Is adhd axis 1 or 2
Axis I and II comorbidity in adults with ADHD
. 2007 Aug;116(3):519-28.
doi: 10.1037/0021-843X.116.3.519.
Torri W Miller 1 , Joel T Nigg, Stephen V Faraone
Affiliations
Affiliation
- 1 Department of Psychology, Michigan State University, East Lansing, MI 48824, USA. [email protected]
- PMID: 17696708
- DOI: 10.1037/0021-843X.116.3.519
Torri W Miller et al. J Abnorm Psychol. 2007 Aug.
. 2007 Aug;116(3):519-28.
doi: 10.1037/0021-843X.116.3.519.
Authors
Torri W Miller 1 , Joel T Nigg, Stephen V Faraone
Affiliation
- 1 Department of Psychology, Michigan State University, East Lansing, MI 48824, USA. [email protected]
- PMID: 17696708
- DOI: 10.1037/0021-843X.116.3.519
Abstract
Ongoing debate over the validity of the attention-deficit/hyperactivity disorder (ADHD) construct in adulthood is fueled in part by uncertainty regarding implications of potentially extensive yet incompletely described comorbid Axis I and II psychopathology. Three hundred sixty-three adults ages 18 to 37 completed semistructured clinical interviews; informants were also interviewed, and best estimate diagnoses were obtained. Results were as follows: First, ADHD combined type (ADHD-C) had an excess of externalizing and internalizing Axis I disorders, suggesting a gradient-of-severity relationship between it and ADHD inattentive type (ADHD-I). Second, ADHD-C and ADHD-I did not differ in frequency of Axis II disorders. Third, however, ADHD overall was associated with increased rates of Axis II disorders, compared with rates in non-ADHD control participants, including both Cluster B (primarily borderline personality disorder) and Cluster C disorders. Fourth, ADHD incrementally accounted for clinician-rated global assessment of functioning scores above and beyond comorbid conditions or symptoms on either Axis I or Axis II. Results further inform nosology of ADHD in adults.
Three hundred sixty-three adults ages 18 to 37 completed semistructured clinical interviews; informants were also interviewed, and best estimate diagnoses were obtained. Results were as follows: First, ADHD combined type (ADHD-C) had an excess of externalizing and internalizing Axis I disorders, suggesting a gradient-of-severity relationship between it and ADHD inattentive type (ADHD-I). Second, ADHD-C and ADHD-I did not differ in frequency of Axis II disorders. Third, however, ADHD overall was associated with increased rates of Axis II disorders, compared with rates in non-ADHD control participants, including both Cluster B (primarily borderline personality disorder) and Cluster C disorders. Fourth, ADHD incrementally accounted for clinician-rated global assessment of functioning scores above and beyond comorbid conditions or symptoms on either Axis I or Axis II. Results further inform nosology of ADHD in adults.
(c) 2007 APA, all rights reserved
Similar articles
-
Family psychiatric history evidence on the nosological relations of DSM-IV ADHD combined and inattentive subtypes: new data and meta-analysis.
Stawicki JA, Nigg JT, von Eye A. Stawicki JA, et al. J Child Psychol Psychiatry. 2006 Sep;47(9):935-45. doi: 10.1111/j.1469-7610.2006.01628.x. J Child Psychol Psychiatry. 2006. PMID: 16930388
-
ADHD with comorbid oppositional defiant disorder or conduct disorder: discrete or nondistinct disruptive behavior disorders?
Connor DF, Doerfler LA. Connor DF, et al. J Atten Disord. 2008 Sep;12(2):126-34. doi: 10.1177/1087054707308486. Epub 2007 Oct 12. J Atten Disord. 2008. PMID: 17934178
-
Comparative study of children with ADHD only, autism spectrum disorder + ADHD, and chronic multiple tic disorder + ADHD.
Gadow KD, DeVincent CJ, Schneider J. Gadow KD, et al. J Atten Disord. 2009 Mar;12(5):474-85.
 doi: 10.1177/1087054708320404. J Atten Disord. 2009. PMID: 19218544
doi: 10.1177/1087054708320404. J Atten Disord. 2009. PMID: 19218544 -
Recognizing ADHD in adults with comorbid mood disorders: implications for identification and management.
Goodman DW, Thase ME. Goodman DW, et al. Postgrad Med. 2009 Sep;121(5):20-30. doi: 10.3810/pgm.2009.09.2049. Postgrad Med. 2009. PMID: 19820271 Review.
-
A review of attention-deficit/hyperactivity disorder complicated by symptoms of oppositional defiant disorder or conduct disorder.
Connor DF, Steeber J, McBurnett K. Connor DF, et al. J Dev Behav Pediatr. 2010 Jun;31(5):427-40. doi: 10.1097/DBP.0b013e3181e121bd. J Dev Behav Pediatr. 2010. PMID: 20535081 Review.
See all similar articles
Cited by
-
Depressive symptoms in youth with ADHD: the role of impairments in cognitive emotion regulation.
Mayer JS, Brandt GA, Medda J, Basten U, Grimm O, Reif A, Freitag CM. Mayer JS, et al. Eur Arch Psychiatry Clin Neurosci. 2022 Aug;272(5):793-806. doi: 10.1007/s00406-022-01382-z. Epub 2022 Feb 2. Eur Arch Psychiatry Clin Neurosci. 2022. PMID: 35107603 Free PMC article.
-
ADHD and Bipolar Disorder in Adulthood: Clinical and Treatment Implications.
Salvi V, Ribuoli E, Servasi M, Orsolini L, Volpe U. Salvi V, et al. Medicina (Kaunas). 2021 May 10;57(5):466. doi: 10.3390/medicina57050466. Medicina (Kaunas). 2021. PMID: 34068605 Free PMC article. Review.
-
Eating behaviors, depression, and anxiety levels of pre bariatric surgery patients with obesity comorbid with or without Attention deficit and hyperactivity disorder: ADHD or Major Depression? Which is more related with eating behaviors?
Şahan E, Zengin Eroğlu M, Sertçelik S.
 Şahan E, et al. Brain Behav. 2021 Jan;11(1):e01915. doi: 10.1002/brb3.1915. Epub 2020 Oct 28. Brain Behav. 2021. PMID: 33118314 Free PMC article.
Şahan E, et al. Brain Behav. 2021 Jan;11(1):e01915. doi: 10.1002/brb3.1915. Epub 2020 Oct 28. Brain Behav. 2021. PMID: 33118314 Free PMC article. -
Bidirectional Associations Between Self-Reported Gaming Disorder and Adult Attention Deficit Hyperactivity Disorder: Evidence From a Sample of Young Swiss Men.
Marmet S, Studer J, Grazioli VS, Gmel G. Marmet S, et al. Front Psychiatry. 2018 Dec 11;9:649. doi: 10.3389/fpsyt.2018.00649. eCollection 2018. Front Psychiatry. 2018. PMID: 30618855 Free PMC article.
-
Six-Month Outcomes for Collaborative Care Management of Depression Among Smoking and Nonsmoking Patients.
Witt DR, Garrison GM, Gonzalez CA, Witt TJ, Angstman KB. Witt DR, et al. Health Serv Res Manag Epidemiol.
 2017 Aug 29;4:2333392817721648. doi: 10.1177/2333392817721648. eCollection 2017 Jan-Dec. Health Serv Res Manag Epidemiol. 2017. PMID: 28890910 Free PMC article.
2017 Aug 29;4:2333392817721648. doi: 10.1177/2333392817721648. eCollection 2017 Jan-Dec. Health Serv Res Manag Epidemiol. 2017. PMID: 28890910 Free PMC article.
See all "Cited by" articles
MeSH terms
ADHD Diagnosis | ADHD institute
How is ADHD diagnosed?
When evaluating individuals for attention-deficit hyperactivity disorder (ADHD), or hyperkinetic disorder (HKD), it is typical to use multiple stages of assessment prior to formal diagnosis, including1-5:
- Clinical assessments
- Assessment tools and rating scales
- Clinical interviews with the individuals and parents/teachers for children and adolescents or partners for adults with ADHD.
The National Institute for Health and Care Excellence (NICE) guidelines state that a diagnosis of ADHD should only be made by a specialist psychiatrist, paediatrician or other appropriately qualified healthcare professional with training and expertise in the diagnosis of ADHD.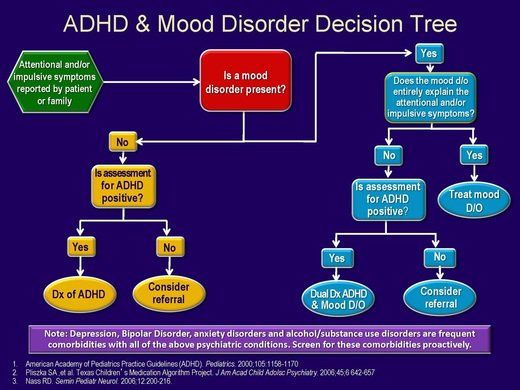 Diagnosis of ADHD should also be based upon a full clinical and psychosocial assessment, a full developmental and psychiatric history, and observer reports of the individual’s mental state. According to the NICE guidelines, for a diagnosis of ADHD, symptoms of hyperactivity-impulsivity and/or inattention should meet the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders – 5th Edition (DSM-5TM) for ADHD and the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) for HKD.1 Note that in 2018, the ICD-10 was updated to the International Classification of Diseases 11th Revision (ICD-11), where HKD is now referred to as ADHD.6
Diagnosis of ADHD should also be based upon a full clinical and psychosocial assessment, a full developmental and psychiatric history, and observer reports of the individual’s mental state. According to the NICE guidelines, for a diagnosis of ADHD, symptoms of hyperactivity-impulsivity and/or inattention should meet the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders – 5th Edition (DSM-5TM) for ADHD and the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) for HKD.1 Note that in 2018, the ICD-10 was updated to the International Classification of Diseases 11th Revision (ICD-11), where HKD is now referred to as ADHD.6
Regardless of which medical classification system is used, the features of ADHD described are similar, with both sets of diagnostic criteria describing ADHD as a pattern of inattention and/or hyperactivity-impulsivity (combined, predominantly inattentive or predominantly hyperactive-impulsive presentations). 6,7 Nevertheless, these medical classification systems should be used in conjunction with a range of rating scales, which often measure the impact of ADHD upon more specific areas of functioning or quality of life.1-4
6,7 Nevertheless, these medical classification systems should be used in conjunction with a range of rating scales, which often measure the impact of ADHD upon more specific areas of functioning or quality of life.1-4
How do the two classification systems define ADHD?
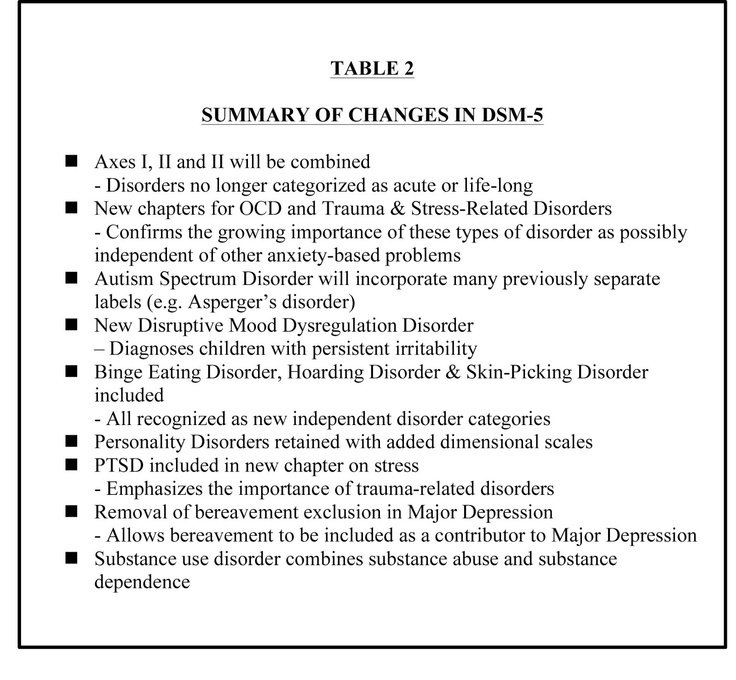
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders – 5th Edition (DSM-5
TM)The DSM-5TM medical classification system for ADHD is published by the American Psychiatric Association, and is used in the US and the rest of the world. This classification system defines ADHD as “a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development”.7 The DSM-5TM includes ADHD among neurodevelopmental disorders, which comprise conditions associated with factors affecting brain development, and gives examples of how ADHD symptoms are expressed across the lifespan.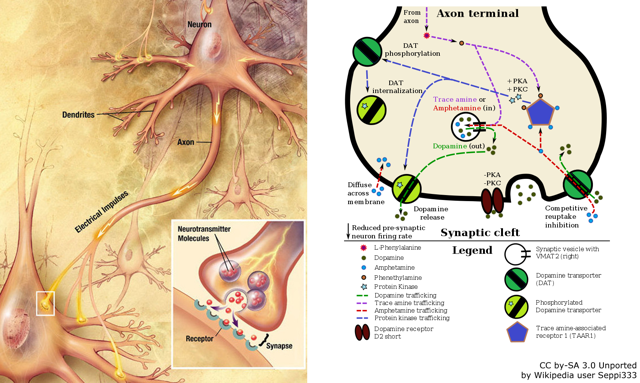 The DSM-5TM states that at least five symptoms must be present prior to age 12 years, and that there should be clear evidence that symptoms interfere with or reduce the level of social, academic and occupational functioning for a diagnosis of ADHD.5
The DSM-5TM states that at least five symptoms must be present prior to age 12 years, and that there should be clear evidence that symptoms interfere with or reduce the level of social, academic and occupational functioning for a diagnosis of ADHD.5
The DSM-5TM replaced the previous version (DSM-IV) in 2013.7,8 The NICE guidelines1 and other clinical guidelines2-5 refer to the DSM-5TM; however, some clinical trials initiated before the new edition also refer to the DSM-IV.
International Classification of Diseases 11th Revision (ICD-11)
Published in 2018, the ICD-11 characterises ADHD as a “persistent pattern (at least 6 months) of inattention and/or hyperactivity-impulsivity that has a direct negative impact on academic, occupational or social functioning.”6
The ICD-11 further states that the onset of these symptoms occurs prior to age 12 years, typically by early- to mid-childhood.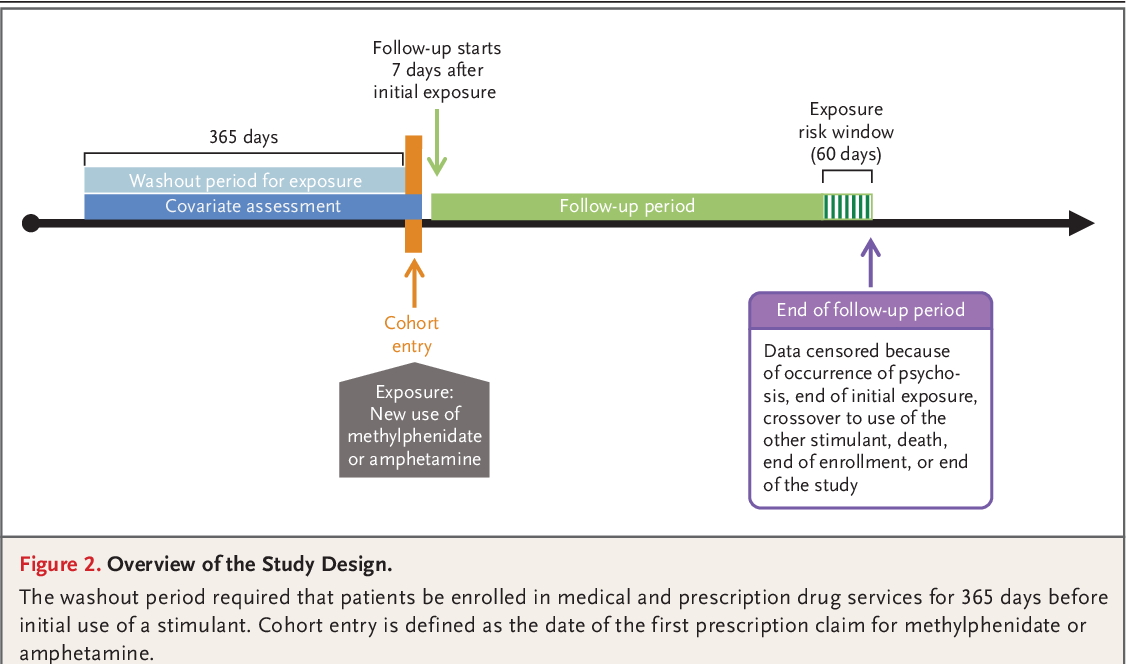 The degree of inattention and hyperactivity-impulsivity is also outside the limits of normal variation expected for age and level of intellectual functioning, and has a direct negative impact on academic, occupational or social functioning.6
The degree of inattention and hyperactivity-impulsivity is also outside the limits of normal variation expected for age and level of intellectual functioning, and has a direct negative impact on academic, occupational or social functioning.6
According to the ICD-11, ADHD can present as6:
- Predominantly inattentive
- Some hyperactive-impulsive symptoms may also be present, but these are not clinically significant in relation to the inattentive symptoms.
- Predominantly hyperactive-impulsive
- Some inattentive symptoms may also be present, but these are not clinically significant in relation to the hyperactive-impulsive symptoms.
- Combined
- Both inattentive and hyperactive-impulsive symptoms are clinically significant, with neither predominating in the clinical presentation.
The ICD-11 indicates that since the balance and specific manifestations of ADHD may vary across individuals, and may change over the course of development, the symptoms must be observable in more than one setting in order for a diagnosis of ADHD to be made. 6
6
- NICE guideline 2018. Attention deficit hyperactivity disorder: diagnosis and management. Available at: https://www.nice.org.uk/guidance/ng87. Accessed January 2021.
- Canadian ADHD Resource Alliance (CADDRA). Canadian ADHD Practice Guidelines. Edition 4.1. Toronto, ON: CADDRA, 2020.
- Banaschewski T, Hohmann S, Millenet S. Aufmerksamkeitsdefizit-/Hyperaktivitätsstörung (ADHS) im Kindes-, Jugend- und Erwachsenenalter. DGKJP, DGPPN and DGSPJ German guidelines. 2018.
- Guías de Práctica Clínica en el SNS. Grupo de trabajo de la Guía de Práctica Clínica sobre las Intervenciones Terapéuticas en el Trastorno por Déficit de Atención con Hiperactividad (TDAH). 2017.
- Kooij JJS, Bijlenga D, Salerno L, et al. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur Psychiatry 2019; 56: 14-34.
- World Health Organization. ICD-11: International Classification of Diseases 11th Revision. 2018. Available at: https://icd.
 who.int/. Accessed January 2021.
who.int/. Accessed January 2021. - American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. 2013.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association, 2004.
Date of preparation: March 2021; Job code: C-ANPROM/EUC/NBU/0003
The so-called attention deficit hyperactivity disorder is close to debunking
The increasingly widespread attention deficit hyperactivity disorder is close to debunking: German and American psychiatrists have presented further evidence that such a disorder simply does not exist, and children are being treated with psychotropic drugs in vain.
Two articles at once questioning the methods and results of diagnosing attention deficit hyperactivity disorder (ADHD) appeared in peer-reviewed scientific periodicals, confirming long-standing doubts of experts, pediatricians, insurers, parents and the media in both treatment methods and existence itself " fashionable syndrome.
The authors of the first article published in the Journal of Consulting and Clinical Psychology (impact factor 5.2) are German psychiatrists Prof. Sylvia Schneider and Jürgen Margraf from the Ruhr University Bochum and Dr. Kathrin Bruchmüller from the University of Basel.
Attention deficit hyperactivity disorder
(abbreviated ADHD; English Attention-Deficit / Hyperactivity Disorder (ADHD)) is a neurological-behavioral developmental disorder that begins in childhood. Manifested by symptoms such as difficulty concentrating...
Determined to find out to what extent clinicians in making a diagnosis of ADHD are guided by their intuition, and to what extent by clear scientific criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and the International Classification of Diseases (ICD-10), they proposed to a thousand children psychotherapists to make a diagnosis and recommend treatment based on a personal file sent to them by mail with a detailed description of the symptoms. Four variants of such a file were compiled. One fully met the ten criteria for diagnosing ADHD in children and adolescents. Three others contained ambiguous cases with descriptions of symptoms that only partially matched this list.
Four variants of such a file were compiled. One fully met the ten criteria for diagnosing ADHD in children and adolescents. Three others contained ambiguous cases with descriptions of symptoms that only partially matched this list.
Based on the responses received, it was found that in ambiguous cases, 16.7% of therapists diagnosed children with ADHD.
By itself, this figure only says that most doctors have exercised reasonable care in identifying ambiguous cases that only partially met the criteria for ADHD accepted by the scientific community. However, the very fact that some German doctors incorrectly diagnose a controversial mental disorder in children, interpreting it more broadly than even accepted in scientific psychiatry, still makes one wonder about the level of their own classification of about one in six child psychotherapists from Germany.
Much more wary was caused by something else.
Dopamine will defeat Parkinson's
Scientists from Italy and Russia have taken a decisive step in the fight against Parkinson's disease. Dopamine neurons -...
Dopamine neurons -...
July 13 09:38
Files of the same revision received by different doctors were deliberately signed with different names - either male or female. In the analysis, it turned out that in "ambiguous" cases, those same 16.7% of therapists were twice as likely to diagnose ADHD in boys than in girls. In other words, “Karl” had ADHD twice as often as “Clara,” even though the set of symptoms was exactly the same for the fictional children.
Researchers explain such an uneven distribution by banal gender stereotypes, according to which the classic symptoms of ADHD - hyperactivity, impulsivity and inability to concentrate - are more readily "hung" on boys due to the fact that male behavior is more strongly associated with more physical activity.
Because of this, boys, even if their symptoms do not fit the list of ADHD criteria, are twice as likely to be misdiagnosed and treated as girls with the same set of symptoms.
Moreover, even the gender of the doctor influences misdiagnosis: male therapists were more likely to misdiagnose boys than their female counterparts.
"Hyperactive children do not need to be treated with amphetamine"
About dopamine, the hormone of pleasure and drug addiction, about treating hyperactive children with amphetamines...
January 12 13:23
Evaluating these results, the authors come to the conclusion that the practiced methods of diagnosing hyperactivity disorder and attention deficit disorder are far from perfect and cause increased alertness, especially against the background of the fact that since 19From 89 to 2003, the number of children and adolescents diagnosed with ADHD increased by 381% in Germany, and the cost of their treatment with psychostimulants, such as methylphenidate, increased 9 times over the same time, while the daily dose of this drug, according to the German insurance company Techniker, increased by an average of 10%.
Another article that compromises not only the diagnosis, but the very existence of ADHD as a specific mental disorder, is published in the Proceedings of the National Academy of Sciences by American researchers - neurophysiologist Damien Fair and psychiatrist Joel Nigg.
In a series of experiments, the authors compared the cognitive abilities of two groups of adolescents - diagnosed with ADHD and control - in several parameters: the ability to comprehend and remember information, concentrate attention, separate information signals from noise, etc.
Adolescents with ADHD showed in general lower results compared to the control group,
but in some respects, some "sick" adolescents outperformed "healthy" ones, and the final picture of the distribution of results turned out to be too contradictory.
That is, adolescents who were diagnosed with one diagnosis actually suffered from various cognitive disorders, which are as wrong to reduce to any one ADHD as it is to measure the average temperature in a hospital.
"The prevalence of mental illness in Europe is 38.2%"
About the current state of psychiatry, about the number of patients in Russia and the world, about how ...
January 16 16:11
Both the Germans (more skeptical, like all European psychiatry, about ADHD than the Americans), and their overseas colleagues have not yet raised the issue of revising the two "sacred cows" of psychiatry and insurers - the Manual for the Diagnosis and Statistics of Mental Disorders and the International classifier of diseases - in terms of diagnostic criteria for an increasingly popular syndrome.
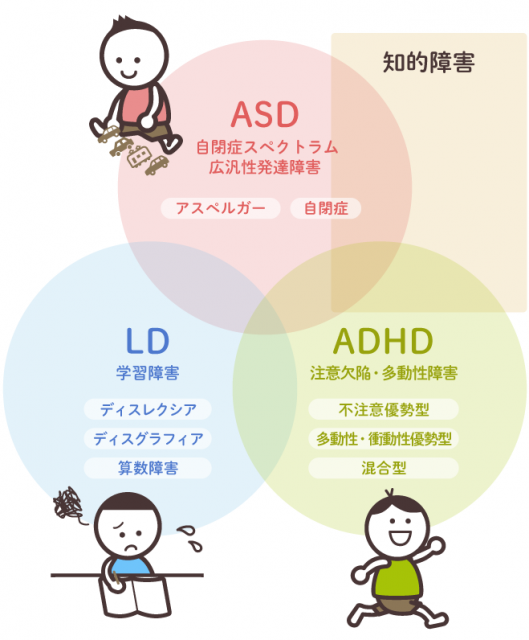
However, as both authors note, there are still surprisingly few statistical studies on this disease, although the number of diagnosed patients, as well as the cost of their treatment, is growing rapidly. Existing studies (including those described in two new articles) rather confirm the suspicions of skeptics that attention deficit hyperactivity disorder is the same fruit of medical fashion as, for example, the notorious "Asperger's syndrome", all the more dangerous because it is used to treat children. strong psychotropic drugs are actively used.
 He affects the emotional, behavioral and academic future of those suffering from it children.
He affects the emotional, behavioral and academic future of those suffering from it children. 
 Therefore, the importance of a clear diagnosis of accompanying disorders, due to their influence on the main symptoms, response on treatment, the course of the disease and prognosis for the future.
Therefore, the importance of a clear diagnosis of accompanying disorders, due to their influence on the main symptoms, response on treatment, the course of the disease and prognosis for the future.