Emotional personality disorder symptoms
Symptoms - Borderline personality disorder
Borderline personality disorder (BPD) can cause a wide range of symptoms, which can be broadly grouped into 4 main areas.
The 4 areas are:
- emotional instability – the psychological term for this is "affective dysregulation"
- disturbed patterns of thinking or perception – "cognitive distortions" or "perceptual distortions"
- impulsive behaviour
- intense but unstable relationships with others
Each of these areas is described in more detail below.
Emotional instability
If you have BPD, you may experience a range of often intense negative emotions, such as:
- rage
- sorrow
- shame
- panic
- terror
- long-term feelings of emptiness and loneliness
You may have severe mood swings over a short space of time.
It's common for people with BPD to feel suicidal with despair, and then feel reasonably positive a few hours later. Some people feel better in the morning and some in the evening. The pattern varies, but the key sign is that your moods swing in unpredictable ways.
If you have suicidal thoughts:
- call your GP or the out-of-hours GP service. If you've taken an overdose or cut or burned yourself, dial 999
- call the Samaritans on 116 123. This organisation provides emotional support 24 hours a day for people experiencing feelings of distress or despair
- contact a friend, family member or someone you trust
If you've been diagnosed with BPD, tell someone you trust about your condition. Give this person the contact details of your care team and ask him or her to contact the team if they become concerned about your behaviour.
Disturbed patterns of thinking
Different types of thoughts can affect people with BPD, including:
- upsetting thoughts – such as thinking you're a terrible person or feeling you do not exist.
 You may not be sure of these thoughts and may seek reassurance that they're not true
You may not be sure of these thoughts and may seek reassurance that they're not true - brief episodes of strange experiences – such as hearing voices outside your head for minutes at a time. These may often feel like instructions to harm yourself or others. You may or may not be certain whether these are real
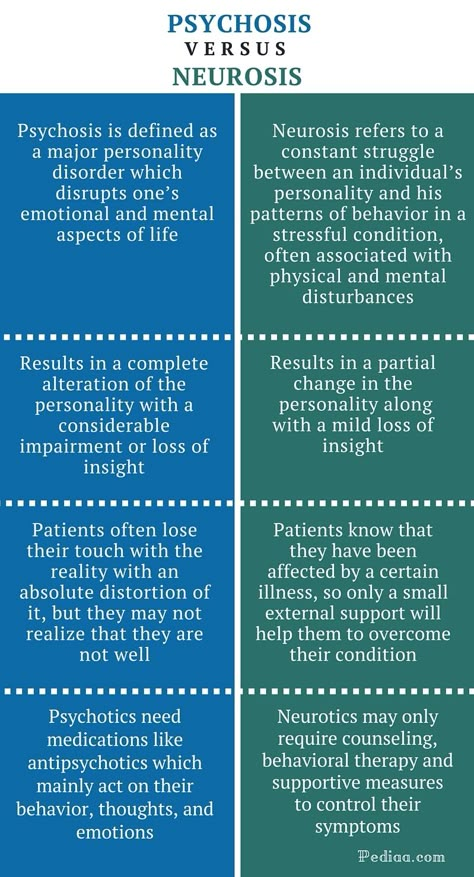
- prolonged episodes of abnormal experiences – where you might experience both hallucinations (voices outside your head) and distressing beliefs that no one can talk you out of (such as believing your family are secretly trying to kill you)
These types of beliefs may be psychotic and a sign you're becoming more unwell. It's important to get help if you're struggling with delusions.
Impulsive behaviour
If you have BPD, there are 2 main types of impulses you may find extremely difficult to control:
- an impulse to self-harm – such as cutting your arms with razors or burning your skin with cigarettes; in severe cases, especially if you also feel intensely sad and depressed, this impulse can lead to feeling suicidal and you may attempt suicide
- a strong impulse to engage in reckless and irresponsible activities – such as binge drinking, drug misuse, going on a spending or gambling spree, or having unprotected sex with strangers
Unstable relationships
If you have BPD, you may feel that other people abandon you when you most need them, or that they get too close and smother you.
When people fear abandonment, it can lead to feelings of intense anxiety and anger. You may make frantic efforts to prevent being left alone, such as:
- constantly texting or phoning a person
- suddenly calling that person in the middle of the night
- physically clinging on to that person and refusing to let go
- making threats to harm or kill yourself if that person ever leaves you
Alternatively, you may feel others are smothering, controlling or crowding you, which also provokes intense fear and anger. You may then respond by acting in ways to make people go away, such as emotionally withdrawing, rejecting them or using verbal abuse.
These 2 patterns may result in an unstable "love-hate" relationship with certain people.
Many people with BPD seem to be stuck with a very rigid "black-white" view of relationships. Either a relationship is perfect and that person is wonderful, or the relationship is doomed and that person is terrible.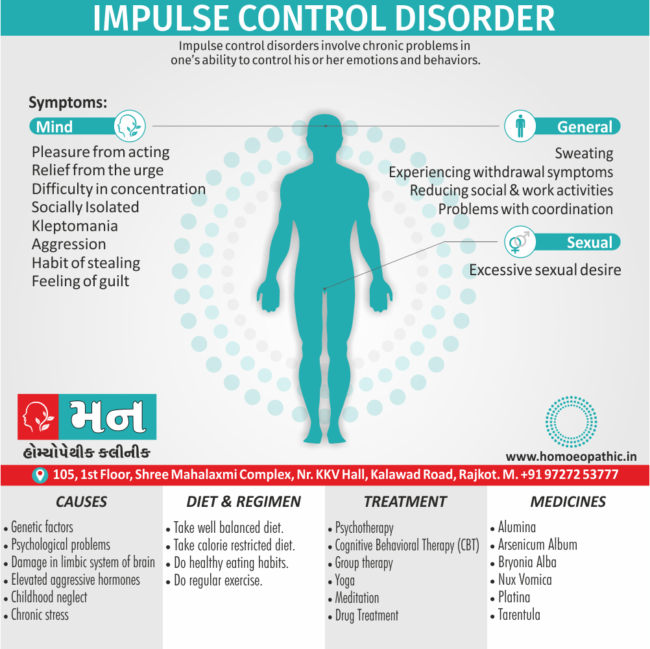 People with BPD seem unable or unwilling to accept any sort of "grey area" in their personal life and relationships.
People with BPD seem unable or unwilling to accept any sort of "grey area" in their personal life and relationships.
For many people with BPD, emotional relationships (including relationships with professional carers) involve "go away/please don't go" states of mind, which is confusing for them and their partners. Sadly, this can often lead to break-ups.
Page last reviewed: 17 July 2019
Next review due: 17 July 2022
What is borderline personality disorder (EUPD)?
This section has information on borderline personality disorder (BPD), including symptoms, causes and treatments. This information is for people affected by BPD in England who are 18 or over. It’s also for their carers, friends and relatives and anyone interested in this subject.
Borderline personality disorder is also called emotionally unstable personality disorder (EUPD) and emotional intensity disorder (EID). In this factsheet, we call it BPD as this is still the most common term for the condition. But we appreciate that all 3 terms can be controversial.
But we appreciate that all 3 terms can be controversial.
If you would like more advice or information you can contact our Advice and Information Service by clicking here.
Download Borderline personality disorder (BPD) factsheet
- Overview
- About
- Symptoms
- Causes and treatment
- Problems and self-care
- Information for carers
- Further reading
- Useful contacts
Overview
- BPD means that you feel strong emotions that you struggle to cope with.
 You may feel upset or angry a lot of the time.
You may feel upset or angry a lot of the time. - Around 1 in 100 people live with BPD.
- There are different reasons why people get BPD. A lot of people who live with a diagnosis of BPD have had traumatic experiences in their childhood.
- If you are someone living with a diagnosis of BPD, it is more likely that you will self-harm. And have challenges with relationships, alcohol or drugs. There is help available.
- There are different ways to treat BPD. The NHS should normally offer you therapy.
Need more advice?
If you need more advice or information you can contact our Advice and Information Service.
Contact us Contact us
About
What is borderline personality disorder (BPD)?
Everyone has different ways of thinking, feeling, and behaving.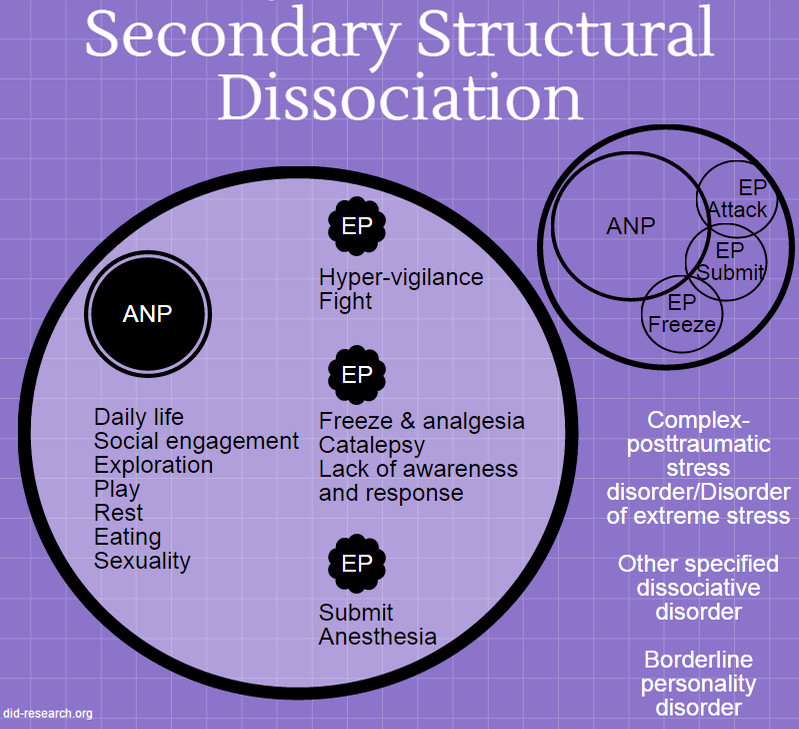 It is these thoughts, feelings, and behaviours that make up our ‘personality’. These are often called our traits. They shape the way we view the world and the way we relate to others. By the time we are adults these will make us part of who we are.
It is these thoughts, feelings, and behaviours that make up our ‘personality’. These are often called our traits. They shape the way we view the world and the way we relate to others. By the time we are adults these will make us part of who we are.
You can think of your traits as sitting along a scale. For example, everyone may feel emotional, get jealous, or want to be liked at times. But it is when these traits start to cause problems that you may be diagnosed as having a personality disorder.
BPD is a type of ‘personality disorder’.
BPD can affect how you cope with life, manage relationships, and feel emotionally. You may find that your beliefs and ways of dealing with day-to-day life are different from others. You can find it difficult to change them.
You may find your emotions confusing, tiring, and hard to control. This can be distressing for you and others. Because it is distressing, you may find that you develop other mental health problems like depression or anxiety. You may also do other things such as drink heavily, use drugs, or selfharm to cope.
You may also do other things such as drink heavily, use drugs, or selfharm to cope.
Research shows that around 1 in 100 people live with BPD. It seems to affect men and women equally, but women are more likely to have this diagnosis. This may be because men are less likely to ask for help. BPD is sometimes called emotionally unstable personality disorder (EUPD). Some people feel that this describes the illness better.
Some people who live with BPD think that the name is insulting or makes them feel labelled. Doctors don’t use this term to make you feel judged or suggest that the illness is your fault. It is meant to describe the way the illness develops. It’s important to remember this is a health condition. And not a judgement of your character or you as a person.
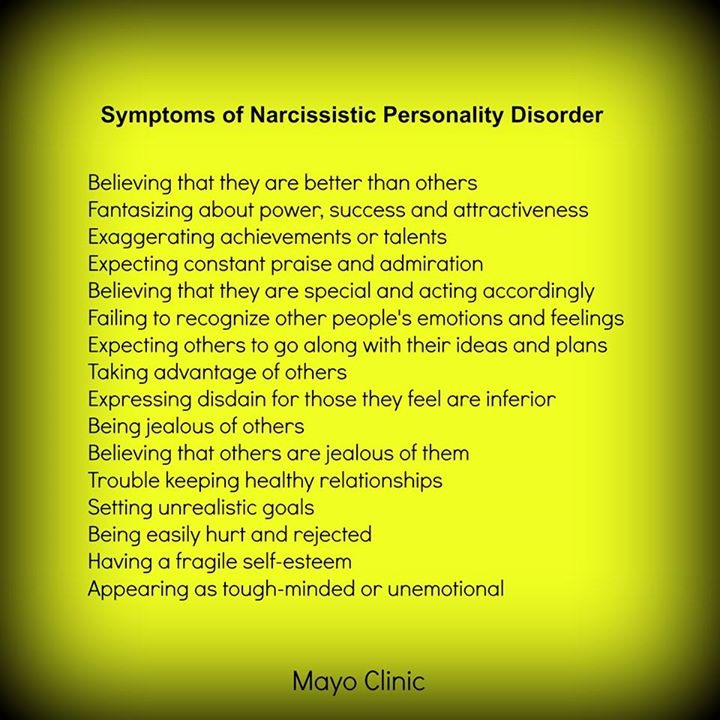
Symptoms
What are the symptoms of BPD?
Everyone will experience BPD differently. If you live with BPD, you may have difficulties with:
- being impulsive. This means that you like to do things on the spur of the moment,
- feeling bad about yourself,
- controlling your emotions,
- self-harming,
- suicidal thoughts and attempts to take your own life,
- feeling 'empty’,
- dissociation.
 This could be a feeling of being disconnected from your own body. Or feeling disconnected from the world around you.
This could be a feeling of being disconnected from your own body. Or feeling disconnected from the world around you. - identity confusion. You might not have a sense of who you are.
- feeling paranoid or depressed,
- hearing voices or noises when you are stressed, and
- intense but unstable relationships with others.
Not everyone will experience all these symptoms.
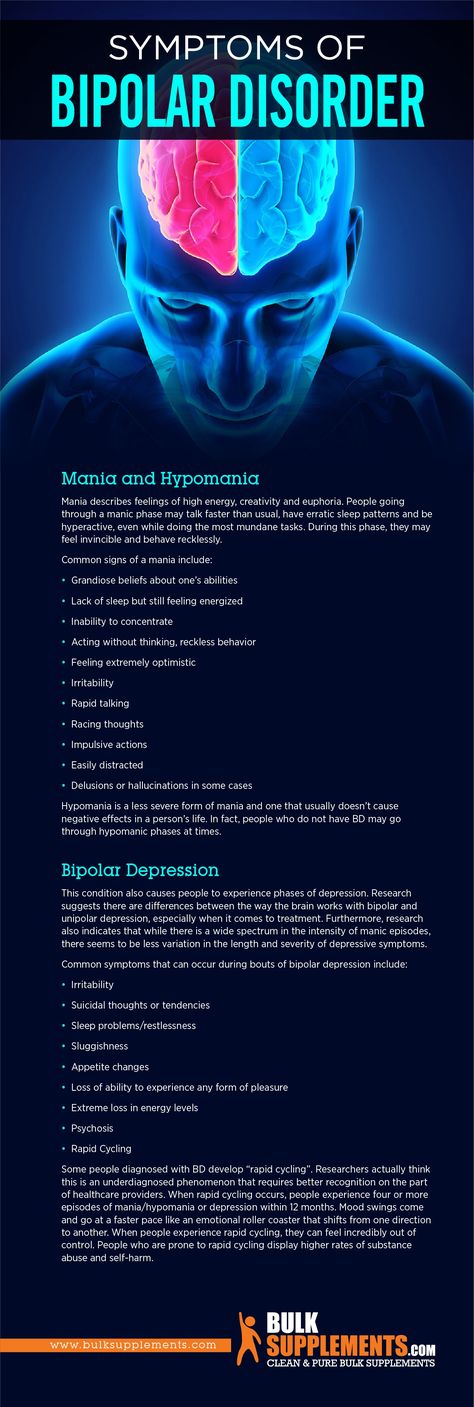
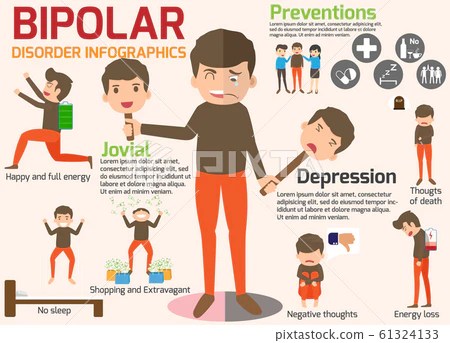
Sam's Story
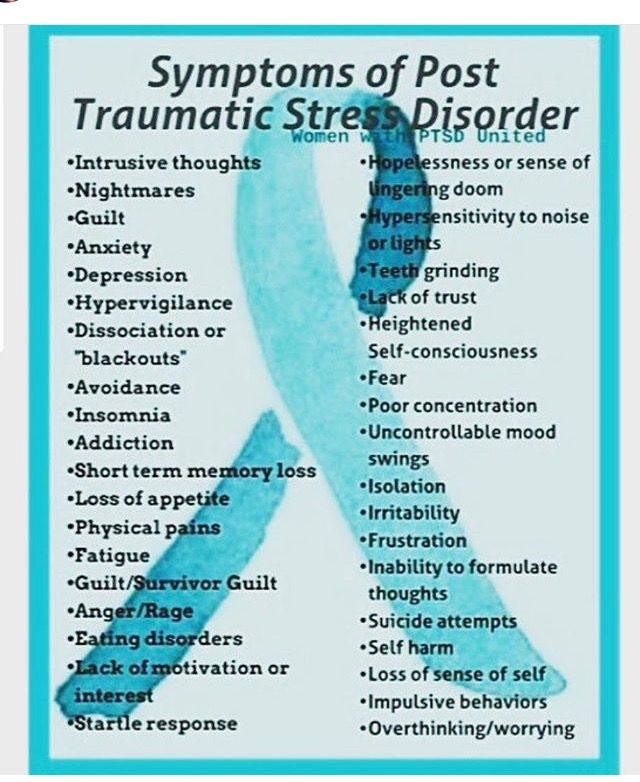
Many people who live with BPD will also experience other mental health problems. Such as depression, anxiety, eating disorders, PTSD and alcohol or drug misuse. People who live with BPD can also be diagnosed with bipolar disorder. The symptoms of bipolar disorder can often be confused with those of BPD.
You can find more information about:
- Personality disorders by clicking here.
- Dissociation and dissociative disorders by clicking here.
- Self-harm by clicking here.
- Anxiety disorders by clicking here.

- Depression by clicking here.
- PTSD by clicking here.
- Drugs, alcohol and mental health by clicking here.
- Bipolar disorder by clicking here.
Causes & treatment
What causes BPD?
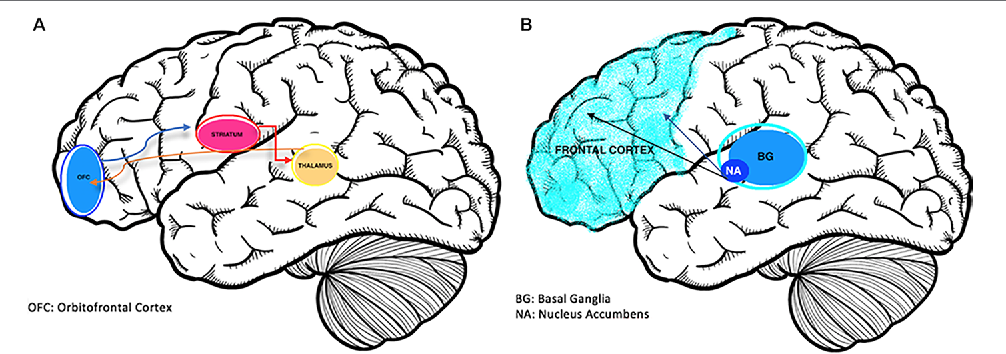
There’s no single reason why some people develop borderline personality disorder (BPD). Professionals can’t use things like blood tests or brain scans to help diagnose people.
It is thought that BPD may be caused by a combination of factors:
- Genetics – you may be more vulnerable to BPD if a close family member also lives with BPD. There is no evidence though of a particular gene being responsible for BPD.
- Brain chemicals – problems with levels of your brain chemicals, particularly serotonin.
- Brain development – many people who live with BPD have smaller, or more active, parts of their brain. These parts of the brain are affected by your early upbringing.
 And can affect the regulation of your emotions, behaviour and self-control. They can also affect you planning and decision making.
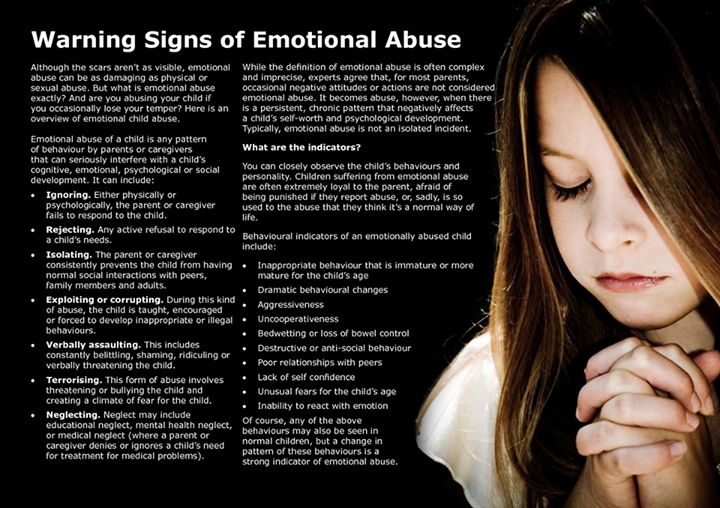
And can affect the regulation of your emotions, behaviour and self-control. They can also affect you planning and decision making. - Environmental factors – a number of environmental factors seem to be common with people who live with BPD. These can include:
- experiencing abuse,
- experiencing long-term fear or distress as a child,
- being neglected by 1, or both, of your care-givers as a child, and
- growing up with a family member who had a serious mental health condition. Such as bipolar disorder or a problem with alcohol or drugs.
How can I get help if I think I have BPD?
The first step to get help is to speak to your GP.
Your GP will look at different things when deciding how best to help you. So, it can help to keep a record of your symptoms. This can help you and your GP to understand what difficulties you are facing. It may help if you keep a record of:
- how distressed you feel,
- any risks to yourself or other people, and
- details of anything you have done to try and reduce your levels of anxiety and distress.
Your GP can’t diagnose BPD. Only a psychiatrist should make a formal diagnosis. A psychiatrist is part of the community mental health team (CMHT). If your GP feels that you need more support they will refer you to the CMHT.
What happens if my GP refers me to the community mental health team (CMHT)?
There may be a waiting list to see your CMHT. You can ask your GP, or contact the CMHT, about how long the waiting list is.
When you have your first appointment with the CMHT they will ask you questions to understand how your mental health is affecting you. They will talk to you about:
- how you manage your day to day life, relationships and work,
- coping strategies that you use,
- your strengths,
- areas in your life that you find difficult.
- any other mental health problems you may have,
- any other social problems that you may have,
- any social care and support needs you may have,
- any support you may need in staying in your job, or finding a job,
- any psychological treatment you may need.
 This is also known as ‘talking therapy’, and
This is also known as ‘talking therapy’, and - the needs of any dependent children that you have.
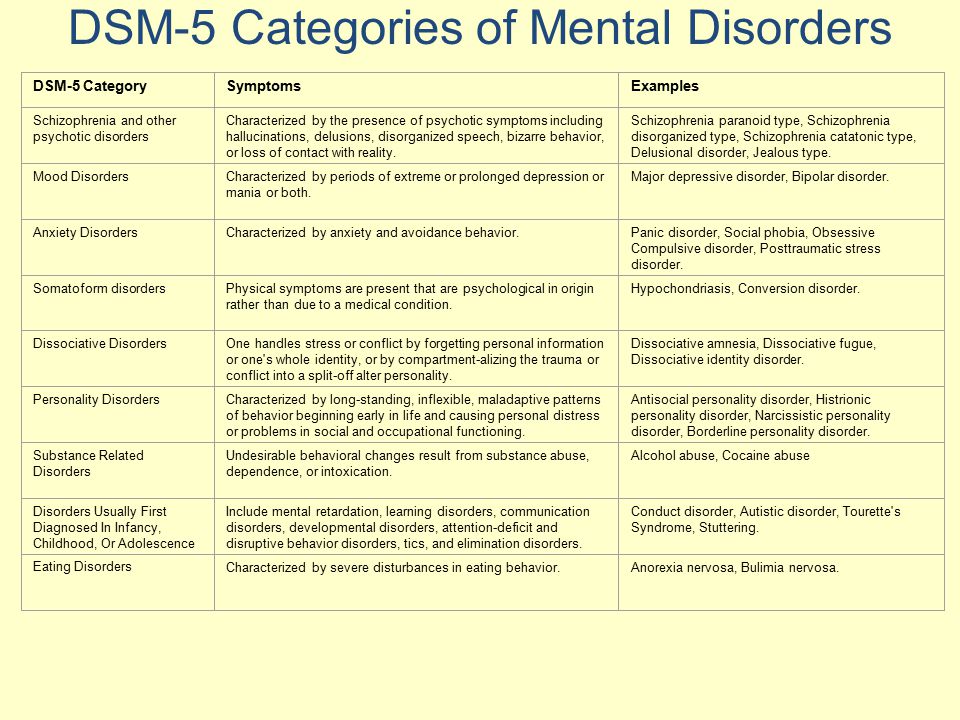
How will the CMHT decide if I have BPD?
Psychiatrists use the following guidelines to decide if you have a mental disorder.
- International Classification of Diseases (ICD-10), produced by the World Health Organisation (WHO).
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5), produced by the American Psychiatric Association.
The guidelines tell your psychiatrist what to look for. They will diagnose you with BPD if you have at least five of the symptoms below.
- Extreme reactions to feeling abandoned.
- Unstable and intense relationships with others
- Confused feelings about your self-image or your sense of identity.
- Being impulsive in ways that could be damaging. For example, spending, sex, substance abuse, reckless driving, and binge eating
- Regular self-harming, suicidal threats or behaviour.

- Long lasting feelings of emptiness or being abandoned.
- Inappropriate or intense anger. And difficulty controlling your anger. For example, losing your temper or getting into fights.
- Intense, highly changeable moods.
- Paranoid thoughts, or severe dissociation, when you’re stressed. Dissociation is a feeling of being disconnected from your own body. Or feeling disconnected from the world around you
You can find more information about:
- NHS Mental Health Teams (MHTs) by clicking here.
- Dissociation and dissociative disorders by clicking here.
What treatment should the NHS offer me?
You can check what treatment and care is recommended for BPD on the National Institute for Health and Care Excellence (NICE) website. NICE produce guidelines for how health professionals should treat certain conditions. You can download these from their website at:
www.nice.org.uk.
The NHS does not have to follow these recommendations. But they should have a good reason for not following them.
But they should have a good reason for not following them.
People who live with BPD have sometimes been excluded from NHS services because of their diagnosis. But the NHS should not refuse to give you specialist help because of your diagnosis. They should have services to support people with BPD.
If your local NHS doesn’t offer you appropriate treatment then there are things that you can do. For information about your options please see further down this page.
Should I be offered medication?
There is no medication to treat BPD. But your doctor may offer you medication if you also have symptoms of another mental illness like anxiety or depression.
What psychological treatment should I be offered?
Psychological therapy is also known as ‘talking therapy’. There are lots of different types of talking therapies and your doctor should talk to you about what is available, how it may help you and what type of therapy you would like.
We have included details below of some of the therapies that your doctor may use.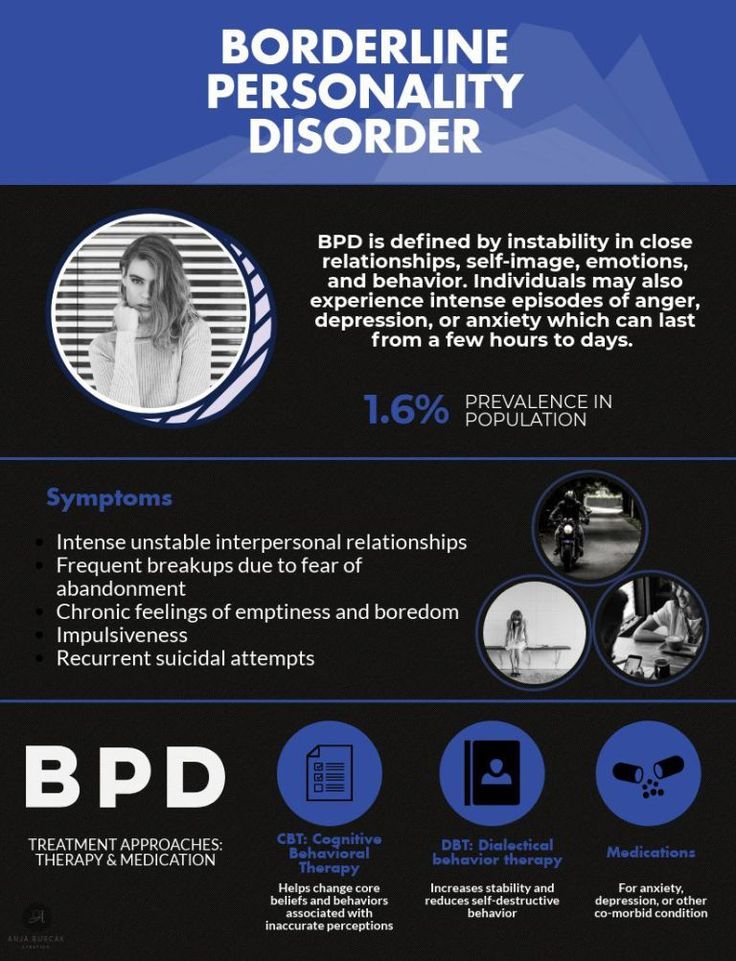 But these are not available everywhere. And your doctor may recommend other types of talking therapy.
But these are not available everywhere. And your doctor may recommend other types of talking therapy.
Your doctor will also think about:
- how much BPD is affecting you,
- how much you are willing to engage with therapy,
- if you want to change how react to your thoughts and feelings,
- if you will be able to work effectively with a counsellor, and
- the personal and professional support that is available.
The therapy you are offered should last at least 3 months. If your doctor decides that talking therapies are not suitable, they should explain why.
Dialectical behavioural therapy (DBT)
The guidance says that the NHS should offer DBT to women with BPD if they self-harm regularly.
DBT is a type pf therapy specifically designed to treat people with BPD. The goal of BPD is to help you accept that your emotions are real and acceptable. And to challenge how you respond to those emotions by being open to ideas and opinions which are different to your own.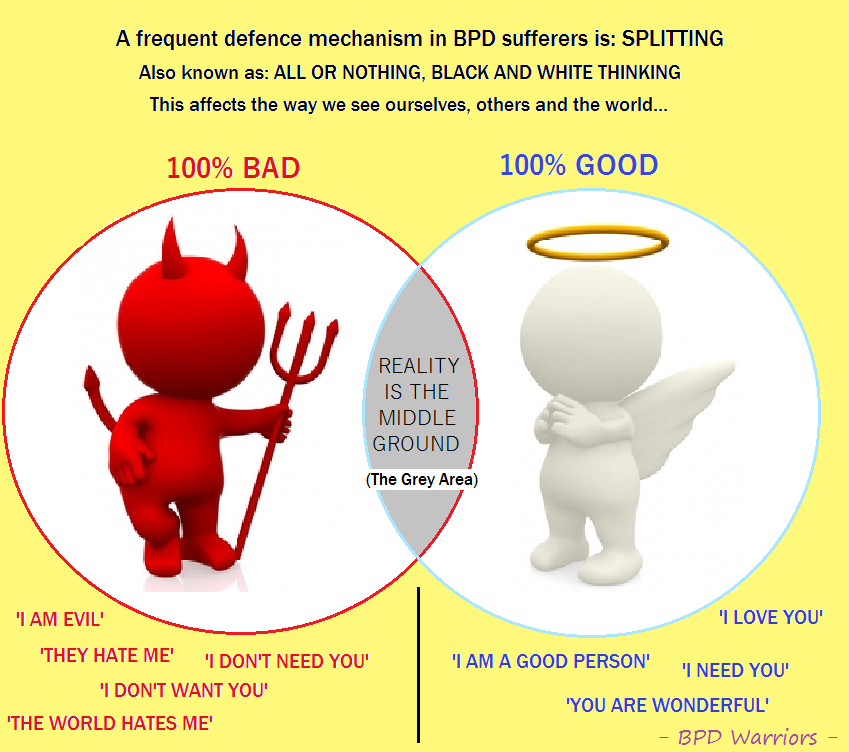
DBT usually involves weekly individual and group sessions. And you should be given an out-of-hours contact number to call if your symptoms get worse.
DBT is based on teamwork. You'll be expected to work with your therapist and the other people in your group sessions. In turn, the therapists work together as a team.
Mentalisation-based therapy (MBT)
Mentalisation means the ability to think about thinking. This means looking at your own thoughts and beliefs. And working out if they are helpful and realistic.
This type of therapy also helps you to recognise that other people have their own thoughts, emotions and beliefs. And that you may not always understand these. The therapy also helps you to think about how your actions might affect what other people think or feel.
A course of MBT usually lasts around 18 months. You may first be offered MBT in a hospital as an inpatient. The treatment usually consists of daily individual sessions with a therapist and group sessions with other people with BPD.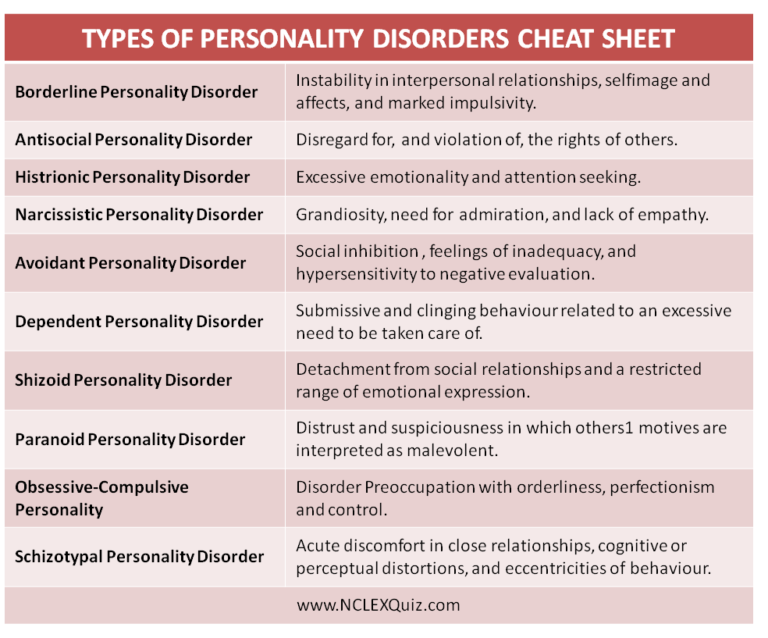
Some hospitals and specialist centres like you to remain in hospital whilst you are having MBT. But others recommend that you leave the hospital after a certain period of time but remain being treated as an outpatient. This means that you will visit the hospital regularly.
Arts therapies
There are different types of arts of creative therapies. These include:
- art therapy,
- drama therapy,
- music therapy, and
- dance movement therapy.
These therapies can be offered individually but they are often done in groups. Sessions are usually weekly. These therapies can be helpful to people who find it hard to talk about their thoughts and feelings.
Therapeutic communities
Therapeutic communities are not a treatment themselves. They are places you can go to have treatment. Most therapeutic communities are residential. They help people with long-term emotional problems, and a history of self-harming, by teaching them skills to help them have better relationships.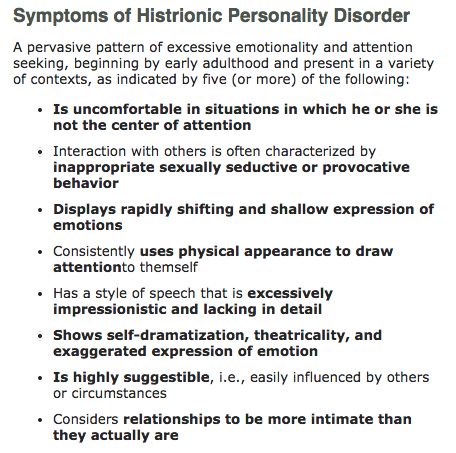
These communities often set strict rules on behaviour. For example, no drinking alcohol, no violence and no attempts at self-harming.
You may stay for a few weeks or months, or you may visit for just a few hours a week. You may have group therapy and self-help sessions. You would be expected to take part in other activities to improve your self-confidence and social skills. These activities may include household chores, games and preparing meals.
Therapeutic communities vary a lot because they are often run by the people who use them. And they shape them based on what they want to achieve.
What happens if the CMHT can’t successfully treat me?
You may get support from a specialist service if your symptoms are getting worse. These specialist services are also called ‘Tier 3’ or ‘Tier 4’ services.
These services are not available in all NHS Trusts. And they can be difficult to access. You can speak to your CMHT and if they can refer you to a specialist service.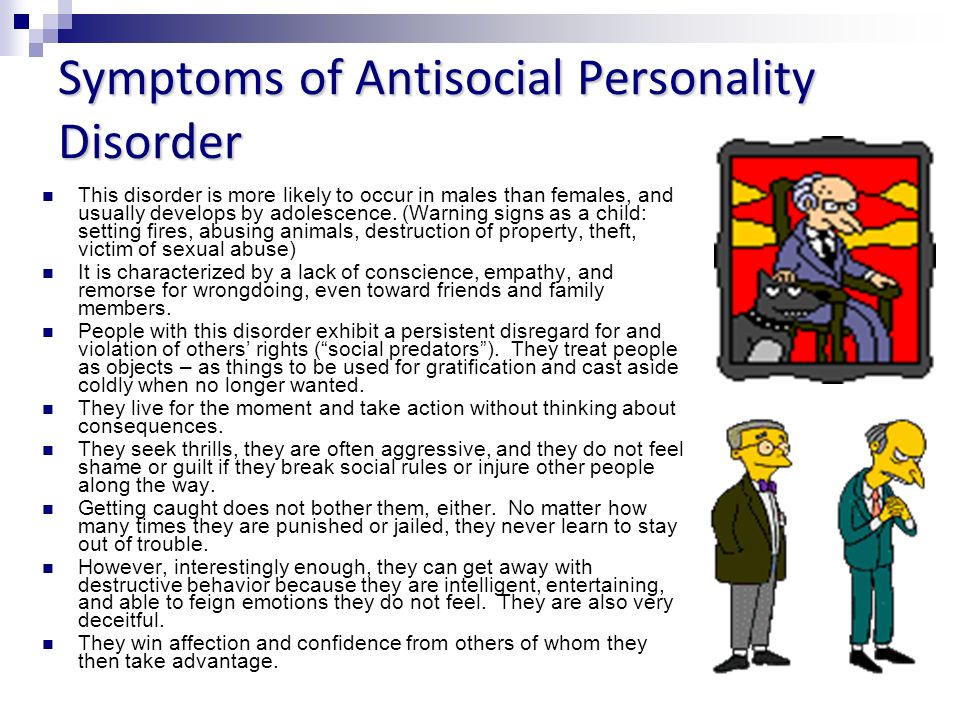
You can find more information about Tier 3 and Tier 4 services in our factsheet ‘Second Opinions’ by clicking here.
What treatment should I get if I am in crisis?
A mental health crisis is when you need urgent help. You may be feeling suicidal or wanting to self-harm. And you don’t think that you can use your normal coping strategies to stop yourself from acting on your feelings.
If you have a diagnosis of BPD but are not under the care of your local community mental health team (CMHT), then you should speak to your GP. Your GP should:
- assess the level of risk to yourself or others,
- talk to you about previous mental health crises. And what skills you have used to cope with these,
- help you to use these skills and focus on your current problems,
- help you to identify changes which you can put in place to manage your current problems, and
- offer you a follow-up appointment.
If you are already under the CMHT, or a specialist service, then you should have a care plan. The care plan should include a crisis plan that you can follow. Your crisis plan is written by you and your mental health team. It should include:
The care plan should include a crisis plan that you can follow. Your crisis plan is written by you and your mental health team. It should include:
- what triggers might lead to a mental health crisis,
- self-management skills which you have used before and find helpful,
- details of how to access help if the self-management skills aren’t helping. This should include a list of support numbers for out-of-hours teams and crisis teams.
Your doctor may think about offering you sedative medication. Sedatives can help you feel more relaxed. But your doctor should not give you sedatives for more than a week.
Some people find it helpful to contact emotional support lines during a mental health crisis. There is a list of contact numbers at the bottom of this page.
You can find more information about ‘Getting help in a crisis’ by clicking here.
Problems & self-care
What risks and complications can BPD cause?
Self-harm
It is common for people who live with BPD to self-harm. Some people find self-harming can help them to deal with painful feelings. But it can cause serious injury, scars, infections, or accidental death. A big focus of BPD treatment is to find other ways to deal with painful emotions.
Some people find self-harming can help them to deal with painful feelings. But it can cause serious injury, scars, infections, or accidental death. A big focus of BPD treatment is to find other ways to deal with painful emotions.
You can find more information about ‘Self-harm’ by clicking here.
Suicide
People who live with BPD are more at risk of suicide or of attempting suicide. Most people who live with BPD who feel suicidal will feel more positive within a few hours. So it is important to use techniques to try and distract from the strong suicidal feelings.
You can find more information about ‘Suicidal thoughts’ by clicking here.
Drugs and alcohol
People who live with BPD may:
- behave impulsively,
- drink too much alcohol,
- misuse prescription medication, or
- take illegal drugs.
You are more likely to die by suicide if you are also using alcohol. So If you are feeling suicidal you can help keep yourself safer by making sure that you don’t use alcohol.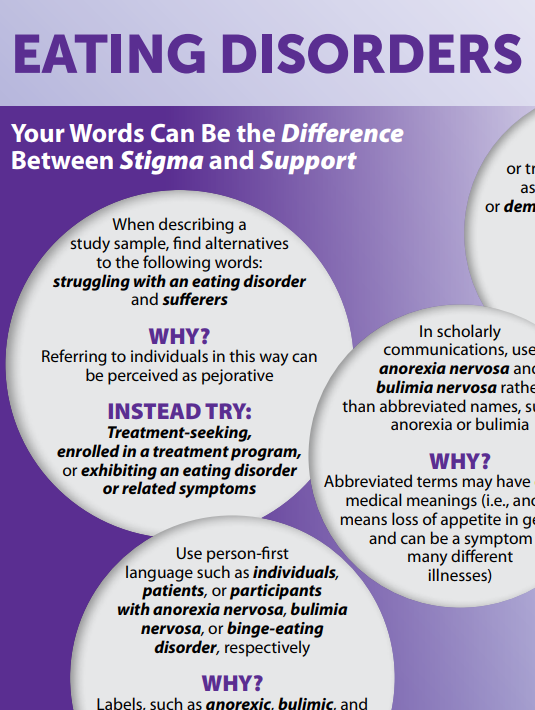
You may be at an increased risk of becoming dependent on alcohol or drugs if you have BPD.
If you drink a lot of alcohol or use drugs, you may find it difficult to get treatment for BPD. But NICE guidelines state that you should be referred to a service that can help with your substance use. And you should be able to continue with BPD treatment where appropriate.
You can find more about ‘Drugs, alcohol and mental health’ by clicking here.
Impulsive behaviours
When people make decisions quickly without thinking about the consequences, doctors call this ‘impulsive’. This can include driving erratically or having multiple sexual partners. Or spending money on things you can't afford or don't need.
If impulsive behaviour leads you to have debt problems you can find more support and information at: www.mentalhealthandmoneyadvice.org.
What if I am not happy with my treatment?
If you are not happy with your treatment you can:
- talk to your doctor about your treatment options,
- ask for a second opinion,
- get an advocate to help you speak to your doctor,
- contact Patient Advice and Liaison Service (PALS) and see whether they can help, or
- make a complaint.
There is more information about these options below.
Treatment options
You should first speak to your doctor about your treatment. Explain why you are not happy with it. You could ask what other treatments you could try.
Tell your doctor if there is a type of treatment that you would like to try. Doctors should listen to your preference. If you are not given this treatment, ask your doctor to explain why it is not suitable for you.
Second opinion
A second opinion means that you would like a different doctor to give their opinion about what treatment you should have. You can also ask for a second opinion if you disagree with your diagnosis.
You don’t have a right to a second opinion. But your doctor should listen to your reason for wanting a second opinion.
Advocacy
An advocate is independent from the NHS. They are free to use. They can be useful if you find it difficult to get your views heard. There are different types of advocates available.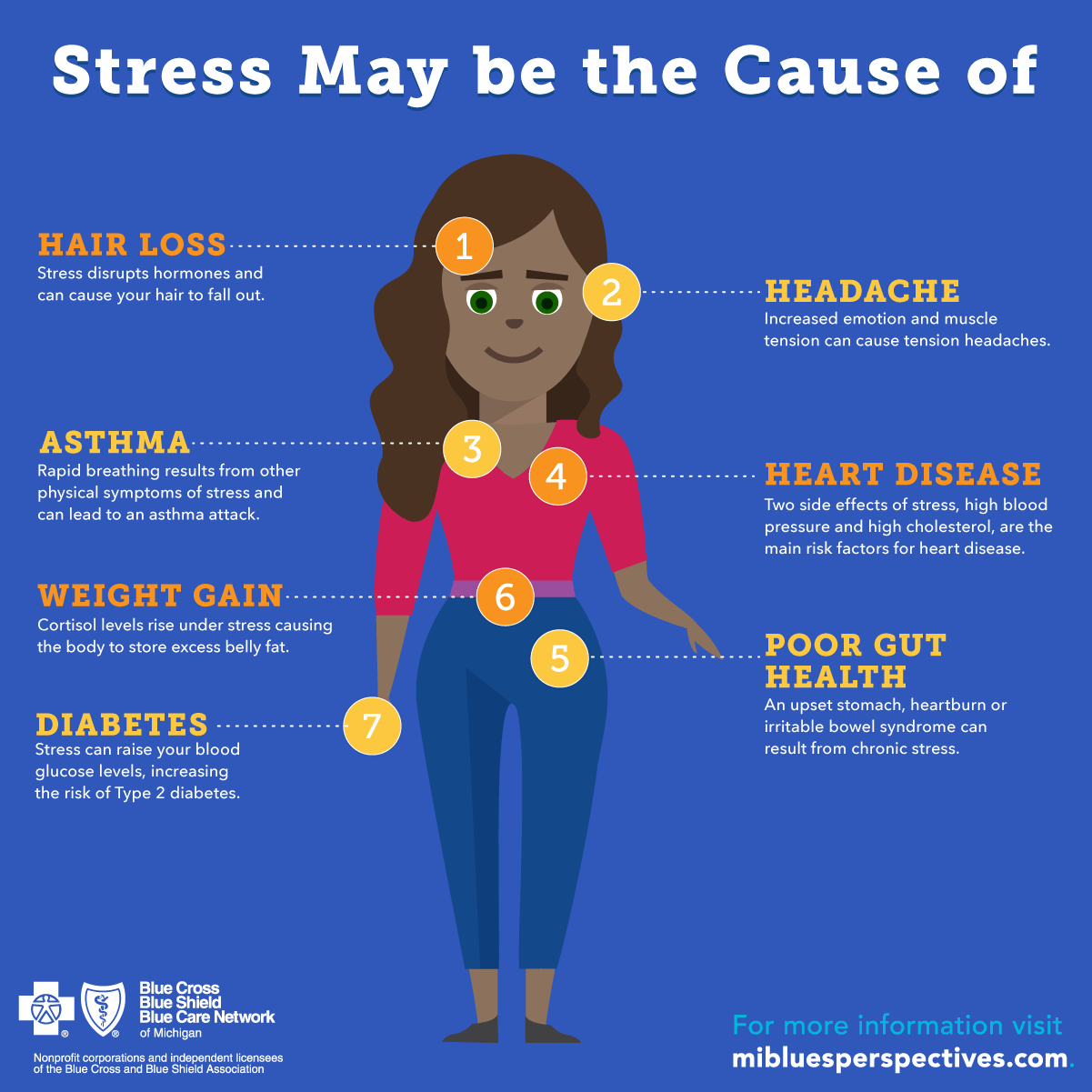
Community advocates can support you to get a health professional to listen to your concerns. And help you to get the treatment that you would like. This type of service doesn’t exist in all areas.
An NHS Complaints Advocate can help you if you want to complain about the NHS. This service exists in all areas.
To search for services, you can try the following.
- Use an internet search engine – use search terms like ‘advocacy Leicestershire’ or ‘mental health advocacy Devon’.
- Ask a support worker or key worker, if you have one.
- Ask your local council whether they have a list.
- Ask your local NHS Patient Advice and Liaison Service (PALS) whether they have a list of local advocacy services.
- Look at local service directories. You can sometimes find useful directories of mental health services online.
- Get in touch with organisations that offer advocacy such as Rethink Mental Illness, Mind, The Advocacy People, Voiceability and POhWER.
The Patient Advice and Liaison Service (PALS)
PALS is part of the NHS. They give information and support to patients.
You can find your local PALS’ details through this website link:
www.nhs.uk/Service-Search/Patient-advice-and-liaison-services-(PALS)/LocationSearch/363.
You can find out more about:
- Medication. Choice and managing problems by clicking here.
- Second opinions by clicking here.
- Advocacy by clicking here.
- Complaining about the NHS or social services by clicking here.
What can I do to manage my symptoms?
You can learn to manage your symptoms by looking after yourself. Selfcare is how you take care of your diet, sleep, exercise, daily routine, relationships and how you are feeling.
Lifestyle
Making small lifestyle changes can improve your wellbeing and can help your recovery.
Routine helps many people with their mental wellbeing. It will help to give a structure to your day and may give you a sense of purpose.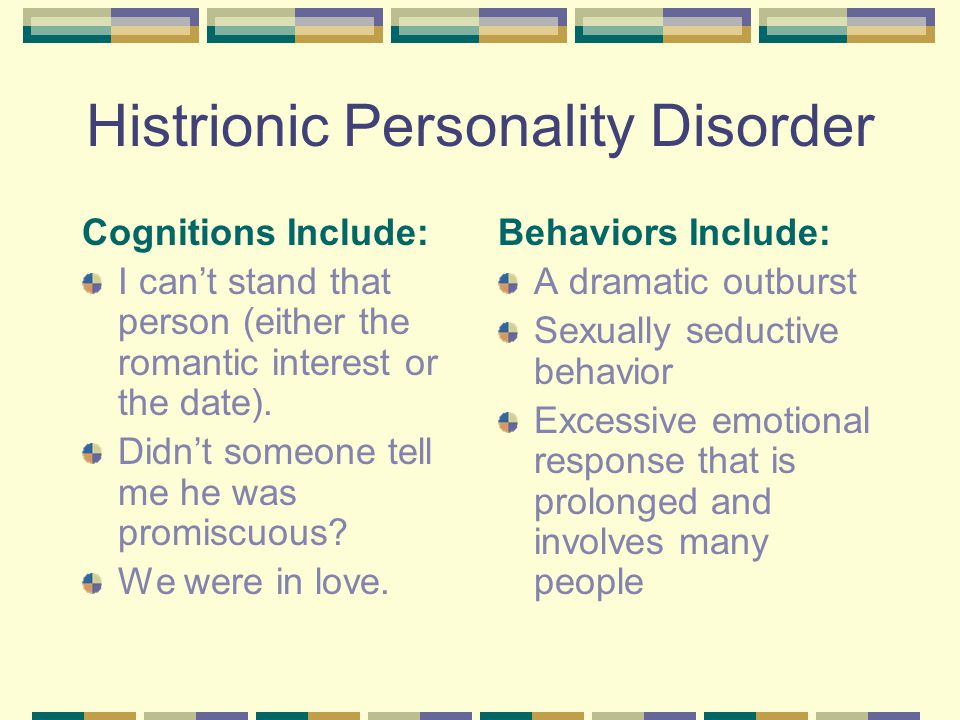 This could be a simple routine such as eating at the same time each day, going to bed at the same time each day and buying food once per week.
This could be a simple routine such as eating at the same time each day, going to bed at the same time each day and buying food once per week.
Breathing exercises
Breathing exercises can help to calm you when you are feeling anxious. You will get the most benefit if you do them regularly, as part of your daily routine.
There is more information about breathing exercises in the further reading section at the bottom of this page.
Support groups
You could join a support group. A support group is where people come together to share information, experiences and give each other support.
You might be able to find a local group by searching online. Rethink Mental Illness have support groups in some areas. You can find out what is available in your area if you follow this link: www.rethink.org/about-us/our-support-groups. Or you can call the Rethink Mental Illness Advice Service on 0808 801 0525 for more information.
Recovery College
Recovery colleges are part of the NHS. They offer free courses about mental health to help you manage your symptoms. They can help you to take control of your life and become an expert in your own wellbeing and recovery. You can usually self-refer to a recovery college. But the college may inform your care team.
They offer free courses about mental health to help you manage your symptoms. They can help you to take control of your life and become an expert in your own wellbeing and recovery. You can usually self-refer to a recovery college. But the college may inform your care team.
Unfortunately, recovery colleges are not available in all areas. To see if there is a recovery college in your area you can use a search engine such as Google. Or contact Rethink Mental Illness Advice Service on 0808 801 0525.
You might also find some of the following things helpful.
- Make sure you speak to a doctor if you think that your relationships with others are being affected.
- Think about how you will benefit from making changes to your lifestyle.
- Don’t pay too much attention to the name of the condition. BPD is a common condition and it is not meant to label you or to suggest that your situation won’t change.
- If you’re offered group therapy or support, give it a chance.
 It may seem intimidating to start with, but a lot of people find it helpful in the long-run.
It may seem intimidating to start with, but a lot of people find it helpful in the long-run. - If something annoys or upsets you, try to wait a while before responding. Think carefully about what you’re going to say and how you’re going to say it.
- Try to find ways of relaxing. Meditation, breathing techniques, listening to music and exercising may be helpful.
- Look for patterns in the ways you respond to things that upset you. This may help you to work through problems in relationships.
- If you self-harm to deal with distress, think of other ways to deal with this. Try punching a pillow or writing about how you feel.
- Use an online mental health forum. Make sure that you check with a mental health professional how trustworthy the website is for helpful information on BPD.
You can find more information about:
- Recovery by clicking here.
- Self-harm by clicking here.
- Suicidal feelings – how to cope by clicking here.

Information for carers, friends and relatives
Information for carers, friends and relatives
As a carer, friend or family member of someone living with borderline personality disorder (BPD), you might find that you need support.
How can I get support?
You can do the following.
- Speak to your relative’s care team about a carer’s assessment.
- Ask for a carer’s assessment from your local social services.
- Join a carers service. They are free and available in most areas.
- Join a carers support group for emotional and practical support. Or set up your own.
- Speak to your GP about medication and talking therapies for yourself if your mental health is affecting your day-to-day life.
What is a carer’s assessment?
A carer’s assessment is an assessment of the support that you need so that you can continue in your caring role.
To get a carers assessment you need to contact your local authority.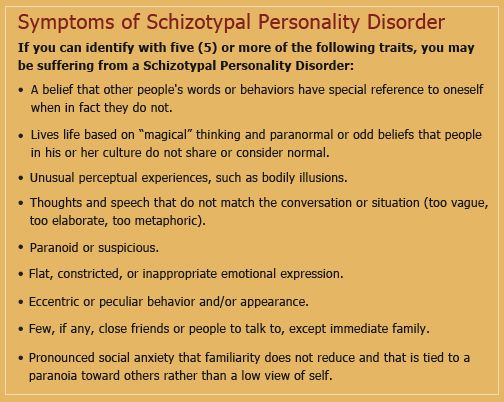
How do I get support from my peers?
You can get peer support through carer support services or carers groups. You can search for local groups in your area by using a search engine such as Google. Or you can contact the Rethink Mental Illness Advice Service and we will search for you.
How can I support the person I care for?
You can do the following.
- Read information about BPD.
- Ask the person you support to tell you what their symptoms are and if they have any self-management techniques that you could help them with.
- Encourage them to see a GP if you are worried about their mental health.
- Ask to see a copy of their care plan, if they have one. They should have a care plan if they are supported by a care coordinator.
- Help them to manage their finances.
How can learning about BPD help?
Learning about BPD can help you to:
- support the person who has BPD,
- understand why they may act in certain ways, and perhaps take things less personally, and
- become more aware of what situations make them more distressed.

Craig's Story
What is a care plan?
The care plan is a written document that says what care your relative or friend will get and who is responsible for it.
A care plan should always include a crisis plan. A crisis plan will have information about who to contact if they become unwell. You can use this information to support and encourage them to stay well and get help if needed.
Can I be involved in care planning?
As a carer you can be involved in decisions about care planning. But you don’t have a legal right to this.
Your relative or friend needs to give permission for the NHS to share information about them and their care.
You can find out more about:
- Supporting someone with a mental illness by clicking here.
- Getting help in a crisis by clicking here.
- Suicidal thoughts. How to support someone by clicking here.
- Responding to unusual thoughts and behaviours by clicking here.
- Carers assessment by clicking here.
- Confidentiality and information sharing. For carers, friends and family by clicking here.
- Money matters: dealing with someone else’s money or benefits by clicking here.
- Worried about someone’s mental health by clicking here.
- Benefits for carers by clicking here.
- Stress by clicking here.
Further reading
North West Boroughs Healthcare NHS Foundation Trust
This NHS website has information dedicated to different breathing techniques. These techniques can help you when you feel anxious.
Website: www.nwbh.nhs.uk/healthandwellbeing/Pages/Breathing-Techniques-.aspx
Centre for Clinical Interventions
This website is provided by the department of Health in Western Australia. They have some useful information sheets and a workbook for people who are experiencing problems with coping with their feelings.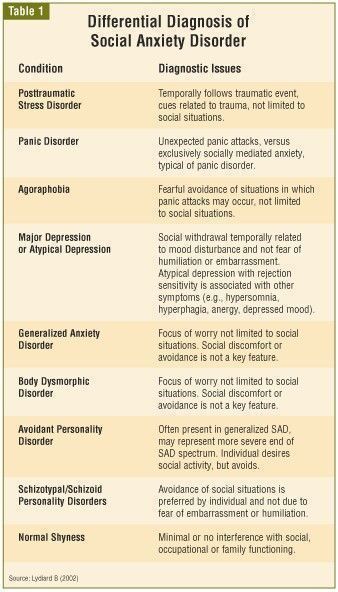 And for people experiencing distress.
And for people experiencing distress.
Website: www.cci.health.wa.gov.au/Resources/For-Clinicians/Distress-Tolerance
You can find out more about:
- Getting help in a crisis by clicking here.
- Suicidal thoughts - How to cope by clicking here.
- Self-harm by clicking here.
- Drugs, alcohol and mental health by clicking here.
- Carers assessment - Under the Care Act 2014 by clicking here.
- Confidentiality and information sharing - For carers, friends and family by clicking here.
- Worried about someone’s mental health by clicking here.
- Stress - How to cope by clicking here.
Useful contacts
BPD World
Provides information and support to people affected by personality disorders. It has an online support forum.
Website: www.bpdworld.org
Samaritans
Can be contacted by telephone, letter, e-mail and mini-com. There's also a face-to-face service, available at their local branches. They are open 24 hours a day, every day of the year.
There's also a face-to-face service, available at their local branches. They are open 24 hours a day, every day of the year.
Telephone: 116 123
Email: [email protected]
Website: www.samaritans.org
ASSISTline
National helpline offering supportive listening service to anyone throughout the UK with thoughts of suicide or thoughts of self-harm. They are open 24/7.
Telephone: 0800 689 5652
Website: www.spbristol.org/
Sane Line
Work with anyone affected by mental illness, including families, friends and carers. They also provide a free text-based support service called Textcare and an online supportive forum community where anyone can share their experiences of mental health.
Telephone: 0300 304 7000
Textcare: www.sane.org.uk/what_we_do/support/textcare
Support Forum: www. sane.org.uk/what_we_do/support/supportforum
sane.org.uk/what_we_do/support/supportforum
Website: www.sane.org.uk
Support Line
They offer confidential emotional support to children, young adults and adults by telephone, email and post. They work with callers to develop healthy, positive coping strategies, an inner feeling of strength and increased self-esteem to encourage healing, recovery and moving forward with life. Their opening hours vary so you need to ring them for details.
Telephone: 01708 765200
E-mail: [email protected]
Website: www.supportline.org.uk
CALM (Campaign Against Living Miserably)
CALM is leading a movement against suicide. They offer accredited confidential, anonymous and free support, information and signposting to people anywhere in the UK through their helpline and webchat service.
Telephone: 0800 58 58 58
Webchat: through the website
Website: www.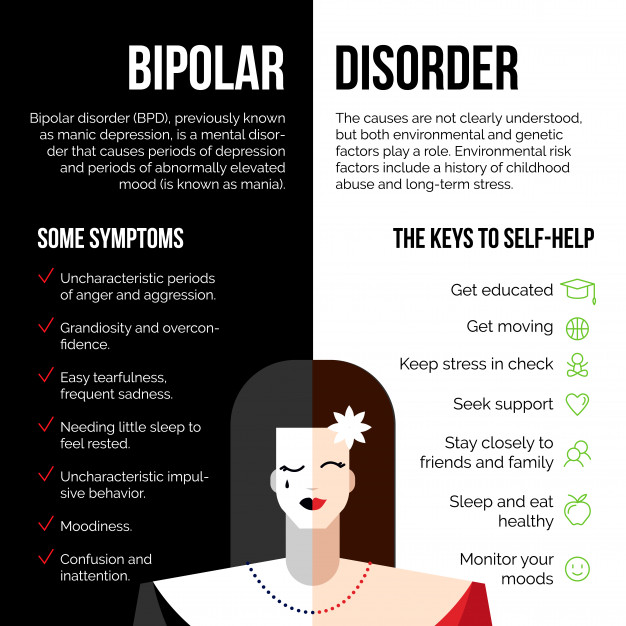 thecalmzone.net
thecalmzone.net
My Black Dog
Provides peer support webchat with volunteers who have experienced mental illness. Available evenings and weekends. Check the website for opening times.
Website: www.myblackdog.co
Papyrus UK
Work with people under 35 who are having suicidal feelings. And with people who are worried about someone under 35.
Telephone: 0800 068 41 41
Email: [email protected]
Text: 07786 209697
Website: www.papyrus-uk.org
Shout
If you’re experiencing a personal crisis, are unable to cope and need support, text Shout to 85258. Shout can help with urgent issues such as suicidal thoughts, abuse or assault, self-harm, bullying and relationship challenges.
Text: Text Shout to 85258
Website: www.giveusashout.org/
Need more advice?
If you need more advice or information you can contact our Advice and Information Service.
Contact us Contact us
More resources
ᐈ How to treat an emotional disorder? ≡ Brain Stimulation Center
brain stimulation center
Kyiv
Kyiv
White church
Addresses of clinics
Kyiv, 13-B Vasily Porik Ave
Kyiv, st. Velyka Vasylkivska, 66, dentistry (On the map)
Skole, st. Stryiska, 19 (opening soon) (On the map)
Kyiv, st. Composer Meitus, 5 (On the map)
Belaya Tserkov, st. Gagarina 37A (On the map)
+38 (044) 364-20-04 +38 (093) 170-16-59
Mon.-Sun. 08:30 - 20:00
+38 (067) 761-63-44 (Dentistry)
Mon.-Sat. 9:00-19:00, Sun. 9:00-18:00
UkrRus
Sign up
Sign up
- 👉 How to treat an emotional disorder?
Emotional disorder
Emotional outbursts, outbursts of aggression, impulsive actions create discomfort in communication with the family and other people. It is worth seeking advice from leading specialists and getting highly qualified assistance in the fight against psycho-emotional disorder.
Enroll
Have you become prone to outbursts of aggression or impulsive actions? Do emotional outbursts scare you and cause your professional activity or family to suffer because of them? To correct the situation, the help of professionals is needed. Contacting the Brain Stimulation Center will help you get an answer to the question of how to treat an emotional disorder and conduct an effective course of therapy using modern methods of evidence-based medicine.
Emotional disorder is one of the personality disorders, which is characterized by imbalance, impulsiveness of actions without considering the consequences and reduced control of actions. Common symptoms of disorders are manifested by a lack of self-control, inability and unwillingness to obey generally accepted rules and norms due to insufficient self-control and impulsivity, difficulties in creating and maintaining contacts with other people.
Common symptoms of disorders are manifested by a lack of self-control, inability and unwillingness to obey generally accepted rules and norms due to insufficient self-control and impulsivity, difficulties in creating and maintaining contacts with other people.
Emotional disorders can be treated psychotherapeutically, and people suffering from these disorders can learn the necessary rules for interacting with society.
Classification of emotional disorders
There are two types of emotional disorders:
- Emotionally unstable personality disorder.
Divided into impulsive and borderline types. Impulsive disturbance is manifested by a lack of self-control and increased emotional lability. For the borderline type, aggression towards others is less characteristic and is characterized by impaired self-perception, a chronic feeling of inner emptiness, unstable and tense interpersonal relationships, a tendency to self-destruction (including suicidal attempts or gestures).
- Dissocial personality disorder.
Violations are manifested by indifference to others and disregard for social norms and duties. Behavior is difficult to correct and does not change even after punishment. People easily succumb to aggression and show violence.
The etiology of emotional disorders
The causes of emotional disorders are associated with disorders of the central nervous system and most often occur against the background of the following factors:
- traumatic situation;
- prolonged stress;
- CNS injury;
- vascular diseases;
- neurological pathologies;
- endocrine disorders;
- mental disorders;
- hereditary predisposition.
The first manifestations of emotional instability may occur in childhood or appear after exposure to the causes of the disorder.
Pathogenesis of emotional disorders
An emotional disorder develops when there is an imbalance between the processes of excitation and inhibition of the central nervous system. Due to the acceleration of neural transmission of impulses, purposefulness decreases and the emotional response becomes inadequate in relation to the strength of the stimulus.
Due to the acceleration of neural transmission of impulses, purposefulness decreases and the emotional response becomes inadequate in relation to the strength of the stimulus.
Clinical manifestations of emotional disorders
The nature of the signs of an emotional disorder depends on the type of disorder.
In the impulsive variety of emotionally unstable personality disorder, there is:
- frequent and unreasonable mood swings;
- predisposition to outbursts of aggression and anger;
- impulsive and uncontrollable actions;
- hypersensitivity to criticism.
The symptoms of an emotional disorder of the impulsive type are often accompanied by a predisposition to manipulation, excessive suspicion and unreasonable jealousy.
With the borderline type, aggression towards others is less pronounced. Patients are prone to the following manifestations:
- increased anxiety and suspiciousness;
- loneliness and feeling of chronic inner emptiness;
- complex relationships with the opposite sex from boundless adoration to complete rejection;
- tendency to self-harm (up to suicidal gestures or attempts).
In case of dissocial personality disorder, the following is observed:
- disregard for social norms and duties;
- no change in behavior even after punishment;
- slight susceptibility to aggression;
- committing violent acts;
- tendency to blame others;
- plausibility of justifications for their inadequate actions.
Specialists also identify general symptoms of emotional disorders:
- disorders create difficulties in professional activities, communication with strangers and close people;
- onset of first signs in early childhood or adolescence;
- self-centeredness;
- there are no obvious phases of exacerbations and remissions;
- low empathy.
Features of the course of emotional disorders during pregnancy
Against the background of gestation, the hormonal background changes significantly and the manifestations of emotional dysregulation are aggravated. The unstable psycho-emotional state of a pregnant woman can negatively affect the state of the fetus and the health of the unborn baby.
The unstable psycho-emotional state of a pregnant woman can negatively affect the state of the fetus and the health of the unborn baby.
Complications of emotional disorders
Lack of qualified help leads to various negative consequences of emotional disorders:
- constant conflicts in the family and with other people;
- development and exacerbation of somatic diseases;
- professional unfulfillment;
- mental strain;
- isolation from society;
- chronic fatigue;
- depression;
- suicide attempts.
With emotional disorders, patients often experience a decrease in motivation to improve their well-being and relationships with society, and they need help from relatives to organize treatment.
Diagnosis of emotional disorders
If an emotional disorder is suspected, a consultation with a psychiatrist and a neurologist is recommended.
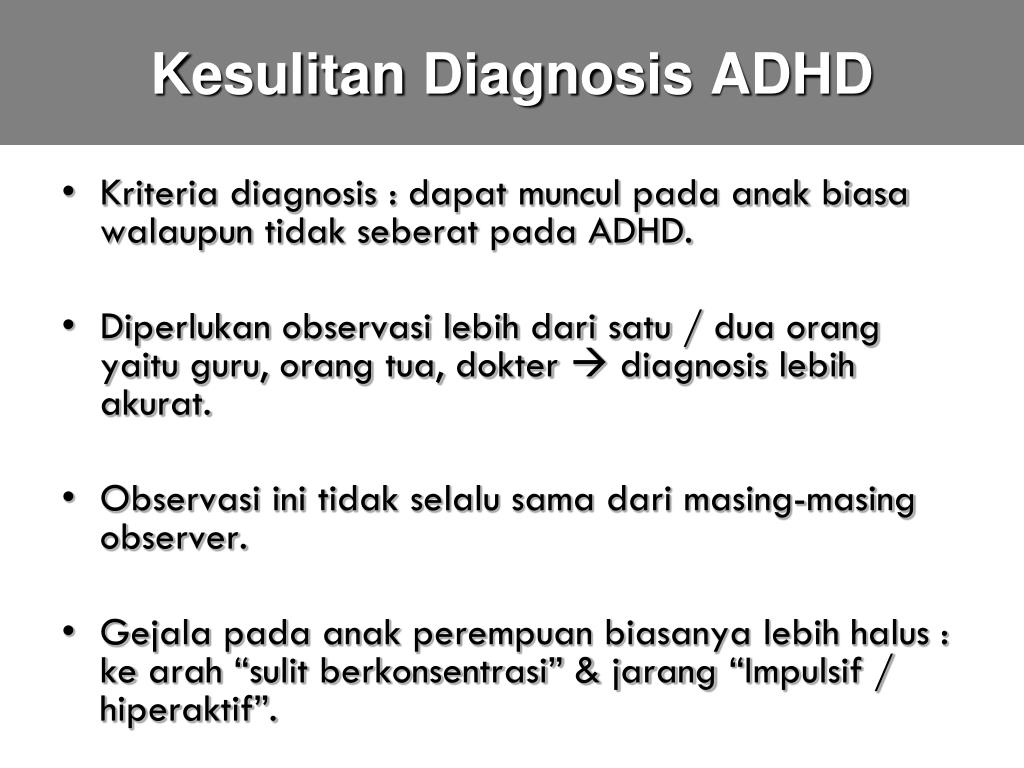
To diagnose emotional disorders, the doctor conducts a conversation with the patient, studies the history of his illness and life, and asks additional questions.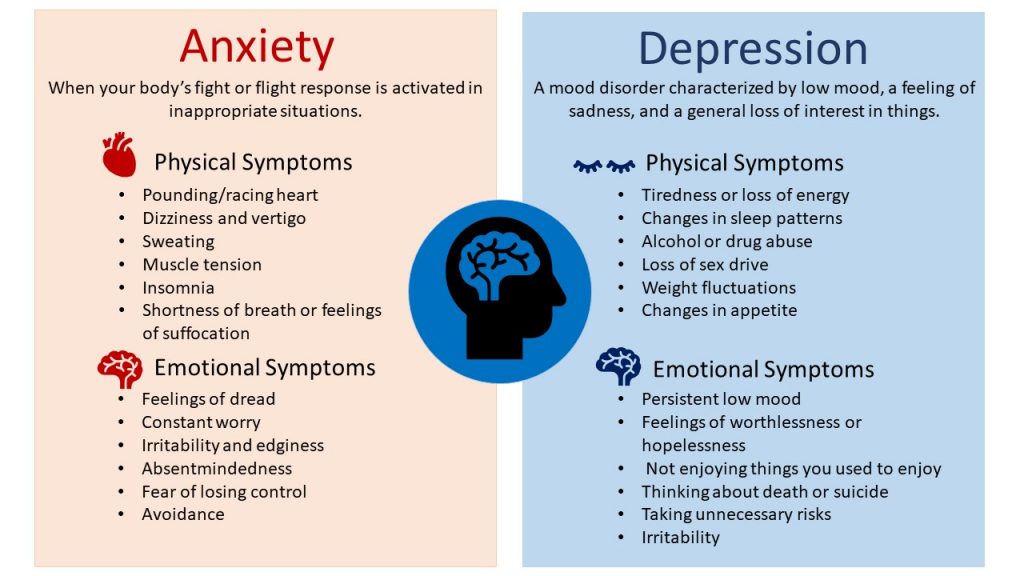 Identification of violations is confirmed by the results of the test for emotional disorder. To exclude errors, an EEG is performed, differential diagnostics is performed for patients with epilepsy, borderline and hysterical personality disorder.
Identification of violations is confirmed by the results of the test for emotional disorder. To exclude errors, an EEG is performed, differential diagnostics is performed for patients with epilepsy, borderline and hysterical personality disorder.
Treatment of emotional disorders
Tactics for the treatment of emotional disorders is determined by the psychotherapist personally after a comprehensive examination. Medication is not always prescribed, and medication is usually required when the disorder is combined with depression or other mental disorders. The main methods of treatment are cognitive-behavioral and dialectical therapy. Individual and group classes are conducted by a psychotherapist and psychologist. They teach patients self-control and help them understand their thoughts and psycho-emotional reactions.
Various physiotherapy procedures can effectively complement psychotherapy and drug treatment:
- Hyperbaric oxygen therapy.
During HBO sessions, tissue oxygenation improves psychological and cognitive functions, tones and eliminates chronic fatigue syndrome. SPECT scans show that low blood flow is usually associated with mental health problems. Therefore, the HBO procedure activates the vital process of blood flow to the brain, which directly positively affects the mental state.
SPECT scans show that low blood flow is usually associated with mental health problems. Therefore, the HBO procedure activates the vital process of blood flow to the brain, which directly positively affects the mental state. - Bioacoustic correction.
BAC procedures stabilize the psycho-emotional state, reduce reactive and personal anxiety, improve well-being and mood. - Transcranial micropolarization.
TCMP sessions help strengthen tissue connections and improve the meaningfulness of actions in response to an incoming signal. The patient stabilizes the processes of excitation and inhibition, normalizes sleep. - Hypoxic therapy.
The procedure consists in inhaling air with a reduced oxygen content, which activates the body's own forces, normalizes the functioning of the immune system. At the same time, a new capillary network is formed in the brain, which increases its blood supply. And this directly affects the improvement of the mental state.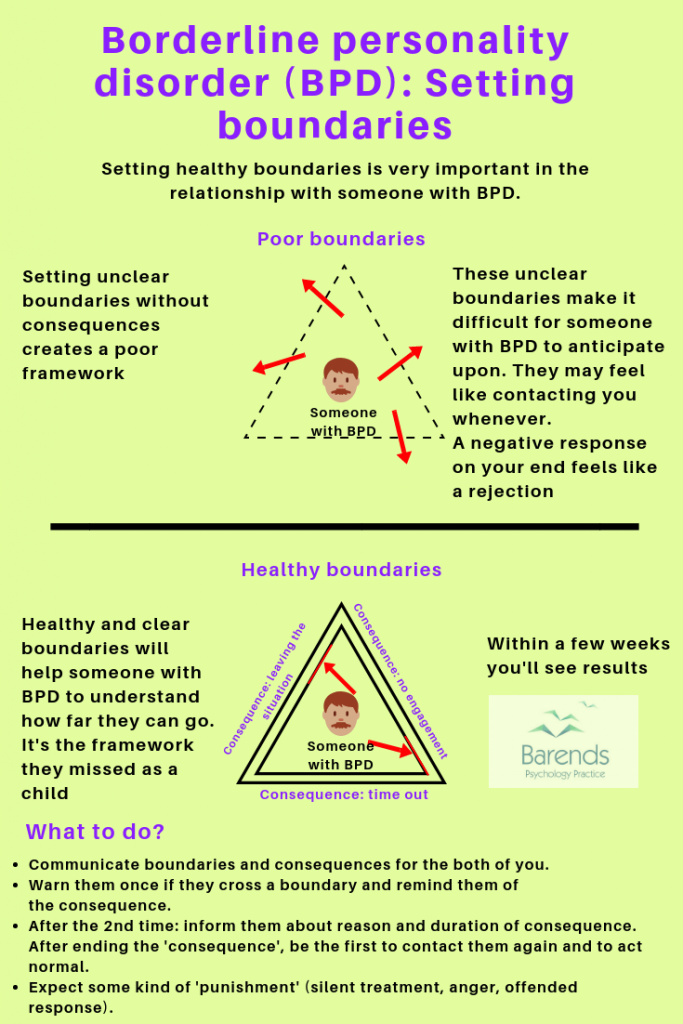
- Physiotherapy.
The use of exercise therapy, massage and other physiotherapy helps to improve cerebral circulation, eliminates emotional stress and fatigue, improves cognitive function and physiological response to stress factors. The use of physiotherapy in the treatment of mental illness is included in the WHO recommendations and adapted by the International Organization for Physical Therapy in Mental Health.
The treatment can also be supplemented with music therapy and art therapy.
Prevention of emotional disorders
To prevent the development of psycho-emotional disorders, it is necessary to follow a number of rules:
- correctly plan the regime of work and rest;
- prevent stressful situations and increase stress resistance;
- timely detect and treat mental disorders, vascular, neurological and endocrine diseases.
- reduce the risk of CNS injury;
Which doctor treats emotional disorders?
Have you made a decision to undergo therapy for an emotional disorder and are looking for experienced specialists? Contacting the "Brain Stimulation Center" will help you get comprehensive professional assistance from experienced doctors.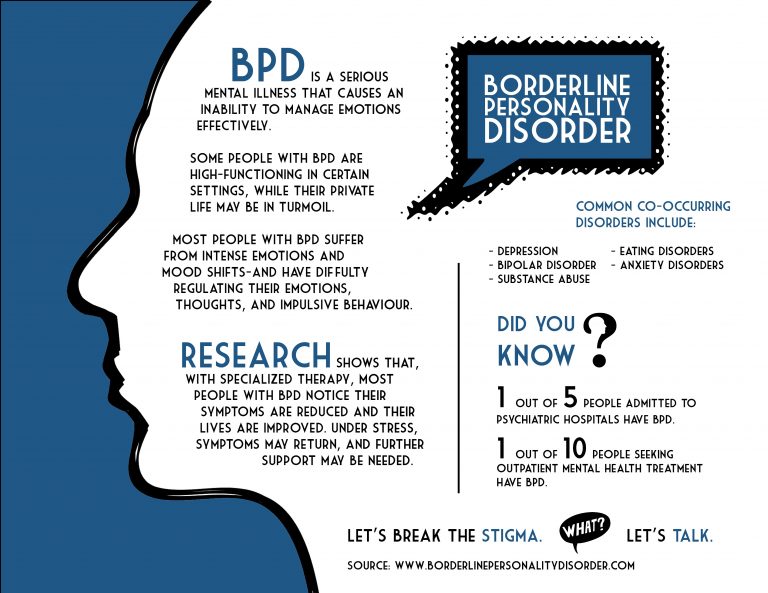 You can make an appointment with a specialist by calling the phone number indicated on the website or by filling out a special form for online appointment or call back. Contact us and we will help you live in harmony with others!
You can make an appointment with a specialist by calling the phone number indicated on the website or by filling out a special form for online appointment or call back. Contact us and we will help you live in harmony with others!
Reviews
leave a review
Leave a review:
ThanksNeutralNegative
Your score:
GratitudeNeutralNegative
Make an appointment
By submitting this form, you agree to the data privacy and privacy practices of this site
By submitting this form, you are consenting to the privacy and privacy practices of this site
Emotional personality disorder - treatment and rehabilitation at the Allianz Central Medical Health Center
Emotionally unstable (labile) personality disorder is hyperexcitability, impulsivity, low ability to self-control and emotional imbalance. Like other personality disorders, it is more of a character pathology ("severe character") rather than a disease.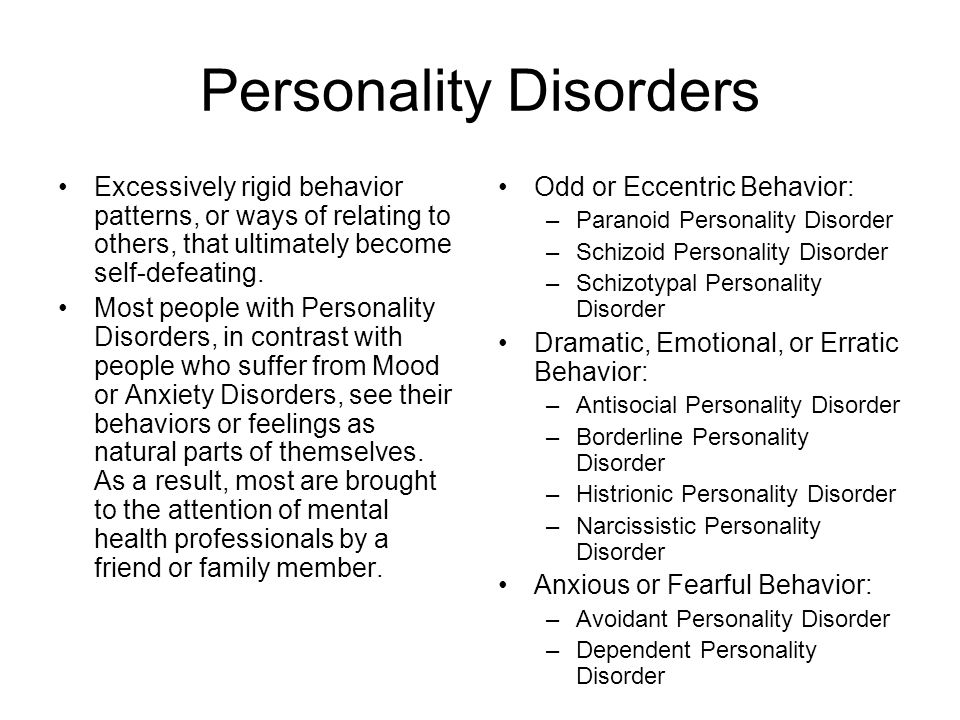 An experienced psychotherapist can help with the disorder.
An experienced psychotherapist can help with the disorder.
Important
"Severe character", the inability to cope with one's emotions is a reason to seek help from a psychotherapist.
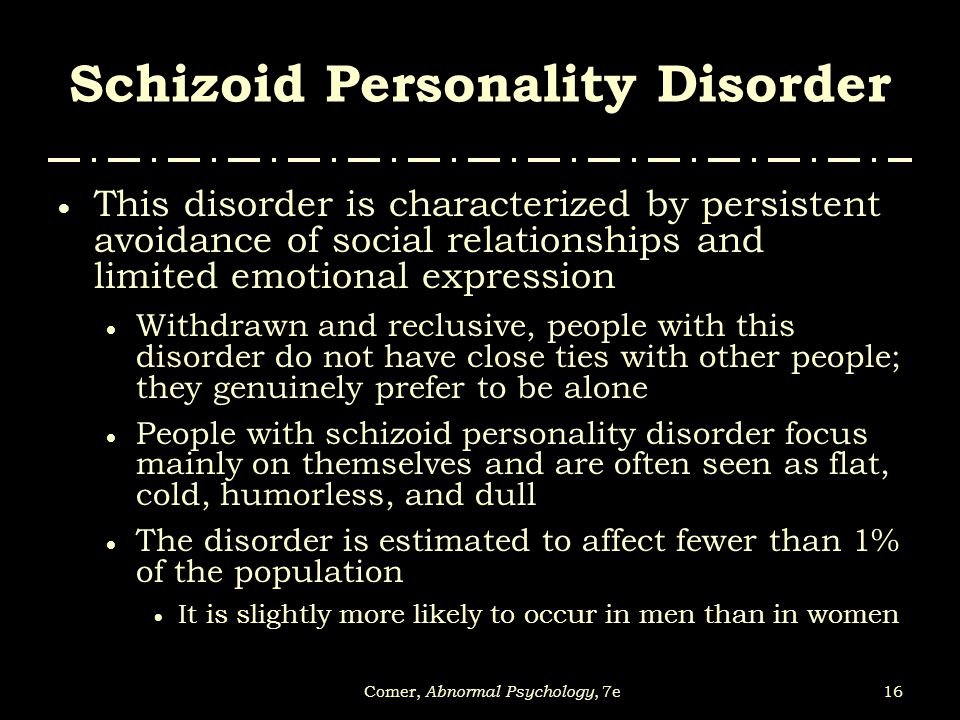
In another way it is called aggressive, epileptoid, excitable, explosive personality disorder. Sometimes doctors treat it as two separate disorders—impulsive personality disorder and borderline personality disorder.
A common feature of people with both variants of emotionally unstable personality disorder is that it is difficult for them to restrain themselves, obey norms and rules due to weak self-control and impulsivity. Character traits make it difficult to establish and maintain contacts with others. Treatment by a psychotherapist for such people is an opportunity to accept the peculiarities of their psyche and learn to live in harmony with others.
Symptoms of epileptoid personality disorder
If we talk about the classification of emotionally unstable personality disorder, ICD-10 divides it into two subspecies:
- Impulsive.
- Border.
An emotionally unstable personality disorder of the impulsive type is characterized by severe emotional lability (frequent unreasonable mood changes), a tendency to impulsive acts and aggressive outbursts with an inability to restrain. People with this disorder have a hard time with criticism and censure.
Epileptoids are characterized by jealousy, suspicion, manipulation, irritability and outbursts of anger.
For an emotionally unstable personality disorder of the borderline type, aggressive behavior towards others is less characteristic, but such people are prone to self-harm, up to suicidal acts. Learn more about borderline disorder.
According to ICD-10, a disorder is characterized by common features of a personality disorder and specific features. The general criteria are as follows:
- begins to appear in childhood and adolescence, persists into adulthood;
- it is difficult to distinguish clear phases of recovery/exacerbation;
- character traits make it difficult to communicate with relatives and strangers, do not allow to take place professionally;
- people are often self-centered, incapable of empathy (sympathy for other people), constantly striving for pleasure.
Specific symptoms of the impulsive (explosive) type of emotionally unstable personality disorder:
- Impulsivity in thoughts and actions.
- Low ability to self-control.
- Outbursts of anger.
- Tendency to cruel and asocial acts.
- Intolerance to censure and criticism.
To diagnose the impulsive type of emotionally unstable personality disorder, the psychotherapist talks in detail with the client.
Differential diagnosis is carried out with other personality disorders (borderline, hysterical), as well as with epilepsy. For this, a pathopsychological study is used (performed by a clinical psychologist), EEG, Neurotest.
An integrated approach to diagnosis is necessary so that the doctor can prescribe the most effective treatment for this person.
Emotionally unstable personality disorder - treatment
People with emotionally unstable personality disorder are especially in dire need of the help of a psychotherapist.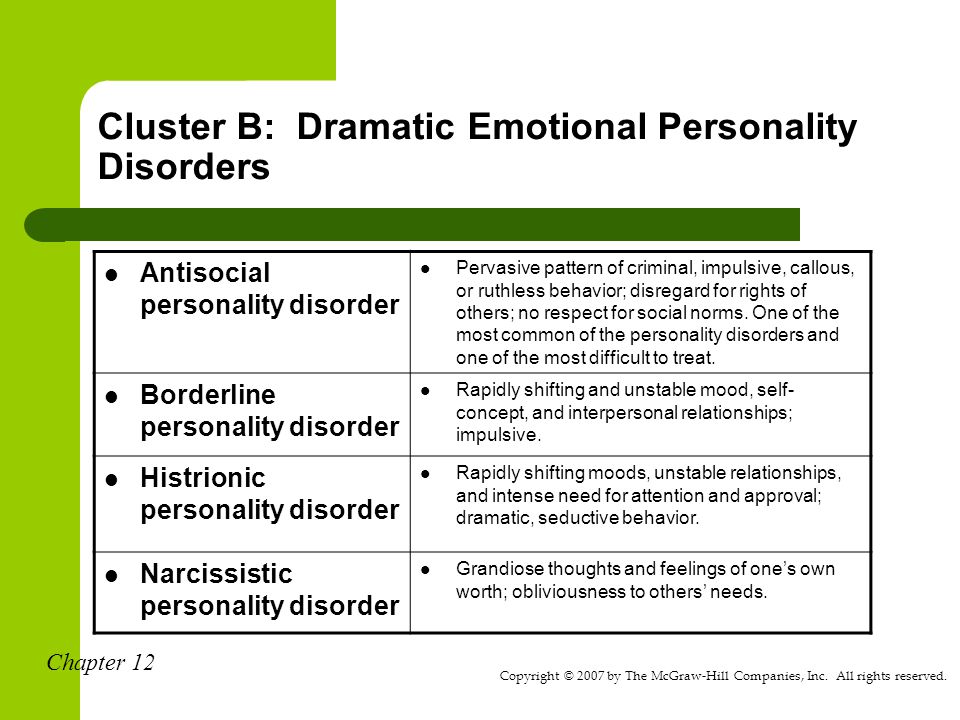 A specialist can teach them to control their emotions and prevent the negative impact of emotional outbursts on others (with impulsive disorder) and on the person himself (with borderline personality disorder).
A specialist can teach them to control their emotions and prevent the negative impact of emotional outbursts on others (with impulsive disorder) and on the person himself (with borderline personality disorder).
Labile personality disorder is described as one of the most difficult diagnoses to treat. Establishing contact with a person who suffers from an emotionally unstable personality disorder is not an easy task for a psychotherapist. Inexperienced professionals avoid a strong alliance with such patients so as not to lose their own peace of mind.
But at the same time, it is important to remember that a personality disorder is not a disease, the patient does not have damage to the nervous system. Therefore, with proper treatment, it achieves serious positive results. People with borderline and aggressive personality disorders should be treated by an experienced psychotherapist.
Important
Psychotherapy is the main non-drug treatment for mental disorders.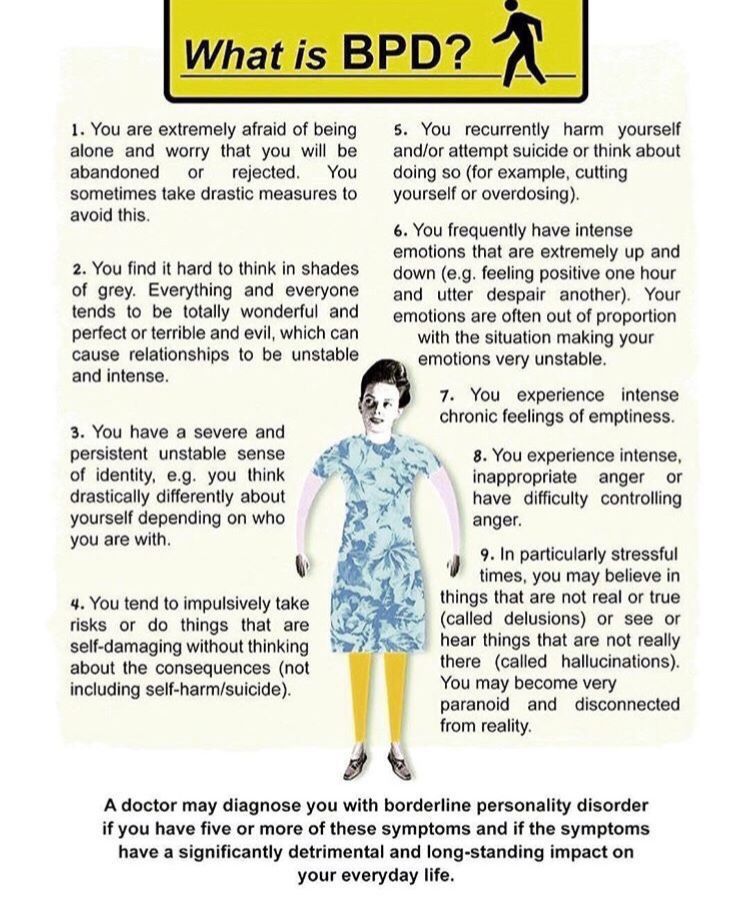 Unlike medicines that eliminate symptoms, it works with the cause - it allows you to achieve a long-term, lasting result.
Unlike medicines that eliminate symptoms, it works with the cause - it allows you to achieve a long-term, lasting result.
The main treatment for emotional personality disorder is psychotherapy. Drug treatment is not used in all cases. Medication support may sometimes be needed if the personality disorder is co-occurring with other illnesses, such as depression.
The most effective techniques when working with people who suffer from emotionally labile personality disorder are cognitive behavioral therapy and dialectical behavioral therapy. They help patients become aware of the thoughts and feelings that influence their actions and teach them to control themselves.
Subject to all the recommendations of the doctor and, most importantly, the desire of the patient to interact with the psychotherapist, the therapy gives a lasting positive effect. At the same time, the specialist does not seek to change the patient's personality, but helps to accept oneself and learn to live in harmony with oneself and others.