Effexor vs sertraline
Effexor vs Zoloft: Which is Right for Me?
Although Effexor and Zoloft are both prescribed to treat depression, there are some major differences between the two drugs.
In this article, we will explore the ways that Effexor and Zoloft are similar and when they may be prescribed.
We’ll also go over how they are different, common dosages, and precautions to know when taking either medication.
Plus, we’ll discuss how you should know when you should see a doctor for symptoms of depression.
What is Effexor?
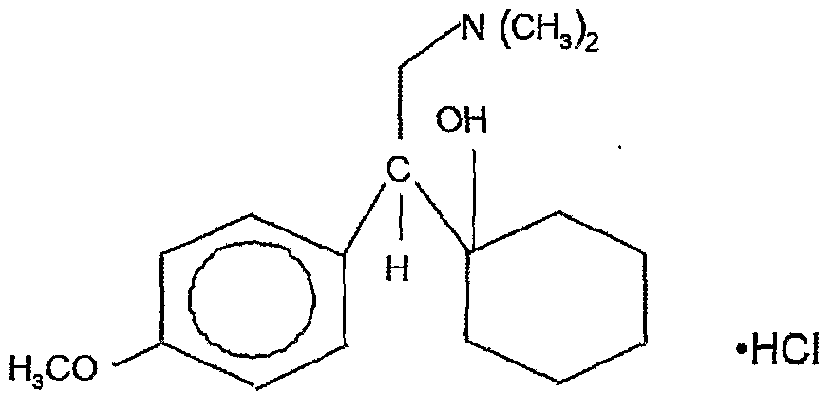
Effexor (venlafaxine hydrochloride) is a serotonin and norepinephrine reuptake inhibitor (SNRI), a class of antidepressant drugs.
Feeling Down?
Take our free assessment and learn about your options.
Get Started
Effexor uses
Effexor is approved by the Food and Drug Administration (FDA) for treatment of the following:
- Major depressive disorder
- Generalized anxiety disorder
- Panic disorder
- Social anxiety disorder
How Effexor works
Effexor is a serotonin and norepinephrine reuptake inhibitor (SNRI).
It works by blocking the reuptake of the neurotransmitters serotonin and norepinephrine, increasing their levels in the brain.
Both of these neurotransmitters are important in providing feelings of balance and energy in the brain and tend to be too low in people who experience symptoms of depression, anxiety, low mood, or fatigue.
What is Zoloft?
Zoloft (sertraline hydrochloride) is a selective serotonin reuptake inhibitor (SSRI) used to treat depression and other mood disorders.
Zoloft uses
Zoloft is FDA-approved as a treatment for the following conditions:
- Major depressive disorder
- Obsessive-compulsive disorder (OCD)
- Panic disorder
- Post-traumatic stress disorder (PTSD)
- Social anxiety disorder
- Premenstrual dysphoric disorder (PMDD)
How Zoloft works
Zoloft prevents the reuptake of serotonin, which leaves more of this calming, balancing neurotransmitter in the brain.
It does not impact the other neurotransmitters, norepinephrine and dopamine.
How Are They Similar?
Effexor and Zoloft have some similarities.
- They are both antidepressants that are taken once per day.
- They are both FDA-approved for treating depression, panic disorder, and social anxiety disorder.
Effectiveness at treating depression
In clinical trials, Effexor was found to be superior to a placebo at treating symptoms of depression, including cognitive disturbance and anxiety.
It also led to fewer relapses.
No differences were found between sexes.
Zoloft has also been shown to be effective for treating many types of depression and mood disorders, including postpartum depression.
Both Effexor and Zoloft are effective, FDA-approved pharmaceutical options for treating depression.
Clinical trials have validated their ability to address symptoms in major depressive disorder.
Since they are in different drug classes, they work differently and one drug may be less effective for an individual than the other.
Responses to antidepressants and other pharmaceuticals depend on a person’s genetic makeup, age, weight, overall health, and other medications they may take.
How Are They Different?
Effexor and Zoloft have quite a few differences.
Drug class
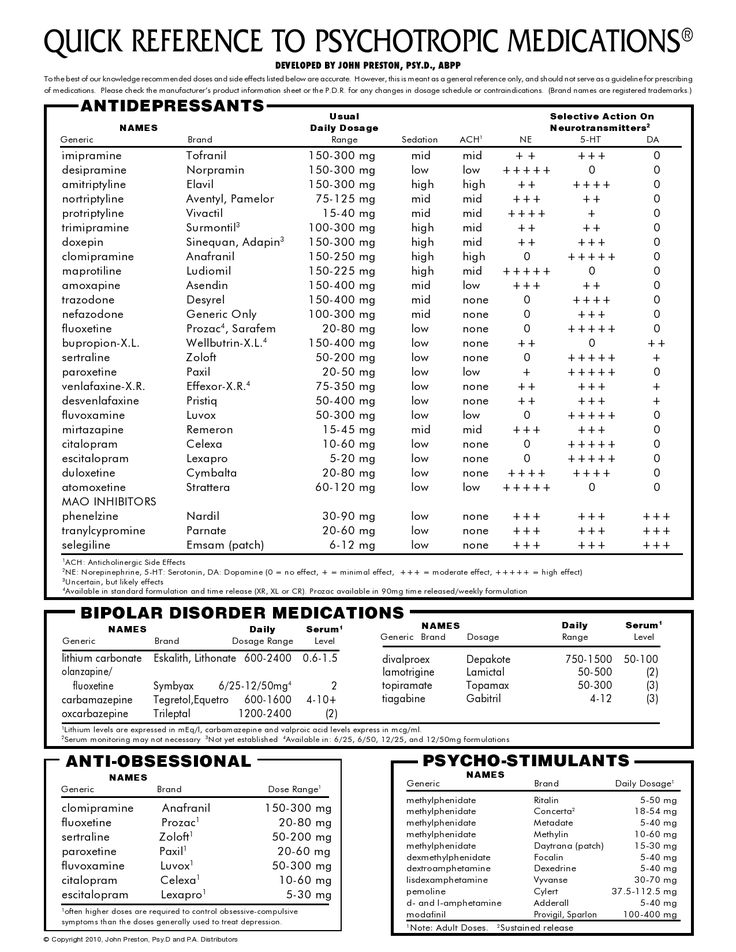
Effexor is a serotonin and norepinephrine reuptake inhibitor (SNRI), whereas Zoloft is a selective serotonin reuptake inhibitor (SSRI).
These medications both work to improve the brain’s access to neurotransmitters, but Effexor works on more than one (serotonin and norepinephrine), while Zoloft only affects serotonin.
However, this does not mean that one is better than the other.
You and your healthcare provider will decide together which medication, if any, will be best suited for you, taking into account your medical history, side effects, and risks and benefits of the medication.
Conditions treated
Effexor and Zoloft are both approved by the FDA for the treatment of the following:
- Major depressive disorder
- Social anxiety disorder
Effexor is also FDA-approved to treat cataplexy.
Zoloft is also an approved treatment for obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), panic disorder, premenstrual dysphoric disorder (PMDD), and for the treatment of OCD in children.
Both drugs may be used for off-label purposes at the discretion of healthcare providers.
Effexor’s off-label use may include:
- Attention deficit disorder (ADD)
- Fibromyalgia
- Diabetic neuropathy
- Complex pain syndromes
- Hot flashes
- Migraine prevention
- PTSD
- OCD
- PMDD
Off-label uses of Zoloft may include:
- Binge eating disorder
- Body dysmorphic disorder
- Bulimia nervosa
- Generalized anxiety disorder (GAD)
- Premature ejaculation
Standard dosage
Effexor and Zoloft are dosed differently.
Effexor is available as a tablet, an extended-release tablet, and an extended-release capsule.
It may be taken with or without food.
Standard dosages are 75 mg for extended-release formulations and 150 mg for the tablet.
Zoloft is available in oral tablets, capsules, and liquid solution.
It is best absorbed when taken with food. Standard dosages may range from 25-200 mg.
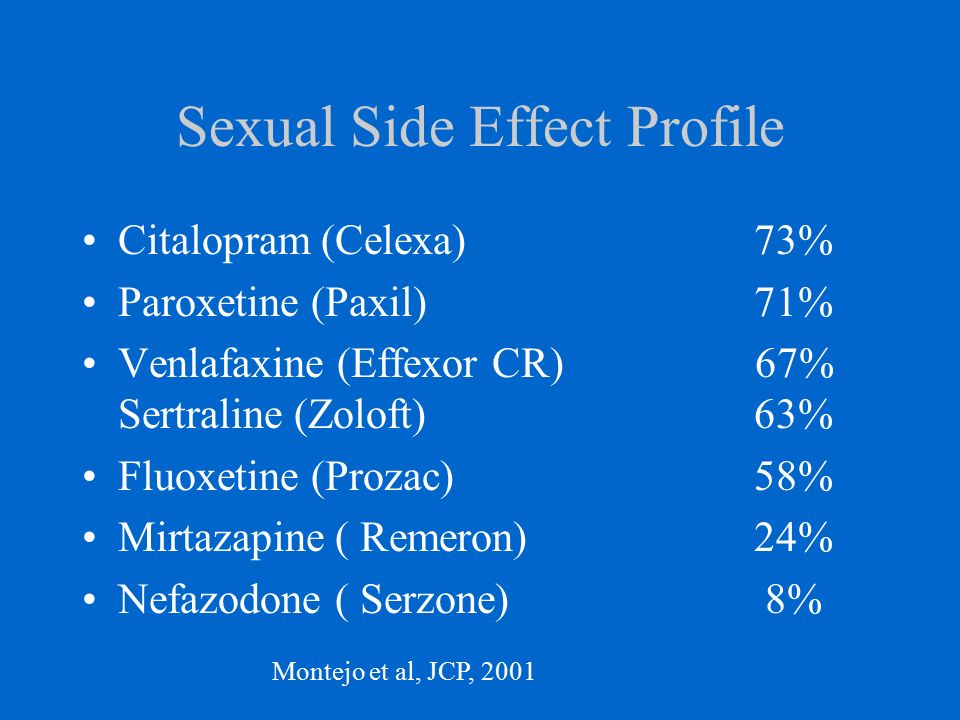
Potential side effects
Common side effects of Effexor include:
- Nausea
- Constipation
- Flatulence
- Dry mouth
- Loss of appetite
- Dizziness
- Insomnia
- Sweating
- Abnormal sexual function for people with penises
- Decreased libido
- Hypertension
- Yawning
Common side effects of Zoloft may include:
- Fainting
- Lightheadedness or dizziness
- Diarrhea
- Nausea
- Sweating
- Dry mouth
- Confusion or hallucinations
- Tremor
- Disorder of ejaculation
- Fatigue
- Female sexual dysfunction
Effexor Precautions
As an antidepressant, Effexor comes with a serious warning that includes the potential risk for increased thoughts of self-harm or suicidality.
This is called a black box warning.
This risk is greater in children, adolescents and young adults, but can happen to anyone.
If you or someone you love is taking Effexor, monitor closely for the following warning signs that require immediate medical attention:
- Unusual changes in behavior
- Worsening symptoms
- Thoughts or talk of self-harm
Effexor may not be safe to take for some people.
Contraindications for Effexor include:
- Taking MAOIs (or discontinuing MAOIs within 14 days)
- Allergies to any ingredients in Effexor formulations
- Abrupt withdrawal
Caution is advised in the following concurrent medical problems:
- Seizure disorder
- Hyponatremia or low sodium, or SIADH
- Liver or kidney impairment
- Bipolar disorder
- Hypertension
- Chronic use of NSAIDs, aspirin, or other anti-clotting medications, or bleeding disorder
- Interstitial lung disease
- Glaucoma
Zoloft Precautions
Zoloft also carries the serious black box warning.
Let a healthcare provider know immediately if any of the following signs develop in someone taking Zoloft:
- Agitation, aggression, or hostility
- Increased or worsening anxiety
- Panic attacks
- Irritability
- Insomnia
- Impulsiveness
- Unusual changes in behavior
- Suicidal thoughts or discussion (this risk can be increased in children, adolescents, and young adults, but can happen to anyone)
- Restlessness
- Manic behavior
Zoloft is contraindicated for the following reasons:
- Taking MAOIs (or discontinuing MAOIs within the past 14 days)
- Taking pimozide
- Sensitivity to any ingredients in Zoloft
- Taking disulfiram (for liquid Zoloft only)
- Liver disease or cirrhosis (Child-Pugh classes A, B, or C impairment)
Always let healthcare providers know anything else that you take—even OTC drugs, herbs, or supplements.
This will help to avoid potentially serious interactions, like gastrointestinal bleeding, heart arrhythmias, serotonin syndrome, all of which can be life-threatening.
Caution is advised in the following medical conditions:
- Medications that can increase the risk for Long QT interval
- Family or personal history of torsades de pointes or QT prolongation
- Arrhythmias, heart disease, or history of heart attack
- Seizure disorder
- Bipolar disorder
- Glaucoma
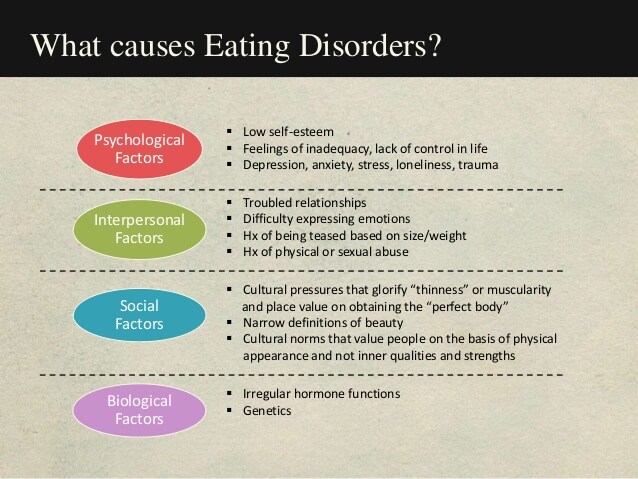
- Eating disorders which can cause electrolyte abnormalities
- Increased risk of bleeding – hereditary or medication-induced (NSAIDs, aspirin, anticoagulants)
- Hyponatremia or SIADH
Feeling Down?
Take our free assessment and learn about your options.
Get Started
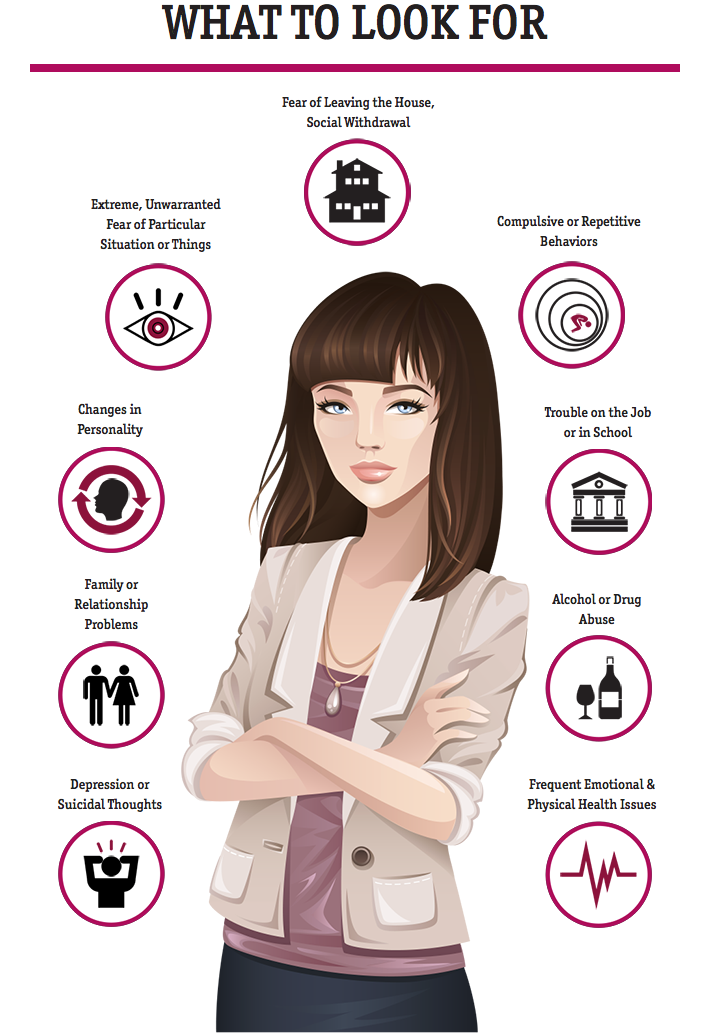
When to See a Doctor for Depression
If you are experiencing signs of depression, low mood, or do not feel like yourself, speak with your doctor.
Some signs of depression do not always make you feel sad.
You may lose interest in things you previously enjoyed, feel agitated or easily angered more often, have changes in sleep patterns or eating habits, or engage in behaviors that are not consistent with your usual activity.
There are many treatment options available for depression, both prescription and non-medication.
You are not alone in your struggle.
Your doctor can help you understand what requires treatment and will help you find treatment options that support your mood, well-being, and quality of life.
Always keep your doctor updated with how you feel, even if you already take antidepressants.
If your mood or symptoms change at any point, you may need a higher dose or a different medication.
Never stop taking antidepressants without speaking to your doctor.
They require tapering to avoid serious reactions and symptom relapse.
How K Health Can Help
Think you might need a prescription for Effexor (Venlafaxine) or a prescription for Zoloft (Sertraline)?
K Health has clinicians standing by 24/7 to evaluate your symptoms and determine which prescription is right for you.
Get started with our free assessment, which will tell you in minutes if treatment could be a good fit. If yes, we’ll connect you right to a clinician who can prescribe medication and have it shipped right to your door.
If yes, we’ll connect you right to a clinician who can prescribe medication and have it shipped right to your door.
.
Frequently Asked Questions
Is Effexor stronger than Zoloft?
Effexor and Zoloft are different medications. They are in two different classes of drugs. Effexor works to balance the neurotransmitters serotonin and norepinephrine, while Zoloft only affects serotonin. The strength of an antidepressant in addressing your symptoms depends on your health condition and the specifics of your situation.
Is Zoloft better than Effexor for anxiety?
Neither Zoloft nor Effexor are FDA approved for treating generalized anxiety disorder. Both are approved to treat social anxiety disorder, but only Zoloft has an off-label use for treating anxiety. Generally, Zoloft is better for addressing symptoms relating to generalized anxiety.
Both are approved to treat social anxiety disorder, but only Zoloft has an off-label use for treating anxiety. Generally, Zoloft is better for addressing symptoms relating to generalized anxiety.
What's the difference between Zoloft and Effexor?
Zoloft and Effexor are in different drug classes. Zoloft is an SSRI, while Effexor is an SNRI. They are approved to treat different conditions and have generally different off-label uses. While they are both approved to treat depression and social anxiety disorder, much of the similarity ends there.
Is there a better antidepressant than Effexor?
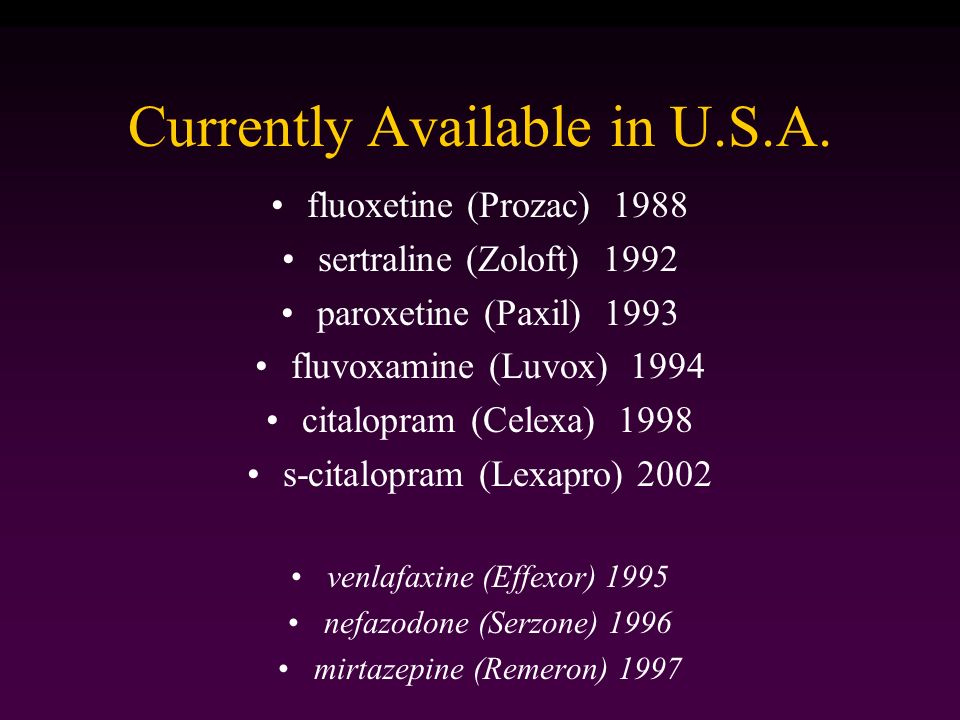
The best antidepressant for you is the one that works. This can be dependent on dosage, type of medication, length of treatment, and how your body reacts to the medication. You and your doctor will create a treatment plan that will take into account the risks and benefits of the medication options, possible interactions with your other medications, your health history, and other factors. If you start medication, it can take up to 6-8 weeks to notice improvement. Please talk to your doctor or healthcare provider about the length of treatment and how to stop the medication in the future. There are many different drug classes and types of antidepressants within each class. Effexor is an SNRI drug. The most commonly prescribed antidepressants are SSRIs, which include drugs like Zoloft, Paxil, Prozac, Celexa, and Lexapro.
You and your doctor will create a treatment plan that will take into account the risks and benefits of the medication options, possible interactions with your other medications, your health history, and other factors. If you start medication, it can take up to 6-8 weeks to notice improvement. Please talk to your doctor or healthcare provider about the length of treatment and how to stop the medication in the future. There are many different drug classes and types of antidepressants within each class. Effexor is an SNRI drug. The most commonly prescribed antidepressants are SSRIs, which include drugs like Zoloft, Paxil, Prozac, Celexa, and Lexapro.
K Health articles are all written and reviewed by MDs, PhDs, NPs, or PharmDs and are for informational purposes only. This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
K Health has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
We avoid using tertiary references.
-
Effexor XR (venlafaxine hydrochloride). (n.d.).
https://www.accessdata.fda.gov/drugsatfda_docs/label/2005/020699s059lbl.pdf -
Venlafaxine. (2022).
https://medlineplus.gov/druginfo/meds/a694020.html -
Zoloft (sertraline hydrochloride).
 (2016).
(2016).
https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/019839S74S86S87_20990S35S44S45lbl.pdf -
Sertraline. (2021).
https://www.ncbi.nlm.nih.gov/books/NBK547689/ -
Sertraline versus other antidepressive agents for depression.
 (2014).
(2014).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4163971/ -
A placebo controlled treatment trial of sertraline and interpersonal psychotherapy for postpartum depression. (2019).
https://pubmed.ncbi.nlm.nih.gov/30447565/
Differences, similarities, and which is better for you
Drug overview & main differences | Conditions treated | Efficacy | Insurance coverage and cost comparison | Side effects | Drug interactions | Warnings | FAQ
Effexor and Zoloft are two popular medications indicated for the treatment of depression, a common mental health condition, among other conditions.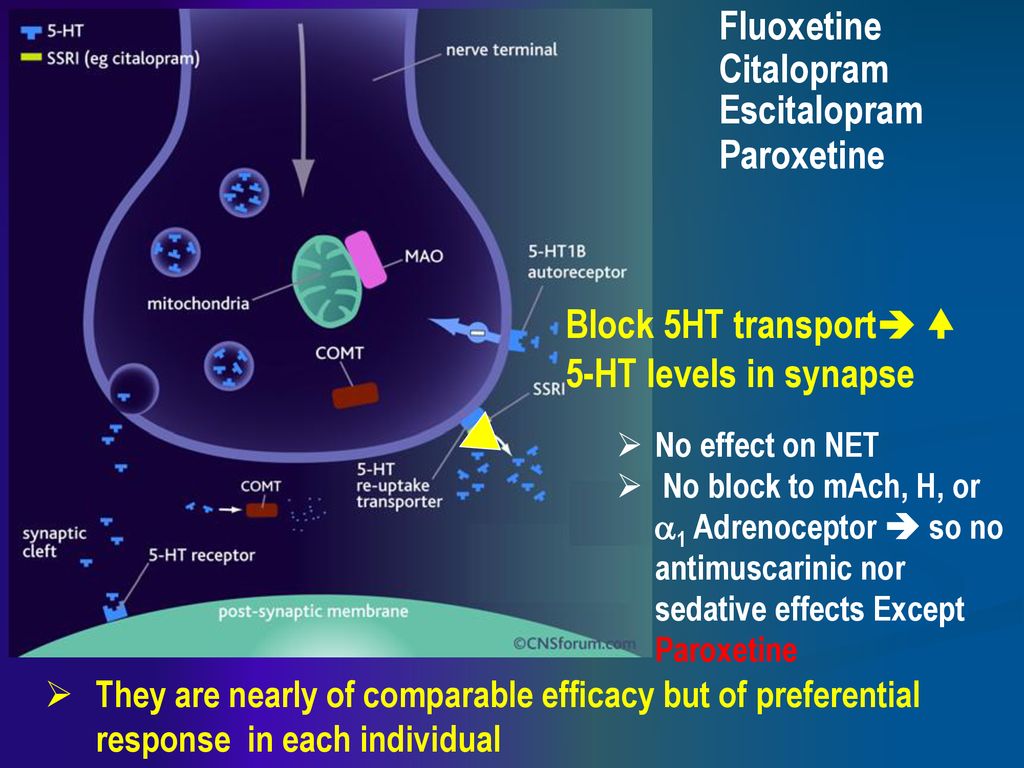 Both prescription drugs are approved by the United States Food and Drug Administration (FDA).
Both prescription drugs are approved by the United States Food and Drug Administration (FDA).
Effexor is part of a group of medications called SNRIs (serotonin-norepinephrine reuptake inhibitors). SNRIs increase levels of serotonin and norepinephrine in the brain.
Zoloft (sertraline) is an SSRI (selective serotonin reuptake inhibitor). An SSRI works by increasing levels of serotonin in the brain.
Treatment with Effexor or Zoloft is often accompanied by psychotherapy with a psychologist or doctor of psychiatry. Although Effexor and Zoloft are popular antidepressants, they are not the same. Continue reading to learn more about both medications.
What are the main differences between Effexor and Zoloft?
Effexor is an SNRI antidepressant and is available in brand (as Effexor XR) and generic form. The generic name is venlafaxine. Effexor is available in tablet form, and also as an extended-release capsule and extended-release tablet.
Zoloft is a selective serotonin reuptake inhibitor (SSRI) that is available in both brand and generic. The generic name is sertraline. Zoloft is available in both tablet and liquid form.
The generic name is sertraline. Zoloft is available in both tablet and liquid form.
Conditions treated by Effexor and Zoloft
Effexor, in its immediate-release form, is indicated for major depressive disorder. Effexor XR (extended-release) is indicated for major depressive disorder, generalized anxiety disorder, social anxiety disorder, and panic disorder.
Zoloft is indicated for treating major depressive disorder, obsessive-compulsive disorder, panic disorder, post-traumatic stress disorder, social anxiety disorder, and premenstrual dysphoric disorder.
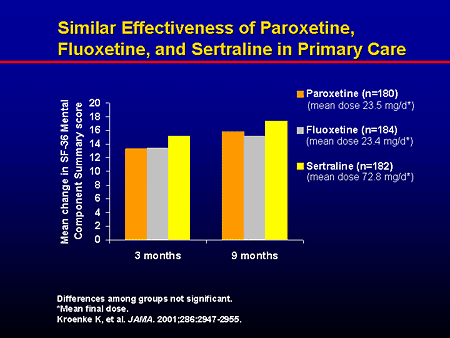
Is Effexor or Zoloft more effective?
One study compared Effexor XR and Zoloft in the treatment of depression and found that both drugs had similar efficacy and similar effect on the quality of life, but that Zoloft had fewer side effects. Also, patients who took Effexor had an increased risk of high blood pressure.
An analysis in The Lancet reviewed many studies to look for the best antidepressant. The researchers looked at 21 antidepressants (including Effexor and Zoloft) and found all antidepressants to be more effective than placebo. Effexor was found to be one of the more effective antidepressants, but Zoloft was better tolerated.
The researchers looked at 21 antidepressants (including Effexor and Zoloft) and found all antidepressants to be more effective than placebo. Effexor was found to be one of the more effective antidepressants, but Zoloft was better tolerated.
The most effective drug for you should be determined by your healthcare provider, who can take into account your medical history, medical conditions, and other medications you take that could interact with Effexor or Zoloft.
Coverage and cost comparison of Effexor vs. Zoloft
Effexor XR, the more popularly prescribed type of Effexor, is covered by most insurance and Medicare prescription plans. The generic version will have a lower copay, and the brand name may have a higher copay or may not be covered. The out-of-pocket price of a typical prescription of 30, 150 mg generic capsules is about $140. You can use a free SingleCare card to buy the generic prescription for around $15.
Zoloft is usually covered by both insurance and Medicare prescription plans.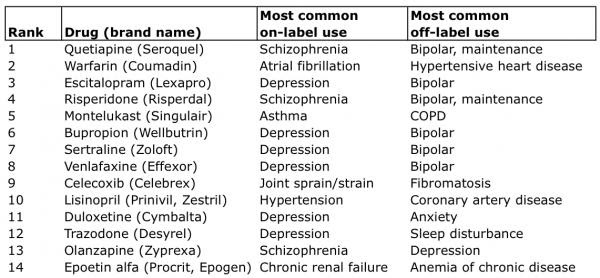 Generic Zoloft will have a lower copay, whereas brand name may have a higher copay or may not be covered at all. The out-of-pocket cost of Zoloft is about $32 for 30 tablets of 100 mg generic sertraline tablets. You can use a free SingleCare card to lower the price to $10 for generic Zoloft.
Generic Zoloft will have a lower copay, whereas brand name may have a higher copay or may not be covered at all. The out-of-pocket cost of Zoloft is about $32 for 30 tablets of 100 mg generic sertraline tablets. You can use a free SingleCare card to lower the price to $10 for generic Zoloft.
As insurance plans vary and are subject to change, contact your health insurance plan for current coverage information.
Common side effects of Effexor vs. Zoloft
The most common side effects of Effexor XR are nausea, sleepiness, dry mouth, sweating, sexual problems, decreased appetite, and constipation.
The most common adverse reactions of Zoloft are nausea, diarrhea, sexual problems, dry mouth, insomnia, and sleepiness.
Other adverse effects may occur. Consult your healthcare professional for a complete list of side effects.
*percentages listed are for Effexor XR, the more commonly prescribed formulation of Effexor.
Source: DailyMed (Effexor XR), DailyMed (Zoloft)
Drug interactions of Effexor vs.
 Zoloft
ZoloftMAO inhibitors should not be used within 14 days of Effexor or Zoloft. The combination may increase the risk of serotonin syndrome, a life-threatening medical emergency due to excess serotonin. Triptans used to treat migraines, as well as other antidepressants, opioids, dextromethorphan, or St. John’s wort should not be used in combination with Effexor or Zoloft due to the risk of serotonin syndrome.
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as Advil, Motrin, and aspirin, or anticoagulants such as warfarin, should not be taken with Effexor or Zoloft because of increased bleeding risk.
Do not drink alcohol while taking Effexor or Zoloft.
Other drug interactions may occur. Consult your healthcare provider for a full list of drug interactions.
Aspirin
Celecoxib
Ibuprofen
Meloxicam
NaproxenNSAIDs (nonsteroidal anti-inflammatory drugs)YesYes
Warnings of Effexor and Zoloft
- Effexor and Zoloft have a black box warning.
 A black box warning is the most severe warning required by the FDA (United States Food and Drug Administration). Children, adolescents, and young adults (up to age 24 years old) who take antidepressant medications have an increased risk of suicidal thoughts and behavior. All patients who take antidepressants should be carefully monitored.
A black box warning is the most severe warning required by the FDA (United States Food and Drug Administration). Children, adolescents, and young adults (up to age 24 years old) who take antidepressant medications have an increased risk of suicidal thoughts and behavior. All patients who take antidepressants should be carefully monitored. - Patients who take Effexor or Zoloft are at risk of serotonin syndrome, a life-threatening medical emergency caused by too much serotonin. This is even more likely with dosage increases and/or if taking other medications that increase serotonin. Monitor for symptoms of hallucinations, fever, tremor, seizures, and/or agitation.
- Withdrawal symptoms, such as agitation, may occur when discontinuing Effexor or Zoloft. Patients should taper off the drug very slowly and never stop abruptly. Your healthcare provider can give you a tapering schedule.
- Use with caution in patients who have seizures or bipolar disorder.
- There is a risk of hyponatremia (low sodium) due to syndrome of inappropriate antidiuretic hormone secretion (SIADH).
 SIADH symptoms may include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may cause falls. Seek immediate treatment if symptoms occur.
SIADH symptoms may include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may cause falls. Seek immediate treatment if symptoms occur. - Avoid Effexor or Zoloft in patients with angle-closure glaucoma.
- Effexor or Zoloft may increase the risk of bleeding. This risk increases with the concomitant use of NSAIDs or warfarin.
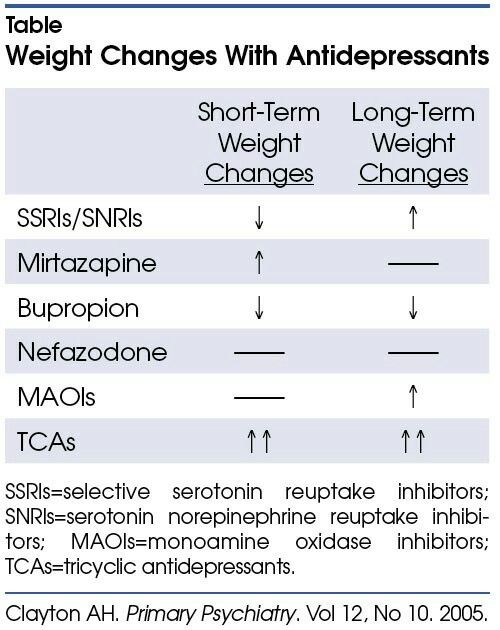
- Loss of appetite and/or weight loss may occur.
- Effexor or Zoloft should only be used in pregnancy if your healthcare provider determines that benefits outweigh risks. Effexor or Zoloft can cause serious complications to the baby, especially if taken in the third trimester. If you are already on Effexor or Zoloft and find out you are pregnant, contact your healthcare provider immediately.
- Zoloft oral solution contains 12% alcohol.
- Effexor may increase blood pressure. Monitor blood pressure before and during treatment with Effexor. Use with caution in patients with high blood pressure or heart problems.

Frequently asked questions about Effexor vs. Zoloft
What is Effexor?
Effexor is an SNRI antidepressant. Effexor treats depression (also called major depressive disorder or major depression) in adults. Effexor XR (extended-release) treats depression, social anxiety disorder, panic disorder, and generalized anxiety disorder. The generic name of Effexor is venlafaxine.
What is Zoloft?
Zoloft (sertraline) is an SSRI (selective serotonin reuptake inhibitor) indicated for the treatment of major depressive disorder, obsessive-compulsive disorder, panic disorder, post-traumatic stress disorder, social anxiety disorder, and premenstrual dysphoric disorder.
Are Effexor and Zoloft the same?
Effexor and Zoloft are not the same. Effexor is part of a drug class called SNRIs, or serotonin-norepinephrine reuptake inhibitors. SNRIs work on serotonin and norepinephrine. Some other drugs in the SNRI class are Cymbalta (duloxetine) and Pristiq (desvenlafaxine).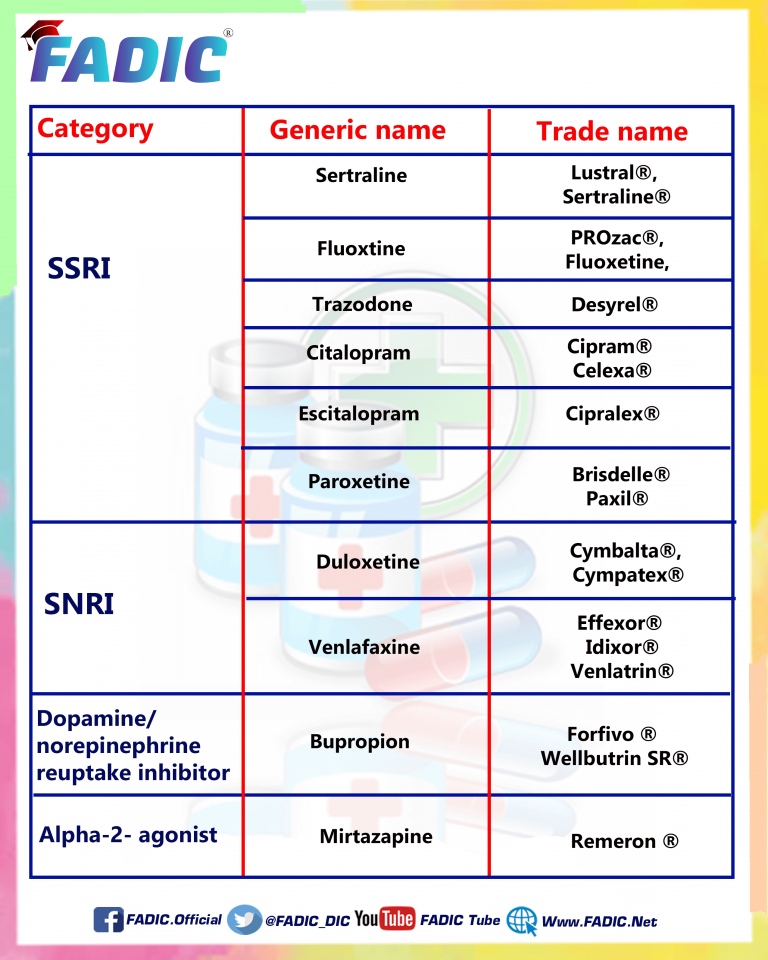
Zoloft is part of a drug class called SSRIs, or selective serotonin reuptake inhibitors. SSRIs work on serotonin. Some other drugs in the SSRI class of medications are Prozac (fluoxetine), Celexa (citalopram), Lexapro (escitalopram), Luvox (fluvoxamine), and Paxil (paroxetine).
Other differences between Effexor and Zoloft are outlined above.
Is Effexor or Zoloft better?
Either drug can be effective, but everyone responds differently to different medications. The best medication can be determined by your healthcare provider, who can consider your medical history and other medications you take that could interact with Effexor or Zoloft.
Can I use Effexor or Zoloft while pregnant?
Taking Effexor or Zoloft in the third trimester can cause serious complications to the baby, resulting in prolonged hospitalizations, tube feeding, and breathing support. Effexor or Zoloft is only prescribed in pregnancy when the benefits outweigh risks and if no other safer alternative is available. If you are already taking Effexor or Zoloft and find out that you are pregnant, contact your healthcare provider for medical advice.
If you are already taking Effexor or Zoloft and find out that you are pregnant, contact your healthcare provider for medical advice.
Can I use Effexor or Zoloft with alcohol?
No. Neither drug should be used with alcohol. Combining an antidepressant, like Effexor or Zoloft, with alcohol, can worsen depression or anxiety symptoms, impair thinking and alertness, and increase the effects of sedation and drowsiness.
Is Zoloft better for anxiety or depression?
Zoloft is indicated for major depressive disorder (depression). Zoloft is not indicated for generalized anxiety disorder, but it is indicated for panic disorder, social anxiety disorder, and OCD. Your healthcare provider can determine the best medication for you, depending on your diagnosis and other factors like your medical history and other medications you take that could interact with Zoloft.
Can Zoloft worsen anxiety?
Zoloft can treat depression and certain types of anxiety disorders. However, some people experience increased anxiety or agitation, especially when beginning treatment. If you take Zoloft and feel anxious or agitated, contact your healthcare provider for medical advice.
If you take Zoloft and feel anxious or agitated, contact your healthcare provider for medical advice.
Also, suicidal thoughts can occur in some cases, and the risk is higher in patients up to age 24 years. If you are having suicidal thoughts, seek emergency treatment. Be sure that your loved ones know about the possibility of suicidal thoughts and/or behavior, so they can be alert for any potential issues and help you seek treatment if necessary.
Is it better to take Zoloft in the morning or at night?
The prescribing information for Zoloft does not specify the best time of day to take it. The best time of day is when you will remember to take it every day. Also, if Zoloft makes you drowsy, you may want to take it at night. For some people, Zoloft causes insomnia. If Zoloft causes insomnia, you may want to take it in the morning. You can ask your prescriber if he or she suggests a recommended time.
Related Reading:- Effexor vs.
 Lexapro
Lexapro - Effexor vs. Wellbutrin
- Pristiq vs. Effexor
- Switching Antidepressants
Changing first-line antidepressants | Attending Doctor is a professional medical publication for physicians. Science articles.
| To achieve the desired clinical effect of antidepressants, it is recommended to switch from tricyclic antidepressants to drugs with a similar mechanism of action, in particular venlafaxine, a modern serotonin and norepinephrine reuptake inhibitor | |
partners Keywords / keywords: Antidepressants, Velaxin, Venlafaxine, Depression, Noradrenergic system, Neuropsychiatry, Serotonergic system, Thymoanaleptic therapy
VEL 25. 09.2020/7
09.2020/7
Thymoanaleptic therapy is a dynamic process, the scenario of which depends on the characteristics of the disease and the response to treatment. According to the current recommendations, the clinical effect of an antidepressant (BP) of more than 50% within 3-4 weeks is considered sufficient [1]. According to statistics, such effectiveness is not achieved in 30-50% of patients with initial therapy with the first-line drug [1]. In such cases, it is recommended to increase the dose of blood pressure to the maximum, and in some cases, especially with the use of SSRIs, improvement still develops: a full effect can be achieved at 4-6 or even 8 weeks of treatment [1]. If this does not happen, and also in cases where increasing the dose is impractical (for example, in case of poor tolerance), it is recommended to change the blood pressure to a drug within the same pharmacological class or with a different mechanism of action [1]. In this case, a special algorithm should be followed. nine0013
nine0013
The classical scheme suggests the gradual withdrawal of the initially prescribed drug, and after a washout period, the appointment of a new one with the selection of its therapeutic dose [2]. This method is used if there is a likely risk of an unwanted interaction that occurs when switching from drugs with a long half-life (such as fluoxetine), if the activity of the liver enzyme systems is reduced in the patient, or if the drugs differ radically in the mechanism of action (for example, when switching from mirtazapine or mianserin to milnacipran). nine0013
Both the patient and the doctor are much more comfortable with the one-time method of “switching” between drugs with a similar mechanism of action, when one day the first drug is canceled, and the second is prescribed immediately in a therapeutic dose. In this context, it seems convenient to switch patients from tricyclic antidepressants, fluvoxamine, sertraline, paroxetine, and milnacipran to a modern serotonin and norepinephrine reuptake inhibitor (SSRI) venlafaxine ( Velaxin ® [3]).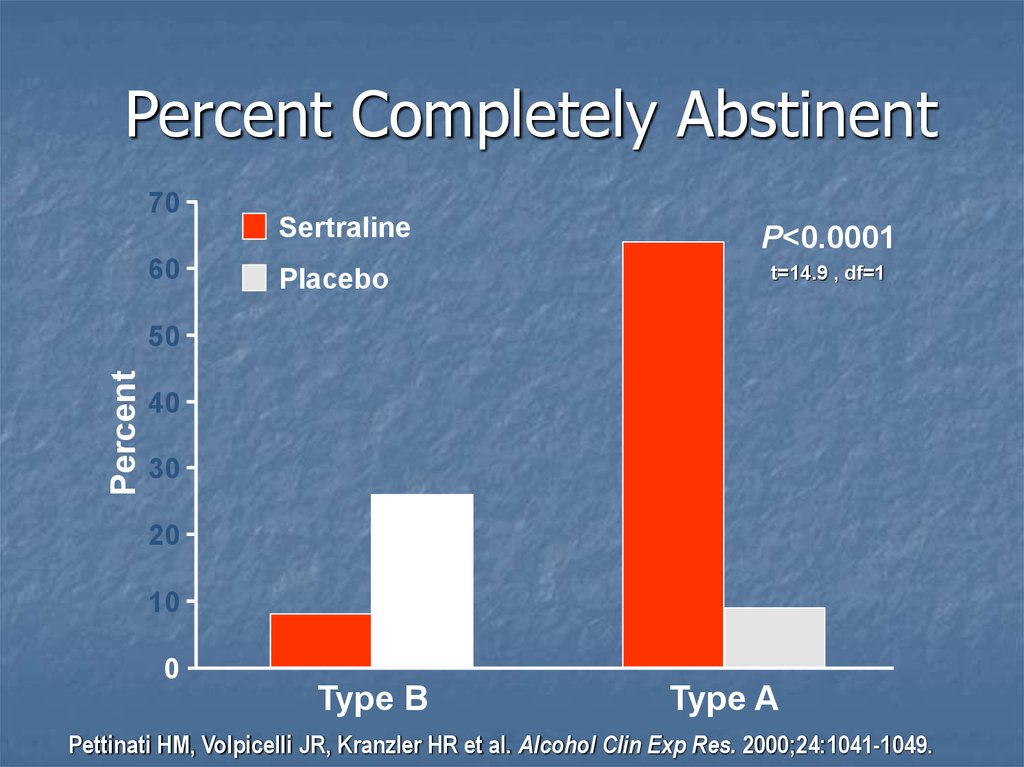 The need for such a transition arises in clinical practice, because. the effectiveness of venlafaxine is somewhat higher than that of SSRIs due to a wider spectrum of neurochemical action [1]. The drug acts immediately on three types of neurotransmitters: serotonin (improves mood), norepinephrine (promotes activation) and dopamine (improves motivation for action) [3]. In addition, the advantage of Velaksin ® is a special form of release in capsules. It provides a prolonged action of the active molecule of the drug [3], a more harmonious distribution in the corresponding synaptic sections of the CNS, which, in turn, reduces the risk of adverse events in the process of simultaneous administration or gradual achievement of a therapeutic dose [4]. nine0013
The need for such a transition arises in clinical practice, because. the effectiveness of venlafaxine is somewhat higher than that of SSRIs due to a wider spectrum of neurochemical action [1]. The drug acts immediately on three types of neurotransmitters: serotonin (improves mood), norepinephrine (promotes activation) and dopamine (improves motivation for action) [3]. In addition, the advantage of Velaksin ® is a special form of release in capsules. It provides a prolonged action of the active molecule of the drug [3], a more harmonious distribution in the corresponding synaptic sections of the CNS, which, in turn, reduces the risk of adverse events in the process of simultaneous administration or gradual achievement of a therapeutic dose [4]. nine0013
It should be taken into account that the transition from fluoxetine to Velaxin ® should be gradual due to the aforementioned long half-life of fluoxetine, in order to avoid unwanted interactions. When switching to Velaxin ® from mirtazapine, you will also have to observe the transition interval of 1-2 weeks, but in this case, due to the fundamentally different mechanisms of action of these drugs [2].
When switching to Velaxin ® from mirtazapine, you will also have to observe the transition interval of 1-2 weeks, but in this case, due to the fundamentally different mechanisms of action of these drugs [2].
- Russian Society of Psychiatrists. Depressive episode, Recurrent depressive disorder. Clinical guidelines. 2019.
- D.V. Hawks. Changing antidepressant therapy: causes and tactics. Medical business. 2007; 3:53-59.
- Instructions for medical use of the drug Velaksin® capsules LSR 000030 dated 05/24/2017.
- R.A. Becker, Yu.V. Bykov. Velaxin® capsules: presentation of a new long-acting form and review of the latest data on efficacy and safety. Psychiatry and psychopharmacotherapy. T.20. No. 1. 2018.
The material is intended for medical professionals. nine0031
Choosing an antidepressant based on efficacy and tolerability
partners Keywords / keywords: Antidepressants, Velaxin, Venlafaxine, Categories of tolerability, Classification, Neuronal, Side effects, Neuropsychiatry, Toxic
Summary
The classification of side effects of antidepressants is presented. Side effects can be toxic or neuronal. Neuronal side effects are divided into "extra-therapeutic" (persistent or reversible), as well as "paratherapeutic". Seven categories of antidepressant tolerance have been identified. The lowest category VII included clomipramine, imipramine, maprotiline, agomelatine. Category VI includes amitriptyline, V - pipofezin, trazodone, mianserin and mirtazapine, IV - vortioxetine, III - venlafaxine and duloxetine, II - sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine and milnacipran, and I - pirlindol and moclobemide. Among the most effective antidepressants (amitriptyline, imipramine, venlafaxine in high daily doses), venlafaxine turned out to be the best tolerability category. This drug is the most effective and well tolerated antidepressant. Other options for the practical use of classifications are discussed. nine0013
Side effects can be toxic or neuronal. Neuronal side effects are divided into "extra-therapeutic" (persistent or reversible), as well as "paratherapeutic". Seven categories of antidepressant tolerance have been identified. The lowest category VII included clomipramine, imipramine, maprotiline, agomelatine. Category VI includes amitriptyline, V - pipofezin, trazodone, mianserin and mirtazapine, IV - vortioxetine, III - venlafaxine and duloxetine, II - sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine and milnacipran, and I - pirlindol and moclobemide. Among the most effective antidepressants (amitriptyline, imipramine, venlafaxine in high daily doses), venlafaxine turned out to be the best tolerability category. This drug is the most effective and well tolerated antidepressant. Other options for the practical use of classifications are discussed. nine0013
Summary
A classification of the side effects of antidepressants is presented. Side effects can be toxic or neuronal. Neuronal side effects are divided into "extratherapeutic" (persistent or reversible), as well as "paratherapeutic". Seven antidepressant tolerance categories have been identified. The lowest VII category included clomipramine, imipramine, maprotiline, agomelatine. Amitriptyline belongs to the VI category, pipofezin, trazodone, mianserin and mirtazapine to the V category, vortioxetine belongs to the IV category, venlafaxine and duloxetine to the III category, sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine and milnacipran to the II category, and pirlindole and moclobemide to the I category. Among the most effective antidepressants (amitriptyline, imipramine, venlafaxine in high daily doses), venlafaxine was in the best category of tolerability. This drug is the most effective and tolerable antidepressant. Other options for the practical use of classifications are discussed. nine0013
Side effects can be toxic or neuronal. Neuronal side effects are divided into "extratherapeutic" (persistent or reversible), as well as "paratherapeutic". Seven antidepressant tolerance categories have been identified. The lowest VII category included clomipramine, imipramine, maprotiline, agomelatine. Amitriptyline belongs to the VI category, pipofezin, trazodone, mianserin and mirtazapine to the V category, vortioxetine belongs to the IV category, venlafaxine and duloxetine to the III category, sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine and milnacipran to the II category, and pirlindole and moclobemide to the I category. Among the most effective antidepressants (amitriptyline, imipramine, venlafaxine in high daily doses), venlafaxine was in the best category of tolerability. This drug is the most effective and tolerable antidepressant. Other options for the practical use of classifications are discussed. nine0013
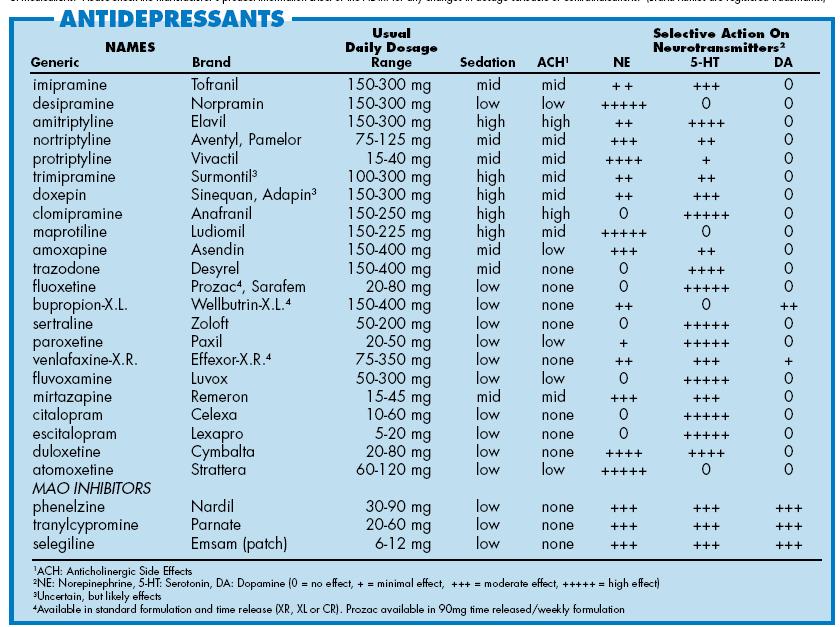
In the previous article, a description of the mechanism of action of various antidepressants (tricyclic - TcA, serotonin-modulating - CMA, four-cyclic - HcA, reversible monoamine oxidase type A inhibitors - RMAO-A, selective serotonin reuptake inhibitors - SSRIs, selective serotonin and norepinephrine reuptake inhibitors) was presented.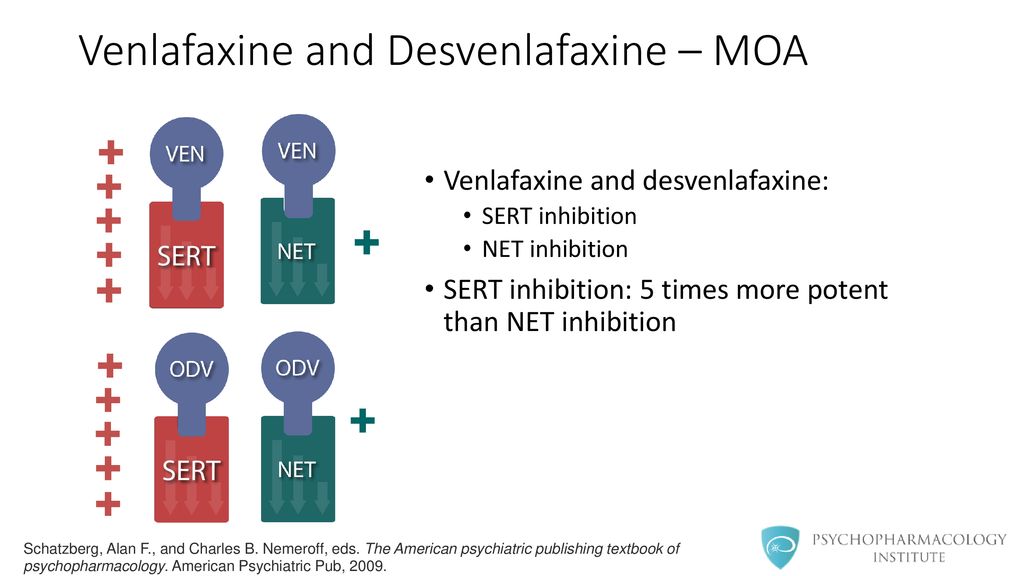 - SNRIs, norepinephrine and selective serotonin - NaSSA, melatonergic - MeA, multimodal - MmA) (Table 1). nine0013
- SNRIs, norepinephrine and selective serotonin - NaSSA, melatonergic - MeA, multimodal - MmA) (Table 1). nine0013
Table 1. Antidepressants known in Russia, their effect on neurons and the "formula" of the mechanism of action (1-4).
* - white color - the drug does not affect neurons, dark gray - a pronounced increase in activity, light gray - a moderate increase in activity, ** - in high doses, IOD - neurotransmitter reuptake inhibitors, NERR - agents that affect regulatory receptors, RMAO-A - reversible inhibitors of monoamine oxidase type "A". nine0013
All these drugs, to varying degrees, contribute to the activation of serotonin (↑C or ↑s), noradrenaline (↑H or ↑n), dopamine (↑D or ↑d) or melatonin (↑M or ↑m) neurons, the “tone” of which decreases with depression. But the most pronounced effect on the vital activity of neurons is ↑SNd-antidepressants: amitriptyline and imipramine (TcA), as well as venlafaxine (SNRI) in high daily doses. It is no coincidence that many experts refer to their most effective drugs for the treatment of depression (5). nine0013
It is no coincidence that many experts refer to their most effective drugs for the treatment of depression (5). nine0013
Of course, the choice of any antidepressant should be associated not only with its medicinal properties (effectiveness), but also with side effects (tolerability). The vast majority of authors agree that tolerability is best with SSRIs and worse with TcA (6-9), with other drugs in between (1). This assessment of the tolerability of antidepressants is correct, but is generalized. To clarify it, one should refer to the data on the mechanisms of the formation of side effects. nine0013
A smaller part of them is due to the toxic effect of antidepressants on the organs and tissues of patients. These “toxic” side effects are very dangerous (10). For example, while taking some TcA (clomipramine, imipramine), as well as MeA (agomelaptin), drug-induced hepatitis is observed, which leads to the death of patients (10, 11). Serious toxic side effects are also found in maprotiline, which causes agranulocytosis and leukopenia (12).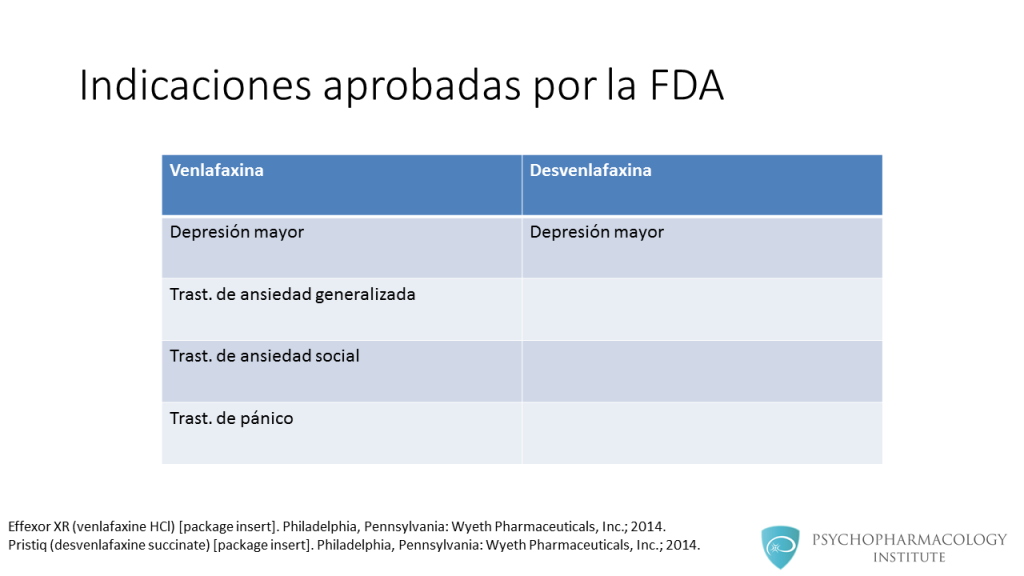 Fortunately, toxic side effects are very rare and can be detected in a timely manner by test results. nine0013
Fortunately, toxic side effects are very rare and can be detected in a timely manner by test results. nine0013
For example, when agomelatine was found to cause severe and drug-induced hepatitis, detailed precautionary instructions were added to its package leaflet (11). They include a biochemical blood test, which is prescribed to all patients (without exception) before prescribing the drug, as well as while taking it. A similar analysis is required for patients receiving clomipramine and imipramine (13,14). However, when prescribing these antidepressants, biochemical analysis is required only for patients with pre-existing liver disease. Finally, regular CBCs to detect agranulocytosis and leukopenia are also required during treatment with maprotiline (12). nine0013
Obviously, the need for additional tests can significantly complicate the use of antidepressants. Fortunately, this is only required when using the listed drugs. When prescribing other antidepressants, you do not need to resort to additional examinations. However, their tolerability may worsen due to the adverse effects of drugs on neurons. As a result, "neuronal" side effects are formed, which, however, do not directly threaten the lives of patients and are easily diagnosed by their complaints. nine0013
However, their tolerability may worsen due to the adverse effects of drugs on neurons. As a result, "neuronal" side effects are formed, which, however, do not directly threaten the lives of patients and are easily diagnosed by their complaints. nine0013
Some of the neuronal side effects are due to the effect of the antidepressant on histamine and acetylcholine neurons, which do not decrease their activity in the formation of mental disorders that are indications for antidepressant prescription (2,15). Accordingly, such pharmacological properties can be designated as "extra-therapeutic" (unnecessary, not related to the treatment process) side effects. They only increase the number of neuronal systems that suffer in the patient. Most often, "extra-curative" side effects are persistent. They may occur throughout the course of treatment, particularly when the antidepressant blocks excitatory receptors on histamine and acetylcholine neurons (15). nine0013
This mechanism of action, which is more characteristic of antipsychotics than antidepressants, leads to a sharp drop in the activity (inhibition) of these nerve cells (↓G and ↓A) (1,2). Moreover, normal histamine and acetylcholine neurons cannot restore their functions, since there are no effective compensatory mechanisms for this. Accordingly, patients develop persistent mental and somatic symptoms that seriously complicate treatment (Table 2).
Moreover, normal histamine and acetylcholine neurons cannot restore their functions, since there are no effective compensatory mechanisms for this. Accordingly, patients develop persistent mental and somatic symptoms that seriously complicate treatment (Table 2).
Table 2. The main "extra-therapeutic" side effects of antidepressants associated with the blockade of excitatory receptors on histamine and acetylcholine neurons (1,2)
Drowsiness, fatigue, deterioration of memory and attention are characteristic. There are complaints of dry mouth, disturbances of accommodation and urination, constipation, pain in the eyes due to an increase in intraocular pressure, heart rhythm disturbances, increased appetite and weight gain.
There is, however, an antidepressant that does not have permanent "off-the-shelf" side effects. This drug is vortioxetine. It does not inhibit histamine and acetylcholine neurons (due to the blockade of excitatory receptors), but increases their "tone" by influencing regulatory receptors (16).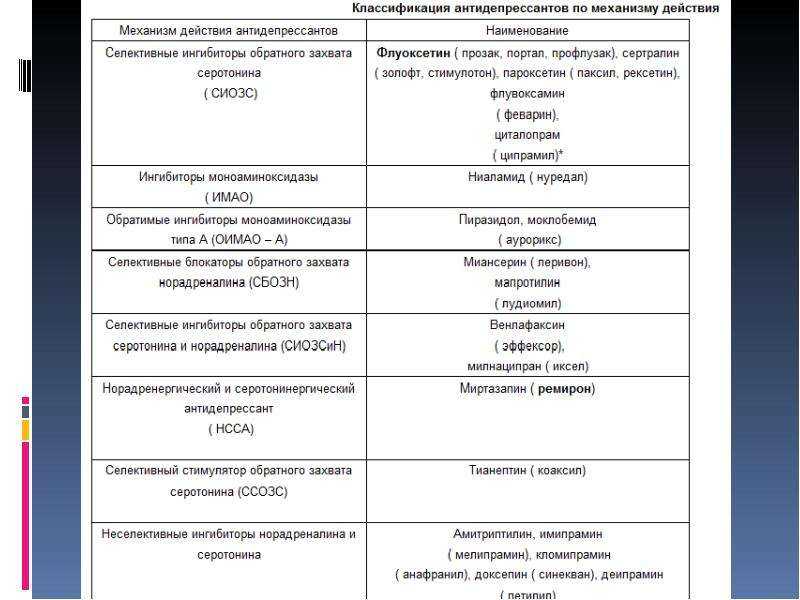 On the one hand, this provides vortioxetine with a unique nature of “non-therapeutic” side effects. In particular, when taking this antidepressant, excitement, anger, "unusual" dreams, and insomnia can be observed (Table 3). nine0013
On the one hand, this provides vortioxetine with a unique nature of “non-therapeutic” side effects. In particular, when taking this antidepressant, excitement, anger, "unusual" dreams, and insomnia can be observed (Table 3). nine0013
Table 3. "Extra-curative" side effects of vortioxetine (16,17).
Characterized by ketoacidosis, somatic complaints of dizziness, itching (including generalized), sweating, hot flashes, nausea, diarrhea, vomiting. On the other hand, these side effects are fundamentally reversible, since neurons have special mechanisms that are aimed at combating excessive activation. To do this, they can, for example, desensitize their regulatory receptors (a mechanism known as self-regulation). Therefore, the “non-therapeutic” side effects of vortioxetine often resolve spontaneously within the first two weeks of treatment (16). nine0013
Turning now to the rest of the antidepressants, we point out that the vast majority of them do not have "extra-curative" side effects at all, which increase the number of affected neuronal systems (2). Many drugs do not affect histamine and acetylcholine neurons. Moreover, they increase the activity of only those neurons (serotonin, norepinephrine and dopamine), whose "tone" is reduced in mental disorders, which are indications for the appointment of antidepressants. However, even this feature cannot save antidepressants from "neuronal" side effects. The latter will arise due to the fact that within any affected system of neurons, the activity of only part of the nerve cells decreases, while the functions of the other part are not disturbed. Antidepressants both activate the "affected" neurons and create therapeutic effects, and increase the "tone" of normally functioning nerve cells and cause side effects. nine0013
Many drugs do not affect histamine and acetylcholine neurons. Moreover, they increase the activity of only those neurons (serotonin, norepinephrine and dopamine), whose "tone" is reduced in mental disorders, which are indications for the appointment of antidepressants. However, even this feature cannot save antidepressants from "neuronal" side effects. The latter will arise due to the fact that within any affected system of neurons, the activity of only part of the nerve cells decreases, while the functions of the other part are not disturbed. Antidepressants both activate the "affected" neurons and create therapeutic effects, and increase the "tone" of normally functioning nerve cells and cause side effects. nine0013
At the same time, the tolerability of antidepressants paradoxically turns out to be a “hostage” of their therapeutic properties. The more effectively the drug activates the affected neurons, the more it affects similar nerve cells that are still functioning at the proper level.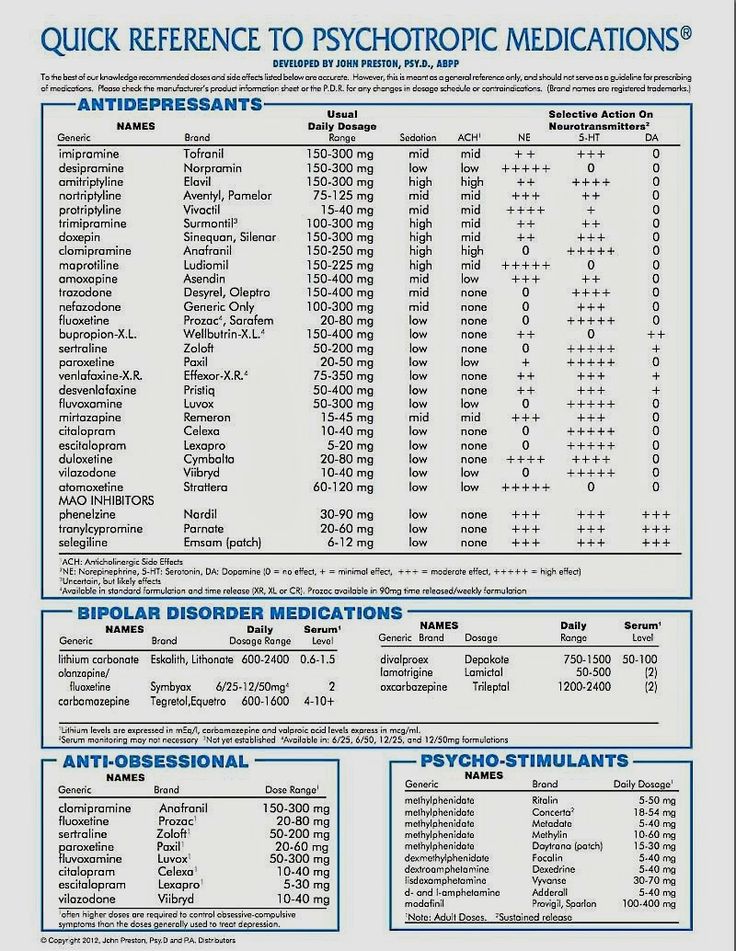 Therefore, it is advisable to designate the side effects under consideration as “paratherapeutic”. They are manifested by anxiety, restlessness, insomnia and anxiety (Table 4).
Therefore, it is advisable to designate the side effects under consideration as “paratherapeutic”. They are manifested by anxiety, restlessness, insomnia and anxiety (Table 4).
Table 4. Main "paratherapeutic" side effects of antidepressants (15)
Somatic complaints are represented by sexual dysfunction, disruption of the digestive organs and heart rhythm, fluctuations in blood pressure. As a rule, "paratherapeutic" side effects are reversible. They may resolve on their own in the second or third week of treatment (18). This is due to the above-mentioned ability of "normal" neurons to quickly adapt to excessive activation, reducing their sensitivity to neurotransmitters (2) 2 .
The presented data on toxic and neuronal side effects can be used to classify antidepressants into seven tolerability categories, where the last, seventh, is the worst, and the first is the best (Table 5).
Table 5. Antidepressant tolerance categories based on toxic and neuronal side effects.
Antidepressant tolerance categories based on toxic and neuronal side effects.
Thus, antidepressants from the lowest category VII (clomipramine, imipramine, maprotiline, agomelatine) have toxic side effects that directly threaten the lives of patients. Moreover, their appointment requires additional examination of patients. Problems with tolerability of other antidepressants are already due to neuronal side effects. All of them are not fatal, and additional examination is usually not required to identify them. nine0013
Neuronal side effects are divided into "extra-therapeutic" and "para-therapeutic". The first, as already mentioned above, are associated with an "additional" dysfunction of histamine and acetylcholine neurons, which do not reduce their activity in mental disorders, which are indications for prescribing antidepressants. Accordingly, "non-therapeutic" side effects, expanding the range of affected neuronal systems, determine the belonging of drugs to lower tolerance categories (VI, V and IV). In particular, amitriptyline contributes to a persistent decrease in the activity of histamine and acetylcholine neurons and is therefore classified as tolerability category VI. “Extra-curative” side effects for Category V antidepressants are more limited. After all, pipofezin, trazodone, mianserin and mirtazapine contribute to a persistent decrease in the activity of only histamine neurons. Vortioxetine is assigned to the next higher tolerance category IV. This antidepressant has the ability to increase the activity of histamine and acetylcholine neurons. However, the associated side effects are often reversible. nine0013
In particular, amitriptyline contributes to a persistent decrease in the activity of histamine and acetylcholine neurons and is therefore classified as tolerability category VI. “Extra-curative” side effects for Category V antidepressants are more limited. After all, pipofezin, trazodone, mianserin and mirtazapine contribute to a persistent decrease in the activity of only histamine neurons. Vortioxetine is assigned to the next higher tolerance category IV. This antidepressant has the ability to increase the activity of histamine and acetylcholine neurons. However, the associated side effects are often reversible. nine0013
The highest tolerance categories I-III include antidepressants that affect only serotonin, norepinephrine and dopamine neurons, which suffer from mental disorders that are indications for prescribing drugs. These drugs are characterized by "paratherapeutic" side effects that do not increase the number of affected neuronal systems (Table 5). They arise due to the activation of a part of serotonin, norepinephrine and dopamine neurons, which still retain their normal "tone" (2).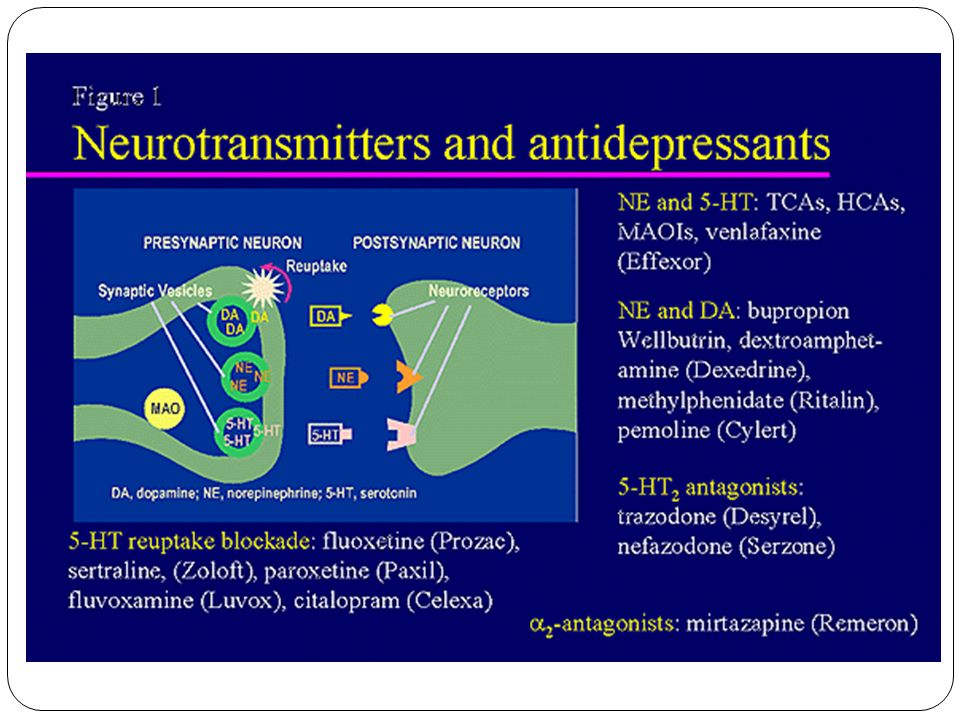 At the same time, the severity of "paratherapeutic" side effects depends, first of all, on the ability of the antidepressant to act on serotonin and norepinephrine nerve cells, since they all have little effect on dopamine (Table 1). nine0013
At the same time, the severity of "paratherapeutic" side effects depends, first of all, on the ability of the antidepressant to act on serotonin and norepinephrine nerve cells, since they all have little effect on dopamine (Table 1). nine0013
Accordingly, antidepressants, which simultaneously effectively activate serotonin and norepinephrine neurons, are assigned to category III of tolerance. These drugs are venlafaxine and duloxetine (Tables 1 and 5). The first of them, depending on the dose, is ↑CH- or ↑CHd-antidepressant. As for duloxetine, it has the properties of a ↑CH drug. Category II includes antidepressants that contribute to a pronounced activation of only serotonin or only norepinephrine neurons (Tables 1 and 5). These include all ↑C-antidepressants (sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine), as well as ↑cHd antidepressant - milnacipran. Finally, drugs that are not capable of strong activation of serotonin and norepinephrine neurons have the highest tolerance category I (Tables 1 and 5). These are two ↑snd antidepressants - pirlindol and moclobemide. nine0013
These are two ↑snd antidepressants - pirlindol and moclobemide. nine0013
In conclusion, it should be noted that the presented classification of antidepressants according to tolerability does not claim to be comprehensive. However, it provides clear criteria for assessing the main side effects, which allow you to compare different drugs with each other. It seems that this is especially important in a situation where there are no clear recommendations for taking into account side effects when prescribing antidepressants. For example, a generalized formula is currently used in various publications and instructions. An antidepressant is suggested to be used "only after careful assessment of the expected benefit/risk ratio in patients" (11). But the results of such a "thorough assessment" tend to be in favor of prescribing the drug. nine0013
In particular, they write about agomelatine that if all the requirements of the instructions for prescribing an antidepressant are met, then the risk of developing drug-induced hepatitis becomes minimal (19). However, the unique mechanism of action attributed to agomelatine suggests that the benefits of prescribing an antidepressant are far greater than the disadvantages associated with its hepatotoxicity (19). Meanwhile, all the uniqueness of the mechanism of action of agomelatine is reduced to the possibility of influencing the neurons of the suprachiasmatic nucleus, the neurotransmitter of which is melatonin. And this effect is not required at all for the treatment of depression, since any antidepressant that activates serotonin and norepinephrine neurons can compensate for the deficiency of melatonin activity (20). nine0013
However, the unique mechanism of action attributed to agomelatine suggests that the benefits of prescribing an antidepressant are far greater than the disadvantages associated with its hepatotoxicity (19). Meanwhile, all the uniqueness of the mechanism of action of agomelatine is reduced to the possibility of influencing the neurons of the suprachiasmatic nucleus, the neurotransmitter of which is melatonin. And this effect is not required at all for the treatment of depression, since any antidepressant that activates serotonin and norepinephrine neurons can compensate for the deficiency of melatonin activity (20). nine0013
The recommendations for "thorough evaluation" presented here are not the only examples of flippant judgments about the tolerability of antidepressants. Some authors believe that side effects are weakly related to the mechanism of action of drugs. Side effects are said to be non-specific, probabilistic and therefore almost unpredictable (18). Other authors are at least looking for the reasons for the formation of side effects in order to take them into account when prescribing antidepressants.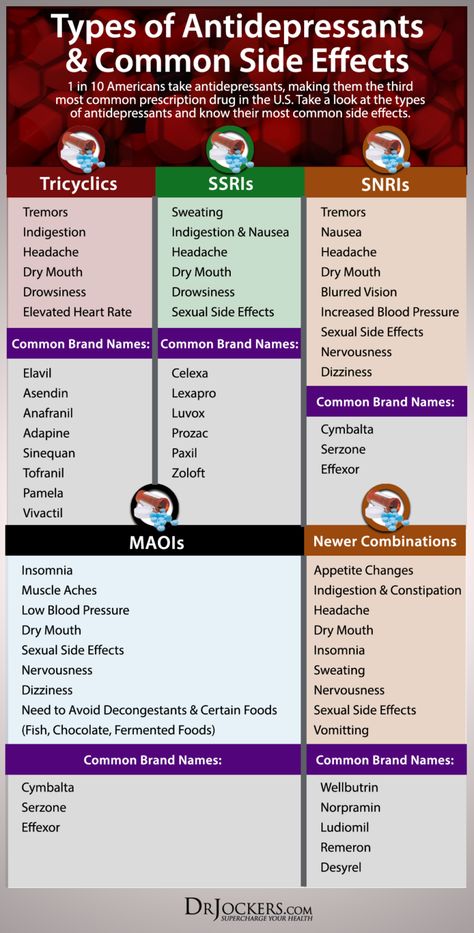 Unfortunately, they find these reasons not in the mechanisms of action of drugs, but in the characteristics of depression, public opinion or the psychology of the patient. nine0013
Unfortunately, they find these reasons not in the mechanisms of action of drugs, but in the characteristics of depression, public opinion or the psychology of the patient. nine0013
Thus, it is reported that even with the use of any of the “most easily tolerated drugs in 80% of patients with mild to moderate depression” (21), heterogeneous adverse events are noted. They are most common in dysthymia, first depressive states, with anxiety and somatic symptoms (21, 22), in persons over 45 years of age, with a high body weight deficit (22), and a history of negative placebo reactions in anamnesis (23). Poor tolerability of antidepressants has been reported to be associated with patients' high demands for quality of life (24) and their anxiety about social exclusion (25). The initially negative attitude towards psychiatry on the part of public opinion, the patient's low awareness of his own illness and the therapy recommended by the doctor, the unsatisfactory experience of previous treatment, etc. , also contribute to the problem. (22, 26). nine0013
, also contribute to the problem. (22, 26). nine0013
The speculation of such constructions is obvious. To refute them, it suffices to say that the side effects of drugs, as defined by the WHO, are caused by their pharmacological properties (37). It is hard to imagine that the inhibition of histamine and acetylcholine neurons arose due to the patient's high demands on the quality of life, the excessive activation of serotonin, norepinephrine and dopamine neurons due to the negative attitude towards psychiatry on the part of public opinion, and drug-induced hepatitis due to anxiety about social maladaptation. nine0013
Thus, the presented classification of antidepressants according to tolerability categories allows us to return the study of side effects to the mainstream of biological psychiatry. In addition, this classification is easy to use in practical medicine. In particular, the lower the tolerability category of an antidepressant, the greater the need for a special justification for prescribing it (effectiveness, positive experience of treatment in the past, the patient's desire, etc. ). In turn, the appearance of such a detailed justification in the history of the disease will help to avoid many problems (psychological, social and others) that arise in the process of treatment between the doctor and his patient. nine0013
). In turn, the appearance of such a detailed justification in the history of the disease will help to avoid many problems (psychological, social and others) that arise in the process of treatment between the doctor and his patient. nine0013
With the help of the presented classification, it is easy to decide on the choice of the most effective and tolerable antidepressant. To do this, it is only necessary to compare the tolerability categories of the most effective drugs: amitriptyline (TcA), imipramine (TcA) and venlafaxine (SNRI) (5). The first of them (amitriptyline) belongs to the VI category of tolerance (Table 5). The side effects of the second antidepressant (imipramine) are even worse. This drug belongs to the VII category of tolerance. As for venlafaxine, the side effects of this antidepressant are much weaker, and this drug belongs to category III tolerance. Thus, venlafaxine, when used at high doses, is the most effective and tolerated drug in the treatment of depression.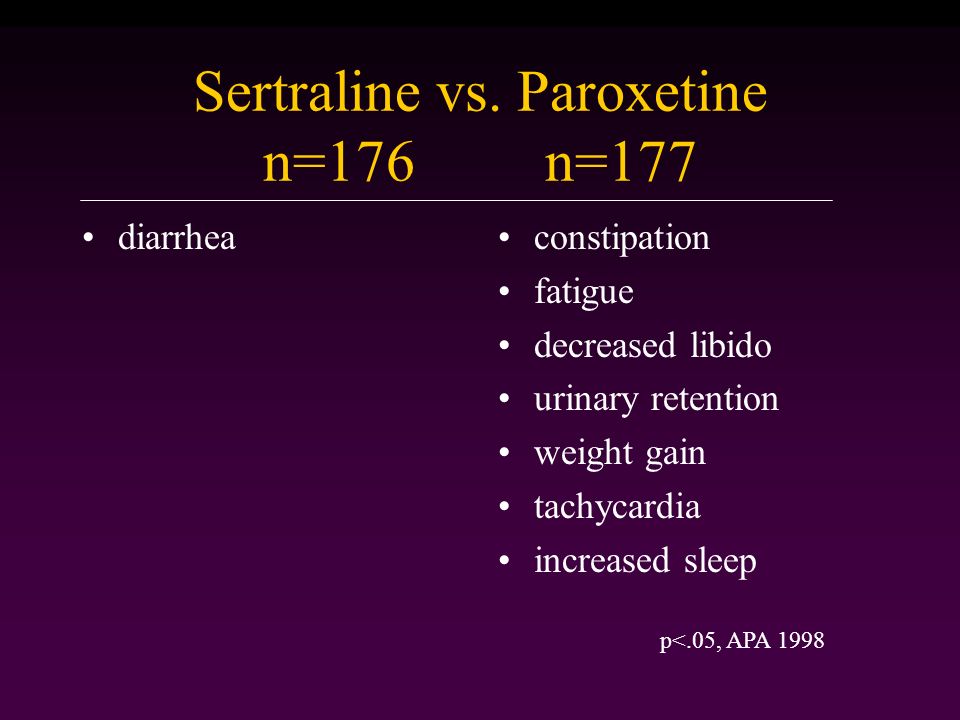 nine0013
nine0013
Venlafaksin is well-known in our country under the trade name Velaksin (Egis). This drug has been studied in leading scientific organizations that carry out cutting-edge research in the field of psychiatry. Among them are the Federal State Budgetary Institutions “State Scientific Center for Social and Forensic Psychiatry named after V.P. Serbsky" and "Moscow Research Institute of Psychiatry" of the Ministry of Health of Russia, St. Petersburg Research Institute. V.M. Bekhterev (28.29). Prolonged-release capsules (Velaxin retard) (30) are also well-known, with the use of which there is a significant reduction in the frequency of such a side effect of the drug as nausea (31). In addition, the study of Velaksin was successfully carried out not only in psychiatry, but also in neurology (32). nine0013
M.Yu Drobizhev's video on the same topic can be viewed at the link: https://www.youtube.com/watch?v=SwtO_bC_838&t=11s
References
- Antidepressant therapy and other treatments for depressive disorders.
 Report of the CINP Working Group based on a review of the evidence. Ed. V.N. Krasnov. M., 2008. - 215 S.
Report of the CINP Working Group based on a review of the evidence. Ed. V.N. Krasnov. M., 2008. - 215 S. - Stahl S.M. Stahl's essential psychopharmacology: neuroscientific basis and practical application. — 3nd ed. Cambridge University Press, 2008. - 1117P. nine0049
- Drobizhev M. Yu., Fedotova A. V., Kikta S. V., Antokhin E. Yu. Between depression and fibromyalgia: the fate of an antidepressant. Journal of Neurology and Psychiatry. S.S. Korsakov. 2016;116(4): 114-120. DOI:10.17116/jnevro201611641114-120.,
- Shagiakhmetov F.Sh., Anokhin P.K., Shamakina I.Yu. Vortioxetine: mechanisms of multimodality and clinical efficacy. Social and Clinical Psychiatry 2016;26(4): 84-96
- Bauer M., Pfennig A., Severus E., Weibrau P.S., J. Angst, Müller H.-J. Clinical guidelines of the World Federation of Societies of Biological Psychiatry for the biological therapy of unipolar depressive disorders. Part 1: Acute and ongoing treatment of unipolar depressive disorders as of 2013.
 Modern therapy of mental disorders 2015;4:33-39.).
Modern therapy of mental disorders 2015;4:33-39.). - Anderson IM. SSRIS versus tricyclic antidepressants in depressed inpatients: a meta-analysis of efficacy and tolerability. depression. Anxiety. 1998;7(Suppl 1):11-17.
- Anderson IM, Nutt DJ, Deakin JF. Evidence based guidelines for treating depressive disorders with antidepressants: a revision of the 1993 British Association for Psychopharmacology guidelines. J Psychopharmacol. 2000;14:3-20.
- Peretti S, Judge R, Hindmarch I. Safety and tolerability considerations: tricyclic antidepressants vs. selective serotonin reuptake inhibitors. Acta Psychiatr. Scand. 2000; Suppl. 403:17-25. nine0049
- Wilson K, Mottram P, Sivanranthan A, Nightingale A. Antidepressant versus placebo for depressed elderly. 2001 Cochrane. database. Syst. Rev. CD000561.) and worse for TcA
- Liver Tox. https://livertox.nlm.nih.gov
- Valdoxan - instructions for the medical use of the drug.
 https://medi.ru/instrukciya/valdoksan_5084/
https://medi.ru/instrukciya/valdoksan_5084/ - Lyudiomil - official instructions for use. https://medi.ru/instrukciya/lyudiomil_9448/
- Anafranil tablets - instructions (information for specialists) on the use of the drug. https://medi.ru/instrukciya/anafranil-tabletki_8616/
- Melipramine tablets - official instructions for use. https://medi.ru/instrukciya/melipramin-tabletki_4780/
- Drobizhev M.Yu., Ovchinnikov A.A., Kikta S.V. Why do antidepressants have side effects? Pharmateka. 2015. No. 20 (313). pp. 72-77.
- Brintellix (Brintellix). https://www.rlsnet.ru/tn_index_id_87791.htm
- Subeesh V, Singh H, Maheswari E, Beulah E. Novel adverse events of vortioxetine: A disproportionality analysis in USFDA adverse event reporting system database. Asian J Psychiatr. 2017 Dec;30:152-156. doi: 10.1016/j.ajp.2017.09.005.
- Borodin V.I. Tolerability of treatment in patients with depressive disorders (complex analysis).
 Abstract for the competition … doc. honey. Sciences. Moscow. 2009.
Abstract for the competition … doc. honey. Sciences. Moscow. 2009. - Freiesleben SD, Furczyk K.J A systematic review of agomelatine-induced liver injury. Mol Psychiatry. 2015 Apr 21;3(1):4. doi: 10.1186/s40303-015-0011-7. eCollection 2015.
- Drobizhev M.Yu. Timing of meta-analyses and efficacy of antidepressants in depression. Social and clinical psychiatry. 2017;4:81-88. nine0049
- Aldushin A.A. Antidepressant therapy tolerance and withdrawal forecast based on the analysis of nocebo effects. Russian psychiatric journal. 2009; 3:55-61.
- Avedisova A.S., Borodin V.I., Aldushin A.A. Comparison of the efficacy and tolerability of antidepressants of different groups in mild and moderate depression. Journal of Neurology and Psychiatry. S.S. Korsakov. 2006;11:15-19.
- Lapin I.P. Personality and medicine. Introduction to the psychology of pharmacotherapy. - St. Petersburg: Dean, 2001.-416C. nine0049
- Roberis H.
 Neurotic patients who terminate their own treatment. Br. J. Psychiatry. 1985; 146(4):443-445.
Neurotic patients who terminate their own treatment. Br. J. Psychiatry. 1985; 146(4):443-445. - Mosolov S.N., red. Reference guide to psychopharmacology. Psychopharmacological and antiepileptic drugs approved for use in Russia: 2nd ed. BINOM, Moscow, 2004. - 304C.
- Avedisova A.S., Borodin V.I. Non-compliance or refusal of psychopharmacotherapy? Russian psychiatric journal. 2006; 1:61-65.
- http://vmede.org/sait/?id=Farmakologija_klin_farm_y4ebnik_kykes_2009&menu=Farmakologija_klin_farm_y4ebnik_kykes_2009&page=7
- Krasnov V.N., Kryukov V.V. Velaxin® (venlafaxine) in modern therapy of depression: results of the first Russian multicenter efficacy and safety study. Psychiatry and psychopharmacotherapy. 2007;9 (4), http://www.consilium-medicum.com/magazines/special/psychiatry/article/15426
- Mosolov S.N., Kostyukova E.G., Gorodnichev A.V., Timofeev I.V., Ladyzhensky M.Ya., Serditov O.V. Clinical efficacy and tolerability of venlafaxine (Velaxin) in the treatment of moderate and severe depression.
 Modern therapy of mental disorders. 2007;3:58-63. nine0049
Modern therapy of mental disorders. 2007;3:58-63. nine0049 - Avedisova A.S., Zakharova K.V., Kanaeva L.S., Vazagaeva T.I., Aldushin A.A. Psychiatry and psychopharmacotherapy. 2009;11(1):36-40.
- Avedisova A.S. Venlafaxine (velaxin): results of international trials of a third-generation antidepressant. Psychiatrist. and a psychopharmacologist. 2006; 11(2):2-7.
- Mosolov S.N. Clinical use of modern antidepressants. SPb., 1995.-565C.).
M.Yu. Drobizhev , Doctor of Medical Sciences, Head of the Educational Department of the Training Center of the Association of Medical and Pharmaceutical Universities of Russia. Contact information – [email protected]
E.Yu. Antokhin , Candidate of Medical Sciences, Associate Professor, Head of the Department of Clinical Psychology and Psychotherapy, Orenburg State Medical University of the Russian Ministry of Health.
nine0030 R.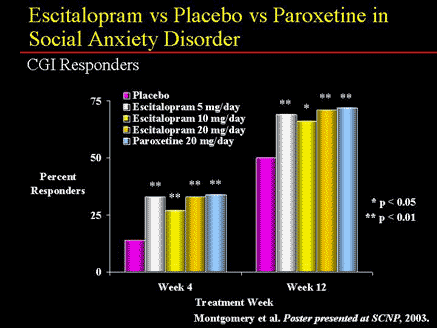 I. Palaeva – Assistant of the Department of Clinical Psychology and Psychotherapy, Orenburg State Medical University, Ministry of Health of Russia.
I. Palaeva – Assistant of the Department of Clinical Psychology and Psychotherapy, Orenburg State Medical University, Ministry of Health of Russia.
S. V. Kikta , candidate of medical sciences, head. Department of the Federal State Budgetary Institution "Polyclinic No. 3" of the Administration of the President of the Russian Federation, Moscow
1 Probably, there are also side effects due to excessive activation of melatonin nerve cells. However, they are not yet described even in the instructions for agomelatine, a melatonergic drug that has a direct effect on them (11). nine0013
2 Theoretically, “paratherapeutic” side effects can be observed even against the background of “extra-therapeutic” ones. After all, any antidepressants to varying degrees activate serotonin, norepinephrine or dopamine neurons. However, drugs are dominated by "extra-curative" side effects, if only because they are most often persistent.