What is rem rebound
REM Rebound Effect - StatPearls
Continuing Education Activity
REM rebound behavior refers to the increased frequency, depth, and intensity of rapid-eye-movement (REM) sleep following sleep deprivation or significant stressors. This activity describes the neurophysiology and hormonal processes the contribute to the phenomenon of REM rebound. The article reviews the role of interprofessional teams in improving care for patients who may be experiencing REM rebound due to medical conditions or psychosocial/physical stressors.
Objectives:
Describe REM rebound behavior.
Outline the basic pathophysiology of REM rebound.
Review the common clinical implications of REM rebound in the context of disorders and stressors that affect sleep.
Identify the importance of enhancing the understanding of sleep deprivation to improve outcomes for patients.
Access free multiple choice questions on this topic.
Introduction
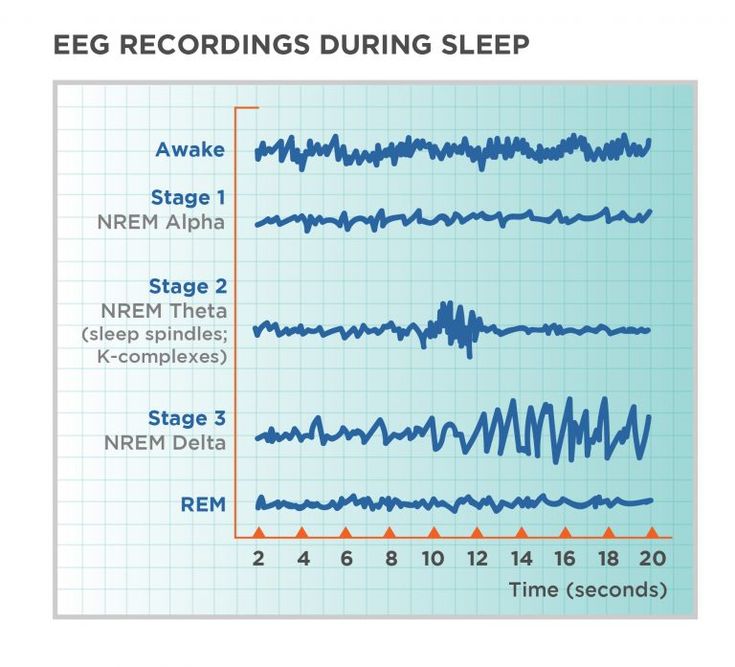
Sleep is a state consisting of several different stages of reversible disconnection from the environment with accompanying reduced consciousness, atonia, and metabolic changes.[1] These stages are primarily divided into rapid-eye-movement (REM) sleep, which is characterized by classic ocular saccadic movement and fast-wave EEG patterns reminiscent of wakefulness, and non-rapid-eye movement (NREM) which can be subdivided further into three stages each distinguished by distinct EEG wave patterns. Normally an individual will progress through a predictable cycle of stages beginning with wakefulness, then through each stage of NREM sleep before quickly reversing through the stages to enter REM sleep.[2]
The maintenance of appropriate sleep architecture appears to play an important role in promoting physiological and mental health.[3][4][5][6] The true purpose of sleep is poorly understood. However some of the health benefits may include energy conservation, restoration, promotion of brain plasticity, modulating memory, emotion, and cognitive integration of stressors and mechanisms are in place to restore sleep homeostasis if sleep is disrupted. One of these mechanisms is REM rebound, which refers to the compensatory increase of the frequency, depth, and intensity of rapid-eye-movement (REM) sleep following sleep deprivation or significant stressors. Several experimental studies utilizing EEG and hormonal measurements have illustrated that human and animal participants who experience sleep deprivation or significant stressors will experience increased frequency and intensity of REM sleep to compensate for said deprivation.[4]
One of these mechanisms is REM rebound, which refers to the compensatory increase of the frequency, depth, and intensity of rapid-eye-movement (REM) sleep following sleep deprivation or significant stressors. Several experimental studies utilizing EEG and hormonal measurements have illustrated that human and animal participants who experience sleep deprivation or significant stressors will experience increased frequency and intensity of REM sleep to compensate for said deprivation.[4]
Etiology
As described earlier, researchers have hypothesized many potential benefits of engaging in REM sleep and that, consequently, REM sleep rebound is an evolutionarily advantageous adaptive strategy with the inability to engage in it having potentially disastrous consequences.[5]
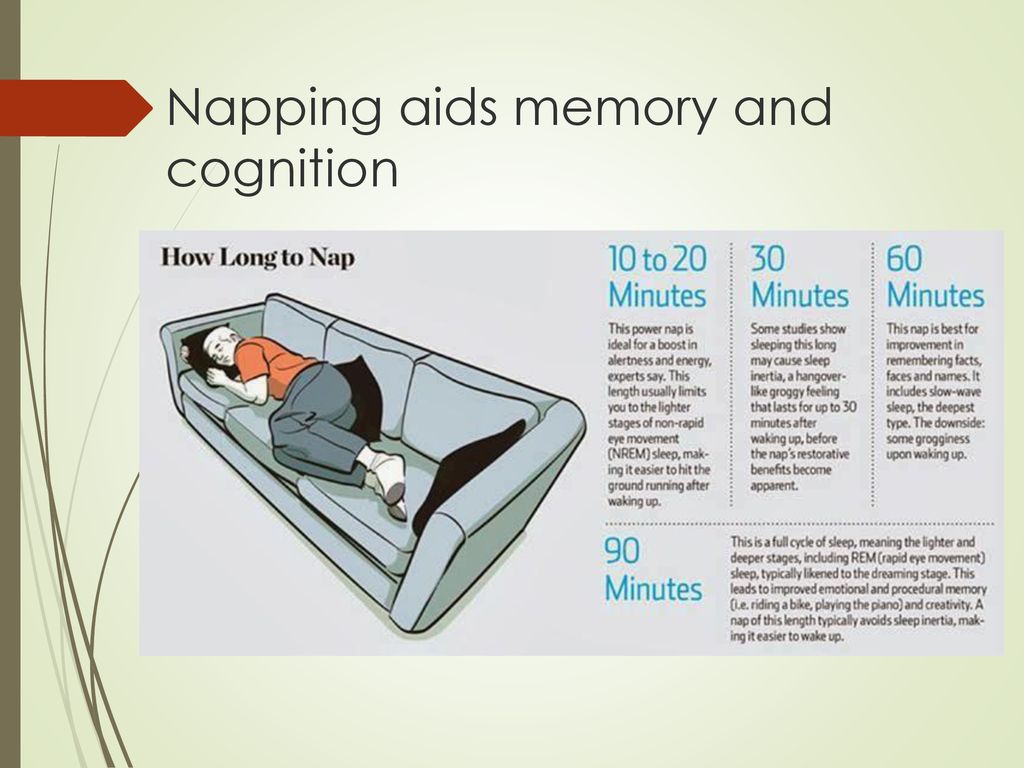
Researchers have hypothesized that REM sleep may be an ideal period of reframing negative experiences and regulating emotional reactivity during a period when stress responses are normally quiescent. This hypothesis has been supported by studies such as one in which human participants expressed diminished negative reactions to images of fearful faces, and positive reactions to happy faces were augmented following a 90-minute nap. [7]
[7]
With that in mind, REM sleep deprivation and stress have been shown to induce changes in hormone release via the hypothalamic-pituitary-adrenal (HPA) axis as well as alterations in levels of neurotransmitters.[3] These signal alterations lead to a reduction in the length and quality of sleep and maintenance of wakefulness, leading to insomnia.[5]
Studies utilizing rat models exposed to multiple types of stress, including footshock, immobilization demonstrated dysregulation of the HPA axis and sympathetic response systems such as those found in the locus coeruleus and adrenal medulla. While rat models have been useful in elucidating the effects of physical stress, the most potent stressors to humans appear to be of a social nature, such as issues in the family, work, and interpersonal relationships.[5]
Epidemiology
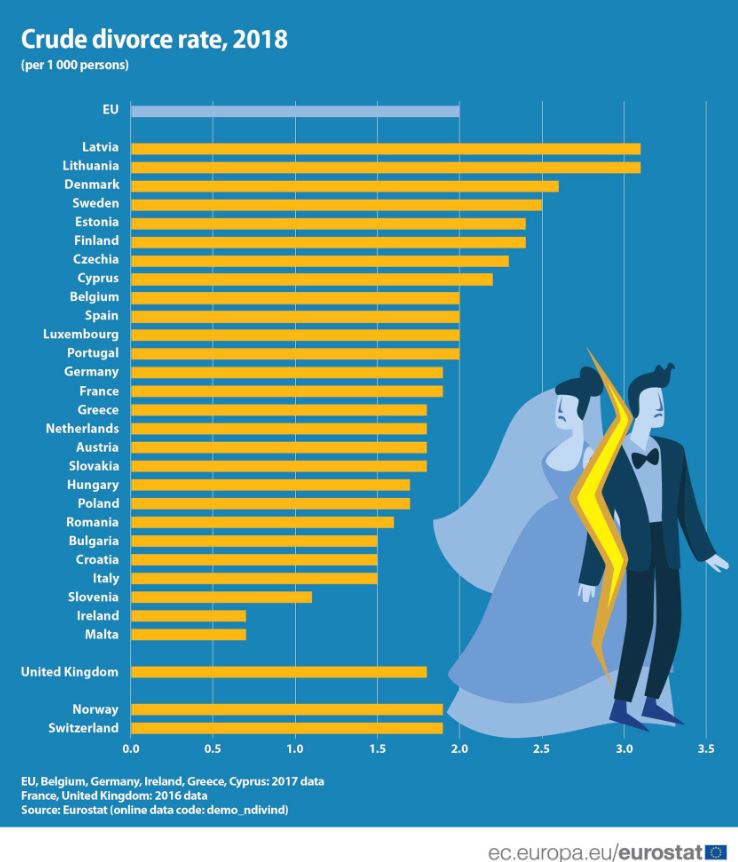
Due to the high prevalence of sleep deprivation and stress, REM sleep rebound appears to be a common phenomenon both in the U.S. and worldwide. According to the CDC, more than a third of the U.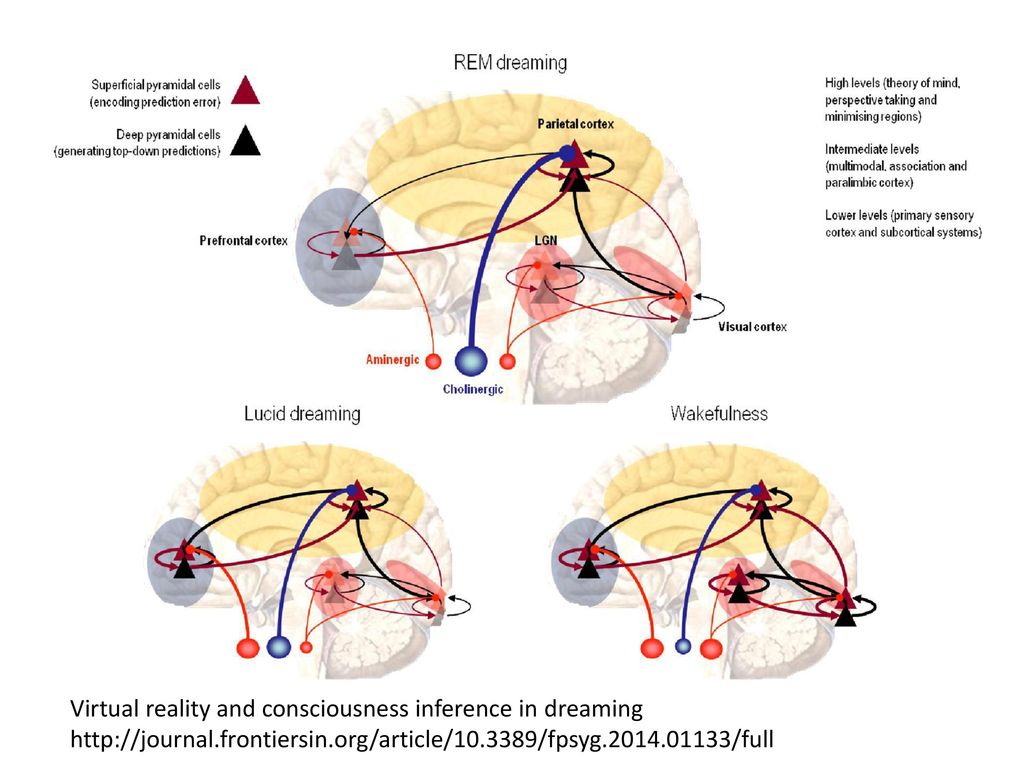 S. population experiences sleep deprivation, which has been defined as less than 7 hours of nightly sleep.[8]
S. population experiences sleep deprivation, which has been defined as less than 7 hours of nightly sleep.[8]
Adequate sleep has been recommended to adults aged 18-60 to promote physical health and well-being, though the true extent of chronic sleep debt in the population remains to be measured accurately.[9] One recent study estimated that the average length of sleep has diminished, on average, 1 hour globally over the last 100 years with the greatest changes corresponding to Europe, North America, and Asia.[10]
Sleep deprivation is associated with the development of a multitude of comorbid conditions, including obesity, metabolic disorders, high blood pressure, vascular pathologies including coronary disease and stroke, and psychiatric morbidity.[5] Such comorbidities combined with motor vehicle accidents, workplace accidents, cardiovascular morbidity, immunosuppression, negative metabolic consequences leading to obesity, increase decline in renal function, medical errors, poor quality of life, and diminished work productivity contribute to national and global concern over the effects of poor sleep. [8]
[8]
Pathophysiology
Sleep is regulated by an interplay of neurotransmitters and neuropeptide systems located primarily in the hypothalamus and brain stem via two main mechanisms: homeostatic and circadian.[3] Homeostatic (“process S”) refers to the physiological drive to sleep, also referred to as “sleep pressure.” Circadian (“process C”) refers to sleep induction as a function of the day/night cycle and acts as the timing mechanism for the waxing and waning of alertness. Both mechanisms interact to induce sleep when sufficient pressure has accumulated, and the light/dark cycle favors sleep, while wakefulness is promoted in the waning of their interaction.
While normal sleep architecture depends heavily on the interaction of the homeostatic and circadian systems, sleep homeostasis appears to depend on the preceding waking period, especially its length and quality.[3] Sleep deprivation is associated with the development of a multitude of comorbid conditions, including obesity, metabolic disorders, high blood pressure, vascular pathologies including coronary disease and stroke, and psychiatric morbidity. [5] Such comorbidities combined with motor vehicle accidents, workplace accidents, cardiovascular morbidity, immunosuppression, negative metabolic consequences leading to obesity, increase decline in renal function, medical errors, poor quality of life, and diminished work productivity contribute to national and global concern over the effects of poor sleep. For example, short periods of sleep deprivation of up to 6 hours are associated with increased non-REM sleep. Those who experience greater sleep deprivation of 12 to 24 hours have a demonstrable increase in both non-REM sleep and REM sleep. Compare both these groups to those who experience approximately 96 hours of sleep deprivation and show nearly exclusive increases in REM sleep.[3] These findings suggest that the severity of sleep deprivation and stress is correlated with increasingly greater compensatory architecture changes.
[5] Such comorbidities combined with motor vehicle accidents, workplace accidents, cardiovascular morbidity, immunosuppression, negative metabolic consequences leading to obesity, increase decline in renal function, medical errors, poor quality of life, and diminished work productivity contribute to national and global concern over the effects of poor sleep. For example, short periods of sleep deprivation of up to 6 hours are associated with increased non-REM sleep. Those who experience greater sleep deprivation of 12 to 24 hours have a demonstrable increase in both non-REM sleep and REM sleep. Compare both these groups to those who experience approximately 96 hours of sleep deprivation and show nearly exclusive increases in REM sleep.[3] These findings suggest that the severity of sleep deprivation and stress is correlated with increasingly greater compensatory architecture changes.
Corticotropin-releasing Hormone (CRH)
Several studies have illustrated the powerful role that CRH plays in sleep regulation and REM sleep rebound. [11][5][6][5] CRH increases during stressful situations simulated in experimental studies utilizing electric footshock, immobilization, restriction of food, and sleep deprivation.[3] CRH has also been shown to reduce REM sleep rebound,[5] REM sleep, and non-REM sleep as well as increase wakefulness when injected intravenously.[3][11] Compare this to findings that CRH hypersecretion in the forebrain is linked with increased REM sleep; this finding provides a possible avenue for utilizing REM sleep as a biomarker for a variety of clinical conditions.[6]
[11][5][6][5] CRH increases during stressful situations simulated in experimental studies utilizing electric footshock, immobilization, restriction of food, and sleep deprivation.[3] CRH has also been shown to reduce REM sleep rebound,[5] REM sleep, and non-REM sleep as well as increase wakefulness when injected intravenously.[3][11] Compare this to findings that CRH hypersecretion in the forebrain is linked with increased REM sleep; this finding provides a possible avenue for utilizing REM sleep as a biomarker for a variety of clinical conditions.[6]
Adrenocorticotropic Hormone (ACTH)
Adrenocorticotropic hormone has been identified as a promoter of wakefulness in both light and dark periods of the circadian rhythm.[5]
Plasma Corticosterone
Cortisol and other steroid hormones analogs appear to play a role in the regulation of sleep, and multiple studies have shown an association between aberrations in plasma cortisol and sleep architecture. For example, Addison disease patients experience more non-REM sleep and less REM sleep, which is corrected with corticoid replacement therapy, whereas patients with excess cortisol in conditions such as Cushing syndrome display less NREM sleep and more awakening associated with excess cortisol secretion.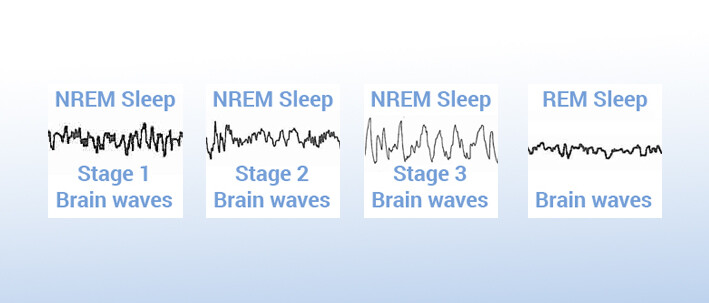 [3][5] Restoring basal levels of cortisol in such conditions restores normal sleep architecture.[5] This suggests that glucocorticoids play an integral role in establishing appropriate sleep patterns in humans, and the full expression of REM sleep rebound following stress.
[3][5] Restoring basal levels of cortisol in such conditions restores normal sleep architecture.[5] This suggests that glucocorticoids play an integral role in establishing appropriate sleep patterns in humans, and the full expression of REM sleep rebound following stress.
Corticotropin-Like Intermediate Peptide (CLIP)
CLIP is derived from proopiomelanocortin (POMC) and is associated with inducing long REM sleep episodes.[3]
Prolactin (PRL)
Prolactin is an important neurotrophic hormone that prevents stress-induced reduction of neurogenesis and constitutes an important mechanism for stress coping and resilience via REM sleep rebound.[3][4] Several studies testing micro-infusions of PRL into the dorsal raphe nucleus (DRN) and the association of anti-PRL antibodies with suppressed REM sleep in rats demonstrated that PRL induces REMS and appears to play a role in regulating the stress-induced REM sleep rebound phenomenon.
Serotonin (5-HT)
Studies of serotonin suggest that it may have a bidirectional relationship with prolactin as studies have correlated the length of REM sleep rebound with increased plasma prolactin and hypothalamic serotonin levels. [4][5]
[4][5]
History and Physical
A thorough clinical evaluation would reveal sleep disruptions and associated pathology that may lead to REM rebound behavior. Gathering a detailed sleep history will likely reveal important information regarding the duration of sleep, the onset of sleep, difficulty in waking, disruptions in sleep maintenance, and quality of sleep. Other pertinent information would include prior medical history and medical comorbidities (e.g., obstructive sleep apnea) and social history, which may influence sleep patterns (e.g., night shift work), medications used.
Such information will prove useful in establishing differential causes for disruptions in sleep and the necessity for further work-up of possible medical comorbidities. A comprehensive physical exam, actigraphy, sleep diary will further hone differential diagnoses or conditions and the appropriateness of polysomnography for further work-up.
Evaluation
Under normal clinical conditions, there is no need to evaluate specifically for REM rebound behavior using EEG or other diagnostic modality.
Treatment / Management
Management of REM rebound is typically consistent with treatment for an identified sleep disorder a patient may be experiencing. The resolution of sleep aberrations has been shown to improve REM sleep once REM pressure has been sufficiently alleviated with quality sleep. Implementing sleep hygiene techniques may improve sleep quality, but research suggests that empirical data regarding their utility is lacking.[12]
Differential Diagnosis
REM rebound behavior itself is not a clinical diagnosis but a phenomenon that accompanies many sleep disorders. Such sleep disorders include a wide range of clinical conditions such as insomnia, psychosocial stress, psychiatric or neuropsychiatric disorders, parasomnias, narcolepsy, obstructive sleep apnea (OSA), or behavioral issues such as poor sleep hygiene or shift work.
Toxicity and Side Effect Management
Many medications can influence normal REM sleep, most notably antidepressants and antipsychotics. For example, research suggests that benzodiazepines normally suppress REM sleep and will increase REM rebound upon discontinuation or in withdrawal.[13] The same effects are seen in barbiturates and ethanol. This is in contrast to new benzodiazepine-like hypnotic sleep aids such as zolpidem that have no associated REM rebound when discontinued. In the case of antidepressants, many patients tend to experience prolonged and more intense dreams associated with REM rebound following the abrupt withdrawal of antidepressant medications.[14]
For example, research suggests that benzodiazepines normally suppress REM sleep and will increase REM rebound upon discontinuation or in withdrawal.[13] The same effects are seen in barbiturates and ethanol. This is in contrast to new benzodiazepine-like hypnotic sleep aids such as zolpidem that have no associated REM rebound when discontinued. In the case of antidepressants, many patients tend to experience prolonged and more intense dreams associated with REM rebound following the abrupt withdrawal of antidepressant medications.[14]
A meta-analysis of multiple substances of abuse showed that withdrawal, recovery, or treatment with a placebo of marijuana, tetrahydrocannabinol (THC), cocaine, heroin, and stimulants result in increased REM sleep rebound, indicating a compensatory return to sleep homeostasis.[15]
Prognosis
The prognosis for resolution of REM rebound is generally favorable but dependent on the resolution of underlying sleep pathology and restoration of normal sleep architecture.![]()
Complications
Several studies have shown that poor sleep can have significant detrimental effects on human health. Such effects include poor mood regulation, diminished memory consolidation, and correlative increased risk of developing psychiatric illnesses such as major depressive disorder, anxiety, and posttraumatic stress disorder (PTSD).[5]
Deterrence and Patient Education
Patient education regarding the consequences of poor sleep and avenues for improving sleep quality is an important part of providing quality care to patients. Poor sleep has been shown to increase the risk of comorbid conditions and diminished well-being illustrated by the following research findings:
One recent study showed a negative correlation between the length of REM sleep episodes and the development of PTSD following a traumatic event.[16] Increased REMS, in general, appears to be protective against the effects of stress in a similar fashion.
Stress and sleep deprivation have both been shown to cause significant changes in hormonal and neurotransmitter regulation.
 One study showed women who suffered from chronic burnout with associated anxiety and poor sleep exhibited reduced prolactin levels, a neurohormone that has neuroprotective properties.[5]
One study showed women who suffered from chronic burnout with associated anxiety and poor sleep exhibited reduced prolactin levels, a neurohormone that has neuroprotective properties.[5]Several epidemiological studies suggest that insomnia and disruptions in normal sleep during stressful periods significantly increase the risk of developing depression.[5]
Nearly all antidepressants are known to reduced REM sleep by approximately 30%, while some antipsychotics such as phenelzine suppress nearly all REM sleep.[17] This has raised questions about the interplay of psychiatric symptoms, REM sleep deprivation, and medications of weight gain in this population.
According to some studies, normal REM sleep appears to lower the risk of developing obesity. Moreover, the loss of the final REM period (fREMP) likely enhances appetite, which can lead to excessive caloric intake and associated weight gain in those with chronic sleep deprivation.[17]
Pearls and Other Issues
REM rebound refers to the compensatory increase of the frequency, depth, and intensity of rapid-eye-movement (REM) sleep following sleep deprivation or significant stressors.

REM deprivation and stress have been shown to induce changes in hormone release via the hypothalamic-pituitary-adrenal (HPA) axis as well as alterations in levels of neurotransmitters.
The most potent stressors to humans appear to be social such as issues in the family, work, and interpersonal relationships.
According to the CDC, more than a third of the U.S. population experiences sleep deprivation, which has been defined as less than 7 hours of nightly sleep.
Sleep deprivation is associated with the development of a multitude of comorbid conditions including obesity, metabolic disorders, high blood pressure, vascular pathologies including coronary disease and stroke, psychiatric morbidity, motor vehicle accidents, workplace accidents, medical errors, and diminished work productivity. Sleep deprivation represents a national and global concern.
Management of REM rebound is typically consistent with treatment for an identified sleep disorder a patient may be experiencing.
 For example, correctly diagnosing and treating obstructive sleep apnea (OSA) will result in REM rebound and promotion of normal sleep homeostasis.
For example, correctly diagnosing and treating obstructive sleep apnea (OSA) will result in REM rebound and promotion of normal sleep homeostasis.Many medications suppress REM sleep and result in REM rebound when discontinued and include benzodiazepines, ethanol, barbiturates, antidepressants, some antipsychotics, marijuana, heroin, cocaine, and other stimulants.
Enhancing Healthcare Team Outcomes
Obstructive sleep apnea (OSA) is a common medical condition that significantly impairs the quality of sleep experienced by patients. OSA is diagnosed using overnight polysomnography, which is considered the diagnostic gold standard, while treatment consists of using overnight continuous positive airway pressure (CPAP) is the most effective treatment.[18][19] [ Level 1] A meta-analysis of OSA treatments reveals that there is no significant difference in outcomes between CPAP and bilevel positive airway pressure (BiPAP) and that compliance remains one of the greatest limiting factors of any OSA treatment excluding surgical intervention.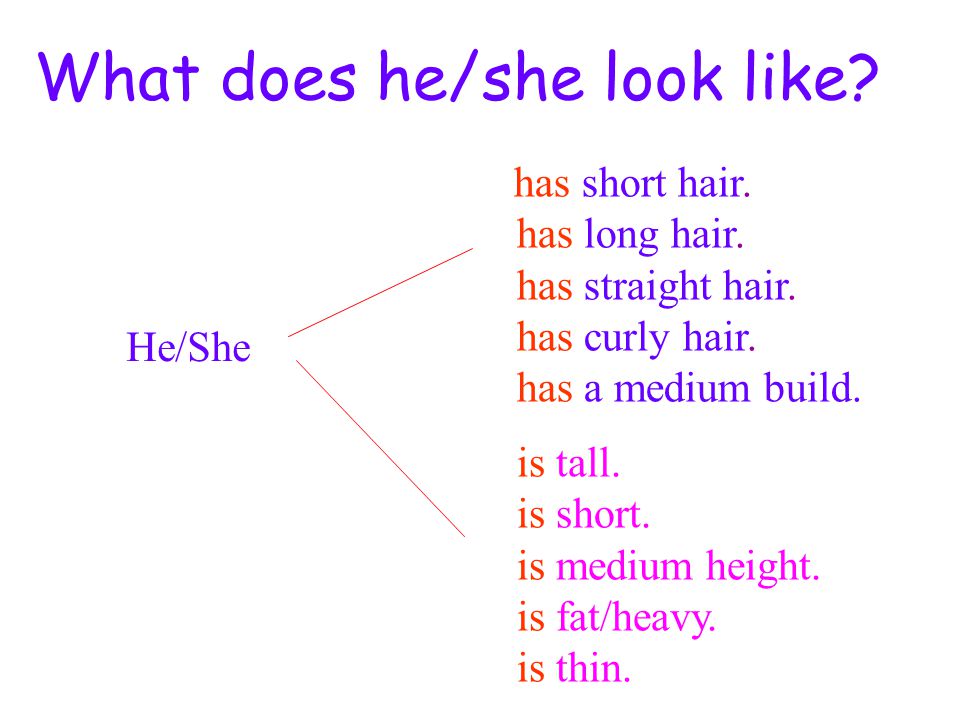 [19] Interestingly, Koo et al. showed that REM sleep rebound following the initial treatment of patients with OSA was correlated with improved sleep quality and mood elevation.[20]
[19] Interestingly, Koo et al. showed that REM sleep rebound following the initial treatment of patients with OSA was correlated with improved sleep quality and mood elevation.[20]
Sleep hygiene is a well-known concept that advocates for behavioral modifications to promote sleep quality, including reducing alcohol and caffeine use prior to bedtime, reducing smoking, consistently exercising, and reducing stress, noise, and light at bedtime. Although these recommendations appear logical at their face, a meta-analysis performed by Irish et al. suggests that there is a paucity of empirical data to support these practices.[12] This issue highlights the need for continued research in sleep and evidence-based interventions to address the growing prevalence of sleep deprivation.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Feriante J, Araujo JF. StatPearls [Internet].
 StatPearls Publishing; Treasure Island (FL): Feb 17, 2022. Physiology, REM Sleep. [PubMed: 30285349]
StatPearls Publishing; Treasure Island (FL): Feb 17, 2022. Physiology, REM Sleep. [PubMed: 30285349]- 2.
Patel AK, Reddy V, Shumway KR, Araujo JF. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Sep 7, 2022. Physiology, Sleep Stages. [PubMed: 30252388]
- 3.
Machado RB, Suchecki D. Neuroendocrine and Peptidergic Regulation of Stress-Induced REM Sleep Rebound. Front Endocrinol (Lausanne). 2016;7:163. [PMC free article: PMC5179577] [PubMed: 28066328]
- 4.
Machado RB, Rocha MR, Suchecki D. Brain prolactin is involved in stress-induced REM sleep rebound. Horm Behav. 2017 Mar;89:38-47. [PubMed: 28017595]
- 5.
Suchecki D, Tiba PA, Machado RB. REM Sleep Rebound as an Adaptive Response to Stressful Situations. Front Neurol. 2012;3:41. [PMC free article: PMC3317042] [PubMed: 22485105]
- 6.
Kimura M, Müller-Preuss P, Lu A, Wiesner E, Flachskamm C, Wurst W, Holsboer F, Deussing JM.
 Conditional corticotropin-releasing hormone overexpression in the mouse forebrain enhances rapid eye movement sleep. Mol Psychiatry. 2010 Feb;15(2):154-65. [PMC free article: PMC2834335] [PubMed: 19455148]
Conditional corticotropin-releasing hormone overexpression in the mouse forebrain enhances rapid eye movement sleep. Mol Psychiatry. 2010 Feb;15(2):154-65. [PMC free article: PMC2834335] [PubMed: 19455148]- 7.
Gujar N, McDonald SA, Nishida M, Walker MP. A role for REM sleep in recalibrating the sensitivity of the human brain to specific emotions. Cereb Cortex. 2011 Jan;21(1):115-23. [PMC free article: PMC3000566] [PubMed: 20421251]
- 8.
Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of Healthy Sleep Duration among Adults--United States, 2014. MMWR Morb Mortal Wkly Rep. 2016 Feb 19;65(6):137-41. [PubMed: 26890214]
- 9.
Stephenson R, Caron AM, Famina S. Behavioral sleep-wake homeostasis and EEG delta power are decoupled by chronic sleep restriction in the rat. Sleep. 2015 May 01;38(5):685-97. [PMC free article: PMC4402665] [PubMed: 25669184]
- 10.
Matricciani L, Olds T, Petkov J.
 In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev. 2012 Jun;16(3):203-11. [PubMed: 21612957]
In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev. 2012 Jun;16(3):203-11. [PubMed: 21612957]- 11.
Steiger A. Neurochemical regulation of sleep. J Psychiatr Res. 2007 Oct;41(7):537-52. [PubMed: 16777143]
- 12.
Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med Rev. 2015 Aug;22:23-36. [PMC free article: PMC4400203] [PubMed: 25454674]
- 13.
Pagel JF, Parnes BL. Medications for the Treatment of Sleep Disorders: An Overview. Prim Care Companion J Clin Psychiatry. 2001 Jun;3(3):118-125. [PMC free article: PMC181172] [PubMed: 15014609]
- 14.
Costa e Silva JA. Sleep disorders in psychiatry. Metabolism. 2006 Oct;55(10 Suppl 2):S40-4. [PubMed: 16979426]
- 15.
Schierenbeck T, Riemann D, Berger M, Hornyak M. Effect of illicit recreational drugs upon sleep: cocaine, ecstasy and marijuana.
 Sleep Med Rev. 2008 Oct;12(5):381-9. [PubMed: 18313952]
Sleep Med Rev. 2008 Oct;12(5):381-9. [PubMed: 18313952]- 16.
Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. REM sleep and the early development of posttraumatic stress disorder. Am J Psychiatry. 2002 Oct;159(10):1696-701. [PubMed: 12359675]
- 17.
Horne J. REM sleep vs exploratory wakefulness: Alternatives within adult 'sleep debt'? Sleep Med Rev. 2020 Apr;50:101252. [PubMed: 31955131]
- 18.
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea With Positive Airway Pressure: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment. J Clin Sleep Med. 2019 Feb 15;15(2):301-334. [PMC free article: PMC6374080] [PubMed: 30736888]
- 19.
Slowik JM, Sankari A, Collen JF. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jun 28, 2022. Obstructive Sleep Apnea. [PubMed: 29083619]
- 20.
Koo BB, Wiggins R, Molina C.
 REM rebound and CPAP compliance. Sleep Med. 2012 Aug;13(7):864-8. [PubMed: 22705243]
REM rebound and CPAP compliance. Sleep Med. 2012 Aug;13(7):864-8. [PubMed: 22705243]
What is REM Rebound? How to Tell if You're Experiencing the REM Rebound Effect
By: SleepScore Labs | July 9th, 2019
Have you ever woken up feeling lost as what day of the month or time of the day it is because you had a very long and eventful (thanks to the adventurous dream you also had) sleep? You probably experienced a “REM rebound” — a period of increased rapid-eye-movement (REM) sleep due to prior periods of sleep deprivation or other stressors.
Sleep is a complex and essential process that helps the body refresh and recharge itself. Suppose, for some reason, your body starts lacking its needed sleep duration. In that case, it’ll start adding up your sleep debt and let many other processes in your body pay for it (in excessive daytime sleepiness, fatigue, irritability, confusion, mood swings, sluggishness, lower attention span, etc. ) until you start having a sufficient amount of sleep quantity (around 7-9 hours, for most healthy adults).
) until you start having a sufficient amount of sleep quantity (around 7-9 hours, for most healthy adults).
The same happens when you don’t get adequate rapid eye movement (REM) sleep. In this case, when your body has the chance, it’ll spend more time in REM sleep (what is known as REM rebound) to make sure it pays up your REM sleep debt.
But what even is REM sleep?
Most healthy people cycle through four stages of sleep throughout the night: NREM (non-rapid eye movement) 1, NREM 2, NREM 3 (AKA, deep sleep), and REM sleep. REM sleep, the state where dreams are most likely to occur, is a sleep state that is thought to generally regulate emotions and consolidate memory. According to the American Sleep Association, three things are associated with REM sleep: limited to no muscle activity (known as muscle atonia, thought to occur so we don’t act out our dreams), rapid eye movements, and dreams.
Research states that REM sleep takes up about 20% to 25% of total sleep time and happens every 90 to 120 minutes of a night’s sleep. A person may go through four to five cycles of REM sleep in one night, although longer periods of REM sleep are more likely to occur during the second half of the night. Research observes that REM sleep helps with mental and emotional recovery from traumatic experiences by suppressing troubling memories through “reverse learning or remodeling process.”
A person may go through four to five cycles of REM sleep in one night, although longer periods of REM sleep are more likely to occur during the second half of the night. Research observes that REM sleep helps with mental and emotional recovery from traumatic experiences by suppressing troubling memories through “reverse learning or remodeling process.”
Because there is a sleep deprivation epidemic, chances are: you’ve experienced REM rebound, as well as many other people.
What is REM Rebound?REM rebound happens when the body stays in the REM sleep stage longer than it usually would. According to the Journal, Hormones and Behaviour, it’s the body’s response to stress and sleep deprivation. When you don’t get enough REM sleep, your body compensates itself by increasing the frequency, depth, and intensity of your REM sleep when it can.
So, instead of REM sleep state taking up only around 20% to 25% of total sleep time, it could take up to 58% of sleep time. Studies suggest that a 20% increase in REM sleep time is a marker of REM rebound in people with obstructive sleep apnea (OSA) who begin continuous positive airway pressure (CPAP) treatment.
Studies suggest that a 20% increase in REM sleep time is a marker of REM rebound in people with obstructive sleep apnea (OSA) who begin continuous positive airway pressure (CPAP) treatment.
Several hormones play a significant role in regulating sleep architecture (the structure of sleep stages—NREM sleep and REM sleep—during sleep) and creating the REM rebound effect. They include:
- Corticotropin-releasing Hormone (CRH)
- Plasma Corticosterone
- Corticotropin-Like Intermediate Peptide (CLIP)
- Prolactin (PRL)
- Serotonin (5-HT)
REM rebound primarily happens when the body is stressed or sleep-deprived. According to the Journal of Clinical Sleep Medicine, five factors may cause an increase in REM sleep time, including: REM sleep deprivation, withdrawal of REM-suppressing recreational drugs, withdrawal of REM suppressing drugs, depression, and undergoing CPAP treatment.
Let’s look into them.
1. Sleep Deprivation
One in three American adults are sleep-deprived—meaning they regularly don’t get the sleep duration their body needs (The CDC recommends getting 7 or more hours of sleep).
Sleep deprivation is one of the major reasons why you may experience REM rebound, particularly as the body won’t also be getting needed REM sleep. Studies suggest that when a person continually doesn’t get enough REM sleep, it’ll attempt to recover “REM sleep-enriched sleep” whenever the opportunity comes.
The more sleep deficit a person has, the more likely their sleep architecture will change to accommodate more REM sleep. Research suggests that people who don’t get enough sleep for 12 to 24 hours will have increased REM and deep sleep when they finally do.
2. Stress
Stress is another widely acknowledged reason why a person may experience the REM rebound effect. According to an article published in the EXCLI journal, depending on the nature and severity of the stressor, stress can trigger different responses on the body, from altering a person’s sleep architecture to severe illnesses.
Stress and sleep have a two-way relationship. Insufficient sleep may exert stress on the body, while acute stress may trigger REM rebound—with chronic stress ultimately affecting overall sleep quality.
Numerous studies suggest that increased REM sleep state is the body’s recovery response to negative and stressful experiences: “Go to bed because you’ll feel better in the morning.” For example, evidence found that victims of motor vehicle accidents who got more REM sleep episodes didn’t later have PTSD. Plus, a 2019 study found that the most distinct effect of acute stress is longer REM sleep time.
3. Withdrawal of REM Suppressing Recreational Substances and Alcohol
Some recreational substances like cocaine, marijuana, and alcohol may suppress REM sleep. So, when a person stops taking them, they can experience the REM rebound effect.
Evidence shows cocaine and amphetamine are stimulants that disturb sleep and reduce REM sleep and overall sleep time. When a person abruptly discontinues use, they may experience excessive daytime sleepiness and REM rebound.
When a person abruptly discontinues use, they may experience excessive daytime sleepiness and REM rebound.
Tetrahydrocannabinol (THC)—a psychoactive constituent of cannabis— in high dose may reduce REM sleep. A 2020 study comparing reduced REM sleep percent in heavy marijuana users and non-marijuana users found that marijuana users had significantly lower REM sleep than non-marijuana users.
According to an article published in the Journal, Advances in Experimental Medicine and Biology, alcohol, even in moderate amounts, can reduce REM sleep. Once a person stops intaking alcohol, they’ll first experience an increase in REM before returning to the average REM sleep duration.
4. Withdrawal of REM Suppressing Drugs
REM suppressing drugs may restrict REM sleep time, so when a person abruptly stops taking them, they may experience a remarkable increase in REM sleep state.
For example, antidepressants, especially those with anticholinergic properties, produce the REM rebound effect after discontinuation. Also, some medications for treating sleep disorders, like barbiturates, significantly reduce REM sleep time. If a person stops them, it also means their REM sleep time will go up.
Also, some medications for treating sleep disorders, like barbiturates, significantly reduce REM sleep time. If a person stops them, it also means their REM sleep time will go up.
5. Depression
Depression is a mental health condition, and one of its distinctive symptoms is poor sleep. Studies suggest that depression alters sleep architecture by reducing deep sleep and disrupting REM sleep. People with depression may experience higher REM sleep duration and intensity. Little wonder studies suggest that REM sleep deprivation in people with depression may improve the condition.
REM sleep quantity has been identified as a marker of depression, that may identify relapse and remission in a person with depression.
6. Starting CPAP Treatment
People with obstructive sleep apnea (OSA), a condition in which the upper airway intermittently collapses all through the night, continually experience sleep deprivation because of this sleep disorder. So when they begin CPAP treatment (the gold standard for preventing OSA episodes), they immediately show increased REM sleep state, taking up as much as 58% of total sleep time.
Similarly, a 2014 study showed that a 34-year-old man who had OSA had a substantial increase in REM sleep after undergoing CPAP treatment that took up 72% of his total sleep time.
How Can You Tell If You’re Experiencing the REM Rebound Effect?The best way to tell if you’re experiencing the REM rebound effect is by seeing a doctor who may conduct a thorough clinical evaluation of sleep disturbances and related pathology that may cause REM rebound.
But people who experience REM rebound may have longer, more vivid dreams while asleep and may wake up feeling disorientated, confused, and with a headache.
Treating underlying sleep disorders and maintaining healthy sleep hygiene may help improve REM sleep and bring it to baseline, which is usually 20 to 25% of total sleep. Consider consulting with a doctor if you suspect that you may have a sleep disorder so they can recommend appropriate treatment for your case and improve your sleep health.
HOTFIX: 235609 | News Arc
This extraordinary update following the release of Swamps of Korsus contains a number of bug fixes, balance changes and a few other nice little things!
version: 235609
The difficulty
The health of ordinary opponents on high, nightmare and apocalyptic difficulties
,The health and damage of the bosses on high, nightmare and apocalyptic difficulties
NOTE: A lot of people have noticed an increase in difficulty across the board (High and Nightmare), so we've tweaked the numbers a bit to get health and damage back on track. It will become more pleasant to play, and individual fights no longer strain so much ... well, except in the Apocalypse!
It will become more pleasant to play, and individual fights no longer strain so much ... well, except in the Apocalypse!
Missing Accessories
Fixed an issue that prevented certain DLC accessories from appearing in Campaign/Adventure
NOTE: An issue has been identified that was preventing some DLC items from appearing in Campaign and Adventure. When zones are restarted, new items will appear in them along with everything else. We hope you find a worthy use for them! nine0003
Fall Damage
Adjusted fall damage to no longer depend on friendly damage modifier.
NOTE: Have you ever crashed to your death on higher difficulties by inadvertently tripping? Call 1-800-OUR-BAD1… that is 1-800-OUR-BAD1. (FIXED).
Bounce Back
Fixed a bug that caused the dodge cancel window to advance 2 frames earlier than
which could be achieved with near-permanent bounce immunity while wearing one piece of Akari's armor and an evasion ring (as long as stamina lasted, of course). Adjusted the window so that everything was fair. nine0003
Adjusted the window so that everything was fair. nine0003
Damage over time / stacking effects
Damage over time effects (Burning/Bleeding) are correctly modified by damage boost bonuses
ModNOTE: A number of Burn and Bleed effects did not benefit from the damage source. Fixed! nine0003
Mod Damage Boost
Mods correctly show armor bonus damage boost
NOTE: Just a visual change.
Emotes
Nerfed "Flirting from afar"
NOTE: joke, didn't touch anything.
Basic
Added a chance to find a consumable item in loot boxes
Added survival version number 9 to the options page0003
NOTE: Players were observed to be running low on consumable ammo and having an excess of ammo (reflected by low demand for Ammo Boxes). To fix two problems at once, instead of ammunition, loot boxes will drop consumables with the same low probability. Also, the version is now indicated in the parameters so that you can see in which patch the world records were set!
Also, the version is now indicated in the parameters so that you can see in which patch the world records were set!
Enemies
Enemies health gain increased by 4% per world level
Bosses health increased by about 15%
NOTE: We noticed that at high levels the bosses somehow died quickly, so the overall health gain was slightly increased, and the bosses got a little more on top. This way they will live longer, but should still crumble if you have a good build!
Armor Gain
Adjusted armor gain from divine nectar in survival from 35 to up to 25%
Adjusted the armor gain from the Woodskin talent in Survival from 15 pts. up to 15%
NOTE: In Survival, Woodskin and Divine Nectar added pure armor instead of a percentage bonus. That is, with maximum skin, armor with a base defense of 50 turned into 350. After the change, all types of armor returned to acceptable values, and Daredevil's Ward no longer receives almost as much armor as a whole set, but without any penalties! As a result of this change, most races will be a little shorter (both armored and unarmored), but we will not be surprised at all by the new insane records from the most avid players! nine0003
Rewards
Ring of Prosperity became a 25-kill reward (account-wide)
Talisman of Perseverance became a 50-kill reward (account-wide)
survival. So we tweaked it and moved it to the 50 kills category. If you already have 50 kills, kill another boss and you will receive a reward. And the ring of prosperity was moved to category 25 (+1 boss, and it will open). If you found tenacity with fauns, the item will remain on the character, but will not be shared for the account until you open it in survival mode. nine0003
So we tweaked it and moved it to the 50 kills category. If you already have 50 kills, kill another boss and you will receive a reward. And the ring of prosperity was moved to category 25 (+1 boss, and it will open). If you found tenacity with fauns, the item will remain on the character, but will not be shared for the account until you open it in survival mode. nine0003
Ravager
The immortality timer no longer resets when touching a World Stone
The cooldown timer now has a secret...
survival. Fixed it. However, they also added a hidden property to the Ravager. Find which one? =O
Beam Rifle
No longer stacks with other players
Slightly reduced slew rate from 0.3 to 0.25
Adjusted hidden effect slew duration from 2s to 1.05s
which was never told to the players). As a result, two or three rifles on the move inflicted maximum damage - and this is too much! We also left the main damage, but added the capricious effect. The weapon still deals the most sustained damage in the game (even with a margin), but this will require more attention to keep the beam on the target. nine0003
The weapon still deals the most sustained damage in the game (even with a margin), but this will require more attention to keep the beam on the target. nine0003
Pride Iskala
Fixed an issue that caused players to charge the mod to full, dealing damage after
is not it? Fixed!
Transfer Token
No longer damages allies. nine0003
Swarm
Fixed an issue that caused the swarm to deal crazy damage close to the target.
NOTE: No change to normal cast... unless your normal method was to run up close to do the most damage. In this case: "Ai-i-i-i!"
Shimmer Shroud
Charge required to activate reduced from 1500 to 1000
Duration increased from 10s to 15s
Introduced a 15 second timer after the shield expires
NOTE: at low levels, the shroud took too long to charge, and at high levels almost instantly. We lowered the activation requirements to make it easier to access at first, increased the duration and added a timer to prevent continuous spamming (invulnerability) on high difficulties.
We lowered the activation requirements to make it easier to access at first, increased the duration and added a timer to prevent continuous spamming (invulnerability) on high difficulties.
Dimensional Jump
Implemented a 20 second timer after applying
NOTE: The jump has become very rough due to almost instantaneous charging. We've added a short cooldown to prevent spam and stay invulnerable forever.
Seeker Beetle
Charge required to activate reduced from 600 to 350
Charges reduced to 3
Nearly halved activation requirements and reduced the number of charges by two. nine0003
Replenishment Aura
Increased effect on NPCs from 50% to 100% (Root Mother, Liz/Liz, etc.)
NOTE: SAVE THEM!
Corrosive Aura
Radius increased from 4.5m to 5m (similar to Scrapper)
NOTE: nice little thing.
General
Fixed an issue where 9 DLC accessories were not appearing in Campaign and Adventure
NOTE: Seek and you shall find. Sorry for the inconvenience!
Daredevil's Ward
Damage bonus increased from 25% per item to 30%
NOTE: Previous version provided about 20% damage over all pure armor and damage builds, but with the penalty of no defense . In the campaign it worked tolerably, but due to the sheer survival armor bonus, the ward became too strong. However, since we fixed the Survival Armor gain issue, the trinket wasn't as attractive anymore, so we've increased the overall damage for all builds to approx. by 30% in all modes. nine0003
Black Sun Stone
Duration increased from 15s to 20s
Bonus increased from 6% to 7%
NOTE: Slightly boosted damage and extended duration to look better against other rings due to requirements!
Cartridge
Cartridges can be knocked out.
NOTE: Convenient!
Thorned Horror
Fixed an issue where the Hunter's Mark would cause the legs of the Thorned Horror to appear. nine0003
NOTE: Well, actually. Why.
Eraser
Fixed an issue where burning would overlap through invulnerability frames (dodge).
NOTE: This is the one we missed. Now fixed!
Torturer
Fixed an issue with bulging health bars in multiplayer
NOTE: Everything is as clean as it should be!
Suppressor
Stun no longer prevents him from returning from teleport
NOTE: Sorry Teawrex!
Queen Iskal
Slightly reduced overall health in all difficulties
Slightly reduced damage in all difficulties
Together with the adjusted difficulty, a small reduction in the main parameters will bring it into full order, while at the same time retaining the spirit of the challenge.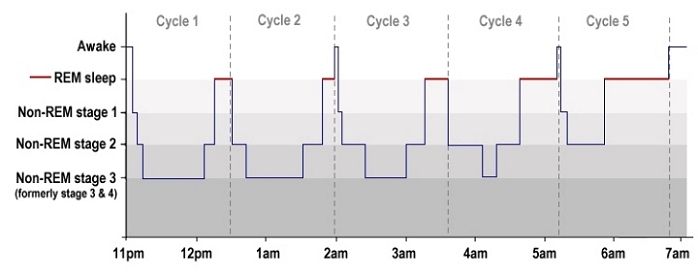 However, if you want something0353 insanely complex, check her out on the Apocalypse!
However, if you want something0353 insanely complex, check her out on the Apocalypse!
9000 Radiant Shell Fixed an issue that caused the anti-cheat to work when passing the Radiant Shell to the game client
A black plane was removed, which appeared in one of the doorways
Widgets/toasts
Fixed a problem, due to which certain notifications were closed by other notifications of
Control points
Failed the problem, the problem was corrected, the problem was correct where the pointer didn't work if tooltips were turned off
Audio: General
Fixed several general audio cues. Nothing mind blowing! nine0003
Art. art: general
Fixed some artistic bugs.
To install the update, you need to restart the game client. In multiplayer, all players must have the same version.
For technical questions and bugs, please visit: https://support.arcgames.com/hc/en.
Follow our Twitter and VK pages to read official announcements! And you can chat with other developers and players on the server in Discord! nine
- ← Older edit
- Newer edit →
Revision as of 08:45, 30 December 2020
337 bytes added , 2 years agoAdapting to Uberman is extremely difficult. While some people may argue that there is an easier method, this is not the case. Any adaptations to this schedule involve long, intense [[wikipedia:Sleep_deprivation|sleep deprivation]], which is necessary to achieve the desired level of sleep compression. nine0003
Adapting to Uberman is extremely difficult. While some people may argue that there is an easier method, this is not the case. Any adaptations to this schedule involve long, intense [[wikipedia:Sleep_deprivation|sleep deprivation]], which is necessary to achieve the desired level of sleep compression.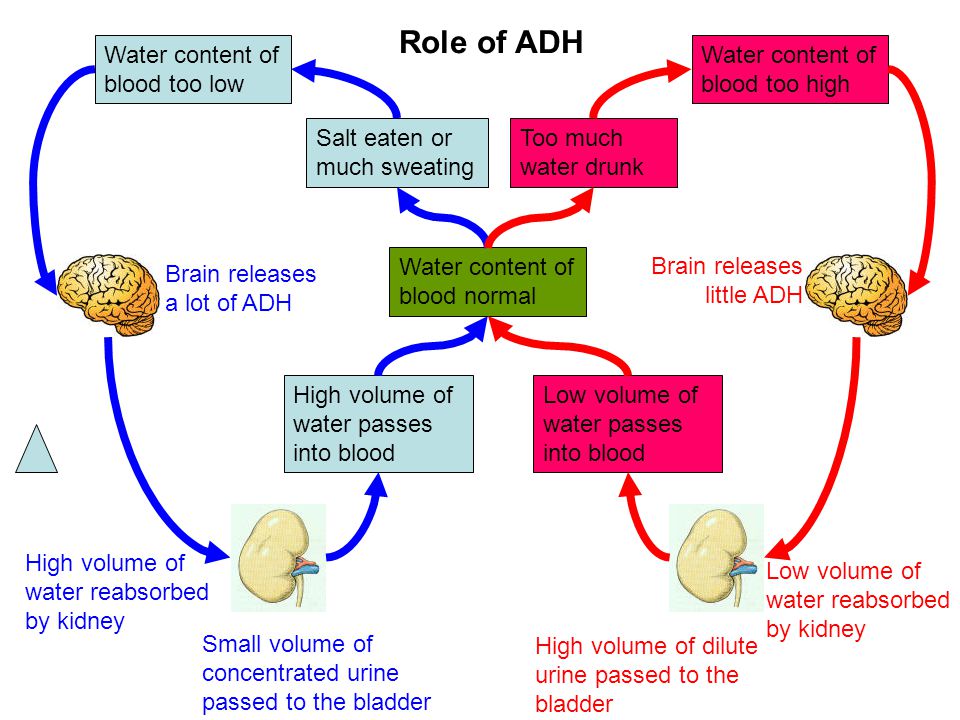
Without previous experience, NEPs will mostly contain [[wikipedia:Non-rapid_eye_movement_sleep|light sleep]] or traces of SWS. As the need for REM is not met, the REM pressure quickly reaches high levels, causing the REM to rebound. This usually happens around 3-5 days. It suddenly alleviates [[wikipedia:Sleep_deprivation|sleep deprivation]], making people prone to over-confidence in adapting. After that, the NEPs mostly contain REM and the SWS pressure starts to rise. The SWS rebound usually occurs around day 7-8 and is the hardest part of adjusting when most people wake up. After avoiding this first failure, subsequent failures every 2-3 days must also be avoided. REM and SWS pressure gradually reach equilibrium and the graph finally stabilizes. This may take weeks and some may take up to 6 weeks to adjust. nine0003
Without previous experience, NEPs will mostly contain [[wikipedia:Non-rapid_eye_movement_sleep|light sleep]] or traces of SWS. As the need for REM is not met, the REM pressure quickly reaches high levels, causing the REM to rebound. This usually happens around 3-5 days. This suddenly alleviates sleep deprivation, making people prone to over-confidence in adapting. After that, the NEPs mostly contain REM and the SWS pressure starts to rise. The SWS rebound usually occurs around day 7-8 and is the hardest part of adjusting when most people wake up. After avoiding this first failure, subsequent failures every 2-3 days must also be avoided. REM and SWS pressure gradually reach equilibrium and the graph finally stabilizes. This may take weeks and some may take up to 6 weeks to adjust. nine0003
As the need for REM is not met, the REM pressure quickly reaches high levels, causing the REM to rebound. This usually happens around 3-5 days. This suddenly alleviates sleep deprivation, making people prone to over-confidence in adapting. After that, the NEPs mostly contain REM and the SWS pressure starts to rise. The SWS rebound usually occurs around day 7-8 and is the hardest part of adjusting when most people wake up. After avoiding this first failure, subsequent failures every 2-3 days must also be avoided. REM and SWS pressure gradually reach equilibrium and the graph finally stabilizes. This may take weeks and some may take up to 6 weeks to adjust. nine0003
* Incompatible with exercise (especially for gaining muscle mass) ref >Dont Panic. Polyphasic Sleeping Discord Server. https: / /discord.com/channels/249219704655183876/249219704655183876/282064
* Weight gain >aeia.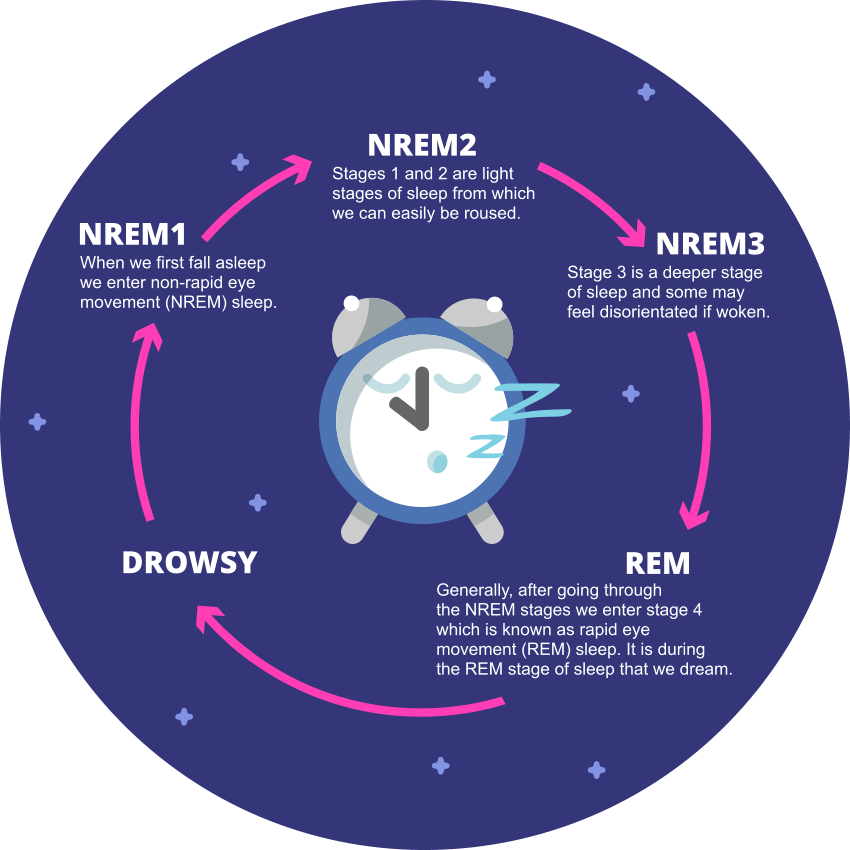 “Giving up Polyphasic Sleep.” YouTube, YouTube, 4 July 2010, www.youtube.com/watch?v =
“Giving up Polyphasic Sleep.” YouTube, YouTube, 4 July 2010, www.youtube.com/watch?v = 0RG44dnwyM0. < / ref >
* Lack of sleep flexibility even after adaptation
* 3 hours and 40 minutes between NEPs is usually not enough for many continuous activities
* 3 hours and 40 minutes between NEPs is usually not enough for many continuous activities between NEPs
Steve Pavlina worked from home while adjusting to Uberman, and Puredoxyk also had flexible work while at university as she adjusted to her schedule.
Steve Pavlina worked from home while adjusting to Uberman, and Puredoxyk also had a flexible job while at university as she adjusted to her schedule.
Severe adaptation is extremely sensitive to sleep skipping. As Puredoxyk states in "Ubersleep", skipping just one NEP causes symptoms of intense [[wikipedia:Sleep_deprivation|sleep deprivation]], as if a person had missed several nights of monophasic sleep in a row. Even after adaptation, there is still a risk of oversleeping, and possibly maintaining an alarm system indefinitely.
Severe adaptation is extremely sensitive to missed sleep. According to Puredoxyk in "Ubersleep", skipping just one NEP causes symptoms of intense sleep deprivation, as if a person had missed several nights of monophasic sleep in a row. Even after adaptation, there is still a risk of oversleeping, and possibly maintaining an alarm system indefinitely.
, as in the case of daytime sleep modes, Uberman prevents the removal of the brain through [[wikipedia: glimphatic System | minutes. Therefore, it is currently unknown what impact Uberman has in the long run, especially for those with an average need for SWS.
Therefore, it is currently unknown what impact Uberman has in the long run, especially for those with an average need for SWS.
As with other daytime sleep patterns, Uberman prevents the removal of brain waste through the [[Wikipedia:glymphatic system|glymphatic system]] because NEPs last only 20 minutes. Therefore, it is currently unknown what impact Uberman has in the long run, especially for those with an average need for SWS.
==Research==
To date, there has been only one official study of Uberman, motivated by its creation of Puredoxyk and its widespread practice over decades. In 2013, research focused on the endocrine and cognitive effects of the Uberman regimen. This study > https://www.researchgate.net/publication/315334680_Endocrine_and_cognitive_effects_of_a_radially_polyphasic_sleep_schedule<
This study sheds light on the ability to support Uberman long-term and its impact on the overall well-being of polyphasic people.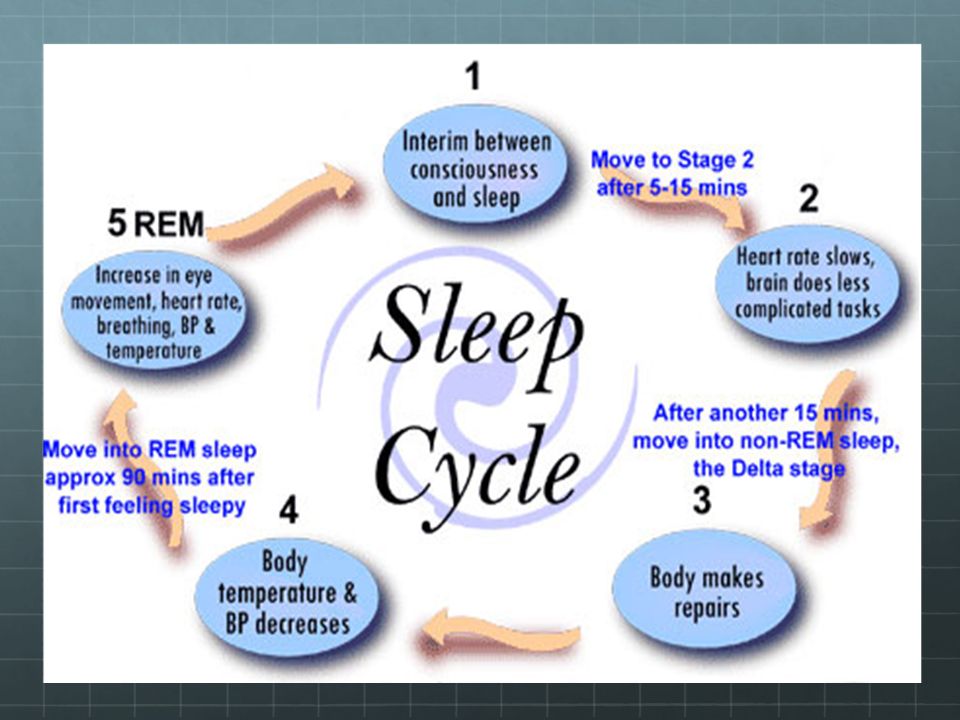 It is noteworthy that most of the subjects left the experiment by the 3rd week due to social life, and not because of debilitating adaptation, and one subject lasted until the end of the 5-week experiment. These participants were monitored 24 hours a day and woken up when needed.
It is noteworthy that most of the subjects left the experiment by the 3rd week due to social life, and not because of debilitating adaptation, and one subject lasted until the end of the 5-week experiment. These participants were monitored 24 hours a day and woken up when needed.
/282064
{{cite journal |vauthors=Rak M, Kunath N, Breitenstein B, Pawlowski M, Steiger A, Dresler M |date=2013 |title=Endocrine and cognitive effects of a radically polyphasic sleep schedule |journal=Pharmacopsychiatry |volume=46 |issue=6 |doi=10.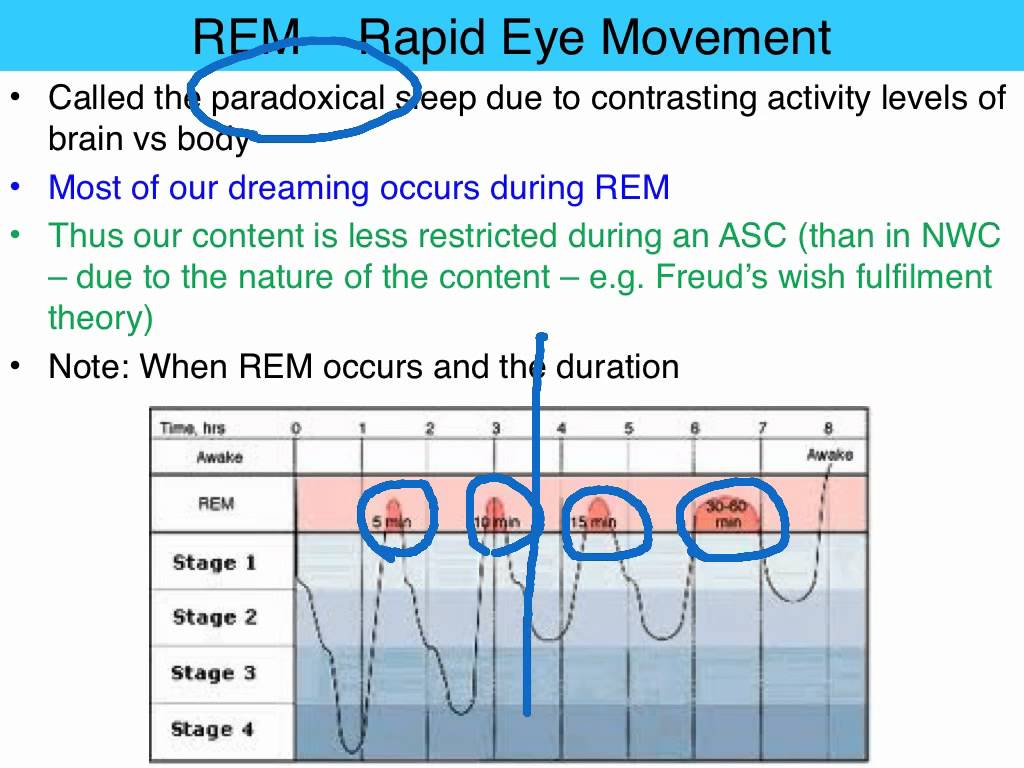
Learn more