Trauma affecting the brain
How Does Trauma Affect the Brain?
Trauma Therapy
Written By Isaac Smith
Introduction
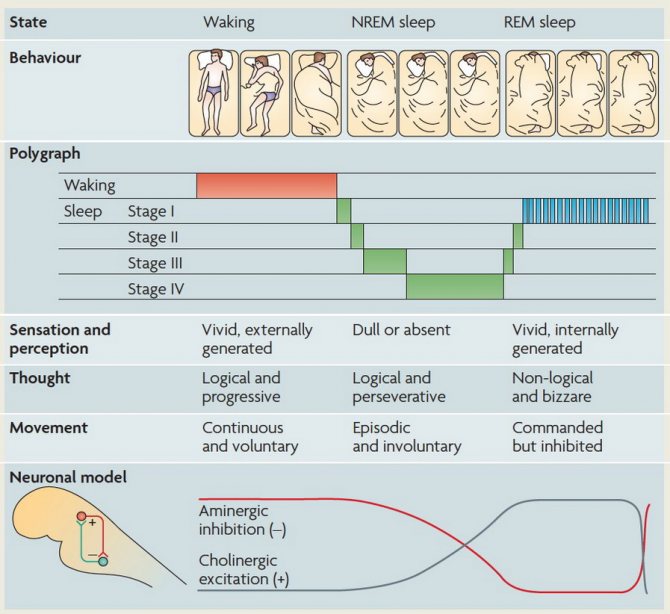
When we go through trauma, our brains don’t function like they normally do. We shift into survival mode. Like a deer in the headlights, our brains direct all our mental and physical energy toward dealing with the immediate threat until it’s gone. In normal situations, this state fades over time. Trauma isn't just something we experience after being in a warzone or in a violent situation, we can be traumatized by our relationships. See: Betrayal Trauma.
Sometimes, though, our initial trauma response sticks, making it difficult for us to function as we’d like. Trauma can change the way we think, feel, and act for a long time after the initial event. For many people, this could mean flashbacks or nightmares, a constant feeling of being on edge, loneliness, anger, intrusive thoughts and memories, self-destructive actions, and more.
All these things are very normal responses to trauma, but they don’t always go away on their own. The good news is that patterns that might seem permanent can actually be reversed--with the right approach and knowledge, you can shift your brain towards healing. However, it can be difficult to see a path forward without first understanding how and why these changes happen.
The Brain’s Response to Trauma
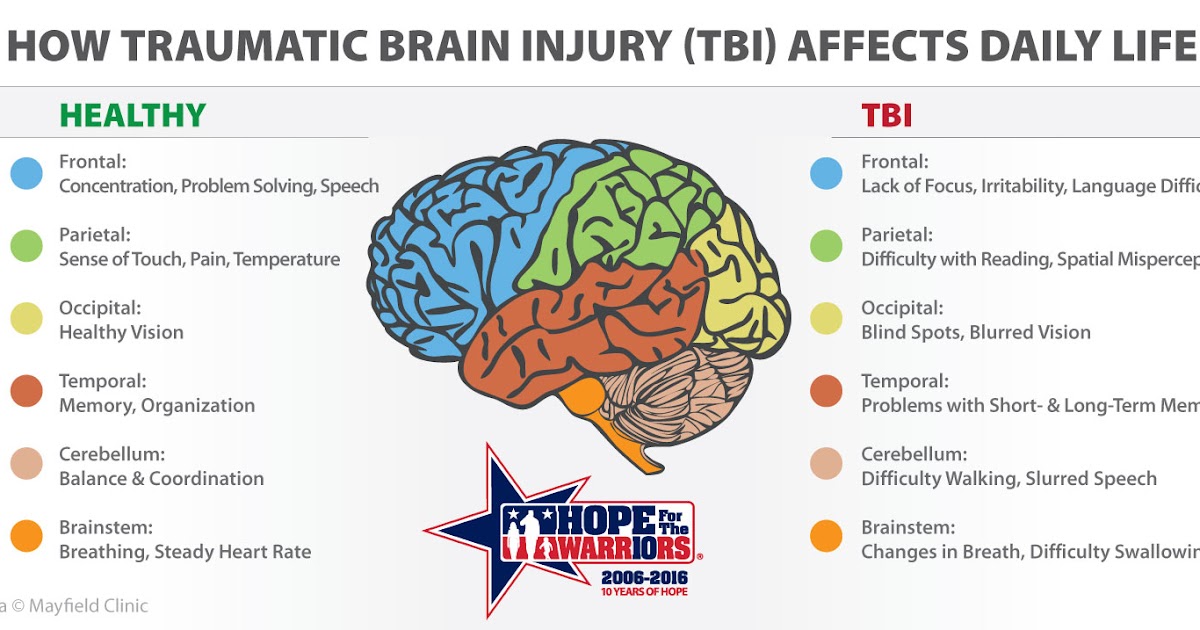
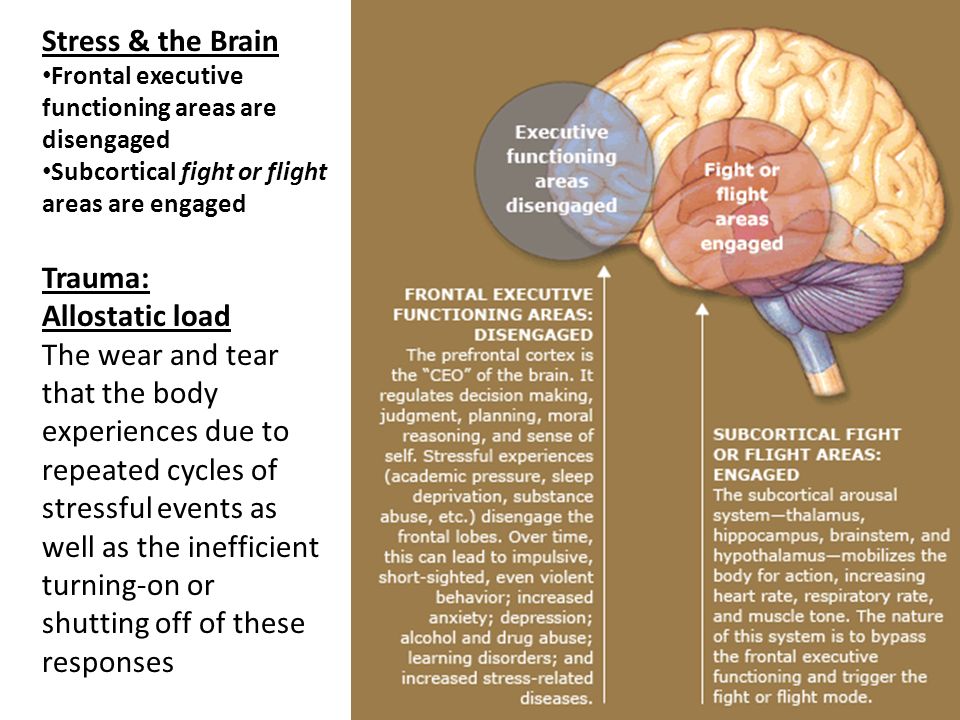
Trauma can change your brain on many levels, from the way you make decisions down to your immediate, subconscious responses to the world around you. Part of the reason it can be so hard to overcome the effects of trauma is that it goes after several areas of your brain at once.
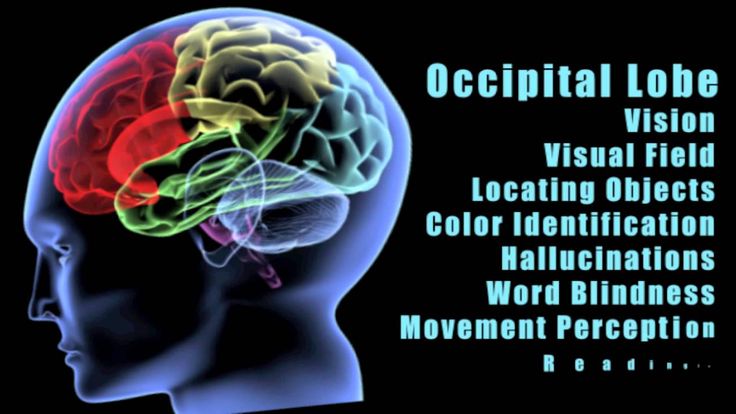
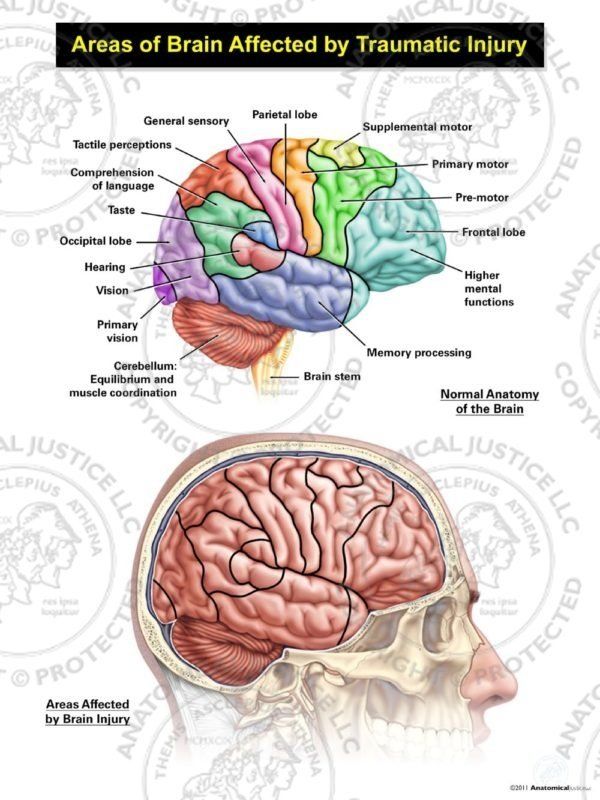
According to a 2006 study by NIH, trauma mainly affects three important parts of your brain: the amygdala, which is your emotional and instinctual center; the hippocampus, which controls memory; and the prefrontal cortex, which is responsible for regulating your emotions and impulses.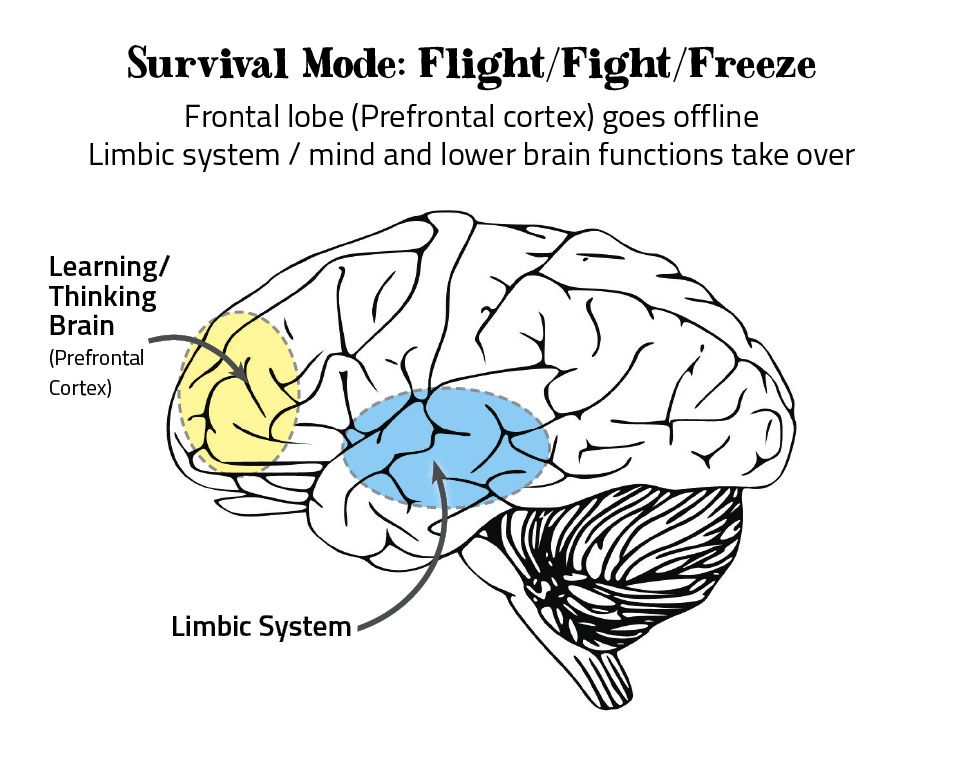 All three parts work together to manage stress.
All three parts work together to manage stress.
When you’re reminded of a traumatic experience, your amygdala (emotional and survival center) goes into overdrive, acting just as it would if you were experiencing that trauma for the first time. Your prefrontal cortex also becomes suppressed, so you’re less capable of controlling your fear--you’re stuck in a purely reactive state.
Meanwhile, trauma also leads to reduced activity in the hippocampus, one of whose functions is to distinguish between past and present. In other words, your brain can’t tell the difference between the actual traumatic event and the memory of it. It perceives things that trigger memories of traumatic events as threats themselves.
Trauma can cause your brain to remain in a state of hypervigilance, suppressing your memory and impulse control and trapping you in a constant state of strong emotional reactivity.
The Healing Process
It might seem like trauma does irreversible damage to your brain--that’s not true. Our brains are extremely adaptable. Neuroplasticity, the brain’s ability to form new connections, explains why we can rewire our brains to reverse trauma’s damaging effects.
Our brains are extremely adaptable. Neuroplasticity, the brain’s ability to form new connections, explains why we can rewire our brains to reverse trauma’s damaging effects.
Our brains are more susceptible to change than many people think, and even though overcoming trauma is a difficult process, you’re actually changing the way your brain works: adding new pathways, increasing the functions of certain areas, and strengthening connections. It’s the same mechanism that allows us to grow and change by learning.
During the healing process, you can actually rewire and retrain your brain to reverse the effects of trauma. You can reinforce your prefrontal cortex and get back rationality and control. You can strengthen your hippocampus and help your memory work how it’s supposed to. And you can subdue the hyperactive amygdala, which will help bring you peace.
With time and the right help and therapeutic methods, you can find a way to overcome trauma, right down to your neurons.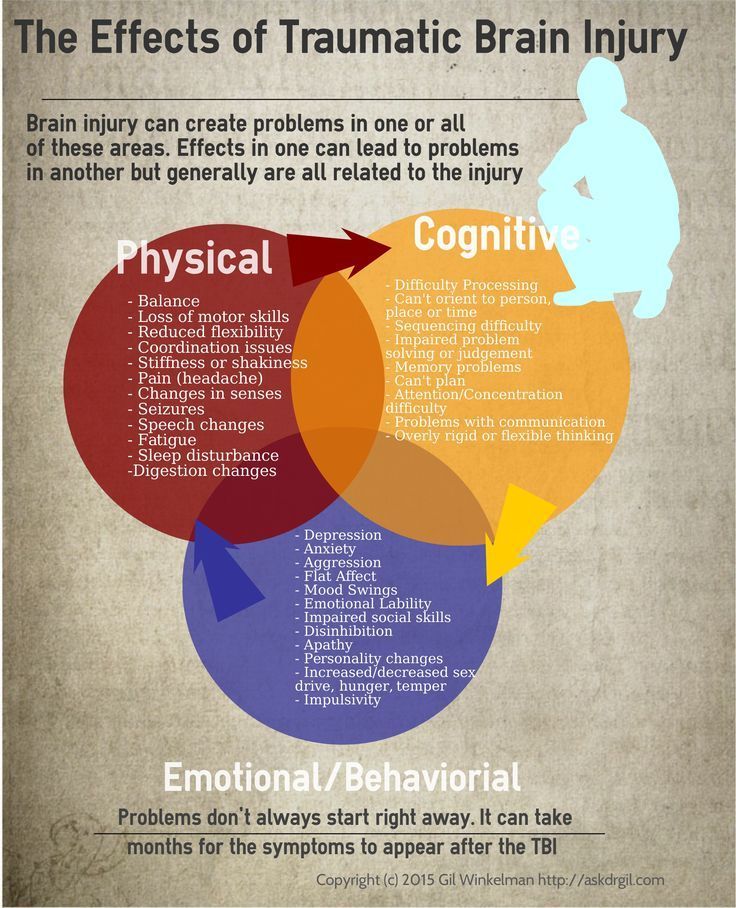
Our approach at Whole Wellness Therapy is based on this simple truth, that our brains physically change based on our surroundings. That means that the best therapeutic environment that we work to create at our offices, puts you in a growth producing environment. This philosophy is what makes us so successful in treating the complexity of past trauma with our unique trauma therapy.
Read More About Brain Science:
https://highlandspringsclinic.org/blog/can-emotional-trauma-cause-brain-damage/
https://brainblogger.com/2015/01/24/how-does-post-traumatic-stress-disorder-change-the-brain/
Read More About Neuroplasticity:
https://positivepsychology.com/neuroplasticity/
About The Author
Isaac Smith, MAT, LCSW, FNTP is the founder of Whole Wellness Therapy, and serves as the Executive Director. Isaac gives presentations on topics including addiction, trauma, grief and loss, and anxiety, in addition to providing professional consultations.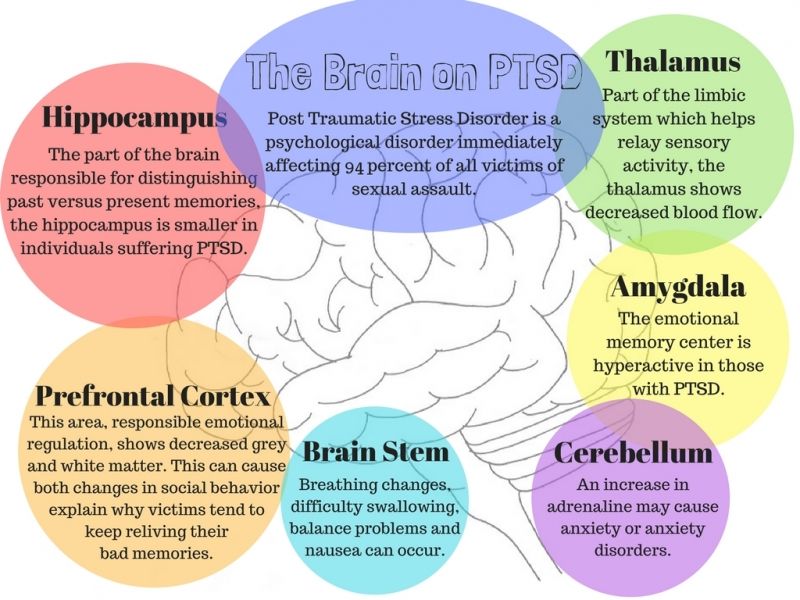 Prior to founding the practice, Isaac worked with UC Davis Health to help them build and launch their substance use disorder treatment program as well as their Collaborative Care program, which focuses on treating chronic depression and anxiety in older adults. Committed to life-long learning, Isaac holds a master's degree in Theology and has advanced training in nutritional therapy. Currently, he is pursuing a doctor of psychology degree at the Wright Institute in Berkeley, CA.
Prior to founding the practice, Isaac worked with UC Davis Health to help them build and launch their substance use disorder treatment program as well as their Collaborative Care program, which focuses on treating chronic depression and anxiety in older adults. Committed to life-long learning, Isaac holds a master's degree in Theology and has advanced training in nutritional therapy. Currently, he is pursuing a doctor of psychology degree at the Wright Institute in Berkeley, CA.
Get Started With Trauma Therapy Today
Isaac Smith
The Effects of Trauma on the Brain
People often talk about how the effects of childhood trauma can carry over into adulthood, and it is true.
Traumatic events and experiences can have a lasting impact on people. For some people, effects will include the development of post-traumatic stress disorder symptoms that can vary in severity and sometimes hinder their lives, especially if they never receive formal PTSD treatment.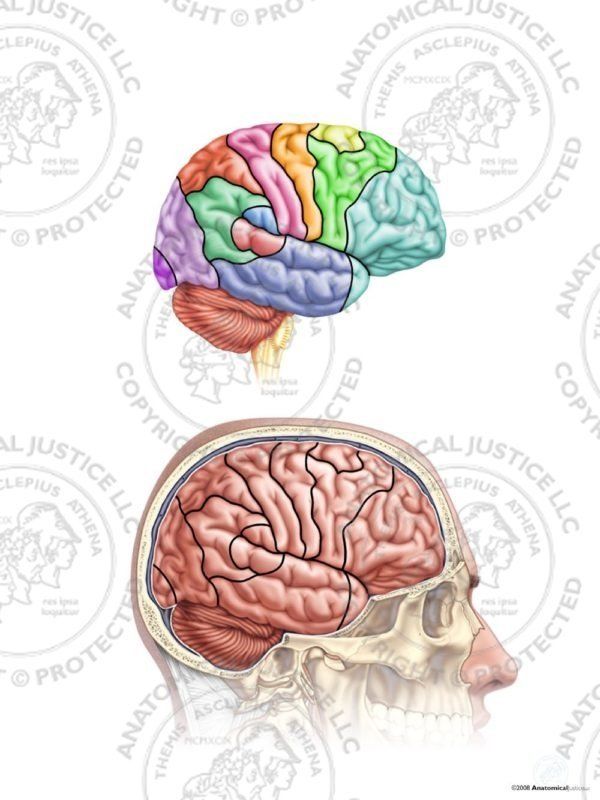 For others, trauma can lead to more subtle changes in their behavior, actions, or thinking. Either way, trauma can impact people in more ways than they may realize.
For others, trauma can lead to more subtle changes in their behavior, actions, or thinking. Either way, trauma can impact people in more ways than they may realize.
What many people do not know is that there could be more going on below the surface. As a mental health care facility, we know that not only can traumatic events impact your behavior, but the brain changes after trauma as well. Depending on the traumatic event as well as the individual, the effects of emotional trauma on the brain can range from minor to dramatic. Trauma changes brain chemistry as well as structure, and these effects can start to impact normal functioning. Specifically, the effects of trauma on the brain seem to impact the amygdala, hippocampus, and prefrontal cortex the most.
Changes in the Amygdala from Trauma
The amygdala is the emotional response center of the brain that helps people perceive and control their emotions.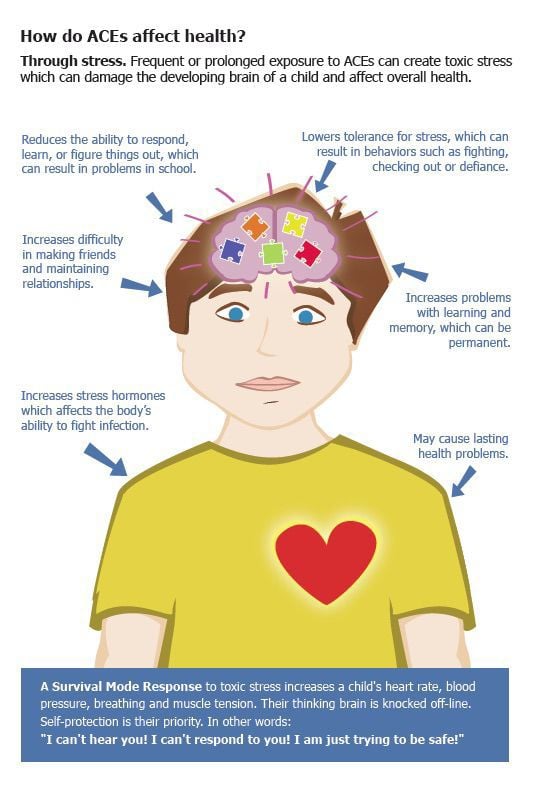 It also plays a role in emotional memories and fear response. When someone experiences a traumatic event and is showing signs of PTSD, their amygdala often becomes more active than it normally would. Studies have continuously found that the amygdala of someone with PTSD has increased function in response to stimuli that remind them of their trauma or other fear-related stimuli.1 Not surprisingly, people with PTSD often have greater fear responses and this research suggests that it may be a result of these changes in the amygdala.
It also plays a role in emotional memories and fear response. When someone experiences a traumatic event and is showing signs of PTSD, their amygdala often becomes more active than it normally would. Studies have continuously found that the amygdala of someone with PTSD has increased function in response to stimuli that remind them of their trauma or other fear-related stimuli.1 Not surprisingly, people with PTSD often have greater fear responses and this research suggests that it may be a result of these changes in the amygdala.
Changes in the Hippocampus from Trauma
The hippocampus is associated primarily with memory and learning. Brain scans have shown that the hippocampus has decreased function in people with PTSD when they are exposed to something that reminds them of trauma.1 Not only is the function of the hippocampus affected by trauma, but also the structure may change as well depending on how severely the person has been affected by their trauma.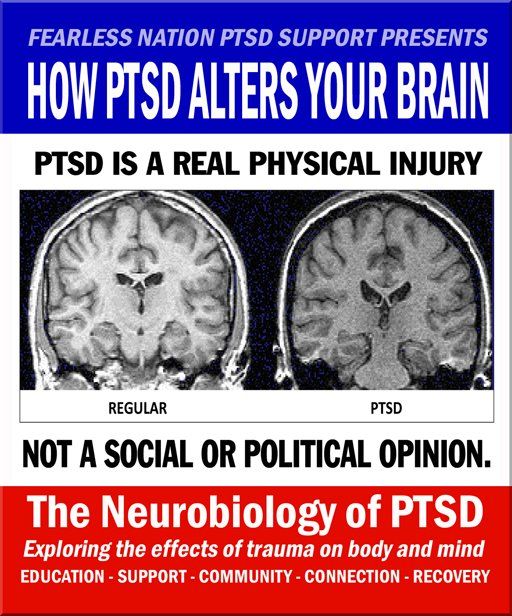 Those with PTSD were found to have significantly smaller hippocampi than those who were exposed to trauma but not experiencing PTSD.2 In this case, the effects of PTSD on the brain are more severe than trauma exposure alone.
Those with PTSD were found to have significantly smaller hippocampi than those who were exposed to trauma but not experiencing PTSD.2 In this case, the effects of PTSD on the brain are more severe than trauma exposure alone.
Changes in the Prefrontal Cortex from Trauma
The effects of trauma on the brain also extend to the prefrontal cortex. The prefrontal cortex is the part of the brain that is responsible for executive functioning or higher-level thinking and reasoning. People with PTSD have been found to have decreased function and activation of the prefrontal cortex when exposed to traumatic reminders.1 This may account for any irrational fears that trauma victims have trouble overcoming.
Whether subtle or significant, trauma changes the brain in several ways and can lead to lasting negative effects. The best way to overcome these challenges is to find a trauma treatment center that can help address these issues and possibly reverse some of these effects.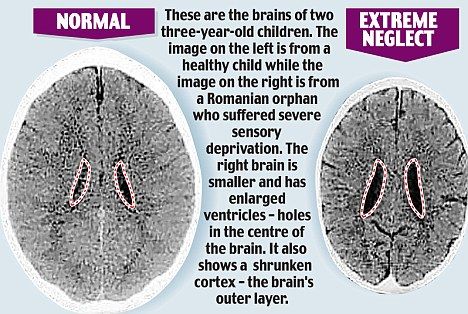
At Banyan Mental Health, we help people better manage their mental health so that they can start moving forward with their lives once more. Stop letting your mental health hinder your life or don’t stand by as your loved one suffers.
To get more information on our various programs and how we may be able to help, call us today at 888-280-4763.
Sources:
- NCBI - Traumatic stress: effects on the brain
- NCBI - Smaller Hippocampal Volume in Posttraumatic Stress Disorder: A Multisite ENIGMA-PGC Study: Subcortical Volumetry Results From Posttraumatic Stress Disorder Consortia
Head Injuries – Spinal Injuries, First Aid and Treatment at ON CLINIC Ryazan
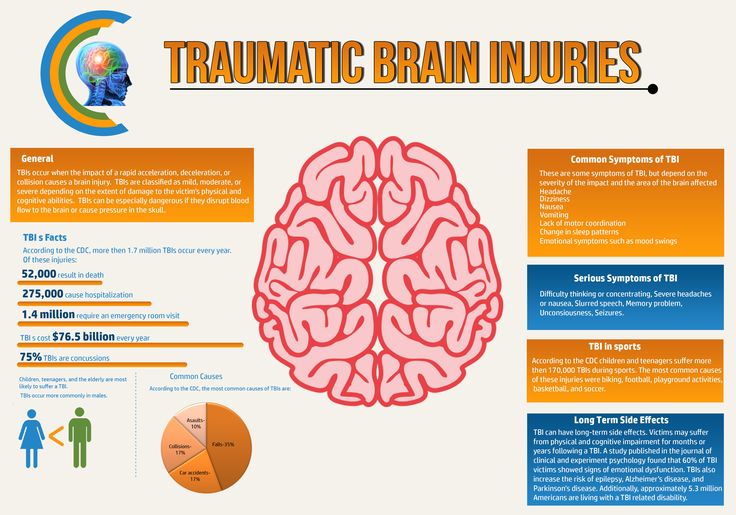
As a result of blows or bruises that violate the integrity of soft and bone tissues, as well as dysfunction of various organs and systems of the body, injuries are formed that can lead to extremely serious consequences. Head and spine injuries are especially dangerous, which can be accompanied by damage to the brain and spinal cord of varying severity.
Head and spine injuries are especially dangerous, which can be accompanied by damage to the brain and spinal cord of varying severity.
Head injury: types, causes, symptoms
More than half of all injuries are due to head injuries. Traumatic brain injury can be obtained even when the bones of the skull are not damaged. However, the deformity of the cranial bones of varying severity that occurred during the injury can seriously aggravate the condition of a patient with post-traumatic brain injury. There are open and closed craniocerebral injuries.
Most often, such injuries result in:
- all kinds of accidents, including traffic accidents;
- falls - both from the upper floors of buildings and from the height of one's own height;
- injuries resulting from fights and attacks, etc.
Traumatic brain injury can cause severe bleeding, all kinds of memory and / or speech disorders, sleep disturbances and nervous system functions of varying severity, visual and hearing impairments, as well as dizziness, nausea and vomiting, convulsions, paralysis, impaired respiratory function and even to whom.
If a patient with a head injury after receiving it is not provided with first aid in a timely manner, this can lead to a life-threatening condition for the patient.
If you witness any incident in which the participant may have suffered a head injury, then call an ambulance. Before the medical team arrives, the victim needs rest. If possible, measures should be taken to stop bleeding, if any.
Spinal injuries
Spinal injuries are classified according to their location. In addition to injuries affecting one or another section of the spine, there are also mixed ones - in cases where two or more sections are injured. However, the most dangerous injuries are those in which the spinal cord is affected. They are called vertebral-spinal. It is these injuries that often lead to disability of the victim.
The most common causes of spinal injuries are:
- various accidents;
- diving into an unfamiliar body of water, as a result of which a person hits his head on the bottom or on stones;
- fall from a height.
The following symptoms may indicate a spinal injury:
- loss of some functions and reflexes - for example, the inability to move the lower limbs;
- neck pain;
- loss of sensation or tingling in various parts of the body;
- fainting;
- slow pulse and low blood pressure.
Sometimes spinal injuries after a blow or bruise can cause a loss of control over the excretory functions of the body. This is accompanied by involuntary urination and fecal eruption. Timely first aid, and then qualified medical care, is simply necessary for victims with an injured spine. Before the arrival of the ambulance team, it is necessary to fix him in such a way that his neck and back are motionless.
Treatment of spinal and head injuries at ON CLINIC Ryazan
To identify the consequences of a neck and / or head injury, in addition to visual examination and palpation, the victim may be sent for the following instrumental studies:
- X-ray of the corresponding part of the spine and/or skull bones;
- CT to rule out internal bleeding;
- various neurological examinations, etc.
In our medical center, qualified neurologists prescribe complex therapy aimed at reducing the harm from the consequences of injuries to patients with craniocerebral and spinal injuries. It is possible to treat injuries both surgically and conservatively. Great attention is paid to the rehabilitation of the patient under the supervision of the attending physician. The course of rehabilitation, as well as treatment, is developed individually for each patient and includes physiotherapy, adherence to a special diet, therapeutic exercises, etc.
Our doctors regularly attend refresher courses. In combination with vast experience, this helps them to put even the most "severe" patients on their feet. The recovery period takes a minimum of time and completely returns the patient to his usual way of life.
Infectious lesions of the brain - Communal non-commercial enterprise "Kherson Regional Clinical Hospital" Kherson Regional for the sake of
- Details
-
Updated: 02 July 2019
-
Created: October 02, 2019
-
Look back: 3521
http://granstroy. ru/
ru/
furniture Joomla templates
interesting facts
Neuroinfections are one of the most dangerous for human life and health. Normally, the brain and spinal cord have reliable protection against the penetration of infectious agents. Unlike other organs, in the brain and spinal cord, each blood capillary is surrounded by an additional "case" of protective cells - the so-called neuroglial cells. These cells create a reliable barrier for many microorganisms and toxins, as well as medicinal substances.
Under certain conditions, for example:
- reduced immunity,
- head and spinal injuries,
- long-term septic infections
The blood-brain barrier fails and pathogens enter the brain or spinal cord. There is an infectious inflammation of its membranes (meningitis) or the medulla itself (encephalitis).
Qualitative diagnostics and treatment of infectious lesions of the brain and spinal cord in the neurosurgical department of the regional hospital of Kherson!
Meningoencephalitis can be caused by:
- bacteria,
- viruses,
- mushrooms,
- parasites.
Microorganisms can enter the brain after injury of its membranes in case of fractures of the bones of the vault of the base of the skull, in the presence of liquorrhea, after neurosurgical operations, in septic conditions against the background of immunodeficiencies.
Clinical manifestations of CNS infection
Clinical manifestations of infection of the central nervous system are very diverse, but common is:
- severe condition of patients,
- symptoms of general intoxication with hyperthermia,
- meningeal syndrome,
- as well as focal symptoms of brain damage in the form of a loss of the corresponding functions.
Diagnosis of lesions of the brain and spinal cord
Diagnosis of infectious lesions of the brain and spinal cord is based on characteristic clinical manifestations, data from blood tests, cerebrospinal fluid, neuroimaging methods - MRI of the brain and spinal cord.
In most cases, the treatment of infections of the central nervous system takes place without surgery, however, in some cases, with a local accumulation of pus in the brain (abscess) or in the spinal canal, an operation is necessary to drain the purulent cavity or remove the entire formation.
Temp. Malyshenko M.P.
Medical treatment
Medical treatment of brain infections
Infections of the brain and spinal cord can be caused by:
- viruses,
- bacteria,
- mushrooms,
- sometimes, protozoa or parasites.
Infectious lesions of the brain are often accompanied by lesions of other parts of the central nervous system, including the spinal cord and its membranes. The brain and spinal cord are usually protected from infection by the natural blood-brain barrier, but when infection occurs, the consequences are often very serious.
Infections can cause brain inflammation ( encephalitis ) or inflammation of the meninges ( meningitis ).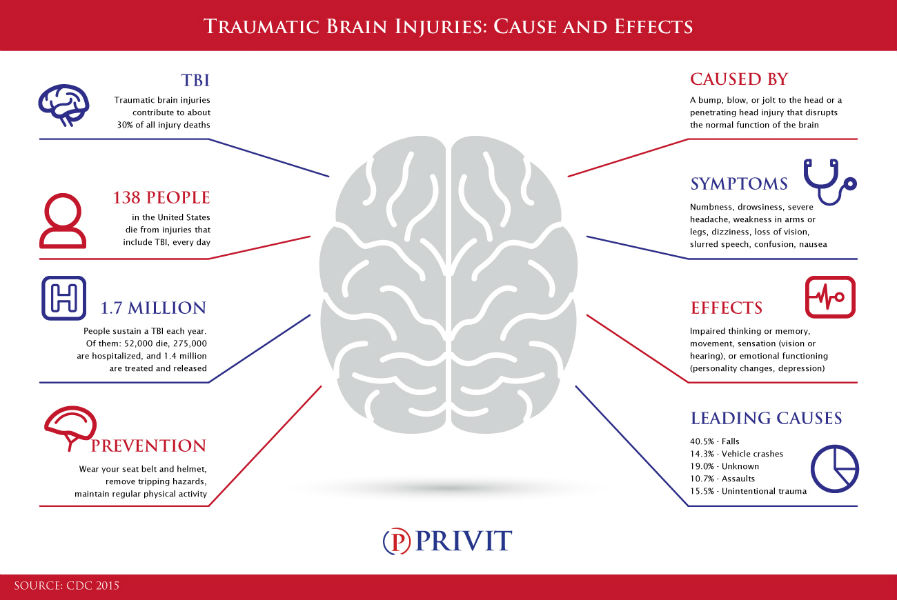 Viruses are the most common causes of encephalitis. Often, bacterial inflammation of the meninges (meningitis) spreads to the brain itself, causing encephalitis.
Viruses are the most common causes of encephalitis. Often, bacterial inflammation of the meninges (meningitis) spreads to the brain itself, causing encephalitis.
High-quality conservative treatment of infectious brain lesions in the neurosurgical department of the Kherson Regional Hospital!
Similarly, viral infections that cause encephalitis often also cause meningitis. When both the brain and the meninges are already infected, this condition is called meningoencephalitis . Usually, in encephalitis and meningitis, the infection is not limited to one area. The inflammatory process can spread throughout the brain or its membranes, along the entire length of the spinal cord. However, in some conditions, the infection is limited to one area in the form of a cavity or pocket of pus called an empyema or abscess.
There are several routes of infection of the brain and its membranes
Bacteria and other infectious organisms can enter the central nervous system in several ways:
- by hematogenous route (infection through blood flow),
- by contact - directly from the outside (for example, through skull fractures or during brain surgery),
- with purulent inflammation of neighboring ENT organs (sinusitis, otitis media).
Conservative treatment of infectious lesions of the brain and spinal cord is a difficult task that requires an integrated approach. Antibacterial therapy begins as early as possible, even before the results of bacteriological seeding of infected material. As a rule, the most modern antibacterial and antiviral agents and their combinations are used. Given the fact that many antibiotics do not penetrate well into the brain through the blood-brain barrier, intrathecal administration with spinal puncture is used.
In particularly difficult cases, long-term external spinal or ventricular drains are required. In parallel with antibiotic therapy, active detoxification therapy is carried out, and immune disorders are corrected.
Surgical treatment
Surgical treatment of infectious brain lesions
The most common causes of infectious lesions of the brain and spinal cord are:
Infectious complications of trauma:
- 0012
- penetrating traumatic brain injury,
- firearms
- and mine-explosive wounds.
Due to the spread of infection from inflammatory foci, or as a result of iatrogenic:
- after punctures,
- blockade,
- injection.
If the therapy is ineffective in the cranial cavity, spinal canal, abscesses are formed - a limited accumulation of purulent contents or empyema - an accumulation of purulent contents without clear boundaries.
High-quality surgical treatment of infectious brain lesions in the neurosurgical department of the Kherson regional hospital!
The most informative methods for diagnosing a purulent process are:
- MSCT
- and MRI with contrast.
Treatment of infectious lesions must necessarily be complex, but if there are indications, surgical treatment should be primary, only if the purulent focus is removed, the patient can be successfully treated.
The main method of surgical treatment is the drainage of the purulent focus: after careful planning of the surgical intervention, the patient under general anesthesia performs a puncture of the accumulation of pus, after which a drainage system is installed in the cavity, through which the remnants of purulent contents are washed out with solutions of antiseptics and antibiotics. During the operation, the contents of the abscess or empyema are taken for analysis to select the most effective antibiotic.
During the operation, the contents of the abscess or empyema are taken for analysis to select the most effective antibiotic.
In the postoperative period, the patient undergoes MSCT to control the dynamics of the cleansing of the purulent focus.
In the presence of a primary infectious process:
- otitis media,
- frontita,
- odontogenic process
- etc.
it must be sanitized by a specialized narrow specialist. One of the latest techniques introduced in the neurosurgical department of the Kherson Regional Clinical Hospital is drainage of purulent brain processes under ultrasound navigation, which increases accuracy and reduces trauma to healthy tissues.
Diagnostic surgery for lesions of the brain
Infectious lesions of the brain and spinal cord may be:
- independent diseases (e.g. bacterial meningitis),
- and complications of trauma (due to open and penetrating head injuries)
- or specific diseases (tuberculous meningitis, HIV).
Considering the similarity of symptoms and data from additional research methods (even such highly informative ones as MSCT and MRI), it is sometimes very difficult to establish an accurate diagnosis.
High-quality diagnostic operations (punctures, biopsies) for infectious brain lesions in the neurosurgical department of the Kherson regional hospital!
Establishing a diagnosis
The main diagnostic manipulation (in the absence of contraindications) that will help to accurately establish the diagnosis is spinal puncture , during which the nature of the cerebrospinal fluid is assessed and sampling is performed. If it is impossible to establish a diagnosis using additional research methods, a diagnostic surgical intervention is performed - in the area of the formation of interest (cyst, abscess, etc.), a burr hole is applied and its puncture is performed, if purulent contents are found, drains are installed in the cavity, if there is content of an unidentified nature is taken for further laboratory testing.
Radical operations: opening and drainage of abscesses, empyema
Opening and drainage of abscesses, empyema
Intracranial and spinal epidural abscesses and subdural empyema is a pocket or local accumulation of pus that develops between the skull and the upper layer of tissues (dura mater) covering the brain.
Subdural empyema
This is a pocket of pus that develops between the dura mater and the middle layer of tissue (arachnoid membrane) that covers the brain.
Intracranial epidural abscesses and subdural empyema
Intracranial epidural abscesses and subdural empyema develop outside the brain itself but inside the skull (intracranial) or spinal canal.
Qualitative radical operations for opening and draining abscesses, empyema in the neurosurgical department of the regional hospital of Kherson!
Inside the skull, the brain is covered with three layers of tissue called meninges:
- Dura mater (outer layer)
- Arachnoid sheath (middle layer)
- Pia mater (inner layer)
Intracranial epidural abscess develops between the dura and the skull.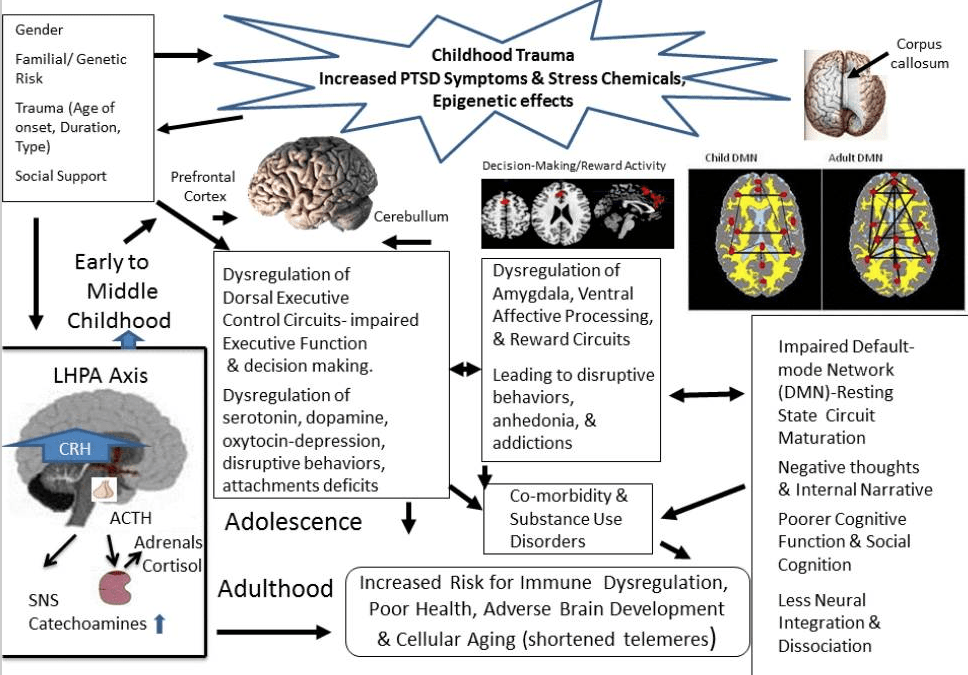 A subdural empyema develops between the arachnoid mother and the dura mater.
A subdural empyema develops between the arachnoid mother and the dura mater.
The main method of treatment of intracranial and spinal abscesses and empyema is surgical.
Spinal (lumbar puncture) is not very effective and can be dangerous if there is a large abscess in the cranial cavity, empyema, removal of cerebrospinal fluid during the puncture can cause the brain to move down and it can be wedged into natural holes and cracks. Infringement of the brain stem sections can lead to death.
For brain abscesses larger than 2 cm in diameter, empyema causing displacement of the brain, a surgical drainage method is used, which consists in inserting a thin tube into the abscess cavity to remove pus and wash with antiseptics. Surgery of such formations is an extremely important and necessary procedure, since a breakthrough of pus into the spaces surrounding the brain leads to severe complications and even death of the patient. Timely treatment is extremely important, since delaying the operation can lead to a significant increase in brain damage.