Depression chest heaviness
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems.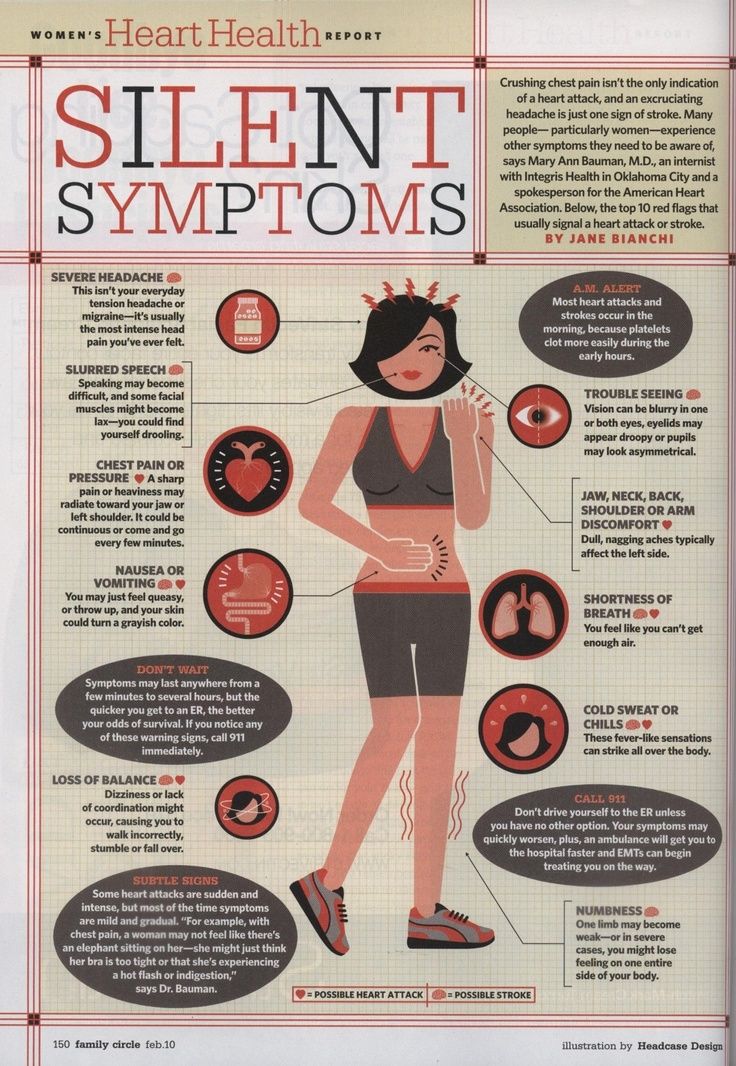 Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse.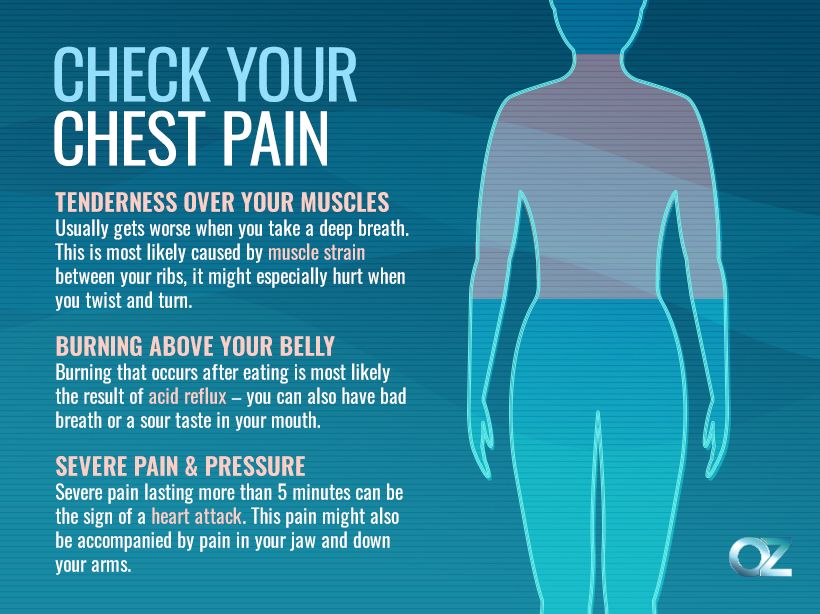 Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
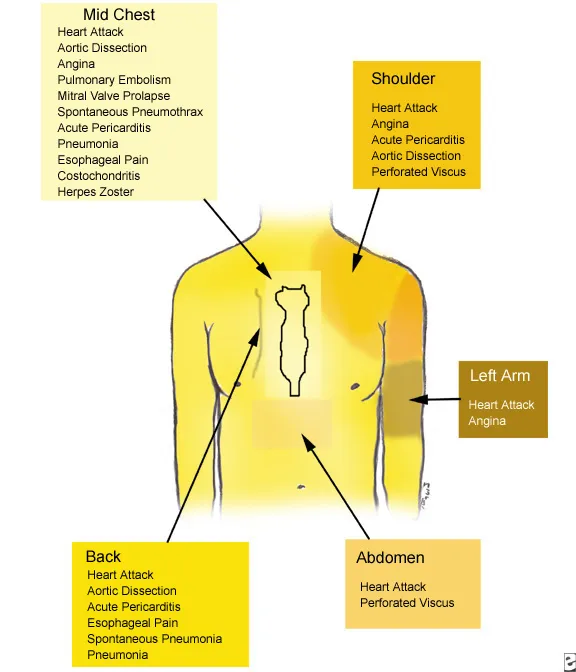
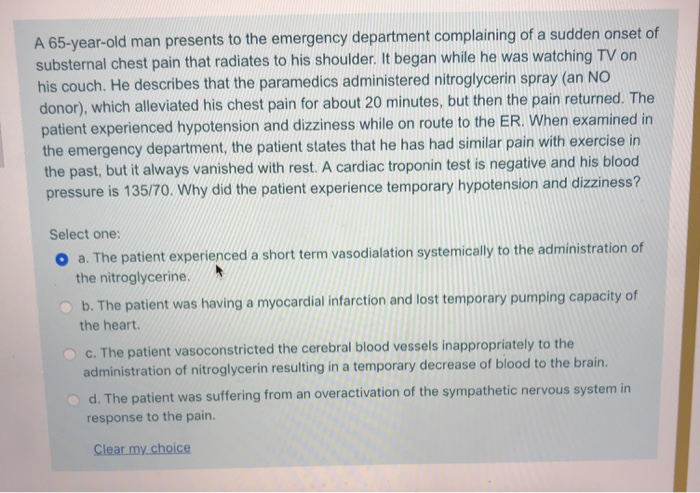
Heaviness in the chest - causes, diagnosis and treatment
Heaviness in the chest appears with psycho-emotional disorders (stress, panic, depression), diseases of the circulatory system (IHD, pericarditis and myocarditis, cardiomyopathy), respiration (pneumonia, bronchial asthma, tuberculosis ). Diagnostic search includes standard instrumental methods: ECG and Holter monitoring, echocardiography, chest x-ray. To clarify what caused the heaviness in the chest area, they also carry out invasive diagnostics - coronary angiography, puncture, scintigraphy. Relief of symptoms is usually performed by medical methods, surgical interventions are less often used.
Relief of symptoms is usually performed by medical methods, surgical interventions are less often used.
Causes of heaviness in the chest
Physiological factors
As a rule, a person encounters an unpleasant heaviness in the chest with severe fear or anxiety. There is a feeling that everything is shrinking inside, pulling or aching pains appear. Symptoms are accompanied by interruptions in work or a feeling of sinking heart. Discomfort in the chest is sometimes perceived as the beginning of a heart attack, but the condition returns to normal immediately after the person calms down, and the traumatic factor disappears.
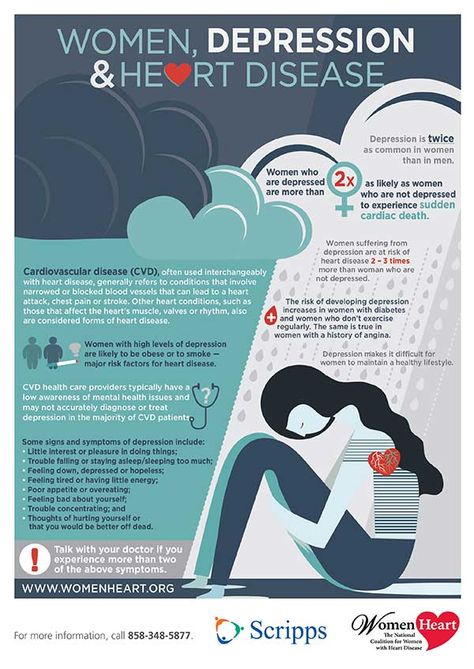
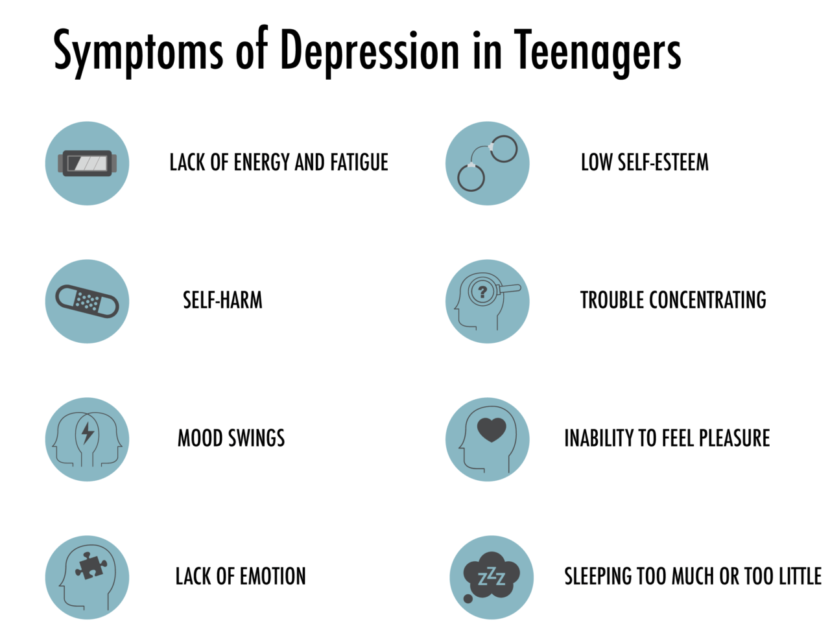
Depression
Heaviness with nagging chest pain, which is most pronounced in the first hours after waking up, is pathognomonic for masked depression. Patients are concerned about discomfort in the precordial region, sometimes the condition is aggravated by pressing or squeezing pain. Characteristically, there are no mood changes typical for depression, so patients are confident that they have a cardiac disease.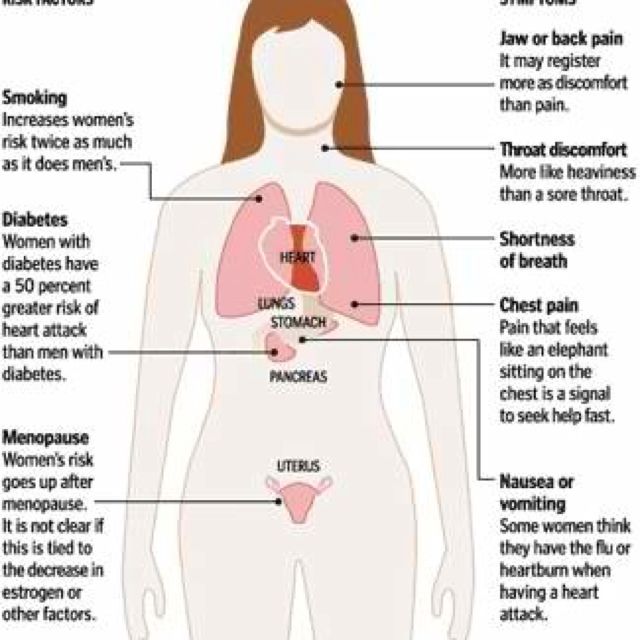
Diseases of the cardiovascular system
Heaviness, discomfort in the projection of the chest are often associated with cardiac problems. In such cases, the symptoms are more typical for middle-aged and elderly people. Unpleasant sensations are often combined with tingling or pain in the heart, shortness of breath during exercise, swelling of the lower extremities. Heaviness in the chest is a manifestation of heart lesions such as:
- ischemic heart disease. Stable angina is characterized by intermittent episodes of chest tightness, constricting pain. Severity develops at the beginning of the paroxysm, provoked by physical activity or stress. Sometimes the symptom continues to disturb the patient even in the periods between angina attacks.
- Myocarditis. Pathology manifests itself suddenly, more often in young patients. A person complains of heaviness with moderate aching pain in the chest, accompanied by shortness of breath, fever.
 Sometimes there are interruptions in the heart rhythm.
Sometimes there are interruptions in the heart rhythm. - Pericarditis. With exudative inflammation of the pericardium, patients feel increasing heaviness, tightness in the chest, progressive shortness of breath. Changing the position of the body does not affect the intensity of symptoms. Swelling of the jugular veins and puffiness of the face are usually noticeable.
- Cardiomyopathy. Non-inflammatory heart disease is characterized by persistent or intermittent heaviness in the chest, which bothers a person for several months or even years. Manifestations are moderate, do not interfere with normal life, so patients go to the doctor only in case of an exacerbation of the problem and the development of heart failure.
- Cardiac tamponade. Patients experience sudden heaviness in the chest, inability to breathe deeply, severe weakness and cold sweat. The condition is life-threatening, without medical help it ends with collapse or acute heart failure.

- Postinfarction syndrome. The disease is characterized by the appearance of pressing pains and heaviness in the chest 2-4 weeks after myocardial infarction. Patients notice a deterioration in well-being, an increase in shortness of breath and weakness, discomfort in the chest cavity. Often the clinical picture is supplemented by fever.
Heaviness in the chest
Diseases of the respiratory organs
Damage to the bronchopulmonary system is another common cause of heaviness, pressing and constricting sensations in different parts of the chest. The symptom most often occurs within the framework of typical inflammatory processes: acute and chronic bronchitis, pneumonia. Discomfort increases during coughing attacks or attempts to take a deep breath. Heaviness in the chest is accompanied by fever, weakness, secretion of mucous or purulent sputum.
In chronic processes - tuberculosis, pneumoconiosis - patients complain of periodic tightness in the chest area, incomprehensible discomfort or aching sensations.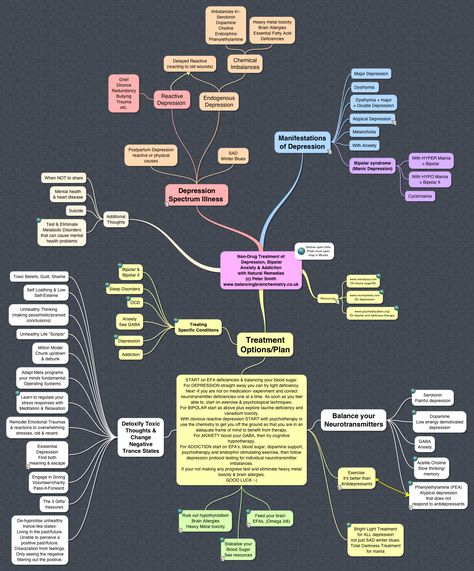 Manifestations occur without a visible provoking factor, persist for many months. With an exacerbation of the pathology, heaviness in the chest is replaced by dull pain.
Manifestations occur without a visible provoking factor, persist for many months. With an exacerbation of the pathology, heaviness in the chest is replaced by dull pain.
Attacks of heaviness and a feeling of chest compression are observed during an exacerbation of bronchial asthma. Unpleasant symptoms develop as harbingers of a paroxysm of suffocation, accompanied by nasal congestion, skin itching, and coughing. In the interictal period, chest heaviness is experienced by patients with moderate and severe asthma.
Damage to the mediastinum
Heaviness and periodic pain in the chest are found in chronic mediastinitis. Symptoms are slightly expressed, periodically they intensify and are supplemented by fever. Patients complain of pressing or dull pains without a clear localization, discomfort at the time of deep inspiration and coughing. Similar manifestations occur with neoplasms of the mediastinum: thymoma, lymphoma, cysts.
Rare causes
- Poisonings : citrate intoxication, hydrogen sulfide poisoning.
- Diseases of the digestive system : GERD, achalasia of the cardia, dilatation of the esophagus.
- Emergencies : anaphylactic shock, heat stroke, toxic pulmonary edema.
Diagnosis
A comprehensive examination is started by a therapist or family doctor. The specialist conducts a physical examination and identifies the leading pathological syndrome, if necessary, sends the patient for a consultation with narrow specialists (pulmonologist, cardiologist). To establish a diagnosis, the results of instrumental and laboratory studies are required, of which the following are prescribed more often than others:
- X-ray of OGK. Radiation diagnostics helps to differentiate cardiac and pulmonary pathology. The defeat of the respiratory system is manifested by focal infiltrates, rounded shadows, increased vascular pattern. Signs of cardiac problems are changes in the size and configuration of the shadow of the heart, congestion in the lungs.

- Electrocardiography. ECG measures the electrical activity of the myocardium. On the cardiogram, a decrease in the voltage of the teeth or their inversion, deviation of the axis of the heart, signs of disturbances in the conduction system of the myocardium are found. Of great diagnostic value is daily ECG monitoring, bicycle ergometric test.
- Echocardiography. Ultrasound diagnostics shows structural and functional abnormalities in the activity of the heart. The method is necessary for the diagnosis of pericarditis (effusion in the heart bag), cardiomyopathy (expansion of cavities or thickening of the walls of the organ). Echocardiography measures the contractile function of the left ventricular myocardium.
- Invasive methods. In case of pathological processes in the pericardium, a diagnostic puncture is performed for bacteriological and cytological examination of the exudate. In coronary artery disease, coronary angiography is performed to assess the degree of vascular damage.
 The functional state of the myocardium is determined by perfusion scintigraphy.
The functional state of the myocardium is determined by perfusion scintigraphy. - Laboratory diagnostics. Analyzes are of secondary importance. In cardiac pathology, an extended biochemical study is indicated with the determination of the lipid spectrum and acute phase parameters, the measurement of myocardial markers. Diagnosis of pulmonary diseases requires microscopy and sputum culture.
Echocardiography
Treatment
Help before diagnosis
Heaviness in the chest occurs when various organs and systems are damaged, so self-treatment at home is unacceptable and is fraught with the progression of the underlying disease, the development of complications. Patients experiencing chest discomfort are advised not to delay contacting a therapist. If compressive pains are felt in the chest, the person has suffocation, febrile fever, and emergency medical care is required.
Conservative therapy
Treatment measures are selected after identifying the causes of the condition. Heaviness in the chest does not require special symptomatic therapy and disappears after the elimination of the underlying pathology. All patients are prescribed a sparing motor regimen, the maximum limitation of stress and psycho-traumatic factors. Medicamentous action includes medicines of the following pharmacological groups:
- Antianginal agents . Used in combination for long-term therapy of coronary heart disease. They are supplemented with antiplatelet agents for the prevention of myocardial infarction and thrombosis. Nitrates are recommended for the relief of angina attacks.
- Anti-inflammatory drugs . Non-steroidal anti-inflammatory drugs are indicated for myocarditis and pericarditis, acute respiratory diseases. They act pathogenetically, and also relieve unpleasant and painful sensations. If non-steroidal drugs are ineffective, corticosteroids are taken.
- Antibiotics . Antimicrobial drugs are prescribed for pneumonia, pleurisy, purulent bronchitis as an etiotropic treatment.
Antibiotics of the penicillin series are effective in inflammatory lesions of the heart against the background of rheumatism. For the treatment of tuberculosis, 3-4 specific drugs are combined.
- Antiallergics . Leukotriene receptor antagonists and mast cell membrane stabilizers are used for the basic therapy of bronchial asthma. Classical antihistamines are used as pathogenetic therapy for many inflammatory processes with an allergic component.
- Metabolic preparations . To improve the delivery and utilization of oxygen in the myocardium under conditions of ischemia, it is necessary to take cytoprotectors. The therapy is enhanced with ascorbic acid and B vitamins, which accelerate metabolic processes in the body.
Surgery
Minimally invasive therapies such as pleural and pericardial puncture are widely used. The intervention is carried out to eliminate exudate, which impedes the normal functioning of the organ, to eliminate heaviness, pain in the chest. Surgical treatment of CAD includes percutaneous balloon angioplasty, stenting, or coronary artery bypass grafting.
Heaviness in the chest - causes, diagnosis and treatment
Heaviness in the chest appears with psycho-emotional disorders (stress, panic, depression), diseases of the circulatory system (IHD, pericarditis and myocarditis, cardiomyopathy), respiration (pneumonia, bronchial asthma, tuberculosis). Diagnostic search includes standard instrumental methods: ECG and Holter monitoring, echocardiography, chest x-ray. To clarify what caused the heaviness in the chest area, they also carry out invasive diagnostics - coronary angiography, puncture, scintigraphy. Relief of symptoms is usually performed by medical methods, surgical interventions are less often used.
Causes of heaviness in the chest
Physiological factors
As a rule, a person encounters an unpleasant heaviness in the chest with severe fear or anxiety. There is a feeling that everything is shrinking inside, pulling or aching pains appear. Symptoms are accompanied by interruptions in work or a feeling of sinking heart. Discomfort in the chest is sometimes perceived as the beginning of a heart attack, but the condition returns to normal immediately after the person calms down, and the traumatic factor disappears.
Depression
Heaviness with nagging chest pain, which is most pronounced in the first hours after waking up, is pathognomonic for masked depression. Patients are concerned about discomfort in the precordial region, sometimes the condition is aggravated by pressing or squeezing pain. Characteristically, there are no mood changes typical for depression, so patients are confident that they have a cardiac disease.
Diseases of the cardiovascular system
Heaviness, discomfort in the projection of the chest are often associated with cardiac problems. In such cases, the symptoms are more typical for middle-aged and elderly people. Unpleasant sensations are often combined with tingling or pain in the heart, shortness of breath during exercise, swelling of the lower extremities. Heaviness in the chest is a manifestation of heart lesions such as:
- ischemic heart disease. Stable angina is characterized by intermittent episodes of chest tightness, constricting pain. Severity develops at the beginning of the paroxysm, provoked by physical activity or stress. Sometimes the symptom continues to disturb the patient even in the periods between angina attacks.
- Myocarditis. Pathology manifests itself suddenly, more often in young patients. A person complains of heaviness with moderate aching pain in the chest, accompanied by shortness of breath, fever. Sometimes there are interruptions in the heart rhythm.
- Pericarditis. With exudative inflammation of the pericardium, patients feel increasing heaviness, tightness in the chest, progressive shortness of breath.
Changing the position of the body does not affect the intensity of symptoms. Swelling of the jugular veins and puffiness of the face are usually noticeable.
- Cardiomyopathy. Non-inflammatory heart disease is characterized by persistent or intermittent heaviness in the chest, which bothers a person for several months or even years. Manifestations are moderate, do not interfere with normal life, so patients go to the doctor only in case of an exacerbation of the problem and the development of heart failure.
- Cardiac tamponade. Patients experience sudden heaviness in the chest, inability to breathe deeply, severe weakness and cold sweat. The condition is life-threatening, without medical help it ends with collapse or acute heart failure.
- Postinfarction syndrome. The disease is characterized by the appearance of pressing pains and heaviness in the chest 2-4 weeks after myocardial infarction. Patients notice a deterioration in well-being, an increase in shortness of breath and weakness, discomfort in the chest cavity.
Often the clinical picture is supplemented by fever.
Heaviness in the chest
Diseases of the respiratory organs
Damage to the bronchopulmonary system is another common cause of heaviness, pressing and constricting sensations in different parts of the chest. The symptom most often occurs within the framework of typical inflammatory processes: acute and chronic bronchitis, pneumonia. Discomfort increases during coughing attacks or attempts to take a deep breath. Heaviness in the chest is accompanied by fever, weakness, secretion of mucous or purulent sputum.
In chronic processes - tuberculosis, pneumoconiosis - patients complain of periodic tightness in the chest area, incomprehensible discomfort or aching sensations. Manifestations occur without a visible provoking factor, persist for many months. With an exacerbation of the pathology, heaviness in the chest is replaced by dull pain.
Attacks of heaviness and a feeling of chest compression are observed during an exacerbation of bronchial asthma. Unpleasant symptoms develop as harbingers of a paroxysm of suffocation, accompanied by nasal congestion, skin itching, and coughing. In the interictal period, chest heaviness is experienced by patients with moderate and severe asthma.
Damage to the mediastinum
Heaviness and periodic pain in the chest are found in chronic mediastinitis. Symptoms are slightly expressed, periodically they intensify and are supplemented by fever. Patients complain of pressing or dull pains without a clear localization, discomfort at the time of deep inspiration and coughing. Similar manifestations occur with neoplasms of the mediastinum: thymoma, lymphoma, cysts.
Rare causes
- Poisonings : citrate intoxication, hydrogen sulfide poisoning.
- Diseases of the digestive system : GERD, achalasia of the cardia, dilatation of the esophagus.
- Emergencies : anaphylactic shock, heat stroke, toxic pulmonary edema.
Diagnosis
A comprehensive examination is started by a therapist or family doctor. The specialist conducts a physical examination and identifies the leading pathological syndrome, if necessary, sends the patient for a consultation with narrow specialists (pulmonologist, cardiologist). To establish a diagnosis, the results of instrumental and laboratory studies are required, of which the following are prescribed more often than others:
- X-ray of OGK. Radiation diagnostics helps to differentiate cardiac and pulmonary pathology. The defeat of the respiratory system is manifested by focal infiltrates, rounded shadows, increased vascular pattern. Signs of cardiac problems are changes in the size and configuration of the shadow of the heart, congestion in the lungs.
- Electrocardiography. ECG measures the electrical activity of the myocardium. On the cardiogram, a decrease in the voltage of the teeth or their inversion, deviation of the axis of the heart, signs of disturbances in the conduction system of the myocardium are found.
Of great diagnostic value is daily ECG monitoring, bicycle ergometric test.
- Echocardiography. Ultrasound diagnostics shows structural and functional abnormalities in the activity of the heart. The method is necessary for the diagnosis of pericarditis (effusion in the heart bag), cardiomyopathy (expansion of cavities or thickening of the walls of the organ). Echocardiography measures the contractile function of the left ventricular myocardium.
- Invasive methods. In case of pathological processes in the pericardium, a diagnostic puncture is performed for bacteriological and cytological examination of the exudate. In coronary artery disease, coronary angiography is performed to assess the degree of vascular damage. The functional state of the myocardium is determined by perfusion scintigraphy.
- Laboratory diagnostics. Analyzes are of secondary importance. In cardiac pathology, an extended biochemical study is indicated with the determination of the lipid spectrum and acute phase parameters, the measurement of myocardial markers.
Diagnosis of pulmonary diseases requires microscopy and sputum culture.
Echocardiography
Treatment
Help before diagnosis
Heaviness in the chest occurs when various organs and systems are damaged, so self-treatment at home is unacceptable and is fraught with the progression of the underlying disease, the development of complications. Patients experiencing chest discomfort are advised not to delay contacting a therapist. If compressive pains are felt in the chest, the person has suffocation, febrile fever, and emergency medical care is required.
Conservative therapy
Treatment measures are selected after identifying the causes of the condition. Heaviness in the chest does not require special symptomatic therapy and disappears after the elimination of the underlying pathology. All patients are prescribed a sparing motor regimen, the maximum limitation of stress and psycho-traumatic factors. Medicamentous action includes medicines of the following pharmacological groups:
- Antianginal agents . Used in combination for long-term therapy of coronary heart disease. They are supplemented with antiplatelet agents for the prevention of myocardial infarction and thrombosis. Nitrates are recommended for the relief of angina attacks.
- Anti-inflammatory drugs . Non-steroidal anti-inflammatory drugs are indicated for myocarditis and pericarditis, acute respiratory diseases. They act pathogenetically, and also relieve unpleasant and painful sensations. If non-steroidal drugs are ineffective, corticosteroids are taken.
- Antibiotics . Antimicrobial drugs are prescribed for pneumonia, pleurisy, purulent bronchitis as an etiotropic treatment. Antibiotics of the penicillin series are effective in inflammatory lesions of the heart against the background of rheumatism. For the treatment of tuberculosis, 3-4 specific drugs are combined.