Symptoms of post traumatic stress disorder include
Post-traumatic stress disorder (PTSD) - Symptoms and causes
Overview
Post-traumatic stress disorder (PTSD) is a mental health condition that's triggered by a terrifying event — either experiencing it or witnessing it. Symptoms may include flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event.
Most people who go through traumatic events may have temporary difficulty adjusting and coping, but with time and good self-care, they usually get better. If the symptoms get worse, last for months or even years, and interfere with your day-to-day functioning, you may have PTSD.
Getting effective treatment after PTSD symptoms develop can be critical to reduce symptoms and improve function.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Post-traumatic stress disorder symptoms may start within one month of a traumatic event, but sometimes symptoms may not appear until years after the event. These symptoms cause significant problems in social or work situations and in relationships. They can also interfere with your ability to go about your normal daily tasks.
PTSD symptoms are generally grouped into four types: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions. Symptoms can vary over time or vary from person to person.
Intrusive memories
Symptoms of intrusive memories may include:
- Recurrent, unwanted distressing memories of the traumatic event
- Reliving the traumatic event as if it were happening again (flashbacks)
- Upsetting dreams or nightmares about the traumatic event
- Severe emotional distress or physical reactions to something that reminds you of the traumatic event
Avoidance
Symptoms of avoidance may include:
- Trying to avoid thinking or talking about the traumatic event
- Avoiding places, activities or people that remind you of the traumatic event
Negative changes in thinking and mood
Symptoms of negative changes in thinking and mood may include:
- Negative thoughts about yourself, other people or the world
- Hopelessness about the future
- Memory problems, including not remembering important aspects of the traumatic event
- Difficulty maintaining close relationships
- Feeling detached from family and friends
- Lack of interest in activities you once enjoyed
- Difficulty experiencing positive emotions
- Feeling emotionally numb
Changes in physical and emotional reactions
Symptoms of changes in physical and emotional reactions (also called arousal symptoms) may include:
- Being easily startled or frightened
- Always being on guard for danger
- Self-destructive behavior, such as drinking too much or driving too fast
- Trouble sleeping
- Trouble concentrating
- Irritability, angry outbursts or aggressive behavior
- Overwhelming guilt or shame
For children 6 years old and younger, signs and symptoms may also include:
- Re-enacting the traumatic event or aspects of the traumatic event through play
- Frightening dreams that may or may not include aspects of the traumatic event
Intensity of symptoms
PTSD symptoms can vary in intensity over time. You may have more PTSD symptoms when you're stressed in general, or when you come across reminders of what you went through. For example, you may hear a car backfire and relive combat experiences. Or you may see a report on the news about a sexual assault and feel overcome by memories of your own assault.
You may have more PTSD symptoms when you're stressed in general, or when you come across reminders of what you went through. For example, you may hear a car backfire and relive combat experiences. Or you may see a report on the news about a sexual assault and feel overcome by memories of your own assault.
When to see a doctor
If you have disturbing thoughts and feelings about a traumatic event for more than a month, if they're severe, or if you feel you're having trouble getting your life back under control, talk to your doctor or a mental health professional. Getting treatment as soon as possible can help prevent PTSD symptoms from getting worse.
If you have suicidal thoughts
If you or someone you know has suicidal thoughts, get help right away through one or more of these resources:
- Reach out to a close friend or loved one.
- Contact a minister, a spiritual leader or someone in your faith community.
- Contact a suicide hotline.
 In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential. - Make an appointment with your doctor or a mental health professional.
When to get emergency help
If you think you may hurt yourself or attempt suicide, call 911 or your local emergency number immediately.
If you know someone who's in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person to keep him or her safe. Call 911 or your local emergency number immediately. Or, if you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
You can develop post-traumatic stress disorder when you go through, see or learn about an event involving actual or threatened death, serious injury or sexual violation.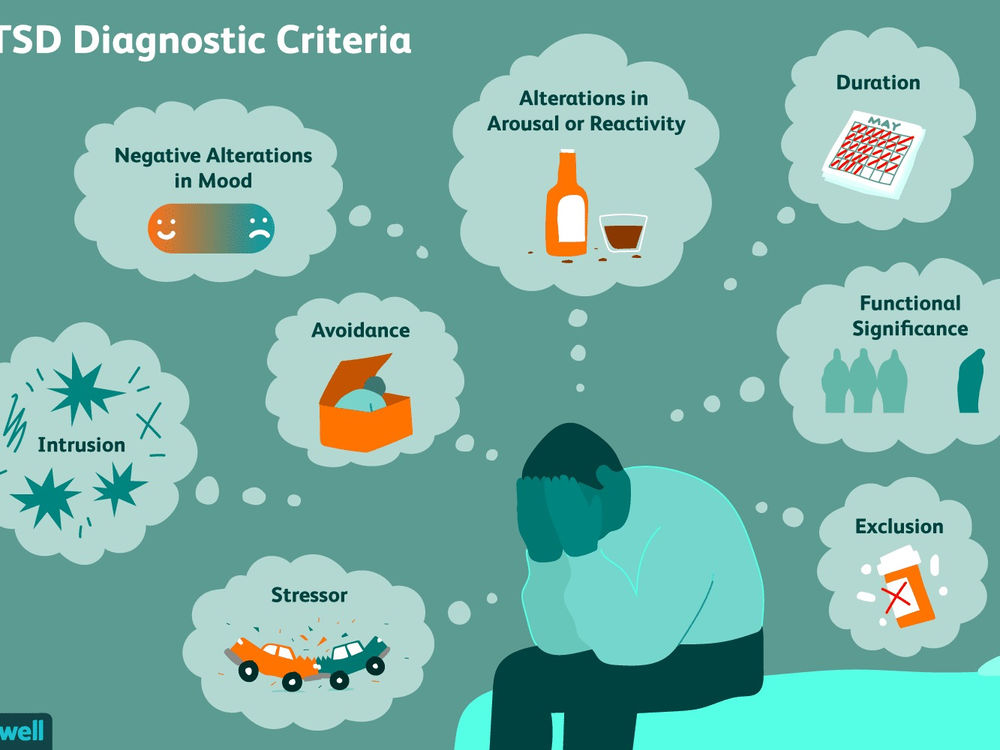
Doctors aren't sure why some people get PTSD. As with most mental health problems, PTSD is probably caused by a complex mix of:
- Stressful experiences, including the amount and severity of trauma you've gone through in your life
- Inherited mental health risks, such as a family history of anxiety and depression
- Inherited features of your personality — often called your temperament
- The way your brain regulates the chemicals and hormones your body releases in response to stress
Risk factors
People of all ages can have post-traumatic stress disorder. However, some factors may make you more likely to develop PTSD after a traumatic event, such as:
- Experiencing intense or long-lasting trauma
- Having experienced other trauma earlier in life, such as childhood abuse
- Having a job that increases your risk of being exposed to traumatic events, such as military personnel and first responders
- Having other mental health problems, such as anxiety or depression
- Having problems with substance misuse, such as excess drinking or drug use
- Lacking a good support system of family and friends
- Having blood relatives with mental health problems, including anxiety or depression
Kinds of traumatic events
The most common events leading to the development of PTSD include:
- Combat exposure
- Childhood physical abuse
- Sexual violence
- Physical assault
- Being threatened with a weapon
- An accident
Many other traumatic events also can lead to PTSD, such as fire, natural disaster, mugging, robbery, plane crash, torture, kidnapping, life-threatening medical diagnosis, terrorist attack, and other extreme or life-threatening events.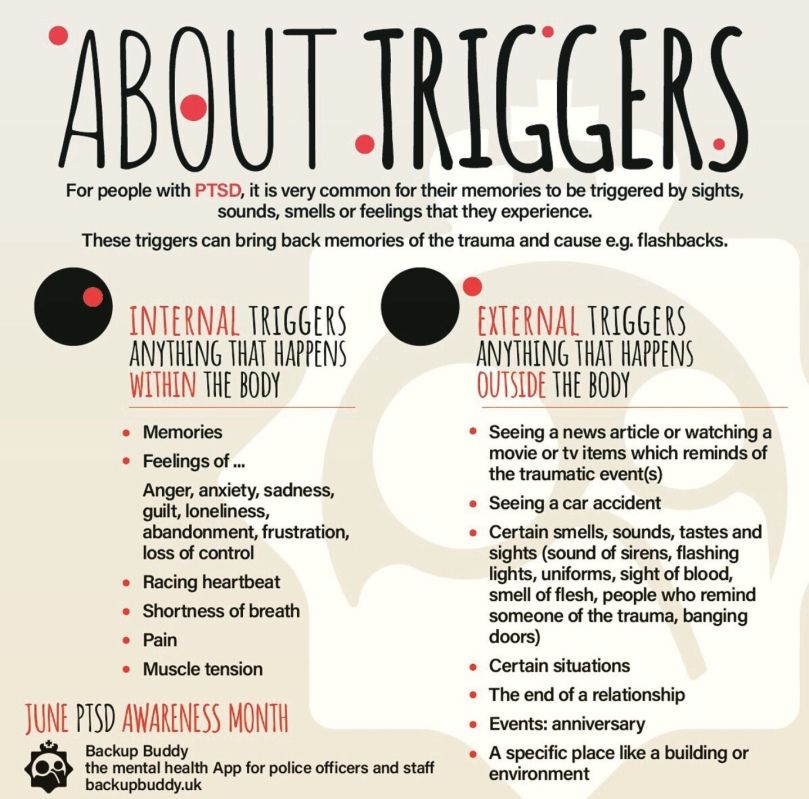
Complications
Post-traumatic stress disorder can disrupt your whole life ― your job, your relationships, your health and your enjoyment of everyday activities.
Having PTSD may also increase your risk of other mental health problems, such as:
- Depression and anxiety
- Issues with drugs or alcohol use
- Eating disorders
- Suicidal thoughts and actions
Prevention
After surviving a traumatic event, many people have PTSD-like symptoms at first, such as being unable to stop thinking about what's happened. Fear, anxiety, anger, depression, guilt — all are common reactions to trauma. However, the majority of people exposed to trauma do not develop long-term post-traumatic stress disorder.
Getting timely help and support may prevent normal stress reactions from getting worse and developing into PTSD. This may mean turning to family and friends who will listen and offer comfort. It may mean seeking out a mental health professional for a brief course of therapy. Some people may also find it helpful to turn to their faith community.
Some people may also find it helpful to turn to their faith community.
Support from others also may help prevent you from turning to unhealthy coping methods, such as misuse of alcohol or drugs.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
NIMH » Post-Traumatic Stress Disorder
What is post-traumatic stress disorder, or PTSD?
Some people develop post-traumatic stress disorder (PTSD) after experiencing a shocking, scary, or dangerous event.
It is natural to feel afraid during and after a traumatic situation. Fear is a part of the body’s normal “fight-or-flight” response, which helps us avoid or respond to potential danger. People may experience a range of reactions after trauma, and most will recover from their symptoms over time. Those who continue to experience symptoms may be diagnosed with PTSD.
Who develops PTSD?
Anyone can develop PTSD at any age. This includes combat veterans as well as people who have experienced or witnessed a physical or sexual assault, abuse, an accident, a disaster, a terror attack, or other serious events. People who have PTSD may feel stressed or frightened, even when they are no longer in danger.
This includes combat veterans as well as people who have experienced or witnessed a physical or sexual assault, abuse, an accident, a disaster, a terror attack, or other serious events. People who have PTSD may feel stressed or frightened, even when they are no longer in danger.
Not everyone with PTSD has been through a dangerous event. In some cases, learning that a relative or close friend experienced trauma can cause PTSD.
According to the National Center for PTSD, a program of the U.S. Department of Veterans Affairs, about seven or eight of every 100 people will experience PTSD in their lifetime. Women are more likely than men to develop PTSD. Certain aspects of the traumatic event and some biological factors (such as genes) may make some people more likely to develop PTSD.
What are the symptoms of PTSD?
Symptoms of PTSD usually begin within 3 months of the traumatic incident, but they sometimes emerge later. To meet the criteria for PTSD, symptoms must last longer than 1 month, and they must be severe enough to interfere with aspects of daily life, such as relationships or work.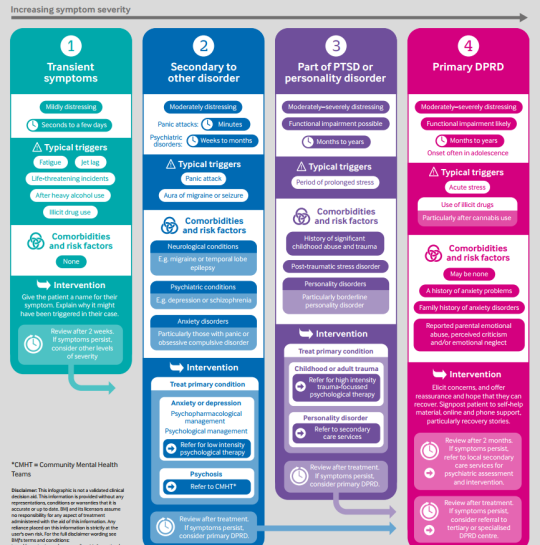 The symptoms also must be unrelated to medication, substance use, or other illness.
The symptoms also must be unrelated to medication, substance use, or other illness.
The course of the illness varies: Although some people recover within 6 months, others have symptoms that last for a year or longer. People with PTSD often have co-occurring conditions, such as depression, substance use, or one or more anxiety disorders.
After a dangerous event, it is natural to have some symptoms or even to feel detached from the experience, as though you are observing things rather than experiencing them. A health care provider—such as a psychiatrist, psychologist, or clinical social worker—who has experience helping people with mental illnesses can determine whether symptoms meet the criteria for PTSD.
To be diagnosed with PTSD, an adult must have all of the following for at least 1 month:
- At least one re-experiencing symptom
- At least one avoidance symptom
- At least two arousal and reactivity symptoms
- At least two cognition and mood symptoms
Re-experiencing symptoms
- Flashbacks—reliving the traumatic event, including physical symptoms such as a racing heart or sweating
- Reoccurring memories or dreams related to the event
- Distressing thoughts
- Physical signs of stress
Thoughts and feelings can trigger these symptoms, as can words, objects, or situations that are reminders of the event.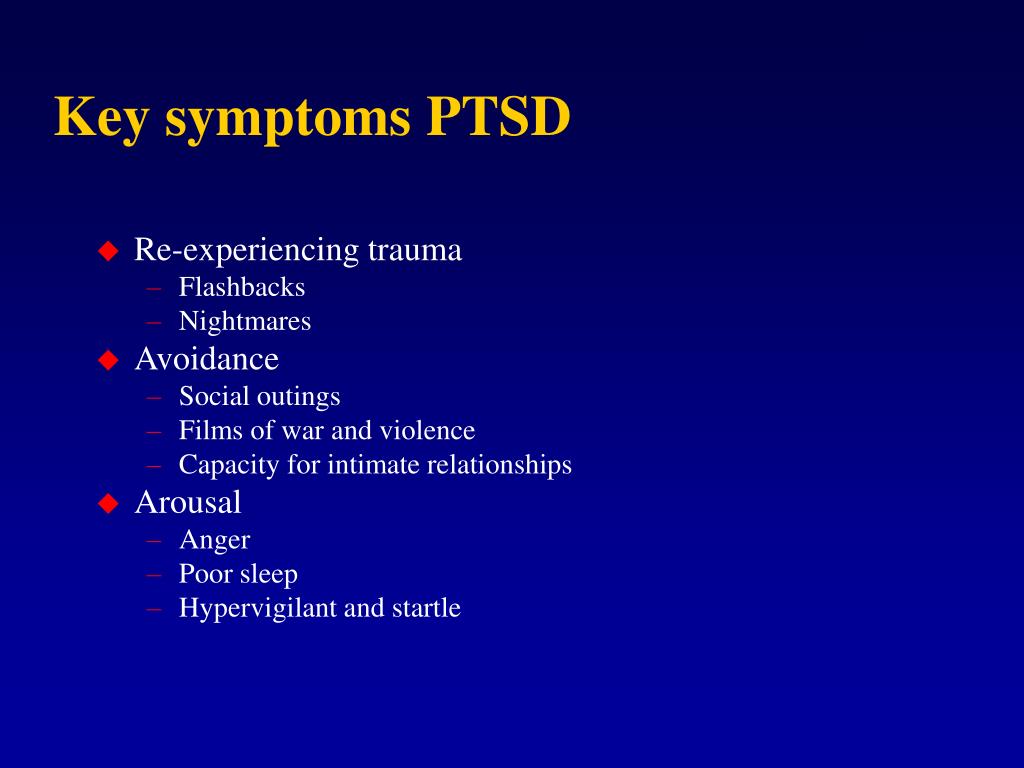
Avoidance symptoms
- Staying away from places, events, or objects that are reminders of the experience
- Avoiding thoughts or feelings related to the traumatic event
Avoidance symptoms may cause people to change their routines. For example, after a serious car accident, a person may avoid driving or riding in a car.
Arousal and reactivity symptoms
- Being easily startled
- Feeling tense, on guard, or “on edge”
- Having difficulty concentrating
- Having difficulty falling asleep or staying asleep
- Feeling irritable and having angry or aggressive outbursts
- Engaging in risky, reckless, or destructive behavior
Arousal symptoms are often present—they can lead to feelings of stress and anger and may interfere with parts of daily life, such as sleeping, eating, or concentrating.
Cognition and mood symptoms
- Trouble remembering key features of the traumatic event
- Negative thoughts about oneself or the world
- Distorted thoughts about the event that cause feelings of blame
- Ongoing negative emotions, such as fear, anger, guilt, or shame
- Loss of interest in previous activities
- Feelings of social isolation
- Difficulty feeling positive emotions, such as happiness or satisfaction
Cognition and mood symptoms can begin or worsen after the traumatic event and can lead a person to feel detached from friends or family members.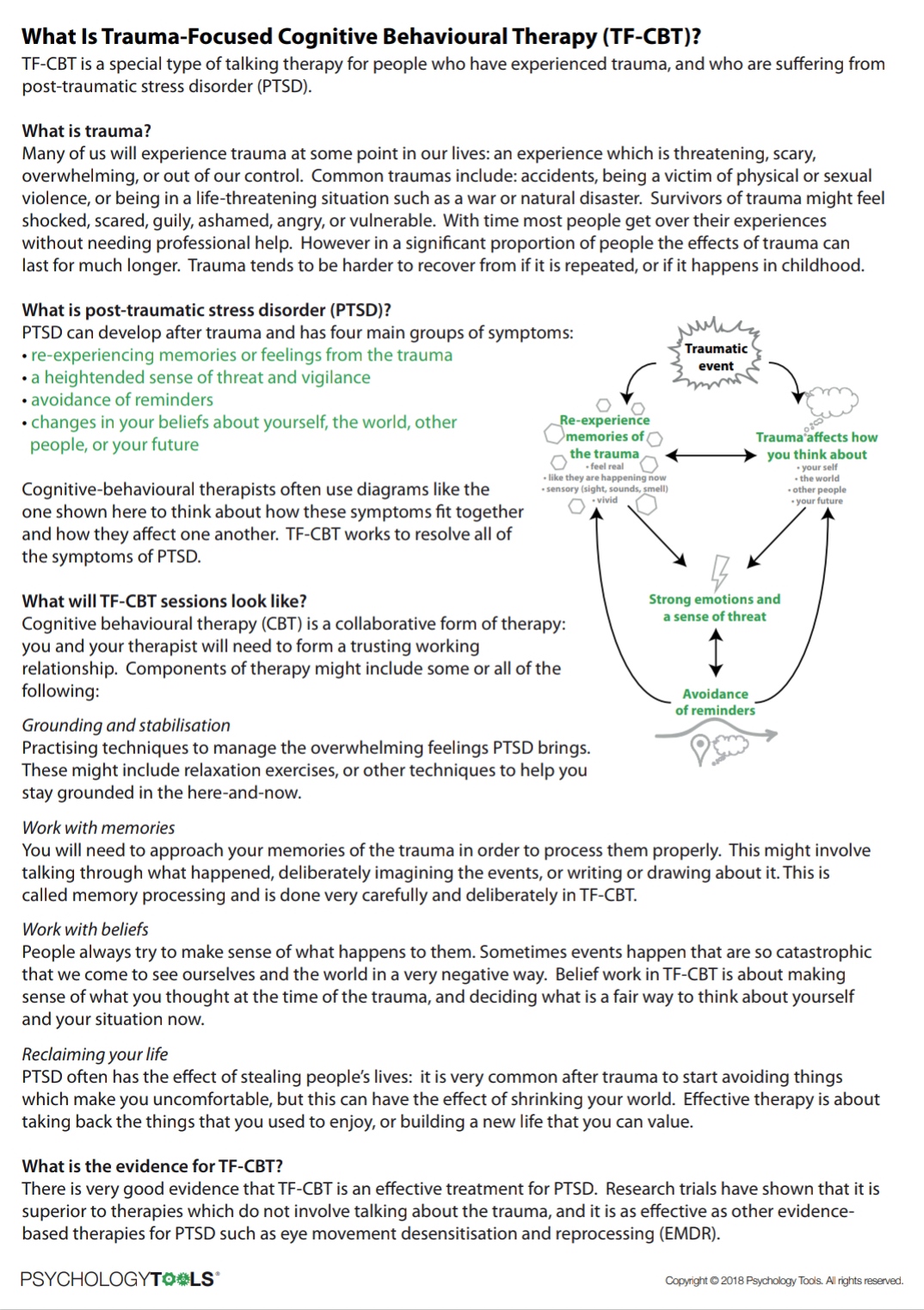
How do children and teens react to trauma?
Children and teens can have extreme reactions to trauma, but their symptoms may not be the same as those seen in adults. In young children under the age of 6, symptoms can include:
- Wetting the bed after having learned to use the toilet
- Forgetting how or being unable to talk
- Acting out the scary event during playtime
- Being unusually clingy with a parent or other adult
Older children and teens usually show symptoms more like those seen in adults. They also may develop disruptive, disrespectful, or destructive behaviors. Older children and teens may feel guilty for not preventing injury or deaths. They also may have thoughts of revenge.
For more information, see the National Institute of Mental Health (NIMH) brochure, Helping Children and Adolescents Cope With Disasters and Other Traumatic Events.
Why do some people develop PTSD and other people do not?
Not everyone who lives through a dangerous event develops PTSD—many factors play a part. Some of these factors are present before the trauma; others become important during and after a traumatic event.
Some of these factors are present before the trauma; others become important during and after a traumatic event.
Risk factors that may increase the likelihood of developing of PTSD include:
- Exposure to dangerous events or traumas
- Getting hurt or seeing people hurt or killed
- Childhood trauma
- Feeling horror, helplessness, or extreme fear
- Having little or no social support after the event
- Dealing with extra stress after the event, such as loss of a loved one, pain and injury, or loss of a job or home
- Having a personal history or family history of mental illness or substance use
Resilience factors that may reduce the likelihood of developing PTSD include:
- Seeking out support from friends, family, or support groups
- Learning to feel okay with one’s actions in response to a traumatic event
- Having a coping strategy for getting through and learning from a traumatic event
- Being prepared and able to respond to upsetting events as they occur, despite feeling fear
How is PTSD treated?
It is important for anyone with PTSD symptoms to work with a mental health professional who has experience treating PTSD. The main treatments are psychotherapy, medications, or both. An experienced mental health professional can help people find the treatment plan that meets their symptoms and needs.
The main treatments are psychotherapy, medications, or both. An experienced mental health professional can help people find the treatment plan that meets their symptoms and needs.
Some people with PTSD may be living through an ongoing trauma, such as being in an abusive relationship. In these cases, treatment is usually most effective when it addresses both the traumatic situation and the symptoms. People who have PTSD or who are exposed to trauma also may experience panic disorder, depression, substance use, or suicidal thoughts. Treatment for these conditions can help with recovery after trauma. Research shows that support from family and friends also can be an important part of recovery.
For tips to help prepare and guide you on how to talk to your health care provider about your mental health and get the most out of your visit, read NIMH’s fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
Psychotherapy
Psychotherapy, sometimes called “talk therapy,” includes a variety of treatment techniques that mental health professionals use to help people identify and change troubling emotions, thoughts, and behaviors.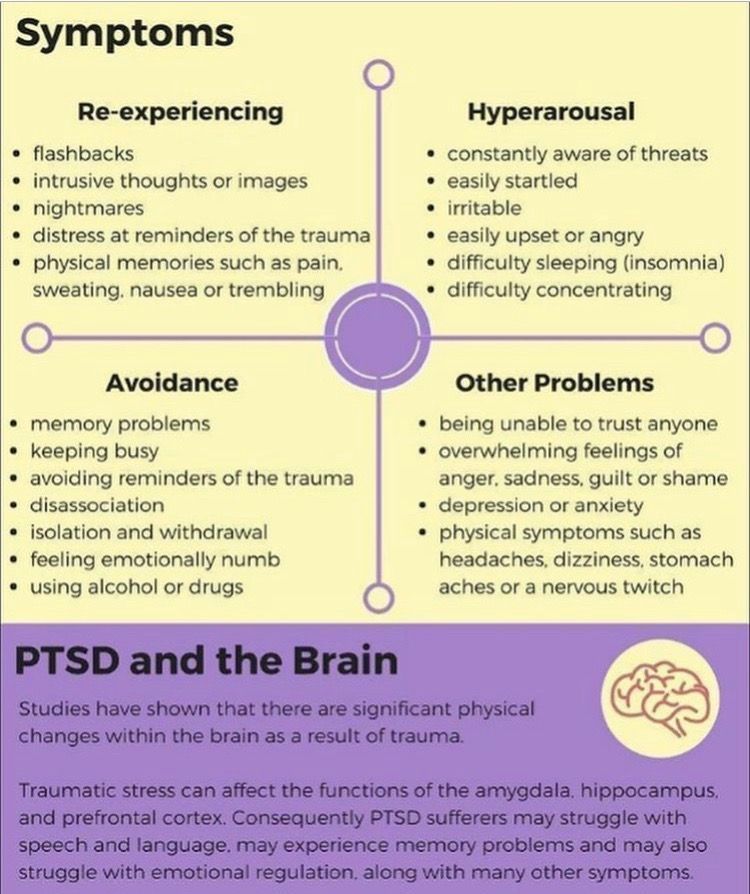 Psychotherapy can provide support, education, and guidance to people with PTSD and their families. This type of treatment can occur one on one or in a group and usually lasts 6 to 12 weeks but can last longer.
Psychotherapy can provide support, education, and guidance to people with PTSD and their families. This type of treatment can occur one on one or in a group and usually lasts 6 to 12 weeks but can last longer.
Some types of psychotherapy target PTSD symptoms, and others focus on social, family, or job-related problems. Effective psychotherapies tend to emphasize a few key components, including learning skills to help identify triggers and manage symptoms.
One common type of psychotherapy, called cognitive behavioral therapy, can include exposure therapy and cognitive restructuring.
- Exposure therapy helps people learn to manage their fear by gradually exposing them, in a safe way, to the trauma they experienced. As part of exposure therapy, people may think or write about the trauma or visit the place where it happened. This therapy can help people with PTSD reduce symptoms that cause them distress.
- Cognitive restructuring helps people make sense of the traumatic event.
 Sometimes people remember the event differently than how it happened, or they may feel guilt or shame about something that is not their fault. Cognitive restructuring can help people with PTSD think about what happened in a realistic way.
Sometimes people remember the event differently than how it happened, or they may feel guilt or shame about something that is not their fault. Cognitive restructuring can help people with PTSD think about what happened in a realistic way.
You can learn more about different types of psychotherapy on the NIMH website.
Medications
The most studied type of medication for treating PTSD is a type of antidepressant medication called selective serotonin reuptake inhibitors (SSRIs). SSRIs may help control PTSD symptoms such as sadness, worry, anger, and feeling emotionally numb. SSRIs and other medications may be prescribed along with psychotherapy. Other medications may help address specific PTSD symptoms, such as sleep problems and nightmares.
Health care providers and patients can work together to find the best medication or combination of medications, as well as the right dose. Check the U.S. Food and Drug Administration website for the latest information on patient medication guides, warnings, or newly approved medications.
How can I find help?
The Substance Abuse and Mental Health Services Administration (SAMHSA) provides the Behavioral Health Treatment Services Locator, an online resource for locating mental health treatment facilities and programs in your state. For additional resources, visit NIMH's Help for Mental Illnesses webpage.
If you or someone you know is in immediate distress or is thinking about hurting themselves, call the National Suicide Prevention Lifeline toll-free at 1-800-273-TALK (8255). You also can text the Crisis Text Line (HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website.
What can I do to help myself?
It is important to know that, although it may take some time, you can get better with treatment. Here are some things you can do to help yourself:
- Talk with your health care provider about treatment options, and follow your treatment plan.
- Engage in exercise, mindfulness, or other activities that help reduce stress.
- Try to maintain routines for meals, exercise, and sleep.
- Set realistic goals and do what you can as you are able.
- Spend time with trusted friends or relatives, and tell them about things that may trigger symptoms.
- Expect your symptoms to improve gradually, not immediately.
- Avoid use of alcohol or drugs.
How can I help a friend or relative who has PTSD?
If you know someone who may be experiencing PTSD, the most important thing you can do is to help that person get the right diagnosis and treatment. Some people may need help making an appointment with their health care provider; others may benefit from having someone accompany them to their health care visits.
If a close friend or relative is diagnosed with PTSD, you can encourage them to follow their treatment plan. If their symptoms do not get better after 6 to 8 weeks, you can encourage them to talk to their health care provider.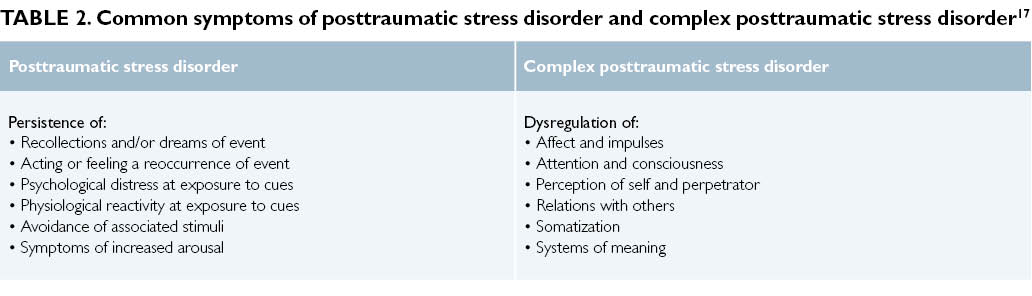 You also can:
You also can:
- Offer emotional support, understanding, patience, and encouragement.
- Learn about PTSD so you can understand what your friend is experiencing.
- Listen carefully. Pay attention to the person’s feelings and the situations that may trigger PTSD symptoms.
- Share positive distractions, such as walks, outings, and other activities.
Where can I find more information on PTSD?
The National Center for PTSD, a program of the U.S. Department of Veterans Affairs, is the leading federal center for research and education on PTSD and traumatic stress. You can find information about PTSD, treatment options, and getting help, as well as additional resources for families, friends, and providers.
What should I know about participating in clinical research?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information, visit NIMH's clinical trials webpage.
Reprints
This publication is in the public domain and may be reproduced or copied without permission from NIMH. Citation of NIMH as a source is appreciated. To learn more about using NIMH publications, visit our reprint guidelines.
For More Information
MedlinePlus (National Library of Medicine) (En español)
ClinicalTrials.gov (En español)
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 20-MH-8124
Revised 2020
Post-traumatic stress disorder (PTSD) | English translation
However, most people realize what happened after a few weeks, sometimes a little longer, and then their symptoms will begin to disappear.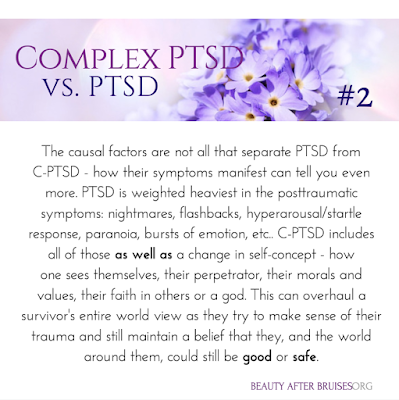
Research shows that certain groups of people are at increased risk of developing post-traumatic stress disorder. The risk of developing PTSD is reduced when a person has:
Any traumatic event can cause PTSD, although the more severe the shock, the more likely it is to develop PTSD. For example, PTSD is more likely to develop if the event:
- is a sudden and unexpected
- lasts a long time
- , it happens when you get into a trap from which
- could not get out of
- deaths
- leads to injuries
- include children
if you are still stressed and in an uncertain state, this will make it difficult to get rid of the symptoms of PTSD.
How do I know that I have overcome a traumatic experience?
You may have already gotten over the traumatic event if you can:
- think about it without worrying
- not feel like you are under constant threat
- not think about it all the time
Why is PTSD not always diagnosed?
There are a number of reasons why a person with PTSD may not be diagnosed.
Stigma and misunderstanding
People with PTSD often avoid talking about their feelings to avoid thinking about the traumatic event.
Some people believe that the symptoms they are experiencing (such as avoidance or emotional numbness) help them cope and do not realize that they are caused by PTSD.
When people are very ill, it is difficult for them to believe that they are able to feel the way they did before the traumatic event. This may discourage them from getting help.
There is also a common misconception that only military personnel suffer from PTSD. In fact, PTSD can happen to anyone, and any experience of PTSD is real.
Misdiagnosis
Some people with PTSD may be misdiagnosed with conditions such as anxiety or depression. Some people have other mental and physical health problems that make PTSD go unnoticed.
They may also experience medically unexplained symptoms such as:
- gastrointestinal disorders
- pain syndromes
- headaches
These symptoms may mean that their PTSD goes unnoticed.
Other difficulties
Some people with PTSD may also have other problems, such as difficulties in human relationships or addiction to alcohol and drugs. They may be caused by post-traumatic stress disorder, but these problems will manifest themselves more clearly than PTSD itself.
Can children develop PTSD?
PTSD can develop at any age. In addition to the symptoms of PTSD common to adults, children may also experience:
- Nightmares - In children, these dreams may or may not reflect an actual traumatic event.
- Repetitive play - some children act out a traumatic event during play. For example, a child who has been in a serious traffic accident may recreate the accident with toy cars.
- Physical symptoms - they may complain of abdominal pain and headaches.
- Fear of imminent death - they may find it hard to believe that they will live long enough to become adults.
What treatments are available for PTSD?
There are a number of different treatments for PTSD, including trauma-focused cognitive behavioral therapy (TF-CBT), eye movement desensitization and processing (EMDR), and medications.
Psychotherapy
Psychotherapy for PTSD will focus on the traumatic experience, not your past life. They will help you:
- Acceptance - learn to accept the fact that although you cannot change what happened, you can think differently about the event, the world around you and your life.
- Memory of the event - remembering what happened, you will not feel fear or anxiety. You will be able to think about what happened when you yourself want it, and not through obsessive thoughts or memories.
- Explaining your experiences in words - by saying out loud what happened, your mind will be able to push the memories away and do other things.
- Finding a sense of security - helps you to better control your feelings. This will make you feel more secure and eliminate the need to avoid memories.
All psychotherapy must be administered by a properly trained and accredited professional. Sessions are usually conducted by the same therapist at least once a week, with a total duration of at least 8-12 weeks.
Sessions usually last about an hour, sometimes they can last up to 90 minutes.
Therapy for PTSD includes:
Trauma-focused Cognitive Behavioral Therapy
A form of talking therapy that can help you change the way you think. Over time, this can help you feel better and behave differently. It is usually done individually, although there is evidence that CBT for trauma can also be done in groups.
Eye Movement Desensitization and Reprocessing (EMDR)
A technique that uses eye movements to help the brain process traumatic memories.
You will be asked to remember the traumatic event and what it made you think and feel. While you do this, you will be prompted to move your eyes or receive other "two-way stimulation" such as tapping your hand. It turns out that this reduces the emotional burden experienced in connection with the traumatic memory and helps to cope with the trauma.
The GERD must be carried out by a qualified person. EPDH usually requires 8-12 sessions, lasting from 60 to 90 minutes.
Some other forms of talking therapy may be useful for treating certain symptoms (eg, poor sleep) in people for whom EMRT or CBT have not been effective for trauma.
Medications
If you have tried various treatments for PTSD and find that they do not work for you, your doctor may prescribe antidepressants for you.
Selective serotonin reuptake inhibitors (SSRIs) are antidepressants that can help reduce symptoms of post-traumatic stress disorder. They can also help you if you are suffering from depression.
If SSRIs are not working for you, you may be offered other drugs, but this should usually be done on the advice of a mental health professional.
Which treatment is more effective?
There is evidence that Cognitive Behavioral Therapy for Trauma and Eye Movement Desensitization and Reprocessing are the best first line treatments. Medication can help those who refuse talking therapy or cannot easily access it.
Which treatment should I take first?
Trauma-focused psychological therapy (TF-CBT or EMBT) should be offered prior to medication, to the extent possible. This is in line with the UK National Institute for Health and Clinical Excellence (NICE) guidelines.
How can I help myself?
There are some things you can do to help you get better if you develop PTSD. Your therapist will help with this and make sure you apply them in a timely manner:
Stick to your daily routine - As far as possible, try to return to or maintain your normal daily routine. By continuing to lead a life as normal as possible, you can gain a sense of support.
Talk to someone you trust - Although you shouldn't feel like you need to talk to everyone about what happened, talking to someone you trust can help you sort out your feelings in a safe environment. It can also help to talk to someone who has gone through the same thing as you, or someone who has gone through something similar before, as long as it doesn't hurt you.
Try relaxation exercises - Try self-meditation and other relaxation exercises. Relaxing with PTSD can be challenging, so talk to your therapist about exercises or activities that can help you.
Return to work or school - if you feel empowered, it can help you return to work, school or university by giving you a sense of routine. However, you should try to avoid situations in which you may be subjected to further injury or severe stress. It is usually best to work in a supportive, low-stress environment before starting treatment.
Eat and exercise regularly - Try to eat at regular times, even if you don't feel hungry. If you feel fit, try to exercise regularly. It can also help you feel tired before bed.
Spend time with others - Spending time with the people you care about will help you feel supported.
Expect to get better - Concentrating on thoughts that you will feel better over time will be useful for your recovery. Remember that you should not strain yourself in an attempt to recover faster.
Go back to where the traumatic event happened - If you feel you can do it, you may want to go back to where the traumatic event happened. Talk to your therapist or doctor if you are considering this so they can support you through this step.
There are also some things you should avoid while recovering. However, doing the "right things" can be very difficult, and you shouldn't feel guilty if you find yourself doing any of the following:
Self-criticism - PTSD symptoms are not a sign of weakness. This is a normal reaction to violent experiences.
Keep your feelings to yourself. If you have PTSD, don't feel guilty about sharing your thoughts and feelings with others. Talking about how you are feeling can help your recovery.
Expect things to get back to normal quickly - PTSD can take some time to heal. Try not to demand too much of yourself in a short amount of time.
Stay away from other people. Spending a lot of time alone can increase your sense of isolation and make you feel less well.
Drink alcohol or smoke. While alcohol can help you relax, and coffee and nicotine can act as stimulants, they can make you feel worse over time if you're experiencing symptoms associated with post-traumatic stress disorder.
Overwork. Post-traumatic stress disorder can make it difficult to sleep, but as much as possible, try to stick to your regular sleep schedule and stay up late, as this can make you feel worse. You can learn more about good sleep in our resource.
Finally, you should be careful while driving. After a traumatic episode, people may have more accidents.
What is complex PTSD?
Some people develop complex post-traumatic stress disorder, caused by an experience or series of events that is extremely threatening or terrifying. These events can occur in childhood or adulthood.
Often such events are difficult or impossible to avoid. For example:
- torture
- slavery
- genocide
- living in war zones
- prolonged domestic violence
- repeated sexual and physical abuse
In addition to PTSD symptoms, people with complex PTSD may also:
- emotions and emotional reactions
- have difficulty maintaining relationships and feelings of closeness with other people
How do I recover from complex PTSD?
People with complex post-traumatic stress disorder are characterized by a lack of trust in other people and in the world at large.
Emotional stabilization
During the stabilization phase, you will learn to trust your therapist and to understand and manage feelings of distress and alienation.
As part of stabilization, you can familiarize yourself with the work with supports - "grounding techniques". This can help you focus on familiar physical sensations and remind you that you are living in the present, not the past.
Stabilization can help you "unplug" your feelings of fear and anxiety from the memories and the emotions they evoke, helping to make those memories less frightening.
The goal of stabilization is so that you can eventually live your life free from anxiety or memories.
Sometimes stabilization may be the only help needed.
Trauma Focused Therapy
Trauma Focused Therapy, including EMDR (Eye Movement Desensitization and Processing) or Trauma Focused Cognitive Behavioral Therapy, can help you deal with traumatic experiences. Other types of psychotherapy, including psychodynamic psychotherapy, may also be helpful. For complex post-traumatic stress disorder, care must be taken as these treatments can make things worse if not used properly.
Reintegration and recovery
Reintegration into normal life can help you adjust to the real world at a time when you have emerged from the dangerous situation you were in before. This can help you begin to see yourself as a person with a choice.
Reintegration can help you:
- be compassionate towards yourself and others
- restore trust in yourself and others
- renew friendships, intimate relationships, and activities that promote your health and well-being
Medications
As with PTSD, antidepressants or other medications may be used along with psychotherapy. Medication may also be used if psychotherapy does not help or is not available to you. It would also be helpful to have a mental health professional help you oversee your medication.
Self Help
If you develop complex PTSD, it may be helpful to try to do ordinary things that have nothing to do with your past traumatic experience. 9Ol000 . However, this can take time, and there is no need to be ashamed that at first these things will seem difficult to you or you will not be able to do them right away.
How do you know if someone has PTSD?
If you know someone who has just experienced a traumatic event, there are a few things you should be aware of. These moments can be signs that a person is not coping:
- Changes in behavior - low productivity at work, lateness, sick leave, minor accidents.
- Changes in emotions - anger, irritability, depression, lack of interest and lack of concentration.
- Changes in thought - preoccupation with threats or fears, negative outlook on the future
- Unexpected physical symptoms such as shortness of breath, nervousness or abdominal pain.
If you think a person may be showing signs of PTSD, you can suggest that they talk to their doctor. If you don't feel close enough to him for such a recommendation, talk to someone in his family or friends who could do it for you.
They may also find it helpful to refer to information about PTSD, such as this resource, to help identify the difficulties they face.
How can I help someone who has experienced a traumatic event?
For those who have experienced a traumatic event, the following actions may help:
- Be there - invite people to be with them. If they refuse, you can reassure them that you will be with them if they change their mind. Should not be imposed, but try to convince them to accept your help.
- Listen - try not to pressure people if they don't want something. If they want to talk, try to listen without interrupting or trying to share your own experience with them.
- Ask general questions - When you ask questions, try to keep them general and non-judgmental. For example, you might ask, "Have you talked about this with anyone else?" or “Can I help you find more help?”
- Offer real (practical) help - Some people may have difficulty taking care of themselves or doing daily activities. Offer help, such as cleaning the house or preparing meals;
Try not to tell people:
- That you know how they feel - even if you have experienced something like this, people experience situations differently. Comparing your experience with that of others is not always helpful;
- How lucky they are to be alive - people who have experienced traumatic events often don't think they are "lucky". Often they feel guilty about the fact that they survived while others died;
- Belittling the significance and seriousness of the experience - try not to tell people that things could be much worse, even if you do it out of good intentions and thereby try to help them.
Such statements can make people feel that their experiences are not being taken seriously by others;
- Giving inappropriate advice - Try not to give advice or suggestions, even if it has helped you in the past. All people are different and often they have already tried what you offer.
References:
This information was prepared by the Public Engagement Editorial Board of the Royal College of Psychiatrists (PEEB). It reflects the best available evidence at the time of writing.
Special thanks to PTSD UK for kindly providing feedback on this resource.
Expert Editor: Prof. Neil Greenberg
Full links to this resource are available upon request.
Translated by Elena Fage, senior intern psychiatrist
Translated by Elena Fage, Specialty doctor in CAMHS
PTSD: what it is, symptoms, treatment
Psychological trauma can sit inside us for years and decades, undermining strength and exacerbating pain from time to time . A practicing psychologist talks about the nature of post-traumatic stress disorder and explains what might help to cope with it.
Arkady Volkov, psychotherapist, specialist of the service for the selection of psychologists Alter
Advertising on RBC www.adv.rbc.ru
What is PTSD
Each person has many mechanisms and resources at their disposal to help them cope with difficult events, cope with difficulties, endure grief and loss, overcome disappointments and tragedies. Nevertheless, sometimes we are faced with an event that, for one reason or another, we cannot cope with: it does not fit into our personal experience at all and turns out to be an insurmountable shock. Such events, usually associated with a real or perceived risk to life and health, are usually called traumas, and they can cause post-traumatic stress disorder - a mental disorder as a result of encountering a traumatic situation.
Studies show that almost 4% of people suffer from PTSD at least once during their lives. At the same time, statistics in different countries vary significantly: in China, 0.3% of respondents faced the problem, in the Netherlands — 7.4%, in Canada — 9.2% [1], [2].
Symptoms of PTSD
Currently, the two main medical diagnostic guidelines (DSM-5, the American Psychiatric Association's guidelines and ICD-11, the World Health Organization's classification), have formulated the following criteria to conclude that a person is suffering from PTSD:
- Encounter with a life or health threatening situation. At the same time, PTSD can develop in a situation where a person has become a victim of such an event, and if he was a witness to it, or if a similar event happened to his loved ones. This criterion also applies to professionals who, by the nature of their work, are faced with the consequences of traumatic events: doctors, firefighters, crisis psychologists, and so on.
- Presence of at least one of the symptoms of involuntary intrusive and disturbing memories of the event, nightmares, flashbacks, distressing experiences, or a physical reaction in situations that are reminiscent of the event.
- Avoidance of memories and thoughts about the event or anything that can remind of it.
- Disturbances in thinking and emotional state due to the experienced event: inability to remember important aspects of what happened, negative thoughts and beliefs about oneself and the world around, blaming oneself or others that the traumatic event occurred, lowered mood and negative emotions, decreased interest in the world around , feelings of isolation and alienation, reduced ability to experience positive emotions.
- Changes such as irritability and outbursts of anger, aggressive and dangerous behavior to self or others, increased alertness, startle response to minor stimuli, problems concentrating and sleeping.
To be diagnosed, the listed symptoms must last more than one month and cause significant distress or social difficulties.
© shutterstock
It is important to note that PTSD is often accompanied by other disorders, primarily depressive ones.
Diagnosis of PTSD, like any other mental disorder, can only be diagnosed by a qualified specialist, but yes to the following questions may be a reason to seek advice and get help (or just be more attentive to yourself or a loved one).
- During your life, have you experienced or witnessed any traumatic event (such as an accident, fire, extreme disaster, physical attack on you or your loved ones)?
During the last month:
- Did you return to this event in your thoughts (not wanting it) or dreams?
- Did you make an effort not to think about this event and avoid being reminded of it?
- Were you more tense than usual?
- Have you ever been frightened for minor reasons?
- Did you feel alienated from your usual activities and loved ones?
- Did you feel guilty or blame yourself or others for the event?
Causes and risk factors
There is still no definite answer to the question of what exactly causes PTSD. But research has led to some important assumptions.
At the physiological level, the development of PTSD can be triggered by:
Increased levels of stress hormones
In case of danger, our body produces stress hormones, such as adrenaline, in order to switch into an active mode and somehow escape from the threat (this reaction is often called "fight or flight"). PTSD victims continue to produce large amounts of stress hormones even when the danger is no longer around. This can cause hyperarousal and emotional changes, and can also cause long-term negative health effects, including migraines, pain, and an increased risk of heart, lung, and digestive problems.
Changes in the way the brain works
Stress caused by trauma can damage the hippocampus, the part of the brain involved in the formation of emotions and memory.
Disorders in the hippocampus can interfere with the proper processing of memories and dreams, so the anxiety they cause does not decrease over time. Such changes may explain the increased levels of fear and anxiety, memory and recall problems suffered by PTSD victims.
© shutterstock
Factors that can increase susceptibility to PTSD:
- Previous traumatic experiences. The stress of a trauma can have a cumulative effect, and a new traumatic experience can exacerbate the negative effects of a previous trauma.
- Experience of violence. People with a history of physical, emotional or sexual abuse tend to be more susceptible to post-traumatic stress.
- PTSD or depression in loved ones.
- Substance use experience.
- Lack of skills to cope with traumatic situations.
- Lack of social support. Good social and family relationships help mitigate the effects of stress and trauma. Conversely, people who lack supportive relationships and environments tend to be more vulnerable to stress and therefore more at risk for PTSD. Being in a social environment that cultivates shame, guilt, stigma, or self-hatred also contributes to the development of post-traumatic stress disorder.
- High level of stress in everyday life.
Treatment of PTSD
Approaches to the treatment of PTSD can be divided into two groups: medication and psychotherapy. Often methods of both groups are used in different combinations.
There are currently no medications specifically designed to treat PTSD, but there are many medications that work well for other conditions, such as depression and anxiety disorders, and have been shown to be effective in treating the symptoms of PTSD.
When it comes to psychotherapeutic methods, or "healing with a word", there are several approaches that demonstrate the greatest (and research-supported) effectiveness.
Cognitive Process Therapy
In this approach, the therapist invites the client to talk about the traumatic event and its aftermath and describe the experience in detail in a diary, which allows them to better see how the trauma is reflected in thoughts and find new ways to deal with it [3 ].
© shutterstock
EMDR - Eye Movement Desensitization and Processing
This approach is based on the notion that trauma disrupts the natural coping mechanisms inherent in each person and cannot be built into their experience and memory. The person is asked to focus on an external stimulus (eye movements from side to side directed by the therapist) and in parallel work through complex memories, thoughts and emotions associated with the trauma [4].
Body and creativity oriented approaches
Body Oriented Therapy aims to find resources through attention to bodily sensations, as well as gaining the opportunity to relive the traumatic experience from the position of an active actor, not a victim. Similar goals are set by approaches that use dance and participation in theatrical productions to gain the freedom and spontaneity that PTSD often deprives its victims of [5].
Living with PTSD
Trauma has a huge impact on many areas of our lives, but this does not mean that the problem cannot be solved, even if for one reason or another you do not have access to professional help.
Of particular difficulty in working with PTSD is the very pain and severity of the traumatic experience, which often makes it necessary to avoid any reminders of the trauma, excluding the possibility of talking about it, as well as the devastating consequences for the view of oneself and the world around. All this makes it extremely difficult to build close relationships, seek support and help.
What can help you cope with PTSD
The first and most important step is often the recognition of the traumatic experience, which opens up opportunities for conversation and subsequent rethinking. The devastating effect of trauma on the psyche is largely due to the fact that the traumatic event is completely knocked out of the normal course of our life, and it is extremely important to return, build it into our personal history.
Research demonstrates the high effectiveness of such a simple tool as writing about your experience: writing down your thoughts and memories of a traumatic event, trying to talk about the impact it had on your life, thoughts about the future.
Since trauma affects the body in one way or another, physical exercise, yoga (or regular stretching), meditation, dancing, and even theater classes can be an important help in overcoming its consequences [6].
The support of relatives and friends plays a huge role. It's important to open yourself up and find someone you can talk to about what's bothering you.
However, overcoming PTSD on your own is not easy and can take a long time. Therefore, at the first opportunity, it is worth contacting a psychotherapist.
If your loved one has PTSD
If you notice symptoms of PTSD in a loved one, you can become a support for him and help him. At the same time, it is important to take into account that it can be extremely difficult for him to talk about the trauma and even return to it in his thoughts, so it is important to indicate your willingness to help and be there without exerting any pressure. Your very understanding and supportive presence, your willingness to share activities that bring joy and pleasure, a sense of stability and confidence can be beneficial.