Chills in chest
5 Reasons Why You Might Have the Chills
Are chills serious? Shivering and goose bumps can accompany a wide range of conditions, from a too-cold environment to cancer.
Maintaining our core temperature is one of the body’s most basic functions, and when that temperature is off — or when our body thinks it’s off — we get the chills.
“Chills occur when the muscles contract and relax in order to make heat,” says Rose Taroyan, MD, a family medicine physician at Keck Medicine of USC and clinical assistant professor of family medicine at the Keck School of Medicine of USC. “This occurs when you are cold, but it can also be your body’s defense mechanism in fighting an infection.”
Everyone knows the sensation of getting the chills when your environment is too cold. That’s usually a signal to put on more layers or turn up the heat. But there are many underlying medical conditions that can cause them, too. Read on for some common — and not so common — causes of chills.
1. You have a viral or bacterial infection.
When chills are accompanied by other symptoms, such as fever, body aches or fatigue, they’re more likely associated with a systemic infection, such as flu or pneumonia.
“Chills boost your body’s core temperature when your immune system attempts to fight off infection,” Taroyan explains. “Your body temperature increases, even though you might feel cold. If you have a viral infection, you will usually notice other symptoms along with chills, such as sore throat, cough, headache, fatigue and muscle aches. Most of the time, it can be self-limiting and will resolve within 2 weeks. It’s important to get plenty of rest and increase your fluid intake.”
2. You have low blood sugar.
Although many people feel a bit shaky and irritable when they need to eat, true hypoglycemia, or low blood sugar, most often occurs in people who have diabetes.
“One of the symptoms of hypoglycemia is a feeling of shakiness, which may mimic chills,” Taroyan says. “Hypoglycemia requires immediate treatment to get blood sugar levels back to normal.”
“Hypoglycemia requires immediate treatment to get blood sugar levels back to normal.”
Defined as blood glucose of less than 70 milligrams per deciliter, hypoglycemia can cause a variety of other symptoms, including sweating, confusion, a rapid heartbeat, blurry vision, lightheadedness and drowsiness.
If you have diabetes and you notice these symptoms, follow the “15-15” rule: Have 15 grams of simple carbs, such as a glucose tablet, juice, honey or hard candy, and check your blood glucose again in 15 minutes. Then eat a meal, but don’t overeat, or your blood sugar will spike.
3. You’re having a panic attack.
Chills can occur if you have a profound or intense emotional reaction to a situation, according to Taroyan. “Emotions that might cause chills include fear or anxiety,” she says.
According to the American Psychiatric Association, nearly 30% of all adults will experience an anxiety disorder during their lifetime. A panic attack can cause a combination of physical as well as psychological symptoms, including chills, shortness of breath, heart palpitations, sweating, dizziness and chest pain. Because of the severity of the symptoms, a panic attack sometimes causes people to think they’re having a heart attack.
Because of the severity of the symptoms, a panic attack sometimes causes people to think they’re having a heart attack.
If you’ve never had a panic attack before, seek medical attention. If you’ve been diagnosed with an anxiety disorder, psychotherapy (“talk” therapy) and medication can help.
4. You have malaria.
Symptoms of malaria, a disease spread by infected mosquitos, can mimic those of a cold or flu. In addition to chills, they can include fever, sweats, head and body aches, nausea and fatigue. A simple blood test can identify the presence of the malaria parasite, but since malaria is relatively rare in the United States, your doctor might not immediately test for it. If you’ve traveled to regions where the disease is common, such as sub-Saharan Africa, Southeast Asia, parts of India and parts of Central and South America within the last 12 months, be sure to mention it when you’re being evaluated, even if you took antimalarial medications.
5. You have leukemia.

Chills can also be a sign of blood cancers, including leukemia. Symptoms of leukemia may include swelling of the lymph nodes, along with fever, chills, fatigue, loss of appetite, night sweats, abdominal pain and recurring infections. If you have a fever and chills that just won’t go away, see your doctor, in case it’s something more serious.
Having the chills may be nothing more than the body’s attempt to warm you up, but if they’re accompanied by other symptoms, that’s the time to seek medical attention. “Please schedule an appointment with your primary care physician for further evaluation,” Taroyan advises.
Topics
chills
Dr. Rose Taroyan
fever
hypoglycemia
leukemia
panic attack
Tina Donvito
Tina Donvito is a freelance writer covering health, culture, travel and parenting.
Causes and When to See a Doctor
Fever and Chest Pain: Causes and When to See a DoctorMedically reviewed by Kevin Martinez, M.D. — By Scott Frothingham on November 19, 2019
Individually, fever and chest pain are often a sign that you should see your doctor. But if you experience fever and chest pain at the same time, it’s important to seek immediate medical attention.
But if you experience fever and chest pain at the same time, it’s important to seek immediate medical attention.
When to see a doctor for a fever
As an adult, you should call your doctor if your fever reaches 103°F or higher. You should get immediate medical care if your fever is accompanied by:
- chest pain
- severe headache
- unusual, worsening rash
- mental confusion
- neck pain
- abdominal pain
- persistent vomiting
- pain when urinating
- seizures or convulsions
When to see a doctor for chest pain
New or unexplained chest pain can raise the concern of a heart attack. If you feel that you’re having a heart attack, immediately seek medical help. Your chances of surviving a heart attack are greater the sooner emergency medical treatment starts.
According to the Centers for Disease Control and Prevention (CDC), along with chest pain and discomfort, the major symptoms of heart attack are:
- lightheadedness
- weakness
- jaw, neck, or back pain
- arm or shoulder discomfort
- shortness of breath
Women may experience other symptoms of a heart attack, including unexplained or unusual:
- fatigue
- nausea
- vomiting
There are a number of health conditions that may cause both fever and chest pain, including:
- flu
- bronchitis
- pneumonia
- myocarditis
- pericarditis
- infectious esophagitis
The flu is a contagious respiratory illness that can be mild, severe, or even fatal. It’s caused by the influenza virus infecting the nose, throat, and lungs.
It’s caused by the influenza virus infecting the nose, throat, and lungs.
According to the CDC, on average about 8 percent of the population of the United States gets infected each flu season.
- Symptoms: headache, muscle ache, cough, stuffy nose, fatigue, chills, sore throat, pressure or pain in chest or abdomen, fever (not everyone with the flu will have a fever)
- Treatment: rest, fluids, antiviral drugs
Bronchitis is an infection of the mucous membrane that lines the bronchial tubes that carry air to and from your lungs.
- Symptoms: cough, slight fever, chest discomfort, fatigue, mucus production, chills, shortness of breath
- Treatment: cough medicine, inhaler, antibiotics (if bacterial), humidifier
Pneumonia is an inflammation of the lungs caused by a viral or bacterial infection.
- Symptoms: fever, cough, shortness of breath, chest pain, fatigue, nausea, chills
- Treatment: over-the-counter (OTC) medications such as aspirin, ibuprofen, or acetaminophen, fluids, humidifier, rest, antibiotics (if bacterial), oxygen therapy
Myocarditis is an inflammation of the heart muscle.
- Symptoms: chest pain, fatigue, fluid retention, arrhythmias, shortness of breath, headache, fever, joint pain, sore throat
- Treatment: beta-blockers (metoprolol, carvedilol), angiotensin converting enzyme (ACE) inhibitors (enalapril, lisinopril), angiotensin II receptor blockers (ARBs) (valsartan, losartan), diuretics
Pericarditis is an inflammation of the sac that surrounds the heart.
- Symptoms: chest pain (center or left side), pain traveling to shoulder and neck, heart palpitations, fatigue, low grade fever, cough, swelling (leg or abdomen)
- Treatment: OTC medications such as ibuprofen or aspirin, colchicine, corticosteroids
Infectious esophagitis is irritation and swelling of the esophagus, the tube connecting your throat to your stomach. It’s caused by a virus, bacteria, or a fungus.
- Symptoms: difficulty swallowing, pain when swallowing, chest pain, fever, nausea
- Treatment: antifungal medication (fluconazole) for fungal esophagitis, antiviral medication (acyclovir) for viral esophagitis, antibiotics for bacterial esophagitis
Individually, fever and chest pain are a reason for concern and a visit with your doctor.
If you have fever and chest pain at the same time, seek immediate medical care. It could be a sign of a serious health condition.
Last medically reviewed on November 19, 2019
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Bronchitis. (n.d.).
nhlbi.nih.gov/health-topics/bronchitis - Flu symptoms & complications. (2019).
cdc.gov/flu/symptoms/symptoms.htm - Heart attack signs & symptoms. (2018).
cdc.gov/heartdisease/signs_symptoms.htm - Influenza (flu). Treatment: What you need to know. (2019).
cdc.gov/flu/treatment/treatment.htm - Key facts about influenza (flu). (2019).
cdc.gov/flu/about/keyfacts. htm
htm - Lehrer J, et al. (n.d.). Infectious esophagitis.
urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=134&ContentID=169 - Mayo Clinic Staff. (2017). Fever.
mayoclinic.org/diseases-conditions/fever/symptoms-causes/syc-20352759 - Mayo Clinic Staff. (2017). Bronchitis.
mayoclinic.org/diseases-conditions/bronchitis/symptoms-causes/syc-20355566 - Mayo Clinic Staff. (2018). Pericarditis.
mayoclinic.org/diseases-conditions/pericarditis/symptoms-causes/syc-20352510 - Mayo Clinic Staff. (2019). Myocarditis.
mayoclinic.org/diseases-conditions/myocarditis/symptoms-causes/syc-20352539 - Perkins J, et al. (n.d.). Fever and chest pain.
antimicrobe.org/e39.asp - Pneumonia symptoms and diagnosis. (2019).
lung.org/lung-health-and-diseases/lung-disease-lookup/pneumonia/symptoms-and-diagnosis.html - Pneumonia treatment and recovery.
 (2019).
(2019).
lung.org/lung-health-and-diseases/lung-disease-lookup/pneumonia/treatment-and-recovery.html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Kevin Martinez, M.D. — By Scott Frothingham on November 19, 2019
Read this next
Everything You Need to Know About Fever
Medically reviewed by Cameron White, M.D., MPH
Find information on the causes, treatment, and prevention of fever. Learn when you should see a doctor about a fever.
READ MORE
10 Causes of Headache and Fever and What to Do
Medically reviewed by Stacy Sampson, D.O.
Headache and fever could be caused by a number of medical issues, including cold and flu, infections, and other more serious conditions.
READ MORE
What Are the Causes of Chest Pain?
Medically reviewed by Lauren Castiello, MS, AGNP-C
When you have chest pain, your first thought may be that it's a heart attack.
 However, other less serious conditions can also cause chest pain. Learn…
However, other less serious conditions can also cause chest pain. Learn…READ MORE
30 Causes for Chest Pain and When to Seek Help
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Chest pain isn’t always a sign of a medical emergency. Here are 30 possible causes for this symptom.
READ MORE
11 Causes of Chest Pain and Cough
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Chest pain and cough can have a simple cause, like the flu. But they could also be a sign of something more serious, like pneumonia, bronchitis, or…
READ MORE
What’s Causing Pain in the Left Side of My Chest?
Medically reviewed by Avi Varma, MD, MPH, AAHIVS, FAAFP
Pain in the left side of your chest may be caused by an underlying heart, digestive, or lung condition, or it could be a symptom of an injury or panic…
READ MORE
What’s Causing Pain in the Right Side of My Chest?
Medically reviewed by Meredith Goodwin, MD, FAAFP
Chest pain on your right side can be caused by muscle strain, heartburn, or another underlying condition.

READ MORE
Why Do I Have Chest Pain When Breathing?
Does it hurt to breathe? Painful respiration is a symptom of an infection or other medical condition. Find out what causes this pain and how to…
READ MORE
What’s Causing My Lung Pain?
Many things can cause lung pain, even conditions in other organs. Learn more about the causes of lung pain and when to seek help here.
READ MORE
Mastitis - ProMedicine Ufa
Mastitis is an inflammatory process in the tissues of the mammary gland. It is manifested by strong arching pains in the chest, swelling, induration, redness of the skin of the gland, a sharp rise in body temperature, chills. Mastitis is diagnosed during a visual examination by a mammologist; additionally, it is possible to conduct an ultrasound of the mammary gland. The disease can lead to the formation of an abscess, phlegmon, necrosis in the mammary gland, the development of sepsis and even death.
The disease can lead to the formation of an abscess, phlegmon, necrosis in the mammary gland, the development of sepsis and even death.
Causes
As the main reason for the development of mastitis, the entry of bacteria directly into the breast tissue is distinguished. This can happen through cracks in the nipples, which in this case act as an open gate for penetration into the specified infection environment, as well as through blood, which occurs in the presence of chronic infectious foci in the body. In the latter case, such foci include pyelonephritis, chronic tonsillitis and other diseases.
It should be noted that in a normal state of health, the entry of a certain amount of bacteria into the mammary gland leads to their corresponding destruction, carried out by the immune system. Meanwhile, the vast majority of cases indicate a weakening of the female body after childbirth, respectively, the immune system ceases to properly fight infections.
As an important point contributing to the development of the disease we are considering, lactostasis should be singled out, in which stagnation occurs in the ducts of the milk glands, which occurs due to insufficient decantation of milk, incomplete decantation, or due to rare feedings. Stagnation of milk in the ducts provides a favorable environment for the process of reproduction of bacteria, because milk as a whole has a mass of nutrients.
Stagnation of milk in the ducts provides a favorable environment for the process of reproduction of bacteria, because milk as a whole has a mass of nutrients.
Symptoms
Usually mastitis is characterized by acute development - this indicates that the symptoms appear quickly (within a few hours - a couple of days)
There are such main signs and symptoms of mastitis: evidence of an inflammatory process in the body. As a result of an increase in temperature, chills, pain in the head, weakness appear;
- persistent pain in the chest of a aching nature, which intensifies during breastfeeding;
- an increase in the volume of the mammary gland, redness of the skin in the area of inflammation, the skin becomes hot.
If mastitis is not treated in the early stages, it progresses to a purulent form.
The main signs and symptoms of purulent mastitis are as follows:
- body temperature rises to 39 degrees or more, sleep disturbance, severe pain in the head, poor appetite,
- severe pain in the mammary gland, pain is felt even from a light touch,
- in the axillary region, there is an increase in lymph nodes, which are presented to the touch as small, dense, painful formations.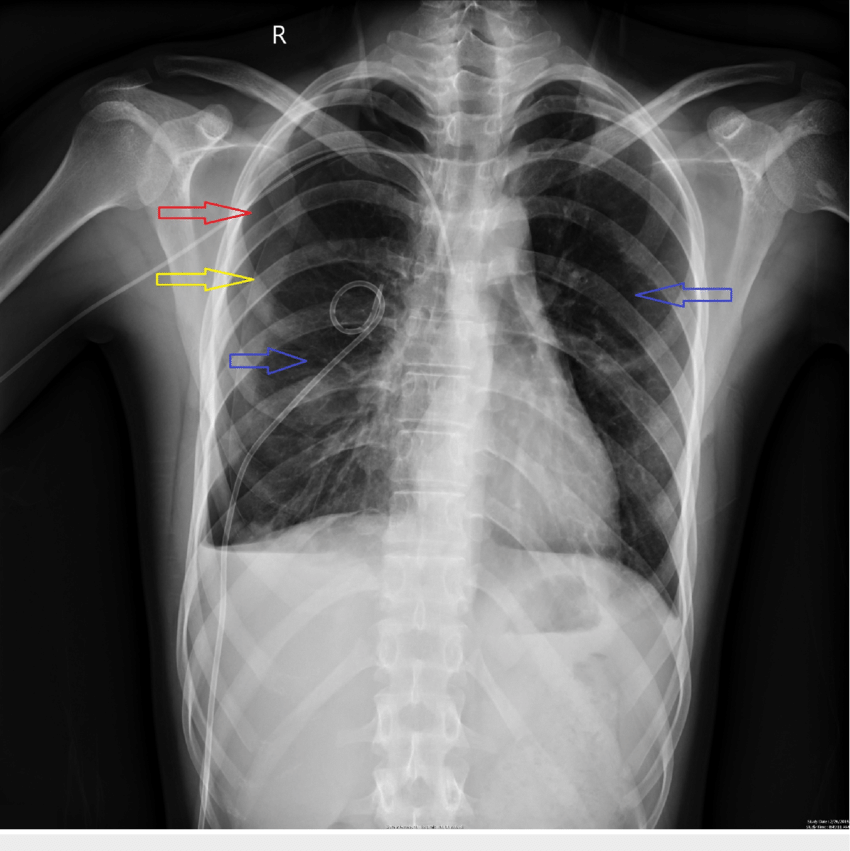
Diagnostics
Diagnostic search for suspected mastitis includes the following tests:
wounds with determination of sensitivity to antibiotics of isolated microorganisms
3) Ultrasound examination of the mammary glands
4) X-ray examination of the mammary glands (mammography), which is especially indicated in case of suspected carcinomatous mastitis (however, the latter can only be excluded after a histological examination)
5) To exclude specific infections, it is necessary to conduct a study for tuberculosis, actinomycosis, etc.
In some cases, it is required to carry out a differential diagnosis of mastitis with other diseases that have similar clinical manifestations.
Treatment
The strategy for treating mastitis depends on the nature, duration of the disease and the volume of the affected area. Infectious forms are treated with targeted antibiotics. In order to achieve the desired result during bakposev, the type of pathogen and its concentration are determined. In the boundary conditions between mastitis and lactostasis, first of all, antiseptics are used and the dynamics are monitored. Only if the situation worsens, they switch to antibiotics.
In the boundary conditions between mastitis and lactostasis, first of all, antiseptics are used and the dynamics are monitored. Only if the situation worsens, they switch to antibiotics.
Need to express milk every 3 hours, but if there is an abscess, the breast should not be touched. If purulent bags have formed, doctors open them surgically or pump out pus through a needle, wash the mammary gland and prescribe antibiotics. In the treatment of mastitis, local use of cold, immunomodulators and physiotherapy are prescribed. Acute non-purulent mastitis is not a hindrance to breastfeeding, but if the milk contains pus, it is forbidden to breastfeed!
Suppurative forms of mastitis usually require surgery. The developed abscess of the mammary gland is an indication for emergency surgical sanitation: opening of mastitis and drainage of the purulent focus.
Progressive mastitis, regardless of its stage, is a contraindication to further feeding (including healthy breasts), since breast milk is usually infected and contains toxic tissue breakdown products. For a child, pathologically altered breast milk can cause the development of dysbacteriosis and disorders of the functional state of the digestive system. Since mastitis therapy includes antibiotics, feeding during this period is also not safe for the baby. Antibiotics can markedly impair the normal development and growth of organs and tissues. During the treatment of mastitis, milk can be expressed, pasteurized, and only then given to the child.
For a child, pathologically altered breast milk can cause the development of dysbacteriosis and disorders of the functional state of the digestive system. Since mastitis therapy includes antibiotics, feeding during this period is also not safe for the baby. Antibiotics can markedly impair the normal development and growth of organs and tissues. During the treatment of mastitis, milk can be expressed, pasteurized, and only then given to the child.
Chest pain - causes, examination and treatment | Symptoms
Myocardial infarction or unstable angina
Signs: Represent an immediate danger to life. Sudden, pressing pain that spreads (radiates) to the jaw or arm, may be constant or transient. Sometimes shortness of breath or nausea. Pain that comes on with exertion and goes away with rest (angina pectoris). Abnormal heart sounds heard through a stethoscope. Frequent warning signs.
Thoracic aortic dissection (tear in the wall of the thoracic aorta)
Signs: Represent an immediate danger to life. Sudden, tearing pain that extends into or begins in the middle of the back. Sometimes dizziness, stroke, and pain, coldness, or numbness in the leg. Sometimes different pulse or blood pressure in the limbs. Usually in people over 55 with a history of high blood pressure. Warning signs.
Sudden, tearing pain that extends into or begins in the middle of the back. Sometimes dizziness, stroke, and pain, coldness, or numbness in the leg. Sometimes different pulse or blood pressure in the limbs. Usually in people over 55 with a history of high blood pressure. Warning signs.
Pericarditis (inflammation of the lining around the heart)
Signs: Potentially life-threatening. Acute pain, constant or transient, aggravated by breathing, swallowing food, or lying on the back. Relaxes when leaning forward. Abnormal heart sounds heard through a stethoscope.
Spontaneous rupture of the esophagus
Signs: Represent an immediate danger to life. Sudden, sharp pain immediately after vomiting or after a medical procedure involving the esophagus (esophageal and gastric endoscopy or transesophageal echocardiography). Some warning signs.
Pancreatitis (inflammation of the pancreas)
Signs: Potentially life-threatening. Severe, persistent pain that: appears in the upper middle abdomen or lower chest. Often aggravated in the supine position, weakened by bending forward. Vomiting and soreness in the upper abdomen, sometimes shock. Often in people who abuse alcohol or have gallstones.
Often aggravated in the supine position, weakened by bending forward. Vomiting and soreness in the upper abdomen, sometimes shock. Often in people who abuse alcohol or have gallstones.
Peptic ulcers
Signs: Periodic vague discomfort that is felt in the upper middle of the abdomen or in the lower chest. Relief with antacids and sometimes after meals. Common in smokers and drinkers, or both. There are no warning signs.
Gastroesophageal reflux (GERD)
Signs: Periodic burning pain that spreads from the upper middle abdomen to the throat, worse when bending over or lying down. Relieves with antacids.
Diseases of the gallbladder and bile ducts (diseases of the biliary tract)
Signs: Intermittent discomfort, which is felt in the upper right side of the abdomen or in the lower middle of the chest, is observed after eating (but not after exercise).
Swallowing disorders (in which the peristalsis of food through the esophagus is impaired)
Signs: Pain that develops gradually over a long period of time may or may not appear during swallowing. Usually difficulty swallowing.
Usually difficulty swallowing.
Pulmonary embolism (blockage of the pulmonary artery by a blood clot)
Signs: Represent an immediate danger to life. Often severe pain when breathing, shortness of breath, rapid breathing and rapid heartbeat. Sometimes a slight fever, coughing up blood, or shock. More likely in patients with risk factors for pulmonary embolism (history of blood clots, recent surgery, especially leg surgery, prolonged bed rest, leg cast or splint, older age, smoking, or cancer).
Tension pneumothorax (collapse of the lung with increased air pressure in the chest)
Signs: Represent an immediate danger to life. Significant shortness of breath. Low blood pressure, swollen neck veins, and decreased breath sounds heard through a stethoscope on one side. It usually occurs only after a severe chest injury.
Pneumonia
Signs: Potentially life-threatening. Fever, chills, cough, and usually yellow or green sputum. Often shortness of breath. Sometimes pain when breathing. Palpitations and congestion in the lungs revealed during the examination.
Often shortness of breath. Sometimes pain when breathing. Palpitations and congestion in the lungs revealed during the examination.
Pneumothorax (collapse of the lung)
Signs: Potentially life-threatening. Sudden sharp pain, usually in one side of the chest. Sometimes shortness of breath, weakening of breath sounds heard through a stethoscope on one side.
Pleurisy (inflammation of the lining around the lung)
Signs: Sharp pain when breathing. Usually in patients who have recently had pneumonia or a viral respiratory infection. Sometimes cough. There are no warning signs.
Musculoskeletal chest wall pain
Signs: Pain that is usually persistent (lasting a few days or more). Increases with movement and/or breathing. May have no apparent cause or result from coughing or physical exertion. Soreness at one point on the chest. There are no warning signs.
Fibromyalgia
Signs: Pain that is almost constant, spreads to large areas of the body, is usually accompanied by fatigue and impaired sleep quality.