How does abilify help depression
Abilify Oral: Uses, Side Effects, Interactions, Pictures, Warnings & Dosing
Warnings:
If you are using aripiprazole in combination with other medication to treat depression, also carefully read the drug information for the other medication.
There may be a slightly increased risk of serious, possibly fatal side effects (such as stroke, heart failure, fast/irregular heartbeat, pneumonia) when this medication is used by older adults with dementia. This medication is not approved for the treatment of dementia-related behavior problems. Discuss the risks and benefits of this medication, as well as other effective and possibly safer treatments for dementia-related behavior problems, with the doctor.
Warnings:
If you are using aripiprazole in combination with other medication to treat depression, also carefully read the drug information for the other medication.
There may be a slightly increased risk of serious, possibly fatal side effects (such as stroke, heart failure, fast/irregular heartbeat, pneumonia) when this medication is used by older adults with dementia. This medication is not approved for the treatment of dementia-related behavior problems. Discuss the risks and benefits of this medication, as well as other effective and possibly safer treatments for dementia-related behavior problems, with the doctor.
... Show More
Uses
Aripiprazole is used to treat certain mental/mood disorders (such as bipolar disorder, schizophrenia, Tourette's syndrome, and irritability associated with autistic disorder). It may also be used in combination with other medication to treat depression. Aripiprazole is known as an antipsychotic drug (atypical type). It works by helping to restore the balance of certain natural chemicals in the brain (neurotransmitters).This medication can decrease hallucinations and improve your concentration.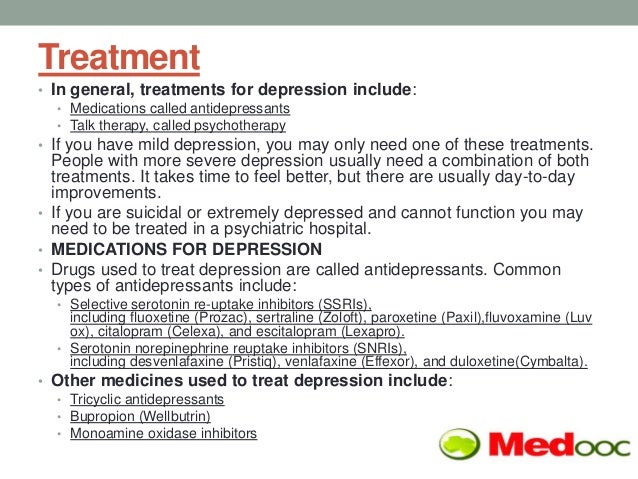 It helps you to think more clearly and positively about yourself, feel less nervous, and take a more active part in everyday life. Aripiprazole can treat severe mood swings and decrease how often mood swings occur.
It helps you to think more clearly and positively about yourself, feel less nervous, and take a more active part in everyday life. Aripiprazole can treat severe mood swings and decrease how often mood swings occur.
How to use Abilify
Read the Medication Guide and, if available, the Patient Information Leaflet provided by your pharmacist before you start taking aripiprazole and each time you get a refill. If you have any questions, ask your doctor or pharmacist.
Take this medication by mouth with or without food as directed by your doctor, usually once daily. The dosage is based on your medical condition, response to treatment, age, and other medications you may be taking. Be sure to tell your doctor and pharmacist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products). To reduce your risk of side effects, your doctor may direct you to start this medication at a low dose and gradually increase your dose. Follow your doctor's instructions carefully.
The manufacturer directs to swallow this medication whole. However, many similar drugs (immediate-release tablets) can be split/crushed. Follow your doctor's direction on how to take this medication.
If you are using the liquid form of this medication, carefully measure the dose using a special measuring device/cup. Do not use a household spoon because you may not get the correct dose.
Do not increase your dose or use this drug more often or for longer than prescribed. Your condition will not improve any faster, and your risk of side effects will increase.
It may take several weeks before you get the full benefit of this drug. Use this medication regularly to get the most benefit from it. To help you remember, take it at the same time each day.
Keep taking this medication even if you feel well. Do not stop taking this medication without consulting your doctor. Some conditions may become worse when this drug is suddenly stopped. Your dose may need to be gradually decreased.
Tell your doctor if your condition does not improve or if it worsens.
Side Effects
See also Warning section.
Dizziness, lightheadedness, drowsiness, nausea, vomiting, tiredness, excess saliva/drooling, blurred vision, weight gain, constipation, headache, and trouble sleeping may occur. If any of these effects last or get worse, tell your doctor or pharmacist promptly.
Dizziness and lightheadedness can increase the risk of falling. Get up slowly when rising from a sitting or lying position.
Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.
Tell your doctor right away if you have any serious side effects, including: fainting, mental/mood changes (such as increased anxiety, depression, suicidal thoughts), trouble swallowing, restlessness (especially in the legs), shaking (tremor), muscle spasm, mask-like expression of the face, seizures, trouble controlling certain urges (such as gambling, sex, eating or shopping), interrupted breathing during sleep.
This medication may rarely make your blood sugar rise, which can cause or worsen diabetes. Tell your doctor right away if you have symptoms of high blood sugar such as increased thirst/urination. If you already have diabetes, check your blood sugar regularly as directed and share the results with your doctor. Your doctor may need to adjust your diabetes medication, exercise program, or diet.
This medication may rarely cause a condition called tardive dyskinesia. In some cases, this condition may be permanent. Tell your doctor right away if you develop any unusual uncontrolled movements (especially of the face, mouth, tongue, arms, or legs).
This medication may rarely cause a very serious condition called neuroleptic malignant syndrome (NMS). Get medical help right away if you have any of the following symptoms: fever, muscle stiffness/pain/tenderness/weakness, severe tiredness, severe confusion, sweating, fast/irregular heartbeat, dark urine, signs of kidney problems (such as change in the amount of urine).
A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: fever, swollen lymph nodes, rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.
This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.
In the US - Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.
In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
Precautions
See also Warning section.
Before taking aripiprazole, tell your doctor or pharmacist if you are allergic to it; or if you have any other allergies. This product may contain inactive ingredients (such as propylene glycol), which can cause allergic reactions or other problems. Talk to your pharmacist for more details.
Talk to your pharmacist for more details.
Before using this medication, tell your doctor or pharmacist your medical history, especially of: problems with blood flow in the brain (such as cerebrovascular disease, stroke), diabetes (including family history), heart problems (such as low blood pressure, coronary artery disease, heart failure, irregular heartbeat), nervous system problems (such as dementia, NMS, seizures), obesity, low white blood cell count (including history of low white blood cell count caused by medications), swallowing problems, breathing trouble during sleep (sleep apnea).
This drug may make you dizzy or drowsy or blur your vision. Alcohol or marijuana (cannabis) can make you more dizzy or drowsy. Do not drive, use machinery, or do anything that needs alertness or clear vision until you can do it safely. Avoid alcoholic beverages. Talk to your doctor if you are using marijuana (cannabis).
This medication may make you sweat less, making you more likely to get heat stroke. Avoid doing things that may cause you to overheat, such as hard work or exercise in hot weather, or using hot tubs. When the weather is hot, drink a lot of fluids and dress lightly. If you overheat, quickly look for a place to cool down and rest. Get medical help right away if you have a fever that does not go away, mental/mood changes, headache, or dizziness.
Avoid doing things that may cause you to overheat, such as hard work or exercise in hot weather, or using hot tubs. When the weather is hot, drink a lot of fluids and dress lightly. If you overheat, quickly look for a place to cool down and rest. Get medical help right away if you have a fever that does not go away, mental/mood changes, headache, or dizziness.
Liquid preparations of this product may contain sugar. Caution is advised if you have diabetes. Ask your doctor or pharmacist about using this product safely.
Older adults may be more sensitive to the side effects of this drug, especially seizures, drowsiness, dizziness, lightheadedness, confusion, tardive dyskinesia, swallowing problems, and other serious (rarely fatal) side effects. (See also Warning section.) Drowsiness, dizziness, lightheadedness, and confusion can increase the risk of falling.
Before having surgery, tell your doctor or dentist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).
During pregnancy, this medication should be used only when clearly needed. Babies born to mothers who have used this drug during the last 3 months of pregnancy may rarely develop symptoms including muscle stiffness or shakiness, drowsiness, feeding/breathing difficulties, or constant crying. If you notice any of these symptoms in your newborn especially during their first month, tell the doctor right away.
Since untreated mental/mood problems (such as bipolar disorder, schizophrenia) can be a serious condition, do not stop taking this medication unless directed by your doctor. If you are planning pregnancy, become pregnant, or think you may be pregnant, immediately discuss with your doctor the benefits and risks of using this medication during pregnancy.
This medication passes into breast milk. Consult your doctor before breast-feeding.
Interactions
Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.
This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.
A product that may interact with this drug is: metoclopramide.
Tell your doctor or pharmacist if you are taking other products that cause drowsiness such as opioid pain or cough relievers (such as codeine, hydrocodone), alcohol, marijuana (cannabis), drugs for sleep or anxiety (such as alprazolam, lorazepam, zolpidem), muscle relaxants (such as carisoprodol, cyclobenzaprine), or antihistamines (such as cetirizine, diphenhydramine).
Check the labels on all your medicines (such as allergy or cough-and-cold products) because they may contain ingredients that cause drowsiness. Ask your pharmacist about using those products safely.
Does Abilify interact with other drugs you are taking?
Enter your medication into the WebMD interaction checker
Overdose
If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call their local poison control center at 1-800-222-1222. Canada residents can call a provincial poison control center. Symptoms of overdose may include: very fast heartbeat, loss of consciousness.
Otherwise, call a poison control center right away. US residents can call their local poison control center at 1-800-222-1222. Canada residents can call a provincial poison control center. Symptoms of overdose may include: very fast heartbeat, loss of consciousness.
Do not share this medication with others.
Laboratory and/or medical tests (such as blood sugar, weight, cholesterol/triglyceride levels) may be performed before you start treatment, periodically to monitor your progress, or to check for side effects. Consult your doctor for more details.
If you miss a dose, take it as soon as you remember. If it is near the time of the next dose, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up.
Store the tablet and the oral liquid at room temperature away from light and moisture. Discard the oral solution 6 months after opening or after the expiration date, whichever comes first. Do not store in the bathroom. Keep all medications away from children and pets.
Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
Images
Next
Related Links
Drug Survey
Are you currently using Abilify?
This survey is being conducted by the WebMD marketing sciences department.
Free RX Coupon
Save up to 80% on your prescriptions.
Available coupons
Save up to 80% on your prescription with WebMDRx
Selected from data included with permission and copyrighted by First Databank, Inc. This copyrighted material has been downloaded from a licensed data provider and is not for distribution, except as may be authorized by the applicable terms of use.
CONDITIONS OF USE: The information in this database is intended to supplement, not substitute for, the expertise and judgment of healthcare professionals. The information is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects, nor should it be construed to indicate that use of a particular drug is safe, appropriate or effective for you or anyone else. A healthcare professional should be consulted before taking any drug, changing any diet or commencing or discontinuing any course of treatment.
The information is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects, nor should it be construed to indicate that use of a particular drug is safe, appropriate or effective for you or anyone else. A healthcare professional should be consulted before taking any drug, changing any diet or commencing or discontinuing any course of treatment.
Aripiprazole (Abilify) | NAMI: National Alliance on Mental Illness
Brand names:
-
- Tablets: 2 mg, 5mg, 10 mg, 15 mg, 20 mg, 30 mg
- Oral disintegrating: 10 mg, 15 mg
- Solution: 1 mg/mL
- Abilify MyCite®
- Tablet with a digestible sensor: 2 mg, 5 mg, 10 mg, 15 mg, 20 mg, 30 mg
- Abilify Maintena®
- Extended-release injectable suspension: 300 mg, 400 mg
- Abilify Aristada® (aripiprazole lauroxil)
- Extended-release injectable suspension: 441 mg, 662 mg, 882 mg, 1064 mg
- Aristada Initio® (aripiprazole lauroxil)
- Extended-release injectable suspension: 675 mg
Generic name: aripiprazole (ay ri PIP ray zole), aripiprazole lauroxil (law rox il)
- Aripiprazole
- Oral tablet: 2 mg, 5mg, 10 mg, 15 mg, 20 mg, 30 mg
- Orally disintegrating tablet: 10 mg, 15 mg
- Oral solution: 1 mg/mL
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
Please review before taking this medication.
What Is Aripiprazole And What Does It Treat?
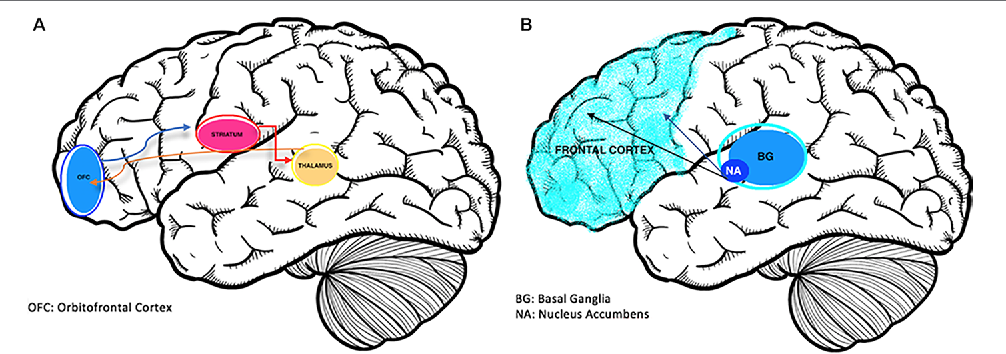
Aripiprazole is a medication that works in the brain to treat schizophrenia. It is also known as a second generation antipsychotic (SGA) or atypical antipsychotic. Aripiprazole rebalances dopamine and serotonin to improve thinking, mood, and behavior.
Symptoms of schizophrenia include:
- Hallucinations — imagined voices or images that seem real
- Delusions — beliefs that are not true (e.g., other people are reading your thoughts)
- Disorganized thinking or trouble organizing your thoughts and making sense
- Little desire to be around other people
- Trouble speaking clearly
- Lack of motivation
Aripiprazole may help some or all of these symptoms.
Aripiprazole is also FDA approved for the following indications:
- Acute treatment of manic or mixed episodes of bipolar disorder (when used alone or with lithium or valproate)
- Maintenance (long-term) treatment of bipolar disorder
- Adjunctive treatment of major depressive disorder.
 This means aripiprazole is used in addition to an antidepressant to help treat depression.
This means aripiprazole is used in addition to an antidepressant to help treat depression. - Irritability associated with autistic disorders
- Tourette's syndrome
This medication sheet will focus primarily on schizophrenia. Find more information about bipolar disorder, depression and autism spectrum disorders here.
Aripiprazole may also be helpful when prescribed “off-label” for borderline personality disorder or drug-induced hyperprolactinemia (elevated prolactin levels caused by other antipsychotics). “Off-label” means that it hasn’t been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending an “off-label” treatment. They should be clear about the limits of the research around that medication and if there are any other options.
What Is The Most Important Information I Should Know About Aripiprazole?
Schizophrenia requires long-term treatment. Do not stop taking aripiprazole, even when you feel better. With input from you, your health care provider will assess how long you will need to take the medicine.
With input from you, your health care provider will assess how long you will need to take the medicine.
Missing doses of aripiprazole may increase your risk for a relapse in your symptoms. Do not stop taking aripiprazole or change your dose without talking to with your health care provider first. For aripiprazole to work properly, it should be taken every day as ordered by your health care provider.
Are There Specific Concerns About Aripiprazole And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider to best manage your medications. People living with schizophrenia who wish to become pregnant face important decisions. This is a complex decision since untreated schizophrenia has risks to the fetus, as well as the mother. It is important to discuss the risks and benefits of treatment with your doctor and caregivers.
Antipsychotic use during the third trimester of pregnancy has a risk for abnormal muscle movements (extrapyramidal symptoms [EPS]) and/or withdrawal symptoms in newborns following delivery. Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.
Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.
In general, infants exposed to SGAs via breast milk should be monitored weekly for the first month of exposure for symptoms, such as appetite changes, insomnia, irritability, or lethargy.
Caution is advised with breastfeeding since aripiprazole does pass into breast milk.
What Should I Discuss With My Healthcare Provider Before Taking Aripiprazole?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you ever had muscle stiffness, shaking, tardive dyskinesia, neuroleptic malignant syndrome, or weight gain caused by a medication
- If you experience side effects from your medications, discuss them with your provider.
Some side effects may pass with time, but others may require changes in the medication
- Any psychiatric or medical problems you have, such as heart rhythm problems, long QT syndrome, heart attacks, diabetes, high cholesterol, or seizures
- If you have a family history of diabetes or heart disease
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment. Your provider can explain how these different treatments work with the medication
- If you are pregnant, plan to become pregnant, or are breast-feeding
- If you smoke, drink alcohol, or use illegal drugs
How Should I Take Aripiprazole?
Aripiprazole tablets and suspension are usually taken 1 time per day with or without food. Typically, patients begin at a low dose of medicine and the dose is increased slowly over several weeks.
The oral dose of aripiprazole usually ranges from 2 mg to 30 mg taken once daily. The dose of aripiprazole maintena extended-release injection ranges from 300 mg to 400 mg given once monthly; the dose of aripiprazole lauroxil extended-release injection ranges from 441 mg to 1064 mg – depending on the dose, it is given once per month, every 6 weeks, or every 2 months. Aripiprazole Maintena requires a two-week oral medication overlap; aripiprazole lauroxil requires a three-week oral overlap. Aripiprazole lauroxil Initio is typically given after an oral dose of aripiprazole along with an aripiprazole lauroxil injection – this allows for a one-day initiation and does not require further oral overlap. Only your health care provider can determine the correct formulation and dose for you.
Use a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member or a friend to remind you or check in with you to be sure you are taking your medication.
What Happens If I Miss A Dose Of Aripiprazole?
If you miss a dose of aripiprazole, take it as soon as you remember, unless it is closer to the time of your next dose. Do not double your next dose or take more than what is prescribed. If you miss an injection, call your doctor or pharmacist right away. Discuss this with your health care provider.
What Should I Avoid While Taking Aripiprazole?
Avoid drinking alcohol or using illegal drugs while you are taking aripiprazole. They may decrease the benefits (e.g., worsen your confusion) and increase adverse effects (e.g., sedation) of the medication.
What Happens If I Overdose With Aripiprazole?
If an overdose occurs call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of aripiprazole does not exist.
What Are Possible Side Effects Of Aripiprazole?
Common side effects
Headache, extrapyramidal symptoms, drowsiness, restlessness, fatigue, sedation, agitation, insomnia, anxiety, weight gain, cholesterol abnormalities, increased glucose, nausea, vomiting, constipation, application site rash (MyCite), tremor
Rare/serious side effects
Rash, dry mouth, muscle aches, seizure, agitation
Aripiprazole may increase the blood levels of a hormone called prolactin. Side effects of increased prolactin levels include females losing their period, production of breast milk and males losing their sex drive or possibly experiencing erectile problems. Long term (months or years) of elevated prolactin can lead to osteoporosis or increased risk of bone fractures.
Side effects of increased prolactin levels include females losing their period, production of breast milk and males losing their sex drive or possibly experiencing erectile problems. Long term (months or years) of elevated prolactin can lead to osteoporosis or increased risk of bone fractures.
Some people may develop muscle-related side effects while taking aripiprazole. The technical terms for these are “extrapyramidal symptoms” (EPS) and “tardive dyskinesia” (TD). Symptoms of EPS include restlessness, tremor, and stiffness. TD symptoms include slow or jerky movements that one cannot control, often starting in the mouth with tongue rolling or chewing movements.
Temperature regulation: Impaired core body temperature regulation may occur; caution with strenuous exercise, heat exposure, and dehydration.
Second generation antipsychotics (SGAs) increase the risk of weight gain, high blood sugar, and high cholesterol. This is also known as metabolic syndrome. Your healthcare provider may ask you for a blood sample to check your cholesterol, blood sugar, and hemoglobin A1c (a measure of blood sugar over time) while you take this medication.
Information on healthy eating and adding exercise to decrease your chances of developing metabolic syndrome may be found at the following sites:
- http://www.helpguide.org/articles/healthy-eating/healthy-eating.htm
- http://www.helpguide.org/home-pages/exercise-fitness.htm
SGAs have been linked with higher risk of death, strokes, and transient ischemic attacks (TIAs) in elderly people with behavior problems due to dementia.
All antipsychotics have been associated with the risk of sudden cardiac death due to an arrhythmia (irregular heart beat). To minimize this risk, antipsychotic medications should be used in the smallest effective dose when the benefits outweigh the risks. Your doctor may order an EKG to monitor for irregular heartbeat.
Neuroleptic malignant syndrome is a rare, life threatening adverse effect of antipsychotics which occurs in <1% of patients. Symptoms include confusion, fever, extreme muscle stiffness, and sweating. If any of these symptoms occur, contact your healthcare provider immediately.
All antipsychotics can cause sedation, dizziness, or orthostatic hypotension (a drop in blood pressure when standing up from sitting or lying down). These side effects may lead to falls which could cause bone fractures or other injuries. This risk is higher for people with conditions or other medications that could worsen these effects. If falls or any of these symptoms occur, contact your healthcare provider.
The U.S. Food and Drug Administration (FDA) is warning that compulsive or uncontrollable urges to gamble, binge eat, shop, and have sex have been reported with the use of aripiprazole. These uncontrollable urges were reported to have stopped when the medicine was discontinued or the dose was reduced. These impulse-control problems are rare, but they may result in harm to the patient and others if not recognized.
Are There Any Risks For Taking Aripiprazole For Long Periods Of Time?
Tardive dyskinesia (TD) is a side effect that develops with prolonged use of antipsychotics. Medications such as aripiprazole have been shown to have a lower risk of TD compared to older antipsychotics, such as Haldol (haloperidol). If you develop symptoms of TD, such as grimacing, sucking, and smacking of lips, or other movements that you cannot control, contact your health care provider immediately. All patients taking either first or second generation antipsychotics should have an Abnormal Involuntary Movement Scale (AIMS) completed regularly by their healthcare provider to monitor for TD.
Medications such as aripiprazole have been shown to have a lower risk of TD compared to older antipsychotics, such as Haldol (haloperidol). If you develop symptoms of TD, such as grimacing, sucking, and smacking of lips, or other movements that you cannot control, contact your health care provider immediately. All patients taking either first or second generation antipsychotics should have an Abnormal Involuntary Movement Scale (AIMS) completed regularly by their healthcare provider to monitor for TD.
Second generation antipsychotics (SGAs) increase the risk of diabetes, weight gain, high cholesterol, and high triglycerides. (See “Serious Side Effects” section for monitoring recommendations).
What Other Medications May Interact With Aripiprazole?
The following medications may increase the levels and effects of aripiprazole:
- The antibiotic clarithromycin (Biaxin®)
- Antidepressants, such as fluoxetine (Prozac®), paroxetine (Paxil®), and nefazodone
- Antifungals, such as fluconazole (Diflucan®), ketoconazole (Nizoral®), and itraconazole (Sporanox®)
- The antiarrhymia agent quinidine
- HIV medications, such as the protease inhibitors indinavir (Crixivan®), ritonavir (Norvir®), saquinavir (Fortovase®, Invirase®), and lopinavir/ritonavir (Kaletra®)
The following medications may decrease the levels and effects of aripiprazole:
- carbamazepine (Tegretol®)
- rifampin (Rifadin®)
How Long Does It Take For Aripiprazole To Work?
It is very important to tell your doctor how you feel things are going during the first few weeks after you start taking aripiprazole.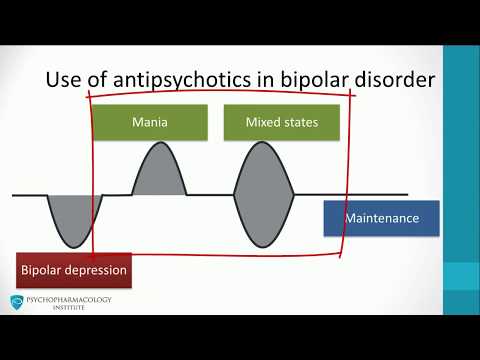 It will probably take several weeks to see big enough changes in your symptoms to decide if aripiprazole is the right medication for you.
It will probably take several weeks to see big enough changes in your symptoms to decide if aripiprazole is the right medication for you.
Antipsychotic treatment is generally needed lifelong for persons with schizophrenia. Your doctor can best discuss the duration of treatment you need based on your symptoms and illness.
- Hallucinations, disorganized thinking, and delusions may improve in the first 1-2 weeks
- Sometimes these symptoms do not completely go away
- Motivation and desire to be around other people can take at least 1-2 weeks to improve
- Symptoms continue to get better the longer you take aripiprazole
- It may take 2-3 months before you get the full benefit of aripiprazole
Summary of FDA Black Box Warnings
Increased mortality in elderly patients with dementia-related psychosis
- Both first generation (typical) and second generation (atypical) antipsychotics are associated with an increased risk of mortality in elderly patients when used for dementia related psychosis.
- Although there were multiple causes of death in studies, most deaths appeared to be due to cardiovascular causes (e.g. sudden cardiac death) or infection (e.g. pneumonia).
- Antipsychotics are not indicated for the treatment of dementia-related psychosis.
Suicidal Thoughts or Actions in Children, Teens, and Young Adults
Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide.
- Patients treated with antidepressants may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking medications. This risk may persist until significant remission occurs.
- Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional.

- All patients being treated with this medication for depression should watch for and notify their healthcare provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Provided by
(July 2022)
©2022 The College of Psychiatric and Neurologic Pharmacists (CPNP) and the National Alliance on Mental Illness (NAMI). CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the College of Psychiatric and Neurologic Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Otrivin,Home
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year.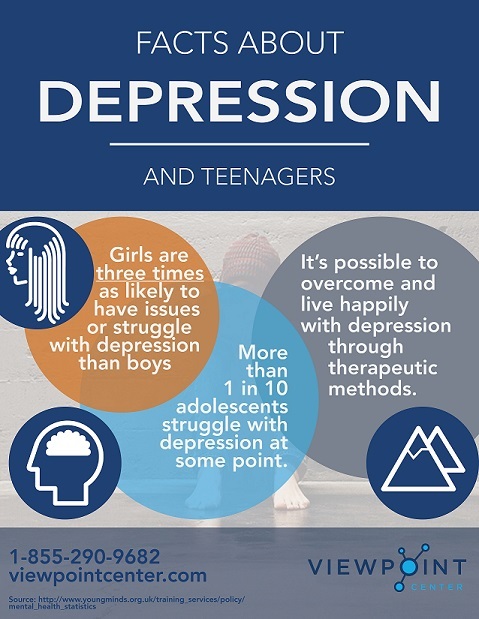 It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by
depression Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases. Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood. Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive.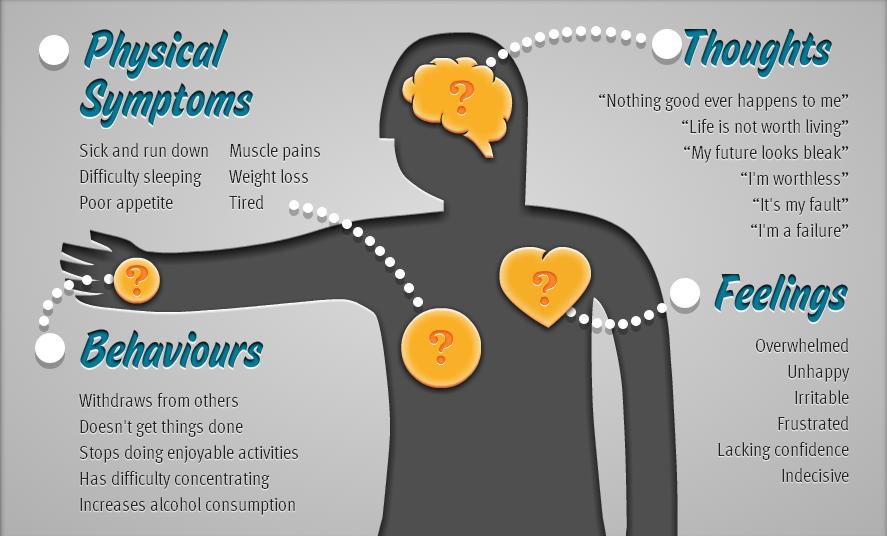 These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
These drugs can only be taken with a doctor's prescription, as many of them are strong stimulants. Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, you need to take remedy, without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
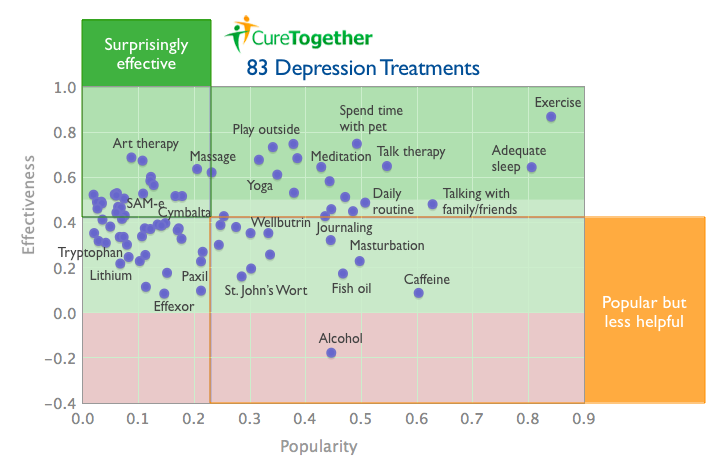
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors. The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No relation to blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters. A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
- Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.
Pluses
+ Lasting effect comes after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
- Anxiety may increase during the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).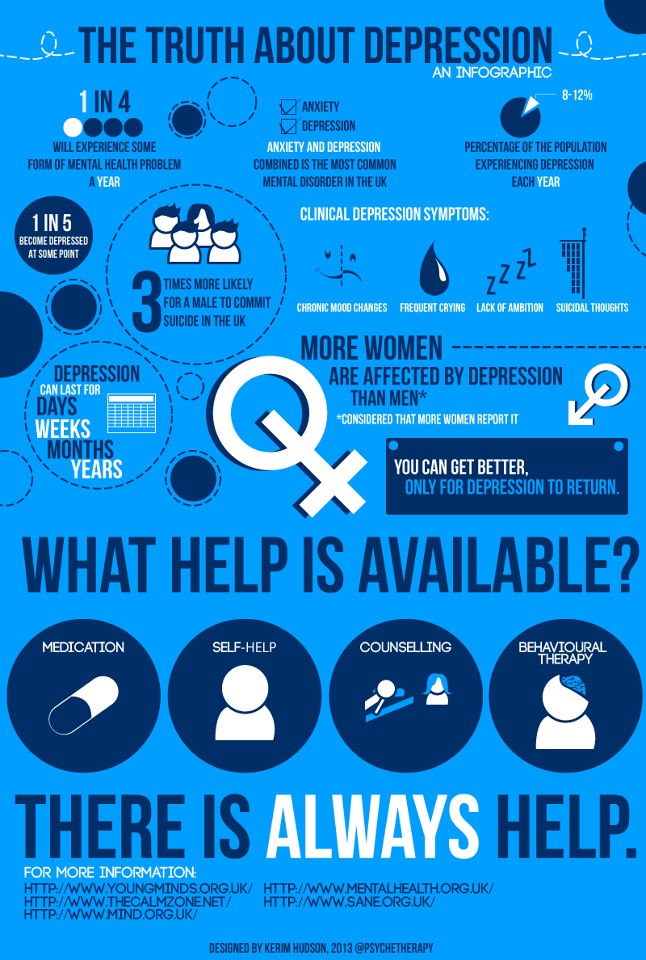
+ Works well with most general medicines.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the appointment, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.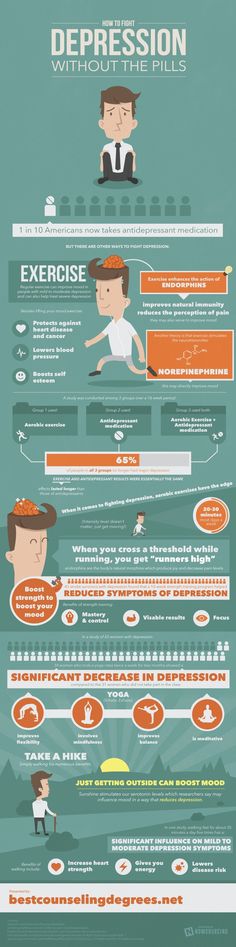
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug. Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.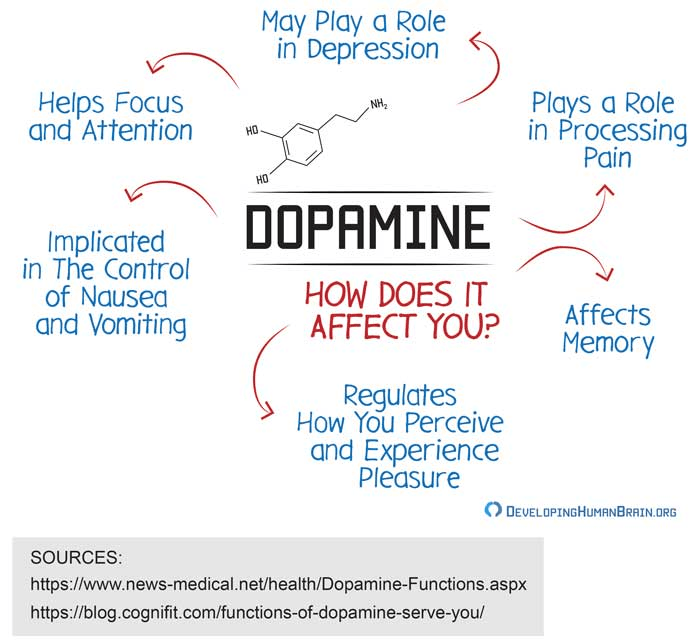
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
— Gastrointestinal disorders, insomnia, agitation are possible.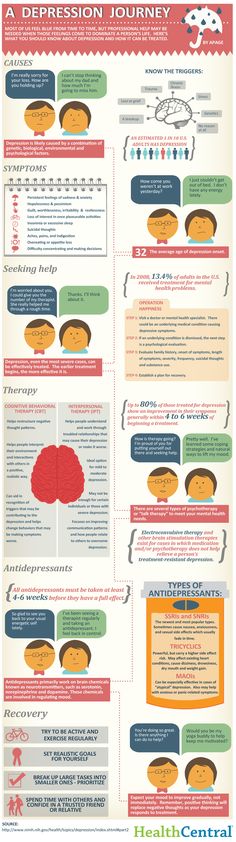
— Use during pregnancy only in extreme cases, incompatible with feeding.
10. Venlafaxine
Belongs to the SNRI group. In addition to blocking the reuptake of serotonin, venlafaxine has a similar effect on another neurotransmitter, norepinephrine. The medicine is prescribed for depressive conditions of various origins, social phobias, anxiety, panic. Usually take 150 mg per day.
Pros
+ Better tolerated by patients than most tricyclics.
+ More pronounced effect than classic SSRIs.
+ Fewer contraindications.
Cons
- Traditional side effects of most antidepressants: nausea, drowsiness, dry mouth, diarrhea or constipation.
- May increase eye pressure.
- The most severe withdrawal syndrome among antidepressant drugs.
This list is not to be used as a recommendation. In any case, consult your doctor before purchasing. Be healthy!
Depression
Russian Academy of Medical Sciences
SCIENTIFIC CENTER FOR MENTAL HEALTH
DEPRESSION (from hope to certainty).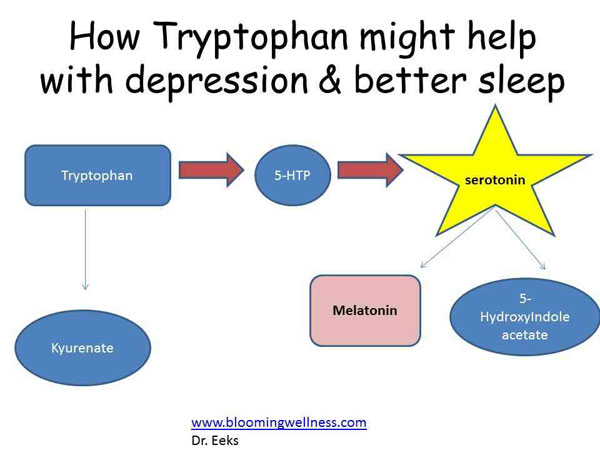
(INFORMATION FOR PATIENTS AND THEIR FAMILIES)
MOSCOW
2008
Oleichik I.V. - Candidate of Medical Sciences, Leading Researcher of the Department for the Study of Endogenous Mental Disorders and Affective States
© 2008, Oleichik I.V.
© 2008, NTsPZ RAMS
The vast experience accumulated by mankind and reflected in many literary works convincingly shows that sadness (sadness, spleen) has always gone side by side with people, being one of the natural human emotions. None of us is immune from failures, illness, breakups, loss of loved ones, financial collapse. Each person can face something inevitable and inevitable, when it seems that life loses its meaning, and despair becomes boundless. However, normally, sadness, sadness and melancholy, as natural reactions to traumatic events, weaken over time and the person's condition returns to normal without special treatment. The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
A depressive state (from the Latin word depressio - suppression, oppression) is a disease that concerns not only an individual specific sick person, but is also a significant burden of modern society, since it is spreading more and more widely in the world, causing enormous damage to the health of the population and the state. economy. And this applies to all countries, regardless of their level of social development. Every year, at least 200 million people in the world fall ill with depression. Perhaps these figures are even higher, since most victims of depression do not seek help because they are not aware of the painfulness of their condition. Scientists have calculated that almost one in five people who have reached adulthood will experience at least one episode of depression during their lifetime.
In the most general sense, a depressive state is one of the possible forms of a person's response to the impact of stress factors. In some cases, depression can be triggered by external negative influences, for example, mental trauma, excessive educational or work overload, infection or other serious somatic disease, traumatic brain injury, changes in the hormonal background, which is especially important for the female body, regular certain medications, such as hormones, blood pressure medications, alcohol or other drug abuse. In other cases, depressive states develop as a manifestation of such mental illnesses, in which the main influence is heredity or characteristics of the nervous system (cyclothymia, dysthymia, manic-depressive psychosis, schizophrenia, etc.). If, based on the description of depressive symptoms set out later in our brochure, you realize that you have indeed developed a depressive state, do not fall into despair, do not “try to control yourself”, remember that depression is not a manifestation of weakness of will or character, on the contrary, weakening of volitional qualities is one of the main symptoms of depression.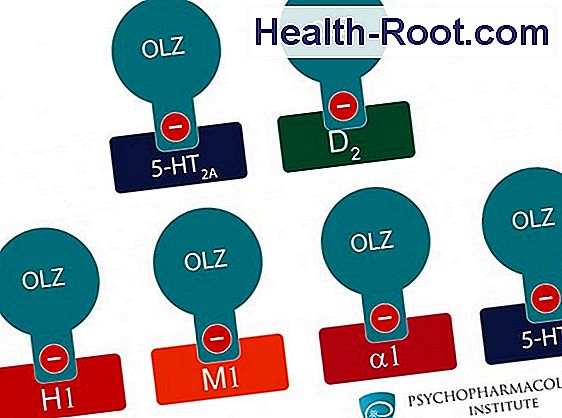 Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
Manifestations of depression
Manifestations of depression can be very different. Depressive states can be manifested by a violation of almost all aspects of mental life: mood, memory, will, activity, which is expressed in the appearance of sadness, sadness, mental and muscle retardation, lasting at least 2 weeks. Depressed mood during depression can manifest itself as mild sadness, sadness, and boundless despair. Often it is accompanied by a feeling of melancholy, unbearable heaviness in the soul, with excruciating pain behind the sternum, a feeling of hopelessness, deep depression, hopelessness, helplessness, despair and uncertainty.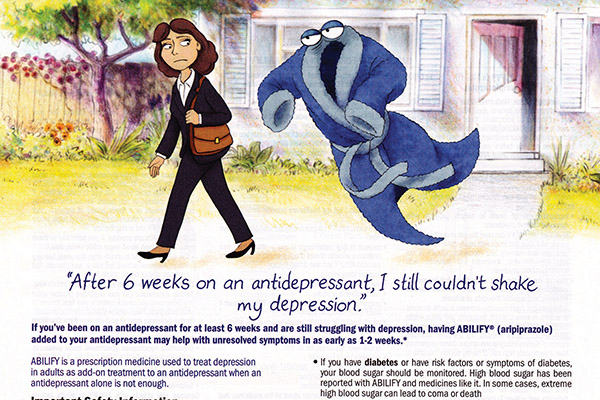 At the same time, the patient is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen the latter. A constant "companion" of a depressive mood is also anxiety of varying severity: from mild anxiety or tension to violent excitement, riot. Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
At the same time, the patient is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen the latter. A constant "companion" of a depressive mood is also anxiety of varying severity: from mild anxiety or tension to violent excitement, riot. Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
The picture of depression is complemented by the disappearance of desires, interests, a pessimistic assessment of everything around, ideas of one's own low value and self-blame. Deficiency of vital impulses is manifested in patients with a variety of symptoms - from lethargy, physical weakness to a state of weakness, loss of energy and complete impotence.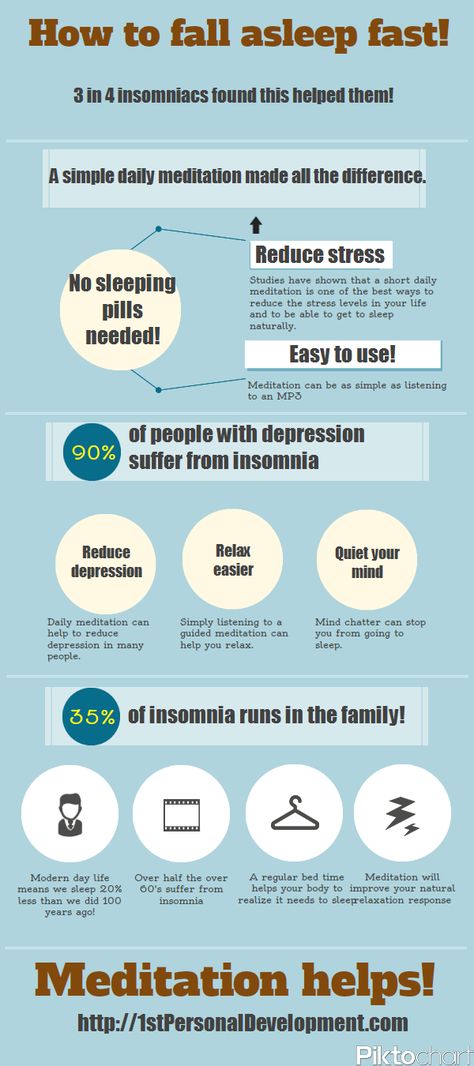 Where an important decision is required, a choice between different options, human activity is sharply hampered. Depressed people are well aware of this: they complain that insignificant everyday tasks, small issues that used to be solved almost automatically, take on the significance of complex, painful, insoluble problems. At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
Where an important decision is required, a choice between different options, human activity is sharply hampered. Depressed people are well aware of this: they complain that insignificant everyday tasks, small issues that used to be solved almost automatically, take on the significance of complex, painful, insoluble problems. At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
People suffering from depression often feel "stupid", "mentally retarded", "feeble-minded". Thinking in depression becomes viscous, painful, requires special efforts, one mental image is hardly forced out by the next. The sick person is oppressed by the feeling of his own intellectual insolvency, professional collapse. Depressed patients can hardly describe their painful experiences to the doctor. Only after getting out of depression, many of them say that the mood at that moment was lowered, thinking was slow, all undertakings (including treatment) seemed in vain, and the years lived were empty and useless. However, at the time of the first visit to the doctor, they could not explain this because of the almost complete absence of thoughts in their heads, “para-lich of thinking”. With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
Only after getting out of depression, many of them say that the mood at that moment was lowered, thinking was slow, all undertakings (including treatment) seemed in vain, and the years lived were empty and useless. However, at the time of the first visit to the doctor, they could not explain this because of the almost complete absence of thoughts in their heads, “para-lich of thinking”. With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
Typical story
Aleksey, 18 years old, 1st year student of a technical university, describes his condition during depression in this way:
“From childhood, I was fond of technology and modeling, I could read special literature for hours, won school and regional olympiads in mathematics and physics. After graduating from school, my dream came true - I brilliantly passed the exams to a prestigious university. Then it seemed to me that the whole world was at my feet, I flew with happiness "as if on wings." In September, I happily began to study. At the beginning, everything worked out well, but after 2 months I began to notice that it was becoming increasingly difficult for me to absorb what I read, I did not remember the simplest text, I could not solve problems that I used to “click like nuts”. Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center.
Then it seemed to me that the whole world was at my feet, I flew with happiness "as if on wings." In September, I happily began to study. At the beginning, everything worked out well, but after 2 months I began to notice that it was becoming increasingly difficult for me to absorb what I read, I did not remember the simplest text, I could not solve problems that I used to “click like nuts”. Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center. After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
Depression can also be accompanied by real setbacks: for example, a decrease in academic performance, the quality of work, family conflicts, sexual disorders and their consequences for personal relationships. As a rule, the significance of these failures is exaggerated and as a result there is a false sense of the irreparability of what happened, "the collapse of all hopes."
Another generally recognized danger of depression is the possibility of suicidal thoughts, which often lead to suicide attempts. The condition of a person suffering from depression can suddenly deteriorate sharply, which happens either without clear external causes, or under the influence of traumatic situations, unpleasant news. It is during these hours, and sometimes even minutes, that a fatal decision is made. Factors that increase the risk of suicide in depression are past suicide attempts, the severity and duration of the depressive state, the presence of anxiety in its structure, prolonged insomnia, loneliness or alienation in the family, alcohol and drug abuse, loss of work and a sharp change in lifestyle, as well as relatives commit suicide.
Typical story
Eugene E., 35 years old, leading manager of the company.
Almost all my life, my career went “on the ascending”, the goals set were clear, clear and achievable. The marriage was extremely harmonious, two beloved children grew up. He devoted almost all the time to the affairs of the company, occasionally, once every 1-2 months, he escaped with his family out of town, to the country. He often lacked sleep, stayed late at work, took home assignments, and was deeply worried about the affairs of the company. Gradually, irritability, fatigue, insomnia, difficulty concentrating appeared, more and more often he suffered a “fiasco” in intimate life. Thoughts appeared that life was lived in vain, that it is a "chain of tragic mistakes" that led to a dead end. He began to believe that the choice of work, friends, family was wrong, for which now "retribution has come." Analyzing the past years for a long time, he found more and more evidence and examples of his "duplicity, hypocrisy, insincerity, etc. " I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car. However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because.
" I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car. However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because. his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared. He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared. He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
Depression is also characterized by sleep disturbances, occurring in approximately 80% of patients. As a rule, these are early awakenings with the inability to fall asleep, lack of a sense of sleep, difficulty falling asleep.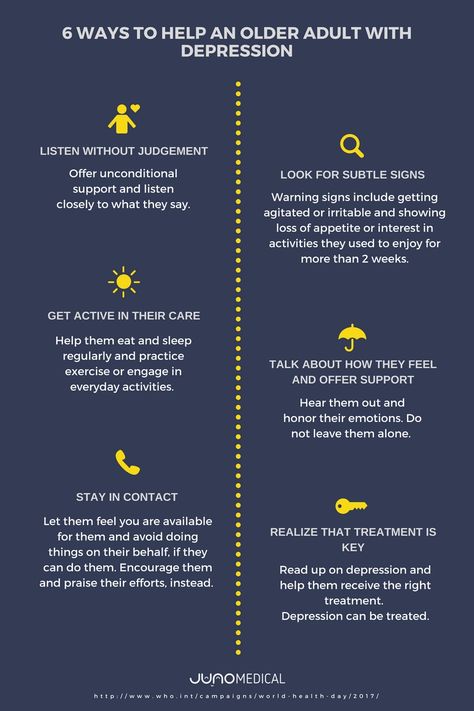 These disorders, as well as restless sleep with unpleasant dreams, are often the very first symptoms of incipient depression.
These disorders, as well as restless sleep with unpleasant dreams, are often the very first symptoms of incipient depression.
If the depression is not deep, it is sometimes difficult to recognize it. This is due to the fact that people are ashamed to tell others about their problems, to admit to "weaknesses". Quite often, especially in Russia, depressive states are masked by alcohol abuse (“vodka heals”). In addition, often patients suffering from depression, in order to "shake themselves up", "throw into all serious", engage in casual sex, are fond of gambling or extreme sports, leave to serve on a contract in "hot spots", lead an idle lifestyle with constant attendance at entertainment events. Surrounding people, relatives who do not have psychiatric knowledge, often accuse them of debauchery, drunkenness, riotous lifestyle, parasitism. Meanwhile, this behavior is a kind of “cry for help”, an attempt to fill the spiritual emptiness brought by depression with new acquaintances and impressions.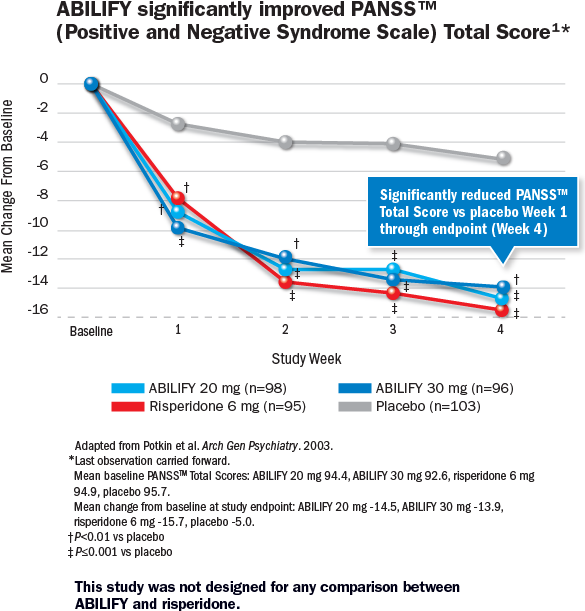
Depressive conditions can occur in shallow forms that are easily treatable, but at least a third of depressions are more severe. Such depressions are characterized by:
- ideas of guilt, sometimes reaching the degree of delirium, i.e. unshakable conviction in their sinfulness, low value (patients consider themselves great sinners, believe that because of them all relatives and Mankind will die, that they are “moral freaks” from birth, supposedly deprived of the foundations of morality and a sense of empathy for other people that they have no place on earth They find in their past numerous "confirmations" of what has been said above, they believe that the doctor and other patients are aware of these transgressions and express contempt and indignation with their facial expressions and gestures, but in the words “they hide, deny the obvious.” Both the patients themselves and their relatives must remember this in order to prevent the impending threat in time: remove all firearms, piercing and cutting objects, ropes, potent drugs and poisonous close household fluids, close windows or shutters, do not let the patient go anywhere alone. If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
- mood swings during the day: in typical cases, the patient, waking up, immediately feels longing. Sometimes, even before full awakening, through a dream he experiences a painful premonition of a heavy coming morning. In the evening, the state of health improves somewhat.
- the patient may experience a feeling of unmotivated hostility towards relatives, friends, constant internal discontent and irritation, which makes him unbearable for the family.
- in a number of people suffering from depression, constant doubts, fear for the health and well-being of loved ones, obsessive ones, come to the fore. arising against the will, ideas about the misfortunes and troubles of family members.
Typical story
Dmitry Petrovich, 58 years old, teacher.
“After minor troubles at work, I began to feel incomprehensible anxiety and agitation. Unpleasant thoughts came into my head that I did something wrong at work, because of which I double-checked everything many times and went home later than everyone else. But even at home, the anxiety did not let go: as soon as the daughter or wife lingered for at least half an hour, terrible pictures of traffic accidents or violence were drawn in the imagination. I fell asleep only in the morning, got up broken and felt sleepy all day. I took Valerian, Corvalol, but it practically did not help. At work, they hinted whether I should take a vacation. Friends advised me to consult a neuropathologist, but he did not find his pathology and sent me to a psychiatrist. I was diagnosed with anxiety depression. After a course of outpatient treatment, I completely recovered.”
Unpleasant thoughts came into my head that I did something wrong at work, because of which I double-checked everything many times and went home later than everyone else. But even at home, the anxiety did not let go: as soon as the daughter or wife lingered for at least half an hour, terrible pictures of traffic accidents or violence were drawn in the imagination. I fell asleep only in the morning, got up broken and felt sleepy all day. I took Valerian, Corvalol, but it practically did not help. At work, they hinted whether I should take a vacation. Friends advised me to consult a neuropathologist, but he did not find his pathology and sent me to a psychiatrist. I was diagnosed with anxiety depression. After a course of outpatient treatment, I completely recovered.”
- in many cases, depression is characterized by unpleasant sensations in the body, disturbances in the activity of internal organs in the absence of objective signs of true somatic, i.e. non-mental illness. At the same time, many patients constantly report pain, internal discomfort. Some complain of headaches, pains in the stomach, joints, lower back, others - of disorders in the intestines: constipation, indigestion, irritation of the colon, others pay attention to a decrease in sexual desire and potency. In women, menstruation often becomes painful and irregular. Approximately 50% of depressed people at the doctor's office complain of such physical ailments, without mentioning the depressed mood or state of mind underlying the depression. Experiencing chronic pain or other unpleasant sensations in the body, patients may not realize that they are suffering from depression, even with severe melancholy, considering the latter a reaction to painful bodily discomfort.
Some complain of headaches, pains in the stomach, joints, lower back, others - of disorders in the intestines: constipation, indigestion, irritation of the colon, others pay attention to a decrease in sexual desire and potency. In women, menstruation often becomes painful and irregular. Approximately 50% of depressed people at the doctor's office complain of such physical ailments, without mentioning the depressed mood or state of mind underlying the depression. Experiencing chronic pain or other unpleasant sensations in the body, patients may not realize that they are suffering from depression, even with severe melancholy, considering the latter a reaction to painful bodily discomfort.
- some patients are convinced that they have some rare and difficult to diagnose disease and insist on numerous examinations in general medical institutions. Doctors call this condition masked (hidden) depression, in which a person may experience pain in the head, in the limbs, behind the sternum, in the abdomen and in any other parts of the body, he may be haunted by anxious fears, he may suffer from insomnia or, on the contrary, too much sleep.
- Patients may experience disturbances in the cardiovascular system, skin itching or lack of appetite. All of these are manifestations of depression.
- the pathological sensations that patients experience during such depressions are quite real, painful, but they are the result of a special mental state, and not an internal disease. It must be remembered that the frequency of latent depressions exceeds the number of explicit ones many times over.
- with such depression, patients, as a rule, also have a changed attitude towards food: they can go without food for a long time and not feel hungry, and sitting down at the table, eat only 1-2 spoons - they have neither strength nor desire for more .
- a sign of depression can serve as a weight loss of more than 5 kg. within a month. In some people, especially women, the appetite for depression, on the contrary, increases, sometimes reaching the level of excruciating hunger, accompanied by severe weakness and pain in the epigastric region. In some cases, food is taken in excess due to an increased craving for sweets or attempts to distract oneself from painful thoughts by frequent eating.
In some cases, food is taken in excess due to an increased craving for sweets or attempts to distract oneself from painful thoughts by frequent eating.
Thus, we see that depression is a disease with many different manifestations that do not go away on their own, requiring special, sometimes long-term, medical intervention. Therefore, when the symptoms described above appear, it is necessary to seek help from a psychiatrist who will prescribe and monitor antidepressant treatment.
TREATMENT OF DEPRESSIVE DISORDERS
To date, it can be argued that the vast majority of cases of depression respond well to treatment. According to modern views, effective treatment of depression consists of a combination of pharmacotherapy, psychotherapy and, if necessary, other types of treatment. At the same time, the main role in therapy, of course, belongs to antidepressants - drugs specially designed for the treatment of various types of depression.
The creation of antidepressants is based on the discovery of scientists that depression develops as a result of a violation of the mechanism of biochemical transmission of nerve impulses in the brain regions responsible for mood, behavior, response to stress, sleep and wakefulness, appetite and some other functions. To ensure the coordination of the work of all these functional divisions, the brain sends special "commands" to them in the form of chemical impulses transmitted from the processes of one nerve cell (neuron) to the processes of another. This transmission is carried out with the help of chemical mediators (neurotransmitters), which, after transmitting a signal, partially return to the original neuron. This process is called neurotransmitter reuptake. Thanks to him, the number of mediators in the microscopic space between the processes of neurons (in the so-called synaptic cleft) decreases, which means that the necessary signals are transmitted worse. Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator.
To ensure the coordination of the work of all these functional divisions, the brain sends special "commands" to them in the form of chemical impulses transmitted from the processes of one nerve cell (neuron) to the processes of another. This transmission is carried out with the help of chemical mediators (neurotransmitters), which, after transmitting a signal, partially return to the original neuron. This process is called neurotransmitter reuptake. Thanks to him, the number of mediators in the microscopic space between the processes of neurons (in the so-called synaptic cleft) decreases, which means that the necessary signals are transmitted worse. Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator. A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
Now antidepressants are used in Russia, which can be conditionally divided into 4 generations according to the time of creation.
The first antidepressants to find wide clinical use were tricyclic drugs: amitriptyline and imipramine. They have a fairly powerful effect on most depressive states by blocking the reuptake of both norepinephrine and serotonin. However, the real clinical effect of these drugs is significantly offset by their undesirable side effects, which drastically reduce the quality of life of patients during treatment. Side effects of tricyclic antidepressants arise due to the nonspecificity of their effect on receptor structures. Acting in addition to the serotonin and norepinephrine system and other neurotransmitters (acetylcholine, histamine, dopamine), these antidepressants cause side effects such as urinary retention, dry mucous membranes, constipation, palpitations, fluctuations in blood pressure, confusion, tremor, sexual dysfunction. functions, weight gain. In such cases, it is necessary to prescribe other drugs to correct side effects or reduce the therapeutic dose of drugs, which naturally affects the effectiveness of the antidepressant action. It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
functions, weight gain. In such cases, it is necessary to prescribe other drugs to correct side effects or reduce the therapeutic dose of drugs, which naturally affects the effectiveness of the antidepressant action. It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
The situation was somewhat improved by the introduction into practice of drugs of the second generation - tetracyclic antidepressants, which, along with the ability to block the reuptake of norepinephrine and serotonin, could also affect some other receptors. Being analogues of tricyclic compounds, these drugs have antidepressant activity comparable to them, but unlike their predecessors, they are safer, since they cause unwanted side effects much less often. In addition to the antidepressant, mianserin (lerivon) has a clear sedative, anti-anxiety and hypnotic effect. Maprotiline (Ludiamil) has a mild balanced antidepressant effect. In general, these drugs are able to cure mild to moderate depression, but are ineffective in patients with severe depression.
Maprotiline (Ludiamil) has a mild balanced antidepressant effect. In general, these drugs are able to cure mild to moderate depression, but are ineffective in patients with severe depression.
To date, antidepressants of the 3rd generation, such as fluoxetine (Prozac), fluvoxamine (Fevarin), paroxetine (Paxil), sertraline (Zoloft), citalopram (Cipralex) and some other drugs that selectively (selectively) affect the serotonin metabolism system, have received widespread recognition today. , preventing its reuptake in the synaptic cleft. Based on the mechanism of action, these antidepressants are combined into a group of selective serotonin reuptake inhibitors. In addition to treating depression, they are used to correct eating disorders, level panic disorders, so-called social phobias, various obsessive-compulsive disorders and chronic pain symptoms. These drugs have gained popularity due to the possibility of a once-daily intake, concomitant anti-anxiety effect, the presence of a psychostimulant component and a small number of side effects. In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
Considering the high frequency of side effects in some of the above drugs and the insufficient antidepressant activity in others, psychopharmacologists have taken the path of developing more effective antidepressants - IV generation drugs that selectively block the reuptake of both serotonin and noradrenaline, without affecting other mediators. system and with minor side effects. Currently, 3 drugs meet these requirements: milnacipran (Ixel), duloxetine (Cymbalta) and venlafaxine (Effexor). Their antidepressant activity in the treatment of patients with severe and moderate depression has been confirmed in a number of specially conducted studies, which at the same time showed that these drugs are well tolerated.
It should be noted that antidepressants of plant origin (negrustin, gelarium hypericum, deprim, etc.) can be effective in mild depressive states, but there are no reliable data guaranteeing their effectiveness. The opinion of a number of doctors that all depression can be treated with herbs or, say, acupuncture, should be recognized as unfounded.
For extremely severe depressions that do not improve despite the use of the most powerful antidepressants, electroconvulsive therapy (ECT) can be effective, but this situation is extremely rare and requires careful justification by the commission of doctors and the consent of the patient.
An important additional role in antidepressant therapy, especially with concomitant anxiety, is played by tranquilizers - anti-anxiety drugs, such as Xanax, phenazepam, diazepam, nitrazepam, atarax, etc. Drugs that can, when taken systematically, prevent mood swings in various depressive disorders include so-called mood stabilizers or mood stabilizers - lithium preparations, carbamazepine, valproic acid salts, lamotrigine, topiramate. With their systematic intake in most patients, the clinical manifestations of depression either completely disappear or become rare and mild, requiring no hospitalization and not significantly affecting the ability to work.
With their systematic intake in most patients, the clinical manifestations of depression either completely disappear or become rare and mild, requiring no hospitalization and not significantly affecting the ability to work.
Antipsychotics play a significant role in the treatment of certain forms of depression. These include both traditional drugs - fluanxol, triftazin, eglonil, teralen, neuleptil, sonapax, and atypical antipsychotics that are gaining more and more recognition among doctors: seroquel, solian, zeldox, rispolept, abilify, serdolect and others.
In drug therapy of depressive conditions, an unconventional, strictly individual approach is used, with the obligatory provision of fruitful cooperation between the patient and the doctor. Otherwise, there may be a violation of medical recommendations regarding doses and regimens for taking medications. The patient's faith in the possibility of recovery, the absence of prejudice against the "harm" caused by psychotropic drugs, the systematic observance of the prescriptions prescribed by the doctor largely contribute to the achievement of therapeutic success.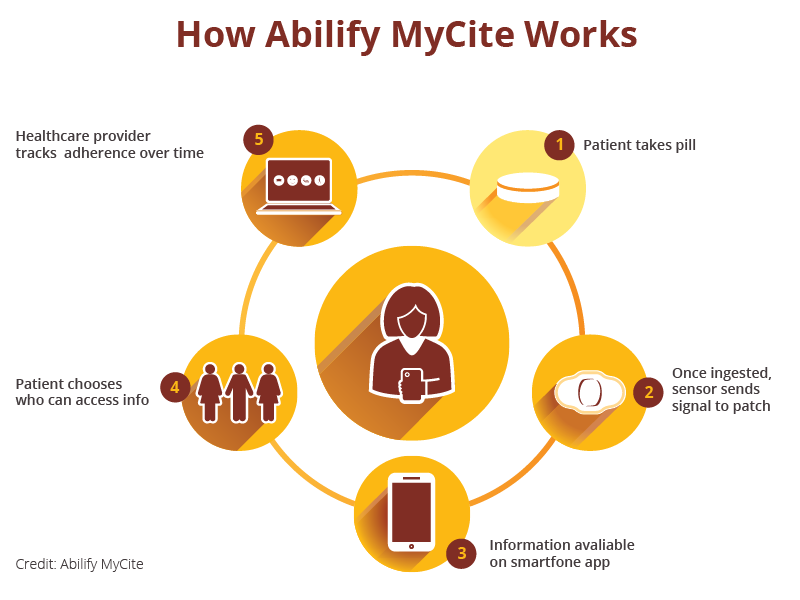
Drug treatment of depression takes time. You should not expect a complete cure already in the first days of taking the drug. It must be remembered that all modern antidepressants begin to act on depressive symptoms no earlier than 1-2 weeks after the start of treatment. Cancellation of an antidepressant, as well as its appointment, should be carried out only by a doctor. Cancellation is usually made no earlier than 6 months from the normalization of the mental state. Even after the complete disappearance of all symptoms of depression, do not rush to stop taking the drug yourself, as there is a risk of an exacerbation of the disease. Therefore, doctors recommend continuing to take the antidepressant for a certain period of time. A common mistake is the premature withdrawal of drugs soon after a significant improvement in the condition or due to "forgetfulness". To avoid this, try to include the drug in the list of daily urgent matters - for example, store it in the bathroom and take it after hygiene procedures.