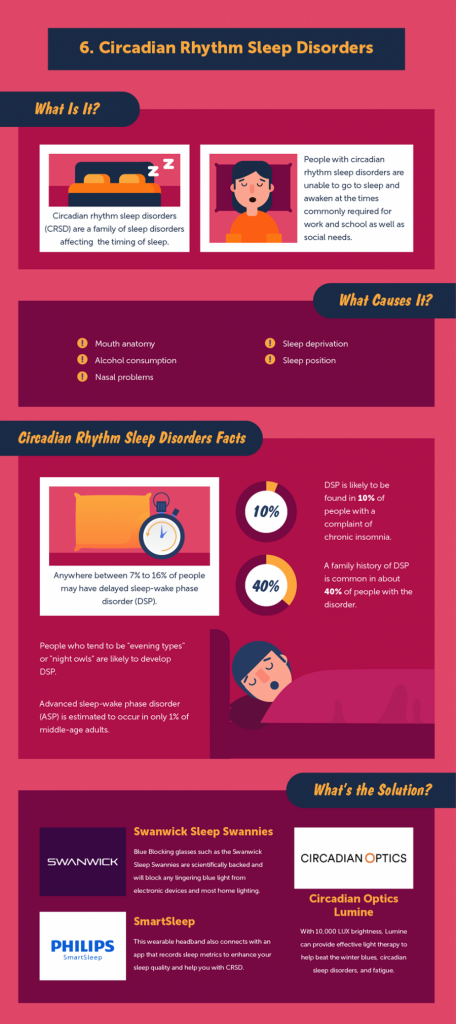
Circadian rhythm sleep disorder symptoms
Circadian Rhythm Sleep Disorders | Sleep Foundation
Most people operate on a 24-hour biological clock that is synchronized with bodily hormone production and natural light and darkness. These 24-hour cycles are collectively known as the circadian rhythm, and they play a major role in our sleep cycle.
Circadian rhythm sleep disorders – formally known as circadian rhythm sleep-wake disorders – are a group of conditions tied to dysfunctions or misalignments with the body’s internal clock. Examples of these disorders include mild conditions such as jet lag, as well as more debilitating conditions such as delayed and advanced sleep-wake disorder, irregular sleep-wake rhythm disorder, and shift work disorder.
What Is Circadian Rhythm?
The circadian rhythm is crucial to different physiological processes. In addition to sleep, this rhythm helps regulate body temperature, eating and digestion, and hormonal activity. The master circadian clock is found in the hypothalamus of the brain and composed of a cluster of proteins known as the suprachiasmatic nucleus (SCN). In a healthy adult, this clock resets – or “entrains” – every 24 hours based on light and darkness cycles. A healthy person who wakes up in the morning will gradually become more tired throughout the day, and feelings of sleepiness will peak in the evening when it is dark out.
A person’s sleep rhythm changes and evolves with age. This is why teenagers often go to bed later than both younger children and adults. As we get older, we tend to go to bed and wake up at earlier times of the day.
What Is a Circadian Rhythm Sleep Disorder?
According to the American Academy of Sleep Medicine (AASM) International Classification of Sleep Disorders, a circadian rhythm sleep-wake disorder occurs because of an alteration to the body’s internal timekeeping system, the clock’s inability to entrain roughly every 24 hours, or a misalignment between the clock and a person’s external environment.
What Are the Symptoms of a Circadian Rhythm Sleep Disorder?
While symptoms for these disorders can vary, most cause excessive daytime sleepiness. Insomnia – difficulty falling or staying asleep – is another common issue associated with these disorders.
Insomnia – difficulty falling or staying asleep – is another common issue associated with these disorders.
A formal diagnosis of a circadian rhythm sleep-wake disorder involves specific criteria including:
- Chronic or recurring sleep disturbances due to alterations of the individual’s internal circadian rhythm or misalignments between their circadian rhythm and their desired or required work or social schedule.
- Insomnia symptoms and/or excessive daytime sleepiness.
- Clinically significant distress or impairments to the individual’s mental, physical, social, occupational, or educational performance that can be attributed to their sleep disturbances.
As these criteria demonstrate, circadian rhythm sleep disorders can provoke significant health effects including problems in work or school as well as an elevated risk of vehicular or workplace accidents.
Types of Circadian Rhythm Sleep-Wake Disorders
Based on AASM classifications, the separate types of circadian rhythm sleep-wake disorders include the following:
Delayed and Advanced Sleep-Wake Phase Disorders
Delayed sleep-wake phase disorder occurs when a person’s sleep-wake cycle is pushed back more than two hours beyond what is considered a typical sleep schedule.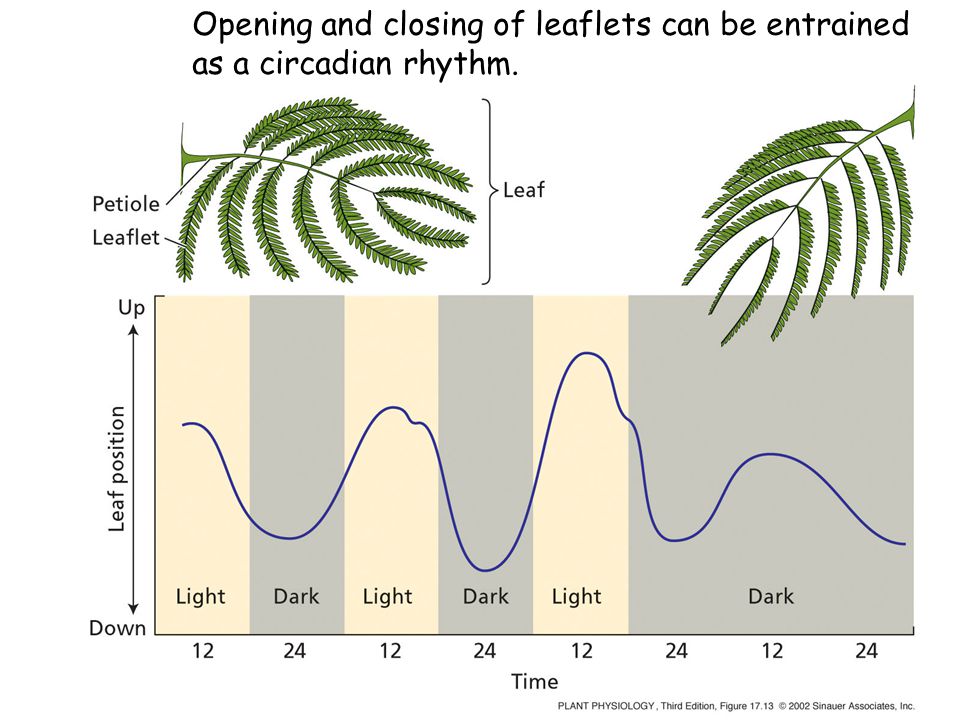 A delayed circadian rhythm can cause people to struggle with falling asleep at night and waking up earlier in the morning.
A delayed circadian rhythm can cause people to struggle with falling asleep at night and waking up earlier in the morning.
People with this condition often suffer from lack of sleep if they have school or work obligations that require an early wake-up time. Many people with this disorder are considered evening chronotypes, or night owls; its prevalence rate for young adults and adolescents is 7 to 16%.
Advanced sleep-wake phase disorder is essentially the opposite: the person tends to fall asleep and wake up more than two hours before their desired times. Advanced age is a major risk factor for this disorder.
In order to receive a diagnosis for delayed or advanced sleep-wake phase disorder, the patient must experience symptoms for at least three months. In addition, they must also report improvements to their sleep quality and duration if allowed to follow their own sleep schedule (rather than a schedule dictated by work or other obligations).
Irregular Sleep-Wake Rhythm Disorder
This disorder is characterized by inconsistent sleep patterns without a stable rhythm or entrainment to day-night cycles. Abnormal sleep periods can cause both difficulty sleeping and excessive daytime sleepiness during the course of the day. Most people with irregular sleep-wake rhythm disorder have neurodevelopmental or neurodegenerative disorder, such as Parkinson’s disease, Alzheimer’s disease, or Huntington’s Disease. The disorder has also been observed in children with developmental disabilities.
Abnormal sleep periods can cause both difficulty sleeping and excessive daytime sleepiness during the course of the day. Most people with irregular sleep-wake rhythm disorder have neurodevelopmental or neurodegenerative disorder, such as Parkinson’s disease, Alzheimer’s disease, or Huntington’s Disease. The disorder has also been observed in children with developmental disabilities.
The fragmented sleep cycle of this disorder typically yields periods of sleep that last four hours or less. As a result, people with irregular sleep-wake rhythm disorder frequently nap throughout the day. Sleep fragmentation may be more severe for Alzheimer’s patients who experience sundowning, which involves restlessness, agitation, or confusion that coincide with sunset.
Non-24-Hour Sleep-Wake Rhythm Disorder
Also known as free-running disorder, non-24-hour sleep-wake rhythm disorder occurs when the internal clock does not reset every 24 hours. As a result, a person’s normal sleep period is constantly shifting, working its way around the clock over a period of days or weeks. Severity of symptoms often depends on the person’s schedule and whether their obligations conflict with their sleep cycle.
Severity of symptoms often depends on the person’s schedule and whether their obligations conflict with their sleep cycle.
People with this condition may have insomnia symptoms and excessive daytime sleepiness when their sleep periods don’t match up with the schedule of their social and professional life. When their schedule aligns with sleep periods, a person with this condition experiences few, if any, sleep disturbances.
This disorder primarily affects people who are totally blind. The eyes of a totally blind person cannot transmit as many light signals to the brain, leading to confusion about the time of day. As a result, their internal clock is often unable to entrain on a 24-hour cycle. Between 50% and 80% of blind people report sleep disturbances, and experts estimate half of totally blind people have non-24-hour sleep-wake rhythm disorder. A diagnosis requires symptoms that persist for at least three months.
Shift Work Disorder
People whose jobs require them to work partly or completely at night often experience shiftwork disorder, which is characterized by insomnia and excessive daytime sleepiness. The term “shift-work” can apply to any shift that falls outside the traditional 9 a.m. to 5 p.m. schedule, but shift work disorder usually affects those who work late at night and/or early in the morning. Rotating shifts composed of daytime and nighttime hours can also lead to sleep disturbances and daytime grogginess.
The term “shift-work” can apply to any shift that falls outside the traditional 9 a.m. to 5 p.m. schedule, but shift work disorder usually affects those who work late at night and/or early in the morning. Rotating shifts composed of daytime and nighttime hours can also lead to sleep disturbances and daytime grogginess.
Most people with shift work disorder lose between one and four hours of sleep for each 24-hour period, and adjusting to work once their shift begins can become increasingly difficult over time.
This disorder can be particularly dangerous because it increases the risk of accidents either at their workplace or on the road during a late-night or early-morning commute.
People with this condition may also develop ulcers, and self-medicate with alcohol or drugs in order to get enough sleep. Estimates vary, but it’s believed as many as 38% of shift workers have this disorder. It is equally prevalent among the sexes and different racial groups.
Jet Lag
Most people experience jet lag after flights that pass over multiple time zones.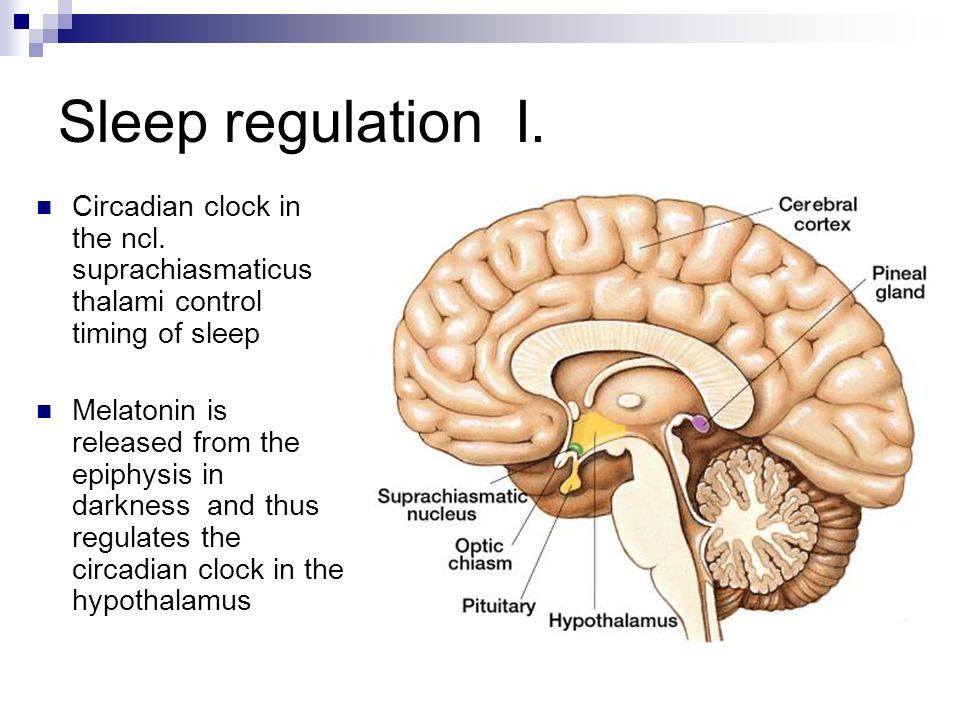 The condition, marked by temporary sleep disturbances and daytime fatigue, represents a transition period during which a person’s internal clock needs to synchronize with local time. Jet lag symptoms typically begin one to two days after the flight and can persist for up to a week or two.
The condition, marked by temporary sleep disturbances and daytime fatigue, represents a transition period during which a person’s internal clock needs to synchronize with local time. Jet lag symptoms typically begin one to two days after the flight and can persist for up to a week or two.
Eastbound travel tends to produce more severe jet lag than westbound travel; northbound and southbound travel usually results in little to no jet lag unless the plane crosses two or more time zones.
Additionally, the severity of symptoms often correlates to the number of time zones crossed; for many people, the body will require one day of adjustment for each time zone.
Jet lag is usually not a serious condition, but it can propel people into a downward spiral if they do not practice healthy sleep hygiene during this post-flight period. Persistent symptoms can lead to insomnia and other more serious sleep disorders.
Other Circadian Rhythm Sleep Disorders
Disorders in this category are usually tied to underlying health conditions.
They resemble the other circadian rhythm sleep disorders listed above in terms of general symptoms, including insomnia and excessive daytime sleepiness, but patients do not meet the diagnostic criteria.
These are rare cases that typically require tailored care from a doctor or sleep specialist.
Circadian Rhythm Sleep Disorder Treatment
Treatment of circadian rhythm sleep disorders depends on the patient’s specific diagnosis. Most treatments emphasize the importance of good sleep hygiene, a healthy sleep environment, and a consistent sleep-wake schedule. These factors can improve entrainment and reduce sleep deprivation for people with these disorders.
Circadian rhythm sleep disorder treatment may include melatonin supplements. These supplements should be prescribed by a doctor and administered at specific times to induce feelings of sleepiness. Properly timed melatonin doses can effectively reorient your circadian rhythm and entrainment schedule. Always consult with a doctor before taking melatonin to ensure you are healthy enough to do so.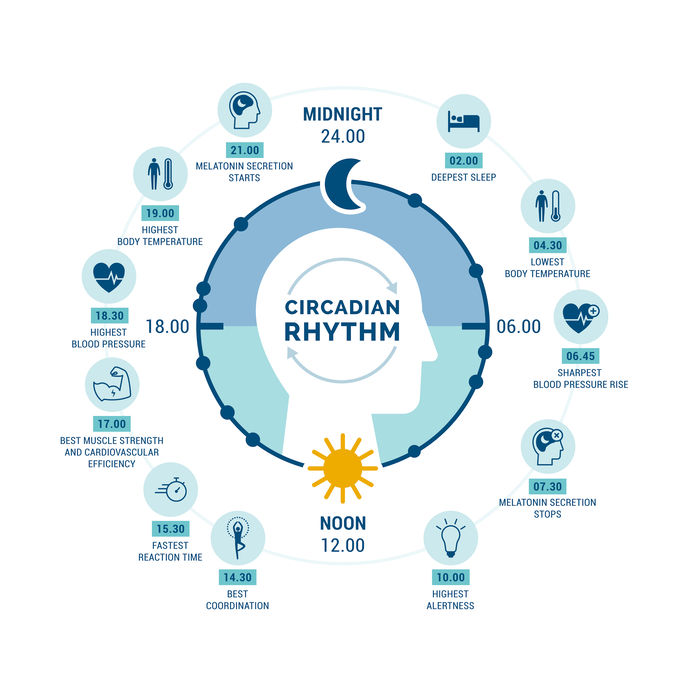
Timed bright light exposure in the morning can aid people with delayed sleep-wake phase disorder, whereas the same exposure in the evening can be used to treat those with advanced sleep-wake phase disorder. This type of light therapy can encourage a healthy shift in circadian rhythm.
For people with shift work disorder, timed light exposure during their shift can be helpful. These patients can also benefit from a regimen of napping before work and moderate caffeine intake during their shift. Coping strategies for staying awake during their shift and sleeping during the day can also be effective. These strategies include avoiding bright light during the day, bright light exposure at work, and maintaining an optimal sleep environment. Melatonin supplements or hypnotics can serve as sleep aids during the day, but these are a temporary fix and will not correct circadian misalignment.
- Was this article helpful?
- YesNo
About Our Editorial Team
Danielle Pacheco
Staff Writer
Danielle writes in-depth articles about sleep solutions and holds a psychology degree from the University of British Columbia.
Dr. Anis Rehman
Endocrinologist
MD
Dr. Rehman, M.D., is a board-certified physician in Internal Medicine as well as Endocrinology, Diabetes, and Metabolism.
References
+5 Sources
-
1.
National Heart, Blood, and Lung Institute. (n.d.). Sleep Deprivation and Deficiency. Retrieved September 3, 2020. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency
-
2.
The National Institute for Occupational Safety and Health (NIOSH). (2020, April 1). Interim NIOSH Training for Emergency Responders: Reducing Risks Associated with Long Work Hours. Centers for Disease Control. Retrieved September 3, 2020. https://www.cdc.gov/niosh/emres/longhourstraining/clock.html
-
3.
National Institutes of Health. (2020, July 13). Circadian Rhythms. Retrieved September 3, 2020. https://www.nigms.nih.gov/education/fact-sheets/Pages/circadian-rhythms.
 aspx
aspx -
4.
National Institute on Aging (NIA). (2017, May 17). Tips for Coping with Sundowning. Retrieved September 3, 2020. https://www.nia.nih.gov/health/tips-coping-sundowning
-
5.
Dodson, E., & Zee, P. (2010). Therapeutics for Circadian Rhythm Sleep Disorders. Sleep Medicine Clinics, 5(4), 701–715. Retrieved September 3, 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3020104/
See More
Circadian Rhythm Sleep Disorder
Your body runs on an internal clock that causes you to feel sleepier at night and more awake and alert during the day.
This natural sleep-wake cycle, which repeats every 24 hours, is known as the circadian rhythm. It relies on environmental cues like light and dark, meal timing, and physical activity.
A disruption of this cycle may be considered a circadian rhythm sleep disorder. This can cause symptoms that range from daytime sleepiness to depression.
Taking steps to get on a more regular sleep schedule may help improve symptoms.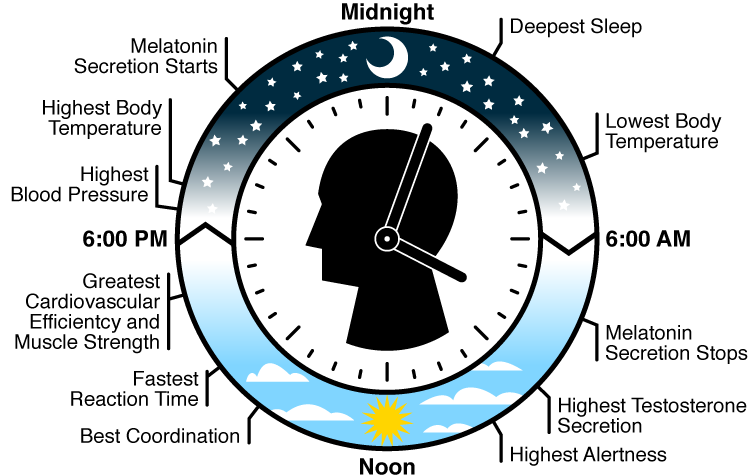
A circadian rhythm sleep disorder can impact many facets of your life. Each disorder type has unique symptoms. Most people with circadian rhythm sleep disorders have one or more of these symptoms:
- difficulty going to sleep
- difficulty staying asleep
- not feeling refreshed after sleeping
- feeling less alert
- memory issues
There are six circadian rhythm sleep disorders. Each one is defined by specific patterns of sleep disruption that result in insomnia or excessive daytime sleepiness. These conditions can have a negative effect on mental and physical health as well as daily functioning.
Advanced sleep-wake phase disorder (ASWPD)
People with this condition go to sleep earlier than most people, typically between 6 p.m. and 9 p.m. They also wake up early, around 2 a.m. to 5 a.m. People with ASWPD are more likely to be older adults.
Delayed sleep-wake phase disorder (DSWPD)
This is the most common circadian rhythm sleep disorder. People with DSWPD typically go to sleep later than others, and either wake up later than most or have trouble waking up on time. This condition is more common in adolescents and young adults.
People with DSWPD typically go to sleep later than others, and either wake up later than most or have trouble waking up on time. This condition is more common in adolescents and young adults.
Non-24-hour sleep-wake rhythm disorder (N24)
People with N24 have sleep patterns that don’t line up with the 24-hour day. Their sleep times become later and later until they’re eventually sleeping during the day. Around 55 to 70 percent of blind people have N24.
Irregular sleep-wake rhythm disorder (ISWRD)
A person with this condition sleeps for short periods that aren’t timed by their circadian system. As a result, they’ll sleep for several short episodes spread across the 24-hour day, with periods of wakefulness in between.
Symptoms include a chronic inability to sleep and excessive sleepiness. Neurological disorders, such as dementia, can contribute to ISWRD.
Jet lag disorder
This condition affects people of all ages and can occur when you travel by air across at least two time zones.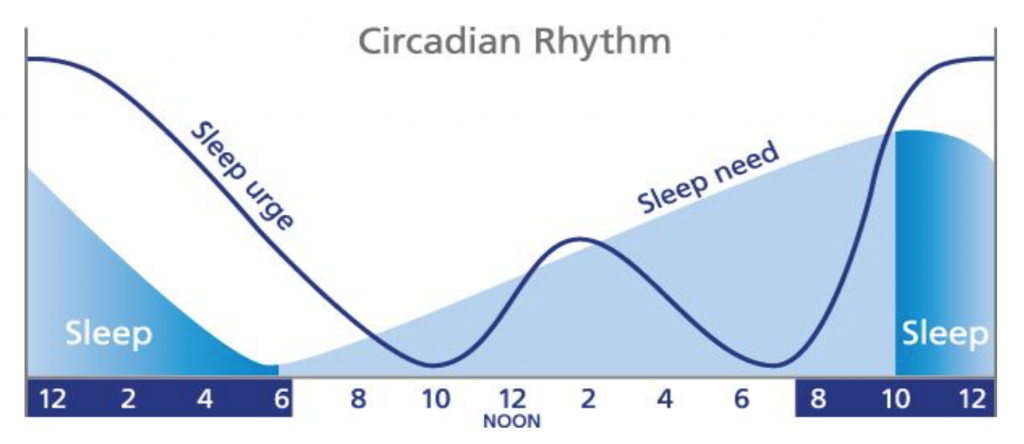 The body often has difficulty adjusting to the new time. The greater the difference between time zones, the more significant the symptoms are.
The body often has difficulty adjusting to the new time. The greater the difference between time zones, the more significant the symptoms are.
Jet lag disorder is usually temporary, and it affects some people more than others.
Shift work disorder
This condition occurs in people who work during the night or early morning hours. People with shift work disorder have difficulty getting enough sleep in the daytime to compensate for lost overnight sleep.
Conditions that influence sleep patterns may be external or internal, and include:
- light exposure
- drinking caffeine at night
- travel across multiple time zones
- non-traditional work hours
- late-night social activities
- levels of physical activity
- medical conditions
- medications
- appropriate timing and release of melatonin, a sleep hormone
Disruptions of one or more of these factors may lead to a circadian rhythm sleep disorder.
You’re more likely to experience a circadian rhythm sleep disorder if you have certain medical conditions, such as:
- blindness
- depression
- brain injury
- genetic conditions, like Smith-Magenis syndrome and Huntington’s disease
- neurodegenerative diseases, like Alzheimer’s disease and dementia
- pregnancy
Additional risk factors include:
- working night shifts
- traveling frequently
- drinking alcohol or caffeine regularly
- using devices like TVs and smartphones at night
- often going to sleep late
Taking certain medications can also stimulate the body and make sleep difficult.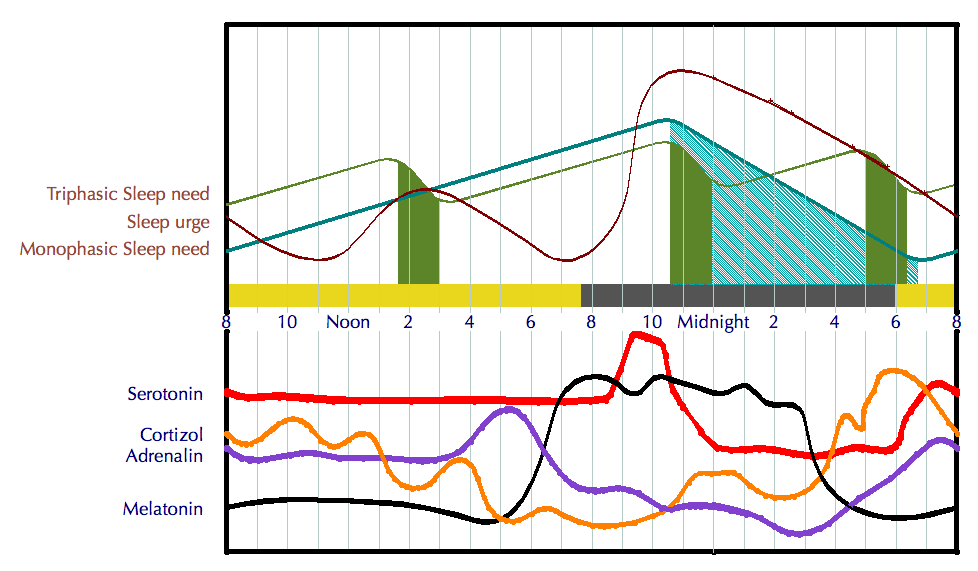 These include:
These include:
- amphetamines
- selective serotonin reuptake inhibitors (SSRIs)
- steroids
- theophylline
A sleep medicine specialist can diagnose a circadian rhythm sleep disorder. They’ll likely ask about your symptoms and your medical history and perform a physical exam. To be diagnosed with a circadian rhythm sleep disorder, you must:
- have a disrupted sleep-wake pattern caused by problems with your circadian system
- experience insomnia, excessive sleepiness, or both
- have lower functioning at work or school or see an effect on your overall health
They will also check that you meet the criteria specific to each disorder.
The specialist may recommend that you keep a sleep diary. This diary details when you went to sleep and woke up for 1 to 2 weeks. Another option is actigraphy, where you wear a small sensor to measure periods of being awake and asleep.
A sleep medicine specialist may also suggest a sleep study.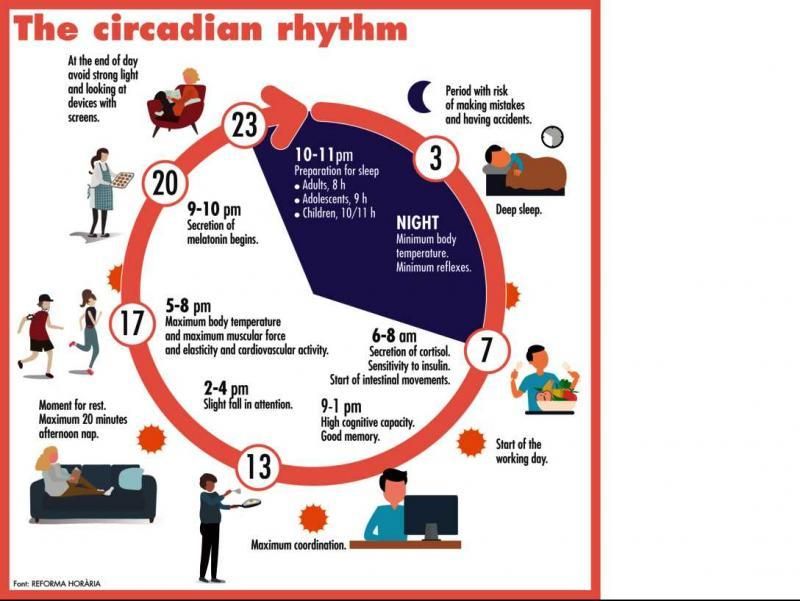 This involves sleeping under observation. You may wear sensors to monitor your heart rate, breathing, brain waves, and other functions during the sleep study. This helps rule out other conditions that may affect your sleep, such as obstructive sleep apnea.
This involves sleeping under observation. You may wear sensors to monitor your heart rate, breathing, brain waves, and other functions during the sleep study. This helps rule out other conditions that may affect your sleep, such as obstructive sleep apnea.
The specific circadian rhythm sleep disorder you have will help determine the treatment. The goal of treatment is to realign your circadian rhythm to your desired sleep-wake schedule.
Common methods involve medications, lifestyle changes, and light therapy. A combination of treatments to promote better sleep may help you find relief.
Medications
Melatonin, a hormone that regulates sleep-wake cycles, can help promote sleep. Your doctor may prescribe a medication called a melatonin receptor agonist, but you can also buy melatonin supplements over the counter.
Remember to check with your doctor when taking a new supplement.
Treatments for insomnia and excessive daytime sleepiness also include cognitive behavioral therapy and, if needed, a class of prescription medications known as benzodiazepines. Examples include:
Examples include:
- flurazepam (Dalmane)
- temazepam (Restoril)
- triazolam (Halcion)
Nonbenzodiazepine sedative-hypnotics are another class of Food and Drug Administration (FDA)-approved medications that treat insomnia. They don’t cause a significant rebound effect, or a return of symptoms, after stopping the medication compared with benzodiazepines.
Still, they may cause confusion, loss of balance, and falls. Medications include:
- eszopiclone (Lunesta)
- zaleplon (Sonata)
- zolpidem (Ambien, Ambien CR, Edluar)
Home care
You may benefit from improving your sleep routine if you have a circadian rhythm sleep disorder. Changes may include:
- avoiding naps during the day
- following a set sleep schedule
- performing quiet activities, such as reading, before going to sleep
- making your bed more comfortable
- avoiding bright lights at night
- sleeping in a cool, quiet room
It’s best to avoid caffeine, nicotine, and strenuous physical activity before bed.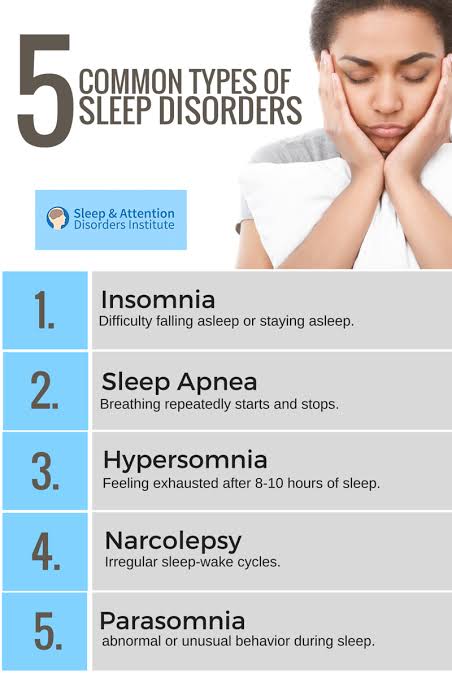 It may also help to limit alcohol, which can disrupt sleep. Other beneficial lifestyle habits may include eating at regularly scheduled times and getting enough exercise.
It may also help to limit alcohol, which can disrupt sleep. Other beneficial lifestyle habits may include eating at regularly scheduled times and getting enough exercise.
You can also try light therapy at home, which can involve using a light-producing box or indoor lights to adjust your sleep cycle. Using the box in the morning may help you wake up earlier, while evening use may help you delay your sleep. A 2019 research review found that light therapy improved sleep in people with DSWPD.
Getting enough sleep is important for your health. If you have a circadian rhythm sleep disorder, it may place you at greater risk of:
- depression
- a weaker immune system
- diabetes
- cardiovascular diseases
- a traffic accident
- trouble concentrating at work or school
Making simple changes to your sleep routine and light exposure may help you adjust your sleep schedule.
Diagnosis and treatment of sleep disorders
For many centuries, sleep has been regarded as a state of rest and reduced reactivity to external stimuli. But recently an increasing number of facts have been accumulating that do not fit into the usual ideas about sleep and make this definition incorrect. What sign of sleep can be considered its necessary condition? The main sign of sleep in the first place is its rhythm. The rhythmic alternation of sleep phases makes it possible to distinguish normal sleep from monotonous "dream-like states". As part of "normal sleep" should alternate 1-2-3-4 stages of slow sleep, and at the end - REM (paradoxical) sleep. Such a radical change in ideas about the nature of sleep was the result of the emergence in the second half of the 20th century of the science of sleep - somnology. Currently, somnology is one of the fastest growing branches of the science of the nervous system.
But recently an increasing number of facts have been accumulating that do not fit into the usual ideas about sleep and make this definition incorrect. What sign of sleep can be considered its necessary condition? The main sign of sleep in the first place is its rhythm. The rhythmic alternation of sleep phases makes it possible to distinguish normal sleep from monotonous "dream-like states". As part of "normal sleep" should alternate 1-2-3-4 stages of slow sleep, and at the end - REM (paradoxical) sleep. Such a radical change in ideas about the nature of sleep was the result of the emergence in the second half of the 20th century of the science of sleep - somnology. Currently, somnology is one of the fastest growing branches of the science of the nervous system.
Currently, doctors and researchers have proven that even small chronic disturbances in sleep and wakefulness are very dangerous for health and are fraught with serious consequences. They can be one of the most important causes of industrial injuries, incidents and disasters, provoking the so-called "human factor".
At the same time, the way of life of a modern person, especially in large cities, is poorly consistent with the requirements of "sleep hygiene". The abundance of bright electric light, increased noise levels, working with a computer, watching television programs at night - all this negatively affects sleep.
The situation continues to worsen, in connection with which in many countries centers for the correction of sleep disorders, institutes for the study of sleep, and drug-free methods of treatment are being developed. One of the most important areas in "sleep medicine" is the creation of effective and harmless drugs of a new generation.
What threatens sleep disturbance?
- Chronic lack of sleep reduces long-term concentration and memory.
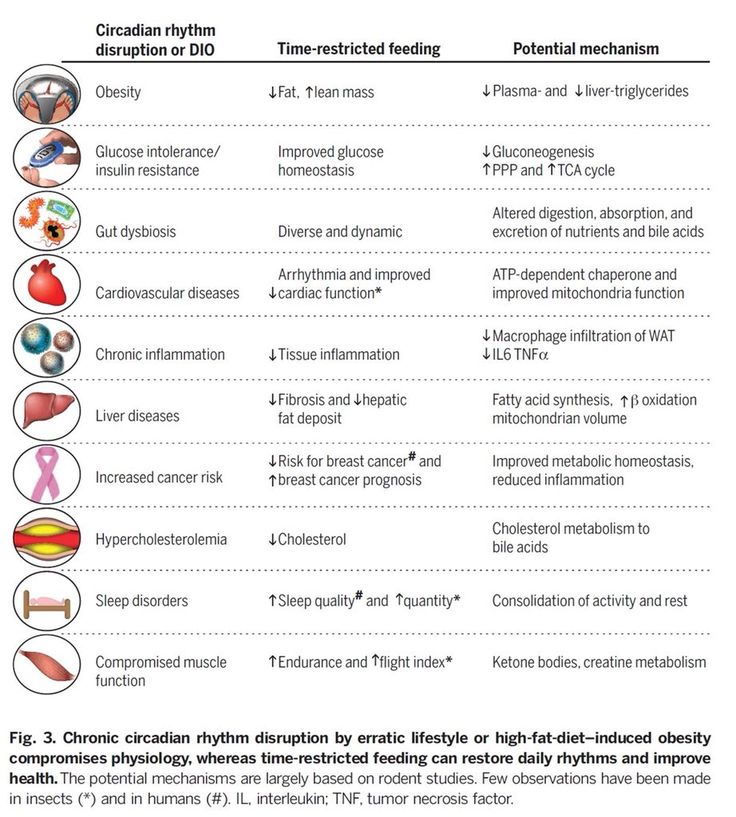
- Lack of sleep affects carbohydrate metabolism and the hormonal system. Currently, many studies confirm that sleep deprivation and metabolic disorders are linked. Obesity, diabetes, and cardiovascular disease are on the rise, in part because we are sleeping less and more erratically.
 In recent years, several experiments have shown that people who sleep very little or poorly are more likely to be obese than others. Hormones that regulate appetite play a decisive role in this. Those who sleep too little have increased levels of the hunger hormone ghrelin in the blood, and the amount of leptin, which curbs appetite, is lowered.
In recent years, several experiments have shown that people who sleep very little or poorly are more likely to be obese than others. Hormones that regulate appetite play a decisive role in this. Those who sleep too little have increased levels of the hunger hormone ghrelin in the blood, and the amount of leptin, which curbs appetite, is lowered. - Lack of sleep weakens the body's immune system. With reduced sleep, the human body produces significantly less growth hormone. This means that lack of sleep reduces the possibility of regeneration for the system of internal organs. If organs do not have the time and material to replace old or diseased cells with new ones, they will perform less well and their resistance to disease will decrease.
How much sleep does a person need?
A study by the American Institute of Health shows that the average person needs 8 hours and 15 minutes of sleep.
In summer, when daylight hours are longer, we need slightly less sleep than in winter. But each person has a different need for sleep. It is genetically determined and depends on many factors. Any number between 5 and 10 hours is considered normal.
But each person has a different need for sleep. It is genetically determined and depends on many factors. Any number between 5 and 10 hours is considered normal.
What to do if sleep is disturbed?
Experts agree that sleep hygiene is very important. These are specific and easy to implement rules that lead to physical and mental readiness for normal sleep:
- Limit your time in bed. Go to bed when you really want to sleep, and get up in the morning as soon as you feel you've had enough sleep.
- Use the bed only for sleeping. Remove the TV from the bedroom, do not eat in bed. If you wake up in the middle of the night and cannot fall asleep, get up at the latest in half an hour and find some quiet activity - reading or doing housework. Don't go back to bed until you feel really sleepy.
- Maintain regular sleep hours. Get up and go to bed at the same time, including on weekends. Compliance with the diet and sports at the same hours also contribute to the synchronization of internal rhythms, their stabilization and strengthening, which has a good effect on the quality of sleep.

- Remove the clock from the bedroom. This will help to avoid looking at the clock at night and the feeling of rushing time that it causes.
- Sleep mostly at night. Avoid daytime sleep, and if this is difficult for you, limit its duration to 1 hour. After 15.00 you should not sleep.
- Get active during the day. Try regularly, preferably daily, to play sports and generally move more - if possible in the fresh air. It is important not to overstrain in the last hours before bedtime. In the evenings, especially just before bedtime, any strenuous activity that activates blood circulation and requires special concentration is prohibited, including hot and very cold baths, mopping, sports and computer work.
- At least 3-4 hours before bedtime, do not drink coffee, tea, Coca-Cola and do not take caffeinated and other stimulant medications. During the day, caffeine should also be consumed in moderation, otherwise the withdrawal syndrome begins at night. Cigarettes have a similar effect.
- Do not drink alcohol 4-6 hours before bedtime. Alcohol interferes with long sleep.
- Don't overeat at night. A heavy dinner can deprive you of sleep for a long time.
- The bedroom should be comfortable, the temperature is about 18 C, ventilate the room well and cover the windows tightly from the light.
- If all these measures do not help, do not be afraid to ask the advice of a doctor - a specialist in sleep disorders - a somnologist.
Sleeping aids
Never take any sleeping pills or sedatives, even harmless ones sold without a prescription, without a doctor's prescription. The main disadvantage of potent sedatives is that the brain gets used to them sooner or later. When you try to refuse them, a withdrawal syndrome occurs. Patients suffer from increased anxiety and very poor sleep. Another thing is if the therapy was prescribed by a somnologist. The doctor knows exactly in what dosage one or another sleeping pill or sedative can be taken. Along with pills for chronic insomnia, behavioral therapy is always used: relaxation, sleep hygiene and adherence to the regimen.
The International Classification of Sleep Disorders (ICSD) is the most widely used classification system for sleep disorders. The third version of ICSD (ICSD-3) includes seven major sleep disorders:
1. Insomnia (insomnia). Includes conditions characterized by problems falling asleep, maintaining sleep, or poor sleep quality.
2. Sleep related respiratory disorders.
Central sleep apnea syndrome.
- Central sleep apnea with Chain-Stokes respiration
- Central sleep apnea due to somatic disease without respiration Chain-Stokes
- Central apnea due to high-amplitude periodic breathing,
- Central sleep apnea due to drugs or substances,
- Primary central sleep apnea,
- Primary neonatal apnea,
- Primary sleep apnea of premature babies,
- Central apnea resulting from treatment.
Obstructive sleep apnea syndrome.
- Adult obstructive sleep apnea,
- Obstructive sleep apnea in children.
Hypoventilation disorders associated with sleep.
- Obesity-hypoventilation syndrome,
- Syndrome of congenital central alveolar hypoventilation in children,
- Late onset central hypoventilation syndrome,
- Idiopathic central hypoventilation,
- Sleep-related hypoventilation due to use of drugs or substances,
- Sleep-related hypoventilation due to medical conditions.
Sleep related hypoxemia.
3. Hypersomnia of central origin.
- Narcolepsy (type 1 and type 2).
- Idiopathic hypersomnia.
- Klein-Levin syndrome.
- Sleep deprivation syndrome (including voluntary sleep deprivation).
- Hypersomnia associated with drug use, somatic and mental illness.
4. Disorders of the circadian rhythm of sleep and wakefulness (chronic or current sleep disturbance due to a mismatch between the environment and the individual's sleep-wake cycle in a person).
- Sleep disorders associated with shift work;
- Jet lag syndrome.
- A sleep-wake disorder characterized by earlier falling asleep and waking up earlier (more common in the elderly).
- Irregular sleep-wake rhythm, characterized by the absence of a definite circadian rhythm. This disorder is commonly associated with childhood disruption and neurodegenerative diseases such as Alzheimer's disease, Parkinson's disease and Huntington's disease.
- Non-24-hour sleep-wake rhythm disorder, characterized by excessive sleepiness or insomnia, which occurs because the internal circadian rhythm is not adapted to the 24-hour daily cycle. In most cases, this disorder affects blind people who are not able to determine circadian rhythms.
- Circadian arrhythmias can also occur due to somatic, psychiatric, or neurological disorders.
5. Parasomnias (abnormal movements, sleep behavior, nightmares).
Non-rapid eye movement (NREM) parasomnias of awakening disorders:
- confused awakenings,
- sleepwalking,
- nightmares,
- eating disorders associated with sleep.
Rapid eye movement (REM) related parasomnias:
- sleep paralysis,
- nightmares.
Non-sleep stage related parasomnias:
- dream hallucinations
- nocturnal enuresis
- parasomnias associated with somatic diseases and medications.
6. Sleep-related movement disorders (characterized by simple, stereotypical movements that interfere with sleep)
- Restless legs syndrome,
- Periodic limb movements,
- Sleep-related crumpy syndrome,
- Sleep-related bruxism (teeth grinding),
- Sleep related rhythmic movement disorders
7. Other sleep disorders
This category includes sleep disorders that do not meet the classification, as well as cases where there is more than one sleep disorder, or cases where there is insufficient evidence to support a diagnosis.
To provide professional medical care to patients with sleep disorders, it is necessary to conduct a comprehensive examination by a specialist. The Clinic of Neurology and Neurosurgery of the European Medical Center offers patients the diagnosis of sleep disorders according to the most modern protocols using the polysomnography method, the gold standard in somnology. Based on the results of the study, treatment is prescribed, which may include pharmacotherapy, behavioral therapy, therapy using CPAP, BIAP devices. (CPAP English Constant Positive Airway Pressure, CPAP - mode of artificial ventilation of the lungs with constant positive pressure and BIPAP English Bilevel Positive Airway Pressure, BPAP - two-level positive airway pressure).
We all know that in order to rest and rejuvenate, we need sufficient quality sleep, which is one of the main factors that determine the quality of human life. Therefore, it is so important to find time and arrange for yourself the possibility of a good sleep.
Circadian rhythm disorder is a risk factor for obesity and chronic anovulation in women of reproductive age
Circadian rhythm disorder is a risk factor for obesity and chronic anovulation in women of reproductive ageAndreeva E.N.
National Medical Research Center for Endocrinology, Ministry of Health of Russia;
Moscow State University of Medicine and Dentistry named after A.I. A.I. Evdokimov” of the Ministry of Health of Russia
Grigoryan O.R.
National Medical Research Center of Endocrinology of the Ministry of Health of Russia
Sheremetyeva E.V.
National Medical Research Center for Endocrinology of the Russian Ministry of Health
Absatarova Yu. S.
National Medical Research Center of Endocrinology of the Ministry of Health of Russia
Fursenko V.A.
National Medical Research Center for Endocrinology of the Ministry of Health of Russia
Circadian rhythm disorder is a risk factor for obesity and chronic anovulation in women of reproductive age
Journal: reproduction problems. 2020;26(5): 36‑42
DOI 10.17116/repro20202605136
How to quote
Andreeva E.N., Grigoryan O.R., Sheremetyeva E.V., Absatarova Yu.S., Fursenko V.A. Disruption of circadian rhythms is a risk factor for the development of obesity and chronic anovulation in women of reproductive age. Problems of reproduction. 2020;26(5):36‑42.
Andreeva EN, Grigoryan OR, Sheremetyeva EV, Absatarova YuS, Fursenko VA. Circadian rhythm disturbance is a risk factor for obesity and chronic anovulation in women of reproductive age. Russian Journal of Human Reproduction. 2020;26(5):36‑42. (In Russ.).
https://doi.org/10.17116/repro20202605136
Authors:
Andreeva E.N.
National Medical Research Center for Endocrinology, Ministry of Health of Russia;
Moscow State University of Medicine and Dentistry named after A.I. A.I. Evdokimov» of the Ministry of Health of Russia
All authors (5)
Read metadata
In the last decade, there has been growing interest in the physiological effects of the hormonal regulation of the sleep-wake system, in particular, in the pineal (pineal gland) hormone melatonin. Melatonin is one of the key mediators of the influence of the pineal gland on the endocrine, immune and other systems of the body, including the regulation of the sleep-wake system. Sleep disorders are closely related to circadian rhythm disorders - jet lag, shift work disorder, weekend insomnia and others. Sleep deprivation along with the presence of a TV in the sleeping room (bedroom) and watching TV before bed are considered as possible causes of obesity. Obesity is a key link in the metabolic syndrome. By 2025, about 50% of women on our planet will be obese. Identification of early markers and risk factors for the development of metabolic syndrome in women of reproductive age is one of the priority areas of endocrine gynecology. Obesity and disruption of circadian rhythms, both individually and in combination, are aggravating factors for chronic anovulation syndrome, which, in turn, leads to infertility, the risk of pathological pregnancy and a threat to the health of the unborn child, as well as the risk of developing cancer in children. women of reproductive age.
Key words:
obesity
sleep
reproduction
ovulation
circadian rhythms
metabolic syndrome
Andreeva.N.
National Medical Research Center for Endocrinology, Ministry of Health of Russia;
Moscow State University of Medicine and Dentistry named after A.I. A.I. Evdokimov” of the Ministry of Health of Russia
- SPIN RSCI: 1239-2937
- Scopus AuthorID: 7102485410
- ResearcherID: B-5889-2017
- ORCID: 0000-0001-8425-0020
Grigoryan O. R.
National Medical Research Center of Endocrinology of the Ministry of Health of Russia
Sheremetyeva E.V.
National Medical Research Center for Endocrinology of the Russian Ministry of Health
- SPIN RSCI: 9413-5136
- Scopus AuthorID: 57193433618
- ORCID: 0000-0001-7177-0254
Absatarova Yu.S.
National Medical Research Center of Endocrinology of the Ministry of Health of Russia
Fursenko V.A.
National Medical Research Center for Endocrinology of the Russian Ministry of Health
References:
- Vitaterna M, King D, Chang A, Kornhauser JM, Lowrey PL, McDonald JD, Dove WF, Pinto LH, Turek FW, Takahashi JS. Mutagenesis and mapping of a mouse gene, clock, essential for circadian behavior. Science. 1994;264(5159):719-725. https://doi.org/10.1126/science.8171325
- Cagnacci A. Melatonin in relation to physiology in adult humans. Journal of Pineal Research. 1996;21(4):200-213.
https://doi.org/10.1111/j.1600-079x.1996.tb00287.x
- Melatonin: prospects for clinical use. Ed. Rapoport S.I. Moscow: IMA-PRESS; 2012.
- Smythe G, Lazarus L. Growth Hormone Regulation by Melatonin and Serotonin. Nature. 1973;244(5413):230-231. https://doi.org/10.1038/244230a0
- Andreeva E.N., Sheremetyeva E.V., Fursenko V.A. Obesity is a threat to Russia's reproductive potential. Obesity and metabolism. 2019;16(3):20-28. https://doi.org/10.14341/omet10340
- Volel B.A., Ragimova A.A., Burchakov D.I., Burchakova M.N., Kuznetsova I.V. Stress related menstrual disorders. Consilium Medicum. 2016;18(6):8-13.
- Kamdar B, Tergas A, Mateen F, Bhayani N, Oh J. Night-shift work and risk of breast cancer: a systematic review and meta-analysis. Breast Cancer Research and Treatment. 2013;138(1):291-301. https://doi.org/10.1007/s10549-013-2433-1
- Yuan X, Zhu C, Wang M, Mo F, Du W, Ma X. Night Shift Work Increases the Risks of Multiple Primary Cancers in Women: A Systematic Review and Meta-analysis of 61 Articles.
Cancer Epidemiology Biomarkers and Prevention. 2018;27(1):25-40. https://doi.org/10.1158/1055-9965.epi-17-0221
- The putative 82 causes of obesity. The downey obesity report. Accessed April 7, 2020. https://www.downeyobesityreport.com/2013/02/the-putative-82-causes-of-obesity
- Smirnova V.O. Possibilities of correcting the components of the metabolic syndrome with melatonin: diss. ... cand. honey. Sciences. Volgograd; 2018.
- Cappuccio F, Taggart F, Kandala N, Currie A, Peile E, Stranges S, Miller MA. Meta-Analysis of Short Sleep Duration and Obesity in Children and Adults. Sleep. 2008;31(5):619-626. https://doi.org/10.1093/sleep/31.5.619
- De Bacquer D, Van Risseghem M, Clays E, Kittel F, De Backer G, Braeckman L. Rotating shift work and the metabolic syndrome: a prospective study. International Journal of Epidemiology. 2009; 38(3):848-854. https://doi.org/10.1093/ije/dyn360
- Jetten AM. Retinoid-Related Orphan Receptors (RORs): Critical Roles in Development, Immunity, Circadian Rhythm, and Cellular Metabolism.
Nuclear Receptor Signaling. 2009;7(1):e003. https://doi.org/10.1621/nrs.07003
- Maemura K, Takeda N, Nagai R. Circadian Rhythms in the CNS and Peripheral Clock Disorders: Role of the Biological Clock in Cardiovascular Diseases. Journal of Pharmacological Sciences. 2007; 103(2):134-138. https://doi.org/10.1254/jphs.fmj06003x2
- Sisson S, Camhi S, Church T, Martin CK, Tudor-Locke C, Bouchard C, Earnest CP, Smith SR, Newton RL Jr, Rankinen T, Katzmarzyk PT . Leisure time sedentary behavior, occupational/domestic physical activity, and metabolic syndrome in U.S. men and women. Metabolic Syndrome and Related Disorders. 2009;7(6):529-536. https://doi.org/10.1089/met.2009.0023
- Tsfasman A.Z., Gorokhov V.D., Alpaev D.V. The circadian rhythm of melatonin during night sleep deprivation. Problems of endocrinology. 2013;59(2):40-44. https://doi.org/10.14341/probl201359240-44
- Cipolla-Neto J, Amaral F, Afeche S, Tan D, Reiter R. Melatonin, energy metabolism, and obesity: a review.
Journal of Pineal Research. 2014;56(4):371-381. https://doi.org/10.1111/jpi.12137
- Reiter R, Tan D, Korkmaz A, Ma S. Obesity and metabolic syndrome: Association with chronodisruption, sleep deprivation, and melatonin suppression. Annals of Medicine. 2012;44(6):564-577. https://doi.org/10.3109/07853890.2011.586365
- Waldhauser F, Frisch H, Waldhauser M, Weiszenbacher G, Zeitlhuber U, Wurtman R. Fall in nocturnal serum melatonin during prepuberty and pubescence. The Lancet. 1984;323(8373):362-365. https://doi.org/10.1016/s0140-6736(84)-4
- Díaz López B, Díaz Rodríguez E, Urquijo C, Fernández Alvarez C. Melatonin Influences on the Neuroendocrine-Reproductive Axis. Annals of the New York Academy of Sciences. 2005;1057(1):337-364. https://doi.org/10.1196/annals.1356.026
- Roy D, Belsham D. Melatonin Receptor Activation Regulates GnRH Gene Expression and Secretion in GT1-7 GnRH Neurons. Journal of Biological Chemistry. 2001;277(1):251-258. https://doi.
org/10.1074/jbc.m1088
- Baker F, Driver H. Circadian rhythms, sleep, and the menstrual cycle. Sleep medicine. 2007;8(6):613-622. https://doi.org/10.1016/j.sleep.2006.09.011
- Lim A, Huang Z, Chua S, Kramer M, Yong E. Sleep Duration, Exercise, Shift Work and Polycystic Ovarian Syndrome-Related Outcomes in a Healthy Population: A Cross-Sectional Study. PLOS One. 2016;11(11):e0167048. https://doi.org/10.1371/journal.pone.0167048
- Labyak S, Lava S, Turek F, Zee P. Effects of shiftwork on sleep and menstrual function in nurses. Health Care for Women International. 2002;23(6-7):703-714. https://doi.org/10.1080/073993302 449
- Lee K. Self-Reported Sleep Disturbances in Employed Women. Sleep. 1992;15(6):493-498. https://doi.org/10.1093/sleep/15.6.493
- Preston FS, Bateman SC, Short RV, Wilkinson RT. Effects of flying and of time changes on menstrual cycle length and on performance in airline stewardesses. Aerospace Medicine. 1973;44(4):438-443.
- Messing K, Saurel-Cubizolles M, Bourgine M, Kaminski M. Menstrual-cycle characteristics and work conditions of workers in poultry slaughterhouses and canneries. Scandinavian Journal of Work, Environment and Health. 1992;18(5):302-309. https://doi.org/10.5271/sjweh.1572
- Uehata T, Sasakawa N. The fatigue and maternity disturbances of night workwomen. Journal of Human Ergology. 1982;11(Suppl):465-474.
- Baumgartner A, Dietzel M, Saletu B, Wolf R, Campos-Barros A, Gräf KJ, Kürten I, Mannsmann U. Influence of partial sleep deprivation on the secretion of thyrotropin, thyroid hormones, growth hormone, prolactin, luteinizing hormone, follicle stimulating hormone, and estradiol in healthy young women. Psychiatry Research. 1993;48(2):153-178. https://doi.org/10.1016/0165-1781(93) -j
- Axelsson G, Rylander R, Molin I. Outcome of pregnancy in relation to irregular and inconvenient work schedules. British Journal of Industrial Medicine. 1989;46(6):393-398.
https://doi.org/10.1136/oem.46.6.393
- Michels K, Mendola P, Schliep K, Yeung EH, Ye A, Dunietz GL, Wactawski-Wende J, Kim K, Freeman JR, Schisterman EF, Mumford SL. The influences of sleep duration, chronotype, and nightwork on the ovarian cycle. Chronobiology International. 2019;37(2): 260-271. https://doi.org/10.1080/07420528.2019.1694938
- Andreeva E.N., Grigoryan O.R., Sheremetyeva E.V., Absatarova Yu.S. Comorbidity: Polycystic ovary syndrome and obesity. Tutorial. Moscow: AMP Group; 2020.
- Spinedi E, Cardinali D. The Polycystic Ovary Syndrome and the Metabolic Syndrome: A Possible Chronobiotic-Cytoprotective Adjuvant Therapy. International Journal of Endocrinology. 2018;1349688. https://doi.org/10.1155/2018/1349868
- Andreeva E.N., Absatarova Yu.S., Sheremetyeva E.V., Derkach D.A., Ponomareva T.A., Tyulpakov A.N. , Ioutsi V.A., Ilyin A.V., Murvatov K.D. Analysis of the informativeness of the determination of melatonin in polycystic ovary syndrome.
Obesity and metabolism. 2016;13(4):15-20. https://doi.org/10.14341/omet2016415-20
- Lowes D, Webster N, Murphy M, Galley H. Antioxidants that protect mitochondria reduce interleukin-6 and oxidative stress, improve mitochondrial function, and reduce biochemical markers of organ dysfunction in a rat model of acute sepsis. British Journal of Anesthesia. 2013;110(3):472-480. https://doi.org/10.1093/bja/aes577
- Soares J, Masana M, Ershahin Ç, Dubocovich M. Functional Melatonin Receptors in Rat Ovaries at Variious Stages of the Estrous Cycle. Journal of Pharmacology and Experimental Therapeutics. 2003; 306(2):694-702. https://doi.org/10.1124/jpet.103.049916
- Reiter R, Tamura H, Tan D, Xu X. Melatonin and the circadian system: contributions to successful female reproduction. Fertility and Sterility. 2014;102(2):321-328. https://doi.org/10.1016/j.fertnstert.2014.06.014
- Tamura H, Takasaki A, Miwa I, Taniguchi K, Maekawa R, Asada H, Taketani T, Matsuoka A, Yamagata Y, Shimamura K, Morioka H, Ishikawa H, Reiter RJ, Sugino N.
Oxidative stress impairs oocyte quality and melatonin protects oocytes from free radical damage and improves fertilization rate. Journal of Pineal Research. 2008; 44(3):280-287. https://doi.org/10.1111/j.1600-079x.2007.00524.x
- Cappuccio F, D’Elia L, Strazzullo P, Miller M. Quantity and Quality of Sleep and Incidence of Type 2 Diabetes: A systematic review and meta-analysis. Diabetes Care. 2009;33(2):414-420. https://doi.org/10.2337/dc09-1124
- Van Cauter E. Sleep disturbances and insulin resistance. Diabetic Medicine. 2011;28(12):1455-1462. https://doi.org/10.1111/j.1464-5491.2011.03459.x
- Shreeve N, Cagampang F, Sadek K, Tolhurst M, Houldey A, Hill CM, Brook N, Macklon N, Cheong Y. Poor sleep in PCOS; is melatonin the culprit? human reproduction. 2013;28(5):1348-1353. https://doi.org/10.1093/humrep/det013
- Shabani A, Foroozanfard F, Kavossian E, Aghadavod E, Ostadmohammadi V, Reiter RJ, Eftekhar T, Asemi Z. Effects of melatonin administration on mental health parameters, metabolic and genetic profiles in women with polycystic ovary syndrome : A randomized, double-blind, placebo-controlled trial.
Journal of Affective Disorders. 2019;250:51-56. https://doi.org/10.1016/j.jad.2019.02.066
- Cardinali DP, Cano P, Jiménez-Ortega V, Esquifino AI. Melatonin and the Metabolic Syndrome: Physiopathologic and Therapeutical Implications. neuroendocrinology. 2011;93(3):133-142. https://doi.org/10.1159/000324699
- Cardinali DP, Hardeland R. Inflammaging, Metabolic Syndrome and Melatonin: A Call for Treatment Studies. neuroendocrinology. 2017;104(4):382-397. https://doi.org/10.1159/000446543
- Rapoport S.I., Molchanov A.Yu., Golichenkov V.A., Burlakova O.V., Suprunenko E.A., Savchenko E.S. Metabolic syndrome and melatonin. Clinical medicine. 2013;91(11):8-14.
Close metadata
Circadian rhythms are fluctuations in human biological rhythms that occur with different intensity and cyclicity and are determined by the regime of day and night, i.e. This is the biological clock of every person. Circadian rhythms are the most important mechanism in the regulation of the whole organism; they provide homeostasis, dynamic balance and the process of adaptation in biological systems. These rhythms have an endogenous genetic nature and are closely related to external environmental factors [1].
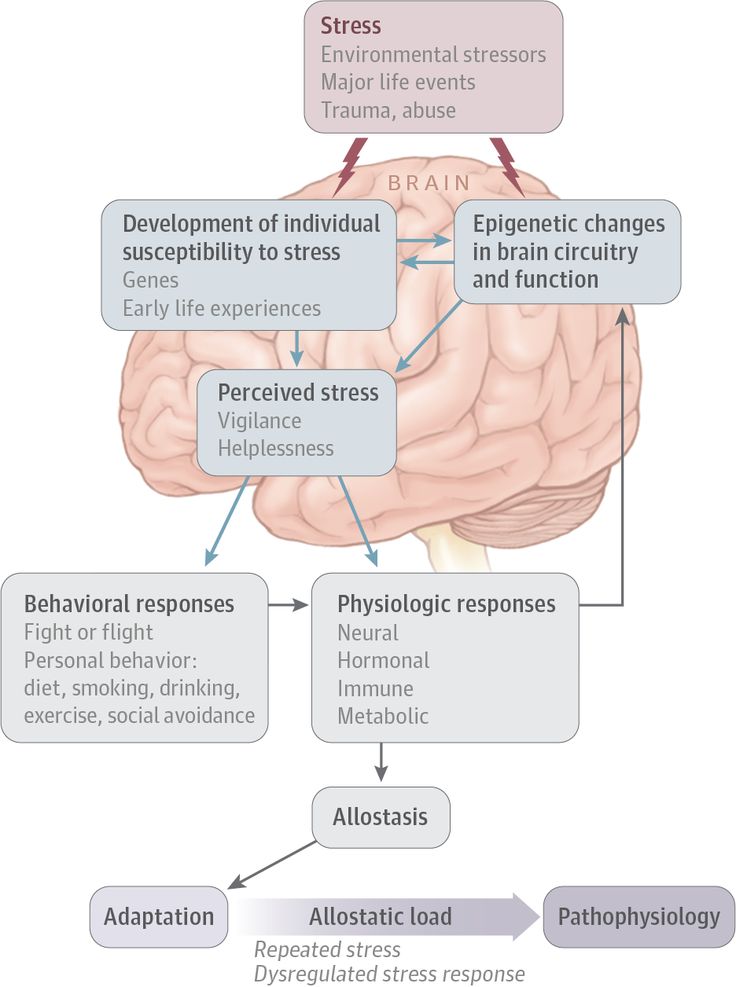
Each person experiences peaks and drops in circadian rhythms during the day, due to life-support processes in the body, for example, changes in body temperature, changes in pulse rate, respiration, etc. [2]. An important function of circadian rhythms is the identification of day and night patterns. Violation of circadian rhythms occurs due to desynchronization of endogenous (early or late falling asleep) and exogenous (change of time zone, change in daily work schedule) factors of biological rhythms. Circadian rhythm disturbances are associated with such sleep disorders as delayed sleep phase syndrome, shift work sleep disorders, jet lag (including social) [2]. In turn, the risk of developing diseases such as type 2 diabetes mellitus (DM), obesity, cardiovascular diseases, menstrual disorders, infertility, oncological diseases, etc. is now actively associated with circadian rhythm disorders and sleep disorders. [ 3].
Disturbance of circadian rhythms and metabolic syndrome
Currently, one of the causes of the development of metabolic syndrome (MS) is called desynchronosis, which is formed as a result of disturbances in the sleep-wake cycle and a decrease in the synthesis of the natural biosynchronizer - melatonin at night. Melatonin is not only a natural regulator of the normal circadian rhythm, but also a moderator of the synthesis of growth hormone, which is a metabolic activator in humans, which accelerates catabolic processes [4].
Obesity is a key link in MS. The frequency of obesity in women of reproductive age is 25-27%. By 2025, about 50% of women on our planet will be obese. An increase in body weight in a woman not only leads to a decrease in fertility, but also negatively affects the course of pregnancy, increasing the risk of developing gestational diabetes, eclampsia, pathology of labor, and is also a risk factor for the development of diseases in the newborn [5]. Violation of circadian rhythms in women of reproductive age first contributes to the disruption of the regularity of the menstrual cycle, and then leads to chronic anovulation syndrome [6], which, in turn, increases the risk of developing such a socially significant disease as breast cancer [7, 8].
The head of the American Obesity Association M. Downey in 2013 named sleep deprivation along with the presence of a TV in the sleeping room (bedroom) and watching TV before bed as one of the possible causes of obesity [9]. Recent studies have shown that disruption of the rhythm "sleep-wakefulness" affects the metabolic health of a person, including the control of body weight [10].
A meta-analysis (2008) found an association between short sleep duration in patients and obesity, confirming the association of habitually short sleep duration with an increased risk of developing obesity (1.55 times). The same researchers concluded that an increase in sleep duration per hour was accompanied by a decrease in body mass index by 0. 35 kg/m 2 [11]. Recent studies show that people with chronically short sleep duration have a higher risk of developing obesity compared to people who sleep 7–8 hours a day [10].
The alternation of the circadian cycle of day and night is an important regulator of various physiological rhythms in both animals and humans [10]. Currently, much attention is paid to the study of the activity of melatonin, one of the leading markers of the circadian rhythm and the regulator of the most important metabolic processes in humans.
Works of the last decade show that a decrease in nocturnal secretion or a violation of the pulse pattern of epiphyseal melatonin production can affect the increase in the prevalence of MS, type 2 diabetes, and oncological diseases [12–15]. The hormone melatonin was discovered in 1958 by A.B. Lerner. Changes in melatonin concentration have a noticeable diurnal rhythm: typically high levels of the hormone during the night and low levels during the day. The maximum values of melatonin concentration in human blood are observed between midnight and 5 o'clock in the morning local solar time. This hormone is produced by the main secretory cells of the pineal gland, pinealocytes, and ensures the daily and seasonal rhythm of the physiological activity of organs and tissues, adapting their work to changing environmental conditions [3]. Changing the lifestyle of women in modern big cities (increasing the duration of waking hours during the daytime, and sometimes at night), artificial lighting, the constant presence of light from TV screens, computer monitors, smartphones, phones disrupt the cyclical circadian rhythms and cause the development of desynchronosis, which , in turn, leads to a change in the daily pattern of melatonin production. In the work of A.Z. Tsfasman et al. it is shown that deprivation 1 nocturnal sleep led to a disruption in the circadian rhythm of melatonin production: synthesis at night sharply decreased and reached the daytime level, whereas in a normal lifestyle with sleep at night, its nocturnal synthesis was 63–75% of the daily production [16].
In recent years, possible associations between melatonin deficiency and obesity have been shown [17, 18].
Circadian rhythms, melatonin, women's reproductive health
The melatonin synthesis rhythm disturbance itself can be the cause of various diseases, including obesity, as shown in the work of J. Cipolla-Neto et al. The authors drew attention to the fact that the violation of biorhythms in the human body, including the metabolic balance, can lead to disadaptation in conditions of circadian rhythm disorders [17].
Research by A. Brzezinski et al. showed that melatonin can change the pulsatile secretion of luteinizing hormone (LH) and regulate folliculogenesis [3]. A high nocturnal concentration of melatonin significantly reduces the concentration of LH in blood plasma due to the prevention of its secretion [19]. It has been repeatedly shown in recent studies that this pineal gland hormone is involved in maintaining the normal maturation of follicles due to an increased concentration (by 3 times) in granulosa cells and follicular fluid (compared to blood levels) [3]. Melatonin regulates the secretion of gonadotropic hormones (LH, follicle-stimulating hormone, FSH), as well as prolactin in accordance with the daily photoperiod 2 [20]. According to D. Roy and D. Belsham, gene expression and pulsatile secretion of gonadotropin-releasing hormone (GnRH), which controls the secretion of LH and FSH, is melatonin-dependent and has a 24-hour cycle [21]. In women of reproductive age with a high concentration of melatonin in the blood serum, suppression of the function of the hypothalamus (as part of the development of hypothalamic functional amenorrhea) was noted with a reduced level of pulsatile secretion of GnRH and LH, which affects the entire process of folliculogenesis. In blind women, melatonin levels during the day are higher than in sighted women, and basal and peak levels of LH and FSH are significantly lower compared to sighted women [3].
Since the early 2000s, there has been a lot of discussion about the impact of sleep and sleep disturbances on ovulatory function.
Ovulation is also part of a woman's endogenous circadian rhythm; chronic anovulation affects the woman's menstrual cycle [22]. A. Lim et al. showed that if in women of reproductive age sleep lasts less than 6 hours, then the menstrual cycle will be disrupted by the type of "delay" or abnormal uterine bleeding [23]. Nurses, flight attendants, and women with shift work have more frequent cases of menstrual irregularities and non-pregnancy associated with chronic anovulation syndrome [24–28]. Menstrual irregularities in these women may be associated with changes in LH pulsation and amplitude as a result of circadian rhythm and sleep disturbances [29], as well as with the "stress" of the hypothalamic-pituitary-ovarian axis. Sleep has a direct suppressive effect on LH secretion, contributing to a decrease in the level of this gonadotropic hormone at night in a woman of reproductive age in the early follicular phase of the menstrual cycle [22]. Since women who work at night or with sleep disturbances have shorter and more superficial, interrupted sleep, ovarian dysfunction may be associated with impaired production and amplitude of gonadotropic hormones through an effect on GnRH [22]. In turn, such menstrual irregularities may be a risk factor for infertility, small fetal size for gestational age, and preterm birth [30].
K. Michels (2019) analyzed in detail the differences in the average concentrations of gonadotropin hormones, the magnitude of the shift in time and the amplitude of the peaks of gonadotropins, as well as the risk of developing sporadic anovulation associated with the nature of sleep and work at night. With an increase in the duration of daily sleep for every hour, the average concentrations of estradiol increased by 3.9%, progesterone in the luteal phase - by 9.4%. Sleeping less than 7 hours per day is associated with an earlier rise in FSH and LH peak levels. Women who worked nights or shifts had lower testosterone levels compared to women who worked during the day. Women with morning chronotype 3 had an earlier increase in estradiol levels during the menstrual cycle and possibly an earlier increase in LH levels. Women with the evening chronotype had a later PH peak. An increase in the risk of developing sporadic anovulation has been shown with a decrease in the amount of sleep, especially for the group with the morning chronotype [31].
An illustrative model showing the relationship between circadian rhythm disorders, melatonin and ovulatory function in a woman is a patient with polycystic ovary syndrome (PCOS) and MS. More than half of women with PCOS are overweight or obese and insulin resistant (IR) [32]. Dysfunction of white adipose tissue has been identified as the main factor contributing to the development of IR in PCOS [33]. The etiology and pathogenesis of the syndrome are still actively discussed. In recent years, the authors of studies have analyzed the role of melatonin in the pathogenesis of PCOS, which, along with its effect on cycle « sleep-wake » has additional functions, incl. immunostimulatory effect [34]. It is known that melatonin is synthesized in the ovaries, endometrium, and placenta, while its production does not depend on the circadian rhythm [35]. The level of melatonin in the follicular fluid is three times higher than in a blood sample [34]. The closer to ovulation, the higher the level of follicular melatonin, and it does not enter the general circulation [34]. In the work of J. Soares et al. it has been shown that the level of melatonin is higher in large follicles than in small ones; this allowed the authors to suggest that its increase in preovulatory follicles may stimulate ovulation. Together with FSH, melatonin plays an important role in folliculogenesis, providing follicle growth, which is confirmed by an increase in the number of atretic follicles in the ovaries after removal of the epiphysis in mice [36]. In the experiment of R. Reiter et al. a direct effect of melatonin on the synthesis of follicular steroids has been shown, however, this depends on the duration of treatment, the experimental model (cell or follicular culture) [37]. Therefore, in relation to folliculogenesis, melatonin is a “protector” of follicles from oxidative stress, has a protective effect against atresia, promoting ovulation [33].
One of the socially significant possible outcomes of PCOS is infertility due to chronic anovulation. When using melatonin in protocols of assisted reproductive technologies, Japanese authors showed that it can improve the quality of human oocytes and embryos [38].
Despite high blood levels (due to negative feedback) in women with PCOS, ovarian melatonin levels may be reduced compared to healthy control women. Decreased levels of melatonin in the follicular fluid impair folliculogenesis, which can lead to anovulation in women [34].
Meta-analysis by F. Cappuccio et al. [39], and an experimental study by E. Van Cauter [40], demonstrate that sleep disturbances and chronic sleep deprivation at night can be risk factors for the development of MS and IR in healthy adults. Mutations in the melatonin receptor gene are also associated not only with an increased risk of developing PCOS itself, but also with impaired insulin secretion and increased fasting glucose levels [33]. Genomic association studies have shown that polymorphisms in the genes encoding human melatonin receptors (MTNR1A and MTNR1B) are involved in the pathogenesis of type 2 DM [33]. Metabolic disorders that are characteristic of women with PCOS in reproductive age are also found in some physiological or pathophysiological conditions associated with a decrease in the level of melatonin in the blood: aging, shift work, high ambient light levels at night [34]. Somnological disorders are a fairly common pathology in PCOS [33, 34]. One of the epigenetic factors affecting the quality of sleep may be changes and fluctuations in melatonin levels. In the work of N. Shreeve et al. showed that in the group of women with PCOS there was a higher proportion of women with "bad sleep" (according to self-reports) compared with the control group. Women with PCOS felt more lethargic during the day due to disturbed sleep compared to women in the control group [41]. At night, the level of 6-sulfatoxymelatonin (a metabolite of melatonin in the urine) was 1.
6 times higher in women in the PCOS group than in women in the control group. Elevated nocturnal melatonin levels in PCOS women could potentially act as a free radical scavenger given the high levels of oxidative stress common in women with PCOS [23, 34]. In many studies, low levels of melatonin as part of a sleep disorder have been identified as a risk factor for the development of MS in women with PCOS [23, 33].
A. Shabani et al. showed that taking melatonin for 12 weeks in women with PCOS had a positive effect on mental health parameters (decrease in anxiety intensity, improved sleep), lowered insulin levels, HOMA-IR levels, total cholesterol and low-density lipoprotein [42 ]. Similar results were demonstrated by E. Spinedi et al.: melatonin therapy can have a protective effect on the development of MS in PCOS and be used in combination with the main pathogenetic therapy of this disease [33]. Therefore, in the literature of recent years, melatonin, as the main chronobiotic, occupies a special place in the prevention and treatment of MS [33, 43, 44]. A circadian rhythm of fluctuations in the concentration of insulin in the blood with a maximum in the daytime has been described [45].
Biological rhythms are a universal and necessary tool for adapting an organism to the environment and cover all manifestations of life from the functions of subcellular structures, cells, tissues, organs to complex behavioral reactions of an organism, populations, ecological systems. In recent years, more and more attention has been drawn to the data on the important regulatory role of the pineal gland and its main hormone melatonin in the physiology of the woman's body, including its effect on reproductive health (menstrual and ovulatory functions, the onset and course of pregnancy). However, melatonin is produced not only in the pineal gland, its synthesis is found in almost all organs, including the gonads. The action of extrapineal melatonin is usually auto- and/or paracrine. Melatonin regulates the secretion of gonadotropic hormones and prolactin in accordance with circadian rhythms. The amplitude of secretion of gonadotropin-releasing hormone, which controls the production of luteinizing and follicle-stimulating hormones, and gene expression are regulated by melatonin and are cyclical with a period of 24 hours. Living in megacities negatively affects the quantity and quality of night sleep. City dwellers are more likely to suffer from insomnia than rural dwellers. This is due to the disorganization of the circadian daily rhythms of sleep and wakefulness. Violation of the photoperiod with an increase in the light gap, light exposure (TV, smartphones, phones, laptops/computers) at night can lead to menstrual disorders, chronic anovulation syndrome, infertility, pathological pregnancy.
In recent years, circadian rhythm disorders have been actively discussed as one of the possible causes of the development of the metabolic syndrome, especially in combination with physical inactivity. Melatonin carries out a change in physiological processes in the body and controls the recovery processes in organs and tissues. Pineal hormone improves sensitivity to inulin, reducing its level to basal, and does not allow compensatory hyperinsulinemia with an increase in glucose levels. The circadian rhythm of fluctuations in the concentration of insulin in the blood with a maximum in the daytime is described. The formation and progression of the metabolic syndrome may be due to desynchronosis. Recently, there has been an increase in the number of works that describe the positive effect of the use of melatonin in combination therapy for various pathological conditions. Based on all of the above data, it can be concluded that melatonin may be an important component in the treatment of such a complex condition as metabolic syndrome in women of reproductive age.
Participation of authors:
Research concept and design — Andreeva E.N., Sheremetyeva E.V.
Collection and processing of material — Grigoryan O.R., Sheremetyeva E.V., Absatarova Yu.