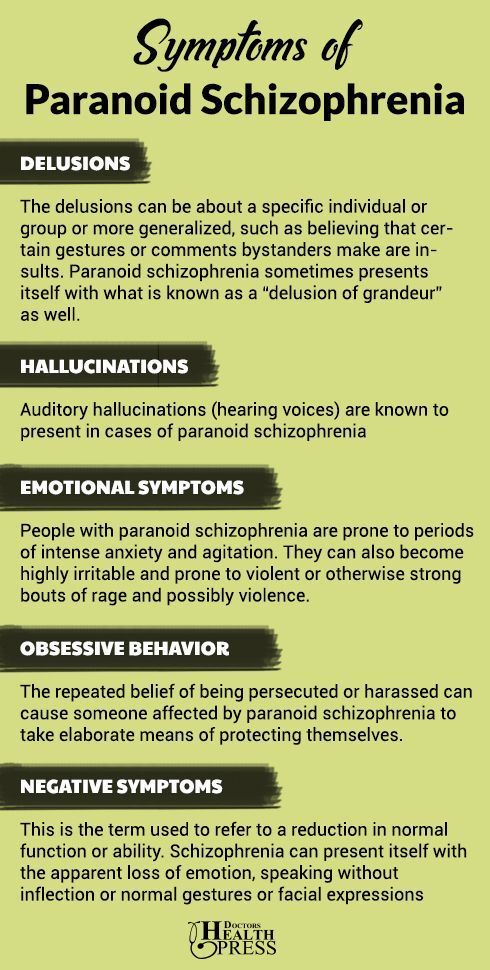 The initial period of the disease with the listed disorders and mild personality changes allows us to characterize it as a stage of a sluggish course, the presence of which does not exclude the further course of the disease according to the laws and stereotype of classical paranoid schizophrenia. But in some patients, already in the initial period of the disease, a narrowing of the circle of interests, rigidity, distrust, and fading of emotional reactions are observed. The duration of this period is different - from 10 years or more.
The initial period of the disease with the listed disorders and mild personality changes allows us to characterize it as a stage of a sluggish course, the presence of which does not exclude the further course of the disease according to the laws and stereotype of classical paranoid schizophrenia. But in some patients, already in the initial period of the disease, a narrowing of the circle of interests, rigidity, distrust, and fading of emotional reactions are observed. The duration of this period is different - from 10 years or more.
The manifestation of the disease is manifested by the development of interpretive delusions with a greater or lesser degree of systematization of delusional ideas.
In the delusional variant of paranoid schizophrenia, the manifest period of the disease is characterized by the formation of an interpretive, highly systematized (paranoid) delusion with a different plot (jealousy, ideas of attitude, invention, reformism, etc.). The possibility of the development of a polythematic delirium (simultaneous existence of several plots of delirium, as a rule, connected with each other) is not excluded.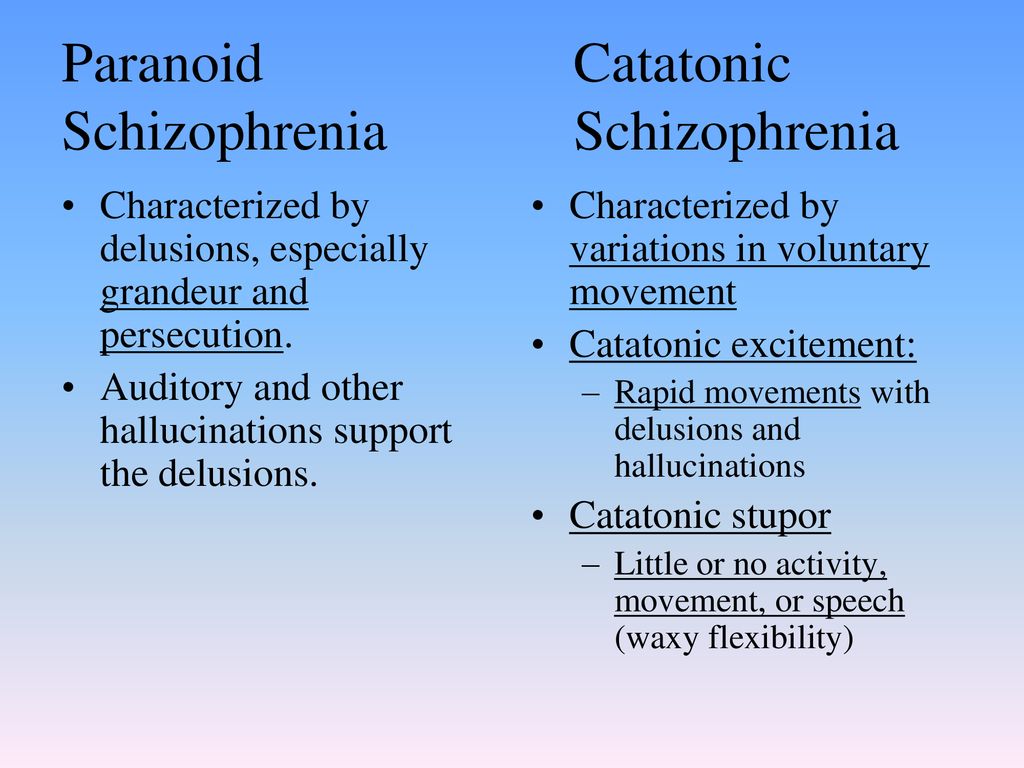 The development of highly systematized syndromes of interpretive delusions occurs gradually, through the stages of overvalued formations and then overvalued delirium [Birnbaum K., 1844].
The development of highly systematized syndromes of interpretive delusions occurs gradually, through the stages of overvalued formations and then overvalued delirium [Birnbaum K., 1844].
The formation of an interpretive delusion with a high degree of systematization is accompanied by a high activity of patients: jealous people do everything possible to search for and expose their imaginary rivals, patients with delusions of reformism or invention turn to various authorities in order to immediately implement their ideas, patients with delusions of persecution seek to discover their enemies. Due to the fact that the content of delusions often reflects real life situations and conflicts, the circle of supporters of patients who naturally do not understand the painful nature of the patient's experiences is revealed and expanded. This circle involves not only individuals, but government agencies and law enforcement agencies.
With the expansion of the plot of delirium, ideas of reassessment of one's personality and capabilities appear.
In some cases, the interpretive mechanism of delusional formation persists throughout the course of the disease. It differs in that the paraphrenia following immediately after this stage of the disease is not accompanied by the development of mental automatisms.
Sometimes psychotic states characterized by a high degree of systematization of delusions (paranoid syndromes) drag on for a sufficiently long period. Such cases are described in the literature as an independent variant of paranoid schizophrenia - paranoid schizophrenia. A state with paranoid delusions, sufficient stabilization of the picture and mild personality changes has a number of features, and in these cases a distinction is required from paranoid states of non-schizophrenic origin.
In the hallucinatory variant of paranoid schizophrenia, the states with interpretive delusions are shorter, the delusions do not reach a high degree of systematization. It is formed relatively quickly by the type of crystallization of delirium or sudden insight, which is accompanied by a subjective feeling of relief and the disappearance of internal tension.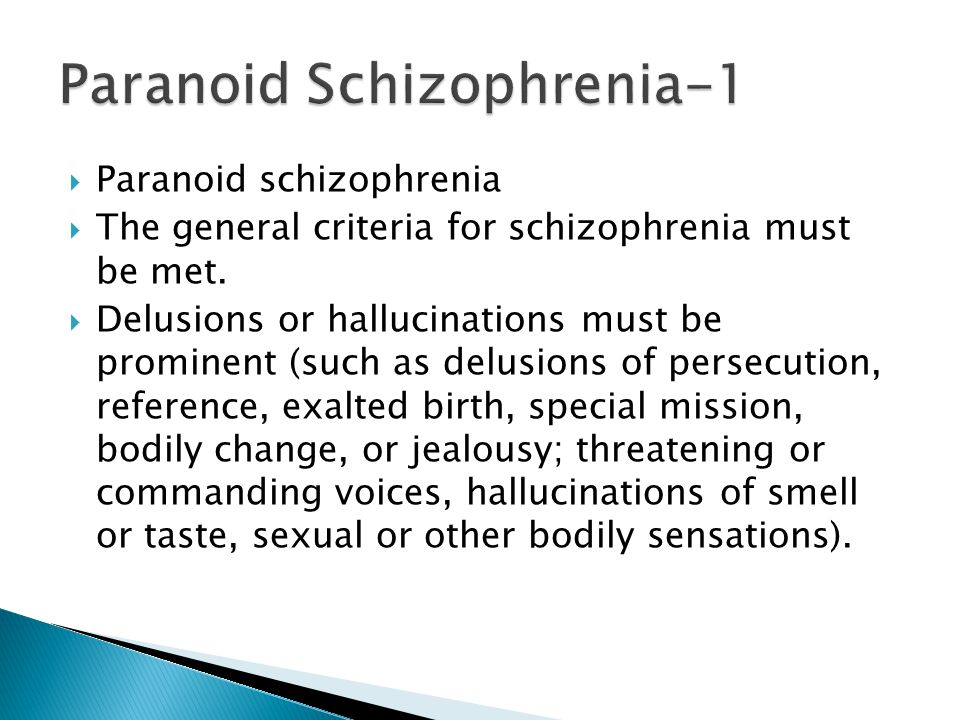
In the initial period of the hallucinatory variant of paranoid schizophrenia, neurosis-like and psychopathic disorders can be observed [Elgazina L. M., 1958].
The development of the Kandinsky-Clerambault syndrome, both in cases of delusional and hallucinatory variants of paranoid schizophrenia, is preceded by an acutely developing state of anxious-fearful arousal with verbal hallucinations, mental automatisms that first appear, a sense of impending danger and fear. Its formation occurs in different ways: in some cases, along with the ideas of persecution and influence, ideational or other types of automatisms develop with a gradual expansion of their range and the formation of a total mastery syndrome; in other cases, its development is limited to delusional disorders and one or two types of mental automatisms, without a tendency to their further expansion.
In the hallucinatory variant of paranoid schizophrenia, verbal illusions arise, individual verbal hallucinations such as hails and swear words addressed to the patient, followed by the development of a true verbal hallucinosis of commentary content, then the voices become “made”, begin to sound in the head, i.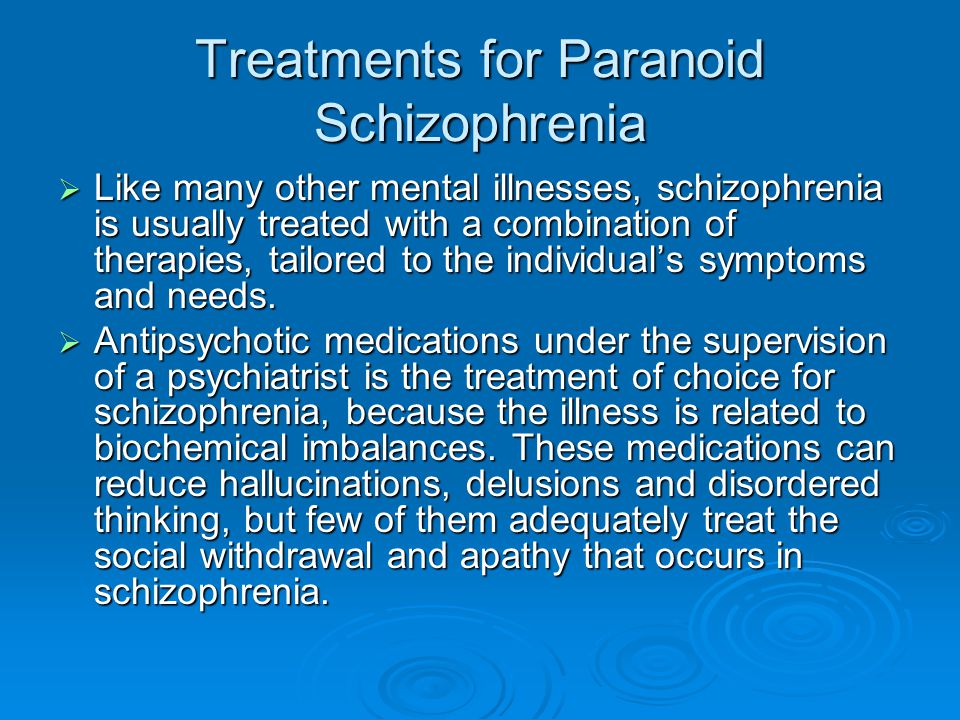 e. transform into pseudohallucinations. Often this transition is not accompanied by signs of an aggravation of the picture of psychosis, and sometimes one has to observe anxiety, fear, episodes of acute sensual delirium. The abundance of pseudohallucinations is combined with individual mental automatisms, however, they occupy a secondary place in the picture of the state, while the core disorder is verbal pseudohallucinosis. Delusional disorders that occur in the picture of the state are closely related to the content of hallucinosis (hallucinatory delusions). Pseudohallucinosis is highly resistant to therapy.
e. transform into pseudohallucinations. Often this transition is not accompanied by signs of an aggravation of the picture of psychosis, and sometimes one has to observe anxiety, fear, episodes of acute sensual delirium. The abundance of pseudohallucinations is combined with individual mental automatisms, however, they occupy a secondary place in the picture of the state, while the core disorder is verbal pseudohallucinosis. Delusional disorders that occur in the picture of the state are closely related to the content of hallucinosis (hallucinatory delusions). Pseudohallucinosis is highly resistant to therapy.
The next stage in the development of paranoid schizophrenia is paraphrenia. Some researchers point out that the development of paraphrenia is preceded by a state of anxiety-fearful excitement, similar to that observed at the moment of transformation of a paranoid state into a hallucinatory-paranoid one. But these observations are not supported by clinical practice. The formation of paraphrenia occurs gradually and the first signs of paraphrenia appear in the picture of the Kandinsky-Clerambault syndrome.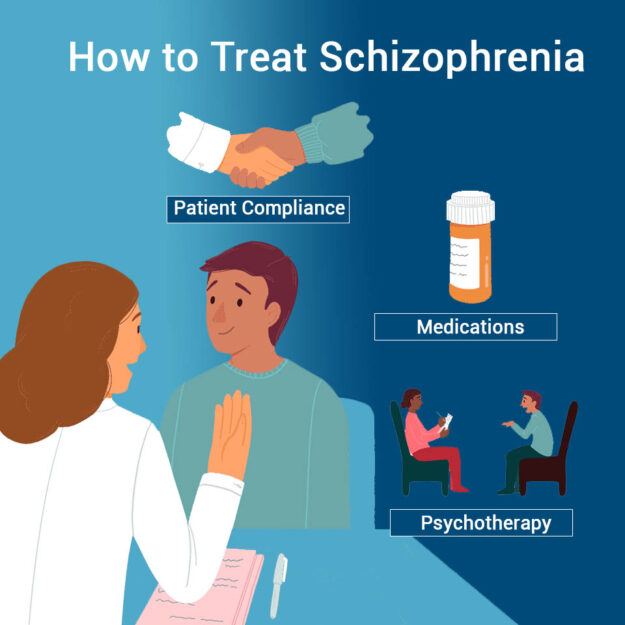
The beginning of the transformation of the syndrome, as a rule, is a change in the nature of the impact experienced by the patient - harmful to "benevolent". This happens against the backdrop of a somewhat elated mood, when patients begin to talk about the emergence of their unusual abilities to recognize the thoughts of others and influence their well-being. There is a symptom of “unwinding of memories”, accompanied by pseudo-hallucinatory memories (according to K. Kahlbaum “memory hallucinations”): the patient is “forced” to recall the events of the past, their details, which were actually absent; they emerge in the patient's memory with a feeling that the oblivion has passed and he again recalled the details of the events of past years. Then, ideas of greatness of fantastic, absurd content, typical of paraphrenia, arise: patients claim that they are special personalities, they are entrusted with special missions, that they influence the fate of people and the universe; patients believe that in the world there is a struggle between the supporters of the patient and his opponents. However, unlike acute paraphrenic conditions, the patient does not see signs of this struggle in his environment. In the pseudohallucinatory variant of paranoid schizophrenia, the paraphrenic state acquires a picture of pseudohallucinatory paraphrenia with the development of delusions that are identical in content to pseudohallucinations. The possibility of developing confabulatory disorders of fantastic content (confabulatory paraphrenia) is not ruled out.
However, unlike acute paraphrenic conditions, the patient does not see signs of this struggle in his environment. In the pseudohallucinatory variant of paranoid schizophrenia, the paraphrenic state acquires a picture of pseudohallucinatory paraphrenia with the development of delusions that are identical in content to pseudohallucinations. The possibility of developing confabulatory disorders of fantastic content (confabulatory paraphrenia) is not ruled out.
The end state of paranoid schizophrenia is characterized by "schizophasia". Its first sign is a symptom of a monologue, manifested by infinitely long answers to simple questions, when the answers (for example, about well-being) contain information that has nothing to do with the content of the question. In the future, the actual phenomenon of schizophasia may develop - grammatically correct speech, devoid of any meaning and content. The appearance of neologisms in speech is characteristic. Quite often in such speech of patients nevertheless it is possible to catch separate fragments of paraphrenic delirium.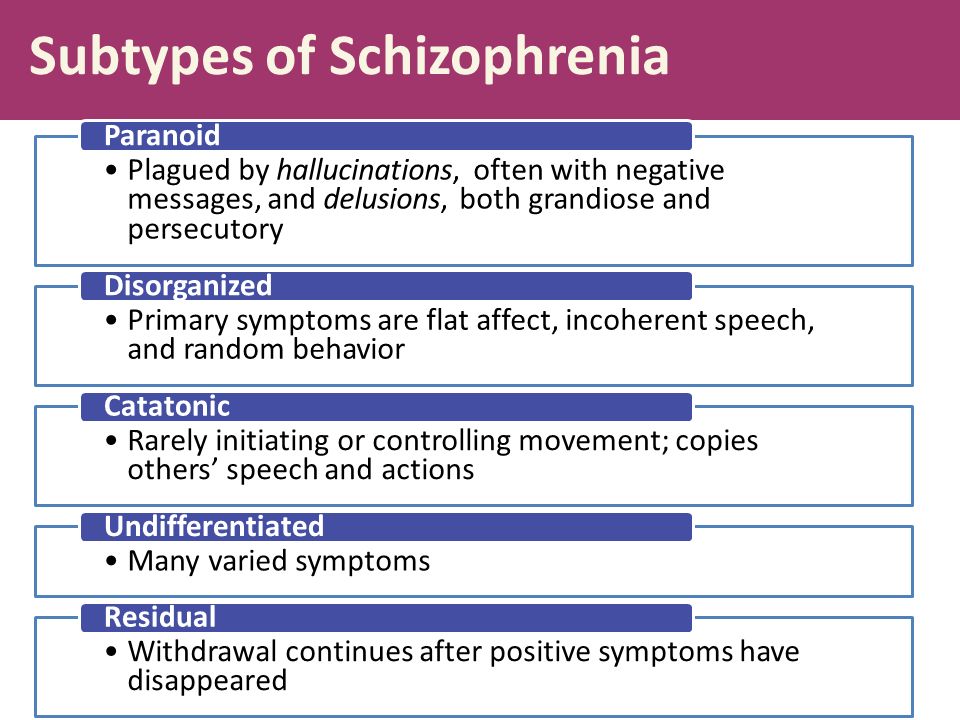 The behavior of patients with schizophasia is outwardly correct. Patients can perform even simple work.
The behavior of patients with schizophasia is outwardly correct. Patients can perform even simple work.
Sometimes in patients at the paraphrenic stage of the disease, short states of arousal may occur, which are explained by the revival of the "extinct" paraphrenic delirium.
The duration of the course of paranoid schizophrenia does not fit into certain periods, since certain stages of the development of the disease, primarily the initial one, can be delayed. However, the pseudo-hallucinatory variant is more fleeting; the duration of the disease in these cases is also affected by the therapeutic resistance of many patients, which complicates not only the relief, but also the stabilization of the disease process at the remote stages.
Symptoms of paranoid schizophrenia, signs of paranoid syndrome - Allianz Central Medical Center
Paranoid schizophrenia is a form of schizophrenia characterized by hallucinatory-delusional symptoms of persecution and exposure. The main criteria for schizophrenia are also met:
The main criteria for schizophrenia are also met:
- loss of unity of mental functions;
- impaired thinking;
- impoverishment of the emotional-volitional sphere.
In articles about paranoid schizophrenia, we use both the medical term "paranoid" and the established language "paranoid", although the first is the correct one.
In paranoid schizophrenia, the symptoms alone do not warrant a diagnosis. It is important to evaluate the development of symptoms in dynamics, find out the order of their appearance over time, and establish causal relationships. Therefore, the main diagnostic method is a clinical and anamnestic examination by a psychiatrist.
The main method for diagnosing paranoid schizophrenia is a clinical and anamnestic examination by a psychiatrist.
A competent conversation with a doctor, which is also carried out with relatives and friends of the patient, makes it possible to clarify:
- Heredity, life history of the patient and his family.
- The debut of the disease, the factors that provoked it and the events that coincided with the debut in time.
- The history of the development of the disease, and it is important to separate the manifestations of the disease from other life situations. This helps to understand the dynamics of the process and predict the further course of the disease.
The doctor always assesses the current condition of the patient according to the following signs:
- delusions and hallucinations that characterize the paranoid syndrome;
- disorders of thinking and speech;
- violations of the emotional-volitional sphere;
- personality traits;
- associated mental and psychological phenomena that may play a role in the process of diagnosis and treatment.
A conversation with a doctor is a key diagnostic method, so you should not neglect communication with a psychiatrist or describe complaints superficially.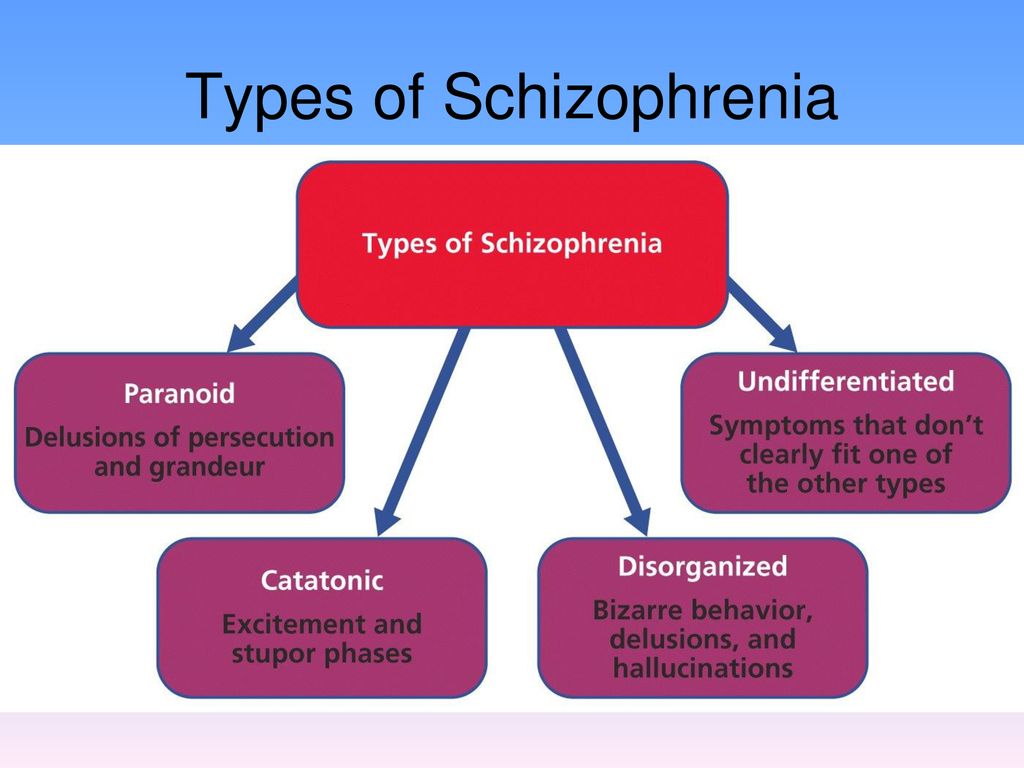
Additional methods for diagnosing paranoid schizophrenia
Any diagnosis in psychiatry is never made without the conclusion of a pathopsychological study conducted by a clinical psychologist. The opinion of a second specialist is necessary for an accurate diagnosis. During the study, the pathopsychologist evaluates the patient's cognitive processes - thinking, memory, attention, his emotional state, motivation and ability to plan. The results allow for differential diagnosis, as well as to track the dynamics of the disease (before and after treatment) and give an objective assessment of therapy.
Modern diagnostic methods - Neurotest and Neurophysiological test system - allow not only to make an accurate diagnosis, but also to give an objective assessment of drug therapy. This allows you to quickly adjust the drugs and their dosages.
For the diagnosis of paranoid schizophrenia, there are modern methods: laboratory (Neurotest) and instrumental (Neurophysiological test system).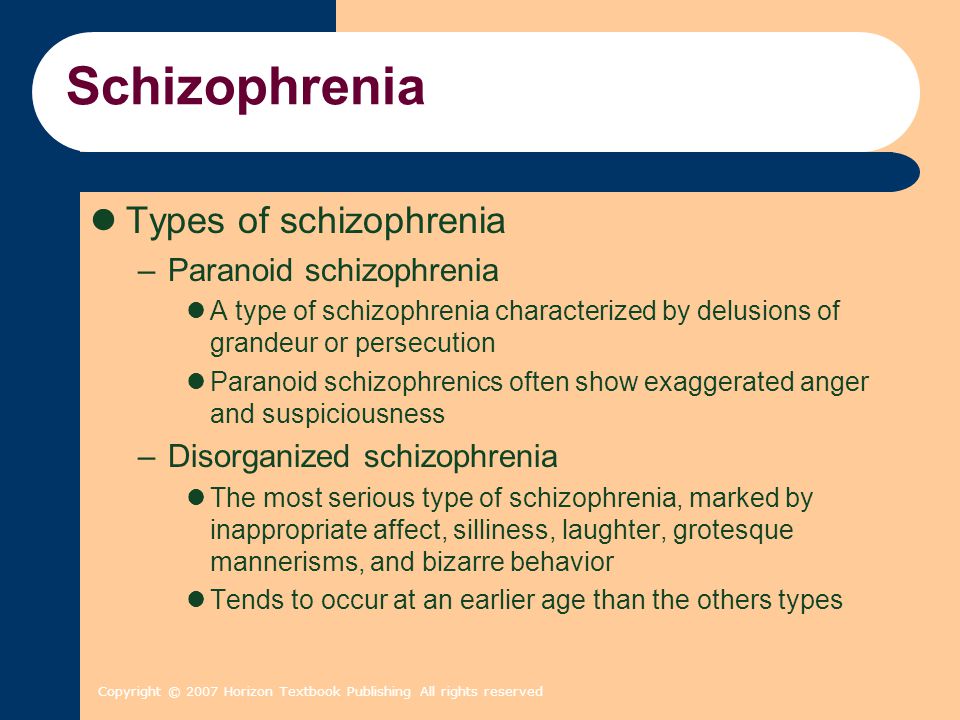 These techniques make it possible to determine the severity of the process, to conduct a differential diagnosis with diseases of a neurotic and affective nature, and therefore, to select a more adequate therapy.
These techniques make it possible to determine the severity of the process, to conduct a differential diagnosis with diseases of a neurotic and affective nature, and therefore, to select a more adequate therapy.
Paranoid schizophrenia: symptoms and signs
The main manifestation of the disease is paranoid delusions (the correct modern name is "paranoia") - painful, unreasonable ideas about stalking the patient on the street and in transport, complexly organized surveillance. Persecutors can leave conventional signs and ciphers for each other and the patient in newspapers, on TV. Gradually, the delirium becomes more complicated, conspiracy theories appear. Delusions include fictitious and real structures, well-known organizations, high-ranking people who wish evil, cause damage.
Important
The disease does not allow a person to distinguish reality from pathological fantasies. A person in this state is confused, anxious and can harm himself and others.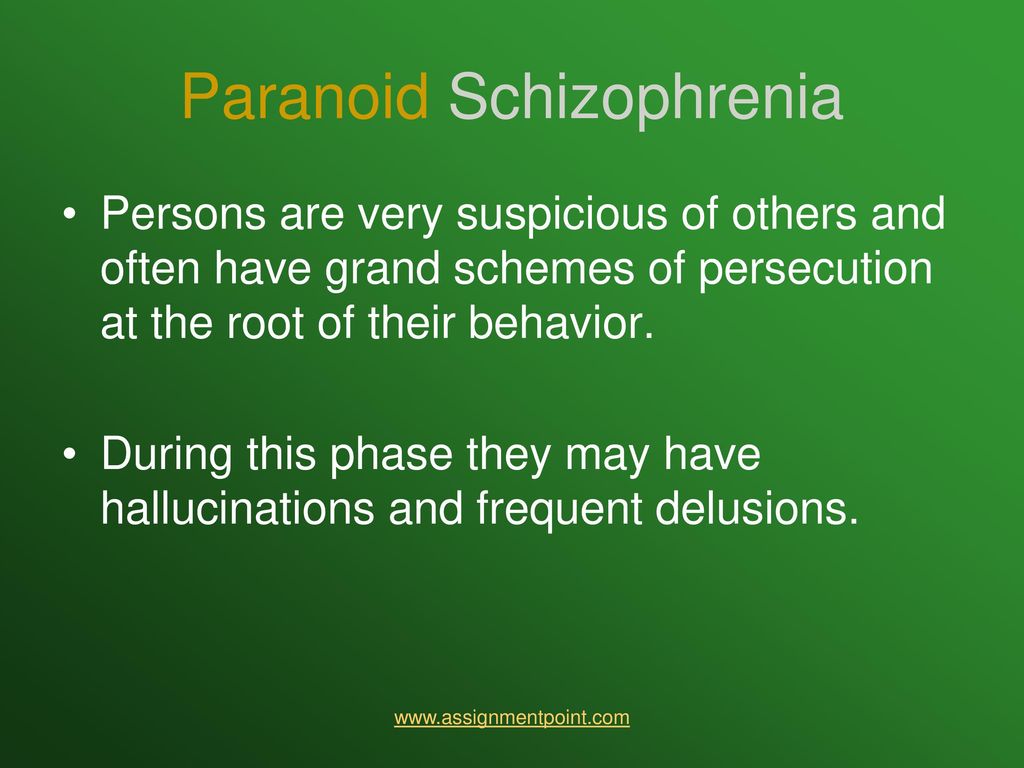
Without treatment, paranoid symptoms become more complicated and completely take over the patient's life. Hallucinations join, which confirm pathological ideas. “Voices” appear: first, “calls”, and then commenting and ordering. They can at any time order the patient to harm themselves and others.
Signs of paranoid schizophrenia in women
During the course of the disease, paranoid schizophrenia does not differ fundamentally in symptoms and signs in women and men. For women, family, reproduction, and appearance are important, so these ideas can be reflected in delusions and hallucinations.
In a woman, the paranoid syndrome is characterized by ideas of harm to the child. She is sure that her life and health, her husband, children, close relatives are threatened. "Detractors" may remain unknown, but often patients directly point to those who cause them suffering - neighbors, relatives, work colleagues, dignitaries. However, for many men, these topics are also important and are presented in painful experiences.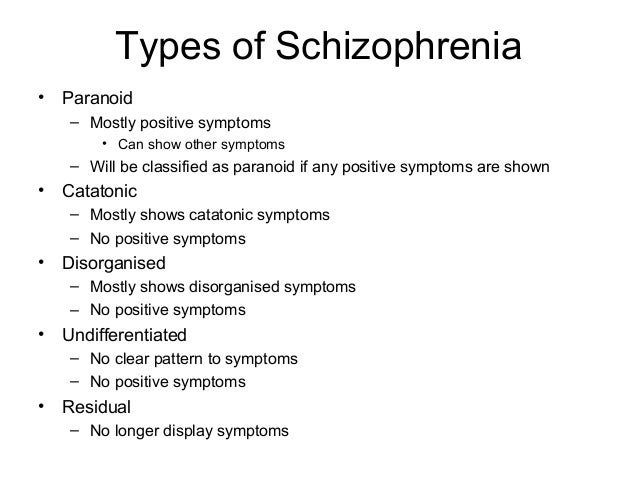
Paranoid schizophrenia: symptoms and signs in men
If you try to isolate the signs of paranoid schizophrenia in a man, then ideas of espionage, persecution by enemies, lovers of a wife or lover, as well as ideas related to work and colleagues come to the fore.
Important
There are no typical symptoms of paranoid schizophrenia - typically "male" or typically "female". A diagnosis can only be made by a competent doctor who has conducted a detailed clinical and anamnestic examination and used additional diagnostic methods.
Unfortunately, the outcome of a neglected disease in both women and men is the same - an increase in a schizophrenic personality defect. First, there is a disorder of speech function - speech in a monologue, endless fruitless arguments on philosophical and near-scientific topics, "speech okroshka", when speech becomes just a set of words. At the same time, there is a growing decrease in initiative and productivity, patients stop working and generally leave their homes.