Dsm v substance use disorder criteria
Table 3, DSM-5 Diagnostic Criteria for Diagnosing and Classifying Substance Use Disorders [abc] - Substance Use Screening and Risk Assessment in Adults
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
McNeely J, Adam A. Substance Use Screening and Risk Assessment in Adults [Internet]. Baltimore (MD): Johns Hopkins University; 2020 Oct.
Show details
Table 3DSM-5 Diagnostic Criteria for Diagnosing and Classifying Substance Use Disorders [
a,b,c]Abbreviations: DSM-5, Diagnostic and Statistical Manual of Mental Disorders–5; PCP, phencyclidine; SUD, substance use disorder.
Notes:
- a
Adapted from [APA 2013].
- b
SUDs are classified as mild, moderate, or severe based on how many of the 11 criteria are fulfilled: mild, any 2 or 3 criteria; moderate, any 4 or 5 criteria; severe, any 6 or more criteria.
- c
Please consult the DSM-5 for substance-specific diagnostic information.
From: Substance Use Screening and Risk Assessment in Adults
Copyright © Johns Hopkins University HIV Clinical Guidelines Program 2000-2020. All Rights Reserved. The use, reproduction, and distribution of original documents and related graphics from this web site is encouraged provided that full credit of source accompanies all uses, in all forms. Please note that if we have adapted or reproduced copyrighted material from another source, with permission, we cannot extend permission to reproduce. Links to pages on this site are also encouraged and may be created without seeking permission.
This book is licensed under the terms of the Attribution-NonCommercial-NoDerivs 3.0 Unported (CC BY-NC-ND 3.0).
- Cite this Page
- PDF version of this title (732K)
Other titles in this collection
- New York State Department of Health AIDS Institute Clinical Guidelines
Similar articles in PubMed
- Review Substance Use Disorder Treatment in Pregnant Adults[ 2021]
- Review Treatment of Alcohol Use Disorder[ 2020]
- Review Therapeutic Use of Medical Cannabis in New York State[ 2022]
- Review Prevention and Management of Hepatitis A Virus in Adults With HIV[ 2021]
- Review Comprehensive Primary Care for Adults With HIV[ 2021]
See reviews...See all...
Recent Activity
ClearTurn OffTurn On
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
See more...
DSM-5 and Addiction — Understanding Changes Over Time
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is a vital diagnostic tool published by the American Psychiatric Association.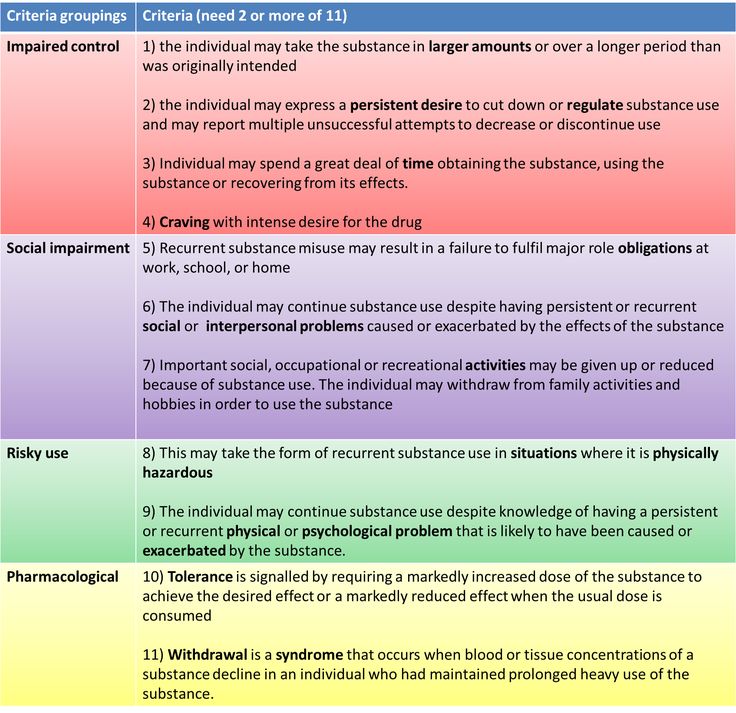 This text is considered the gold standard on mental health and influences how disorders are investigated, diagnosed and treated — including addiction. DSM-5 is the fifth edition, which was updated in 2013 with input from the top experts in the mental health field.
This text is considered the gold standard on mental health and influences how disorders are investigated, diagnosed and treated — including addiction. DSM-5 is the fifth edition, which was updated in 2013 with input from the top experts in the mental health field.
This latest version improves the DSM’s approach to substance use disorders. No longer is addiction divided into two vague and ill-defined disorders — substance dependence and abuse. Instead, DSM-5 focuses less on withdrawal and more on 11 criteria, or symptoms, that characterize the severity of an individual’s addiction. Let’s explore how these features can better help healthcare professionals recognize and address addiction.
Download Info Sheet
DSM-5’s 11 Criteria for Addiction
According to DSM-5, a substance use disorder (SUD) involves patterns of symptoms caused by using a substance that an individual continues taking despite its negative effects. Based on decades of research, DSM-5 points out 11 criteria that can arise from substance misuse.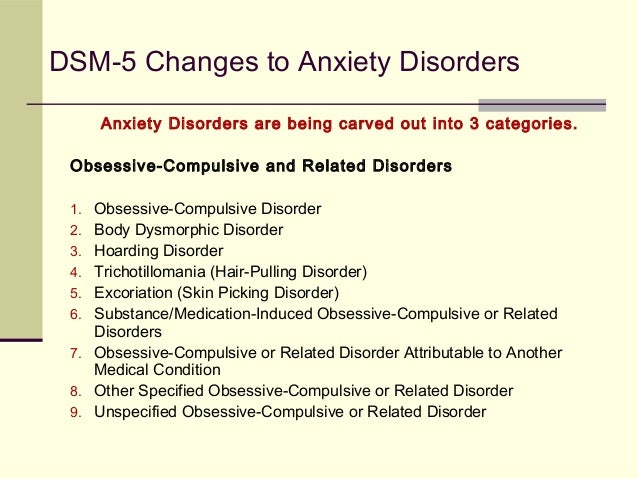 These criteria fall under four basic categories — impaired control, physical dependence, social problems and risky use:
These criteria fall under four basic categories — impaired control, physical dependence, social problems and risky use:
- Using more of a substance than intended or using it for longer than you’re meant to.
- Trying to cut down or stop using the substance but being unable to.
- Experiencing intense cravings or urges to use the substance.
- Needing more of the substance to get the desired effect — also called tolerance.
- Developing withdrawal symptoms when not using the substance.
- Spending more time getting and using drugs and recovering from substance use.
- Neglecting responsibilities at home, work or school because of substance use.
- Continuing to use even when it causes relationship problems.
- Giving up important or desirable social and recreational activities due to substance use.
- Using substances in risky settings that put you in danger.
- Continuing to use despite the substance causing problems to your physical and mental health.
3 Levels of Severity
Like other illnesses, substance misuse worsens over time. The substance use disorder criteria explained in the DSM-5 allow clinicians to determine how severe a substance use disorder has become depending on how many symptoms are present. For example:
- One symptom could indicate an individual is at risk.
- Two or three criteria point to a mild substance use disorder.
- Four or five symptoms show someone has a moderate substance use disorder.
- Six or more criteria indicate a severe substance use disorder, which signals an addiction to that substance.
Knowing how severe a substance use disorder is can help physicians and addiction specialists determine the best course of treatment for the individual struggling with substance misuse.
Find Evidence-Based Care for Addiction
If you recognize any of these criteria in yourself or someone you care for, it’s time to get help before you’re trapped in a cycle of full-blown addiction.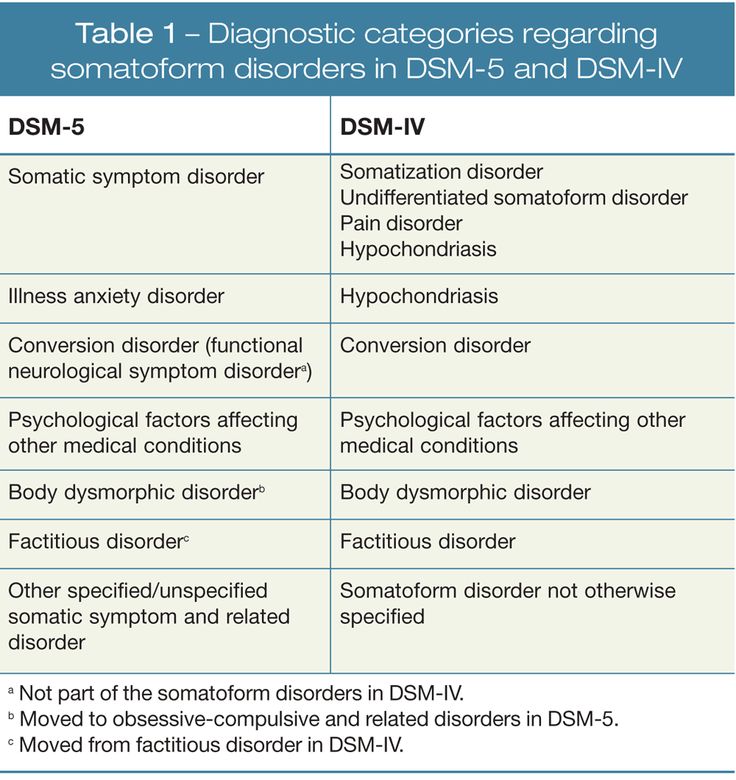 At Gateway Foundation, we use a medical, evidence-based approach that relies on the latest addiction treatment options and advanced therapies to help you find long-term success in recovery. If you would like to learn more, please contact us today.
At Gateway Foundation, we use a medical, evidence-based approach that relies on the latest addiction treatment options and advanced therapies to help you find long-term success in recovery. If you would like to learn more, please contact us today.
Call Gateway for Help
What role do the DSM-5 criteria for substance use and addictive disorders play in diagnosing addiction? | Addiction & Recovery articles | Emotional & Mental Health center
Although the DSM-5 lists numerous different addictions, their diagnostic criteria are very similar - because addictions affect a person's life and behavior in the same way, regardless of substance or behavior. What should you know?
Addiction is an insidious disease that can start with a number of options, but then take over the brain - and depending on what you are addicted to, and sometimes the body. Once you're in the clutches of an addiction, the all-encompassing call for more drugs, alcohol, gambling, shopping, food, sex, or whatever you're used to becomes almost impossible to refuse.
The American Society for Addiction Medicine describes addiction as a chronic and often progressive disease that may include periods of remission and relapse. We now know that becoming an addict is not a moral failing or a permanent choice. Once you are addicted, your addiction robs you of much of your control.
Addiction can be a serious disease, but it is indeed treatable. This treatment can take many forms, but it starts with the decision that you are ready to go into remission. If you're an addict, you've likely tried - and ultimately failed - to stop using the substance or stopped participating in the behavior multiple times and realized that professional help would be needed to break your chains. nine0003
This help starts with a diagnosis, and in the US, clinicians will use the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition - DSM-5 for short - to determine if you have an addiction and how severe it is.
What do drug addicts and their loved ones need to know about the diagnostic criteria for DSM-5 addiction?
The DSM-5 is an incredibly long document filled with diagnostic criteria for many different mental and cognitive disorders, from depression to autism spectrum disorder and schizophrenia to narcissistic personality disorder. Addiction is described in the chapter on Substances and Dependence Disorders. This chapter covers many different addictions, including alcohol, tobacco, opioids, sedatives, sleeping pills, cannabis, and even caffeine. It also includes gambling, but has a strong addiction to psychoactive substances and is rather devoid of behavioral addictions. nine0003
Addiction is described in the chapter on Substances and Dependence Disorders. This chapter covers many different addictions, including alcohol, tobacco, opioids, sedatives, sleeping pills, cannabis, and even caffeine. It also includes gambling, but has a strong addiction to psychoactive substances and is rather devoid of behavioral addictions. nine0003
DSM-5 includes those passions that were backed by hard science at the time of publication. Not all addictions described in the medical literature, such as addictions to food, shopping, sex, gaming, and Internet use, are official diagnostic categories in the DSM-5. If you are (as you think) addicted to something that is not covered in this document, you can still get the help you need. If something is not in the DSM-5, it does not mean that it does not exist. nine0003
Look at the Diagnostic Criteria for Addiction
When you look at the diagnostic criteria for all the different addictions included in the DSM-5, you will begin to realize that they are all pretty similar - no matter what substance or behavior is being discussed in the document. We will make these diagnostic criteria more general so that you can get a general picture of the types of symptoms that signify addiction. Since the DSM-5 mainly deals with substance addiction, we will refer to "substance" - but very similar symptoms will be seen among people suffering from behavioral addictions. nine0003
We will make these diagnostic criteria more general so that you can get a general picture of the types of symptoms that signify addiction. Since the DSM-5 mainly deals with substance addiction, we will refer to "substance" - but very similar symptoms will be seen among people suffering from behavioral addictions. nine0003
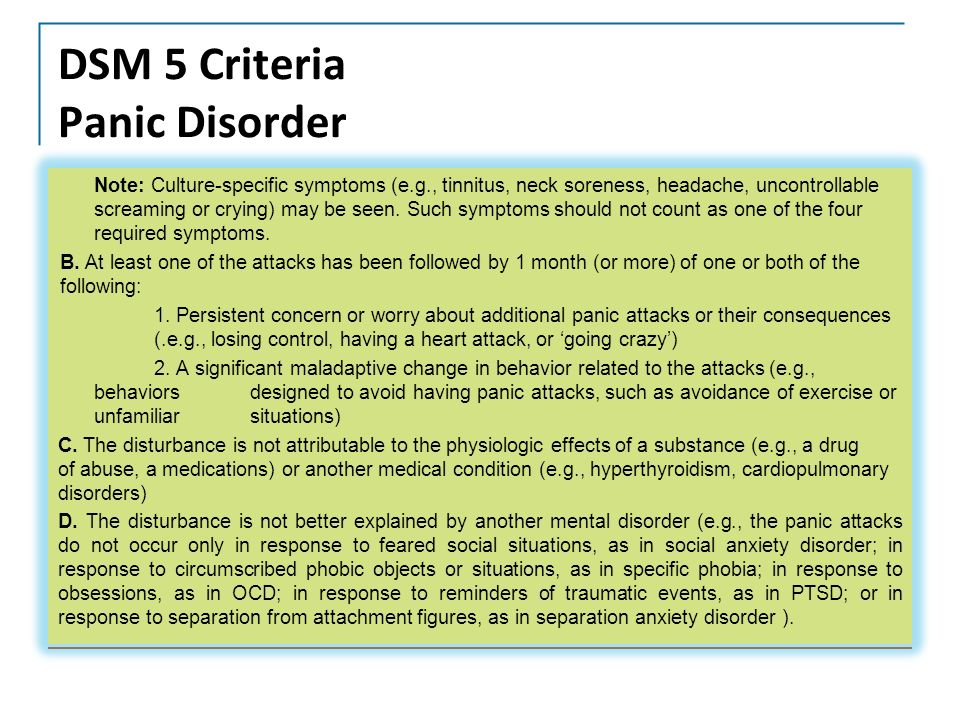
First of all, the DSM-5 will require that at least two of the symptoms be present for one year resulting in significant distress or aggravation:
- The person uses more of the substance, or longer, than they intended.
- The person wants to reduce or stop the use of the substance, but is unsuccessful in these efforts.
- The person spends a lot of time using the substance, getting it, or recovering from it. nine0026
- The person experiences a strong craving for the substance.
- The use of a substance causes a person to fail to fulfill their important responsibilities in life.
- Substance use causes or exacerbates interpersonal problems, but does not cause the person to contract or stop.
- A person misses important events due to substance abuse.
- A person uses the substance in situations where it is physically dangerous (for example, while driving or operating heavy machinery). nine0026
Then there is tolerance - the person no longer achieves the same effect from using the same amount (or, in the case of a behavioral addiction, for example, from gambling with the same amount of money), or starts using more to return to the same effect . Finally, there is withdrawal symptoms - a person experiences withdrawal symptoms associated with the substance in question when they try to stop using the substance.
You also need to know that:
- When someone is diagnosed with an addiction, the doctor indicates how serious it is. The presence of two or three of these symptoms typically indicates a milder addiction, a score of four or five for a moderately severe addiction, and a severe addiction is marked by six or more symptoms.
- If you have used within the last year but not within the last three months, you may be diagnosed with early remission.
 If you have previously met the diagnostic criteria for any addiction but have been abstaining from use for more than a year, you are in stable remission. nine0026
If you have previously met the diagnostic criteria for any addiction but have been abstaining from use for more than a year, you are in stable remission. nine0026
While diagnostic criteria form the basis of a diagnosis, anyone an addict turns to for help doesn't just sneak down the list asking if they check the boxes. More “handy” screening tools and questionnaires can be used.
If you think you have an alcohol use disorder (alcoholism) and, for example, contact your family doctor, they may start with questions such as:
- How much do you drink and how often? nine0026
- How often do you feel guilty or remorseful after drinking alcohol?
- Have you ever drunk in the morning to be functional?
- How often were you unable to do what was expected of you because you drank?
- Has a relative or doctor expressed concern about your drinking?
- Have you ever been injured because you drank? Is there anyone else?
These questions ultimately try to determine if you meet the diagnostic criteria, but in more practical and specific terms.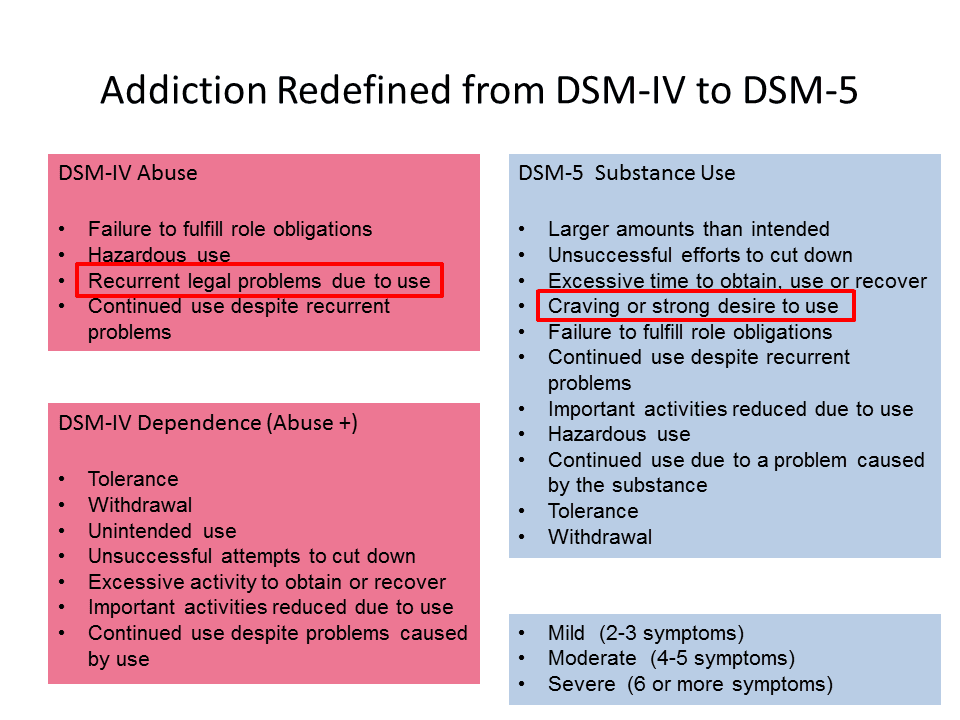 nine0003
nine0003
Determining whether you are an addict and how addicted you are is only the first step, often a very scary first step. It is, however, a step that will enable addicts to receive the help they need to achieve remission.
Therapeutic Strategies for Modification Prevention in the Dependence Syndrome Caused by the Combined Use of Psychoactive Substances: A Review of Literature Data
Currently, there is an alarming trend in the growth of polydrug addiction in the structure of which the combined use of narcotic drugs and prescription drugs predominates [1]. This trend has become clearly noticeable since the early 2000s, when reports began to appear in a number of Western European countries (Spain, France, Italy, the Netherlands, Great Britain) of an increase in the spread of polydrug addiction and an increase in the number of deaths from the use of a combination of morphine, benzodiazepine tranquilizers and alcohol. [2]. The same pattern is observed in Russia. Epidemiological data of recent years indicate that the overall incidence of polydrug addiction (F19- mental and behavioral disorders caused by the use of several psychoactive substances - PAS) are steadily growing from year to year.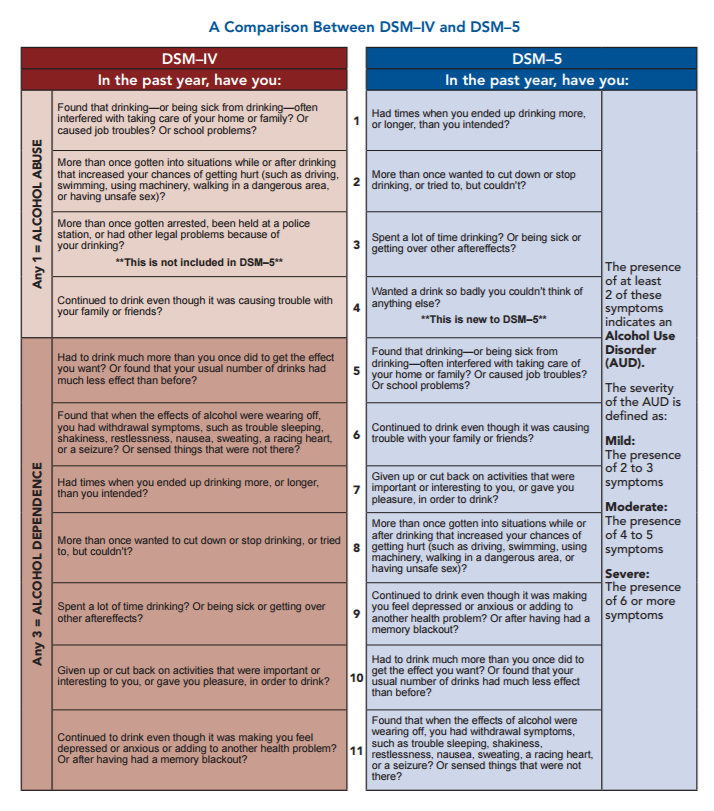 So, if we consider the structure of the incidence of drug addiction, then the proportion of patients with polydrug addiction in 2013 was 8.3%, in 2014 - 10.6%, in 2015 - 12.9%, in 2016 - 15, 8% [3–5].
So, if we consider the structure of the incidence of drug addiction, then the proportion of patients with polydrug addiction in 2013 was 8.3%, in 2014 - 10.6%, in 2015 - 12.9%, in 2016 - 15, 8% [3–5].
The increase in the proportion of polydrug addiction is one of the main trends in the modern pathomorphism of narcological diseases [2]. The reasons for the formation of polydrug addiction are different: the reduction of the euphoric effect of surfactants, which occurs during its long-term use, the initial intake of several surfactants, the vicarious use of other surfactants, which soon contributes to the formation of a syndrome of dependence on it, which eventually manifests itself as polydrug addiction. There are other reasons that are associated with the characteristics of the individual and its forms of response. nine0003
The most common patterns of polydrug addiction in Europe now include the use of heroin in combination with methadone, benzodiazepines or cocaine, cannabis, stimulants; cocaine in combination with alcohol or stimulants [2].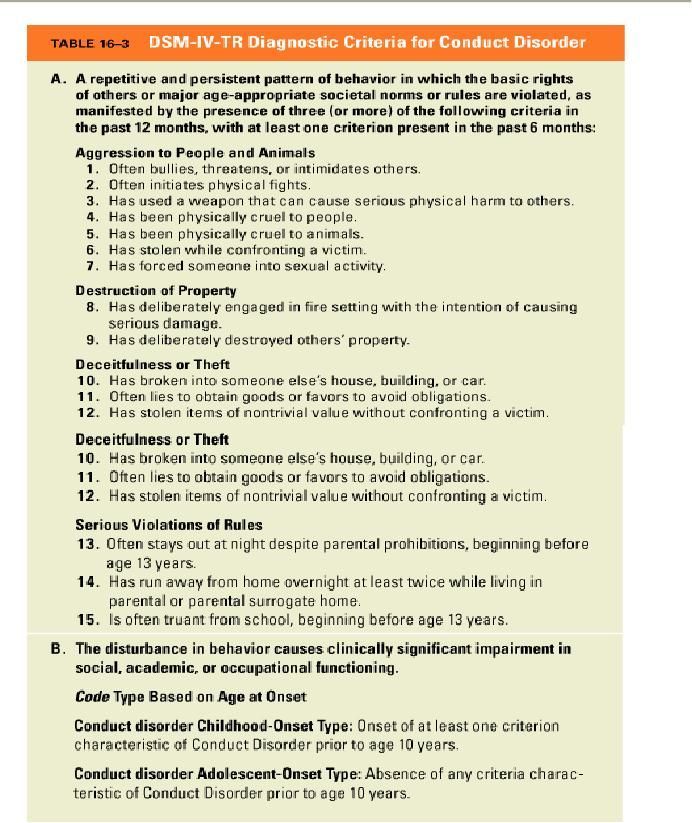 According to Spanish researchers [6], in the structure of patients who use several PASs in combination, the following picture is observed: the frequency of occurrence of combined use of cocaine and opiates is 37%, stimulants, opiates and benzodiazepines - 25.3%, opiates, cannabinoids and alcohol - 12 ,nine%, and the combination of alcohol with various surfactants occurs in 24.7% of cases.
According to Spanish researchers [6], in the structure of patients who use several PASs in combination, the following picture is observed: the frequency of occurrence of combined use of cocaine and opiates is 37%, stimulants, opiates and benzodiazepines - 25.3%, opiates, cannabinoids and alcohol - 12 ,nine%, and the combination of alcohol with various surfactants occurs in 24.7% of cases.
In the US, patterns of use are similar to those in Europe, with cannabinoids, tranquilizers and stimulants considered to be the most common PASs used in combination with opioids [7].
In Russia, the most common patterns of drug use of the opium group are in combination with prescription drugs (anticholinergics, anticonvulsants), opium group drugs in combination with amphetamine-type psychostimulants, as well as the combination of alcohol with opium group drugs and other PAS. nine0003
A factor that complicates both clinical diagnosis and treatment is the high incidence of comorbid psychiatric pathology among patients who use several PAS in combination.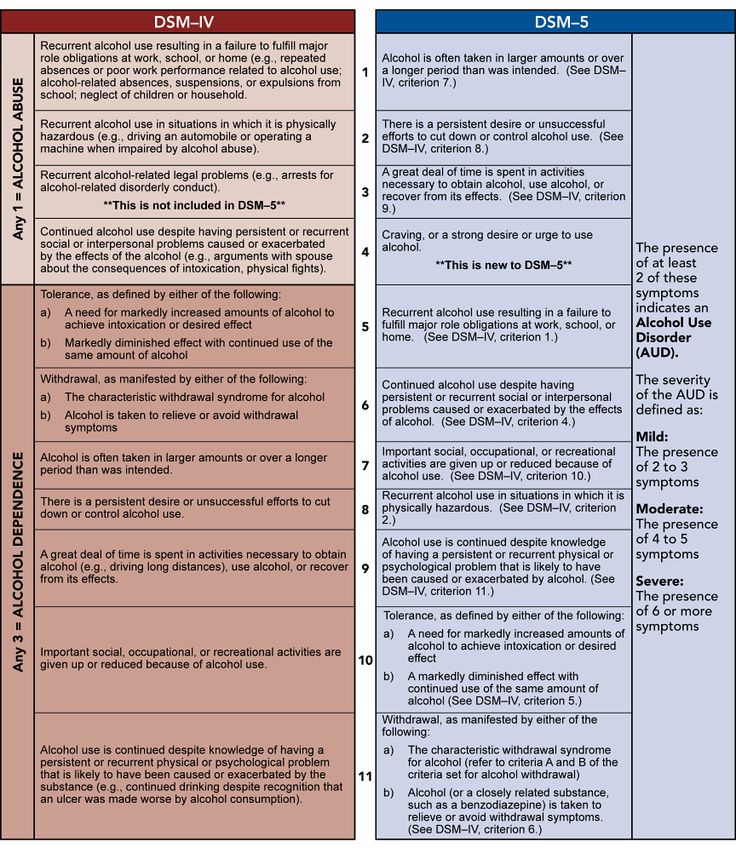 For example, in the course of scientific studies [8–10] it has been shown that in adolescence, people with polydrug addiction are more likely to be diagnosed with various forms of antisocial behavior, in adulthood, attention deficit hyperactivity disorder (ADHD), other personality disorders, anxiety and depressive disorders, endogenous mental illnesses (schizo-phrenia, schizotypal disorder, etc.). In the literature [11-13] there are also indications that in the last decade the frequency of cases of substance use among patients suffering from mental disorders has been growing, as well as the opposite situation - according to epidemiological data, schizophrenia and schizophrenia spectrum disorders (schizotypal disorder, schizoaffective psychosis) are diagnosed in 9.6% of patients with alcohol dependence and 9.4% of patients with opioid dependence.
For example, in the course of scientific studies [8–10] it has been shown that in adolescence, people with polydrug addiction are more likely to be diagnosed with various forms of antisocial behavior, in adulthood, attention deficit hyperactivity disorder (ADHD), other personality disorders, anxiety and depressive disorders, endogenous mental illnesses (schizo-phrenia, schizotypal disorder, etc.). In the literature [11-13] there are also indications that in the last decade the frequency of cases of substance use among patients suffering from mental disorders has been growing, as well as the opposite situation - according to epidemiological data, schizophrenia and schizophrenia spectrum disorders (schizotypal disorder, schizoaffective psychosis) are diagnosed in 9.6% of patients with alcohol dependence and 9.4% of patients with opioid dependence.
The questions of classification of polydrug addiction, despite their apparent simplicity, are still at the forefront of discussions in the scientific world.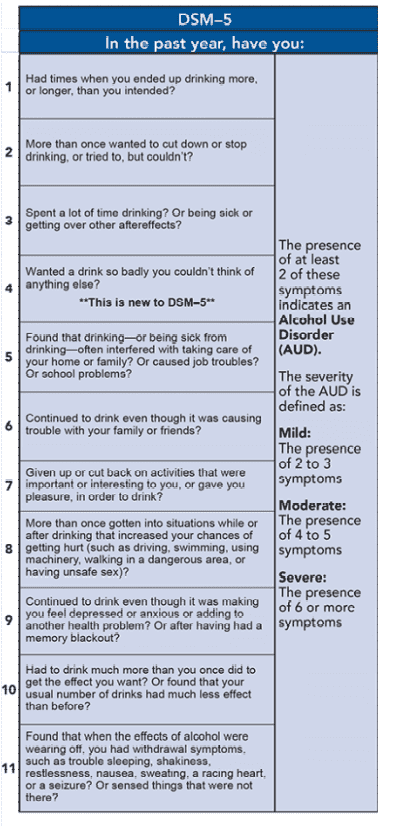 Section ICD-10 and DSM-IV "Mental and behavioral disorders caused by the combined use of drugs and other psychoactive substances" (F19) is collective. This cipher can encode the following states:
Section ICD-10 and DSM-IV "Mental and behavioral disorders caused by the combined use of drugs and other psychoactive substances" (F19) is collective. This cipher can encode the following states:
1) Multiple substance dependence syndrome (synonym: polydrug addiction) is a disease caused by the use of two or more PAS simultaneously or alternately in the presence of diagnostic criteria characteristic of the dependence syndrome (pathological attraction, withdrawal syndrome, tolerance dynamics, etc.), to each of the used surfactants; nine0003
2) other forms of combined use of PAS - for example, when the syndrome of dependence on PAS, including alcohol, is combined with the harmful use of another PAS or a specific drug (drug).
There can be quite a lot of combinations, it is often not possible to unambiguously diagnose the syndrome of dependence on several psychoactive substances (i.e., polydrug addiction), but to determine the therapeutic tactics, it is simply necessary to understand the pattern of use, the severity of the formed syndrome, and its possible options. Apparently, due to the variety of forms and combinations encountered in practice, this section was removed from the ICD-11 and DSM-V classification systems [14, 15], precisely because it would be more correct, understandable and informative for the doctor to indicate separately every condition associated with the use of PAS. Category F19in these classifications, it proposes to consider “a syndrome of dependence on other, unknown surfactants, such as anabolic steroids, non-steroidal anti-inflammatory drugs, cortisol, antiparkinsonian and antihistamine drugs, nitric oxide, amyl-, butyl- or isobutyl-nitriles, betel nut, kava, cathinones, as well as other unknown, not yet identified substances” [15].
Apparently, due to the variety of forms and combinations encountered in practice, this section was removed from the ICD-11 and DSM-V classification systems [14, 15], precisely because it would be more correct, understandable and informative for the doctor to indicate separately every condition associated with the use of PAS. Category F19in these classifications, it proposes to consider “a syndrome of dependence on other, unknown surfactants, such as anabolic steroids, non-steroidal anti-inflammatory drugs, cortisol, antiparkinsonian and antihistamine drugs, nitric oxide, amyl-, butyl- or isobutyl-nitriles, betel nut, kava, cathinones, as well as other unknown, not yet identified substances” [15].
Medical prevention of narcological diseases is considered as a set of measures implemented through the healthcare system by specialists of the narcological service independently and together with specialists of intradepartmental and interdepartmental interaction. nine0003
For persons with developed dependence syndrome, the most important role is given to tertiary (modification) prevention measures, where the treatment process is fully integrated into the system of a set of procedures aimed at maintaining and strengthening health. At the same time, the main tasks of modification prevention and the treatment process (prevention of further development of the disease, reduction of harmful consequences, prevention of relapses) coincide and, in fact, are links in one process - treatment and rehabilitation. nine0003
At the same time, the main tasks of modification prevention and the treatment process (prevention of further development of the disease, reduction of harmful consequences, prevention of relapses) coincide and, in fact, are links in one process - treatment and rehabilitation. nine0003
Questions of treatment of conditions caused by the combined use of several PAS remain relevant due to their complexity and little development. To date, many interesting and even seemingly promising drugs for the treatment of drug addiction have been developed and studied, but the main, recommended and available therapy has changed very little over time. This circumstance causes alarm and annoyance [16]. Currently, most pharmacological treatment options for drug addiction show moderate efficacy, especially in the long term. Therefore, the development of new treatment strategies, including new drugs, their combinations, the use of various biomarkers to predict responses, is still relevant [17]. In situations where a patient suffers from polydrug addiction or uses several psychoactive substances, there is no other way out but to use those methods of treatment that have shown their effectiveness in dependence on each substance, used in this case simultaneously or sequentially.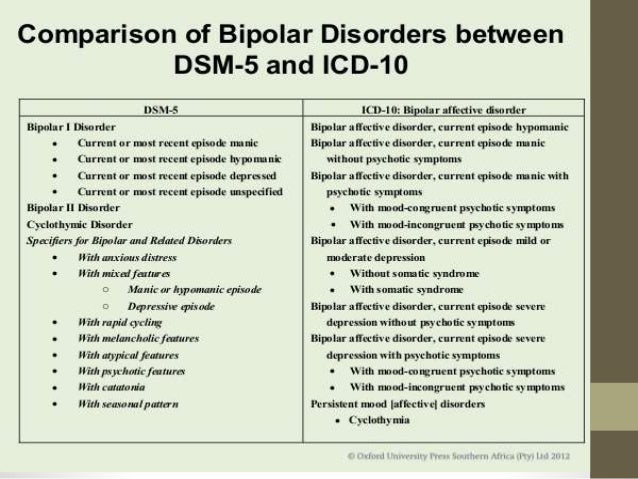 nine0003
nine0003
For a unified and uniform understanding of the quality of the accumulated therapeutic tactics to date, the presented recommendations used rating schemes for assessing the level of evidence reliability (Ia, Ib, IIa, IIb, III, IV) ( Table 1) Table 1. Rating scheme for assessment the level of certainty of evidence and the level of persuasiveness of recommendations (A, B, C, D) ( Table 2). Table 2. Rating scheme for assessing the level of persuasiveness of recommendations
Clinical diagnostics
The combined use of several surfactants affects the overall clinical picture of the disease and leads to more severe medical and social consequences. The pattern of use depends on gender, age, and often even on social status. Under conditions of an already formed dependence on one surfactant, dependence on other surfactants is formed rather quickly. The defining symptom of the disease in such cases is the formed mental dependence - a pathological attraction to another surfactant, expressed as clearly as to the predecessor. In the dynamics of the disease, the formation of a stable long-term remission is difficult and unlikely. The form of PAS use tends to be constant: the patient, as a rule, is not able to live without intoxication. nine0003
In the dynamics of the disease, the formation of a stable long-term remission is difficult and unlikely. The form of PAS use tends to be constant: the patient, as a rule, is not able to live without intoxication. nine0003
Co-administration of alcohol and opioids is common in clinical practice. Often, the first trials of opioids occur with the aim of alleviating the withdrawal syndrome (AS) - the so-called "vicarious use". Another common option is the use of surfactants in remission. Against the background of the actualization of a pathological craving, for example, for opioids, the patient tries to satisfy this craving by taking other, socially acceptable PAS, which is alcohol.
Combined use of alcohol and cocaine, other psychostimulants. Patients suffering from addiction to cocaine or other psychostimulants quite often switch to alcohol in the course of the disease. As a rule, this is due to attempts to "soften" the withdrawal syndrome of cocaine and other psychostimulants. The combined use of cocaine and alcohol is more typical for Europe and the USA: the diagnosis of alcohol dependence can be established in 50–90% of cocaine addicts [18]. In Russia, cocaine dependence is not so widespread, but the use of psychostimulants by patients with alcohol dependence in clinical practice is not uncommon. nine0003
The combined use of cocaine and alcohol is more typical for Europe and the USA: the diagnosis of alcohol dependence can be established in 50–90% of cocaine addicts [18]. In Russia, cocaine dependence is not so widespread, but the use of psychostimulants by patients with alcohol dependence in clinical practice is not uncommon. nine0003
The combined use of opioids and psychostimulants (cocaine, amphetamines) is a common option. Patients with opioid addiction begin the use of psychostimulants either in search of new sensations, wanting to experience the multidirectional effects of two drugs (to arrange the so-called "swing"), or in order to alleviate the course of opium withdrawal syndrome (OSA).
Concomitant use of alcohol and sleeping pills and sedatives. The main motives for the formation of addiction to hypnotics and sedatives in patients with alcohol dependence are either the desire to increase intoxication or to mitigate the manifestations of alcohol withdrawal syndrome (AAS). nine0003
nine0003
Concomitant use of opioids and sedative-hypnotics. In patients with developed opioid dependence, the reason for the transition to the combined use of hypnotics and sedatives is the leveling of euphoria with the isolated use of opiates. At the first trials, the addition of sedative-hypnotics not only allows you to relive the euphoria, but also to reduce the dose of opioids [2].
Combined use of cannabinoids, synthetic cannabinoids (“Spices”) and other substances. nine0118 The formation of most known variants of drug addiction in most cases begins with the first samples of cannabinoids. Since addiction to cannabinoids takes quite a long time to develop, it is often difficult to determine whether the use of cannabinoids is harmful or if addiction has already formed. Spice smoking is common among young people. The hedonistic motivation of the use prevails. The formation of dependence on synthetic cannabinoids is often vicarious, it corresponds to the general patterns of the formation of the syndrome of dependence on surfactants.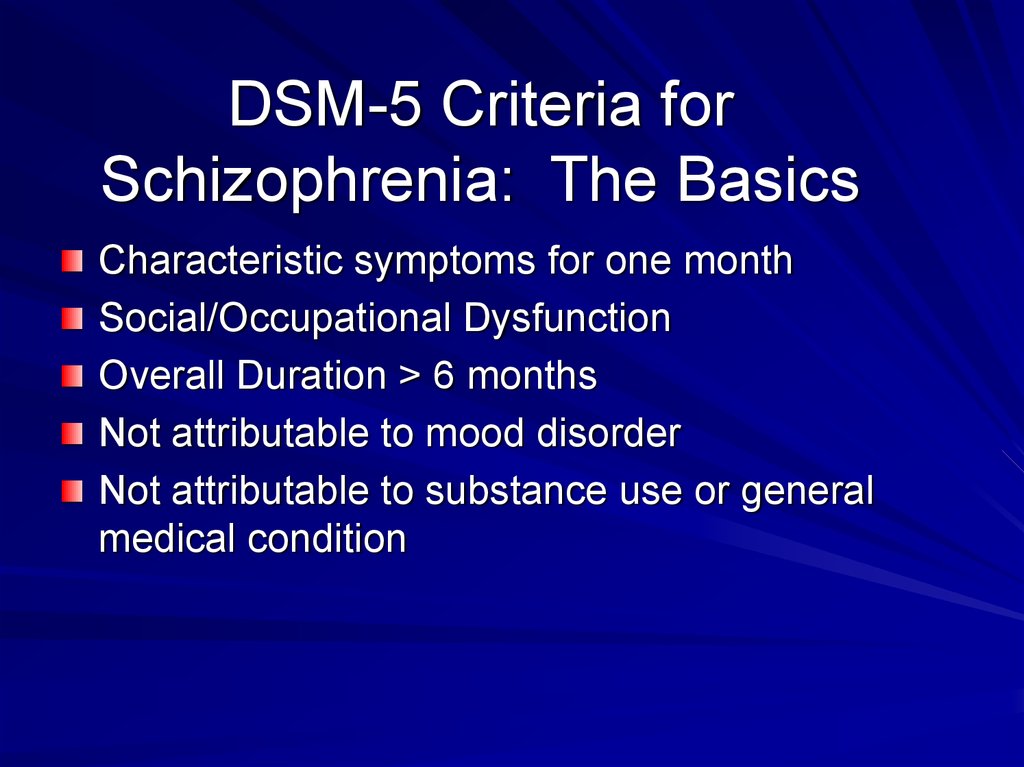 nine0003
nine0003
Laboratory diagnostics
The following biomarkers of alcohol abuse are currently used for diagnostic purposes: aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (gamma-GT), mean red cell volume (MCV) and carbohydrate-deficient transferrin (UDT, CDT), ratio AST/AlAT and MCV [2, 19-24].
In the laboratory diagnosis of other surfactants, two main types of testing are used: immunoassay (ELISA) and chromatography—gas chromatography (GC), mass spectrometry (MS), or high performance liquid chromatography (HPLC). ELISA is used as a primary screening due to its simplicity and low cost, chromatography is used in complex diagnostic cases, to confirm the results of ELISA and to obtain high-precision results [21, 25-27]. Each surfactant has its own duration of detection in urine by ELISA [21, 26, 27] (Table 3). Table 3. Detection of psychoactive substances during enzyme immunoassay
Therapeutic tactics
Since the disease of addiction is a chronic disease with a relapsing character, long-term supportive treatment with maximum individualization of the process is an essential guarantee of success.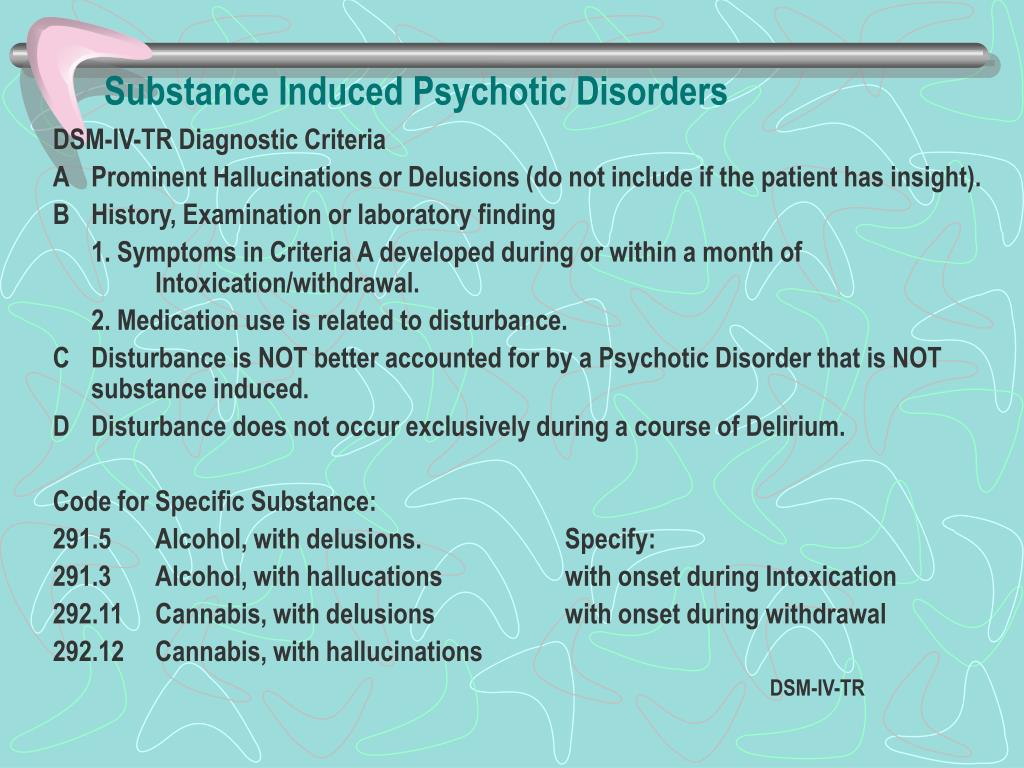
Relief of the syndrome of pathological craving for PAS is the most complex and difficult task. This is a complex syndrome that includes affective, behavioral, ideational, vegetative, and sometimes sensory components. This structure indicates a complex pathogenesis of its formation, which involves many neurotransmitter systems of the brain: adrenergic, dopaminergic, serotonergic, endogenous opiate and glutamate receptor systems, and possibly some others. This dictates the need to use many groups of drugs, including psychotropic ones. The data accumulated to date on the pathogenesis of the disease, as well as practical experience in working with patients with drug addiction and alcoholism, allow us to confidently say that the differentiated and correct use of antidepressants, antipsychotics, and anticonvulsants makes it possible to form a stable and long-term remission [2]. Despite the continuing shortage of randomized clinical trials of various groups of psychotropic drugs in the treatment of narcological pathology, nonetheless, the drugs of the above groups are successfully used in clinical practice [2, 28–30].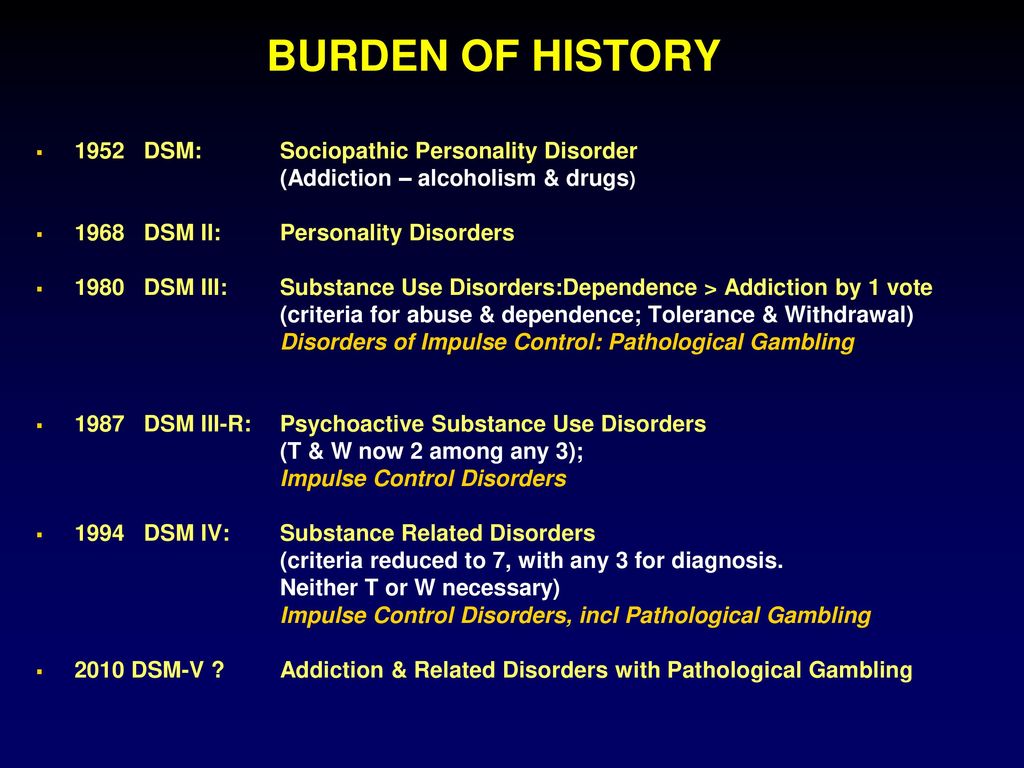 nine0003
nine0003
For combined use of alcohol and opioids , the same treatment is recommended as for opioid dependence syndrome (III C) [2, 30, 31]. After stopping the withdrawal syndrome, it is recommended to prescribe long-acting opioid receptor blockers - naltrexone (IA) [28, 32-44]. In the dependence syndrome caused by the combined use of opioids and alcohol, disulfiram (III C) is recommended [2, 30, 31].
Combined use of alcohol and cocaine, other psychostimulants. nine0118 For the relief of mixed withdrawal syndrome, a protocol for the treatment of alcohol withdrawal syndrome is used. For the stage of post-withdrawal disorders and remission, there are well-established, effective clinical practices: first, the appointment of disulfiram (III C) [45, 46]; secondly, the combined use of disulfiram and naltrexone (IA) [47].
Concomitant use of opioids and psychostimulants (cocaine, amphetamines). In foreign practice (European countries, the USA, Canada, etc.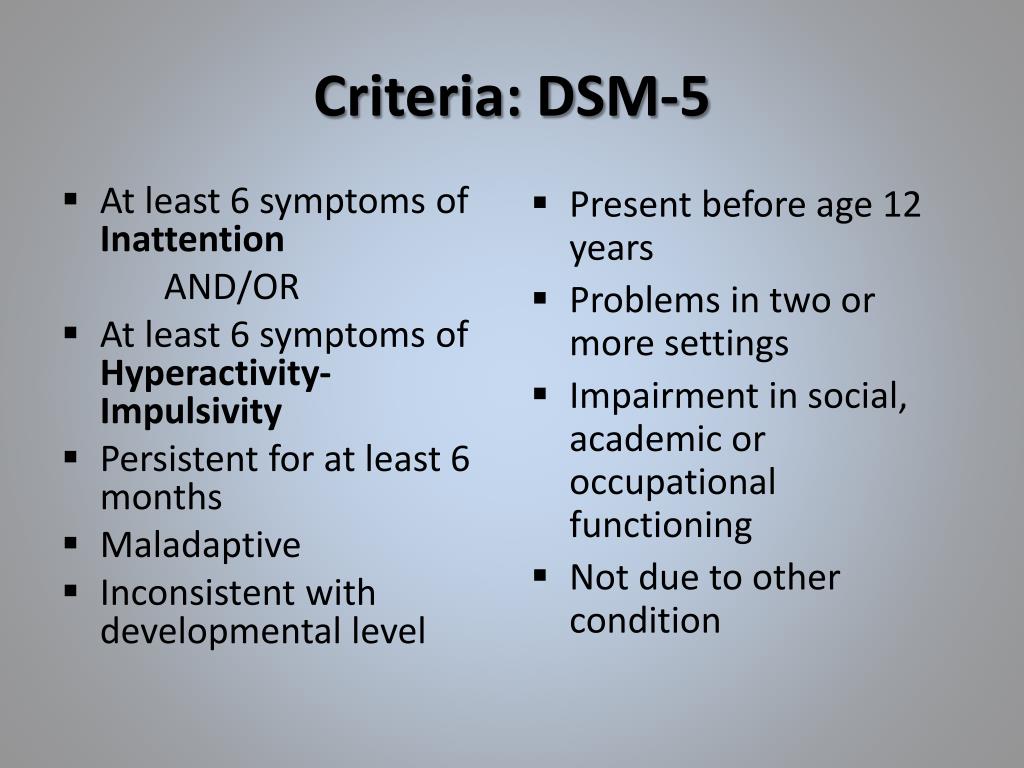 ), patients with combined use of opioids and psychostimulants are prescribed substitution therapy programs, where cocaine is used directly along with opioid receptor agonists [30]. The use of disulfiram at a dose of 250 mg/day against the background of substitution therapy programs showed a significant reduction in cocaine (Ib) consumption [48]. The use of cocaine vaccine is considered as a promising treatment (Ib) [49].
), patients with combined use of opioids and psychostimulants are prescribed substitution therapy programs, where cocaine is used directly along with opioid receptor agonists [30]. The use of disulfiram at a dose of 250 mg/day against the background of substitution therapy programs showed a significant reduction in cocaine (Ib) consumption [48]. The use of cocaine vaccine is considered as a promising treatment (Ib) [49].
In Russia, the treatment of withdrawal syndrome is carried out taking into account what drug use has prevailed recently, in what doses, regimens. With the chaotic use of opioids and psychostimulants, preference should be given to the protocol for the treatment of opium withdrawal syndrome. After stopping the withdrawal syndrome, opioid receptor blockers, disulfiram, or a combination thereof are prescribed [2].
Concomitant use of alcohol and sleeping pills and sedatives. nine0118 Therapy issues in most of these cases are related to detoxification.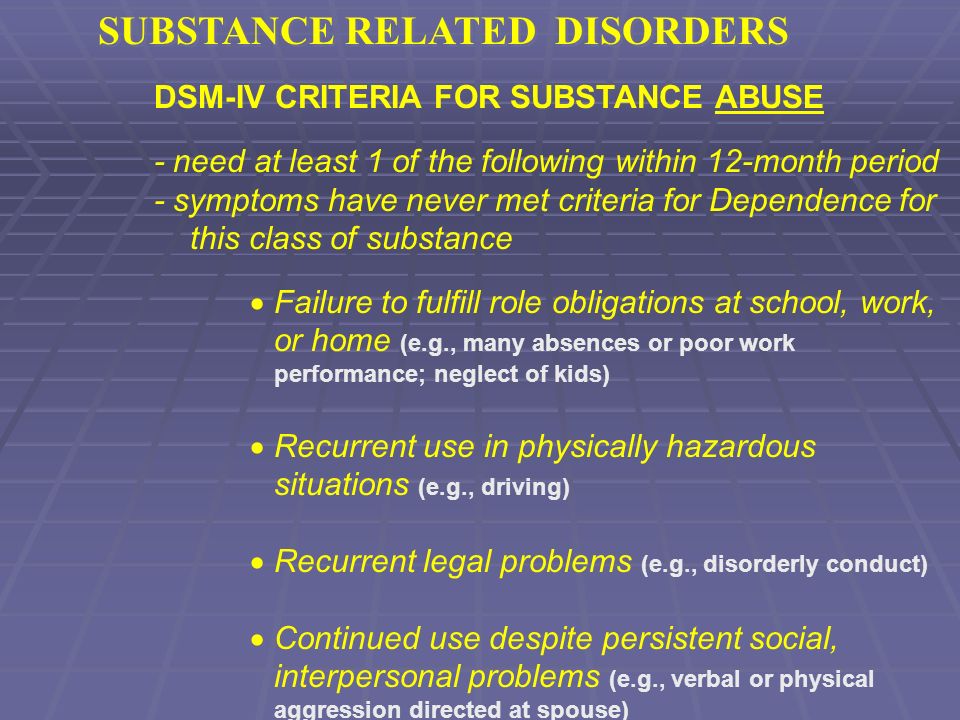 Depending on the doses of hypnotics and sedatives used, an individual therapeutic regimen is selected using tranquilizers with a gradual decrease in doses. An alternative treatment regimen is the use of carbamazepine or valproic acid preparations. Supportive anti-relapse programs are usually focused on abstinence from alcohol (disulfiram, opioid receptor blockers), since there is no specific therapy for the treatment of dependence on hypnotics and sedatives at the present stage. nine0003
Depending on the doses of hypnotics and sedatives used, an individual therapeutic regimen is selected using tranquilizers with a gradual decrease in doses. An alternative treatment regimen is the use of carbamazepine or valproic acid preparations. Supportive anti-relapse programs are usually focused on abstinence from alcohol (disulfiram, opioid receptor blockers), since there is no specific therapy for the treatment of dependence on hypnotics and sedatives at the present stage. nine0003
Concomitant use of opioids and sedative-hypnotics. Therapy issues in most cases are associated with detoxification. The results of comparative studies have shown that complex treatment increases the efficiency of detoxification, in particular, the addition of carbamazepine (IIIC) to the basic therapy regimens [30]. In the post-withdrawal phases, opioid dependence treatment protocols are used.
Combined use of various surfactants and cannabinoids. Due to the fact that there is no specific therapy for cannabinoid addiction to date, treatment is carried out according to protocols consistent with other used psychoactive substances.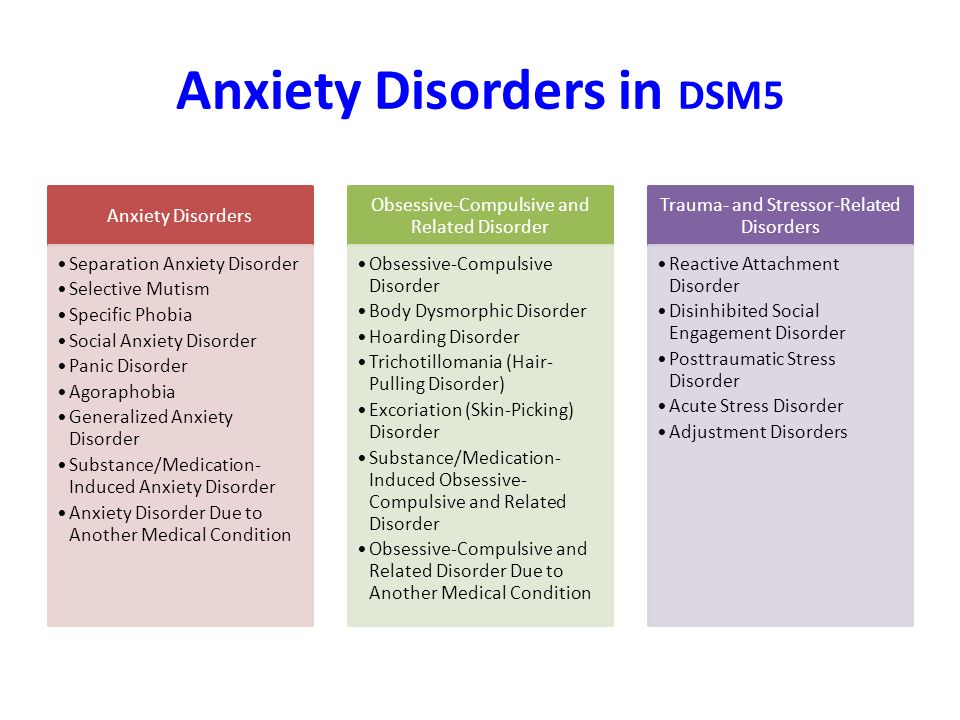
Concomitant use of several surfactants aggravates the clinical picture of the disease as a whole, causing significant differential diagnostic difficulties. Collected together, the available evidence-based clinical guidelines are intended for their wide use by psychiatrists and narcologists and are aimed at solving the main task of improving the quality of remissions and preventing relapses in patients with combined use of various types of psychoactive substances. nine0003
It is recommended to determine the activity of gamma-GT (I A), AST (I A), MCV (I A), CDT (I A) [2, 22-24].
ELISA is recommended for primary screening of urine for surfactants, confirmation by GC/MS or HPLC in case of positive ELISA results (III C) [21, 26, 27].
It is recommended to expand the panel of opioids to detect commonly used surfactants: fentanyl, hydrocodone, methadone, oxycodone, buprenorphine, tramadol (III C) [21, 26, 27].
Combined use of several surfactants uses those methods (or protocols) of treatment that have shown their effectiveness in dependence on each surfactant; they are applied simultaneously or sequentially.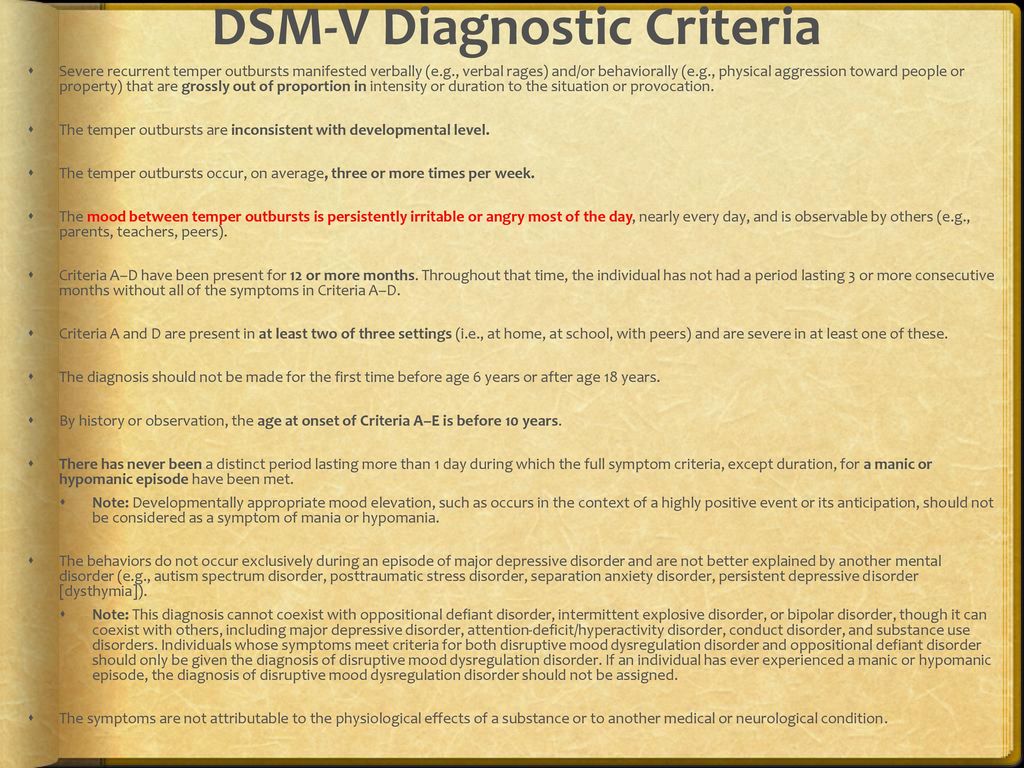 nine0003
nine0003
The use of additional pharmacotherapeutic agents such as antidepressants, anticonvulsants, antipsychotics, nootropics in the treatment of dependence syndrome is recommended to be considered on an individual basis (III C) [2, 30].
The same treatment is recommended for the combined use of opioids and alcohol as for the dependence syndrome caused by the use of opioids (III C) [2, 30].
In the combined use of opioids and alcohol after relief of the withdrawal syndrome, it is recommended to prescribe long-acting opioid receptor blockers - naltrexone (I A) [28, 32-40], disulfiram (III C) [30], or the appointment of naltrexone in combination with disulfiram (I A) [36]. nine0003
In the combined use of psychostimulants and alcohol, the appointment of disulfiram (III C) [45, 46] or the appointment of naltrexone in combination with disulfiram (I A) [47] is recommended.
In the combined use of psychostimulants and opioids, the appointment of disulfiram (Ib) [48], or the appointment of naltrexone in combination with disulfiram [2], is recommended.