Help depressed loved one
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 03/22/2023
Help and support for a person with depression
Among relatives and friends of any person, people suffering from depression can meet. The help and support that a healthy person can provide to another person tormented by a depressive disorder is invaluable; the main thing is to do it as efficiently as possible and at the same time avoid common mistakes.
Contents
- 10 tips for helping a loved one with depression
- What not to do
- When intervention is needed
- Crisis Support
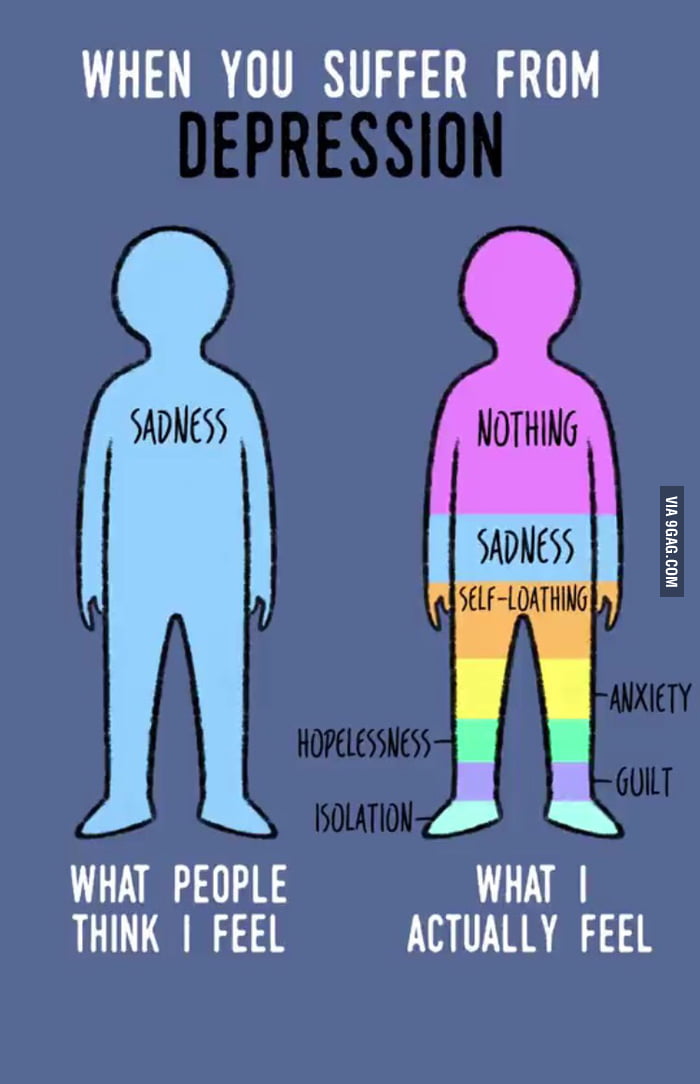
According to the National Institute of Mental Health, more than 300,000,000 adults and children worldwide are living with depression worldwide. But not everyone experiences depression in the same way, and symptoms can vary from person to person.
But not everyone experiences depression in the same way, and symptoms can vary from person to person.
If your friend or relative has a real depressive disorder, they may have specific symptoms, such as:
- the person becomes sad, tends to cry;
- depressed people seem more pessimistic than usual, or who have lost all hope of the future;
- the patient often begins to talk about his feelings of guilt, spiritual emptiness or his own worthlessness;
- people with depression lose interest in communicating with others, begin to seek loneliness;
- such patients are easily upset or become extremely irritable;
- their general tone decreases, patients move slowly or seem to be generally limp;
- they lose interest in their appearance or neglect basic hygiene, such as regular showering and brushing their teeth;
- depressed patients have trouble sleeping or sleep much more than usual;
- patients care much less about their usual activities and interests;
- they become forgetful, have trouble concentrating or problem solving;
- depressed patients often eat more or less than usual;
- is often spoken of as death or suicide.
Below are 10 tips for helping a loved one with depression, as well as a few tips on what to avoid when dealing with someone with depression.
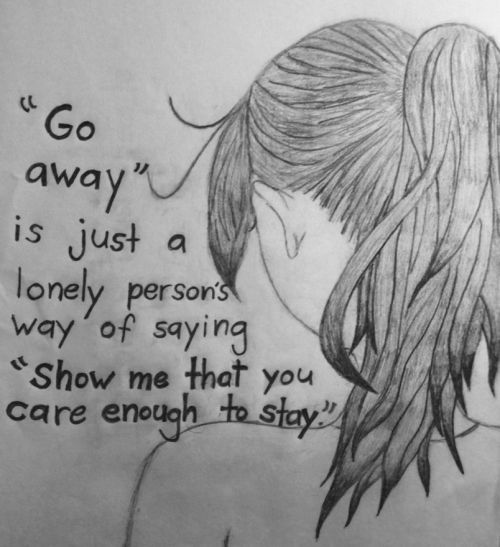
1. The importance of listening to others
Tell a friend or loved one that you would like to help him or her in some way. You can start a conversation by sharing your own concerns and asking a specific question. For example: “You seem to be having a hard time lately. What happened that worries you? Keep in mind that your friend may really want to talk about how he feels, but at the same time, he may not want advice from others. A simple tactic of talking with the patient will help to better understand his condition, his mental problems:
- Ask questions to get more information, instead of "thinking out" what the patient's messages mean.
- Make it clear to the interlocutor that you are dealing with his problems. You might say, “It really does sound like you have a problem. I'm sorry to hear it".

- Show empathy and concern with your body language, that is, with appropriate movements and gestures. Your friend may not feel like being open about their problems right away, so it's worth continuing to talk to them about your concerns and desire to help from time to time. Keep asking open-ended questions (without being too pushy) and express your concerns. Try to keep conversations exclusively in private, tête-à-tête, whenever possible. If you live in different regions, try video chatting.
2. Help the person find qualified support
Your friend or relative may not know they are dealing with depression or may not be sure where or how to seek help. Even if he understands that therapy can help him solve problems, he may hesitate to start looking for a doctor and visit him for a long time. If your friend is interested in counseling, offer to help them find potential therapists. You can help your friends or loved ones make a list of questions to discuss with the doctor and identify the most pressing issues that they should definitely remember during the first visit. Encouraging and supporting the patient in finding a doctor and scheduling a date/time visit to his office is of great importance for the success of the treatment, especially when the patient does not dare to do it on his own.
Encouraging and supporting the patient in finding a doctor and scheduling a date/time visit to his office is of great importance for the success of the treatment, especially when the patient does not dare to do it on his own.
3. About supporting the patient during the course of therapy
On a particularly difficult day, your friend may not even feel like leaving the house. Depression can drain energy and increase the desire to self-isolate. If a friend or loved one starts saying things like, "I don't think I'll be going to psychotherapy anymore," start encouraging them to keep going.
You might say, “Last week you said that the treatment session was really productive, and after that you felt much better. What if today's session also significantly improves your condition?
The same applies to drugs. If your friend wants to stop taking medication because of unpleasant side effects, encourage him not to break his prescribed medication regimen, but at the same time start encouraging him to talk to his psychiatrist about switching to another antidepressant or stopping the drugs completely. Abruptly stopping antidepressants without permission/supervision from a healthcare professional can have serious consequences.
Abruptly stopping antidepressants without permission/supervision from a healthcare professional can have serious consequences.
4. Don't forget to take care of yourself too
When you are caring for someone who is living with depression, it is tempting to drop everything to be close to the person who is depressed and provide them with all kinds of support. If you want to help a friend, it's a noble gesture, but it's also important to take care of your own needs. If you begin to give all your energy to support a friend or loved one, you will have very little self-care left. And if later you start to feel "burnt out" or exhausted, this will not help your friend much.
Benefits of setting boundaries in communication
Setting boundaries can help you maintain your strength. For example, you can tell your friend that you can talk to him when you get home from work, but not before. If you're worried that a loved one or friend will worry about not being able to contact you, offer to help them come up with a contingency plan should they need to communicate with you during the work day. This may include looking up a hotline number they can call or a code word they can send you in a text message if they have a moment of crisis. You can suggest to the patient that you will visit him every other day or have lunch or dinner with him twice a week, instead of trying to help daily. Inviting other friends can help build a great support network.
This may include looking up a hotline number they can call or a code word they can send you in a text message if they have a moment of crisis. You can suggest to the patient that you will visit him every other day or have lunch or dinner with him twice a week, instead of trying to help daily. Inviting other friends can help build a great support network.
Take care of your own emotions
Spending a lot of time with a loved one who is depressed can cause emotional loss. Determine your limits on experiencing difficult emotions and make sure you have the time and opportunity to regenerate your soul. If you need to let your friend know that you will be unavailable for a short period of time, you can say something like, “I can't talk on the phone at certain times. But then I will definitely call you.
5. Raise your own awareness of depression
Imagine having to educate every person in your life about your mental or physical health problems - explaining it over and over again. It would become too exhausting for you. You can talk to your friend about his specific symptoms or how he is feeling, but avoid asking him to tell you about depression in general. Read on your own about depression symptoms, causes, diagnostic criteria, and treatments.
It would become too exhausting for you. You can talk to your friend about his specific symptoms or how he is feeling, but avoid asking him to tell you about depression in general. Read on your own about depression symptoms, causes, diagnostic criteria, and treatments.
Although people experience depression differently, becoming familiar with common symptoms and terminology can help you have deeper conversations with your friend.
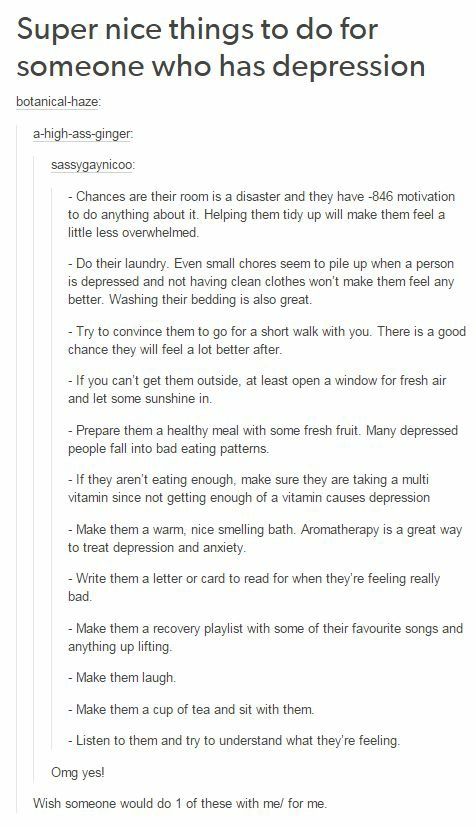
6. Offer help with daily life
Depression can make daily tasks seem overwhelming. Really simple things like doing laundry, grocery shopping, or paying bills can get left undone and start to pile up, and it ends up making it really, really hard to decide where to start. Your friend may appreciate the offer of help, but at the same time, it is also possible that he will not be able to clearly say what exactly he needs help with. So instead of telling the patient, "Let me know if I can do something," you should ask him, "What exactly do you need help with most today?" If you notice his fridge is empty, say, "Can we go shopping together, or will I buy what you need if you write me a list?" A perfectly acceptable option is: "Let's go grocery shopping and cook dinner together. "
"
If your friend has stopped doing the dishes, if he has a lot of dirty laundry or other unfinished household chores, call him, turn on the music and do the work together. Your presence and assistance will make it easier for him to do the job and it will not be given to him by an impossible task.
7. Inviting guests can improve the mood of the patient
People living with depression may find it difficult to maintain relationships with friends and make plans for the future or stick to them. But canceling plans can contribute to the feelings of guilt that are common in those who suffer from depression. Refusal of invitations can lead to a decrease in their number, and this can increase the patient's self-isolation. This in turn can worsen the symptoms of depression. You can help put your friend at ease by continuing to send out invitations to visit, even if you know for sure that he's unlikely to have to. Tell him that you understand that he may not follow through when he is especially depressed and there is no pressure on your part for him to come over until he is in the mood to do so. Just remind a friend or relative that you are always happy to see them whenever they feel like it.
Just remind a friend or relative that you are always happy to see them whenever they feel like it.
8. Be patient
Depression usually improves with treatment, but it can be a slow process that usually involves trial and error. Your friend and doctor may need to try several different approaches to counseling or medication before they find the best option. Even successful treatment does not always mean that depression is completely gone. Your friend may still have symptoms from time to time. Because of this, he will have good days and bad days - that is, days with a more or less normal or depressed mood. Avoid assuming that a good day means the friend is "completely cured" and try not to get frustrated if a series of bad days gives the impression that your friend's condition will never get better. Depression has no clear recovery timeline. Expecting your friend to return to their normal self after a few weeks of therapy is not a realistic approach to this illness.
9.
 Stay in touch
Stay in touch Reminding your friend that you care about them can help improve outcomes. Even if you can't spend a lot of time with your friend on a regular basis, keep in touch with them regularly via text, phone, or short visits to their home. Just by sending a short text with the message: “I think of you and care about you”, you can significantly improve your mood. People who live with depression may become more withdrawn and avoid socializing, so you may find that the situation requires you to make more efforts to maintain friendships. But the fact that you continue to be present in your friend's life as a positive character can go a long way towards improving his condition. Remind yourself regularly to your friend during his treatment for depression.
10. Depression can come in many forms
Depression often involves sadness or low mood, but it has other, less well-known symptoms. For example, many people do not realize that depression can have the following manifestations:
- temper tantrums and irritability;
- confusion, problems with memory or concentration;
- excessive fatigue or trouble sleeping;
- physical symptoms such as indigestion, frequent headaches, or pain in the back and other muscles.
Your friend may often be in a bad mood or feel exhausted for a long time. Try to understand that what he is feeling is still part of the depression, even if the symptoms do not fit into the stereotypical manifestations of this illness. Even if you don't know how to help your friend feel better, just tell them, “I'm sorry you're feeling bad. I'm here to help you if there's anything I can do" and maybe that will help.
What not to do
1. Don't take things too personally
Your friend's depression is not your fault, nor is it his fault. Try not to let it affect you if he seems to lash out at you in anger or frustration, keeps canceling plans (or forgets to follow up), or avoids a lot of work. You may need to take a break from your friend at some point. It's okay if you're feeling emotionally drained, but it's also important to avoid blaming your friend or saying things that might contribute to negative feelings. Instead, consider talking to a therapist or other person about how you feel.
2. Do not try to correct the patient's behavior
Depression is a serious mental health disorder that requires professional treatment. It is difficult for a person who has never had depression to understand exactly what the patient feels. Clinical depression is not just a mood swing that can be improved with phrases like "you should be grateful for the good things in your life" or "just stop thinking about the sad things." If you don't want to say something vulnerable to someone who is living with a severe physical illness like diabetes or cancer, you probably shouldn't say that kind of thing to your friend with depression either. Positive support can let your friend know that they really matter to you.
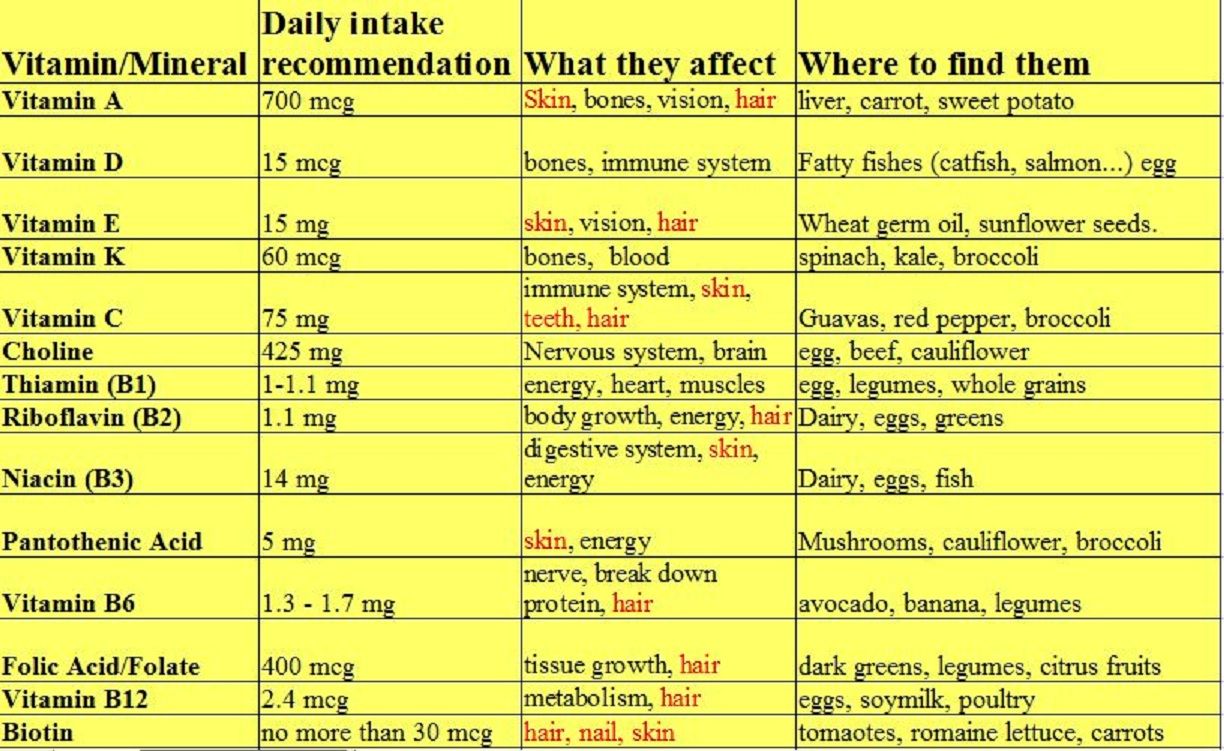
3. Don't give unsolicited advice
While certain lifestyle changes often improve symptoms of depression, making these changes is difficult in the midst of a depressive episode. You may want to help a friend by offering advice, such as exercising more or eating healthier foods. But, even if it's good advice, your friend may not want to listen to it at the moment. There may come a day when your friend wants to find out what foods can help with depression or how exercise can relieve symptoms. However, by this time, it may be best to stick to empathic listening and avoid offering advice unless he asks for it. Encourage positive change by taking a depressed friend out for a walk or cooking delicious meals together.
But, even if it's good advice, your friend may not want to listen to it at the moment. There may come a day when your friend wants to find out what foods can help with depression or how exercise can relieve symptoms. However, by this time, it may be best to stick to empathic listening and avoid offering advice unless he asks for it. Encourage positive change by taking a depressed friend out for a walk or cooking delicious meals together.
4. Don't belittle the patient's symptoms
If your friend is talking about depression, you can say something like, "I understand" or "We've all been through this." But if you've never dealt with depression, it can reduce your empathy to a minimum. Depression goes beyond just feeling sad or depressed. Sadness usually goes away fairly quickly, while depression can linger and affect mood, relationships, work, school, and every other aspect of life for months or even years. Comparing what a depressed person is going through to other people's troubles, or saying things like, "But it could have been a lot worse," usually doesn't help. Your friend's heartache is what is real to him. Say something like, “I can't imagine how hard it is to deal with this. I know I can't make you feel better, but remember that you are not alone."
Your friend's heartache is what is real to him. Say something like, “I can't imagine how hard it is to deal with this. I know I can't make you feel better, but remember that you are not alone."
5. Don't comment on prescription medications
Medicines can be very helpful for depression, but they are not for everyone. Some people have a very hard time with the side effects of antidepressants and prefer to treat their depression with psychotherapy or natural products. Even if you think your friend should be taking an antidepressant, remember that medication choice is a personal decision. Also, if you personally do not believe in medicines, avoid discussing this when talking to the sick. For some people, medication is the only way to start the steps towards recovery. In the end, whether or not to take antidepressants is a very personal decision for the patient, which he usually has to make on his own after a detailed conversation with the doctor.
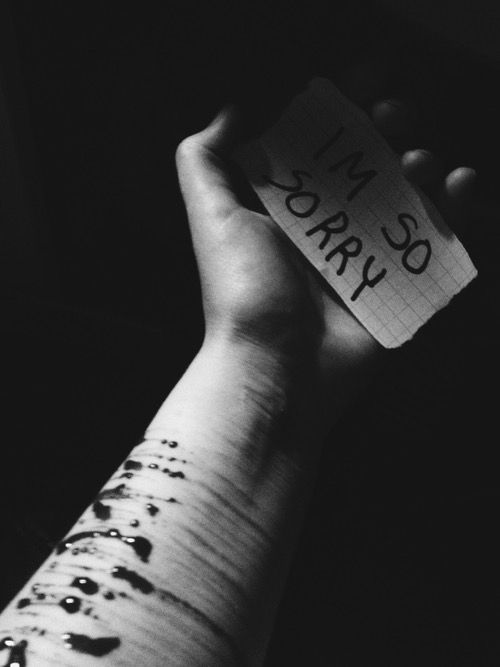
When Intervention Is Necessary
Depression can increase a person's risk of suicide or self-harm, so it's good to know how to recognize the danger signs. Below is a list of some of the signs that may indicate the presence of suicidal thoughts:
Below is a list of some of the signs that may indicate the presence of suicidal thoughts:
- frequent mood or personality changes;
- talk or death;
- acquisition of weapons;
- increase in alcohol consumption or initiation of drug use;
- risky or dangerous behaviour;
- disposal of own belongings or distribution of property;
- talking about feelings of being trapped or wanting to end all problems at once;
- self-isolation;
- too expressive farewell after each meeting.
If you think your friend is thinking about suicide, ask him to call his therapist while you are with him, or ask your friend for permission to call his doctor instead.
Crisis Support
You can also take your friend to a mental health emergency room. If possible, stay with him until he has no more suicidal thoughts. Make sure he can't access weapons or drugs. If you're worried about your friend's mental state, you might start to worry that mentioning it might make them think about suicide. But in general it will be useful to discuss this complex situation. Ask your friend if he is seriously considering suicide. He may be tempted to talk to someone about it, but he doesn't know how to start a conversation on such a difficult topic. Encourage your friend to talk to their therapist about these thoughts if they haven't already. Invite a friend to help you create a special safety plan (crisis plan) that he can use in case of obsessive thoughts about suicide.
But in general it will be useful to discuss this complex situation. Ask your friend if he is seriously considering suicide. He may be tempted to talk to someone about it, but he doesn't know how to start a conversation on such a difficult topic. Encourage your friend to talk to their therapist about these thoughts if they haven't already. Invite a friend to help you create a special safety plan (crisis plan) that he can use in case of obsessive thoughts about suicide.
Electronic source:
https://www.healthline.com/health/how-to-help-a-depressed-friend
to the list of articles Know the doctor
Support for a partner with depression
11/22/2019
Depression is one of the most common mental disorders, affecting more than 350 million people of all age groups.
Annually about 150 million people worldwide are disabled by depression
The support of family and friends is essential in the treatment of mental disorders. However, depression can negatively impact relationships and leave loved ones feeling helpless, frustrated, or afraid.
However, depression can negatively impact relationships and leave loved ones feeling helpless, frustrated, or afraid.
There are ways people can support a partner with depression on their journey to recovery.
Questions to ask about symptoms
To understand the severity of a person's depression, it is helpful to study how these symptoms affect their life.
Asking about symptoms also shows a person that his partner is interested in his feelings and experiences.
Useful questions to ask include:
- Can you help me understand how you feel?
- What activities do you find enjoyable right now?
- Do you enjoy spending time with other people?
- What's wrong with your energy?
- Do you sleep more or less than usual?
- Do you eat more or less than usual?
- Can you focus on things right now?
- Do you have thoughts of death or suicide?
Questions to avoid
Avoid asking questions that seem judgmental or that place blame on the person with depression. They may already be blaming themselves for their symptoms and need support rather than further judgment.
They may already be blaming themselves for their symptoms and need support rather than further judgment.
It is also important not to oversimplify depression, which is a serious illness.
Examples of questions to avoid include:
- Why can't you just cheer up?
- Don't I make you happy?
- When will you feel better?
- Don't you realize that it's all in your head?
- Why do you attach such importance to this?
- Do you know that others are in a much worse situation than you?
Partner support
1. Learn about depression
Learning about depression can make it easier to support those with depression. Learning about symptoms often helps people recognize symptoms in their loved ones.
Symptoms can range from mild to severe and may change over time. However, symptoms must last at least 2 weeks before a doctor can diagnose depression.
Symptoms of depression may include:
- feelings of sadness, worthlessness or guilt
- loss of interest in previously enjoyable activities
- changes in appetite or weight
- changes in sleep habits
- fatigue and loss of energy
- difficulty concentrating or making decisions
- thoughts of death or suicide
2. Understand and acknowledge your partner's feelings
It is important to listen to a person with depression and express empathy, which is the ability to understand and share other people's feelings. One way to show empathy is to mirror what the person is saying.
For example, if he says, "I just feel like things will never get better," their partner might reflect this by saying, "that sounds like you're not looking forward to the future."
Constant attempts to cheer up a person are useless, as this devalues his condition and feelings. Phrases like “tomorrow will be better” or “try to cheer up” do not take into account the nature of the disease.
Phrases like “tomorrow will be better” or “try to cheer up” do not take into account the nature of the disease.
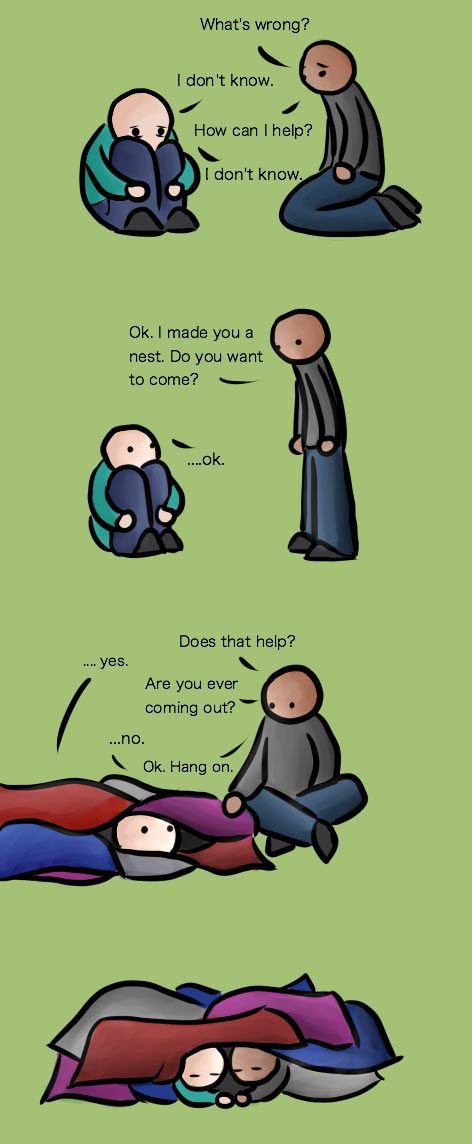
3. Ask your partner what they want from you
To show further understanding and support, ask the person what they need. He may need:
- medication reminders
- company when visiting a doctor or visiting therapy
- homemade meals
- encouragement to socialize or exercise
- hug or hold hands
- to be left alone sometimes
Useful questions to ask include:
- How can I help you?
- Would it be helpful if I...?
4. Encourage your partner to heal
Depression can cause a person to lose their motivation, which can be a barrier to seeking treatment. However, most people with depression need treatment to get better.
Those who support someone with depression can play an important role in their recovery by encouraging them to seek medical help.
To inspire a partner to seek treatment, a person can try:
- joint detection and documentation of your partner's symptoms
- expression of desire to help
- discussion of treatment options such as medication, psychotherapy and lifestyle changes
- accompaniment to doctor appointments
5. Support your partner during recovery
Recovery from depression can sometimes be difficult. To support a partner in the recovery process:
- help them keep track of their prescriptions and medications
- do some physical exercise together
- plan and prepare healthy meals together
- try to reduce stressors at home
- make your goals small and achievable
- encourage them to associate with other people
- plan fun activities together
- pay attention to the person's progress towards recovery
- avoid forcing treatment on the person
Let your partner know they are not alone when you say:
- I'm here for you.
- We'll deal with this together.
6. Accept that there will be bad days
People with depression have good days and bad days. To cope with bad days:
- expect them to happen
- understand that this is a normal part of depression
- don't give up love and support at this time
- take some time and do something nice, either alone or with others
- remember that not every day will be like this - there will be good days
7. Take care of yourself
When a person supports a partner with depression, it is very important to take the time to enjoy hobbies and other activities for yourself.
Caring for a partner with depression can be draining, frustrating, and intimidating.
Research shows that having a spouse with depression increases a person's risk of developing depressive symptoms. This risk is especially high when a man is supportive of a depressed woman.
Those caring for someone with a mental illness should also take care of their own mental health. They can do it:
- trying to stay positive
- having realistic expectations about the recovery process
- knowing that they also have the right to be heard and respected
- taking time out and doing pleasurable activities and hobbies
- interacting with other people besides their partner
- seeking help from friends or relatives
- doing regular exercise
- eating healthy
- trying to get more sleep and rest
- visiting a psychologist or psychological support groups
Professional support
Professional treatment is an important part of the recovery process. The first step is often to see a doctor, who can recommend treatment, psychotherapy, or both.
For particularly severe depressive symptoms or in life-threatening situations, seek emergency care.
Beginning of form
People with depression may be at risk of suicide. According to the American Foundation for Suicide Prevention, more than half of those who die by suicide suffer from major depression.
Partners of those who suffer from depression should be aware of the warning signs of suicide so that they can take prompt action if necessary. Warning signs include:
- talking about death or suicide
- having a suicide plan
- preparation of means of suicide, e.g. collection of pills
- preparation for death, e.g. by making a will
- distribution of things
- farewell to family and friends
- engaging in risky or reckless behavior
- extreme changes in mood or personality
- withdrawal from society
If a person suspects that someone is in imminent danger of suicide, they should seek emergency help.
If someone believes that a loved one is contemplating suicide but is not in immediate danger, they should contact the person's doctor and seek support from other family members or a support group.