History of the dsm
DSM: A History of Psychiatry’s Bible
The Diagnostic and Statistical Manual of the American Psychiatric Association has been called “the most important book of the twentieth century.” While this evaluation is debatable, the history of the DSM is certainly one of the most interesting stories in recent times. When its first edition appeared in 1952, the manual was a slight, spiral-bound pamphlet that required just 32 pages to define all of its 106 diagnosis. The most recent edition, the DSM-5, was published in 2013; it is a massive 947-page tome that defines about 300 conditions in precise detail. The imposing nature of the extant DSM-5, however, disguises the intense uncertainty, factionalism, hostility, and political wrangling that has accompanied the development of each DSM since its third edition in 1980.
By 1980, the cultural and institutional matrix of psychiatry had transformed from its post-World War II immersion in psychoanalytic theory, highly generalized concepts such as neuroses and psychoses, and psychoactive drugs that were targeted at a wide range of conditions. Psychiatry faced a host of interests that scorned the nebulous extant DSM diagnoses: third-party insurers demanded specific diagnoses before they would reimburse clinical treatment; the National Institute of Mental Health had turned from its initial social focus toward more traditional medical conceptions; the Food and Drug Administration mandated drug companies to demonstrate that their products targeted specific disease conditions; medical schools had come to require their disciplines adhere to commonly accepted scientific procedures rather than theoretical speculations. The existing DSM was a serious handicap in an environment that had changed from one that had no use for any but the most general conditions to one that required specific diagnostic entities.
The DSM-III marked the key change of psychiatric diagnoses from theoretically-infused to seemingly scientific and precisely defined mental disorders. Research psychiatrists, led by Robert Spitzer, developed descriptive criteria and decision rules to specify who should or should not receive each diagnosis.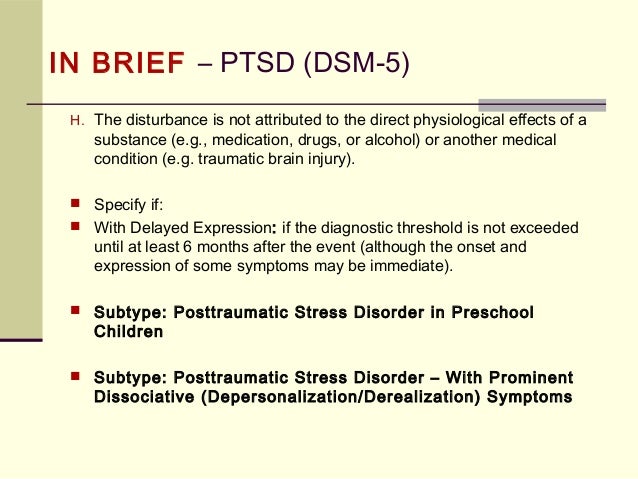 Its publication was hailed as a revolutionary development that transformed psychiatry from believing that something was true because Freud said so to deriving from evidence-based facts. For two decades the DSM-III conditions led the field to believe that is was on the verge of uncovering the biological basis that presumably underlay its diagnostic entities. Although clinicians initially resisted the manual’s exorcising of analytic concepts, they soon realized that the manual’s scientific-seeming diagnoses could garner reimbursement from third-party insurers as well as medical prestige.
Its publication was hailed as a revolutionary development that transformed psychiatry from believing that something was true because Freud said so to deriving from evidence-based facts. For two decades the DSM-III conditions led the field to believe that is was on the verge of uncovering the biological basis that presumably underlay its diagnostic entities. Although clinicians initially resisted the manual’s exorcising of analytic concepts, they soon realized that the manual’s scientific-seeming diagnoses could garner reimbursement from third-party insurers as well as medical prestige.
The DSM quickly became the basis for the acceptable scope of thinking about mental disorders among researchers and clinicians alike. It was institutionalized among all mental health professions, government bureaucrats, hospital administrators, mental health educators, advocacy groups, pharmaceutical companies, the insurance industry, and the judicial system. Patients, too, acquired a new language to interpret their distressing conditions and explain their emotional lives. Specific diagnoses became foundational for mental health practice, research, and theory.
Specific diagnoses became foundational for mental health practice, research, and theory.
Toward the end of the twentieth century, a startling reversal came in the evaluation of the DSM’s diagnostic criteria. The same group of researchers who imposed the manual’s categorical entities on initially resistant clinicians became their most ardent critics. They had come to realize that the nature of mental disorder was more dimensional than categorical, generalized than specific, and overlapping than discrete. The DSM-III revolution was proving to be an obstacle to realizing understandings from neuroscientific studies.
The latest revision that resulted in the DSM-5 in 2013 featured political dynamics that were the diametric opposite of those that created the DSM-III revolution. Researchers strove to replace the manual’s categorical diagnoses with dimensional continua that viewed mental illnesses as gradients ranging from mild to moderate to severe. They were opposed by clinicians who had come to depend on the DSM entities for compensation, were unfamiliar with dimensional notions, and rejected the complicated system researchers wanted to impose.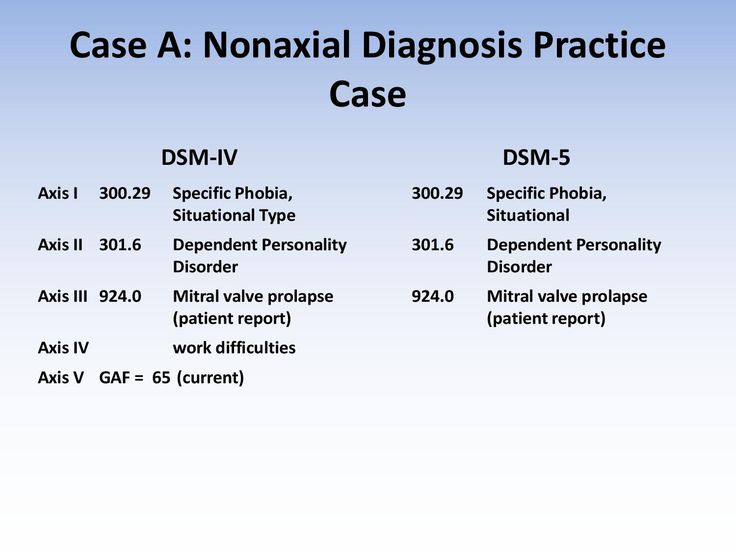 In addition, by the twenty-first century the value connotations of most psychiatric diagnoses had radically changed from stigmatizing labels imposed on resistant and often involuntary patients to valued resources that brought treatment, services, and, often, monetary compensation to patients and their families. Indeed, patient and family advocacy groups had become some of the most fervent defenders of the DSM categorical diagnoses.
In addition, by the twenty-first century the value connotations of most psychiatric diagnoses had radically changed from stigmatizing labels imposed on resistant and often involuntary patients to valued resources that brought treatment, services, and, often, monetary compensation to patients and their families. Indeed, patient and family advocacy groups had become some of the most fervent defenders of the DSM categorical diagnoses.
The bitter controversies that marked the DSM’s latest revision sunk the credibility of the manual to levels not seen since the anti-psychiatric climate that marked the 1960s and 1970s. The new critics of the DSM-5 were not the anti-psychiatrists, feminists, and gay advocates who objected to earlier versions but eminent figures within the profession including former NIMH directors and the leaders of the DSM-5 Task Force itself. Ironically, the major guardians of the classification were clinicians who were initially the manual’s harshest critics. The future of the DSM is clearly at a crossroads, but the path it should take has no roadmap.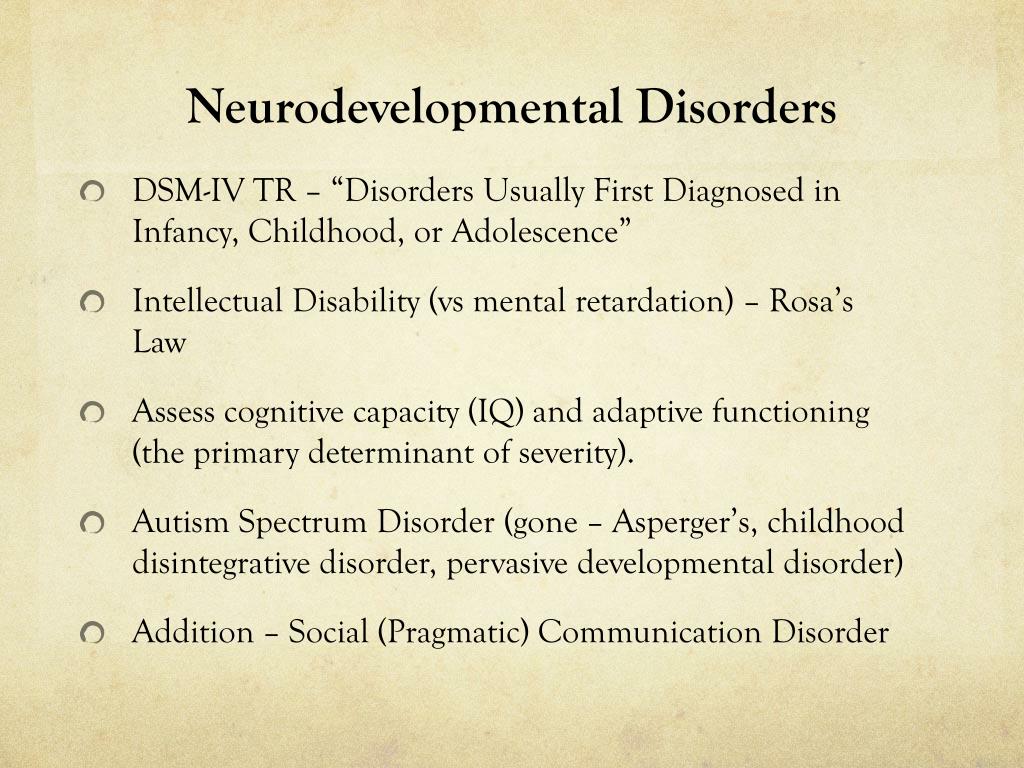
Order DSM: A History of Psychiatry’s Bible at the following link: https://jhupbooks.press.jhu.edu/title/dsm
Allan V. Horwitz is a Board of Governors Distinguished Professor of Sociology Emeritus at Rutgers University. He is the author or coauthor of eleven books, including DSM: A History of Psychiatry’s Bible, Anxiety: A Short History, PTSD: A Short History, and Creating Mental Illness.
History of the Diagnostic and Statistical Manual of Mental Disorders
This article reviews the history of the DSM from its early conception to its present day use.
The information provided in this article is taken from the book The DSM-5 in Perspective: Philosophical Reflections on the Psychiatric Babel and from the journal articles:
- A brief historicity of the Diagnostic and Statistical Manual of Mental Disorders: Issues and implications for the future of psychiatric canon and practice
- A review of American psychiatry through its diagnoses: the history and development of the Diagnostic and Statistical Manual of Mental Disorders
- Adopting a continuous improvement model for future DSM revisions
Early Conceptualizations of the DSM
In the 1800s, there was a movement to find successful treatments for individuals who had been filling up mental hospitals in America, Britain, and Continental Europe.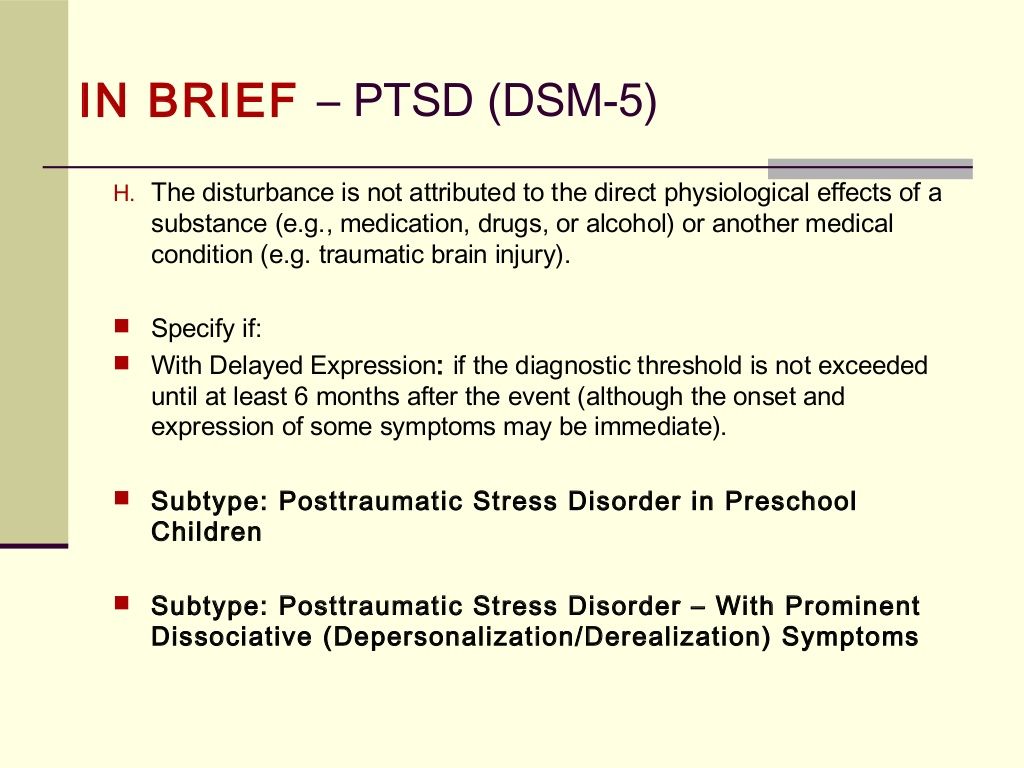 The treatment in these hospitals focused on the use of “moral treatment” as opposed to the harsher methods used in medieval asylums.
The treatment in these hospitals focused on the use of “moral treatment” as opposed to the harsher methods used in medieval asylums.
The need to determine more successful modes of treatment for individuals with mental health disorders led to the need to also classify these disorders. The first recognized attempt to classify mental health disorders came from the French psychiatrist Jean-Etienne-Dominique Esquirol and was titled Concerning Mental Illnesses.
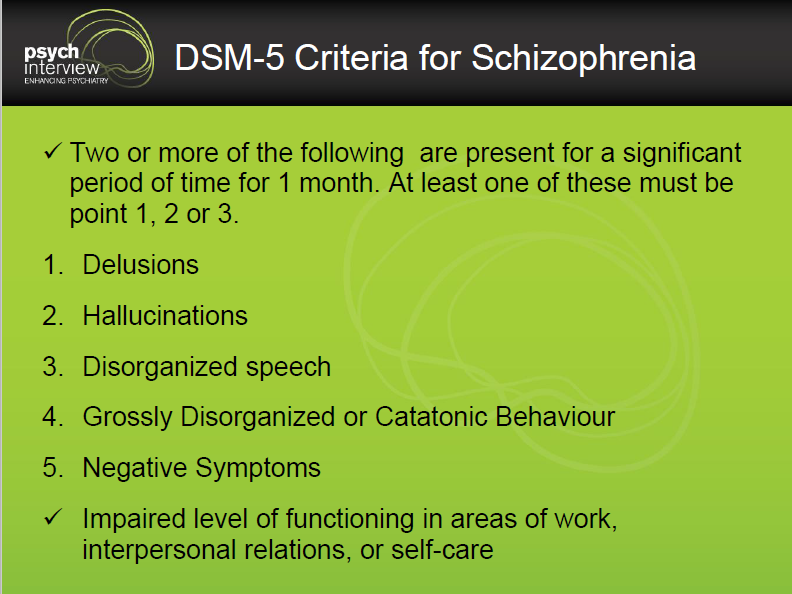
Some years later, German psychiatrist Emil Kraepelin developed his classification of mental illness, Compendium der Psychiatrie. Kraepelin distinguished two major forms of mental illness: dementia praecox (which would later be classified as schizophrenia) and manic-depressive disorder (which later would form the basis for clinical depression and bipolar disorder). Kraepelin also documented three different presentations of dementia praecox that included:
- Paranoia, which primarily consisted of hallucinations and delusions
- Hebephrenia, which mainly presented with inappropriate behaviors and inappropriate types of reactions
- Catatonia, which presented as posturing, odd mannerisms, or extreme agitation
Kraepelin’s classification system would later become the basis for the modern Diagnostic and Statistical Manual of Mental Disorders series (DSM).
Bringing the DSM to America
In 1840, the term idiocy/insanity was used to describe certain individuals in the census. The government decided that it needed to collect data on the prevalence of mental illness. As time went on, the idiocy/insanity category grew to seven categories that included melancholia, paresis, mania, monomania, dipsomania, dementia, and epilepsy. The expanded categories resulted in confusion regarding mental illness diagnoses and led to issues with uncertainty attempting to formally identify these diagnostic categories.
In 1917, the Statistical Manual for the Use of Institutions for the Insane was created by the Committee on Statistics of the American Medico-Psychological Association (which later became the American Psychiatric Association [APA]) and another organization, the National Commission on Mental Hygiene. These two committees separated forms of mental illness into 22 different groups, and this information was used by the Bureau of Census.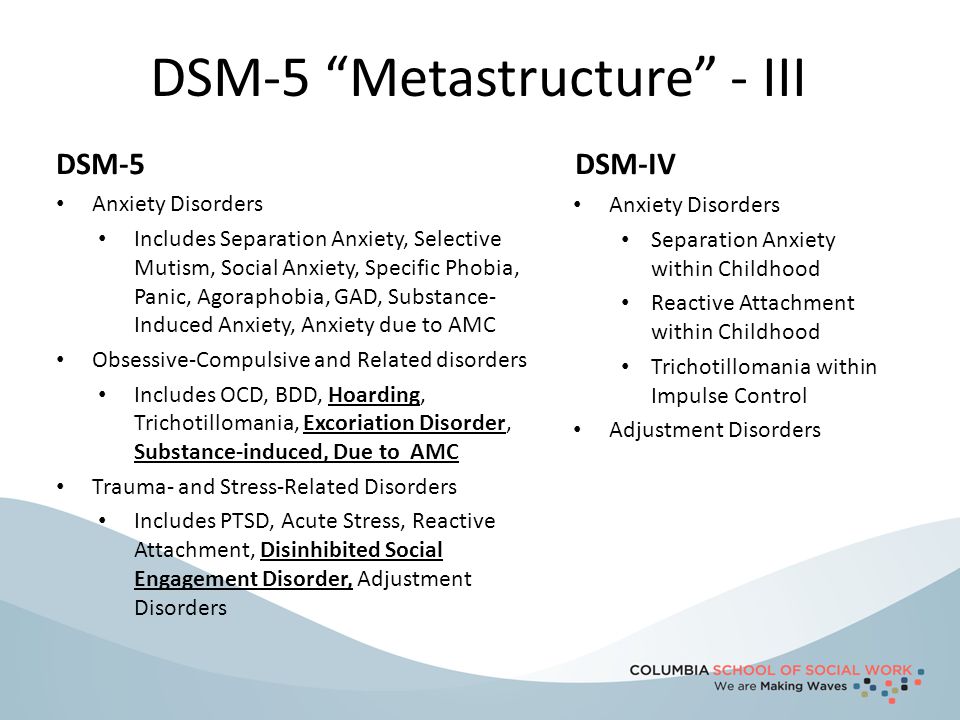
The publication continued to be revised and went through 10 editions up until 1942. This manual is considered to be the predecessor to the first edition of the DSM. It contained very broad categorizations of mental disorders and had very limited use in diagnosing them. In addition, the Freudian model was predominant in psychiatry during this period, and diagnoses represented this influence.
DSM-1
The confusion regarding what to diagnose was enhanced by a number of other different diagnostic systems that were present in the US. There was a real need to develop a classification system that minimized this situation and resulted in agreement in the area of psychiatry as well as the provision of a common diagnostic scheme that could be used nationwide. The APA decided to create a new classification system, and in 1952, the first edition of the DSM (DSM-1) was released.
The DSM-1 contained 102 very broad diagnostic categories that were based on psychodynamic (Freudian) principles. The diagnostic categories were divided into two major groups of mental disorders that included:
The diagnostic categories were divided into two major groups of mental disorders that included:
- Conditions that were assumed to be caused by some type of brain dysfunction.
- Conditions that were assumed to be the result of the effects of environmental stress in a person and resulted in an inability to adapt.
The second group was subdivided into (1) psychoses: severe conditions, such as schizophrenia and manic depressive disorder, and (2) psychoneuroses, which included personality disorders, depression, and anxiety related conditions.
Despite the development of an organized classification system with diagnostic categories, the manual had very little diagnostic utility and exhibited little influence on the diagnostic process. This set the stage for the development of a second edition of the DSM.
DSM-2
In an effort to compensate for the deficiencies of the DSM-1, a second edition of the DSM was published in 1968.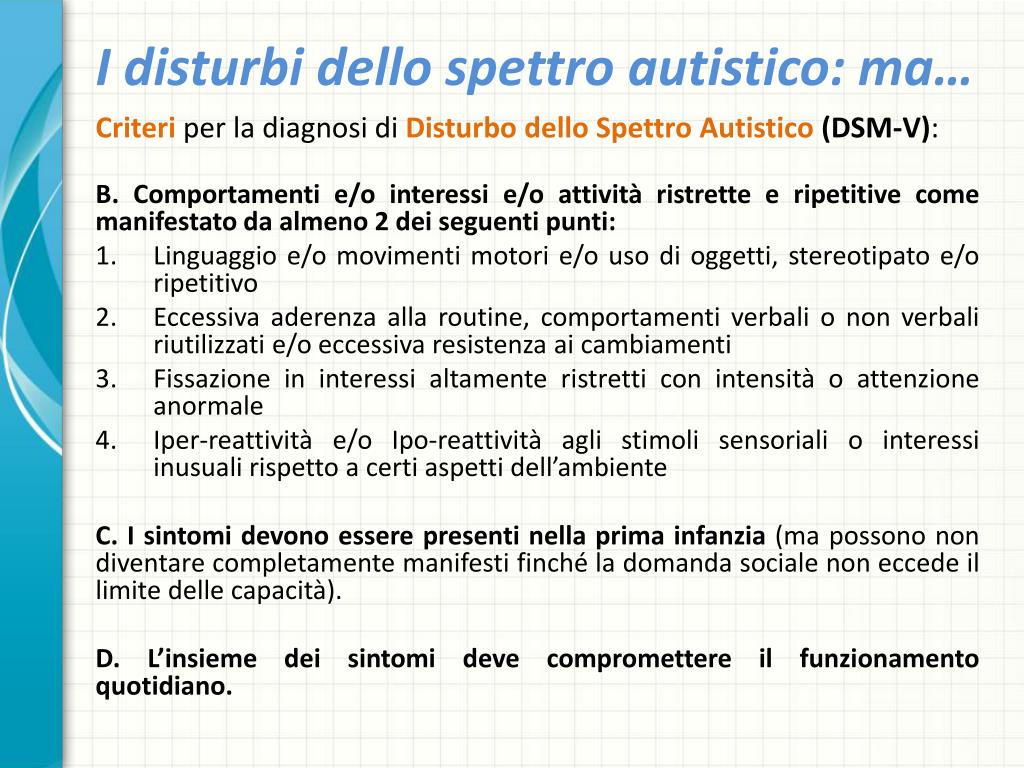 The DSM-2 was still heavily influenced by Freudian principles even though these principles were losing popularity during this time. DSM-2 had two major modifications.
The DSM-2 was still heavily influenced by Freudian principles even though these principles were losing popularity during this time. DSM-2 had two major modifications.
- There was an expansion of the definition of mental illness that took into account milder conditions that occurred in the general population. Some of these conditions appear to be obvious attempts to broaden the client base of psychiatry, such as conditions without manifest psychiatric disorder (normal individuals who nevertheless need to be examined by a psychiatrist). While the inclusion of some of these categories was designed to account for reactions to environmental stresses, it also produced quite a bit of confusion.
- There was also an increased categorization that resulted in multiple subdivisions of existing categories. For example, there was an addition of eight different “alcoholic brain syndromes” and an increased number of qualifiers for diagnoses. The DSM-1 contained four qualifiers for a diagnosis, whereas the DSM-2 contained nine qualifiers for many of the diagnoses.
The number of diagnostic categories was increased to 182, and the descriptions were still not useful in developing a formal diagnosis. They required subjective interpretations of prose-like descriptions of behaviors.
DSM-3
A number of critics had surfaced during the 1960s and 1970s. Many of these, such as psychiatrist Thomas Szasz, brought up serious challenges to the fundamental principle of the DSM that psychiatric conditions were actually real illnesses. In addition, the total lack of clear boundaries between mental health, normal behavior, and illness, and the low reliability of the psychiatric categories in the DSM-2, was criticized almost universally.
The National Institute of Mental Health (NIMH) withdrew research support and insurance providers demonstrated a lack of confidence in the diagnostic scheme. Competition from nonmedical mental health treatment providers also made the conditions for psychiatrists rather tenuous. In addition, the development of more biologically oriented schools of thought and psychiatry, the development of quantitative assessment tools such as rating scales, and the need to decrease the overall treatment time of individuals also led to the need for a new classification system.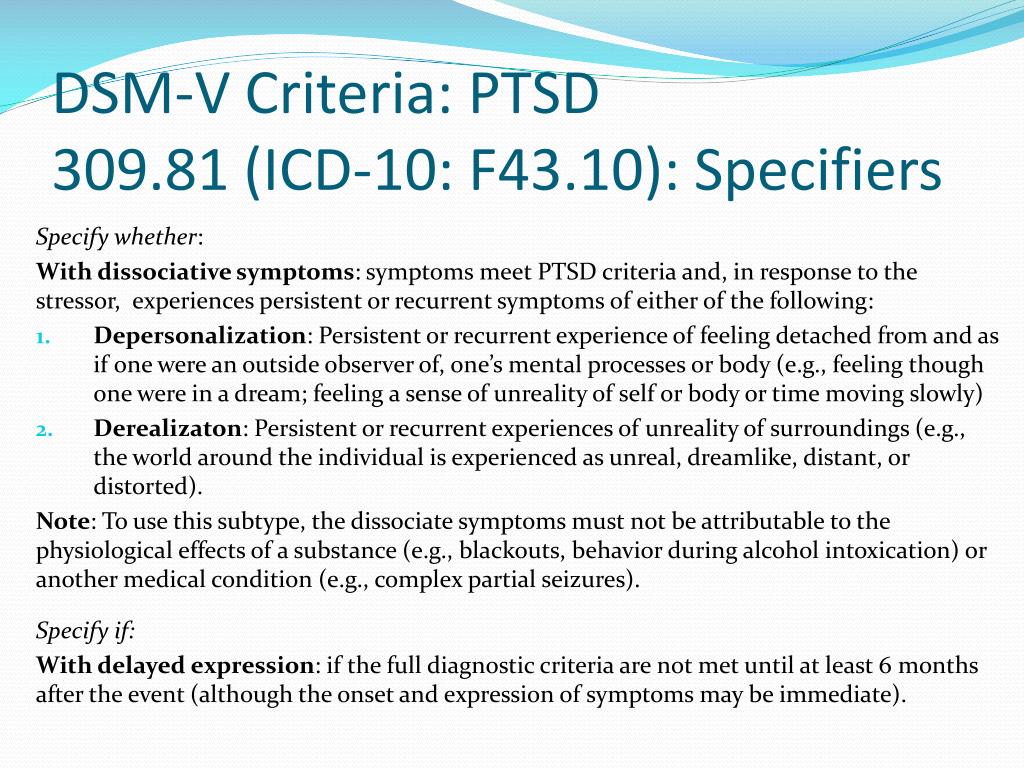
The DSM-3 was released in 1980. The number of diagnostic categories increased to 265, and the removal of many psychiatric terms used in earlier editions was replaced by more biologically based terminology. Several disorders were divided into a number of distinct categories (e.g., the old “feeding disturbance” category was replaced by four types of “eating disorders”). A number of diagnoses that contained labels that were obviously Freudian in nature were also renamed; the most common change was using the term disorder in place of the former term neurosis.
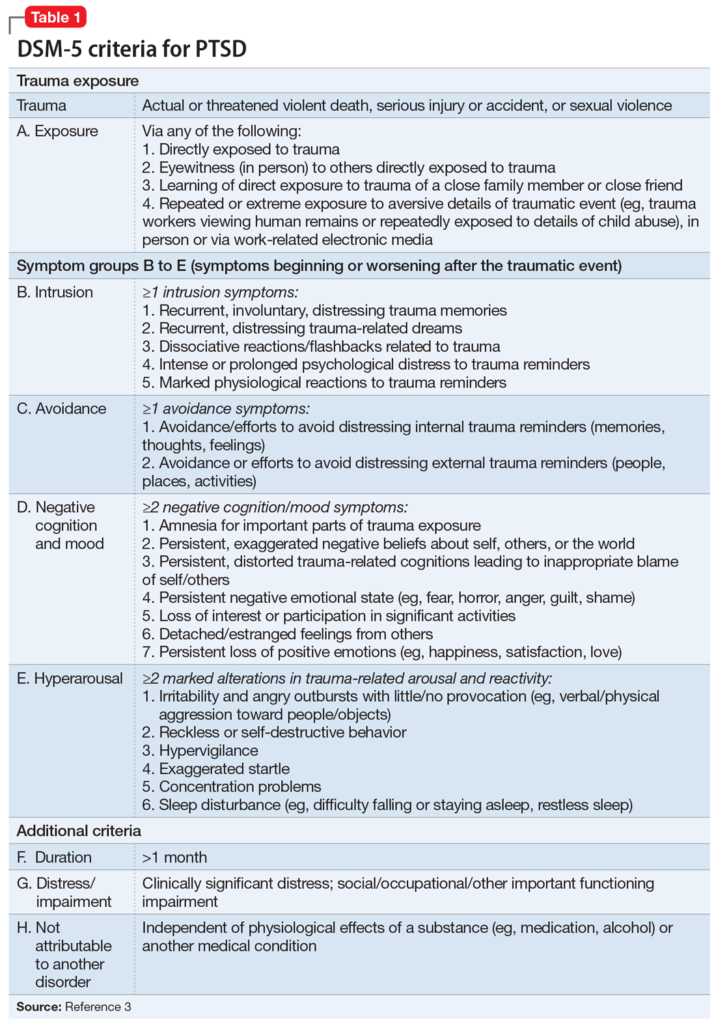
Many novel disorders were also included in this edition, including post-traumatic stress disorder, attention deficit disorder, etc. In addition, homosexuality as a disorder was deleted in the DSM-3; it had actually been removed in the seventh printing of the DSM-2 that occurred in 1974, but this edition was the first new one to exclude homosexuality as a category of mental illness.
However, the notion of ego-dystonic homosexuality remained in the manual (defined as individuals who are homosexual and suffer emotional distress because of their sexual orientation). Several other modifications designed to depict the diagnostic categories as mutually exclusive illnesses were also made.
Several other modifications designed to depict the diagnostic categories as mutually exclusive illnesses were also made.
The DSM-3 is considered by many to be the benchmark in the change of focus of the diagnostic system of psychiatry. These changes included a move toward more biologically oriented views of mental illness consistent with a medical approach to diagnoses and a shunning of the Freudian principles that had been predominant in psychiatry up to this point. The subsequent editions of the DSM revisions continue the tradition set by the DSM-3.
DSM-3-R
In 1987, the APA published a revised edition of the DSM-3 that renamed and reorganized certain categories and made changes in the diagnostic criteria of others. The DSM-3-R contained 292 diagnostic categories and removed a number of controversial diagnoses including ego-dystonic homosexuality. Interestingly, this manual was significantly longer than other manuals (567 pages).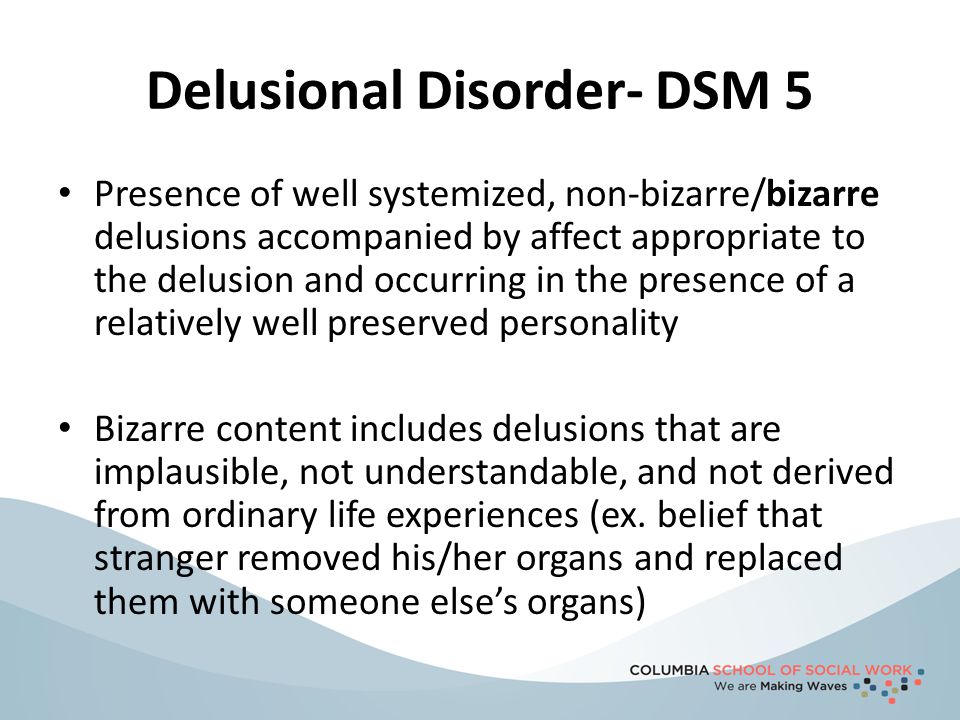
Efforts to make the diagnostic categories purely descriptive, list specific symptoms as opposed to using prose descriptions, and concentrate on the reliability of the diagnoses were continued. A major issue with former editions of the DSM was the reliability of the diagnostic categories. This refers to the ability of different clinicians in different areas giving the same person the same psychiatric diagnosis as a result of using the DSM.
The concentration on diagnostic reliability began with the DSM-3, and it continued in the DSM-3-R. Prior to these editions, it was not uncommon for two different psychiatrists assessing the same individual to give totally different diagnoses. This was a major criticism of earlier editions of the DSM.
DSM-4
By the 1990s, the pattern of the development of the diagnostic categories and their diagnostic criteria had been established. The revision in 1994, the DSM-4 was published, listing 297 different disorders over 886 pages.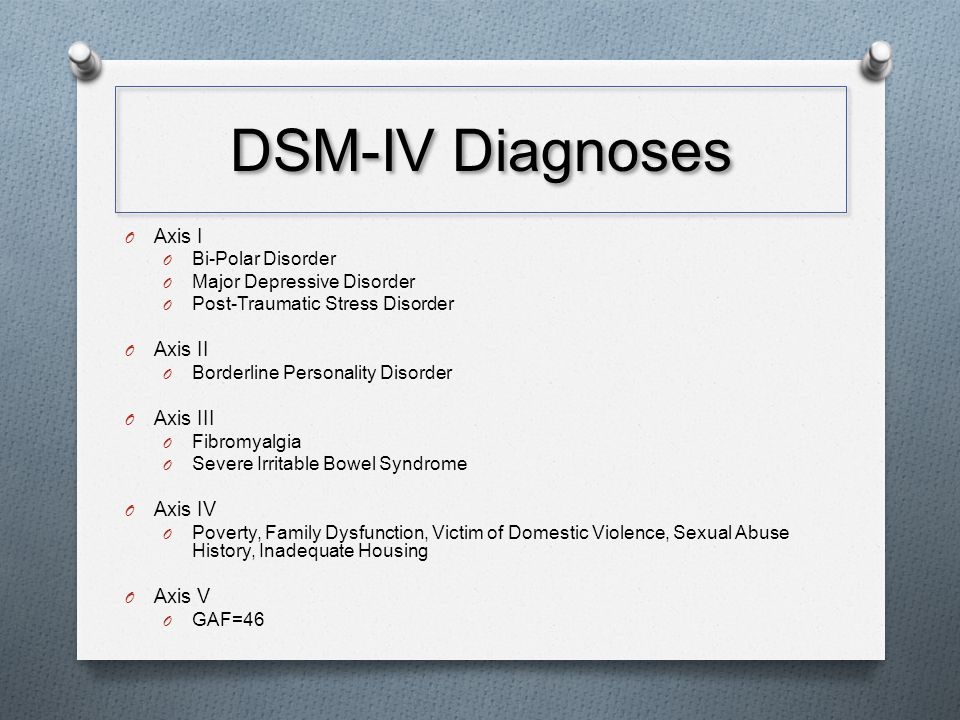 The other major change from the DSM-3-R was the addition of the descriptive diagnostic term clinical significance. This criterion indicated that the symptoms displayed by the person must result in “clinically significant distress or impairment in social, occupational, or other important areas of functioning” in order for them to receive a specific diagnosis. Other minor changes and diagnoses were deleted or removed.
The other major change from the DSM-3-R was the addition of the descriptive diagnostic term clinical significance. This criterion indicated that the symptoms displayed by the person must result in “clinically significant distress or impairment in social, occupational, or other important areas of functioning” in order for them to receive a specific diagnosis. Other minor changes and diagnoses were deleted or removed.
DSM-4-TR
In 2000, the DSM-4-TR was published. The diagnostic categories in this revision remained essentially the same, and the text sections describing certain aspects of the diagnostic criteria were updated and revised. In addition, the manual used a five-part axial diagnostic system that incorporated several different dimensions of diagnoses, including:
- Axis I: the clinical syndromes
- Axis II: personality and developmental disorders (mental retardation)
- Axis III: general medical conditions
- Axis IV: psychosocial and environmental issues
- Axis V: global assessment of functioning (rated on a scale of 0-100)
DSM-5
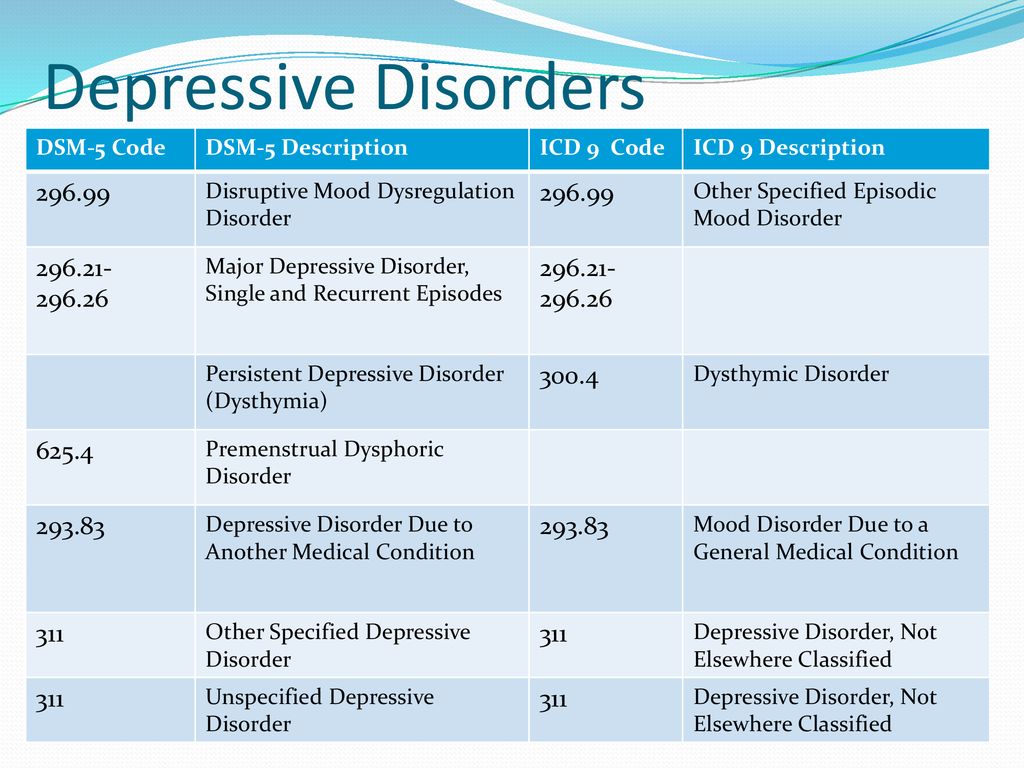
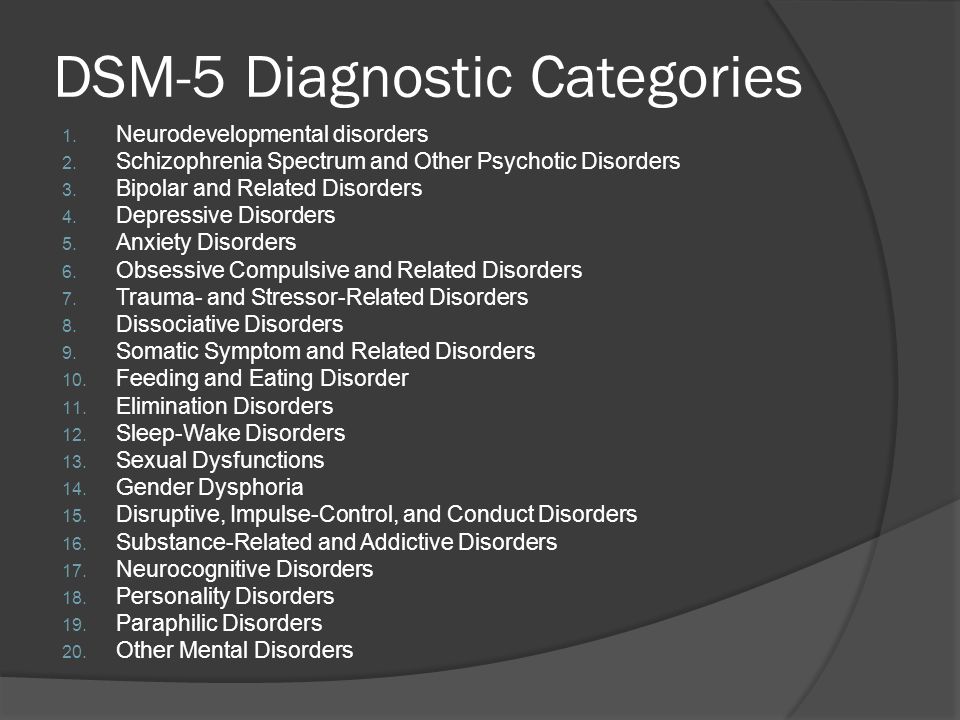
In 2013, the DSM-5 was released, which had a number of significant changes. For example:
For example:
- A number of disorders were deleted (e.g., subsets of autism spectrum disorder, such as Asperger’s syndrome, classic autism, Rett syndrome, etc., in favor of one overall diagnosis).
- The traditional five subtypes of schizophrenia were deleted.
- Schizophrenia was conceptualized as a singular disorder.
- Other disorders were given their own category (e.g., post traumatic stress disorder) or changed significantly (e.g., somatization disorder).
A number of these changes were very controversial, such as the designation of a bereavement disorder.
The use of the axial diagnostic system in the DSM-4-TR was also dropped. The long-awaited revision stirred quite a bit of controversy, and a number of organizations, including the National Institute of Mental Health, vowed to begin research to develop their own diagnostic system for mental illnesses.
General Issues and Problems with the DSM
Entire books have been written critiquing the DSM series. Descriptions of some of the major critiques follow.
Descriptions of some of the major critiques follow.
- The process of determining a specific diagnosis, selecting diagnostic criteria, and evaluating the information is performed by a committee as opposed to using actual medical evidence or tests. For example, nearly all of the diagnostic criteria in all of the DSM editions are behavioral observations and not formal biological or medical test results. Despite numerous attempts to make these diagnostic criteria objective, they are descriptions that are entirely subjective and require a lot of interpretation from the clinician. The National Institute of Mental Health has proposed research to develop specific biological markers or biological tests to identify mental health disorders.
- The composition of the committees in the past was suspect, although in the current edition, this may not be as big of an issue. Many of the committee members contributing to the diagnostic categories and past editions had significant ties to the pharmacological industry.
 This was a major criticism of previous editions of the DSM, but is not as salient a criticism of the DSM-5.
This was a major criticism of previous editions of the DSM, but is not as salient a criticism of the DSM-5. - The concentration on reliability is problematic. First of all, the actual reliability of the DSM diagnostic categories is relatively poor even though the committee focused on the reliability of the categories. Secondly, the concentration on reliability does not guarantee that the diagnostic categories are valid. Validity refers to the truthfulness of some issue. There are many critiques regarding the actual validity of many of the diagnostic categories in the DSM
- The DSM pathologizes many normal behaviors. This is a critique that has been ongoing since the inception of the series. For example, in the DSM-5, quite a bit of controversy was generated by the notion of a bereavement disorder. Many individuals believe that classifying bereavement as a potential mental illness was inappropriate.
- The choice of how many diagnostic criteria should be used to satisfy the actual diagnosis appears to be relatively arbitrary.
 Some diagnoses required four diagnostic criteria, some five, some two, etc. Critics ponder if the difference between having three diagnostic criteria compared to four diagnostic criteria is actually based on any meaningful assumptions.
Some diagnoses required four diagnostic criteria, some five, some two, etc. Critics ponder if the difference between having three diagnostic criteria compared to four diagnostic criteria is actually based on any meaningful assumptions. - Individuals who receive the same diagnosis may have totally different presentations. Because only a certain number of diagnostic criteria need to be satisfied in order to receive a diagnosis (e.g., four of nine total diagnostic criteria), there are a number of different scenarios where individuals receiving the exact same diagnostic label have clearly different presentations. This makes no conceptual sense.
- Finally, the designation of mental disorders into mutually exclusive categories is not consistent with the understanding of human behavior. As it turns out, the so-called mutually exclusive diagnostic categories in the DSM series are not mutually exclusive, and other more functional approaches for certain diagnostic categories, such as personality disorders, have been suggested but have not been implemented by the committees.
 The conceptualization of mental illness by the committees and the APA is often not consistent with much of the research in the field, even though the committees that form the diagnoses review this research and use it to develop their diagnostic criteria and categories. Attempting to classify mental disorders in the same way that physical diseases are classified may not be a valid approach.
The conceptualization of mental illness by the committees and the APA is often not consistent with much of the research in the field, even though the committees that form the diagnoses review this research and use it to develop their diagnostic criteria and categories. Attempting to classify mental disorders in the same way that physical diseases are classified may not be a valid approach.
How the DSM Is Used Today
Today, the DSM is used by clinicians to diagnose mental disorders consistently and reliably.1 This resource provides a common language and concise criteria that allows clinicians to objectively assess patient symptoms.
Additionally, the DSM is used as a tool and educational resource by students, researchers, and professionals involved in mental health care. It provides a structured method of understanding, communicating about, and diagnosing mental disorders.
Using the DSM in Addiction Treatment for Dual Diagnosis
The DSM is used to diagnose co-occurring disorders, or in other terms, a dual diagnosis.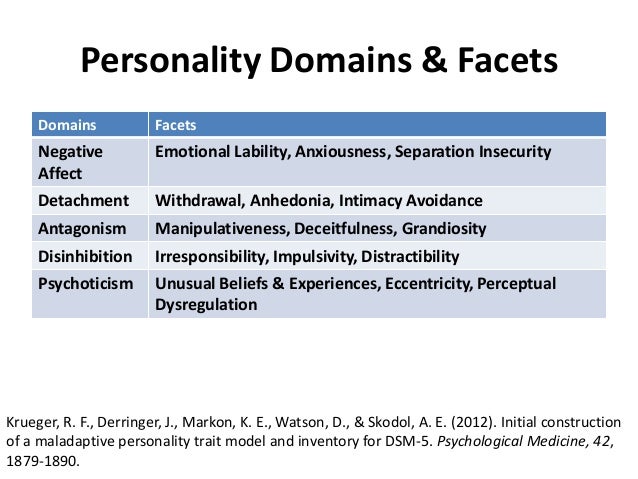 When a patient exhibits symptoms for both a mental health disorder and a substance use disorder, it is termed a co-occurring disorder.2 In those with substance use disorder, it is common to also have a mental health disorder.
When a patient exhibits symptoms for both a mental health disorder and a substance use disorder, it is termed a co-occurring disorder.2 In those with substance use disorder, it is common to also have a mental health disorder.
By recognizing both disorders, more effective treatment protocols can be enacted. Research shows that an integrated treatment approach that addresses both the substance use disorder and the mental health disorder is the most effective approach.3
DSM: From Diagnosis to Treatment
The DSM was developed as a diagnostic manual to classify different forms of mental illness and to provide objective diagnostic criteria used in identifying them in the field.
The DSM has undergone a number of different revisions, and for the most part, the DSM series remains highly criticized despite still being “the only game in town.”
Other organizations, such as the National Institute of Mental Health, have decided to attempt to develop their own diagnostic scheme for mental illness as a result of their dissatisfaction with the DSM; however, any new approach to diagnosing mental illness is most likely far off.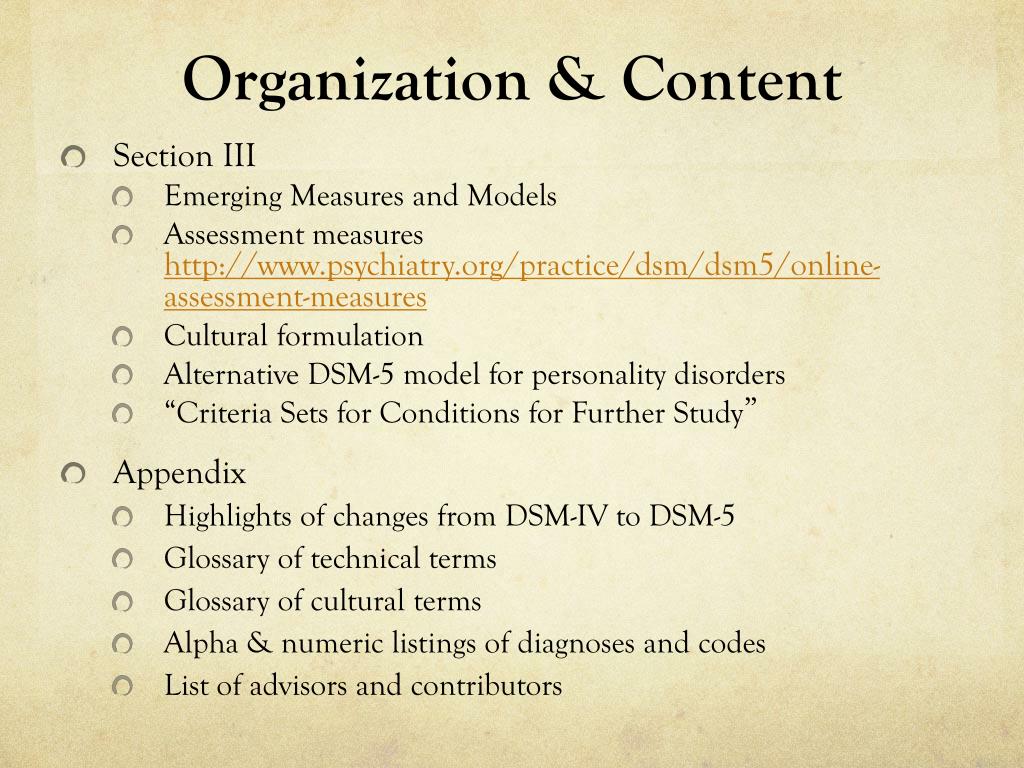 Mental health clinicians will continue to use the DSM-5 despite reservations or current concerns.
Mental health clinicians will continue to use the DSM-5 despite reservations or current concerns.
If you or someone you love is struggling with a co-occurring disorder, help is available at our substance abuse rehab in Las Vegas. Desert Hope Treatment Center offers specialized levels of addiction treatment for those with co-occurring substance use and mental health disorders.
Our premier Nevada rehab is in-network with many insurance providers, which makes paying for rehab with health insurance easy. online by completing our secure form. At Desert Hope, we also offer several other rehab payment options, including financing.
When you’re ready for recovery, we’re here for you. Call one of our admissions navigators to start the rehab admissions process today at .
History of the DSM - PsyAndNeuro.ru
In 1952 the American Psychiatric Association published the DSM-I. This "catalogue" of mental illness had a theoretical basis - the views of the authoritative psychiatrist Adolf Meyer.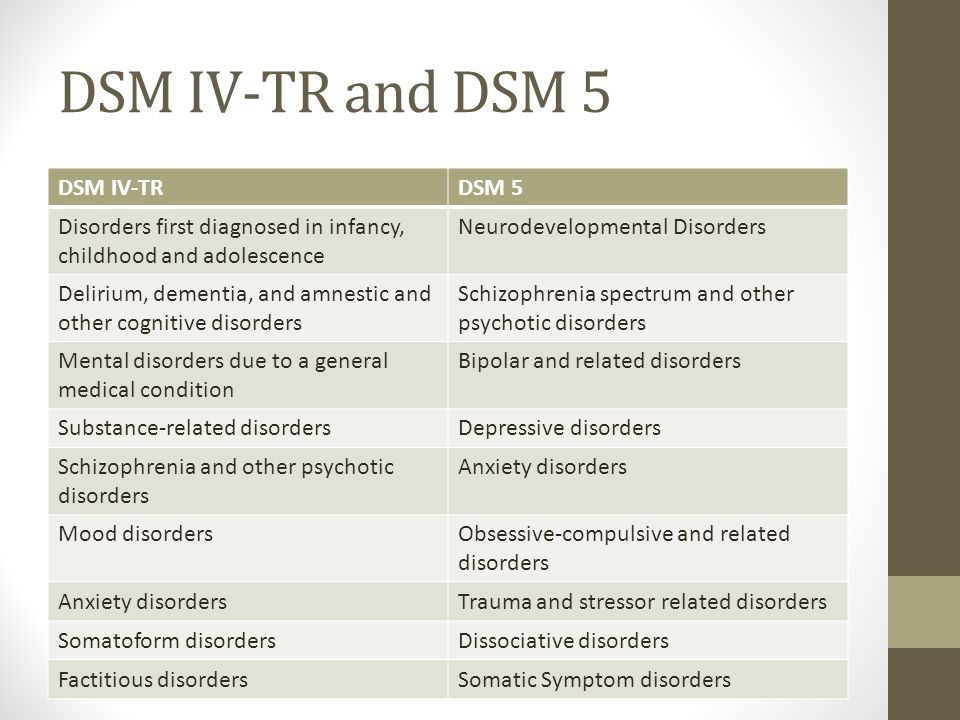 Meyer's main idea, which influenced the DSM-I, is associated with a certain point of view on symptoms, which are interpreted not as external manifestations of some disturbance in the biology of the organism, but as a complex reaction to life circumstances. The key word is reaction. The DSM-I has a section on “Disorders of psychogenic origin or without a physical cause or structural changes in the brain” which lists the following diagnoses:
Meyer's main idea, which influenced the DSM-I, is associated with a certain point of view on symptoms, which are interpreted not as external manifestations of some disturbance in the biology of the organism, but as a complex reaction to life circumstances. The key word is reaction. The DSM-I has a section on “Disorders of psychogenic origin or without a physical cause or structural changes in the brain” which lists the following diagnoses:
- affective reaction
- schizophrenic reaction
- psychophysiological cardiovascular response
In addition to Meyer, the DSM-I was influenced by psychoanalysis. Personally, Meyer distanced himself from Freud, but the Freudian influence is hard to miss. Take, for example, the diagnostic definition of “psychoneurotic disorder”—anxiety that is experienced or placed under automatic control of various kinds of defense systems such as depression, dissociation, phobia, obsessions, etc.
Biological psychiatry at the beginning.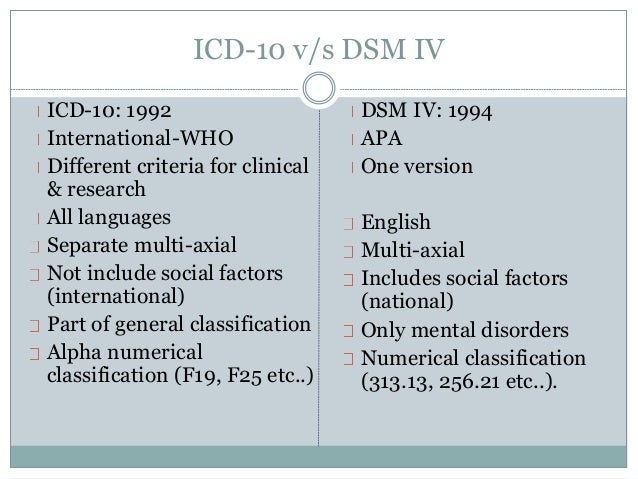 1950s in America has not yet acquired the influence that it will later receive. At that time, the psychodynamic direction dominated, which many modern psychiatrists, for sure, would reproach for excessive “psychologization” of diseases.
1950s in America has not yet acquired the influence that it will later receive. At that time, the psychodynamic direction dominated, which many modern psychiatrists, for sure, would reproach for excessive “psychologization” of diseases.
However, the DSM-I was not totally influenced by psychoanalysis. Firstly, its goal was to create an adequate diagnostic system for modern psychiatry and neurology (!). Secondly, Meyer's theory of man as a "psychobiological" unity, sometimes pathologically reacting to certain events, manifested itself in DSM-I in a limited way, practically only in one part. In other parts, we find descriptions of disorders caused by organic lesions of the brain, that is, completely biological causes. Thus, it was recognized that in psychiatry there are diseases that are not subject to psychodynamic interpretation, and should be considered as manifestations of brain dysfunction. nine0003
The DSM-II is said to be the successor to the DSM-I in terms of continuing the psychodynamic tradition.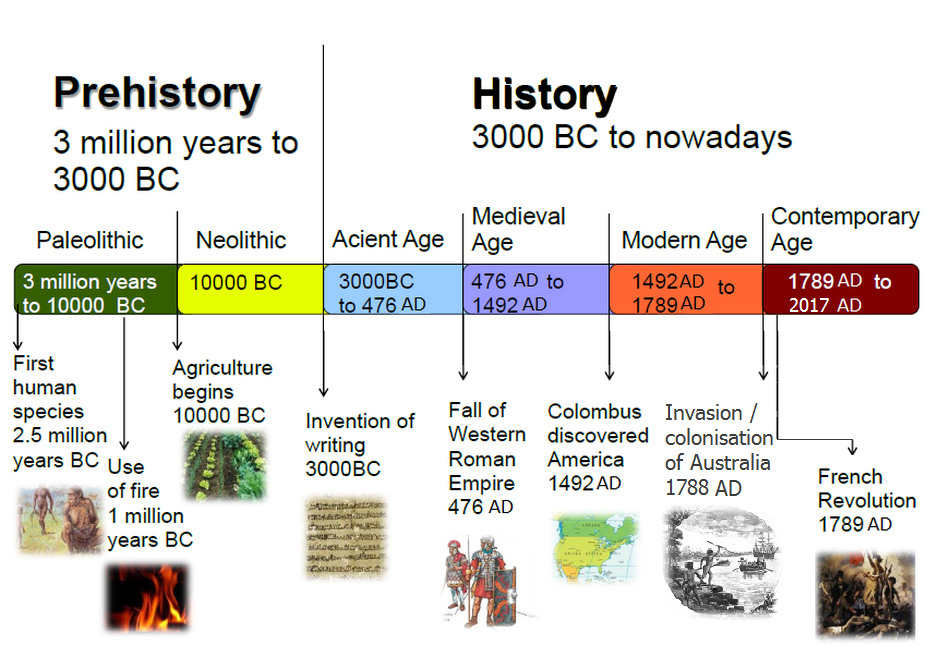 Indeed, the new edition of the classification still uses the controversial term “neurosis”. The meaning of this word, which came into use even before psychoanalysis, often changed and gradually became elusive for unambiguous understanding.
Indeed, the new edition of the classification still uses the controversial term “neurosis”. The meaning of this word, which came into use even before psychoanalysis, often changed and gradually became elusive for unambiguous understanding.
At the same time, the DSM-II takes a step away from the theoretical base, which was considered very important when compiling the DSM-I. DSM-II was consistent with ICD-8, and there was no bias towards psychodynamic theory in the international psychiatric systematization. The ICD at that time reflected the orientation of European psychiatrists, who, unlike their American counterparts, were rather skeptical of psychoanalysis. nine0003
DSM-III has been called a “revolution”, “turning point”, “diagnostic style shift”, “paradigm shift”, “the first scientific paradigm in psychiatric nosology”.
The drafters of the DSM-III wanted to create an “atheoretical” document, a guide for practitioners who do not have time to delve into discussions about the etiology of diseases.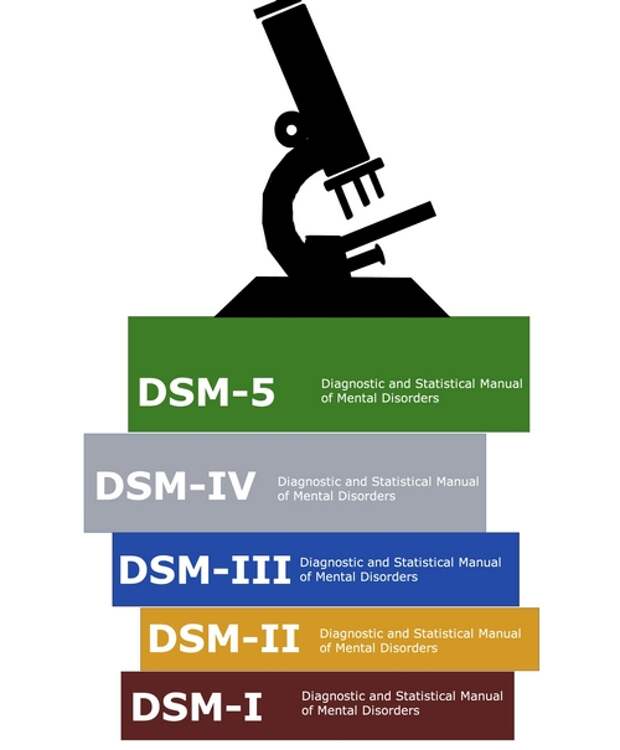 Therein lies the revolutionary nature of the DSM-III.
Therein lies the revolutionary nature of the DSM-III.
In American psychiatry, the departure from psychodynamic theory and the transition to a purely descriptive classification of diseases was officially recorded (the movement in this direction began in DSM-II). nine0049 The novelty of the DSM-III is associated with two fundamental methodological prerequisites.
1) Neo-positivist theory of classification.
It is extremely important to ensure that nothing "unscientific" penetrates into psychiatry as a medical discipline. The concept of neurosis may prove effective in the process of psychoanalysis, but it does not pass the test of being "scientific." Therefore, this concept must be excluded, as well as other meaningless, from the point of view of diagnostics, concepts. The psychiatrist must believe that the information he receives in the process of objective observation is sufficient for diagnosis. Of course, he is limited in his abilities as an observer and interpreter.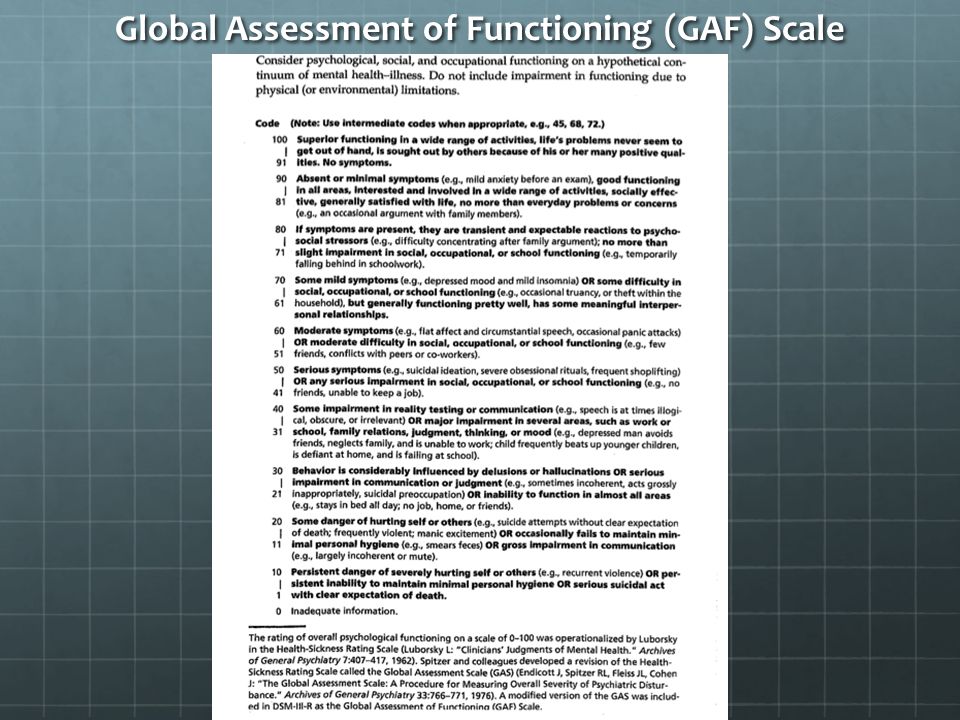 Nevertheless, the value of scientific psychiatry is that it recognizes the presence of objective signs of illness, which the doctor is able to fix. The purpose of books, textbooks and DSM-type standards should be to describe the criteria by which observed symptoms are attributed to a particular pathology. nine0003
Nevertheless, the value of scientific psychiatry is that it recognizes the presence of objective signs of illness, which the doctor is able to fix. The purpose of books, textbooks and DSM-type standards should be to describe the criteria by which observed symptoms are attributed to a particular pathology. nine0003
2) Return to Kraepelin.
By the end of the 1970s the neo-Krepelinian understanding of the goals and objectives of psychiatry finally prevailed. The essence of this medical specialization is no different from the meaning of all other medical specializations: a psychiatrist looks for a biological breakdown in a person and repairs it.
DSM-I and Meyer believed that the patient should be assessed as a person, a "psychobiological" unit. Kraepelin at one time proposed to completely ignore everything personal, to study diseases as objects of the material world. Based on this "impersonal" approach, he compiled his list of mental illnesses.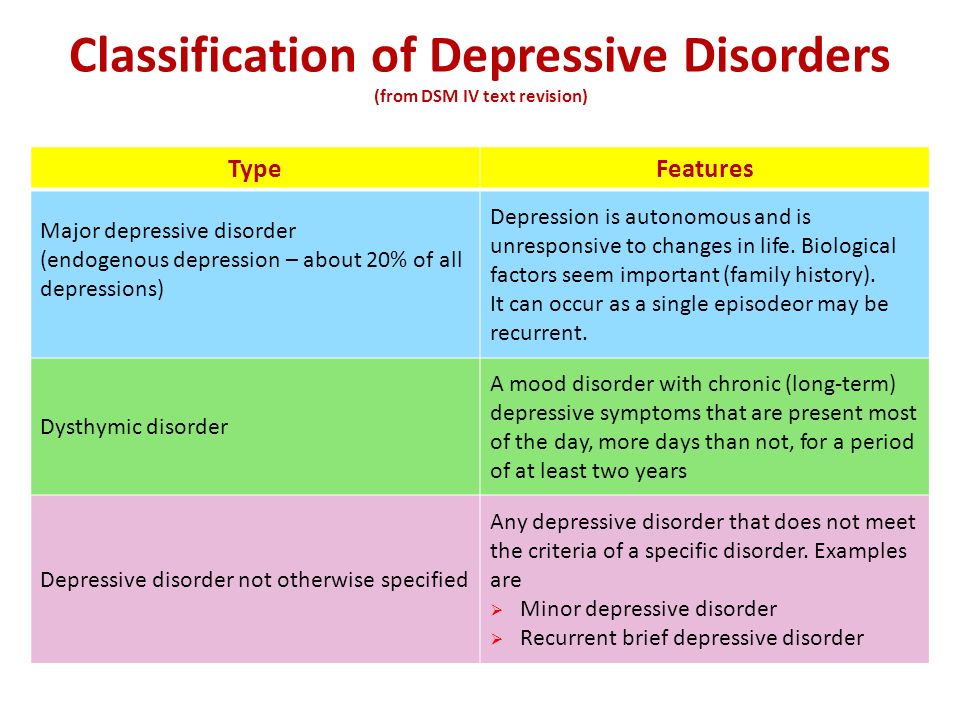 nine0003
nine0003
The Kraepelinian approach was used by the authors of the ICD, including the ICD-8, which was the basis for the drafting of the DSM-III. In 1907, Kraepelin wrote that he could not classify diseases according to their etiology, because their etiology was not yet known to science. He can only systematize the collected observations in a form convenient for learning. Similarly, DSM-III evades etiological issues and proposes a classification of diagnoses based on the practical needs of the doctor. nine0003
The Kraepelinian paradigm found expression in the Feiner Criteria, published in 1972 principles for the validation of diagnostic categories in psychiatry. American specialists proposed five criteria, five objective elements of the overall picture, by which one can judge whether a disease belongs to one category or another.
Clinical picture - that information about the disease, in which certain specific, characteristic features can be distinguished.
Laboratory tests. Feiner himself recognized this criterion as desirable, but, unfortunately, does not exist in psychiatry. And even the highest quality psychological tests cannot be compared with laboratory diagnostics in terms of the degree of objective value for a doctor.
Differential diagnosis. It is necessary to strive to ensure that the diagnostic category in psychiatry is as homogeneous as possible.
How is the recovery going? In the same disease, in theory, the same treatment should give the same result. nine0003
Heredity, i.e. family history. In preparing the DSM-III, this criterion and verification of the diagnosis by laboratory tests were excluded.
The result is a document that is Kraepelinian in spirit: DSM-III assumes that psychiatry needs to be guided by how things are organized in internal medicine; one must finally admit that the causes of mental illness are in the brain; etiology should be postponed until later. Closing the etiological problems will be a triumphant conclusion to the study of the disease, and at the beginning it is necessary to write descriptions of symptoms and carefully conduct differential diagnosis. nine0049 At this point, the DSM-III coincides with Kraepelin's methodology: by making the diagnosis more accurate, psychiatrists will eventually come to understand the pathogenesis.
Closing the etiological problems will be a triumphant conclusion to the study of the disease, and at the beginning it is necessary to write descriptions of symptoms and carefully conduct differential diagnosis. nine0049 At this point, the DSM-III coincides with Kraepelin's methodology: by making the diagnosis more accurate, psychiatrists will eventually come to understand the pathogenesis.
DSM-III-R, DSM-IV, DSM-IV-TR made minor changes to DSM-III. The DSM-III-R finally got rid of the term "neurosis". DSM-IV, DSM-IV-TR are important because they emphasize the importance of empirical evidence over expert opinion. At the time the DSM-III was drafted, the opinion of expert groups could be placed above the results of “field” studies. DSM-IV reflects a new vogue for evidence-based medicine, in which reasoning by the power of authority is not taken seriously. nine0003
DSM-5 marks the beginning of a new process in psychiatry. The path from clarification of diagnoses to etiology turned out to be longer than expected. But it was the etiology that should have become the main validator for the diagnosis. The DSM-III has two validators: the course of the disease (what the illness “looks like”) and the response to treatment (what recovery “looks like”).
But it was the etiology that should have become the main validator for the diagnosis. The DSM-III has two validators: the course of the disease (what the illness “looks like”) and the response to treatment (what recovery “looks like”).
By early 2000 there is a need to change the paradigm and update the philosophy of diagnostics. But, apparently, by the time the DSM-5 was published, the new paradigm had not yet matured. Science has not yet produced descriptions of the neurobiological factors underlying mental illness that can be used as criteria for classifying diseases. As a result, DSM-5 retained the categorical approach, although small inclusions of the dimensional approach were allowed in the organization of the material in chapters. Diagnosis in psychiatry is still based on the analysis of the clinical picture. nine0003
Prepared by: Filippov D.S.
Retrieved : Massimiliano Aragona “Rethinking received views on the history of psychiatric nosology: minor shifts, major continuities” // Alternative perspectives on psychiatric validation: DSM, IDC, RDOC and beyond, Oxford University Press, 2014
What is GSM - encyclopedia lanmarket.
 ua
ua GSM is the second generation 2G mobile network standard. nine0003
In the 1980s, a group was formed to develop a common mobile communication standard. According to Groupe Speciale Mobile (which used to stand for GSM), its main task was to develop a single, consistent network for all of Europe and offer a better and more efficient technical solution for wireless communications.
Although the standard is based on a time division multiple access (TDMA) system, its technology uses digital signaling and voice channels and is considered a second system (2G) for mobile phones. nine0003
GSM end users were the first to use the low cost implementation of SMS (Short Messaging System), which is better known as text message.
Being a cellular network, the cellular communication standard uses cells to provide wireless communication to subscribers in close proximity to these cells. The four main cells that make up the GSM network are called macro, micro, pico and femto.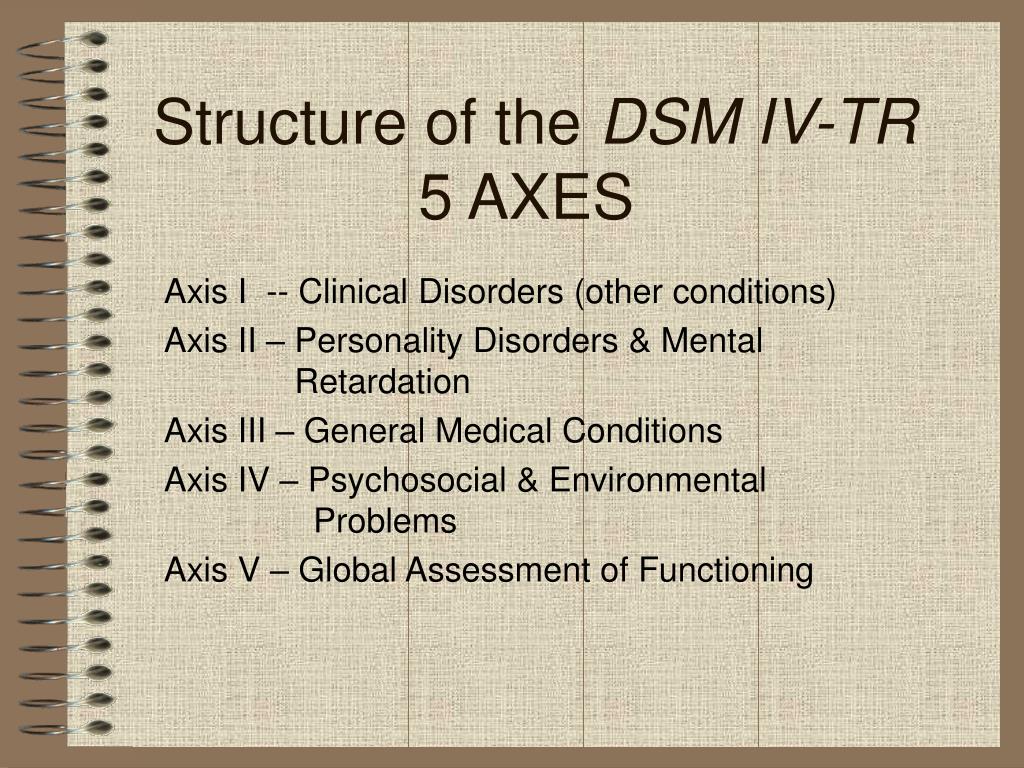 Outdoor coverage is usually provided by macro and micro cells, while indoor coverage is usually provided by pico and femto cells. nine0003
Outdoor coverage is usually provided by macro and micro cells, while indoor coverage is usually provided by pico and femto cells. nine0003
GSM phones can be identified by the presence of a Subscriber Identity Module (SIM). This tiny object, about the size of a finger, is a removable smart card containing the user's subscription information, as well as some contact records. This SIM card allows the user to switch from one GSM phone to another. In some countries, especially in Asia, GSM phones are locked to a specific operator. However, if the user manages to unlock the phone, they can insert any SIM card from any carrier into the same phone. nine0003
One of the main advantages of the GSM standard is the ability to move and switch between operators using individual mobile devices (if partner networks are located at the destination).
History GSM
As stated, work began on what would eventually become the GSM standard in 1981 when CEPT formed the Groupe Spécial Mobile committee to work on a European standard for digital cellular phone technology.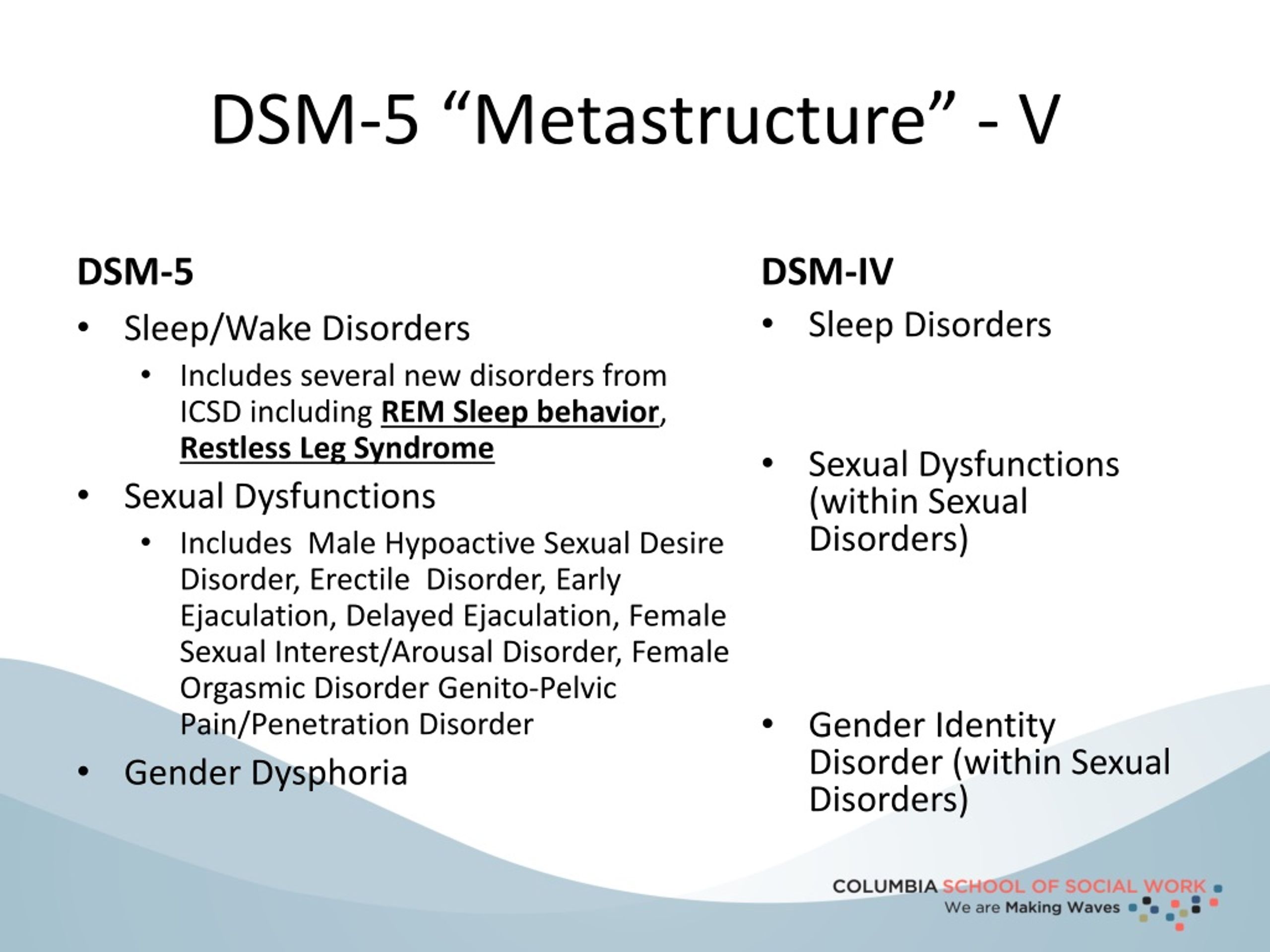 More than five years later, representatives from 13 European countries signed a Memorandum of Understanding in Copenhagen, which agreed to develop and then deploy a common cellular system across Europe. nine0003
More than five years later, representatives from 13 European countries signed a Memorandum of Understanding in Copenhagen, which agreed to develop and then deploy a common cellular system across Europe. nine0003
The first GSM technical specification was published in February 1987. To build on a common mobile standard for Europe, ministers from the four larger EU countries made another political confirmation of their support for the GSM standard through the Bonn Declaration on Global Information Networks in May 1987 (Germany, UK, France and Italy). "MGS GSM" was signed in September 1987 and helped secure cash contributions for investment in the network. As a result, the European GSM network was able to see a much faster rollout than previously thought possible. At 19In 1986, the European Commission proposed that the 900 MHz frequency band be reserved exclusively for GSM use.
The first GSM specification became available in 1990. Just a year later, former Finnish Prime Minister Harri Holkeri made the first telephone call in the world.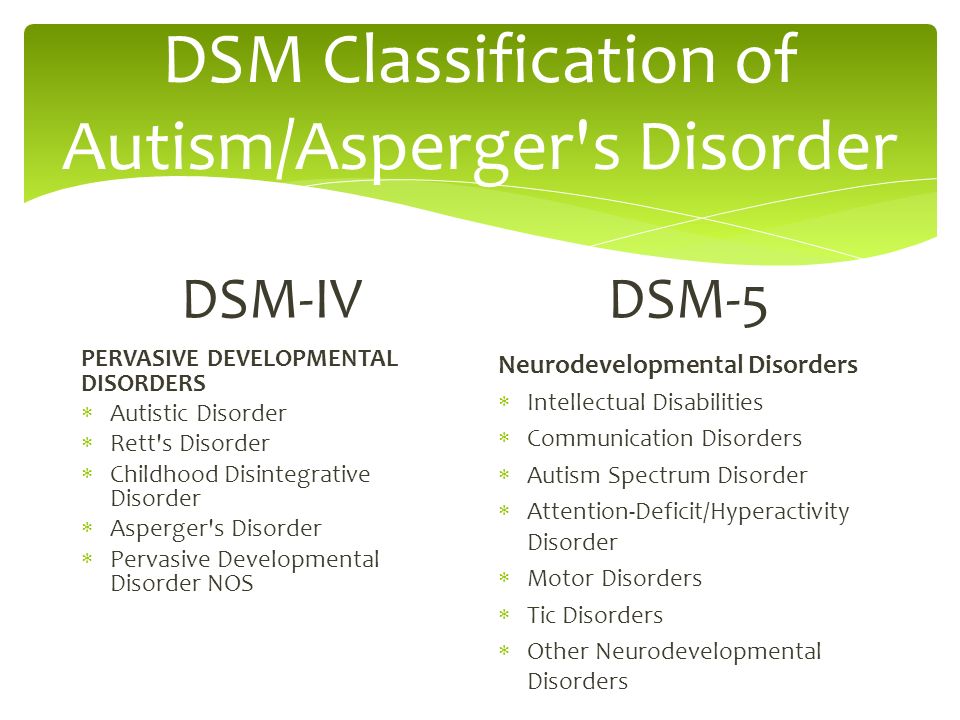 The call was made over a network powered by Radiolinja and built by Telenokia and Siemens. And in 1992, the first SMS was sent over the GSM network. During this year, Vodafone UK and Telecom Finland also signed the first international roaming agreement. nine0003
The call was made over a network powered by Radiolinja and built by Telenokia and Siemens. And in 1992, the first SMS was sent over the GSM network. During this year, Vodafone UK and Telecom Finland also signed the first international roaming agreement. nine0003
Standard features
GSM is a circuit switched system. It divides all 200 kHz channels into eight 25 kHz time slots. The standard operates on three different carrier frequencies: 900 MHz, which was used by the original GSM system; 1800MHz, which was added to support the number of swellable subscribers, and 1900MHz, which is used primarily in the US.
The 850 MHz band is also used for GSM and 3GSM in Australia, Canada and many countries in South America. GSM supports data rate up to 9.6 kbps, which allows the transmission of basic data services such as SMS.
Another important advantage is the possibility of international roaming, allowing users to access the same services as at home when traveling abroad.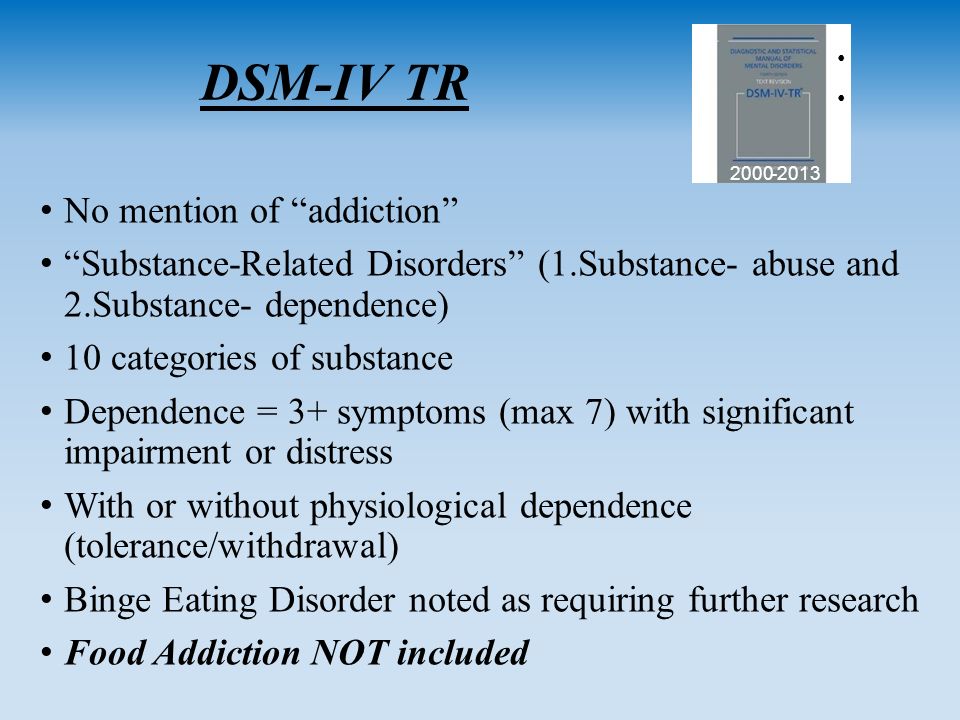 This gives consumers a seamless and consistent connectivity experience in over 210 countries. GSM satellite roaming has also expanded access to services in areas where terrestrial coverage is not available.
This gives consumers a seamless and consistent connectivity experience in over 210 countries. GSM satellite roaming has also expanded access to services in areas where terrestrial coverage is not available.
GSM900/GSM1800
These two standards are used by most countries in the world.
GSM-900 operates on the frequency range 890-915MHz, and is used to exchange information between the mobile station and the base transceiver station (uplink) and 935-960MHz for the downlink. This provides 124 RF channels (channels 1 - 124) spaced at 200 kHz.
In this case, a duplex interval of 45 MHz is used. nine0003
To cover a wider frequency range, an "extended GSM900 or E-GSM" was created. It operates on frequencies from 880 MHz to 915 MHz (uplink) and from 925 MHz to 960 MHz (downlink), which allows you to add 50 channels (975-1023 and 0) to the GSM-900 band. The specification also has the GSM-R standard, which uses frequencies from 876 MHz to 915 MHz (upstream) and from 921 MHz to 960 MHz (downstream).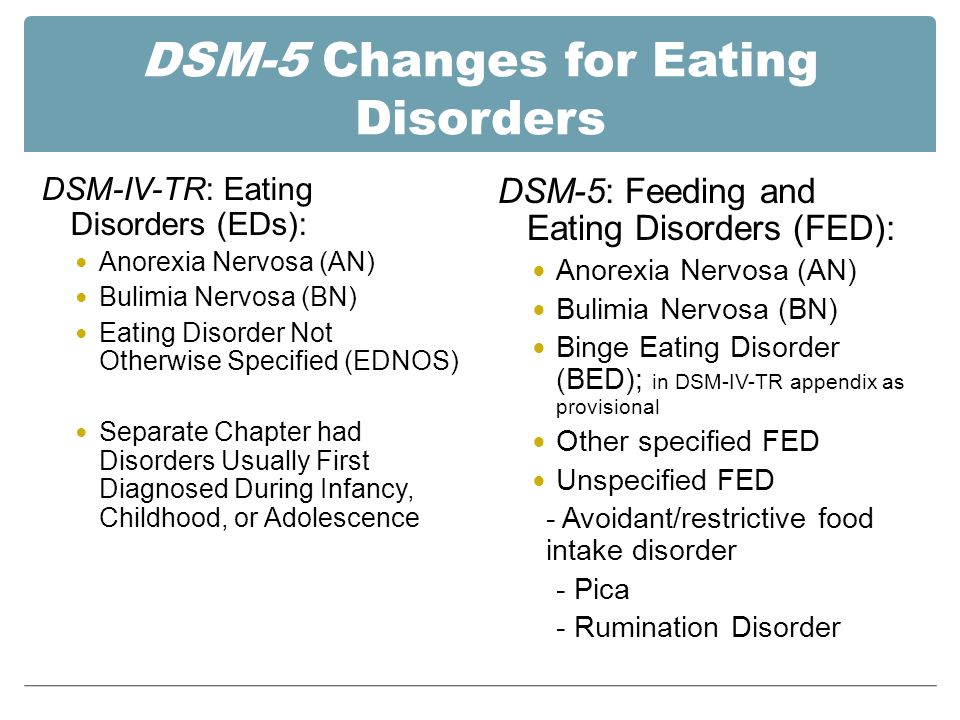 The channel numbers are 955-1023. GSM-R offers specialized channels and services that are used by railway personnel. All these modifications are included in the GSM-9 specification.00.
The channel numbers are 955-1023. GSM-R offers specialized channels and services that are used by railway personnel. All these modifications are included in the GSM-9 specification.00.
GSM-1800, in turn, operates in the frequency range from 1710 MHz to 1785 MHz when transmitting data from a mobile station to a base transceiver and 1805-1880 MHz for another direction. It provides 374 channels (512-885) and 95 MHz duplex.
GSM-1800 is also called PCS in Hong Kong and UK. Most GSM operators in India use the 900 MHz band. Carriers such as Hutch, Airtel, Idea and some others use 900 MHz in rural areas and 1800 MHz in urban areas.
The difference between GSM-900 and GSM-1800 is that GSM-900 has double coverage compared to GSM-1800. This is because as frequency increases, cell size decreases due to increased path loss. Therefore, to ensure full coverage of a specific area in GSM-1800, it is necessary to install more towers than in GSM-900. But since there are more frequencies in the GSM-1800 bands, more opportunities can be provided by good traffic. This allows GSM-1800 to handle more subscribers than GSM-900. A balance of both can help achieve good coverage.
This allows GSM-1800 to handle more subscribers than GSM-900. A balance of both can help achieve good coverage.
GSM-850
GSM-850 and GSM-1900 are used in the USA, Canada and many other countries in North and South America. GSM-850 is also sometimes erroneously referred to as GSM-800. In Australia, GSM 850 is the frequency allocated to NextG Network Telstra which was switched on in October 2006. The NextG network is a step up from the 3G network and is available at higher speeds in Australia compared to the 3G network, which is limited to major cities only. nine0003
GSM-850 uses 824 - 849 MHz to transmit information from the mobile station to the base transceiver station (uplink) and 869 - 894 MHz for the other direction (downlink). Channel numbers from 128 to 251.
Cellular is the term used to describe the 850 MHz band because the original analog cellular mobile communications system was allocated to that spectrum. Providers typically operate on one or both frequency bands.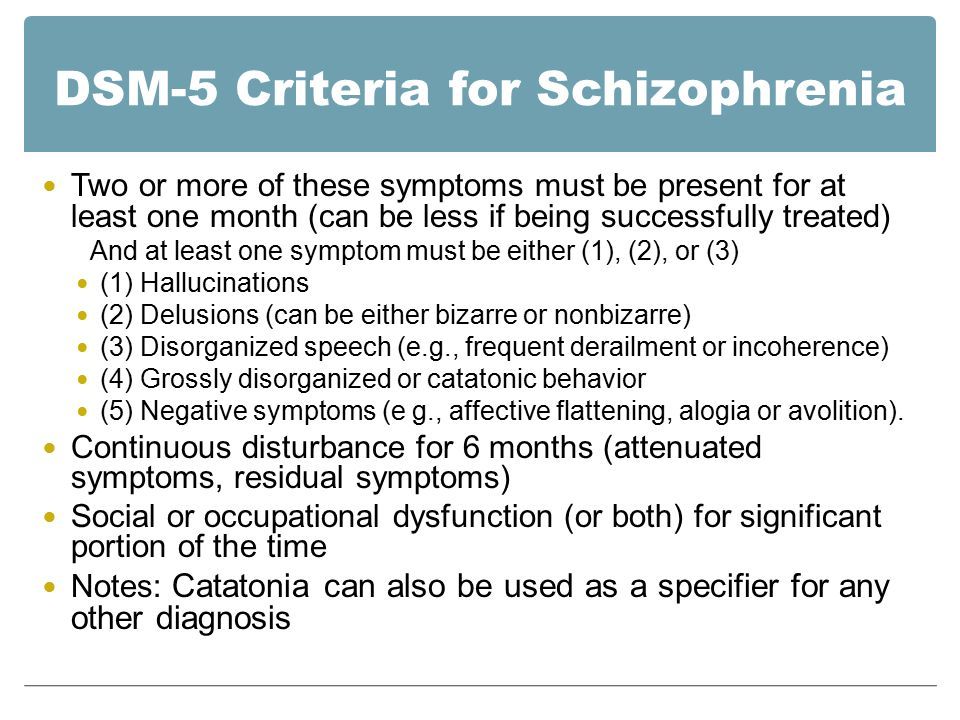 nine0003
nine0003
GSM uses modulations: QPSK, 8PSK, 16-QAM.
GSM works on the principle of a combination of two well-known technologies TDMA and FDMA - multiple access with time and frequency division of channels. The second, in turn, provides frequency division of a band with a maximum width of 25 MHz into 124 carrier frequencies, which are spaced 200 kHz from each other.
Each base station has one or more assigned carrier frequencies. Then, each of the carriers is time-divided using TDMA. The base unit of time in this TDMA scheme is called the pulse period and is ~0.578 ms. Eight periods are grouped into a TDMA frame (~4.62 ms) which forms the base block for defining logical channels. One physical channel represents one burst period for a TDMA frame. nine0003
GSM voice codecs
GSM uses voice codecs to match 3.1 kHz audio at the maximum data rate in the GSM frequency bands. The original codecs used by the GSM standard were Full Rate (13 kbps) and Half Rate (6.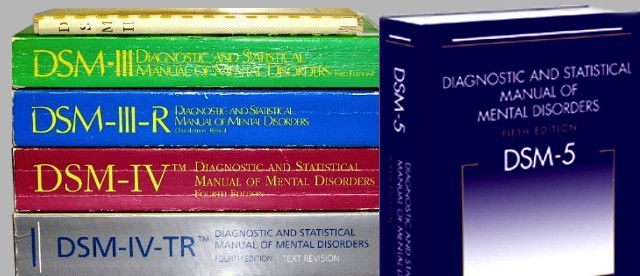 5 kbps). Each of them used a system based on LPC (Linear Predictive Coding). These codecs helped bring maximum efficiency to the bitrate and also made it possible to prioritize and protect the more important components of the transmitted audio signal. nine0003
5 kbps). Each of them used a system based on LPC (Linear Predictive Coding). These codecs helped bring maximum efficiency to the bitrate and also made it possible to prioritize and protect the more important components of the transmitted audio signal. nine0003
In 1997, the EFR codec was published and implemented in the GSM standard. EFR provided a GSM network of 12.2k/s and used a full speed channel. Once UMTS was developed, EFR evolved into AMR-Narrowband CODEC, which is more resistant to interference and is considered to be of higher quality than older GSM codecs.
How does the GSM security service work?
The GSM standard was designed with security in mind from the very beginning. The network was created with the ability to authenticate subscribers using a pre-shared key and challenge response methodology. In GSM, the communication between a mobile handset and a base station can also be encrypted. With the development of UMTS, there is also an optional USIM (Universal Subscriber Identity Module) that provides a longer authentication key to provide enhanced security, and also provides base station authentication to protect the user from spoofing.